Abstract
Self-inflicted injury (SII) in adolescence marks heightened risk for suicide attempts, completed suicide, and adult psychopathology. Although several studies have revealed elevated rates of depression among adolescents who self injure, no one has compared adolescent self injury with adolescent depression on biological, self-, and informant-report markers of vulnerability and risk. Such a comparison may have important implications for treatment, prevention, and developmental models of self injury and borderline personality disorder. We used a multi-method, multi-informant approach to examine how adolescent SII differs from adolescent depression. Self-injuring, depressed, and typical adolescent females (n = 25 per group) and their mothers completed measures of psychopathology and emotion regulation, among others. In addition, we assessed electrodermal responding (EDR), a peripheral biomarker of trait impulsivity. Participants in the SII group (a) scored higher than depressed adolescents on measures of both externalizing psychopathology and emotion dysregulation, and (b) exhibited attenuated EDR, similar to patterns observed among impulsive, externalizing males. Self-injuring adolescents also scored higher on measures of borderline pathology. These findings reveal a coherent pattern of differences between self-injuring and depressed adolescent girls, consistent with theories that SII differs from depression in etiology and developmental course.
Self-inflicted injury (SII) in adolescence is associated with poor psychological functioning, interpersonal conflict, academic problems, and risk for suicide (e.g., Johnson et al., 2002; Skegg, 2005; Williams & Hasking, 2010). Accordingly, SII is recognized by the National Center for Injury Prevention and Control (2009) and the U.S. Public Health Service (1999) as an urgent public health problem. In 2006, close to 400,000 adolescents and adults were treated medically for SII (CDC, 2006) a number that likely represents fewer than 30% of persons who engaged in the behavior (Crosby, Cheltenham, & Sacks, 1999). In community samples, between 8% and 56% of young people self-injure (Gratz, 2006; Hilt, Cha, & Nolen-Hoeksema, 2008; Hooley, 2008; Lloyd-Richardson, Perrine, Dierker, & Kelley, 2007; Plener, Libal, Keller, Fegert, & Muehlenkamp, 2009; Ross & Heath, 2002). Unfortunately, these behaviors remain poorly understood, in spite of their prevalence and potential lethality (Nock & Prinstein, 2005).
There are several approaches to characterizing and conceptualizing SII. One approach follows from current diagnostic convention. The Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR; American Psychiatric Association [APA], 2000) includes self-injury in the criterion lists of both major depression (e.g., suicide attempt), and borderline personality disorder (BPD; e.g., recurrent suicidal behaviors, gestures, threats, or self-mutilating behavior). Among these, BPD is a controversial diagnosis for adolescents (see Beauchaine, Klein, Crowell, Derbidge, & Gatzke-Kopp, 2009). This has led many practitioners to assign one or more Axis I diagnoses to self-injuring youth, especially major depression (Miller, Rathus, & Linehan, 2007). Although many self-injuring adolescents meet diagnostic criteria for depression (e.g., Crowell et al., 2005), to our knowledge no study has examined whether self-injuring adolescents differ from depressed, non-self-injuring participants across multiple markers of vulnerability and risk.
Many believe that the DSM-IV fails to capture the variegated nature of SII, particularly among adolescents (see e.g., APA, 2010). The developmental psychopathology perspective provides an alternative means of conceptualizing SII. Developmental psychopathologists examine biosocial mechanisms associated with SII and potential etiological overlap between depression, self-injury, BPD, and externalizing behavior disorders (e.g., Beauchaine et al., 2009; Crowell, Beauchaine, & Linehan, 2009; Crowell et al., 2005). From this standpoint, factors that differentiate SII from depression might suggest alternative etiological pathways, different developmental outcomes, and/or improved treatment strategies for self-injuring youth (e.g., Preskorn & Baker, 2002).
A Developmental Approach to Self-Injury and Borderline Personality Disorder
As noted above, diagnosing BPD in adolescents is controversial. Nevertheless, there is emerging consensus that risk for BPD can be identified by adolescence (Beauchaine et al., 2009; Crowell et al., 2009; Miller, Muehlenkamp, & Jacobson, 2008). Yet it remains unclear precisely which traits and behaviors are the most promising markers of early vulnerability and risk. We have articulated a developmental model in which SII and BPD represent two points along a heterotypically continuous borderline trajectory, with SII emerging prior to BPD among some though certainly not all individuals (Crowell et al., 2009; see also, Beauchaine et al., 2009).
Specifically, we have outlined five developmental hypotheses of BPD (Crowell et al., 2009): (1) poor impulse control, which is largely heritable, emerges early in the lives of those who develop BPD; (2) emotion dysregulation emerges later, and is shaped and maintained within the caregiving environment; (3) Biological Vulnerability × Environmental Risk interactions potentiate more extreme emotional and behavioral dyscontrol; (4) by mid- to late-adolescence, a constellation of identifiable features and maladaptive coping strategies (such as SII) mark heightened risk for BPD; and (5) these traits and behaviors exacerbate risk across development via evocative effects on interpersonal relationships and interference with healthy emotional development. Following from this model, two broad behavioral features appear to confer risk for borderline personality development—trait impulsivity and emotion dysregulation1.
Importantly, those who engage in SII and those who are depressed both suffer from emotion dysregulation (Kring & Sloan, 2010). In contrast, the groups may be differentiated by trait impulsivity, which is highly heritable, confers risk for externalizing behavior disorders, and is often reflected in peripheral physiological measures such as electrodermal responding (e.g., Beauchaine et al., 2009; Crowell et al., 2009). In spite of these potential differences, self-injury is commonly viewed as a symptom of depression. For example, in the Adolescent Depression Antidepressants and Psychotherapy Trial (ADAPT), 58 of 163 depressed adolescents had engaged in non-suicidal self-injury in the month prior to being enrolled into the treatment study (see Wilkinson, Kelvin, Roberts, Dubicka, & Goodyer, 2011). Many of these adolescents responded poorly to intervention, leading the authors to conclude that there may be “a subtype of depression characterized by self-injury that leads to a poor response to treatment” (p. 499). However, no study has examined whether self-injuring adolescents differ from depressed, non-self-injuring teens across biological, self- and mother-reported measures of behavioral inhibition, internalizing and externalizing psychopathology, emotion dysregulation, and borderline personality traits.
Biological Vulnerability: Electrodermal Responding and Behavioral Inhibition
Self-injury and BPD are both associated with serotonergic (5HT) dysfunction (e.g., Arango, Huang, Underwood, & Mann, 2003; Paris et al., 2004). Moreover, emerging evidence suggests that suicide attempts and mood disorders may have partially independent etiologies, with different 5HT genes moderating the gene-gene and gene-environment outcomes that lead to mood disorders versus suicide attempts (Brezo et al., 2010). Serotonergic projections from the raphe nuclei innervate widespread brain regions including the amygdala and septo-hippocampal system. These structures form a neural network that inhibits prepotent behaviors in response to competing motivational goals (Brenner, Beauchaine, & Sylvers, 2005; Fowles, 2000). For example, those who self-injure are often unable to inhibit harmful behavior, even though SII can lead to interpersonal conflict, scarring, or death. Peripherally, low electrodermal responding (EDR) is a reliable biomarker of poor behavioral inhibition, observed among those with severe externalizing disorders (Beauchaine, 2001; Beauchaine, Katkin, Strassberg, & Snarr, 2001; Crowell et al., 2006; Lorber, 2004).
In a recent meta-analysis, Thorell (2009) reported electrodermal hypoactivity among self-injuring individuals. In a subsequent study, very severe suicide attempters (e.g., firearm, hanging) showed attenuated EDR relative to less severe attempters (e.g., pills), and both groups showed low EDR compared with those who are only depressed (Jandl, Steyer, & Kaschka, 2010). Most studies also reveal either hypoactivation or no EDR differences among those with BPD (Ebner-Priemer et al., 2005; Herpertz, Kunert, Schwenger, & Sass, 1999; Schmahl et al., 2004). Furthermore, in the one study in which higher baseline EDR was found, EDR decreases in response to sad mood induction were reported among those with BPD, but not among those with social anxiety disorder (Kuo & Linehan, 2009). Thus, low EDR and reduced EDR reactivity have been found in both SII and BPD, consistent with deficits in biological systems governing behavioral inhibition. In contrast, non-suicidal depression, mixed depression/anxiety, and trait neuroticism are more often associated with normal or heightened EDR (Kopp & Gruzelier, 1989; Norris, Larsen, & Cacioppo, 2007; Papousek & Schulter, 2001; Thorell, 2009). No studies, however, have (a) examined EDR among self-injuring adolescents who may be at risk for developing BPD, or (b) compared patterns of EDR among groups of self-injuring vs. depressed adolescents. Following from the adult literature, we predicted reduced EDR in the SII group compared with both typical and depressed controls.
