Abstract
Mindfulness involves nonjudgmental attention to present-moment experience. In its therapeutic forms, mindfulness interventions promote increased tolerance of negative affect and improved well being. However, the neural mechanisms underlying mindful mood regulation are poorly understood. Mindfulness training appears to enhance attentional monitoring systems in the brain, supported by the anterior cingulate and lateral prefrontal cortices. In emotion regulation, this prefrontal training seems to promote the stable recruitment of a non-conceptual sensory pathway, an alternative to conventional cognitive reappraisal strategies. In neural terms, the transition to non-conceptual awareness involves reducing habitual evaluative processing supported by midline structures of the prefrontal cortex. Instead, attentional resources are directed towards a limbic pathway for present-moment sensory awareness, involving the thalamus, insula, and primary sensory regions. In patients with affective disorders, mindfulness training acts as an alternative to cognitive efforts to control emotion, instead directing attention towards broadly monitoring fluctuations in momentary experience. Limiting cognitive elaboration in favor of momentary awareness appears to reduce automatic negative self-evaluation, increase tolerance for negative affect and pain, and help to engender self-compassion and empathy in chronically dysphoric individuals.
Keywords: Attention, Emotion Regulation, Intervention, MBCT, MBSR, Mechanism, Meditation, Mindfulness, Neuroscience, Stress
Over the past 30 years, numerous patients have benefited from mindfulness-based group interventions (Baer 2003; Ospina et al., 2007), such as Mindfulness-Based Stress Reduction (MBSR; Kabat-Zinn, 1990) and Mindfulness-Based Cognitive Therapy (MBCT; Segal et al., 2002) that are designed to target a range of physical (MBSR) or mental health (MBCT) symptoms. While recent clinical studies have validated the efficacy of these interventions, our understanding of the mechanisms underlying adaptive affect regulation through the practice of mindfulness is still nascent. In this article, we review findings from cognitive neuroscience to identify potential neural pathways through which sustained training in mindfulness meditation alters dysregulated emotional experience in order to improve well-being.
Normative strategies for emotion regulation are predicated on reappraising aversive events in a more positive, narrative based-context, or on behavioral strategies for the suppression of emotionally expressive behaviour (Goldin et al. 2008; Gross, 2002). Mood disorders, however, are broadly characterized by a failure to adaptively regulate emotion, due to heightened negative reactivity and increased self-focus (Clark et al., 1994). These can combine to reduce a patient’s ability to enact reappraisal in the face of stressful stimuli. In such situations, mindful emotion regulation may be of service, offering a non-evaluative means by which to attend to negative emotional experience.
Mindfulness has been described as “paying attention to relevant aspects of experience in a nonjudgmental manner” (Ludwig & Kabat-Zinn, 2008) and differs from conventional emotional regulation strategies such as cognitive reappraisal, which relies on memory and evaluation to re-interpret negative experiences (Gross, 2002; Ochsner et al., 2004). While both reappraisal and mindful emotion regulation likely share common features of attention, we argue that a model of mindful emotion regulation requires two processes that are distinct from reappraisal: 1) attention to present moment sensation, as distinct from delving into memory or cognitive elaboration, and 2) equanimity, the suspension of judging experience to be intrinsically good or bad.
For example, when waiting to make a safe turn in traffic, another driver behind in the cue may honk irately, heedless of pedestrians crossing ahead. Following this event, one’s thoughts may focus repetitively on evaluations of the situation, both to justify one’s own behavior, and to rail against the improbity and ignorance of the offending party. In the absence of emotion regulation, an unintended effect of such cognition is rumination: the constant recollection of the stressful situation, recreating feelings of upset and negativity. In the case of reappraisal, the tone of evaluation may shift: perhaps the honk-happy motorist was rushing to get home to a sick child, a mitigating circumstance that renders the behavior less egregious. However, even in this case of gracious reappraisal, attention is repeatedly directed towards the inciting event, again recalling the stressor it is intended to defuse. In mindfulness however, the individual allows the stressful event to remain in the past, and instead focuses on present moment sensations, questioning: how does the body feel in reaction to what’s happened? Is there tightness in one’s hands on the wheel, in the chest? Are thoughts beginning to race, creating an almost palpable pull to replay and dissect recent events? Mindfulness training seeks to limit the need to manipulate emotions through evaluation, to rationally control the situation, in favor of bringing curiosity and acceptance to present moment experience. The offending driver, regardless of his or her true motivations, is left in the past where they can cause no further upset.
