Abstract
OBJECTIVE
The aim of the current study was to determine the influence of implicated affective circuitry disturbance in pediatric bipolar disorder (PBD) on behavioral inhibition. The differential influence of an antipsychotic and an anti-epileptic medication on the functional connectivity across affective and cognitive neural operations in PBD was examined..
METHODS
This was a six-week double blind randomized fMRI trial of risperidone plus placebo vs. divalproex plus placebo for patients with mania (n=22; 13.6±2.5 years). Healthy controls (HC; n=14, 14.5±2.8 years) were also scanned for normative comparison. Participants performed a response inhibition fMRI task where a motor response, already ‘on the way’ to execution, had to be voluntarily inhibited on trials where a stop signal was presented. Independent component analysis was used to map functional connectivity across the whole brain.
RESULTS
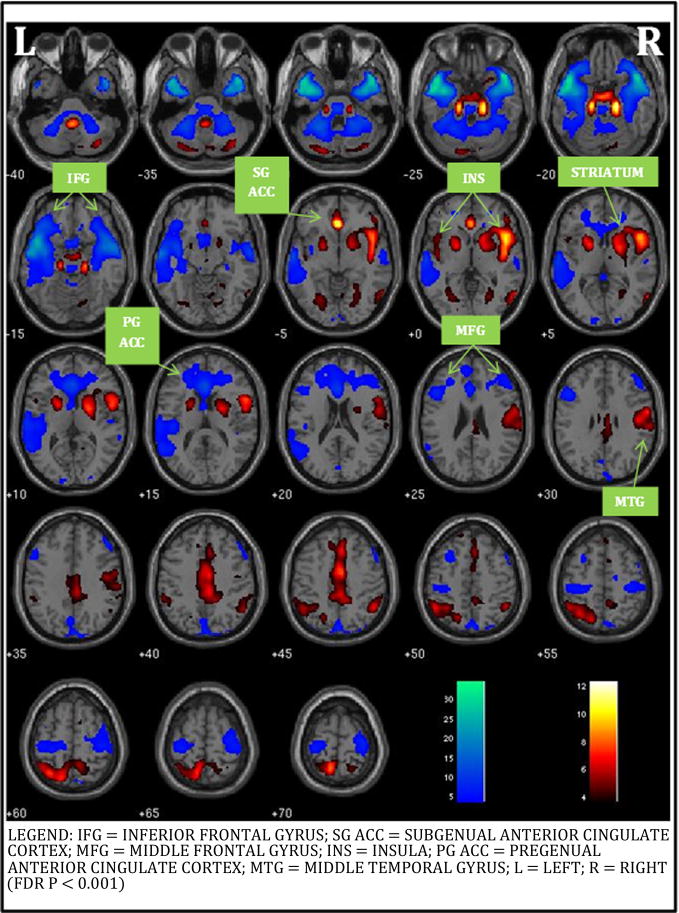
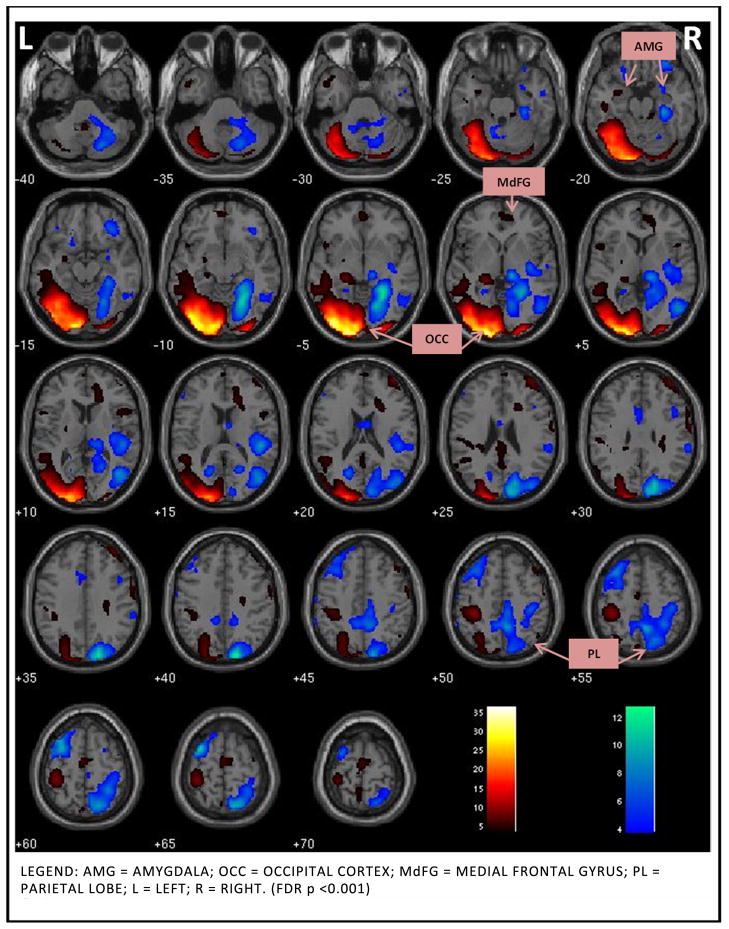
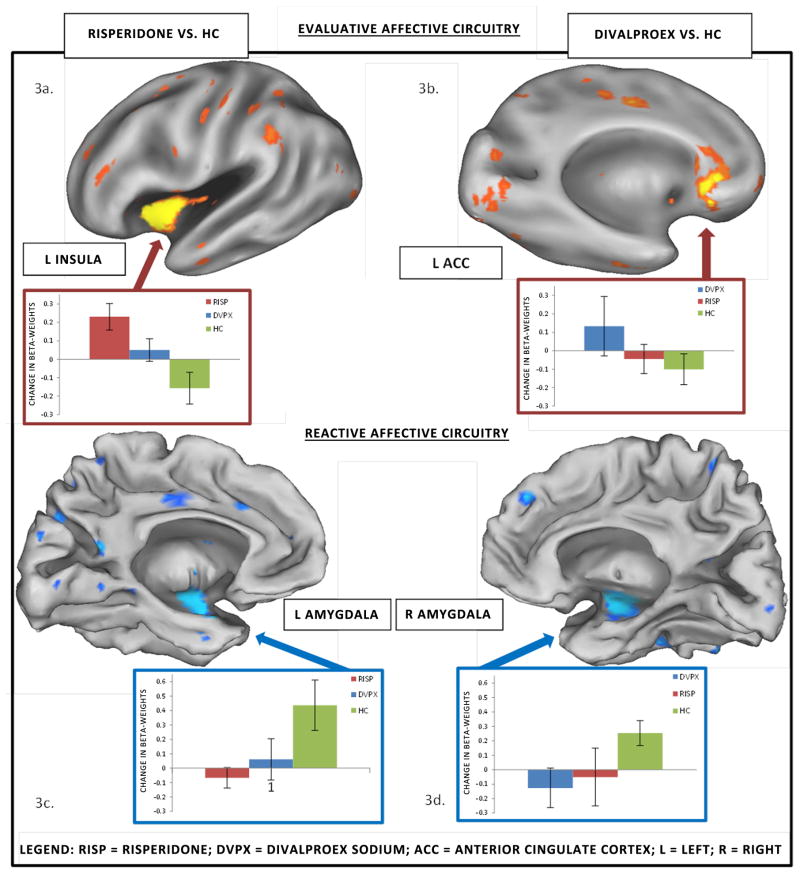
While there were no behavioral differences between the groups at pre- or post-drug trial, there was significant improvement on manic symptoms in the patient groups. All participants engaged an Evaluative Affective Circuit (EAC: bilateral inferior frontal gyrus, middle frontal gyrus, anterior cingulate cortex (ACC), middle temporal gyrus, insulae, caudate and putamen) and a Reactive Affective Circuit (RAC: bilateral occipital cortex, amygdala, medial frontal gyrus and insula) during task performance. Within the EAC, post treatment and relative to HC, greater engagement was seen in left insula in risperidone group and left subgenual ACC in divalproex group. Within the RAC, greater baseline amygdala connectivity in patients did not alter with treatment.
CONCLUSION
EAC and RAC are two key circuits that moderate emotional influence on response inhibition in PBD. Risperidone and divalproex differentially engage the EAC. Limited change in amygdala activity with treatment in all patients indicates a likely trait deficit in PBD.
Keywords: Functional connectivity, bipolar disorder, pediatric, response inhibition, affect
1. INTRODUCTION
Overcoming the important challenges in understanding how affective abnormalities contribute to disinhibition and impulsivity in pediatric bipolar disorder (PBD) will help discover how interventions can alter these neural operations. To date, numerous studies of pediatric mania have focused on affective processing with or without cognitive challenge which have typically shown underactivity in ventrolateral prefrontal cortex (VLPFC), medial PFC (MPFC), dorsolateral PFC (DLPFC) [1] [2] [3] and overactivity in anterior cingulate cortex (ACC), amygdala, and striatum [2] [3] [4] [5] [6] [7]. In addition, reduced connectivity in PBD was found in an emotional face response circuit consisting of the amygdala, posterior cingulate/precuneus, and fusiform/parahippocampal gyrus [8], suggesting further dysfunction at multiple circuitry-wide levels. Similarly, decreased functional connectivity during mania between DLPFC and temporal circuitry has even been found while participants were in a resting state [9]. Further, pharmacological fMRI studies of pediatric mania with risperidone, divalproex and lamotrigine have shown increased activity during cognitive control under emotional challenge in VLPFC, DLPFC, MPFC, subgenual ACC, temporal lobe, and striatum [10] [11] [12] [13], but the amygdala remained overactive relative to healthy controls (HC) [13]. Such affective circuitry level disturbance in PBD is likely to influence cognitive function, given our previous findings illustrating a strong interlink between affective and cognitive systems [7] [14] [15]. Therefore, in the current study, we sought to further examine how affective neural systems commonly involved in PBD influence impulsivity and disinhibition using cognitive paradigms without any affective stimuli [16].
