Abstract
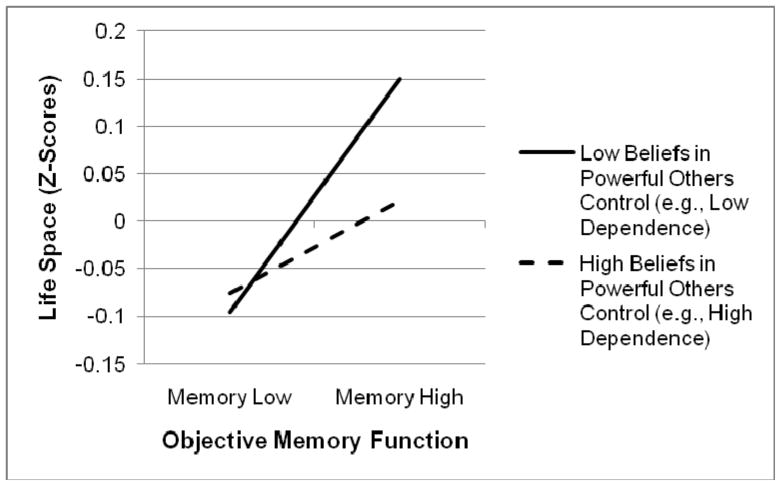
We examined the relationship of cognitive and functional measures with life space (a measure of spatial mobility examining extent of movement within a person’s environment) in older adults, and investigated the potential moderating role of personal control beliefs. Internal control beliefs reflect feelings of competence and personal agency, while attributions of external control imply a more dependent or passive point of view. Participants were 2,737 adults from the ACTIVE study, with a mean age of 74 years. Females comprised 76% of the sample, with good minority representation (27% African American). In multiple regression models controlling for demographic factors, cognitive domains of memory, reasoning, and processing speed were significantly associated with life space (p<.001 for each), and reasoning ability appeared most predictive (B=.117). Measures of everyday function also showed significant associations with life space, independent from the traditional cognitive measures. Interactions between cognitive function and control beliefs were tested, and external control beliefs moderated the relationship between memory and life space, with the combination of high objective memory and low external control beliefs yielding the highest life space (t=−2.07; p=.039). In conclusion, older adults with better cognitive function have a larger overall life space. Performance-based measures of everyday function may also be useful in assessing the functional outcome of life space. Additionally, subjective external control beliefs may moderate the relationship between objective cognitive function and life space. Future studies examining the relationships between these factors longitudinally appear worthwhile to further elucidate the interrelationships of cognitive function, control beliefs, and life space.
Keywords: aging, cognition, control beliefs, life space
Cognitive Function with Aging
Changes in cognition are relatively common among older individuals. While some aging persons are able to maintain high cognitive performance throughout life, many will experience a decline in memory and cognitive functions: an estimated 56% of older adults report such age-related changes in memory (Ellison, 2008). Much of the time, these slight declines in cognitive function are not pathological; rather, they are simply normative effects of aging. Age-Related Cognitive Decline (ARCD), as defined by the Diagnostic and Statistical Manual of Mental Disorders-IV-TR (2000), is characterized as deterioration in cognitive function that is within normal limits for age. Cognitive processes affected by age most often include processing speed, working memory, and both selective and divided attention (e.g., Clay et al., 2009; Ellison, 2008). Even if the nature of the decline is not pathological – that is, it can be considered a normal consequence of the aging process – these age-related changes can cause frustration to the individual, may affect daily routines and lifestyles, and can incite the implementation of compensatory strategies to optimize performance (Baltes & Baltes, 1990).
Additionally, poor cognitive performance is associated with a heightened perceived threat of dementia among older adults (Suhr & Kinkela, 2007), and evidence indicates that this relationship is bi-directional, perhaps due to pervasive negative stereotypes associated with aging (Hess, Auman, Colcombe, & Rahl, 2003). Notably, research on memory-related beliefs suggests that general beliefs held by individuals regarding aging can impact self-ratings of memory functioning and cognitive impairment, and manipulation of such beliefs can actually influence objective memory performance (Hummert, 1999; Hess et al., 2003; Levy, 1996).
Life Space and Aging
Another possible consequence of changes in memory and cognition is restriction of life space (Barnes, Wilson, Bienias, Mendes de Leon, & Kim, 2007), a measure of spatial mobility. The concept of life space was originally defined by May, Nayak, and Isaacs (1985) as the area in which a person moves within a specific time period (e.g., within a day, week, or month). Restriction of life space can often indicate decreased autonomy and can be a precursor to the development of difficulties in the execution of certain activities of daily living (Baker, Bodner, & Allman, 2003). Prevalence of mobility limitations in older adults approaches 45%, with approximately 88% of these individuals reporting mobility impairment lasting over one year’s time (Yeom, Fleury, & Keller, 2008). Mobility declines can also signify increased reliance on others, often family members and spouses who are older adults themselves. Depending on the degree of mobility constriction, quality of life can be compromised while risks for depression, nursing home placement, frailty, and mortality are increased (Yeom et al., 2008; Xue, Fried, Glass, Laffan, & Chaves, 2007). Range of life space among older adults appears to be influenced by physical and mental health problems, particularly depressive symptoms (Barnes et al., 2007). Interestingly, Stalvey, Owsley, Sloane, and Ball (1999) found scores on a life space questionnaire to be independent from age after adjusting for other factors, indicating that it is not simply advanced age that may limit mobility. Likewise, a study of community-dwelling adults demonstrated that even after accounting for demographic variables, visual function, and lower extremity motor function, cognitive function was strongly associated with life space restriction. Specifically, for every unit increase in global cognition (as measured by a standardized composite score), odds of life space restriction decreased by 50% (Barnes et al., 2007).
Although a relationship between lower cognitive function and restriction in life space has been documented (Barnes et al., 2007), not all older individuals experiencing decline in cognitive ability restrict their life space to the same degree, suggesting that other factors may be moderating this relationship. In an effort to create a new theoretical framework for the concept of mobility, Webber, Porter, and Menec (2010) describe the impact that subjective beliefs in one’s capability may have in determining life space and mobility outcomes, while acknowledging that such beliefs may not accurately mirror mobility capability. However, much of the literature on subjective beliefs and mobility includes measures of physical self-efficacy beliefs (e.g., beliefs in walking ability or balance maintenance), and does not address the impact of other forms of beliefs, such as perceived control (an extension of self-efficacy). To date, no studies have directly assessed the role control beliefs may play in the relationship between cognitive function and life space despite evidence to suggest that control beliefs can influence functional outcomes (Mirowsky & Ross, 2003; Rowe & Kahn, 1998). Likewise, prior studies examining mobility restriction and cognition have emphasized the need to investigate the role of personality and psychological variables, which includes personal control beliefs (Barnes et al., 2007; Yeom et al., 2008).
Aging and Control Beliefs
Sense of control can have important implications for older adults in particular (Langer & Rodin, 1976), and Rowe and Kahn (1987, 1998) have highlighted autonomy and personal control as critical factors for successful aging – a multidimensional concept characterized in part by optimal functioning in multiple domains including cognition, mobility, and psychosocial function. Lachman (1986) has largely advanced the concept of perceived control in its relation to self-efficacy. In this line of research, control beliefs are thought to be relatively stable individual attributions. While self-efficacy and control beliefs are related, they are distinct concepts – primarily in that self-efficacy places a greater role on the environment and underscores mastery of one’s environment through experiences (Welch & West, 1995).
