Abstract
The efflux pump AcrAB is important in the antibiotic resistance and virulence of several pathogenic bacteria. We report that deletion of the Yersinia pestis AcrAB-TolC homolog leads to increased susceptibility to diverse substrates, including, though unlike in Escherichia coli, the aminoglycosides. Neither is the Y. pestis pump affected by the efflux pump inhibitor phenylalanine-arginine beta-naphthylamide. In mouse plague models, pump deletion does not have a significant effect on tissue colonization.
TEXT
Increased activity of efflux pumps is a major route to decreased susceptibility (8, 15, 21, 22, 39, 41) in many bacteria. An important pump in active efflux is AcrAB-TolC (26, 35). TolC is located in the outer membrane and is linked to the inner membrane AcrB through AcrA, thus forming a channel from the cytoplasm to the extracellular space (25). AcrAB-TolC has an extremely broad substrate range but favors lipophilic substrates (25). Efflux pumps are also involved in the pathogenicity of several bacteria, including Pseudomonas aeruginosa, Salmonella enterica serovar Typhimurium, Vibrio cholerae, Francisella tularensis, Klebsiella pneumoniae, and the plant pathogen Erwinia amylovora (3, 27, 30); although not fully understood, the pumps could affect virulence through removal of antibacterial molecules such as bile (25), mammalian steroid hormones (7), and antimicrobial peptides (34, 37, 40) and therefore would aid survival in the host.
To explore the function of the AcrAB-TolC pump in susceptibility of Yersinia pestis to antibiotics and virulence, deletion and complemented strains were engineered using splicing by overlap extension, as described previously (11, 19), in the attenuated Y. pestis strain KIM 1001 pgm (18), a gift from John Goguen (University of Massachusetts Medical School). Sites of genetic manipulation were verified by sequencing. Growth studies showed no difference in the doubling times of the engineered strains compared with that of the wild-type (WT) strain (data not shown).
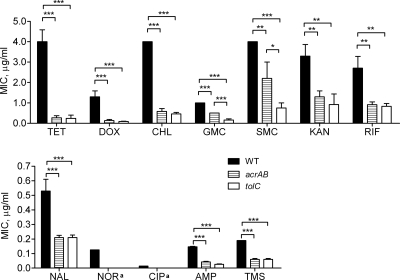
Drug susceptibility studies were carried out using Etests (AB Biodisk) against antibiotics from different classes, including antibiotics favored in plague treatment and prophylaxis (streptomycin, gentamicin, tetracycline, chloramphenicol, ciprofloxacin, and trimethoprim-sulfamethoxazole) (9). Figure 1 shows the average MIC (from at least three experiments) against selected antibiotics chosen to represent different antibiotic classes. Statistical analysis was performed using one-way analysis of variance (ANOVA) with Tukey's posttest. Deletion of acrAB increased susceptibility to all the antibiotics by 50 to 92%. tolC deletion increased susceptibility to the aminoglycosides by 52 to 66%, but not to the other drugs (9 to 23% increase in susceptibility), compared to the levels for the acrAB strain (Fig. 1; Table 1). Resistance was restored when strains were complemented with ectopically expressed acrAB or tolC (Table 1). The reason for the variation in the MICs for chloramphenicol between the two tolC strains is uncertain, but as it is only a 2-fold difference, this is within the acceptable range for MIC determination. This finding suggests that, of the efflux pumps that interact with TolC, AcrAB is the major one for antibiotic efflux, with the caveat that our results do not take into account changes in susceptibility brought about by membrane perturbation resulting from the absence of pump components. Increased susceptibility to the aminoglycosides was unexpected, as this antibiotic class is not a substrate for the Escherichia coli AcrAB-TolC pump (24), although it is a substrate for the homologous Pseudomonas aeruginosa and Klebsiella pneumoniae complexes (25, 27). A ClustalW alignment of AcrB primary sequences from E. coli, Y. pestis, and P. aeruginosa showed no obvious reason why AcrAB-TolC from Y. pestis should efflux aminoglycosides (data not shown).