Cognitive neuroscience has begun to identify neural correlates of nonjudgmental, momentary attention, an emergent pattern of activity associated with mindfulness-based interventions. Indeed, there appear to be distinct pathways in the brain that distinguish unfettered emotional reactivity from cognitive reappraisal and mindfulness. We provide a theoretical account of these distinctions, in the hopes of laying the groundwork for a scientific understanding of mindful emotion regulation. Before proceeding, it should be mentioned that mindfulness is but one format of practice within the larger family of meditation techniques; it is distinct from many forms of meditation in that it aims to broaden rather than focus attention, differing from purely concentrative practices that seek to sustain attention towards a single sensory object (Dunn et al., 1999; Lutz et al., 2008a). Mindfulness interventions do begin with concentrative attention practices, such as attending to parts of the body or one’s breath, initially seeking to strengthen attentional control. Practice however then transitions to more ‘open monitoring’ practices of widespread attention to all sensations, thoughts and emotions. We will begin by addressing focal attention training in this review, and then focus primarily on the neural correlates of ‘open’ mindful emotion regulation.
A Neural Account of Emotion Regulation
At its heart, emotional experience involves the integration of visceral signals from the limbic cortices through the cognitive appraisal of these signals in the prefrontal cortex (PFC) (Scherer et al., 2001; Davidson, 2002). In healthy individuals, cognitive reappraisal of emotion can occur through the top-down prefrontal regulation of limbic activity, using elaboration to recast initially negative appraisals as being less negative (Ochsner et al. 2002, 2004; Phan et al., 2005). In mood disorders however, this cognitive control appears to be impaired, as evidenced by compromised connectivity between the PFC and limbic regions such as the amygdala (Johnstone et al., 2007; Ressler & Mayberg, 2007). Thus, activating PFC regions in efforts to reappraise negative feelings may backfire, bringing attention to focus on dysphoric mood without a commensurate reduction in the intensity of negative feelings.
Subjective reports from patients with mood disorders corroborate the theory of impaired top-down control: effortful down-regulation of sadness is perceived as more difficult by patients with a mood disorder (Keightley et al., 2003), for whom self-compassion seems like a worthwhile but unachievable strategy (Pauley & McPherson, 2010). An important clinical implication of these findings is that for patients with a mood disorder, instructions to cognitively regulate negative emotion may be maladaptive, as emotional information from the limbic system is not impacted by efforts to engage the prefrontal cortices. Instead, habitual dysphoric interpretations are recreated during attempts to reappraise negative emotion, leading to rumination, in which elaborating on negative affect ironically perpetuates dysphoric mood (Nolen-Hoeksema, 2000; Watkins et al., 2008).
In addition to reduced fronto-limbic connectivity, compromised emotion regulation also manifests in maladaptive patterns of neural activation: a potential consequence of impaired top-down cognitive control is the emergence of exaggerated prefrontal recruitment in afflicted patients. Atypically diffuse prefrontal recruitment has been found in depressed patients during the performance of cognitive tasks (Sheline et al., 2009), and during task-free neuroimaging (Sheline et al., 2010). Furthermore, the extent of prefrontal activation in response to an emotional stressor appears to predict depressive relapse in patients with recurrent unipolar depression (Farb et al., 2011). The identification of heightened prefrontal reactivity as a marker of depression vulnerability belies suggestions that patients are simply not exerting enough effort to reappraise negative experience. Instead, it appears that for individuals with mood disorders, cognitive reappraisal may simply be an ineffective strategy; it is therefore important for these afflicted individuals to find an emotion regulation strategy that is less reliant upon top-down prefrontal modulation of emotion.
