Abstract
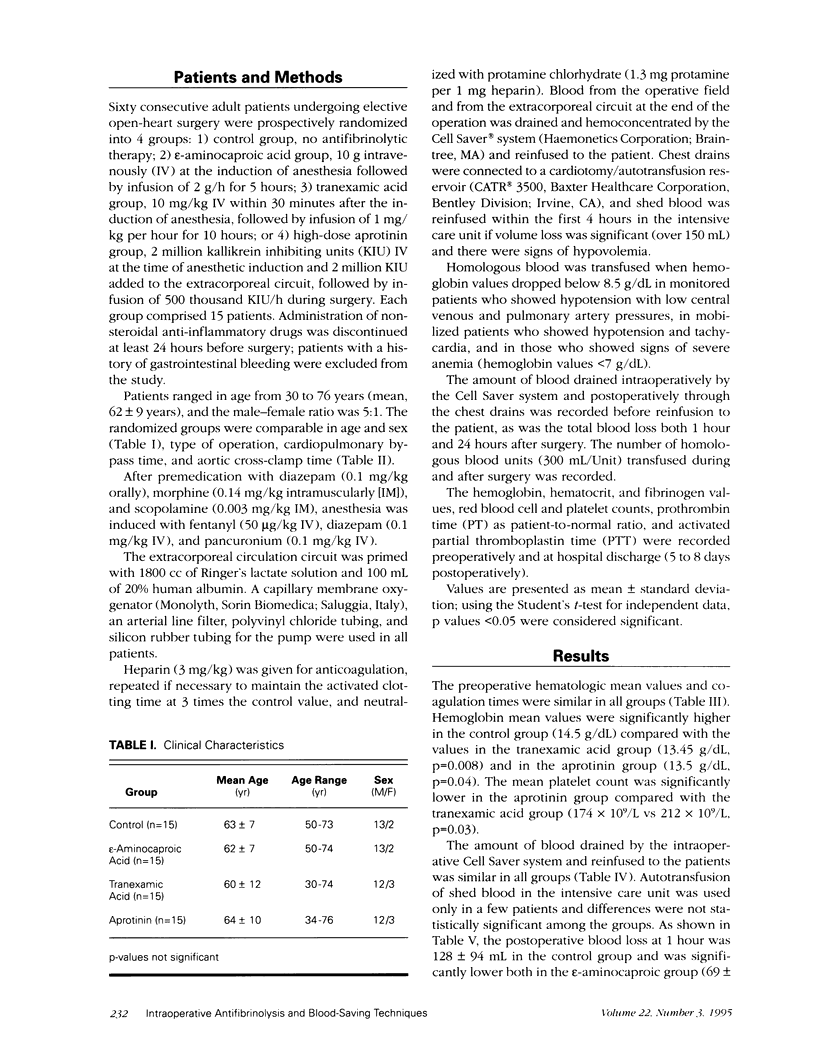
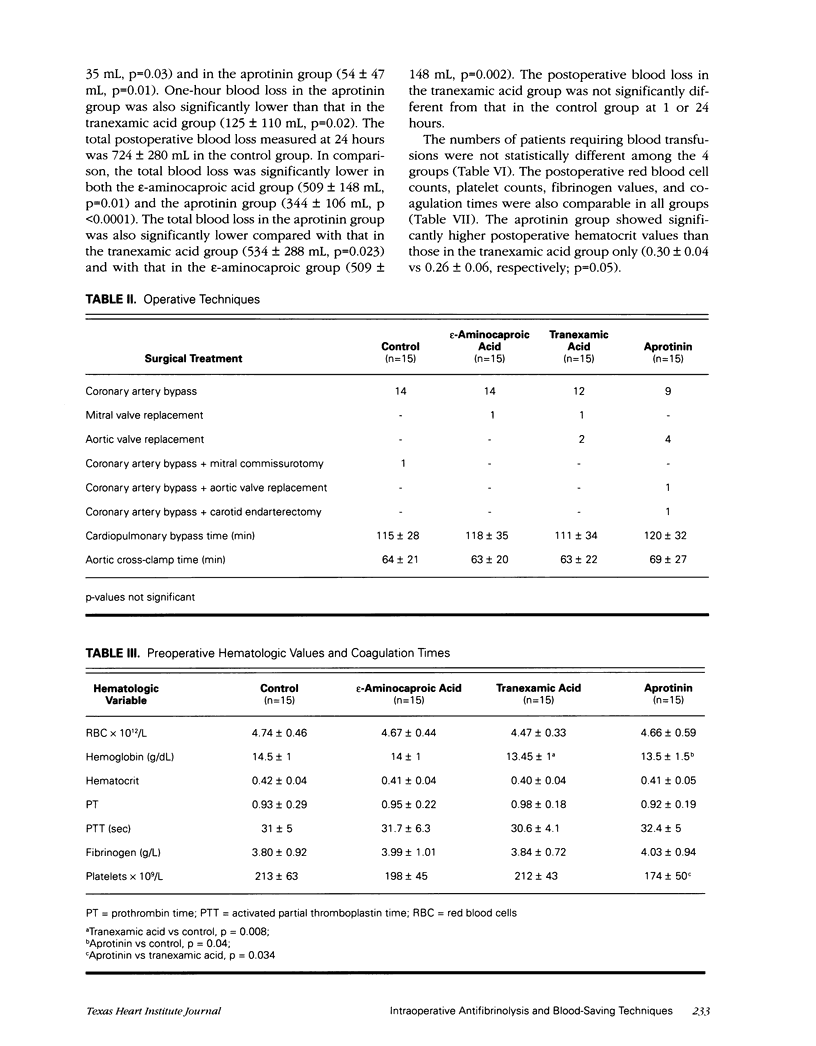
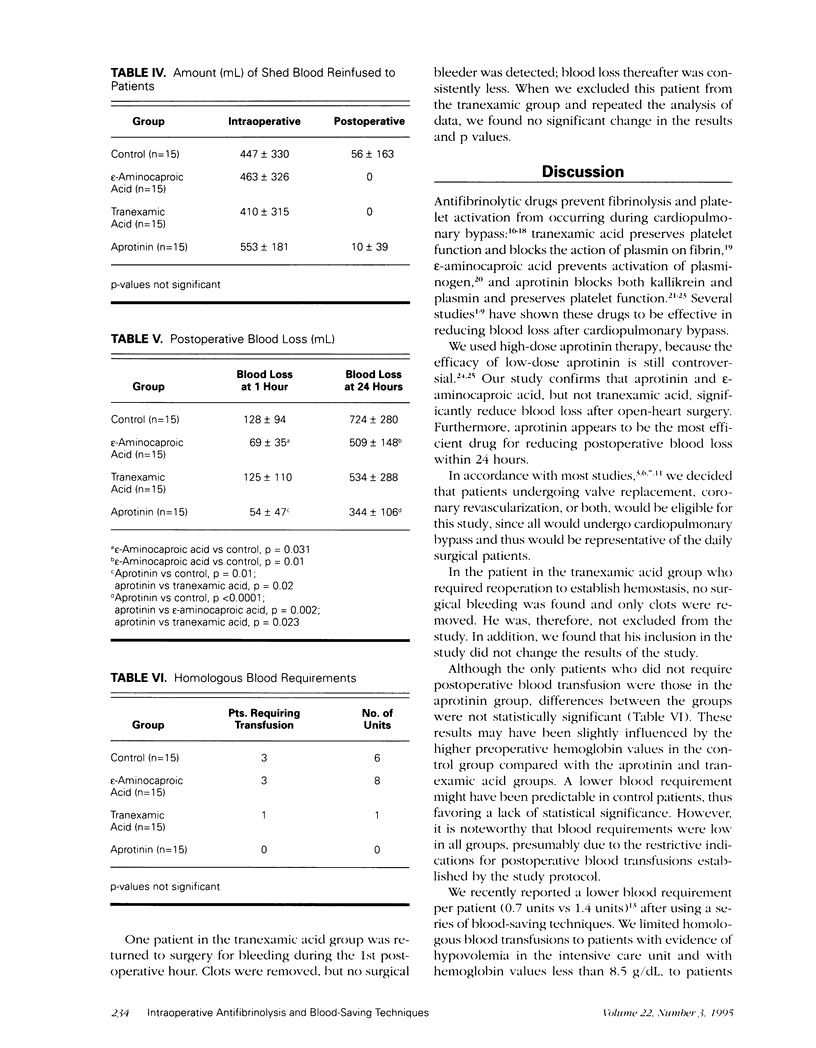
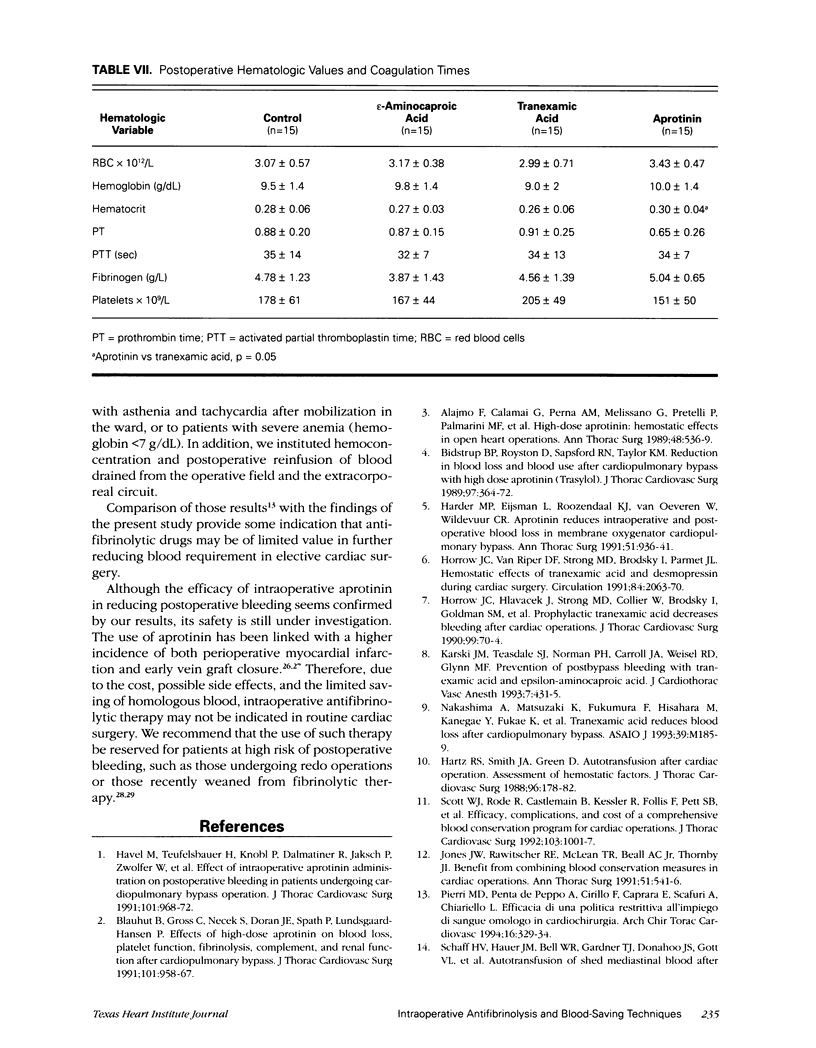
Sixty consecutive patients undergoing elective open-heart surgery were prospectively enrolled in a study to compare the efficacy of 3 different antifibrinolytic drugs to reduce postoperative bleeding and to reduce homologous blood requirements in combination with blood-saving techniques and restrictive indications for blood transfusion. The patients were randomized to 1 of 4 intraoperative treatment regimens: 1) control (no antifibrinolytic therapy); 2) epsilon-aminocaproic acid (10 g IV at induction of anesthesia, followed by infusion of 2 g/h for 5 hours); 3) tranexamic acid (10 mg/kg IV within 30 minutes after induction of anesthesia, followed by infusion of 1 mg/kg per hour for 10 