SUMMARY
While the abuse of opiate drugs continues to rise, the neuroadaptations that occur with long-term drug exposure remain poorly understood. We describe here a series of chronic morphine-induced adaptations in ventral tegmental area (VTA) dopamine neurons, which are mediated via downregulation of AKT-mTORC2 (mammalian target of rapamycin complex-2). Chronic opiates decrease the size of VTA dopamine neurons in rodents, an effect seen in humans as well, and concomitantly increase the excitability of the cells but decrease dopamine output to target regions. Chronic morphine decreases mTORC2 activity, and overexpression of Rictor, a component of mTORC2, prevents morphine-induced changes in cell morphology and activity. Further, local knock-out of Rictor in VTA decreases DA soma size and reduces rewarding responses to morphine, consistent with the hypothesis that these adaptations represent a mechanism of reward tolerance. Together, these findings demonstrate a novel role for AKT-mTORC2 signaling in mediating neuroadaptations to opiate drugs of abuse.
INTRODUCTION
A major neural substrate for the rewarding actions of opiates are dopaminergic (DA) neurons within the ventral tegmental area (VTA). Opiates acutely activate VTA DA neurons by inhibiting their GABAergic input through hyperpolarization of local GABA interneurons (Johnson and North, 1992), and decreasing long-term potentiation of GABAergic synapses onto DA neurons (Niehaus et al., 2010). Additionally, VTA DA neuron activity in vivo is increased in morphine-dependent rats, an effect normalized by either spontaneous or naloxone-precipitated withdrawal (Georges et al., 2006). However, the influence of chronic opiates on the intrinsic excitability of VTA DA neurons remains unknown.
At a cellular level, we have shown that both chronic morphine administration and heroin self-administration in rats decreases the soma size of VTA DA neurons (Russo et al., 2007; Sklair-Tavron et al., 1996). This reduced soma size is mediated by downregulation of a specific brain-derived neurotrophic factor (BDNF) signaling pathway involving insulin receptor substrate 2 (IRS2): the decrease in DA cell size is blocked by local infusion of BDNF (Sklair-Tavron et al., 1996) or viral-mediated overexpression of IRS2 in VTA, and mimicked by viral-mediated overexpression of a dominant-negative mutant of IRS2 (IRS2dn) in this brain region (Russo et al., 2007). Importantly, the decrease in soma size correlates with reward tolerance (Russo et al., 2007), where repeated drug use decreases the rewarding effect of the drug and leads to an escalation of drug intake, as seen in humans (O'Brien, 2001). While these studies suggest that the protein kinase, AKT, which is downstream of IRS2, is necessary and sufficient for the morphine-induced decrease in VTA cell size, the downstream signaling mechanisms involved remain unexplored. Moreover, the net effect of this decrease in VTA DA neuron soma size, along with any change in cell excitability, is unknown, although there are several reports of altered VTA DA soma size under other conditions (see Discussion).
Here, we focused on adaptations that chronic opiates induce in VTA DA neurons by further characterizing morphine-induced changes in VTA soma size, excitability, and functional output to target brain regions. We focus on AKT and one of its major downstream pathways, mammalian target of rapamycin (mTOR), as the critical mediators of morphine action, given the widely established role of this signaling pathway in cell growth. The serine/threonine kinase activity of mTOR, and its downstream substrates, depend on mTOR's association into two distinct complexes designated mTORC1 and mTORC2 (Foster and Fingar, 2010; Laplante and Sabatini, 2009). Both contain mTOR, mammalian lethal with Sec13 protein 8, and DEP-domain-containing mTOR interacting protein in addition to proteins specific to each complex. mTORC1 includes regulatory-associated protein of mTOR (Raptor) and proline-rich AKT substrate 40 kDa and promotes protein synthesis and cell growth through phosphorylation of two main substrates, eukaryotic initiation factor 4E -binding protein 1 (4EBP1) and p70 ribosomal S6 kinase 1 (p70S6K). This complex is sensitive to inhibition by rapamycin and is activated in response to several stimuli including nutrients and amino acids. In contrast, mTORC2 specifically contains rapamycin-insensitive companion of mTOR (Rictor), mammalian stress-activated protein kinase interacting protein, and protein observed with rictor-1, and phosphorylates the hydrophobic motif (HM) of multiple kinases including AKT, protein kinase Cα (PKCα), and serum- and glucocorticoid-inducible kinase 1. mTORC2 activity was originally implicated in cytoskeletal remodeling (Sarbassov et al., 2004), and recent evidence suggests a role in cell survival and growth as well, however, the upstream activators are poorly understood (Pearce et al., 2010).
Results of the present study show that the morphine-induced decrease in VTA DA soma size occurs concomitantly with an increase in the intrinsic excitability of these neurons, and that the net functional effect of chronic morphine is to decrease DA output to target regions. This net effect is consistent with morphine reward tolerance observed under these conditions. We go on to show that these adaptations induced by chronic morphine—including decreased soma size, increased excitability, and reward tolerance—are mediated via downregulation of IRS2-AKT and mTORC2 activity in this brain region. These results are surprising since our starting hypothesis was that chronic morphine might decrease mTORC1 activity, in concert with downregulation of IRS2-AKT, based on several reports that tie mTORC1 activity to regulation of neuronal growth and size (Kwon et al., 2003; Zhou et al., 2009). Counter to this hypothesis, mTORC1 signaling was increased in VTA by chronic morphine, an effect not related to the other actions of morphine on VTA DA neurons. Together, the findings reported here describe a fundamentally novel molecular pathway, involving decreased mTORC2 signaling, possibly as a result of decreased IRS2 signaling, through which chronic opiates alter the phenotype of VTA DA neurons to produce reward tolerance.
RESULTS
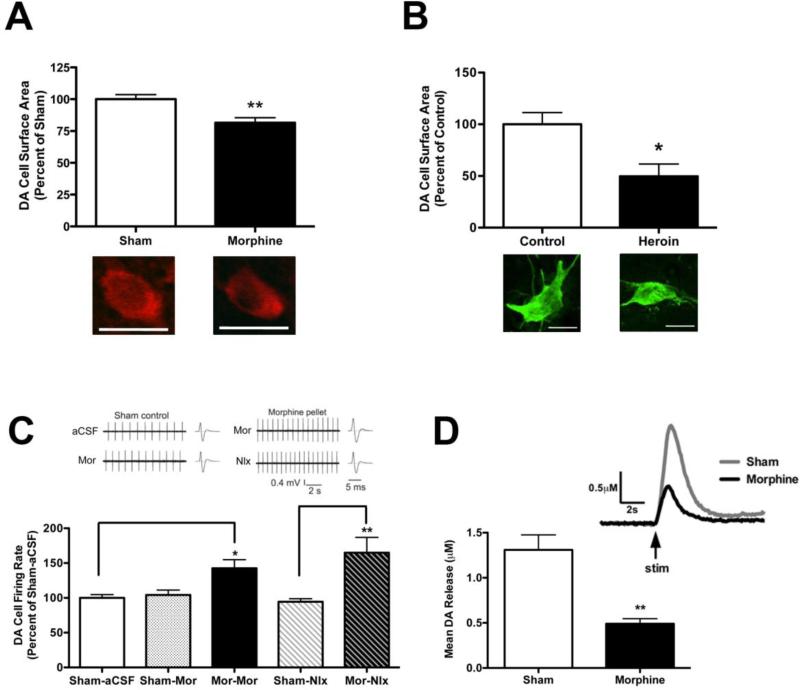
Chronic morphine alters VTA DA neuron morphology, activity, and output to NAc
We set out to characterize the effects of chronic morphine on several phenotypic characteristics of VTA DA neurons. We first determined whether morphine induces a morphological change in the mouse VTA similar to that seen in rats. We found a ~25% decrease in the mean surface area of mouse VTA DA neurons in response to chronic morphine (Figure 1A), very similar to the magnitude of soma size decrease observed in rats (Russo et al., 2007; Sklair-Tavron et al., 1996). To study the clinical relevance of this finding, we examined postmortem sections of human brain and observed a significant decrease in the soma size of VTA DA neurons in heroin users compared to controls (Figure 1B).
Figure 1. Morphine Alters VTA DA Neuronal Morphology, Activity, and Output to NAc.
(A) Chronic morphine decreased the cell surface area of TH+ cells in the mouse VTA. Student's t-test, **p<0.01, n=4, 6 mice/group (6-12 cells/mouse). (B) VTA DA neuron soma size is decreased in postmortem human heroin addicts compared to controls. Student's t-test, *p<0.05, n=3, 5 subjects/group (4-13 cells/subject). (C) VTA DA neurons in slices taken from chronic morphine-treated mice exhibited increased spontaneous firing rates compared to sham-treated mice as measured by extracellular single unit recording. One-way ANOVA, Tukey's post-hoc test, *p<0.05 compared to Sham-aCSF, **p<0.01 compared to Sham-naloxone (Nlx), n=6-8 mice per group (4-17 cells/mouse). Representative traces are shown above the graph. (D) Chronic morphine significantly decreased electrically-evoked DA release in NAc. Student's t-test, **p<0.01, n=5, 6 rats (50, 66 observations/condition). Representative traces are shown above the graph. All scale bars are 20μm.
We next examined whether the chronic opiate-induced morphological change was correlated with changes in DA neuronal excitability. We found that chronic morphine-treated mice, compared to sham-treated mice, exhibited an increase in the spontaneous firing rate of VTA DA neurons in brain slices (Figure 1C). This effect was not dependent on residual morphine in the slice, since blockade of opioid receptors with naloxone did not affect cell excitability (Figure 1C). Moreover, the inclusion of a low dose of morphine (5 μM) in the bath solution to prevent “withdrawal” in the slice did not alter DA neuron firing rate (Figure 1C).