There have been several fMRI studies of motor inhibition in pediatric mania, including one treatment study. Leibenluft et al. [17] showed that failed inhibition during a Stop Signal task in PBD involved decreased activation in right VLPFC and bilateral striatum when compared to healthy controls (HC). In addition, a recent study employing a blocked Go/NoGo task similar to the Stop Signal task used in the current study found increased activation in the DLPFC in participants with PBD relative to controls [18]. However, the Go/NoGo task employed in the Singh et al. study involved withholding a prepotent response, rather than interrupting a response that was already on the way to completion, so the results of that study might not be directly comparable with the present study. Recent studies by Passarotti et al. [13] [16] [14] showed that emotionally linked brain regions such as the VLPFC and pregenual ACC are implicated both in the cognitive control of emotional processing and in behavior inhibition in pediatric mania relative to attention deficit hyperactivity disorder (ADHD). Therefore, a particular challenge in PBD studies is to unravel the relationship between emotional systems and inhibitory control systems in manic states. In addition, understanding the effects of medication treatments on the neural networks involved in response inhibition in PBD would help us understand the intervention effects on the neural function. For example, lamotrigine monotherapy has been shown to enhance underactive MPFC and temporal lobe regions during a response inhibition task, suggesting that mood stabilizers which improve function in affective regions can also influence the brain networks involved in response inhibition [19]. Examining how dysfunction in the neural networks central to affective disturbance in PBD [1] [2] [3] [4] [5] [6] [7] impacts motor inhibition will more conclusively link the affective disturbance that is the hallmark of PBD to its behavioral consequences.
Informed by the aforementioned fMRI studies of PBD, we have proposed theoretical models of functional networks [20] involving regions of higher cortical evaluation of emotional and behavioral control in the VLPFC, [2] [4] emotional evaluation in the MPFC, [21] and executive function of emotion modulation in the DLPFC [1] [4] [7] [21]. Additionally, emotional and cognitive control and modulation is accompanied by greater activity in the ACC in PBD [1] [4] [7] [21] involved in both compensatory error correction and the complex interface of affective and cognitive processing [22]. This collection of brain regions can be considered an Evaluative Affective Circuit (EAC) that is likely to contribute to behavioral disinhibition in PBD by interfering with oversight of behavioral control. Another proposed complementary posterior circuit was an occipito-limbic associative circuit [20] linking the occipital cortex and amygdala, which is activated in response to incidental emotional processing [23] [24]. This Reactive Affective Circuit (RAC) contributes to impulsive automatic response tendencies, which are moderated by evaluative MPFC region.
The regions within EAC and RAC inter-communicate and are important for task success. We implemented a novel approach to study functional connectivity among specific brain regions within the EAC and RAC networks that influence activity in distal regions within each network during task performance [25]. Independent Component Analysis (ICA), used in the current study, is a model-free technique that robustly identifies distinct spatiotemporal profiles of distributed brain function that closely correspond to known anatomical neural networks. This approach was used as a means to test hypotheses regarding regional functional connectivity during response inhibition. Although previous studies have documented impairments in specific brain regions underlying response inhibition in PBD [17] [19] [26] [18], and other studies have documented networks involved in response inhibition in normal adolescents, [27] to date, there have been no direct tests of whether brain regions in the EAC or RAC show disrupted functional connectivity in PBD during demands for behavioral control. Therefore, the first goal of this study was to use functional connectivity to map PBD pathophysiology within the hypothesized EAC and RAC. We predicted that PBD patients would show less functional connectivity within each of these key networks during response inhibition.
A second goal was to link the hypothesized functional connectivity deficits to clinical improvement in response to two different classes of medications known to stabilize affect in PBD. One of the medications, risperidone, an antipsychotic that acts by serotonin dopamine antagonism, [28] is known to reduce manic symptoms in PBD, [29] and improves VLPFC and MPFC activity [12]. We predicted that risperidone would improve EAC functional connectivity and that the treatment-induced reduction in manic symptoms will correlate with the change in EAC connectivity. The other medication, divalproex sodium (divalproex), is an anti-epileptic that modulates intracellular pathways [30] and also serves as a traditional mood stabilizer known to reduce both manic and depressive symptoms [31] [32]. Given that a similar anti-epileptic, lamotrigine, led to greater subgenual and MPFC activity in pediatric mania during response inhibition [19], we predicted that divalproex would also improve functional connectivity in EAC and that reduction in both the manic and depressive symptoms will correlate with the change in EAC. With regards to the RAC, previous functional imaging results are equivocal, with persistent increase in amygdala activity, relative to HC, with treatment of mania [13] and decreased activity with reduction in depression within patients [33]. Our findings will inform if functional connectivity in this circuit will be altered by either of the medications. Essentially, given that this is the first study comparing divalproex and risperidone effect on behavior inhibition in pediatric mania, we began with the premise that both medications would have an equal impact on EAC and RAC.
2. METHODS
2.1 Design
This was an NIH-funded (1 K23 RR018638-01) six-week outpatient double blind randomized controlled trial (DBRCT) of risperidone plus placebo (that resembled a divalproex capsule) vs. divalproex plus placebo (that resembled a risperidone tablet) for manic and mixed episodes of bipolar disorder. This study was approved by the University of Illinois at Chicago’s Institutional Review Board (IRB).
2.2 Sample
Inclusion criteria were a DSM-IV diagnosis of mixed or manic bipolar disorder; 12 to 18 years old; and medication free or currently clinically unstable on medication, justifying termination of the ineffective regimen (with consent, all subjects were washed out and free of any medication for a week prior to baseline scanning, and 4 weeks in case of fluoxetine or aripiprazole). Prior exposure to SGAs and anti-epileptic medications was acceptable. Exclusion criteria included: active substance abuse; serious medical problems; autism and non-affective psychotic disorders. Participants who had a diagnosis of ADHD preceding the onset of PBD were excluded to reduce the confound of comorbid attentional disorders, relevant specifically in probing response inhibition. Using these criteria, we recruited 44 subjects into the study. After excluding subjects whose data were unusable due to motion artifacts (HC: n=2; risperidone group: n=3; divalproex group: n=3), the final sample included in the analyses consisted of 14 HC, and 22 patients randomized to either risperidone (n=11) or divalproex (n=11). No subjects dropped out of the study. Sample characteristics are summarized in Table 1.
Table 1.
Demographic Variables and Clinical Characteristics
| DVPX (N = 11) | RISP (N= 11) | HC (N = 14) | RISP vs. DVPX | ||
|---|---|---|---|---|---|
| Variable | Mean (SD) | Mean (SD) | Mean (SD) | F (2, 33), p | t(20), p |
| Age in Years (Age Range: 10 – 19) | 12.09 (2.47) | 12.64 (1.69) | 14.14 (3.01) | 2.29, p = .117 | .61, p = .552 |
| Estimated IQa (IQ Range: 70–139) | 96.17 (18.2) | 94.67 (9.7) | 106.5 (12.0) | 2.96, p = .07 | .45, p = .774 |
| YMRS pre | 25.5 (7.6) | 27.2 (6.6) | .9 (1.5) | 88.54, p < .001 | .54, p = .595 |
| YMRS post | 12.6 (9.3) | 11.6 (11.7) | 1.1 (1.9) | 7.67, p = .002 | .22, p = .826 |
| YMRS change | 12.9 (9.4) | 15.5 (9.4) | −0.2 (1.8) | 16.73, p < .001 | .66, p = .517 |
| CDRS-R pre | 39.6 (15.3) | 45.7 (14.9) | 19.5 (2.5) | 17.04, p < .001 | .96, p = .348 |
| CDRS-R post | 30.0 (7.7) | 26.3 (6.8) | 18.6 (1.4) | 8.93, p = .001 | 1.21, p = .242 |
| CDRS-R change | 9.6 (11.2) | 19.4 (14.1) | .9 (1.5) | 5.35, p = .01 | 1.83, p = .083 |
| Variable | N (%) | N (%) | N (%) | X2(df = 2), p | Fisher’s Exact p |
| Sex | |||||
| Male | 9 (82%) | 7 (64%) | 7 (50%) | 2.70, p = .259 | p = .635 |
| Female | 2 (18%) | 4 (36%) | 7 (50%) | ||
| Handedness | |||||
| Left | 2 (18%) | 0 (0%) | 0 (0%) | 4.83, p =.090 | p = .476 |
| Right | 9 (82%) | 14 (100%) | 14 (100%) | ||
| Race Composition | |||||
| Caucasian | 7 (64%) | 7 (64%) | 8 (57%) | .152, p = .927 | p = 1.0 |
| Other | 4 (36%) | 4 (36%) | 6 (43%) |
Legend: DVPX=Divalproex; RISP=Risperidone; HC=Healthy Control; YMRS=Young Mania Rating Scale; CDRS-R=Child Depression Rating Scale-Revised; SES=socioeconomic status.
Estimated with Wechsler Abbreviated Scale of Intelligence (WASI; Matrix Reasoning and Vocabulary Subtests).
2.3 Assessment and efficacy measures
Each child and their parent or legal guardian were interviewed using the Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U-KSADS) supplemented by the episode characterization of bipolar disorder from the KSADS - Present and Lifetime version [34]. Diagnostic interviews were completed by doctoral-level clinicians with established inter-rater reliability. The primary clinical efficacy measure was the Young Mania Rating Scale (YMRS) [35]. The Child Depression Rating Scale-Revised was also administered (CDRS-R) [36].
