Abstract
The development of a mouse model for Kaposi's sarcoma-associated herpesvirus (KSHV) infection has been impeded by the limited host range of the virus. Here, we have examined the molecular basis of this host range restriction. KSHV efficiently enters murine cells and establishes latency. However, ectopic expression of the lytic switch protein RTA (replication and transcription activator) in these cells induces little viral gene expression and no virus production. Upon treatment with histone deacetylase inhibitors, KSHV-infected murine cells display more extensive but aberrant viral transcription and do not support either viral DNA synthesis or the production of infectious virions. These aberrantly infected cells also display markedly enhanced apoptosis. Genetic ablation of the mitochondrial apoptotic pathway in these cells prolongs their survival and permits viral DNA replication but does not rescue the generation of virions. We conclude that multiple defects, both prior to and following DNA synthesis, restrict lytic KSHV infection in murine cells.
TEXT
Kaposi's sarcoma-associated herpesvirus (KSHV; HHV-8) is a lymphotropic herpesvirus linked to several clinical disorders, including Kaposi's sarcoma (KS), primary effusion lymphoma (PEL), and multicentric Castleman's disease (MCD) (3, 5, 8, 11, 12). The development of biological systems with which to study KSHV infection in vivo would provide much-needed knowledge about viral transmission and disease pathogenesis. However, animal models of KSHV infection have eluded the field for a number of reasons. The host range of KSHV is narrow, with natural infection limited to humans. Moreover, to date, only a few human cell lines have been shown to be capable of supporting the full KSHV infectious cycle (1, 2, 22). Experimental transmission to other animal species, including mice, has generally failed, with common marmosets being the only known exception (7). In SCID-hu mice exposed to KSHV, no murine tissue displayed signs of infection (9). Recently, Mutlu et al. engineered a KSHV-dependent mouse model of KS, which required genetic manipulation of the KSHV genome in combination with a bacterial artificial chromosome system. Although a proliferative lesion was generated, even here, no evidence of productive KSHV replication was found (19).
True herpesviral infection is characterized by the following: (i) establishment of latency, (ii) entry into the lytic cycle, (iii) viral DNA replication, and (iv) proper assembly and release of infectious virions. We evaluated these criteria of KSHV infection in murine cells to begin to define at which stage the block occurs. In this study, we used r.KSHV.219, which constitutively expresses green fluorescent protein (GFP) from the E1α promoter. This fluorescent readout of infectivity greatly improves the ability to sensitively quantify infection by flow cytometry. In addition, r.KSHV.219 encodes red fluorescent protein (RFP) downstream from an RTA (replication and transcription activator)-responsive promoter (PAN), resulting in a quantitative assay to detect expression of the lytic switch protein RTA and entry into the lytic cycle (25). Using the increased sensitivity of the r.KSHV.219 system, we determined the steps at which KSHV infection of murine cells is blocked and investigated the possibility of overcoming this inhibition.
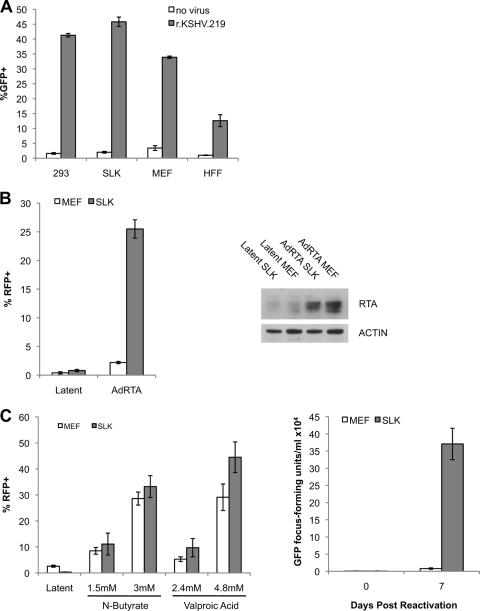
Earlier studies showed that mouse cells can support viral entry, genome circularization, and the expression of LANA-1 (as judged by immunofluorescence) (1, 15, 22). In the experiment whose results are shown in Fig. 1A, we confirmed that entry of r.KSHV.219 into a murine cell line (mouse embryonic fibroblasts [MEFs]) occurs, as assayed by GFP expression detected by flow cytometry. The results in Fig. 1A also show that such entry occurs with an efficiency comparable to that of its entry into permissive human cell lines (e.g., 293 cells, SLK cells, and human foreskin fibroblasts [HFFs]). When such infected cells are examined for viral transcripts by hybridization of their extracted RNA to a custom KSHV genomic tiling array (6), a highly restricted pattern of gene expression is observed (Fig. 2A, under Latent). The principal transcripts detected in this array correspond to the major latency locus encoding LANA, v-cyclin, and v-FLIP (Fig. 2A, arrow).