hours); or 4) high-dose aprotinin (2 million KIU IV at induction of anesthesia and 2 million KIU added to the extracorporeal circuit, followed by infusion of 500 thousand KIU/h during surgery). Hemoconcentration and reinfusion of blood drained from the operative field and the extracorporeal circuit after operation were used in all patients. Indications for blood transfusion were hypotension, tachycardia, or both, with hemoglobin values < 8.5 g/dL; or severe anemia with hemoglobin values < 7 g/dL. Compared with the blood loss in the control group, patients receiving aprotinin and epsilon-aminocaproic acid showed significantly less postoperative blood loss at 1 hour (control, 128 +/- 94 mL; aprotinin, 54 +/- 47 mL, p = 0.01; and epsilon-aminocaproic acid, 69 +/- 35 mL, p = 0.03); this trend continued at 24 hours after operation (control, 724 +/- 280 mL; aprotinin, 344 +/- 106 mL, p < 0.0001; and epsilon-aminocaproic acid, 509 +/- 148 mL, p = 0.01). Aprotinin was significantly more efficient than epsilon-aminocaproic acid (p=0.002). Tranexamic acid did not have a statistically significant effect on blood loss. Homologous blood requirements were not significantly different among the groups; postoperative hematologic values and coagulation times were also comparable. Despite the efficacy of aprotinin and epsilon-aminocaproic acid shown in the present study, the blood requirements were not significantly different from those that are found when transfusions are restricted, autotransfusions are used, and blood from the operative field and extracorporeal circuit is concentrated and reinfused. Therefore, intraoperative antifibrinolysis may not be indicated in routine cardiac surgery when other blood-saving techniques are adopted.