Given the observations that chronic morphine decreases the size of VTA DA neurons, but concomitantly increases their excitability, it was important to determine whether net DA output from VTA is altered. We examined levels of extracellular DA in nucleus accumbens (NAc) in vivo, widely considered a key determinant of reward (Hyman et al., 2006). In opposition to the increased firing rate, we found that chronic morphine dramatically decreased electrically-evoked DA output in NAc of rats as measured by fast-scan cyclic voltammetry (Figure 1D). This reduction in DA output from VTA DA neurons supports the notion that the reduced soma size of the neurons, induced by chronic morphine, correlates with functional output, consistent with the reward tolerance induced by chronic morphine under these conditions (Russo et al., 2007).
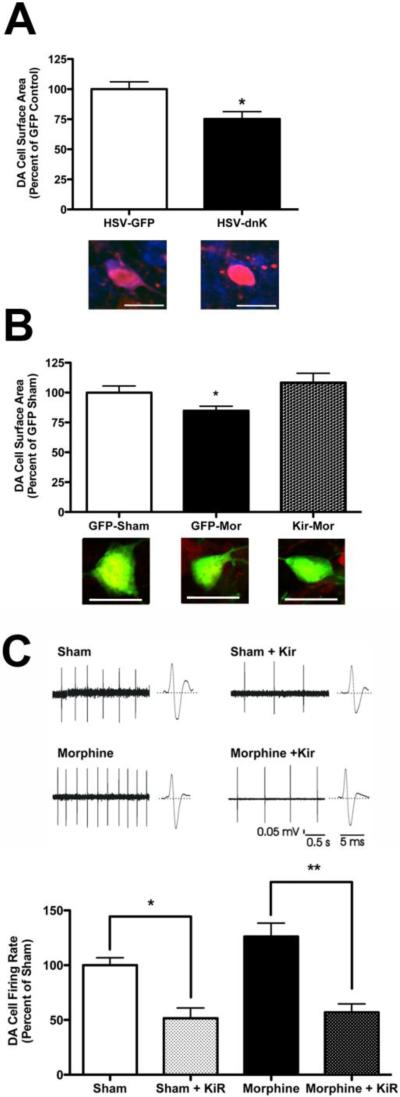
Alteration of VTA neuronal activity regulates DA soma size
Next, we examined a possible relationship between the increase in VTA DA neuron firing rate and soma size decrease, with the hypothesis that the increased firing rate per se induces changes in soma size. We virally overexpressed a dominant-negative K+ channel subunit (dnK, KCNAB2-S188A, R189L) locally within VTA; we showed previously that this mutant channel increases the firing rate of VTA DA neurons (Krishnan et al., 2007). Overexpression of dnK was sufficient to decrease the surface area of VTA DA neurons (Figure 2A). To obtain the converse type of information, we virally overexpressed wild-type Kir2.1 in VTA, which we showed decreases DA neuron firing rate (Krishnan et al., 2007). While overexpression of Kir2.1 alone did not affect VTA DA soma size (data not shown), it completely blocked the ability of chronic morphine both to decrease soma size (Figure 2B) and to increase DA neuron firing rate (Figure 2C). These findings support our hypothesis that the morphine-induced increase in VTA DA neuron excitability is both necessary and sufficient for mediating the decrease in soma size.
Figure 2. Alteration of VTA DA Firing Rate is Necessary and Sufficient for Morphine-Induced Changes in Soma Size.
(A) Increasing DA neuron firing rate via HSV-dnK decreased VTA DA soma size. Student's t-test, *p<0.05, n=3-4 mice per group (2-5 cells/mouse). Representative cells are shown below bars, TH-blue, GFP-red. (B) Preventing the morphine-induced increase in DA neuron firing rate via HSV-Kir2.1 prevented the morphine-induced decrease in soma size. One-way ANOVA followed by Tukey's post-hoc test, *p<0.05 compared to Kir-Mor, n=5-12 mice/group (2-9 cells/mouse). Representative cells are shown below bars, TH-red, GFP-green. (C) HSV-Kir2.1 blocked the morphine-induced increase in DA firing rate. One-way ANOVA, Tukey's post-hoc test, *p<0.05 sham compared to sham-Kir2.1, **p<0.01 morphine compared to morphine-Kir2.1, n=2 mice/group (13-15 cells/mouse). All scale bars are 20μm.
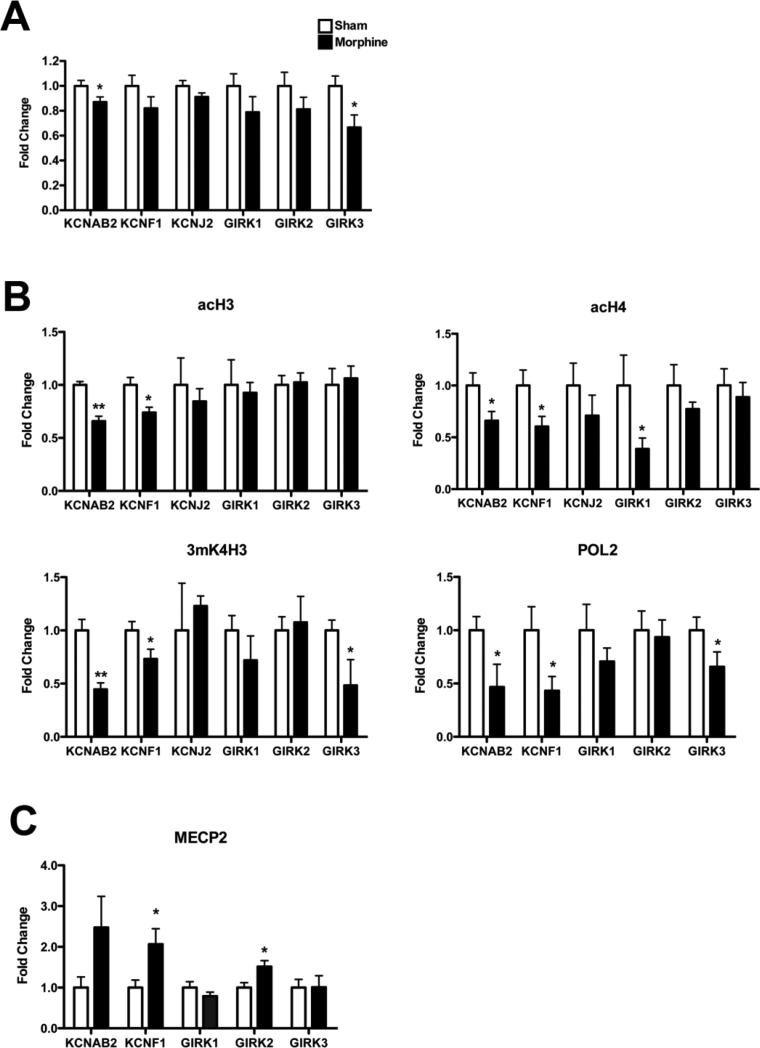
Chronic morphine alters K+ channel expression in VTA
Given the increase in VTA DA neuronal firing rate observed in response to chronic morphine, we examined possible underlying mechanisms. One possibility is that morphine, by downregulating AKT activity in these neurons (Russo et al., 2007), might increase GABAA currents, as demonstrated previously (Krishnan et al., 2008). Another possibility is that K+ channels may be modulated, since many conditions associated with altered neuronal excitability involve changes in K+ channel expression (Luscher and Slesinger, 2010). To test this possibility, we examined VTA from mice that received sham or morphine pellets and analyzed by PCR the expression of K+ channels whose regulation has been implicated in other systems. We observed a significant decrease in expression levels of two K+ channel subunits, KCNAB2 and GIRK3, with a trend seen for several others (Figure 3A).
Figure 3. Chronic Morphine Decreases the Expression of K+ Channel Subunits in VTA.
(A) RT-PCR analysis revealed a significant decrease in levels of KCNAB2 and GIRK3 mRNA in the mouse VTA following chronic morphine. Student's t-test, *p<0.05, n=9-11 mice/group. (B) Epigenetic changes associated with increased gene expression were significantly decreased at the promoters of KCNAB2, KCNF1, GIRK1, and GIRK3 genes in VTA by chronic morphine. Antibodies to acH3, acH4, 3mK4H3, and POL2 were used for ChIP. Student's t-test, *p<0.05, **p<0.01, n=3-7 samples/group (4-5 rats pooled/sample). (C) An epigenetic change consistent with decreased expression (MeCP2 binding) was increased at the KCNF1 and GIRK2 gene promoters in VTA by chronic morphine. Student's t-test, *p<0.05, n=3-4 samples/group (4-5 rats pooled/sample).
To examine whether decreased K+ channel expression is regulated at the transcriptional level, we performed chromatin immunoprecipitation (ChIP) on VTA dissected from sham- and morphine-treated rats. Overall, we observed epigenetic changes consistent with K+ channel downregulation (Figure 3B,C). Modifications consistent with increased transcription—acetylation of histones H3 and H4, trimethylation of Lys-4 of H3, and binding of RNA polymerase II (POL2)—were significantly decreased at the KCNAB2 and KCNF1 promoters (Figure 3B) and decreased trimethylation of Lys-4 of H3 and binding of RNA polymerase II (POL2) was observed at the GIRK3 promoter. These changes suggest that, in addition to morphine potentially reducing GABAA responses in VTA DA neurons, expression of specific K+ channel subunits is reduced via transcriptional mechanisms to further mediate enhanced excitability of these neurons.
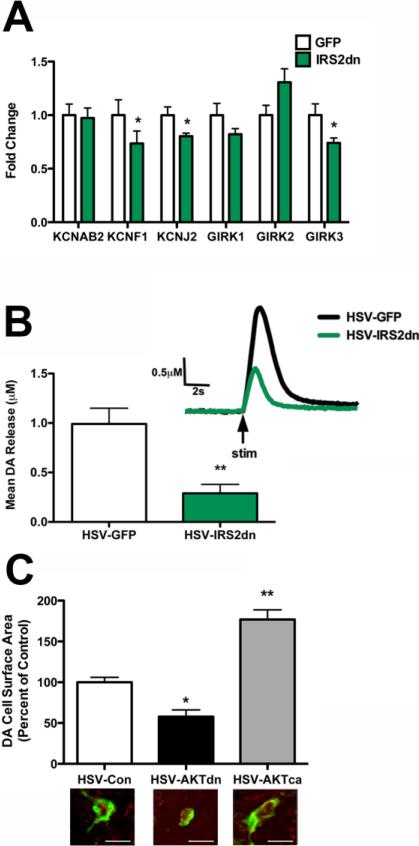
Since both chronic morphine and decreased AKT signaling increase VTA DA neuron firing rate, we next examined whether decreasing AKT activity also decreases K+ channel expression similarly to chronic morphine. To test this possibility, we analyzed VTA from mice that had received intra-VTA injections of either HSV-GFP or HSV-IRS2dn. We overexpressed IRS2dn because this is the most direct way of reducing AKT activity without affecting total levels of the enzyme, as seen with chronic morphine. We observed a significant decrease in levels of expression of three K+ channel subunits, KCNF1, KCNJ2, and GIRK3 (Figure 4A). These data suggest that, in addition to altering DA neuronal activity via GABAA channel regulation, altering AKT signaling can also modulate K+ channel expression.
