Abstract
Summary: Chronic hepatitis B virus (HBV) infection is a complex clinical entity frequently associated with cirrhosis and hepatocellular carcinoma (HCC). The persistence of HBV genomes in the absence of detectable surface antigenemia is termed occult HBV infection. Mutations in the surface gene rendering HBsAg undetectable by commercial assays and inhibition of HBV by suppression of viral replication and viral proteins represent two fundamentally different mechanisms that lead to occult HBV infections. The molecular mechanisms underlying occult HBV infections, including recently identified mechanisms associated with the suppression of HBV replication and inhibition of HBV proteins, are reviewed in detail. The availability of highly sensitive molecular methods has led to increased detection of occult HBV infections in various clinical settings. The clinical relevance of occult HBV infection and the utility of appropriate diagnostic methods to detect occult HBV infection are discussed. The need for specific guidelines on the diagnosis and management of occult HBV infection is being increasingly recognized; the aspects of mechanistic studies that warrant further investigation are discussed in the final section.
INTRODUCTION
Chronic hepatitis B virus (HBV) infection is a major global problem despite the availability of an efficacious vaccine. In chronic HBV infection, liver cirrhosis and hepatocellular carcinoma (HCC) are associated with considerable morbidity and mortality. The detection of hepatitis B virus surface antigen (HBsAg) in serum remains the mainstay in the diagnosis of chronic HBV infection and screening for HBV in most developing countries. The majority of individuals positive for HBsAg are also positive for HBV DNA in the serum. Occult HBV infection is characterized by the presence of HBV DNA in the absence of detectable HBsAg. Occult HBV infection is a complex clinical entity documented worldwide. Significant advances in understanding the pathogenesis of occult HBV infection have been reported in the last decade. This review is aimed at providing a detailed account of the molecular mechanisms leading to occult HBV infection.
HBV VIROLOGY
HBV contains a 3.2-kb partially double-stranded DNA genome with 4 open reading frames encoding 7 proteins. The presence of partially overlapping open reading frames (151) and the absence of noncoding regions (134) allow for compact organization of the HBV genome. The biological functions of HBV proteins and their role in the pathogenesis of HBV infection are summarized in Table 1.
Table 1.
HBV ORFs and proteins
| ORF | Protein | Function/role in pathogenesis of HBV infection |
|---|---|---|
| P | Viral polymerase | DNA polymerase, reverse transcriptase, and RNase H activity; contains functional domains essential for encapsidation of the pregenomic RNA |
| S | HBV surface proteins | Pre-S1 protein plays a key role in attachment of the virus to the hepatocyte (200) |
| C | Core protein | Forms the capsid and encapsidates HBV nucleic acids |
| HBeAg | Biological role is poorly understood; however, strong epidemiological associations between HBeAg and HBV DNA level (53) and the risk of progression to hepatocellular carcinoma (290) are well documented | |
| X | HBx protein | Transactivator of viral regulatory elements and host gene promoters (60, 248), essential for establishment of infection in vivo (300), potential role in hepatocarcinogenesis (60) |
Replication begins with the attachment of mature virions to the host cell membrane to enter the cell. The pre-S proteins mediate the entry of HBV into hepatocytes (200). The HBV receptor on hepatocytes still remains elusive. Once inside the cell, the viral genome is uncoated to release relaxed circular DNA (RC-DNA). This RC-DNA is transported to the nucleus (126) and converted into covalently closed circular DNA (cccDNA) by cellular enzymes (14). The mechanism for the transport of RC-DNA is not clearly understood. The cccDNA is a stable form of the viral genome that is associated with proteins in the nucleus in the form of viral minichromosomes (201), and it also serves as a template for the production of progeny genomes. Genomic transcripts, including pregenomic RNA (pgRNA), precore RNA, and subgenomic HBV RNAs, are transcribed from HBV cccDNA by the host cell enzyme RNA polymerase II. The pgRNA serves as a template for the synthesis of HBV DNA and also as the mRNA of core protein and polymerase. The pgRNA and the HBV polymerase are first packaged into the HBV core protein. Subsequently, pgRNA is reverse transcribed to HBV DNA by the viral polymerase. Subgenomic transcripts serve as mRNAs for surface proteins (i.e., large HBsAg, middle HBsAg, and small HBsAg) and the hepatitis B virus x (HBx) protein. Nucleocapsids are packed into envelope glycoproteins in the cytoplasm and pass through the endoplasmic reticulum and the Golgi apparatus prior to secretion (167). Alternatively, the nucleocapsids can reenter the nucleus, resulting in the amplification of the nuclear cccDNA pool. HBV replication is regulated by 4 promoters, 2 enhancers, and a negative regulatory element (189). Recent studies have demonstrated the role of epigenetic regulation of HBV replication by acetylation of H3/H4 histones (215) and the methylation of HBV DNA (271, 272).
HBV INFECTION AND CLINICAL DISEASE
The incubation period for acute hepatitis B ranges from 1 to 6 months. Acute HBV infection can be either asymptomatic or symptomatic. Asymptomatic acute HBV infection associated with mild or subclinical disease often goes undiagnosed. Clinically inapparent or asymptomatic acute HBV infections are more common in children less than 4 years of age than in adults over 30 years of age (182). Clinically apparent cases have a prodromal phase with nausea, vomiting, malaise, anorexia, fever, and flu-like symptoms. The prodromal phase may be followed by an icteric phase with jaundice, clay-colored or pale stools, discomfort in the right upper quadrant, and hepatomegaly (172). Symptoms in acute HBV infection are clinically indistinguishable from those in other acute viral hepatitis infections. Several HBV markers, including HBV DNA, HBsAg, hepatitis B virus e antigen (HBeAg), and anti-hepatitis B virus core IgM (anti-HBc IgM), are detectable in the serum during acute HBV infection. Biochemical abnormalities such as increased transaminase levels and increased bilirubin levels may also be detected. Seroconversion to antibody to HBsAg (anti-HBs) indicates resolution from acute HBV infection. Fulminant hepatitis B virus infection is associated with high mortality (20, 156). Mutations in the precore region of the HBV genome have been associated with small outbreaks of fulminant hepatitis B (156).
Extrahepatic manifestations occur in up to 20% of HBV-infected individuals (30) and may involve the gastrointestinal, renal, and nervous systems (68). The mechanisms leading to extrahepatic manifestations of hepatitis B virus infection are poorly understood. Circulating immune complexes containing HBV have been demonstrated in patients with extrahepatic manifestations of chronic HBV infection (102, 213). Circulating immune complexes and complement-mediated injury are implicated in extrahepatic manifestations of HBV infection, including arthralgia, serum sickness-like syndrome, polyarteritis nodosa, and glomerulonephritis (2, 30, 163, 263).
Chronic HBV infection is defined as the persistence of HBsAg for 6 months or longer. Chronic HBV infections are more common following anicteric disease (283). The risk of developing chronic HBV infection decreases with age at infection; about 80 to 90% of neonates, 30% of children less than 6 years of age, and fewer than 5% of adults infected progress to chronicity. In addition to age at infection (182), host genetic factors such as polymorphisms in the interleukin-18 gene (47), tumor necrosis factor alpha promoter polymorphisms (136), and human leukocyte antigen-DP gene variants (100) have been linked to persistence of HBV. It is well accepted that CD8+ T cells play a crucial role in the clearance of acute HBV infection (173, 257).
Chronic HBV infection may be classified into 3 phases, consisting of the immune tolerant phase, the immune active phase, and the inactive carrier phase (180). The immune tolerant phase is associated with the presence of HBsAg, HBeAg, and high levels of HBV DNA in the serum. Alanine transaminase (ALT) levels are normal, and no major pathological changes are observed in liver biopsy specimens. The immune tolerant phase may last for several years and is characterized by mild disease. The progression of chronic liver disease is very slow in the immune tolerant phase despite high HBV DNA levels (122); this phase is also referred to as the “highly replicative phase.” The immune active phase is associated with elevated ALT levels, detectable HBV DNA, and inflammation of the liver with or without fibrosis. The “tolerance” to HBV is lost, and damage to the hepatocytes is mediated by the host immune responses to HBV; for this reason, the immune active phase is also referred to as the “immune clearance” phase. The immune active phase is seen in patients with or without HBeAg. The HBV DNA levels are generally higher in HBeAg-positive patients than in HBeAg-negative patients in the immune active phase. Patients with an HBeAg-negative status in the immune active phase are also classified as having “HBeAg-negative chronic hepatitis B.” The loss of HBeAg may be associated with mutations in the precore region or the core promoter regions (97, 161). About 70% of chronic HBV patients seroconvert from HBeAg to antibody to HBeAg (anti-HBe) within 10 years of diagnosis. However, reversion to HBeAg-positive status occurs in a small proportion of HBeAg-negative individuals (181). The inactive carrier phase is characterized by an HBeAg negative- and anti-HBe positive status with low HBV DNA levels (typically <2,000 IU/ml) and minimal or no fibrosis. The rates of spontaneous seroclearance of HBsAg among inactive carriers range from 0.5% per year to as high as 40% in 25 years of follow-up (55, 181). Symptoms in chronic HBV infection may range from mild nonspecific symptoms such as fatigue and right upper quadrant discomfort in patients with minimal liver damage to ascites, peripheral edema, and encephalopathy in patients with advanced liver disease.
Progression to cirrhosis is associated with multiple episodes of severe acute exacerbations, hepatic decompensation, and reversion to HBeAg-positive status from an anti-HBe positive status (158). The 5-year survival rate in chronic HBV patients with cirrhosis is less than 60% (282).
Hepatocellular carcinoma is a major global problem. In areas with a high prevalence of HBV infection such as Southeast Asia, higher rates of HCC are documented (209). The risk of developing HCC may be increased up to 100-fold in patients with chronic HBV infection (12). The roles of host, viral, and extraneous factors associated with progression to HBV-related HCC are summarized in Table 2. Hepatocellular carcinoma is a leading cause of cancer-related deaths. The morbidity and mortality associated with HBV-related HCC necessitate improved surveillance measures for early diagnosis and newer therapeutic options.
Table 2.
Factors associated with increased risk of developing HBV-related HCC
| Factor | Reference(s) |
|---|---|
| Demographics | |
| Male sex | 42, 82 |
| Age (increased risk with advancing age) | 42, 82 |
| Race | 5 |
| Social and environmental | |
| Alcohol | 42, 82 |
| Smoking | 42 |
| Aflatoxin | 285 |
| HBV factors | |
| HBV DNA levels | 41, 42 |
| Presence of HBeAg | 42 |
| Genotype (C more than B) | 289 |
| Core promoter mutations | 289, 292 |
| Liver damage | |
| Cirrhosis | 42, 82 |
| Increased transaminase levels | 42 |
| Miscellaneous | |
| Coinfection with HCV | 82, 142 |
| Superinfection with HDV | 82 |
Direct and indirect mechanisms of hepatocarcinogenesis have been identified in HBV-related HCC. The inflammation associated with chronic active hepatitis is a major contributor in hepatocarcinogenesis (13). Integration of HBV DNA fragments into chromosomal DNA is detected in the majority of HBV-related HCCs (192). The precise time of HBV DNA integration remains unclear, though it may occur as early as the acute phase of HBV infection (193, 137). Integration of subgenomic fragments of HBV DNA into host chromosomal DNA was initially thought to be a random process (176). Subsequent studies have identified recurrent HBV DNA integration sites on human chromosomes, including the human telomerase reverse transcriptase (RT) gene (212). The other HBV DNA integration sites identified include cancer-related genes, tumor suppressor genes, and genes involved in key signaling pathways (192). Integration of HBV DNA could potentially modulate expression profiles of genes involved in carcinogenesis, including tumor suppressor genes and oncogenes. Furthermore, HBV DNA integration could be associated with chromosomal aberrations such as translocations, inversions, and deletions leading to chromosomal instability (176).
Interestingly, the expression of HBx protein (a protein that is not an integral part of HBV) is preferentially retained in HBV-related HCC tissue compared to the expression of HBsAg and hepatitis B virus core antigen (HBcAg) (251). The role of HBx protein in HBV-related HCC has been extensively studied and is summarized in Table 3.
Table 3.
Role of HBx protein in hepatocarcinogenesisa
| Mechanism | Comment | Reference(s) |
|---|---|---|
| Inhibition of p53 | Inhibition of sequence-specific binding of p53 | 279 |
| Centrosome abnormalities | Induction of multipolar spindle formation | 84 |
| Telomerase activity | Increases telomerase activity and expression of hTERT | 164 |
| Inhibition of apoptosis | Activates p38/MAPK pathway and upregulates survivin, an antiapoptotic protein | 143 |
| Jak1/STAT signaling | Activates Jak1/STAT pathway | 152 |
| TGF-β | Shifts TGF-β signaling from tumor suppression to oncogenesis | 194 |
| Defective DNA repair | Defective nucleotide excision repair | 217 |
| Hypermethylation of TSGs | Induction of DNA methyltransferases and suppression of TSGs | 150, 211 |
Abbreviations: hTERT, human telomerase reverse transcriptase; TGF-β, transforming growth factor β; MAPK, mitogen-activation protein kinase; TSG, tumor suppressor gene.
It is generally accepted that HBV is not directly cytopathic and that liver injury is immune mediated. However, direct cytopathic effects of HBV have been demonstrated in individuals with an impaired immune system (184). Increased production of the large surface protein is associated with severe hepatic injury, triggering a cascade of events, including dysregulation of cellular genes and secondary genetic events leading to hepatocarcinogenesis in transgenic mice (50, 72). Defective HBV particles are associated with singly spliced HBV RNA that encodes the hepatitis B virus splice-generated protein (HBSP), a novel protein associated with a frameshift during splicing in HBV (256, 245). An increased relative abundance of defective HBV particles is associated with inflammation and fibrosis of the liver (246). HBSP modulates apoptosis and secretion of inflammatory cytokines (247), suggesting a potential role for the protein in hepatocarcinogenesis.
HBV EPIDEMIOLOGY
It is estimated that over 2 billion people have been exposed to HBV infection, of which about 350 million people remain chronically infected (http://www.who.int/mediacenter/factsheets/fs204/en/). The prevalence of chronic HBV infection varies greatly worldwide. Regions of the world may be classified into areas of high (≥8%), intermediate (>2% and <8%), or low (≤2%) prevalence (http://www.who.int/mediacenter/factsheets/fs204/en/, 149). The majority of HBV infections in areas of high and intermediate endemicity are acquired through vertical transmission or horizontal transmission during the preschool years (149, 151). In contrast, infection in areas of low endemicity is acquired by adolescents or adults predominantly through parenteral or sexual routes (104). Percutaneous transmission among intravenous-drug abusers (IVDA) sharing contaminated needles remains the predominant mode of transmission in developed countries (151, 162). Transmission of HBV through sexual modes is well established; sexual transmission is particularly efficient among homosexual men (146) and in individuals with multiple partners (87). While intrauterine infections are infrequent (286), vertical transmission is primarily perinatal. Horizontal transmission through close nonsexual contact among family members (160) and from one child to another in the community is well documented (63). Inadequate infection control measures are associated with nosocomial transmission (3); higher rates of HBV infection have been reported in health care workers than in the general population (258). Hemodialysis patients represent a high-risk group for acquiring HBV infection (77). In addition, lower rates of response to HBV vaccination among patients with renal insufficiency (138) make this group of patients particularly susceptible to HBV infection. Transmission of HBV from surgeons to patients has also been reported (106, 249).
The correlation between the presence of HBeAg in serum and infectivity was recognized within a few years of the discovery of the virus (240). HBV DNA testing gradually replaced HBeAg as a sensitive and accurate indicator of infectivity (58). The presence of maternal serum HBeAg has been identified as a major risk factor for transplacental transmission of HBV (286). High HBV DNA levels in mothers are associated with failure of hepatitis B virus immune globulin (HBIG) and vaccination in infants (243, 280).
HBV vaccination is now a part of the national immunization programs of over 175 countries (http://www.who.int/immunization/topics/hepatitis_b/en/index.html). The mass HBV vaccination program has led to marked reduction in HBV infection and also in the incidence of HCC (35).
The classical serotyping of HBV (134) has been replaced by genotyping since the early 1990s. Hepatitis B virus genotypes A to I have been described, based on the divergence of the complete genome sequences by 8% or more. Subgenotypes within many HBV genotypes have been described (140). Genotype D is the most widespread genotype (207), while the other HBV genotypes are geographically restricted (8, 134). Infection with multiple genotypes, though infrequent, has been documented (275). An increased prevalence of infection with multiple genotypes has been reported among drug users (40).
DIAGNOSIS
Testing for hepatitis B virus surface antigenemia remains the mainstay in the diagnosis of acute hepatitis B virus infection. Anti-HBc IgM is a useful marker during the “core window,” a short period in resolving acute HBV infection between the loss of serum HBsAg and the appearance of anti-HBs. HBV DNA is the earliest detectable marker in acute HBV infection. HBV DNA testing is particularly useful in the detection of the early phase of acute HBV infection prior to the appearance of serum HBsAg; for this reason HBV DNA is tested using nucleic acid amplification technology (NAT) in blood and blood products in resource-rich countries (66, 118). The appearance of anti-HBe followed by the appearance of anti-HBs is characteristic of acute resolving HBV infection (172). The anti-HBs response remains detectable for several years following recovery from acute HBV infection, and it indicates protective immunity. Anti-HBc IgG persists for several decades, if not for life, following acute HBV infection. In areas of low HBV endemicity, anti-HBc screening of blood and blood products in addition to HBsAg testing is performed to identify past exposure to HBV (118).
