Abstract
Throughout life, one's blood supply depends on sustained division of hematopoietic stem cells (HSCs) for self-renewal and differentiation. Within the bone marrow microenvironment, an adhesion-dependent or -independent niche system regulates HSC function. Here we show that a novel adhesion-dependent mechanism via integrin-β3 signaling contributes to HSC maintenance. Specific ligation of β3-integrin on HSCs using an antibody or extracellular matrix protein prevented loss of long-term repopulating (LTR) activity during ex vivo culture. The actions required activation of αvβ3-integrin “inside-out” signaling, which is dependent on thrombopoietin (TPO), an essential cytokine for activation of dormant HSCs. Subsequent “outside-in” signaling via phosphorylation of Tyr747 in the β3-subunit cytoplasmic domain was indispensable for TPO-dependent, but not stem cell factor-dependent, LTR activity in HSCs in vivo. This was accompanied with enhanced expression of Vps72, Mll1, and Runx1, 3 factors known to be critical for maintaining HSC activity. Thus, our findings demonstrate a mechanistic link between β3-integrin and TPO in HSCs, which may contribute to maintenance of LTR activity in vivo as well as during ex vivo culture.
Introduction
Hematopoietic stem cells (HSCs) are clonogenic cells capable of both self-renewal and multilineage differentiation, enabling life-long maintenance of blood cell generation. To maintain HSCs, at least one HSC daughter cell must always be capable of self-renewal and multilineage differentiation, but the mechanism by which HSCs retain that capability is not yet defined. It has been proposed that there is a specialized microenvironment, called “niche,” within the BM, where the balance among self-renewal, differentiation, and quiescence is regulated by both adhesion-dependent (eg, osteopontin [OPN]/integrin-α9β1 or α4β1, Tie-2/angiopoetin-1 interaction) and -independent machinery (eg, thrombopoietin [TPO], TGF-β).1–5
Recently, we found that the mouse CD34−KSL HSC fraction, but not the CD34+KSL hematopoietic progenitor fraction, dominantly expresses the integrin-β3 subunit (CD61) bound to the αv (CD51) or αIIb (CD41) subunit.6 In particular, the αvβ3 complex, but not the αIIbβ3 complex, appears to be involved in the function of HSCs, as αv positivity, but not αIIb positivity, enhances long-term repopulating (LTR) activity in CD34−KSL HSCs after transplantation.7 This led us to conclude that αvβ3 is crucial for HSC function.
Integrins are heterodimeric receptors consisting of an α- and β-subunit, and their active and inactive conformations (forms with higher and lower affinities for ligands) are tightly regulated by “inside-out” signaling, mediated through external stimulation of several receptors on the cell surface.8 After integrin activation, specific ligand binding to the protein initiates “outside-in” signaling, which coordinates with signaling cascades initiated through growth factor-, cytokine-, and G protein-coupled receptors to regulate actin reorganization, cell survival, and proliferation.9–11 With regard to β3-integrin, inside-out signaling results in the binding of talin to the specific binding amino acids within the intracellular tail of the β3 subunit, which is essential for integrin activation.12 Of these sequences, tyrosine phosphorylation of the β3 subunit, at least on Tyr747 (pY747), appears to be required for the outside-in signaling cascade, such as that seen during stable thrombus formation in platelets.13 Although the roles of bidirectional integrin signaling by β3-integrin in other hematopoietic cells remain unclear, evidence suggests that an interaction between integrins α4β1 and α9β1 and OPN is required for regulation of HSC proliferation, which is indicative of the crucial contribution made by integrins to HSC maintenance.2 Integrin-αvβ3 reportedly interacts with OPN, as well as with vitronectin (VN), fibronectin, and CD31. Interestingly, CD31-null mice exhibit greater numbers of KSL cells but with less functionality than wild-type (WT) mice, which could reflect the absence of interaction with αvβ3-integrin.14 From these results, it seems apparent that, although integrin-αvβ3 appears to be involved in the regulation of HSC function, its precise role in that process remains unclear.
It is well known that TPO is essential for megakaryopoiesis15 and also contributes to the maintenance and expansion of HSCs.16–18 Mice deficient in TPO or its receptor (c-mpl) show not only impaired megakaryopoiesis but also reduced HSC number and function.16,19,20 Moreover, recent reports indicate that TPO is required for the maintenance of HSCs in a quiescent state within the BM.3,4
Here, we demonstrate that integrin-αvβ3 on HSCs plays essential roles in maintaining their stem cell activity. Furthermore, we show that specific ligation of β3-integrin contributes to the maintenance of LTR activity in HSCs through collaboration with TPO/c-mpl-mediated signaling, which inhibits the loss of LTR activity during ex vivo culture. Our approach to clarifying integrin function in HSCs entailed the use of knock-in mutant mice that display defective β3-integrin inside-out or outside-in signaling because of blockade of talin-binding to specific amino acids in the β3-integrin tail.21 This enabled us to show that outside-in signaling via pY747 of integrin-β3 (β3PY747) after activation of αvβ3-integrin by TPO-mediated inside-out signaling is indispensable for TPO-mediated maintenance of HSC activity in vitro. In addition, outside-in signaling via β3PY747 is also essential for maintenance of LTR activity in vivo within the BM niche.
Methods
Animals
C57BL/6-Ly5.2 and C57BL/6-Ly5.1 mice were from Sankyo Labo Service, and β3-integrin-deficient mice were from The Jackson Laboratory unless otherwise noted. β3-integrin Y747A and L746A knock-in mutant mice were described previously.21 Each strain was back-crossed for more than 5 generations and used at 8 to 10 weeks of age. All animal experiments were approved by the Institutional Review Board for Animal Care and Use at the University of Tokyo.
Antibodies
The following monoclonal antibodies were used for cell sorting and flow cytometric analysis: anti–c-Kit (2B8, BioLegend), anti-CD34 (RAM34, eBiosciences, San Diego, CA), anti-CD150 (TC15-12F12.2, BioLegend), and anti-CD48 (HM48-1, BioLegend). Anti–integrin-β3 (2C9.G2), anti-Sca-1 (E13-161.7), anti-CD45.2,(104) anti-CD45.1 (A20), anti-B220/CD45R (RA3-6B2), anti–Mac-1 (M1/70), anti–Gr-1 (RB6-8C5), anti–CD4 (RM4-5), and anti-CD8 (53-6.72) antibodies were from BD Biosciences (BD Biosciences Pharmingen) unless otherwise noted. For in vitro assays, low endotoxin and azide-free anti–integrin-β3 (2C9.G2, BioLegend) and its isotype control IgG (HTK888, BioLegend) were used.
Cell preparation
Suspensions of BM cells were prepared from mice as described previously.6,7
Cell sorting and flow cytometric analysis
We used an EPICS ALTRA (Beckman Coulter) or MoFlo XDP (Beckman Coulter) for cell sorting and flow cytometric analysis, as described previously.6,7
Long-term competitive repopulation assays
Long-term competitive repopulation (LTCR) assays were performed by transplantation of the indicated cells into lethally irradiated (9.5 Gy) C57BL/6-Ly5.2 or C57BL/6-Ly5.1 congenic mice, as described previously.6 Twelve or 20 weeks after transplantation, recipient mice with donor cell chimerism (> 1.0% for myeloid and B- and T-lymphoid lineages) were considered to be multilineage-reconstituted mice (positive mice). For serial transplantation, 106 whole BM cells were obtained from primary transplanted mice and transplanted into other irradiated recipient mice.
Whole transcriptome analysis using a SOLiD system
After sorting 1000 to 1500 CD34−KSL cells, SOLiD sequencing was performed as described in the supplemental Methods (available on the Blood Web site; see the Supplemental Materials link at the top of the online article). The whole transcriptomes obtained through SOLiD sequencing were analyzed using GeneSpring (Agilent Technologies). After filtration based on a significant (P < .05 ANOVA) and more than 2-fold changes in expression, the selected genes were subjected to hierarchical cluster analysis. In addition, whole transcriptomes were subjected to gene set enrichment analysis (GSEA) using GSEA Version 2.06 software available from the Broad Institute (http://www.broad.mit.edu/gsea). Changed gene sets were selected based on a threshold set at a P value < .05 and false discovery rate (FDR; q-value < 0.25).
