Abstract
Retroviral coinfections with HIV-1 and HTLV-1 or with HIV-1 and HTLV-2 occur with variable frequencies throughout the world with the highest prevalence in large metropolitan areas in the Americas, Europe, and Africa. The recognition that retroviral coinfections exist dates back to the discovery of HIV-1 over 25 years ago. Despite the large body of published information regarding the biological and clinical significance of retroviral coinfections, controversy throughout several decades of research was fueled by several flawed epidemiologic studies and anecdotal reports that were not always supported with ample statistical and scientific evidence. However, the growing consensus obtained from recent systematic and well-devised research provides support for at least three conclusions: (1) HIV-1 and HTLV-1 coinfections are often seen in the context of patients with high CD4+ T cell counts presenting with lymphoma or neurological complications; (2) HIV-1 and HTLV-2 coinfections have been linked in some cases to a “long term nonprogressor” phenotype; and (3) differential function and/or overexpression of the HTLV-1 and HTLV-2 Tax proteins likely play a pivotal role in the clinical and immunologic manifestations of HIV/HTLV-1 and -2 coinfections. This review will recount the chronology of work regarding retroviral coinfections from 1983 through the present.
Introduction
The recognition that coinfections with multiple retroviruses occur is not new, yet debate continues regarding their clinical and biological significance. In the case of HIV-1/HIV-1 coinfections, both intrasubtype and intersubtype infections have been described.1,2 On one hand, intrasubtype HIV-1 superinfections are known to occur following infection with the founder strain, but apparently this is a relatively uncommon event.3,4 On the other hand, intersubtype HIV-1 superinfections may occur more frequently, and these have been associated with recombination events leading to major shifts in the biological characteristics of the virus.5,6 Therefore, these recombination events may have great significance in view of the fact that they contribute to rapid genetic evolution of HIV-1, which clearly is an obstacle with respect to devising therapeutic and vaccine targets against HIV-1.7
As we look at more divergent retroviruses such as HTLV-1 and HTLV-2, it is known that HIV-1/HTLV coinfections occur with greater frequency.8–14 This is particularly the case in large metropolitan areas where HIV-1 and HTLV-1/2 viral transmission events occur through sharing of needles and through sexual activities. HTLV-1 and HTLV-2 have a worldwide distribution; prevalence rates range from 5% to 27%, with the higher rates occurring in certain populations in which HTLV-1 is highly endemic.15,16 In the United States, HTLV-1/2 seroprevalence rates range from 0.025% in blood donors to 7–49% among injection drug users (IDUs) and commercial sex workers (CSWs), but lower rates among men having sex with men (MSM).15 Serologic assays that reliably distinguish between HTLV-1 and HTLV-2 have subsequently shown that the majority of HTLV infections in IDUs are caused by HTLV-2 infections.17,18 The origin of the HTLV-2 epidemic is not entirely defined but it is likely that the initial epidemic in the United States occurred in IDUs as early as the late 1960s.19 The first demonstration of HTLV-2 infections among European IDUs was in 1990.20 An extraordinarily high rate of HTLV-2 infections among South Vietnamese IDUs was probably introduced by U.S. military personnel during the Vietnam war.21 Despite the introduction of clean needle practices and needle exchange programs, the “intersecting epidemic,” or “syndemic” between HIV transmission and smoking of crack-cocaine among inner city adults is an additional risk factor for viral transmission events as a result of high-risk sexual behaviors during binging.22 While the National Institute of Drug Abuse reports a decline in crack-cocaine use in the United States, rates have steadily increased in other parts of the world.23
HIV-1/HTLV-1 and HIV-1/HTLV-2 coinfections probably occur more frequently than physicians are aware, since routine testing for HTLV-1/2 in outpatient clinics is not usually performed.8–13 It is estimated that rates of HTLV-1 or HTLV-2 coinfections in HIV-1-infected individuals are at least 100 to 500 times greater than in the general population.10–14 In some geographic regions 5–10% of HIV-1-infected individuals may be coinfected with HTLV-1 or HTLV-2.12–14
To make sense of a large body of published information pertaining to retroviral coinfections, this review will be organized as a chronology of key clinical and laboratory studies, starting with the identification of HTLV-1, HTLV-2, and HIV-1 in the early 1980s, recounting key seroepidemiological studies that provide a foundation for work done in the past decade.
The Early 1980s
Speculation of a possible association of human retroviruses and cancer during the 1970s fueled intense investigations that bore fruition in 1980 with the discovery of HTLV-1 as the causative agent of adult T cell leukemia/lymphoma (ATLL).24–26 The strategy employed by Yoshida and colleagues to characterize HTLV-1 employed the cocultivation of ATLL cells with cord blood lymphocytes, which resulted in the propagation of the HTLV-1-producing cell line known as MT-2.27 Discovery of the second human retrovirus, HTLV-2, followed in short order.28 Greater attention, however, was directed toward the link between HTLV-1 with ATLL and the neurodegenerative disease known as tropical spastic paraparesis/HTLV-1-associated myelopathy (TSP/HAM) or HAM/TSP, depending in which part of the world one resides.29,30
The discovery of the HTLV-III, also known as lymphadenopathy virus (LAV), as the causative agent of AIDS in 1983 followed the discovery of the first two human retroviruses.31,32 HTLV-III was propagated in the MT-2 derivative cell line, MT-4, producing HTLV-III-specific antigens within 24 h postinfection, yet eventually resulted in cytotoxicity and cell death.33 The recognition of HTLV-III as a virus separate and distinct from HTLV-1 and HTLV-2 resulted in its redesignation as HIV-1.34,35 This recognition evolved from several important lines of evidence: (1) HTLV-III was cytopathic for HTLV-transformed cells and indeed interrupted the transformation process.33 (2) While heteroduplexes of HTLV-1 and HTLV-2 demonstrated a significant amount of homology, HTLV-III molecular clones did not except in conserved regions of the gag/pol region.36 (3) While HTLV-1 and HTLV-2 could infect many cell types, initial infection of HTLV-III was observed to be restricted to cells bearing the CD4 cell surface receptor37 (4) ultrastructural studies distinguished key morphological differences.36,38 (5) And ultimately the complete nucleotide sequences of all three retroviruses were elucidated.39–41
Clinical and Biological Consequences of Retroviral Coinfections
Since HIV-1, HTLV-1, and HTLV-2 share tropism for T cells, retrovirologists were interested in studying the dynamics of retroviral coinfections in vivo and in vitro. Key questions to answer included the following: (1) Do HIV and HTLV inhabit the same cells? (2) Does the transactivating protein of one virus promote the replication of the other? (3) Does cross-immunity occur and if so, does immunity from the founder virus protect against infection with the second retrovirus? (4) Do retroviral coinfections broaden or alter cellular tropism for either HIV or HTLV? While answers to many of these challenging questions are still lacking, work related to the virology and immunopathology of retroviral coinfections will be summarized at the end of this review after reviewing the chronology of epidemiologic research concerning HIV/HTLV dual infections.