Symptoms of Psychopathology and Emotion Dysregulation
If SII is best conceptualized as a severe variant of depression, we should expect self-injurers to report higher levels of internalizing symptoms compared with depressed, non-self-injuring teens. However, if SII shares common vulnerabilities with BPD, as we have proposed (Beauchaine et al., 2009; Crowell et al., 2009), we should also expect higher endorsement of externalizing symptoms, including conduct disorder (CD), oppositional defiant disorder (ODD), and substance use disorders (SUDs). Based on a concurrent internalizing and externalizing vulnerability model, we predicted that SII would be associated with more symptoms of both forms of psychopathology compared with depressed participants. We also hypothesized that the SII group would score higher than depressed adolescents on borderline features, even when excluding the self-injury criterion.
Finally, self-injury is associated with severe emotion dysregulation. Indeed, Linehan’s (1987, 1993) biosocial theory suggests that self-injury emerges as a form of coping with pervasive and persistent emotion dysregulation (see Crowell et al., 2009; Kuo & Linehan, 2009 for recent examinations). According to this account, self-injury persists because it is sometimes effective in relieving emotional distress (e.g., Esposito, Spirito, Boergers, & Donaldson, 2003; Johnson, Hurley, Benkelfat, Herpertz, & Taber, 2005; Nock, 2009). Several studies support the emotion dysregulation model among self-injuring adolescents and adults (for a review of this and other models see Klonsky, 2007). Therefore, we predicted that self-injuring adolescents would report high levels of emotion dysregulation. We also hypothesized that self-injuring adolescents would report more difficulty regulating impulsive behaviors in the face of emotional distress.
Method
Participants
Study procedures were approved by the institutional review board at Seattle Children’s Hospital and Regional Medical Center (CHRMC). Written informed assent and consent were obtained from adolescents and their mothers, respectively. Participants included 75 adolescent girls, ages 13–17, who were placed into one of three groups: self-injuring, depressed with no SII history, and typical control. In total, 84 participants were enrolled in order to obtain the final sample. Nine participants had insufficient data to be included in all analyses due to their inability/refusal to return for Visit 2 (n=4), failure of physiological equipment (n=3), or arriving with a guardian other than the mother (n=2). As a group, these 9 participants were not different from the overall sample on any demographic or diagnostic variables, all Fs > 0.0, all ps > .29, all η2 < .02. Thus, their data were included in analyses when available. Mean ages were 16.3 (SD = 1.0) for the SII group, 15.6 (SD=1.4) for the depressed group, and 16.1 (SD=1.3) for controls, F(2, 81) = 2.02, p = .14, η2 = .05. The sample was 70.2% Caucasian, 7.1% African American, 4.8% Latina, 6.0% Asian American, 1.2% Native American, and 10.7% of mixed racial/ethnic heritage. Mean family incomes, in thousands, were $68.5 (SD=$31.2) for the SII group, $58.5 (SD=$32.9) for the depressed group, and $72.9 (SD=$30.6) for controls, F(2, 79) = 1.50, p = .23 η2 = .04. Participants were recruited using (1) online and print classified ads; (2) banners displayed on local busses; (3) brochures distributed at local schools, inpatient treatment facilities, outpatient clinics; and (4) ads distributed through a direct mailing company. Self-injuring and depressed participants were recruited in roughly equal numbers from the community (depressed = 14; SII = 13) and from clinical settings (depressed = 12; SII = 15), χ2(1)=0.30, p=.59.
Interested participants and their mothers contacted the study personnel via phone, and were interviewed separately to determine whether they met criteria. Self-injuring teens were included if they engaged in self-injurious behaviors three or more times in the past six months, or five or more lifetime events, at least one of which occurred in the prior six months. Depressed teens were included if they met criteria for at least one episode of unipolar depression in the past year. Exclusion criteria for all groups included mental retardation or a schizophrenia spectrum disorder, as SII may have a distinct etiology within these diagnoses. Otherwise, SII adolescents were not excluded for (or required to meet) any clinical diagnosis. Depressed adolescents were excluded if they reported mania or any lifetime SII (i.e., one or two SII episodes. Any adolescents who met the appropriate criteria were enrolled in the SII group). Controls were excluded if they reported lifetime SII or an Axis I disorder. Due to potential effects on EDR, participants in all groups were excluded if they were currently taking beta blockers, mood stabilizers, benzodiazepines, or recreational drugs (confirmed via urinalysis) in the week of the physiological assessment. Those taking stimulants were included only if they and their mother consented to a 36-hour washout prior to the assessment. Participants who met these criteria were invited to two visits lasting approximately 2–3 hrs. A $60 incentive was divided across the visits.
Procedure
Visit 1
Once consent and assent were obtained, adolescents and mothers were escorted separately into quiet rooms where they each completed a packet of questionnaires, described below. Adolescents provided self-reports of psychopathology, behavior problems, substance use, emotions, and emotion regulation. Mothers provided reports of their daughter’s psychopathology and behavior problems. At the end of the visit, adolescents and mothers were scheduled to return for the physiological assessment, which occurred approximately two weeks later.
Visit 2
At the second visit, adolescents and mothers were interviewed separately by a trained graduate research assistant, who obtained more detailed reports of psychopathology and self-injury. In addition, psychophysiological assessments were conducted in a dimly lit, sound-attenuated room that was monitored with audio-video recording equipment. Electrodermal responding was first measured during the last min of a 5 min resting baseline. Next, EDR was assessed during a sad emotion induction using a 3 min clip from The Champ, which depicts a young boy reacting to the death of his father. This clip has been demonstrated repeatedly to evoke sadness (Gross & Levenson, 1995; Marsh, Beauchaine, & Williams, 2008), and to induce autonomic responses among self-injuring adolescents (Crowell et al., 2005). Physiological recordings continued for 1 min post-task to evaluate recovery following the movie.
Measures
Adolescent self-report
Adolescent measures of psychopathology and behavior problems included the Youth’s Inventory (YI; Gadow et al., 2002), the Youth Self-Report (YSR; Achenbach, 1991b), the Children’s Depression Inventory (CDI; Kovacs, 1992), and a questionnaire assessing onset, frequency, and problems associated with substance use (Hawkins & Catalano, 2001). The 120-item YI is a self-report checklist that yields dimensional scores and diagnostic cutoffs for several Axis I disorders from the DSM-IV (APA, 2000). Each item is rated on a 4-point scale (0 = never, 1 = sometimes, 2 = often, and 3 = very often), with a score of 2 or higher considered positive for a given diagnostic criterion. All raw scores presented for the YI maintain the 4-point scale. Specificity and sensitivity of the YI are adequate to excellent (Gadow et al., 2002). The YSR is a 112-item measure of adolescent behavior problems, including several psychopathology subscales and broadband internalizing and externalizing factors. The YSR is used widely and is well-validated, with excellent psychometric properties (Achenbach, 1991b). Items are rated on a three-point scale (0 = never, 1 = sometimes, 2 = often). The CDI is a 27-item questionnaire that assesses difficulties associated with depression. The measure has adequate psychometric properties and yields five subscales and an overall depression score (Kovacs, 1992). We report the total score. The substance use questionnaire assesses whether or not adolescents have tried any of a number of substances (e.g., alcohol), age at first use, and the number of times used in the past month. At the end of the questionnaire there are several yes/no questions regarding problems associated with use (e.g., has substance use ever caused problems with family or friends). A total problem score was created by summing questions on problematic use (range = 0–15; Hawkins & Catalano, 2001).
Adolescents also provided self-reports of their difficulties with emotions and emotion regulation using the Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004), the Pediatric Anger Expression Scale (PAES; Jacobs, Phelps, & Rohrs, 1989), and the Generalized Expectancies for Negative Mood Regulation (NMR; Catanzaro & Mearns, 1990). In addition to a total ER difficulties score, the DERS yields six subscales including non-acceptance of emotions, difficulties engaging in goal-directed behavior when upset, poor impulse control when emotionally dysregulated, lack of emotional awareness, limited access to emotion regulation strategies, and lack of emotional clarity. The DERS has high internal consistency, adequate construct and predictive validity, and good test-retest reliability (Gratz & Roemer, 2004). It has been validated among children and adolescents, and predicts physiological reactivity during episodes of emotion dysregulation among youth with and without psychopathology (Vasilev, Crowell, Beauchaine, Mead, & Gatzke-Kopp, 2009). The 15-item PAES assesses three styles of anger expression among youth, including anger-out (outward expression of anger), anger-reflection/control (ability to maintain control of anger), and anger-suppression (directing anger internally). Items are rated on a 3-point scale (1 = hardly ever, 2 = sometimes, 3 = often). Reliability coefficients for the PAES range from adequate to excellent (Jacobs et al., 1989). The NMR is a 30-item measure that assesses individual beliefs about the ability to cope successfully with negative mood. The NMR has acceptable internal consistency, temporal stability, and discriminant validity (Catanzaro & Mearns, 1990). Items are rated on a 5-point scale, ranging from strongly disagree to strongly agree.