Chronic HBV infection is defined by the persistence of serum HBsAg for more than 6 months. The presence of HBeAg correlates strongly with HBV DNA levels and an aggressive course of liver disease in chronic HBV infection (105). The loss of HBeAg in chronic HBV carriers generally represents a late phase in the course of chronic HBV infection (89). Low levels of anti-HBc IgM are frequently detected in patients with chronic HBV infection, albeit without any diagnostic significance (244). Estimation of HBV DNA levels is one of the most useful markers in the management of chronic hepatitis B. Estimation of HBV DNA and ALT levels in serum, the presence of HBeAg, and the assessment of liver histology help in the evaluation and identification of patients requiring antiviral treatment for chronic hepatitis B (268). Loss of HBeAg, ALT levels within the upper limit of normal, and reduction in HBV DNA levels are indicators of response to antiviral therapy. In addition, periodic assessment of HBV DNA levels is performed during antiviral treatment to determine therapeutic endpoints and identify the emergence of both drug resistance and primary/secondary treatment failure. Highly sensitive nucleic acid amplification-based methods are commercially available for estimation of HBV DNA levels (274). With the availability of a variety of therapeutic options for chronic hepatitis B, testing for antiviral resistance is being increasingly used. Genotypic (159), phenotypic, and virtual phenotyping methods are used for antiviral resistance testing (274). Clinical differences among HBV genotypes are gaining relevance (294, 289). However, HBV genotyping is not a part of the routine management of chronic hepatitis B.
REACTIVATION OF HBV
Resolution of acute HBV infection is marked by the appearance of anti-HBe in the serum followed by the appearance of anti-HBs. A pool of HBV cccDNA persists in hepatocytes after resolution of infection (153, 221). Reactivation of HBV is characterized by a sudden rise in HBV DNA and serum transaminase levels in patients with past exposure to HBV infection (117). Reactivation of HBV is frequently associated with immunosuppressive therapy (18), cancer chemotherapy (123), sudden withdrawal of antiviral therapy (70), and progressive immunodeficiency in human immunodeficiency virus (HIV) infection (22). In addition, reactivation of HBV may be spontaneous (117). Hepatitis B reactivation following liver transplantation is linked to past HBV exposure of the organ donor (223). The reappearance of HBV DNA in liver transplant recipients with past exposure to HBV is best described as reinfection. Clinical manifestations of HBV reactivation are variable and may include liver dysfunction (168). The rate of HBV reactivation varies greatly across different clinical groups (18, 174, 291). Reactivation of HBV occurs in individuals who are HBsAg positive (168) and also in HBsAg-negative individuals with occult HBV infection (107). Among HBsAg-positive patients on chemotherapy for hematological malignancies, the prophylactic use of lamivudine in preventing reactivation of HBV infection is well recognized (227). Reactivation of occult HBV infection leading to clinical hepatitis may occur in HBsAg-negative patients undergoing chemotherapy (123); however, the need for early identification of occult HBV infection in this group of patients is not widely appreciated. The role for anti-HBV prophylaxis in occult HBV patients undergoing chemotherapy needs further investigation. Emergence of drug resistance following prophylactic antiviral treatment among occult HBV-infected chemotherapy recipients is another potential problem.
HBV DNA contains a glucocorticoid response element (264), and patients receiving corticosteroids had a demonstrable increase in HBV DNA levels (145). The use of glucocorticoids in chemotherapeutic regimens is linked to increased risk of HBV reactivation (46).
Reactivation of HBV in HIV-infected patients with serological markers of past HBV infection is well documented (22, 103). Occult HBV infection is reported in 0.6% of HIV-infected patients with isolated anti-HBc reactivity (197). Reactivation of both overt HBV infection (70) and occult HBV infection (4, 22) has been reported in HIV-infected patients, especially after cessation or interruption of antiretroviral therapy. Recurrent monitoring of HBV DNA levels in HIV-infected patients with markers of past HBV infection may assist in early diagnosis and better management of HBV reactivation in this group of patients.
OCCULT HBV INFECTION
The loss of HBsAg or the presence of detectable anti-HBs indicates resolution from acute HBV infection. Both HBsAg and HBV DNA are detected in the majority of chronically infected patients (276). However, a small proportion of individuals have detectable HBV DNA in the serum and/or the liver in the absence of circulating HBsAg (218, 219, 259). Occult hepatitis B virus infection is defined as the presence of HBV DNA in the liver (with or without detectable HBV DNA in the serum) in HBsAg-negative individuals (219, 259). Seropositive occult hepatitis B virus infection is characterized by the presence of anti-HBc and/or anti-HBs, while neither anti-HBc nor anti-HBs is detected in seronegative occult hepatitis B virus infection (219). HBV antibodies, including anti-HBc, anti-HBs, and anti-HBe, are frequently detected in occult HBV infection (259). In many instances, individuals with occult HBV infection lack hepatitis B virus “e” antigenemia and have virus loads of <103 copies/ml (259, 295), though exceptions have been reported (26). HBV DNA levels can vary considerably in occult HBV infection among individuals positive for anti-HBs (9, 111). Occult HBV infection was not recognized as a clinical entity until the early 1990s (229, 284). With the extensive use of sensitive molecular techniques for HBV DNA detection there have been an increasing number of studies in the last decade investigating various aspects of occult HBV infection.
Prevalence
Occult HBV infection has been reported from several parts of the world, including areas of low HBV endemicity (187). The prevalence of occult HBV infection varies greatly across the globe, with higher rates being reported from Asia than from the rest of the world (259). Despite high HBV endemicity, a very low prevalence of occult HBV infection among low-risk populations such as blood donors has been confirmed by various groups in Asia and Africa (15, 74, 296, 299). Prevalence rates for occult HBV infection ranging from less than 1% to as high as 87% have been reported from different parts of the world (132, 266, 296). However, these prevalence rates need to be interpreted with caution. Several factors that could potentially influence estimated rates of occult HBV infection are summarized in Table 4. Unfortunately, multicenter studies using identical methods of recruitment of subjects, sampling, and testing methods are lacking. The geographical distribution of occult HBV infection worldwide warrants further investigation. However, it is well known that certain groups of patients are at a much higher risk of having occult HBV infection regardless of the geographical location. The groups with high risk for occult HBV infection are summarized in Table 5.
Table 4.
Factors influencing estimated prevalence of occult HBV infection
| Factor | Comment | Reference(s) |
|---|---|---|
| Population studied | ||
| Risk group | Prevalence rates vary between high-risk groups and low-risk groups | 29, 259 |
| Sampling | ||
| No. of samples | Occult HBV DNA may be intermittently detected in serum; serial sampling is ideal | 113 |
| HBV DNA may be detected in liver but not in serum | 108, 238 | |
| Testing | ||
| HBsAg testing | Some commercial assays are better suited for detection of HBsAg mutants | 147 |
| HBV DNA testing | Targeting multiple regions of the HBV genome improves detection; differences between amplification methods for HBV DNA testing exist | 108, 260 |
| Geographical region | ||
| HBV prevalence | Endemicity of HBV infection correlates with prevalence of occult HBV infection | 166 |
| Coinfections | HCV/HIV coinfections are associated with higher rates of occult HBV infection | 29, 170 |
Table 5.
High-risk groups for occult HBV infection
| Patient group | Reported prevalence (%)a | Reference(s) |
|---|---|---|
| Chronic HCV infection | 15–33 | 29, 128 |
| HIV infection | 10–45 | 103, 169 |
| Injection drug users | 45 | 260 |
| Hemodialysis | 27 | 69 |
| Hepatocellular carcinoma | 62 | 108 |
| Cryptogenic liver cirrhosis | 32 | 34 |
| Liver transplant | 64 | 93 |
Rounded to the nearest integer.
Clinical Relevance
Apart from posing diagnostic challenges, occult HBV infection may often be associated with a variety of clinical conditions. The role of occult HBV infection in chronic hepatitis C virus (HCV) infection is perhaps the most extensively studied. Cacciola et al. (29) not only found higher rates of occult HBV infection among patients with HCV-related chronic liver disease but also found liver cirrhosis more frequently among chronic HCV patients with occult HBV infection (33%) than among monoinfected patients (19%). In another study, transient lower response rates during interferon (IFN) therapy were seen in anti-HBc-positive chronically HCV-infected patients. Only a fraction of the anti-HBc-positive individuals had demonstrable HBV DNA (65). Other studies have failed to demonstrate an association between occult HBV infection and lower rates of response to anti-HCV therapy in coinfected patients (44, 241). A functional assessment of IFN response was done by Fukuda et al. (86) by estimation of intrahepatic mRNA expression of the type I IFN receptor gene. Chronic hepatitis C patients with occult HBV infection had lower expression of the IFN receptor gene and a poorer response to IFN than monoinfected patients. It still remains unclear how occult HBV infection affects the treatment of chronic HCV infection (76, 91, 128, 133, 191, 241).
Occult HBV infection has been associated with liver enzyme flares during chronic HCV infection (235) without changes in HCV RNA levels (127). Occult HBV infection in chronically HCV-infected patients has been associated with higher histological activity and advanced fibrosis (191), while other studies failed to demonstrate this association (76, 132). Differences in geographical region, infecting HBV and HCV genotypes, and environmental cofactors could partially explain these contrasting findings.
Occult HBV infection is frequently detected in cryptogenic chronic liver diseases, including chronic hepatitis and cirrhosis (17, 38, 116). In individuals with chronic hepatitis, the presence of HBV proteins and HBV DNA has been confirmed by immunostaining and in situ hybridization (38). The HBV DNA level in individuals with cryptogenic liver disease is generally less than 104 copies/ml (38). While the causal role of occult HBV infection in cryptogenic liver disease and chronic hepatitis is still debated (37, 116, 144), the usefulness of monitoring liver enzymes and HBV DNA levels in the management of occult HBV infection has been demonstrated (39). However, specific guidelines for the management of occult HBV-related liver diseases are yet to evolve.
Sequence analysis identified mutations in the surface gene, core gene, and polymerase gene of occult HBV genomes from patients with chronic liver diseases. In addition to sequence changes, differences in the ratios of the large and small surface proteins were also attributed to the loss of HBsAg in serum (37). Another study identified mutations in the X gene which reduced viral replication in occult HBV cases with chronic hepatitis (228). Occult HBV infections have also been reported in patients with nonalcoholic steatohepatitis (NASH) (17) and autoimmune hepatitis (116). Despite detection of HBV DNA and HBV proteins in patients with chronic liver diseases of unknown etiology, the causal role of occult HBV infection and the underlying pathogenic mechanisms remain elusive.
Occult HBV infections are detected in as many as 73% of HCV-related HCC patients (188, 250) and at a lower frequency (18%) in non-B non-C HCC (NBNC HCC) (144). The occult HBV sequences from NBNC HCC lack core promoter mutations that are frequently detected in HBsAg-positive HCC. In addition, diabetes and obesity are frequently detected in the NBNC HCC group compared to the HBsAg-positive HCC group. The authors argue that a higher incidence of nonalcoholic steatohepatitis in the NBNC HCC group weakens the causal association of occult HBV infection in the development of HCC (144). The presence of core promoter mutations in occult HBV genomes in HCV-related HCC argues for a contributory role of occult HBV infections in the pathogenesis of HCC (188). The detection of transcriptionally active and replication-competent episomal HBV in addition to integrated HBV sequences in occult HBV infection-related HCC further strengthens the causative role of occult HBV infection in HCC (214).
The risk of acquiring posttransfusion HBV infection is low with implementation of improved screening procedures. Occult HBV infections and to a lesser extent window-period infections contribute to the risk of transfusion-transmitted HBV infection (296, 299). The increased prevalence of occult HBV infection in high-risk groups was discussed above and is summarized in Table 5. Increased rates of occult HBV infection within the high-risk groups do not necessarily imply transmissibility of occult HBV. Nonetheless, it may not be speculative to anticipate transmission of HBV within these groups, considering the risk of multiple exposures in individuals within the high-risk groups. However, large-scale studies confirming transmission rates in high-risk groups from index cases with occult HBV infection are lacking. Intrafamilial horizontal transmission (61) and vertical transmission (228) from individuals with occult HBV infection have been reported.
Methods for Diagnosis of Occult HBV Infection
Chronic HBV infection is generally ruled out in the absence of detectable HBsAg in the serum. Differences among commercial assays in their ability to detect HBsAg associated with mutations in the “a” determinant are well recognized (281). Assays using polyclonal tracer antibodies for the detection of HBsAg vary in their ability to detect mutant HBsAg (281). However, assays using a polyclonal tracer antibody outperform assays using a monoclonal tracer for the detection of mutant HBsAg (124). Furthermore, HBsAg assays differ in their lower limits of detection (231). Highly sensitive commercial assays for HBsAg that consistently detect frequently encountered “a” determinant mutants (56, 57) should be preferentially used for HBsAg testing.
Detection of HBV DNA from serum or liver samples is considered the gold standard for the diagnosis of occult HBV infection. Experts have recently recommended the use of highly sensitive nested PCR or real-time PCR assays that can detect fewer than 10 copies of HBV DNA for the diagnosis of occult HBV infection (219). In addition, testing for multiple targets on the HBV genome increases HBV DNA detection rates (108) in patients with occult HBV infection. Intermittent viremia can occur in occult HBV infection, and periodic testing of HBV DNA will improve detection of occult HBV infection (127, 113). Periodic sampling for HBV DNA testing may be particularly appropriate for clinical groups at risk for occult HBV infection (Table 5). When available, testing of a liver biopsy specimen for HBV DNA will further augment the diagnosis of occult HBV infections, as HBV DNA is frequently detected in the liver in the absence of HBV DNA in the serum (108). Different screening methods are used across the world for screening blood and blood products (36, 141, 190). Individuals with occult hepatitis B virus infection can potentially transmit the infection through blood transfusions (154). Occult HBV infection is a major cause of posttransfusion hepatitis B (165). The prevalence of chronic HBV infection and availability of resources are major determinants of the screening methods used for HBV. For example, HBsAg with anti-HBc (total) and/or NAT is used for screening in resource-rich areas with a low prevalence of chronic HBV infection (208, 233). A good proportion of blood donors with occult hepatitis B virus infection have anti-HBc as the only serological marker of HBV infection (129, 242). Blood donors with isolated anti-HBc status are more infectious than those with low titers of anti-HBs (1). However, high rejection rates in areas of high HBV endemicity preclude anti-HBc screening of blood donors (36, 67). Although NAT testing for HBV DNA will reduce the risk of HBV transmission, its cost-effectiveness is still being questioned (125). The suitability of anti-HBc testing and NAT for screening blood and blood products is determined by (i) endemicity of HBV infection, (ii)) rates of anti-HBc detection in the population, and (iii) availability of resources.
MOLECULAR MECHANISMS LEADING TO OCCULT HBV INFECTION
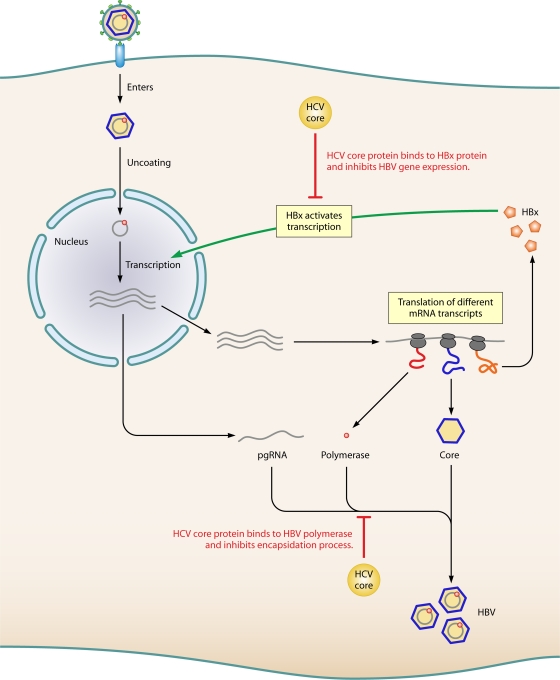
There have been significant advances in understanding the molecular mechanisms underlying occult HBV infection in the last decade; an overview of these mechanisms is shown in Fig. 1. Each of these mechanisms is reviewed in detail below.
Fig 1.
Overview of mechanisms leading to occult hepatitis B virus (HBV) infection.
Mutations and Deletions in the HBV Genome
Sequence variation in HBV genomes, including (i) mutations in the “a” determinant of HBsAg, (ii) treatment-associated mutations, (iii) splicing, and (iv) mutations in the pre-S region have been linked to occult HBV infection.
Mutations in the “a” determinant of HBsAg.
A mutation in the “a” determinant of the surface antigen was one of the earliest recognized mechanisms leading to occult HBV infection. Mutations in HBsAg lead to conformational changes rendering the protein undetectable by some of the commercially available HBsAg assays (219). Recently, the term “false” occult hepatitis B virus infection has been used to describe occult hepatitis B virus infections in individuals with HBV DNA levels comparable to those in individuals with overt HBV infection. “False” occult hepatitis B virus infections are usually associated with surface gene mutants that are not detectable by some commercial HBsAg assays (219, 165). Individuals with isolated anti-HBc-positive status with virus loads of greater than 104 copies/ml frequently harbor HBsAg mutants (148). The “a” determinant of HBsAg is a 2-loop structure that includes amino acids (aa) 124 to 147 (31, 32). It is rich in cysteine residues which are involved in disulfide bond formation and maintain the conformation of this region. Carman et al. first reported the sG145R mutation in the “a” determinant of HBsAg in a child who became infected with HBV despite active and passive immunoprophylaxis (31). This sG145R mutant has lower binding affinity to monoclonal antibody against HBsAg. Subsequently, several other mutations within the “a” determinant (49) and mutations in the surface gene outside the “a” determinant (32) were reported to have reduced binding affinity to monoclonal anti-HBs. Oon et al. (210) detected mutations in the “a” determinant among children born to HBsAg- and HBeAg-positive mothers who received both HBIG and the HBV vaccine at birth.