HSC cultures
CD34−KSL cells were sorted and cultured for 5 days in S-Clone SF-03 medium (Sanko-Junyaku) supplemented with 0.5% BSA (Sigma-Aldrich) and 50 ng/mL mouse SCF and/or 50 ng/mL mouse TPO (all from R&D Systems). To induce integrin signaling via β3PY747, 2C9.G2 (50 μg/mL; BioLegend) was added to the medium; hamster IgG (BioLegend) was used as a control. Activation of β3-integrin was also exogenously induced by adding to the medium 0.015mM MnCl2, an activator of integrin receptors. Total cell numbers were then counted under a light-phase microscope after the culture.
Estimation of integrin activation (inside-out signaling)
CD34−KSL cells were cultured for 18 hours with AlexaFluor 647–conjugated human fibrinogen (Invitrogen) in S-Clone SF-03 medium supplemented with 50 ng/mL SCF or 50 ng/mL TPO. Samples without cytokine stimulation served as the control. The cells were washed twice in PBS and analyzed for fluorescence intensity using flow cytometry to assess the degree of fibrinogen binding to cells.
Ligand-coated plates
Ninety-six-well plates were coated with 5 μg/mL VN (Molecular Innovations) or 5 μg/mL OPN (R&D Systems) overnight at 4°C. They were then blocked with 1% BSA for 1 hour at 37°C, after which they were used as ligand-coated plates. BSA-coated plates served as the control.
Limiting-dilution assay
After culture, exactly 10, 30, 50, 100, or 500 whole cultured cells were counted and sorted using a cell sorter and transplanted along with 2 × 105 BMCs from Ly5.2 mice as competitor cells. Twelve weeks after transplantation, HSC frequency was estimated from the input cell number and the percentage of multilineage reconstructed mice (positive mice), based on the Poisson distribution.22 As a control, single fresh (uncultured) CD34−KSL cells were also assessed using the same procedure.
Calculation of parameters on HSCs after ex vivo expansion
HSC numbers were estimated based on the total cell number counted using a phase-contrast microscope and the HSC frequency determined from limiting dilution assays. Repopulating unit (RU) values were calculated from the results of LTCR assays using 40 fresh CD34−KSL cells or their progeny with 5 × 105 Ly5.2 whole bone marrow competitor cells with the following formula:
RU = (% donor chimerism/% competitor chimerism) × 5
In addition, mean activity of stem cell (MAS) values, which reflect the repopulation ability of single HSCs, were estimated by dividing the RU values by the calculated HSC number.
DNA microarray
Using CD48−KSL cells that were sorted after culture of CD34−KSL cells for 5 days with 2C9.G2 antibody or control IgG under the indicated conditions, RNA extraction, amplification, and microarray analyses were performed as described in the supplemental Methods. All microarray data are available for viewing at the Gene Expression Omnibus under accession number GSE33696.
Real-time quantitative RT-PCR
Using 5000 sorted cells from each sample, mRNA expression was assessed using real-time quantitative RT-PCR as described previously.6
Results
Outside-in signaling via pY747 of β3-integrin, but not inside-out signaling, is required for the maintenance of the TLR activity on HSCs in vivo
We previously reported that CD34−KSL cells expressed higher levels of β3-integrin than CD34+KSL cells, whereas other reports suggested that β1 integrin is involved in the maintenance of HSCs.1,2 Our aim was to investigate why HSCs, and not progenitor cells, dominantly express β3, and whether this integrin has a distinct function in HSCs that differs from its function in other KSL cell populations.
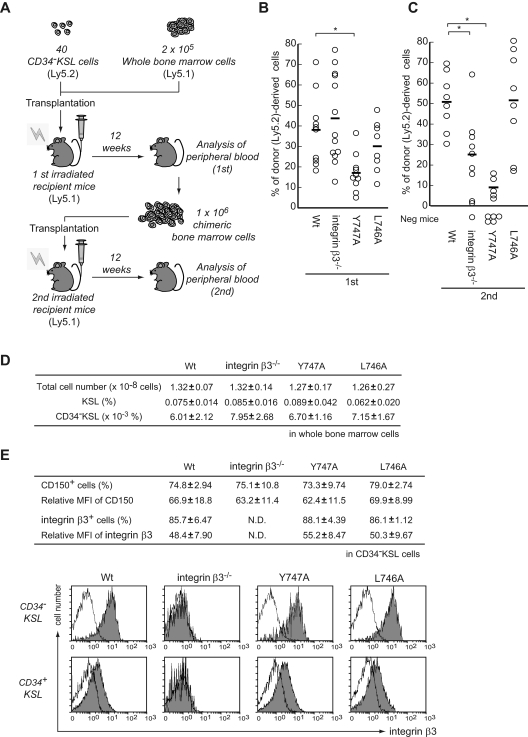
We initially focused on intracellular signaling by β3-integrin in HSCs. It has been demonstrated that β3−/− mice exhibit osteopetrosis induced by a lack of interaction between the tail of the β3-cytoplasmic domain and c-Src, leading to impaired osteoclast differentiation.23 Although it has been proposed that dysregulation of osteoclasts leads to impairment of HSCs,24,25 evaluation of the LTR activity of β3−/− HSCs after transplantation into irradiated mice in vivo showed that β3-integrin might be involved in HSC function (Figure 1A-C). To clearly rule out the effects of osteoclast dysregulation on specific integrin signaling in HSCs, we simultaneously used L746A (leucine-to-alanine substitution) and Y747A (tyrosine-to-alanine) knock-in mice, which have normal osteoclasts (data not shown).21,23 β3-Integrin “inside-out” signaling is mediated by talin binding to the Leu746 and Tyr747 residues in the β3 tail.12 Consequently, Y747A mutation disrupted both signals, whereas L746A mutation disrupted inside-out signaling without affecting outside-in signaling, for which pY747 is indispensable.21 Neither mutation altered the total cell number or the frequency of the HSC population (Figure 1D). In addition, there was also no difference between the expression profiles of integrin-β3 and CD150, a reliable maker of mouse HSCs,26 within CD34−KSL cells derived from both mutant mice (Figure 1E).
Figure 1.
Tyr747 of β3-integrin is essential for the long-term in vivo repopulating and self-renewal activities of mouse HSCs, independent of ex vivo expansion. (A) HSCs from WT or mutant mice were used for serial competitive repopulation assays. Forty sorted CD34−KSL cells (Ly5.2) were transplanted into lethally irradiated mice (Ly5.1) along with 2 × 105 BM competitor cells (Ly5.1). Twelve weeks later, the percentage of donor cells (Ly5.2) was determined in peripheral blood (B). A total of 106 BM cells from primary recipient mice were then transplanted into other irradiated mice, followed by secondary analysis of peripheral blood (C). The plot indicates donor-derived cells (percentage of Ly5.2+ cells) in the peripheral blood. In addition, recipient mice with donor cell chimerism of < 1.0% for any lineage were considered not to be reconstituted (negative mice). Bars represent mean values. *P < .01. (D) The table shows the total cell number and frequency of HSC subsets among BMCs from both femurs and tibias. (E) Also shown are the frequencies or relative mean fluorescent intensity (MFI) in CD150+ and integrin-β3+ cells among the CD34−KSL population. The value of the MFI obtained in the presence of the isotype control IgG was used as the control. Data are mean ± SD (n = 6-8). The histograms represent the expression of β3-integrin in murine HSCs (CD34−KSL) or hematopoietic progenitors (CD34+KSL) derived from WT, integrin-β3−/−, and Y747A or L746A mutants, all of which are shown in white. The isotype control is in gray.
However, when we performed a serial competitive repopulation assay, chimerism in primary recipients 12 weeks after transplantation showed defective reconstitution with Y747A HSCs, but not with L746A HSCs (Figure 1B). This finding was further confirmed by secondary transplantation (Figure 1C). Given the input HSC number used in the primary transplantation assays, these results indicate that stem cell activity was diminished in Y747A HSCs compared with WT HSCs, which suggests outside-in signaling via at least pY747 of β3PY747, but not inside-out signaling or formation of an αvβ3/c-Src complex,27 contributes to both the LTR and self-renewal activities of HSCs in vivo.