Mother-report
Mothers reported on adolescent psychopathology and behavior problems using the Adolescent Symptom Inventory (ASI; Gadow et al., 2002) and the Child Behavior Checklist (CBCL; Achenbach, 1991a), parent-report versions of the YI and YSR, respectively.
Interview measures
Borderline symptoms were assessed using the Structured Clinical Interview for DSM-IV personality disorders (SCID-II; First, Spitzer, Gibbon, & Williams, 1996). The SCID-II is a widely used semi-structured interview with excellent reliability. Items are rated on a 3-point scale (1 = not present, 2 = subthreshold, 3 = threshold). A continuous BPD score was created by converting items to a 0–2 scale and summing them. Thus, scores could range from a low of 0, indicating no BPD criteria, to a high of 18, indicating that all nine criteria were met at or above threshold. Adolescents and their mothers were also interviewed separately with the mood disorders supplement of the Schedule for Affective Disorders and Schizophrenia for school-age children (K-SADS-PL; Kaufman et al., 1997). Both were asked to report on the adolescent’s most severe episode of depression and/or mania in the past year. The interview includes questions assessing symptoms and correlates of depression (30 items) mania (8 items). Each item is tallied on a 3-point scale (1 = not present, 2 = subthreshold, 3 = threshold). A score of zero was also possible, indicating no information. Although rare, there were some zeros, therefore the original 1–3 scale was maintained. When all information was available, scores could range from 30–90 (depression) and 8–24 (mania) The K-SADS is a semi-structured diagnostic interview and has excellent test-retest reliability and concurrent validity.
Finally, adolescents and their mothers reported on the adolescent’s self-injury history using the Lifetime-Suicide Attempt Self-Injury (L-SASI; formerly Lifetime Parasuicide Count; Linehan & Comtois, 1996), a structured interview for gathering information regarding lethality, suicidal intent, level of medical treatment received, and specific details about the adolescent’s first, most recent, and most severe SII episodes. With interviewer assistance, informants tally the number of lifetime events of (a) different forms of self-injury, (b) self-injury with intent to die, (c) self-injury with ambivalence, (d) self-injury without suicidal intent, and (e) medical treatment received. The highest lethality event in each category of SII was also assessed. Lethality rankings range from 1 = very low, including events such as scratching or head banging, to 6 = severe, including events such as Russian roulette or asphyxiation. In separate interviews, participants and mothers were read a description of SII and asked to report whether the adolescent had ever self-injured. Positive indications were followed up by administration of the full interview. There are no psychometric studies of the L-SASI. However, the items are identical to a longer measure, the Suicide Attempt Self-Injury Interview (SASII; Linehan, Comtois, Brown, Heard, & Wagner, 2006), which has very good inter-rater reliability and adequate validity.
Psychophysiological Assessment
Electrodermal responding was recorded continuously using a Biopac MP100 system (Goleta, CA) with appropriate amplifiers and signal conditioners, at a sampling rate of 1kHz. Data were acquired with two standard 0.8-cm2 Ag-AgCl electrodes, attached to the thenar eminence of the participant’s nondominant hand with adhesive electrode washers and a 0.05 molar NaCl solution. Nonspecific skin conductance responses were scored as fluctuations exceeding 0.05 μS.
Results
Psychological and Diagnostic Data
L-SASI
Descriptive statistics on self-injury are summarized for adolescents in the SII group in Table 1. Participants reported a wide range of lifetime self-injury events (3–1350). Mothers also reported a wide range of events (1–266). Although SII participants were recruited for multiple episodes of self-injury, independent of suicidal intent, 81.5% of the SII group (n = 22) reported some intent to die (either ambivalent or certain intent) on at least one occasion. As observed in our previous work (Crowell et al., 2005), mothers reported fewer episodes of self-injury than their daughters across nearly all categories. Nevertheless, mothers recalled a greater number of events requiring medical attention. Based upon both mother and adolescent reports, the average lethality of attempts was low (a ranking of 2, including such items as superficial cuts or overdoses of ≤ 10 pills). Mother–child agreement on the L-SASI was poor, consistent with research showing low agreement on internalizing psychopathology (Stanger & Lewis, 1993). The only significant correlation across raters was for lethality of attempts, r =.95, p <.001. Correlations were not significant for total events, episodes with intent to die, episodes with ambivalent intent, episodes with no intent, or events requiring medical attention, all rs ≤ .11, all ps ≥ .39. Most of the SII group engaged in cutting as the method of choice (n = 24). Stabbing (n = 1), head banging (n = 1), and overdosing (n = 1) were the primary methods for remaining SII participants. All but three participants had engaged in at least one other method of SII.
Table 1.
Self-Injurious Events on the “Lifetime Suicide Attempt Self-Injury” (L-SASI) by Adolescents and their Mothers
| Item | N (%)a | M | SD | Median | Range |
|---|---|---|---|---|---|
| Self-report | |||||
| Total self-injurious events | 27 (100.0) | 143.5 | 288.7 | 42.0 | 3–1350 |
| Events with intent to die | 12 (44.4) | 2.0 | 4.7 | 2.0 | 0–24 |
| Events with ambivalence | 22 (81.5) | 28.0 | 64.1 | 4.0 | 0–308 |
| Events without intending to die | 24 (88.8) | 83.4 | 216.6 | 15.0 | 0–1018 |
| Events requiring medical attention | 13 (48.1) | 0.8 | 1.3 | 0.0 | 0–6 |
| Lethality of self-injury | 27 (100.0) | 2.4 | 0.9 | 2.2 | 1–4 |
| Parent-report | |||||
| Total self-injurious events | 26 (96.2) | 32.0 | 71.0 | 5.0 | 1–266 |
| Events with intent to die | 8 (31.0) | 0.5 | 1.2 | 0.0 | 0–6 |
| Events with ambivalence | 14 (53.8) | 1.8 | 3.1 | 0.5 | 0–12 |
| Events without intending to die | 26 (100.0) | 29.0 | 70.3 | 4.5 | 0–262 |
| Events requiring medical attention | 12 (46.2) | 1.4 | 4.0 | 0.0 | 0–20 |
| Lethality of self-injury | 27 (100.0) | 2.3 | 1.0 | 2.0 | 1–5 |
The number and percentage of participants reporting at least one incident of this type. All participants with available Lifetime-Suicide Attempt Self-Injury count data (n=26) were included.
Psychopathology
Self- and parent-report measures of psychopathology are summarized by group in Table 2. For both the YSR and CBCL, self-injuring and depressed adolescents met or exceeded clinical cutoffs (T = 67, 95th percentile) on most scales. To assess group differences, analyses of variance (ANOVAs) were conducted. Omnibus group effects significant at p < .01 were followed up with group contrasts using Tukey tests. Given the large number of such contrasts, only effects significant at p < .01 are interpreted.
Table 2.
