Abstract
Previous studies using cross-sectional designs suggest that asthma trigger recognition and management are suboptimal in clinical practice. The objective of this study was to assess gaps between asthma guideline recommendations and clinical practice regarding asthma trigger recognition and management by tracking poorly controlled asthma patients over a 2-year period. A retrospective cohort study of a representative sample of 102 children and adult residents of Olmsted County, MN, with poor asthma control in 2003–2004 was performed. All medical records from each asthma-related visit were examined for documented asthma trigger inquiries, specific trigger avoidance advice, and for adherence to the trigger avoidance advice. One hundred two subjects made 686 asthma-related visits that were included for analysis. At least 1 trigger inquiry occurred in 83% of visits, with an average of 2.0 triggers queried per visit. The most common trigger inquiries were for infection (47%), environmental tobacco smoke (41%), and allergens (29%). The mean number of triggers queried was higher during exacerbation visits versus nonexacerbation visits (2.1 versus 1.8; p < 0.001) and in the emergency care settings compared with outpatient settings (2.4 versus 1.7; p < 0.001). Advice for managing asthma triggers was given in 30% of visits and adherence to trigger advice was evaluated at 6% of visits. Future interventions for improving asthma trigger management should be targeted to routine asthma outpatient visits, where trigger avoidance advice is infrequent and rarely addressed in follow-up visits.
Asthma affects nearly 300 million people worldwide and is responsible for ~250,000 deaths each year.1 Asthma exacerbations have significant direct (hospital and emergency department [ED] visits) and indirect costs (school and work absenteeism and preventable deaths). Identification of asthma triggers is an essential component of comprehensive asthma management programs recommended in asthma guidelines.2,3
Data from several studies suggest that asthma trigger management is suboptimal in clinical practice.4–10 In the 2003 National Survey on Environmental Management of Asthma and Children’s Exposure to Environmental Tobacco Smoke (ETS) of 2353 children with asthma revealed that only 58% reported their triggers were diagnosed by a physician.4 More importantly, the survey reported that only 7% of respondents were following all recommended actions to reduce exposure to environmental triggers.4 People with asthma who reported that their triggers were diagnosed by a physician and had a comprehensive asthma management plan were more likely to enact the highest level of trigger management.4 In a survey of asthma and allergy experts, 82% of respondents thought that their asthma patients implemented only a few of the recommended environmental trigger control measures (as opposed to “some,” “many,” or “most” of the measures).5 Children enrolled in the Childhood Asthma Management Program had significant levels of exposure to allergens and ETS, suggesting that many patients had either not received advice from their clinician or did not adhere to the clinician’s recommendations.6 A survey of parents caring for children with asthma found that 43% of visits involved some type of environmental control discussion.7 Audiotapes from pediatric inner-city ED encounters for asthma exacerbation recorded 78% of clinicians asking about triggers, but also found that only 16% of clinicians stressed the importance of avoiding triggers.8 Another survey found that 80% of parents perceive triggers in their asthmatic children but that 51% of the initiated environmental control measures were inconsistent with published guidelines, suggesting that parents were either not discussing these measures with their clinicians or that the clinicians were giving advice inconsistent with published guidelines.9 Taken together, the existing data from patient surveys, clinician surveys, medical charts, and audiotaped encounters suggest that there is a significant difference between the guideline recommendations for asthma trigger management and current clinical practice.
The contention that asthma trigger management is suboptimal is largely based on cross-sectional studies.6–9 The cross-sectional study design is limited by an inability to track patients to determine if they are receiving trigger management advice in future health care encounters of if they are adhering to the trigger management advice. Previous studies have not addressed the follow-up, if any, that patients receive regarding asthma trigger management. Asthma patients likely need reminders to continue managing their asthma triggers—similar to reminders that are required for adhering to their asthma controller medications. A retrospective cohort study design, taking advantage of a uniquely linked database, allows for an examination of where in the health care system asthma trigger management may be suboptimal. Are there particular health care settings in which asthma trigger management is delivered more effectively? Where in the health care delivery system are there opportunities to improve asthma trigger management? If a patient presents for an asthma exacerbation, is trigger identification and management more likely than if presenting for a routine outpatient visit? The first goal of this study is to quantify and confirm the gap between guideline-suggested asthma trigger management and determine if this gap persists in multiple health care settings over a 2-year period. The second goal of this study is to identify the best opportunities within the health care system to improve asthma trigger management.