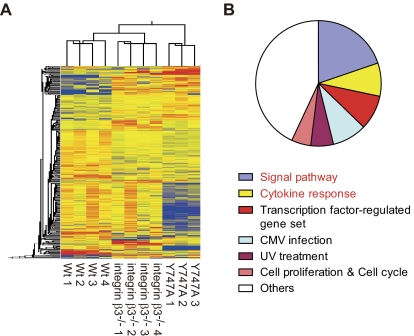
Given the specificity of the effects of β3PY747, we wondered why β3−/− HSCs did not exhibit impaired LTR activity after primary transplantation (Figure 1A-C). Cluster analysis of the whole transcriptome revealed that the gene expression pattern of Y747A HSCs differed from that of WT or β3−/− HSCs (Figure 2A). GSEA identified 102 gene sets up-regulated (and 0 down-regulated gene sets) in WT HSCs compared with Y747A HSCs, based on thresholds set at a P value < .05 and FDR (q-value) < 0.25 (supplemental Table 1). On the other hand, there was no differential set between WT and β3−/− HSCs (data not shown). These results indicate that the phenotype of β3−/− HSCs is significantly closer to that of WT HSCs than Y747A HSCs, suggesting that an as yet undetected molecule (perhaps other integrin receptors) might exert a compensatory effect mitigating the β3 deficiency.
Figure 2.
The gene expression profile in Y747A-mutant HSCs differed from that in WT and integrin-β3−/− HSCs. (A) After whole transcriptome analysis of WT, integrin-β3−/− and Y747A HSCs using SOLiD sequencing, hierarchical cluster analysis was performed after filtration based on ANOVA (P < .05) and a > 2-fold change against WT (at least one pair). Up-regulated and down-regulated genes are shown in red and blue, respectively. (B) GSEA was performed using the whole transcriptome of WT and Y747A HSCs. The pie chart represents the distribution of 102 gene sets up-regulated in WT HSCs, compared with Y747A HSCs, into the indicated categories. The threshold was set at P < .05 and FDR (q < 0.25).
In addition, our GSEA study also showed that Y747A mutation significantly reduced enrichment of a gene set “DORSAM_HOXA9_UP,” which are up-regulated by Hoxa9 (supplemental Table 1), whereas the level of Hox-a9 expression did not significantly differ between Y747A and WT HSCs (data not shown). Hoxa9 is well known to be an essential factor involved in the maintenance of HSCs,28 and TPO signaling reportedly promotes its transfer into the nucleus.29 Moreover, Y747A HSCs also exhibited less enrichment of gene sets involved in “signal transduction” and “cytokine responses,” than WT HSCs (Figure 2B; supplemental Table 1). Thus, our results suggest that impaired cytokine-mediated maintenance of HSC activity in the TPO/c-mpl axis leads to reduced LTR activity in Y747A HSCs, probably resulting in a diminished capacity for engraftment in transplantation assays (Figure 1A-C).
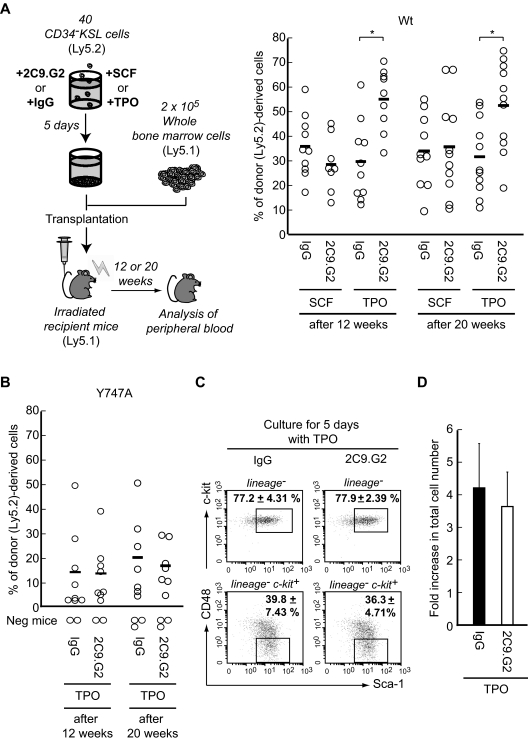
β3-integrin signaling contributes to HSC maintenance, which is dependent on TPO
Because outside-in signaling, at least via β3PY747, appeared to be involved in the TPO-mediated effects on HSCs, we next examined whether this signaling would also mediate the effects of TPO on ex vivo cultures of HSCs. For exogenous manipulation of β3PY747, we used 2C9.G2, a β3-integrin antibody that acts as a ligand stimulating transduction of αvβ3-integrin–mediated intracellular signaling in smooth muscle cells and neutrophils.30,31 We also confirmed that 2C9.G2 ligation to β3-integrin induced phosphorylation of β3PY747 as well as c-SrcPY418 and Syk, hallmarks of outside-in signaling from β3-integrin in mouse platelets (supplemental Figure 1).9,32 After culture of HSCs in the presence of TPO alone, we assessed the effect of 2C9.G2 on the LTR activity of HSCs 12 and 20 weeks after transplantation. Interestingly, 2C9.G2 treatment in the presence of TPO positively influenced HSC LTR activity (Figure 3A), and this effect was blocked by Y747A mutation (Figure 3B). By contrast, this positive action of 2C9.G2 disappeared during culture in the presence of SCF, a crucial cytokine involved in the maintenance and proliferation of HSCs (Figure 3A). These results indicate that the β3PY747-mediated effects on LTR activity in HSCs and the positive action by 2C9.G2 on the LTR activity of HSCs are both TPO-dependent. Interestingly, 2C9.G2 treatment had little effect on the frequency of KSL or CD48−KSL cells, a population enriched in HSCs after culture33 (Figure 3C) or on total cell number (Figure 3D) after culture in the presence of TPO. Outside-in signaling via β3PY747 per se appears to be independent of HSC expansion in the presence of TPO. This suggests that, given the effects of 2C9.G2 on LTR activity and HSC expansion, outside-in signaling via β3PY747 may contribute to the enhanced LTR activity of individual HSCs only by collaborating with TPO, rather than through HSC amplification.
Figure 3.
β3-Integrin-mediated maintenance of long-term HSC repopulating activity during ex vivo expansion is dependent on TPO, but not SCF. (A) To assess the influence of β3-integrin signaling, 40 CD34−KSL cells (Ly5.2) derived from WT (A) or Y747A mice (B) were cultured for 5 days in the presence of 2C9.G2 or IgG in serum-free medium supplemented with 50 ng/mL SCF or 50 ng/mL TPO. After the culture, whole cultured cells were transplanted with 2 × 105 BM competitor cells (Ly5.1) into lethally irradiated Ly5.1 mice. The plots depict the percentage of donor (Ly5.2)–derived cells in the peripheral blood of individual mice 12 weeks or 20 weeks after transplantation. Bars represent mean values. *P < .01. Recipient mice with donor cell chimerism of less than 1.0% for any lineage were considered not to be reconstituted (negative mice). (C) After culture of 1000 sorted WT CD34−KSL cells (Ly5.1) for 5 days with 2C9.G2 or hamster IgG (isotype control) in the presence of TPO, the percentages of KSL and CD48−KSL cells were determined by flow cytometric analysis. The values in the dot plots are mean ± SD. (D) After culture, the total cell number was counted. The graph shows the fold increase in total cell number after 5 days of culture. Data are mean ± SD.