Early Epidemiologic Studies: 1983–1990
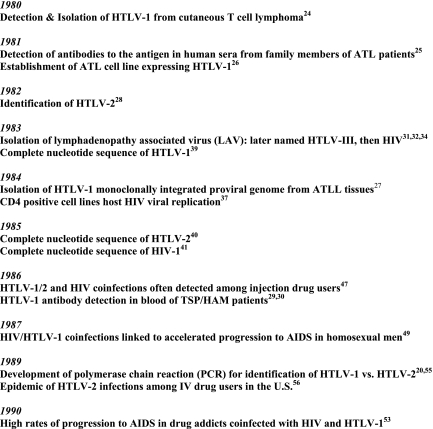
Early studies of retroviral coinfections focused on efforts to identify transmission events of both HIV-1 and HTLV-1 or HTLV-2 (Fig. 1). Seroprevalence data may have been somewhat flawed because of inadequately specific reagents to differentiate infections caused by different human retroviruses sharing antigenic cross-reactivity under lower stringency.42,43 Subsequent generation of higher stringency reagents quickly obviated these concerns.44 Purification of a homogeneic p24 Gag protein for use in a competition immunoassay showed that sera from 70% of AIDS patients and >90% of lymphadenopathy syndrome patients exhibited high-titered antibodies to HTLV-III p24 but not to analogous sequences of HTLV-1 and HTLV-2 p24.45 This work contributed to the renaming of HTLV-III to HIV-1 in recognition of the major genotypic and phenotypic characteristics distinguishing this virus from HTLV-1 and HTLV-2.34,35
FIG. 1.
Chronology of key events related to retroviral coinfections.
With all of this said, it still appeared certain that sera from some patients (especially hemophiliacs receiving cryoprecipitate, or patients who were transfusion dependent) contained antibodies to HTLV-1 (or HTLV-2) and HIV-1.46 One of the first studies to examine the prevalence of coinfections was a publication by Robert-Guroff et al. in which it was shown that approximately 7% of persons with AIDS or AIDS-related complex demonstrated coinfection with HTLV-1 (at that time differentiation between HTLV-1 and HTLV-2 was not possible).47 The only conclusion made by the authors was that HTLV-1 was not occurring in a sufficient frequency to be associated with AIDS. The host effects of HTLV-1 in this study were not determined.
1985–1990
During the latter half of the 1980s it was confirmed that cotransmission of HIV-1 and HTLV-1 was ongoing in Europe, the Americas, and Africa. Co transmission events were most commonly reported among a variety of risk groups, especially hemophiliacs, IDUs, MSM, and CSWs. A key study performed among New York IDUs in 1986 demonstrated that dual infections with HIV-1 and HTLV-1 or HIV-1 and HTLV-2 occurred in over 25% of African American IDUs tested.48 Bartholomew et al. (1987) reported that among 100 MSM in Trinidad, 15 were HTLV-1 infected, 34 were HIV-1 infected, and 6 were coinfected with both HTLV-1 and HIV-1. Among those coinfected, 3 of the 6 progressed to AIDS within 48 months of observation in contrast to only 3 out of the 34 who were infected with HIV-1 alone.49 While these numbers are small, the authors suggested that HTLV-1, through its transactivating gene, could amplify the cytopathic effects caused by HIV-1. In vitro research substantiating this hypothesis will be discussed later in this review. Similar conclusions were made by Hattori and colleagues, who reported that HTLV-1 coinfection occurred more frequently among HIV-infected hemophiliacs with AIDS, in contrast to HIV-infected hemophiliacs without AIDS.50 Additional case reports of dually infected patients developing aggressive lymphomas and death were in agreement with the assertion that HIV-1 and HTLV-1 coinfection leads to accelerated progression to AIDS.51,52 A third study conducted in Miami suggested that IDUs who were coinfected with both HIV-1 and HTLV-1 or HTLV-2 were three times more likely to die from AIDS during follow-up than were those infected with HIV-1 only.53 All three of these studies provided a consensus at that time that HTLV seropositivity adversely affected the clinical outcomes of persons with HIV-1. From a natural history perspective, this work is important because the patients were untreated with antiretroviral therapy. Also nearly all of the individuals in these studies were coinfected with HIV-1 and HTLV-1 and not HTLV-2. An additional limitation of these studies is the lack of information regarding time of onset of either HIV-1 or HTLV-1 infection.
Differentiation of HTLV-1 from HTLV-2 infections in many of the earlier studies was difficult because of the serological cross-reactivity of the assays employed during that time. The application of type-specific identification of HTLVs by polymerase chain reaction (PCR) helped to refine epidemiologic research. The use of PCR quickly and reliably demonstrated that a predominance of HTLV-2 infection existed among American and European IDUs whereas sexual transmission of HIV-1 with HTLV-1 predominated in the Caribbean, South America, Japan, and Africa.55–57 In contrast to HTLV-1, HTLV-2 was rarely implicated with malignancies or other disease, raising the question of whether coinfections with HIV-1 and HTLV-2 may result in the same clinical outcomes as those with HTLV-1. Therefore these molecular epidemiologic investigations prompted a number of investigations regarding the natural history of both HTLV-2 monoinfection and also HIV/HTLV-2 coinfections during the subsequent decades.
1990–2000
A recognition that HIV/HTLV-1 and HIV/HTLV-2 coinfections differed with respect to geographic area and risk factors was quite apparent by 1990. The clinical, virologic, and immunologic parameters associated with retroviral coinfections remained a work in process. Two large U.S. seroepidemiological studies were published in 1992.10,11 A CDC-sponsored study examined the seroprevalence of HTLV-1 and HTLV-2 in drug treatment centers and STD clinics in eight cities during 1988–1989.10 Again, as in previous investigations, IDU was strongly linked to infection with HTLV-2, and rates increased sharply with age. A second study published in that same year used specimens that were collected in 1987 from over 6000 patients attending sexually transmitted disease clinics in Baltimore and New Orleans, with approximately 5% of patient samples showing coinfection with HIV-1 and HTLV-1 or HTLV-2.11 In both cities, HTLV-1/2 seroprevalence increased significantly with age. Most patients attending the clinic were African American men. Overall, the seroprevalence of HTLV-1/2 infection was higher in women than men, but this difference was significant only in older subjects in New Orleans. IDUs were identified to be at highest risk, followed by sexual partners of IDUs or MSM. A Western blot algorithm was used in attempt to differentiate HTLV-1 from HTLV-2 infections but was later proven to show erroneous results in some cases.58 However, both HTLV-1 and HTLV-2 infections were observed among HIV-1-infected individuals at both sites.
The pair of 1992 studies did not specifically address the health outcomes associated with dual infections. However, several large studies published during 1995–1998 did address this question and also took into account the differential virulence properties of HTLV-1 and HTLV-2. Chavance et al. suggested that HTLV-1 infection acquired during adulthood is a marker of high-risk behavior and that it might be associated with early or multiple exposures to HIV-1.59 They concluded that this may account for acceleration of HIV-1 disease progression in their cohort study of HIV/HTLV-1 coinfected individuals in Martinique. A study conducted by Gotuzzo et al. among Peruvian men with HIV-1/HTLV-1 dual infection arrived at a similar conclusion.60 The report prompted an editorial in the same publication, pointing out shortcomings in the study. For example, time of infection was not known, and longitudinal follow-up was not recorded.61 Other investigators also pointed out that quantifying CD4+ T cells as a mechanism for staging of HIV/HTLV-1 coinfection may lead to erroneous conclusions as a skewed subset of these patients presented with unexpectedly high CD4+ T cell counts.62
Hershow and his collaborators performed a careful study with good statistical analysis, which pooled information to assess the effects of HTLV-2 infection on progression of HIV infection among 370 IDUs.63 Dates of HIV seroconversion were also known. This team arrived at the conclusion that HTLV-2 did not appear to affect progression of HIV infection. The authors did acknowledge that there was a lack of uniformity among the study sites that could affect outcome surveillance, and that some sites had higher rates of progression to AIDS than others. Nonetheless, the studies of Chavance et al. and Hershow et al. illustrated the importance of discrimination between HTLV-1 and HTLV-2 as cofactors for HIV disease, since the viruses appeared to be resulting in divergent outcomes.