Fig 1.
Drug susceptibilities of wild-type KIM 1001 pgm and acrAB and tolC deletion mutants. The data are representative of at least 3 experiments for each antibiotic. In all instances, deletion caused major increases in drug susceptibility. a, norfloxacin and ciprofloxacin MICs could not be shown for the tolC and acrAB strains, as the boundary of bacterial growth was below the lowest antibiotic concentration of the Etest strip. Asterisks denote significance as calculated by one-way ANOVA with Tukey's posttest, as follows: *, P value of 0.01 to 0.05; **, P value of 0.001 to 0.01; ***, P value of <0.001. AMP, ampicillin; CHL, chloramphenicol; CIP, ciprofloxacin; DOX, doxycycline; GMC, gentamicin; KAN, kanamycin; NAL, nalidixic acid; NOR, norfloxacin; RIF, rifampin; SMC, streptomycin; TET, tetracycline; TMS, trimethoprim-sulfamethoxazole.
Table 1.
MICs of various strains as a percentage of WT Y. pestis MIC
| Strain genotypea | % mutant MIC/WT MICb |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TET | DOX | CHL | GMC | SMC | KAN | RIF | NAL | NOR | CIP | AMP | TMS | Bile | PMB | |
| WT | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| lacZ | 100 | ND | 100 | ND | 118 | 100 | ND | ND | 88 | ND | ND | 89 | 100 | 100 |
| acrAB | 10*** | 8*** | 18*** | 50*** | 49*** | 40*** | 34*** | 36*** | NA | NA | 35*** | 29*** | <17*** | 23*** |
| acrAB lacZ::acrAB | 95 | 98 | 89 | 107 | 100 | 105 | ND | 103 | 91 | ND | ND | 84 | 100 | 100 |
| tolC | 10*** | 6*** | 16*** | 19*** | 17*** | 19*** | 31** | 25*** | NA | NA | 22*** | 29*** | ND | ND |
| tolC lacZ::kan | 10*** | 4*** | 8*** | 24*** | 16*** | R | ND | 24*** | NA | NA | ND | 25*** | <4*** | 0.1*** |
| tolC::tolC lacZ::kan | 100 | ND | 100 | ND | 88 | ND | ND | ND | 86 | ND | ND | 83 | 100 | 100 |
| tolC/acrABc | 100 (NS) | 77 (NS) | 100 (NS) | 38*** | 34*** | 48 (NS) | 91 (NS) | 71 (NS) | NA | NA | 67 (NS) | 100 (NS) | 23*** | 0.4*** |
Genes were deleted and complemented using splicing by overlap extension. In complemented strains, acrAB was inserted into the lacZ gene and tolC was inserted into the original deletion site after lacZ deletion by insertion of a kanamycin resistance gene. Boldface type denotes deletion strains.
MICs used to calculate percentages were an average of at least 3 experiments. Abbreviations: AMP, ampicillin; Bile, OxGall; CHL, chloramphenicol; CIP, ciprofloxacin; DOX, doxycycline; GMC, gentamicin; KAN, kanamycin; NAL, nalidixic acid; NOR, norfloxacin; RIF, rifampin; SMC, streptomycin; TET, tetracycline; TMS, trimethoprim-sulfamethoxazole; PMB, polymyxin B; NA, not available (the MIC was below the lowest value of 0.016 μg/ml on the Etest strip by 2 to 6 mm); ND, not determined; R, complete resistance due to kanamycin resistance gene chromosomal integration. Significance is denoted as follows: **, P value of 0.001 to 0.01; ***, P value of <0.001; NS, not significant. Boldface type denotes results for deletion strains.
tolC MIC as a percentage of the acrAB MIC.