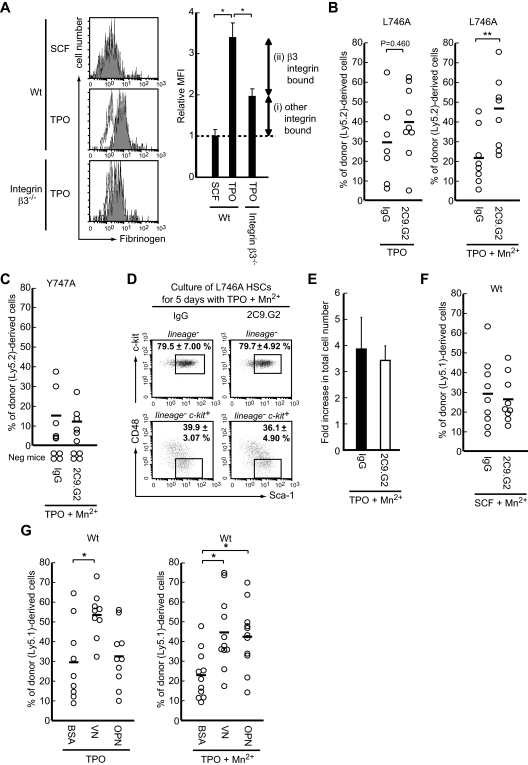
TPO promotes activation of at least β3-integrin possibly via inside-out signaling
We have so far proposed a strong link between TPO and β3PY747 signaling. As for why β3PY747-mediated function in HSCs is dependent on TPO, we initially wondered whether TPO enhanced expression of integrin-β3 on HSCs. We found that, indeed, TPO-treated HSCs showed slightly less expression of integrin-β3 than fresh HSCs or SCF-treated HSCs (supplemental Figure 2). We next hypothesized that TPO might regulate integrin affinity via a conformational change for activation. Accordingly, purified CD34−KSL cells (from WT or β3−/− mice as negative control) were treated with TPO or SCF for 18 hours, after which the binding of AlexaFlour 647–labeled fibrinogen, a ligand for αvβ3, αIIbβ3, and/or αMβ2, was assessed.34 As shown in Figure 4A, TPO, but not SCF, increased fibrinogen binding to WT HSCs detected with flow cytometry. However, fibrinogen also bound to β3−/− HSCs, indicating an interaction with another receptor, probably αMβ2 integrin.34,35 After subtracting the binding to β3−/− HSCs from that to WT HSCs, we were likely left with the binding to αvβ3 rather than αIIbβ3-integrin (Figure 4A). This is because we used Mg2+-containing Ca2+-free medium, which was previously shown to exclude binding to αIIbβ3-integrin (data not shown).36,37 Thus, TPO apparently contributes to the activation of at least αvβ3-integrin via the inside-out intracellular machinery in HSCs.
Figure 4.
TPO changes the activation status of β3-integrin through inside-out signaling, and post-ligation outside-in signaling via β3PY747 is indispensable for maintenance of HSC function during ex vivo expansion. (A) CD34−KSL cells derived from WT and β3−/− mice were cultured with AlexaFlour 647–labeled fibrinogen in S-Clone SF-03 medium, with or without SCF or TPO. The fluorescence intensity of the bound fibrinogen was analyzed by flow cytometry: white represents no cytokine; and gray, stimulation of cytokine. The graphs represent the relative mean fluorescence intensity (MFI); binding in the absence of cytokine served as the control. Data are mean ± SD; n > 3. *P < .01. (B-C) Forty CD34−KSL cells obtained from BM of L746A (Ly5.2; B) or Y747A mice (Ly5.2; C) were cultured with TPO for 5 days in the presence of 2C9.G2 or IgG and examined using transplantation assays, as described in Figure 2. To exogenously induce integrin activation (change the structure to the activated state), Mn2+ was added to TPO-containing medium. (D) After culture of 1000 sorted L746A-mutant CD34−KSL cells (Ly5.1) for 5 days with 2C9.G2 or hamster IgG (isotype control) in the presence of TPO and Mn2+, the percentages of KSL and CD48−KSL cells were determined by flow cytometry. The values in the dot plots are mean ± SD. (E) After the culture, the total cell number was counted. The graph represents the fold increase in total cell number after 5 days of culture. Data are mean ± SD. (F) Forty WT CD34−KSL cells (Ly5.1) were also cultured for 5 days in medium containing SCF and Mn2+ along with 2C9.G2 or IgG. (G) Using plates coated with VN, OPN, or BSA, 40 WT CD34−KSL cells (Ly5.1) were cultured with TPO for 5 days in the absence or presence of Mn2+. After the culture, cells were transplanted along with 2 × 105 BM competitor cells into irradiated recipient mice. The plots represent the percentage of donor (Ly5.2 or Ly5.1)-derived cells in the peripheral blood of individual mice 12 weeks after transplantation. *P < .01. **P < .05. Recipient mice with donor cell chimerism of < 1.0% for any lineage were considered not to be reconstituted (negative mice).
Extracellular circumstances affect integrin activation status and full integrin activation is required for LTR activity of HSCs
Although it has already been shown that disrupting inside-out signaling without affecting outside-in signaling through L746A mutation has little effect on the capacity of HSCs for reconstitution in vivo (Figure 1A-C), we again tested whether the L746A mutation is independent of 2C9.G2-mediated β3PY747 effects on the LTR activity of HSCs. Interestingly, L746A mutation did not appear to increase chimerism by 2C9.G2 treatment in a manner similar to Y747A mutation, even in the presence of TPO (Figure 4B left). Whereas the addition of Mn2+, a strong external inducer of integrin activation that acts independently of intracellular signaling, ameliorated the effect of 2C9.G2 on LTR activity in L746A HSCs (Figure 4B right), it had no such effect on Y747A HSCs (Figure 4C). There was also no effect of 2C9.G2 administration on the frequency of KSL or CD48−KSL cells (Figure 4D) or on total cell number (Figure 4E) after culture of L746A HSCs in the presence of TPO plus Mn2+, again indicating that the collaboration between TPO and outside-in signaling via β3PY747 is independent of HSC expansion in vitro. Taken together, these results indicate that activation of integrin-αvβ3 and subsequent outside-in signaling via β3PY747 are required to enhance LTR capability per individual HSC via an integrin-mediated function and suggest that these results are consistent with the in vivo study summarized in Figure 1A-C. On the other hand, forcing integrin activation with Mn2+ did not restore 2C9.G2 activity in the presence of SCF in WT HSCs (Figure 4F). We therefore concluded that not only outside-in signaling via β3PY747, but also activation of integrin-αvβ3 per se, is required for TPO-dependent, but not SCF-dependent, full LTR maintenance in HSCs. We also sought to identify endogenous αvβ3-integrin ligands involved in the HSC function that maintains LTR. VN and OPN are well-known αvβ3 ligands. Interestingly, LTR activity was enhanced when HSCs were cultured with TPO for 5 days on plates coated with VN alone (Figure 4G). On the other hand, OPN exerted a positive effect on LTR activity only when Mn2+ was simultaneously administered (Figure 4G). Moreover, these natural ligands had no effect on HSC expansion, as evidenced by the similar frequency of HSC subsets (supplemental Figure 3A) and total cell numbers (supplemental Figure 3B) under all culture conditions. These findings again allowed us to consider the possibility that factors in the microenvironment other than TPO might influence integrin activation status and that full activation of integrin bound to extracellular matrix or other ligands might be required for β3PY747-mediated enhancement of LTR activity per individual HSC.
