Abstract
While Crimean-Congo hemorrhagic fever (CCHF) has a high mortality rate in humans, the associated virus (CCHFV) does not induce clinical symptoms in animals, but animals play an important role in disease transmission to humans. Our aim in this study was to examine the immunogenicity of the CCHFV glycoprotein when expressed in the root and leaf of transgenic plants via hairy roots and stable transformation of tobacco plants, respectively. After confirmatory analyses of transgenic plant lines and quantification of the expressed glycoprotein, mice were either fed with the transgenic leaves or roots, fed the transgenic plant material and injected subcutaneously with the plant-made CCHFV glycoprotein (fed/boosted), vaccinated with an attenuated CCHF vaccine (positive control), or received no treatment (negative control). All immunized groups had a consistent rise in anti-glycoprotein IgG and IgA antibodies in their serum and feces, respectively. The mice in the fed/boosted group showed a significant rise in specific IgG antibodies after a single boost. Our results imply that oral immunization of animals with edible materials from transgenic plants is feasible, and further assessments are under way. In addition, while the study of CCHF is challenging, our protocol should be further used to study CCHFV infection in the knockout mouse model and virus neutralization assays in biosafety level 4 laboratories.
INTRODUCTION
Crimean-Congo hemorrhagic fever (CCHF) is a frequently fatal disease in humans. The CCHF virus (CCHFV) belongs to the family Bunyaviridae and the genus Nairovirus and contains a three-segment RNA genome, including S (small), M (medium), and L (large) segments which encode a viral nucleoprotein, a precursor glycoprotein, and an RNA-dependent RNA polymerase, respectively (18, 23). Subsequently, the precursor is matured to GN and GC glycoproteins by proteolytic cleavages (1, 41). In addition to transmission via tick bite and nosocomial infections, humans are mainly infected by exposure to the tissue and blood of infected livestock, which are asymptomatic. The virus is widely distributed, with outbreaks and epidemics occurring throughout much of Asia, extending from China to the Middle East and southern Russia, and in focal areas of endemicity over much of Africa and parts of southeastern Europe (11, 14, 25, 31).
The average case fatality rate ranges from 30 to 50%, but mortality rates from 10% to 80% have been reported during various outbreaks (42, 50, 52). The current approach to the treatment of CCHF is based on general supportive measures, including monitoring the patient's hematologic and coagulation status, replacing cells and factors as needed, and administering ribavirin (22, 47). Therefore, immunization is considered to be essential in mitigating the high rate of mortality from viral hemorrhagic fevers. It was recently shown that Ebola virus glycoprotein can confer protection in vaccinated mice (26). Similarly, specific antibodies against CCHFV are protective in a suckling mouse animal model (6). A CCHFV DNA vaccine expressing the viral glycoprotein elicits in some vaccinated mice neutralizing antibodies that can be precipitated with radiolabeled viruses (43). Although an inactivated CCHFV vaccine could reduce CCHF outbreaks (36), there is a stigma attached to using attenuated vaccines due to a fear of reversion of virulence or possible reversion to wild-type virus (38). Hence, the use of recombinant subunit vaccines renders a remarkable benefit to immunization programs.
Transgenic plants have been used for the production of edible vaccines and as delivery vehicles of immunogenic subunits (32). Plant-based vaccines have several advantages: they are easily scaled up, the recombinant protein can be transported and stored without the need for a cold chain, processing is simple, and there is no risk of contamination with human pathogens (15, 32, 33, 44). Thus far, studies have shown the efficacy of plant-derived antigens in preventing the onset of disease in animals under experimental conditions and their safety and efficacy in human clinical trials (4, 34, 46, 48). We postulated that the distribution rate of the CCHFV can be decreased using an effective and edible vaccine for animals, preventing both virus reproduction in the animal and subsequent transmission to humans since domestic animals play a critical role in the transmission cycle of the virus (21, 50).
In this study we utilize both transgenic tobacco leaves and hairy roots (HRs). We evaluate the oral immunogenicity of the CCHFV glycoproteins (GC and GN; here, named G1 and G2) produced by transgenic plants when they are delivered as food to mice. We compared the two different strategies of antigen production with the CCHF vaccine that is presently used for human vaccination in Eastern Europe. We found that oral immunization with transgenic plants producing the G1/G2 glycoprotein from CCHFV elicits a humoral immune system response against the G1/G2 glycoprotein.
MATERIALS AND METHODS
The G1/G2 glycoprotein used both as the antigen in the final immunization boost of the mice and as the solid-phase coating antigen was purified from agro-infiltrated tobacco leaves through affinity chromatography, and its purity was monitored by SDS-PAGE and immunoblotting. Also, the anti-G1/G2 serum taken from the immunized mice by this plant-purified G1/G2 glycoprotein was used as the antibody (polyclonal) in both enzyme-linked immunosorbent assays (ELISAs) and Western blotting (data not shown).
Stable plant transformation.