Mindful Emotion Regulation
If the engagement of a patient’s cognitive faculties only serves to exacerbate negative mood states, one might question how any behavioral intervention can effect positive change. Since cognitive elaboration automatically triggers negative self-judgments that cannot be voluntarily overridden, mindfulness training attempts to correct automatic dysphoric evaluation through an attention to sensation rather than evaluation. Through the cultivation of attention to unelaborated, present moment sensation, mindfulness presents patients with a task that does not require the deployment of evaluative cognition. Furthermore, by explicitly practicing equanimity, patients can begin to recognize and disengage from conceptual judgment in response to their sensory experiences. Encouragingly, such sensory practices seem to activate distinct cortical regions from the dysfunctional prefrontal-limbic loop.
The therapeutic method for reducing reliance on PFC activation is simple but challenging: mindfulness training exercises begin with the concentrative practice of attending to physical sensations, such as fine grained ‘body scans’, in which individuals attend to physical sensation from specific body parts or feelings of respiration (Kabat-Zinn, 1990). The goal of such practices are to improve access to the constantly shifting sensory experiences available in present-moment sensation, and to develop insight as to when one’s mind has wandered so that attention may be redirected to the present moment. Encouragingly, short term mindfulness interventions appear to increase the ability to notice changes in the sensory field and refocus attention appropriately (Jha et al., 2007). In comparisons of concentrative meditation against active control conditions such as simple arithmetic (Holzel et al., 2007), or visual object discrimination (Baron Short et al., 2007), meditation increases recruitment of the anterior cingulate, supporting an account of its role in non-elaborative monitoring during meditative states. As mindfulness-based interventions begin with such concentrative practices, an early property of mindful emotion regulation appears to be the cingulate-driven cultivation of sustained awareness, despite the presence of salient impulses to evaluate or elaborate upon experience.
Mindfulness, however, is not limited to the cultivation of focal attention, but also involves leveraging this increased attentional control to reduce habitual patterns of evaluation. Mindfulness training appears to help reduce cognitive rumination (Ramel et al., 2004), a pattern of self-critical elaboration liked to midline PFC reactivity in depression (Grimm et al., 2008; Cooney et al., 2010; Farb et al., 2011). The midline PFC appears to be recruited in response to negative mood induction (Farb et al., 2010), reading self-referential trait words (Farb et al., 2007) and exposure to negative-self beliefs (Goldin et al., 2010). In community samples, MBSR has been associated with decreased activation of these cortical midline structures (Goldin et al., 2009; Farb et al., 2010), and efforts to mindfully attend to experience can reduce cortical midline activity even in untrained individuals (Farb et al., 2007). Several other studies have observed more extensive reductions in cortical activity during meditation (Lou et al., 1999, Lazar et al., 2000, Baerensten et al., 2010, Ives-Deliperi 2011), an effect that appears to increase with greater meditation experience (Brefczynski-Lewis, 2007). Thus, it may be argued that one function of mindfulness training is to suspend or disrupt negative or self-critical appraisal associated with cortical midline activity.
It would be reasonable at this point to infer from discussions of reduced cortical activity that mindful emotion regulation involves the suppression of cognitive processing, a sort of nihilistic regulatory strategy. However, mindful emotion regulation does not aim to inhibit elaborative processing through thought avoidance, a strategy that predicts dysphoric affect (Ottenbreit & Dobson, 2004). Instead, attention is positively directed towards present moment sensation, providing a non-conceptual and non-threatening focus for attention that does not rely upon cortical midline activity. In one recent study by our group (Farb et al., 2007), the engagement of open, present-moment attention was associated with reductions in midline cortical activation but demonstrated novel activation of a right-lateralized network that was primarily characterized by sensory representations in the insula and secondary somatosensory cortices. These lateral regions may support more detached, objective, interoceptive and somatic awareness (Craig, 2002) that may serve as the primitive sensory representations of the “self”; whereas PFC activation, particularly along the cortical midline, may be more diagnostic of a cognitively elaborated, conceptual self whose representation is extended to account for the permanence of the individual as a stable object over time (Kelley et al., 2002; Northoff et al., 2004). In this fashion, mindful emotion regulation can be construed as a process of ‘turning toward’ momentary experience rather than an inhibition of cognition.