β3-integrin signaling maintains HSC activity during ex vivo expansion
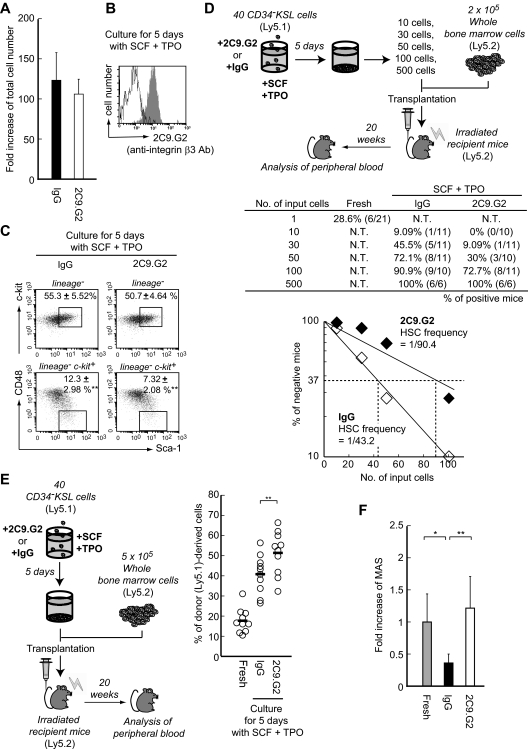
We found that bidirectional β3-integrin signaling contributed to the maintenance of HSC activity at the single-cell level through collaboration with TPO. Ema et al previously reported that, under various conditions, SCF and TPO act together to effectively induce ex vivo expansion of HSCs through rapid cell division.38 We therefore examined the effect of β3PY747 signaling on the LTR activity of HSCs during ex vivo expansion induced by the combination of SCF plus TPO. Application of 2C9.G2 or control IgG to 40 HSCs during 5 days of ex vivo culture in the presence of SCF plus TPO did not alter total cell numbers (Figure 5A), and levels of β3-integrin bound with 2C9.G2 were not affected (Figure 5B). By contrast, the number of CD48−KSL cells was reduced by 2C9.G2 treatment (Figure 5C), suggesting that the frequency of HSCs after ex vivo culture was reduced by cellular manipulation via β3PY747. Indeed, in cultures treated with 2C9.G2 for 5 days, the HSC frequency was lower and the number of HSC in transplantation assays was reduced (Figure 5D; supplemental Table 2), suggesting that outside-in β3-integrin signaling suppresses the amplification of HSCs. But interestingly, 2C9.G2-treated cells eventually showed a tendency toward increased HSC activity compared with cells cultured with IgG in LTRC assays (Figure 5E). This tendency was confirmed through in vivo evaluation of RU values, which imply LTR activity39 and are based on the percentage of donor-derived cells in the peripheral blood of recipients 20 weeks after transplantation (supplemental Table 2), and the MAS values (RU divided by the number of detectable HSCs in recipient mice)40 (Figure 5F). MAS values clearly showed that ex vivo culture with IgG reduced LTR activity per single HSC compared with uncultured fresh HSCs (Figure 5F). By contrast, 2C9.G2 treatment enabled purified HSCs to expand ex vivo without diminishing LTR activity (Figure 5F; supplemental Table 2). Thus, β3-integrin signaling may also be able to maintain LTR capability at the single-HSC level during ex vivo expansion.
Figure 5.
Integrin-β3–mediated signaling leads to the suppression of expansion and cell division on HSCs during ex vivo culture. Forty sorted WT CD34−KSL cells (Ly5.1) were cultured for 5 days with 2C9.G2 or hamster IgG (isotype control) in S-Clone SF-03 serum-free medium supplemented with 50 ng/mL SCF plus 50 ng/mL TPO. (A) After the culture, total cell number was counted. Graph represents fold increase of total cell number after 5 days of culture. Data are mean ± SD. (B) To confirm 2C9.G2 binding to cells during culture, cells were stained with fluorescently labeled hamster IgG and analyzed by flow cytometry: white represents IgG; and gray, 2C9.G2. (C) The percentages of KSL and CD48−KSL cells were also determined by flow cytometry after culture. **P < .05. (D) HSC frequency among the cultured cells was determined using limiting dilution assays. After groups of 10, 30, 50, 100, or 500 whole cultured cells were counted exactly and sorted, the groups were individually transplanted into lethally irradiated Ly5.2 mice along with 2 × 105 BM cells from Ly5.2 mice. This was followed by analysis for chimerism 20 weeks after the transplantation. The table shows the rate of positive mice (multilineage reconstituted mice); the numbers in parentheses are the positive mice/tested mice. In the case of fresh CD34−KSL cells, a single cell was transplanted. After determining the percentage of reconstructed mice (table), the percentage of unreconstructed mice (percentage of negative mice on y-axis) was plotted versus the number of input cells, leading to a theoretical HSC frequency based on a Poisson distribution. Inputting 500 cells resulted in 0% negative mice, and these data are not plotted. (E) Fresh or whole cultured cells (Ly5.1) were transplanted into lethally irradiated mice (Ly5.2) along with 5 × 105 BM cells (Ly5.2). Twenty weeks later, peripheral blood from the recipient mice was analyzed by flow cytometry. The plots represent the percentage of donor-derived cells (percentage of Ly5.1+ cells) in the peripheral blood of individual recipients. Bars represent the mean values. **P < .05. (F) In addition, the MAS reflects the repopulating ability of single HSCs, as estimated from the RU value (supplemental Table 2) and HSC number (supplemental Table 2). Data are mean ± SD. *P < .01. **P < .05.
The collaboration between β3-integrin signaling and TPO enhanced genes involved in the maintenance of HSC activity
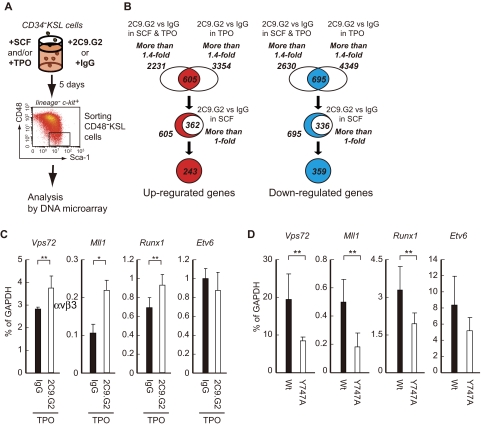
Finally, to determine the molecules involved in β3-integrin signaling and acting in concert with TPO, we carried out DNA microarray analyses using purified HSCs. In sorted CD48−KSL cells after ex vivo culture, we selected genes showing elevated or reduced expression on administration of 2C9.G2 (vs IgG) in the presence of only TPO (Figure 6A-B; supplemental Table 3; supplemental Figure 4). Eleven of the up-regulated gene sets and 5 of the down-regulated sets were picked up by gene ontology (GO) enrichment analysis (Table 1). Interestingly, chromatin modification (GO 0016568), one of up-regulated gene sets, contained Vps72, which is known to be a key gene involved in LTR activity, and Mll1 (Table 1), which is involved in the maintenance of HSCs.41,42 Similarly, Runx1 and Etv6, which are required for definitive HSC generation and maintenance, were also included among the up-regulated genes (supplemental Table 3).43,44 Subsequent real-time quantitative RT-PCR confirmed the 2C9.G2-induced enhancement of Vps72, Mll1, and Runx1 expression in the presence of TPO alone, although Etv6 was not apparent (Figure 6C), and that effect was reversed by Y747A mutation in fresh HSCs (Figure 6D). These results suggest that the contribution of β3-integrin signaling to the maintenance of LTR activity by HSCs is related at least to the enhanced expression of these 3 genes.
Figure 6.
Integrin-β3–mediated signaling enhanced expression of stemness-related genes by cooperating TPO presence. (A) DNA array analysis was performed using CD48−KSL cells after culture. The cells were sorted after culturing CD34−KSL cells for 5 days with 2C9.G2 or IgG in the presence of SCF and/or TPO. (B) Genes whose expression had changed from the DNA microarray data and genes that showed > 1.4-fold up-regulation (with TPO: 2231 genes or SCF + TPO: 3354 genes) or down-regulation (with TPO: 4349 genes or SCF + TPO: 2630 genes) in 2C9.G2-treated cells were selected for extraction. This was followed by extraction of genes included in both populations (up-regulation, 605 genes; down-regulation, 695 genes). In addition, to clearly focus on the effect of the combination by TPO and β3-integrin signaling, genes only showing > 1.0-fold up-regulation (362 genes) or down-regulation (336 genes) in the presence of SCF were excluded. This left 243 genes that were up-regulated and 359 that were down-regulated in HSCs by 2C9.G2 in the presence of TPO. (C) Expression of candidate genes involved in the maintenance of LTR activity of HSCs was assessed using real-time RT-PCR with 2C9.G2- or IgG-treated CD34−KSL cells cultured in the presence of TPO. The graphs represent mRNA expression of the indicated genes. Data are mean ± SD; n > 3. **P < .05. (D) Fresh (uncultured) CD34−KSL cells obtained from the BM of WT or Y747A mice were also subjected to real-time RT-PCR to examine expression of these genes. The graphs represent mRNA expression of the indicated genes. Data are mean ± SD; n > 3. **P < .05.
Table 1.