Figure 4. VTA DA Neuron Firing Rate, Cell Morphology, and Output to NAc are Functionally Linked.
(A) Decreased AKT signaling in VTA via HSV-IRS2dn induced a significant decrease in levels of KCNF1, KCNJ2, and GIRK3 by RT-PCR. Student's t-test, *p<0.05, n=8-10 mice/group. (B) HSV-IRS2dn in VTA, which reduces VTA DA soma size (Russo et al., 2007), significantly decreased electrically-evoked DA release in NAc. Student's t-test, **p<0.01, n=6 rats (66 observations/condition). Representative traces are shown above graph. (C) Modulation of AKT activity in the mouse VTA regulated DA soma size. Intra-VTA injections of HSV-AKTdn significantly decreased, while HSV-AKTca increased soma size. One-way ANOVA, Dunnett's post-hoc test. *p<0.05, **p<0.01 compared to HSV-Con, n=4-6 mice/group (23-28 cells/group). All scale bars are 20μm.
Finally, since both chronic morphine and decreased IRS2/AKT signaling control VTA DA neuronal morphology and excitability, we determined whether decreased AKT signaling also affects DA output to NAc. As found with chronic morphine, HSV-IRS2dn in VTA decreased electrically-evoked DA output in rat NAc (Figure 4B).
Based on our prior research in rats showing that IRS2 downregulation mediates the chronic morphine-induced decrease in VTA DA soma size (Russo et al., 2007), we assumed that this morphological change was likewise dependent on AKT downregulation. To verify this directly, we virally overexpressed either a dominant-negative (AKTdn) or constitutively-active (AKTca) AKT mutant and examined VTA DA neuron morphology. As predicted, AKTdn significantly decreased VTA soma size, while AKTca increased it (Figure 3F). Together, these data establish that chronic morphine and reduced IRS2/AKT signaling decrease VTA DA soma size, K+ channel expression, and DA output to NAc.
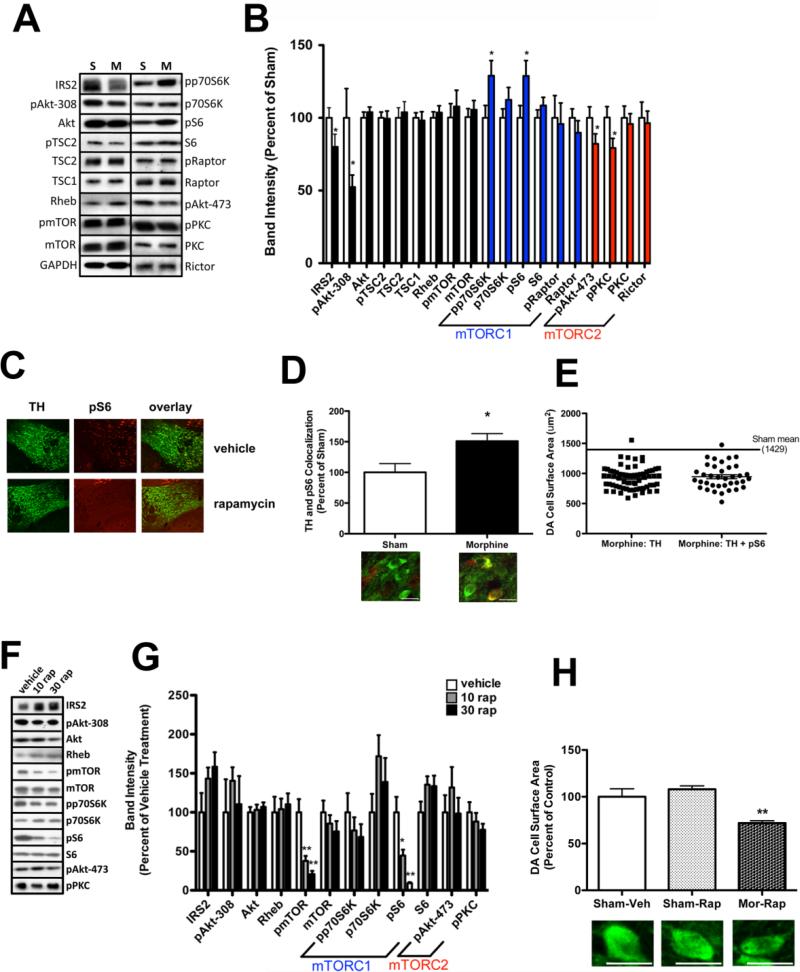
Chronic morphine alters mTOR signaling in VTA
To investigate other signaling changes associated with IRS2/AKT that mediate morphological and physiological adaptations to opiates, we first collected VTA from chronic morphine-treated rats. Consistent with previous observations (Russo et al., 2007; Wolf et al., 1999), we found a morphine-induced decrease in levels of total IRS2 and of phospho-AKT, with no change in total levels of AKT, in VTA (Figure S1A). The decrease in phospho-AKT was associated, as would be expected, with a decrease in levels of phospho-glycogen synthase kinase-3β (GSK3β), a major downstream target of AKT, with no change in total GSK3β levels. Another indirect downstream target of AKT is mTORC1. However, in contrast to an expected decrease in mTORC1 activity, we obtained evidence for increased mTORC1 signaling in VTA in response to chronic morphine, based on increased levels of phospho-S6 and phospho-4EBP (Figure S1A). Total levels of S6 and 4EBP were also increased, as was the positive regulator of mTORC1 activity, ras homolog enriched in brain (Rheb). There was also a non-significant trend for increased phosphomTOR and phospho-p70S6K, a direct target of mTORC1. These data indicate that morphine increases mTORC1 signaling in VTA coincident with a decrease in upstream IRS2/AKT signaling.
We determined whether these changes in IRS2/AKT and mTORC1 signaling were specific to VTA or were a generalized response to chronic opiates. In contrast to VTA, we did not observe any opiate-induced changes in the IRS2/AKT/mTORC1 signaling pathway in NAc (Figure S1B), suggesting some specificity of opiate-induced adaptations within the brain reward circuit.
We next examined whether chronic morphine produced comparable biochemical changes in mice. We found, analogous to data from rats, that levels of IRS2 and phospho-AKT (Thr-308) were decreased in mouse VTA by chronic morphine, while levels of phospho-S6 were increased (Figure 5A,B). Total levels of AKT and S6 were unaffected. We also observed increased levels of phospho-p70S6K. In contrast, we observed no morphine regulation of proteins immediately upstream of mTORC1, including Rheb, TSC1, or TSC2. Note that we were unable to assess levels of phospho- and total 4EBP in mouse VTA, since available antibodies did not yield a reliable signal.
Figure 5. Morphine Regulation of mTORC1 and mTORC2 Activity in VTA.
(A/B) Chronic morphine decreased IRS2 and phospho-AKT in the mouse VTA, while mTORC1 signaling is increased (blue) and mTORC2 signaling is decreased (red). Student's t-test, *p<0.05, n=9-29 mice/group. Representative blots are shown in (A) and means are shown in (B). (C) mTORC1 activity was further assessed in the mouse VTA by immunohistochemical labeling of phospho-S6. VTA sections were labeled for phospho-S6 (red) and tyrosine hydroxylase (TH) (green). Phospho-S6 labeling was specific, as treatment with the mTORC1 inhibitor rapamycin (30 mg/kg daily, 6 days) eliminated the signal detected in VTA. (D) The proportion of TH and phospho-S6 colabeled cells increased in mice treated with chronic morphine. Student's t-test, *p<0.05, n=9 mice/group (9-29 colabeled cells/mouse). Representative scans are shown below the bar graph. (E) Soma size did not differ between phospho-S6-+ and - cells. n=9 mice, (3-9 cells/mouse). (F/G) Rapamycin (10 or 30 mg/kg daily, 6 days) decreased mTORC1 signaling in VTA without affecting mTORC2. One-way ANOVA, Tukey's post-hoc test, *p<0.05, **p<0.01, ***p<0.001 compared to vehicle treatment, n=8 mice/group. Representative blots are shown in (F). (H) Rapamycin treatment does not prevent the morphine-induced decrease in DA soma size. Mice were pretreated with rapamycin for 5 days before pelleting for morphine. One-way ANOVA, Tukey's post-hoc test, **p<0.01 compared to both Sham-Veh and Sham-Rap, n=2-4 mice/group (5-18 cells/group). Representative cells are shown below bars. All scale bars are 20μm.