Mutations in the “a” determinant of the surface protein are associated with HBV reinfection following liver transplantation despite HBIG prophylaxis. Withdrawal of HBIG after liver transplantation led to reversion of the mutant to wild type in majority of the patients, indicating the role of HBIG-induced immune pressure in leading to “a” determinant mutants (92). Schilling et al. found that anti-HBs IgG is endocytosed by hepatocyte cell lines, leading to the intracellular accumulation of wild-type HBsAg while the sG145R-associated HBsAg was unaffected. HBIG was also found to inhibit the secretion of HBsAg into the serum without affecting HBV DNA replication, thus making HBsAg inaccessible to antibody used for detection of the surface antigen by some commercial assays (232). A recent study has demonstrated that in addition to blocking HBsAg release, anti-HBs can also partially block virion release from infected hepatocytes, contributing to HBV clearance from circulation (199).
The inability of some but not all commercial assays to detect HBsAg from samples associated with mutations in the “a” determinant is well documented (147). The emergence of “a” determinant mutants is a serious health concern not only because they are not detectable by some commercial HBsAg assays but also because they can infect both unvaccinated and vaccinated individuals.
Treatment-associated mutations.
Double mutations in the HBV polymerase associated with the emergence of a mutation in YMDD motif during lamivudine treatment result in amino acid changes in both the HBV polymerase and the surface gene (Q563S in the polymerase and sS207R in the surface gene) (278). In addition, other lamivudine-induced mutations that result in synonymous changes in the polymerase gene open reading frame (ORF) but nonsynonymous changes in the surface gene ORF were reported by Wakil et al. (278). They also reported (i) another novel mutation (V539I) in the “C” domain of the HBV polymerase that was associated with a premature stop codon in the surface gene and (ii) the emergence of a substitution within the “a” determinant of HBsAg (sS143L) in lamivudine-treated patients.
Lamivudine-associated polymerase gene mutations M204I and L180M/M204I, corresponding to sI195M and sW196S in HBsAg, have been shown to be associated with reduced binding to anti-HBs antibodies, suggesting that these mutants may escape detection in some of the commercially available assays for HBsAg (262); these mutants may potentially escape neutralization by vaccine-induced anti-HBs. Mutations that confer resistance to lamivudine also reduce the affinity of the HBV polymerase to natural deoxynucleoside triphosphate (dNTP) substrates, resulting in reduced replication competence (88). Therefore, lamivudine-selected mutants have reduced replication fitness compared to wild-type HBV (64). Lamivudine is used in combination with HBIG in HBV-related liver transplantation. Interestingly, HBIG-induced vaccine escape mutants (sP120T, sT123N, and sG145R) restored the replication fitness of lamivudine-resistant mutants (261). Therefore, a combination of lamivudine-resistant mutations and vaccine escape mutations renders HBsAg undetectable in some commercial assays and also confers replication competence comparable to that of the wild type in addition to resistance to lamivudine and HBIG. These mutants are of particular public health concern because of their ability to escape detection by some commercial HBsAg assays, infect vaccinated individuals, and resist treatment with lamivudine.
RNA splicing.
Splicing has been shown to have a significant effect on gene expression in HBV (107). Hass et al. demonstrated that a G-to-A mutation at position 458 of the surface gene altered the splicing of the S gene mRNA. Nucleotide (nt) 458 is close to the 5′ splice site of the S gene mRNA, and a mutation at this site interferes with the splicing of S gene mRNA. This mutation acts through a co-/posttranscriptional mechanism affecting the S gene mRNA export or RNA folding and is associated with a lack of HBsAg expression and a low-replication phenotype (107). Another mechanism of loss of HBsAg expression related to splicing has been reported in genotype D strains (269). A group of genotype D strains that represented a separate evolutionary branch was associated with positive selection (due to accumulation of substitutions) and had an acceptor site at nt 202. The authors report that the acceptor site at nt 202 and the donor site at nt 2986 are involved in a splice event resulting in the loss of the spacer region from the viral polymerase gene while retaining the original reading frame. The functions of the HBV polymerase are retained, while the expression of the small, middle, and large surface proteins are affected by this splice event. Therefore, it appears that alteration of splicing in surface gene mRNA results in reduced HBsAg secretion, thus leading to occult HBV infection (269).
Pre-S mutants.
Mutations in the pre-S region, especially deletions, have also been associated with a lack of detectable HBsAg in the serum. Deletions in the pre-S region are associated with reduced expression of HBV surface proteins and also help in viral persistence by eliminating HLA-restricted B-cell and T-cell epitopes. Pre-S1/pre-S2 mutations are frequently detected in occult HBV infection (37, 277). Mutations in the pre-S2/S promoters were detected in patients with occult HBV-related chronic liver disease; serum HBsAg was not detectable in these patients (37). In another study, a 183-bp deletion (nt 3019 to 3201) in the pre-S1 region was detected in occult HBV patients. The deletion covered the CCAAT element that is required for transcription factor binding. Other point mutations in the pre-S genes were also detected. The association of mutations and deletions in the pre-S gene with a lack of secreted HBsAg and low levels of HBeAg and HBV DNA was demonstrated using functional analysis by transfection into hepatocyte cell lines (80).
Xu and Yen (288) demonstrated that a 129-bp in-frame deletion in the S promoter region is associated with reduced levels of middle and small surface protein transcripts, resulting in a marked reduction in the expression of the two proteins. This S promoter deletion mutant, despite being replication competent, is associated with large amounts of intracellular retention of nonsecretable surface proteins. Melegari et al. (183) found deletions in the pre-S1 and pre-S2 regions following interferon therapy. Many of these pre-S deletion mutants selected after interferon therapy are associated with reduced HBsAg secretion in cell culture systems. Furthermore, extensive study of pre-S1 deletion mutants in Huh7 cells suggests that the loss of HBsAg titers is associated with the loss of the SP1 transcription factor binding site. Interestingly, despite retaining polymerase activity, the pre-S1 mutants required help from the wild-type HBV for secretion of encapsidated defective genomes into the serum. Fan et al. (79) showed that deletions in the pre-S region are detected in a significantly higher proportion of individuals with low HBV DNA levels than in those with higher virus loads. Among individuals with low HBV DNA levels, the deletions ranged from 70 to 141bp in the pre-S1 region and from 54 to 72 bp in the pre-S2 region.
Coinfection with Other Microbes
Coinfection with HCV.
Coinfection of HBV and HCV is well documented (27, 33, 43, 81, 236). Numerous studies have demonstrated decreased numbers of HBV replicative intermediates in HCV-coinfected individuals. Cacciola et al. found that about a third of the patients with chronic hepatitis C liver disease have detectable HBV DNA but no HBsAg in serum. They established a significant association between occult HBV infection and cirrhosis among HCV-infected patients. Their study also found a trend toward a response to interferon therapy among patients with chronic HCV infection and concurrent occult HBV infection (29). Occult HBV infection in chronically HCV-infected patients has been associated with an increased risk of HCC (177). The predominance of certain HBV genotypes in concurrent chronic HCV infection and occult HBV infection and their potential role in determining the clinical outcome have also been suggested recently (108). Higher rates of occult hepatitis B virus infection were detected in patients infected with HCV genotype 1b than in those with genotype 2a (85). Increased HBV DNA levels with occult HBV infection among HCV-infected patients have been associated with a simultaneous increase in liver enzymes (transaminases), suggesting a plausible mechanism leading to liver injury (127). In contrast, a lack of occult HBV infection-related clinical implications among patients with HCV-related liver diseases has been reported by other investigators. Kao et al. found that the prevalence of occult HBV infection did not correlate with the severity of HCV-related liver disease. Additionally, therapeutic responses to combination therapy (interferon and ribavirin) against HCV infection were comparable in patients with and without occult HBV infection (128).
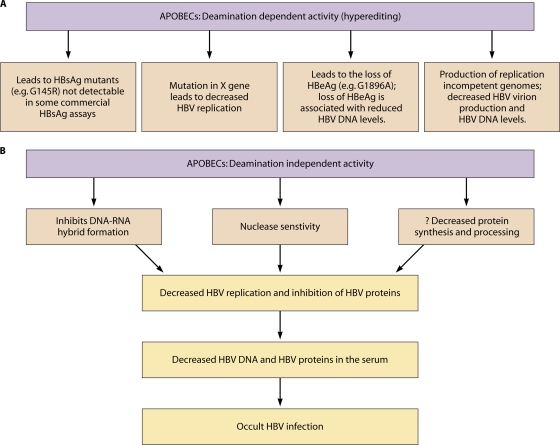
Rates of HCV coinfection in patients with chronic HBV infection vary considerably depending on the geographical location. Occult HBV infection in up to 52% of patients with chronic HCV infection has been reported (21, 85, 96, 116, 157). Several studies have shown that HBV and HCV coinfection results in lower levels of HBV replication (54, 59, 83) and decreased expression of HBsAg in the liver (54). Furthermore, superinfection with HCV in HBV-infected chimpanzees led to decreased HBsAg levels in serum (24). Similarly, coinfection with HCV was associated with significantly higher spontaneous HBsAg clearance rates than infection with HBV alone (237), strongly suggesting an interplay between the two viruses/viral proteins. Studies further investigating the inhibition of HBV replication and HBV protein production by HCV have demonstrated several interesting underlying mechanisms (Fig. 2).
Fig 2.
HCV coinfection in occult HBV infection. HCV core protein inhibits HBV gene expression by directly interacting with HBx protein and suppresses HBV replication by interfering with the binding of core and polymerase to package signal “ε” present in pregenomic RNA (pgRNA) within the hepatocyte, thereby preventing HBV encapsidation.
(i) Colocalization of HBV and HCV genomes in the nucleus.
Interference with HBV replication by HCV can take place if both viruses coexist in the same hepatocyte. Double fluorescent in situ hybridization was used to understand the role of HCV in inhibiting HBV replication in 6 liver biopsy specimens from patients with chronic HCV and occult HBV infection (224). The intensities of fluorescence signals corresponding to HBV DNA and HCV RNA were measured in singly infected and doubly infected hepatocytes using digital image analysis. The analysis showed that fluorescence in hepatocytes infected only with HBV was 1.6 ± 0.16 times higher than that in hepatocytes coinfected with HBV and HCV, although the difference was not statistically significant.
In contrast, another study using cell culture-propagated HCV and replication-competent HBV genomes in Huh-7 cells demonstrated a lack of strong interactions between the two viruses in coinfected hepatocytes in cell culture, suggesting a role for host responses in establishing viral dominance in coinfected cells (75). Nonetheless, they found extensive colocalization of HCV and HBV envelope proteins.
(ii) HCV core protein-mediated HBV suppression.
The HCV core protein is a part of the viral capsid, and it inhibits HBV replication and gene expression and suppresses activity of HBV enhancers (45, 234). Chen et al. elucidated several mechanisms of HCV core protein-mediated suppression of HBV (45). They cotransfected full-length or truncated versions of HCV structural genes (core and envelope 1) with cloned HBV DNA into Huh-7 cells and showed that the HCV core protein is required for the suppressive activity of HCV on HBV replication as well as the expression of HBsAg. Their findings also suggested impairment in HBV pregenomic RNA encapsidation as a possible mechanism of HBV suppression.
In another study, Shih et al. showed that phosphorylation at Ser-116 and Ser-99 of the HCV core protein is required for suppressive activity of HCV core protein. The replacement of Ser-99 and the Ser-116 with alanine or aspartate residues did not affect HCV core protein expression or nuclear localization; however, it resulted in loss of HBV suppression activity (239).
The package signal (ε) is present at the 5′ end of HBV pregenomic RNA; the HBV core and polymerase proteins interact with this signal to initiate the encapsidation process (10, 112). Chen et al. demonstrated that HCV core protein binds with HBV polymerase and inhibits binding of the polymerase to its package signal, preventing the encapsidation of HBV pregenomic RNA into its capsid (45). Given that HBx is a transactivator and activates HBV promoters and enhancers (52, 78, 195), Chen et al. hypothesized that HCV core protein inhibits HBV gene transcription by directly interacting with HBx. They cotransfected HBx null plasmid or wild-type HBV plasmid along with plasmids encoding HCV core protein. The HCV core protein-mediated inhibition of HBsAg, HBeAg, and HBV transcripts is dependent on the presence of HBx protein colocalized with the HCV core protein in both the nucleus and the cytoplasm. However, the ability of the HCV core protein to inhibit HBV replication is independent of HBx protein expression. Chen et al. further delinked the HCV core protein-mediated suppression of HBV gene expression and HBV replication. They demonstrated that a 22-amino-acid segment (from aa 101 to aa 122) of the C terminus of the HCV core protein plays a vital role in suppressing HBV gene expression, while the HCV core in its entirety is required for the suppression of HBV replication. In an attempt to understand the role of arginine residues in the HCV core protein, Chen et al. performed site-directed mutagenesis experiments on six arginine residues. The mutagenesis studies showed that Arg-101, Arg-113, Arg-114, and Arg-115 are required for the inhibitory activity of HCV core protein on both HBV gene expression and HBV replication. Arg-104 inhibits HBV encapsidation, but it has no effect on HBV gene expression.
Schuttler et al. showed that HCV core protein suppresses the activity of HBV enhancers I and II (234). They identified nucleotides 1115 to 1236 of HBV enhancer I and nucleotides 1730 to 1822 of HBV enhancer II as regions that are crucial for HCV core protein-mediated suppression of HBV. Interestingly, the regions from enhancers I and II essential for HBV suppression by HCV core protein also represent binding sites for members of the nuclear receptor family such as HNF4 and RXR. These nuclear factors play important regulatory roles in HBV replication by interacting with HBV enhancer I (90). Schuttler et al. also showed that HBV with mutations in the binding sites for nuclear receptors within HBV enhancers is less susceptible to repression by HCV core protein, and hence they proposed that the nuclear receptors bind to a leucine zipper motif present at the C terminus of the HCV core protein and suppress HBV enhancers. They also found that the repressor effect of the HCV core protein is more pronounced on HBV enhancer I than on HBV enhancer II. In their study, Schuttler et al. found differences among HCV core proteins from different HCV genotypes in their ability to suppress HBV enhancer I (234).
(iii) HCV NS2 protein-mediated HBV suppression.
NS2 is a nonstructural protein of HCV with autoproteolytic activity (62, 198). Dumoulin et al. (71) cotransfected NS2-encoding plasmids with HBV dimers and demonstrated that the HCV NS2 protein inhibited HBsAg and HBeAg secretion into the supernatant and also inhibited HBV replication. This inhibitory activity of the HCV NS2 protein is associated with its amino terminus. In addition, they demonstrated the role of the HCV NS2 protein in inhibiting various cellular promoters and viral promoters, including gene expression from HBV liver-specific and non-liver-specific promoters.
Coinfection with HIV.
Human immunodeficiency virus (HIV) and HBV share modes of transmission. Occult HBV infection in HIV-infected individuals is well recognized. The reported prevalence of occult HBV infection among HIV-positive patients varies based on the methods used for the detection of HBV DNA, the endemicity of HBV in the geographical region studied, and the history of antiretroviral treatment. In a longitudinal follow-up study, HBV DNA was detected at least once in almost 90% of a cohort of Swiss HIV-positive patients, compared to 25% detection rates for HBsAg (113). This finding suggests that (i) occult HBV infections are common among HIV-positive individuals and (ii) HBV DNA is intermittently detected in HIV-positive individuals, necessitating multiple sampling for HBV DNA in this group of patients. Another study, by Gupta et al. (103), found occult HBV infection in treatment-naïve HIV-infected patients; interestingly, about a fifth of the patients with occult HBV infection had detectable anti-HBs. However, the specific mechanisms leading to occult HBV infection in HIV-infected individuals still remain unknown.
Coinfection with Schistosoma mansoni.
Schistosoma mansoni is a parasite that affects over 200 million people worldwide, particularly in Asia and Africa (226). Coinfection with HBV and Schistosoma occurs frequently in areas where both agents are endemic (19, 73). When transgenic mice supporting HBV replication were infected with Schistosoma mansoni, a Th1-type response was followed by both Th1 and Th2 responses. HBV replication levels remained suppressed during both the Th1 response and the subsequent Th1 and Th2 responses (179). In gamma interferon (IFN-γ) knockout mice coinfected with Schistosoma mansoni, the suppression of HBV replication was minimal, suggesting that IFN-γ is the major antiviral cytokine in Schistosoma mansoni infection. HBV replication remained inhibited when both Th1 and Th2 responses were detected, suggesting that Th2 cytokines do not interfere in the antiviral activity of IFN-γ (179).
Apolipoprotein B mRNA-Editing Enzyme Catalytic Polypeptide and Occult HBV Infection
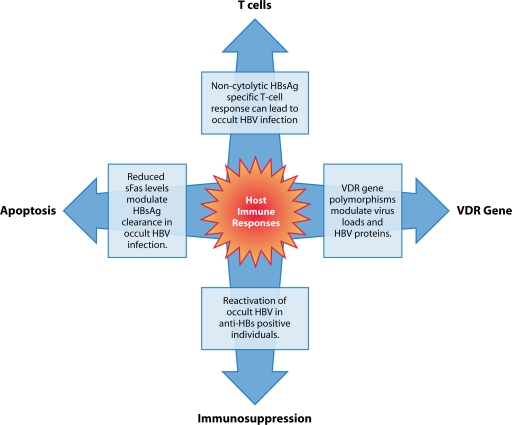
The physiological function of apolipoprotein B mRNA-editing enzyme catalytic polypeptides (APOBECs) is cytidine deamination (196, 255). The role of APOBECs in inhibiting and editing HIV replication has been well studied (114, 115). Subsequently, the ability of APOBEC3G to inhibit HBV replication was demonstrated. The expression of APOBEC3G in cells replicating HBV resulted in a 50-fold reduction in HBV DNA levels (265). Both deamination-dependent and deamination-independent mechanisms of inhibition of HBV replication have been reported for APOBECs (Fig. 3).
Fig 3.
Role of APOBEC deaminases in occult HBV infection. (A) Deamination activity of APOBEC protein converts cytosine to uracil in the HBV genome, leading to various mutations associated with occult HBV infection. (B) Deamination-independent activity of APOBEC deaminases inhibits DNA-RNA hybrid formation, increases susceptibility to nuclease digestion, and decreases protein processing, eventually leading to occult HBV.