METHODS
Experimental Design
The study is a retrospective cohort study following subjects for 2 years using existing medical record. The subjects were randomly selected from a group of Olm-sted County (Minnesota) residents meeting a predetermined definition of poor asthma control. Approval was obtained from both the Olmsted County Medical Center and from the Mayo Foundation institutional review boards. For each selected subject, all asthma visits were reviewed and data were recorded for the visit site, reason for visit, documented evaluation of specific triggers, documented trigger avoidance advice, or assessment of adherence to avoidance advice. Clinician notes (including physician, physician assistants, nurse practitioners, nurses, and asthma educators), referral letters, and consultation letters were reviewed using a standardized chart abstraction form.
Subject Identification and Selection
The cohort of asthma subjects was identified using the Rochester Epidemiology Project (REP). Starting over 45 years ago, the REP is a data linkage project that makes it possible to identify all health care diagnoses and utilization at any health care facilities in Olmsted County, Minnesota. After excluding all patients with less than two asthma visits (ICD-9 code of 493.xx) during 2003–2004, patients were included in the study analysis if they were (1) aged from birth to 45 years old11 and (2) met at least one of the following proxy measures of poor asthma control: four or more asthma-related visits in either 2003 or 2004, any hospitalization or emergency care (including urgent care) visit for asthma in 2003–2004, or a cluster of three or more visits within 14 days for asthma in either 2003 or 2004.12 Exclusion criteria were (1) subjects that refused research authorization and/or (2) subjects with a diagnosis of chronic obstructive pulmonary disease or another major respiratory disease. From this group, 102 patients were randomly selected and as subjects of this study.
Definitions
An asthma exacerbation was defined by a visit to a specific site (ED, urgent care, or hospital), a prescription for systemic corticosteroids, or a cluster of three visits for asthma in 14 days.12 Only visits that listed asthma as a diagnosis in the impression, assessment, recommendation, or plan sections for that visit were included in the study. The sites of care are any sites where care for asthma is provided within the usual medical care systems. Primary care is defined as family medicine, pediatrics, and internal medicine. Asthma specialty care is defined as allergy and pulmonology care. Emergency care is defined as visits to the ED or urgent care. Asthma trigger inquiries were collected by category (see Table 1 for a list of the most common categories).
Table 1.