Since mTOR forms two distinct signaling complexes, mTORC1 and mTORC2, we investigated whether activity of both complexes was altered by chronic morphine. While the Thr-308 site of AKT is phosphorylated by PDK, the Ser-473 site is a substrate of mTORC2, and phosphorylation of both sites is associated with increased AKT catalytic activity (Sarbassov et al., 2005b). As with the Thr-308 site, we observed a morphine-induced decrease in levels of phospho-AKT at Ser-473 in VTA (Figure 4A/B). Chronic morphine also decreased the phosphorylation state of another target of mTORC2, PKCα, in this brain region. We did not detect any changes in levels of phospho- or total mTOR, nor changes in its associated proteins, Raptor or Rictor. Together, these data show that chronic morphine decreases AKT signaling in VTA, which is associated with an increase in mTORC1 signaling but a decrease in mTORC2 signaling. Importantly, we did not observe any changes in IRS2/AKT, mTORC1, or mTORC2 signaling in VTA of mice that overexpressed dnK (Figure S1C), suggesting that increased VTA neuronal activity per se is not sufficient to induce changes in these signaling pathways. While it is well established that IRS2/AKT signaling is an upstream mediator of mTORC1 activity, regulation of mTORC2 activity is not well defined. It has been suggested that decreased growth factor signaling may decrease mTORC2 activity through reduced phosphatidylinositol-3-kinase (PI3K) activity (which is downstream of IRS2) (Foster and Fingar, 2010; Oh and Jacinto, 2011). In support of this possibility, we found that IRS2dn overexpression in cultured pheochromocytoma cells decreases phospho-AKT at its mTORC2 (Ser-473) site (Russo et al., 2007). When we overexpresssed IRS2dn in mouse VTA, we observed the expected decrease in phospho-AKT Thr-308 (GFP:100.0±8.8% n=5, IRS2dn:65.7±7.6% n=8, t-test, p<0.05), plus a trend for decreased phospho-AKT Ser-473 (GFP:100.0±7.5 n=5, IRS2dn:68.8±11.4% n=8, t-test, p=0.07), suggesting that this regulation may also occur in VTA in vivo.
Since the increase in mTORC1 signaling was unexpected given the decreases in phospho-AKT and VTA DA soma size, we determined whether induction of mTORC1 activity was occurring within VTA DA neurons. We performed immunohistochemistry on VTA sections taken from morphine- or sham-treated mice and found increased colocalization of phospho-S6 and tyrosine hydroxylase (TH), a marker of DA neurons, in response to chronic morphine (Figure 5D). The specificity of the phospho-S6 signal was validated by rapamycin (a selective inhibitor of mTORC1): sections from mice treated with rapamycin (30 mg/kg, i.p. daily, 6 days) showed no detectable phospho-S6 signal within VTA (Figure 5C). Further, the morphine-induced increase in phospho-S6+ cells was specific for TH+ cells within VTA, as there was no evidence for an increase in the number of phospho-S6+, TH– cells (sham: 2.39±0.69 cells/scan, morphine: 1.5±0.31 cells/scan, N=18 mice, p>0.1). However, there was no difference in mean soma size of TH+ DA neurons that were either phospho-S6+ or – (Figure 5E), showing that phospho-S6 status was not correlated to DA soma size.
We next used rapamycin to directly assess whether the increase in mTORC1 activity was integral to the morphine-induced morphology changes. We administered rapamycin (10 or 30 mg/kg i.p. daily for 6 days) to mice and found the expected dose-dependent decrease in levels of phospho-mTOR and phospho-S6 in VTA (Figure 5F/G). We did not observe a significant decrease in phospho-p70S6K, but this may be due to an increase in total p70S6K levels induced by this treatment. This effect of rapamycin was specific for mTORC1, since there was no evidence of altered mTORC2 activity, based on normal levels of phospho-AKT (Ser-473) and phospho-PKCα, in VTA. Rapamycin treatment of morphine-naïve mice had no effect on VTA DA cell surface area, demonstrating that decreasing mTORC1 activity per se is not sufficient to alter the size of these neurons (Figure 5H). Further, when mice were pretreated with rapamycin and then treated chronically with morphine, we still observed the expected morphine-induced decrease in DA soma size. These findings show that preventing the morphine-induced increase in mTORC1 signaling in VTA does not block the morphine-induced decrease in soma size.
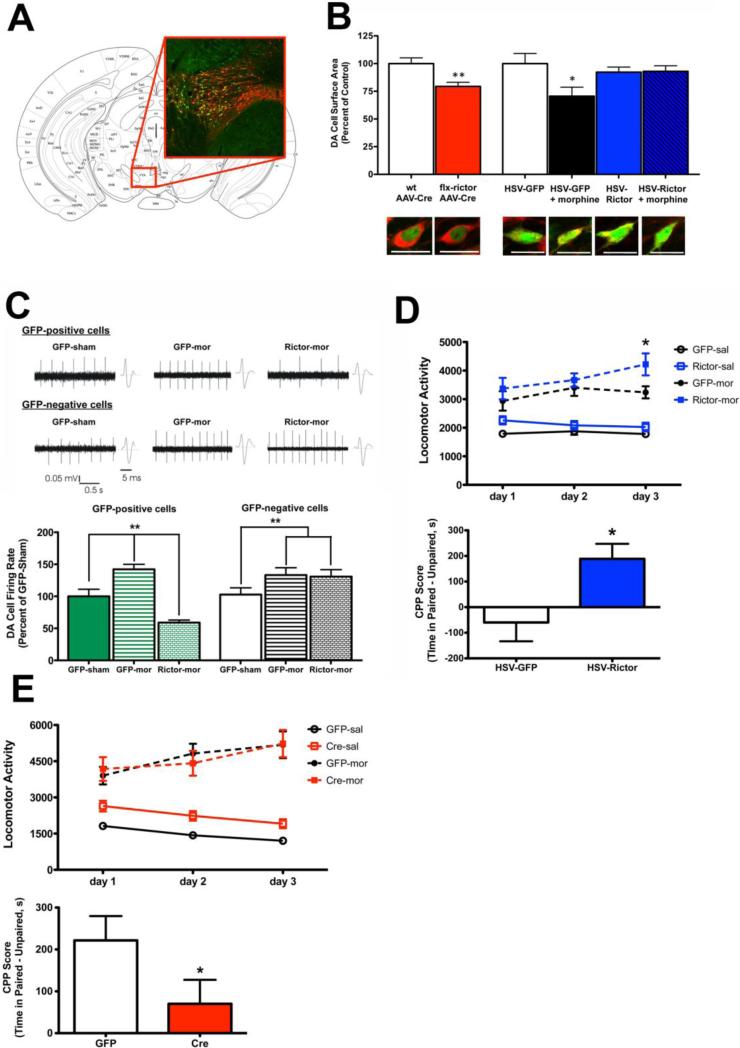
mTORC2 activity regulates morphine-induced changes in cell morphology, cell physiology, and behavior
Since there is no selective small molecule inhibitor of mTORC2, we used a conditional neuronal knockout strategy, with recently developed floxed-Rictor mice (Siuta et al., 2010) to directly study the contribution of mTORC2 in morphine action. Knocking out Rictor enables a selective reduction in mTORC2 activity, without any discernable effect on mTORC1. To achieve a local knock-out of Rictor from VTA, we injected AAV-Cre into VTA of floxed-Rictor mice or into wild-type littermates as a control (Figure 6A). Knock-out was validated by RT-PCR and western blot analysis, where we observed a significant decrease in Rictor mRNA in VTA and decreased phosphorylation of the mTORC2 substrates AKT (Ser-473) and PKCα (Figure S2A). Local Rictor knock-out also decreased DA cell surface area by ~20% (Figure 6B). We next developed an HSV to overexpress Rictor-T1135A. This Rictor mutant increases mTORC2 activity, and lacks the p70S6K phosphorylation site, eliminating the possibility of mTORC1 negative feedback regulation of mTORC2 (see Discussion). This vector increased Rictor expression and mTORC2 signaling in VTA (Figure S2B), and blocked the morphine-induced decrease in DA neuron soma size (Figure 6B). These results demonstrate that downregulation of mTORC2 signaling in VTA is both necessary and sufficient for mediating the morphine-induced decrease in DA soma size.
Figure 6. Downregulation of mTORC2 Activity Mediates Morphine Effects on VTA Morphology and Neuronal Activity and on Reward Behavior.
(A) Viral-mediated overexpression was used to target the mouse VTA. Inset shows DA neurons of VTA (red) and AAV-Cre (green). (B) Local knockout of Rictor in floxed-Rictor mice, achieved via AAV-Cre injection into VTA, decreased VTA DA soma size compared to wild-type injected mice. Student's t-test *p<0.05 compared to wild-type mice, n=2 (wild-type) or 4 (floxed-Rictor) mice/group (6-13 cells/mouse). Representative cells are shown below bars. HSV-Rictor-T1135A blocked the decrease in VTA DA soma size induced by morphine. One-way ANOVA, Dunnett's post-hoc *p<0.05 GFP-sham compared to GFP-morphine, n=4-6 mice/group (2-9 cells/mouse). (C) HSVRictor-T1135A also blocked the morphine-induced increase in DA neuron firing rate. One-way ANOVA, Tukey's post-hoc test, **p<0.01, n= 4-7 mice/group (3-14 cells/mouse). (D) Rictor-T1135A in VTA induced morphine place conditioning to a low dose of morphine (5 mg/kg, i.p.) that did not induce preference in GFP-treated mice. Rictor-T1135A also increased morphine-induced locomotor activity. Top panel, mean locomotor activity. Two-way repeated measures ANOVA, treatment variable significant, Bonferroni post-test, day 3 Rictor vs. GFP, *p<0.05, n=12-13 mice/group. Bottom panel, place preference, n= 9-10 mice/group, Student's t-test, *p<0.01. (E) Local knockout of Rictor in floxed-Rictor mice significantly decreased morphine CPP without affecting morphine locomotor activity (15 mg/kg i.p.). Top panel, mean locomotor activity, Two-way repeated measures ANOVA p>0.05, n=12-13 mice/group, bottom panel, CPP, n=12-13 mice/group, Student's t-test, *p<0.05. All scale bars are 20 μm.
In addition to the mTOR pathway, another downstream target of AKT that has been observed to affect neuronal size and structure in other systems is GSK3β (van Diepen et al., 2009). Since we observe changes consistent with increased GSK3β activity (decreased phospho-GSK3β, Figure S1A) in VTA after chronic morphine, we studied the possible influence of GSK3β in regulating VTA DA soma size. Overexpression of wild-type GSK3β in VTA, which mimics morphine regulation of the protein, did not alter soma size (Figure S3). Additionally, when we overexpressed a dominant-negative mutant of GSK3β (K85A-K86A) to block the morphine-induced increase in enzyme activity, we still observed the expected decrease in soma size. These data suggest that GSK3β activity in VTA is not involved in morphine-induced changes in the morphology of VTA DA neurons.