Bacteria entering host organisms such as humans and rodents use defenses against antimicrobial peptides which are secreted by epithelial cells as part of the innate immune response and by other resident bacteria (2, 5, 12, 13, 17). We used polymyxin B (PMB), as a representative antimicrobial peptide, and determined the susceptibility of Y. pestis using plate dilution assays (14), taking the average of at least 3 experiments. The MICs for PMB of the WT (350 μg/ml), acrAB (80 μg/ml), and tolC (0.35 μg/ml) strains suggest that while PMB is a substrate for AcrAB, the dramatic increase in susceptibility with a tolC deletion (0.4% of the AcrAB MIC [Table 1]) indicates that TolC likely acts as the exit duct for other pumps associated with PMB efflux. In E. coli, the PMB MIC is far lower (0.03 μg/ml) and only 50% lower than that of the WT for both the acrAB and the tolC deletion mutants (40). As for the antibiotic MICs, these findings suggest that the related pumps of different bacterial species may have different substrate affinities.
Enteric pathogens must survive passage through bile in the small intestine. Bile is a substrate of AcrAB-TolC in E. coli, V. cholerae, F. tularensis, and S. enterica (3, 6, 23, 36). We used plate dilution assays (14) with OxGall (Sigma) to determine the MICs of Y. pestis WT, acrAB, and tolC strains as >9 mg/ml, 1.5 mg/ml, and 0.35 mg/ml, respectively. As for PMB, these findings show that Y. pestis AcrAB is not the only bile efflux pump, as the tolC deletion mutant causes a further increase in susceptibility. In contrast to PMB, this finding compares well with the E. coli TolC pumps, where bile salts are the substrates of several pumps as well as AcrAB-TolC and deletion of tolC increases susceptibility above that of the acrB or acrAB deletion strains (35).
It has been shown that deletion of tolC results in an increase in the levels or activity of the transcriptional regulators MarA, SoxS, and Rob (32). Porins are among the many genes that are regulated by these transcription factors (1, 31). It is highly probable that the loss of AcrAB-TolC induces changes in membrane permeability beyond simply loss of efflux which may also affect susceptibility.
Multidrug-resistant clinical strains show a high frequency of mutations in efflux pump genes (8, 15, 21, 22, 39, 41). Dual therapy involving treatment with an antibiotic and an efflux pump inhibitor (EPI) is proposed as a way to restore the efficacy of the antibiotic in resistant strains. We used the broad-spectrum EPI phenylalanine-arginine β-naphthylamide (PAβN), a potentiator of susceptibility to chloramphenicol, tetracycline, macrolides, fluoroquinolones, and aminoglycosides (4, 10, 16), to determine if this would increase the susceptibility of Y. pestis to antibiotics. Etest studies on plates with and without 20 μg/ml of PAβN showed that WT susceptibility to nalidixic acid and rifampin increased only by ∼50%. Susceptibility to other antibiotics was not affected. For comparison, we tested the effect of PAβN on the drug susceptibility of the E. coli MG1655 strain and found a 77 to 96% increase in susceptibility for chloramphenicol, nalidixic acid, and rifampin (Table 2). These findings are similar to results reported previously (33). For norfloxacin, ciprofloxacin, streptomycin, and ampicillin, there was, in fact, an unexpected decrease in susceptibility of E. coli in the presence of PAβN (Table 2).
Table 2.
Effect of PAβN on drug susceptibility of the various strains
| Straina | % MIC +PaβN/−PAβN (SD)b |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| TET | KAN | SMC | CHL | CIP | NOR | NAL | RIF | TMS | AMP | |
| Y. pestis | ||||||||||
| WT | 100 (0)NS | 100 (0)NS | 83 (19)NS | 69 (24)NS | 179 (20)* | 134 (25)NS | 46 (8)** | 50 (0)*** | 101 (41)NS | 116 (27)NS |
| acrAB strain | 50 (0)*** | 40 (9)NS | 60 (20)NS | 69 (6)* | NA | NA | 31 (5)** | 50 (0)*** | 101 (28)NS | NA |
| tolC lacZ::kan strain | 41 (9)* | R | 78 (19)NS | 31 (17)* | NA | NA | 28 (5)** | 25 (0)*** | 56 (10)NS | NA |
| E. coli MG1655 | 172 (86)NS | 164 (97)NS | 300 (0)*** | 13 (0)*** | 228 (67)** | 253 (48)** | 23 (4)** | 4 (2)*** | 69 (6)NS | 117 (76)NS |
Genes were deleted and a kanamycin resistance gene was inserted into the lacZ gene of the tolC strain using splicing by overlap extension.
