Abstract
Prostaglandin (PG)D2 is a key mediator of allergic inflammatory diseases that is mainly synthesized by mast cells, which constitutively express high levels of the terminal enzyme involved in PGD2 synthesis, the hematopoietic PGD synthase (H-PGDS). Here, we investigated whether eosinophils are also able to synthesize, and therefore, supply biologically active PGD2. PGD2 synthesis was evaluated within human blood eosinophils, in vitro-differentiated mouse eosinophils, and eosinophils infiltrating inflammatory site of mouse allergic reaction. Biological function of eosinophil-derived PGD2 was studied by employing inhibitors of synthesis and activity.
Constitutive expression of H-PGDS was found within non-stimulated human circulating eosinophils. Acute stimulation of human eosinophils with A23187 (0.1 – 5 μM) evoked PGD2 synthesis, which was located at the nuclear envelope and was inhibited by pre-treatment with HQL-79 (10 μM), a specific H-PGDS inhibitor. Pre-stimulation of human eosinophils with arachidonic acid (AA; 10 μM) or human eotaxin (6 nM) also enhanced HQL-79-sensitive PGD2 synthesis, which, by acting on membrane-expressed specific receptors (DP1 and DP2), displayed an autocrine/paracrine ability to trigger leukotriene (LT)C4 synthesis and lipid body biogenesis, hallmark events of eosinophil activation. In vitro-differentiated mouse eosinophils also synthesized paracrine/autocrine active PGD2 in response to AA stimulation. In vivo, at late time point of the allergic reaction, infiltrating eosinophils found at the inflammatory site appeared as an auxiliary PGD2-synthesizing cell population.
Our findings reveal that eosinophils are indeed able to synthesize and secrete PGD2, hence representing during allergic inflammation an extra cell source of PGD2, which functions as an autocrine signal for eosinophil activation.
Keywords: PGD2, eosinophils, mast cells, cysteinyl leukotrienes, allergy, lipid droplets, CCL11
Introduction
Mast cells and eosinophils, two of the principal effector cell types activated at the sites of allergic inflammation, are major participants in the pathogenesis of asthma and other forms of allergic disorders (1,2). Mast cells and eosinophils have the potential to generate and release diverse lipid mediators that are critical to the development and perpetuation of allergic inflammation, including prostaglandins and leukotrienes derived from the oxidative metabolism of arachidonic acid (AA). Both mast cells and eosinophils express the sole leukotriene (LT)C4-synthesizing enzyme, named LTC4 synthase (LTC4S) and are major cell sources of cysteinyl leukotrienes (cysLTs). LTC4 and its extracellular derivatives, LTD4 and LTE4, have many well-recognized functions as mediators of the allergic response, causing bronchoconstriction, mucous hypersecretion, increased microvascular permeability, bronchial hyperresponsiveness, and eosinophil infiltration and activation (3,4). Different from LTC4-synthesizing capabilities, specific prostanoids produced by mast cells and eosinophils appear to differ according to their differential expression of prostanoid-synthesizing terminal isoenzymes (5,6). Concerning prostanoids with allergy-relevant functions, mast cells are considered the predominant cellular domain of hematopoietic prostaglandin (PG)D2 synthase (H-PGDS) among resident and recruited cells in allergic inflammatory tissues (7); PGD2 is also the major prostanoid produced by mast cells (8). Indeed, PGD2 and its metabolites have been proposed to be selective markers for mast cell activation in vivo (9–11). But recently, the dogma that mast cells are the single PGD2 source in allergic inflammatory conditions has been challenged. New findings unveiled that although PGD2 synthesis seems to be primarily controlled by allergy-relevant cells, it is not restricted to mast cells. Among these additional PGD2-synthesizing cellular sources are: (i) both direct and indirect endothelium-mediated generation of PGD2 (12,13); (ii) Th2 lymphocytes capability of synthesizing small, yet significant, amounts of PGD2 (14); (iii) skin dendritic cells as supplier of PGD2 with roles in skin inflammation (15); (iv) host defense-related PGD2 synthesis by activated macrophages (16,17); and (v) basophil-driven PGD2 release (18). What about eosinophils? Among prostanoids, it is well accepted that eosinophils are producers of the putative mediators, thromboxane A2 and PGE2, rather than mediators of allergic reactions. It is presumed that the lack of PGD2-synthesizing capability by eosinophils relies on anecdotal evidence of no H-PGDS expression within eosinophils. Nevertheless, while some indications of PGD2-synthesizing activity may exist (19–21), definitive demonstration that eosinophils can generate PGD2 is still lacking.
Understanding the mechanisms governing PGD2 synthesis, including the identification of specific PGD2 -producing cells, is important as PGD2 has emerged as a key mediator of the pathogenesis of allergic diseases. PGD2 recruits and activates eosinophils, as well as basophils and Th2 lymphocytes (22–24). In vivo, PGD2 administration in human volunteers or animals imitates a variety of allergic features (25,26). PGD2 effects are mediated by the activation of the two known PGD2 receptors, namely D prostanoid receptor 1 (DP1) and DP2 (also known as CRTH2) (22,27–29). Eosinophils co-express both the classic DP1 receptors coupled to adenylyl cyclase, as well as, pertussis toxin (PTX)-sensitive DP2 (23). It has been shown that PGD2 ability to activate eosinophils may be determined by a balance between these DP1- versus DP2-driven opposing downstream signaling pathways (e.g. PGD2-induced eosinophil chemotaxis) (23,30,31), but alternatively may well be dependent on an initially unexpected DP1/DP2 cooperative effect (e.g. PGD2-elicited enhanced LTC4 synthesis by eosinophils) (32). The appeal of PGD2 as a therapeutic target in allergic diseases, such as asthma, can be promptly attested by the rapid development of selective pharmacological tools to examine the pro-allergic contributions of these two receptors. Of note, since a variety of prostanoid molecules, including PGD2 metabolites, PGF2 and 11-dehydro-TBX2 are capable to activate DP2 (22,33–38), one can hypothesize physiopathological outcomes of activation of PGD2 receptors even in the absence of PGD2 production. However, the concentrations of PGD2 are indeed elevated in a variety of chronic allergic tissues, including in the nasal mucosa of allergic rhinitis (39), the airways of asthmatics (40,41), and the skin of patients with atopic dermatitis (42). Although in these conditions, PGD2 synthesis is portrayed as a predominantly mast cell-derived product (41), little is known about the alternative and complementary cell sources of PGD2.
Our study reports that, upon proper stimulation, both human and mouse eosinophils can produce significant amounts of biologically relevant PGD2. PGD2 intracellular synthesis within eosinophils was catalyzed by eosinophil-expressed H-PGDS and led to PGD2 receptor-mediated paracrine/autocrine functions, contributing to eosinophil activation.
Material and Methods
Animals
Swiss and BALB/c mice of 16–20 g from both sexes were used. The animals were obtained from the Oswaldo Cruz Foundation breeding unit (Rio de Janeiro, Brazil). The protocols were approved by the Oswaldo Cruz Foundation Animal Welfare Committee.
Allergic pleurisy in sensitized mice
As previously described (43), mice were sensitized with a subcutaneous injection (0.2 mL) of ovalbumin (OVA; 50 μg) and Al(OH)3 (5 mg) in a 0.9% NaCl solution (saline) at days 1 and 7. Allergic challenge was performed at day 14 by means of an intrapleural (i.pl.) injection of OVA (12 μg/cavity; 0.1 mL). Control animals received vehicle (saline; 0.1 mL). The mice were euthanized by CO2 inhalation 48 h after challenge. The pleural cavities were rinsed with 500 μL of Ca2+/Mg2+free HBSS; pH 7.4 (HBSS−/−).
Pleural eosinophil counts
Total leukocyte counts were performed using a Neubauer chamber under an optical microscope, after dilution with Turk fluid (2% acetic acid). Differential counts of mononuclear cells, neutrophils, and eosinophils were performed under an oil immersion objective using cytopins (Cytospin 3; Shandon Inc., Pittsburgh, PA) stained by the May-Grunwald-Giemsa method. Counts are reported as eosinophils per cavity.
Isolation of human blood eosinophils
Peripheral blood was obtained with informed consent from normal donors. Briefly, following dextran sedimentation and Ficoll gradient steps, eosinophils were isolated from contaminating neutrophils by negative immunomagnetic selection using the EasySep™ system (StemCell Technologies Inc.), which includes antibodies against human CD2, CD3, CD14, CD16, CD19, CD20, CD36, CD56, CD123 and glycophorin A coupled to magnetic particles (cell purity ~ 99%; cell viability ~ 95%) (32). The protocol was approved by ethical review boards of both the Federal University of Rio de Janeiro and the Oswaldo Cruz Foundation (Rio de Janeiro, Brazil).