To investigate whether mTORC2 downregulation might also contribute to the morphine-induced increase in DA neuron firing rate, we injected HSV-Rictor-T1135A into mouse VTA, treated the mice with sham or morphine pellets, and recorded DA neuron firing rates in acute VTA slices. Similarly to Figure 1C, chronic morphine increased DA neuron firing rate in both GFP-positive and GFP-negative cells compared to sham-treated mice (Figure 6C). However, in cells that overexpressed Rictor, the morphine-induced increase in firing rate was completely abolished (Figure 6C). Further, it was the overexpression of Rictor in the DA neurons themselves driving the effect, as GFP-negative DA neurons from the Rictor-morphine mice still showed the morphine-induced increase in firing rate. These data support a cell-autonomous link between decreased mTORC2 activity and increased VTA DA neuron excitability induced by chronic morphine.
Given that Rictor overexpression prevented morphine-induced changes in VTA neuron morphology and excitability, we next assessed whether altered mTORC2 activity might also affect morphine reward as measured by place conditioning. We found that Rictor overexpression caused a significant place preference to a low dose of morphine (5 mg/kg) that does not induce preference in GFP-injected mice (Figure 6D). Rictor overexpression also increased morphine-induced locomotor activity (Figure 6D). Conversely, local knock-out of Rictor in VTA decreased morphine place preference (15 mg/kg) without affecting locomotor activity (Figure 6E). These data are consistent with our previous findings that treatments that decrease VTA DA soma size—chronic morphine or decreased AKT signaling—decrease morphine reward.
DISCUSSION
Results of the present study establish that chronic morphine induces a pattern of phenotypic changes in VTA DA neurons characterized by decreased soma size, increased cell excitability, and decreased DA output to NAc. The dramatic decrease in DA output is consistent with the profound reward tolerance observed previously (Russo et al., 2007). Such reward tolerance would be expected to lead to an escalation of drug intake to overcome this cellular break, as seen clinically (O'Brien, 2001). These morphine-induced changes in VTA could thus be viewed as homeostatic adaptations to counter the effects of sustained morphine exposure. We provide several lines of evidence that these adaptations to chronic morphine are mediated via downregulation of AKT-mTORC2 signaling in VTA DA neurons. Our data suggest that AKT-mTORC2 downregulation increases the excitability of these neurons in part through the repression of specific K+ channel subunits and that this increased excitability triggers a decrease in VTA soma size, the net effect of which is to decrease DA output and dampen reward. The findings of reduced DA soma size and DA output are consistent with earlier reports that chronic morphine decreases levels of neurofilament proteins in VTA and impairs axoplasmic transport from VTA to NAc (Beitner-Johnson et al., 1992; Beitner-Johnson and Nestler, 1993). Some of these neuroadaptations may also contribute to withdrawal symptoms from chronic morphine, as decreased VTA DA soma size (Spiga et al., 2003), neuronal activity (Diana et al., 1995), and output to NAc (Pothos et al., 1991; Rossetti et al., 1992a, 1992b) are reported in morphine-withdrawn rats.
Opiate-Induced Structural Plasticity and Neuronal Excitability are Linked
Our observation that chronic morphine increases the intrinsic excitability of VTA DA neurons in brain slices is consistent with previous findings of increased VTA neuronal firing rate in morphine-dependent rats in vivo (Georges et al., 2006). Previous data and our current findings suggest that chronic morphine induces this increased excitability of VTA DA neurons by at least two mechanisms: downregulation of AKT which reduces GABAA currents in these neurons (Krishnan et al., 2008), and repression of KCNAB2 and perhaps other K+ channel subunits (Figure 3). The reduced expression of K+ channel genes, which reflects a transcriptional effect based on our ChIP assays, appears to be mediated by reduced AKT signaling, as overexpression of IRS2dn was sufficient to decrease expression of several K+ channel subunits. Downregulation of mTORC2 is also required for the morphine-induced increase in VTA excitability, since Rictor overexpression, which prevented morphine-downregulation of AKT activity, was sufficient to rescue this morphine effect, although whether this action was through AKT modulation of GABAA channels, K+ channels, or another mTORC2 target has yet to be determined. Since we only observed the rescue of firing rate in VTA DA neurons that overexpressed Rictor, and not in nearby GFP-negative DA neurons, we believe that restoration of AKT/mTORC2 activity within DA neurons is sufficient to rescue opiate-induced changes. However, this does not preclude the possible influence of VTA GABA neurons in morphine-induced changes, as our viral manipulations were not specific for DA neurons. For example, HSV-dnK might also increase the activity of VTA GABA neurons, which would then decrease the activity of nearby DA neurons. However, we see a decrease in DA soma size with morphine, which is known to decrease GABA activity, making dnK activation of GABA neurons an unlikely contributor. A direct test of this hypothesis awaits the development of viral vectors that target specific neuronal subpopulations.
Interestingly, we show here that the morphine-induced increase in VTA neuronal firing is integrally linked to the morphine-induced decrease in VTA soma size: overexpression of a K+ channel subunit that inhibits cell firing also prevents the morphine-induced decrease in cell size, while overexpression of a dominant-negative K+ channel that increases cell firing mimics morphine action. There has been a lot of attention in recent years to “homeostatic plasticity,” where the intrinsic activity of a cell adapts to a chronic stimulus in an attempt to compensate for the effects of that stimulus (Turrigiano and Nelson, 2004). Our findings suggest the novel idea that such homeostatic adaptations also involve visible changes in the overall size of neuronal cell bodies, and further establish structural plasticity as a necessary concomitant of plasticity in neuronal excitability. A similar phenomenon was recently described by Coque et al. (2011) in ClockΔ19 mice, which also exhibit decreased VTA DA soma size and increased DA firing rate. The authors observed that lithium treatment rescued both the VTA DA morphological and activity changes, as did overexpression of wild-type Kir2.1.
mTORC2 Activity is Critical for Opiate-induced Changes in VTA Morphology and Excitability
We demonstrated previously that a morphine-induced decrease in IRS2 signaling is an obligatory step in the mechanism by which chronic morphine decreases the size of VTA DA neurons (Russo et al., 2007). We had presumed, based on this study and on reports in other systems, that AKT, a downstream mediator of IRS2, is a key determinant of cell size (Chen et al., 2001; Easton et al., 2005), and that consequent decreased AKT activity—downstream of reduced IRS2 signaling—is responsible for this morphine effect. Indeed, we show here that AKTdn mimics the ability of chronic morphine to decrease VTA cell size. The next step was to determine how a decrease in AKT signaling results in a decrease in VTA DA neuron size. We show that one mechanism may be through increased neuronal excitability as noted above. In addition, our expectation was that a decrease in mTORC1 signaling was also likely to mediate this effect, given the wealth of evidence that mTORC1 signaling plays a critical role in cell growth (Sarbassov et al., 2005a) including neuronal hypertrophy (Kwon et al., 2003; Zhou et al., 2009). Surprisingly, we observed increased phosphorylation of mTORC1 substrates at a time-point when we observe a decrease in VTA soma size. To determine whether this increase could be a compensatory response and actually lead to a decrease in IRS2 and phospho-AKT, as has been shown in cell culture with constitutive Rheb activity (Shah et al., 2004), we pretreated mice with rapamycin and studied its effects on VTA cell size. Rapamycin did not impede the ability of chronic morphine to decrease DA neuron size, suggesting that the increase in mTORC1 signaling is not necessary to induce the soma size changes. Given recent evidence that increased mTORC1 signaling can contribute to neurological and neuropsychiatric conditions (Ehninger et al., 2009; Hoeffer and Klann, 2010; Hoeffer et al., 2008), it is important to investigate whether elevated mTORC1 activity plays a role in other effects of morphine.
In contrast to the morphine-induced increase in mTORC1 activity in VTA, we show here that chronic morphine decreases mTORC2 activity in this brain region, based on reduced phosphorylation of two key substrates for this complex, AKT (Ser-473) and PKCα. This raised the novel possibility that perhaps the downregulation of mTORC2 is responsible for the actions of morphine in VTA. Much less is known about the mTORC2 pathway, largely due to the lack of a specific inhibitor for this enzyme complex and the embryonic lethality of knocking out its constituent proteins. Recently, the importance of mTORC2 signaling in brain has been shown through the use of a conditional knock-out of Rictor (Siuta et al., 2010). Here, we locally knocked out Rictor by injecting AAV-Cre into VTA of adult floxed Rictor mice and showed that this knock-out was sufficient to decrease VTA DA soma size. Conversely, overexpression of Rictor blocked the morphine-induced decrease in soma size as well as the increase in neuronal activity, as noted above, thereby implicating mTORC2 activity in both of these morphine-induced changes. Such a role was further solidified in behavioral studies where we demonstrated that decreased mTORC2 activity decreased morphine reward as measured by conditioned place preference, while increasing mTORC2 activity increased it. These data suggest that mTORC2 activity might play an important role in morphine addiction, a possibility that now warrants direct examination in more sophisticated behavioral paradigms. The mechanism of the morphine-induced decrease in mTORC2 activity remains unknown, although our preliminary evidence suggests that this may be dependent on downregulation of IRS2.
VTA Soma Size is a Homeostatic Adaptation to Chronic Stimulation
While our findings show that shrinkage of VTA DA neurons in response to morphine is closely correlated with important functional consequences, it is not possible technically to demonstrate a direct causal relationship due to the inability to specifically decrease cell size without also altering many other cellular activities. Nevertheless, other groups have corroborated the morphine-induced decrease in DA soma size (Chu et al., 2007; Spiga et al., 2003) and we show here an equivalent decrease in human heroin addicts. Also, similar decreases have been reported in rats after chronic cannabinoid administration (Spiga et al., 2010). Moreover, several molecular manipulations that decrease VTA DA soma size (decreased BDNF, IRS2-AKT signaling, mTORC2 signaling, and K+ channel activity) are associated with increased VTA excitability and reward tolerance. It was also reported recently that acupuncture reverses the morphine-induced decrease in VTA DA soma size and restores morphine reward in opiate-dependent rats (Chu et al., 2007; Hu et al., 2009). Together, these data suggest that the decreased size of VTA DA neurons represents a functionally important, homeostatic adaptation in response to chronic activation of the reward circuit, although definitive proof must await tools that make it possible to experimentally alter cell size per se.