Deamination-dependent inhibition of HBV replication.
Initially it was believed that only the cytidines in the minus strand of the HBV genome are edited, which is reflected as G-to-A mutations in the plus strand of HBV (204). However, Suspene et al. demonstrated that the plus strand of HBV is also deaminated by APOBEC enzymes (253). The overexpression of APOBEC3G is associated with hyperedited HBV genomes and a reduction in the replicative intermediates of HBV. Regions of the HBV genome encoding the surface proteins, polymerase, and the HBx protein are hyperedited by APOBECs (204). Normal human livers express low levels of APOBEC proteins (23). Several APOBEC3 genes are upregulated in HBV-related cirrhotic livers compared to cirrhotic tissue from alcoholic liver disease (270). It has been demonstrated that up to 35% of the HBV genomes in the liver may be edited by APOBECs (270). Of note, common mutations leading to the loss of HBeAg (G1896A) and lack of detectable HBsAg (sG145R) result from G-to-A mutations; these mutations have also been linked to APOBEC editing of HBV (270).
APOBEC hyperedited sequences have been reported from both occult and nonoccult cases of chronic HBV infection (271). It remains clear that the majority of HBV genomes in occult HBV infection are not hyperedited (271). However, minimal editing by APOBEC proteins, for example, the sG145R mutation that results due to a G-to-A mutation, is sufficient to cause occult HBV infection. Therefore, APOBEC-mediated occult HBV infection can occur in the absence of extensive HBV DNA editing. A growing body of literature in the last few years has demonstrated the role of APOBEC proteins in noncytolytic clearance of HBV infection. An increase in serum ALT levels is linked to an increase in hyperediting of the HBV genome, loss of HBeAg, and a reduction in HBV DNA levels, suggesting that hyperediting and the associated reduction in virus loads represent a strong host immune response (205).
Deamination-independent inhibition of HBV replication.
Although deamination-inactive APOBEC3G lacked the ability to hyperedit the HBV genome, it still retained the ability to inhibit HBV replication (206), suggesting the presence of deaminase-independent mechanisms inhibiting HBV replication. Rosler et al. reported increased nuclease susceptibility of HBV core-protein-associated pregenomic RNA (225). In another study, Nguyen et al. demonstrated the inhibition of HBV reverse transcriptase (RT) activity by APOBEC3G. They also showed that APOBEC3G inhibited early stages of HBV DNA synthesis by targeting HBV DNA-RNA hybrids and single-stranded HBV DNA (203). APOBEC3G copellets with HBV capsids, and encapsidation of APOBEC3G by replication-competent HBV nucleocapsids renders it resistant to proteinase K digestion. Further, it has been suggested that multiple copies of APOBEC3G may be packaged into HBV nucleocapsids by its interaction with HBV RT and the HBV RNA packaging signal (ε) (202). APOBEC proteins bind to the HBV core protein and hinder HBV capsid formation (11). Apart from APOBEC3G, other APOBEC proteins, including APOBEC3F and APOBEC3B, can inhibit HBV replication (23). In addition to inhibiting HBV replication, APOBEC3B can inhibit secretion of both HBsAg and HBeAg. The mechanisms underlying APOBEC-mediated inhibition of HBV proteins remain unclear, but interference with protein synthesis or processing has been suggested as a potential mechanism (23, 298). While the inhibitory mechanisms of APOBEC proteins that could produce occult infection are being increasingly recognized in vitro, large-scale studies comparing patients with and without occult infection are required to confirm and better understand the role of these proteins in vivo.
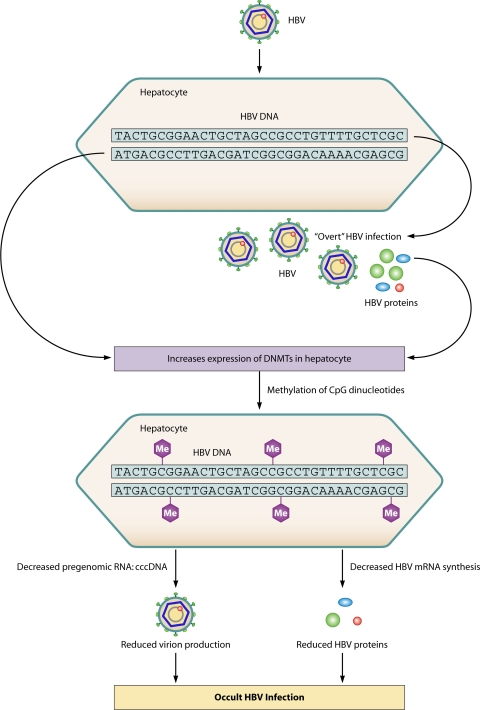
Host Immune Responses and Occult HBV Infection
Virus-host interactions play a crucial role in determining the outcome of hepatitis B virus infection. Host immune responses are involved in viral clearance, viral persistence, and immunopathogenesis of HBV infection. Interestingly, several host immune response-related mechanisms, such as apoptosis, cytolytic and noncytolytic T-cell responses, and vitamin D receptor (VDR) polymorphisms, have been linked to modulation of HBV replication and HBV protein synthesis (Fig. 4). However, only a few studies have implicated modulation of the host immune response as a stand-alone mechanism leading to occult hepatitis B virus infection. Martin et al. compared the serum cytokine expression profiles in HIV-infected patients with chronic HBV infection or with occult HBV infection. Lower soluble Fas (sFas) levels were detected in occult HBV infection than in chronic HBV infection (P = 0.01) (175). The Fas expression system is known to modulate apoptosis of infected hepatocytes and also plays a key role in the removal of aged hepatocytes and maintenance of normal liver homeostasis (110). Martin et al. argued that their finding of lower sFas levels in occult HBV infection indicates decreased apoptotic inhibition in occult HBV infection and could be one of the mechanisms for clearance of HBsAg and downregulating HBV replication in occult HBV infection (175). It has been suggested that reduced expression of CXCL12, a chemokine that modulates apoptosis, may play a role in occult HBV infection (109). Additional studies are required to evaluate the role of apoptosis in modulating the course of HBV infection.
Fig 4.
Host immunological responses leading to occult HBV infection. Host-derived responses, including a noncytolytic T-cell response, VDR polymorphism, immunosuppression, and differential regulation of apoptosis, contribute to the etiopathogenesis of occult HBV infection.
Differences in the HBV-specific cell-mediated immune response have been described in occult HBV infection. Anti-HBc-positive occult HBV patients had T-cell responses concurrent with protective memory, while anti-HBc-negative occult HBV patients had inadequacies in maturation of protective memory (297). The presence of HBV-specific CD8+ T cells in occult HBV infection without anti-HBc was demonstrated by staining with class I major histocompatibility complex tetramers (297). Guidotti et al. (98) demonstrated that clearance of more than 90% of HBV DNA in chimpanzees does not require destruction of HBV-infected hepatocytes, suggesting that some noncytolytic immune responses are critical in the clearance of acute HBV infection. Additionally, they showed that even HBV cccDNA is susceptible to these noncytolytic mechanisms. A noncytolytic HBsAg-specific T-cell response has been suggested as the potential mechanism for occult HBV infections associated with very low and undetectable levels of HBsAg (26).
Woodchucks inoculated with a low, non-liver-pathogenic dose of woodchuck hepatitis virus (WHV) developed occult infection but did not have surface antigenemia or antibody responses to viral proteins (99). Of note, the woodchucks with occult infection had WHV-specific T-cell responses against WHV proteins, and the secondary T-cell proliferative responses were comparable to those seen after primary WHV infection. These findings make occult infection with WHV an immunologically unique and recognizable entity. The authors also suggested that assessment of HBV-specific T-cell responses may be helpful in estimating the burden of occult HBV infection in high-risk groups such as health care workers and family members of infected individuals, who are likely to be exposed to low doses of HBV.
In a long-term follow-up study to assess the cytotoxic-T-lymphocyte (CTL) response following acute HBV infection, HBV-specific CTLs persisted in the blood for decades after clinical and serological recovery from acute HBV infection. Additionally, the strength of the CTL response directly correlates with the presence of HBV DNA in the serum. Furthermore, it is suggested that small quantities of virus may remain after recovery from acute HBV infection and help maintain the CTL response for decades; the CTL responses in turn play a significant role in keeping active viral replication under control (222). It appears that both humoral and cell-mediated responses are likely to play significant roles in the development of occult hepatitis B virus infection.
Vitamin D3 and the VDR regulate several cytokines (139) and are important determinants of the anti-HBV response (120). Polymorphisms in the VDR gene have been linked to the outcome of chronic HBV infection (120). In addition, differences in HBV DNA levels (252) and loss of HBeAg (120) have been linked to certain VDR genotypes. Recently, polymorphisms in the VDR gene have been detected in occult HBV infections (7).
Reactivation of occult HBV infection in unvaccinated patients with anti-HBs-positive status associated with past exposure to HBV may result in vaccine escape mutants (9). The inability of some commercial assays to detect the HBsAg associated with vaccine escape mutants despite high virus loads further complicates the picture (48).
Epigenetic Changes
Methylation.
In the human genome, regions rich in CpG dinucleotides are referred to as CpG islands. Methylation of cytosines in CpG dinucleotides within CpG islands in gene promoters leads to gene silencing (216). Methylation is a key mechanism for regulation of transcriptional activity. Methylation of HBV DNA represents a novel epigenetic mechanism that impairs HBV proteins, HBV replication, and HBV virion production, leading to occult HBV infection (Fig. 5). Nearly 2 decades ago it was demonstrated that HBV DNA integrated into the host genome is methylated. Methylation of HBV DNA encoding the HBV core protein leads to loss of HBV core protein in PLC/PRF/5, a human hepatoma cell line with integrated HBV DNA sequences (186). It was generally accepted that only integrated HBV DNA sequences are methylated. However, the observation of chromatin-like minichromosomes during replication prompted the search for CpG islands in episomal DNA, and three were recently identified (271). Interestingly, key regulatory elements of the HBV genome were located within or adjacent to the 3 CpG islands (271). Episomal HBV DNA from human liver tissue and from cell culture can be methylated. Of note, methylation of CpG island 2 in the HBV genome is frequently detected in occult HBV infection (271). HBV cccDNA is frequently methylated in human liver tissues (272). Transfection of in vitro-methylated HBV DNA constructs into hepatocyte cell lines was associated with a >90% decrease in secreted HBsAg. In addition, HBeAg and HBcAg expression was markedly reduced by methylation of HBV, clearly demonstrating the role of CpG islands in regulating HBV gene expression (272). HBV replication in cell culture induced the expression of DNA methyltransferases (DNMTs), enzymes vital for DNA methylation. The HBV-induced DNMTs could methylate HBV DNA, resulting in the inhibition of HBV transcription and HBV replication (273). Hypermethylated HBV DNA sequences are frequently detected in HCC patients with occult HBV infection (130). Methylation of cccDNA is associated with low serum HBV DNA levels and decreased virion production in patients with liver cirrhosis (135). The association between HBeAg and high virus loads is well known (53, 119). It was recently demonstrated that a higher ratio of methylated cccDNA to total cccDNA is detected in HBeAg-negative individuals than that in HBeAg-positive individuals. In addition, methylation of cccDNA correlated with reduced HBV replication (101). Recent studies have demonstrated a pivotal role for HBV methylation in occult HBV infection. However, additional studies will throw more light on the role of this recently identified epigenetic mechanism in occult HBV infection.
Fig 5.
Mechanism of occult HBV infection via methylation of HBV DNA. HBV induces expression of cellular DNA methyltransferases (DNMTs), leading to methylation of CpG dinucleotides in the HBV genome. Hypermethylation impairs HBV replication, virion production, and HBV protein levels, leading to occult HBV infection.
Acetylation.
The role of acetylation of histones bound to HBV DNA in regulating HBV replication and transcription has been convincingly demonstrated in several studies. In the mid 1990s, Newbold et al. (201) discovered that the hepatitis B viral nucleoprotein complex is arranged in the form of a minichromosome composed of nucleosomes, suggestive of transcriptional regulation of HBV DNA. Hyperacetylation of cccDNA-bound histones is associated with increased HBV replication in cell culture. In the presence of histone deacetylase inhibitors (valproic acid or trichostatin A), high HBV transcript levels and increased HBV replication are correlated with an increase in acetylated histones bound to cccDNA. Furthermore, acetylation of H3 and H4 bound to cccDNA in liver tissues from patients with chronic hepatitis B virus infection correlated with serum HBV DNA levels. Hypoacetylation of histones bound to cccDNA seen in liver tissue from patients with low virus loads is linked to recruitment of histone deacetylase (215). Subsequently, the recruitment of HBx protein to the cccDNA minichromosome along with histones has been demonstrated (16). Interestingly, an HBx mutant with a single nucleotide substitution is associated with rapid hypoacetylation of histones bound to cccDNA, impairing recruitment of p300, a transcriptional coactivator. The HBx mutant was associated with reduced HBV pregenomic RNA and reduced HBV replication, suggesting a key role for the HBx protein in regulating HBV replication. Recently, remodelling of the HBV minichromosome by phosphorylation and methylation of histones has been shown to regulate HBV replication (95). However, this recently reported mechanism and its potential role in occult HBV infection have not yet been investigated by use of molecular epidemiological studies.
Genome Integration
Integration of HBV DNA sequences into the host genome is frequently detected in patients with chronic HBV infection and is found to precede HCC (267). Disruption and rearrangement of genes during integration into chromosomal DNA can result in (i) loss of HBsAg in the serum, (ii) reduction in virion production, and (iii) loss of detectable HBV DNA in serum. Therefore, integration of HBV DNA represents a key mechanism underlying occult HBV infection, especially following several years of chronic HBV infection. Integrated HBV DNA rather than episomal HBV is frequently detected in HBV-related HCC (220). Integrated HBV DNA is often defective (25), and integration of certain HBV genes is observed more frequently than that of others (267). While high rates of HBV DNA integration have been reported from HBsAg-positive HCC (131), HBV DNA integration in HBsAg-negative HCC is also widely reported (178, 188, 254), especially among anti-HCV-positive patients. Specific integration patterns disrupting the expression of HBsAg have not been reported in HBV-HCV dual infection. The inhibition of HBV replication and HBV proteins has been discussed above.
The HBV core gene may often be lost during integration of HBV DNA, resulting in reduction or loss of the HBV core protein. The loss of the HBV core protein is associated with suboptimal virus assembly and the accumulation of unencapsidated HBV DNA within the hepatocyte. This may explain why patients with HCC related to HBV lack detectable HBV DNA in blood though HBV DNA may be readily detected in the liver (220).
Overexpression of large HBs protein prevents secretion of all forms of surface protein and leads to intrahepatic accumulation of surface proteins as granules (51). The large HBs protein constitutes a small proportion of total surface proteins. Huang and Yen (121) studied the role of disruptions and rearrangements in HBV DNA that occur during integration in regulating HBsAg expression. Replacement of a region downstream of the S gene ORF containing enhancer I and II with the pre-S1 promoter resulted in decreased S gene transcripts without affecting the levels of pre-S transcripts. Changes in the ratios of S gene transcripts to pre-S1 transcripts blocked the secretion of S protein. Similarly, other rearrangements resulting in the loss of HBV enhancers lead to intracellular retention of surface proteins that remain undetectable in serum.
Immune Complexes in Occult Hepatitis B Virus Infection
Entrapment of HBsAg in immune complexes with anti-HBs can impair HBsAg detection by conventional serological assays. In general, the appearance of detectable anti-HBs correlates with a decrease or complete disappearance of HBsAg-containing immune complexes (213). Interestingly, immune complexes containing HBsAg have been detected in HBsAg-negative occult HBV infection among patients with HCC (28). HBV DNA was detected in about 40% of HBsAg-negative but anti-HBc total positive blood donors, with HBV-containing immune complexes present in a majority of the HBV DNA-positive donors (293). Sequencing of HBV DNA from these donors demonstrated the lack of nucleic acid changes that alter major epitopes of HBsAg, confirming the role of circulating immune complexes in occult HBV infections. Michalak et al. demonstrated that HBV DNA from convalescent-phase sera cosedimented with HBsAg in a sucrose gradient column representing naked core particles or intact virions in circulating immune complexes. These data suggest that hepatitis B virus can persist despite recovery from acute infection (185). Circulating HBsAg-containing immune complexes have been demonstrated in patients with acute HBV infection, in asymptomatic HBsAg carriers, and also in chronic HBV infection (6). HBsAg-containing immune complexes have also been found in the presence of detectable anti-HBs (230). Madalinski et al. found anti-pre-S1 antibodies to be frequently involved in the formation of HBV-containing immune complexes in patients with chronic hepatitis B virus infection (171). Levya et al. correlated the presence of HBsAg-containing immune complexes and the course of hepatitis. Interestingly, they found that HBsAg-containing immune complexes are consistently present in patients with chronic hepatitis B virus infection compared to those with acute resolving hepatitis (155). Other studies have shown the opposite finding (6). Differences in the methods used could in part account for these contrasting observations. Increases in levels of immune complexes containing woodchuck hepatitis virus surface antigen (WHsAg) and anti-WHs correlated with the peaks of serum viremia and antigenemia, indicating the presence of surface antigen-containing complexes in WHV similar to those in HBV (94). It is clear that circulating HBsAg-containing immune complexes can be associated with occult HBV infection; however, the magnitude of the problem in the settings of acute resolving hepatitis and chronic hepatitis remains poorly understood.
EMERGING ISSUES
The persistence of HBV cccDNA in the liver tissues of both occult and nonoccult HBV cases has been demonstrated (277). Host immune responses play a critical role in controlling HBV replication. Differences, if any, in host immune responses between occult and nonoccult HBV cases in controlling the replication of HBV from the intrahepatic pool of cccDNA are poorly understood. The role of host immune responses in occult HBV infection remains elusive; large-scale studies focusing on this area may provide novel insights on the mechanisms leading to occult HBV infection.