Psychopathology Scores by Group
| Self-Report
|
Parent-Report
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Self-Injuring | Depressed | Control | F | η2 | Self-Injuring | Depressed | Control | F | η2 | |
| n = 28 | n = 25 | n = 25 | n = 21 | n = 19 | n = 25 | |||||
| Achenbach scales1 | ||||||||||
| Withdrawn | 62.4 (1.4) | 60.0 (1.5) | 50.4 (1.5) | 18.3†† | .33 | 63.9 (1.8) | 69.9 (1.9) | 52.6 (1.7) | 24.7†† | .44 |
| Somatic complaints | 60.2 (1.3) | 57.9 (1.4) | 50.6 (1.4) | 13.3†† | .26 | 65.1 (1.9) | 65.0 (2.0) | 54.4 (1.7) | 11.7†† | .27 |
| Anxious/depressed | 70.4 (1.7) | 62.4 (1.8) | 50.2 (1.8) | 32.5** | .46 | 64.4 (1.6) | 66.7 (1.7) | 51.2 (1.5) | 29.6†† | .49 |
| Social problems | 62.9 (1.4) | 58.2 (1.5) | 51.3 (1.5) | 15.7†† | .30 | 57.2 (1.2) | 58.7 (1.3) | 50.7 (1.1) | 13.2†† | .30 |
| Thought problems | 59.1 (1.3) | 55.3 (1.4) | 51.2 (1.4) | 8.6†† | .19 | 58.1 (1.4) | 58.8 (1.4) | 51.1 (1.2) | 10.9†† | .26 |
| Attention problems | 67.3 (1.6) | 62.8 (1.7) | 51.0 (1.7) | 24.5†† | .39 | 61.7 (1.5) | 63.6 (1.5) | 50.9 (1.3) | 23.5†† | .43 |
| Delinquent behavior | 69.4 (1.3) | 59.4 (1.4) | 52.8 (1.4) | 38.4** | .50 | 66.4 (1.6) | 59.7 (1.7) | 51.8 (1.5) | 22.5†† | .42 |
| Aggressive behavior | 60.6 (1.2) | 56.0 (1.3) | 50.7 (1.3) | 15.0†† | .29 | 60.3 (1.3) | 57.1 (1.4) | 51.2 (1.2) | 13.8†† | .31 |
| Total externalizing | 65.0 (1.7) | 55.5 (1.8) | 44.7 (1.8) | 34.5** | .48 | 62.0 (2.1) | 56.2 (2.3) | 42.6 (2.0) | 23.7†† | .43 |
| Total internalizing | 66.2 (1.8) | 60.5 (1.9) | 40.6 (1.9) | 50.1†† | .57 | 65.8 (2.0) | 69.4 (2.1) | 46.0 (1.8) | 43.5†† | .58 |
|
| ||||||||||
| n = 28 | n = 26 | n = 26 | n = 28 | n = 26 | n = 26 | |||||
|
| ||||||||||
| DSM-IV scales (YI and ASI)2 | ||||||||||
| ADHD combined type | 24.6 (1.6) | 23.8 (1.7) | 10.0 (1.7) | 23.9†† | .37 | 14.5 (1.6) | 18.4 (1.6) | 6.2 (1.6) | 16.2†† | .29 |
| Conduct disorder | 5.4 (0.5) | 3.0 (0.5) | 0.4 (0.5) | 23.7** | .37 | 4.3 (0.8) | 3.0 (0.8) | .39 (0.8) | 15.9†† | .29 |
| Oppositional defiant disorder | 10.5 (0.8) | 8.6 (0.8) | 3.6(0.8) | 21.0†† | .34 | 10.4 (1.0) | 10.1 (1.0) | 3.7 (1.0) | 15.0†† | .28 |
| Generalized anxiety | 14.3 (0.9) | 12.5 (0.9) | 4.7 (0.9) | 33.2†† | .45 | 10.0 (0.7) | 10.3 (0.7) | 3.4 (0.7) | 32.4†† | .46 |
| Obsessive compulsive disorder | 2.6 (0.9) | 1.6 (0.9) | 0.3 (0.9) | 19.9†† | .33 | .82 (0.2) | .96 (0.2) | .12 (0.2) | 15.0†† | .17 |
| Post-traumatic stress | 3.9 (0.3) | 2.5 (0.3) | 0.4 (0.3) | 31.3** | .44 | 2.2 (0.3) | 0.2 (0.3) | 1.6 (0.3) | 14.4†† | .27 |
| Social phobia | 2.2 (0.3) | 2.2 (0.3) | 0.6 (0.3) | 22.9†† | .16 | |||||
| Separation anxiety | 1.7 (0.4) | 2.5 (0.4) | 0.3 (0.4) | 34.5 | .17 | 1.3 (0.5) | 2.4 (0.6) | 0.5 (0.6) | 2.9 | .07 |
| Schizoid personality | 2.0 (0.2) | 2.1 (0.2) | 1.2 (0.2) | 6.7 | .11 | 2.0 (0.3) | 2.6 (0.3) | 0.8 (0.3) | 11.3†† | .23 |
| Major depression | 14.6 (0.9) | 12.6 (0.9) | 3.8 (0.9) | 41.7†† | .51 | 10.3 (0.7) | 9.3 (0.8) | 0.8 (0.8) | 43.2** | .53 |
| Manic symptoms | 10.0 (0.7) | 8.6 (0.7) | 8.9 (0.7) | 1.2 | .03 | 5.3 (0.6) | 4.6 (0.6) | 1.7 (0.6) | 8.8†† | .19 |
| Anorexia | 4.3 (0.4) | 2.9 (0.4) | 1.5 (0.4) | 103†† | .20 | 1.6 (0.3) | 1.5 (0.3) | 0.6 (0.3) | 2.6†† | .06 |
| Bulimia | 3.3 (0.5) | 2.7 (0.5) | 0.7 (0.5) | 8.1†† | .16 | 1.4 (0.4) | 2.3 (0.4) | 0.6 (0.4) | 5.3 | .12 |
| Substance use | 3.7 (0.4) | 0.5 (0.5) | 0.3 (0.5) | 18.4** | .31 | 1.9 (0.3) | 0.7 (0.3) | 0.4 (0.3) | 15.1** | .28 |
| KSADS depression symptoms | 63.3 (1.6) | 54.7 (1.6) | 30.8 (1.6) | 115.7†† | .76 | 58.4 (1.5) | 55.4 (1.7) | 30.2 (1.6) | 94.8†† | .73 |
| KSADS manic symptoms | 11.4 (0.5) | 9.4 (0.5) | 8.8 (0.5) | 8.4** | .19 | 10.3 (0.4) | 9.0 (0.4) | 8.5 (0.4) | 5.6 † | .13 |
| Children’s Depression Inventory (CDI) | 68.8 (1.6) | 62.0 (1.7) | 41.3 (1.7) | 72.4** | .64 | |||||
Notes. YI = Youth’s Inventory; ASI = Adolescent Symptom Inventory; K-SADS = Kiddie Schedule for Affective Disorders and Schizophrenia.
T-scores.
Raw scores.
p ≤ .001 SII vs. typical adolescents only.
p ≤ .01 SII vs. typical adolescents only.
p ≤ .001 SII compared with both groups.
For YSR internalizing psychopathology, SII adolescents scored higher than controls across all five internalizing scales, and higher than depressed adolescents on the anxious/depressed scale, all ps ≤ .01 (see Table 2). For YSR externalizing T-scores, self-injuring adolescents scored higher than controls across all five externalizing subscales, all ps ≤ .001. Differences between the SII and depressed group included delinquent behavior and overall externalizing, both ps ≤ .001.
ANOVAs were also conducted on all CBCL scales. For internalizing psychopathology, self-injuring adolescents scored higher than controls on all five problem scales, all ps ≤ .01. However, the SII group did not differ from depressed adolescents on any CBCL internalizing scale. For the five externalizing scales, adolescents in the SII group scored higher than controls, all ps ≤ .001, but not higher that depressed participants.
Means for the continuous DSM-IV symptom scores are also presented by group in Table 2. Considerable psychopathology was observed among self-injuring adolescents. On the YI, SII adolescents reported higher symptom counts than control adolescents across nearly all (13 of 16) categories, all ps ≤ .01. The only exceptions were for separation anxiety, manic symptoms, and schizoid personality disorder, the latter two of which were rule-outs. Compared with those in the depressed group, SII adolescents scored higher on CD, PTSD, and substance use. Similarly, self-injuring adolescents scored higher than controls on nearly all diagnostic categories of the ASI (excluding separation anxiety, hyperactive symptoms of ADHD, and anorexia). However, they scored higher than the depressed comparison group only on the substance use scale, p < .01.
Group contrasts on other measures are also included in Table 2. Significant effects emerged for the CDI total T-score F(2, 81) = 72.4, p < .001, η2 = .64, self-reported depressive symptoms F(2, 74) = 115.7, p < .001 η2 = .76, and mother-reported depressive symptoms, F(2, 71) = 94.9, p < .001 η2 = .73. Group differences were also found for self-reported manic symptoms, F(2, 73) = 8.3, p = .001 η2 = .19, and mother-reported manic symptoms, F(2, 73) = 5.6, p < .01 η2 = .13. Self-injuring adolescents scored higher than both comparison groups on most of these measures of psychopathology, all ps ≤ .001, except for mother-reported depression and mania, where only the comparison between the SII and control group was significant, both ps < .012.
Substance use
Group differences were assessed with ANOVAs comparing frequency of use for tobacco, alcohol, marijuana, other substances, and total problems associated with use. Self-injuring adolescents reported higher rates of use than both comparison groups for tobacco, F(2, 81) = 11.5, p < .001 η2 = .22, and higher rates of marijuana use than typical controls, F(2, 81) = 6.4, p < .01 η2 = .14. Self-injuring adolescents had greater substance use problems than both depressed and typical adolescents F(2, 81) = 23.5, p < .001 η2 = .37.