The entire G1 (GC) and G2 (GN) portions of the CCHFV glycoprotein gene were derived from the M segment of the Iranian strain (GenBank accession number DQ446215) on the basis of previously published reports (1, 41). A plant-optimized G1/G2 (GC/GN) glycoprotein gene (HM537014) was genetically engineered into one reading frame, chemically synthesized, cloned into pBI121 (Novagen) at the Cfr9I and SacI restriction enzyme sites, and introduced into Agrobacterium tumefaciens strain LBA4404 and Agrobacterium rhizogenes (ATCC 15834) by a standard freeze-thaw method (40). In order to obtain stable transgenic tobacco leaves and tobacco hairy roots, 4- to 6-week-old tobacco leaves were transformed, regenerated, and screened as previously described (7, 49).
Nucleic acid analyses of the G1/G2 gene.
Genomic DNA was extracted from the leaves of transgenic lines as previously described (17). The genomic DNA from each regenerated line was screened by PCR using the following primers, which amplified the junction of the G1/G2 gene: JG2G1F, (5′-GGCATTCCTCTTTTGGTTCAGTTTC-3′) and JG2G1R (5′-TTGATTCAGACCTTCCAGACACGA-3′). To determine the gene copy number, Southern blotting was carried out on 50 μg of genomic DNA from wild-type and transgenic lines that had been digested with the BglII restriction endonuclease. Digested DNA was electrophoresed in a 0.8% agarose gel and blotted on Hybond N membrane (Roche, Germany) following a standard procedure (40). A digoxigenin (DIG)-labeled probe (602 bp) was generated with PCR DIG Labeling Mix (Roche, Germany) using the G1/G2 gene as a template and the previously mentioned specific primers. Hybridization was performed using a PCR DIG DNA Labeling and Detection kit following the supplier's instructions (Roche, Germany).
Expression analyses of transgenic plants.
For Western blot analysis, 100 μl of total soluble protein (TSP) was boiled in loading buffer (300 mM Tris-HCl, pH 6.8, 600 mM dithiothreitol, 12% SDS, 0.6% bromophenol blue, 60% glycerol) and run on a 12% SDS-PAGE gel. The separated proteins were transferred from the gel to a polyvinylidene difluoride (PVDF) membrane (Roche, Germany) using a Mini-Trans-Blot electrophoretic transfer cell (Bio-Rad) in transfer buffer (50 mM Tris, 40 mM glycine, 0.04% SDS, 20% methanol, pH 8.3) according to a standard protocol (40). The membrane was then blocked with 4% skim milk in phosphate-buffered saline (PBS) with 0.05% Tween 20 (PBST) for 2 h at room temperature. After a brief wash in PBST, the membrane was incubated with anti-G1/G2 murine serum at a dilution of 1:250 in 1% in PBST for 1 h at 37°C. After a washing step, the membrane was incubated with horseradish peroxidase (HRP) conjugated to goat polyclonal IgG antibody against mouse (Sigma) at a dilution of 1:4,000 in PBST. Finally, the color on the membrane was developed using HRP staining solution (Sigma) and then stopped by rinsing the membrane in distilled water.
For ELISAs, 10 μg of TSP from each sample was coated onto an ELISA plate (Nunc, Denmark) using 100 μl of coating buffer (64 mM Na2CO3, 136 mM NaHCO3, pH 9.8) and incubated for 2 h at 37°C. Each subsequent step was followed by three washes with PBST. Plate wells were blocked with 3% (wt/vol) skim milk in PBST for 1 h at 37°C. Then, 100 μl of the previously mentioned antiserum (1:500 dilution) was added and incubated for 2 h at 37°C. The wells were then treated with a 1:4,000 dilution of goat anti-murine IgG conjugated to peroxidase (Sigma) and incubated for 1 h at 37°C. Colorimetric detection was performed using the peroxidase substrate o-phenylenediamine dihydrochloride (OPD; Sigma). The reaction was stopped after 5 min with 1N H2SO4, and the optical density was read at 492 nm (OD492) (3, 12). To calculate the relative amount of G1/G2 glycoprotein in the plant material, the OD of the wild-type plant sample was deducted from the OD of the transgenic plant. The resulting OD was then converted to the amount of glycoprotein based on a standard curve based on ELISAs using 0.2 to 1.9 μg of the purified G1/G2 glycoprotein.
For more confirmations, both ELISAs and Western blotting were also performed with human antiserum taken from a recovered CCHF patient (provided by National Reference Laboratory of Arboviruses and Viral Hemorrhagic Fevers, Pasteur Institute of Iran).
Mouse immunization.
Female BALB/c mice, 6 to 8 weeks old and grown under pathogen-free conditions (purchased from Pasteur Institute of Iran), were used in this study. The mice were divided into six groups for immunization through feeding, injection, or a feed/boost strategy. The two feeding groups were separately immunized five times with 10 μg of the G1/G2 glycoprotein expressed in a pellet of the transgenic tobacco leaves (leaf group) and tobacco hairy roots (root group) at 1-week intervals. The leaf-fed/boosted and root-fed/boosted groups were fed four times at 1-week intervals with 10 μg of the G1/G2 glycoprotein expressed in a pellet of the transgenic tobacco leaves and tobacco hairy roots, respectively, and received a boost of 5 μg of the plant-purified G1/G2 glycoprotein. The fifth group (vaccinated group) was subcutaneously injected with four doses of the CCHF vaccine, an inactivated form of the CCHF virus approved for human vaccination (BulBio Company, Bulgaria), at 2-week intervals. The negative-control (nonimmunized) group received a mixed pellet of wild-type leaves and roots.
Measuring antibody responses in the animal model serum and feces.