2.4 Study dosing of risperidone and divalproex
The mean (standard deviation, SD) risperidone dose at endpoint was 1.43 (±0.35) mg/day in non-responders and 1.33 (±.43) mg/day in responders (defined as improvement >=50% on the YMRS scores). The mean (SD) divalproex dose at endpoint was 863.64 (±210.54) mg/day in non-responders and 855.14 (±245.23) mg/day in responders. The mean serum valproic level at end point was 98 μg/mL, and 95% of patients achieved a therapeutic serum valproic level of > 75 μg/mL by the 5th day. No titration of medications was allowed after day 7. One subject in the divalproex group received lorazepam as a rescue medication at a dose of 2 mg for severe agitation during the first week of the trial. No other rescue medications or stimulants were used during the trial.
2.5 fMRI Session: Response Inhibition Task (http://www.psych.uic.edu/brain-center/response_inhibition.html)
The fMRI behavioral paradigm was a block design task in which a motor response, already ‘on the way’ from planning to execution, had to be voluntarily inhibited when a cue instructing subjects to stop an impending response was presented on some trials [19]. At the beginning of each trial a fixation cross appeared for 850 ms. On Go trials, a target stimulus (a green airplane) was presented for 800 ms. On Stop trials, a Stop signal (a man holding a Stop signal in his hands) replaced the airplane with equal probability 250, 350, or 450 ms after the airplane appeared and subjects had to inhibit their response. The task lasted 6.11 minutes and consisted of six experimental blocks, three of which were Go blocks (G) and three of which were Stop blocks (S), and there were 7 resting blocks (F) of 10 sec fixation each. Each experimental block had 30 trials and lasted 49.5 sec. The experimental and fixation blocks were pseudo-randomly interspersed as follows: (F) G (F) S (F) S (F) G (F) S (F) G (F). We adopted this 70/30 proportion of trials in both the Go and Stop blocks (e.g., 70% Stop trials in Stop block and 70% of Go trials in Go block) so that subjects would not habituate to fixed trial presentation within a certain block.
2.6 MRI Protocols
Gradient-echo echo-planar functional imaging and structural acquisitions were performed with a 3.0 Tesla whole body scanner (Signa, General Electric Medical System, Milwaukee, WI) at the MR Center within the UIC Hospital. To minimize head motion we restricted the participants’ head with foam cushions. T2*-weighted functional images were acquired with a gradient-echo echo-planar sequence (TR=2500ms, TE=25ms, flip angle=90°, FOV 20 × 20 cm2, 64 × 64 matrix, 3.125 by 3.125 mm in plane resolution, 5-mm slice thickness, 1-mm gap, 25 slices). Anatomical images were also acquired in the axial plane (three-dimensional spoiled gradient recalled, 1.5mm thick contiguous axial slices) and were later co-registered with the functional data. The experiment run consisted of 240 time points including a 5 sec rest session at the beginning that was collected to allow for T1 effects to stabilize. These initial two images were not included in the analyses.
2.7 fMRI Image Processing and Motion Correction
FIASCO software (Functional Imaging Analysis Software - Computational Olio) [37] was used to implement 3D motion estimation and correction, removal of slow signal drift, and identification of images with artifacts such as high shot noise or displacement that cannot be readily corrected by motion correction algorithms. We excluded from the analyses individual volumes from the time series if head displacement from the median head position was greater than 1.5 mm, or if head rotation from the median head position was greater than 0.5 degrees. There were no significant group differences in the number of volumes retained after discarding those with motion artifact. Individual volumes were excluded from analyses if, relative to median head position, head displacement was greater than 1.5mm or head rotation was greater than 0.5 degrees. T-tests revealed no significant group differences in the number of volumes retained after discarding those with motion artifact. After motion correction and de-trending using FIASCO, the functional images were preprocessed with SPM5 (http://www.fil.ion.ucl.ac.uk/spm/software/spm5/). Slice timing correction was applied to the data to remove signal variation due to slice acquisition temporal onset differences. The first functional image volume of each participant was used to determine parameters for spatial normalization into Montreal Neurological Institute (MNI) standardized space employed in SPM5 using non-linear transformation. The normalization parameters determined for the first functional volume were subsequently applied to all of the 240 functional image volumes for each participant. The normalized functional images were then smoothed with a 12-mm full width at half-maximum Gaussian filter.
2.8 Independent Component Analysis
fMRI time series from all participants for the response inhibition task were analyzed using a group ICA algorithm (GIFT v1.3h; http://icatb.sourceforge.net) [38] [39]. The fMRI time series data for all participants were concatenated, then subjected to two principal component analysis data reduction stages [38]. The data underwent a final ICA rotation using Infomax that produced 37 maximally independent components [40]. The number of components to estimate was determined using the minimum description length criteria [41]. Using the ICA-derived group solution, data for each participant were then back-reconstructed [42] so that individual participant variability was retained for hypothesis testing. For each component, this back-reconstruction method produced a spatial map representing brain regions within each component “network”, and a time course of BOLD signal change across the fMRI paradigm. Group analyses of spatial maps determined differences in degree of regional functional connectivity, while analyses of time-course information allowed us to determine whether or not study groups engaged each network during the fMRI task.
A systematic process was used on the 37 independent components to identify those that would be retained for further analysis. The correlation of each component’s spatial map with a priori probabilistic maps of gray matter, white matter, and cerebral spinal fluid (CSF) within MNI space (templates provided in SPM5) was calculated for all components. After discarding components with an r-squared value > .025 with CSF or white matter, or with low correlation to gray matter that could be an artifact, 28 components were retained. This step primarily identified and excluded obvious signal artifacts (e.g., head motion, cardiac inflow pulsatile motion). We then discarded components not engaged by the fMRI task. To assess task engagement, component time courses were parameterized using multiple regression to provide association coefficients (β-weights) between component time courses and an overall condition model of the response inhibition task (i.e., one condition model for both stop and go blocks). One sample t-tests against zero were carried out on the β weights (pooled across groups) to determine if the evidence for task engagement was greater than zero (i.e., whether or not the network was engaged by the task). Only 14 components were significantly (p < .05) associated with the overall-condition model and were retained. Estimates were then derived for Stop and Go blocks separately to investigate the effects of task set on brain networks. To identify and visualize which brain regions were significantly engaged in each component, individual participants’ spatial maps were entered into an SPM5 voxel-wise one-sample t-test for each component. Component spatial structure was visualized by overlaying these results on axial slices of representative brain anatomy. Significance was evaluated using p < 0.05 family-wise error rate correction for the whole brain [43].
2.9 Clinical Effects of Treatment and Behavioral Analyses
Participants’ YMRS and CDRS-R values were analyzed with 2 × 3 time (pre- vs. post-trial) by group (risperidone, divalproex, HC) Analyses of variance (ANOVA). Participants’ reaction time and accuracy were examined using a series of 2 × 2 × 3 ANOVAs; block (Go vs. Stop) by time (pre- vs. post-trial) by group (risperidone, divalproex, HC). In accordance with signal detection theory, sensitivity (d-prime) and criterion bias (c-bias) measures were computed from participants’ hit (correct Go) and false alarm (incorrect Stop) rates. The d-prime score represents participants’ ability to adequately detect whether or not a signal is present – in this case, it is a proxy for their ability inhibit or reverse an already in progress response in response to the Stop signal. The c-bias score represents participants’ overall tendency to respond, with higher positive values indicating a greater likelihood to respond to any trial. These measures were examined using separate 2 × 2 × 3 ANOVAs: block type (Go vs. Stop) by session (pre- vs. post-trial) by group (risperidone, divalproex, HC).
2.10 Identification of Task-Engaged Networks Affected by Treatment
Given that the focus of this study was to examine differential changes between medication groups in the engagement of brain circuits during the response inhibition task over the course of treatment, with the HC group serving as a control for practice effects and development, our analyses focused on two networks that showed a significant group by time interaction. ANOVA compared the beta weights between groups in SPSS using group (risperidone, divalproex, HC) as the between-subjects factor, and time (Pre vs. Post) as the within-subjects factor. Because the Stop blocks and Go blocks likely engaged different, albeit related cognitive processes, separate ANOVAs were conducted for Stop and Go blocks (Table 2).
Table 2.