Deciphering Complex Neurotrophic Signaling Pathways in VTA In Vivo
This study is, to our knowledge, the first to show opposite regulation of mTORC1 and mTORC2 signaling in brain. This opposing regulation has been demonstrated in epithelial cells, where mTORC1 signaling was increased and mTORC2 signaling was decreased due to the knockout of Syndecan 4 (Partovian et al., 2008). Interestingly, it was noted that epithelial cell size was decreased, suggesting that decreased mTORC2 signaling, even in the presence of increased mTORC1 signaling, is capable of decreasing cell size. Recent evidence, in cultured cells, suggests that the interplay between these two mTOR complexes may be mediated in part by the ability of the mTORC1 substrate p70S6K to phosphorylate Rictor at residue Thr-1135 (Dibble et al., 2009; Julien et al., 2010; Treins et al., 2010). Such phosphorylation of Rictor may decrease mTORC2 activity, as two groups have found that mutation of Thr-1135 to Ala increases phosphorylation of AKT at Thr-473, an mTORC2 specific site (Dibble et al., 2009; Julien et al., 2010), although other groups do not observe such an alteration in mTORC2 activity (Boulbes et al., 2010; Treins et al., 2010).
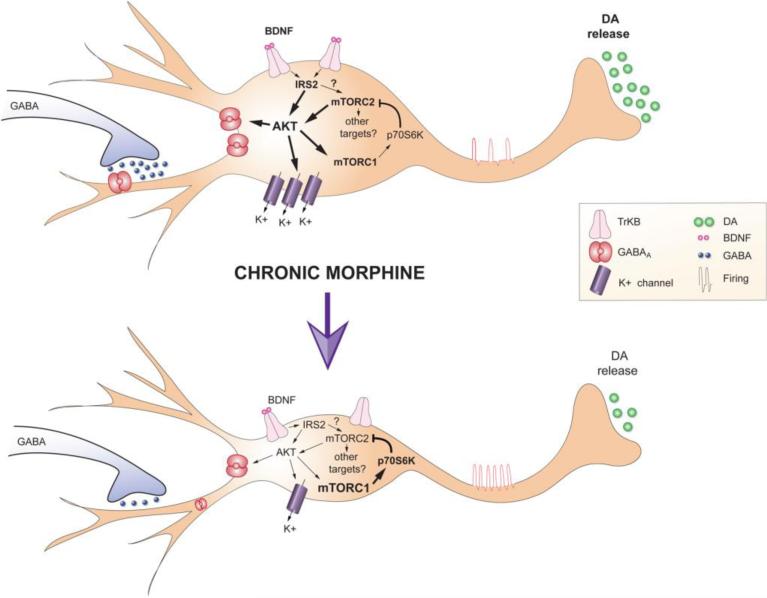
The potential interplay between mTORC1 and mTORC2 signals highlights the complexity of dissecting their roles in the opiate-mediated effects in VTA in vivo. We propose the model depicted in Figure 7. Chronic opiates, through a reduction in BDNF signaling, reduce AKT activity via reduced phosphorylation at its two main sites. This occurs through two mechanisms: a decrease in total levels of IRS2 and a decrease in mTORC2 activity. These mechanisms may not be functionally distinct, as downregulation of IRS2 may also lead to decreased mTORC2 activity, consistent with the idea that phosphorylation of the two AKT sites occurs sequentially (Pearce et al., 2010; Oh and Jacinto, 2011). Reduced AKT-mTORC2 activity then increases VTA neuronal excitability via reduced phosphorylation of GABAA β-subunits (Krishnan et al., 2008; Wang et al., 2003) and decreased expression of K+ channels. Whether mTORC2 decreases VTA DA activity only via AKT modulation of GABAA and K+ channel activity or via additional mechanisms has yet to be determined. Such increased VTA DA neuron excitability directly triggers shrinkage in the soma size of these neurons, which we propose is a key cellular adaptation that impairs DA output to target regions and mediates reward tolerance. Given that mTORC2's first noted function was in regulating actin cytoskeleton organization (Sarbassov et al., 2004), decreased mTORC2 activity may alter VTA DA morphology independent of AKT and cell excitability, but this will require identification of additional mTORC2 substrates, a major gap of knowledge in the field. This scheme leaves unanswered two key questions. By what mechanism does chronic morphine repress IRS2 expression, and by what mechanism does chronic morphine induce mTORC1 activity despite a reduction in AKT signaling and lack of alteration in several other upstream proteins. The two events may be related, since induction of mTORC1 has been shown to decrease IRS2 in cultured cells via increased degradation of the protein (Shah et al., 2004), however, we see no effect of rapamycin on morphine-induced downregulation of the AKT-mTORC2 pathway.
Figure 7. Working Model of Chronic Morphine-Induced Adaptations in VTA DA Neurons.
Chronic morphine decreases VTA DA soma size yet increases neuronal excitability, while DA transmission to NAc is decreased. The net effect of morphine is a less responsive reward pathway, i.e., reward tolerance. Downregulation of IRS2-AKT signaling in VTA mediates the effects of chronic morphine on soma size and electrical excitability; the effect on excitability is mediated via decreased GABAA currents and suppression of K+ channel expression. Morphine-induced downregulation of mTORC2 activity in VTA is crucial for these morphine-induced morphological and physiological adaptations as well as for reward tolerance. In contrast to mTORC2, chronic morphine increases mTORC1 activity, which does not influence these morphine-induced adaptations.
Clearly, delineating these complex signaling pathways underlying chronic morphine regulation of VTA DA neurons is very difficult using an in vivo paradigm, yet morphine regulation of VTA DA soma size is not observed in cultured neurons (unpublished observations), demonstrating the unique importance of focusing on in vivo systems. Indeed, we show here unique patterns of regulation of IRS2/AKT/mTOR signaling in VTA DA neurons in response to chronic morphine in vivo. Our evidence for a novel role of mTORC2 signaling in mediating morphine's regulation of VTA DA neuron excitability and size raises fundamentally new approaches for the development of treatment agents that counteract these effects of chronic morphine and its important downstream functional consequences related to opiate addiction.
EXPERIMENTAL PROCEDURES
Subjects and Drugs
For all experiments, animals were male, fed ad libitum, and kept on a 12-hour light/dark cycle. Sprague-Dawley rats (250-275 g, Charles River) and 8-9 week c57BL/6 mice (Jackson Labs) were given s.c. morphine pellets (75 mg or 25 mg, respectively) as described previously (McClung et al., 2005, Fischer et al., 2008). Homozygous floxed-Rictor mice and wild-type littermates were generated as described previously (Shiota et al., 2006; Siuta et al., 2010). See Supplemental Methods for further details.
Human Postmortem Study
Human specimens were obtained from the Forensic Medicine Departments of Semmelweis University (Budapest, Hungary) and of Karolinska Institutet (Stockholm, Sweden) under approved local protocols (Horvath et al., 2007). Fresh-frozen brain sections (20 μm) were analyzed from control or heroin-overdose subjects. All samples had a postmortem interval (PMI) of <24 hr and were tested for common drugs of abuse and therapeutic drugs; demographic data are given in Supplemental Table 1.
Viral-Mediated Gene Transfer
For stereotaxic surgeries, mice were anaesthetized with ketamine (100 mg/kg) and xylazine (100 mg/kg) and VTA was targeted using established coordinates. Bilateral 33 g syringes were used to infuse HSV at a flow rate of ~0.1 μl/min. HSV vectors encoding GFP, IRS2dn, AKTdn, AKTca, dnK, Kir2.1, GSK3β, and GSK3βdn have been previously used and validated (Krishnan et al., 2007; Russo et al., 2007). Rictor cDNA (T1135A mutant) was provided by Dr. Brandon Manning (Harvard) and was cloned into the p1005 HSV vector. Rictor overexpression was verified by RT-PCR and western blot analysis (Supplemental Figure 2B). AAV-GFP and AAV-Cre-GFP were used as described previously (Berton et al., 2006).
Western Blotting
Tissue was collected and processed as described previously (Krishnan et al., 2008; Russo et al., 2007). Samples were processed in RIPA buffer, quantified, electrophoresed, transferred to PVDF, and blotted using standard procedures.
Immunohistochemistry and Confocal Microscopy
Mice were perfused and sections (30 μm) sections containing VTA were selected for analysis. Immunohistochemistry was completed for TH, GFP, and/or Cre and DA cell size analysis was completed as described previously (Russo et al., 2007). For colocalization studies, sections were incubated with antibodies to TH and phospho-S6, confocal scans were obtained, and the number of TH+, p-S6+, and dual-labeled cells were counted by a blind observer.
Electrophysiology
Mice were implanted with sham or morphine pellets, perfused ~48 hours later with cold artificial CSF (aCSF), and 250 μm slices containing VTA were cut and transferred into a recording chamber containing aCSF, 5 μM morphine, or the opioid receptor antagonist naloxone (1 μM). The firing rates of VTA DA neurons from sham- or morphine-pelleted mice were determined using extracellular single unit recording and for Kir2.1 channel studies, single unit recordings were obtained from DA neurons in VTA slice cultures generated ~48 hours after the last pellet, as described previously (Krishnan et al., 2007). For HSV-Rictor-T1135A studies, mice were pelleted with sham or morphine ~48 hour after HSV injection, perfused ~48 later and VTA slices were made. VTA DA firing rate of GFP-+ and - neurons was determined by cell-attached recording configuration as described previously (Cao et al., 2010).