The application of the HIV-1 viral load assay as a standard of care became a key marker to assess the ability of HTLV-1 and HTLV-2 to exert direct effects on HIV-1 viral levels in the clinic setting. One of the first studies to apply the viral load assay was conducted in a large hospital in Brazil.64 A total of 23 subjects with HIV-1 and HTLV-1 had HIV-1 viral load measurements and were compared with 92 patients with HIV-1 monoinfection. Persons with HTLV-2 infection were excluded in this study. The investigators found no difference in HIV-1 viral copy number in singly versus dually infected patients, even after adjustment of the results for zidovudine use and CD4+ T cell counts. This study was a significant advance from earlier work done, not only because of the use of this critical virologic marker, but additionally because of the homogeneity of the study group and the ability to account for antiretroviral drug therapy and clinical staging based on CD4 counts. Unfortunately, despite the strengths of the study, clinical outcomes were not assessed in the patients tested.
Significance of Retroviral Infections among Patients Receiving Highly Active Antiretroviral Therapy (HAART)
Given lack of availability of potent antiretroviral therapy before 1996, the above studies essentially recounted the natural history of AIDS progression with HTLV-1 or HTLV-2 coinfection. With the introduction of protease inhibitors and nonnucleoside reverse transcriptase inhibitors in 1996, investigations would need to consider the ability of these potent combinations to significantly prolong the life of persons living with HIV. Additionally, various HAART regimens could be variably active against the replication of HTLV-1 or HTLV-2. Hill and colleagues had done some work to assess the differential effects of reverse transcriptase inhibitors on HTLV-1 viral replication,65 but the effects of newer drugs, including protease inhibitors, had not been addressed.
Coincidental to the availability of HAART, it seemed as though work to further elucidate the clinical, virologic, and immunologic parameters of HIV/HTLV coinfections was nearly at a standstill. The success of HAART coupled with data calling into question the significance of HIV/HTLV coinfection resulted in a decline in coinfection studies. Directors of most large HIV clinics did not view screening and testing for HTLV-1/2 infection to be a priority and some experts in fact discouraged testing.66 Few U.S. clinics incorporated baseline HTLV-1/2 testing of HIV-1-infected individuals outside the context of research. Thus, what information could be obtained subsequent to 1995 resided in only a few clinical settings in the United States, South America, and Europe.
Recent studies provide clinical, immunologic, and virologic information concerning dually infected patients in different parts of the world. Two teams in Spain and Italy reported upon coinfections with HIV-1 and HTLV-2 among IDUs.67,68 Turci et al. enrolled approximately 3600 Italian IDUs of white origin, beginning in 1986.67 Patients were followed clinically for outcomes including neurologic manifestations, pulmonary and urinary tract infections, liver disease, and development of opportunistic infections. Additionally, patients were screened for hepatitis C coinfection, and had serial monitoring of HIV-1 viral loads, T-lymphocyte subsets, HTLV-2 proviral loads, and HTLV-2 subtyping. Available for analysis were 2371 patients with HIV-1 infection, of whom 6.7% had HTLV-2 coinfection. Coinfections were associated with older age, higher baseline CD4+ and CD8+ T cell counts, and delayed progression to AIDS. The authors concluded that HTLV-2 exerted a protective role among coinfected IDUs. In this study, antiretroviral therapy had no demonstrable effects on HTLV-2 proviral load and in some cases was associated with a significant increase in HTLV-2 proviral copy number. Bassani et al. examined the influence of HTLV-2 coinfection on virological and immunological indices among treatment-naive, HIV-1-infected IDUs in Spain.68 Their findings corroborated the conclusions of Turci et al. HTLV-2 coinfection was linked to lower levels of HIV-1 RNA and a decrease in the CD38 immune activation marker on CD8+ T cells. Unfortunately, the study was limited only to the laboratory investigations and thus clinical correlates of these findings were not available.
In contrast to HTLV-2, subsequent studies conducted in Brazil after the introduction of HAART support the contention that HIV-1 and HTLV-1 coinfections are linked to shortened survival and possibly to an increased risk for TSP/HAM and other neurologic manifestations.69 Brites et al. (2001) conducted a retrospective study of 63 patients with HIV-1 and HTLV-1 coinfection in Bahia, Brazil and matched the cases to monoinfected patients based on the date of diagnosis of HIV infection.70 IDU was the predominant mode of transmission. During follow-up, the overall mean survival time was significantly lower among those coinfected with HTLV-1. Treatment effects of antiviral therapy were not taken into account. Ten years later, the same group published the only available study concerning survival time in a pediatric population with HIV/HTLV-1 coinfection.71 Coinfected children were more likely to present with signs and symptoms of disease when compared with HIV-monoinfected children despite having significantly higher CD4+ T cell counts at presentation. The proportion of deaths was higher for children with HTLV-1/HIV coinfection, and survival time was significantly shortened.
In work conducted by Beilke et al. we performed both a retrospective and a prospective study of patients with both HIV/HTLV-1 and HIV-1/HTLV-2 coinfections in New Orleans, Louisiana.72 The HIV Outpatient Clinic at the Medical Center of Louisiana (New Orleans) initiated testing for HTLV-1/2 antibodies in 1993. Between 1993 and 2002, approximately 3600 patients received testing. From this group, 288 patients (8.0%) were found to have a positive screening ELISA test. Western blot testing confirmed HIV/HTLV-1 coinfections in 62 patients and HIV/HTLV-2 coinfections in 141. A total of 824 HIV-monoinfected patients were compared at baseline based on time of enrollment into the clinic. Factors associated with either HTLV-1 or HTLV-2 infection in multivariable models included age >36 years, African American race, history of self-reported injection drug use, and higher baseline CD4+ T cell counts that continued through time. Coinfection with HIV-1 and HTLV-2 was statistically associated with delayed progression to both AIDS and death. A similar trend was noted among patients with HIV-1/HTLV-1 dual infections; however, inadequate numbers of patients with HIV/HTLV-1 limited any conclusions. Four of 62 patients with HIV/HTLV-1 infection were found to have a diagnosis of TSP/HAM.73
In a subsequent study, we investigated the relationship between HTLV-1/2 proviral load and HIV plasma RNA levels, using primers amplifying the tax/rex region of the HTLV genome.74 When patients were stratified according to HTLV-1/2 proviral copy number, those with >20,000 HTLV-1/2 proviral copies/106 peripheral blood mononuclear cells had lower levels of HIV-1 plasma RNA. These results were adjusted for administration of HAART therapy.
Taking Stock: Explaining the Clinical Significance of Retroviral Coinfections
Taken collectively, there are now data that suggest that the natural histories of HIV-1/HTLV-1 and HIV-1/HTLV-2 coinfections are different. Both before and during the era of HAART, available evidence suggested that HTLV-1 renders no appreciable health benefit to the HIV-1-infected individual. Although studies are not definitive, HTLV-1 may be detrimental to the HIV-1-infected individual, with increasing risk for development of neurologic complications including TSP/HAM, leukemia, and lymphoma.69,73,75 This often occurs in the scenario of a patient with relatively normal or even elevated CD4+ T cell counts. In contrast, several studies in the United States and Europe now support the contention that HIV-1/HTLV-2 coinfection may confer an immunologic and survival benefit with little evidence of increased neurologic disease or malignancy.76 How are these differences explained?