Fig 1.
Mouse cells are efficiently infected by KSHV and express lytic transcripts in response to HDAc inhibitors. (A) Mouse embryonic fibroblasts (MEF), SLK cells, 293 cells, and human foreskin fibroblasts (HFF) were infected with 5 × 104 GFP focus-forming units/ml of r.KSHV.219. Infection efficiency was measured by quantifying GFP-expressing cells. (B) Left: stably r.KSHV.219-infected MEFs and SLK cells were treated for 48 h with AdRTA and 1.2 mM valproate. Lytic reactivation was measured by quantification of RFP-positive (RFP+) cells by flow cytometry. Right: immunoblot of RTA expression in AdRTA-treated MEF r.KSHV and SLK r.KSHV cells after 48 h. (C) Left: stably r.KSHV.219-infected MEFs and SLK cells were treated for 48 h with valproic acid and N-butyrate. Lytic reactivation was measured by quantification of RFP-positive cells by flow cytometry. Right: stably r.KSHV.219-infected MEFs and SLK cells were treated for 0 and 7 days with 4.8 mM valproic acid. MEF and SLK cell supernatants were incubated with 293 cells, and virus production was quantified 24 h after supernatant transfer by flow cytometric analysis of GFP-expressing 293 cells. Error bars show standard deviations.
Fig 2.
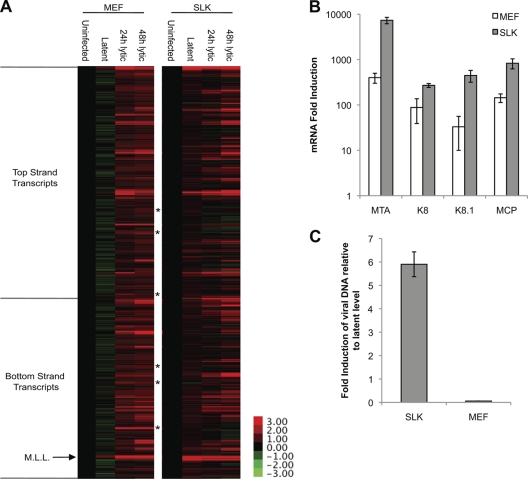
Evaluation of lytic cycle progression in mouse cells. (A) Microarray analysis of KSHV mRNA transcription in stably r.KSHV.219-infected MEFs and SLK cells induced for 0, 24, and 48 h with 4.8 mM valproic acid. Using Agilent technology, 13,746 60-mer KSHV-specific oligonucleotide probes specific to the KSHV genome sequence (GenBank accession no. U75698.1) were printed in duplicate. Each probe overlapped a neighboring probe by 40 nucleotides, resulting in a tiling design with probes offset by 20 nucleotides. The arrow indicates the major latency locus (M.L.L.). Asterisks indicate transcripts upregulated in MEFs that are absent in SLK cells. (B) Fold induction of lytic mRNA in MEFs and SLK cells upon 24 h of treatment with 4.8 mM valproic acid in comparison to latent levels. MTA, mRNA transport and accumulation protein; K8, KSHV ORF 8; K8.1, KSHV ORF 8.1; MCP, major capsid protein. (C) KSHV DNA replication in MEFs and SLK cells following 72 h of 4.8 mM valproic acid treatment. Viral DNA replication was measured by qPCR of LANA DNA. Error bars show standard deviations.
Next, we evaluated the ability of cell lines stably infected with r.KSHV.219 (MEF r.KSHV and SLK r.KSHV) to be lytically induced from latency. First, the cells were infected with an adenovirus expressing the lytic switch protein RTA (AdRTA). Forty-eight hours later, cells were examined microscopically and by flow cytometry for RFP expression. Interestingly, under conditions in which ∼30% of SLK cells expressed RFP, only sporadic MEF r.KSHV cells (∼2% of the culture) were RFP positive (Fig. 1B, left). Western blotting of the two cultures for RTA (Fig. 1B, right) confirmed that both lines were comparably infected with adenovirus and expressed equivalent amounts of RTA. Since RFP in r.KSHV.219 is directly controlled by RTA, this suggests that RTA functions inefficiently in a murine environment. Furthermore, supernatant from MEF r.KSHV cells infected with AdRTA for 5 days did not contain detectable infectious virions (data not shown).