Influence of Pharmacotherapy on Response Inhibition
| Region of Interest | Co- ordinates x, y, z in MNI | Effect Size | t- value | p- value |
|---|---|---|---|---|
| Results in the Evaluative Affective Circuit | ||||
| HC > PBD at Baseline (Pre-treatment) | ||||
| Left Insula | −39, −7, 9 | 0.79 | 2.29 | 0.03 |
| Risperidone > HC Changes over treatment (Post- vs. Pre-treatment) | ||||
| L Insula | −39, −7, 9 | 1.34 | 3.22 | 0.003 |
| R Insula | 39, −7, 9 | 0.8 | 1.9 | 0.07 |
| L Subgenual ACC | −5, 17, −15 | 0.43 | 1.03 | 0.31 |
| R Subgenual ACC | 6, 17, −14 | 0.06 | 0.15 | 0.88 |
| L Inferior Frontal Gyrus | −34, 24, −18 | −0.13 | −0.31 | 0.76 |
| R Inferior Frontal Gyrus | 35, 26, −18 | −0.26 | −0.63 | 0.53 |
| R Medial Frontal Gyrus | 8, 45, 17 | −0.57 | −1.37 | 0.18 |
| L Medial Frontal Gyrus | −7, 50, 19 | −0.51 | −1.22 | 0.23 |
| Divalproex > HC Changes over treatment (Post- vs. Pre-treatment) | ||||
| L Insula | −39, −7, 9 | 0.77 | 1.84 | 0.08 |
| R Insula | 39, −7, 9 | 0.63 | 1.5 | 0.15 |
| L Subgenual ACC | −5, 17, −15 | 0.83 | 1.98 | 0.05 |
| R Subgenual ACC | 6, 17, −14 | 0.49 | 1.17 | 0.25 |
| L Inferior Frontal Gyrus | −34 24 −18 | 0.09 | 0.21 | 0.84 |
| R Inferior Frontal Gyrus | 35, 26, −18 | 0.04 | 0.1 | 0.92 |
| R Medial Frontal Gyrus | 8, 45, 17 | 0.2 | 0.47 | 0.64 |
| L Medial Frontal Gyrus | −7, 50, 19 | 0.07 | 0.16 | 0.87 |
| Results in the Reactive Affective Circuit | ||||
| HC > PBD at Baseline (Pre-treatment) | ||||
| Left Amygdala | −23, −4, −19 | 0.36 | 1.05 | 0.04 |
| Risperidone > HC Changes over treatment (Post- vs. Pre-treatment) | ||||
| L Occipital Lobe | −20, −84, 2 | −0.33 | −0.8 | 0.43 |
| L Amygdala | −23, −4, −19 | −0.94 | −2.25 | 0.03 |
| L Parietal Lobe | −30, −53, 43 | 0.08 | 0.19 | 0.85 |
| Divalproex > HC Changes over treatment (Post- vs. Pre-treatment) | ||||
| L Occipital Lobe | −20, −84, 2 | 0.3 | 0.72 | 0.48 |
| R Amygdala | 23, −4, −19 | −0.38 | −2.44 | 0.02 |
| L Parietal Lobe | −30, −53, 43 | 0.38 | 0.9 | 0.38 |
Legend: L=Left; R=Right; ACC: Anterior cingulate cortex; HC = Healthy Controls, PBD = Pediatric Bipolar Disorder
2.11 Whole-Brain ANOVAS and Region-of-Interest (ROI) Analyses of Functional Connectivity
As described above, ICA produced a spatial map for each participant × fMRI sessions (i.e., pre- vs. post-treatment) that depicted the voxelwise strength of functional connectivity. These were examined in a series of SPM5 2 × 2 (pre- vs. post-treatment session by group) ANOVA models that contrasted PBD drug effects of divalproex vs. healthy controls, risperidone vs. healthy controls, and finally risperidone vs. divalproex. The defined ROIs from the EAC and RAC networks used two-tailed α=0.05, corrected for the number of ROIs searched (ROI masks in Supplementary Material).
2.12 Correlations of ROI-Derived Functional Connectivity Values and Clinical Indices
To investigate the effect of changes in brain regions on the clinical indices, correlations were conducted within each drug treatment group between the areas that showed significant changes in the ANOVAs and the changes in YMRS and CDRS-R scores. In all, eight correlations were conducted: for the risperidone group, the YMRS and CDRS-R scores were correlated with the connectivity in the left insula after treatment and the change in connectivity from pre- to post-treatment, and in the divalproex group, the two clinical indices were each correlated with post and change in connectivity in the left BA25, given that those were the areas that changed in each group.
2.13 Correlations of Brain and Clinical Data to Behavioral Indices
To investigate the effect of changes in brain regions on the participants’ behavioral performance, similar correlations were conducted within each drug treatment group between the areas that showed significant changes in the ANOVAs and the changes in sensitivity (d-prime) and response threshold (c-bias) scores. In all, eight additional correlations were conducted: for the risperidone group, the d-prime and c-bias scores were correlated with the connectivity in the left insula after treatment and the change in connectivity from pre- to post-treatment, and in the divalproex group, the two behavioral indices were each correlated with post and change in connectivity in the left BA25, given that those were the areas that changed in each group. Finally, four correlations between the changes in clinical data and the changes in behavioral data were also conducted, but no significant results were found.
3. RESULTS
Sample demographic and clinical data are summarized in Table 1. Comorbid diagnosis included separation anxiety disorder (n=1) and conduct disorder (n=1) in risperidone group, and generalized anxiety disorder (n=1) and a history of substance abuse (n=1) in divalproex group.
3.1 Behavioral Results
Patient groups and HC did not differ in Reaction time (RT) at baseline or in degree of change with time between groups, and all subjects slowed down with time. Accuracy did not differ between groups in the Go Blocks or the Stop Blocks and did not change with time.
Patient groups and HC did not show any significant differences on the 2 × 2 × 3 block type by session by group ANOVA for d-prime scores, except for a significant difference between the groups’ overall d-prime scores, F(2,30) = 3.59, p = .040. Post hoc tests revealed that although the two patient groups did not differ from each other, they both showed significantly less sensitivity overall than the HC. All groups, however, did show increases in sensitivity on the Go Blocks – albeit nonsignificantly – and the HC showed an increase on the Stop Blocks, whereas the patients showed slight decreases. In addition, although there was a significant difference in sensitivity between the HC and the two patient groups in the first session, F(2,30) = 5.07, p = .013, there was no such difference in the second session, F(2,30) = 1.95, p = .160. Thus there is some evidence that the PBD group became slightly better at the task, relative to HC, before and after medication treatment. The criterion bias scores suggest a possible mechanism for these slight increases in sensitivity. All of the participants shifted from a more liberal responding threshold (higher c-bias) in the first session to a more conservative one (lower c-bias) in the second session, F(2,30) = 9.65, p = .004, with no other effects of group or block type. Taken together, the behavioral results indicate that both patients’ and controls were able to strategically adjust their response criteria in the second session to attempt to improve their performance above the first session, but that HC were slightly more successful than patients in actually doing so.
(A table and additional detail that summarizes the behavioral data is available under ‘Supplementary Material’ at http://www.psych.uic.edu/brain-center/response_inhibition.html).
3.2 fMRI Whole Brain Analyses Results
Only two networks survived our selection process that identified non-artifactual, task-associated components with evidence for significant effects of treatment in the PBD group. The first component (henceforth known as the EAC) showed functionally-integrated activity in the bilateral inferior frontal gyrus, middle frontal gyrus, anterior cingulate cortex (ACC), middle temporal gyrus, insulae, and striatum (FDR p<.001, Figure 1). The second component (henceforth known as the RAC) showed functionally-integrated activity in the bilateral occipital lobe, parietal lobe, and amygdala (FDR p<.001, Figure 2). The increase or decrease in activity within the networks signifies their connectivity within the component in all subjects, PBD and HC included, during the task performance.
FIGURE 1. EVALUATIVE AFFECTIVE CIRCUIT DURING RESPONSE INHIBITION.
IFG = INFERIOR FRONTAL GYRUS; SG ACC = SUBGENUAL ANTERIOR CINGULATE CORTEX; MFG = MIDDLE FRONTAL GYRUS; INS = INSULA; PG ACC = PREGENUAL ANTERIOR CINGULATE CORTEX; MTG = MIDDLE TEMPORAL GYRUS; L = LEFT; R = RIGHT (FDR P < 0.001)
FIGURE 2. REACTIVE AFFECTIVE CIRCUIT DURING RESPONSE INHIBITION.
AMG = AMYGDALA; OCC = OCCIPITAL CORTEX; MDFG = MEDIAL FRONTAL GYRUS; PL = PARIETAL LOBE; L = LEFT; R = RIGHT. (FDR P < 0.001)
Next, the change in ROI within the EAC and RAC were examined to determine the change in connectivity among these networks within each patient group in response to risperidone or divalproex, relative to HC. In the EAC, the risperidone group showed greater increase in functional connectivity across treatment, relative to HC, in the left and (t(23)=3.22, p= 0.003) and the right insula (t (23)=1.90, p=0.07) (Table 2, Figure 3a). Also in the EAC, the divalproex group showed greater connectivity across treatment, relative to HC, in the left subgenual ACC (BA25) (t(23)= 0.98, p=0.05), and the left insula (t(23)=1.84, p=0.03)(Table 2, Figure 3b). When compared directly with each other, the risperidone group, relative to the divalproex group, showed a trend toward greater functional connectivity in the left insula ROI (t(20)= 1.91, p=0.07).
FIGURE 3. REGION OF INTEREST WITHIN FUNCTIONAL CIRCUITS: MEDICATION EFFECTS OVER TREATMENT PERIOD.
RISP = RISPERIDONE; DVPX = DIVALPROEX SODIUM; ACC = ANTERIOR CINGULATE CORTEX; L = LEFT; R = RIGHT
In the RAC, risperidone group showed decreased change in functional connectivity in the left amygdala, relative to HC (t(23)=2.47, p=0.01) (Table 2, Figure 3c). Similarly, the divalproex group showed decreased change in functional connectivity, relative to HC, in the right amygdala (t(23)=2.44, p=0.01) (Table 2, Figure 3d). With regards to occipital cortex, relative to HC, the risperidone group showed an increase in the right middle occipital gyrus (t(23)= 2.96, p=0.003) and the divalproex group showed an increase in functional connectivity in the right superior occipital gyrus (t(23)=2.14, p=0.02).
3.3 Correlations of ROI Values and Clinical Indices
For the risperidone group, there was a significant correlation between the change in YMRS scores and the level of functional connectivity of the insula after treatment (r(9)= −.629, p=0.038). For the divalproex group, there was a significant correlation between the change in functional connectivity in the left subgenual ACC between sessions and the decrease in CDRS-R score (r(9)= −.713, p=0.014). No other correlations between clinical indices and activity changes in these ROIs were found.