Additional support for the idea that enhanced sensory access is a core feature of mindfulness comes from analyses of neural networks following mindfulness training. Baerensten et al. (2010) found that meditation introduced a pattern of brain connectivity recruiting auditory, thalamic, limbic and insular cortices, potentially constituting an up-regulated sensory network, the anterior aspects of which have been argued to support the attribution of emotional salience to events (Seeley et al., 2007). A second study related MBSR training to greater connectivity within auditory and visual sensory networks, and during a listening task, greater PFC connectivity with auditory cortex and inhibition of visual cortex (Kilpatrick et al., 2011). Thus, one important function of mindful attention may be the recruitment and integration of primary sensory cortices into prefrontal regions supporting conscious awareness, as well as refining such integration to prevent distraction from unintended distracting stimuli.
While mindfulness training influences transitory brain activity, it also appears to effect longer-term structural changes commensurate with the repeated activation of limbic and interoceptive cortices. Lazar and colleagues (2005) observed increased grey matter volume in interoceptive and sensory regions such as the insula, somatosensory cortex and parietal regions. Grey matter changes have been observed after as short a period as the 8-week MBSR training intervention, predicting increased hippocampal and posterior attention network volume (Holzel et al, 2011), and decreased amygdala grey matter volume correlated with reduced stress ratings following MBSR (Holzel et al., 2010). These structural change data suggest that mindfulness training may be increasing the habitual capacity for encoding momentary experience while reducing the tendency to orient reflexively to emotionally arousing stimuli.
Interestingly, the connectivity and grey matter plasticity data tend to include more limbic than prefrontal cortical regions, again suggesting that prefrontal regions may not be the critical targets of mindfulness training, but rather the PFC is affected by the redeployment of cognitive resources to less-rehearsed sensory pathways. The lack of grey matter changes in prefrontal regions is consistent with the idea that the locus of present moment, nonjudgmental awareness may lie outside the conventional PFC attention network. The finding of hippocampal and insula grey matter changes with meditation training suggests that this alternate attention network may instead be situated in these paralimbic structures.
Of course, some executive control is required to manipulate the focus of attention in mindful emotion regulation. Yet rather than engaging widespread PFC regions, mindfulness training appears to target areas bridging the prefrontal and limbic regions, such as the anterior cingulate (Lane et al., 1997), subgenual cingulate (Mayberg et al., 1999) and anterior insula (Seeley, 2007). Dysregulation of fronto-limbic control regions such as the anterior cingulate may lead to maladaptive, ruminative, and egocentric attention contributing to depressive affect (Pizzagalli, 2011), as these ‘bridge’ regions between the PFC and limbic system have been argued to play a critical role in switching between evaluative and more task-oriented processes (Sridharan et al., 2008). In keeping with this theory, meditation practice has been associated with increased activity among the limbic system, thalamus, and anterior cingulate cortex, linking sensory information to the cortex (Newberg et al., 2001; Brefczynski-Lewis et al., 2007). The more lateral aspects of the PFC also appear to be important for the direction of mindful attention. Across several studies, participants showed increased lateral PFC activity when prompted to mindfully respond to emotionally provocative stimuli (Davidson et al., 2003; Farb et al., 2007). This lateral PFC activity may be a consequence of having to inhibit prepotent elaborative responses, as the inferior lateral PFC appears to be critical for inhibitory control (Aron et al., 2004; Chambers et al., 2006).