Overexpression of the HTLV-1 and HTLV-2 tax gene with HIV/HTLV coinfection with or without HAART has been observed in several but not all studies.74, 77–79 HTLV-1 Tax (Tax1) is centrally involved in the complex steps of leukemogenesis following years of subclinical HTLV-1 infection. Tax1 affects a wide variety of cellular signaling pathways leading to transcriptional activation, proliferation, and ultimately transformation. Tax1 induces the expression of a wide range of host cell proteins, including transcription factors and cytokines interleukin-2 (IL-2), tumor necrosis factor (TNF), and others.80,81 While Tax2 shares many properties characteristic of the Tax1, its potential to induce cellular transformation and its ability to induce cytokine gene expression are lower than Tax1.82,83 The differential functional and structural characteristics of Tax1 and Tax2 proteins may explain the differences in disease potential associated with HTLV-1 and HTLV-2.83,84 In clinical scenarios where overexpression of Tax1 and Tax2 occurs, increased transactivation of cellular genes might result in immune dysregulation in affected individuals.82
Previous reports by Lewis et al. documented the spontaneous production of CC-chemokines by individuals infected with HTLV-2 or with HIV-1/HTLV-2 coinfections.85 CC-chemokines have been identified as playing an important beneficial role in innate immunity inducing the directional migration of a number of inflammatory cells and activating specific leukocyte populations. Casoli et al. demonstrated that HTLV-2 downregulated HIV-1 replication in IL-2-stimulated peripheral blood mononuclear cells (PBMCs) of coinfected individuals through expression of MIP-1α.86 The same group had previously reported that leukocytes from coinfected nonprogressors were found to have postgenomic upregulation of a CCL3L1 isoform, which seems to have a profound inhibitory effect on HIV-1 viral replication.87 The CC-chemokines are the natural ligands for CCR5, the receptor necessary for HIV-1 entry.88,89 HIV-1-exposed individuals who remained uninfected produce high levels of these chemokines.90 Additionally, it has been shown that CC-chemokines suppress HIV-1 viral replication in vitro,91 which suggests a positive role for these molecules in controlling the natural course of HIV infection.91–93
In a recent study, we reported that both Tax1 and Tax2 recombinant proteins displayed the ability to downregulate CCR5 receptor expression on lymphocytes along with the induction of CC-chemokines.94 These findings support the hypothesis that Tax2 via CC-chemokine induction could prevent interaction of the HIV-1 env/CD4 complex with the CCR5 receptor, and potentially hamper the virus from infecting the target cell. Therefore, Tax2 could play a key role in PBMCs survival in patients with HIV-1/HTLV-2 coinfection. While overexpression of Tax1 would also be suggested to convey a survival benefit through this mechanism, it is possible that the composite effects of this potent activator of other key cellular genes would counter this effect.
Finally, the recent work related to regulation of Tax1 and Tax2 gene expression by proteins expressed by an antisense transcript (i.e., the HTLV-1 bZIP factor and the antisense protein of HTLV-2 known as APH-2) may further identify key differences in the way Tax1 and Tax2 are expressed and function among coinfected individuals.95,96 At present, there is no information to prove or disprove this hypothesis.
Conclusions
The past 25 years of research into the pathobiology of the first three described human retroviruses has had an exciting evolution, in which geographic differences, virus-specific and host-specific genetic variations, and human behavior all contribute to the unique clinical, immunologic, and virologic consequences of retroviral coinfections. It is certain that the interplay of HIV-1 and HTLV-1 or HTLV-2 in different study populations will continue to broaden our knowledge and insights concerning the pathobiology of human retroviruses.
Acknowledgments
Appreciation is extended to John Fangman, M.D., Andrew Petroll, M.D., and Christy Barrios, Ph.D for helpful peer review of the manuscript. Dr. Beilke's research is supported through the Department of Veterans Affairs (BLS R&D Merit Review Grant No. 5I01BX000488-02).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.van der Kuyl AC. Cornelissen M. Identifying HIV-1 dual infections. Retrovirology. 2007;4(67):1–12. doi: 10.1186/1742-4690-4-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McCutchan FE. Hoelscher M. Tovanabutra S. Piyasirisilp S. Sanders-Buell E. Ramos G. Jagodzinski L. Polonis V. Maboko L. Mmbando D. Hoffmann O. Riedner G. von Sonnenburg F. Robb M. Birx DL. In-depth analysis of a heterosexually acquired human immunodeficiency virus type 1 superinfection: Evolution, temporal fluctuation, and intercompartment dynamics from the seronegative window period through 30 months postinfection. J Virol. 2005;79(18):11693–11704. doi: 10.1128/JVI.79.18.11693-11704.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taylor JE. Korber BT. HIV-1 intra-subtype superinfection rates: Estimates using a structured coalescent with recombination. Infect Genet Evol. 2005;5(1):85–95. doi: 10.1016/j.meegid.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 4.Chakraborty B. Valer L. De Mendoza C. Soriano V. Quinones-Mateu ME. Failure to detect human immunodeficiency virus type 1 superinfection in 28 HIV-seroconcordant individuals with high risk of reexposure to the virus. AIDS Res Hum Retroviruses. 2004;20(9):1026–1031. doi: 10.1089/aid.2004.20.1026. [DOI] [PubMed] [Google Scholar]
- 5.Fang G. Weiser B. Kuiken C. Philpott SM. Rowland-Jones S. Plummer F. Kimani J. Shi B. Kaul R. Bwayo J. Anzala O. Burger H. Recombination following superinfection by HIV-1. AIDS. 2004;18(2):153–159. doi: 10.1097/00002030-200401230-00003. [DOI] [PubMed] [Google Scholar]
- 6.Hu DJ. Subbarao S. Vanichseni S. Mock PA. Ramos Artur. Nguyen L. Chaowanachan T. Griensven F. Choopanya K. Mastro TD. Tappero JW. Frequency of HIV-1 dual subtype infections, including intersubtype superinfections, among injection drug users in Bangkok, Thailand. AIDS. 2005;19(3):303–308. [PubMed] [Google Scholar]
- 7.Fultz PN. HIV-1 superinfections: Omens for vaccine efficacy? AIDS. 2004;18(1):115–119. doi: 10.1097/00002030-200401020-00014. [DOI] [PubMed] [Google Scholar]