Blood samples were taken from mice before immunization as controls, after the third dose, and 1 week after the final immunization (i.e., 6 to 8 weeks after the first dose) for analysis of systemic anti-G1/G2 IgG and IgA antibodies. Fecal pellets, collected from mice weekly, were lyophilized. PBS containing 0.2 mg/ml trypsin inhibitor, 0.05% sodium azide (wt/vol), and a cocktail of protease inhibitors (Roche, Germany) was added at 10 μl/mg of dry fecal material. The homogenates were centrifuged at 20,000 × g for 10 min at 4°C, and the supernatants were analyzed for IgA. The ELISA was performed by coating 3 μg of the plant-purified G1/G2 glycoprotein according to the protocol described above. A 1:1,000 dilution of anti-mouse IgA (Sigma) and a 1:2,500 dilution of anti-mouse IgG, both conjugated to horseradish peroxidase (Sigma), were used for IgA and IgG measurements, respectively. Sera from negative-control mice were serially diluted and used in the ELISA to subtract the OD from samples, as previously described. Furthermore, any cross-reaction between the immunized sera (i.e., sera of the fed, fed/boosted, and vaccinated groups) and variant antigens (i.e., plant-made G1/G2 glycoprotein and the attenuated CCHF virus in the vaccine) was examined with the same ELISA (12).
Data analysis.
All data were processed and analyzed by SPSS, version 13.0, Data Editor (SPSS Inc., Chicago, IL). Groups were considered to be different at a P value of <0.05 and significantly different at a P value of ≤0.01.
RESULTS
Transgenic plants contain the G1/G2 glycoprotein gene.
A synthetic G1/G2 glycoprotein gene 2,661 bp in length, which encodes the G1 (GC) and G2 (GN) portions of the CCHFV glycoprotein, was subcloned into the pBI121 binary vector (designated pBIg1/g2) for expression in plant cells under the control of the cauliflower mosaic virus 35S promoter (CaMV 35S), which provides strong and constitutive transgene expression in tobacco (Fig. 1). The pBIg1/g2 vector was used for stable nuclear transformation of tobacco plants by A. tumefaciens and A. rhizogenes, the latter of which was for tobacco hairy root production. The plantlets were regenerated in the presence of the antibiotic kanamycin, and the putative transformants were screened by PCR (Fig. 2a). Results are shown in Table 1.
Fig. 1.
Schematic of the T-DNA region of binary vectors used for the expression of the G1/G2 glycoprotein gene. The synthetic G1/G2 glycoprotein gene consisting of the coding sequences for the G1 and G2 portions of the CCHFV glycoprotein was expressed under the control of the CaMV 35S promoter. RB, right border; LB, left border.
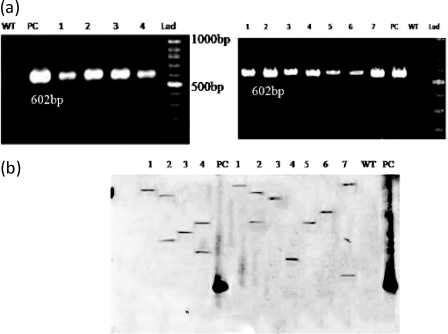
Fig. 2.
PCR and Southern blot analyses of genomic DNA extracts from transgenic plants. (a) Gene-specific primers were used to amplify a 602-bp fragment. The G1/G2 gene was present in seven lines of tobacco plants (lanes 1 to 7, right) and four lines of hairy root (lanes 1 to 4, left). (b) The corresponding genomic DNA was examined by Southern blotting using a 602-bp gene-specific probe on tobacco plant lines (lanes 1 to 7, right) and hairy root lines (lanes 1 to 4, left). PC, positive control; WT, wild-type genome as a negative control; Lad, 100-bp DNA ladder.
Table 1.
Transgenic plants transformed by pBIg1/g2
| Transgenic plant type | No. of regenerated lines | No. of PCR-positive lines | Transformation efficiency (%) | No. of lines positive by RT-PCR | No. of lines positive for the G1/G2 protein |
|---|---|---|---|---|---|
| Tobacco leaves | 9 | 7 | 78 | 7 | 3 |
| Tobacco hairy root | 6 | 4 | 67 | 4 | 1 |
Transgene copy number can affect the level and stability of transgene expression, determining the susceptibility of the gene to silencing in most cases (2). Hence, the G1/G2 transgene copy number in the transgenic plants was assayed by Southern blotting. The expected band of approximately 3 kb was present with one to three copies in the transgenic lines except in wild-type and nontransformed plants (Fig. 2b). For analysis of G1/G2 gene expression, reverse transcription-PCR (RT-PCR) was performed on total RNA extracted from transgenic plants, revealing that 34% and 17% of regenerated transgenic leaves and hairy roots expressed G1/G2 mRNA, respectively (data not shown).
Transgenic plants express the G1/G2 glycoprotein.