Locus of control in the context of cognitive aging has been conceptualized as consisting of three subunits: internal control (personal intellectual control), chance control (the degree to which intellectual decline over time is seen as inevitable), and powerful others control (the extent to which others are regarded as more competent or whether one depends more on others) (Lachman, 1986). Researchers have found a positive correlation between perceived control and cognition in older adults (Levenson, 1974; Lachman & Leff, 1989; Soederberg & Lachman, 1999), and evidence suggests that higher perceived control and mastery over one’s environment can have beneficial effects, including more positive mood and lower mortality rates (Langer & Rodin, 1976). Consequences of a lowered sense of control and self-efficacy have also been suggested. Welch and West (1995) propose that an increase in memory errors, social stereotypes regarding memory and aging, and memory anxiety can all interact, leading older adults to lose confidence in their abilities and perhaps encourage memory dependence – the culmination of which can produce a decline in memory self-efficacy and perceived control. Similar findings have been shown for self-perceptions of aging and changes in functional health. Levy, Slade, and Kasl (2002) reported that older adults with more positive aging perceptions reported better functional health compared to those with more negative perceptions of aging, and these self-perceptions were partially explained by control beliefs.
Indeed, dependence on others may also relate to older adults’ control beliefs. Lachman and Leff (1989) administered intellectual tests and perceived control scales to 63 older adults at baseline and five-year follow-up time points. Of the three locus of control scales (internal control, chance control, powerful others control), only beliefs in powerful others control changed significantly (increased) over the five years. Interestingly, the increase on this scale occurred in the absence of a decline in actual intellectual performance. The researchers explained these findings as an indication that some older adults may feel less competent compared to others (depending on group of reference) and therefore increase dependence on other people to carry out cognitively demanding tasks. Because actual performance did not change, they argued that perhaps changes in control beliefs are influenced by acceptance of social stereotypes regarding aging and cognitive decline. This finding is not surprising, given that expectations of declines in memory and other cognitive abilities could cause older adults to lose confidence in their intellectual capabilities and place more confidence in others. Furthermore, according to Miller (1989) these insecurities can prompt some elders to restrict their range of activities and increase dependence upon others. What may follow is something of a self-fulfilling prophecy: by restricting day-to-day activities, such persons limit their opportunities for mastery experiences, thus perpetuating low self-efficacy and control beliefs while creating what Avorn and Langer (1982) call “induced disability” (Welch & West, 1995). It is therefore feasible that personal control beliefs may influence the relationship between cognitive function and life space.
It is evident from the literature that there are relationships between [objective or subjective] cognitive function and mobility, cognitive function and control beliefs, and control beliefs and dependence. However, to our knowledge, analyses including all of these variables have not yet been conducted. Additionally, existing research examining cognition and life space has examined overall or global cognitive function and has not included measures of specific cognitive domains in relation to life space. Inclusion of such measures is important because changes in older adults’ cognitive functions are heterogeneous; that is, domains of cognition are affected differentially with age across individuals. Therefore, awareness of associations between specific cognitive domains and life space may offer further understanding of the impact that changes in specific cognitive abilities may have on mobility outcomes. Previous studies have also primarily utilized traditional neurocognitive measures, despite evidence to suggest that everyday performance-based tasks may provide greater ecological validity (Chaytor & Schmitter-Edgecombe, 2003) and can provide predictive utility for functional outcomes (Marson et al., 2000). Therefore, the present study examined cognition (via both traditional cognitive tests and everyday performance-based measures), life space, and control beliefs to better understand the interplay of such factors and their effect on older adults – specifically, how the outcome of mobility may be affected. A better understanding of these factors and their relation to aging may eventually help improve strategies aimed at increasing mobility or decreasing the occurrence of self-induced disability.
The specific objectives of this study were (1) to examine the relationship between cognitive function and life space, (2) to determine whether performance-based tests of everyday function are associated with life space independent from cognitive measures, and (3) to investigate the role of personal control beliefs in the relationship between cognitive function and life space. It was hypothesized that after adjusting for demographic factors, depressive symptoms and physical function, poorer performance on cognitive measures would predict greater restriction on life space. Functional cognitive tests measuring everyday problem-solving ability were expected to increase predictive utility beyond that provided solely by more the more traditional cognitive tests. Personal control beliefs were additionally hypothesized to act as modifiers in the relationship between cognitive function and life space.
Method
Participants
The sample included participants from the longitudinal Advanced Cognitive Training for Independent and Vital Elderly (ACTIVE) study. The ACTIVE study recruited adults age 65 + who were living largely independent of formal care. Participants were drawn from multiple geographic areas, including communities in the Northeast, Midwest, and Southeast United States. Potential participants were eligible for inclusion if the following criteria were met: Age ≥65 years; Mini-Mental State Examination (MMSE; Folstein, Folstein, & McHugh, 1975) score ≥23; vision score >20/50; no dependence in hygiene, bathing or dressing; no diagnosis of Alzheimer’s disease; no stroke in previous 12 months; no cancer with limited life expectancy; no current chemotherapy or radiation treatment; no communication problems. Participant recruitment was conducted from March 1998 through October 1999, and a total of 5,000 potential participants were identified (Jobe et al., 2001). Of the potential participant pool, 935 (18%) were subsequently excluded for prespecified reasons. Another 1,263 potential participants (25%) declined study participation. The 2,802 remaining potential participants were screened, met protocol criteria, and signed written Institutional Review Board-approved informed consent; thus, a large sample of relatively healthy older adults with a mean age of 74 years was enrolled in the ACTIVE trial (Jobe et al., 2001). The present study utilized cross-sectional data obtained from 2,737 ACTIVE participants with complete data for all measures of interest at baseline.
Measures
Cognitive function. For purposes of the ACTIVE protocol, cognitive function is divided into three domains: memory, reasoning, and processing speed. Tests of memory in ACTIVE included the Hopkins Verbal Learning Test (HVLT; Brandt, 1991), Rey Auditory Verbal Learning Test (AVLT; Rey, 1941), and the Rivermead Behavioral Memory Test paragraph recall (Wilson, Cockburn, & Baddeley, 1985). Reasoning ability was measured via tests requiring participants to identify patterns in letter or word series problems, including Word Series (Gonda & Schaie, 1985), Letter Series (Thurstone & Thurstone, 1949), and Letter Sets (Ekstrom, French, Harman, & Derman, 1976). Processing speed measures were timed and computer-administered, and required participants to identify and localize information at 75% accuracy under varying levels of cognitive demand. These included the three timed Useful Field of View (Ball & Roenker, 1998) subtests – stimulus identification, divided attention, and selective attention. Because multiple scores were collected for each underlying dimension, raw scores for each domain (memory, reasoning, and processing speed) were standardized so that a single composite score for each domain could be created. This composite score was then represented as the linear combination of the standardized measures, and Blom transformations were applied to yield more normally distributed scores (see Ball et al., 2002).