Functional studies on full-length HBV genomes from occult HBV cases did not identify a predominant role for any particular mechanism leading to occult HBV infection, suggesting that occult HBV infection is often a result of multiple mechanisms (37, 80). With a few exceptions, it is likely that the mechanisms discussed above act in tandem, leading to occult HBV infection. Additional studies on full-length HBV genomes from occult HBV cases may throw more light on the interplay between the mechanisms leading to occult HBV infection.
Some of the recently identified molecular mechanisms leading to occult HBV infection play a direct role in carcinogenesis. Increased expression of APOBEC3B in HCC tissue conferred a selective clonal growth advantage to preneoplastic hepatocytes (287). Similarly, HBV-induced DNMTs led to aberrant methylation of the host genes, including tumor suppressor genes, apart from contributing to methylation of the HBV genome (273). Additional studies investigating the mechanisms underlying occult HBV infections and their contribution to hepatocarcinogenesis will help us better understand the causative role of occult HBV in HCC.
Biographies
Jasmine Samal graduated in biomedical sciences in 2008 from Delhi University. She received her master of science in biochemistry from Hamdard University. She is currently pursuing her Ph.D. degree at IIT Delhi, India, studying the role of HBeAg in HBV replication.
Manish Kandpal received his bachelor's degree in biochemical engineering from Kumaun University and then his M.Tech. degree in biotechnology from Anna University. He is currently working on the biological role of HBeAg in HBV-related liver disease for his Ph.D. degree from IIT Delhi, India.

Perumal Vivekanandan is an Assistant Professor at the Kusuma School of Biological Sciences, IIT Delhi, India. He received his Ph.D. degree in basic medical sciences from the Christian Medical College, Vellore. He studied the molecular biology of HBV and the biology of HBV-related hepatocellular carcinoma as a postdoctoral fellow at the Johns Hopkins University School of Medicine, Baltimore, MD. His contributions to the field include (i) elucidation of novel mechanisms leading to occult HBV infection and (ii) pioneering work in epigenetic regulation of HBV and its proteins. He is currently working on understanding the biological role of HBeAg in the pathogenesis of chronic HBV infection.
REFERENCES
- 1. Allain JP, Cox L. 2011. Challenges in hepatitis B detection among blood donors. Curr. Opin. Hematol. 18: 461–466 [DOI] [PubMed] [Google Scholar]
- 2. Alpert E, Isselbacher KJ, Schur PH. 1971. The pathogenesis of arthritis associated with viral hepatitis. Complement-component studies. N. Engl. J. Med. 285: 185–189 [DOI] [PubMed] [Google Scholar]
- 3. Alter MJ, Favero MS, Maynard JE. 1986. Impact of infection control strategies on the incidence of dialysis-associated hepatitis in the United States. J. Infect. Dis. 153: 1149–1151 [DOI] [PubMed] [Google Scholar]
- 4. Altfeld M, et al. 1998. Reactivation of hepatitis B in a long-term anti-HBs-positive patient with AIDS following lamivudine withdrawal. J. Hepatol. 29: 306–309 [DOI] [PubMed] [Google Scholar]
- 5. Amin J, et al. 2007. Liver cancer and hepatitis B and C in New South Wales, 1990–2002: a linkage study. Aust. N. Z. J. Public Health 31: 475–482 [DOI] [PubMed] [Google Scholar]
- 6. Anh-Tuan N, Novak E. 1980. Detection and quantitation of hepatitis B surface antigen immune complexes (HBsAg-ICs) by an antigen-specific method. II. Circulating immune complexes (CICs) in patients with hepatitis B and asymptomatic HBsAg carriers. J. Immunol. Methods 35: 307–318 [DOI] [PubMed] [Google Scholar]
- 7. Arababadi MK, Pourfathollah AA, Jafarzadeh A, Hassanshahi G, Rezvani ME. 2010. Association of exon 9 but not intron 8 VDR polymorphisms with occult HBV infection in south-eastern Iranian patients. J. Gastroenterol. Hepatol. 25: 90–93 [DOI] [PubMed] [Google Scholar]
- 8. Arauz-Ruiz P, Norder H, Robertson BH, Magnius LO. 2002. Genotype H: a new Amerindian genotype of hepatitis B virus revealed in Central America. J. Gen. Virol. 83: 2059–2073 [DOI] [PubMed] [Google Scholar]
- 9. Awerkiew S, et al. 2007. Reactivation of an occult hepatitis B virus escape mutant in an anti-HBs positive, anti-HBc negative lymphoma patient. J. Clin. Virol. 38: 83–86 [DOI] [PubMed] [Google Scholar]
- 10. Bartenschlager R, Junker-Niepmann M, Schaller H. 1990. The P gene product of hepatitis B virus is required as a structural component for genomic RNA encapsidation. J. Virol. 64: 5324–5332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Baumert TF, Rosler C, Malim MH, von Weizsacker F. 2007. Hepatitis B virus DNA is subject to extensive editing by the human deaminase APOBEC3C. Hepatology 46: 682–689 [DOI] [PubMed] [Google Scholar]
- 12. Beasley RP. 1988. Hepatitis B virus. The major etiology of hepatocellular carcinoma. Cancer 61: 1942–1956 [DOI] [PubMed] [Google Scholar]
- 13. Beasley RP, Hwang LY, Lin CC, Chien CS. 1981. Hepatocellular carcinoma and hepatitis B virus. A prospective study of 22 707 men in Taiwan. Lancet ii: 1129–1133 [DOI] [PubMed] [Google Scholar]
- 14. Beck J, Nassal M. 2007. Hepatitis B virus replication. World J. Gastroenterol. 13: 48–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Behzad-Behbahani A, et al. 2006. Anti-HBc & HBV-DNA detection in blood donors negative for hepatitis B virus surface antigen in reducing risk of transfusion associated HBV infection. Indian J. Med. Res. 123: 37–42 [PubMed] [Google Scholar]
- 16. Belloni L, et al. 2009. Nuclear HBx binds the HBV minichromosome and modifies the epigenetic regulation of cccDNA function. Proc. Natl. Acad. Sci. U. S. A. 106: 19975–19979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Berasain C, et al. 2000. Pathological and virological findings in patients with persistent hypertransaminasaemia of unknown aetiology. Gut 47: 429–435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Berger A, Preiser W, Kachel HG, Sturmer M, Doerr HW. 2005. HBV reactivation after kidney transplantation. J. Clin. Virol. 32: 162–165 [DOI] [PubMed] [Google Scholar]
- 19. Berhe N, Myrvang B, Gundersen SG. 2007. Intensity of Schistosoma mansoni, hepatitis B, age, and sex predict levels of hepatic periportal thickening/fibrosis (PPT/F): a large-scale community-based study in Ethiopia. Am. J. Trop. Med. Hyg. 77: 1079–1086 [PubMed] [Google Scholar]
- 20. Bernuau J, Rueff B, Benhamou JP. 1986. Fulminant and subfulminant liver failure: definitions and causes. Semin. Liver Dis. 6: 97–106 [DOI] [PubMed] [Google Scholar]
- 21. Besisik F, et al. 2003. Occult HBV infection and YMDD variants in hemodialysis patients with chronic HCV infection. J. Hepatol. 38: 506–510 [DOI] [PubMed] [Google Scholar]
- 22. Bloquel B, et al. 2010. Occult hepatitis B infection in patients infected with HIV: report of two cases of hepatitis B reactivation and prevalence in a hospital cohort. J. Med. Virol. 82: 206–212 [DOI] [PubMed] [Google Scholar]
- 23. Bonvin M, et al. 2006. Interferon-inducible expression of APOBEC3 editing enzymes in human hepatocytes and inhibition of hepatitis B virus replication. Hepatology 43: 1364–1374 [DOI] [PubMed] [Google Scholar]
- 24. Bradley DW, et al. 1983. Non-A, non-B hepatitis in chimpanzees: interference with acute hepatitis A virus and chronic hepatitis B virus infections. J. Med. Virol. 11: 207–213 [DOI] [PubMed] [Google Scholar]
- 25. Brechot C, et al. 2010. Hepatitis B virus (HBV)-related hepatocellular carcinoma (HCC): molecular mechanisms and novel paradigms. Pathol. Biol. (Paris) 58: 278–287 [DOI] [PubMed] [Google Scholar]
- 26. Bremer CM, et al. 2009. Transient occult hepatitis B virus infection in a blood donor with high viremia. Transfusion 49: 1621–1629 [DOI] [PubMed] [Google Scholar]
- 27. Brotman B, et al. 1983. Interference between non-A, non-B and hepatitis B virus infection in chimpanzees. J. Med. Virol. 11: 191–205 [DOI] [PubMed] [Google Scholar]
- 28. Brown SE, Howard CR, Steward MW, Ajdukiewicz AB, Whittle HC. 1984. Hepatitis B surface antigen containing immune complexes occur in seronegative hepatocellular carcinoma patients. Clin. Exp. Immunol. 55: 355–359 [PMC free article] [PubMed] [Google Scholar]
- 29. Cacciola I, et al. 1999. Occult hepatitis B virus infection in patients with chronic hepatitis C liver disease. N. Engl. J. Med. 341: 22–26 [DOI] [PubMed] [Google Scholar]
- 30. Cacoub P, Terrier B. 2009. Hepatitis B-related autoimmune manifestations. Rheum. Dis. Clin. North Am. 35: 125–137 [DOI] [PubMed] [Google Scholar]
- 31. Carman WF, et al. 1990. Vaccine-induced escape mutant of hepatitis B virus. Lancet 336: 325–329 [DOI] [PubMed] [Google Scholar]
- 32. Carman WF, et al. 1995. Fulminant reactivation of hepatitis B due to envelope protein mutant that escaped detection by monoclonal HBsAg ELISA. Lancet 345: 1406–1407 [DOI] [PubMed] [Google Scholar]
- 33. Chan CY, et al. 1991. Superinfection with hepatitis C virus in patients with symptomatic chronic hepatitis B. Scand. J. Infect. Dis. 23: 421–424 [DOI] [PubMed] [Google Scholar]
- 34. Chan HL, et al. 2002. Occult HBV infection in cryptogenic liver cirrhosis in an area with high prevalence of HBV infection. Am. J. Gastroenterol. 97: 1211–1215 [DOI] [PubMed] [Google Scholar]
- 35. Chang MH, et al. 2009. Decreased incidence of hepatocellular carcinoma in hepatitis B vaccinees: a 20-year follow-up study. J. Natl. Cancer Inst. 101: 1348–1355 [DOI] [PubMed] [Google Scholar]
- 36. Chaudhuri V, Nanu A, Panda SK, Chand P. 2003. Evaluation of serologic screening of blood donors in India reveals a lack of correlation between anti-HBc titer and PCR-amplified HBV DNA. Transfusion 43: 1442–1448 [DOI] [PubMed] [Google Scholar]
- 37. Chaudhuri V, Tayal R, Nayak B, Acharya SK, Panda SK. 2004. Occult hepatitis B virus infection in chronic liver disease: full-length genome and analysis of mutant surface promoter. Gastroenterology 127: 1356–1371 [DOI] [PubMed] [Google Scholar]
- 38. Chemin I, et al. 2001. High incidence of hepatitis B infections among chronic hepatitis cases of unknown aetiology. J. Hepatol. 34: 447–454 [DOI] [PubMed] [Google Scholar]
- 39. Chemin I, Guillaud O, Queyron PC, Trepo C. 2009. Close monitoring of serum HBV DNA levels and liver enzymes levels is most useful in the management of patients with occult HBV infection. J. Hepatol. 51: 824–825 [DOI] [PubMed] [Google Scholar]
- 40. Chen BF, et al. 2004. High prevalence of mixed genotype infections in hepatitis B virus infected intravenous drug users. J. Med. Virol. 74: 536–542 [DOI] [PubMed] [Google Scholar]
- 41. Chen CJ, et al. 2006. Risk of hepatocellular carcinoma across a biological gradient of serum hepatitis B virus DNA level. JAMA 295: 65–73 [DOI] [PubMed] [Google Scholar]
- 42. Chen CJ, Wang LY, Yu MW. 2000. Epidemiology of hepatitis B virus infection in the Asia-Pacific region. J. Gastroenterol. Hepatol 15(Suppl.): E3–E6 [DOI] [PubMed] [Google Scholar]
- 43. Chen DS, et al. 1990. Hepatitis C virus infection in an area hyperendemic for hepatitis B and chronic liver disease: the Taiwan experience. J. Infect. Dis. 162: 817–822 [DOI] [PubMed] [Google Scholar]
- 44. Chen LW, et al. 2010. Therapeutic effects of pegylated interferon plus ribavirin in chronic hepatitis C patients with occult hepatitis B virus dual infection. J. Gastroenterol. Hepatol. 25: 259–263 [DOI] [PubMed] [Google Scholar]
- 45. Chen SY, et al. 2003. Mechanisms for inhibition of hepatitis B virus gene expression and replication by hepatitis C virus core protein. J. Biol. Chem. 278: 591–607 [DOI] [PubMed] [Google Scholar]
- 46. Cheng AL, et al. 2003. Steroid-free chemotherapy decreases risk of hepatitis B virus (HBV) reactivation in HBV-carriers with lymphoma. Hepatology 37: 1320–1328 [DOI] [PubMed] [Google Scholar]
- 47. Cheong JY, et al. 2010. Association of interleukin-18 gene polymorphisms with hepatitis B virus clearance. Dig. Dis. Sci. 55: 1113–1119 [DOI] [PubMed] [Google Scholar]
- 48. Cheung WI, et al. 2010. Reactivation of hepatitis B virus infection with persistently negative HBsAg on three HBsAg assays in a lymphoma patient undergoing chemotherapy. J. Clin. Virol. 47: 193–195 [DOI] [PubMed] [Google Scholar]
- 49. Chiou HL, Lee TS, Kuo J, Mau YC, Ho MS. 1997. Altered antigenicity of ‘a’ determinant variants of hepatitis B virus. J. Gen. Virol. 78: 2639–2645 [DOI] [PubMed] [Google Scholar]
- 50. Chisari FV, et al. 1989. Molecular pathogenesis of hepatocellular carcinoma in hepatitis B virus transgenic mice. Cell 59: 1145–1156 [DOI] [PubMed] [Google Scholar]
- 51. Chisari FV, et al. 1986. Expression of hepatitis B virus large envelope polypeptide inhibits hepatitis B surface antigen secretion in transgenic mice. J. Virol. 60: 880–887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Choi BH, Park GT, Rho HM. 1999. Interaction of hepatitis B viral X protein and CCAAT/enhancer-binding protein alpha synergistically activates the hepatitis B viral enhancer II/pregenomic promoter. J. Biol. Chem. 274: 2858–2865 [DOI] [PubMed] [Google Scholar]
- 53. Chu CJ, et al. 2003. Prevalence of HBV precore/core promoter variants in the United States. Hepatology 38: 619–628 [DOI] [PubMed] [Google Scholar]
- 54. Chu CM, Yeh CT, Liaw YF. 1998. Low-level viremia and intracellular expression of hepatitis B surface antigen (HBsAg) in HBsAg carriers with concurrent hepatitis C virus infection. J. Clin. Microbiol. 36: 2084–2086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Chu CM, Liaw YF. 2007. HBsAg seroclearance in asymptomatic carriers of high endemic areas: appreciably high rates during a long-term follow-up. Hepatology 45: 1187–1192 [DOI] [PubMed] [Google Scholar]
- 56. Coleman PF. 2006. Detecting hepatitis B surface antigen mutants. Emerg. Infect. Dis. 12: 198–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Coleman PF, Chen YC, Mushahwar IK. 1999. Immunoassay detection of hepatitis B surface antigen mutants. J. Med. Virol. 59: 19–24 [DOI] [PubMed] [Google Scholar]
- 58. Corden S, et al. 2003. HBV DNA levels and transmission of hepatitis B by health care workers. J. Clin. Virol. 27: 52–58 [DOI] [PubMed] [Google Scholar]
- 59. Crespo J, et al. 1994. Prevalence and significance of hepatitis C viremia in chronic active hepatitis B. Am. J. Gastroenterol. 89: 1147–1151 [PubMed] [Google Scholar]
- 60. Cromlish JA. 1996. Hepatitis B virus-induced hepatocellular carcinoma: possible roles for HBx. Trends Microbiol. 4: 270–274 [DOI] [PubMed] [Google Scholar]
- 61. Datta S, Banerjee A, Chandra PK, Chowdhury A, Chakravarty R. 2006. Genotype, phylogenetic analysis, and transmission pattern of occult hepatitis B virus (HBV) infection in families of asymptomatic HBsAg carriers. J. Med. Virol. 78: 53–59 [DOI] [PubMed] [Google Scholar]
- 62. De Francesco R. 1999. Molecular virology of the hepatitis C virus. J. Hepatol 31(Suppl. 1): 47–53 [DOI] [PubMed] [Google Scholar]
- 63. Degertekin H, Tuzcu A, Yalcin K. 2000. Horizontal transmission of HBV infection among students in Turkey. Public Health 114: 411–412 [DOI] [PubMed] [Google Scholar]
- 64. Delaney WEIV, et al. 2003. The hepatitis B virus polymerase mutation rtV173L is selected during lamivudine therapy and enhances viral replication in vitro. J. Virol. 77: 11833–11841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. De Maria N, et al. 2000. The impact of previous HBV infection on the course of chronic hepatitis C. Am. J. Gastroenterol. 95: 3529–3536 [DOI] [PubMed] [Google Scholar]
- 66. Dettori S, et al. 2009. Identification of low HBV-DNA levels by nucleic acid amplification test (NAT) in blood donors. J. Infect. 59: 128–133 [DOI] [PubMed] [Google Scholar]
- 67. Dhawan HK, et al. 2008. Anti-HBc screening in Indian blood donors: still an unresolved issue. World J. Gastroenterol. 14: 5327–5330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Dienstag JL. 1981. Immunopathogenesis of the extrahepatic manifestations of hepatitis B virus infection. Springer Semin. Immunopathol. 3: 461–472 [DOI] [PubMed] [Google Scholar]