- 8.Shine D. Moll B. Emeson E. Spigland I. Harris C. Small CB. Friedland G. Weiss SH. Bodner AJ. Serologic, immunologic, and clinical features of parenteral drug users from contrasting populations. Am J Drug Alcohol Abuse. 1987;13(4):401–412. doi: 10.3109/00952998709001524. [DOI] [PubMed] [Google Scholar]
- 9.Pierik LT. Murphy EL. The clinical significance of HTLV-I and HTLV-II infection in the AIDS epidemic. AIDS Clin Rev. 1991;1:39–57. [PubMed] [Google Scholar]
- 10.Khabbaz RF. Onorato IM. Cannon RO. Hartley TM. Roberts B. Hosein B. Kaplan JE. Seroprevalence of HTLV-I and HTLV-II among intravenous drug users and persons in clinics for sexually transmitted diseases. N Engl J Med. 1992;326(6):375–380. doi: 10.1056/NEJM199202063260604. [DOI] [PubMed] [Google Scholar]
- 11.Wiktor SZ. Cannon RO. Atkinson WL. Lutz B. Hook EW. Blattner WA. Quinn TC. Infection with HTLV-II and -II in sexually transmitted disease clinics in Baltimore and New Orleans. J Infect Dis. 1992;165(5):920–924. doi: 10.1093/infdis/165.5.920. [DOI] [PubMed] [Google Scholar]
- 12.Briggs NC. Battjes RJ. Cantor KP. Blattner WA. Yellin FM. Wilson S. Ritz AL. Weiss SH. Goedert JJ. Seroprevalence of HTLV-II infection, with or without HIV-1 coinfection, among US intravenous drug users. J Infect Dis. 1995;172(1):51–58. doi: 10.1093/infdis/172.1.51. [DOI] [PubMed] [Google Scholar]
- 13.Bessinger R. Beilke M. Kissinger P. Jarrott C. Tabak OF. Retroviral coinfections at a New Orleans HIV outpatient clinic. J AIDS Human Retrovirol. 1997;14(1):67–71. doi: 10.1097/00042560-199701010-00011. [DOI] [PubMed] [Google Scholar]
- 14.Kaplan JE. Khabbaz RF. The epidemiology of human T-lymphotropic virus types I and II. Rev Med Virol. 1993;3:137. [Google Scholar]
- 15.Dezzutti CS. Lal RB. Human T-cell lymphotropic virus types I and II. In: Murray PR, editor; Baron KJ, editor; Pfaller MA, editor. Manual of Clinical Microbiology. American Society for Microbiology; Washington, DC: 1999. p. 871. [Google Scholar]
- 16.Araujo A. Sheehy N. Takahashi H. Hall WW. Concomitant infections with human immunodeficiency virus type 1, human T-lymphotropic virus types 1, 2. In: Brogden KA, editor; Guthmiller JM, editor. Polymicrobial Diseases. ASM Press; Washington, DC: 2002. Chapter 5. [PubMed] [Google Scholar]
- 17.Schreiber GB. Murphy EL. Horton JA. Wright DJ. Garfein R. Chien HC. Nass CC. Risk factors for human T-cell lymphotropic virus types I and II (HTLV-I and -II) in blood donors: The retrovirus epidemiology donor study. NHLBI retrovirus epidemiology donor study. J Acquir Immune Defic Syndr Hum Retrovirol. 1997;14(3):263–271. doi: 10.1097/00042560-199703010-00011. [DOI] [PubMed] [Google Scholar]
- 18.Barcellos NT. Fuchs SC. Mondini LG. Murphy EL. Human T lymphotropic virus type I/II infection: Prevalence and risk factors in individuals testing for HIV in counseling centers from Southern Brazil. Sex Trans Dis. 2006;33(5):302–306. doi: 10.1097/01.olq.0000194598.47821.b6. [DOI] [PubMed] [Google Scholar]
- 19.Murphy EL. Watanabe K. Nass CC. Ownby H. Williams A. Nemo G. Evidence among blood donors for a 30-year old epidemic of human T lymphotropic virus type II infection in the United States. J Infect Dis. 1999;180(6):1777–1783. doi: 10.1086/315139. [DOI] [PubMed] [Google Scholar]
- 20.Zella D. Mori L. Sala M. Ferrante P. Casoli C. Magnani G. Achilli G. Cattaneo E. Lori F. Bertazzoni U. HTLV-II infection in Italian drug abusers. Lancet. 1990;336(8714):575–576. doi: 10.1016/0140-6736(90)92140-d. [DOI] [PubMed] [Google Scholar]
- 21.Fukushima Y. Takahashi H. Hall WW. Nakasone T. Nakata S. Song P. Duc DD. Hien B. Quang NX. Trinh TN. Nishioka K. Kitamura K. Komuro K. Vahlne A. Honda M. Extraordinary high rate of HTLV type II seropositivity in intravenous drug abusers in south Vietnam. AIDS Res Hum Retroviruses. 1995;11(5):637–645. doi: 10.1089/aid.1995.11.637. [DOI] [PubMed] [Google Scholar]
- 22.Edlin BR. Irwin KL. Faruque S. McCoy CB. Word C. Serrano Y. Inciardi JA. Bowser BP. Schilling RF. Holmberg SD and the Multicenter Crack Cocaine and HIV Infection Study Team. Intersecting epidemics––crack cocaine use and HIV infection among inner-city young adults. N Engl J Med. 1994;331(21):1422–1427. doi: 10.1056/NEJM199411243312106. [DOI] [PubMed] [Google Scholar]
- 23.Substance Abuse and Mental Health Services Administration (SAMHSA) Report. National survey shows a rise in illicit drug use from 2008 to 2010. Sep 8, 2011. http://www.samhsa.gov http://www.samhsa.gov SAMHSA News Report.
- 24.Poiesz BJ. Buscetti FW. Gazdar AF. Bunn PA. Minna JD. Gallo RC. Detection and isolation of type C retrovirus particles from fresh and cultured lymphocytes of a patient with cutaneous T-cell lymphoma. Proc Natl Acad Sci USA. 1980;77(12):7415–7419. doi: 10.1073/pnas.77.12.7415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hinuma Y. Nagata K. Hanaoka M. Nakai M. Matsumoto T. Kinoshita KI. Shirahawa S. Miyoshi I. Adult T-cell leukemia: Antigen in an ATL cell line and detection of antibodies to the antigen in human sera. Proc Natl Acad Sci USA. 1981;78(10):6476–6480. doi: 10.1073/pnas.78.10.6476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Miyoshi I. Kubonishi I. Yoshimoto S. Akagi T. Ohtsuki Y. Shiraishi Y. Nagata K. Hinuma Y. Type C virus particles in a cord T-cell line derived by co-cultivating normal human cord leukocytes and human leukaemic T cells. Nature. 1981;294(5843):770–771. doi: 10.1038/294770a0. [DOI] [PubMed] [Google Scholar]
- 27.Yoshida M. Seiki M. Yamaguchi K. Takatsuki K. Monoclonal integration of human T-cell leukemia provirus in all primary tumors of adult T-cell leukemia suggests causative role of human T-cell leukemia virus in the disease. Proc Natl Acad Sci USA. 1984;81(8):2534–2537. doi: 10.1073/pnas.81.8.2534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kalyanaraman VS. Sarngadharan MG. Robert-Guroff M. Miyoshi I. Golde D. Gallo RC. A new subtype of human T-cell leukemia virus (HTLV-II) associated with a T-cell variant of hairy cell leukemia. Science. 1982;218(4572):571–573. doi: 10.1126/science.6981847. [DOI] [PubMed] [Google Scholar]
- 29.Gessain A. Barin F. Vernant JC. Gout O. Maurs L. Calender A. de The G. Antibodies to human T-lymphotropic virus type-I in patients with tropical spastic paraparesis. Lancet. 1985;2(8452):407–410. doi: 10.1016/s0140-6736(85)92734-5. [DOI] [PubMed] [Google Scholar]