3.4 Correlations of ROI Values and Behavioral Indices
For the risperidone group, there was a significant correlation between the change in participants’ response threshold and the level of functional connectivity of the insula after treatment (r(9)=.84, p=0.009), as well as a trend toward a correlation between participants’ threshold change and the change in left insula connectivity (r(9)= −.690, p=0.05). For the divalproex group, none of the correlations were significant.
4. DISCUSSION
There are four key findings in this study. First, the ICA methods found evidence for the two hypothesized functional circuits engaged during response inhibition, the “appraising” EAC (bilateral inferior frontal gyrus, middle frontal gyrus, ACC, middle temporal gyrus, insulae, striatum) and the “automatic” RAC (bilateral occipital lobe, parietal lobe, and amygdala). Second, ROI analysis within the EAC and RAC confirmed our hypothesis that medications altered the functional connectivity. Patients, relative to HC and within EAC, showed greater engagement of left insula with risperidone and left subgenual ACC with divalproex. Third, as predicted, reduction in manic symptoms correlated with increased connectivity of insula within EAC with risperidone. The reduction in depressive symptoms correlated with increased left subgenual engagement with divalproex. Fourth, amygdala functional connectivity did not alter with either of the medications. This could be a trait abnormality in patients where prefrontal effects, rather than subcortical activity changes, are seen during treatment, during motor inhibition. An alternate explanation may be that the amygdala activity reduces with treatment, but relative to HC, it remains high.
Both groups engaged in the behavioral strategy of becoming more conservative in their responses, but were only slightly successful in translating this strategy into improved performance to perform the task in the second session than the patients were, but both groups showed a similar shift in strategy. Thus, these results suggest that as patients’ mood symptoms abated with treatment, they were able to employ the same response strategy as HC.
4.1 ICA reveals EAC and RAC engagement in PBD during response inhibition
We were able to map two distinct functional networks, the EAC and the RAC, in PBD and HC. Interestingly, these putative emotional networks were significantly engaged differently in patients, relative to HC. On tasks where performance might be challenging and elicit emotional reactions to success or failures, demanding the need to modulate responses in the context of performing an arduous task, evaluative higher cortical regions have come into play [26]. It is now well established that inferior frontal gyrus engages in affective and response inhibition control, [19] [44] [45] [46] and has strong connectivity to the “cognitive” middle frontal gyrus [47]. These cortical regions of EAC work in concert with opercular regions of insula, ACC, and temporo-striatal regions [48] establishing a liaison between affective and cognitive regions of decision control, error correction, and emotional moderation, as in this study. For example, in previous work, the pregenual cingulate-insular cortex elements of the EAC network described in this study have been linked to cognitive set maintenance [49] and they increase in response to errors during ongoing performance of a similar Go/No-Go response inhibition task [50]. This suggests that impairment of processing due to abnormal integration of insular cortex might disrupt these executive control abilities, with inability to monitor inhibition in the light of manic symptoms. The RAC is a posterior affective circuit that also emerged during response inhibition task performance. The functional connectivity that emerged in RAC is in line with our previous findings in support of direct connectivity between visual association cortex to the amygdale [51] [52] via the occipito-temporal inferior longitudinal fasciculus [23]. Given the high level of frustration associated with having to inhibit responses in this study, amygdala was engaged on the left side [3] [4]. The amygdala is found to play a key role in the interaction of emotion and cognition such as emotion’s influence on attention and perception [53]. Our findings support the notion of emotional impulsivity [13] [16] [14] [54] [55] and this early automatic response is proportional to the attention directed to the stimuli [56] We have yet to establish the sequence of signal pathways [27] to determine whether EAC activity is preceded by that in RAC or vice versa.
4.2 Medication-Specific Effects on Functional Connectivity
While biomarkers of medication outcome and prognosis are an ideal goal, given the preliminary nature and the complexity of our studies, it may be optimal to provide a bio-signature based on a cluster of biological findings that maps any given drug’s operation. Also, findings on fMRI studies of drug mechanism must always be interpreted based on the paradigm chosen to probe a specific domain, the illness status, and the class of drug.
4.2.1 Risperidone increases insular engagement within EAC
Our main finding with risperidone is of critical importance as risperidone is often administered to address aggression and negative reactivity within acute mania [57] [29] [58] [59]. In parallel, insula increased activation while processing negative emotions in healthy humans with increased serotonin neurotransmission [60] as well as in PBD [21] [61]. Furthermore, the insula showed hypometabolism during omission errors on an attentional task in euthymic bipolar adults [62], a finding that aligns with structural studies showing decreased grey matter in left insula in patients and their relatives [63]. Risperidone appears to engage this critical region in the EAC to a greater extent, likely by the virtue of its serotonin-dopamine antagonism, due to greater serotonin HT 1A receptors in the insula [64] modulating emotion and attention during task performance. The increased functional connectivity of insula in the EAC with risperidone treatment and its correlation with change in manic symptoms underscores the mechanism behind the effect of risperidone in mania. However, given that HT 1A receptors are abundantly present in hippocampus and amygdala, these results of insular hyperconnectivity must be interpreted as potentially specific to risperidone and during behavior inhibition. Alternatively, risperidone administered in a larger sample may illustrate a more wide spread and significantly increased engagement of these other regions that are rich in HT 1A receptors.
4.2.2 Divalproex increases subgenual ACC engagement within EAC
Within the EAC, left subgenual ACC showed greater functional connectivity in divalproex patients, relative to HC. This finding is consistent with the underactive subgenual ACC in untreated patients with adult bipolar disorder while performing an attentional task [65]. This key region modulates autonomic responses and neurotransmission in animals [66]. Indeed, stimulation of subgenual ACC ameliorated symptoms in adult depression [67] and perfusion was normalized with treatment in the same region [68] [69]. Subgenual ACC also exhibited decreased grey matter in adult mood disorders where there was reduction in glia [65] [70]. Further, we were able to show that subgenual ACC engagement significantly correlated with reduced depressive symptoms in the current study, although we failed to show such correlation with manic symptoms. Finally, while divalproex engaged subgenual ACC greater than HC, risperidone did not differ from divalproex when we compared the two patient groups. These results are in line with our findings from a previous study of risperidone illustrating increased subgenual ACC activity during a cognitive control task performed under emotional challenge [12]. An alternate explanation for this lack of difference on direct comparison between the two medications may be due to the fact that the brain circuitry engagement may be specific to a mood state than a specific medication. The brain functional signature may be more specific to a manic episode vs. a depressive episode or a euthymic state.
4.2.3 Risperidone and Divalproex fail to dampen amygdala connectivity within RAC
The amygdala showed significantly increased functional connectivity within RAC, at baseline that failed to change with treatment. There is consistent evidence from functional studies in PBD showing increased amygdala activity [4] [33] that remained hyperactive, relative to HC, regardless of treatment for mania [13] and during euthymic illness state [2] [7] [21]. In addition to functional neuroimaging abnormalities in the PFC and amygdala, structural neuroimaging studies indicate smaller amygdala volumes in PBD patients relative to HC, [71] [72] [73] [74] which contrasts with adult studies that report larger [75] [76] or normal [77] [78] amygdala volumes. Larger amygdala in adult studies [75] [76] [79] [80] has in fact been hypothesized to result from hypertrophy due to chronic and excessive activation in manic patients [80]. While findings of altered size do not necessarily imply intrinsic primary abnormalities in the amygdala, they may correlate with functional abnormalities in the amygdala such as increased connectivity in response to the emotional and cognitive challenges posed by the task (e.g. frustration, effortful inhibition of responses), regardless of dysfunction in PFC input to the amygdala. Given the central role that the amygdala plays in arousal and emotional reactivity [81] [82] [83] and its role in the emotion-cognition interface [53], it is meaningful that amygdala did not alter its task-engagement following treatment with either medication in PBD as was seen in controls. The change in amygdala connectivity found in HC might be the result of the increase in automaticity due to task familiarity in the RAC and decreased need to use the EAC.
4.3 Clinical Symptoms Influence Response Inhibition
The novel findings are that both risperidone and divalproex groups showed greater connectivity in two distinct regions in EAC, relative to HC, and that both of these regions correlated significantly and differentially with the reduction in manic and depressive symptoms, respectively. The increased engagement of insula in the EAC after treatment with risperidone illustrates the alterations in neural connectivity underlying the reduction in manic symptoms. The increase in the functional connectivity in subgenual ACC provides insight into the mechanisms of the traditional mood stabilizer divalproex, which additionally addresses depressive symptoms [84] and subsyndromal depressive symptoms [85] that commonly coexist with pediatric mania. Depressive symptoms paired with expending attentional resources during response inhibition task performance would lead to “emotional impulsivity” in PBD, [16] especially because cognitive conflicts require effortful processing and, therefore, can be aversive and evoke negative emotions [86]. If the patients were dealing with mood symptoms, they could have interfered with their ability to implement a more conservative response strategy similar to that found by the HC. Thus, our study is significant in exhibiting the effects of risperidone and divalproex during motor inhibition, with significant reductions in manic and depressive mood symptoms and engagement of the EAC through insula and subgenual ACC, respectively, to moderate patients’ emotional impulsivity.
A major strength of this study is that the ICA method is a data-driven (i.e. model-blind) technique to measure dynamic changes in brain network circuits working in concert, rather than isolated changes in activity. A weakness of this study is the relatively small sample size, although couched in a strong study design. The use of a block design for the task also did not permit us to compare the networks that were engaged for stop vs. go trials or correct vs. incorrect trials, unlike some previous studies [17] [27]. However, given that that the study is based on a model of the neural circuits that takes into account overall performance during the response inhibition task, the fact that the study was a block design is less relevant. Moreover, given that we found comparable levels of performance between patients and HCs, we avoided the potential confound that large differences in task difficulty between groups caused the neural changes we observed. We were able to compare two types of medications in an unmedicated manic patient sample, using monotherapy, with a normative HC sample for comparison. It is compelling to see that previous findings can now be incorporated into more sophisticated circuit-level models that serve as potential bio-signatures of treatment outcome. These results are beginning to inform why clinicians would need to combine two classes of medications because they exhibit complementary mechanisms of action within specific functional neural circuits.