- 69. Di Stefano M, et al. 2009. Occult HBV infection in hemodialysis setting is marked by presence of isolated antibodies to HBcAg and HCV. J. Nephrol. 22: 381–386 [PubMed] [Google Scholar]
- 70. Dore GJ, et al. 2010. Frequent hepatitis B virus rebound among HIV-hepatitis B virus-coinfected patients following antiretroviral therapy interruption. AIDS 24: 857–865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Dumoulin FL, et al. 2003. Hepatitis C virus NS2 protein inhibits gene expression from different cellular and viral promoters in hepatic and nonhepatic cell lines. Virology 305: 260–266 [DOI] [PubMed] [Google Scholar]
- 72. Dunsford HA, Sell S, Chisari FV. 1990. Hepatocarcinogenesis due to chronic liver cell injury in hepatitis B virus transgenic mice. Cancer Res. 50: 3400–3407 [PubMed] [Google Scholar]
- 73. el-Sayed HF, Abaza SM, Mehanna S, Winch PJ. 1997. The prevalence of hepatitis B and C infections among immigrants to a newly reclaimed area endemic for Schistosoma mansoni in Sinai, Egypt. Acta Trop. 68: 229–237 [DOI] [PubMed] [Google Scholar]
- 74. El-Zayadi AR, et al. 2008. Anti-HBc screening in Egyptian blood donors reduces the risk of hepatitis B virus transmission. Transfus. Med. 18: 55–61 [DOI] [PubMed] [Google Scholar]
- 75. Eyre NS, et al. 2009. Hepatitis B virus and hepatitis C virus interaction in Huh-7 cells. J. Hepatol. 51: 446–457 [DOI] [PubMed] [Google Scholar]
- 76. Fabris P, et al. 2004. Occult hepatitis B virus infection does not affect liver histology or response to therapy with interferon alpha and ribavirin in intravenous drug users with chronic hepatitis C. J. Clin. Virol. 29: 160–166 [DOI] [PubMed] [Google Scholar]
- 77. Fabrizi F, Messa P, Martin P. 2008. Hepatitis B virus infection and the dialysis patient. Semin. Dial. 21: 440–446 [DOI] [PubMed] [Google Scholar]
- 78. Faktor O, Shaul Y. 1990. The identification of hepatitis B virus X gene responsive elements reveals functional similarity of X and HTLV-I tax. Oncogene 5: 867–872 [PubMed] [Google Scholar]
- 79. Fan YF, et al. 2001. Prevalence and significance of hepatitis B virus (HBV) pre-S mutants in serum and liver at different replicative stages of chronic HBV infection. Hepatology 33: 277–286 [DOI] [PubMed] [Google Scholar]
- 80. Fang Y, et al. 2009. Molecular characterization and functional analysis of occult hepatitis B virus infection in Chinese patients infected with genotype C. J. Med. Virol. 81: 826–835 [DOI] [PubMed] [Google Scholar]
- 81. Fattovich G, et al. 1991. Hepatitis C virus infection in chronic hepatitis B virus carriers. J. Infect. Dis. 163: 400–402 [DOI] [PubMed] [Google Scholar]
- 82. Fattovich G, Stroffolini T, Zagni I, Donato F. 2004. Hepatocellular carcinoma in cirrhosis: incidence and risk factors. Gastroenterology 127: S35–S50 [DOI] [PubMed] [Google Scholar]
- 83. Fong TL, Di Bisceglie AM, Waggoner JG, Banks SM, Hoofnagle JH. 1991. The significance of antibody to hepatitis C virus in patients with chronic hepatitis B. Hepatology 14: 64–67 [DOI] [PubMed] [Google Scholar]
- 84. Forgues M, et al. 2003. Involvement of Crm1 in hepatitis B virus X protein-induced aberrant centriole replication and abnormal mitotic spindles. Mol. Cell. Biol. 23: 5282–5292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Fukuda R, et al. 1999. Serologically silent hepatitis B virus coinfection in patients with hepatitis C virus-associated chronic liver disease: clinical and virological significance. J. Med. Virol. 58: 201–207 [DOI] [PubMed] [Google Scholar]
- 86. Fukuda R, et al. 2001. Coinfection by serologically-silent hepatitis B virus may contribute to poor interferon response in patients with chronic hepatitis C by down-regulation of type-I interferon receptor gene expression in the liver. J. Med. Virol. 63: 220–227 [DOI] [PubMed] [Google Scholar]
- 87. Fulford KW, Dane DS, Catterall RD, Woof R, Denning JV. 1973. Australia antigen and antibody among patients attending a clinic for sexually transmitted diseases. Lancet i: 1470–1473 [DOI] [PubMed] [Google Scholar]
- 88. Gaillard RK, et al. 2002. Kinetic analysis of wild-type and YMDD mutant hepatitis B virus polymerases and effects of deoxyribonucleotide concentrations on polymerase activity. Antimicrob. Agents Chemother. 46: 1005–1013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Ganem D, Prince AM. 2004. Hepatitis B virus infection—natural history and clinical consequences. N. Engl. J. Med. 350: 1118–1129 [DOI] [PubMed] [Google Scholar]
- 90. Garcia AD, Ostapchuk P, Hearing P. 1993. Functional interaction of nuclear factors EF-C, HNF-4, and RXR alpha with hepatitis B virus enhancer I. J. Virol. 67: 3940–3950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Georgiadou SP, et al. 2004. Occult hepatitis B virus infection in Greek patients with chronic hepatitis C and in patients with diverse nonviral hepatic diseases. J. Viral Hepat. 11: 358–365 [DOI] [PubMed] [Google Scholar]
- 92. Ghany MG, et al. 1998. Hepatitis B virus S mutants in liver transplant recipients who were reinfected despite hepatitis B immune globulin prophylaxis. Hepatology 27: 213–222 [DOI] [PubMed] [Google Scholar]
- 93. Ghisetti V, et al. 2004. Occult hepatitis B virus infection in HBsAg negative patients undergoing liver transplantation: clinical significance. Liver Transpl. 10: 356–362 [DOI] [PubMed] [Google Scholar]
- 94. Glebe D, et al. 2009. Correlation of virus and host response markers with circulating immune complexes during acute and chronic woodchuck hepatitis virus infection. J. Virol. 83: 1579–1591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Gong Q, et al. 2011. Chromosome remodeling related to hepatitis B virus replication in HepG2 cells. DNA Cell Biol. 30: 347–354 [DOI] [PubMed] [Google Scholar]
- 96. Goral V, Ozkul H, Tekes S, Sit D, Kadiroglu AK. 2006. Prevalence of occult HBV infection in haemodialysis patients with chronic HCV. World J. Gastroenterol. 12: 3420–3424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Grandjacques C, et al. 2000. Rapid detection of genotypes and mutations in the pre-core promoter and the pre-core region of hepatitis B virus genome: correlation with viral persistence and disease severity. J. Hepatol. 33: 430–439 [DOI] [PubMed] [Google Scholar]
- 98. Guidotti LG, et al. 1999. Viral clearance without destruction of infected cells during acute HBV infection. Science 284: 825–829 [DOI] [PubMed] [Google Scholar]
- 99. Gujar SA, Michalak TI. 2009. Primary occult hepadnavirus infection induces virus-specific T-cell and aberrant cytokine responses in the absence of antiviral antibody reactivity in the woodchuck model of hepatitis B virus infection. J. Virol. 83: 3861–3876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Guo X, et al. 2011. Strong influence of human leukocyte antigen (HLA)-DP gene variants on development of persistent chronic hepatitis B virus carriers in the han Chinese population. Hepatology 53: 422–428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Guo Y, Li Y, Mu S, Zhang J, Yan Z. 2009. Evidence that methylation of hepatitis B virus covalently closed circular DNA in liver tissues of patients with chronic hepatitis B modulates HBV replication. J. Med. Virol. 81: 1177–1183 [DOI] [PubMed] [Google Scholar]
- 102. Gupta RC, Kohler PF. 1984. Identification of HBsAg determinants in immune complexes from hepatitis B virus-associated vasculitis. J. Immunol. 132: 1223–1228 [PubMed] [Google Scholar]
- 103. Gupta S, Singh S. 2010. Occult hepatitis B virus infection in ART-naive HIV-infected patients seen at a tertiary care centre in north India. BMC Infect. Dis. 10: 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Gust ID. 1996. Epidemiology of hepatitis B infection in the Western Pacific and South East Asia. Gut 38(Suppl 2): S18–S23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Hadziyannis SJ, Lieberman HM, Karvountzis GG, Shafritz DA. 1983. Analysis of liver disease, nuclear HBcAg, viral replication, and hepatitis B virus DNA in liver and serum of HBeAg vs. anti-HBe positive carriers of hepatitis B virus. Hepatology 3: 656–662 [DOI] [PubMed] [Google Scholar]
- 106. Harpaz R, et al. 1996. Transmission of hepatitis B virus to multiple patients from a surgeon without evidence of inadequate infection control. N. Engl. J. Med. 334: 549–554 [DOI] [PubMed] [Google Scholar]
- 107. Hass M, et al. 2005. Functional analysis of hepatitis B virus reactivating in hepatitis B surface antigen-negative individuals. Hepatology 42: 93–103 [DOI] [PubMed] [Google Scholar]
- 108. Hassan ZK, Hafez MM, Mansor TM, Zekri AR. 2011. Occult HBV infection among Egyptian hepatocellular carcinoma patients. Virol. J. 8: 90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Hassanshahi G, Arababadi MK, Khoramdelazad H, Yaghini N, Zarandi ER. 2010. Assessment of CXCL12 (SDF-1alpha) polymorphisms and its serum level in posttransfusion occult HBV-infected patients in Southeastern Iran. Arch. Med. Res. 41: 338–342 [DOI] [PubMed] [Google Scholar]
- 110. Hayashi N, Mita E. 1999. Involvement of Fas system-mediated apoptosis in pathogenesis of viral hepatitis. J. Viral Hepat. 6: 357–365 [DOI] [PubMed] [Google Scholar]
- 111. Hennig H, et al. 2002. Frequency and load of hepatitis B virus DNA in first-time blood donors with antibodies to hepatitis B core antigen. Blood 100: 2637–2641 [DOI] [PubMed] [Google Scholar]
- 112. Hirsch RC, Lavine JE, Chang LJ, Varmus HE, Ganem D. 1990. Polymerase gene products of hepatitis B viruses are required for genomic RNA packaging as well as for reverse transcription. Nature 344: 552–555 [DOI] [PubMed] [Google Scholar]
- 113. Hofer M, Joller-Jemelka HI, Grob PJ, Luthy R, Opravil M. 1998. Frequent chronic hepatitis B virus infection in HIV-infected patients positive for antibody to hepatitis B core antigen only. Swiss HIV Cohort Study. Eur. J. Clin. Microbiol. Infect. Dis. 17: 6–13 [DOI] [PubMed] [Google Scholar]
- 114. Holmes RK, Koning FA, Bishop KN, Malim MH. 2007. APOBEC3F can inhibit the accumulation of HIV-1 reverse transcription products in the absence of hypermutation. Comparisons with APOBEC3G. J. Biol. Chem. 282: 2587–2595 [DOI] [PubMed] [Google Scholar]
- 115. Holmes RK, Malim MH, Bishop KN. 2007. APOBEC-mediated viral restriction: not simply editing? Trends Biochem. Sci. 32: 118–128 [DOI] [PubMed] [Google Scholar]
- 116. Honarkar Z, Alavian SM, Samiee S, Saeedfar K, Zali MR. 2005. Occult hepatitis B among chronic liver disease patients. Saudi Med. J. 26: 601–606 [PubMed] [Google Scholar]
- 117. Hoofnagle JH. 2009. Reactivation of hepatitis B. Hepatology 49: S156–S165 [DOI] [PubMed] [Google Scholar]
- 118. Hourfar MK, et al. 2009. Sensitivity and specificity of anti-HBc screening assays—which assay is best for blood donor screening? Int. J. Lab Hematol. 31: 649–656 [DOI] [PubMed] [Google Scholar]
- 119. Hsu YS, et al. 2002. Long-term outcome after spontaneous HBeAg seroconversion in patients with chronic hepatitis B. Hepatology 35: 1522–1527 [DOI] [PubMed] [Google Scholar]
- 120. Huang YW, et al. 2010. Vitamin D receptor gene polymorphisms and distinct clinical phenotypes of hepatitis B carriers in Taiwan. Genes Immun. 11: 87–93 [DOI] [PubMed] [Google Scholar]
- 121. Huang ZM, Yen TS. 1993. Dysregulated surface gene expression from disrupted hepatitis B virus genomes. J. Virol. 67: 7032–7040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Hui CK, et al. 2007. Natural history and disease progression in Chinese chronic hepatitis B patients in immune-tolerant phase. Hepatology 46: 395–401 [DOI] [PubMed] [Google Scholar]
- 123. Hui CK, et al. 2006. Kinetics and risk of de novo hepatitis B infection in HBsAg-negative patients undergoing cytotoxic chemotherapy. Gastroenterology 131: 59–68 [DOI] [PubMed] [Google Scholar]
- 124. Ireland JH, et al. 2000. Reactivity of 13 in vitro expressed hepatitis B surface antigen variants in 7 commercial diagnostic assays. Hepatology 31: 1176–1182 [DOI] [PubMed] [Google Scholar]
- 125. Jackson BR, Busch MP, Stramer SL, AuBuchon JP. 2003. The cost-effectiveness of NAT for HIV, HCV, and HBV in whole-blood donations. Transfusion 43: 721–729 [DOI] [PubMed] [Google Scholar]
- 126. Kann M, Schmitz A, Rabe B. 2007. Intracellular transport of hepatitis B virus. World J. Gastroenterol. 13: 39–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Kannangai R, et al. 2007. Liver enzyme flares and occult hepatitis B in persons with chronic hepatitis C infection. J. Clin. Virol. 39: 101–105 [DOI] [PubMed] [Google Scholar]
- 128. Kao JH, Chen PJ, Lai MY, Chen DS. 2002. Occult hepatitis B virus infection and clinical outcomes of patients with chronic hepatitis C. J. Clin. Microbiol. 40: 4068–4071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Katsoulidou A, et al. 2009. Molecular characterization of occult hepatitis B cases in Greek blood donors. J. Med. Virol. 81: 815–825 [DOI] [PubMed] [Google Scholar]
- 130. Kaur P, et al. 2010. DNA methylation of hepatitis B virus (HBV) genome associated with the development of hepatocellular carcinoma and occult HBV infection. J. Infect. Dis. 202: 700–704 [DOI] [PubMed] [Google Scholar]
- 131. Kawai S, Yokosuka O, Imazeki F, Maru Y, Saisho H. 2001. State of HBV DNA in HBsAg-negative, anti-HCV-positive hepatocellular carcinoma: existence of HBV DNA possibly as nonintegrated form with analysis by Alu-HBV DNA PCR and conventional HBV PCR. J. Med. Virol. 64: 410–418 [DOI] [PubMed] [Google Scholar]
- 132. Kazemi-Shirazi L, Petermann D, Muller C. 2000. Hepatitis B virus DNA in sera and liver tissue of HBsAg negative patients with chronic hepatitis C. J. Hepatol. 33: 785–790 [DOI] [PubMed] [Google Scholar]
- 133. Khattab E, et al. 2005. Analysis of HCV co-infection with occult hepatitis B virus in patients undergoing IFN therapy. J. Clin. Virol. 33: 150–157 [DOI] [PubMed] [Google Scholar]
- 134. Kidd-Ljunggren K, Miyakawa Y, Kidd AH. 2002. Genetic variability in hepatitis B viruses. J. Gen. Virol. 83: 1267–1280 [DOI] [PubMed] [Google Scholar]
- 135. Kim JW, et al. 2011. Replicative activity of hepatitis B virus is negatively associated with methylation of covalently closed circular DNA in advanced hepatitis B virus infection. Intervirology 54: 316–325 [DOI] [PubMed] [Google Scholar]
- 136. Kim YJ, et al. 2003. Association of TNF-alpha promoter polymorphisms with the clearance of hepatitis B virus infection. Hum. Mol. Genet. 12: 2541–2546 [DOI] [PubMed] [Google Scholar]
- 137. Kimbi GC, Kramvis A, Kew MC. 2005. Integration of hepatitis B virus DNA into chromosomal DNA during acute hepatitis B. World J. Gastroenterol. 11: 6416–6421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Kohler H, Arnold W, Renschin G, Dormeyer HH, Meyer zum Buschenfelde KH. 1984. Active hepatitis B vaccination of dialysis patients and medical staff. Kidney Int. 25: 124–128 [DOI] [PubMed] [Google Scholar]
- 139. Kong J, Grando SA, Li YC. 2006. Regulation of IL-1 family cytokines IL-1alpha, IL-1 receptor antagonist, and IL-18 by 1,25-dihydroxy-vitamin D3 in primary keratinocytes. J. Immunol. 176: 3780–3787 [DOI] [PubMed] [Google Scholar]
- 140. Kramvis A, et al. 2008. Relationship of serological subtype, basic core promoter and precore mutations to genotypes/subgenotypes of hepatitis B virus. J. Med. Virol. 80: 27–46 [DOI] [PubMed] [Google Scholar]
- 141. Kuhns MC, Busch MP. 2006. New strategies for blood donor screening for hepatitis B virus: nucleic acid testing versus immunoassay methods. Mol. Diagn. Ther. 10: 77–91 [DOI] [PubMed] [Google Scholar]
- 142. Kumar M, et al. 2007. Risk factors analysis for hepatocellular carcinoma in patients with and without cirrhosis: a case-control study of 213 hepatocellular carcinoma patients from India. J. Gastroenterol. Hepatol. 22: 1104–1111 [DOI] [PubMed] [Google Scholar]
- 143. Kuo TC, Chao CC. 2010. Hepatitis B virus X protein prevents apoptosis of hepatocellular carcinoma cells by upregulating SATB1 and HURP expression. Biochem. Pharmacol. 80: 1093–1102 [DOI] [PubMed] [Google Scholar]
- 144. Kusakabe A, et al. 2007. A weak association between occult HBV infection and non-B non-C hepatocellular carcinoma in Japan. J. Gastroenterol. 42: 298–305 [DOI] [PubMed] [Google Scholar]