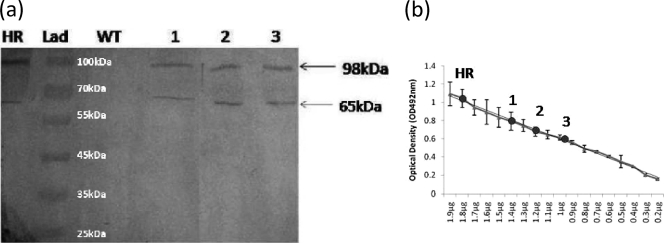
TSP was extracted from all regenerated tobacco leaves and hairy roots and then analyzed by Western blotting and specific ELISA. A specific band of approximately 98 kDa corresponding to the G1/G2 glycoprotein was detected in three transgenic tobacco leaf lines and one hairy root line (Fig. 3a). An extra band was also observed at a lower molecular mass (∼65 kDa) and may be related to the degradation of the intact protein during purification or processing in the endoplasmic reticulum (ER).
Fig. 3.
Analysis of expression of the G1/G2 glycoprotein in transgenic plants by Western blotting and ELISA using anti-G1/G2 mouse serum. (a) Western blot of three transgenic tobacco lines (lanes 1 to 3) and one transgenic tobacco hairy root (HR) line. All samples were standardized to contain 40 μg of TSP. (b) Quantification of the G1/G2 glycoprotein in 1 g (fresh weight) of the transgenic lines using a standard curve of the purified G1/G2 glycoprotein. WT, wild-type plant; Lad, protein molecular mass marker.
To quantify the expression of the G1/G2 protein in the transgenic plants, a standard curve for the G1/G2 glycoprotein was calculated by specific ELISA using the linear range of 0.2 to 1.9 μg at 0.1-μg increments. The amount of the G1/G2 glycoprotein in the transgenic lines was 1.8 μg (0.45% of TSP) per 1 g (fresh weight) of the transgenic hairy root (HR) and 1.4 μg (0.34% of TSP), 1.2 μg (0.32% of TSP), and 0.96 μg (0.29% of TSP) per 1 g (fresh weight) of the transgenic leaves (Fig. 3b).
Plant-derived CCHFV glycoprotein is orally immunogenic in mice.
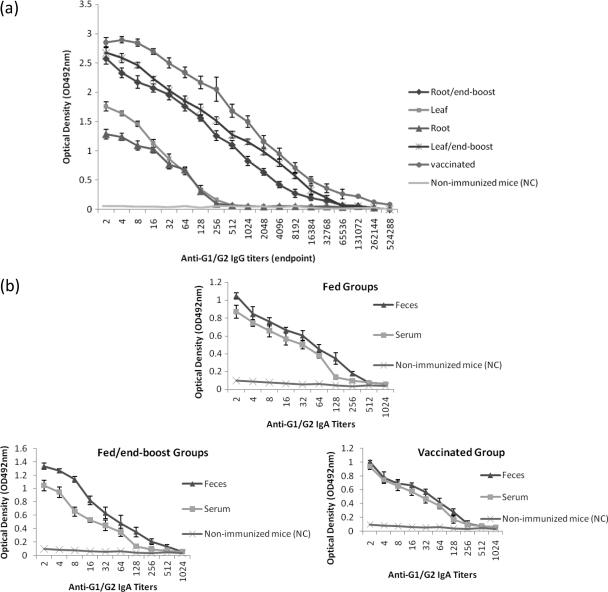
To determine whether G1/G2 glycoprotein from transgenic plants is able to induce serum and mucosal antibodies, we employed two different strategies. Two groups of mice (leaf and root groups) were fed transgenic plants while two other groups were fed the transgenic plants and were injected with the purified G1/G2 as a final boost. The positive-control group was immunized with the CCHF vaccine. Anti-G1/G2 IgG antibodies were detected in 100% of the mice that were immunized with transgenic plants and the vaccine. The average serum IgG in the leaf group was higher than in the root group (P < 0.05) although the levels in both groups gradually declined and the titers were not detected after 1:256 (Fig. 4a). Similarly, the level of the G1/G2-specific IgG in the serum of the leaf-fed/boosted group remained slightly higher than that of the root-fed/boosted group (P < 0.05), but both boosted groups had significantly higher levels of serum IgG antibodies than the fed mice (P ≤ 0.01) even though the level dropped and the titers were not detected after 1:65,536. The concentration of the G1/G2-specific IgG antibodies in the boosted groups was remarkably high at an OD above 2 at the lower dilutions. As expected, the vaccinated group had the highest level of serum anti-CCHFV antibodies that were detected up to a dilution of 1:524,288. Moreover, all immune sera showed high cross-reactivity to the antigens (i.e., the plant-made G1/G2 and the inactivated CCHFV particle in the vaccine). Interestingly, anti-G1/G2 IgA antibodies were detected in the fecal pellets (up to a dilution of 1:512) and serum (up to a dilution of 1:256) from all immunized groups (Fig. 4b). However, not only was the amount of IgA detected in fecal pellets clearly higher than in the serum, but also the level of G1/G2 IgA detected in feces and serum of fed/ boosted groups was remarkably higher than that of the other two groups (P ≤ 0.01). The nonimmunized group had no significant increase in IgG or IgA antibodies in serum or feces.
Fig. 4.
Anti-G1/G2 antibody quantification by ELISA in serum and fecal samples from mice immunized with transgenic plant material. The curves show anti-G1/G2 IgG antibodies in serum (a) and anti-G1/G2 IgA antibodies in serum and feces (b). The six groups of mice included those fed leaf or root, those fed leaf or root and given a booster injection of the purified G1/G2, those subcutaneously vaccinated by the CCHF vaccine, and a nonimmunized group (as a negative control [NC]). In the IgA assay, the same groups were pooled as fed, fed/boosted, and vaccinated group.