BPD
Continuous measures of BPD criteria are presented by group in Table 3. As predicted, self-injuring adolescents scored higher on borderline pathology than depressed adolescents, even when excluding the self-harm criterion, F(2, 74) = 34.6 p < .001, η2 = .48. The SII group scored higher than both the depressed and control groups on SCID-II BPD features, p < .001. Follow-up tests comparing self-injuring teens with typical controls were significant for all criteria, all ps < .001. Self-injuring adolescents reported more self-damaging impulsivity and frantic efforts to avoid abandonment than depressed adolescents, both ps ≤ .001. Ten participants in the SII group met the full adult criteria for BPD on the SCID-II. Even though depressed participants showed elevations on some BPD criteria (the most common being chronic feelings of emptiness), only two participants in the depressed comparison group met criteria for BPD (Kruskal-Wallis test, p = .03). Thus, self-injuring adolescents, recruited solely based upon SII behavior, exhibited elevations in borderline pathology compared with both typical and clinical controls.
Table 3.
Patterns of Borderline Personality Criteria across Diagnostic Groups
| Self-Injuring (n = 27) | Depressed (n = 26) | Control (n = 24) | F | η2 | |
|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | |||
| Continuous borderline personality disorder (BPD) scores | |||||
| BPD | 9.9 (.7) | 4.7 (.7) | .08 (.7) | 51.2 | .58** |
| BPD without self-injury | 8.1 (.7) | 4.7 (.7) | .08 (.7) | 34.6 | .48** |
|
| |||||
| N (%)a | N (%) | N (%) | F | η2 | |
|
| |||||
| BPD criterion items | |||||
| Recurrent suicidal or self-mutilating behavior | 23 (85.2%) | 0 (0%) | 0 (0%) | 498.4 | .93** |
| Chronic feelings of emptiness | 15 (55.6%) | 9 (34.6%) | 0 (0%) | 23.7 | .39†† |
| Self-damaging impulsivity | 12 (44.4%) | 2 (7.7%) | 0 (0%) | 21.7 | .37** |
| Unstable interpersonal relationships | 11 (40.7%) | 5 (19.2%) | 0 (0%) | 9.0 | .20†† |
| Stress-related paranoia or dissociation | 11 (40.7%) | 5 (19.2%) | 0 (0%) | 10.1 | .22†† |
| Inappropriate intense anger | 11 (40.7%) | 4 (15.4%) | 0 (0%) | 13.0 | .26†† |
| Affective instability and mood reactivity | 10 (37.0%) | 6 (23.1%) | 0 (0%) | 12.3 | .25†† |
| Frantic efforts to avoid abandonment | 9 (33.3%) | 1 (3.8%) | 0 (0%) | 26.6 | .42** |
| Identity disturbance | 4 (14.8%) | 3 (11.5%) | 0 (0%) | 9.1 | .20†† |
| Number of participants meeting full diagnostic criteria | 10 (37.0%) | 2 (7.7%) | 0 (0%)* | ||
Notes.
Number and percentage meeting threshold criteria.
p ≤ .001 on comparison of SII vs. typical controls only.
p ≤ .001 on both comparisons (SII vs. depressed & SII vs. control).
Kruskal-Wallis ANOVA, p = .03.
Emotions and emotion dysregulation
Group differences in self-report measures of emotions and ER difficulties are presented in Table 4. ANOVAs examining total scores on emotion-related measures were significant for the DERS, F(2,82) = 50.1, p < .001, η2 = .55, the NMR, F(2,82) = 41.9, p < .001, η2 = .51, and the PAES, F(2,82) = 16.3, p < .001, η2 = .29. Follow-up contrasts indicated that those in the SII group reported more ER difficulties across all measures compared with typical controls. Compared with depressed participants, self-injuring adolescents scored higher on the DERS impulse control subscale and the DERS total score, both ps <.001. These were the only emotion regulation variables that differentiated the two clinical groups.
Table 4.
Measures of Emotions and Emotion Regulation
| Self-Injuring | Depressed | Control | |||
|---|---|---|---|---|---|
| Item | n = 29 | n = 28 | n = 27 | F | η2 |
| M (SD) | M (SD) | M (SD) | |||
| DERS | |||||
| Total | 3.1 (.11) | 2.6 (.11) | 1.6 (.11) | 50.1** | .55 |
| Acceptance | 2.9 (.17) | 2.2 (.17) | 1.5 (.17) | 18.6†† | .32 |
| Goals | 3.4 (.18) | 3.4 (.18) | 2.0 (.18) | 20.7†† | .34 |
| Impulse Control | 2.8 (.14) | 2.0 (.14) | 1.2 (.15) | 29.3** | .42 |
| Awareness | 3.0 (.17) | 2.9 (.18) | 2.0 (.18) | 10.2†† | .20 |
| Strategies | 3.2 (.15) | 2.7 (.15) | 1.7 (.16) | 39.4†† | .49 |
| Clarity | 3.2 (.15) | 2.7 (.15) | 1.7 (.16) | 24.3†† | .38 |
| NMR Total | 81.9 (3.1) | 89.1 (3.1) | 120.5 (3.2) | 41.9†† | .51 |
| PAES | |||||
| Anger Out | 10.2 (.40) | 8.9 (.41) | 6.9 (.42) | 16.3†† | .29 |
| Anger Suppression | 10.0 (.44) | 10.1 (.45) | 10.2 (.46) | 0.1 | .00 |
| Anger Control | 9.7 (.34) | 10.8 (.34) | 12.9 (.35) | 22.9†† | .36 |
Notes: DERS = Difficulty with Emotion Regulation Scale; NMR = Negative Mood Regulation; PAES = Pediatric Anger Expression Scale.
p ≤ .001 on comparison of SII vs. typical controls only.
p ≤ .001 on both comparisons (SII vs. depressed & SII vs. control).
Psychophysiological Data
EDR
We assessed group differences in EDR at rest and during the emotion-induction task (The Champ). To test for resting differences in EDR, a multilevel model (MLM) was created that included four non-task epochs (2 pre-induction, 2 post-induction) as a repeated measures outcome variable. Analyses were conducted using HLM 6.08 (Raudenbush, Bryk, & Congdon, 2000). The full maximum likelihood model followed this form:
At Level 1, intercepts and slopes in physiological responding were grand mean-centered across resting epochs. At Level 2, nested orthogonal group contrasts (clinical vs. typical controls, SII vs. depressed) and age were added as predictors of Level 1 slopes and intercepts. In addition to resting EDR, a parallel model was created examining EDR across the six epochs of the emotion-induction task, where Champ EDR was entered as the Level 1 outcome variable.
As predicted, there was a negative coefficient for the resting EDR intercept on the comparison of clinical vs. control (both depressed and typical) adolescents, β=−0.24, t(65) = −1.95, p = .05, and between self-injuring and depressed adolescents, β=−0.52, t(65) = −2.05, p = .04. Thus, lower EDR was observed among self-injuring participants. This finding is presented in Figure 1. The model predicting changes in EDR across The Champ was not significant, all βs ≤ 0.04, all ts(65) ≥ −1.65, all ps ≥ .10.
Figure 1.
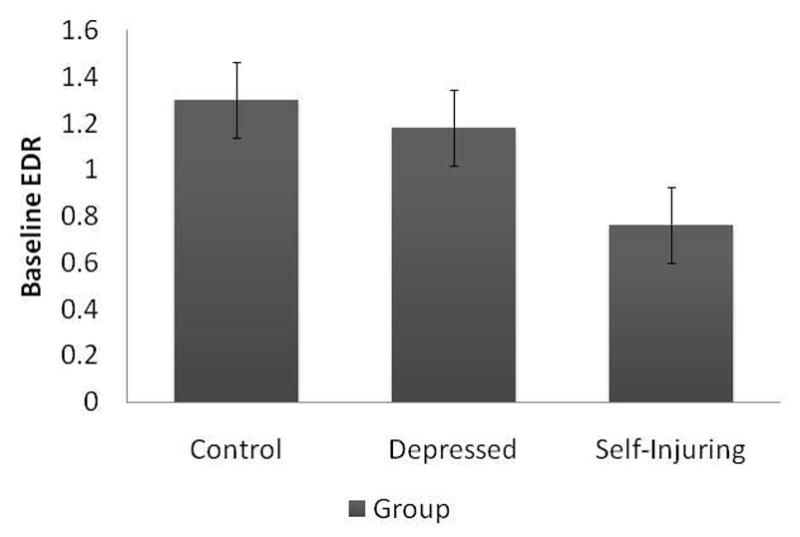
Resting Differences in Electrodermal Responding Across Groups
Discussion
With this study, we sought to identify factors that differentiate self-injuring adolescents from depressed adolescents with no SII history and typical controls. We hypothesize that the diagnostic and biological features that differentiate these groups are potential markers of heightened risk for BPD. This is not the only study finding that self-injuring adolescents meet diagnostic criteria for disorders other than depression (e.g., Crowell et al., 2005; Nock, Hwang, Sampson, & Kessler, 2010; Nock et al., 2006). However, our study is the first to compare self-injuring adolescent females with depressed and typical control groups across self-report, mother-report, and autonomic assessments. One major contribution of this study is the inclusion of a depressed comparison group that was similar to self-injuring participants across many parent- and self-report measures of concurrent impairment.