Since ectopic RTA expression in mouse cells has earlier been shown to function in the activation of transfected reporter genes (13, 14, 23), we wondered if the defects observed might have to do with the nature of the chromatinized DNA template. Accordingly, we asked if lytic reactivation would be more efficient if induction was triggered by exposure to histone deacetylase (HDAc) inhibitors like valproic acid or sodium butyrate (N-butyrate). Consistent with this idea, we found that in the presence of either HDAc inhibitor, induction of RTA-dependent RFP expression proceeded nearly as efficiently in KSHV-positive MEFs as in SLK cells (Fig. 1C, left). However, despite this fact, we observed that the supernatants of MEFs induced by prolonged valproate exposure still displayed barely detectable infectious virus (Fig. 1C, right).
To determine at what stage this block to virus production occurs, we analyzed viral transcript accumulation in valproate-reactivated MEF r.KSHV cells by expression profiling on the KSHV genomic array (6) (Fig. 2A). This revealed the accumulation of RNAs homologous to large segments of the viral genome, including late genes such as those encoding capsid and envelope proteins. The array data were confirmed by quantitative PCR (qPCR) analysis of a subset of specific viral transcripts (Fig. 2B). However, although inhibition of histone deacetylation rescued extensive lytic transcription, several lines of evidence suggested that this transcriptional program was not correctly executed. First, several transcripts that were strongly expressed in MEF r.KSHV cells upon lytic entry are absent in human cell line infection (denoted by asterisks in Fig. 2A), suggesting that they are aberrant. Second, despite extensive delayed early transcription, viral DNA synthesis did not occur in induced MEF r.KSHV cells. This is shown in Fig. 2C, which shows the levels of total viral DNA prior to and 72 h after valproic acid treatment as quantitated by qPCR. This fact suggests that the delayed early transcription program is defective, indicating that the observed extensive transcription of the viral genome does not faithfully reflect correct lytic gene expression. This inference is also sustained by the observation (Fig. 2A and B) that abundant expression of RNAs for late genes occurs despite the absence of lytic DNA replication. This aberrant lytic RNA profile could be due to defects in epigenetic modifications in viral chromatin, primary abnormalities in transcription, and/or abnormalities in viral RNA turnover; further studies will be necessary to distinguish among these possibilities.
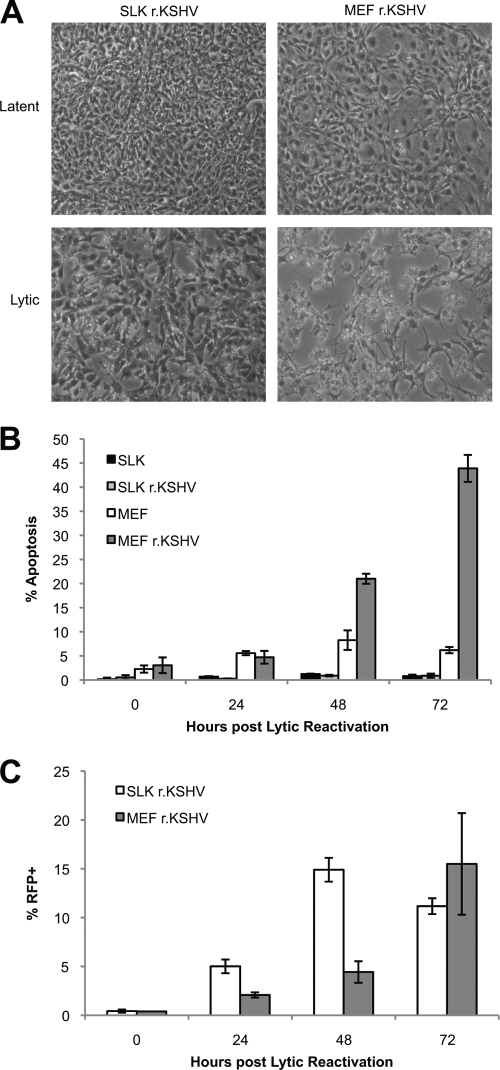
Interestingly, by 72 h after valproic acid treatment, MEF r.KSHV cells display extensive cytopathic effects (CPE) (Fig. 3A). This is in stark contrast to SLK r.KSHV cells, which display no visible CPE until approximately 6 days after lytic reactivation. This observation led us to measure the kinetics of apoptosis following lytic reactivation in MEFs and SLK cells, as judged by flow cytometry for annexin V. This revealed that approximately 50% of MEF r.KSHV cells are apoptotic by 72 h after lytic reactivation (4.8 mM valproic acid), while uninfected MEFs, SLK cells, or SLK r.KSHV cells remain viable in response to similar treatment with valproic acid at this time point (Fig. 3B). SLK r.KSHV and MEF r.KSHV cells both efficiently enter the lytic cycle (as judged by RFP expression) under these conditions (Fig. 3C). These observations suggest that although valproate-induced murine cells express many KSHV transcripts, apoptosis is initiated prematurely in these cells, which could account for many of the subsequent defects in viral replication (see below). Furthermore, according to array data, transcripts encoding KSHV anti-apoptotic factors, including v-cyclin, v-Bcl-2, K7, and K1, are expressed upon lytic cycle entry (Fig. 2A). However, the array data indicate that these transcripts are expressed at somewhat lower levels in MEFs than in SLK cells. It is possible that these lower expression levels of anti-apoptotic transcripts are not sufficient to prevent premature apoptosis in MEFs.