Everyday function. Everyday functional tasks included in ACTIVE were the Everyday Problems Test (EPT; Willis & Marsiske, 1993), Observed Tasks of Daily Living (OTDL; Diehl, Willis, & Schaie, 1995), and Timed Instrumental Activities of Daily Living (TIADL; Owlsey, Sloane, McGwin, & Ball, 2002). ACTIVE employed a shortened version of the EPT, which required participants to solve problems that may occur in everyday living that utilize printed materials (e.g., what to do when a washing machine won’t fill or agitate). Areas assessed included nutrition, medication, telephone use, household management, and transportation. Total scores ranged from 0 to 28, and represented number of items correctly answered (Willis & Marsiske, 1993). The OTDL addressed three instrumental activities of daily living domains (medications, phone usage, and financial management) and assessed functional ability via behavioral simulations through use of real-world props (e.g., money, pharmacy medication bottles). The OTDL consisted of 28 items on which scores were assigned. Thus, total scores ranged from 0 to 28 on this test (Diehl et al., 1995). The TIADL measure assessed five common domains of activities of daily living – communication, finances, cooking, shopping, and medicine – via behavioral simulations and tasks were scored on completion time. Deficits in accuracy on the TIADL tasks were penalized through standardized additions to completion time (Owsley et al., 2002).
Personal control beliefs. Personal control was measured by three Locus of Control scales derived from the Personality in Intellectual Aging Contexts (PIC) Inventory (Lachman, Baltes, Nesselroade & Willis, 1982). These scales were modeled after Levenson’s (1974) multidimensional locus of control instrument and include Internal, Chance, and Powerful Others. Additionally, the PIC contains three other scales concerned with intellectual behavior and aging that were not included in the present study because they are less clearly focused on control beliefs: Anxiety, Achievement-Motivation, and Attitude Toward Intellectual Aging. PIC scales demonstrate good reliability, with alpha coefficients ranging from .76 to .91 (Lachman et al., 1982). Other studies assessing reliability of the PIC Locus of Control scales yield similar coefficients (Grover & Hertzog, 1991; Miller & Gagne, 2005). In an effort to reduce participant burden, the PIC was shortened during the ACTIVE piloting phase. Items were arrayed in order from smallest to largest item-total correlation, and 50% of the items with the highest item-total correlation were selected. Alphas were recomputed for the shortened scales and these coefficients were virtually unchanged from the originals. The resulting instrument reduced each scale from 12 to 6 items. Responses are scored on a 6-point Likert-type scale ranging from 1 (strongly agree) to 6 (strongly disagree). For the scales focused on external loci of control (Chance and Powerful Others scales), higher total scores reflect greater beliefs in the control of external forces on aging outcomes (e.g., negative attitudes toward aging), whereas higher scores on the internal locus of control scale (Internal scale) signify stronger beliefs in one’s own capabilities (e.g., positive aging attitudes).
Life Space. The Life Space Questionnaire (LSQ; Stalvey et al., 1999) measures the spatial extent of mobility. An advantage of the LSQ is that it reflects actual behavior instead of perceived ability, the latter of which may be more subject to distortion. The questionnaire is comprised of nine items, with each item addressing a specific life-space zone or level. Zones can be conceptualized as concentric circles of geographic space, with zones farther from the center indicative of larger life space. Items on the LSQ represent these zones and progress from movement within the home to immediately outside of the home, within the neighborhood, and eventually to outside one’s region of the United States. Though the original LSQ scale measures movement across all nine zones within a 3-day period, this time frame was modified for the ACTIVE trial. In this modified version, respondents are asked whether or not they have been to certain zones within “the past seven days, not including today” (Questions 1–6) or within “the past two months, not including today” (Questions 7–9), regardless of whether they drove themselves or not. A “yes” response receives 1 point, while a “no” response is scored as 0. Total LSQ scores can range from 0 (complete restriction) to 9 (no restriction); thus, higher scores are indicative of larger life space. The LSQ was originally examined in a sample of older adults ranging in age from 55–85 years, with African Americans comprising 17% of the sample. Test-retest reliability for most LSQ items was excellent (over 90% agreement), with a resulting Cronbach’s reliability coefficient alpha of 0.80 (Stalvey et al., 1999). Both construct and criterion validity were found to be good.
Covariates. The following factors were controlled for in all analyses: age, race (white/non-white), gender, years of education, depressive symptoms, and physical function. Depressive symptoms were ascertained from the 12-item version of the Center for Epidemiological Studies-Depression scale (CES-D), a reliable and valid measure of depressive symptomatology (Radloff, 1977). Responses to each question are based on a Likert scale from 0 (“rarely or none of the time”) to 3 (“most or all of the time”). Therefore, total scores on the questionnaire can range from 0 (no depressive symptoms) to 36 (depressive symptoms endorsed most or all of the time). Physical function was assessed via the Physical Functioning scale of the Short Form-36 Questionnaire (SF-36 PF). The Physical Functioning Scale is a self-rated measure comprised of 10 items that evaluate current physical function. It is scored from 0 to 100 points by coding, summating, and transforming individual item scores in accordance with the SF-36 manual and scoring software, with higher scores indicative of greater overall physical functioning (Ware, Snow, Kosinski, & Gandek, 1993).
Statistical Analyses
Prior to the secondary data analyses for the current study, data were screened for data-entry errors, outliers, and missing data. Frequencies and descriptive statistics were used to review characteristics of the current sample, and correlations between variables were examined for both demographic factors and cognitive measures.
The relationship between cognitive function and life space was examined based on a series of multiple regression models. Comparisons between predictive values of the different domains of cognition (memory, reasoning, and processing speed) were made by examining each domain in separate models including covariates. A hierarchical model was utilized to ascertain whether tests of everyday problem-solving abilities (functional tests) accounted for a significant portion of variance over and above that accounted for by the more traditional cognitive tests.
To assess potential moderation by personal control beliefs (as measured by the three PIC scales) on the relationship between cognitive function and life space, the predictor variables were first mean centered. Interaction terms were created using the cross-products of each of the centered PIC scores and the respective measure of cognitive function. Interaction terms were added to each separate model and tested for significance, with alpha set at .05. Age, gender, years of education, and race were accounted for in all models, as were depressive symptoms and physical health status.
Results
Sample Descriptives
During the data screening process, outliers were detected on the CES-D 12-item scale, a measure of depressive symptoms. Post-hoc analyses were conducted with and without these participants, with no change in results. Given that these outliers had virtually no effect on the data analyses and were deemed to be representative of the population from which they were drawn, they were included in the final analyses. Furthermore, this allowed controlling for depressive symptoms of all severity. Data were incomplete for some measures of interest, thereby reducing the sample size for all complete measures to 2,737 persons. However, missingness on any one measure was less than 2.5% of the complete sample.
The current sample was mostly female (76%), with good minority representation (27% African American). Mean global cognitive function, as measured by the MMSE, was in the normal range (mean MMSE = 27; standard deviation = 2.0). Mean scores on the Life Space Questionnaire indicated that the average participant had ventured outside his or her county or city within the past two months (mean LSQ = 7; standard deviation = 1.3). The sample was generally well-educated, reported few depressive symptoms, and was in good physical health (see Table 1).
Table 1.
