Abstract
Matrix metalloproteinases (MMPs) play a key role in the development of atherosclerosis and its complications. In vivo detection and quantification of MMP activation can help track the propensity to complications and response to therapy. We sought to establish an in vivo imaging approach for monitoring MMP activation in atherosclerotic mouse aorta and use it to assess the response to dietary modification.
Method and Results
Apo E−/− mice were fed normal chow or a high fat diet (HFD) for up to 3 months or HFD for 2 months followed by 1 month on normal chow. After three months of HFD, there was considerable atherosclerosis in the aorta. In vivo microSPECT/CT imaging using RP782 (an 111In-labeled tracer targeting activated MMPs) showed a heterogeneous pattern of tracer uptake along the aorta. Heterogeneity of RP782 uptake was confirmed by autoradiography, and specificity was demonstrated using excess unlabeled precursor. Tracer uptake quantified by microSPECT imaging significantly correlated with uptake quantified by autoradiography. Comparison of Oil Red O staining with autoradiography demonstrated areas of discordance between plaque presence and tracer uptake. HFD withdrawal led to significant reduction in RP782 uptake beyond the effect on plaque area. MMP expression and macrophage infiltration were similarly heterogeneous along the aorta and significantly reduced following withdrawal from the HFD. Finally, RP782 uptake significantly correlated with aortic macrophage content.
Conclusion
Molecular imaging of MMP activation reveals the heterogeneity of atherosclerotic plaques and is a useful tool for tracking plaque biology and response to therapy.
Keywords: Atherosclerosis, Imaging, Matrix metalloproteinases, Nuclear medicine
Introduction
Atherosclerotic plaques often develop near branching segments of the artery where flow-mediated changes in shear stress are believed to contribute to early endothelial activation and injury that culminate in advanced atherosclerotic lesions. In addition to spatial heterogeneity, a key characteristic of atherosclerosis is the considerable heterogeneity in plaque structure and composition. High risk plaques exhibit specific anatomical and biological features, including the presence of a thin fibrous cap, large necrotic core, outward remodeling and large number of inflammatory cells. The inflammatory cells promote a protease (including matrix metalloproteinase (MMP))-rich milieu that leads to plaque rupture and the resulting acute coronary syndromes (1,2). Preventive and therapeutic measures (e.g., dietary intervention) aim at ameliorating these pathological features to reduce the incidence of plaque rupture. However, despite a number of effective measures introduced in recent years, atherosclerosis remains a morbid disease. Recent advances in vessel wall imaging present an opportunity to detect in vivo structural and biological features of atherosclerotic plaque which have an impact on the clinical outcome (3,4).
Murine models are valuable experimental tools for studies of atherosclerosis biology. Similar to human disease, murine atherosclerosis consists of heterogeneous lesions with a variety of cellular and biological compositions. Molecular imaging of targets such as MMP activation, angiogenesis and apoptosis (5-7) can potentially provide unique quantitative information on plaque biology, including determinants of morbid events and response to therapeutic interventions. However, the small size of the aorta has often limited the quantification of imaging targets in the mouse to ex vivo measurements or in vivo measurements without ex vivo validation (5,8-10). Here, we detect and quantify MMP activation associated with atherogenesis by microSPECT/CT imaging in vivo, show its considerable heterogeneity along the aorta in high fat-fed apoE−/− mice, and demonstrate an effect of dietary intervention on MMP activation in atherosclerosis that extends beyond the effect on plaque development.
Materials and Methods
Reagents
Reagents were obtained from Sigma (St Louis, MI), unless otherwise specified. RP782, an 111In-labeled tracer with specificity for activated MMPs was provided by Lantheus Medical Imaging (North Billerica, MA). The structure, binding characteristics and biodistribution in mouse of MMP tracers were previously reported (5,11,12).
Animal model
Six to eight week old female apoE−/− mice (Jackson Laboratory, Bar Harbor, ME) were fed a high-cholesterol diet (1.25% cholesterol, Harlan Teklad, Madison, WI) ad libitum for one month (n=10), two months (n=8) or three months (n=10). In an additional group of animals, the high fat diet was replaced with normal chow after 2 months (n=10). Other animals were fed with normal chow for 3 months (n=3). Experiments were performed according to regulations of West Haven VA and Yale University’s Animal Care and Use Committees.
Imaging
Thirty seven (± 6.3) MBq RP782 (111In-labeled tracer targeting MMP activation epitope) (11) was administered to animals through a right jugular vein catheter placed under anesthesia (isofluorane 1–3%). Animals were imaged after 2 hours on a high-resolution small animal imaging system (X-SPECT, Gamma Medica-Ideas, Northridge, CA) with 1-mm medium-energy pinhole collimators (12). This system has a spatial resolution of ~2mm for In-111. Anesthetized mice were placed in a fixed position on the animal bed. Three point sources (37 to 185 KBq) were placed in the field of view to verify the accuracy of image fusion. The following acquisition parameters were used for microSPECT imaging: 360 degree, 128 projections, 30 seconds/projection (~80 minute image acquisition), 174 and 242 keV photopeaks ±10% window, matrix:82×82. After completion of microSPECT imaging, animals were injected with a continuous infusion of iodinated CT contrast (iohexol 350 mg/mL, rate: 100 µL/min) over 2 minutes, and CT imaging was performed (energy 75 kVP/280 µA, matrix 512×512) to identify anatomic structure. To demonstrate tracer uptake specificity, two animals fed the high fat diet for one month were injected with 50-fold excess unlabeled precursor 15 minutes prior to RP782 administration. The imaging protocol lasted ~1.5 hour, after which (3.5 hours after tracer administration) aortae were harvested for autoradiography.
MicroSPECT images were reconstructed by iterative reconstruction using system software (X-Flex). CT projection images were reconstructed with Cobra EXIM software that implements a cone-beam reconstruction algorithm. Reconstructed microSPECT images were reoriented according to the CT anatomic images, fused, and exported in the Interfile format for further processing with Amide, a medical imaging data examiner (isotropic voxel size 0.314 mm). For quantitative analysis of tracer uptake, nine serial cylindrical (2×2×2 mm) regions of interest (ROIs) were drawn along the aorta starting at the level of right brachiocephalic artery and ending proximal to take off of renal arteries. A ROI immediately anterior to thoracic descending aorta was used to calculate the background activity. Data were expressed as background-corrected counts per voxel (cpv)/MBq injected. Despite the presence of potentially confounding factors, e.g., scatter and partial volume effects, this approach yielded an excellent correlation with ex vivo measurements of tracer uptake. Multi-planar reconstruction was performed on successive images (thickness ~0.314mm) of the aorta and IVC using EViewBox (Java Medical Imaging Software).
Autoradiography
Explanted aortae were exposed to high-sensitivity, X-radiographic X-OMAT Kodak Scientific Imaging Film (Eastman Kodak, Rochester, NY) for various times to optimize detection. Linearity of the signal was confirmed using a set of standards with known activity deposited on absorbent paper which also served for tracer uptake quantification. Signal intensity was quantified on serial 2 mm square ROIs drawn along the aorta starting at the level of right brachiocephalic artery using Kodak 1D software (Kodak Scientific Imaging Systems, New Haven, CT). Data were background corrected and expressed as % injected dose. The small size of aortic sections and their dehydration during autoradiography prevented accurate weight measurements.
Oil Red O staining
Aortae were fixed in 4% formaldehyde. Staining with Oil Red O was performed according to a standard protocol. Briefly, after rinsing with water, the aorta was exposed to isopropanol (60%) for two minutes, followed by one hour staining with a solution of Oil Red O dissolved in isopropanol (10 mg/ml) and diluted to 60% in water. The excess stain was removed with isopropanol and water, and the aorta was photographed using a microscope equipped a digital camera (Leica, Heerbrugg, Switzerland). The red stained areas representing atherosclerotic lesions were measured using NIH ImageJ software (National Institutes of Health, Bethesda, MD), as previously described (13). The results were expressed as the ratio of total plaque area over total vessel area.