Full text
PDF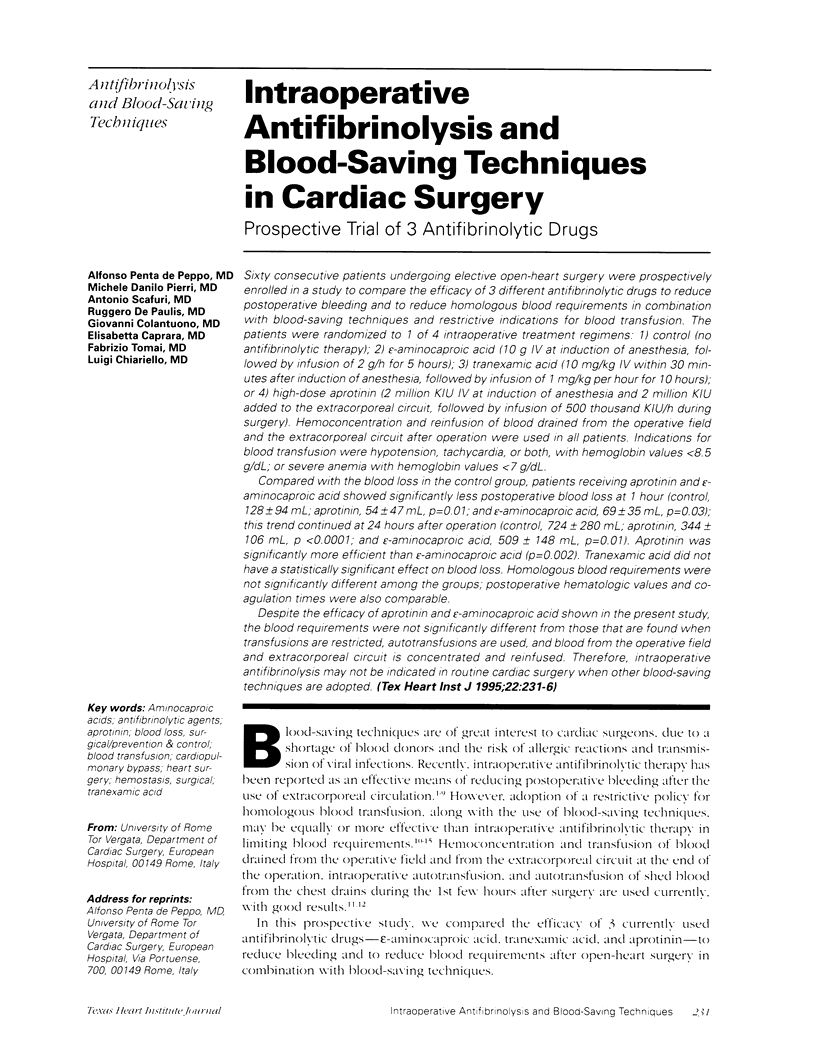

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alajmo F., Calamai G., Perna A. M., Melissano G., Pretelli P., Palmarini M. F., Carbonetto F., Noferi D., Boddi V., Palminiello A. High-dose aprotinin: hemostatic effects in open heart operations. Ann Thorac Surg. 1989 Oct;48(4):536–539. doi: 10.1016/s0003-4975(10)66857-9. [DOI] [PubMed] [Google Scholar]
- Bidstrup B. P., Royston D., Sapsford R. N., Taylor K. M. Reduction in blood loss and blood use after cardiopulmonary bypass with high dose aprotinin (Trasylol). J Thorac Cardiovasc Surg. 1989 Mar;97(3):364–372. [PubMed] [Google Scholar]
- Blauhut B., Gross C., Necek S., Doran J. E., Späth P., Lundsgaard-Hansen P. Effects of high-dose aprotinin on blood loss, platelet function, fibrinolysis, complement, and renal function after cardiopulmonary bypass. J Thorac Cardiovasc Surg. 1991 Jun;101(6):958–967. [PubMed] [Google Scholar]
- Cosgrove D. M., 3rd, Heric B., Lytle B. W., Taylor P. C., Novoa R., Golding L. A., Stewart R. W., McCarthy P. M., Loop F. D. Aprotinin therapy for reoperative myocardial revascularization: a placebo-controlled study. Ann Thorac Surg. 1992 Dec;54(6):1031–1038. doi: 10.1016/0003-4975(92)90066-d. [DOI] [PubMed] [Google Scholar]
- Efstratiadis T., Munsch C., Crossman D., Taylor K. Aprotinin used in emergency coronary operation after streptokinase treatment. Ann Thorac Surg. 1991 Dec;52(6):1320–1321. doi: 10.1016/0003-4975(91)90022-i. [DOI] [PubMed] [Google Scholar]
- Gravlee G. P., Haddon W. S., Rothberger H. K., Mills S. A., Rogers A. T., Bean V. E., Buss D. H., Prough D. S., Cordell A. R. Heparin dosing and monitoring for cardiopulmonary bypass. A comparison of techniques with measurement of subclinical plasma coagulation. J Thorac Cardiovasc Surg. 1990 Mar;99(3):518–527. [PubMed] [Google Scholar]
- Harder M. P., Eijsman L., Roozendaal K. J., van Oeveren W., Wildevuur C. R. Aprotinin reduces intraoperative and postoperative blood loss in membrane oxygenator cardiopulmonary bypass. Ann Thorac Surg. 1991 Jun;51(6):936–941. doi: 10.1016/0003-4975(91)91009-k. [DOI] [PubMed] [Google Scholar]
- Hardy J. F., Desroches J., Belisle S., Perrault J., Carrier M., Robitaille D. Low-dose aprotinin infusion is not clinically useful to reduce bleeding and transfusion of homologous blood products in high-risk cardiac surgical patients. Can J Anaesth. 1993 Jul;40(7):625–631. doi: 10.1007/BF03009699. [DOI] [PubMed] [Google Scholar]