DISCUSSION
The oral delivery of antigens is capable of inducing immune responses in the mucosa of the gastrointestinal tract, in serum, and at secondary mucosal surfaces (44). Parenterally administered antigens typically stimulate systemic responses, while mucosal delivery is capable of inducing both systemic and mucosal immune responses (8, 9, 28). To date, mucosal immunization has been commonly and successfully used as an alternative to injection in vaccination programs (10, 29, 35).
Here, we examined the oral immunogenicity of a plant-derived G1/G2 glycoprotein of the CCHF virus in mice. The optimized G1/G2 gene was successfully expressed, and Western blot analysis confirmed the intact G1/G2 glycoprotein with a mass of about 98 kDa. In spite of the absence of proteolytic sites in this peptide sequence, a band of almost 65 kDa was detected in Western blotting for the TSP from transgenic lines, which is consistent with the size of the G1 portion of the glycoprotein. The latter band might be the result of protein degradation during protein purification or indicate the presence of a new proteolytic site in the optimized sequence of the G1/G2 glycoprotein.
The G1/G2 protein was accumulated in the fresh weight of transgenic plants up to approximately 0.45% of TSP in hairy roots and 0.34% in tobacco leaves. Previous reports have yielded other recombinant proteins in stable transgenic tobacco plants at different amounts, including a viral chitinase at 0.2% of TSP (19), glycoprotein 5 of porcine reproductive and respiratory syndrome virus at 0.01% (13), a recombinant antibody specific to microcystin-LR at 0.6% (20), and rabies surface glycoprotein at 0.4% (39). Our yield of the G1/G2 glycoprotein reached as high as 0.45% of TSP, which is comparably higher than the previous yields of mouse interleukin-12 production and human acetyl-cholinesterase by hairy roots (37, 51).
While questions remain about the characteristics of such a response that will provide protection, there is general agreement that a protective vaccine will require the induction of neutralizing antibodies. Since neutralizing antibodies play a pivotal role in protection against CCHF virus, some evidence demonstrated immunogenic epitopes within GN (G2) and GC (G1) parts of the viral glycoprotein. Systemic IgG has previously been found to increase in mice immunized by the DNA vaccine of the CCHFV glycoprotein (43), and some neutralizing epitopes on this protein have been identified by monoclonal antibodies (1). When the viral glycoprotein of the Ebola virus, a very lethal hemorrhagic fever virus, was expressed in mammalian cells, it was able to elicit an efficient immune response (24, 45). Moreover, immunization of mice with purified influenza H5 virus-like particles (VLPs) triggered a strong immune response against the homologous virus (16). We found that a humoral immune response was elicited in mice fed with transgenic plant materials, with serum anti-G1/G2 IgG antibodies rising to a titer of 1:256 in both root and leaf groups. Our results on the oral immunogenicity of the CCHFV glycoprotein are comparable with other findings for the intimin, Tir, and EspA proteins of Escherichia coli O157:H7 (3), the VP7 antigen of rotavirus (30), the hepatitis B surface antigen (48), and the E. coli heat-labile enterotoxin (33).
The plant-derived G1/G2 glycoprotein was recognized by gut-associated lymphoid tissue (GALT), which was demonstrated by measuring anti-G1/G2 IgA antibodies in the feces. We measured the level of G1/G2-specific IgA in the feces and serum of each group in order to detect the mucosal stimulation of antibodies. The amount of the IgA in feces was greater than in the serum of the immunized mice (Fig. 4b). It is worth mentioning that the amount and level of IgA in the fed/boosted groups were significantly higher than those in the fed and injection groups (P ≤ 0.01). Considering both the increase of anti-G1/G2 IgG in the serum and the measurable amount of specific IgA in the feces, it is likely that a proper immune response against the CCHFV glycoprotein was primed in the mice by feeding them transgenic plants. Our data on immunological evaluation suggest that transgenic plants can be used to develop an efficient vaccine against the CCHFV, but a virus neutralization assay and infection simulation in the STAT1 knockout mouse (5) in biosafety level 4 laboratories should first be performed.
We compared the oral immunization of mice with plant-made G1/G2 to oral immunization supplemented with a boost in order to determine the most efficient approach for an edible vaccine against the CCHF virus for animals. We found that the fed/boosted groups showed a remarkable increase in anti-G1/G2 IgG antibodies after a single final boost of the G1/G2 antigen, with the IgG concentration jumping to almost 1:32,000 compared with 1:256 in the fed groups. Similar results from primary boosting have been found previously (2, 3, 27). While mice vaccinated with the CCHF virus had a significantly larger increase in anti-G1/G2 IgG than mice from the fed/boosted groups and fed groups (P ≤ 0.01), both other approaches elicited immune responses (P < 0.05). Massive vaccination by an injectable vaccine is time-consuming and costly. In contrast, an edible vaccine against CCHF would be cost-effective and could be used to vaccinate animals, which are much easier to vaccinate than humans.