Voltammetric Assessment of DA Release
3-4 days following viral surgery, rats were anesthetized with urethane (300 μg/kg), placed in a stereotactic frame, and prepared for recordings of electrically-evoked DA transmission using fast-scan cyclic voltammetry (Cheer et al., 2004). For morphine studies, rats were pelleted as described above, then anesthetized 3-7 days later, a time range previously shown to exhibit decreased DA soma size (Russo et al., 2007). A bipolar stainless-steel stimulating electrode was advanced to VTA, a glass-encased cylindrical carbon fiber microelectrode targeted the medial shell of the NAc and a reference electrode (Ag/AgCl) was inserted the right hemisphere posterior to Bregma. Electrical stimulation of VTA was delivered through the stimulating electrode and DA release was evoked using trains of 60 bipolar pulses of 300 μA amplitude at 60 Hz. DA was detected using fast-scan cyclic voltammetry at the carbon fiber micro-electrode. The two hemispheres were recorded from successively and the order of recording was counterbalanced across rats. Experiments were only included in analysis when a full set of dorso-ventral recordings from both hemispheres was obtained.
RNA Isolation and Quantitative Real-Time PCR
Punches from rat or mouse VTA were homogenized in Trizol and processed according to the manufacturer's protocol. RNA was then purified using RNAesy Micro columns (Qiagen) and quality was assessed by spectroscopy. RNA was the reverse transcribed (iScript, BioRad) and quantified by quantitative PCR using SYBR green. Glyceraldehyde-3-phosphate was utilized as a normalization control and all samples were run in triplicate and analyzed using the ΔΔCt method as described previously (Tsankova et al., 2006).
Chromatin Immunoprecipitation
Tissue punches were obtained from rat VTA, cross-linked with 1% formaldehyde, quenched with 2 M glycine, and frozen at -80°C as described previously (Tsankova et al., 2006). Briefly, punches were pooled (4-5 rats/sample) and chromatin was sonicated to ~500 bp. Sonicated chromatin was immunoprecipitated, Dynabeads (Invitrogen) were used to collect the immunoprecipitates, and chromatin was reverse crosslinked. DNA was then purified and quantified using real-time PCR.
Conditioned Place Preference (CPP)
Morphine CPP was completed as described previously (Kelz et al., 1999). Briefly, mice were placed in a three-chambered CPP box for 20 minutes to assess pre-test preferences and ensure that there was no chamber bias. For the next three days mice were restrained to one chamber for 45 minutes in both the morning (saline) and the afternoon (5 or 15 mg/kg morphine). Locomotor activity was assessed during each pairing session. On day 5 mice were placed in the center chamber and allowed to move throughout the chamber for a twenty-minute test session. Data are represented as time spent in the paired – time spent in the unpaired chamber.
Statistics
All values reported are mean ± SEM. Unpaired Student t-tests were used for the analysis of studies with two experimental groups. One-way analysis of variance (ANOVA) was used for analysis of three or more groups, followed by Tukey or Dunnett's post-hoc tests, when appropriate. Main effects were considered significant at p<0.05. For the locomotor activity data, a repeated-measures two-way ANOVA was completed (main effects and interaction considered significant at p<0.05) followed by Bonferroni post-test, if appropriate.
Supplementary Material
HIGHLIGHTS.
- Morphine decreases VTA DA soma size, increases cell activity and decreases DA output
- Morphine and reduced IRS2/AKT activity decrease K+ channel expression in the VTA
- Morphine increases mTORC1 and decreases mTORC2 signaling in the VTA
- Decreased mTORC2 signaling in the VTA mediates morphine-induced adaptations
ACKNOWLEDGEMENTS
We thank Ezekiell Mouzon and Veronica Szarejko for excellent technical and artistic assistance. This work was supported by grants from the National Institute on Drug Abuse (R01 DA14133 (EJN), F32 DA025381 (MMR)), and a Rubicon Grant from the Dutch Scientific Organization (CSL).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Beitner-Johnson D, Guitart X, Nestler EJ. Neurofilament proteins and the mesolimbic dopamine system: common regulation by chronic morphine and chronic cocaine in the rat ventral tegmental area. J Neurosci. 1992;12:2165–2176. doi: 10.1523/JNEUROSCI.12-06-02165.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beitner-Johnson D, Nestler EJ. Chronic morphine impairs axoplasmic transport in the rat mesolimbic dopamine system. Neuroreport. 1993;5:57–60. doi: 10.1097/00001756-199310000-00014. [DOI] [PubMed] [Google Scholar]
- Berton O, McClung CA, Dileone RJ, Krishnan V, Renthal W, Russo SJ, Graham D, Tsankova NM, Bolanos CA, Rios M, et al. Essential role of BDNF in the mesolimbic dopamine pathway in social defeat stress. Science. 2006;311:864–868. doi: 10.1126/science.1120972. [DOI] [PubMed] [Google Scholar]
- Boulbes D, Chen CH, Shaikenov T, Agarwal NK, Peterson TR, Addona TA, Keshishian H, Carr SA, Magnuson MA, Sabatini DM, Sarbassov dos D. Rictor phosphorylation on the Thr-1135 site does not require mammalian target of rapamycin complex 2. Mol Cancer Res. 2010;8:896–906. doi: 10.1158/1541-7786.MCR-09-0409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao JL, Vialou VF, Lobo MK, Robison AJ, Neve RL, Cooper DC, Nestler EJ, Han MH. Essential role of the cAMP-cAMP response-element binding protein pathway in opiate-induced homeostatic adaptations of locus coeruleus neurons. Proc Natl Acad Sci U S A. 2010;107:17011–17016. doi: 10.1073/pnas.1010077107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheer JF, Wassum KM, Heien ML, Phillips PE, Wightman RM. Cannabinoids enhance subsecond dopamine release in the nucleus accumbens of awake rats. J Neurosci. 2004;24:4393–4400. doi: 10.1523/JNEUROSCI.0529-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen WS, Xu PZ, Gottlob K, Chen ML, Sokol K, Shiyanova T, Roninson I, Weng W, Suzuki R, Tobe K, et al. Growth retardation and increased apoptosis in mice with homozygous disruption of the Akt1 gene. Genes Dev. 2001;15:2203–2208. doi: 10.1101/gad.913901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu NN, Zuo YF, Meng L, Lee DY, Han JS, Cui CL. Peripheral electrical stimulation reversed the cell size reduction and increased BDNF level in the ventral tegmental area in chronic morphine-treated rats. Brain Res. 2007;1182:90–98. doi: 10.1016/j.brainres.2007.08.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coque L, Mukherjee S, Cao JL, Spencer S, Marvin M, Falcon E, Sidor MM, Birnbaum SG, Graham A, Neve RL, et al. Specific Role of VTA Dopamine Neuronal Firing Rates and Morphology in the Reversal of Anxiety-Related, but not Depression-Related Behavior in the ClockDelta19 Mouse Model of Mania. Neuropsychopharmacology. 2011;36:1478–1488. doi: 10.1038/npp.2011.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diana M, Pistis M, Muntoni A, Gessa G. Profound decrease of mesolimbic dopaminergic neuronal activity in morphine withdrawn rats. J Pharmacol Exp Ther. 1995;272:781–785. [PubMed] [Google Scholar]
- Dibble CC, Asara JM, Manning BD. Characterization of Rictor phosphorylation sites reveals direct regulation of mTOR complex 2 by S6K1. Mol Cell Biol. 2009;29:5657–5670. doi: 10.1128/MCB.00735-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Easton RM, Cho H, Roovers K, Shineman DW, Mizrahi M, Forman MS, Lee VM, Szabolcs M, de Jong R, Oltersdorf T, et al. Role for Akt3/protein kinase Bgamma in attainment of normal brain size. Mol Cell Biol. 2005;25:1869–1878. doi: 10.1128/MCB.25.5.1869-1878.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehninger D, de Vries PJ, Silva AJ. From mTOR to cognition: molecular and cellular mechanisms of cognitive impairments in tuberous sclerosis. J Intellect Disabil Res. 2009;53:838–851. doi: 10.1111/j.1365-2788.2009.01208.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer SJ, Arguello AA, Charlton JJ, Fuller DC, Zachariou V, Eisch AJ. Morphine blood levels, dependence, and regulation of hippocampal subgranular zone proliferation rely on administration paradigm. Neuroscience. 2008;151:1217–1224. doi: 10.1016/j.neuroscience.2007.11.035. [DOI] [PubMed] [Google Scholar]
- Foster KG, Fingar DC. Mammalian target of rapamycin (mTOR): conducting the cellular signaling symphony. J Biol Chem. 2010;285:14071–14077. doi: 10.1074/jbc.R109.094003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Georges F, Le Moine C, Aston-Jones G. No effect of morphine on ventral tegmental dopamine neurons during withdrawal. J Neurosci. 2006;26:5720–5726. doi: 10.1523/JNEUROSCI.5032-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoeffer CA, Klann E. mTOR signaling: at the crossroads of plasticity, memory and disease. Trends Neurosci. 2010;33:67–75. doi: 10.1016/j.tins.2009.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoeffer CA, Tang W, Wong H, Santillan A, Patterson RJ, Martinez LA, Tejada-Simon MV, Paylor R, Hamilton SL, Klann E. Removal of FKBP12 enhances mTOR-Raptor interactions, LTP, memory, and perseverative/repetitive behavior. Neuron. 2008;60:832–845. doi: 10.1016/j.neuron.2008.09.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvath MC, Kovacs GG, Kovari V, Majtenyi K, Hurd YL, Keller E. Heroin abuse is characterized by discrete mesolimbic dopamine and opioid abnormalities and exaggerated nuclear receptor-related 1 transcriptional decline with age. J Neurosci. 2007;27:13371–13375. doi: 10.1523/JNEUROSCI.2398-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, Chu NN, Sun LL, Zhang R, Han JS, Cui CL. Electroacupuncture treatment reverses morphine-induced physiological changes in dopaminergic neurons within the ventral tegmental area. Addict Biol. 2009;14:431–437. doi: 10.1111/j.1369-1600.2009.00163.x. [DOI] [PubMed] [Google Scholar]