- Hartz R. S., Smith J. A., Green D. Autotransfusion after cardiac operation. Assessment of hemostatic factors. J Thorac Cardiovasc Surg. 1988 Jul;96(1):178–182. [PubMed] [Google Scholar]
- Havel M., Teufelsbauer H., Knöbl P., Dalmatiner R., Jaksch P., Zwölfer W., Müller M., Vukovich T. Effect of intraoperative aprotinin administration on postoperative bleeding in patients undergoing cardiopulmonary bypass operation. J Thorac Cardiovasc Surg. 1991 Jun;101(6):968–972. [PubMed] [Google Scholar]
- Horrow J. C., Hlavacek J., Strong M. D., Collier W., Brodsky I., Goldman S. M., Goel I. P. Prophylactic tranexamic acid decreases bleeding after cardiac operations. J Thorac Cardiovasc Surg. 1990 Jan;99(1):70–74. [PubMed] [Google Scholar]
- Horrow J. C., Van Riper D. F., Strong M. D., Brodsky I., Parmet J. L. Hemostatic effects of tranexamic acid and desmopressin during cardiac surgery. Circulation. 1991 Nov;84(5):2063–2070. doi: 10.1161/01.cir.84.5.2063. [DOI] [PubMed] [Google Scholar]
- Johnson R. G., Rosenkrantz K. R., Preston R. A., Hopkins C., Daggett W. M. The efficacy of postoperative autotransfusion in patients undergoing cardiac operations. Ann Thorac Surg. 1983 Aug;36(2):173–179. doi: 10.1016/s0003-4975(10)60452-3. [DOI] [PubMed] [Google Scholar]
- Jones J. W., Rawitscher R. E., McLean T. R., Beall A. C., Jr, Thornby J. I. Benefit from combining blood conservation measures in cardiac operations. Ann Thorac Surg. 1991 Apr;51(4):541–546. doi: 10.1016/0003-4975(91)90305-a. [DOI] [PubMed] [Google Scholar]
- Karski J. M., Teasdale S. J., Norman P. H., Carroll J. A., Weisel R. D., Glynn M. F. Prevention of postbypass bleeding with tranexamic acid and epsilon-aminocaproic acid. J Cardiothorac Vasc Anesth. 1993 Aug;7(4):431–435. doi: 10.1016/1053-0770(93)90165-h. [DOI] [PubMed] [Google Scholar]
- Kirklin J. K., Westaby S., Blackstone E. H., Kirklin J. W., Chenoweth D. E., Pacifico A. D. Complement and the damaging effects of cardiopulmonary bypass. J Thorac Cardiovasc Surg. 1983 Dec;86(6):845–857. [PubMed] [Google Scholar]
- Lambert C. J., Marengo-Rowe A. J., Leveson J. E., Green R. H., Thiele J. P., Geisler G. F., Adam M., Mitchel B. F. The treatment of postperfusion bleeding using epsilon-aminocaproic acid, cryoprecipitate, fresh-frozen plasma, and protamine sulfate. Ann Thorac Surg. 1979 Nov;28(5):440–444. doi: 10.1016/s0003-4975(10)63153-0. [DOI] [PubMed] [Google Scholar]