- 30.Osame M. Usuku K. Izumo S. Ijichi N. Amitani H. Igata A. Matsumoto M. Tara M. HTLV-I associated myelopathy, a new entity. Lancet. 1986;1(8488):1031–1032. doi: 10.1016/s0140-6736(86)91298-5. [DOI] [PubMed] [Google Scholar]
- 31.Barre-Sinoussi F. Chermann JC. Rey F. Nugeyre MT. Chamaret S. Gruest J. Dauguet C. Axler-Blin C. Vezinet-Brun F. Rouzioux C. Rozenbaum W. Montagnier L. Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS) Science. 1983;220(4599):868–871. doi: 10.1126/science.6189183. [DOI] [PubMed] [Google Scholar]
- 32.Broder S. Gallo RC. A pathogenic retrovirus (HTLV-III) linked to AIDS. N Engl J Med. 1984;311(20):1992–1297. doi: 10.1056/NEJM198411153112006. [DOI] [PubMed] [Google Scholar]
- 33.Harada S. Koyangi Y. Yamamoto N. Infection of HTLV-III/LAV in HTLV-I-carrying cells MT-2 and MT-4 and application in a plaque assay. Science. 1985;229(4713):563–566. doi: 10.1126/science.2992081. [DOI] [PubMed] [Google Scholar]
- 34.Coffin J. Haase A. Levy JA. Montagnier L. Oroszlan S. Teich N. Temin H. Toyoshima K. Varmus H. Vogt P. Weiss R. Human immunodeficiency viruses [letter] Science. 1986;232(4751):697. doi: 10.1126/science.3008335. [DOI] [PubMed] [Google Scholar]
- 35.Coffin J. Haase A. Levy JA. Montagnier L. Oroszlan S. Teich N. Temin H. Toyoshima K. Varmus H. Vogt P. Weiss R. What to call the AIDS virus? [letter] Nature. 1986;821(6065):10. doi: 10.1038/321010a0. [DOI] [PubMed] [Google Scholar]
- 36.Gonda MA. Wong-Staal F. Gallo RC. Clements JE. Narayan O. Gilden RV. Sequence homology and morphologic similarity of HTLV-III and Visna virus, a pathogenic lentivirus. Science. 1985;227(4683):173–177. doi: 10.1126/science.2981428. [DOI] [PubMed] [Google Scholar]
- 37.Popovic M. Read-Connole E. Gallo RC. T4 positive human neoplastic cell lines susceptible to and permissive for HTLV-III. Lancet. 1984;2(8417–8418):1472–1473. doi: 10.1016/s0140-6736(84)91666-0. [DOI] [PubMed] [Google Scholar]
- 38.Koenig S. Gendelman HE. Orenstein JM. Dal Canto MC. Pezeshkpour GH. Yungbluth M. Janott F. Aksamit A. Martin MA. Fauci AS. Detection of AIDS virus in macrophages in brain tissue from AIDS patients with encephalopathy. Science. 1986;233(4768):1089–1093. doi: 10.1126/science.3016903. [DOI] [PubMed] [Google Scholar]
- 39.Seiki M. Hattori S. Hirayama Y. Yoshida M. Human adult T-cell leukemia virus: Complete nucleotide sequence of the provirus genome integrated in leukemia cell DNA. Proc Natl Acad Sci USA. 1983;80(12):3618–3622. doi: 10.1073/pnas.80.12.3618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shimotohno K. Takahashi Y. Shimizu N. Gojobori T. Golde DW. Chen ISY. Miwa M. Sugimura T. Complete nucleotide sequence of an infectious clone of human T-cell leukemia virus type II: An open reading frame for the protease gene. Proc Natl Acad Sci USA. 1985;82(10):3101–3105. doi: 10.1073/pnas.82.10.3101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ratner L. Haseltine W. Patarca R. Livak KJ. Starcich B. Josephs SF. Doran E. Rafalski JA. Whitehorn EA. Baumeister K, et al. Complete nucleotide sequence of the AIDS virus, HTLV-III. Nature. 1985;313(6000):277–284. doi: 10.1038/313277a0. [DOI] [PubMed] [Google Scholar]
- 42.Schüpbach J. Gilden R. Gonda MA. Sarngadharan MG. Gallo RC. Serological analysis of a subgroup of human T-lymphotropic retroviruses (HTLV-III) associated with AIDS. Science. 1984;224(4648):503–505. doi: 10.1126/science.6200937. [DOI] [PubMed] [Google Scholar]
- 43.Essex M. McLane MF. Lee TH. Tachibana N. Mullins JI. Kreiss J. Kasper CK. Poon M-C. Landay A. Stein SF. Francis DP. Cabradilla C. Lawrence DN. Evatt BL. Antibodies to human T-cell leukemia virus membrane antigens (HTLV-MA) in hemophiliacs. Science. 1983;221(4615):1061–1064. doi: 10.1126/science.6603659. [DOI] [PubMed] [Google Scholar]
- 44.Sarngadharan MG. Bruch L. Popovic M. Gallo RC. Immunological properties of the Gag protein p24 of the acquired immunodeficiency syndrome retrovirus (human T-cell leukemia virus type III) Proc Natl Acad Sci USA. 1985;82(10):3481–3484. doi: 10.1073/pnas.82.10.3481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Casey JM. Kim Y. Andersen PR. Watson KF. Fox JL. Devare SG. Human T-cell lymphotropic virus type III: Immunologic characterization and primary structure analysis of the major internal protein, p24. J Virol. 1985;55(2):417–423. doi: 10.1128/jvi.55.2.417-423.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Abe T. Kinoshita T. Matsuda J. Ryu T. Ting RC. Aoki T. Robert-Guroff M. Miyakoshi H. Gallo RC. Detection of antibodies to HTLV-I and -III in sera from Japanese hemophiliacs. Cancer Res. 1985;45(9 Suppl):4621s–4623s. [PubMed] [Google Scholar]
- 47.Robert-Guroff M. Blayney DW. Safai B. Lange M. Gelmann M. Gutteman EP. Mansell JW. Goedtert PW. Groopman JL. Steigbigel JE, et al. HTLV-1-specific antibody in AIDS patients and others at risk. Lancet. 1984;2(8395):128–131. doi: 10.1016/s0140-6736(84)91047-x. [DOI] [PubMed] [Google Scholar]
- 48.Robert-Guroff M. Weiss SH. Giron JA. Jennings AM. Ginzburg HM. Margolis IB. Blattner WA. Gallo RC. Prevalence of antibodies to HTLV-I, -II, and -III in intravenous drug abusers from an AIDS endemic region. JAMA. 1986;255(22):3133–3137. [PubMed] [Google Scholar]
- 49.Bartholomew C. Blattner W. Cleghorn F. Progression to AIDS in homosexual men co-infected with HIV and HTLV-I in Trinidad. Lancet. 1987;2(8573):1469. doi: 10.1016/s0140-6736(87)91172-x. [DOI] [PubMed] [Google Scholar]
- 50.Hattori T. Koito A. Takatsuki K. Ikematsu S. Matsuda J. Mori H. Fukui M. Akashi K. Matsumoto K. Frequent infection with human T-cell lymphotropic virus type I in patients with AIDS but not in carriers of human immunodeficiency virus type 1. J Acquir Immune Defic Syndr Hum Retrovirol. 1989;2(3):272–276. [PubMed] [Google Scholar]
- 51.Harper ME. Kaplan MH. Marselle LM. Pahwa SG. Chayt KJ. Sarngadharan MG. Wong-Staal F. Gallo RC. Concomitant infection with HTLV-I and HTLV-III in a patient with T8 lymphoproliferative disease. N Eng J Med. 1986;315(17):1073–1078. doi: 10.1056/NEJM198610233151707. [DOI] [PubMed] [Google Scholar]
- 52.Shibata D. Brynes RK. Rabinowitz A. Hanson CA. Slovak M. Spira TJ. Gill P. Human T-cell lymphotropic virus type I (HTLV-I)-associated adult T-cell leukemia-lymphoma in a patient infected with human immunodeficiency virus type 1 (HIV-1) Ann Intern Med. 1989;111(11):871–875. doi: 10.7326/0003-4819-111-11-871. [DOI] [PubMed] [Google Scholar]