Standard deviations were calculated from 3 experiments. Significance is denoted as follows: *, P value of 0.01 to 0.05; **, P value of 0.001 to 0.01; ***, P value of <0.001; NS, not significant. R denotes complete resistance due to the kanamycin resistance gene integrated into the lacZ gene. NA denotes that data were not available as the boundary of bacterial growth was below that of the lowest Etest antibiotic concentration with and/or without PAβN supplementation. Numbers in bold show significant percent changes less than or equal to 50%. Numbers in italics show percent changes where susceptibility decreased in the presence of PAβN.
Etests on the acrAB and tolC strains showed increases in susceptibility to tetracycline, nalidixic acid, chloramphenicol, and rifampin (50 to 75% [Table 2]) in the presence of PAβN, suggesting that PAβN is effluxed by AcrAB in the WT strain, and with the loss of the pump in the deletion strains, PAβN is able to inhibit other pumps. Further, unlike WT Y. pestis, acrAB or tolC strains were not able to grow at 50 or 100 μg/ml PAβN, suggesting that in the absence of AcrAB or TolC, PAβN is lethal.
Together, these findings suggest that Y. pestis AcrAB-TolC plays a role in efflux of PAβN but is minimally inhibited by it. In contrast, the E. coli AcrAB pump and the P. aeruginosa MexAB pump efflux PAβN but are also inhibited by it (4, 20, 21, 42).
As there is a slight but significant decrease in the susceptibility of certain antibiotics in the presence of PAβN (ciprofloxacin, norfloxacin, and streptomycin), checkerboard assays were performed with E. coli MG1655 at 5 × 105 CFU/ml in 96-well microtiter plates. A series of 7 twofold dilutions were made such that the MIC of the antibiotic in question was approximately the median concentration of the series. A series of 7 twofold dilutions of PAβN was also made, the highest concentration being 80 μg/ml and the lowest in the series being 1.25 μg/ml. FIC thresholds used were ≤0.5 to denote synergy, >0.5 to ≤4 to denote indifference, and >4 to denote antagonism. Three separate checkerboard assays were performed. FICs were calculated as the sum of the combination MIC divided by the MIC for each compound and are shown in Table 3. Synergy was found for nalidixic acid, and indifference was found for ciprofloxacin. MIC values were higher overall in the microtiter format then by Etest, and this difference was more marked for ciprofloxacin than for nalidixic acid but the trend of decreased susceptibility in the presence of PAβN for ciprofloxacin and increased susceptibility of nalidixic acid held. These data support our Etest findings. A literature search was done to compare our findings with those of other studies, particularly with regard to fluoroquinolones, as the initial study on PAβN on P. aeruginosa (21) saw an 8-fold increase in susceptibility to fluoroquinolone and levofloxacin. Other studies show that the effect of PAβN is dependent on strain and antibiotic (4, 29, 33) for both E. coli and P. aeruginosa and that the fold increase in susceptibility varies from 1 to 8. Pasquali and Manfreda (29) also show that E. coli strain ATCC 25922 had MICs of 0.016 to <0.06 μg/ml in the absence and presence of 80 μg/ml PAβN. This shows that there is variation between strains as to the effect on PAβN and that our findings do not contradict the findings from other groups.
Table 3.