Trigger inquiry definitions
| Viral and bacterial infection | Fever, symptoms of upper respiratory infection, and symptoms of sinusitis or pneumonia |
| Allergen | Animal dander (including cat, dog, mouse, or any other furred animal), pollen (tree, grass, and weed), molds, and house-dust mites |
| Tobacco smoke exposure | First-hand or second-hand exposure including cigarette, pipe, cigar, or other smoke exposure |
| Air pollution | Worsening symptoms that relate to poor air quality as perceived by the patient or parent |
| Occupational | Any documentation of a work history or specific chemical exposure history |
| Medications | Medications that were potentially contributing to worsened asthma control; listing of all of the patient’s medications was not considered a query |
| Foods | Specific foods as asthma triggers |
| Comorbid conditions | Allergic rhinitis, sinusitis, gastroesophageal reflux disease, obstructive sleep apnea, allergic bronchopulmonary aspergillosis, and psychological stress |
Statistical Analysis
Descriptive statistics are presented in tables and figures. Percents are compared between groups using chi-squared tests. Numbers of triggers per visit are compared between groups using Wilcoxon rank-sum tests or Kruskal-Wallis tests. Multivariate logistic regression models were created for the trigger advice using the predictors of age, gender, exacerbation visit versus nonexacerbation visit, provider type, and site of care. The sample size was not based on a power calculation because no preliminary rates of trigger advice or adherence assessment were available from the medical literature to report those calculations. From clinical experience, it was estimated that ~100 subjects would provide the necessary diversity to describe trigger recognition and management in the Olmsted County population. The data were abstracted by the first author (M.R.); five randomly selected charts were reviewed by another abstractor (L.P.) and the interrater reliability was >90%.13
RESULTS
Subject and Visit Descriptions
The 102 randomly selected subjects with poorly controlled asthma had 686 asthma-related visits in 2003–2004. The subjects were 61% female patients and 65% white ethnicity (21% unknown; Table 2). Slightly more than one-half (51%) of the 686 asthma visits were defined as asthma exacerbation visits using the predetermined definition. Subjects had a mean of 6.7 asthma visits over the 2-year study period. Overall, children and adults had similar visit rates although girls and women had significantly more visits/subject compared with boys and men (7.5 versus 5.5; p = 0.01). The majority of asthma visits occurred in primary care (59%) followed by allergy (21%) and emergency clinicians (17%). Table 3 summarizes the asthma visit descriptions.
Table 2.
Subject demographics
| No. of subjects | 102 |
| Female | 61% |
| Median age, yr | 22 |
| Ethnicity | |
| White | 65% |
| Black | 7% |
| Asian | 5% |
| Hispanic | 4% |
| Unknown or other | 21% |
| Qualifying event for poor asthma control* | |
| ED visit for asthma | 61% |
| Hospitalization for asthma | 17% |
| ≥3 asthma visits in 2 wk | 37% |
| ≥4 asthma visits in 1 yr | 60% |
Subjects can qualify in more than one category.
ED = emergency department.
Table 3.
Asthma visit descriptions
| No. of asthma visits | 686 | |
| Mean asthma visits per subject | 6.7 visits/person | |
| No. of exacerbation visits | 352 (51%) | |
| Exacerbation visits by age | ||
| Adult | 6.4 visits/person | |
| Children | 7.2 visits/person | p = 0.63 |
| Exacerbation visits by gender | ||
| Female | 7.5 visits/person | |
| Male | 5.5 visits/person | p = 0.01 |
| Visit specialties | ||
| Primary care | 59% | |
| Allergy | 21% | |
| Emergency | 17% | |
| Pulmonology | 2% | |
| Other | 2% | |
| Visit site type | ||
| Outpatient | 73% | |
| Emergency department | 15% | |
| Urgent care | 8% | |
| Inpatient hospital | 4% | |
Trigger Inquiries
The mean number of documented trigger inquiries per asthma visit was 2.0, with 83% of asthma visits recording ≥1 trigger inquiry. The most common documented trigger inquiries were for infection (47%), ETS exposure (41%), and allergens (29%). The mean number of trigger inquiries per visit was higher in EDs compared with primary care and allergy office visits (2.4 versus 1.7; p < 0.001). The mean number of inquires did not differ by age or gender (p > 0.05 for both). Exacerbation visits had ≥1 trigger inquiry 86% of the time, compared with 80% at nonexacerbation visits (p = 0.05) and mean trigger inquiries were more common during exacerbation visits than nonexacerbation visits (2.1 versus 1.8; p < 0.001). Rates of noninfection trigger inquiries did not differ between exacerbation and nonexacerbation visits (p > 0.05; Table 4).
Table 4.