- 145. Lai FM, Tam JS, Li PK, Lai KN. 1989. Replication of hepatitis B virus with corticosteroid therapy in hepatitis B virus related membranous nephropathy. Virchows Arch. A Pathol. Anat. Histopathol. 414: 279–284 [DOI] [PubMed] [Google Scholar]
- 146. Lama JR, et al. 2010. Hepatitis B infection and association with other sexually transmitted infections among men who have sex with men in Peru. Am. J. Trop. Med. Hyg. 83: 194–200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. La'ulu SL, Roberts WL. 2006. The analytic sensitivity and mutant detection capability of six hepatitis B surface antigen assays. Am. J. Clin. Pathol. 125: 748–751 [DOI] [PubMed] [Google Scholar]
- 148. Launay O, et al. 2011. High levels of serum hepatitis B virus DNA in patients with ‘anti-HBc alone’: role of HBsAg mutants. J. Viral Hepat. 18: 721–729 [DOI] [PubMed] [Google Scholar]
- 149. Lavanchy D. 2004. Hepatitis B virus epidemiology, disease burden, treatment, and current and emerging prevention and control measures. J. Viral Hepat. 11: 97–107 [DOI] [PubMed] [Google Scholar]
- 150. Lee JO, et al. 2005. Hepatitis B virus X protein represses E-cadherin expression via activation of DNA methyltransferase 1. Oncogene 24: 6617–6625 [DOI] [PubMed] [Google Scholar]
- 151. Lee WM. 1997. Hepatitis B virus infection. N. Engl. J. Med. 337: 1733–1745 [DOI] [PubMed] [Google Scholar]
- 152. Lee YH, Yun Y. 1998. HBx protein of hepatitis B virus activates Jak1-STAT signaling. J. Biol. Chem. 273: 25510–25515 [DOI] [PubMed] [Google Scholar]
- 153. Le Mire MF, Miller DS, Foster WK, Burrell CJ, Jilbert AR. 2005. Covalently closed circular DNA is the predominant form of duck hepatitis B virus DNA that persists following transient infection. J. Virol. 79: 12242–12252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Levicnik-Stezinar S, Rahne-Potokar U, Candotti D, Lelie N, Allain JP. 2008. Anti-HBs positive occult hepatitis B virus carrier blood infectious in two transfusion recipients. J. Hepatol. 48: 1022–1025 [DOI] [PubMed] [Google Scholar]
- 155. Leyva A, Bernal MC, Piedrola G, Maroto MC. 1988. A study of the evolution of specific and non-specific immune complexes in acute hepatitis B and chronic hepatitis. J. Med. Microbiol. 26: 237–239 [DOI] [PubMed] [Google Scholar]
- 156. Liang TJ, Hasegawa K, Rimon N, Wands JR, Ben-Porath E. 1991. A hepatitis B virus mutant associated with an epidemic of fulminant hepatitis. N. Engl. J. Med. 324: 1705–1709 [DOI] [PubMed] [Google Scholar]
- 157. Liaw YF. 1995. Role of hepatitis C virus in dual and triple hepatitis virus infection. Hepatology 22: 1101–1108 [DOI] [PubMed] [Google Scholar]
- 158. Liaw YF, Tai DI, Chu CM, Chen TJ. 1988. The development of cirrhosis in patients with chronic type B hepatitis: a prospective study. Hepatology 8: 493–496 [DOI] [PubMed] [Google Scholar]
- 159. Libbrecht E, Doutreloigne J, Ve, et al. 2007. Evolution of primary and compensatory lamivudine resistance mutations in chronic hepatitis B virus-infected patients during long-term lamivudine treatment, assessed by a line probe assay. J. Clin. Microbiol. 45: 3935–3941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Lin CL, et al. 2005. Application of hepatitis B virus genotyping and phylogenetic analysis in intrafamilial transmission of hepatitis B virus. Clin. Infect. Dis. 41: 1576–1581 [DOI] [PubMed] [Google Scholar]
- 161. Lindh M, Hannoun C, Dhillon AP, Norkrans G, Horal P. 1999. Core promoter mutations and genotypes in relation to viral replication and liver damage in East Asian hepatitis B virus carriers. J. Infect. Dis. 179: 775–782 [DOI] [PubMed] [Google Scholar]
- 162. Lindh M, Horal P, Norkrans G. 2000. Acute hepatitis B in Western Sweden—genotypes and transmission routes. Infection 28: 161–163 [DOI] [PubMed] [Google Scholar]
- 163. Lisker-Melman M, et al. 1989. Glomerulonephritis caused by chronic hepatitis B virus infection: treatment with recombinant human alpha-interferon. Ann. Intern. Med. 111: 479–483 [DOI] [PubMed] [Google Scholar]
- 164. Liu H, et al. 2010. Hepatitis B virus X protein upregulates transcriptional activation of human telomerase reverse transcriptase. Virus Genes 40: 174–182 [DOI] [PubMed] [Google Scholar]
- 165. Lledo JL, Fernandez C, Gutierrez ML, Ocana S. 2011. Management of occult hepatitis B virus infection: an update for the clinician. World J. Gastroenterol. 17: 1563–1568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Lo YM, et al. 1993. Geographical variation in prevalence of hepatitis B virus DNA in HBsAg negative patients. J. Clin. Pathol. 46: 304–308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Locarnini S, McMillan J, Bartholomeusz A. 2003. The hepatitis B virus and common mutants. Semin. Liver Dis. 23: 5–20 [DOI] [PubMed] [Google Scholar]
- 168. Lok AS, et al. 1991. Reactivation of hepatitis B virus replication in patients receiving cytotoxic therapy. Report of a prospective study. Gastroenterology 100: 182–188 [DOI] [PubMed] [Google Scholar]
- 169. Lo Re V, III, et al. 2007. Prevalence, risk factors, and outcomes for occult hepatitis B virus infection among HIV-infected patients. J. Acquir. Immune Defic. Syndr. 44: 315–320 [DOI] [PubMed] [Google Scholar]
- 170. Lukhwareni A, Burnett RJ, Selabe SG, Mzileni MO, Mphahlele MJ. 2009. Increased detection of HBV DNA in HBsAg-positive and HBsAg-negative South African HIV/AIDS patients enrolling for highly active antiretroviral therapy at a Tertiary Hospital. J. Med. Virol. 81: 406–412 [DOI] [PubMed] [Google Scholar]
- 171. Madalinski K, Burczynska B, Heermann KH, Uy A, Gerlich WH. 1991. Analysis of viral proteins in circulating immune complexes from chronic carriers of hepatitis B virus. Clin. Exp. Immunol. 84: 493–500 [PMC free article] [PubMed] [Google Scholar]
- 172. Mahoney FJ. 1999. Update on diagnosis, management, and prevention of hepatitis B virus infection. Clin. Microbiol. Rev. 12: 351–366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Maini MK, et al. 1999. Direct ex vivo analysis of hepatitis B virus-specific CD8(+) T cells associated with the control of infection. Gastroenterology 117: 1386–1396 [DOI] [PubMed] [Google Scholar]
- 174. Manzano-Alonso ML, Castellano-Tortajada G. 2011. Reactivation of hepatitis B virus infection after cytotoxic chemotherapy or immunosuppressive therapy. World J. Gastroenterol. 17: 1531–1537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Martin CM, et al. 2009. Cytokine expression during chronic versus occult hepatitis B virus infection in HIV co-infected individuals. Cytokine 47: 194–198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Matsubara K, Tokino T. 1990. Integration of hepatitis B virus DNA and its implications for hepatocarcinogenesis. Mol. Biol. Med. 7: 243–260 [PubMed] [Google Scholar]
- 177. Matsuoka S, et al. 2008. Influence of occult hepatitis B virus coinfection on the incidence of fibrosis and hepatocellular carcinoma in chronic hepatitis C. Intervirology 51: 352–361 [DOI] [PubMed] [Google Scholar]
- 178. Matsuzaki Y, et al. 1997. HBV genome integration and genetic instability in HBsAg-negative and anti-HCV-positive hepatocellular carcinoma in Japan. Cancer Lett. 119: 53–61 [DOI] [PubMed] [Google Scholar]
- 179. McClary H, Koch R, Chisari FV, Guidotti LG. 2000. Inhibition of hepatitis B virus replication during schistosoma mansoni infection in transgenic mice. J. Exp. Med. 192: 289–294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. McMahon BJ. 2009. The natural history of chronic hepatitis B virus infection. Hepatology 49: S45–55 [DOI] [PubMed] [Google Scholar]
- 181. McMahon BJ, Holck P, Bulkow L, Snowball M. 2001. Serologic and clinical outcomes of 1536 Alaska Natives chronically infected with hepatitis B virus. Ann. Intern. Med. 135: 759–768 [DOI] [PubMed] [Google Scholar]
- 182. McMahon BJ, et al. 1985. Acute hepatitis B virus infection: relation of age to the clinical expression of disease and subsequent development of the carrier state. J. Infect. Dis. 151: 599–603 [DOI] [PubMed] [Google Scholar]
- 183. Melegari M, Bruno S, Wands JR. 1994. Properties of hepatitis B virus pre-S1 deletion mutants. Virology 199: 292–300 [DOI] [PubMed] [Google Scholar]
- 184. Meuleman P, et al. 2006. Immune suppression uncovers endogenous cytopathic effects of the hepatitis B virus. J. Virol. 80: 2797–2807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. Michalak TI, Pasquinelli C, Guilhot S, Chisari FV. 1994. Hepatitis B virus persistence after recovery from acute viral hepatitis. J. Clin. Invest. 93: 230–239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Miller RH, Robinson WS. 1983. Integrated hepatitis B virus DNA sequences specifying the major viral core polypeptide are methylated in PLC/PRF/5 cells. Proc. Natl. Acad. Sci. U. S. A. 80: 2534–2538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187. Minuk GY, et al. 2005. Occult hepatitis B virus infection in a North American community-based population. J. Hepatol. 42: 480–485 [DOI] [PubMed] [Google Scholar]
- 188. Momosaki S, Nakashima Y, Kojiro M, Tabor E. 2005. HBsAg-negative hepatitis B virus infections in hepatitis C virus-associated hepatocellular carcinoma. J. Viral Hepat. 12: 325–329 [DOI] [PubMed] [Google Scholar]
- 189. Moolla N, Kew M, Arbuthnot P. 2002. Regulatory elements of hepatitis B virus transcription. J. Viral Hepat. 9: 323–331 [DOI] [PubMed] [Google Scholar]
- 190. Mosley JW, et al. 1995. Donor screening for antibody to hepatitis B core antigen and hepatitis B virus infection in transfusion recipients. Transfusion 35: 5–12 [DOI] [PubMed] [Google Scholar]
- 191. Mrani S, et al. 2007. Occult HBV infection may represent a major risk factor of non-response to antiviral therapy of chronic hepatitis C. J. Med. Virol. 79: 1075–1081 [DOI] [PubMed] [Google Scholar]
- 192. Murakami Y, et al. 2005. Large scaled analysis of hepatitis B virus (HBV) DNA integration in HBV related hepatocellular carcinomas. Gut 54: 1162–1168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Murakami Y, Minami M, Daimon Y, Okanoue T. 2004. Hepatitis B virus DNA in liver, serum, and peripheral blood mononuclear cells after the clearance of serum hepatitis B virus surface antigen. J. Med. Virol. 72: 203–214 [DOI] [PubMed] [Google Scholar]
- 194. Murata M, et al. 2009. Hepatitis B virus X protein shifts human hepatic transforming growth factor (TGF)-beta signaling from tumor suppression to oncogenesis in early chronic hepatitis B. Hepatology 49: 1203–1217 [DOI] [PubMed] [Google Scholar]
- 195. Nakatake H, Chisaka O, Yamamoto S, Matsubara K, Koshy R. 1993. Effect of X protein on transactivation of hepatitis B virus promoters and on viral replication. Virology 195: 305–314 [DOI] [PubMed] [Google Scholar]
- 196. Navaratnam N, et al. 1993. The p27 catalytic subunit of the apolipoprotein B mRNA editing enzyme is a cytidine deaminase. J. Biol. Chem. 268: 20709–20712 [PubMed] [Google Scholar]
- 197. Neau D, et al. 2005. Occult hepatitis B virus infection in HIV-infected patients with isolated antibodies to hepatitis B core antigen: Aquitaine cohort, 2002–2003. Clin. Infect. Dis. 40: 750–753 [DOI] [PubMed] [Google Scholar]
- 198. Neddermann P, et al. 1997. The nonstructural proteins of the hepatitis C virus: structure and functions. Biol. Chem. 378: 469–476 [PubMed] [Google Scholar]
- 199. Neumann AU, et al. 2010. Novel mechanism of antibodies to hepatitis B virus in blocking viral particle release from cells. Hepatology 52: 875–885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200. Neurath AR, Kent SB, Strick N, Parker K. 1986. Identification and chemical synthesis of a host cell receptor binding site on hepatitis B virus. Cell 46: 429–436 [DOI] [PubMed] [Google Scholar]
- 201. Newbold JE, et al. 1995. The covalently closed duplex form of the hepadnavirus genome exists in situ as a heterogeneous population of viral minichromosomes. J. Virol. 69: 3350–3357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Nguyen DH, Hu J. 2008. Reverse transcriptase- and RNA packaging signal-dependent incorporation of APOBEC3G into hepatitis B virus nucleocapsids. J. Virol. 82: 6852–6861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Nguyen DH, Gummuluru S, Hu J. 2007. Deamination-independent inhibition of hepatitis B virus reverse transcription by APOBEC3G. J. Virol. 81: 4465–4472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204. Noguchi C, et al. 2005. G to A hypermutation of hepatitis B virus. Hepatology 41: 626–633 [DOI] [PubMed] [Google Scholar]
- 205. Noguchi C, et al. 2009. G-to-A hypermutation in hepatitis B virus (HBV) and clinical course of patients with chronic HBV infection. J. Infect. Dis. 199: 1599–1607 [DOI] [PubMed] [Google Scholar]
- 206. Noguchi C, et al. 2007. Dual effect of APOBEC3G on hepatitis B virus. J. Gen. Virol. 88: 432–440 [DOI] [PubMed] [Google Scholar]
- 207. Norder H, et al. 1993. Genetic relatedness of hepatitis B viral strains of diverse geographical origin and natural variations in the primary structure of the surface antigen. J. Gen. Virol. 74: 1341–1348 [DOI] [PubMed] [Google Scholar]
- 208. Ocana S, Casas ML, Buhigas I, Lledo JL. 2011. Diagnostic strategy for occult hepatitis B virus infection. World J. Gastroenterol. 17: 1553–1557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209. Okuda K. 2000. Hepatocellular carcinoma. J. Hepatol. 32: 225–237 [DOI] [PubMed] [Google Scholar]
- 210. Oon CJ, et al. 1995. Molecular epidemiology of hepatitis B virus vaccine variants in Singapore. Vaccine 13: 699–702 [DOI] [PubMed] [Google Scholar]
- 211. Park IY, et al. 2007. Aberrant epigenetic modifications in hepatocarcinogenesis induced by hepatitis B virus X protein. Gastroenterology 132: 1476–1494 [DOI] [PubMed] [Google Scholar]
- 212. Paterlini-Brechot P, et al. 2003. Hepatitis B virus-related insertional mutagenesis occurs frequently in human liver cancers and recurrently targets human telomerase gene. Oncogene 22: 3911–3916 [DOI] [PubMed] [Google Scholar]
- 213. Pernice W, Sodomann CP, Luben G, Seiler FR, Sedlacek HH. 1979. Antigen-specific detection of HBsAG-containing immune complexes in the course of hepatitis B virus infection. Clin. Exp. Immunol. 37: 376–380 [PMC free article] [PubMed] [Google Scholar]
- 214. Pollicino T, et al. 2004. Hepatitis B virus maintains its pro-oncogenic properties in the case of occult HBV infection. Gastroenterology 126: 102–110 [DOI] [PubMed] [Google Scholar]
- 215. Pollicino T, et al. 2006. Hepatitis B virus replication is regulated by the acetylation status of hepatitis B virus cccDNA-bound H3 and H4 histones. Gastroenterology 130: 823–837 [DOI] [PubMed] [Google Scholar]
- 216. Portela A, Esteller M. 2010. Epigenetic modifications and human disease. Nat. Biotechnol. 28: 1057–1068 [DOI] [PubMed] [Google Scholar]
- 217. Qadri I, Fatima K, Abdel-Hafiz H. 2011. Hepatitis B virus X protein impedes the DNA repair via its association with transcription factor, TFIIH. BMC Microbiol. 11: 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218. Raimondo G, et al. 2008. Occult hepatitis B virus in liver tissue of individuals without hepatic disease. J. Hepatol. 48: 743–746 [DOI] [PubMed] [Google Scholar]
- 219. Raimondo G, et al. 2008. Statements from the Taormina expert meeting on occult hepatitis B virus infection. J. Hepatol. 49: 652–657 [DOI] [PubMed] [Google Scholar]
- 220. Raimondo G, et al. 1988. Interrupted replication of hepatitis B virus in liver tissue of HBsAg carriers with hepatocellular carcinoma. Virology 166: 103–112 [DOI] [PubMed] [Google Scholar]
- 221. Reaiche GY, Le Mire MF, Mason WS, Jilbert AR. 2010. The persistence in the liver of residual duck hepatitis B virus covalently closed circular DNA is not dependent upon new viral DNA synthesis. Virology 406: 286–292 [DOI] [PubMed] [Google Scholar]
- 222. Rehermann B, Ferrari C, Pasquinelli C, Chisari FV. 1996. The hepatitis B virus persists for decades after patients' recovery from acute viral hepatitis despite active maintenance of a cytotoxic T-lymphocyte response. Nat. Med. 2: 1104–1108 [DOI] [PubMed] [Google Scholar]
- 223. Roche B, et al. 1997. De novo and apparent de novo hepatitis B virus infection after liver transplantation. J. Hepatol. 26: 517–526 [DOI] [PubMed] [Google Scholar]