In vitro stimulation of human eosinophils
Purified human eosinophils at 2 × 106 cells/mL in Ca2+/Mg2+ HBSS (HBSS+/+; pH 7.4) were incubated with A23187 (0.1 – 5 μM; Sigma) for 15 min in a water bath (37 °C). Alternatively, eosinophils were stimulated with AA (10 μM; Cayman), human recombinant eotaxin (also known as CCL11 or eotaxin-1; 6 nM; R&D), macrophage migration inhibitory factor (MIF; 50 ng/mL; R&D), PAF (1 μM) or PGD2 (25 nM) in HBSS−/− for 1 h. To enable detection of released PGD2 or LTC4 by EIA, AA or eotaxin-stimulated eosinophils were also challenged with 0.1 μM A23187 (Sigma) for an additional 15 min in HBSS+/+. Each condition was repeated at least three times with eosinophils purified from different donors.
In vitro eosinophil differentiation from mouse bone marrow cells
With slight modifications, eosinophils were differentiated in vitro from mouse bone marrow cells as previously described (44). Briefly, bone marrow cells were collected from femurs and tibiae of wild-type BALB/c mice with RPMI 1640 (Sigma) containing 20% FBS. After RBC lysis, cells were cultured at 106 cells/mL in RPMI 1640 containing 20% FBS (VitroCell), 100 IU/ml penicillin, 10 μg/ml streptomycin, 2 mM glutamine (Sigma) and 1 mM sodium pyruvate (Sigma), 100 ng/mL stem cell factor (SCF; PeproTech) and 100 ng/mL FLT3 ligand (PeproTech) from days 0 to 4. On day 4, the SCF and FLT3-L were replaced with IL-5(10 ng/mL; Peprotech). On day 14, eosinophils were enumerated (purity ≥ 75%), resuspended in HBSS−/− (2 × 106 cells/mL) and stimulated with AA (10 μM; Cayman), rm eotaxin (6 nM), PAF (1 μM), or PGD2 (25 nM).
Treatments
For in vitro studies, human or mouse eosinophils in HBSS−/− were pre-treated for 30 min with the H-PGDS inhibitor HQL-79 (10 μM), DP1 receptor antagonist BWA868c (200 nM), or CRTH2 receptor antagonists Bay-u3405 (200 nM) and Cay 10471 (200 nM), or concomitantly with antibodies against PGD2 (10 μL) (all from Cayman Chemicals) or its isotype control. Notably, pre-treatments did not modify the eosinophil basal lipid body content, nor did they affect eosinophil viability (~90%) (data not shown). For in vivo assays using the pleurisy model, animals were pre-treated with i.p. injections of HQL-79 (1 mg/Kg) 30 min before allergic challenge.
Stock solutions of stimuli and inhibitors were prepared in HBSS−/− containing 0.1% endotoxin-free ovalbumin, aliquoted, and stored at −20 °C. Specifically, concentration of HQL-79 stock solution was 5 mM in DMSO (DMSO final concentration during cell incubations was 0.02% and had no effect on eosinophils). A23187, BWA868c Bay-u3405 and Cay 10471 were also diluted in DMSO, while AA, PAF and PGD2 were diluted in ethanol. The final vehicle concentration was < 0.01% and had no effect on eosinophils.
H-PGDS immunolocalization
Human eosinophils (2 × 105 cells) were cytocentrifuged (500 rpm, 5 min) onto glass slides, and fixed in 2% paraformaldehyde for 10 min. After washing (3 × 10 min) with 0.05% saponin (Sigma) containing 1% BSA (Sigma) in HBSS−/−, the slides were incubated for 30 min with rabbit polyclonal antiserum anti-H-PGDS (Cayman) or with normal rabbit serum, washed with saponin/BSA, incubated for 30 min with Alexa Fluor 488-labeled goat anti-rabbit IgG antibody (Molecular Probes), washed with saponin, washed with HBSS−/−, and then an aqueous medium containing DAPI (Vector Laboratories). The images were obtained using an Olympus BX51 fluorescence microscope equipped with a Plan Apo 100× 1.4 Ph3 objective and an Olympus 72 digital camera (Olympus Optical CO., Japan) in conjunction with CellF Imaging Software for Life Science Microscopy (Olympus Life Science Europe GMBH). The images were edited using Adobe Photoshop 5.5 software (Adobe Systems).
Quantification of eicosanoids
PGD2, PGE2 or cysLTs found in cell-free pleural fluid and eosinophil supernatants were measured by commercial EIA kits, according to the manufacturer’s instructions (Cayman).
EicosaCell for intracellular PGD2 immuno-detection
By using EicosaCell (45) to detect intracellular PGD2 at its sites of synthesis, in vitro-stimulated eosinophils (in HBSS+/+) or pleural cells were mixed with an equal volume of EDAC solution (0.2% in HBSS−/− containing 1% BSA). After a 15 min incubation at 37oC with EDAC, eosinophils were washed with HBSS−/−, cytospun onto glass slides, incubated with HBSS−/− with 1% BSA for 30 min, and then incubated with rabbit anti-PGD2 antibodies (Assay Designs) overnight. Notably, PGD2 immuno-detection was also achieved when another anti-PGD2 antibody (Cayman) was employed (data not shown). The anti-ADRP (Adipose differentiation-related protein) antibody was also added overnight to distinguish cytoplasmic lipid bodies within eosinophils. The cells were washed with HBSS−/− containing 1% BSA (3x 10 min) and then incubated with DyLight488 anti-mouse IgG and DyLight549 anti-guinea pig secondary antibodies (Jackson) for 1 h. EicosaCell images were obtained using a LEICA TCS – SP5 confocal fluorescence microscope, equipped with a 63X objective in conjunction with LAS-AF 2.2.0 Software.
Alternatively, to detect PGD2-synthesizing eosinophils by flow cytometry, after incubation with EDAC, pleural fluid cells were washed with HBSS−/−, incubated overnight with rabbit anti-PGD2 antibodies, washed with HBSS−/−, and then incubated with DyLight488 anti-mouse IgG and antibody anti-SiglecF-PE (or isotype-PE) (from eBioscience) for 30 min. After washings, cells were analyzed by flow cytometry in a FACScalibur (BD) flow cytometer.
RT-PCR
mRNA was extracted from 106 non-stimulated or AA-stimulated human eosinophils according to the manufacturer’s protocol (RNeasy Kit, Qiagen, Germantown, MD). cDNA synthesis and RT-PCR conditions followed standard protocols. Primer sequences for human H-PGDS were the same as previously published (46) and for human β-actin were, 5′-GACAGGATGCAGAAGGAGAT-3′ and 5′-TGTGTGGACTTGGGAGAGGACT-3′ (based on GenBank sequence X00351).
Lipid body staining and enumeration
Cytospun cells, while still moist, were fixed in 3.7% formaldehyde (diluted in HBSS−/−), rinsed in 0.1 M cacodylate buffer (pH 7.4), stained with 1.5% OsO4 for 30 min, rinsed in distilled H2O, immersed in 1.0% thiocarbohydrazide for 5 min, rinsed in 0.1 M cacodylate buffer, restained with 1.5% OsO4 for 3 min, rinsed in distilled water, and then dried and mounted. The cell morphology was observed, and the lipid bodies were enumerated by light microscopy. Fifty consecutively scanned eosinophils were evaluated in a blinded fashion by more than one individual, and the results were expressed as the number of lipid bodies per eosinophil.
Statistical analysis
The results were expressed as mean ± SEM and were analyzed statistically by means of ANOVA followed by Student-Newman-Keuls test, with the level of significance set at P< 0.05.
Results
Human circulating eosinophils are enzymatically competent cells for prompt synthesis of PGD2
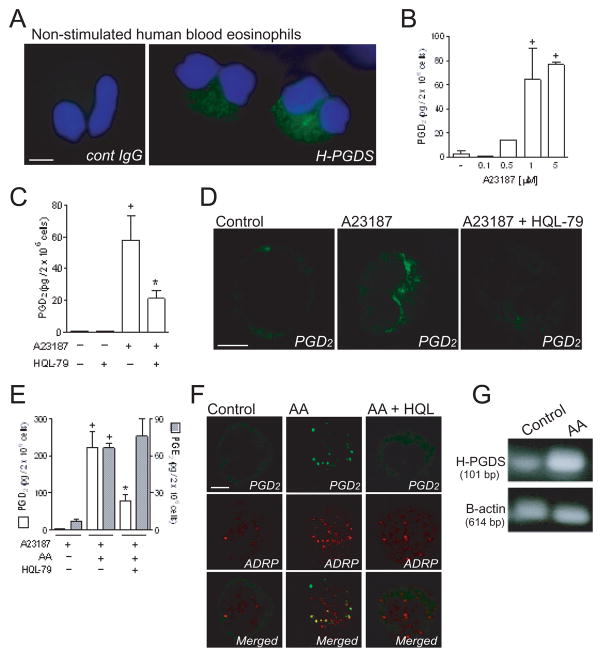
Analyses by fluorescence microscopy demonstrated that H-PGDS is constitutively expressed by human circulating eosinophils freshly isolated from healthy donors. As shown in Figure 1A, H-PGDS-labeling within non-stimulated human blood eosinophils displayed a cytoplasmic staining pattern. No immunoreactivity was detected within eosinophils incubated with control normal rabbit serum (Figure 1A). Thus, in addition to H-PGDS expression within activated human eosinophils, such as those recruited to nasal mucosa of patients with allergic rhinitis (21) or polyps of chronic rhinosinusitis patients (20), resting eosinophils also contained detectable amounts of cytoplasmic H-PGDS.