Factors that differentiated SII from depressed adolescents included self-reported anxiety/depression, delinquent behavior, conduct disorder, broad externalizing scores, PTSD symptoms, and both parent- and self-reports of adolescent substance use. Additionally, adolescents in the SII group reported higher depression and manic symptoms on the K-SADS, higher levels of suicidal ideation, greater hopelessness, more tobacco use, and higher emotion dysregulation and impulsivity. The two BPD criteria that differentiated SII from depressed participants were impulsive behaviors (e.g., shoplifting) and frantic efforts to avoid abandonment (e.g., threatening, pleading). In addition, the SII group scored higher than typical controls on nearly all measures of psychopathology and behavior problems, replicating and extending our previous work conducted without a psychiatric control group (Crowell et al., 2005).
Self-injuring adolescents also exhibited lower resting EDR than both the depressed and typical control groups. As reviewed above, attenuated EDR is a biomarker associated reliably with externalizing behavior disorders, and is believed to relate specifically to impulsivity/behavioral disinhibition (see Beauchaine, 2001; Fowles, 1988, 2000). Attenuated EDR is consistent with models of borderline personality development that specify heritable externalizing vulnerability as an etiological factor (Beauchaine et al., 2009; Crowell et al., 2009).
Possible Implications for Borderline Personality Development
Although there is a growing literature on the development of BPD, researchers have only begun to identify developmental precursors and longitudinal trajectories leading to the disorder (Crawford et al., 2006; Johnson et al., 1999; Lenzenweger & Cicchetti, 2005; Yen et al., 2004). With this study we found a coherent pattern of differences between self-injuring and depressed adolescents, including biological, self- and mother-reported differences across measures of externalizing vulnerability. This suggests that SII may differ from depression in its origins and developmental course. Our findings also reveal that by adolescence, self-injuring teens show higher levels of borderline pathology compared with depressed, non-self-injuring adolescents. Nevertheless, future studies should follow both groups into adulthood to determine which adolescents manifest continued problems during this critical developmental transition.
It is noteworthy that many of the depressed adolescents also showed subthreshold elevations on BPD symptoms, and that two depressed adolescents met diagnostic criteria. Without longitudinal data it is unclear which depressed adolescents, if any, are at risk for adult BPD, or whether predictors other than self-injury are better prospective markers of risk (e.g., severity of psychopathology, number of comorbid diagnoses, interpersonal conflict). Moreover, relative to adult studies of BPD, our sample is small. Thus, we were not able to examine, for example, potential moderators (e.g., BPD symptoms) of psychophysiological responding. The sample was also too small to perform subgroup analyses for adolescents who met criteria for BPD. Finally, this sample includes only self-injuring females and their mothers. Future research should examine whether the diagnostic and physiological correlates of self-injury are similar among adolescent males. It is possible that self-injuring males will show developmental trajectories that differ from those seen among young women (Beauchaine et al., 2009).
Clinical Implications
Since the BPD literature has lacked a developmental focus, there are few prevention approaches targeted specifically toward youth at risk for later BPD. However, the common assumption that self-injury is an internalizing behavior problem—similar to depression—has implications for treatment development. This could influence downward extensions of efficacious adult interventions and which behavioral and pharmacological treatments are applied to self-injuring adolescents. Regardless of possible developmental outcomes, self-injuring girls may not respond adequately to interventions targeting only mood disorders. Indeed, there is long-standing evidence that treating Axis I disorders alone may be insufficient to reduce suicidality, delinquency, academic failure, interpersonal problems, and substance use among those with borderline traits (e.g., Kernberg, Weiner, & Bardenstein, 2000; Linehan, 1993). For example, in a longitudinal study of adults with co-occurring depression and BPD, remission of BPD was not affected by the presence of MDD; however, the presence of BPD delayed improvements in MDD significantly (Gunderson et al., 2004). In other words, improvements in MDD were predicted by prior improvements in BPD but not vice versa.
Identifying whether BPD features are present may also improve care for self-injuring and depressed adolescents. In addition to targeting negative mood, interventions that address impulsive behaviors, interpersonal conflict, and other BPD traits are most likely to help these adolescents. Dialectical behavior therapy is one such treatment, and has been modified recently for younger populations (Miller et al., 2007). Our results are consistent with treatment-outcome studies finding that self-injuring adolescents differ from depressed teenagers and may therefore require more targeted forms of care (Wilkinson et al., 2011).
Acknowledgments
This work was supported by grants F31 MH074196 to Sheila E. Crowell and R01 MH63699 to Theodore P. Beauchaine from the National Institute of mental Health
Footnotes
Although this study is cross sectional and does not provide for direct inferences about borderline personality development, self-inflicted injury (SII) is a fruitful criterion to examine as a potential precursor to BPD (Crowell et al., 2009). As stated previously, most who self-injure are both impulsive and dysregulated emotionally—core features of BPD (e.g., Trull et al., 2003; Zlotnick et al., 1997). Self-injury also emerges in adolescence, often before other BPD criteria (Kessler et al., 1999; Yen et al., 2004). Moreover, although SII is observed without BPD, their high co-occurrence likely results from shared biological vulnerabilities (e.g., genetic, neural), contextual risk factors (e.g., early adversity), and acquired coping strategies (e.g., self-injury) (see Beauchaine et al., 2009). Rates of SII among adults with BPD are also extremely high, with 40–90% attempting suicide or engaging in non-suicidal self-injury at some point in their lifetimes (APA; 2004), and nearly two-thirds first initiating self-injury before age 18. Moreover, about 50% of adolescent self-injurers can be diagnosed with BPD, with no adjustment to adult criteria (Nock et al., 2006). Finally, there is an extensive literature linking adolescent SII to personality disorders, especially borderline and antisocial pathologies (Brent et al., 1994; Clarkin et al., 1984; Johnson et al., 1999; Linehan, Rizvi, et al., 2006; Marton et al., 1989; Marttunen et al., 1994; Pfeffer et al., 1991; Runeson & Beskow, 1991).
At the time of the assessment, 20 SII and 15 depressed adolescents met full diagnostic criteria for depression on the Youth’s Inventory. This difference was not significant, Mann-Whitney U, p = .085.
References
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991a. [Google Scholar]
- Achenbach TM. Manual for the youth self-report and profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991b. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, D.C: Author; 2000. Text Revision. [Google Scholar]
- American Psychiatric Association. Practice guidlines for the treatment of psychiatric disorders. Washington, DC: Author; 2004. [Google Scholar]
- American Psychiatric Association. DSM-5 development: Non-suicidal self-injury. 2010 Retrieved April, 14, 2010, from http://www.dsm5.org/ProposedRevisions/Pages/proposedrevision.aspx?rid=443.