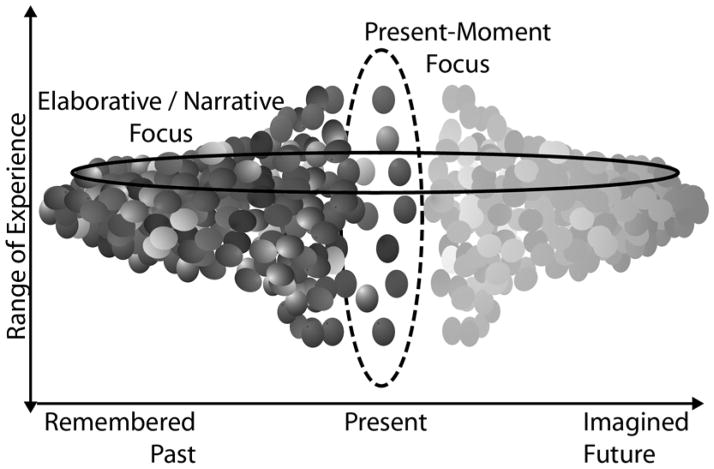
Mindfulness involves attending to contextual salience without concomitant recruitment of prefrontal evaluative processes, deploying attentional resources to recruit a network that limits habitual elaboration and self-referential narrative. In this fashion, automatic recruitment of temporally-extended, self-referential narrative generation may undergo a form of neural extinction, restoring autonomy to the central executive system and freeing it from its habitual applications; the tension between these two attentional frameworks is illustrated in Figure 1. Of course, as has been articulated by Siegle (2007), mindfulness is more than simply engaging in this present-moment awareness; the rich forms of evaluation for empathetic, moral, and self-referential processing associated with prefrontal default mode activity are valid and important aspects of experience. Rather, by practicing the disengagement of habitual interpretative and evaluative responses during cognition, it may be possible to widen the scope of interpretation to form new meaning previously inhibited by a habitual way of seeing the world.
Figure 1.
Theoretical schematic of the trade-off between present-moment and temporally extended elaborative attentional focus. Each sphere represents a potential aspect of experience: in the present moment these include physical sensations, emotions, and thoughts; in the past or anticipated future, these spheres are cognitive constructs rather than physical sensations. Typically, a small subset of available present moment experience is linked to a broad set of cognitive representations, providing an interpretive narrative (solid oval). By expanding the breadth of attention to include multiple aspects of present moment sensation such as thoughts, feelings and bodily sensations (dotted oval), attentional capacity for conceptual information such as judgments and personal narratives is reduced.
Clinical Implications
Reducing Automatic Affective Processing
The principle of non-judgment may seem to contradict the preceding principle of present moment attention, in that one could conceive of non-judgment as a distraction or inhibition of critical evaluation of one’s situation and the consequences of one’s actions. However, mindful attention does not inhibit initial evaluations insomuch as it limits the automatic expansion of initial evaluative reactions into activation of a broader set of implications about the self and the world. For example, a mindfulness intervention led to improved quality of life, depression, and fatigue scores in a Multiple Sclerosis population, but did not alter on ratings of physical symptoms such as lower and upper limb mobility (Grossman et al., 2010), suggesting that improvements were limited to subjective assessments of well-being rather than reducing patient awareness of physical symptoms.
While mindfulness training hopes to hone emotion regulation skills, the tendency to respond mindfully to emotional challenges may be detectable in a trait-like fashion between individuals. Way et al. (2010) linked the trait measure of dispositional mindfulness to protective non-reactivity in the amygdala during rest and also in response to sadness challenge, whereas depressive trait measures predicted an opposite, activating response. In a congruent finding, patients with social anxiety disorder demonstrated a reduced amygdala response to a negative emotional challenge following MBSR, and reduced subjective sadness ratings when using the regulatory strategy of attending to their breath (Goldin et al. 2010). Thus one long-term index of mindful emotion regulation is the reduction of salient threat detection in the face of emotional challenge, which may be useful in the assessment of treatment efficacy and patient vulnerability in behaviorally normalized cases.
Key to this employment of equanimity to reduce emotional reactivity is the intentional cultivation of awareness towards emotional information. Awareness for instance has been shown to eliminate subliminal priming effects on preferences (Murphy & Zajonc, 1993), and this effect was elegantly extended in a neuroimaging study of dispositional mindfulness, in which participants were asked to attend or ignore emotional information from face stimuli (Creswell et al., 2007). When emotional information was consciously attended, the emotional faces evoked less of an amygdala response and engaged greater prefrontal cortical resources. Dispositional mindfulness predicted a greater magnitude of this limbic-frontal tradeoff, suggesting that mindful participants were better able to leverage prefrontal attention networks to reduce stimulus-driven emotional reactivity. While such an investigation does not directly examine the proclivity of mindful individuals to voluntarily regulate emotion in this fashion, the experimental task of consciously bringing attention to the emotional aspects of sensation is highly consistent with the instructions found in a mindfulness intervention, and might again provide a useful clinical index for the internalization of mindful regulatory habits.