Sample Characteristics (N = 2,737)
| Range | Number (%) | Mean (SD) | |
|---|---|---|---|
| Age | 65 – 94 | 73.6 (5.9) | |
| Female gender | 2080 (75.9) | ||
| African-American | 731 (26.7) | ||
| Years of education | 4 – 20 | 13.5 (2.7) | |
| MMSE | 23 – 30 | 27.3 (2.0) | |
| CES-D 12-item | 0 – 34 | 5.2 (5.1) | |
| SF-36 Physical Component | 0 – 100 | 68.8 (24.1) | |
| Memory Composite | −8.2 – 8.3 | 0 (2.5) | |
| Reasoning Composite | −7.8 – 10.5 | 0 (2.7) | |
| Processing Speed Composite | −7.9 – 4.1 | 0 (2.5) | |
| TIADL | 46.0 – 606.5 | 139.2 (74.1) | |
| OTDL | 1 – 28 | 17.6 (4.4) | |
| EPT | 0 – 28 | 18.7 (5.7) | |
| PIC1 (Internal) | 5 – 36 | 30.9 (4.5) | |
| PIC2 (Chance) | 5 – 36 | 17.5 (7.3) | |
| PIC3 (Powerful Others) | 3 – 36 | 15.1 (6.7) | |
| Life space | 1 – 9 | 7.2 (1.3) |
Note: SD = standard deviation
TIADL: Timed Activities of Daily Living; OTDL: Observed Tasks of Daily Living; EPT: Everyday Problems Test
PIC1: Internal Control Scale; PIC2: Chance Control Scale; PIC3: Powerful Others Control Scale
Correlations among demographic variables and life space were examined. Life space was significantly correlated with gender, age, race, education, global cognitive function, and physical health (see Table 2). Specifically, male gender, younger age, Caucasian race, and greater education were all associated with larger life space. Additionally, those with greater global mental status and better physical health had higher life space scores.
Table 2.
Correlations among Participant Characteristics and Life Space
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1 Gender (female) | 1 | |||||||
| 2 Race (white) | −.103** | 1 | ||||||
| 3 Age | −.028 | .141** | 1 | |||||
| 4 Years of Education | −.194** | .114** | −.043* | 1 | ||||
| 5 MMSE | −.052** | .208** | −.146** | .299** | 1 | |||
| 6 CES-D 12-item | .072** | .011** | .110** | −.189** | −.165** | 1 | ||
| 7 SF-36 Physical Component | −.129** | .095** | −.184** | .173** | .151** | −.302** | 1 | |
| 8 Life space | −.079** | .092** | −.153** | .239** | .171** | −.141** | .229** | 1 |
Notes: N=2,737
p<.05,
p<.001
MMSE: Mini-Mental State Examination; CES-D: Center for Epidemiological Studies-Depression Scale; SF-36: Short Form-36 Questionnaire
Table 3 displays the correlations between the cognitive domains, control beliefs, and life space. The cognitive domain scores were significantly correlated, and each of the PIC scales was significantly correlated with memory, reasoning, and processing speed domains, with the strongest associations for memory and reasoning. All cognitive variables shared significant associations with life space. The PIC1 scale (Internal Control) was positively correlated with life space, while the PIC2 (Chance Control) and PIC3 (Powerful Others) scales were negatively correlated with life space, indicating that negative aging beliefs and increased dependence on others are related to smaller life space (see Table 3).
Table 3.
Significant (p<.001) Correlations among Cognitive and Everyday Measures, Control Beliefs, and Life Space
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 Memory | 1 | |||||||||
| 2 Reasoning | .580 | 1 | ||||||||
| 3 Processing Speed | −.433 | −.516 | 1 | |||||||
| 4 TIADL | −.469 | −.523 | .382 | 1 | ||||||
| 5 OTDL | .492 | .550 | −.394 | −.512 | 1 | |||||
| 6 EPT | .578 | .700 | −.417 | −.599 | .608 | 1 | ||||
| 7 PIC1 | .288 | .338 | −.225 | −.245 | .285 | .356 | 1 | |||
| 8 PIC2 | −.328 | −.324 | .220 | .270 | −.299 | −.355 | −.350 | 1 | ||
| 9 PIC3 | −.346 | −.478 | .284 | .339 | −.371 | −.499 | −.519 | .524 | 1 | |
| 10 Life space | .206 | .259 | −.185 | −.232 | .212 | .268 | .144 | −.166 | −.192 | 1 |
Notes: N=2737
TIADL: Timed Activities of Daily Living; OTDL: Observed Tasks of Daily Living; EPT: Everyday Problems Test
PIC1: Internal Control Scale; PIC2: Chance Control Scale; PIC3: Powerful Others Control Scale
Objective Cognitive Function and Life Space
A series of multiple regression models was utilized to separately evaluate the relationships between memory, reasoning, and processing speed composites and life space. Each model controlled for age, race, gender, years of education, depressive symptoms, and physical functioning. In the memory composite model, life space was significantly associated with memory function F (7, 2729) = 52.49, p < .001, with R2 of .119. The adjusted R2 value indicates that approximately 11.5% of the variability in life space is predicted by the demographic factors and objective memory function. When composite reasoning was examined, it too yielded a significant test statistic, F (7, 2729) = 53.80, p < .001, with R2 of .121 and an adjusted R2 of .119. The regression model for speed of processing was also significant, F (7, 2705) = 50.41, p < .001. R2 was .115, and adjusted R2 was .113.
Similarly, each composite domain of cognitive function predicted life space in separate models (memory β =.089, p < .001; reasoning β = .117, p < .001; speed of processing β = −.067; p = .001), after controlling for the demographic factors previously mentioned. Though each composite yielded predictive value, reasoning most strongly predicted life space outcome. Additionally, age, years of education, and physical functioning were significantly associated with life space in all three composite models. Specifically, lower age, more years of education, and higher ratings of physical functioning contributed to larger life space independently from cognitive function. Race also emerged as a significant predictor, where Caucasian race was associated with larger life space (see Table 4).
Table 4.
Standardized† Associations for Measures of Cognitive Function and Life Space
| Predictor | Total Life Space | |||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |
| Age | −.122*** | −.091*** | −.087*** | −.092*** |
| Race (white)† | .205*** | .140** | .106* | .190*** |
| Gender (female)† | −.045 | −.103 | −.060 | −.036 |
| Years Education | .188*** | .166*** | .146*** | .181*** |
| CES-D 12-item | −.046** | −.036 | −.034 | −.044* |
| SF-36 PF | .151*** | .144*** | .145*** | .143*** |
| Memory Composite | .093*** | |||
| Reasoning Composite | .117*** | |||
| Speed Composite | −.067*** | |||
| Adjusted R-square | .111 | .116 | .119 | .113 |
| R-square | .113 | .119 | .121 | .115 |
| R-square change | .006*** | .009*** | .003*** | |
Notes: Model 1: Demographic factors (age, race, gender, years of education, CES-D 12-item score, and SF-36 Physical Component score) as predictors of life-space
Model 2: Memory composite score added to model (demographic factors as covariates)
Model 3: Reasoning composite score added to model (demographic factors as covariates)
Model 4: Processing speed composite score added to model (demographic factors as covariates)
p < .05;
p < .01;
p < .005
Unstandardized coefficients reported for race and gender only
To investigate whether performance-based measures of everyday function added predictive utility, these measures were included in additional separate multiple regression models controlling for demographic factors and the three cognitive composite scores. The addition of the TIADL to the model significantly improved predictive value, F (10, 2700) = 40.17, p < .001, with R2 of .130 and adjusted R2 of .126. The TIADL was also a significant predictor of life space (β = −.097, p < .001) in the context of the model. Addition of the EPT measure improved predictive value of the overall model, F (10, 2702) = 38.77, p < .001, with R2 of .125 (adjusted R2 = .122), and it emerged as a significant predictor of life space (β = .086, p = .003). Age, years of education, and physical functioning also remained significant demographic predictors of life space. While race was a significant factor in the previous analyses separately testing composite memory, reasoning, and processing domains, it was no longer significant in models that simultaneously included the three cognitive composites and everyday cognitive function (see Table 5).