GO enrichment analysis using genes extracted based on a change in their expression level
| GO ID | Function name | Corrected P | Gene symbol |
|---|---|---|---|
| Up-regulated | |||
| 0045598 | Regulation of fat cell differentiation | .011 | Alms1, Tbn, Lpin1 |
| 0007165 | Regulation of osteoblast differentiation | .057 | Apc, Ctnnb1 |
| 0045667 | Glial cell fate determination | .078 | Ralgds, Myo9a, Pde2a, Arhgap17 |
| 0007403 | Signal transduction | .078 | Smarca4, Ctnnb1 |
| 0030858 | Positive regulation of epithelial cell differentiation | .078 | Apc, Ctnnb1 |
| 0035116 | Embryonic hindlimb morphogenesis | .078 | Smarca4, Ctnnb1, Lrp6 |
| 0007049 | Heart development | .078 | Acvr1, Trp53bps2, Smarca4, Pbm1, Ctnnb1, Tnni3, Txnrd2 |
| 0007507 | Cell cycle | .078 | Tacc1, Trp53bps, Apc, Evi5, Zwilch, Rbl2, Rb1, Aspm, Lig3, Ccnh, Wtap, Nf2, Sass6 |
| 0006915 | Apoptosis | .078 | Cflar, Trp53bps2, Alms1, Rffl, Slk, Bcl7c, Bc1212, Axud1, Ctnnb1, Bfar, 2810055G22Rik, Ctnnbl1 |
| 0016568 | Chromatin modification | .091 | Vps72, Pbrm1, Ezh1, Whsc1, Rbl2, Rb1, Mll1 |
| Down-regulated | |||
| 0007186 | G-protein coupled receptor protein signaling pathway | .00012 | Arhger12, Ptafr |
| 0007165 | Signal transduction | .001 | Stambp, Plcb2, Arhgap12, Ptafr, Rin3 |
| 0051301 | Cell division | .056 | Chfr, Ppp1cc, Sept6, Setd8, Cdc23, Timeless, Mtap9, Prr6, Cdca3, Ccnk, Pafh1b1, Hmga2 |
| 0007067 | Mitosis | .056 | Chfr, Setd8, Cdc23, Timeless, Mtap9, Prr6, Cdca3, Ccnk, Pafah1b1, Hmga2 |
The genes extracted from DNA arrays were subjected to GO enrichment analysis. P values were corrected by FDR (Benjamini-Hochberg), and the threshold was set at the corrected P < 0.1.
Discussion
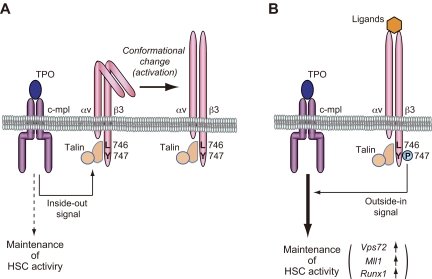
In the present study, we showed that β3-integrin signaling contributed to HSC regulation by collaborating with TPO signaling. In Figure 7, we propose a model in which HSC maintenance is regulated by αvβ3-integrin-mediated bidirectional (inside-out and outside-in) signaling. Downstream signaling via β3PY747 in the presence of TPO may also involve Vps72, Mll1, and Runx1, which contribute to the regulation of HSC LTR activity (Figure 6C-D). Perhaps through a still undetected mechanism, treatment with 2C9.G2 or a natural ligand not only contributes to enhanced LTR activity after culture in the presence of TPO alone (Figures 3 and 4), but also to the maintenance of HSC activity at the single-cell level, even after ex vivo expansion induced with SCF plus TPO, by compensating for the reduction in activity that occurs during the culture (Figure 5F).
Figure 7.
Model depicting the role of β3-integrin in TPO-dependent regulation of HSC division leading to the maintenance of LTR ability. Integrin-β3 bidirectional signaling and TPO were dependent on each other in the maintenance of HSCs. (A) TPO/c-mpl signaling leads to conformational change of integrin-αvβ3 into high-affinity form for their ligands (the activation of integrin-αvβ3) by inducing inside-out signaling. (B) Outside-in signaling via Tyr747 phosphorylation of integrin-β3 induces enhanced expression of stemness-related genes after their ligation.
HSCs treated with 2C9.G2 in the presence of TPO exhibited enhanced expression of genes related to chromatin modification (GO 0016568; Table 1), and the positive effect of 2C9.G2 on the LTR activity of HSCs was dependent on the presence of TPO, but not SCF (Figure 3A). These results suggest that outside-in signaling via β3PY747 contributes to the maintenance of HSC LTR activity, possibly via chromatin modification in the presence of TPO signal. Consistent with that idea, integrin signaling reportedly acts in concert with cytokine stimulation to influence chromatin modification for the maintenance of tissue-specific function in mammary gland cells.45 We therefore propose that a change in the TPO concentration (possibly a large increase) eventually elicits outside-in signaling via β3PY747 that mediates chromatin modification related to cell division and/or maintenance of the stemness of HSCs. GO enrichment analysis also revealed a number of down-regulated gene sets, 2 of which were “cell division ” (GO 0051301) and “mitosis” (GO 0007067; Table 1). Moreover, 4 genes, Apc, Rb, Rbl2, and Nf2, within the up-regulated gene set “cell cycle ” (GO 0007507) also belonged to the GO term “negative regulation of cell cycle” (GO 0045786; Table 1). These data suggest that TPO and outside-in signaling via β3PY747 act collaboratively to regulate expression of these genes, which may imply that HSC amplification is repressed during ex vivo expansion through a combination of SCF and TPO signaling (Figure 5D; supplemental Table 2). Indeed, single-cell culture of an HSC showed suppressed cell division in the presence of 2C9.G2 (supplemental Figure 4), again confirming the repressive effects of integrin-β3 signaling on HSC division during the ex vivo expansion trial with SCF and TPO. However, neither BrdU uptake assays nor Hoechst staining revealed a direct link between β3PY747 and the regulation of the cell cycle in HSCs in vivo (supplemental Figure 5) or during ex vivo expansion (data not shown).
This suppressive action of integrin-β3 signaling was apparent in HSCs undergoing rapid cell division (ie, ex vivo expansion induced by SCF plus TPO; Figure 5D; supplemental Table 2), but not in slowly dividing HSCs (ie, in cultures exposed to TPO alone; Figure 3C-D; Figure 4D-E) or quiescent HSCs (ie, in vivo; Figure 1D). Because the effect of integrin-β3 signaling appears to be small, as discussed in the previous paragraph, we suggest that the suppressive action may be masked by the state of the slowly dividing or quiescent HSCs. By contrast, rapidly dividing HSCs (ie, during ex vivo expansion requiring by both SCF and TPO) may emphasize the suppressive effect of integrin-β3 on HSC expansion (Figure 5D; supplemental Table 2). We therefore suggest that suppression of cell division via a β3PY747-dependent mechanism could contribute to the maintenance of HSCs through the prevention of excess cell division. But the true mechanism by which β3-integrin ligation associates with TPO signaling and influences HSC function remains to be elucidated.
Fresh L746A HSCs without ex vivo culture exhibited LTR activity similar to that of WT HSCs in primary and secondary transplantation assays (Figure 1A). This confirms the dominant importance of outside-in signaling via β3PY747, as L746A is only critical for inside-out signaling, which implies a “change in the integrin conformational change.”21 But L746A mutants affected impaired outside-in based function (Figure 4B left), whereas ligation with 2C9.G2 in the presence of TPO plus Mn2+ augmented the LTR activity of HSCs (Figure 4B right). To explain this apparent discrepancy, we consider that at least outside-in signaling via β3PY747 may require the fully activated form of αvβ3-integrin during ex vivo culture. Alternatively, stimulants other than TPO may be required for this action. An investigation of extrinsic factors that induce the fully active conformation of αvβ3-integrin in HSCs via a pathway not involving the talin-binding motif, particularly Leu746 of β3-integrin, or an unknown TPO-dependent ligand from surrounding cells, may enable us to suggest or clarify the “true” niche circumstances of BM.
In our limited studies, VN-coated plates favored TPO-dependent enhancement of LTR activity in HSCs without Mn2+ (Figure 4G), whereas OPN required Mn2+ for its effect (Figure 4G). This suggests that VN, a major component of the BM sinusoid,46 rather than OPN, a component of the osteoblastic niche,2 is preferentially involved in HSC division via αvβ3-integrin. As has been claimed previously, the osteoblastic niche may preferentially use the interaction of β1 integrin (α4β1, α9β1) with OPN.1,2 Alternatively, there may be a TPO gradient within the BM microenvironment (ie, the TPO concentration in the osteoblastic niche is lower than in the sinusoid). Because a higher TPO concentration would accelerate HSC division into progenitors and further megakaryopoiesis, TPO-dependent activation of αvβ3-integrin via inside-out signaling may induce subsequent ligation with an appropriate ligand, leading to Tyr747 phosphorylation and, in turn, inhibition of cell division and maintenance of LTR activity on HSCs.