Figure 1. Human eosinophils are able to synthesize PGD2 in an H-PGDS-dependent manner.
Panel A presents epifluorescence images of cytoplasmic immuno-detection of H-PGDS (green) in non-stimulated human eosinophils. Blue fluorescence shows eosinophil nuclei stained with DAPI. Eosinophils incubated with isotype irrelevant IgG are shown. Panel B shows PGD2 amounts secreted by human eosinophils stimulated for 15 min with A23187 (0.1 to 5 μM). In C, eosinophils were pre-treated for 30 min with HQL-79 and then stimulated with 5 μM of A23187. Panel D displays confocal images of intracellular immuno-fluorescence for PGD2 in non-stimulated, A23187 (0.1 μM)-stimulated, and HQL-79-treated A23187-stimulated human eosinophils (as indicated). Arrows indicate PGD2 immuno-staining at the nuclear envelope of A23187-stimulated human eosinophils. Panel E shows production of PGD2 and PGE2 by human eosinophils stimulated for 1 h with AA (10 μM) and then challenged with A23187 (0.1 μM). Eosinophils were pre-treated for 30 min with HQL-79. In F, confocal images of EicosaCell preparations display intracellular immuno-detection of newly formed PGD2 (green) and of ADRP (red) in human eosinophils stimulated with AA (10 μM). Eosinophils were pre-treated with HQL-79 for 30 min. Overlay images of identical fields are shown in the larger images. In G, constitutive levels of H-PGDS mRNA and its up-regulation in human eosinophils that were stimulated for 1 h with AA (10 μM) were assessed by RT-PCR. Values are expressed as means ± SEM of at least three distinct donors. + P ≤ 0.05 compared with control. * P ≤ 0.05 compared with A23187- or AA-stimulated eosinophils. All the images are representative of three independent experiments with distinct donors. Bar, 5 μm.
It is now well recognized that merely the expression of eicosanoid-forming enzymes does not determine successful eicosanoid synthesis (for a review see (47)). To investigate whether eosinophil H-PGDS could couple to upstream prostanoid-synthesizing enzymes and mount an active PGD2-synthesizing machinery, human blood eosinophils were stimulated with calcium ionophore A23187. As shown in Figure 1B, A23187 dose-dependently (0.1 – 5μM) elicited acute (within 15 min) secretion of PGD2 from eosinophils. The pre-treatment with a selective inhibitor of H-PGDS, HQL-79 (10 μM), inhibited PGD2 synthesis/release induced by A23187 (5 μM) (Figure 1C), but failed to attenuate concomitant LTC4 secretion (not shown), therefore validating both PGD2 detection by EIA and the specificity of HQL-79 treatment, while evidencing that eosinophils can rapidly organize an effective H-PGDS-dependent PGD2 synthesis.
EicosaCell, an immuno-assay that immobilizes the newly formed eicosanoid at its intracellular synthesizing compartments (45), confirmed eosinophil’s ability to synthesize PGD2. As illustrated in Figure 1D, non-stimulated eosinophils exhibited no immunofluorescent staining for PGD2. In contrast, virtually all eosinophils (more than 90%) activated for 15 min with 0.1 μM A23187 yielded intense and localized immunofluorescent staining for PGD2 with a perinuclear localization, a well-established eicosanoid-forming site (Figure 1D). The specificity of EicosaCell staining for PGD2 was ascertained, since (i) there was no immunostaining when an isotype control antibody was used (not shown), and mainly (ii) HQL-79, which blocks H-PGDS activity, completely abolished PGD2 staining in A23187-stimulated eosinophils (Figure 1D). Although A23187-driven activation easily elicits the enzymatic pathways for eicosanoid production, it is supraphysiologic and may not depict physiopathologic mechanisms of PGD2 synthesis. Therefore, the unsaturated fatty acid AA, which functions as both substrate and physiologic stimulus of eicosanoid synthesis (48,49), was employed.
As illustrated in Figure 1E, AA (10 μM) very effectively primed eosinophils for increased PGD2 release in response to a submaximal, 0.1 μM concentration of A23187 (Figure 1E). AA-stimulated eosinophils released about 200 fold as much PGD2 as eosinophils challenged with 0.1 μM A23187 alone. Moreover, HQL-79 inhibited AA-primed PGD2 production by eosinophils, while failing to affect concurrent synthesis of PGE2 (Figure 1E). This inhibition confirmed the specificity of HQL-79 and reinforced H-PGDS role in AA-driven PGD2 synthesis by eosinophils. Moreover, it is not surprising that while the amounts of secreted PGD2 are not that different from those picograms of PGE2 found in the supernatant of AA-stimulated A23187-challenged eosinophils (Figure 1E), under same conditions eosinophils synthesize larger amounts (nanograms) of LTC4.
Although minute quantities of PGD2 produced by eosinophils stimulated only with AA was not sufficient to be detectable in supernatants by EIA (data not shown), it was intracellularly detected by EicosaCell. As shown in Figure 1F, AA (10 μM) was able to trigger within human eosinophils PGD2 synthesis which was immuno-detected within 30 min of stimulation. A detailed analysis revealed that part of newly synthesized PGD2 (green labeling) was in a punctate cytoplasmic pattern proximate to, but separate from, the nucleus and fully consistent in size and form with eosinophil lipid bodies. The specific compartmentalization of newly formed PGD2 within eosinophil lipid bodies was ascertained by the co-localization with ADRP, a protein marker of lipid bodies (Figure 1F, red labeling). Virtually no PGD2 immunolabeling was observed within non-stimulated eosinophils (Figure 1F), whereas about 91% of eosinophils stimulated with AA exhibited lipid body-localized staining for immunoreactive PGD2, which was fully inhibitable by HQL-79 (Figure 1F). Collectively these data evidences the role of H-PGDS in AA-induced PGD2 synthesis by eosinophils and ascertains the specificity of the PGD2 immuno-labeling. Therefore, newly formed lipid bodies of AA-stimulated eosinophils are inducible and enzymatically skilled organelles for effective PGD2 synthesis. Concurrently, RT-PCR analysis showed that non-stimulated human circulating eosinophils express H-PGDS mRNA, which may represent a potential target for an AA-driven priming effect on PGD2 production by eosinophils since, in parallel, AA stimulation increased levels of H-PGDS message (Figure 1G).
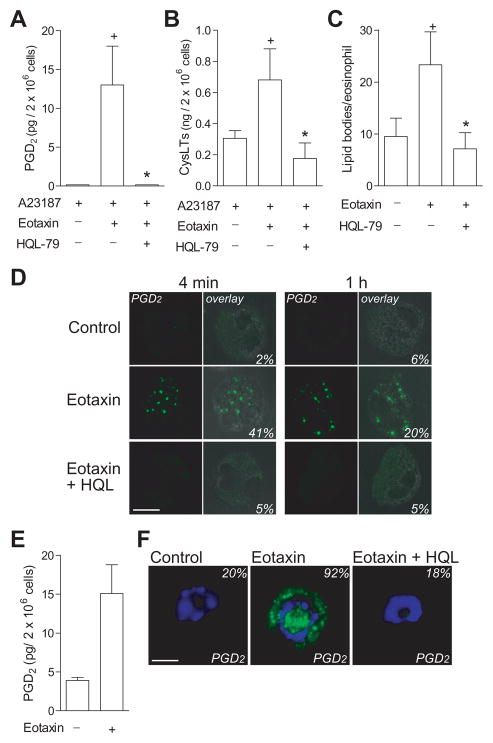
Eotaxin elicits the synthesis of biologically active PGD2
Eotaxin – a key mediator in the development of allergic eosinophilia that is known by its potent eosinophilotactic activity – has recently emerged as a potent mediator of eosinophil activation, with the particular ability to enhance LTC4 synthesis by eosinophils (50). Here, we showed that, aside from activating LO pathways, eotaxin is also able to control COX-driven prostanoid synthesis within eosinophils. As shown in Figure 2A, the pre-stimulation with eotaxin (6 nM) effectively primed eosinophils for HQL-79-sensitive enhanced PGD2 release in response to suboptimal concentration of A23187. Eotaxin-pre-stimulated eosinophils released about 13-fold as much PGD2 as did eosinophils challenged with A23187 alone (0.1 μM). Although eosinophils stimulated with eotaxin alone released levels of PGD2 that are not detectable by EIA (not shown), our findings demonstrate eotaxin ability to initiate H-PGDS-driven PGD2-synthesizing machinery within eosinophils. To definitively establish eotaxin ability to trigger H-PGDS-driven PGD2-synthesizing machinery within eosinophils, more sensitive EicosaCell assay was employed with eotaxin stimulation of either human or mouse eosinophils. As shown in Figures 2D and 2F, eotaxin triggered HQL-sensitive lipid body-compartmentalized PGD2 synthesis within human and mouse eosinophils. In human cells, immuno-fluorescence PGD2 was detected, as acute as, 4 min of stimulation with eotaxin in about ~ 40% of eosinophils (Figure 2D), whereas about 90% of eotaxin-stimulated mouse eosinophils displayed PGD2 immuno-labeling (Figure F). Corroborating such cell primed state of in vitro differentiated mouse eosinophils, eotaxin stimulation per se was able to elicit PGD2 production that was detected even by EIA in cell supernatants (Figure 2E). It is also noteworthy that any speculation, that other PGD2-synthesizing cells contaminating eosinophil preparations (e.g. basophils) were the actual cell type responsible for PGD2 synthesis, was ruled out by the high percentage of cells in eosinophil preparations synthesizing PGD2. Either in AA-stimulated human eosinophils (Figure 1E) or eotaxin-stimulated mouse eosinophils (Figure 2F), by EicosaCell about 90% of cells were PGD2 immunoreactive.