Altered Relationship to Pain
One of the most direct tests of altered emotion regulation lies in the examination of individuals’ responses to pain. In expert meditators, open monitoring rather than concentrative attention lowered the affective rather than sensory components of pain (Perlman et al., 2010). Two recent studies of meditation’s effects on pain found reduction of cortical midline elaborative processing regions as well as increased activation of primary nocioceptive and sensory integration regions such as the insula and anterior cingulate (Zeidan, 2011; Grant, 2011). This finding of increased primary sensation with a decoupling of affective appraisal is a direct analogue to mindful approach for dealing with negative emotions, to engage directly with the sensation rather than allow the habitual interpretation of these sensations to dominate cognition.
Cultivation of Empathy/Compassion
An important extension from the research of pain regulation is how these same affective systems can be engaged constructively in the cultivation of empathy and compassion. Non-judgmental attention appears to allow for novel and emergent feelings of self-compassion, which can powerfully attenuate an individual’s negative response to unpleasant events (Leary et al., 2007). In mood disorders, self-compassion is endorsed as a meaningful therapeutic construct by many patients, whose chief difficulty lies in finding a way to realize this compassionate state (Pauley & McPherson, 2010). A recent neuroimaging study linked self criticism to dorsal prefrontal regions such as the dorsolateral PFC and dorsal anterior cingulate, whereas self-reassurance was linked to activity in the ventrolateral PFC, temporal pole and insula (Longe et al., 2010).
In repeated studies, compassion and empathy appear to activate the affective components of pain perception, namely the anterior cingulate and anterior insula (Carr et al., 2003; Singer et al., 2004). More abstract feelings of social compassion appear to activate a similar network, though social compassion is longer lasting and later activating than empathy for physical pain (Immordino-Yang et al., 2009). Meditation experience has been linked to increased ability to recruit the insula and a proximal corticolimbic network during the volitional generation of compassion known as ‘loving-kindness-compassion’ meditation, in which participants focus their attention on generating and experiencing feelings of compassion for themselves and others (Lutz et al. 2008b).
It should be noted that empathic concern is not purely a visceral and perceptual process articulated through limbic and inferior parietal regions respectively; more analytic approaches to taking on another’s perspective appear to also recruit cortical midline regions such as the medial PFC and posterior cingulate (Decety and Jackson, 2004). However, the primary experience of empathic feeling that may give rise to new interpretations about others again seem first to be driven by paralimbic activity in the thalamus and insula, which may then feed into new conceptual interpretations that recruit the cortical midline.
Current Issues and Future Directions
While the neuroscience of mindfulness has sprung into existence over the past decade, a great deal of work is still required to fully understand the mechanisms by which it promotes adaptive emotion regulation. Future research must more carefully distinguish between concentrative and open states of attention, preferably within the same paradigm. It would be of interest to determine whether enhanced attentional maintenance can be cultivated through only the concentrative practices of breath monitoring and body scanning, and, if so, whether such attention is sufficient to enable patients to engage once more in more conventional forms of cognitive reappraisal. Alternatively, it may be the case that the long term practice of equanimity to all experience is required before highly practiced patterns of dysphoric elaboration cease to characterize patients’ obligatory interpretive stances.
Beyond looking at subcomponents of mindfulness interventions, it will also be importantly too explicitly contrast mindful forms of emotion regulation against common clinical approaches such as reappraisal, suppression, and distraction, especially those found in traditional psychotherapies. This will allow us to illustrate the shared attentional processes across diverse regulation strategies that have established clinical efficacy, thereby potentially isolating the most critical components for adaptive emotion regulation.
Highlights.
Mindfulness training first involves practicing focused attention to sensations from the body, developing a prefrontal attention network
Mindful emotion regulation increases emotional awareness by reducing midline prefrontal reactivity in favor of sustained limbic network activation
Conscious awareness of emotion may disrupt habitual dysphoric reactions and allow for novel appraisals such as self-compassion or acceptance
Limitations.
Training-related changes to focal and broad forms of attention have not been investigated together in a single experimental paradigm
Neuroscience studies are needed contrasting mindful emotion regulation against traditional psychotherapy techniques such as reappraisal, suppression, and distraction
Acknowledgments
This work is generously supported by funding from the Women of Baycrest (NASF), National Institute of Mental Health Grant MH 087723 (ZVS) & CIHR Grant: #MT81164 (AKA).