Our results show that the phenotype of β3−/− HSCs in transplantation assay and hierarchal cluster analysis is much closer to that of WT HSCs than Y747A HSCs (Figures 1A-C and 2A). This suggests that, in β3−/− HSCs, an as yet undetected system exerts a compensatory effect in response to the deficiency in the β3 molecular component. By contrast, impairment of outside-in signaling through Y747A point mutation might effectively and negatively affect LTR activity without inducing compensation because the β3 molecular component is retained in Y747A HSCs. Identification of the mechanisms that redundantly compensate for the absence of integrin-β3 signaling in β3−/− HSCs will require further investigation.
In conclusion, our findings demonstrate, for the first time, the critical role played by bidirectional β3-integrin signaling, especially outside-in signaling via β3PY747, in the maintenance of LTR activity in HSCs in vitro and in vivo. Moreover, activation of integrin-αvβ3, but not inside-out signaling, is required for β3PY747-mediated maintenance of HSC activity per each cell. This implies that the induction of activated integrin-αvβ3 can be regarded as a novel function of the HSC niche. We also show that outside-in signaling via β3PY747 plays an essential role in HSC maintenance mediated by TPO but not SCF, which suggests a novel mechanism for HSC maintenance by TPO. These results thus open a new area of inquiry into the link not only between integrin-αvβ3 activation and the surrounding microenvironment within the BM niche, but also between integrin and cytokine signaling in the maintenance of hematopoietic homeostasis.
Supplementary Material
Acknowledgments
The authors thank Dr M. H. Ginsberg (University of California–San Diego, La Jolla, CA) and Bristol-Myers Squibb (New York, NY) for providing L746A and Y747A KI mice, all of the members of our research group for discussion, and Drs S. Mitani and T. Furukawa for their great help in sequencing the whole transcriptome using the SOLiD system.
This work was supported in part by the Formation of Innovation Center for Fusion of Advanced Technologies in the Special Coordination Funds for Promoting Science and Technology Cell Sheet Tissue Engineering Center (M.Y. and T.O.), KIBAN (B, K.E.), and the Ministry of Education, Culture, Sports, Science and Technology, Japan (Special Promoted Grant, K.E.), the Mitsubishi Pharma Foundation (K.E.), and the National Institutes of Health (grant HL078784 RO1, B.G.P.).
Footnotes
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: T.U. and K.E. designed the study; T.U. performed most of the cellular and molecular experiments and wrote the paper; K.E. edited the manuscript; J.I. and M.U. helped with the cellular experiments; H.T. bred and kept the mice; Y.S., M.T., and T.S. helped with transplantation assays; B.G.P. generated integrin knock-in mice; and Y.M., M.Y., K.N., Y.K., H.N., and T.O. supervised aspects of the project and helped with manuscript preparation.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
The current affiliation for K.N. is Department of Ophthalmology, Osaka University, Graduate School of Medicine, Osaka, Japan.
Correspondence: Masayuki Yamato, Institute of Advanced Biomedical Engineering and Science, Tokyo Women's Medical University, Tokyo 162-8666, Japan; e-mail: myamato@abmes.twmu.ac.jp; and Koji Eto, Clinical Application Section, Center for iPS Cell Research and Application, Kyoto University, 53 Shogoin-Kawaharamachi, Sakyo-ku, Kyoto 606-8507, Japan; e-mail: kojieto@cira.kyoto-u.ac.jp.
References
- 1.Arai F, Hirao A, Ohmura M, et al. Tie2/angiopoietin-1 signaling regulates hematopoietic stem cell quiescence in the bone marrow niche. Cell. 2004;118(2):149–161. doi: 10.1016/j.cell.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 2.Nilsson SK, Johnston HM, Whitty GA, et al. Osteopontin, a key component of the hematopoietic stem cell niche and regulator of primitive hematopoietic progenitor cells. Blood. 2005;106(4):1232–1239. doi: 10.1182/blood-2004-11-4422. [DOI] [PubMed] [Google Scholar]
- 3.Qian H, Buza-Vidas N, Hyland CD, et al. Critical role of thrombopoietin in maintaining adult quiescent hematopoietic stem cells. Cell Stem Cell. 2007;1(6):671–684. doi: 10.1016/j.stem.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 4.Yoshihara H, Arai F, Hosokawa K, et al. Thrombopoietin/MPL signaling regulates hematopoietic stem cell quiescence and interaction with the osteoblastic niche. Cell Stem Cell. 2007;1(6):685–697. doi: 10.1016/j.stem.2007.10.020. [DOI] [PubMed] [Google Scholar]
- 5.Yamazaki S, Iwama A, Takayanagi S, Eto K, Ema H, Nakauchi H. TGF-beta as a candidate bone marrow niche signal to induce hematopoietic stem cell hibernation. Blood. 2009;113(6):1250–1256. doi: 10.1182/blood-2008-04-146480. [DOI] [PubMed] [Google Scholar]
- 6.Umemoto T, Yamato M, Shiratsuchi Y, et al. CD61 enriches long-term repopulating hematopoietic stem cells. Biochem Biophys Res Commun. 2008;365(1):176–182. doi: 10.1016/j.bbrc.2007.10.168. [DOI] [PubMed] [Google Scholar]
- 7.Umemoto T, Yamato M, Shiratsuchi Y, et al. Expression of integrin beta3 is correlated to the properties of quiescent hemopoietic stem cells possessing the side population phenotype. J Immunol. 2006;177(11):7733–7739. doi: 10.4049/jimmunol.177.11.7733. [DOI] [PubMed] [Google Scholar]
- 8.Ginsberg MH, Partridge A, Shattil SJ. Integrin regulation. Curr Opin Cell Biol. 2005;17(5):509–516. doi: 10.1016/j.ceb.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 9.Hynes RO. Integrins: bidirectional, allosteric signaling machines. Cell. 2002;110(6):673–687. doi: 10.1016/s0092-8674(02)00971-6. [DOI] [PubMed] [Google Scholar]
- 10.Juliano RL, Reddig P, Alahari S, Edin M, Howe A, Aplin A. Integrin regulation of cell signalling and motility. Biochem Soc Trans. 2004;32(3):443–446. doi: 10.1042/BST0320443. [DOI] [PubMed] [Google Scholar]
- 11.Gong H, Shen B, Flevaris P, et al. G protein subunit Galpha13 binds to integrin alphaIIbbeta3 and mediates integrin “outside-in” signaling. Science. 2010;327(5963):340–343. doi: 10.1126/science.1174779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tadokoro S, Shattil SJ, Eto K, et al. Talin binding to integrin beta tails: a final common step in integrin activation. Science. 2003;302(5642):103–106. doi: 10.1126/science.1086652. [DOI] [PubMed] [Google Scholar]
- 13.Takizawa H, Nishimura S, Takayama N, et al. Lnk regulates integrin alphaIIbbeta3 outside-in signaling in mouse platelets, leading to stabilization of thrombus development in vivo. J Clin Invest. 2010;120(1):179–190. doi: 10.1172/JCI39503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu Y, Welte T, Michaud M, Madri JA. PECAM-1: a multifaceted regulator of megakaryocytopoiesis. Blood. 2007;110(3):851–859. doi: 10.1182/blood-2006-05-022087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaushansky K. Thrombopoietin: the primary regulator of megakaryocyte and platelet production. Thromb Haemost. 1995;74(1):521–525. [PubMed] [Google Scholar]
- 16.Kimura S, Roberts AW, Metcalf D, Alexander WS. Hematopoietic stem cell deficiencies in mice lacking c-Mpl, the receptor for thrombopoietin. Proc Natl Acad SciU S A. 1998;95(3):1195–1200. doi: 10.1073/pnas.95.3.1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buza-Vidas N, Antonchuk J, Qian H, et al. Cytokines regulate postnatal hematopoietic stem cell expansion: opposing roles of thrombopoietin and LNK. Genes Dev. 2006;20(15):2018–2023. doi: 10.1101/gad.385606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Solar GP, Kerr WG, Zeigler FC, et al. Role of c-mpl in early hematopoiesis. Blood. 1998;92(1):4–10. [PubMed] [Google Scholar]