Table 5.
Standardized† Associations for Measures of Everyday Function and Life Space
| Predictor | Total Life Space | |||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |
| Age | −.069*** | −.062*** | −.065*** | −.069*** |
| Race (white)† | .102 | .072 | .101 | .064 |
| Gender (female)† | −.087 | −.121* | −.086 | −.071 |
| Years Education | .147*** | .139*** | .144*** | .128*** |
| CES-D 12-item | −.032 | −.031 | −.030 | −.028 |
| SF-36 PF | .136*** | .130*** | .135*** | .139*** |
| Memory Composite | .048* | .032 | .039 | .028 |
| Reasoning Composite | .086*** | .059* | .076*** | .052 |
| Speed Composite | −.023 | −.013 | −.020 | −.020 |
| TIADL | −.097*** | |||
| OTDL | .037 | |||
| EPT | .084*** | |||
| Adjusted R-square | .120 | .126 | .120 | .122 |
| R-square | .123 | .130 | .123 | .125 |
| R-square change | .006*** | .001 | .003*** | |
Notes: Model 1: Demographic factors and memory, reasoning, and processing speed composite scores as predictors of life-space
Model 2: TIADL score added to model (demographic factors and cognitive composites as covariates)
Model 3: OTDL score added to model (demographic factors and cognitive composites as covariates)
Model 4: EPT score added to model (demographic factors and cognitive composites as covariates)
p < .05;
p < .01;
p < .005
Unstandardized Coefficients reported for Race and Gender only
Interaction of Control Beliefs and Cognitive Function
For the interaction analyses including cognitive composite scores and control beliefs, neither PIC1 (Internal Beliefs) nor PIC2 (Chance Control) showed significant moderator effects on the relationships between any of the three cognitive composites and life space. However, there was a significant interaction between PIC3 (Powerful Others) and composite memory (t = −2.07, p = .039), (see Tables 6a –c; Figure 1). The combination of high objective memory and low beliefs in the control of powerful others was associated with the highest life space.
Table 6a.
Interaction of Control Beliefs and Memory Predicting Life Space
| interaction b (SE) | interaction β | test statistic t | p-value for interaction | |
|---|---|---|---|---|
| PIC1 | .003 (.002) | .031 | 1.680 | .092 |
| PIC2 | .000 (.001) | −.010 | −.577 | .564 |
| PIC3 | −.003 (.001) | −.037 | −2.071 | .039 |
Table 6c.
Interaction of Control Beliefs and Processing Speed Predicting Life Space
| interaction b (SE) | interaction β | test statistic t | p-value for interaction | |
|---|---|---|---|---|
| PIC1 | −.002 (.002) | −.017 | −.924 | .355 |
| PIC2 | .000 (.001) | −.008 | −.443 | .658 |
| PIC3 | .001 (.001) | .007 | −.406 | .685 |
Notes: PIC1: Internal Control Scale
PIC2: Chance Control Scale
PIC3: Powerful Others Control Scale
Figure 1.
The Interaction of Memory Function and Beliefs in Powerful Others Control
Post-hoc interaction analyses including everyday performance-based measures and control beliefs yielded a significant interaction between PIC3 (Powerful Others) and Observed Tasks of Daily Living (OTDL) scales (t = 2.56, p = .011). The combination of low scores on the OTDL and high beliefs in powerful others control resulted in the lowest life space. No moderator effects were found for PIC1 (Internal Beliefs) or PIC2 (Chance Beliefs) on the relationships between any of the everyday performance-based measures and life space.
We also tested whether addition of an objective measure of physical function (number of steps to make a complete turn in place) and a social status measure (marital status) affected the relationship between cognitive function and life space. We tested each of the regression models with these variables included. While marital status was significantly associated with life space (p<.001) in all analyses (with married persons having higher life space scores), the addition of this variable into the models did not change previously significant relationships. The inclusion of objective physical function did not change previous results, and this variable was not a significant predictor of life space in the context of these regression models.
Discussion
This study examined the relationship between different domains of objective cognitive function and life space in a large sample of older adults, and also evaluated the potential influence of subjective control beliefs on this relationship. It is the first study to incorporate both objective cognitive function and subjective belief measures in relation to life space, as well as to examine the predictive utility of traditional cognitive measures in comparison to everyday functional tasks on life space.
Our results indicate that a positive relationship between cognitive function and life space exists among older adults, with memory, reasoning, and processing speed domains strongly and separately predictive of life space. Reasoning ability emerged as the strongest overall predictor in our analyses, and this is not surprising given that reasoning is considered a higher-order cognitive domain, encompassing many complex executive functions that include planning, organizing, decision-making, and judgment. Work by Royall, Palmer, Chiodo, and Polk (2004) found declines in executive function, which includes reasoning ability, to be predictive of changes in functional status in non-institutionalized older adults. Furthermore, these researchers found that executive control function predicted participants’ functional status independent of global cognitive function, as measured by the MMSE. Additionally, within the context of ACTIVE, Willis et al. (2006) discovered that among groups of older adults randomized to one of three cognitive training groups (memory, reasoning, processing speed), only those receiving reasoning training showed less functional decline on outcomes of activities of daily living. It therefore follows that the ability to navigate one’s environment (a similar functional outcome) – especially outside of smaller, more familiar geographic zones – is highly related to intact and efficient reasoning ability and executive function. Moreover, larger life space has been hypothesized to connote greater environmental complexity (Crowe et al., 2008), which may in turn require more reliance on executive functions such as reasoning for the planning, organization, and decision-making necessary for successful environmental navigation. In the present study, reasoning ability also mediated the largest portions of effects due to age, education, depressive symptoms, and race, suggesting that reasoning ability can be regarded as a complex cognitive domain that is related to one’s cognitive, environmental, and emotional experiences.
The present study also found that everyday performance-based measures with potentially more ecological validity are predictive of life space, even after controlling for cognitive composite scores comprised of traditional cognitive tests. The EPT and TIADL instruments emerged as significant predictors of life space, while the OTDL did not. Given the high correlation between OTDL and reasoning composite scores, and the strength of reasoning itself as a predictor, it is likely that the reasoning composite suppressed the association between OTDL and life space (when cognitive composites were excluded from the analysis, the association between OTDL and life space became significant). This finding adds to the growing body of literature supporting the utility of everyday cognitive measures in assessing functional outcomes (see work by Allaire & Marsiske, 1999; Willis, 1996; Chaytor & Schmitter-Edgecombe, 2003). Among older adults, effective means of predicting and assessing “real-life” functional outcomes – such as life space – are crucial given that, for this population especially, these types of factors are closely tied to quality of life and in many cases are necessary for maintaining independence (Gabriel & Bowling, 2004).