In addition to transgenic tobacco leaves, tobacco hairy roots were used for production of the G1/G2 glycoprotein. The hairy root system has some advantages over the tobacco leaf system, including simple and massive cultivation in medium, faster growth, a relatively greater content of the protein, and lower turnover of cellular proteins. However, since there was no significant difference in the immunogenicity of the G1/G2 glycoproteins between the mice fed leaves and the mice fed roots, both approaches can be used to encapsulate the G1/G2 glycoprotein for delivery.
The murine model provides a meaningful indication of the efficacy of immunization. The CCHF virus has no animal model with which to observe the disease challenge in an immunized animal, except for the STAT1 knockout mouse, which was recently studied for CCHF pathogenesis a in biosafety level 4 laboratory (5). However, in the absence of a mouse model and/or level 4 containment, the disease challenge can be simulated by a feed/boost strategy in which the injection of the G1/G2 antigen mimics the CCHF virus, leading to a rapid rise of anti-G1/G2 antibodies in the fed/ boosted groups.
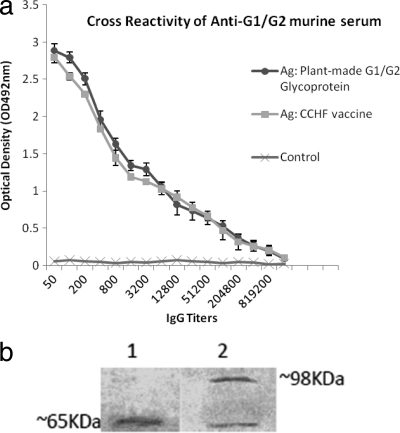
The question was then to know the specificity of anti-G1/G2 murine IgG antibodies as well as their cross-reactivity with the CCHF vaccine. As shown in Fig. 5, the tests of cross-reactivity and specificity were done by ELISAs and immunoblot analyses. The results implied that the sera of the fed and fed/boosted groups recognized the glycoprotein epitopes of the viral particles in the vaccine and the plant-made G1/G2 (Fig. 5). The anti-G1/G2 antibodies detected the virus particle at slightly above 65 kDa, whereas the same size in plant-made G1/G2, indicating a variant strain of glycoprotein in the vaccine strain even though presence of similar epitopes in its glycoprotein. Both are proposed to be G1 (GC). Since the strain in the vaccine was isolated from Eastern Europe, it is quite different from the G1/G2 glycoprotein in the Iranian CCHFV strain. Our data suggest the existence of common epitopes in the optimized G1/G2 glycoprotein expressed in the transgenic plants. Nonetheless, the plant-purified G1/G2 reacted to human antiserum taken from a recovered CCHF patient (provided by the National Reference Laboratory of Arboviruses and Viral Hemorrhagic Fevers, Pasteur Institute of Iran) at a dilution of 1:500 (data not shown), but using monoclonal antibodies could more precisely confirm the GC and GN epitopes of the CCHF virus glycoprotein.
Fig. 5.
Specificity and cross-reactivity of anti-G1/G2 murine serum with both plant-made G1/G2 glycoprotein and CCHF vaccine containing inactivated CCHF virus as antigen determined by ELISA and Western blotting. (a) The ELISA shows that anti-G1/G2 IgG antibodies in serum reacted with both antigens. (b) Illustration of cross-reaction of the antiserum with both antigens by Western blot analysis. Lane 1, CCHF vaccine containing inactivated CCHF virus; lane 2, plant-made G1/G2 glycoprotein. Ag, antigen.
Using transgenic plants to produce an oral vaccine against CCHFV without the need for protein purification and with minimal processing may provide a cost-effective alternative to current vaccine production strategies. Here, we show that the glycoprotein of the CCHFV can be orally immunogenic when produced in and delivered by plant tissues although some confirmatory analyses, such as mass spectrometry of the plant-made G1/G2 glycoprotein for glycan identifications and the efficacy determination of the immune sera with a virus neutralization test in level 4 containments, remain for further study. Plant-expressed G1/G2 has the potential to be useful as a booster vaccine against CCHF since it is able to elicit specific mucosal IgA and serum IgG responses. Also, the ability to prime immune responses against CCHFV by distributing transgenic plants in areas of endemicity and of high risk could prevent future outbreaks.
ACKNOWLEDGMENTS
We thank J. Amani, J. Salimian, and the staff of the plant biotechnology department of the National Institute of Genetic Engineering and Biotechnology (NIGEB) for their technical assistance and the Arboviruses and Viral Hemorrhagic Fevers Laboratory (National Reference Laboratory) for providing antiserum.
This investigation was funded by project numbers 368 and 394 of the NIGEB.
We have no conflicts of interest to declare.
Footnotes
Published ahead of print on 19 October 2011.