- 224. Rodriguez-Inigo E, et al. 2005. Hepatitis C virus (HCV) and hepatitis B virus (HBV) can coinfect the same hepatocyte in the liver of patients with chronic HCV and occult HBV infection. J. Virol. 79: 15578–15581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225. Rosler C, et al. 2005. APOBEC-mediated interference with hepadnavirus production. Hepatology 42: 301–309 [DOI] [PubMed] [Google Scholar]
- 226. Ross AG, et al. 2002. Schistosomiasis. N. Engl. J. Med. 346: 1212–1220 [DOI] [PubMed] [Google Scholar]
- 227. Rossi G, Pelizzari A, Motta M, Puoti M. 2001. Primary prophylaxis with lamivudine of hepatitis B virus reactivation in chronic HbsAg carriers with lymphoid malignancies treated with chemotherapy. Br. J. Haematol. 115: 58–62 [DOI] [PubMed] [Google Scholar]
- 228. Saito T, et al. 1999. Quantitative DNA analysis of low-level hepatitis B viremia in two patients with serologically negative chronic hepatitis B. J. Med. Virol. 58: 325–331 [DOI] [PubMed] [Google Scholar]
- 229. Sallie R, Rayner A, Naoumov N, Portmann B, Williams R. 1993. Occult HBV in NANB fulminant hepatitis. Lancet 341: 123. [DOI] [PubMed] [Google Scholar]
- 230. Sansonno DE, et al. 1986. Demonstration of HBsAg as the antigen component in circulating immune complexes detected by peg-solid phase test. J. Virol. Methods 14: 141–151 [DOI] [PubMed] [Google Scholar]
- 231. Scheiblauer H, Soboll H, Nick S. 2006. Evaluation of 17 CE-marked HBsAg assays with respect to clinical sensitivity, analytical sensitivity, and hepatitis B virus mutant detection. J. Med. Virol. 78(Suppl 1): S66–S70 [DOI] [PubMed] [Google Scholar]
- 232. Schilling R, et al. 2003. Endocytosis of hepatitis B immune globulin into hepatocytes inhibits the secretion of hepatitis B virus surface antigen and virions. J. Virol. 77: 8882–8892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233. Schmidt M, et al. 2010. Blood donor screening with cobas s 201/cobas TaqScreen MPX under routine conditions at German Red Cross institutes. Vox Sang. 98: 37–46 [DOI] [PubMed] [Google Scholar]
- 234. Schuttler CG, et al. 2002. Suppression of hepatitis B virus enhancer 1 and 2 by hepatitis C virus core protein. J. Hepatol. 37: 855–862 [DOI] [PubMed] [Google Scholar]
- 235. Selim HS, Abou-Donia HA, Taha HA, El Azab GI, Bakry AF. 2011. Role of occult hepatitis B virus in chronic hepatitis C patients with flare of liver enzymes. Eur. J. Intern. Med. 22: 187–190 [DOI] [PubMed] [Google Scholar]
- 236. Sheen IS, Liaw YF, Chu CM, Pao CC. 1992. Role of hepatitis C virus infection in spontaneous hepatitis B surface antigen clearance during chronic hepatitis B virus infection. J. Infect. Dis. 165: 831–834 [DOI] [PubMed] [Google Scholar]
- 237. Sheen IS, Liaw YF, Lin DY, Chu CM. 1994. Role of hepatitis C and delta viruses in the termination of chronic hepatitis B surface antigen carrier state: a multivariate analysis in a longitudinal follow-up study. J. Infect. Dis. 170: 358–361 [DOI] [PubMed] [Google Scholar]
- 238. Shetty K, Hussain M, Nei L, Reddy KR, Lok AS. 2008. Prevalence and significance of occult hepatitis B in a liver transplant population with chronic hepatitis C. Liver Transpl. 14: 534–540 [DOI] [PubMed] [Google Scholar]
- 239. Shih CM, Chen CM, Chen SY, Lee YH. 1995. Modulation of the trans-suppression activity of hepatitis C virus core protein by phosphorylation. J. Virol. 69: 1160–1171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240. Shikata T, et al. 1977. Hepatitis B e antigen and infectivity of hepatitis B virus. J. Infect. Dis. 136: 571–576 [DOI] [PubMed] [Google Scholar]
- 241. Silva C, Jr, et al. 2004. The influence of occult infection with hepatitis B virus on liver histology and response to interferon treatment in chronic hepatitis C patients. Braz. J. Infect. Dis. 8: 431–439 [DOI] [PubMed] [Google Scholar]
- 242. Silva CM, et al. 2005. Low rate of occult hepatitis B virus infection among anti-HBc positive blood donors living in a low prevalence region in Brazil. J. Infect. 51: 24–29 [DOI] [PubMed] [Google Scholar]
- 243. Singh AE, et al. 2011. Factors associated with vaccine failure and vertical transmission of hepatitis B among a cohort of Canadian mothers and infants. J. Viral Hepat. 18: 468–473 [DOI] [PubMed] [Google Scholar]
- 244. Smith HM, et al. 1992. Significance of serum IgM anti-HBc in chronic hepatitis B virus infection. J. Med. Virol. 36: 16–20 [DOI] [PubMed] [Google Scholar]
- 245. Soussan P, et al. 2000. In vivo expression of a new hepatitis B virus protein encoded by a spliced RNA. J. Clin. Invest. 105: 55–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246. Soussan P, et al. 2008. Expression of defective hepatitis B virus particles derived from singly spliced RNA is related to liver disease. J. Infect. Dis. 198: 218–225 [DOI] [PubMed] [Google Scholar]
- 247. Soussan P, et al. 2003. The expression of hepatitis B spliced protein (HBSP) encoded by a spliced hepatitis B virus RNA is associated with viral replication and liver fibrosis. J. Hepatol. 38: 343–348 [DOI] [PubMed] [Google Scholar]
- 248. Spandau DF, Lee CH. 1988. trans-activation of viral enhancers by the hepatitis B virus X protein. J. Virol. 62: 427–434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249. Spijkerman IJ, et al. 2002. Transmission of hepatitis B virus from a surgeon to his patients during high-risk and low-risk surgical procedures during 4 years. Infect. Control Hosp. Epidemiol. 23: 306–312 [DOI] [PubMed] [Google Scholar]
- 250. Squadrito G, et al. 2006. Occult hepatitis B virus infection is associated with the development of hepatocellular carcinoma in chronic hepatitis C patients. Cancer 106: 1326–1330 [DOI] [PubMed] [Google Scholar]
- 251. Su Q, et al. 1998. Expression of hepatitis B virus X protein in HBV-infected human livers and hepatocellular carcinomas. Hepatology 27: 1109–1120 [DOI] [PubMed] [Google Scholar]
- 252. Suneetha PV, et al. 2006. Association between vitamin D receptor, CCR5, TNF-alpha and TNF-beta gene polymorphisms and HBV infection and severity of liver disease. J. Hepatol. 44: 856–863 [DOI] [PubMed] [Google Scholar]
- 253. Suspene R, et al. 2005. Extensive editing of both hepatitis B virus DNA strands by APOBEC3 cytidine deaminases in vitro and in vivo. Proc. Natl. Acad. Sci. U. S. A. 102: 8321–8326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254. Tamori A, et al. 2003. HBV DNA integration and HBV-transcript expression in non-B, non-C hepatocellular carcinoma in Japan. J. Med. Virol. 71: 492–498 [DOI] [PubMed] [Google Scholar]
- 255. Teng B, Burant CF, Davidson NO. 1993. Molecular cloning of an apolipoprotein B messenger RNA editing protein. Science 260: 1816–1819 [DOI] [PubMed] [Google Scholar]
- 256. Terre S, Petit MA, Brechot C. 1991. Defective hepatitis B virus particles are generated by packaging and reverse transcription of spliced viral RNAs in vivo. J. Virol. 65: 5539–5543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257. Thimme R, et al. 2003. CD8(+) T cells mediate viral clearance and disease pathogenesis during acute hepatitis B virus infection. J. Virol. 77: 68–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258. Thomas DL, et al. 1993. Viral hepatitis in health care personnel at The Johns Hopkins Hospital. The seroprevalence of and risk factors for hepatitis B virus and hepatitis C virus infection. Arch. Intern. Med. 153: 1705–1712 [PubMed] [Google Scholar]
- 259. Torbenson M, Thomas DL. 2002. Occult hepatitis B. Lancet Infect. Dis. 2: 479–486 [DOI] [PubMed] [Google Scholar]
- 260. Torbenson M, et al. 2004. High prevalence of occult hepatitis B in Baltimore injection drug users. Hepatology 39: 51–57 [DOI] [PubMed] [Google Scholar]
- 261. Torresi J, et al. 2002. Restoration of replication phenotype of lamivudine-resistant hepatitis B virus mutants by compensatory changes in the “fingers” subdomain of the viral polymerase selected as a consequence of mutations in the overlapping S gene. Virology 299: 88–99 [DOI] [PubMed] [Google Scholar]
- 262. Torresi J, et al. 2002. Reduced antigenicity of the hepatitis B virus HBsAg protein arising as a consequence of sequence changes in the overlapping polymerase gene that are selected by lamivudine therapy. Virology 293: 305–313 [DOI] [PubMed] [Google Scholar]
- 263. Trepo C, Guillevin L. 2001. Polyarteritis nodosa and extrahepatic manifestations of HBV infection: the case against autoimmune intervention in pathogenesis. J. Autoimmun. 16: 269–274 [DOI] [PubMed] [Google Scholar]
- 264. Tur-Kaspa R, Burk RD, Shaul Y, Shafritz DA. 1986. Hepatitis B virus DNA contains a glucocorticoid-responsive element. Proc. Natl. Acad. Sci. U. S. A. 83: 1627–1631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265. Turelli P, Mangeat B, Jost S, Vianin S, Trono D. 2004. Inhibition of hepatitis B virus replication by APOBEC3G. Science 303: 1829. [DOI] [PubMed] [Google Scholar]
- 266. Uchida T, et al. 1997. Hepatitis C virus is frequently coinfected with serum marker-negative hepatitis B virus: probable replication promotion of the former by the latter as demonstrated by in vitro cotransfection. J. Med. Virol. 52: 399–405 [DOI] [PubMed] [Google Scholar]
- 267. Urashima T, et al. 1997. Identification of hepatitis B virus integration in hepatitis C virus-infected hepatocellular carcinoma tissues. J. Hepatol. 26: 771–778 [DOI] [PubMed] [Google Scholar]
- 268. Valsamakis A. 2007. Molecular testing in the diagnosis and management of chronic hepatitis B. Clin. Microbiol. Rev. 20: 426–439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269. van Hemert FJ, Zaaijer HL, Berkhout B, Lukashov VV. 2008. Occult hepatitis B infection: an evolutionary scenario. Virol. J. 5: 146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270. Vartanian JP, et al. 2010. Massive APOBEC3 editing of hepatitis B viral DNA in cirrhosis. PLoS Pathog. 6: e1000928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271. Vivekanandan P, Thomas D, Torbenson M. 2008. Hepatitis B viral DNA is methylated in liver tissues. J. Viral Hepat. 15: 103–107 [DOI] [PubMed] [Google Scholar]
- 272. Vivekanandan P, Thomas D, Torbenson M. 2009. Methylation regulates hepatitis B viral protein expression. J. Infect. Dis. 199: 1286–1291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273. Vivekanandan P, Daniel HD, Kannangai R, Martinez-Murillo F, Torbenson M. 2010. Hepatitis B virus replication induces methylation of both host and viral DNA. J. Virol. 84: 4321–4329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274. Vivekanandan P, Singh OV. 2010. Molecular methods in the diagnosis and management of chronic hepatitis B. Expert Rev. Mol. Diagn. 10: 921–935 [DOI] [PubMed] [Google Scholar]
- 275. Vivekanandan P, et al. 2004. Distribution of hepatitis B virus genotypes in blood donors and chronically infected patients in a tertiary care hospital in southern India. Clin. Infect. Dis. 38: e81–e86 [DOI] [PubMed] [Google Scholar]
- 276. Vivekanandan P, et al. 2004. High frequency of the 1896 precore mutation in patients and blood donors with hepatitis B virus infection from the Indian subcontinent. Mol. Diagn. 8: 51–56 [DOI] [PubMed] [Google Scholar]
- 277. Vivekanandan P, Kannangai R, Ray SC, Thomas DL, Torbenson M. 2008. Comprehensive genetic and epigenetic analysis of occult hepatitis B from liver tissue samples. Clin. Infect. Dis. 46: 1227–1236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278. Wakil SM, et al. 2002. Prevalence and profile of mutations associated with lamivudine therapy in Indian patients with chronic hepatitis B in the surface and polymerase genes of hepatitis B virus. J. Med. Virol. 68: 311–318 [DOI] [PubMed] [Google Scholar]
- 279. Wang XW, et al. 1994. Hepatitis B virus X protein inhibits p53 sequence-specific DNA binding, transcriptional activity, and association with transcription factor ERCC3. Proc. Natl. Acad. Sci. U. S. A. 91: 2230–2234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280. Wang Z, et al. 2003. Quantitative analysis of HBV DNA level and HBeAg titer in hepatitis B surface antigen positive mothers and their babies: HBeAg passage through the placenta and the rate of decay in babies. J. Med. Virol. 71: 360–366 [DOI] [PubMed] [Google Scholar]
- 281. Weber B, et al. 2006. Evaluation of a new automated assay for hepatitis B surface antigen (HBsAg) detection VIDAS HBsAg Ultra. J. Virol. Methods 135: 109–117 [DOI] [PubMed] [Google Scholar]
- 282. Weissberg JI, et al. 1984. Survival in chronic hepatitis B. An analysis of 379 patients. Ann. Intern. Med. 101: 613–616 [DOI] [PubMed] [Google Scholar]
- 283. Wright R. 1980. Type B hepatitis: progression to chronic hepatitis. Clin. Gastroenterol. 9: 97–115 [PubMed] [Google Scholar]
- 284. Wright TL, et al. 1992. Hepatitis B virus and apparent fulminant non-A, non-B hepatitis. Lancet 339: 952–955 [DOI] [PubMed] [Google Scholar]
- 285. Wu HC, et al. 2009. Aflatoxin B1 exposure, hepatitis B virus infection, and hepatocellular carcinoma in Taiwan. Cancer Epidemiol. Biomarkers Prev. 18: 846–853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286. Xu DZ, et al. 2002. Risk factors and mechanism of transplacental transmission of hepatitis B virus: a case-control study. J. Med. Virol. 67: 20–26 [DOI] [PubMed] [Google Scholar]
- 287. Xu R, et al. 2007. Association of human APOBEC3 cytidine deaminases with the generation of hepatitis virus B x antigen mutants and hepatocellular carcinoma. Hepatology 46: 1810–1820 [DOI] [PubMed] [Google Scholar]
- 288. Xu Z, Yen TS. 1996. Intracellular retention of surface protein by a hepatitis B virus mutant that releases virion particles. J. Virol. 70: 133–140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289. Yang HI, et al. 2008. Associations between hepatitis B virus genotype and mutants and the risk of hepatocellular carcinoma. J. Natl. Cancer Inst. 100: 1134–1143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290. Yang HI, et al. 2002. Hepatitis B e antigen and the risk of hepatocellular carcinoma. N. Engl. J. Med. 347: 168–174 [DOI] [PubMed] [Google Scholar]
- 291. Yeo W, et al. 2009. Hepatitis B virus reactivation in lymphoma patients with prior resolved hepatitis B undergoing anticancer therapy with or without rituximab. J. Clin. Oncol. 27: 605–611 [DOI] [PubMed] [Google Scholar]
- 292. Yin J, et al. 2011. Association between the various mutations in viral core promoter region to different stages of hepatitis B, ranging of asymptomatic carrier state to hepatocellular carcinoma. Am. J. Gastroenterol. 106: 81–92 [DOI] [PubMed] [Google Scholar]
- 293. Yotsuyanagi H, et al. 2001. Frequent presence of HBV in the sera of HBsAg-negative, anti-HBc-positive blood donors. Transfusion 41: 1093–1099 [DOI] [PubMed] [Google Scholar]
- 294. Yu MW, et al. 2005. Hepatitis B virus genotype and DNA level and hepatocellular carcinoma: a prospective study in men. J. Natl. Cancer Inst. 97: 265–272 [DOI] [PubMed] [Google Scholar]
- 295. Yuan Q, et al. 2010. Molecular characteristics of occult hepatitis B virus from blood donors in southeast China. J. Clin. Microbiol. 48: 357–362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296. Yuen MF, et al. 2010. Prevalence of occult hepatitis B infection in a highly endemic area for chronic hepatitis B: a study of a large blood donor population. Gut 59: 1389–1393 [DOI] [PubMed] [Google Scholar]
- 297. Zerbini A, et al. 2008. The characteristics of the cell-mediated immune response identify different profiles of occult hepatitis B virus infection. Gastroenterology 134: 1470–1481 [DOI] [PubMed] [Google Scholar]
- 298. Zhang W, et al. 2008. Cytidine deaminase APOBEC3B interacts with heterogeneous nuclear ribonucleoprotein K and suppresses hepatitis B virus expression. Cell. Microbiol. 10: 112–121 [DOI] [PubMed] [Google Scholar]
- 299. Zheng X, et al. 2011. Characterization of occult hepatitis B virus infection from blood donors in China. J. Clin. Microbiol. 49: 1730–1737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300. Zoulim F, Saputelli J, Seeger C. 1994. Woodchuck hepatitis virus X protein is required for viral infection in vivo. J. Virol. 68: 2026–2030 [DOI] [PMC free article] [PubMed] [Google Scholar]