Quantitative RT-PCR
Starting at the level of right brachiocephalic artery, four consecutive 400 µm segments of the aorta, each at 4 mm interval, were used for RNA isolation. Total RNA was isolated from each aortic section using Absolutely RNA® Nanoprep Kit (Stratagene, La Jolla, CA), and reverse transcribed using QuantiTect® Reverse Transcription Kit (QIAGEN, Valencia, CA). Quantitative PCR was performed on this cDNA in triplicates using Taqman® primers (Applied Biosystems, Foster City, CA) and an Applied Biosystems 7500 Real-Time PCR System following the manufacturer’s instructions. The results were normalized to glyceraldehyde 3-phosphate dehydrogenase (GAPDH). The following primer sets were used: MMP-2 (Mm00439506_m1), MMP-3 (Mm00440295_m1), MMP-9 (Mm00442991_m1), MMP-12 (Mm00500554_m1), MMP-13 (Mm01168713_m1), CD68 (Mm00839636_g1), EMR1 (Mm00802529_m1); smooth muscle α-actin (Mm01546133_m1), CD31 (Mm00476702_m1) and GAPDH (Mm99999915_g1).
Statistical Analysis
Statistical analysis was performed using GraphPad Prism (La Jolla, CA). Data are presented as mean ± standard error (SE). Differences between two groups were tested using two-tailed unpaired Student’s t test. Multiple groups were compared using one way ANOVA with Dunn’s multiple comparison test or two way ANOVA followed by Bonferroni post-hoc analysis. Pearson correlation was used to test the association between 2 variables. Significance was set at the 0.05 level.
Results
MMP activation heterogeneity in atherosclerotic aorta
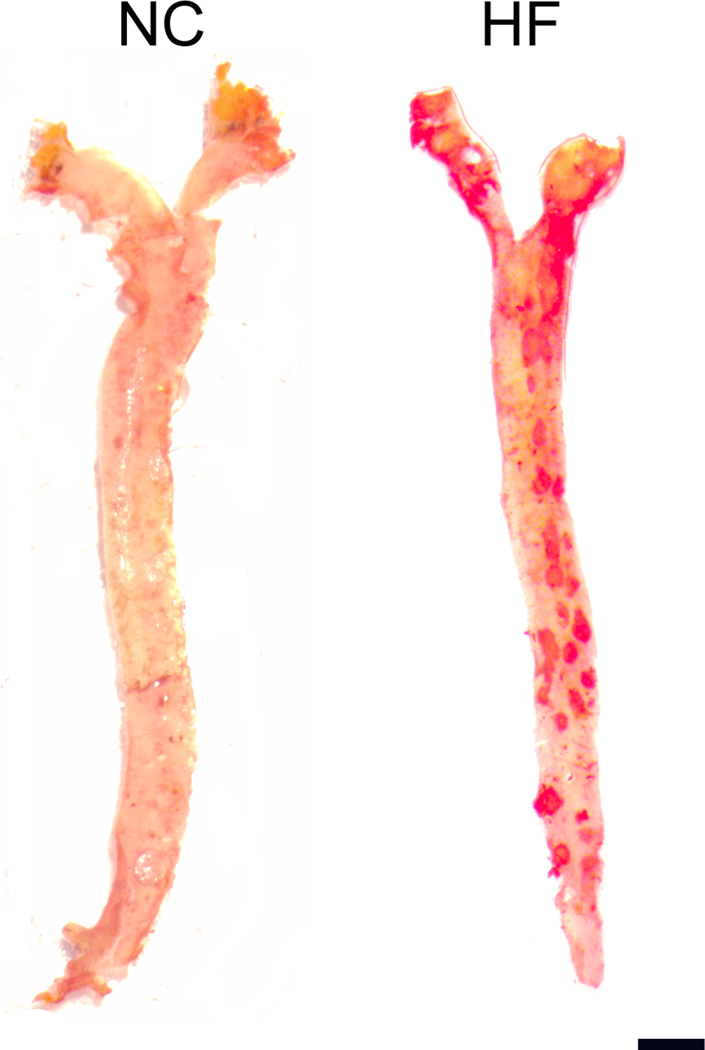
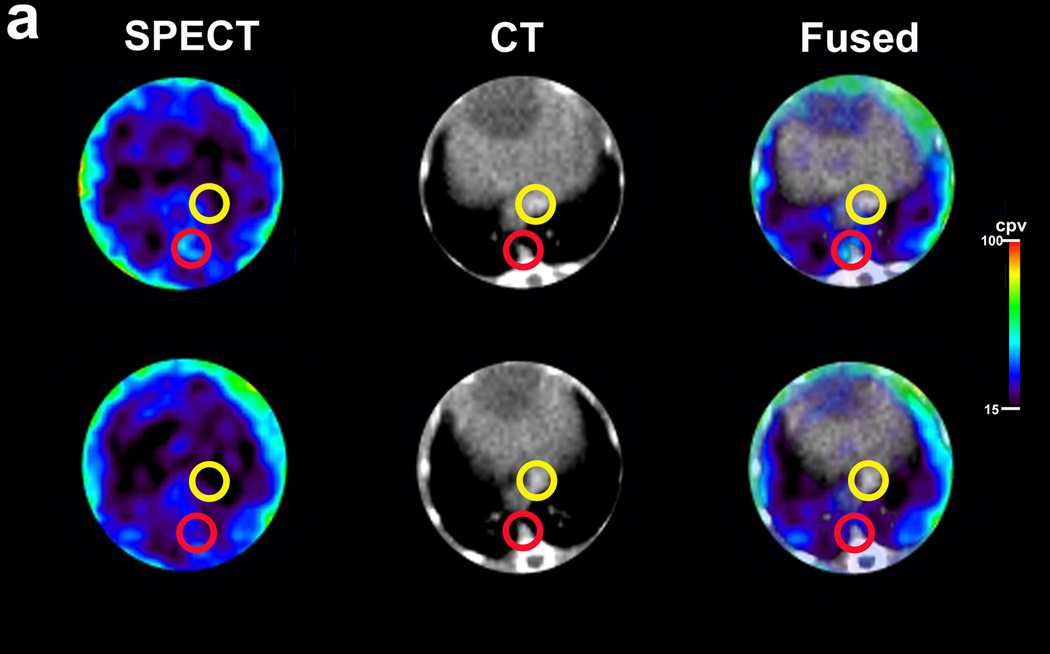
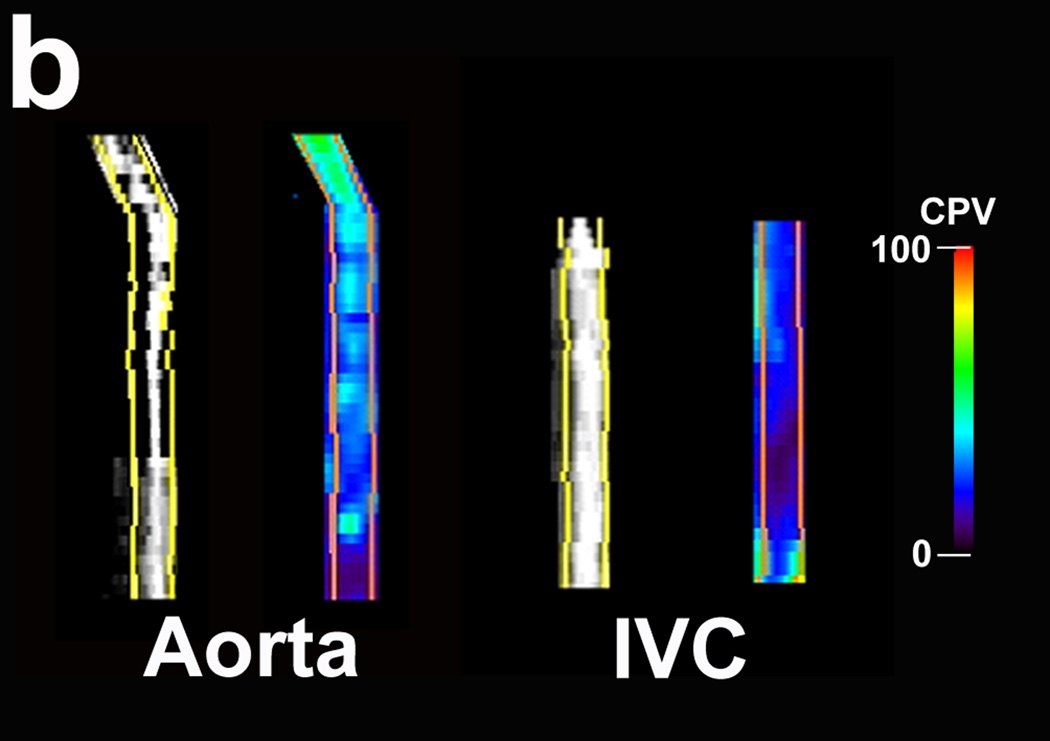
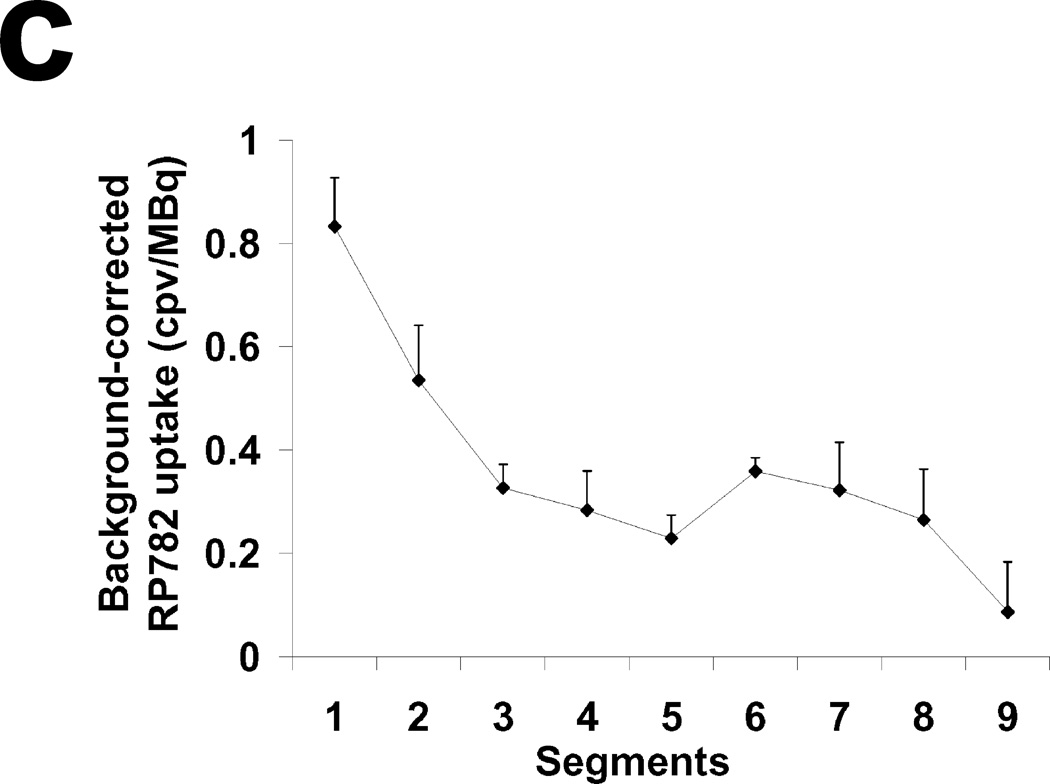
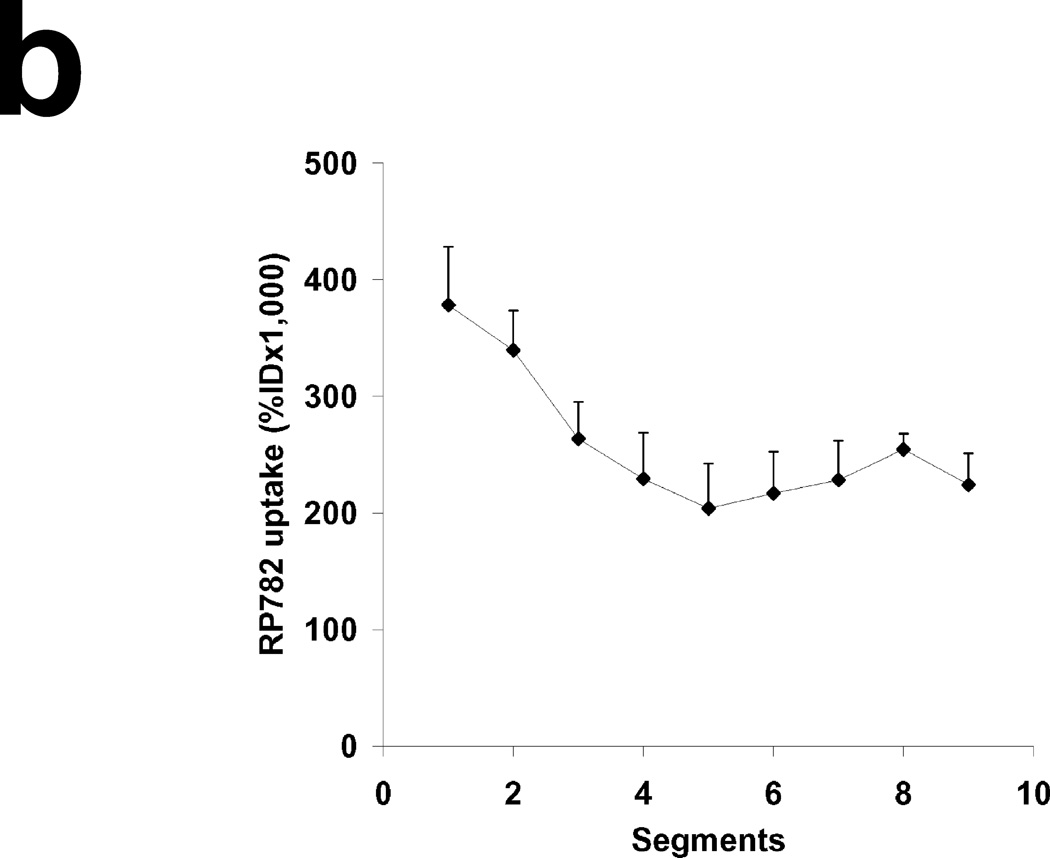
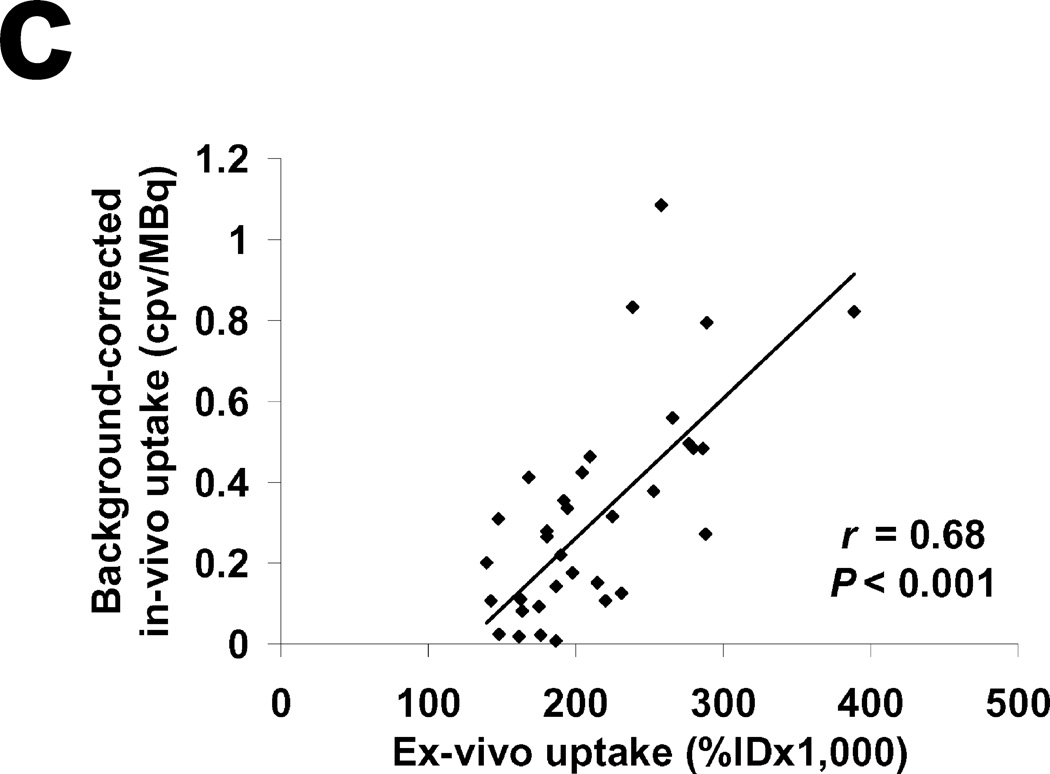