- 19.Alexander WS, Roberts AW, Nicola NA, Li R, Metcalf D. Deficiencies in progenitor cells of multiple hematopoietic lineages and defective megakaryocytopoiesis in mice lacking the thrombopoietic receptor c-Mpl. Blood. 1996;87(6):2162–2170. [PubMed] [Google Scholar]
- 20.Carver-Moore K, Broxmeyer HE, Luoh SM, et al. Low levels of erythroid and myeloid progenitors in thrombopoietin-and c-mpl-deficient mice. Blood. 1996;88(3):803–808. [PubMed] [Google Scholar]
- 21.Petrich BG, Fogelstrand P, Partridge AW, et al. The antithrombotic potential of selective blockade of talin-dependent integrin alpha IIb beta 3 (platelet GPIIb-IIIa) activation. J Clin Invest. 2007;117(8):2250–2259. doi: 10.1172/JCI31024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Szilvassy SJ, Humphries RK, Lansdorp PM, Eaves AC, Eaves CJ. Quantitative assay for totipotent reconstituting hematopoietic stem cells by a competitive repopulation strategy. Proc Natl Acad SciU S A. 1990;87(22):8736–8740. doi: 10.1073/pnas.87.22.8736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Feng X, Novack DV, Faccio R, et al. A Glanzmann's mutation in beta 3 integrin specifically impairs osteoclast function. J Clin Invest. 2001;107(9):1137–1144. doi: 10.1172/JCI12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kollet O, Dar A, Shivtiel S, et al. Osteoclasts degrade endosteal components and promote mobilization of hematopoietic progenitor cells. Nat Med. 2006;12(6):657–664. doi: 10.1038/nm1417. [DOI] [PubMed] [Google Scholar]
- 25.Shivtiel S, Kollet O, Lapid K, et al. CD45 regulates retention, motility, and numbers of hematopoietic progenitors, and affects osteoclast remodeling of metaphyseal trabecules. J Exp Med. 2008;205(10):2381–2395. doi: 10.1084/jem.20080072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kiel MJ, Yilmaz OH, Iwashita T, Terhorst C, Morrison SJ. SLAM family receptors distinguish hematopoietic stem and progenitor cells and reveal endothelial niches for stem cells. Cell. 2005;121(7):1109–1121. doi: 10.1016/j.cell.2005.05.026. [DOI] [PubMed] [Google Scholar]
- 27.Arias-Salgado EG, Lizano S, Shattil SJ, Ginsberg MH. Specification of the direction of adhesive signaling by the integrin beta cytoplasmic domain. J Biol Chem. 2005;280(33):29699–29707. doi: 10.1074/jbc.M503508200. [DOI] [PubMed] [Google Scholar]
- 28.Lawrence HJ, Christensen J, Fong S, et al. Loss of expression of the Hoxa-9 homeobox gene impairs the proliferation and repopulating ability of hematopoietic stem cells. Blood. 2005;106(12):3988–3994. doi: 10.1182/blood-2005-05-2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kirito K, Fox N, Kaushansky K. Thrombopoietin induces HOXA9 nuclear transport in immature hematopoietic cells: potential mechanism by which the hormone favorably affects hematopoietic stem cells. Mol Cell Biol. 2004;24(15):6751–6762. doi: 10.1128/MCB.24.15.6751-6762.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wu X, Mogford JE, Platts SH, Davis GE, Meininger GA, Davis MJ. Modulation of calcium current in arteriolar smooth muscle by alphav beta3 and alpha5 beta1 integrin ligands. J Cell Biol. 1998;143(1):241–252. doi: 10.1083/jcb.143.1.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mocsai A, Zhou M, Meng F, Tybulewicz VL, Lowell CA. Syk is required for integrin signaling in neutrophils. Immunity. 2002;16(4):547–558. doi: 10.1016/s1074-7613(02)00303-5. [DOI] [PubMed] [Google Scholar]
- 32.Obergfell A, Eto K, Mocsai A, et al. Coordinate interactions of Csk, Src, and Syk kinases with [alpha]IIb[beta]3 initiate integrin signaling to the cytoskeleton. J Cell Biol. 2002;157(2):265–275. doi: 10.1083/jcb.200112113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Noda S, Horiguchi K, Ichikawa H, Miyoshi H. Repopulating activity of ex vivo-expanded murine hematopoietic stem cells resides in the CD48-c-Kit+Sca-1+lineage marker- cell population. Stem Cells. 2008;26(3):646–655. doi: 10.1634/stemcells.2007-0623. [DOI] [PubMed] [Google Scholar]
- 34.Lishko VK, Podolnikova NP, Yakubenko VP, et al. Multiple binding sites in fibrinogen for integrin alphaMbeta2 (Mac-1). J Biol Chem. 2004;279(43):44897–44906. doi: 10.1074/jbc.M408012200. [DOI] [PubMed] [Google Scholar]
- 35.Wright SD, Weitz JI, Huang AJ, Levin SM, Silverstein SC, Loike JD. Complement receptor type three (CD11b/CD18) of human polymorphonuclear leukocytes recognizes fibrinogen. Proc Natl Acad SciU S A. 1988;85(20):7734–7738. doi: 10.1073/pnas.85.20.7734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smith JW, Piotrowicz RS, Mathis D. A mechanism for divalent cation regulation of beta 3-integrins. J Biol Chem. 1994;269(2):960–967. [PubMed] [Google Scholar]
- 37.Hu DD, Barbas CF, Smith JW. An allosteric Ca2+ binding site on the beta3-integrins that regulates the dissociation rate for RGD ligands. J Biol Chem. 1996;271(36):21745–21751. doi: 10.1074/jbc.271.36.21745. [DOI] [PubMed] [Google Scholar]
- 38.Ema H, Takano H, Sudo K, Nakauchi H. In vitro self-renewal division of hematopoietic stem cells. J Exp Med. 2000;192(9):1281–1288. doi: 10.1084/jem.192.9.1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Harrison DE, Jordan CT, Zhong RK, Astle CM. Primitive hemopoietic stem cells: direct assay of most productive populations by competitive repopulation with simple binomial, correlation and covariance calculations. Exp Hematol. 1993;21(2):206–219. [PubMed] [Google Scholar]
- 40.Ema H, Nakauchi H. Expansion of hematopoietic stem cells in the developing liver of a mouse embryo. Blood. 2000;95(7):2284–2288. [PubMed] [Google Scholar]
- 41.Jude CD, Climer L, Xu D, Artinger E, Fisher JK, Ernst P. Unique and independent roles for MLL in adult hematopoietic stem cells and progenitors. Cell Stem Cell. 2007;1(3):324–337. doi: 10.1016/j.stem.2007.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Deneault E, Cellot S, Faubert A, et al. A functional screen to identify novel effectors of hematopoietic stem cell activity. Cell. 2009;137(2):369–379. doi: 10.1016/j.cell.2009.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hock H, Meade E, Medeiros S, et al. Tel/Etv6 is an essential and selective regulator of adult hematopoietic stem cell survival. Genes Dev. 2004;18(19):2336–2341. doi: 10.1101/gad.1239604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Growney JD, Shigematsu H, Li Z, et al. Loss of Runx1 perturbs adult hematopoiesis and is associated with a myeloproliferative phenotype. Blood. 2005;106(2):494–504. doi: 10.1182/blood-2004-08-3280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xu R, Nelson CM, Muschler JL, Veiseh M, Vonderhaar BK, Bissell MJ. Sustained activation of STAT5 is essential for chromatin remodeling and maintenance of mammary-specific function. J Cell Biol. 2009;184(1):57–66. doi: 10.1083/jcb.200807021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.van Aken BE, Seiffert D, Thinnes T, Loskutoff DJ. Localization of vitronectin in the normal and atherosclerotic human vessel wall. Histochem Cell Biol. 1997;107(4):313–320. doi: 10.1007/s004180050116. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.