- Arango V, Huang YY, Underwood MD, Mann JJ. Genetics of the serotonergic system in suicidal behavior. Journal of Psychiatric Research, Brain Imaging, and Post-Mortem Studies in Affective Disorders. 2003;37:375–386. doi: 10.1016/s0022-3956(03)00048-7. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP. Vagal tone, development, and Gray’s motivational theory: Toward an integrated model of autonomic nervous system functioning in psychopathology. Development and Psychopathology. 2001;13:183–214. doi: 10.1017/s0954579401002012. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Katkin ES, Strassberg Z, Snarr J. Disinhibitory psychopathology in male adolescents: Discriminating conduct disorder from attention-deficit/hyperactivity disorder through concurrent assessment of multiple autonomic states. Journal of Abnormal Psychology. 2001;110:610–624. doi: 10.1037//0021-843x.110.4.610. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Klein DN, Crowell SE, Derbidge C, Gatzke-Kopp LM. Multifinality in the development of personality disorders: A Biology × Sex × Environment interaction model of antisocial and borderline traits. Development and Psychopathology. 2009;21:735–770. doi: 10.1017/S0954579409000418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenner SL, Beauchaine TP, Sylvers PD. A comparison of psychophysiological and self-report measures of BAS and BIS activation. Psychophysiology. 2005;42:108–115. doi: 10.1111/j.1469-8986.2005.00261.x. [DOI] [PubMed] [Google Scholar]
- Brent DA, Johnson BA, Perper J, Connolly J, Bridge J, Bartle S, et al. Personality disorder, personality traits, impulsive violence, and completed suicide in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;32:69–75. doi: 10.1097/00004583-199410000-00003. [DOI] [PubMed] [Google Scholar]
- Brezo J, Bureau A, Merette C, Jomphe V, Barker ED, Vitaro F, et al. Differences and similarities in the serotonergic diathesis for suicide attempts and mood disorders: A 22-year longitudinal gene-environment study. Molecular Psychiatry. 2010;15:831–843. doi: 10.1038/mp.2009.19. [DOI] [PubMed] [Google Scholar]
- Catanzaro SJ, Mearns J. Measuring generalized expectancies for negative mood regulation: Initial scale development and implications. Journal of Personality Assessment. 1990;54:546–563. doi: 10.1080/00223891.1990.9674019. [DOI] [PubMed] [Google Scholar]
- Clarkin JF, Friedman RC, Hurt SW, Corn R, Aronoff M. Affective and character pathology of suicidal adolescent and young adult inpatients. Journal of Clinical Psychiatry. 1984;45:19–22. [PubMed] [Google Scholar]
- Crawford TN, Shaver PR, Cohen P, Pilkonis PA, Gillath O, Kasen S. Self-reported attachment, interpersonal aggression, and personality disorder in a prospective community sample of adolescents and adults. Journal of Personality Disorders. 2006;20:331–351. doi: 10.1521/pedi.2006.20.4.331. [DOI] [PubMed] [Google Scholar]
- Crosby AE, Cheltenham MP, Sacks JJ. Incidence of suicidal ideation and behavior in the United States, 1994. Suicide and Life-Threatening Behavior. 1999;30:177–179. [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, Gatzke-Kopp L, Sylvers PD, Mead H, Chipman-Chacon J. Autonomic correlates of attention-deficit/hyperactivity disorder and oppositional defiant disorder in preschool children. Journal of Abnormal Psychology. 2006;115:174–178. doi: 10.1037/0021-843X.115.1.174. [DOI] [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, Linehan MM. A biosocial developmental model of borderline personality: Elaborating and extending Linehan’s theory. Psychological Bulletin. 2009;135:495–510. doi: 10.1037/a0015616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, McCauley E, Smith C, Stevens AL, Sylvers PD. Psychological, physiological, and serotonergic correlates of parasuicidal behavior among adolescent girls. Development and Psychopathology. 2005;17:1105–1127. doi: 10.1017/s0954579405050522. [DOI] [PubMed] [Google Scholar]
- Ebner-Priemer UW, Badeck S, Beckmann C, Wagner A, Feige B, Weiss I, et al. Affective dysregulation and dissociative experience in female patients with borderline personality disorder: A startle response study. Journal of Psychiatric Research. 2005;39:85–92. doi: 10.1016/j.jpsychires.2004.05.001. [DOI] [PubMed] [Google Scholar]
- Esposito C, Spirito A, Boergers J, Donaldson D. Affective, behavioral, and cognitive functioning in adolescents with multiple suicide attempts. Suicide and Life-Threatening Behavior. 2003;33:389–399. doi: 10.1521/suli.33.4.389.25231. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. User’s guide for the Structured Clinical Interview for DSM-IV personality disorders (SCID-II) Washington: American Psychiatric Press; 1996. [Google Scholar]
- Fowles DC. Electrodermal hyporeactivity and antisocial behavior: Does anxiety mediate the relationship? Journal of Affective Disorders. 2000;61:177–189. doi: 10.1016/s0165-0327(00)00336-0. [DOI] [PubMed] [Google Scholar]
- Gadow KD, Sprafkin J, Carlson G, Schneider J, Nolan EE, Mattison RE, et al. A DSM-IV-referenced adolescent self-report rating scale. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:671–679. doi: 10.1097/00004583-200206000-00006. [DOI] [PubMed] [Google Scholar]
- Gratz KL. Risk factors for deliberate self-harm among female college students: The role and interaction of childhood maltreatment, emotional inexpressivity, and affect intensity/reactivity. American Journal of Orthopsychiatry. 2006;76:238–250. doi: 10.1037/0002-9432.76.2.238. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;26:41–54. [Google Scholar]
- Gross JJ, Levenson RW. Emotion elicitation using films. Cognition and Emotion. 1995;9:87–108. [Google Scholar]
- Gunderson JG, Morey LC, Stout RL, Skodol AE, Shea MT, McGlashan TH, et al. Major depressive disorder and borderline personality disorder revisited: Longitudinal interactions. Journal of Clinical Psychiatry. 2004;65:1049–1056. doi: 10.4088/jcp.v65n0804. [DOI] [PubMed] [Google Scholar]
- Hawkins J, Catalano R. Unpublished survey. Center for Law and Justice; 2001. Social development of youth project, third and ninth grade survey. [Google Scholar]
- Herpertz SC, Kunert HJ, Schwenger UB, Sass H. Affective responsiveness in borderline personality disorder: A psychophysiological approach. American Journal of Psychiatry. 1999;156:1550–1556. doi: 10.1176/ajp.156.10.1550. [DOI] [PubMed] [Google Scholar]
- Hilt LM, Cha CB, Nolen-Hoeksema S. Nonsuicidal self-injury in young adolescent girls: Moderators of the distress-function relationship. Journal of Consulting and Clinical Psychology. 2008;76:63–71. doi: 10.1037/0022-006X.76.1.63. [DOI] [PubMed] [Google Scholar]
- Hooley JM. Self-harming behavior: Introduction to the special series on non-suicidal self-injury and suicide. Applied and Preventive Psychology. 2008;12:155–158. [Google Scholar]
- Jacobs GA, Phelps M, Rohrs B. Assessment of anger expression in children: The Pediatric Anger Expression Scale. Personality and Individual Differences. 1989;10:59–65. [Google Scholar]
- Jandl M, Steyer J, Kaschka WP. Suicide risk markers in major depressive disorder: A study of electrodermal activity and event-related potentials. Journal of Affective Disorders. 2010;123:138–149. doi: 10.1016/j.jad.2009.09.011. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Gould MS, Kasen S, Brown J, Brook JS. Childhood adversities, interpersonal difficulties, and risk for suicide attempts during late adolescence and early adulthood. Archives of General Psychiatry. 2002;59:741–749. doi: 10.1001/archpsyc.59.8.741. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Skodol AE, Oldham JM, Kasen S, Brook JS. Personality disorders in adolescence and risk of major mental disorders and suicidality during adulthood. Archives of General Psychiatry. 1999;56:805–811. doi: 10.1001/archpsyc.56.9.805. [DOI] [PubMed] [Google Scholar]
- Johnson PA, Hurley RA, Benkelfat C, Herpertz SC, Taber KH. Understanding emotion regulation in borderline personality disorder: Contributions of neuroimaging. Focus. 2005;3:478–483. doi: 10.1176/jnp.15.4.397. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kernberg PF, Weiner AS, Bardenstein KK. Personality disorders in children and adolescents. New York: Basic Books; 2000. [Google Scholar]
- Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Archives of General Psychiatry. 1999;56:617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- Klonsky ED. The functions of deliberate self-injury: A review of the evidence. Clinical Psychology Review. 2007;27:226–239. doi: 10.1016/j.cpr.2006.08.002. [DOI] [PubMed] [Google Scholar]
- Kopp M, Gruzelier J. Electrodermally differentiated subgroups of anxiety patients and controls. II: Relationships with auditory, somatosensory and pain thresholds, agoraphobic fear, depression and cerebral laterality. International Journal of Psychophysiology. 1989;7:65–75. doi: 10.1016/0167-8760(89)90032-9. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Children’s Depression Inventory. Niagra Falls, NY: Multi-Health Systems; 1992. [Google Scholar]
- Kring AM, Sloan DM, editors. Emotion regulation and psychopathology: A transdiagnostic approach to etiology and treatment. New York: The Guilford Press; 2010. [Google Scholar]
- Kuo JR, Linehan MM. Disentangling emotion processes in borderline personality disorder: Physiological and self-reported assessment of biological vulnerability, baseline intensity, and reactivity to emotionally evocative stimuli. Journal of Abnormal Psychology. 2009;118:531–544. doi: 10.1037/a0016392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenzenweger MF, Cicchetti D. Toward a developmental psychopathology approach to borderline personality disorder. Development and Psychopathology. 2005;17:893–898. doi: 10.1017/s095457940505042x. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Dialectical behavior therapy for borderline personality disorder: Theory and method. Bulletin of the Menninger Clinic. 1987;51:261–276. [PubMed] [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press; 1993. [Google Scholar]
- Linehan MM, Comtois KA. Unpublished Manuscript. 1996. Lifetime Parasuicide Count. [Google Scholar]
- Linehan MM, Comtois KA, Brown MZ, Heard HL, Wagner AW. Suicide attempt self-injury interview (SASII): Development, reliability, and validity of a scale to assess suicide attempts and intentional self-injury. Psychological Assessment. 2006;18:303–312. doi: 10.1037/1040-3590.18.3.303. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Rizvi SL, Welch SS, Page B. Suicide and personality disorders. In: Hawton K, van Heeringen K, editors. International handbook of suicide and attempted suicide. Chichester, UK: Wiley; 2006. pp. 147–178. [Google Scholar]
- Lloyd-Richardson EE, Perrine N, Dierker L, Kelley ML. Characteristics and functions of non-suicidal self-injury in a community sample of adolescents. Psychological Medicine. 2007;37:1183–1192. doi: 10.1017/S003329170700027X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorber MF. Psychophysiology of aggression, psychopathy, and conduct problems: A meta-analysis. Psychological Bulletin. 2004;130:531–552. doi: 10.1037/0033-2909.130.4.531. [DOI] [PubMed] [Google Scholar]
- Marsh P, Beauchaine TP, Williams B. Dissociation of sad facial expressions and autonomic nervous system responding in boys with disruptive behavior disorders. Psychophysiology. 2008;45:100–110. doi: 10.1111/j.1469-8986.2007.00603.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marton P, Korenblum M, Kutcher S, Stein B, Kennedy B, Pakes J. Personality dysfunction in depressed adolescents. Canadian Journal of Psychiatry. 1989;34:810–813. doi: 10.1177/070674378903400814. [DOI] [PubMed] [Google Scholar]
- Marttunen MJ, Aro HM, Henriksson MM, Lönnqvist JK. Antisocial behaviour in adolescent suicide. Acta Psychiactra Scandinavica. 1994;89:167–173. doi: 10.1111/j.1600-0447.1994.tb08087.x. [DOI] [PubMed] [Google Scholar]
- Miller AL, Muehlenkamp JJ, Jacobson CM. Fact or fiction: Diagnosing borderline personality disorder in adolescents. Clinical Psychology Review. 2008;28:969–981. doi: 10.1016/j.cpr.2008.02.004. [DOI] [PubMed] [Google Scholar]
- Miller AL, Rathus JH, Linehan MM. Dialectical behavior therapy with suicidal adolescents. New York: The Guilford Press; 2007. [Google Scholar]
- National Center for Injury Prevention and Control. CDC Injury Fact Book. Atlanta, GA: Centers for Disease Control and Prevention; 2006. [Google Scholar]
- National Center for Injury Prevention and Control. CDC Injury Research Agenda, 2009–2018. 2009 Available from http://www.cdc.gov/injury/ResearchAgenda/index.html.