REFERENCES
- 1. Ahmed A. A., et al. 2005. Presence of broadly reactive and group-specific neutralizing epitopes on newly described isolates of Crimean-Congo hemorrhagic fever virus. J. Gen. Virol. 86:3327–3336 [DOI] [PubMed] [Google Scholar]
- 2. Alvarez M. L., et al. 2006. Plant-made subunit vaccine against pneumonic and bubonic plague is orally immunogenic in mice. Vaccine 24:2477–2490 [DOI] [PubMed] [Google Scholar]
- 3. Amani J., Mousavi S. L., Rafati S., Salmanian A. H. 2011. Immunogenicity of a plant-derived edible chimeric EspA, intimin and Tir of Escherichia coli O157:H7 in mice. Plant Sci. 180:620–627 [DOI] [PubMed] [Google Scholar]
- 4. Arlen P. A., et al. 2008. Effective plague vaccination via oral delivery of plant cells expressing F1-V antigens in chloroplasts. Infect. Immun. 76:3640–3650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bente D. A., et al. 2010. Pathogenesis and immune response of Crimean-Congo hemorrhagic fever virus in a STAT-1 knockout mouse model. J. Virol. 84:11089–11100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bertolotti-Ciarlet A., et al. 2005. Cellular localization and antigenic characterization of Crimean-Congo hemorrhagic fever virus glycoproteins. J. Virol. 79:6152–6161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Borisjuk N. V., et al. 1999. Production of recombinant proteins in plant root exudates. Nat. Biotechnol. 17:466–469 [DOI] [PubMed] [Google Scholar]
- 8. Boyaka P. N., et al. 2003. Therapeutic manipulation of the immune system: enhancement of innate and adaptive mucosal immunity. Curr. Pharm. Des. 9:1965–1972 [DOI] [PubMed] [Google Scholar]
- 9. Boyaka P. N., et al. 2003. Effective mucosal immunity to anthrax: neutralizing antibodies and Th cell responses following nasal immunization with protective antigen. J. Immunol. 170:5636–5643 [DOI] [PubMed] [Google Scholar]
- 10. Bramwell V. W., Perrie Y. 2005. The rational design of vaccines. Drug Discov. Today 10:1527–1534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Burt F. J., Swanepoel R. 2005. Molecular epidemiology of African and Asian Crimean-Congo haemorrhagic fever isolates. Epidemiol. Infect. 133:659–666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Burt F. J., Swanepoel R., Braack L. E. 1993. Enzyme-linked immunosorbent assays for the detection of antibody to Crimean-Congo haemorrhagic fever virus in the sera of livestock and wild vertebrates. Epidemiol. Infect. 111:547–557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chia M. Y., et al. 2010. Immunogenicity of recombinant GP5 protein of porcine reproductive and respiratory syndrome virus expressed in tobacco plant. Vet. Immunol. Immunopathol. 135:234–242 [DOI] [PubMed] [Google Scholar]
- 14. Chinikar S., Ghiasi S. M., Hewson R., Moradi M., Haeri A. 2010. Crimean-Congo hemorrhagic fever in Iran and neighboring countries. J. Clin. Virol. 47:110–114 [DOI] [PubMed] [Google Scholar]
- 15. Daniell H., Singh N. D., Mason H., Streatfield S. J. 2009. Plant-made vaccine antigens and biopharmaceuticals. Trends Plant Sci. 14:669–679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. D'Aoust M. A., et al. 2008. Influenza virus-like particles produced by transient expression in Nicotiana benthamiana induce a protective immune response against a lethal viral challenge in mice. Plant Biotechnol. J. 6:930–940 [DOI] [PubMed] [Google Scholar]
- 17. Dellaporta S. L., Wood J., Hicks J. B. 1983. A plant DNA minipreparation: version II. Plant Mol. Biol. Rep. 1:19–21 [Google Scholar]
- 18. Deyde V. M., Khristova M. L., Rollin P. E., Ksiazek T. G., Nichol S. T. 2006. Crimean-Congo hemorrhagic fever virus genomics and global diversity. J. Virol. 80:8834–8842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Di Maro A., et al. 2010. Purification and characterization of a viral chitinase active against plant pathogens and herbivores from transgenic tobacco. J. Biotechnol. 147:1–6 [DOI] [PubMed] [Google Scholar]
- 20. Drake P. M., et al. 2010. Generation of transgenic plants expressing antibodies to the environmental pollutant microcystin-LR. FASEB J. 24:882–890 [DOI] [PubMed] [Google Scholar]
- 21. Ergonul O. 2006. Crimean-Congo haemorrhagic fever. Lancet Infect. Dis. 6:203–214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ergonul O. 2008. Treatment of Crimean-Congo hemorrhagic fever. Antiviral Res. 78:125–131 [DOI] [PubMed] [Google Scholar]
- 23. Flick R., Whitehouse C. A. 2005. Crimean-Congo hemorrhagic fever virus. Curr. Mol. Med. 5:753–760 [DOI] [PubMed] [Google Scholar]
- 24. Geisbert T. W., Bausch D. G., Feldmann H. 2010. Prospects for immunisation against Marburg and Ebola viruses. Rev. Med. Virol. 20:344–357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hoogstraal H. 1979. The epidemiology of tick-borne Crimean-Congo hemorrhagic fever in Asia, Europe, and Africa. J. Med. Entomol. 15:307–417 [DOI] [PubMed] [Google Scholar]