5. CONCLUSION
Behavioral response inhibition in pediatric mania engages two functionally connected circuits, the EAC and the RAC. Risperidone works by engaging insula to a greater degree than HC, and divalproex works by engaging subgenual ACC relative to HC within the EAC. Reduction in manic symptoms for the risperidone group and depressive symptoms in the divalproex group distinctly showed correlations with change in the functional connectivity of EAC. However, amygdala activity did not alter with treatment within RAC with either risperidone or divalproex, suggesting a probable trait of dysfunctional emotional reactivity in PBD, relative to HC. These patterns of activity contribute to the development of biosignatures of treatment response in PBD.
Supplementary Material
HIGHLIGHTS.
Treatment effects with either risperidone or divalproex for PBD were investigated using novel functional connectivity methods
During Response Inhibition task, fronto-striatal and occipito-limbic networks were found to be dysfunctionally engaged in PBD prior to treatment
Both drugs failed to dampen disordered amygdala connectivity in the occipito-limbic network
Footnotes
DISCLOSURE: This research was funded by NIH 1 K23 RR018638-01 and NIH-MO1-RR-13987.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Mani N. Pavuluri, Pediatric Brain Research and Intervention Center, Institute for Juvenile Research, Colbeth Clinic, University of Illinois at Chicago.
James Ellis, Pediatric Brain Research and Intervention Center, Institute for Juvenile Research, Colbeth Clinic, University of Illinois at Chicago.
Ezra Wegbreit, Pediatric Brain Research and Intervention Center, Institute for Juvenile Research, Colbeth Clinic, University of Illinois at Chicago.
Alessandra M. Passarotti, Pediatric Brain Research and Intervention Center, Institute for Juvenile Research, Colbeth Clinic, University of Illinois at Chicago.
Michael C. Stevens, Olin Neuropsychiatry Research Center, The Institute of Living/Hartford Hospital, Yale University School of Medicine.
Reference List
- 1.Chang K, Adleman NE, Dienes K, Simeonova DI, Menon V, Reiss A. Anomalous prefrontal-subcortical activation in familial pediatric bipolar disorder: a functional magnetic resonance imaging investigation. Arch Gen Psychiatry. 2004 Aug;61(8):781–92. doi: 10.1001/archpsyc.61.8.781. [DOI] [PubMed] [Google Scholar]
- 2.Pavuluri MN, Schenkel LS, Aryal S, Harral EM, Hill SK, Herbener ES, et al. Neurocognitive function in unmedicated manic and medicated euthymic pediatric bipolar patients. Am J Psychiatry. 2006 Feb;163(2):286–93. doi: 10.1176/appi.ajp.163.2.286. [DOI] [PubMed] [Google Scholar]
- 3.Pavuluri MN, O’Connor MM, Harral EM, Sweeney JA. Affective neural circuitry during facial emotion processing in pediatric bipolar disorder. Biol Psychiatry. 2007 Jul 15;62(2):158–67. doi: 10.1016/j.biopsych.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 4.Rich BA, Vinton DT, Roberson-Nay R, Hommer RE, Berghorst LH, McClure EB, et al. Limbic hyperactivation during processing of neutral facial expressions in children with bipolar disorder. Proc Natl Acad Sci U S A. 2006 Jun 6;103(23):8900–5. doi: 10.1073/pnas.0603246103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blumberg HP, Martin A, Kaufman J, Leung HC, Skudlarski P, Lacadie C, et al. Frontostriatal abnormalities in adolescents with bipolar disorder: preliminary observations from functional MRI. Am J Psychiatry. 2003 Jul;160(7):1345–7. doi: 10.1176/appi.ajp.160.7.1345. [DOI] [PubMed] [Google Scholar]
- 6.Blumberg HP, Kaufman J, Martin A, Charney DS, Krystal JH, Peterson BS. Significance of adolescent neurodevelopment for the neural circuitry of bipolar disorder. Ann N Y Acad Sci. 2004 Jun;1021:376–83. doi: 10.1196/annals.1308.048. [DOI] [PubMed] [Google Scholar]
- 7.Pavuluri MN, Passarotti AM, Harral EM, Sweeney JA. An fMRI Study of the Neural Correlates of Incidental versus Directed Emotion Processing in Pediatric Bipolar Disorder. J Am Acad Child Adolesc Psychiatry. 2009 doi: 10.1097/CHI.0b013e3181948fc7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rich BA, Fromm SJ, Berghorst LH, Dickstein DP, Brotman MA, Pine DS, et al. Neural connectivity in children with bipolar disorder: impairment in the face emotion processing circuit. J Child Psychol Psychiatry. 2008 Jan;49(1):88–96. doi: 10.1111/j.1469-7610.2007.01819.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dickstein DP, Gorrostieta C, Ombao H, Goldberg LD, Brazel AC, Gable CJ, et al. Fronto-temporal spontaneous resting state functional connectivity in pediatric bipolar disorder. Biol Psychiatry. 2010 Nov 1;68(9):839–46. doi: 10.1016/j.biopsych.2010.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pavuluri MN, Passarotti AM, Parnes SA, Fitzgerald JM, Sweeney JA. A pharmacological functional magnetic resonance imaging study probing the interface of cognitive and emotional brain systems in pediatric bipolar disorder. J Child Adolesc Psychopharmacol. 2010 Oct;20(5):395–406. doi: 10.1089/cap.2009.0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pavuluri MN, Passarotti AM, Mohammed T, Carbray JA, Sweeney JA. Enhanced working and verbal memory after lamotrigine treatment in pediatric bipolar disorder. Bipolar Disord. 2010 Mar;12(2):213–20. doi: 10.1111/j.1399-5618.2010.00792.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pavuluri MN, Passarotti AM, Lu LH, Carbray JA, Sweeney JA. Double-blind randomized trial of risperidone versus divalproex in pediatric bipolar disorder: fMRI outcomes. Psychiatry Res. 2011 Jul 30;193(1):28–37. doi: 10.1016/j.pscychresns.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Passarotti AM, Sweeney JA, Pavuluri MN. Fronto-limbic dysfunction in mania pre-treatment and persistent amygdala over-activity post-treatment in pediatric bipolar disorder. Psychopharmacology (Berl) 2011 Mar 10; doi: 10.1007/s00213-011-2243-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Passarotti AM, Sweeney JA, Pavuluri MN. Differential engagement of cognitive and affective neural systems in pediatric bipolar disorder and attention deficit hyperactivity disorder. J Int Neuropsychol Soc. 2010 Jan;16(1):106–17. doi: 10.1017/S1355617709991019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Passarotti AM, Sweeney JA, Pavuluri MN. Neural Correlates of Incidental and Directed Facial Emotion Processing in Adolescents and Adults. Soc Cogn Affect Neurosci. 2009 doi: 10.1093/scan/nsp029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Passarotti AM, Pavuluri MN. Brain functional domains inform therapeutic interventions in attention-deficit/hyperactivity disorder and pediatric bipolar disorder. Expert Rev Neurother. 2011 Jun;11(6):897–914. doi: 10.1586/ern.11.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leibenluft E, Rich BA, Vinton DT, Nelson EE, Fromm SJ, Berghorst LH, et al. Neural circuitry engaged during unsuccessful motor inhibition in pediatric bipolar disorder. Am J Psychiatry. 2007 Jan;164(1):52–60. doi: 10.1176/ajp.2007.164.1.A52. [DOI] [PubMed] [Google Scholar]
- 18.Singh MK, Chang KD, Mazaika P, Garrett A, Adleman N, Kelley R, et al. Neural correlates of response inhibition in pediatric bipolar disorder. J Child Adolesc Psychopharmacol. 2010 Feb;20(1):15–24. doi: 10.1089/cap.2009.0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pavuluri MN, Passarotti AM, Harral EM, Sweeney JA. Enhanced prefrontal function with pharmacotherapy on a response inhibition task in adolescent bipolar disorder. J Clin Psychiatry. 2010 Nov;71(11):1526–34. doi: 10.4088/JCP.09m05504yel. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pavuluri MN, Sweeney JA. Integrating functional brain neuroimaging and developmental cognitive neuroscience in child psychiatry research. J Am Acad Child Adolesc Psychiatry. 2008 Nov;47(11):1273–88. doi: 10.1097/CHI.0b013e318185d2d1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pavuluri MN, O’connor MM, Harral EM, Sweeney JA. An fMRI study of the interface between affective and cognitive neural circuitry in pediatric bipolar disorder. Psychiatry Res. 2008 Feb;162(3):244–55. doi: 10.1016/j.pscychresns.2007.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Devinsky O, Morrell MJ, Vogt BA. Contributions of anterior cingulate cortex to behaviour. Brain. 1995 Feb;118(Pt 1):279–306. doi: 10.1093/brain/118.1.279. [DOI] [PubMed] [Google Scholar]