Trigger inquiry descriptions
| Mean no. of trigger inquiries | 2.0 ± 1.4 | |
| Visits with ≥1 trigger inquiry | 83% | |
| Mean no. of inquires by provider | ||
| Emergency | 2.4 ± 1.1 | |
| Allergy | 2.3 ± 2.3 | |
| Primary care | 1.7 ± 1.4 | p < 0.0001 |
| Mean no. of inquires by age | ||
| Children | 2.0 ± 1.7 | |
| Adult | 1.9 ± 1.6 | p = 0.71 |
| Mean no. of inquires by gender | ||
| Female | 1.9 ± 1.6 | |
| Male | 2.1 ± 1.7 | p = 0.10 |
| Any trigger inquiry by visit type | ||
| Exacerbation visit | 86% | |
| Nonexacerbation visit | 80% | p = 0.05 |
| Mean asthma trigger inquiry by visit type | ||
| Exacerbation visit | 2.0 ± 1.4 | |
| Nonexacerbation visit | 1.9 ± 1.8 | p = 0.001 |
| Any trigger inquiry (noninfection) | ||
| Exacerbation visit | 64% | |
| Nonexacerbation visit | 67% | p = 0.64 |
| Trigger inquiry types | ||
| Infection | 47% | |
| Tobacco smoke | 41% | |
| Allergens | 29% | |
| Exercise | 15% | |
| Sinusitis | 5% | |
| Cold air | 5% | |
Trigger Advice
Advice to the subjects on trigger management was documented in 30% of asthma visits, with the most common advice relating to infection (14%), allergen (9%), and ETS (6%). Multivariate logistic regression for trigger advice examined the predicting factors of age (child versus adult), gender, asthma exacerbation visit (versus nonexacerbation visit), and provider type. Provider type was confounded with exacerbation visit and using provider type yielded a better predictive model. Results were significantly different between trigger advice related to infection and noninfection trigger advice and therefore were analyzed separately.
Patient demographics and provider types appeared to influence asthma trigger management. Adults were more likely than children to receive trigger management advice (odds ratio [OR] = 1.7 [1.1–2.8]). Adults were also more likely than children to receive noninfection trigger advice (OR = 2.3 [1.5–3.6]). Male subjects received noninfection trigger advice more frequently than female subjects (OR = 2.0 [1.3–3.2]). Emergency room clinicians were more likely than out-patient clinicians to give infection trigger advice (OR = 1.8 [1.1–3.0]) and less likely to give noninfection trigger advice (OR = 0.2 [0.1–0.5]).
Trigger Management Adherence
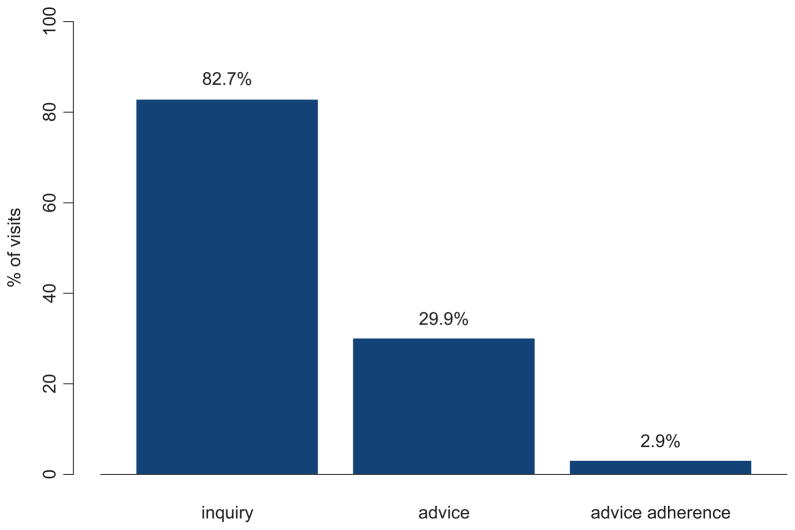
To further explore trigger management, medical records were reviewed for documentation of follow-up on trigger avoidance advice and whether patients reported adherence to the advice. Asking about adherence to any trigger advice was recorded at 44 visits (6%); subject reported following the advice in 43% of the visits for which it was assessed. Overall, adherence to trigger management advice was confirmed in 3% of all asthma visits abstracted in this study (Fig. 1). Considered another way, follow-up to assess adherence to trigger avoidance advice was only documented in 10% of instances in which advice was given. Not all subjects that received trigger avoidance advice necessarily followed up with the clinician giving the advice.