- Nock MK. Why do people hurt themselves? Current Directions in Psychological Science. 2009;18:78–83. doi: 10.1111/j.1467-8721.2009.01613.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Hwang I, Sampson NA, Kessler RC. Mental disorders, comorbidity and suicidal behavior: Results from the National Comorbidity Survey Replication. Molecular Psychiatry. 2010;15:868–876. doi: 10.1038/mp.2009.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Joiner TE, Gordon KH, Lloyd-Richardson E, Prinstein MJ. Non-suicidal self-injury among adolescents: Diagnostic correlates and relation to suicide attempts. Psychiatry Research. 2006;144:65–72. doi: 10.1016/j.psychres.2006.05.010. [DOI] [PubMed] [Google Scholar]
- Nock MK, Prinstein MJ. Contextual features and behavioral functions of self-mutilation among adolescents. Journal of Abnormal Psychology. 2005;114:140–146. doi: 10.1037/0021-843X.114.1.140. [DOI] [PubMed] [Google Scholar]
- Norris CJ, Larsen JT, Cacioppo JT. Neuroticism is associated with larger and more prolonged electrodermal responses to emotionally evocative pictures. Psychophysiology. 2007;44:823–826. doi: 10.1111/j.1469-8986.2007.00551.x. [DOI] [PubMed] [Google Scholar]
- Papousek I, Schulter G. Associations between EEG asymmetries and electrodermal lability in low vs. high depressive and anxious normal individuals. International Journal of Psychophysiology. 2001;41:105–117. doi: 10.1016/s0167-8760(01)00131-3. [DOI] [PubMed] [Google Scholar]
- Paris J, Zweig-Frank H, Ng Ying Kin NMK, Schwartz G, Steiger H, Nair NPV. Neurobiological correlates of diagnosis and underlying traits in patients with borderline personality disorder compared with normal controls. Psychiatry Research. 2004;121:239–252. doi: 10.1016/s0165-1781(03)00237-3. [DOI] [PubMed] [Google Scholar]
- Pfeffer CR, Klerman GL, Hurt SW, Lesser M, Peskin JR, Siefker CA. Suicidal children grow up: Demographic and clinical risk factors for adolescent suicide attempts. Journal of the American Academy of Child and Adolescent Psychiatry. 1991;30:609–616. doi: 10.1097/00004583-199107000-00013. [DOI] [PubMed] [Google Scholar]
- Plener PL, Libal G, Keller F, Fegert JM, Muehlenkamp JJ. An international comparison of adolescent non-suicidal self-injury (NSSI) and suicide attempts: Germany and the USA. Psychological Medicine. 2009;39:1549–1558. doi: 10.1017/S0033291708005114. [DOI] [PubMed] [Google Scholar]
- Preskorn SH, Baker B. The overlap of DSM-IV syndromes: Potential implications for the practic of psychopharmacology, psychiatric drug development, and the human genome project. Journal of Psychiatric Practice. 2002;8:170–177. doi: 10.1097/00131746-200205000-00006. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS, Congdon RT. HLM 6: Hierarchical linear and nonlinear modeling. Chicago: Scientific Software International; 2000. [Google Scholar]
- Ross S, Heath N. A study of the frequency of self-mutilation in a community sample of adolescents. Journal of Youth and Adolescence. 2002;31:67–77. [Google Scholar]
- Runeson B, Beskow J. Borderline personality disorder in young Swedish suicides. Journal of Nervous and Mental Disease. 1991;179:153–156. doi: 10.1097/00005053-199103000-00007. [DOI] [PubMed] [Google Scholar]
- Schmahl CG, Elzinga BM, Ebner UW, Simms T, Sanislow C, Vermetten E, et al. Psychophysiological reactivity to traumatic and abandonment scripts in borderline personality and posttraumatic stress disorders: A preliminary report. Psychiatry Research. 2004;126:33–42. doi: 10.1016/j.psychres.2004.01.005. [DOI] [PubMed] [Google Scholar]
- Skegg K. Self-harm. The Lancet. 2005;366:1471–1483. doi: 10.1016/S0140-6736(05)67600-3. [DOI] [PubMed] [Google Scholar]
- Stanger C, Lewis M. Agreement among parents, teachers, and children on internalizing and externalizing behavior problems. Journal of Clinical Child Psychology. 1993;22:107–116. [Google Scholar]
- Thorell LH. Valid electrodermal hyporeactivity for depressive suicidal propensity offers links to cognitive theory. Acta Psychiatrica Scandinavica. 2009;119:338–349. doi: 10.1111/j.1600-0447.2009.01364.x. [DOI] [PubMed] [Google Scholar]
- Trull TJ, Stepp SD, Durrett CA. Research on borderline personality disorder: An update. Current Opinion in Psychiatry. 2003;16:77–82. [Google Scholar]
- U.S. Public Health Service. The surgeon general’s call to action to prevent suicide. Washington, DC: 1999. [Google Scholar]
- Vasilev CA, Crowell SE, Beauchaine TP, Mead HK, Gatzke-Kopp LM. Correspondence between physiological and self-report measures of emotion dysregulation: A longitudinal investigation of youth with and without psychopathology. Journal of Child Psychology and Psychiatry. 2009;50:1357–1364. doi: 10.1111/j.1469-7610.2009.02172.x. [DOI] [PubMed] [Google Scholar]
- Wilkinson P, Kelvin R, Roberts C, Dubicka B, Goodyer I. Clinical and psychosocial predictors of suicide attempts and nonsuicidal self-injury in the adolescent depression antidepressants and psychotherapy trial (ADAPT) American Journal of Psychiatry. 2011;168:495–501. doi: 10.1176/appi.ajp.2010.10050718. [DOI] [PubMed] [Google Scholar]
- Williams F, Hasking P. Emotion regulation, coping and alcohol use as moderators in the relationship between non-suicidal self-injury and psychological distress. Prevention Science. 2010;11:33–41. doi: 10.1007/s11121-009-0147-8. [DOI] [PubMed] [Google Scholar]
- Yen S, Shea MT, Sanislow CA, Grilo CM, Skodol AE, Gunderson JG, et al. Borderline personality disorder criteria associated with prospectively observed suicidal behavior. American Journal of Psychiatry. 2004;161:1296–1298. doi: 10.1176/appi.ajp.161.7.1296. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Donaldson D, Spirito A, Pearlstein T. Affect regulation and suicide attempts in adolescent inpatients. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:793–798. doi: 10.1097/00004583-199706000-00016. [DOI] [PubMed] [Google Scholar]