Figure 2. Eotaxin elicits production of biologically active PGD2.
Both human and mouse eosinophils were pre-treated for 30 min with HQL-79 before eotaxin stimulation. In A and B, for analysis of PGD2 and cysLTs synthesis, human eosinophils were stimulated for 1 h with eotaxin (6 nM) and then challenged with A23187 (0.1 μM). In C, for analysis of lipid body biogenesis, human eosinophils were stimulated for 1 h with eotaxin (6 nM). In D, confocal images of EicosaCell preparations display intracellular immuno-detection of newly formed PGD2 (green) in human eosinophils stimulated with rh eotaxin (6 nM). Overlay images of immuno-fluorescence and light microscopy of identical fields are shown in the larger images. In E, for analysis of PGD2 synthesis, mouse eosinophils were stimulated for 1 h with rm eotaxin (6 nM). Panel F shows confocal images of PGD2 immuno-detection of H-PDS (green) in mouse eosinophils stimulated with rm eotaxin (6 nM). Blue fluorescence shows eosinophil nuclei stained with DAPI. Bar, 5 μm. Results are expressed as means ± SEM for at least three independent experiments with eosinophils from distinct donors. + P ≤ 0.05 compared with control. * P ≤ 0.05 compared with eotaxin-stimulated eosinophils.
To characterize whether eotaxin-induced eosinophil-derived PGD2 was a bioactive mediator, by employing HQL-79 as a pharmacological strategy, we evaluated the role of endogenous PGD2 on two parameters of eosinophil functions triggered by eotaxin (6 nM): enhanced LTC4-synthesizing ability and induction of lipid body biogenesis. As shown in Figure 2B and C, eotaxin-induced enhancement of cysLTs production and lipid body biogenesis were blocked by HQL-79. The inhibition of eotaxin-induced eosinophil functions by HQL-79, besides reinforcing that eosinophils do in fact synthesize PGD2, shows that eosinophil-derived PGD2 displays biological activity, which can be very acute (even within 4 min), with allergy-relevant impacts on eosinophil activation.
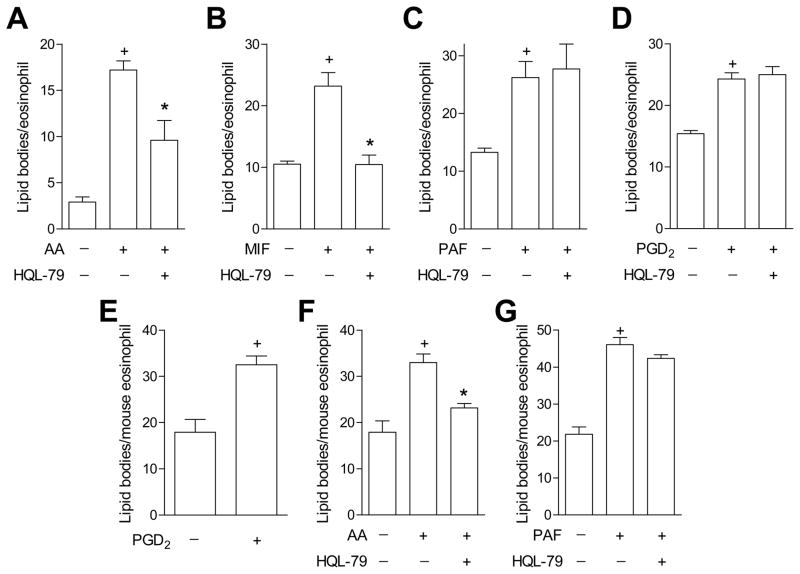
Induction of synthesis of bioactive PGD2 is stimulus-specific
As a functional approach to further screen potential physiological stimuli of PGD2 synthesis by eosinophils, lipid body biogenesis – a complex cellular outcome (47) that can be triggered by PGD2 (43) – was induced by a variety of stimuli undergoing HQL-79 treatment. As shown in Figure 3A and B, either AA- and MIF-induced biogenesis of cytoplasmic lipid bodies within eosinophils was significantly reduced by HQL-79, indicating that, at least in part, lipid body assembly triggered by these stimuli is dependent on endogenously produced PGD2. Among eosinophil-relevant agonists with a recognized capacity to trigger lipid body biogenesis, PAF and PGD2 itself, also trigger the rapid, receptor-mediated assembly of lipid bodies through signaling mechanisms distinct from those of AA and eotaxin (47). Here, we highlighted such signaling diversity and characterized the eosinophil PGD2-synthesizing ability as a stimulus-specific process, because HQL-79 treatment failed to modify either PAF- (Figure 3C) or PGD2-elicited lipid body biogenesis (Figure 3D). Of note, corroborating PAF lack of ability to induce PGD2 synthesis within eosinophils, distinct from eotaxin (Figure 2D), PAF-stimulated eosinophils fail to mount PGD2-synthesizing machinery (within 4 min or 1 h), since EicosaCell preparations of PAF-stimulated human eosinophils did not displayed PGD2 immuno-fluorescence (data not shown).
Figure 3. Endogenous eosinophil-derived PGD2 mediates AA- and eotaxin-, but not PAF or PGD2-induced lipid body biogenesis.
For in vitro analysis of lipid body biogenesis, human (A, B, C and D) or mouse (E, F and G) eosinophils were pre-treated for 30 min with HQL-79 and then stimulated for 1 h with AA (10 μM; A and F), MIF (50 ng/mL; B), PAF (1 μM; C and G) or PGD2 (25 nM; D and E). In vitro results are expressed as means ± SEM for at least three independent experiments with eosinophils from distinct donors. + P ≤ 0.05 compared with control. * P ≤ 0.05 compared with stimulated eosinophils.
Mouse eosinophils-derived PGD2 is also an endogenous bioactive molecule
Similar to human eosinophils, mouse eosinophils-derived PGD2 also displayed endogenous stimulatory effects. After establishing that exogenous PGD2 is capable of triggering lipid body biogenesis within mouse eosinophils (Figure 3E), we demonstrated that endogenous PGD2 released from AA-stimulated (Figure 3F), but not from PAF-stimulated, mouse eosinophils (Figure 3G) also participates in subsequent lipid body assembly. Taken together, these findings discard potential unspecific effects of HQL-79 on eosinophils, confirm that eosinophil-derived PGD2 contributes to lipid body assembly in a stimulus-specific fashion, and demonstrate the PGD2-synthesizing properties of mouse eosinophils. Therefore, rather than a species-specific phenomenon, the eosinophil PGD2-synthesizing ability appears to be a broad function displayed by the eosinophil cell type.