- 26. Konduru K., et al. 2011. Ebola virus glycoprotein Fc fusion protein confers protection against lethal challenge in vaccinated mice. Vaccine 29:2968–2977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kostrzak A., et al. 2009. Oral administration of low doses of plant-based HBsAg induced antigen-specific IgAs and IgGs in mice, without increasing levels of regulatory T cells. Vaccine 27:4798–4807 [DOI] [PubMed] [Google Scholar]
- 28. Lajeunesse M., Zhang Q., Finn A. 2004. Mucosal immunity to infections and its importance in future vaccinology. Adv. Exp. Med. Biol. 549:13–22 [DOI] [PubMed] [Google Scholar]
- 29. Levine M. M., Sztein M. B. 2004. Vaccine development strategies for improving immunization: the role of modern immunology. Nat. Immunol. 5:460–464 [DOI] [PubMed] [Google Scholar]
- 30. Li J. T., et al. 2006. Immunogenicity of a plant-derived edible rotavirus subunit vaccine transformed over fifty generations. Virology 356:171–178 [DOI] [PubMed] [Google Scholar]
- 31. Maltezou H. C., et al. 2010. Crimean-Congo hemorrhagic fever in Europe: current situation calls for preparedness. Euro. Surveill. 15:19504. [PubMed] [Google Scholar]
- 32. Mason H. S., Arntzen C. J. 1995. Transgenic plants as vaccine production systems. Trends Biotechnol. 13:388–392 [DOI] [PubMed] [Google Scholar]
- 33. Mason H. S., Haq T. A., Clements J. D., Arntzen C. J. 1998. Edible vaccine protects mice against Escherichia coli heat-labile enterotoxin (LT): potatoes expressing a synthetic LT-B gene. Vaccine 16:1336–1343 [DOI] [PubMed] [Google Scholar]
- 34. Modelska A., et al. 1998. Immunization against rabies with plant-derived antigen. Proc. Natl. Acad. Sci. U. S. A. 95:2481–2485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Neutra M. R., Kozlowski P. A. 2006. Mucosal vaccines: the promise and the challenge. Nat. Rev. Immunol. 6:148–158 [DOI] [PubMed] [Google Scholar]
- 36. Papa A., Papadimitriou E., Christova I. 2011. The Bulgarian vaccine Crimean-Congo haemorrhagic fever virus strain. Scand. J. Infect. Dis. 43:225–229 [DOI] [PubMed] [Google Scholar]
- 37. Pizzuti F., Daroda L. 2008. Investigating recombinant protein exudation from roots of transgenic tobacco. Environ. Biosafety Res. 7:219–226 [DOI] [PubMed] [Google Scholar]
- 38. Richardson J. S., Dekker J. D., Croyle M. A., Kobinger G. P. 2010. Recent advances in Ebolavirus vaccine development. Hum. Vaccin. 6:439–449 [DOI] [PubMed] [Google Scholar]
- 39. Roy S., et al. 2010. Rabies glycoprotein fused with B subunit of cholera toxin expressed in tobacco plants folds into biologically active pentameric protein. Protein Expr. Purif 70:184–190 [DOI] [PubMed] [Google Scholar]
- 40. Sambrook J., Russell D. W. 2001. Molecular cloning: a laboratory manual, 3rd ed. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, NY. [Google Scholar]
- 41. Sanchez A. J., Vincent M. J., Nichol S. T. 2002. Characterization of the glycoproteins of Crimean-Congo hemorrhagic fever virus. J. Virol. 76:7263–7275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Schwarz T., Schwarz T. F., Nsanze H., Ameen A. M. 1997. Clinical features of Crimean-Congo haemorrhagic fever in the United Arab Emirates. Infection 25:364–367 [DOI] [PubMed] [Google Scholar]
- 43. Spik K., et al. 2006. Immunogenicity of combination DNA vaccines for Rift Valley fever virus, tick-borne encephalitis virus, Hantaan virus, and Crimean Congo hemorrhagic fever virus. Vaccine 24:4657–4666 [DOI] [PubMed] [Google Scholar]
- 44. Streatfield S. J. 2006. Mucosal immunization using recombinant plant-based oral vaccines. Methods 38:150–157 [DOI] [PubMed] [Google Scholar]
- 45. Sullivan N. J., et al. 2006. Immune protection of nonhuman primates against Ebola virus with single low-dose adenovirus vectors encoding modified GPs. PLoS Med. 3:e177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Tacket C. O., et al. 1998. Immunogenicity in humans of a recombinant bacterial antigen delivered in a transgenic potato. Nat. Med. 4:607–609 [DOI] [PubMed] [Google Scholar]
- 47. Tasdelen Fisgin N., Ergonul O., Doganci L., Tulek N. 2009. The role of ribavirin in the therapy of Crimean-Congo hemorrhagic fever: early use is promising. Eur. J. Clin. Microbiol. Infect. Dis. 28:929–933 [DOI] [PubMed] [Google Scholar]
- 48. Thanavala Y., et al. 2005. Immunogenicity in humans of an edible vaccine for hepatitis B. Proc. Natl. Acad. Sci. U. S. A. 102:3378–3382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Topping J. F. 1998. Tobacco transformation. Methods Mol. Biol. 81:365–372 [DOI] [PubMed] [Google Scholar]
- 50. Whitehouse C. A. 2004. Crimean-Congo hemorrhagic fever. Antiviral Res. 64:145–160 [DOI] [PubMed] [Google Scholar]
- 51. Woods R. R., Geyer B. C., Mor T. S. 2008. Hairy-root organ cultures for the production of human acetylcholinesterase. BMC Biotechnol. 8:95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Yen Y. C., et al. 1985. Characteristics of Crimean-Congo hemorrhagic fever virus (Xinjiang strain) in China. Am. J. Trop. Med. Hyg. 34:1179–1182 [PubMed] [Google Scholar]