Figure 1.
Identifying gaps in asthma trigger recognition and management.
DISCUSSION
For this population of children and adults with poorly controlled asthma, most visits for asthma contained documentation of trigger inquiries. However, advice for managing triggers was documented in less than one-third of asthma visits, and documented assessment of adherence to trigger avoidance advice was rare. This is the first study that we are aware of that has addressed asthma trigger recognition and management over time and across multiple care settings. Because poor asthma control and asthma exacerbations are linked to trigger exposure, failure to document trigger information may represent an important gap in asthma care among these subjects.
The first goal of this study was to quantify and confirm the gap between guideline-suggested asthma trigger management and determine if this gap persists in multiple health care settings over a 2-year period. The largest gaps appear to be in giving asthma management advice and following up to ensure adherence to the advice. However, we should not overlook the initial step in asthma trigger management—identification of potential asthma triggers. By only inquiring about an average of only 2 triggers/visit, many potentially relevant triggers may have gone unidentified. The number of triggers identified in our community-based study across multiple clinical settings fell far short of those identified using structured interviews in study settings: pollen, 67–84%; pets, 46–59%; mold or dampness, 60–63%; dust, 59–79%; cold air, 71–77%; weather change, 71–85%; ETS, 71–76%; exercise, 79–88%; and aspirin, 14%.6,14 Therefore, we believe that our findings of limited trigger identification is not caused by the lack of potentially identifiable triggers; rather, asthma triggers are not being effectively identified and managed in the clinical settings studied.
The second goal of this study was to identify the best opportunities within the health care system to improve asthma trigger management. The findings from our study suggest that asthma trigger identification is different depending on the setting (ED or outpatient visit) and whether the patient is presenting for an asthma exacerbation or not. Trigger inquiries were less common during nonexacerbation visits; therefore, we believe that nonexacerbation outpatient visits represent an opportunity not only to improve trigger inquiry, but also to provide advice and follow-up. The infrequent documentation of trigger avoidance advice during asthma visits could be caused by the limited time that clinicians have with asthma patients as well as the lack of effective tools for identifying asthma triggers. Asthma tools designed for use in outpatient primary care settings may be helpful. For example, the Asthma APGAR tool is tailored for busy primary care providers and specifically addresses trigger identification.10 A second example of a tool for asthma trigger management is the Asthma Trigger Inventory.15 A third potential solution is the increased the use of written asthma action plans and ensuring that these plans adequately address trigger management.
We considered alternative explanations for our findings. Trigger advice during asthma visits may be infrequent due to the perception that environmental trigger advice is of limited value in asthma management. However, previous survey studies have suggested that clinicians favorably view asthma trigger control measures.5 A 2004 survey of asthma and allergy experts revealed that 60% of respondents felt that environmental trigger control was at least as important as pharmacotherapy and immunotherapy for asthma.5 A survey of primary care providers and allergists found that 96% felt that trigger identification is required in an ED visit and 72% felt it should be required to stress the importance of avoiding triggers.8 Several studies support trigger management for viral infection,16–21 bacterial infection,22–24 allergens,25–32 and ETS.33–35 In fact, a large study of adult acute asthma care found that the most prominent modifiable risks for asthma health care use are ETS exposure and a positive allergy skin test to cats or dogs.36 Several studies have evaluated programs that attempted to decrease exposure to asthma triggers. Those interventions that included an educational component and used a multifaceted approach were the most successful at reducing asthma symptoms.25,37 The results from these studies suggest a favorable impression of asthma trigger management among clinicians; this favorable impression suggests that our data can not be explained alone by clinicians’ perception that asthma trigger management is of limited value.