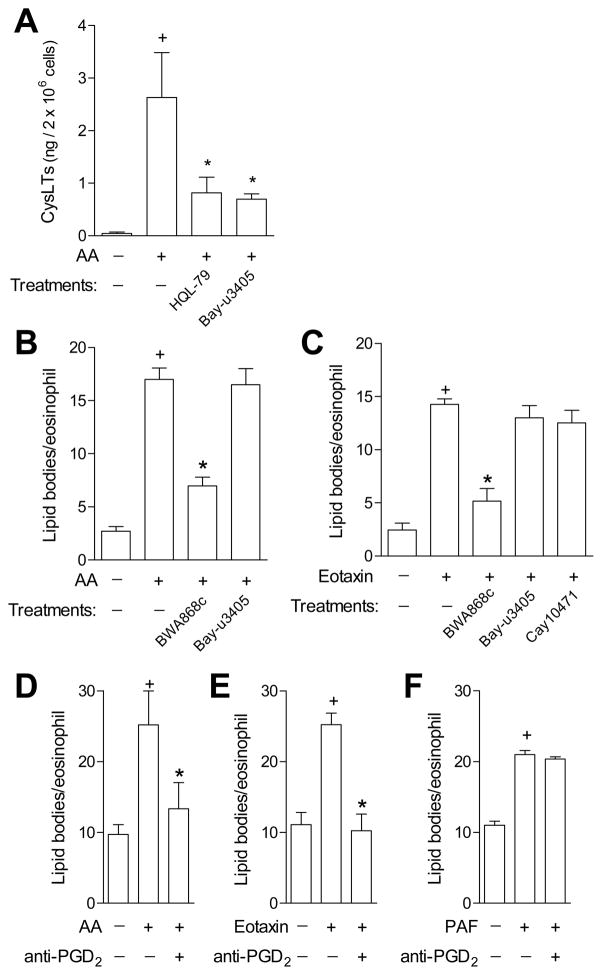
Eosinophil-derived PGD2 triggers eosinophil activation via interaction with specific receptors
We hypothesized that eosinophil-derived PGD2 may regulate AA- and eotaxin-induced eosinophil activation by acting on its specific receptors DP1 and DP2. Pre-treatments with HQL-79 or Bay-u3405 (antagonist of the PGD2 receptor DP2) significantly inhibited eosinophil cysLTs production triggered by AA, thus showing that newly synthesized PGD2 functions as an agonist of eosinophil-expressed DP2 receptors under specific stimulation (Figure 4A). Similarly, lipid body assembly triggered by either AA (Figure 4B) or eotaxin (Figure 4C) was significantly reduced when the DP1 receptor was blocked with the selective DP1 antagonist BWA868c, indicating that AA- and eotaxin-stimulated eosinophils release biologically active PGD2, which binds to DP1 receptors expressed on eosinophils to initiate lipid body biogenesis-eliciting signaling. Figure 4 also shows that pre-treatments with antagonists of the PGD2 receptor DP2, Bay-u3405 or Cay10471, as expected, failed to affect AA- (Figure 4B) or eotaxin-induced lipid body biogenesis (Figure 4C), confirming that the lipid body biogenic process within eosinophils triggered by exogenous or endogenous PGD2 is controlled selectively by DP1 activation (32).
Figure 4. Eosinophil-derived PGD2 controls eosinophil activation via interaction with specific PGD2 receptors.
In A, for analysis of cysLTs production, human eosinophils were pre-treated for 30 min with HQL-79 or Bay-u3405, stimulated for 1 h with AA (10 μM) and then challenged with A23187 (0.1 μM). From B to F, for in vitro analysis of lipid body biogenesis, human eosinophils were pre-treated for 30 min with neutralizing anti-PGD2 antibody, BWA868c, Bay-u3405 or Cay10471 and then stimulated for 1 h with AA, eotaxin, or PAF, as indicated. The results are expressed as the means ± SEM for at least three independent experiments with eosinophils purified from distinct donors. + P ≤ 0.05 compared with control. * P ≤ 0.05 compared with stimulated eosinophils.
Endogenous PGD2 displays an autocrine/paracrine, rather than an intracrine, effect on eosinophils
Acting extracellularly, PGD2 has emerged as key paracrine mediator pertinent to asthma and other allergic diseases. However, it is increasingly accepted that eicosanoids including PGD2 may also display intracrine roles in regulating cell functions. Indeed, signaling evoked by intracellular eicosanoid receptors has been shown in eosinophils and other cells (51–53). To verify whether autocrine/paracrine versus intracrine activity of eosinophil-synthesized PGD2 control eosinophil activation, intact viable eosinophils were pre-treated with anti-PGD2 antibodies whose neutralizing activity is excluded from intracellular compartment. Pertinent to PGD2 functions as a paracrine/autocrine mediator of eosinophil activation (Figure 4), the neutralization of endogenous PGD2 by the anti-PGD2, but not by an isotype control (data not shown), inhibited lipid body biogenesis induced by either AA (Figure 4D) or eotaxin (Figure 4E) within human eosinophils. Supporting antibody specificity, anti-PGD2 treatment failed to affect PAF-induced lipid body formation within eosinophils (Figure 4F). Thus, rather than functioning as an intracrine signal-transducing molecule, eosinophil-derived PGD2 is secreted from eosinophils and then, by acting extracellularly on PGD2 specific receptors, mediates eosinophil activation initiated by AA or eotaxin.
Eosinophils recruited to sites of allergic inflammation function as a late cellular source of PGD2
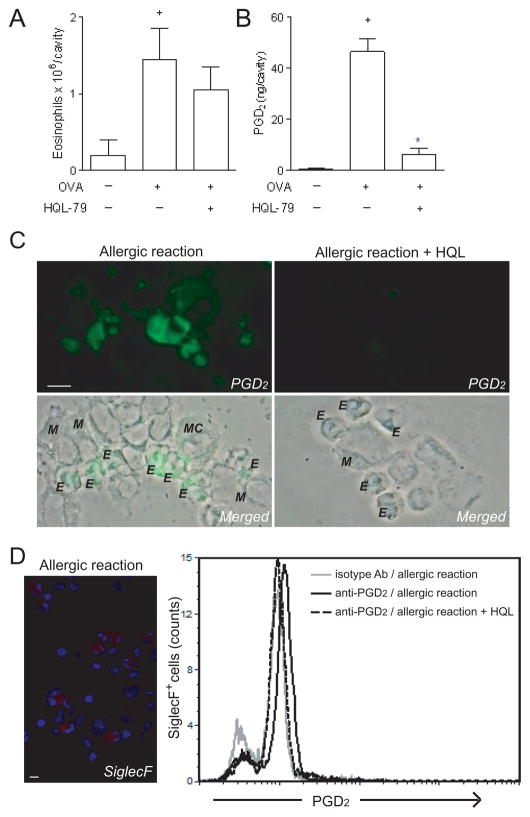
As activation of infiltrating eosinophils is a critical feature in the pathogenesis of allergic diseases, we hypothesized that activated eosinophils found at sites of allergic inflammation may synthesize and release PGD2. As previously described (43,54,55), allergic challenge in actively sensitized mice induces a marked eosinophil recruitment to the pleural cavity in a mouse model of allergic inflammation. Infiltrating eosinophils are not detectable within 1 h, peak at 24 h, are detectable within the pleural space up to at least 96 h after allergic challenge, and are concurrent with a resident population of mast cells and a discrete but significant accumulation of other mononuclear cells (macrophages and lymphocytes), but no neutrophil is found (54). It is noteworthy that at acute time points (within 1 h) in absence of allergic eosinophilia, pleural inflammatory fluid presents a significant increase in PGD2 amounts (from 13 ± 10 to 61 ± 12 ng/cavity of PGD2 in saline- versus OVA-challenged mice, respectively; p ≤ 0.05; n = 3); such synthesis can be attributed to resident mast cells. Notably, 48 h-related pleural eosinophilia (Figure 5A), which is insensitive to HQL-79, parallels an increased pleural level of PGD2 (Figure 5B). Such delayed allergen-elicited PGD2 production appears to depend on H-PGDS activity, since HQL-79 impairs it (Figure 5B). To identify the cell source of delayed pleural PGD2, EicosaCell preparations of pleural leukocytes recovered from allergic inflammatory sites were immuno-labeled with anti-PGD2. As shown in Figure 5C (left panel), virtually all eosinophils infiltrating the pleural space yielded focal immunofluorescent staining for PGD2. Of note, in EicosaCell preparations, the eosinophil population was readily identified by visual inspection of nucleus morphology, since as defined by direct counting of eosin-stained cells, the eosinophils (~ 35 % of total pleural cells) were the single polymorphonucelar cell type found infiltrating allergic site of inflammation. The specificity of PGD2 immunostaining within recruited eosinophils was validated because (i) leukocytes from sensitized, non-challenged mice exhibited no PGD2 staining; (ii) pre-treatment with HQL-79 completely abolished PGD2 staining within infiltrating eosinophils (Figure 5C, right panel);and (iii) mononuclear cells (e.g. macrophages), also found in the pleural space after an allergic challenge in sensitized mice, did not show any staining for intracellular PGD2 (Figure 5C, left panel) at this time point. Even though mast cells are the professional PGD2-synthesizing cells, at late time points mast cell contribution to PGD2 generation appears to be very limited (Figure 5C, left panel – arrows). The ability of eosinophils recruited to site allergic inflammation to produce PGD2 was further confirmed by analyzing EicosaCell preparations by flow cytometry (Figure 5 D). To study eosinophils, we employed double-immunolabeling by anti-SiglecF, an effective approach at detecting eosinophils in mixed cell populations (56). Indeed, as expected the SiglecF staining yielded results that matched visual inspection of eosin-stained cytospin preparations by specifically labeling eosinophilic polymorphonuclear cells (Figure 5D, left panel), immunodetecting 32.1 ± 6.2 % of cells infiltrating allergic inflammatory space as SiglecF+ eosinophils (n = 5). Specifically analyzing these SiglecF+ cells in Eicosacell preparations of allergic reaction by flow cytometry (Figure 5D, right panel), we extended our microscopic findings by demonstrating that all recruited SiglecF+ eosinophils synthesized PGD2, as evidenced by an HQL-79-sensitive uniformly positive, unimodal pattern of intracellular PGD2 immunoreactivity (Figure 5D). Collectively, our data implicates infiltrating eosinophils as an additional cell population responsible for maintenance of PGD2 production during allergic inflammatory reactions.