Fig 3.
KSHV lytic cycle induces early apoptosis in mouse cells. (A) Cytopathic effects observed in MEF r.KSHV.219 cells following 72 h of 4.8 mM valproic acid treatment. (B) Apoptotic kinetics were measured by annexin V staining following lytic reactivation (4.8 mM valproic acid) of stably r.KSHV.219-infected MEFs and SLK cells. (C) Quantification of RFP-positive cells as a measurement of lytic reactivation upon 4.8 mM valproic acid treatment. Error bars show standard deviations.
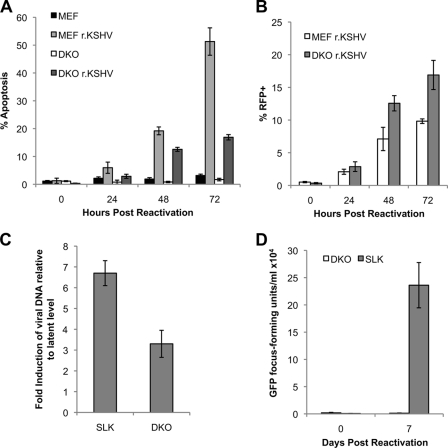
Intrinsic cell damage culminates in activation of the mitochondrial apoptotic pathway, which requires the proapoptotic BCL-2 family proteins BAX and BAK (20). Homo-oligomerization of BAX and/or BAK consequently results in mitochondrial permeability, release of proapoptotic factors (e.g., cytochrome c), activation of effector caspases, and cell death (10, 18, 24). Therefore, cells doubly deficient in bax and bak are significantly resistant to multiple forms of intrinsic cell death (17, 26). To determine if early apoptosis is the primary block to viral replication in murine cells, we established a stably r.KSHV.219-infected bax−/− bak−/− MEF line (double knockout [DKO] r.KSHV). We hypothesized that inhibition of intrinsic apoptosis could delay apoptosis long enough in the murine cells to permit proper viral DNA replication and virion assembly. As predicted, apoptosis is substantially delayed in DKO r.KSHV cells in comparison to that in MEF r.KSHV cells but still occurs earlier than in SLK r.KSHV cells (Fig. 4A). As judged by RTA-dependent RFP expression, DKO r.KSHV cells reactivate at least as efficiently as MEF r.KSHV cells, probably due to the delay in cell death-initiated degradation of viral transcripts and proteins (Fig. 4B). Importantly, delaying the apoptotic kinetics permits viral DNA replication in DKO r.KSHV cells, albeit to a lower level than in human SLK r.KSHV cells (Fig. 4C). However, despite these changes, no infectious virions are produced by DKO r.KSHV cells (Fig. 4D).