Mounting evidence, including the present study, supporting an association between life space and cognitive function carries important implications for older adults. While mobility declines can clearly have significant functional consequences, Crowe et al. (2008) found reduced life space to be predictive of future cognitive decline in older adults. Similarly, recent work by James, Boyle, Buchman, Barnes, and Bennett (in press) indicates that constricted life space is associated with increased risk of incident Alzheimer’s disease and mild cognitive impairment. Given that impairment in cognitive function carries its own set of risks and consequences, including depression, dependency, and mortality (Kelman, Thomas, Kennedy, & Cheng, 1994), these findings add further support for the importance of maintaining optimal range of life space and mobility in old age.
External control beliefs showed a significant moderator effect in our analyses. Specifically, stronger beliefs in powerful others control (i.e., greater dependence on others) resulted in smaller life space across levels of medium to high objective memory function. At lower levels of memory function, amount of life space did not appear to be as strongly affected by external control beliefs. However, at medium to high levels of objective memory function, it appears that a strong belief in powerful others control is associated with a reduction in overall life space compared to those with lower external control beliefs. This finding is notable and may be viewed as consistent with the notion of self-induced dependence (Langer & Benevento, 1978) in that some people may not have physical or cognitive problems yet still limit their mobility, perhaps in part due to negative aging self-perceptions and in accordance with the implicit expectations of others (influenced by negative aging stereotypes). Indeed, research suggests that older adults may be particularly vulnerable to such expectations (Sarkisian, Hays, & Mangione, 2002; Levy et al., 2002; Lineweaver, Berger, & Hertzog, 2009). Similar to the concept of the “social facilitation of the nonuse of competence” put forth by Bieman-Copland, Ryan, and Cassano (1998), it is possible this subset of older adults is particularly susceptible to negative social stereotypes of aging and, rather than functioning at their true ability level, they instead behave in ways that are believed to be expected of older persons. According to Hummert (1999), society is rife with negative stereotypes related to aging, and activation of such stereotypes can influence both the treatment of older adults by others and older adults’ own awareness of these negative beliefs. Furthermore, evidence indicates that aging stereotypes can not only heighten older adults’ awareness of others’ negative perceptions, they can actually impact and impede memory performance when activated (Hess et al., 2003; Levy, 1996). These findings are notable given that, relative to younger counterparts, older adults are more likely to attribute poor memory or cognitive performance to stable or dispositional factors rather than to situational variables (Lachman & McArthur, 1986; Weaver & Lachman, 1990). Likewise, exposure to positive beliefs on aging has been shown to enhance cognitive performance under certain conditions (Hess et al., 2003, Levy, 1996), while also demonstrating a protective effect against cardiovascular stress response (Levy, Hausdorff, Hencke, & Wei, 2000; Levy, Zonderman, Slade, and Ferrucci, 2009). Despite evidence to suggest that positive aging attitudes can be cognitively (and functionally) beneficial, many negative stereotypes continue to prevail in our society, and cognitive impairment or “senility” is frequently viewed as an anticipated consequence of aging. However, it is important to note that in our study sample, the majority of older adults reported generally large life space areas, an encouraging finding that supports the phenomenon of successful aging (Rowe & Kahn, 1987, 1998; Baltes & Baltes, 1990).
Beliefs in powerful others control also emerged as a moderator of the relationship between performance on the Observed Tasks of Daily Living (OTDL) – a measure of functional ability – and life space in post-hoc analyses. Persons with low OTDL scores and high beliefs in the control of powerful others exhibited the lowest life space. These findings indicate that high beliefs in powerful others control may exacerbate the effect of poor functional ability, in certain instances, on life space.
Interestingly, internal control beliefs did not demonstrate a moderator effect in the relationship between objective cognitive performance and life space. Given that internal control beliefs can be viewed as relatively stable attributions (Lachman & Leff, 1989), these beliefs may not be as vulnerable to the effects of aging stereotypes and negative self-perceptions as beliefs in powerful others control, thus reducing the possibility for interaction with objective cognitive performance on life space outcome. Additionally, study participants were high-functioning and mobile, with high mean self-ratings of internal locus of control; therefore, there was little range across levels of these variables, limiting the probability of significant moderation effects.
Although the present study highlighted a relationship between cognitive function and life space, and demonstrated that subjective control beliefs may, in some instances, moderate this relationship, there are several study limitations. The first limitation is the cross-sectional and correlational design of this analysis. Interpretations must be made with caution, and causal inferences or directionality cannot be determined. Additionally, the study sample was taken from baseline, shortly after study entry, and therefore the people included were largely cognitively healthy and intact, with good overall physical functioning and relatively large life space. Along the same vein, the dataset was comprised of participants who were able to attend the baseline study visit, and it is reasonable to assume that those experiencing moderate to extreme difficulties with respect to mobility would be less likely to join the study. Therefore, the select nature of the study sample may compromise the generalizability of our results to other populations. Overall, however, the sample was large and relatively diverse, and the findings that emerged appeared to be fairly robust across the different models. Finally, we acknowledge that income may be related to life space, and may partially explain the associations found for age, education, race, and gender. Adjustment for income was not possible since ACTIVE baseline assessment did not include a measure of income, and therefore this presents an additional study limitation.
Findings from the present study indicate that life space is strongly associated with cognitive function, and that those with better cognitive function (particularly reasoning ability) have a larger life space. This study also lends support to the utilization of everyday cognitive measures in assessing functional outcomes. Subjective control beliefs appeared to have moderation effects in certain conditions, indicating that future studies aimed at modifying attributions of powerful others control may be worthwhile for improving everyday function. Given that these results were found in a cross-sectional sample, future studies examining the relationships between these factors longitudinally may be able to further elucidate the important interrelationship of cognitive function, control beliefs, and life space.
Table 6b.
Interaction of Control Beliefs and Reasoning Predicting Life Space
| interaction b (SE) | interaction β | test statistic t | p-value for interaction | |
|---|---|---|---|---|
| PIC1 | .003 (.002) | .027 | 1.478 | .139 |
| PIC2 | .000 (.001) | .000 | .008 | .994 |
| PIC3 | .000 (.001) | −.007 | −.389 | .697 |
Acknowledgments
This research was supported in part by sponsorship from the UAB Center for Aging Research Scholarship in Aging, 2009–2010.
This research was conducted at the University of Alabama at Birmingham and was supported by grants from the National Institute on Aging for ACTIVE’s six field sites and the coordinating center (including: Hebrew Senior Life, Boston [NR04507], the Indiana University School of Medicine [NR04508], the Johns Hopkins University [AG14260], the New England Research Institutes [AG14282], the Pennsylvania State University [AG14263], the University of Alabama at Birmingham [AG14289], and the University of Florida [AG014276]) and Edward R. Roybal Center, p30 AG022838.
Contributor Information
Andrea C. Sartori, Department of Psychology, University of Alabama at Birmingham
Virginia G. Wadley, Division of Gerontology, Geriatrics, and Palliative Care, University of Alabama at Birmingham School of Medicine
Olivio J. Clay, Department of Psychology, University of Alabama at Birmingham
Jeanine M. Parisi, Department of Mental Health, Johns Hopkins Bloomberg School of Public Health
George W. Rebok, Department of Mental Health, Johns Hopkins Bloomberg School of Public Health
Michael Crowe, Department of Psychology, University of Alabama at Birmingham.