Checkerboard fractional inhibitory concentration results and comparison of MICs obtained from checkerboard and Etest assays at 20 μg/ml PAβN on E. coli strain MG1655a
| Antibiotic | Etest |
CB |
|||||
|---|---|---|---|---|---|---|---|
| MIC (μg/ml) | MIC+ (μg/ml) | % difference | MIC (μg/ml) | MIC+ (μg/ml) | % difference | FIC | |
| NAL | 1.67 (0.29) | 0.38 (0.00) | 23 | 3.3 (1.4) | 0.31 (0) | 9 | 0.078 (0.016) |
| CIP | 0.003 (0.001) | 0.007 (0.001) | 233 | 0.032 (0.000) | 0.043 (0.018) | 134 | 1.80 (0.58) |
MIC denotes MIC in the absence of PAβN; MIC+ denotes MIC in the presence of 20 μg/ml PAβN. Numbers in parentheses show standard deviations from three experiments. The percent difference was calculated as MIC+/MIC × 100. CB, checkerboard; FIC, fractional inhibitory concentration.
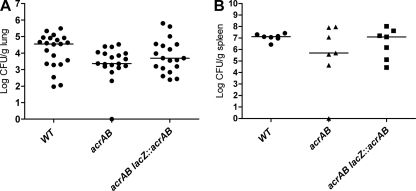
Since the homologs of the AcrAB-TolC pump in other pathogens are important in virulence (3, 27, 30), we studied the contribution of acrAB in organ colonization in pneumonic and septicemic models of plague and the contribution of tolC in the pneumonic plague model. Seven- to 8-week-old female BALBc mice were infected intranasally or intravenously with 20 and 10 times the 50% lethal dose (LD50), respectively (28, 38). Four (intravenous) or 5 (intranasal) days postinfection, mice were euthanized; tissues were harvested, homogenized, serially diluted, and plated for CFU. Strikingly, no difference was seen for the tolC strain (results not shown). While a trend toward lower colonization levels by the acrAB mutant was observed, it was not significant (Fig. 2). These findings suggest that unlike in other pathogens, Y. pestis AcrAB does not play a significant role in establishing infections in pneumonic or septicemic plague in mice.
Fig 2.
Intranasal (A) and intravenous (B) mouse infections. Each symbol in the graphs shows the results for one mouse. The horizontal bar denotes the median.
ACKNOWLEDGMENTS
We thank Hortensia Garcia-Rolan for performing the intravenous injections in the mouse model of septicemia.
This work was supported in part by the New England Regional Center of Excellence (NERCE) and Biodefense and Emerging Infectious Diseases (BEID) and PHS grant AI 56021.
We thank AB Biodisk for providing Etests for this work.
Footnotes
Published ahead of print 14 November 2011
REFERENCES
- 1. Barbosa TM, Levy SB. 2000. Differential expression of over 60 chromosomal genes in Escherichia coli by constitutive expression of MarA. J. Bacteriol. 182:3467–3474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bhor VM, Thomas CJ, Surolia N, Surolia A. 2005. Polymyxin B: an ode to an old antidote for endotoxic shock. Mol. Biosyst. 1:213–222 [DOI] [PubMed] [Google Scholar]
- 3. Bina XR, Lavine CL, Miller MA, Bina JE. 2008. The AcrAB RND efflux system from the live vaccine strain of Francisella tularensis is a multiple drug efflux system that is required for virulence in mice. FEMS Microbiol. Lett. 279:226–233 [DOI] [PubMed] [Google Scholar]
- 4. Bohnert JA, Kern WV. 2005. Selected arylpiperazines are capable of reversing multidrug resistance in Escherichia coli overexpressing RND efflux pumps. Antimicrob. Agents Chemother. 49:849–852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bulet P, Stocklin R, Menin L. 2004. Anti-microbial peptides: from invertebrates to vertebrates. Immunol. Rev. 198:169–184 [DOI] [PubMed] [Google Scholar]
- 6. Chatterjee A, Chaudhuri S, Saha G, Gupta S, Chowdhury R. 2004. Effect of bile on the cell surface permeability barrier and efflux system of Vibrio cholerae. J. Bacteriol. 186:6809–6814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Elkins CA, Mullis LB. 2006. Mammalian steroid hormones are substrates for the major RND- and MFS-type tripartite multidrug efflux pumps of Escherichia coli. J. Bacteriol. 188:1191–1195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Escribano I, Rodriguez JC, Pertegas V, Cebrian L, Royo G. 2006. Relation between induction of the mar operon and cyclohexane tolerance and reduction in fluoroquinolone susceptibility in Salmonella spp. J. Infect. Chemother. 12:177–180 [DOI] [PubMed] [Google Scholar]