The limitations of the study are the reliance on medical record documentation, the modest sample size, and that the sample was from a single region of the country with limited racial and ethnic diversity. Audiotape from pediatric ED encounters found similar trigger inquiry rates (78% compared with 83% in this study) and advice rates (16% for inquiry compared with 30% in this study).8 This same pediatric ED study compared the audiotape findings to the medical record and did not find a statistically significant difference (possibly because of small sample size).8 In a different study, a phone call to the parent 2 weeks after the visit may be an even more reliable measurement of the information shared during a pediatric asthma visit.38 Although verbal (not documented) instructions and parent recall with phone interviewing may capture details of the asthma visit better than chart documentation, chart documentation is, nonetheless, important for ongoing care. It is unlikely that the same provider will recall the trigger management issues at a subsequent visit if it was not documented in the medical record (and difficult for a different provider to know that verbal advice was given previously).
CONCLUSION
This study has found asthma trigger recognition and management over time and across multiple health care settings to be suboptimal and a prime target for future asthma care interventional efforts. Future interventions for improving asthma trigger management should be targeted to routine asthma outpatient visits.
Acknowledgments
Supported by the Mayo Foundation
M. Rank has received a research grant to his institution from Purezone, Inc. P. Wollan, J. Li, and B. Yawn have nothing to declare pertaining to this article Approved by the Mayo Foundation Institutional Review Board
We acknowledge the REP and its funding source (NIH/NHMS RO1 AR30582), Mayo Clinic Rochester Center for Translational Science Activities, and Linda Paradise, R.N., of the Olmsted Medical Center for assistance on this project.
References
- 1.Masoli M, Fabian D, Holt S, et al. The global burden of asthma: Executive summary of the GINA dissemination committee report. Allergy. 2004;59:469–478. doi: 10.1111/j.1398-9995.2004.00526.x. [DOI] [PubMed] [Google Scholar]
- 2.National Heart, Lung, and Blood Institute. Expert Panel Report 3 (EPR3): Guidelines for the diagnosis and management of asthma. [last accessed December 12, 2007.];:109–111. 170–183. Available online at www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm.
- 3.Global Initiative for Asthma (GINA) [last accessed December 12, 2007.];Global strategy for asthma management and prevention. :55–57. Available online at www.ginaasthma.com.
- 4. [last accessed December 12, 2008.];National Survey on Environmental Management of Asthma and Chidlren’s Exposure to Environmental Tobacco Smoke. Available online at www.epa.gov/asthma/pdfs/survey_fact_sheet.pdf.
- 5.Brandt DM, Levin L, Matsui E, et al. Allergists’ attitudes toward environmental control: Insights into its current application in clinical practice. J Allergy Clin Immunol. 2008;121:1053–1054. doi: 10.1016/j.jaci.2007.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weiss ST, Horner A, Shapiro G, et al. The prevalence of environmental exposure to perceived asthma triggers in children with mild-to-moderate asthma: Data from the Childhood Asthma Management Program (CAMP) J Allergy Clin Immunol. 2001;107:634–640. doi: 10.1067/mai.2001.113869. [DOI] [PubMed] [Google Scholar]