To investigate MMP activation pattern in native atherosclerotic lesions, apoE−/− mice were fed either a high fat diet or normal chow for three months. In animals fed with normal chow, Oil Red O staining demonstrated the presence of a few fatty deposits along the aorta (Figure 1). After 3 months of high fat diet there was extensive atherosclerosis along the aorta with the most prominent lesions localized in the proximal aorta (Figure 1). In these animals, microSPECT imaging of MMP activation with 111In-labeled RP782 (11,12), a radiotracer which specificity targets the MMP activation epitope, followed by CT angiography for anatomical localization demonstrated a heterogeneous MMP activation pattern along the aorta (Figure 2 and Supplemental Figure 1). Despite its larger size and blood volume, little tracer uptake could be detected in IVC which served as control for imaging studies. The heterogeneous pattern of RP782 uptake was more readily visible following multi-planar reformation of aorta based on CT angiography images (Figure 2B). In vivo quantification of RP782 uptake showed significantly higher mean uptake of the tracer in aorta as compared to IVC (0.36 ± 0.05 vs 0.09 ± 0.06 cpv/MBq, n=4, p=0.04), with the highest tracer uptake localized in the proximal aorta (Figure 2C). The heterogeneous pattern of tracer uptake along the aorta was confirmed by ex-vivo autoradiography (Figure 3A & B). There was a strong correlation between in vivo and ex vivo quantification of RP782 uptake along the aorta (r=0.68, p<0.001, Figure 3C). Oil Red O staining of explanted aortae demonstrated that while there was in general a good match between the presence of atherosclerosis and RP782 uptake in the aorta, areas of mismatch could be identified (Supplemental Figure 2).