- 53.Page JB. Lai S. Chitwood DD. Klimas NG. Smith PC. Fletcher MA. HTLV-I/II positivity and death from AIDS among HIV-1 seropositive intravenous drug users. Lancet. 1990;335(8703):1439–1441. doi: 10.1016/0140-6736(90)91456-k. [DOI] [PubMed] [Google Scholar]
- 54.Heneine W. Khabbaz RF. Lal RB. Kaplan JE. Sensitive and specific polymerase chain reaction assays for diagnosis of human T-cell lymphotropic virus type I (HTLV-I) and HTLV-III infections in HTLV-I/II-seropositive individuals. J Clin Micro. 1992;30(6):1605–1607. doi: 10.1128/jcm.30.6.1605-1607.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ehrlich GD. Glaser JB. LaVigne K. Quan D. Mildvan D. Sninsky JJ. Kwok S. Papsidero L. Poiesz BJ. Prevalence of human T-cell leukemia/lymphoma virus (HTLV) type II infection among high-risk individuals: Type-specific identification of HTLVs by polymerase chain reaction. Blood. 1989;74(5):1658–1664. [PubMed] [Google Scholar]
- 56.Lee H. Swanson P. Shorty VS. High rate of HTLV-II infection in seropositive IV drug abusers in New Orleans. Science. 1989;244(4903):471–475. doi: 10.1126/science.2655084. [DOI] [PubMed] [Google Scholar]
- 57.Wattel E. Mariotti M. Agis F. Gordien E. Prou O. Courouce AM. Rouger P. Wain-Hobson S. Chen IS. Lefrere JJ. Human T lymphotropic virus (HTLV) type I and II DNA amplification in HTLV-I/II-seropositive blood donors of the French West Indies. J Infect Dis. 1992;165(2):369–372. doi: 10.1093/infdis/165.2.369. [DOI] [PubMed] [Google Scholar]
- 58.Wiktor SZ. Alexander SS. Shaw GM. Weiss SH. Murphy EL. Wilks RJ. Shortly VJ. Hanchard B. Blattner WA. Distinguishing between HTLV-I and HTLV-II by Western blot [letter] Lancet. 1990;335(8704):1533. doi: 10.1016/0140-6736(90)93078-4. [DOI] [PubMed] [Google Scholar]
- 59.Chavance M. Neisson-Vernant C. Quist D. Monplaisir N. Armengaud B. Chout R. HIV/HTLV-I coinfection and clinical grade at diagnosis. J Acquir Immune Defic Syndr Hum Retrovirol. 1995;8(1):91–95. [PubMed] [Google Scholar]
- 60.Gotuzzo E. Escamilla J. Phillips IA. Sanchez J. Wignall FS. Antigoni J. The impact of human T-lymphotrophic virus type I/II infection on the prognosis of sexually acquired cases of acquired immunodeficiency syndrome. Arch Intern Med. 1992;152(7):1429–1373. [PubMed] [Google Scholar]
- 61.Cleghorn FR. Blattner WA. Does human T-cell lymphotropic virus type I and human immunodeficiency virus type 1 coinfection accelerate acquired immunodeficiency syndrome? The jury is still out (editorial) Arch Intern Med. 1992;152(7):1372–1373. [PubMed] [Google Scholar]
- 62.Volberding PA. HIV, HTLV-I, and CD4+ lymphocytes: Troubles in the relationship (editorial) JAMA. 1994;271(5):392–393. [PubMed] [Google Scholar]
- 63.Hershow RC. Galai N. Fukuda K. Graber J. Vlahov D. Rezza G. Klein RS. Des Jarlais DC. Vitek C. Khabbaz R. Freels S. Zuckerman R. Pezzotti P. Kaplan JE. An international collaborative study of the effects of coinfection with human T-lymphotropic virus type II on human immunodeficiency virus type 1 disease progression in injection drug users. J Infect Dis. 1996;174(2):309–317. doi: 10.1093/infdis/174.2.309. [DOI] [PubMed] [Google Scholar]
- 64.Schechter M. Moulton LH. Harrison LH. HIV Viral load and CD4+ lymphocyte counts in subjects coinfected with HTLV-I and HIV-1. J Acquir Immune Defic Syndr Hum Retrovirol. 1997;15(4):308–311. doi: 10.1097/00042560-199708010-00010. [DOI] [PubMed] [Google Scholar]
- 65.Hill SA. Lloyd PA. McDonald S. Wykoff J. Derse D. Susceptibility of human T cell leukemia virus type I to nucleoside reverse transcriptase inhibitors. J Infect Dis. 2003;188(2):424–427. doi: 10.1086/376531. [DOI] [PubMed] [Google Scholar]
- 66.Powderly WG. Significance of HIV/HTLV coinfection? Editorial. http://www.medscape.com/viewarticle/440640. 2002. http://www.medscape.com/viewarticle/440640
- 67.Turci M. Pilotti E. Ronzi P. Magnani G. Boschini A. Parisi SG. Zipeto D. Lisa A. Casoli C. Bertazzoni U. Coinfection with HIV-1 and human T-cell lymphotropic virus type II in intravenous drug users is associated with delayed progression to AIDS. J Acquir Immune Defic Syndr Hum Retrovirol. 2006;41(1):100–106. doi: 10.1097/01.qai.0000179426.04166.12. [DOI] [PubMed] [Google Scholar]
- 68.Bassini S. Lopez M. Toro C. Jiménez V. Sempere JM. Soriano V. Benito JM. Influence of human T cell lymphotropic virus type 2 coinfection on virological and immunological parameters in HIV type 1-infected patients. Clin Infect Dis. 2007;44(1):105–110. doi: 10.1086/510076. [DOI] [PubMed] [Google Scholar]
- 69.Brites C. Sampaio J. Oliveira A. HIV/Human T-cell lymphotropic virus coinfection revisited: Impact on AIDS progression. AIDS Rev. 2009;11(1):8–16. [PubMed] [Google Scholar]
- 70.Brites C. Alencar R. Gusmão R. Pedroso C. Netto EM. Pedral-Sampalo D. Bardaró R. Co-infection with HTLV-1 is associated with a shorter survival time for HIV-1-infected patients in Bahia, Brazil. AIDS. 2001;15(15):2053–2055. doi: 10.1097/00002030-200110190-00023. [DOI] [PubMed] [Google Scholar]
- 71.Pedroso C. Netto EM. Weyll N. Brites C. Coinfection by HIV-1 and human lymphotropic virus type 1 in Brazilian children is strongly associated with a shorter survival time. J Acquir Immune Defic Syndr Hum Retrovirol. 2011;57(Suppl 3):S208–S211. doi: 10.1097/QAI.0b013e31821e9baf. [DOI] [PubMed] [Google Scholar]
- 72.Beilke MA. Theall KP. O'Brien M. Clayton JL. Benjamin SM. Winsor EL. Kissinger PJ. Clinical outcomes and disease progression among patients coinfected with HIV and human T lymphotropic virus types 1 and 2. Clin Infec Dis. 2004;39(2):256–263. doi: 10.1086/422146. [DOI] [PubMed] [Google Scholar]
- 73.Beilke MA. Japa S. Moeller-Hadi C. Martin-Schild S. Tropical spastic paraparesis/human T leukemia virus type 1-associated myelopathy in HIV type 1-coinfected patients. Clin Infect Dis. 2005;41(6):e57–e63. doi: 10.1086/432890. [DOI] [PubMed] [Google Scholar]
- 74.Beilke MA. Traina-Dorge VL. Sirois M. Bhuiyan A. Murphy EL. Walls JM. Fagan R. Winsor EL. Kissinger PJ. Relationship between human T lymphotropic virus (HTLV) type 1/2 viral burden and clinical and treatment parameters among patients with HIV type 1 and HTLV-1/2 coinfection. Clin Infect Dis. 2007;44(9):1229–1234. doi: 10.1086/513428. [DOI] [PubMed] [Google Scholar]
- 75.Casseb J. Posada-Vergara MP. Montanheira P. Fukumori LMI. Olah I. Smid J. Duarto AJ. Penaiva de Oliveira AC. T CD4+ cell counts among patients co-infected with human immunodeficiency virus type 1 (HIV-1) and human T-cell leukemia virus type 1 (HTLV-1): High prevalence of tropical spastic paraparesis/HTLV-1-associated myelopathy (TSP/HAM) Revist Instit Med Trop Sao Paulo. 2007;49(4):231–233. doi: 10.1590/s0036-46652007000400007. [DOI] [PubMed] [Google Scholar]