References
- Allaire JC, Marsiske M. Everyday cognition: Age and intellectual ability correlates. Psychology and Aging. 1999;14:627–644. doi: 10.1037//0882-7974.14.4.627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: 2000. text revision. [Google Scholar]
- Avorn J, Langer E. Induced disability in nursing home patients: A controlled trial. Journal of the American Geriatrics Society. 1982;30:397–400. doi: 10.1111/j.1532-5415.1982.tb02839.x. [DOI] [PubMed] [Google Scholar]
- Baker PS, Bodner EV, Allman RM. Measuring life-space mobility in community-dwelling older adults. Journal of the American Geriatric Society. 2003;51:1610–1614. doi: 10.1046/j.1532-5415.2003.51512.x. [DOI] [PubMed] [Google Scholar]
- Ball KK, Roenker DL. UFOV Useful Field of View Manual. San Antonio, TX: The Psychological Corporation; 1998. [Google Scholar]
- Ball K, Berch DB, Helmers KF, Jobe JB, Leveck MD, Marsiske M, Morris JN, Rebok GW, Smith DM, Tennstedt SL, Unverzagt FW, Willis SL. Effects of cognitive training interventions with older adults: A randomized controlled trial. Journal of the American Medical Association. 2002;288:2271–2281. doi: 10.1001/jama.288.18.2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baltes PB, Baltes MM. Psychological perspectives on successful aging: The model of selective optimization with compensation. In: Baltes PB, Baltes MM, editors. Successful aging: Perspectives from the behavioral sciences. New York: Cambridge University Press; 1990. pp. 1–27. [Google Scholar]
- Barnes LL, Wilson RS, Bienias JL, Mendes de Leon CF, Kim HJN. Correlates of life space in a volunteer cohort of older adults. Experimental Aging Research. 2007;33:77–93. doi: 10.1080/03610730601006420. [DOI] [PubMed] [Google Scholar]
- Bieman-Copland S, Ryan EB, Cassano J. Responding to the challenges of late life. In: Pushkar D, Bukowski WM, Schwartzman AE, Stack DM, White DR, editors. Improving competence across the lifespan: Building interventions based on theory and research. New York: Plenum; 1998. pp. 141–157. [Google Scholar]
- Brandt J. The Hopkins Verbal Learning Test: Development of a new memory test with six equivalent forms. Clinical Neuropsychologist. 1991;5:125–142. [Google Scholar]
- Chaytor N, Schmitter-Edgecombe M. The ecological validity of neuropsychological tests: A review of the literature on everyday cognitive skills. Neuropsychology Review. 2003;13:181–197. doi: 10.1023/b:nerv.0000009483.91468.fb. [DOI] [PubMed] [Google Scholar]
- Clay OJ, Edwards JD, Ross LA, Okonkwo O, Wadley VG, Roth DL, Ball KK. Visual function and cognitive speed of processing mediate age-related decline in memory span and fluid intelligence. Journal of Aging & Health. 2009;21:547–566. doi: 10.1177/0898264309333326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowe M, Andel R, Wadley VG, Okonkwo OC, Sawyer P, Allman RM. Life-space and cognitive decline in a community-based sample of African American and Caucasian older adults. The Journal of Gerontology: Biological Sciences. 2008;63A:1241–1252. doi: 10.1093/gerona/63.11.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diehl M, Willis SL, Schaie KW. Everyday problem solving in older adults: Observational assessment and cognitive correlates. Psychology and Aging. 1995;10:478–491. doi: 10.1037//0882-7974.10.3.478. [DOI] [PubMed] [Google Scholar]
- Ekstrom RB, French JW, Harman H, Derman D. Kit of factor referenced cognitive tests. Princeton, NJ: Educational Testing Service; 1976. rev. [Google Scholar]
- Ellison JM. A review of mild cognitive impairment: Normal cognitive aging, mild cognitive impairment, and dementia. Journal of the American Medical Association. 2008;300:1566–1574. doi: 10.1001/jama.300.9.jrr80008. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. ‘Mini-Mental State’: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gabriel Z, Bowling A. Quality of life from the perspectives of older people. Ageing and Society. 2004;24:675–691. [Google Scholar]
- Gonda J, Schaie KW. Schaie-Thurstone Mental Abilities Test: Word Series Test. Palo Alto, CA: Consulting Psychologists Press; 1985. [Google Scholar]
- Grover DR, Hertzog C. Relationships between intellectual control beliefs and psychometric intelligence in adulthood. Journal of Gerontology. 1991;46:109–115. doi: 10.1093/geronj/46.3.p109. [DOI] [PubMed] [Google Scholar]
- Hess TM, Auman C, Colcombe SJ, Rahhal TA. The impact of stereotype threat on age differences in memory performance. The Journal of Gerontology: Psychological Sciences. 2003;58B:3–11. doi: 10.1093/geronb/58.1.p3. [DOI] [PubMed] [Google Scholar]
- Hummert ML. A social cognitive perspective on age stereotypes. In: Hess TM, Blanchard-Fields F, editors. Social cognition and aging. San Diego, CA: Academic Press; 1999. pp. 175–196. [Google Scholar]
- James BD, Boyle PA, Buchman AS, Barnes LL, Bennett DA. Life space and risk of Alzheimer’s disease, mild cognitive impairment, and cognitive decline in old age. The American Journal of Geriatric Psychiatry: Advanced Access. doi: 10.1097/JGP.0b013e318211c219. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jobe JB, Smith DM, Ball K, Tennstedt SL, Marsiske M, Willis SL, Rebok GW, Morris JN, Helmers KF, Leveck MD, Kleinman K. ACTIVE: A cognitive intervention trial to promote independence in older adults. Controlled Clinical Trials. 2001;22:453–479. doi: 10.1016/s0197-2456(01)00139-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelman HR, Thomas C, Kennedy GJ, Cheng J. Cognitive impairment and mortality in older community residents. American Journal of Public Health. 1994;84:1255–1260. doi: 10.2105/ajph.84.8.1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachman ME, Baltes P, Nesselroade JR, Willis SL. Examination of personality-ability relationships in the elderly: The role of the contextual (interface) assessment mode. Journal of Research in Personality. 1982;16:485–501. [Google Scholar]
- Lachman ME. Locus of control in aging research: A case for multidimensional and domain-specific assessment. Journal of Psychology and Aging. 1986;1:34–40. doi: 10.1037//0882-7974.1.1.34. [DOI] [PubMed] [Google Scholar]
- Lachman ME, McArthur LZ. Adulthood age differences in causal attributions for cognitive, physical and social performance. Psychology and Aging. 1986;1:127–132. doi: 10.1037//0882-7974.1.2.127. [DOI] [PubMed] [Google Scholar]
- Lachman ME, Leff R. Perceived control and intellectual functioning in the elderly: A 5-year longitudinal study. Developmental Psychology. 1989;25:722–728. [Google Scholar]
- Langer EJ, Rodin J. The effects of choice and enhanced personal responsibility for the aged: A field experiment in an institutional setting. Journal of Personality and Social Psychology. 1976;34:191–198. doi: 10.1037//0022-3514.34.2.191. [DOI] [PubMed] [Google Scholar]