Fig. 1.
Representative examples of Oil Red O staining of aortae of apoE−/− mice fed normal chow (NC) or high fat (HF) diet for 3 months, demonstrating the heterogeneous pattern of plaque development along the aorta. Scale bar: 2mm
Fig. 2.
RP782 microSPECT/CT imaging of MMP activation in atherosclerosis in apoE−/− mice fed a high fat diet for 3 months. A) Transversal SPECT, CT and fused SPECT and CT images demonstrating areas of high (top row) and low (bottom row) tracer uptake in the aorta (red circles). Little tracer uptake can be detected in inferior vena cava (yellow circles). B) Multiplanar reconstruction of SPECT (right) and CT (left) images of aorta and inferior vena cava (IVC) demonstrating heterogeneous RP782 uptake along the aorta. C) MicroSPECT-derived quantification of RP782 uptake on serial 2 mm-segments of the aorta, starting at the level of aortic arch. n= 4, cpv: counts per voxel.
Fig. 3.
A) Example of RP782 autoradiography demonstrating heterogeneity of tracer uptake in atherosclerotic aorta of a mouse on high fat diet for 3 months. B) Autoradiography-derived quantification of RP782 uptake on serial 2 mm-segments of the aorta. n= 4 C) Correlation between microSPECT- and autoradiography-derived quantification of RP782 uptake on 2 mm aortic segments. ID: injected dose, cpv: counts per voxel.
Temporal pattern and specificity of RP782 uptake in the aorta
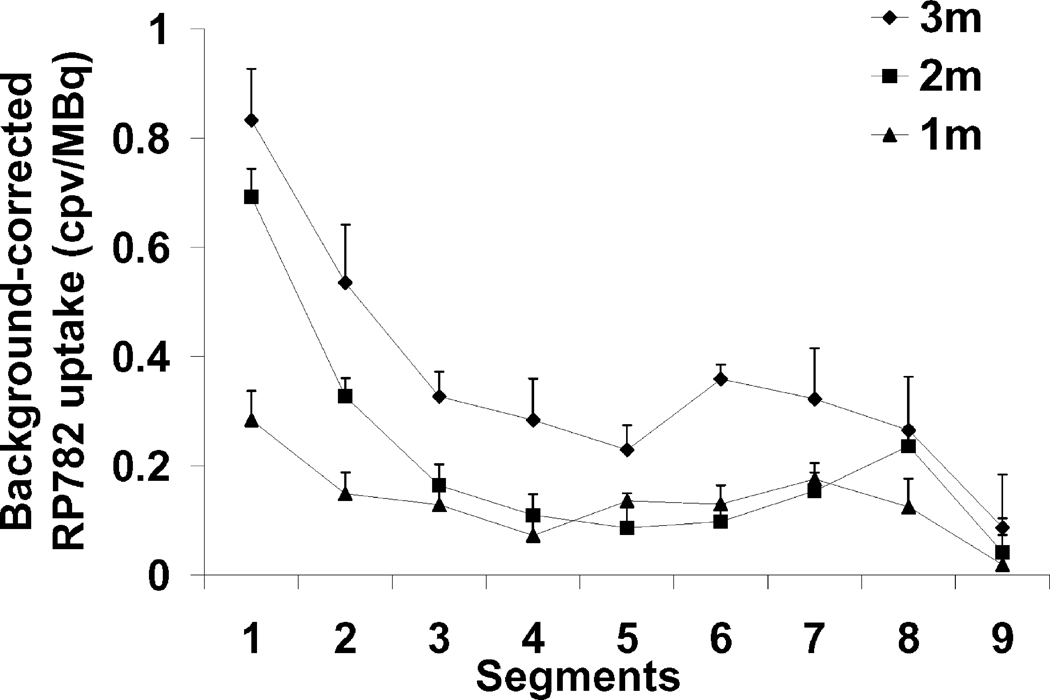
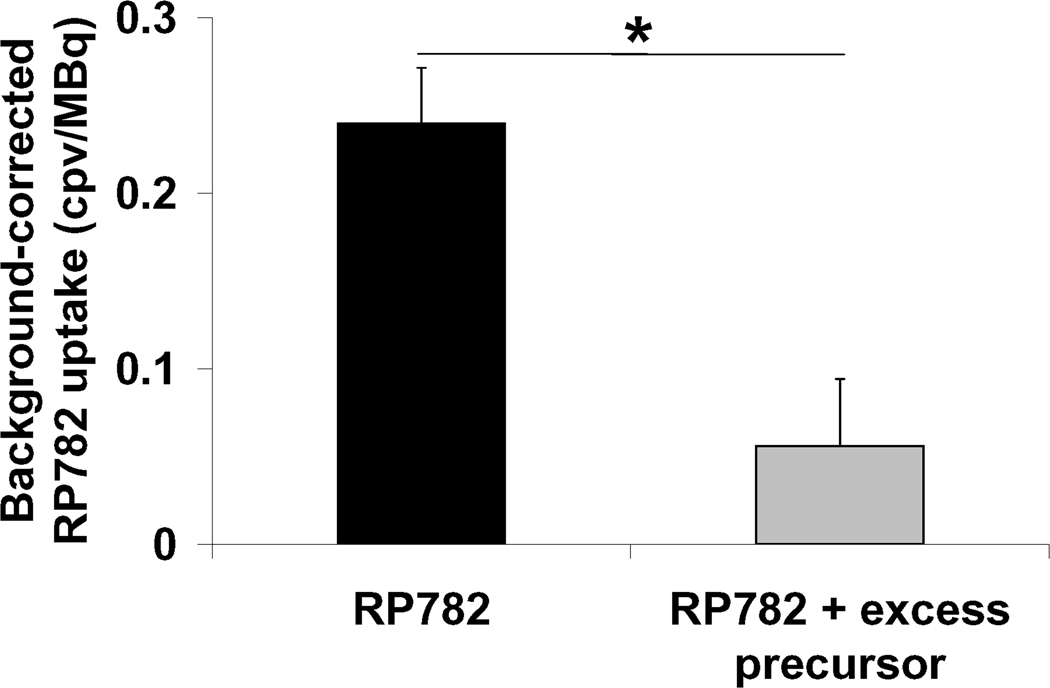
To investigate the temporal pattern of MMP activation in the aorta, additional groups of mice underwent RP782 microSPECT/CT imaging at 1 and 2 months after the initiation of the high fat diet. RP782 uptake along the aorta gradually increased over time with the mean uptake increasing from 0.13±0.02 cpv/MBq injected after one month (n=8) to 0.21±0.03 cpv/MBq after 2 months (n=8) and 0.36±0.05 cpv/MBq (n=4) after 3 months of high fat diet (p<0.01 between 1 month and three months, Figure 4 and Supplemental Figure 3). RP782 uptake heterogeneity along the aorta appeared more pronounced with progression of atherosclerosis over time. Tracer uptake specificity was demonstrated in a group of animals injected with 50-fold excess non-labeled precursor prior to RP782 administration which led to a significant reduction in RP782 uptake in the aorta (mean aortic arch uptake 0.24±0.03 cpv/MBq injected without precursor, n=8 vs 0.06±0.04 cpv/MBq with excess non-labeled precursor, n=2, p=0.02, Figure 5 and Supplemental Figure 4).