- 7.Halterman JS, Kitzman H, McMullen A, et al. Quantifying preventive asthma care delivered at office visits: The preventive asthma care-composite index (PAC-CI) J Asthma. 2006;43:559–564. doi: 10.1080/02770900600859172. [DOI] [PubMed] [Google Scholar]
- 8.Crain EF, Mortimer KM, Bauman LJ, et al. Pediatric asthma care in the emergency department: Measuring the quality of history-taking and discharge planning. J Asthma. 1999;36:129–138. doi: 10.3109/02770909909065156. [DOI] [PubMed] [Google Scholar]
- 9.Cabana MD, Slish KK, Lewis TC, et al. Parental management of asthma triggers within a child’s environment. J Allergy Clin Immunol. 2004;114:352–357. doi: 10.1016/j.jaci.2004.04.047. [DOI] [PubMed] [Google Scholar]
- 10.Yawn BP, Betram S, Wollan P. Introduction of asthma APGAR tools improve asthma management in primary care practices. J Asthma Allergy. 2008;2008:1–10. doi: 10.2147/jaa.s3595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tinkelman DG, Price DB, Nordyke RJ, et al. Misdiagnosis of COPD and asthma in primary care patients 40 years of age and older. J Asthma. 2006;43:75–80. doi: 10.1080/02770900500448738. [DOI] [PubMed] [Google Scholar]
- 12.Yawn BP, Wollan PC, Bertram SL, et al. Asthma treatment in a population-based cohort: Putting step-up and step-down treatment changes in context. Mayo Clin Proc. 2007;82:414–421. doi: 10.4065/82.4.414. [DOI] [PubMed] [Google Scholar]
- 13.Yawn BP, Wollan P. Interrater reliability: Completing the methods description in medical records review studies. Am J Epidemiol. 2005;161:1974–1977. doi: 10.1093/aje/kwi122. [DOI] [PubMed] [Google Scholar]
- 14.Chen H, Johnson CA, Haselkorn T, et al. Subspecialty differences in asthma characteristics and management. Mayo Clin Proc. 2008;83:786–793. doi: 10.4065/83.7.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ritz T, Steptoe A, Bobb C, et al. The Asthma Trigger Inventory: Validation of a questionnaire for perceived triggers of asthma. Psychosom Med. 2006;68:956–965. doi: 10.1097/01.psy.0000248898.59557.74. [DOI] [PubMed] [Google Scholar]
- 16.Walter MJ, Castro M, Kunselman SJ, et al. Predicting worsening asthma control following the common cold. Eur Respir J. 2008;32:1548–1554. doi: 10.1183/09031936.00026808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnston SL, Pattermore PK, Sanderson G, et al. Community study of role of viral infections in exacerbations of asthma in 9–11 year-old children. BMJ. 1995;310:1225–1229. doi: 10.1136/bmj.310.6989.1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nicholson KG, Kent J, Ireland DC. Respiratory viruses and exacerbations of asthma in adults. BMJ. 1993;307:982–986. doi: 10.1136/bmj.307.6910.982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jackson DJ, Gangnon RE, Evans MD, et al. Wheezing rhinovirus illnesses in early life predict asthma development in high-risk children. Am J Respir Crit Care Med. 2008;178:667–672. doi: 10.1164/rccm.200802-309OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Green RM, Custovic A, Sanderson G. Risk factors for hospital admission with acute asthma: Synergism between sensitization and exposure to allergens and viral respiratory infections. BMJ. 2002;324:763–766. doi: 10.1136/bmj.324.7340.763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chauhan AJ, Inskip HM, Linaker CH, et al. Personal exposure to nitrogen dioxide (NO2) and the severity of virus-induced asthma in children. Lancet. 2003;361:1939–1944. doi: 10.1016/S0140-6736(03)13582-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnston SL, Martin RJ. Chlamydophila pneumoniae and mycoplasma pneumoniae: A role in asthma pathogenesis? Am J Respir Crit Care Med. 2005;172:1078–1089. doi: 10.1164/rccm.200412-1743PP. [DOI] [PubMed] [Google Scholar]