Figure 5. Infiltrating eosinophils are an auxiliary cell source of PGD2 at sites of allergic inflammation.
In A and B, for in vivo analysis of eosinophil influx and PGD2 production, respectively, sensitized mice were sacrificed 48 h after allergic challenge with ovalbumin. Animals received HQL-79 1 h prior to allergic challenge. In vivo results are expressed as the means ± SEM for at least eight animals. + P ≤ 0.05 compared with control. * P ≤ 0.05 compared with ovalbumin-challenged animals. In C, EicosaCell images show intracellular immuno-fluorescence for PGD2 pleural leukocytes recovered from non- and HQL-79-treated ovalbumin-challenged mice (as indicated). Overlay images of identical phase contrast fields are shown to facilitate the identification of the immuno-fluorescent cell type. E, M, and MC indicate eosinophils, macrophages, and mast cells, respectively. Arrows show immuno-labeled PGD2 within a resident mast cell. Bar, 10 μm. In D, epifluorescence image (left panel) shows allergic infiltrating eosinohils as SiglecF+PE-labeled (red staining) cells with DAPI-stained polymorphic nuclei (blue staining). Right panel shows EicosaCell analysis of PGD2 synthesis within SiglecF+ pleural eosinophils found in the site of allergic inflammation of HQL-treated and non-treated animals. Histogram is a representative data of 5 animals per group.
Discussion
PGD2 is a key lipid mediator of allergic airway inflammation that is released following allergen exposure in patients with asthma (40,41). Because PGD2 modulates key aspects of this prevalent pathology, PGD2 has emerged as a major mediator of allergic inflammatory disorders and, therefore, is an interesting target for anti-allergic treatments. Among PGD2-driven asthma-relevant actions are the synthesis of cysLTs, as well as both recruitment and subsequent activation of eosinophils, which is one of the principal cell types recruited to and activated at sites of allergic inflammation.
PGD2 is a major COX pathway product of mast cells, which are acknowledged as a key cell population providing PGD2 within inflammatory sites of allergic reactions. This view is mostly based on a rather restricted expression of the limiting PGD2-forming enzyme H-PGDS within mast cells. Extending the findings of an earlier study that evaluated human tissue eosinophils found infiltrating mucosa of patients with allergic rhinitis (21) or polyps of chronic rhinosinusitis patients (20), H-PGDS expression (both at mRNA and protein levels) was detected within human circulating eosinophils freshly isolated from healthy donors, thus indicating that, in addition to mast cells, eosinophils could also contribute to PGD2 synthesis in allergic inflammatory sites. However, it is now well established that the successful production of PGD2, or any other eicosanoid, is not merely determined by the proper expression of restrictive enzymes. In addition, it requires AA availability, the presence of all other relevant protein/enzymes, coordinated phosphorylation of some enzymes, correct spatial assembly of enzymatic complexes, and regulated intracellular compartmentalization of these complexes (for a review, see (47)). By simply finding H-PGDS within eosinophils, it cannot be ascertained whether these cells are capable of mounting a successful PGD2 production and, consequently, contribute to allergy-related elevated PGD2 generation. Therefore, our main aim here was to prove that, as in mast cells, eosinophil H-PGDS could couple to an active prostanoid-synthesizing machinery at specific, intracellular compartments within eosinophils, which would generate and release bioactive PGD2. By employing several experimental techniques, we attest that both human and mouse eosinophils are indeed able to synthesize PGD2 because (i) PGD2 was detected within supernatants of purified human eosinophils stimulated in vitro with A23187; (ii) AA and eotaxin were able to up-regulate PGD2 production/release by eosinophils; (iii) AA- and eotaxin-primed, as well as A23187-induced, PGD2 production/release were inhibited by HQL-79; (iv) A23187- and AA-induced, HQL-79-sensitive PGD2 synthesis was differentially compartmentalized within the perinuclear membrane and lipid bodies, respectively; and (v) functional assays showing that AA- and eotaxin-induced eosinophil activation were inhibited by pre-treatments with HQL-79, antibody anti-PGD2 or receptor antagonists of DP1 and DP2. More specifically, these data show that such PGD2 synthesis by eosinophils is an H-PGDS-dependent event that culminates in an extracellular release of a biologically active PGD2, which displays autocrine/paracrine activities on eosinophils via the activation of its specific receptors, DP1 and DP2.
What about eosinophil contribution to allergic airway inflammation as a PGD2 source following allergen exposure? To definitively demonstrate that eosinophils also play such an additional role in allergic inflammatory reactions by providing PGD2, we employed a direct strategy for the in situ immunolocalization of intracellular PGD2 to identify the cell population responsible for PGD2 production in a mouse model of allergic inflammation that displays increased levels of PGD2 at later time points. Eosinophils recruited to the inflammatory site, which also had concurrent macrophage and mast cell populations, was the predominant cell type generating PGD2, thus challenging the prevailing notion of mast cells as the single PGD2 cell source during allergic reactions and placing eosinophils as responsible for continued production of PGD2.
Eosinophil-derived, biologically active PGD2 may modulate eosinophil activation in sites of allergic inflammation. PGD2-driven eosinophil activation during allergic airway inflammation is known to elicit LTC4 production by eosinophil themselves (43). Therefore, even at minute amounts and in part due to its autocrine feature, such eosinophil-derived PGD2 activity emerges as a key up-regulatory mechanism for the local generation of pro-allergic mediators. Considering both our findings and the disappointing clinical trial results of DP1 antagonist laropiprant in asthmatics and allergic rhinitis patients (57), it appears that therapies targeting PGD2 synthesis, rather than receptor antagonism, may display superior beneficial outcomes. Therefore, our data, in addition to reinforcing the notion of eosinophils as major effector cells of allergic disorders, identify the PGD2-synthesizing property of eosinophils as a novel alternative target for anti-allergic therapies.
Acknowledgments
Financial Support: CNPq and FAPERJ from Brazil and NIH (Bethesda, MD) grants to P.F.W (AI020241, AI051645 and AI022571).