- Langer EJ, Benevento A. Self-induced dependence. Journal of Personality and Social Psychology. 1978;36:886–893. [Google Scholar]
- Levenson H. Activism and powerful others: Distinctions within the concept of internal-external control. Journal of Personality Assessment. 1974;38:377–383. [Google Scholar]
- Levy BR. Improving memory in old age by implicit self-stereotyping. Journal of Personality and Social Psychology. 1996;71:1092–1107. doi: 10.1037//0022-3514.71.6.1092. [DOI] [PubMed] [Google Scholar]
- Levy BR, Hausdorff JM, Hencke R, Wei JY. Reducing cardiovascular stress with positive self-stereotypes of aging. Journal of Gerontology: Psychological Sciences. 2000;55B:205–231. doi: 10.1093/geronb/55.4.p205. [DOI] [PubMed] [Google Scholar]
- Levy BR, Slade MD, Kasl SV. Longitudinal benefit of positive self-perceptions of aging on functional health. Journal of Gerontology: Psychological Sciences. 2002;57B:409–417. doi: 10.1093/geronb/57.5.p409. [DOI] [PubMed] [Google Scholar]
- Levy BR, Zonderman AB, Slade MD, Ferrucci L. Age stereotypes held earlier in life predict cardiovascular events in later life. Psychological Science. 2009;20:296–298. doi: 10.1111/j.1467-9280.2009.02298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lineweaver TT, Berger AK, Hertzog C. Expectations about memory change across the life span are impacted by aging stereotypes. Psychology and Aging. 2009;24:169–176. doi: 10.1037/a0013577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marson DC, Sawrie SM, Snyder S, McInturff B, Stalvey T, Boothe A, Aldridge T, Chatterjee A, Harrell LE. Assessing financial capacity in patients with Alzheimer’s disease: A conceptual model and prototype instrument. Archives of Neurology. 2000;57:877–884. doi: 10.1001/archneur.57.6.877. [DOI] [PubMed] [Google Scholar]
- May D, Nayak USL, Isaacs B. The life space diary: A measure of mobility in old people at home. International Rehabilitation Medicine. 1985;7:182–186. doi: 10.3109/03790798509165993. [DOI] [PubMed] [Google Scholar]
- Miller PH. Theories of developmental psychology. 2. New York: W.H. Freeman and Company; 1989. [Google Scholar]
- Miller LM, Gagne DD. Effects of age and control beliefs on resource allocation during reading. Aging, Neuropsychology, and Cognition. 2005;12:129–148. [Google Scholar]
- Mirowsky J, Ross CE. Education, social status, and health. New York: Aldine de Gruyter; 2003. [Google Scholar]
- Owsley C, Sloane M, McGwin G, Ball Timed Instrumental Activities of Daily Living: Relationship to cognitive function and everyday performance assessments in older adults. Gerontology. 2002;48:254–265. doi: 10.1159/000058360. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Applied Psychological Measures. 1977;1:385–401. [Google Scholar]
- Rey A. L’examen psychologique dans les cas d’encephalopathie tramatique. Archives de Psychologie. 1941;28:215–285. [Google Scholar]
- Rowe JW, Kahn RL. Human aging: Usual and successful. Science. 1987;237:143–149. doi: 10.1126/science.3299702. [DOI] [PubMed] [Google Scholar]
- Rowe JW, Kahn RL. Successful aging. New York: Plenum; 1998. [Google Scholar]
- Royall DR, Palmer R, Chiodo LK, Polk MJ. Declining executive control in normal aging predicts change in functional status: The Freedom House Study. Journal of the American Geriatrics Society. 2004;52:346–352. doi: 10.1111/j.1532-5415.2004.52104.x. [DOI] [PubMed] [Google Scholar]
- Sarkisian CA, Hays RD, Mangione CM. Do older adults expect to age successfully? The association between expectations regarding aging and beliefs regarding healthcare seeking among older adults. Journal of the American Geriatrics Society. 2002;50:1837–1843. doi: 10.1046/j.1532-5415.2002.50513.x. [DOI] [PubMed] [Google Scholar]
- Soederberg LM, Lachman ME. The sense of control and cognitive aging: Toward a model of mediational processes. In: Hess TM, Blanchard-Fields F, editors. Social cognition and aging. New York: Academic Press; 1999. pp. 17–41. [Google Scholar]
- Stalvey BT, Owsley C, Sloane ME, Ball K. The Life Space Questionnaire: A measure of the extent of mobility of older adults. Journal of Applied Gerontology. 1999;18:460–478. [Google Scholar]
- Suhr JA, Kinkela JH. Perceived threat of Alzheimer Disease (AD): The role of personal experience with AD. Alzheimer Disease and Associated Disorders. 2007;21:225–231. doi: 10.1097/WAD.0b013e31813e6683. [DOI] [PubMed] [Google Scholar]
- Thurstone LL, Thurstone TG. Examiner manual for the SRA Primary Mental Abilities Test (Form 10–14) Chicago: Science Research; 1949. [Google Scholar]
- Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey: Manual and interpretation guide. Boston: The Health Institute; 1993. [Google Scholar]
- Weaver SL, Lachman ME. When Memory Fails: Adulthood Age Differences in Attributions for Memory. Paper presented at the American Psychological Association Meetings; Boston, Massachusetts. 1990. Aug, [Google Scholar]
- Weber SC, Porter MM, Menec VH. Mobility in older adults: A comprehensive framework. The Gerontologist. 2010;50:443–450. doi: 10.1093/geront/gnq013. [DOI] [PubMed] [Google Scholar]
- Welch DC, West RL. Self-efficacy and mastery: Its application to issues of environmental control, cognition, and aging. Developmental Review. 1995;15:150–171. [Google Scholar]
- Willis SL, Marsiske M. Manual for the Everyday Problems Test. University Park: Department of Human Development and Family Studies, Pennsylvania State University; 1993. [Google Scholar]
- Willis SL. Everyday cognitive competence in elderly persons: conceptual issues and empirical findings. The Gerontologist. 1996;36:595–601. doi: 10.1093/geront/36.5.595. [DOI] [PubMed] [Google Scholar]
- Willis SL, Tennstedt SL, Marsiske M, Ball KK, Elias J, Koepke KM, Morris JN, Rebok GW, Unverzagt FW, Stoddard AM, Wright E. Long-term effects of cognitive training on everyday functional outcomes in older adults. Journal of the American Medical Association. 2006;296:2805–2814. doi: 10.1001/jama.296.23.2805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson BA, Cockburn J, Baddeley A. The Rivermead Behavioral Memory Test. Reading, UK: Thames Valley Test; 1985. [Google Scholar]
- Xue QL, Fried LP, Glass TA, Laffan A, Chaves PHM. Life-space constriction, the development of frailty, and the competing risk of mortality. American Journal of Epidemiology: Advanced Access Online. 2007:1–9. doi: 10.1093/aje/kwm270. [DOI] [PubMed] [Google Scholar]
- Yeom HA, Fleury J, Keller C. Risk factors for mobility limitation in community-dwelling older adults: A social ecological perspective. Geriatric Nursing. 2008;29:133–140. doi: 10.1016/j.gerinurse.2007.07.002. [DOI] [PubMed] [Google Scholar]