- 23.Catani M, Jones DK, Donato R, Ffytche DH. Occipito-temporal connections in the human brain. Brain. 2003 Sep;126(Pt 9):2093–107. doi: 10.1093/brain/awg203. [DOI] [PubMed] [Google Scholar]
- 24.Morris JS, Ohman A, Dolan RJ. Conscious and unconscious emotional learning in the human amygdala. Nature. 1998 Jun 4;393(6684):467–70. doi: 10.1038/30976. [DOI] [PubMed] [Google Scholar]
- 25.Friston K. Beyond phrenology: what can neuroimaging tell us about distributed circuitry? Annu Rev Neurosci. 2002;25:221–50. doi: 10.1146/annurev.neuro.25.112701.142846. Epub;%2002 Mar;%19.:221–50. [DOI] [PubMed] [Google Scholar]
- 26.Passarotti AM, Sweeney JA, Pavuluri MN. Neural correlates of response inhibition in pediatric bipolar disorder and attention deficit hyperactivity disorder. Psychiatry Res. 2010 Jan 30;181(1):36–43. doi: 10.1016/j.pscychresns.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stevens MC, Kiehl KA, Pearlson GD, Calhoun VD. Functional neural networks underlying response inhibition in adolescents and adults. Behav Brain Res. 2007 Jul;%19;181(1):12–22. doi: 10.1016/j.bbr.2007.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Konarski JZ, Kennedy SH, Segal ZV, Lau MA, Bieling PJ, McIntyre RS, et al. Predictors of nonresponse to cognitive behavioural therapy or venlafaxine using glucose metabolism in major depressive disorder. J Psychiatry Neurosci. 2009 May;34(3):175–80. [PMC free article] [PubMed] [Google Scholar]
- 29.Pandina G, DelBello M, Kushner S, Van Hove I, Augustyns I, Kusumakar V, et al. Risperidone for the treatment of acute mania in bipolar youth [poster]. 2007 Oct 23; Boston, MA. Presented at the 54th annual meeting of the American Academy of of Child and Adolescent Psychiatry (AACAP); 2007. [Google Scholar]
- 30.Monti B, Polazzi E, Contestabile A. Biochemical, molecular and epigenetic mechanisms of valproic acid neuroprotection. Curr Mol Pharmacol. 2009 Jan;2(1):95–109. doi: 10.2174/1874467210902010095. [DOI] [PubMed] [Google Scholar]
- 31.Kowatch RA, Findling R, Scheffer R, Stanford KE. Placebo controlled trial of divalproex versus lithium for bipolar disorder. 2007 Oct 23; Boston, MA. Presented at the Annual Meeting of the American Academy of Child and Adolescent Psychiatry; 2007. [Google Scholar]
- 32.Wagner KD, Redden L, Kowatch RA, Wilens TE, Segal S, Chang K, et al. A double-blind, randomized, placebo-controlled trial of divalproex extended-release in the treatment of bipolar disorder in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2009 May;48(5):519–32. doi: 10.1097/CHI.0b013e31819c55ec. [DOI] [PubMed] [Google Scholar]
- 33.Chang KD, Wagner C, Garrett A, Howe M, Reiss A. A preliminary functional magnetic resonance imaging study of prefrontal-amygdalar activation changes in adolescents with bipolar depression treated with lamotrigine. Bipolar Disord. 2008 May;10(3):426–31. doi: 10.1111/j.1399-5618.2007.00576.x. [DOI] [PubMed] [Google Scholar]
- 34.Kaufman J, Birmaher B, Brent DA, Ryan ND, Rao U. K-SADS-PL. J Am Acad Child Adolesc Psychiatry. 2000 Oct;39(10):1208. doi: 10.1097/00004583-200010000-00002. [DOI] [PubMed] [Google Scholar]
- 35.Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978 Nov;133:429–35. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- 36.Poznanski EO, Mokros HB. Children’s Depression Rating Scale, Revised (CDRS-R) Los Angeles, CA: Western Psychological Services; 1995. [Google Scholar]
- 37.Eddy WF, Fitzgerald M, Genovese CR, Mockus A, Noll DC. Functional image analysis software - computational olio. In: Prat A, editor. Proceedings in Computational Statistics. Heidelberg: Physica-Verlag; 1996. pp. 39–49. [Google Scholar]
- 38.Calhoun VD, Adali T, Pearlson GD, Pekar JJ. A method for making group inferences from functional MRI data using independent component analysis. Hum Brain Mapp. 2001 Nov;14(3):140–51. doi: 10.1002/hbm.1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Calhoun VD, Kiehl KA, Pearlson GD. Modulation of temporally coherent brain networks estimated using ICA at rest and during cognitive tasks. Hum Brain Mapp. 2008 Jul;29(7):828–38. doi: 10.1002/hbm.20581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bell AJ, Sejnowski TJ. An information-maximization approach to blind separation and blind deconvolution. Neural Comput. 1995 Nov;7(6):1129–59. doi: 10.1162/neco.1995.7.6.1129. [DOI] [PubMed] [Google Scholar]
- 41.Li YO, Adali T, Calhoun VD. Estimating the number of independent components for functional magnetic resonance imaging data. Hum Brain Mapp. 2007 Nov;28(11):1251–66. doi: 10.1002/hbm.20359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Erhardt EB, Rachakonda S, Bedrick EJ, Allen EA, Adali T, Calhoun VD. Comparison of multi-subject ICA methods for analysis of fMRI data. Hum Brain Mapp. 2010 Dec 15; doi: 10.1002/hbm.21170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Worsley KJ, Marrett S, Neelin P, Vandal AC, Friston KJ, Evans AC. A unified statistical approach for determining significant signals in images of cerebral activation. Hum Brain Mapp. 1996;4(1):58–73. doi: 10.1002/(SICI)1097-0193(1996)4:1<58::AID-HBM4>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 44.Leibenluft E, Rich BA. Pediatric bipolar disorder. Annu Rev Clin Psychol. 2008;4:163–87. doi: 10.1146/annurev.clinpsy.4.022007.141216. [DOI] [PubMed] [Google Scholar]
- 45.Rubia K, Russell T, Overmeyer S, Brammer MJ, Bullmore ET, Sharma T, et al. Mapping motor inhibition: conjunctive brain activations across different versions of go/no-go and stop tasks. Neuroimage. 2001 Feb;13(2):250–61. doi: 10.1006/nimg.2000.0685. [DOI] [PubMed] [Google Scholar]
- 46.Durston S, Thomas KM, Worden MS, Yang Y, Casey BJ. The effect of preceding context on inhibition: an event-related fMRI study. Neuroimage. 2002 Jun;16(2):449–53. doi: 10.1006/nimg.2002.1074. [DOI] [PubMed] [Google Scholar]
- 47.Petrides M, Pandya DN. Comparative cytoarchitectonic analysis of the human and the macaque ventrolateral prefrontal cortex and corticocortical connection patterns in the monkey. Eur J Neurosci. 2002 Jul;16(2):291–310. doi: 10.1046/j.1460-9568.2001.02090.x. [DOI] [PubMed] [Google Scholar]
- 48.Fair DA, Cohen AL, Power JD, Dosenbach NU, Church JA, Miezin FM, et al. Functional brain networks develop from a “local to distributed” organization. PLoS Comput Biol. 2009 May;5(5):e1000381. doi: 10.1371/journal.pcbi.1000381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dosenbach NU, Fair DA, Cohen AL, Schlaggar BL, Petersen SE. A dual-networks architecture of top-down control. Trends Cogn Sci. 2008 Mar;12(3):99–105. doi: 10.1016/j.tics.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stevens MC, Kiehl KA, Pearlson GD, Calhoun VD. Brain network dynamics during error commission. Hum Brain Mapp. 2009 Jan;30(1):24–37. doi: 10.1002/hbm.20478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Amaral DG, Price JL, Pitkanen A, Carmichael ST. Anatomical organization of the primate amygdaloid complex. In: Aggleton J, editor. The Amygdala: Neurobiological Aspects of Emotion, Memory, and Mental Dysfunction. New York: Wiley-Liss; 1992. pp. 1–66. [Google Scholar]
- 52.Armony JL, Servan-Schreiber D, Cohen JD, LeDoux JE. An anatomically constrained neural network model of fear conditioning. Behav Neurosci. 1995 Apr;109(2):246–57. doi: 10.1037//0735-7044.109.2.246. [DOI] [PubMed] [Google Scholar]
- 53.Phelps EA. Emotion and cognition: insights from studies of the human amygdala. Ann Rev Psychol. 2006;57:27–53. doi: 10.1146/annurev.psych.56.091103.070234. [DOI] [PubMed] [Google Scholar]
- 54.Whalen PJ, Bush G, McNally RJ, Wilhelm S, Mcinerney SC, Jenike MA, et al. The emotional counting stroop paradigm: a functional magnetic resonance imaging probe of the anterior cingulate affective division. Biol Psychiatry. 1998;44:1219–28. doi: 10.1016/s0006-3223(98)00251-0. [DOI] [PubMed] [Google Scholar]
- 55.Pessoa L, McKenna M, Gutierrez E, Ungerleider LG. Neural processing of emotional faces requires attention. Proc Natl Acad Sci U S A. 2002 Aug 20;99(17):11458–63. doi: 10.1073/pnas.172403899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Davis M, Whalen PJ. The amygdala: vigilance and emotion. Mol Psychiatry. 2001 Jan;6(1):13–34. doi: 10.1038/sj.mp.4000812. [DOI] [PubMed] [Google Scholar]