Fig 4.
bax−/−bak−/− (DKO) MEFs are resistant to KSHV apoptosis induced by KSHV lytic replication and support viral DNA replication but produce no infectious virions. (A) Apoptosis was measured by annexin V staining following lytic reactivation (4.8 mM valproic acid) of stably r.KSHV.219-infected DKO cells, MEFs, and SLK cells. (B) Quantification of RFP-positive cells as a measurement of lytic reactivation upon 4.8 mM valproic acid treatment. (C) DNA replication in DKO cells and SLK cells following 72 h of 4.8 mM valproic acid treatment. DNA replication was measured by qPCR of LANA gene copies. (D) Virus production (GFP-expressing cells) measured by infecting 293 cells with supernatant from DKO r.KSHV and SLK r.KSHV cells treated for 0 and 7 days with 4.8 mM valproic acid. Error bars show standard deviations.
We speculate that the induction of premature cell death may be due to the dysregulation of immediate early and delayed early genes, many of which can be proapoptotic when overexpressed (4, 21). Aberrant expression of late genes could also contribute to this phenotype. By inhibiting the intrinsic apoptotic pathway with DKO MEFs, we can delay cell death long enough to permit viral DNA replication (Fig. 4C). However, despite this apoptotic delay, few virions are produced. This suggests that other defects in late gene expression or in virion assembly or egress are also present in infected murine cells. Alternatively (or additionally), the premature engagement of other forms of cell death, such as extrinsic apoptosis or necrosis, may be responsible. Consistent with this idea, induced DKO r.KSHV cells display morphological signs of cell injury a full 48 h before such changes are evident in infected human SLK cells (data not shown).
We note that our results differ slightly from those of earlier experiments published by Liang and Ganem (16). They observed very low level virus production following superinfection with high titers of AdRTA of a single, spontaneously immortalized line of mouse fibroblasts transiently infected with wild-type (unmarked) KSHV at very high multiplicities (estimated at 5,000 to 10,000 viruses per cell) (16). The high multiplicity of infection used, the transient nature of the infection prior to reactivation, and the fact that they employed a single, multiply passaged mouse line are important differences between that study and the present one and probably account for this disparity. While those results suggest that there are conditions in vitro under which limited KSHV growth can occur in murine cells, our present results, in accord with those of all earlier in vitro animal experiments, suggest that this situation is a laboratory phenomenon unlikely to be encountered in vivo.
Taken together, our data indicate that multiple postentry blocks to KSHV lytic replication exist. Viral episomes in stably infected latent mouse cells respond incorrectly to exogenous RTA expression, with extremely attenuated lytic gene expression. When these defects are (partially) bypassed via HDAc inhibition, the resulting lytic program remains aberrant; this dysregulation does not allow viral DNA replication, and it is associated with premature apoptosis. When the latter is blocked experimentally, DNA replication can proceed but additional blocks continue to prevent infectious virion production. Thus, murine cells block lytic KSHV replication at multiple stages in the cycle, rendering it unlikely that any single genetic manipulation of transgenic mice can bypass these obstacles.
ACKNOWLEDGMENT
This work was supported by a grant from the NIH (grant P01DE019085).
Footnotes
Published ahead of print 30 November 2011
REFERENCES
- 1. Bechtel JT, Liang Y, Hvidding J, Ganem D. 2003. Host range of Kaposi's sarcoma-associated herpesvirus in cultured cells. J. Virol. 77:6474–6481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Blackbourn DJ, et al. 2000. The restricted cellular host range of human herpesvirus 8. AIDS 14:1123–1133 [DOI] [PubMed] [Google Scholar]
- 3. Boshoff C, Weiss RA. 1998. Kaposi's sarcoma-associated herpesvirus. Adv. Cancer Res. 75:57–86 [DOI] [PubMed] [Google Scholar]
- 4. Cannon ML, Cesarman E. 2004. The KSHV G protein-coupled receptor signals via multiple pathways to induce transcription factor activation in primary effusion lymphoma cells. Oncogene 23:514–523 [DOI] [PubMed] [Google Scholar]
- 5. Cesarman E, Chang Y, Moore PS, Said JW, Knowles DM. 1995. Kaposi's sarcoma-associated herpesvirus-like DNA sequences in AIDS-related body-cavity-based lymphomas. N. Engl. J. Med. 332:1186–1191 [DOI] [PubMed] [Google Scholar]