- 23.Juhn YJ, Kita H, Yawn BP, et al. Increased risk of serious pneumococcal disease in patients with asthma. J Allergy Clin Immunol. 2008;122:719–723. doi: 10.1016/j.jaci.2008.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Talbot TR, Hartert TV, Mitchel E, et al. Asthma is a risk factor for invasive pneumococcal disease. N Engl J Med. 2005;352:2082–2090. doi: 10.1056/NEJMoa044113. [DOI] [PubMed] [Google Scholar]
- 25.Woodcock A, Foster L, Matthews E, et al. Control of exposure to mite allergen and allergen-impermeable bed covers for adults with asthma. N Engl J Med. 2003;349:225–236. doi: 10.1056/NEJMoa023175. [DOI] [PubMed] [Google Scholar]
- 26.Morgan WJ, Crain EF, Gruchalla RS, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004;351:1068–1080. doi: 10.1056/NEJMoa032097. [DOI] [PubMed] [Google Scholar]
- 27.Carter MC, Perzanowski MS, Raymond A, et al. Home intervention in the treatment of asthma among inner-city children. J Allergy Clin Immunol. 2001;108:732–737. doi: 10.1067/mai.2001.119155. [DOI] [PubMed] [Google Scholar]
- 28.Klinnert MD, Liu AH, Pearson MR, et al. Short-term impact of a randomized multifaceted intervention for wheezing infants in low-income families. Arch Pediatr Adolesc Med. 2005;159:75–82. doi: 10.1001/archpedi.159.1.75. [DOI] [PubMed] [Google Scholar]
- 29.Krieger JW, Takaro TK, Song L, et al. The Seattle-King County Healthy Homes Project: A randomized, controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. Am J Public Health. 2005;95:652–659. doi: 10.2105/AJPH.2004.042994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eggleston PA, Butz A, Rand C, et al. Home environmental intervention in inner-city asthma: A randomized controlled clinical trial. Ann Allergy Asthma Immunol. 2005;95:518–524. doi: 10.1016/S1081-1206(10)61012-5. [DOI] [PubMed] [Google Scholar]
- 31.Bush RK. Indoor allergens, environmental avoidance, and allergic respiratory disease. Allergy Asthma Proc. 2008;29:575–579. doi: 10.2500/aap.2008.29.3172. [DOI] [PubMed] [Google Scholar]
- 32.Barnes CS, Kennedy K, Gard L, et al. The impact of home cleaning on quality of life for homes with asthmatic children. Allergy Asthma Proc. 2008;29:197–204. doi: 10.2500/aap.2008.29.3099. [DOI] [PubMed] [Google Scholar]
- 33.Chalmers GW, Macleod KJ, Little SA, et al. Influence of cigarette smoking on inhaled corticosteroid treatment in mild asthma. Thorax. 2002;57:226–230. doi: 10.1136/thorax.57.3.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chaudhuri R, Livingston E, McMahon AD, et al. Cigarette smoking impairs the therapeutic response to oral corticosteroids in asthma. Am J Repir Crit Care Med. 2003;168:1308–1311. doi: 10.1164/rccm.200304-503OC. [DOI] [PubMed] [Google Scholar]
- 35.Bernstein JA, Alexis N, Barnes C, et al. Health effects of air pollution. J Allergy Clin Immunol. 2004;114:1116–1123. doi: 10.1016/j.jaci.2004.08.030. [DOI] [PubMed] [Google Scholar]
- 36.Osborne ML, Pedula KL, O’Hollaren M, et al. Assessing future need for acute care in adult asthmatics. Chest. 2007;132:1151–1161. doi: 10.1378/chest.05-3084. [DOI] [PubMed] [Google Scholar]
- 37.Custovic A, van Wijk RG. The effectiveness of measures to change the indoor environment in the treatment of allergic rhinitis and asthma: ARIA update. Allergy. 2005;60:1112–1115. doi: 10.1111/j.1398-9995.2005.00934.x. [DOI] [PubMed] [Google Scholar]
- 38.Senturia YD, Bauman LJ, Coyle YM, et al. The use of parent report to assess the quality of care in primary care visits among children with asthma. Ambul Pediatr. 2001;1:194–200. doi: 10.1367/1539-4409(2001)001<0194:tuoprt>2.0.co;2. [DOI] [PubMed] [Google Scholar]