- 76.Casoli C. Pilotti E. Bertazzoni U. Molecular and cellular interactions of HIV-1/HTLV coinfection and impact on AIDS progression. AIDS Rev. 2007;9(3):140–149. [PubMed] [Google Scholar]
- 77.Beilke MA. Japa S. Vinson DG. HTLV-I and HTLV-II virus expression increase with HIV-1 coinfection. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;17(5):391–397. doi: 10.1097/00042560-199804150-00002. [DOI] [PubMed] [Google Scholar]
- 78.Murphy EL. Grant RM. Kropp J. Oliviera A. Lee T-H. Busch MP. Increased human T-lymphotropic virus type II proviral load following highly active retroviral therapy in HIV-coinfected patients. J Acquir Immune Defic Syndr Hum Retrovirol. 2003;33(5):655–656. doi: 10.1097/00126334-200308150-00019. [DOI] [PubMed] [Google Scholar]
- 79.Cesaire R. Dehee A. Lezin A. Desire N. Bourdonne O. Dantin F. Bera O. Smadja D. Abel S. Cabie A. Sobesky G. Nicolas JC. Quantification of HTLV type I and HIV type 1 DNA load in coinfected patients: HIV type 1 infection does not alter HTLV type I proviral amount in the peripheral blood compartment. AIDS Res Hum Retrovirus. 2001;17(9):799–805. doi: 10.1089/088922201750251990. [DOI] [PubMed] [Google Scholar]
- 80.Boxus M. Twizere JC. Legros S. Dewulf JF. Kettmann R. Willems L. The HTLV-1 Tax interactome. Retrovirology. 2008;5(76):1–24. doi: 10.1186/1742-4690-5-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Banerjee P. Rochford R. Antel J. Canute G. Wrzesinski S. Sieburg M. Feuer G. Proinflammatory cytokine gene induction by human T-cell leukemia virus type 1 (HTLV-1) and HTLV-2 Tax in primary human glial cells. J Virol. 2007;81(4):1690–1700. doi: 10.1128/JVI.01513-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Yamano Y. Nagai M. Brennan M. Mora CA. Soldan SS. Tomaru U. Takenouchi N. Izumo S. Osame M. Jacobson S. Correlation of human T-cell lymphotropic virus type 1 (HTLV-1) mRNA with proviral DNA load, virus-specific CD8(+) T cells, and disease severity in HTLV-1-associated myelopathy (HAM/TSP) Blood. 2002;99(1):88–94. doi: 10.1182/blood.v99.1.88. [DOI] [PubMed] [Google Scholar]
- 83.Higuchi M. Fujii M. Distinct functions of HTLV-1 Tax1 from HTLV-2 Tax2 contribute key roles to viral pathogenesis. Retrovirology. 2009;6(117):1–11. doi: 10.1186/1742-4690-6-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bertazzoni U. Turci M. Avesani F. DiiGennaro G. Bidoia C. Romanelli MG. Intracellular localization and cellular factors interaction of HTLV-1 and HTLV-2 Tax proteins: Similarities and functional differences. Viruses. 2011;3(5):541–560. doi: 10.3390/v3050541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lewis MJ. Gautier VW. Wang XP. Kaplan MH. Hall WW. Spontaneous production of C-C chemokines by individuals infected with human T lymphotropic virus type II (HTLV-II) alone and HTLV-II/HIV-1 coinfected individuals. J Immunol. 2000;165(7):4127–4132. doi: 10.4049/jimmunol.165.7.4127. [DOI] [PubMed] [Google Scholar]
- 86.Casoli C. Vicenzi E. Cimarelli A. Magnani G. Ciancianaini P. Cattaneo E. Dall'Algio PP. Poli G. Bertazzoni U. HTLV-II down-regulates HIV-1 replication in IL-2-stimulated primary PBMC of coinfected individuals through expression of MIP-1a. Blood. 2000;95(9):2760–2769. [PubMed] [Google Scholar]
- 87.Pilotti E. Elviri L. Vicenzi E. Bertazzoni Um Re MC. Allibardi S. Poli G. Casoli C. Postgenomic up-regulation of CCL3L1 expression in HTLV-2-infected persons curtails HIV-1 replication. Blood. 2007;109(5):1850–1856. doi: 10.1182/blood-2006-07-036046. [DOI] [PubMed] [Google Scholar]
- 88.Dragic T. Litwin V. Allaway GP. Martin SR. Huang Y. Nagashima KA. Cayanan C. Maddon PJ. Koup RA. Moore JP. Paxton WA. HIV-1 entry into CD4+ cells is mediated by the chemokines receptor CC-CKR-5. Nature. 1996;381(6584):667–673. doi: 10.1038/381667a0. [DOI] [PubMed] [Google Scholar]
- 89.Bates P. Chemokine receptors and HIV-1: An attractive pair? Cell. 1996;86(1):1–3. doi: 10.1016/s0092-8674(00)80070-7. [DOI] [PubMed] [Google Scholar]
- 90.Paxton WA. Martin SR. Tse D. O'Brien TR. Skurnick J. VanDevanter NL. Padian N. Braun JF. Kotler DP. Wolinsky SM. Koup RA. Relative resistance to HIV-1 infection of CD4 lymphocytes from persons who remain uninfected despite multiple high-risk sexual exposures. Nat Med. 1996;2(4):412–417. doi: 10.1038/nm0496-412. [DOI] [PubMed] [Google Scholar]
- 91.Cocchi F. DeVico AL. Garzino-Demo A. Arya SK. Gallo RC. Lusso P. Identification of RANTES, MIP-1α, and MIP-1β as the major HIV-suppressive factor produced by CD8+ T cells. Science. 1995;270(5243):1811–1815. doi: 10.1126/science.270.5243.1811. [DOI] [PubMed] [Google Scholar]
- 92.Garzino-Demo A. Moss RB. Margolick JB. Cleghorn F. Sill A. Blattner WA. Cocchi F. Carlo DJ. DeVico AL. Gallo RC. Spontaneous and antigen-induced production of HIV-inhibitory beta-chemokines are associated with AIDS-free status. Proc Natl Acad Sci USA. 1999;96(21):11986–11991. doi: 10.1073/pnas.96.21.11986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Cocchi F. DeVico AL. Yarchoan R. Redfield R. Cleghorn F. Blattner WA. Garzino-Demo A. Colombini-Hatch S. Margolis D. Gallo RC. Higher macrophage inflammatory protein (MIP)-1alpha and MIP-1beta levels from CD8+ T cells are associated with asymptomatic HIV-1 infection. Proc Natl Acad Sci USA. 2000;97(25):13812–13817. doi: 10.1073/pnas.240469997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Barrios CS. Abuerreish M. Lairmore MD. Wu L. Castillo L. Giam C-Z. Beilke MA. Recombinant human T-cell leukemia virus types 1 and 2 Tax proteins induce high levels of CC-chemokines and downregulate CCR5 in human peripheral blood mononuclear cells. Viral Immunol. 2011;24(6):1–11. doi: 10.1089/vim.2011.0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Matsuoka M. Green PL. The HBZ gene, a key player in HTLV-1 pathogenesis. Retrovirology. 2009;6:71. doi: 10.1186/1742-4690-6-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Halin M. Douceron E. Clerc I. Journo C. Ko NL. Landry S. Murphy EL. Gessain A. Lemasson I. Mesnard J-M. Barbeau B. Mahieux R. Human T-cell leukemia virus type 2 produces a spliced antisense transcript encoding a protein that lacks a classic bZIP domain but still inhibits Tax2-mediated transcription. Blood. 2009;114(12):2724–2438. doi: 10.1182/blood-2008-09-179879. [DOI] [PMC free article] [PubMed] [Google Scholar]