- 6. Chandriani S, Ganem D. 2010. Array-based transcript profiling and limiting-dilution reverse transcription-PCR analysis identify additional latent genes in Kaposi's sarcoma-associated herpesvirus. J. Virol. 84:5565–5573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chang H, et al. 2009. Non-human primate model of Kaposi's sarcoma-associated herpesvirus infection. PLoS Pathog. 5:e1000606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chang Y, et al. 1994. Identification of herpesvirus-like DNA sequences in AIDS-associated Kaposi's sarcoma. Science 266:1865–1869 [DOI] [PubMed] [Google Scholar]
- 9. Dittmer D, et al. 1999. Experimental transmission of Kaposi's sarcoma-associated herpesvirus (KSHV/HHV-8) to SCID-hu Thy/Liv mice. J. Exp. Med. 190:1857–1868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Du C, Fang M, Li Y, Li L, Wang X. 2000. Smac, a mitochondrial protein that promotes cytochrome c-dependent caspase activation by eliminating IAP inhibition. Cell 102:33–42 [DOI] [PubMed] [Google Scholar]
- 11. Dupin N, et al. 1999. Distribution of human herpesvirus-8 latently infected cells in Kaposi's sarcoma, multicentric Castleman's disease, and primary effusion lymphoma. Proc. Natl. Acad. Sci. U. S. A. 96:4546–4551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ganem D. 2006. KSHV infection and the pathogenesis of Kaposi's sarcoma. Annu. Rev. Pathol. 1:273–296 [DOI] [PubMed] [Google Scholar]
- 13. Lan K, et al. 2005. Induction of Kaposi's sarcoma-associated herpesvirus latency-associated nuclear antigen by the lytic transactivator RTA: a novel mechanism for establishment of latency. J. Virol. 79:7453–7465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Liang Y, Chang J, Lynch SJ, Lukac DM, Ganem D. 2002. The lytic switch protein of KSHV activates gene expression via functional interaction with RBP-Jkappa (CSL), the target of the Notch signaling pathway. Genes Dev. 16:1977–1989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Liang Y, Ganem D. 2003. Lytic but not latent infection by Kaposi's sarcoma-associated herpesvirus requires host CSL protein, the mediator of Notch signaling. Proc. Natl. Acad. Sci. U. S. A. 100:8490–8495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Liang Y, Ganem D. 2004. RBP-J (CSL) is essential for activation of the K14/vGPCR promoter of Kaposi's sarcoma-associated herpesvirus by the lytic switch protein RTA. J. Virol. 78:6818–6826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lindsten T, et al. 2000. The combined functions of proapoptotic Bcl-2 family members bak and bax are essential for normal development of multiple tissues. Mol. Cell 6:1389–1399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Liu X, Kim CN, Yang J, Jemmerson R, Wang X. 1996. Induction of apoptotic program in cell-free extracts: requirement for dATP and cytochrome c. Cell 86:147–157 [DOI] [PubMed] [Google Scholar]
- 19. Mutlu AD, et al. 2007. In vivo-restricted and reversible malignancy induced by human herpesvirus-8 KSHV: a cell and animal model of virally induced Kaposi's sarcoma. Cancer Cell 11:245–258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Oakes SA, Lin SS, Bassik MC. 2006. The control of endoplasmic reticulum-initiated apoptosis by the BCL-2 family of proteins. Curr. Mol. Med. 6:99–109 [DOI] [PubMed] [Google Scholar]
- 21. Ojala PM, et al. 1999. Kaposi's sarcoma-associated herpesvirus-encoded v-cyclin triggers apoptosis in cells with high levels of cyclin-dependent kinase 6. Cancer Res. 59:4984–4989 [PubMed] [Google Scholar]
- 22. Renne R, Blackbourn D, Whitby D, Levy J, Ganem D. 1998. Limited transmission of Kaposi's sarcoma-associated herpesvirus in cultured cells. J. Virol. 72:5182–5188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Spadavecchia S, Gonzalez-Lopez O, Carroll KD, Palmeri D, Lukac DM. 2010. Convergence of Kaposi's sarcoma-associated herpesvirus reactivation with Epstein-Barr virus latency and cellular growth mediated by the notch signaling pathway in coinfected cells. J. Virol. 84:10488–10500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Susin SA, et al. 1999. Molecular characterization of mitochondrial apoptosis-inducing factor. Nature 397:441–446 [DOI] [PubMed] [Google Scholar]
- 25. Vieira J, O'Hearn PM. 2004. Use of the red fluorescent protein as a marker of Kaposi's sarcoma-associated herpesvirus lytic gene expression. Virology 325:225–240 [DOI] [PubMed] [Google Scholar]
- 26. Wei MC, et al. 2001. Proapoptotic BAX and BAK: a requisite gateway to mitochondrial dysfunction and death. Science 292:727–730 [DOI] [PMC free article] [PubMed] [Google Scholar]