- 57.Biederman J, Mick E, Hammerness P, Harpold T, Aleardi M, Dougherty M, et al. Open-label, 8-week trial of olanzapine and risperidone for the treatment of bipolar disorder in preschool-age children. Biol Psychiatry. 2005 Oct 1;58(7):589–94. doi: 10.1016/j.biopsych.2005.03.019. [DOI] [PubMed] [Google Scholar]
- 58.Pavuluri MN, Henry DB, Devineni B, Carbray JA, Naylor MW, Janicak PG. A pharmacotherapy algorithm for stabilization and maintenance of pediatric bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2004 Jul;43(7):859–67. doi: 10.1097/01.chi.0000128790.87945.2f. [DOI] [PubMed] [Google Scholar]
- 59.Pavuluri MN, Henry DB, Findling RL, Parnes S, Carbray JA, Mohammed T, et al. Double-blind randomized trial of risperidone versus divalproex in pediatric bipolar disorder. Bipolar Disord. 2010 Sep;12(6):593–605. doi: 10.1111/j.1399-5618.2010.00850.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Takano H, Ito H, Takahashi H, Arakawa R, Okumura M, Kodaka F, et al. Serotonergic neurotransmission in the living human brain: A positron emission tomography study using [(11)C]dasb and [(11)C]WAY100635 in young healthy men. Synapse. 2010 Nov 23; doi: 10.1002/syn.20883. [DOI] [PubMed] [Google Scholar]
- 61.Lamotrigine effects of neurocognition in Pediatric Bipolar Disorder [Poster] Florida: Am College of Psychopharmacol; 2006. [Google Scholar]
- 62.Brooks JO, III, Hoblyn JC, Ketter TA. Metabolic evidence of corticolimbic dysregulation in bipolar mania. Psychiatry Res. 2010 Feb 28;181(2):136–40. doi: 10.1016/j.pscychresns.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 63.Matsuo K, Kopecek M, Nicoletti MA, Hatch JP, Watanabe Y, Nery FG, et al. New structural brain imaging endophenotype in bipolar disorder. Mol Psychiatry. 2011 Feb 15; doi: 10.1038/mp.2011.3. [DOI] [PubMed] [Google Scholar]
- 64.Kodaka F, Ito H, Takano H, Takahashi H, Arakawa R, Miyoshi M, et al. Effect of risperidone on high-affinity state of dopamine D2 receptors: a PET study with agonist ligand [11C](R)-2-CH3O-N-n-propylnorapomorphine. Int J Neuropsychopharmacol. 2010 Sep;22:1–7. doi: 10.1017/S1461145710001148. [DOI] [PubMed] [Google Scholar]
- 65.Strakowski SM, Adler CM, Holland SK, Mills N, DelBello MP. A preliminary FMRI study of sustained attention in euthymic, unmedicated bipolar disorder. Neuropsychopharmacology. 2004 Sep;29(9):1734–40. doi: 10.1038/sj.npp.1300492. [DOI] [PubMed] [Google Scholar]
- 66.Drevets WC, Savitz J, Trimble M. The subgenual anterior cingulate cortex in mood disorders. CNS Spectr. 2008 Aug;13(8):663–81. doi: 10.1017/s1092852900013754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mayberg HS, Lozano AM, Voon V, McNeely HE, Seminowicz D, Hamani C, et al. Deep brain stimulation for treatment-resistant depression. Neuron. 2005 Mar 3;45(5):651–60. doi: 10.1016/j.neuron.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 68.Drevets WC, Bogers W, Raichle ME. Functional anatomical correlates of antidepressant drug treatment assessed using PET measures of regional glucose metabolism. Eur Neuropsychopharmacol. 2002 Dec;12(6):527–44. doi: 10.1016/s0924-977x(02)00102-5. [DOI] [PubMed] [Google Scholar]
- 69.Mayberg HS, Brannan SK, Tekell JL, Silva JA, Mahurin RK, McGinnis S, et al. Regional metabolic effects of fluoxetine in major depression: serial changes and relationship to clinical response. Biol Psychiatry. 2000 Oct 15;48(8):830–43. doi: 10.1016/s0006-3223(00)01036-2. [DOI] [PubMed] [Google Scholar]
- 70.Mayberg HS, Liotti M, Brannan SK, McGinnis S, Mahurin RK, Jerabek PA, et al. Reciprocal limbic-cortical function and negative mood: converging PET findings in depression and normal sadness. Am J Psychiatry. 1999 May;156(5):675–82. doi: 10.1176/ajp.156.5.675. [DOI] [PubMed] [Google Scholar]
- 71.Dickstein DP, Milham MP, Nugent AC, Drevets WC, Charney DS, Pine DS, et al. Frontotemporal alterations in pediatric bipolar disorder: results of a voxel-based morphometry study. Arch Gen Psychiatry. 2005 Jul;62(7):734–41. doi: 10.1001/archpsyc.62.7.734. [DOI] [PubMed] [Google Scholar]
- 72.Chang K, Karchemskiy A, Barnea-Goraly N, Garrett A, Simeonova DI, Reiss A. Reduced amygdalar gray matter volume in familial pediatric bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2005 Jun;44(6):565–73. doi: 10.1097/01.chi.0000159948.75136.0d. [DOI] [PubMed] [Google Scholar]
- 73.DelBello MP, Zimmerman ME, Mills NP, Getz GE, Strakowski SM. Magnetic resonance imaging analysis of amygdala and other subcortical brain regions in adolescents with bipolar disorder. Bipolar Disord. 2004 Feb;6(1):43–52. doi: 10.1046/j.1399-5618.2003.00087.x. [DOI] [PubMed] [Google Scholar]
- 74.Frazier JA, Ahn MS, DeJong S, Bent EK, Breeze JL, Giuliano AJ. Magnetic resonance imaging studies in early-onset bipolar disorder: a critical review. Harv Rev Psychiatry. 2005 May;13(3):125–40. doi: 10.1080/10673220591003597. [DOI] [PubMed] [Google Scholar]
- 75.Altshuler L, Bartzokis G, Grieder T, Curran J, Mintz J. Amygdala enlargement in bipolar disorder and hippocampal reduction in schizophrenia: an MRI study demonstrating neuroanatomic specificity. Arch Gen Psychiatry. 1998;55:663–4. doi: 10.1001/archpsyc.55.7.663. [DOI] [PubMed] [Google Scholar]
- 76.Strakowski SM, DelBello MP, Sax KW, Zimmerman ME, Shear PK, Hawkins JM, et al. Brain magnetic resonance imaging of structural abnormalities in bipolar disorder. Arch Gen Psychiatry. 1999 Mar;56(3):254–60. doi: 10.1001/archpsyc.56.3.254. [DOI] [PubMed] [Google Scholar]
- 77.Swayze VW, Andreasen NC, Alliger RJ, Yuh WT, Ehrhardt JC. Subcortical and temporal structures in affective disorder and schizophrenia: a magnetic resonance imaging study. Biol Psychiatry. 1992 Feb 1;31(3):221–40. doi: 10.1016/0006-3223(92)90046-3. [DOI] [PubMed] [Google Scholar]
- 78.Strakowski SM, Adler CM, DelBello MP. Volumetric MRI studies of mood disorders: do they distinguish unipolar and bipolar disorder? Bipolar Disord. 2002 Apr;4(2):80–8. doi: 10.1034/j.1399-5618.2002.01160.x. [DOI] [PubMed] [Google Scholar]
- 79.Brambilla P, Harenski K, Nicoletti M, Sassi RB, Mallinger AG, Frank E, et al. MRI investigation of temporal lobe structures in bipolar patients. J Psychiatr Res. 2003 Jul;37(4):287–95. doi: 10.1016/s0022-3956(03)00024-4. [DOI] [PubMed] [Google Scholar]
- 80.Altshuler LL, Bartzokis G, Grieder T, Curran J, Jimenez T, Leight K, et al. An MRI study of temporal lobe structures in men with bipolar disorder or schizophrenia. Biol Psychiatry. 2000 Jul 15;48(2):147–62. doi: 10.1016/s0006-3223(00)00836-2. [DOI] [PubMed] [Google Scholar]
- 81.Gorno-Tempini ML, Pradelli S, Serafini M, Pagnoni G, Baraldi P, Porro C, et al. Explicit and incidental facial expression processing: an fMRI study. Neuroimage. 2001 Aug;14(2):465–73. doi: 10.1006/nimg.2001.0811. [DOI] [PubMed] [Google Scholar]
- 82.Critchley H, Daly E, Phillips M, Brammer M, Bullmore E, Williams S, et al. Explicit and implicit neural mechanisms for processing of social information from facial expressions: a functional magnetic resonance imaging study. Hum Brain Mapp. 2000 Feb;9(2):93–105. doi: 10.1002/(SICI)1097-0193(200002)9:2<93::AID-HBM4>3.0.CO;2-Z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Keightley ML, Winocur G, Graham SJ, Mayberg HS, Hevenor SJ, Grady CL. An fMRI study investigating cognitive modulation of brain regions associated with emotional processing of visual stimuli. Neuropsychologia. 2003;41(5):585–96. doi: 10.1016/s0028-3932(02)00199-9. [DOI] [PubMed] [Google Scholar]
- 84.Geller B, Fox LW, Clark KA. Rate and predictors of prepubertal bipolarity during follow-up of 6- to 12-year-old depressed children. J Am Acad Child Adolesc Psychiatry. 1994 May;33(4):461–8. doi: 10.1097/00004583-199405000-00003. [DOI] [PubMed] [Google Scholar]
- 85.Findling RL, Youngstrom EA, McNamara NK, Stansbrey RJ, Demeter CA, Bedoya D, et al. Early symptoms of mania and the role of parental risk. Bipolar Disord. 2005 Dec;7(6):623–34. doi: 10.1111/j.1399-5618.2005.00260.x. [DOI] [PubMed] [Google Scholar]
- 86.Botvinick MM. Conflict monitoring and decision making: reconciling two perspectives on anterior cingulate function. Cogn Affect Behav Neurosci. 2007 Dec;7(4):356–66. doi: 10.3758/cabn.7.4.356. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.