Abbreviations
- 5-LO
5-lipoxygenase
- COX
cyclooxygenase
- AA
arachidonic acid
- ADRP
adipose differentiation-related protein
- CRTH2
chemoattractant receptor-homologous molecule expressed on T helper type 2 cell (Th2) cells
- cysLTs
cysteinyl leukotrienes
- DP1
D prostanoid receptor 1
- DP2
D prostanoid receptor 2
- EDAC
1-ethyl-3-(3-dimethylamino-propyl) carbodiimide
- LTC4
leukotriene C4
- PGD2
prostaglandin D2
- PAF
platelet-activating factor
References
- 1.Barrett NA, Austen KF. Innate cells and T helper 2 cell immunity in airway inflammation. Immunity. 2009;31:425–437. doi: 10.1016/j.immuni.2009.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boyce JA. The role of mast cells in asthma. Prostaglandins, Leukotrienes and Essential Fatty Acids. 2008;69:195–205. doi: 10.1016/s0952-3278(03)00081-4. [DOI] [PubMed] [Google Scholar]
- 3.Ogawa Y, Calhoun WJ. The role of leukotrienes in airway inflammation. J Allergy Clin Immunol. 2006;118:789–798. doi: 10.1016/j.jaci.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 4.Lee TH, Woszczek G, Farooque SP. Leukotriene E4: Perspective on the forgotten mediator. Journal of Allergy and Clinical Immunology. 2009;124:417–421. doi: 10.1016/j.jaci.2009.04.020. [DOI] [PubMed] [Google Scholar]
- 5.Kanaoka Y, Urade Y. Hematopoietic prostaglandin D synthase. Prostaglandins Leukot Essent Fatty Acids. 2003;69:163–167. doi: 10.1016/s0952-3278(03)00077-2. [DOI] [PubMed] [Google Scholar]
- 6.Bandeira-Melo C, Bozza PT, Weller PF. The cellular biology of eosinophil eicosanoid formation and function. J Allergy Clin Immunol. 2002;109:393–400. doi: 10.1067/mai.2002.121529. [DOI] [PubMed] [Google Scholar]
- 7.Nantel F, Fong C, Lamontagne S, Wright DH, Giaid A, Desrosiers M, Metters KM, O’Neill GP, Gervais FG. Expression of prostaglandin D synthase and the prostaglandin D2 receptors DP and CRTH2 in human nasal mucosa. Prostaglandins Other Lipid Mediat. 2004;73:87–101. doi: 10.1016/j.prostaglandins.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 8.Lewis RA, Soter NA, Diamond PT, Austen KF, Oates JA, Roberts LJ. Prostaglandin D2 generation after activation of rat and human mast cells with anti-IgE. J Immunol. 1982;129:1627–1631. [PubMed] [Google Scholar]
- 9.O’Sullivan S, Dahlen B, Dahlen SE, Kumlin M. Increased urinary excretion of the prostaglandin D2 metabolite 9 alpha, 11 beta-prostaglandin F2 after aspirin challenge supports mast cell activation in aspirin-induced airway obstruction. J Allergy Clin Immunol. 1996;98:421–432. doi: 10.1016/s0091-6749(96)70167-7. [DOI] [PubMed] [Google Scholar]
- 10.Bochenek G, Nagraba K, Nizankowska E, Szczeklik A. A controlled study of 9alpha,11beta-PGF2 (a prostaglandin D2 metabolite) in plasma and urine of patients with bronchial asthma and healthy controls after aspirin challenge. J Allergy Clin Immunol. 2003;111:743–749. doi: 10.1067/mai.2003.1387. [DOI] [PubMed] [Google Scholar]
- 11.Dahlen SE, Kumlin M. Monitoring mast cell activation by prostaglandin D2 in vivo. Thorax. 2004;59:453–455. doi: 10.1136/thx.2004.026641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hamberg M, Fredholm BB. Isomerization of prostaglandin H2 into prostaglandin D2 in the presence of serum albumin. Biochim Biophys Acta. 1976;431:189–83. doi: 10.1016/0005-2760(76)90273-3. [DOI] [PubMed] [Google Scholar]
- 13.Taba Y, Sasaguri T, Miyagi M, Abumiya T, Miwa Y, Ikeda T, Mitsumata M. Fluid Shear Stress Induces Lipocalin-Type Prostaglandin D2 Synthase Expression in Vascular Endothelial Cells. Circ Res. 2000;86:967–973. doi: 10.1161/01.res.86.9.967. [DOI] [PubMed] [Google Scholar]
- 14.Tanaka K, Ogawa K, Sugamura K, Nakamura M, Takano S, Nagata K. Cutting edge: differential production of prostaglandin D2 by human helper T cell subsets. J Immunol. 2000;164:2277–2280. doi: 10.4049/jimmunol.164.5.2277. [DOI] [PubMed] [Google Scholar]
- 15.Shimura C, Satoh T, Igawa K, Aritake K, Urade Y, Nakamura M, Yokozeki H. Dendritic cells express hematopoietic prostaglandin D synthase and function as a source of prostaglandin D2 in the skin. Am J Pathol. 2010;176:227–237. doi: 10.2353/ajpath.2010.090111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Joo M, Kwon M, Sadikot RT, Kingsley PJ, Marnett LJ, Blackwell TS, Peebles RS, Urade Y, Christman JW. Induction and Function of Lipocalin Prostaglandin D Synthase in Host Immunity. J Immunol. 2007;179:2565–2575. doi: 10.4049/jimmunol.179.4.2565. [DOI] [PubMed] [Google Scholar]
- 17.Gandhi UH, Kaushal N, Ravindra KC, Hegde S, Nelson SM, Narayan V, Vunta H, Paulson RF, Prabhu KS. Selenoprotein-dependent Up-regulation of Hematopoietic Prostaglandin D2 Synthase in Macrophages Is Mediated through the Activation of Peroxisome Proliferator-activated Receptor (PPAR) γ. J Biol Chem. 2011;286:27471–27482. doi: 10.1074/jbc.M111.260547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ugajin T, Satoh T, Kanamori T, Aritake K, Urade Y, Yokozeki H. Fc[epsilon]RI, but Not Fc[gamma]R, Signals Induce Prostaglandin D2 and E2 Production from Basophils. The American Journal of Pathology. 2011;179:775–782. doi: 10.1016/j.ajpath.2011.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parsons WG, III, Roberts LJ. Transformation of prostaglandin D2 to isomeric prostaglandin F2 compounds by human eosinophils. A potential mast cell-eosinophil interaction. J Immunol. 1988;141:2413–2419. [PubMed] [Google Scholar]
- 20.Hyo S, Kawata R, Kadoyama K, Eguchi N, Kubota T, Takenaka H, Urade Y. Expression of prostaglandin D2 synthase in activated eosinophils in nasal polyps. Arch Otolaryngol Head Neck Surg. 2007;133:693–700. doi: 10.1001/archotol.133.7.693. [DOI] [PubMed] [Google Scholar]
- 21.Okano M, Fujiwara T, Sugata Y, Gotoh D, Masaoka Y, Sogo M, Tanimoto W, Yamamoto M, Matsumoto R, Eguchi N, Kiniwa M, Isik AU, Urade Y, Nishizaki K. Presence and characterization of prostaglandin D2-related molecules in nasal mucosa of patients with allergic rhinitis. Am J Rhinol. 2006;20:342–348. doi: 10.2500/ajr.2006.20.2865. [DOI] [PubMed] [Google Scholar]
- 22.Hirai H, Tanaka K, Yoshie O, Ogawa K, Kenmotsu K, Takamori Y, Ichimasa M, Sugamura K, Nakamura M, Takano S, Nagata K. Prostaglandin D2 selectively induces chemotaxis in T helper type 2 cells, eosinophils, and basophils via seven-transmembrane receptor CRTH2. J Exp Med. 2001;193:255–261. doi: 10.1084/jem.193.2.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Monneret G, Gravel S, Diamond M, Rokach J, Powell WS. Prostaglandin D2 is a potent chemoattractant for human eosinophils that acts via a novel DP receptor. Blood. 2001;98:1942–1948. doi: 10.1182/blood.v98.6.1942. [DOI] [PubMed] [Google Scholar]
- 24.Kabashima K, Narumiya S. The DP receptor, allergic inflammation and asthma. Prostaglandins, Leukotrienes and Essential Fatty Acids. 2008;69:187–194. doi: 10.1016/s0952-3278(03)00080-2. [DOI] [PubMed] [Google Scholar]
- 25.Hardy CC, Robinson C, Tattersfield AE, Holgate ST. The bronchoconstrictor effect of inhaled prostaglandin D2 in normal and asthmatic men. N Engl J Med. 1984;311:209–213. doi: 10.1056/NEJM198407263110401. [DOI] [PubMed] [Google Scholar]
- 26.Patterson R, Harris KE, Greenberger PA. Effect of prostaglandin D2 and I2 on the airways of rhesus monkeys. J Allergy Clin Immunol. 1980;65:269–273. doi: 10.1016/0091-6749(80)90154-2. [DOI] [PubMed] [Google Scholar]
- 27.Hirata M, Kakizuka A, Aizawa M, Ushikubi F, Narumiya S. Molecular characterization of a mouse prostaglandin D receptor and functional expression of the cloned gene. PNAS. 1994;91:11192–11196. doi: 10.1073/pnas.91.23.11192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boie Y, Sawyer N, Slipetz DM, Metters KM, Abramovitz M. Molecular Cloning and Characterization of the Human Prostanoid DP Receptor. J Biol Chem. 1995;270:18910–18916. doi: 10.1074/jbc.270.32.18910. [DOI] [PubMed] [Google Scholar]
- 29.Nagata K, Hirai H, Tanaka K, Ogawa K, Aso T, Sugamura K, Nakamura M, Takano S. CRTH2, an orphan receptor of T-helper-2-cells, is expressed on basophils and eosinophils and responds to mast cell-derived factor(s) FEBS Lett. 1999;459:195–199. doi: 10.1016/s0014-5793(99)01251-x. [DOI] [PubMed] [Google Scholar]
- 30.Schuligoi R, Sturm E, Luschnig P, Konya V, Philipose S, Sedej M, Waldhoer M, Peskar BA, Heinemann A. CRTH2 and D-Type Prostanoid Receptor Antagonists as Novel Therapeutic Agents for Inflammatory Diseases. Pharmacology. 2010;85:372–382. doi: 10.1159/000313836. [DOI] [PubMed] [Google Scholar]