- Hyman SE, Malenka RC, Nestler EJ. Neural mechanisms of addiction: the role of reward-related learning and memory. Annu Rev Neurosci. 2006;29:565–598. doi: 10.1146/annurev.neuro.29.051605.113009. [DOI] [PubMed] [Google Scholar]
- Johnson SW, North RA. Opioids excite dopamine neurons by hyperpolarization of local interneurons. J Neurosci. 1992;12:483–488. doi: 10.1523/JNEUROSCI.12-02-00483.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Julien LA, Carriere A, Moreau J, Roux PP. mTORC1-activated S6K1 phosphorylates Rictor on threonine 1135 and regulates mTORC2 signaling. Mol Cell Biol. 2010;30:908–921. doi: 10.1128/MCB.00601-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelz MB, Chen J, Carlezon WA, Jr., Whisler K, Gilden L, Beckmann AM, Steffen C, Zhang YJ, Marotti L, Self DW, et al. Expression of the transcription factor deltaFosB in the brain controls sensitivity to cocaine. Nature. 1999;401:272–276. doi: 10.1038/45790. [DOI] [PubMed] [Google Scholar]
- Krishnan V, Han MH, Graham DL, Berton O, Renthal W, Russo SJ, Laplant Q, Graham A, Lutter M, Lagace DC, et al. Molecular adaptations underlying susceptibility and resistance to social defeat in brain reward regions. Cell. 2007;131:391–404. doi: 10.1016/j.cell.2007.09.018. [DOI] [PubMed] [Google Scholar]
- Krishnan V, Han MH, Mazei-Robison M, Iniguez SD, Ables JL, Vialou V, Berton O, Ghose S, Covington HE, 3rd, Wiley MD, et al. AKT signaling within the ventral tegmental area regulates cellular and behavioral responses to stressful stimuli. Biol Psychiatry. 2008;64:691–700. doi: 10.1016/j.biopsych.2008.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon CH, Zhu X, Zhang J, Baker SJ. mTor is required for hypertrophy of Pten-deficient neuronal soma in vivo. Proc Natl Acad Sci U S A. 2003;100:12923–12928. doi: 10.1073/pnas.2132711100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laplante M, Sabatini DM. mTOR signaling at a glance. J Cell Sci. 2009;122:3589–3594. doi: 10.1242/jcs.051011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luscher C, Slesinger PA. Emerging roles for G protein-gated inwardly rectifying potassium (GIRK) channels in health and disease. Nat Rev Neurosci. 2010;11:301–315. doi: 10.1038/nrn2834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClung CA, Nestler EJ, Zachariou V. Regulation of gene expression by chronic morphine and morphine withdrawal in the locus ceruleus and ventral tegmental area. J Neurosci. 2005;25:6005–6015. doi: 10.1523/JNEUROSCI.0062-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niehaus JL, Murali M, Kauer JA. Drugs of abuse and stress impair LTP at inhibitory synapses in the ventral tegmental area. Eur J Neurosci. 2010;32:108–117. doi: 10.1111/j.1460-9568.2010.07256.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Brien CP. Drug Addiction and Drug Abuse. In: Hardman JG, Gilman AG, editors. Goodman and Gilman's The Pharmacological Basis of Therapeutics, L.L.E. McGraw-Hill; 2001. pp. 621–642. [Google Scholar]
- Oh WJ, Jacinto E. mTOR complex 2 signaling and functions. Cell Cycle. 2011;10:2305–2316. doi: 10.4161/cc.10.14.16586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Partovian C, Ju R, Zhuang ZW, Martin KA, Simons M. Syndecan-4 regulates subcellular localization of mTOR Complex2 and Akt activation in a PKCalpha-dependent manner in endothelial cells. Mol Cell. 2008;32:140–149. doi: 10.1016/j.molcel.2008.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce LR, Komander D, Alessi DR. The nuts and bolts of AGC protein kinases. Nat Rev Mol Cell Biol. 2010;11:9–22. doi: 10.1038/nrm2822. [DOI] [PubMed] [Google Scholar]
- Pothos E, Rada P, Mark GP, Hoebel BG. Dopamine microdialysis in the nucleus accumbens during acute and chronic morphine, naloxone-precipitated withdrawal and clonidine treatment. Brain Res. 1991;566:348–350. doi: 10.1016/0006-8993(91)91724-f. [DOI] [PubMed] [Google Scholar]
- Rossetti ZL, Hmaidan Y, Gessa GL. Marked inhibition of mesolimbic dopamine release: a common feature of ethanol, morphine, cocaine and amphetamine abstinence in rats. Eur J Pharmacol. 1992a;221:227–234. doi: 10.1016/0014-2999(92)90706-a. [DOI] [PubMed] [Google Scholar]
- Rossetti ZL, Melis F, Carboni S, Gessa GL. Dramatic depletion of mesolimbic extracellular dopamine after withdrawal from morphine, alcohol or cocaine: a common neurochemical substrate for drug dependence. Ann N Y Acad Sci. 1992b;654:513–516. doi: 10.1111/j.1749-6632.1992.tb26016.x. [DOI] [PubMed] [Google Scholar]
- Russo SJ, Bolanos CA, Theobald DE, DeCarolis NA, Renthal W, Kumar A, Winstanley CA, Renthal NE, Wiley MD, Self DW, et al. IRS2-Akt pathway in midbrain dopamine neurons regulates behavioral and cellular responses to opiates. Nat Neurosci. 2007;10:93–99. doi: 10.1038/nn1812. [DOI] [PubMed] [Google Scholar]
- Sarbassov DD, Ali SM, Kim DH, Guertin DA, Latek RR, Erdjument-Bromage H, Tempst P, Sabatini DM. Rictor, a novel binding partner of mTOR, defines a rapamycin-insensitive and raptor-independent pathway that regulates the cytoskeleton. Curr Biol. 2004;14:1296–1302. doi: 10.1016/j.cub.2004.06.054. [DOI] [PubMed] [Google Scholar]
- Sarbassov DD, Ali SM, Sabatini DM. Growing roles for the mTOR pathway. Curr Opin Cell Biol. 2005a;17:596–603. doi: 10.1016/j.ceb.2005.09.009. [DOI] [PubMed] [Google Scholar]
- Sarbassov DD, Guertin DA, Ali SM, Sabatini DM. Phosphorylation and regulation of Akt/PKB by the rictor-mTOR complex. Science. 2005b;307:1098–1101. doi: 10.1126/science.1106148. [DOI] [PubMed] [Google Scholar]
- Shah OJ, Wang Z, Hunter T. Inappropriate activation of the TSC/Rheb/mTOR/S6K cassette induces IRS1/2 depletion, insulin resistance, and cell survival deficiencies. Curr Biol. 2004;14:1650–1656. doi: 10.1016/j.cub.2004.08.026. [DOI] [PubMed] [Google Scholar]
- Shiota C, Woo JT, Lindner J, Shelton KD, Magnuson MA. Multiallelic disruption of the rictor gene in mice reveals that mTOR complex 2 is essential for fetal growth and viability. Dev Cell. 2006;11:583–589. doi: 10.1016/j.devcel.2006.08.013. [DOI] [PubMed] [Google Scholar]
- Siuta MA, Robertson SD, Kocalis H, Saunders C, Gresch PJ, Khatri V, Shiota C, Kennedy JP, Lindsley CW, Daws LC, et al. Dysregulation of the norepinephrine transporter sustains cortical hypodopaminergia and schizophrenia-like behaviors in neuronal rictor null mice. PLoS Biol. 2010;8:e1000393. doi: 10.1371/journal.pbio.1000393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sklair-Tavron L, Shi WX, Lane SB, Harris HW, Bunney BS, Nestler EJ. Chronic morphine induces visible changes in the morphology of mesolimbic dopamine neurons. Proc Natl Acad Sci U S A. 1996;93:11202–11207. doi: 10.1073/pnas.93.20.11202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiga S, Lintas A, Migliore M, Diana M. Altered architecture and functional consequences of the mesolimbic dopamine system in cannabis dependence. Addict Biol. 2010;15:266–276. doi: 10.1111/j.1369-1600.2010.00218.x. [DOI] [PubMed] [Google Scholar]
- Spiga S, Serra GP, Puddu MC, Foddai M, Diana M. Morphine withdrawal-induced abnormalities in the VTA: confocal laser scanning microscopy. Eur J Neurosci. 2003;17:605–612. doi: 10.1046/j.1460-9568.2003.02435.x. [DOI] [PubMed] [Google Scholar]
- Treins C, Warne PH, Magnuson MA, Pende M, Downward J. Rictor is a novel target of p70 S6 kinase-1. Oncogene. 2010;29:1003–1016. doi: 10.1038/onc.2009.401. [DOI] [PubMed] [Google Scholar]
- Tsankova NM, Berton O, Renthal W, Kumar A, Neve RL, Nestler EJ. Sustained hippocampal chromatin regulation in a mouse model of depression and antidepressant action. Nat Neurosci. 2006;9:519–525. doi: 10.1038/nn1659. [DOI] [PubMed] [Google Scholar]
- Turrigiano GG, Nelson SB. Homeostatic plasticity in the developing nervous system. Nat Rev Neurosci. 2004;5:97–107. doi: 10.1038/nrn1327. [DOI] [PubMed] [Google Scholar]
- van Diepen MT, Parsons M, Downes CP, Leslie NR, Hindges R, Eickholt BJ. MyosinV controls PTEN function and neuronal cell size. Nat Cell Biol. 2009;11:1191–1196. doi: 10.1038/ncb1961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q, Liu L, Pei L, Ju W, Ahmadian G, Lu J, Wang Y, Liu F, Wang YT. Control of synaptic strength, a novel function of Akt. Neuron. 2003;38:915–928. doi: 10.1016/s0896-6273(03)00356-8. [DOI] [PubMed] [Google Scholar]
- Wolf DH, Numan S, Nestler EJ, Russell DS. Regulation of phospholipase Cgamma in the mesolimbic dopamine system by chronic morphine administration. J Neurochem. 1999;73:1520–1528. doi: 10.1046/j.1471-4159.1999.0731520.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou J, Blundell J, Ogawa S, Kwon CH, Zhang W, Sinton C, Powell CM, Parada LF. Pharmacological inhibition of mTORC1 suppresses anatomical, cellular, and behavioral abnormalities in neural-specific Pten knock-out mice. J Neurosci. 2009;29:1773–1783. doi: 10.1523/JNEUROSCI.5685-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.