Fig. 4.
Temporal pattern of RP782 uptake in atherosclerotic aorta. MicroSPECT-derived quantification of RP782 uptake on serial 2 mm-segments of the aorta of mice fed a high fat diet for 1 (n=8), 2 (n=8) or 3 (n=4) months demonstrating gradual increase in tracer uptake over time.
Fig. 5.
RP782 uptake specificity in atherosclerosis. MicroSPECT derived quantification of RP782 signal in aortic arch in animals without or with injection with 50-fold excess unlabeled precursor prior to tracer administration. *: p=0.02.
Effect of dietary intervention on MMP activation and cellular composition of atherosclerotic aorta
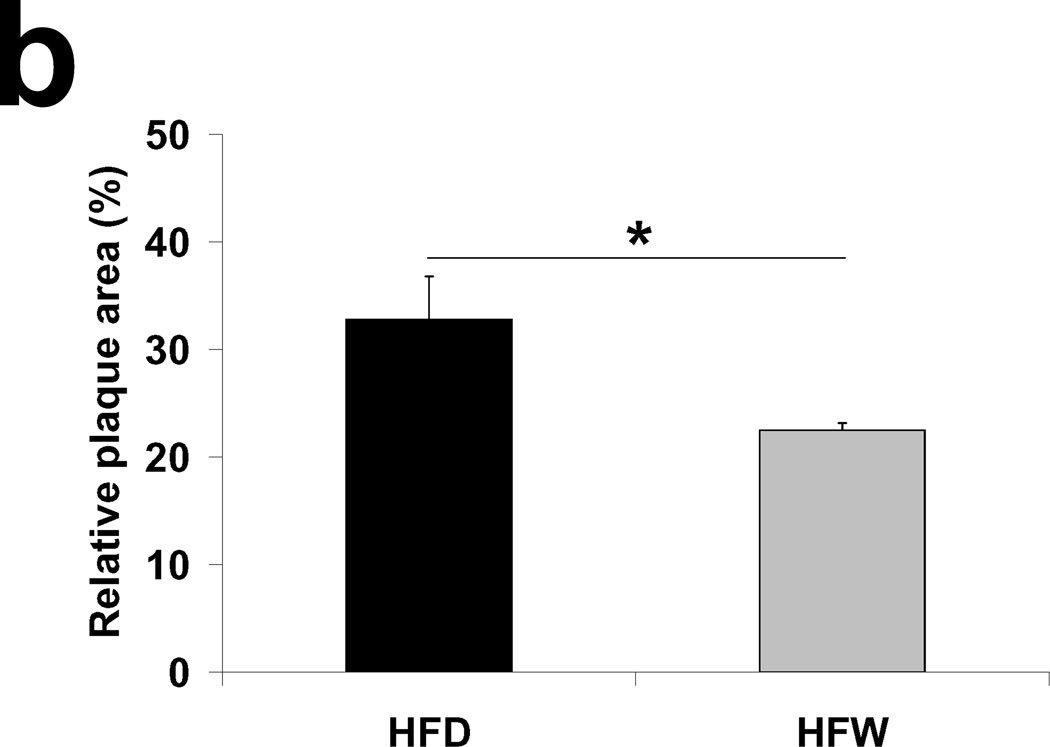
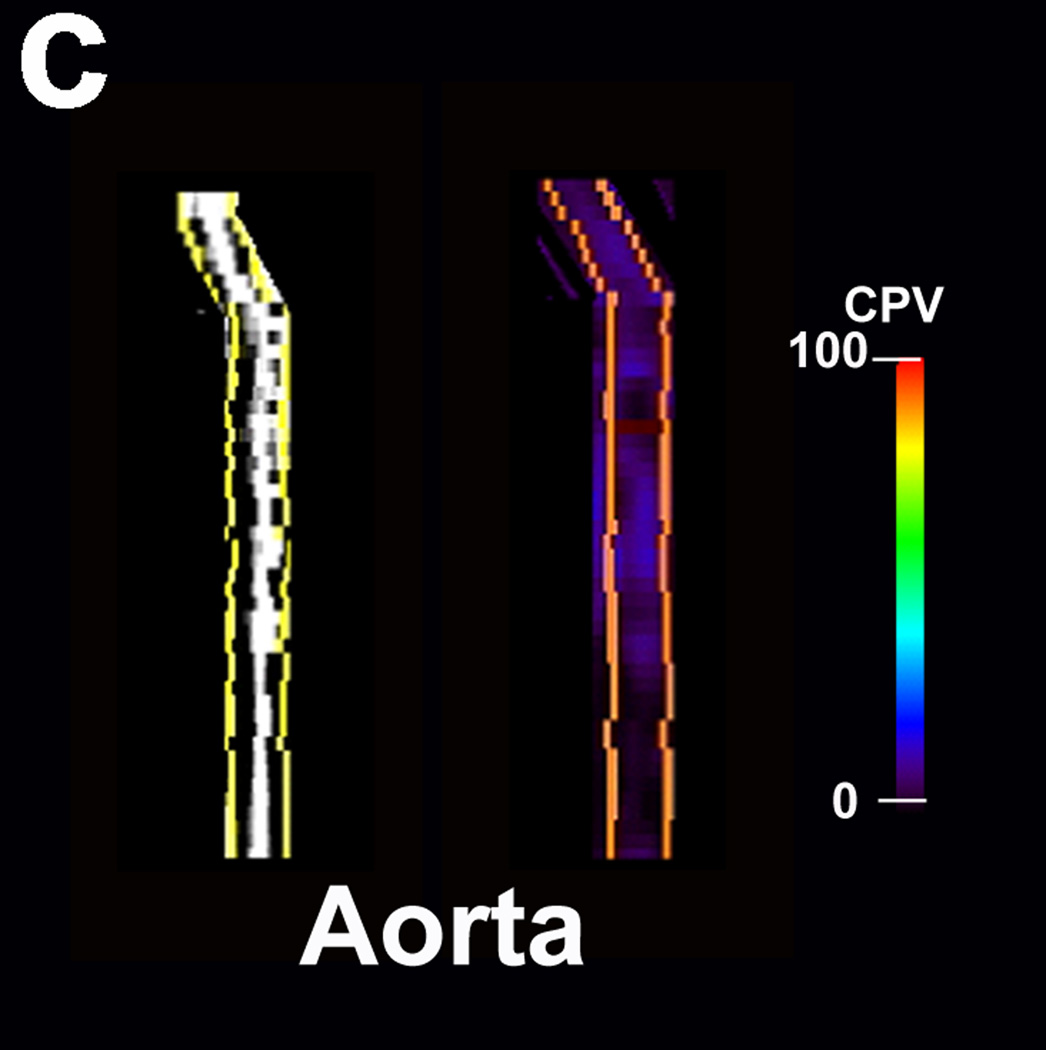
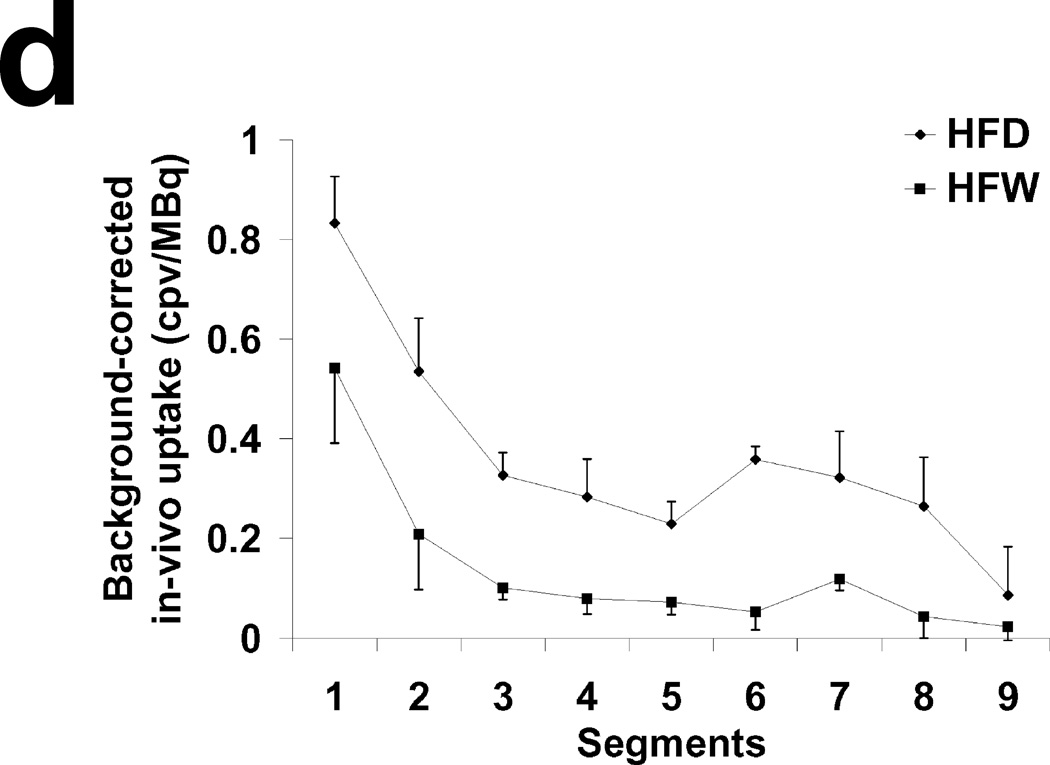
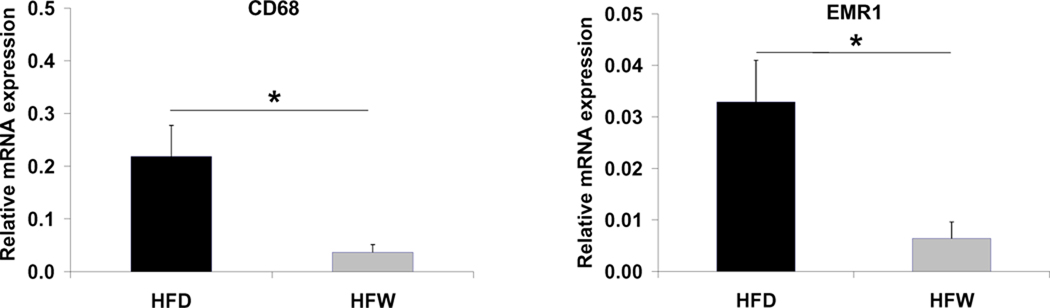
Therapeutic interventions aimed at reducing vascular risk may be associated with a reduction in MMP activity in the vessel wall. To address the effect of dietary intervention on MMP activation in atherosclerosis, animals were placed on normal chow after two months of high fat diet. Withdrawal from the high fat diet for one month led to a ~30% reduction in the relative plaque area detected by Oil Red O staining compared to animals kept on high fat diet for three months (22.5±0.7% in the withdrawal group versus 32.8±4.0% in the high fat diet group, n=3 in each group, p=0.01) (Fig. 6A&B). A significant (and considerably more pronounced) reduction in aortic MMP activation was detected by RP782 imaging in the withdrawal group (mean aortic uptake 0.14±0.05 cpv/MBq injected in the withdrawal group versus 0.36±0.05 cpv/MBq in the high fat diet group, n=4, p=0.02, Figure 6C&D and Supplemental Figure 5). However, dietary intervention did not appear to alter the heterogeneity of MMP activation along the aorta. Importantly, while the withdrawal of the high fat diet had no effect on aortic CD31 [endothelial cell (EC) marker] and SM α-actin [vascular smooth muscle cell (VSMC) marker] mRNA expression (Supplemental Figure 6), it significantly reduced aortic CD68 and EMR-1 expression, reflecting a reduction in vessel wall macrophage infiltration following dietary intervention (p<0.05, Fig 7).
Fig. 6.
A) Representative example of Oil Red O staining of the aorta of an apoE−/− mouse fed high fat diet for 2 months followed by normal chow for one month. Scale bar: 2mm. B) Relative plaque area detected by Oil Red O staining of aortae of animals fed high fat diet for 3 months (HFD) or high fat diet for 2 months followed by 1 month of normal chow (HFW). n=3 in each group. *: p=0.01. C) Representative examples of multiplanar reconstruction of SPECT (left) and CT (right) images of aorta in the HFW group. D) MicroSPECT-derived quantification of RP782 uptake in HFD and HFW animals. n=4 in each group. cpv: counts per voxel.
Fig. 7.