- 9. Galimand M, Carniel E, Courvalin P. 2006. Resistance of Yersinia pestis to antimicrobial agents. Antimicrob. Agents Chemother. 50:3233–3236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hasdemir UO, Chevalier J, Nordmann P, Pages JM. 2004. Detection and prevalence of active drug efflux mechanism in various multidrug-resistant Klebsiella pneumoniae strains from Turkey. J. Clin. Microbiol. 42:2701–2706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Heckman KL, Pease LR. 2007. Gene splicing and mutagenesis by PCR-driven overlap extension. Nat. Protoc. 2:924–932 [DOI] [PubMed] [Google Scholar]
- 12. Izadpanah A., R, L Gallo. 2005. Antimicrobial peptides. J. Am. Acad. Dermatol. 52:381–390; quiz, 391–392 [DOI] [PubMed] [Google Scholar]
- 13. Jenssen H, Hamill P, Hancock RE. 2006. Peptide antimicrobial agents. Clin. Microbiol. Rev. 19:491–511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jerse AE, et al. 2003. A gonococcal efflux pump system enhances bacterial survival in a female mouse model of genital tract infection. Infect. Immun. 71:5576–5582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kaczmarek FS, et al. 2004. Genetic and molecular characterization of {beta}-lactamase-negative ampicillin-resistant Haemophilus influenzae with unusually high resistance to ampicillin. Antimicrob. Agents Chemother. 48:1630–1639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kern WV, et al. 2006. Effect of 1-(1-naphthylmethyl)-piperazine, a novel putative efflux pump inhibitor, on antimicrobial drug susceptibility in clinical isolates of Escherichia coli. J. Antimicrob. Chemother. 57:339–343 [DOI] [PubMed] [Google Scholar]
- 17. Kwa AL, Tam VH, Falagas ME. 2008. Polymyxins: a review of the current status including recent developments. Ann. Acad. Med. Singapore 37:870–883 [PubMed] [Google Scholar]
- 18. Lahteenmaki K, Virkola R, Saren A, Emody L, Korhonen TK. 1998. Expression of plasminogen activator pla of Yersinia pestis enhances bacterial attachment to the mammalian extracellular matrix. Infect. Immun. 66:5755–5762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lister IM, Mecsas J, Levy SB. 2010. Effect of MarA-like proteins on antibiotic resistance and virulence in Yersinia pestis. Infect. Immun. 78:364–371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lomovskaya O, Bostian KA. 2006. Practical applications and feasibility of efflux pump inhibitors in the clinic—a vision for applied use. Biochem. Pharmacol. 71:910–918 [DOI] [PubMed] [Google Scholar]
- 21. Lomovskaya O, et al. 2001. Identification and characterization of inhibitors of multidrug resistance efflux pumps in Pseudomonas aeruginosa: novel agents for combination therapy. Antimicrob. Agents Chemother. 45:105–116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mazzariol A, Zuliani J, Cornaglia G, Rossolini GM, Fontana R. 2002. AcrAB efflux system: expression and contribution to fluoroquinolone resistance in Klebsiella spp. Antimicrob. Agents Chemother. 46:3984–3986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nikaido E, Yamaguchi A, Nishino K. 2008. AcrAB multidrug efflux pump regulation in Salmonella enterica serovar Typhimurium by RamA in response to environmental signals. J. Biol. Chem. 283:24245–24253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nikaido H. 2009. Multidrug resistance in bacteria. Annu. Rev. Biochem. 78:119–146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nikaido H, Takatsuka Y. 2009. Mechanisms of RND multidrug efflux pumps. Biochim. Biophys. Acta 1794:769–781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nishino K, Yamaguchi A. 2001. Analysis of a complete library of putative drug transporter genes in Escherichia coli. J. Bacteriol. 