- Murkin J. M., Lux J., Shannon N. A., Guiraudon G. M., Menkis A. H., McKenzie F. N., Novick R. J. Aprotinin significantly decreases bleeding and transfusion requirements in patients receiving aspirin and undergoing cardiac operations. J Thorac Cardiovasc Surg. 1994 Feb;107(2):554–561. [PubMed] [Google Scholar]
- Nakashima A., Matsuzaki K., Fukumura F., Hisahara M., Kanegae Y., Fukae K., Miyamoto K., Nishida T., Tokunaga S., Tominaga R. Tranexamic acid reduces blood loss after cardiopulmonary bypass. ASAIO J. 1993 Jul-Sep;39(3):M185–M189. [PubMed] [Google Scholar]
- Schaff H. V., Hauer J. M., Bell W. R., Gardner T. J., Donahoo J. S., Gott V. L., Brawley R. K. Autotransfusion of shed mediastinal blood after cardiac surgery: a prospective study. J Thorac Cardiovasc Surg. 1978 Apr;75(4):632–641. [PubMed] [Google Scholar]
- Schönberger J. P., Everts P. A., Ercan H., Bredée J. J., Bavinck J. H., Berreklouw E., Wildevuur C. R. Low-dose aprotinin in internal mammary artery bypass operations contributes to important blood saving. Ann Thorac Surg. 1992 Dec;54(6):1172–1176. doi: 10.1016/0003-4975(92)90089-m. [DOI] [PubMed] [Google Scholar]
- Scott W. J., Rode R., Castlemain B., Kessler R., Follis F., Pett S. B., Wernly J. A. Efficacy, complications, and cost of a comprehensive blood conservation program for cardiac operations. J Thorac Cardiovasc Surg. 1992 May;103(5):1001–1007. [PubMed] [Google Scholar]
- Soslau G., Horrow J., Brodsky I. Effect of tranexamic acid on platelet ADP during extracorporeal circulation. Am J Hematol. 1991 Oct;38(2):113–119. doi: 10.1002/ajh.2830380208. [DOI] [PubMed] [Google Scholar]
- Tanaka K., Takao M., Yada I., Yuasa H., Kusagawa M., Deguchi K. Alterations in coagulation and fibrinolysis associated with cardiopulmonary bypass during open heart surgery. J Cardiothorac Anesth. 1989 Apr;3(2):181–188. doi: 10.1016/s0888-6296(89)92642-2. [DOI] [PubMed] [Google Scholar]
- Westaby S. Aprotinin in perspective. Ann Thorac Surg. 1993 Apr;55(4):1033–1041. doi: 10.1016/0003-4975(93)90149-c. [DOI] [PubMed] [Google Scholar]
- van Oeveren W., Harder M. P., Roozendaal K. J., Eijsman L., Wildevuur C. R. Aprotinin protects platelets against the initial effect of cardiopulmonary bypass. J Thorac Cardiovasc Surg. 1990 May;99(5):788–797. [PubMed] [Google Scholar]
- van Oeveren W., Jansen N. J., Bidstrup B. P., Royston D., Westaby S., Neuhof H., Wildevuur C. R. Effects of aprotinin on hemostatic mechanisms during cardiopulmonary bypass. Ann Thorac Surg. 1987 Dec;44(6):640–645. doi: 10.1016/s0003-4975(10)62153-4. [DOI] [PubMed] [Google Scholar]