GAPDH-normalized CD68 and EMR-1 mRNA expression detected by real time RT-PCR in the aortae of animals fed a high fat diet for 3 months (HFD) or high fat diet for 2 months followed by 1 month of normal chow (HFW). n=3 in each group, *: p<0.05.
Biological correlates of the heterogeneity of RP782 uptake in atherosclerotic aorta
To identify the biological correlates of RP782 uptake, MMP expression and cellular composition of the vessel wall was assessed in 4 segments at regular intervals along the aorta. Similar to imaging data, there was considerable regional variation in the expression of most members of the MMP family studied (with the notable exception of MMP-9) which paralleled and significantly correlated with MMP activation in the same segments detected by microSPECT imaging (Supplemental Figure 7 and table 1). Dietary intervention led to a significant reduction in MMP-2, MMP-3, MMP-12 and MMP-13 (but not MMP-9) mRNA expression in the proximal aorta (Supplemental Figure 7). A number of vascular cells, including ECs, VSMCs and monocyte-macrophages can produce MMPs and contribute to MMP proteolytic activity in the aorta. While we found no significant correlation between CD31 (EC) or SM α-actin (VSMC) expression and RP782 uptake, CD68 expression (reflecting the presence of macrophages) significantly correlated with MMP activation detected by in vivo imaging (r=0.65, p=0.04, Table 1).
Table 1.
Correlation between RP782 uptake in-vivo and mRNA expression level in serial 4 mm-segments of the aorta of animals fed high fat diet for 3 months or high fat diet for 2 months followed by 1 month of normal chow. NS: not-significant
| r | P | |
|---|---|---|
| MMP-2 | 0.7 | 0.03 |
| MMP-3 | 0.81 | 0.008 |
| MMP-9 | 0.18 | NS |
| MMP-12 | 0.66 | 0.04 |
| MMP-13 | 0.9 | 0.003 |
| CD68 | 0.65 | 0.04 |
| α-actin | 0.58 | NS |
Discussion
Molecular imaging is emerging as a potentially powerful tool for in vivo quantitative assessment of vessel wall biology in atherosclerosis (3,4). Despite differences with human pathology, murine models are important experimental tools for preclinical studies of atherosclerosis. However, the small size of the mouse raises a number of technical challenges that hamper access to full potential of molecular imaging in this species. To circumvent this problem, radionuclide-based molecular imaging studies of atherosclerosis in murine models have relied on ex vivo measurements to obtain quantitative data on plaque biology, including local MMP activity (5,7,14–16). Here, we expand the scope of previous studies to image, and quantify in vivo MMP activation in murine atherosclerosis by microSPECT/CT imaging. Considerable heterogeneity of MMP activation along atherosclerotic mouse aorta was demonstrated by in vivo imaging which correlated well with the presence of macrophages. Investigating the effect of dietary intervention on MMP activation and its heterogeneity in atherosclerosis we detected changes in vessel wall biology which extend beyond the expected effect on plaque development.