183:5803–5812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Padilla E, et al. 2010. Klebsiella pneumoniae AcrAB efflux pump contributes to antimicrobial resistance and virulence. Antimicrob. Agents Chemother. 54:177–183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Parent MA, et al. 2005. Cell-mediated protection against pulmonary Yersinia pestis infection. Infect. Immun. 73:7304–7310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Pasquali F, Manfreda G. 2007. Mutant prevention concentration of ciprofloxacin and enrofloxacin against Escherichia coli, Salmonella Typhimurium and Pseudomonas aeruginosa. Vet. Microbiol. 119:304–310 [DOI] [PubMed] [Google Scholar]
- 30. Piddock LJ. 2006. Multidrug-resistance efflux pumps—not just for resistance. Nat. Rev. Microbiol. 4:629–636 [DOI] [PubMed] [Google Scholar]
- 31. Pomposiello PJ, Bennik MH, Demple B. 2001. Genome-wide transcriptional profiling of the Escherichia coli responses to superoxide stress and sodium salicylate. J. Bacteriol. 183:3890–3902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rosner JL, Martin RG. 2009. An excretory function for the Escherichia coli outer membrane pore TolC: upregulation of marA and soxS transcription and rob activity due to metabolites accumulated in tolC mutants. J. Bacteriol. 191:5283–5292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Saenz Y, et al. 2004. Effect of the efflux pump inhibitor Phe-Arg-beta-naphthylamide on the MIC values of the quinolones, tetracycline and chloramphenicol, in Escherichia coli isolates of different origin. J. Antimicrob. Chemother. 53:544–545 [DOI] [PubMed] [Google Scholar]
- 34. Shafer WM, Qu X, Waring AJ, Lehrer RI. 1998. Modulation of Neisseria gonorrhoeae susceptibility to vertebrate antibacterial peptides due to a member of the resistance/nodulation/division efflux pump family. Proc. Natl. Acad. Sci. U. S. A. 95:1829–1833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sulavik MC, et al. 2001. Antibiotic susceptibility profiles of Escherichia coli strains lacking multidrug efflux pump genes. Antimicrob. Agents Chemother. 45:1126–1136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Thanassi DG, Cheng LW, Nikaido H. 1997. Active efflux of bile salts by Escherichia coli. J. Bacteriol. 179:2512–2518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Tzeng YL, et al. 2005. Cationic antimicrobial peptide resistance in Neisseria meningitidis. J. Bacteriol. 187:5387–5396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Une T, Brubaker RR. 1984. In vivo comparison of avirulent Vwa- and Pgm- or Pstr phenotypes of yersiniae. Infect. Immun. 43:895–900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wang H, Dzink-Fox JL, Chen M, Levy SB. 2001. Genetic characterization of highly fluoroquinolone-resistant clinical Escherichia coli strains from China: role of acrR mutations. Antimicrob. Agents Chemother. 45:1515–1521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Warner DM, Levy SB. 2010. Different effects of transcriptional regulators marA, soxS, and rob on susceptibility of Escherichia coli to cationic antimicrobial peptides (CAMPs): Rob-dependent CAMP induction of the marRAB operon. Microbiology 156:570–578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Yang H, et al. 2008. The AcrAB-TolC pump is involved in multidrug resistance in clinical Shigella flexneri isolates. Microb. Drug Resist. 14:245–249 [DOI] [PubMed] [Google Scholar]
- 42. Yu EW, Aires JR, McDermott G, Nikaido H. 2005. A periplasmic drug-binding site of the AcrB multidrug efflux pump: a crystallographic and site-directed mutagenesis study. J. Bacteriol. 187:6804–6815 [DOI] [PMC free article] [PubMed] [Google Scholar]