- 31.Arima M, Fukuda T. Prostaglandin D and T(H)2 inflammation in the pathogenesis of bronchial asthma. Korean J Intern Med. 2011;26:8–18. doi: 10.3904/kjim.2011.26.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mesquita-Santos F, Bakker-Abreu I, Luna-Gomes T, Bozza P, Diaz B, Bandeira-Melo C. Co-operative signalling through DP(1) and DP(2) prostanoid receptors is required to enhance leukotriene C(4) synthesis induced by prostaglandin D(2) in eosinophils. Br J Pharmacol. 2011;162:1674–1685. doi: 10.1111/j.1476-5381.2010.01086.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sandig H, Andrew D, Barnes AA, Sabroe I, Pease J. 9α,11β-PGF2 and its stereoisomer PGF2α are novel agonists of the chemoattractant receptor, CRTH2. FEBS Letters. 2006;580:373–379. doi: 10.1016/j.febslet.2005.11.052. [DOI] [PubMed] [Google Scholar]
- 34.Sawyer N, Cauchon E, Chateauneuf A, Cruz RP, Nicholson DW, Metters KM, O’Neill GP, Gervais FG. Molecular pharmacology of the human prostaglandin D2 receptor, CRTH2. Br J Pharmacol. 2002;137:1163–1172. doi: 10.1038/sj.bjp.0704973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gazi L, Gyles S, Rose J, Lees S, Allan C, Xue L, Jassal R, Speight G, Gamble V, Pettipher R. Delta12-prostaglandin D2 is a potent and selective CRTH2 receptor agonist and causes activation of human eosinophils and Th2 lymphocytes. Prostaglandins Other Lipid Mediat. 2005;75:153–167. doi: 10.1016/j.prostaglandins.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 36.Monneret G, Li H, Vasilescu J, Rokach J, Powell WS. 15-Deoxy-{Delta}12,1412,14-prostaglandins D2 and J2 Are Potent Activators of Human Eosinophils. J Immunol. 2002;168:3563–3569. doi: 10.4049/jimmunol.168.7.3563. [DOI] [PubMed] [Google Scholar]
- 37.Heinemann A, Schuligoi R, Sabroe I, Hartnell A, Peskar BA. Delta 12-prostaglandin J2, a plasma metabolite of prostaglandin D2, causes eosinophil mobilization from the bone marrow and primes eosinophils for chemotaxis. J Immunol. 2003;170:4752–4758. doi: 10.4049/jimmunol.170.9.4752. [DOI] [PubMed] [Google Scholar]
- 38.Böhm E, Sturm GJ, Weiglhofer I, Sandig H, Shichijo M, McNamee A, Pease JE, Kollroser M, Peskar BA, Heinemann A. 11-Dehydro-thromboxane B2, a Stable Thromboxane Metabolite, Is a Full Agonist of Chemoattractant Receptor-homologous Molecule Expressed on TH2 Cells (CRTH2) in Human Eosinophils and Basophils. J Biol Chem. 2004;279:7663–7670. doi: 10.1074/jbc.M310270200. [DOI] [PubMed] [Google Scholar]
- 39.Naclerio RM, Meier HL, Kagey-Sobotka A, Adkinson NF, Jr, Meyers DA, Norman PS, Lichtenstein LM. Mediator release after nasal airway challenge with allergen. Am Rev Respir Dis. 1983;128:597–602. doi: 10.1164/arrd.1983.128.4.597. [DOI] [PubMed] [Google Scholar]
- 40.Murray JJ, Tonnel AB, Brash AR, Roberts LJ, Gosset P, Workman R, Capron A, Oates JA. Release of prostaglandin D2 into human airways during acute antigen challenge. N Engl J Med. 1986;315:800–804. doi: 10.1056/NEJM198609253151304. [DOI] [PubMed] [Google Scholar]
- 41.Balzar S, Fajt ML, Comhair SA, Erzurum SC, Bleecker E, Busse WW, Castro M, Gaston B, Israel E, Schwartz LB, Curran-Everett D, Moore CG, Wenzel SE. Mast cell phenotype, location, and activation in severe asthma: data from the severe asthma research program. Am J Respir Crit Care Med. 2011;183:299–309. doi: 10.1164/rccm.201002-0295OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Charlesworth EN, Kagey-Sobotka A, Schleimer RP, Norman PS, Lichtenstein LM. Prednisone inhibits the appearance of inflammatory mediators and the influx of eosinophils and basophils associated with the cutaneous late-phase response to allergen. J Immunol. 1991;146:671–676. [PubMed] [Google Scholar]
- 43.Mesquita-Santos FP, Vieira-de-Abreu A, Calheiros AS, Figueiredo IH, Castro-Faria-Neto HC, Weller PF, Bozza PT, Diaz BL, Bandeira-Melo C. Cutting Edge: Prostaglandin D2 Enhances Leukotriene C4 Synthesis by Eosinophils during Allergic Inflammation: Synergistic In Vivo Role of Endogenous Eotaxin. J Immunol. 2006;176:1326–1330. doi: 10.4049/jimmunol.176.3.1326. [DOI] [PubMed] [Google Scholar]
- 44.Dyer KD, Moser JM, Czapiga M, Siegel SJ, Percopo CM, Rosenberg HF. Functionally Competent Eosinophils Differentiated Ex Vivo in High Purity from Normal Mouse Bone Marrow. J Immunol. 2008;181:4004–4009. doi: 10.4049/jimmunol.181.6.4004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bandeira-Melo C, Weller PF, Bozza PT. EicosaCell - an immunofluorescent-based assay to localize newly synthesized eicosanoid lipid mediators at intracellular sites. Methods Mol Biol. 2011;689:163–181. doi: 10.1007/978-1-60761-950-5_10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Le Mee S, Hennebert O, Ferrec C, Wulfert E, Morfin R. 7beta-Hydroxy-epiandrosterone-mediated regulation of the prostaglandin synthesis pathway in human peripheral blood monocytes. Steroids. 2008;73:1148–1159. doi: 10.1016/j.steroids.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 47.Bozza PT, Melo RC, Bandeira-Melo C. Leukocyte lipid bodies regulation and function: contribution to allergy and host defense. Pharmacol Ther. 2007;113:30–49. doi: 10.1016/j.pharmthera.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 48.Bozza PT, Payne JL, Morham SG, Langenbach R, Smithies O, Weller PF. Leukocyte lipid body formation and eicosanoid generation: cyclooxygenase-independent inhibition by aspirin. Proc Natl Acad Sci U S A. 1996;93:11091–11096. doi: 10.1073/pnas.93.20.11091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Moreira LS, Piva B, Gentile LB, Mesquita-Santos FP, D’Avila H, Maya-Monteiro CM, Bozza PT, Bandeira-Melo C, Diaz BL. Cytosolic phospholipase A2-driven PGE2 synthesis within unsaturated fatty acids-induced lipid bodies of epithelial cells. Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids. 2009;1791:156–165. doi: 10.1016/j.bbalip.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 50.Bandeira-Melo C, Phoofolo M, Weller PF. Extranuclear lipid bodies, elicited by CCR3-mediated signaling pathways, are the sites of chemokine-enhanced leukotriene C4 production in eosinophils and basophils. J Biol Chem. 2001;276:22779–22787. doi: 10.1074/jbc.M101436200. [DOI] [PubMed] [Google Scholar]
- 51.Devchand PR, Keller H, Peters JM, Vazquez M, Gonzalez FJ, Wahli W. The PPARalpha-leukotriene B4 pathway to inflammation control. Nature. 1996;384:39–43. doi: 10.1038/384039a0. [DOI] [PubMed] [Google Scholar]
- 52.Bhattacharya M, Peri K, Ribeiro-Da-Silva A, Almazan G, Shichi H, Hou X, Varma DR, Chemtob S. Localization of functional prostaglandin E2 receptors EP3 and EP4 in the nuclear envelope. J Biol Chem. 1999;274:15719–15724. doi: 10.1074/jbc.274.22.15719. [DOI] [PubMed] [Google Scholar]
- 53.Bandeira-Melo C, Woods LJ, Phoofolo M, Weller PF. Intracrine Cysteinyl Leukotriene Receptor-mediated Signaling of Eosinophil Vesicular Transport-mediated Interleukin-4 Secretion. J Exp Med. 2002;196:841–850. doi: 10.1084/jem.20020516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vieira-de-Abreu A, Assis EF, Gomes GS, Castro-Faria-Neto HC, Weller PF, Bandeira-Melo C, Bozza PT. Allergic challenge-elicited lipid bodies compartmentalize in vivo leukotriene C4 synthesis within eosinophils. Am J Respir Cell Mol Biol. 2005;33:254–261. doi: 10.1165/rcmb.2005-0145OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vieira-de-Abreu A, Calheiros AS, Mesquita-Santos FP, Magalhaes ES, Mourao-Sa D, Castro-Faria-Neto HC, Bozza MT, Bandeira-Melo C, Bozza PT. Crosstalk between MIF and Eotaxin in Allergic Eosinophil Activation Forms LTC4-Synthesizing Lipid Bodies. Am J Respir Cell Mol Biol. 2011;44:509–516. doi: 10.1165/rcmb.2010-0004OC. [DOI] [PubMed] [Google Scholar]
- 56.Dyer KD, Garcia-Crespo KE, Killoran KE, Rosenberg HF. Antigen profiles for the quantitative assessment of eosinophils in mouse tissues by flow cytometry. Journal of Immunological Methods. 2011;369:91–97. doi: 10.1016/j.jim.2011.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Philip G, van AJ, Loeys T, Liu N, Wong P, Lai E, Dass SB, Reiss TF. Clinical studies of the DP1 antagonist laropiprant in asthma and allergic rhinitis. J Allergy Clin Immunol. 2009;124:942–948. doi: 10.1016/j.jaci.2009.07.006. [DOI] [PubMed] [Google Scholar]