MMPs are a large family of specialized endopeptidases specific for extracellular matrix and other proteins (17). Their enzymatic activity is dependent on the expression level, activation state and presence of inhibitors. MMPs play a key role in the development atherosclerosis and its complications through remodeling of extracellular matrix and activation of cytokines, chemokines and growth factors. ECs, VSMCs, and inflammatory cells, including monocyte-macrophages are the main sources of MMP activity in the vessel wall (17). The critical role of MMPs in the pathogenesis of atherosclerosis is supported by several lines of evidence, including observations in MMP knock out and transgenic mice (17). For example, atherogenesis is reduced in MMP-2 deficient apoE−/− mice (18) while deletion of MMP-9 appears to have an opposite effect, promoting plaque development (19). In addition to their role in development of atherosclerosis, MMPs modulate plaque stability through regulation of extracellular matrix protein deposition and degradation, VSMC proliferation, and inflammation (17,20,21). In apoE/MMP-12 double knockout mice, brachiocephalic artery atherosclerotic lesions show increased VSMC and reduced macrophage content compared to controls, features associated with plaque stability (19). Similarly, VSMC content is increased in apoE/MMP-7 double knockout mice, while knocking down MMP-3 or MMP-9 confers features of plaque instability (19).
MMP-targeted imaging appears as a promising approach to atherosclerotic plaque characterization for identifying high risk features. A number of studies have demonstrated the feasibility of imaging MMPs (and other relevant targets) using various imaging modalities in animal models of atherosclerosis (5,8,15,22,23). The high sensitivity of nuclear imaging (PET, SPECT) and its applicability to human studies make it an especially promising approach for studies of vessel wall biology in vivo. To acquire quantitative information on MMP activation pattern in atherosclerosis, we used RP782, an 111In-labeled tracer with specificity for MMP activation epitope (11), to image MMP activation along the aorta in atherosclerotic apoE−/− mice. The use of 111In-labeled RP782, rather than a 99mTc-labeled homologue, allowed us to analyze the samples by relatively high quality autoradiography. MicroSPECT imaging was combined with CT angiography to localize major blood vessels with accuracy. Despite potential confounding factors, including partial volume effect and scatter from adjacent structures, we found a strong correlation between in vivo and ex vivo measurements of RP782 uptake along the aorta, validating our approach to in vivo quantification. Comparison of ex vivo and in vivo quantification indicates overcorrection of the background activity on in vivo images. This may be explained by our choice of the area anterior to thoracic aorta, which probably has some degree of specific tracer uptake, to calculate the background activity.
In vivo images showed considerable heterogeneity of MMP activation along the aorta which was confirmed by autoradiography. In general, aortic segments with prominent atherosclerotic lesions were found to have high levels of RP782 uptake. However, there were areas with discordance between the presence of atherosclerotic plaque and MMP tracer uptake. A similar heterogeneity of plaque distribution, biology and composition has been observed in animal (7,24) and human (25–27) studies of atherosclerosis. In rabbit atherosclerosis, plaque temperature heterogeneity detected by thermography has been linked to macrophage content and MMP-9 activity (24). In our study, in addition to heterogeneity of MMP expression and activation along the aorta, we detected considerable heterogeneity of MMP activity and expression in adjacent 100 µm-segments of atherosclerotic aorta with comparable histology (data not shown). This heterogeneity of MMP expression is also present in human carotid atherectomy samples and has been attributed to lesion location, size and composition (28). The potential sampling errors caused by this remarkable heterogeneity of MMP expression in atherosclerosis highlights the importance of more global in vivo assessment of MMP activity which can be achieved by molecular imaging (29). Interestingly, withdrawal of the high fat diet in our study led to a significant reduction in MMP activation in the aorta. However, the heterogeneity of MMP activation along the aorta persisted in the withdrawal group. The relevance of this observation to human coronary artery disease and its potential clinical implications remains to be determined.
Plaque heterogeneity also indicates that immunostaining of random histological sections is not a reliable approach to quantification of protein expression or cell infiltration in atherosclerosis. Therefore, to identify correlates of tracer uptake in vivo, we quantified MMP expression and cellular content of aortic segments by real time RT-PCR. Expression of several MMPs, with the notable exception of MMP-9, correlated well with tracer uptake in atherosclerotic aorta, highlighting the concerted changes of MMP expression in atherosclerosis. Of note, the exact role of MMP-9 in atherosclerosis remains controversial (19,30–32), and further studies to address these discrepancies are warranted. Plaque composition, e.g., the presence of macrophages, is a key determinant of its propensity to rupture (1,33). While we did not detect any significant correlation between tracer uptake and CD31 or smooth muscle α-actin expression, MMP activation detected by molecular imaging correlated well with CD68, a macrophage marker, expression. Withdrawal from high fat diet led to a significant reduction in aortic macrophage, but not EC or VSMC content in parallel with the significant reduction in RP782 uptake. Importantly, the reduction in MMP tracer uptake (as well as macrophage markers) extended beyond the modest reduction in aortic plaque area, indicating the presence of a more “stable” phenotype in the withdrawal group.
Conclusion
In vivo imaging and quantification of MMP activation in atherosclerosis provides an opportunity to characterize atherosclerotic lesions in vivo and track the effect of therapeutic interventions on plaque biology. It remains to be determined whether differences in MMP tracer uptake can predict differences in the outcome between different patient populations. If validated as such, MMP targeted imaging could have a major impact on risk stratification and tracking the effect of therapeutic interventions in atherosclerotic diseases.
Supplementary Material
Acknowledgments
Funding Sources
This work was supported by National Institutes of Health R01 HL85093, Program Project HL-70295, and a Department of Veterans Affairs Merit Award to Mehran M. Sadeghi.
Footnotes
Disclosures:
Simon Robinson and Michael Azure are employees of Lantheus Medical Imaging. Albert Sinusas and Mehran Sadeghi receive experimental tracers from Lantheus Medical Imaging. In addition, Albert Sinusas has received research grants from Lantheus Medical Imaging.
References
- 1.Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005 Apr 21;352(16):1685–1695. doi: 10.1056/NEJMra043430. [DOI] [PubMed] [Google Scholar]
- 2.Virmani R, Burke AP, Farb A, Kolodgie FD. Pathology of the vulnerable plaque. J Am Coll Cardiol. 2006 Apr 18;47(8 Suppl):C13–C18. doi: 10.1016/j.jacc.2005.10.065. [DOI] [PubMed] [Google Scholar]
- 3.Nahrendorf M, Sosnovik DE, French BA, et al. Multimodality Cardiovascular Molecular Imaging, Part II. Circ Cardiovasc Imaging. 2009 January 1;2(1):56–70. doi: 10.1161/CIRCIMAGING.108.839092. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sadeghi MM, Glover DK, Lanza GM, Fayad ZA, Johnson LL. Imaging atherosclerosis and vulnerable plaque. J Nucl Med. 2010 May 1;(51 Suppl 1):51S–65S. doi: 10.2967/jnumed.109.068163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fujimoto S, Hartung D, Ohshima S, et al. Molecular imaging of matrix metalloproteinase in atherosclerotic lesions: resolution with dietary modification and statin therapy. J Am Coll Cardiol. 2008 Dec 2;52(23):1847–1857. doi: 10.1016/j.jacc.2008.08.048. [DOI] [PubMed] [Google Scholar]
- 6.Winter PM, Morawski AM, Caruthers SD, et al. Molecular imaging of angiogenesis in early-stage atherosclerosis with alpha(v)beta3-integrin-targeted nanoparticles. Circulation. 2003 Nov 4;108(18):2270–2274. doi: 10.1161/01.CIR.0000093185.16083.95. [DOI] [PubMed] [Google Scholar]
- 7.Ishino S, Kuge Y, Takai N, et al. 99mTc-Annexin A5 for noninvasive characterization of atherosclerotic lesions: imaging and histological studies in myocardial infarction-prone Watanabe heritable hyperlipidemic rabbits. Eur J Nucl Med Mol Imaging. 2007 Jun;34(6):889–899. doi: 10.1007/s00259-006-0289-x. [DOI] [PubMed] [Google Scholar]
- 8.Lancelot E, Amirbekian V, Brigger I, et al. Evaluation of matrix metalloproteinases in atherosclerosis using a novel noninvasive imaging approach. Arterioscler Thromb Vasc Biol. 2008 Mar;28(3):425–432. doi: 10.1161/ATVBAHA.107.149666. [DOI] [PubMed] [Google Scholar]
- 9.Kaufmann BA, Carr CL, Belcik JT, et al. Molecular imaging of the initial inflammatory response in atherosclerosis: implications for early detection of disease. Arterioscler Thromb Vasc Biol. 2010 Jan;30(1):54–59. doi: 10.1161/ATVBAHA.109.196386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nahrendorf M, Waterman P, Thurber G, et al. Hybrid in vivo FMT-CT imaging of protease activity in atherosclerosis with customized nanosensors. Arterioscler Thromb Vasc Biol. 2009 Oct;29(10):1444–1451. doi: 10.1161/ATVBAHA.109.193086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Su H, Spinale FG, Dobrucki LW, et al. Noninvasive targeted imaging of matrix metalloproteinase activation in a murine model of postinfarction remodeling. Circulation. 2005 Nov 15;112(20):3157–3167. doi: 10.1161/CIRCULATIONAHA.105.583021. [DOI] [PubMed] [Google Scholar]
- 12.Zhang J, Nie L, Razavian M, et al. Molecular imaging of activated matrix metalloproteinases in vascular remodeling. Circulation. 2008 Nov 4;118(19):1953–1960. doi: 10.1161/CIRCULATIONAHA.108.789743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sadeghi MM, Krassilnikova S, Zhang J, et al. Detection of injury-induced vascular remodeling by targeting activated alphavbeta3 integrin in vivo. Circulation. 2004 Jul 6;110(1):84–90. doi: 10.1161/01.CIR.0000133319.84326.70. [DOI] [PubMed] [Google Scholar]
- 14.Hartung D, Petrov A, Haider N, et al. Radiolabeled Monocyte Chemotactic Protein 1 for the detection of inflammation in experimental atherosclerosis. J Nucl Med. 2007 Nov;48(11):1816–1821. doi: 10.2967/jnumed.107.043463. [DOI] [PubMed] [Google Scholar]
- 15.Ohshima S, Petrov A, Fujimoto S, et al. Molecular imaging of matrix metalloproteinase expression in atherosclerotic plaques of mice deficient in apolipoprotein e or low-density-lipoprotein receptor. J Nucl Med. 2009 Apr;50(4):612–617. doi: 10.2967/jnumed.108.055889. [DOI] [PubMed] [Google Scholar]
- 16.Laitinen I, Marjamaki P, Nagren K, et al. Uptake of inflammatory cell marker [11C]PK11195 into mouse atherosclerotic plaques. Eur J Nucl Med Mol Imaging. 2009 Jan;36(1):73–80. doi: 10.1007/s00259-008-0919-6. [DOI] [PubMed] [Google Scholar]
- 17.Galis ZS, Khatri JJ. Matrix metalloproteinases in vascular remodeling and atherogenesis: the good, the bad, and the ugly. Circ Res. 2002 Feb 22;90(3):251–262. [PubMed] [Google Scholar]
- 18.Kuzuya M, Nakamura K, Sasaki T, Cheng XW, Itohara S, Iguchi A. Effect of MMP-2 deficiency on atherosclerotic lesion formation in apoE-deficient mice. Arterioscler Thromb Vasc Biol. 2006 May;26(5):1120–1125. doi: 10.1161/01.ATV.0000218496.60097.e0. [DOI] [PubMed] [Google Scholar]
- 19.Johnson JL, George SJ, Newby AC, Jackson CL. Divergent effects of matrix metalloproteinases 3, 7, 9, and 12 on atherosclerotic plaque stability in mouse brachiocephalic arteries. Proc Natl Acad Sci U S A. 2005 Oct 25;102(43):15575–15580. doi: 10.1073/pnas.0506201102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dollery CM, Libby P. Atherosclerosis and proteinase activation. Cardiovasc Res. 2006 Feb 15;69(3):625–635. doi: 10.1016/j.cardiores.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 21.Newby AC. Dual role of matrix metalloproteinases (matrixins) in intimal thickening and atherosclerotic plaque rupture. Physiol Rev. 2005 Jan;85(1):1–31. doi: 10.1152/physrev.00048.2003. [DOI] [PubMed] [Google Scholar]
- 22.Amirbekian V, Aguinaldo JG, Amirbekian S, et al. Atherosclerosis and matrix metalloproteinases: experimental molecular MR imaging in vivo. Radiology. 2009 May;251(2):429–438. doi: 10.1148/radiol.2511080539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ohshima S, Fujimoto S, Petrov A, et al. Effect of an antimicrobial agent on atherosclerotic plaques: assessment of metalloproteinase activity by molecular imaging. J Am Coll Cardiol. Mar 23;55(12):1240–1249. doi: 10.1016/j.jacc.2009.11.056. [DOI] [PubMed] [Google Scholar]
- 24.Krams R, Verheye S, van Damme LC, et al. In vivo temperature heterogeneity is associated with plaque regions of increased MMP-9 activity. Eur Heart J. 2005 Oct;26(20):2200–2205. doi: 10.1093/eurheartj/ehi461. [DOI] [PubMed] [Google Scholar]
- 25.Verheye S, De Meyer GR, Van Langenhove G, Knaapen MW, Kockx MM. In vivo temperature heterogeneity of atherosclerotic plaques is determined by plaque composition. Circulation. 2002 Apr 2;105(13):1596–1601. doi: 10.1161/01.cir.0000012527.94843.bf. [DOI] [PubMed] [Google Scholar]
- 26.Stefanadis C, Diamantopoulos L, Vlachopoulos C, et al. Thermal heterogeneity within human atherosclerotic coronary arteries detected in vivo: A new method of detection by application of a special thermography catheter. Circulation. 1999 Apr 20;99(15):1965–1971. doi: 10.1161/01.cir.99.15.1965. [DOI] [PubMed] [Google Scholar]
- 27.Naghavi M, John R, Naguib S, et al. pH Heterogeneity of human and rabbit atherosclerotic plaques; a new insight into detection of vulnerable plaque. Atherosclerosis. 2002 Sep;164(1):27–35. doi: 10.1016/s0021-9150(02)00018-7. [DOI] [PubMed] [Google Scholar]
- 28.Choudhary S, Higgins CL, Chen IY, et al. Quantitation and localization of matrix metalloproteinases and their inhibitors in human carotid endarterectomy tissues. Arterioscler Thromb Vasc Biol. 2006 Oct;26(10):2351–2358. doi: 10.1161/01.ATV.0000239461.87113.0b. [DOI] [PubMed] [Google Scholar]
- 29.Libby P. Perplexity of plaque proteinases. Arterioscler Thromb Vasc Biol. 2006 Oct;26(10):2181–2182. doi: 10.1161/01.ATV.0000240249.88921.d8. [DOI] [PubMed] [Google Scholar]
- 30.Cho A, Reidy MA. Matrix metalloproteinase-9 is necessary for the regulation of smooth muscle cell replication and migration after arterial injury. Circ Res. 2002 Nov 1;91(9):845–851. doi: 10.1161/01.res.0000040420.17366.2e. [DOI] [PubMed] [Google Scholar]
- 31.Johnson C, Galis ZS. Matrix metalloproteinase-2 and -9 differentially regulate smooth muscle cell migration and cell-mediated collagen organization. Arterioscler Thromb Vasc Biol. 2004 Jan;24(1):54–60. doi: 10.1161/01.ATV.0000100402.69997.C3. [DOI] [PubMed] [Google Scholar]
- 32.Gong Y, Hart E, Shchurin A, Hoover-Plow J. Inflammatory macrophage migration requires MMP-9 activation by plasminogen in mice. J Clin Invest. 2008 Sep;118(9):3012–3024. doi: 10.1172/JCI32750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Libby P. Inflammation in atherosclerosis. Nature. 2002 Dec 19–26;420(6917):868–874. doi: 10.1038/nature01323. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.