The Canadian Psychiatry Association proudly supports the In Review Series by providing an honorarium to the authors.
Abbreviations
- EEG
Electroencephalogram
- MBCT
Mindfulness Based Cognitive Therapy
- MBSR
Mindfulness Based Stress Reduction
- PFC
Prefrontal Cortex
References
- Aron AR, Robbins TW, Poldrack RA. Inhibition and the right inferior prefrontal cortex. Trends Cognit Sci. 2004;8:170–177. doi: 10.1016/j.tics.2004.02.010. [DOI] [PubMed] [Google Scholar]
- Baerensten KB, Stodkilde-Jorgensen H, Sommerlund B, et al. An investigation of brain processes supporting meditation. Cogn Process. 2010;11(1):57–84. doi: 10.1007/s10339-009-0342-3. [DOI] [PubMed] [Google Scholar]
- Baer RA. Mindfulness Training as a Clinical Intervention: A Conceptual and Empirical Review. Clinical Psychology Science and Practice. 2003;10(2):125–143. [Google Scholar]
- Baron Short E, Kose S, Mu Q, et al. Regional Brain Activation During Meditation Shows Time and Practice Effects: An Exploratory FMRI Study. Evidence Based Complimentary Alternative Medicine. 2007;7(1):121–127. doi: 10.1093/ecam/nem163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brefczynski-Lewis JA, Lutz A, Schaefer HS, et al. Neural correlates of attentional expertise in long-term meditation practitioners. Proc Natl Acad Sci U S A. 2007;104(7):11483–11488. doi: 10.1073/pnas.0606552104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr L, Iacoboni M, Dubeau MC, et al. Neural mechanisms of empathy in humans: A relay from neural systems for imitation to limbic areas. Proc Natl Acad Sci U S A. 2003;100:5497–502. doi: 10.1073/pnas.0935845100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers CD, Bellgrove MA, Stokes MG, et al. Executive “Brake Failure” following deactivation of human prefrontal lobe. Journal of Cognitive Neuroscience. 2006;18:444–55. doi: 10.1162/089892906775990606. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D, Mineka S. Temperament, personality, and the mood and anxiety disorders. Journal of Abnormal Psychology. 1994;103(1):103–116. [PubMed] [Google Scholar]
- Cooney RE, Joormann J, Eugene F, et al. Neural correlates of rumination in depression. Cognitive Affective and Behavioral Neuroscience. 2010;10(4):470–478. doi: 10.3758/CABN.10.4.470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig A. How do you feel? Interoception: The sense of the physiological condition of the body. Nature Reviews Neuroscience. 2002;3:655–666. doi: 10.1038/nrn894. [DOI] [PubMed] [Google Scholar]
- Creswell JD, Way BM, Eisenberger NI, Lieberman MD. Neural correlates of dispositional mindfulness during affect labeling. Psychosom Med. 2007;69(6):560–565. doi: 10.1097/PSY.0b013e3180f6171f. [DOI] [PubMed] [Google Scholar]
- Davidson RJ. Anxiety and affective style : role of prefrontal cortex and amygdala. Biol Psychiatry. 2002;51 :68–80. doi: 10.1016/s0006-3223(01)01328-2. [DOI] [PubMed] [Google Scholar]
- Davidson RJ, Kabat-Zinn J, Schumacher J, et al. Alterations in brain and immune function produced by mindfulness meditation. Psychosomatic Medicine. 2003;65(4):564–570. doi: 10.1097/01.psy.0000077505.67574.e3. [DOI] [PubMed] [Google Scholar]
- Decety J, Jackson PL. The functional architecture of human empathy. Behavioral and Cognitive Neuroscience Reviews. 2004;3:71–100. doi: 10.1177/1534582304267187. [DOI] [PubMed] [Google Scholar]
- Dunn BR, Hartigan JA, Mikulas WL. Concentration and mindfulness meditations: unique forms of consciousness? Appl Psychophysiol Biofeedback. 1999;24(3):147–165. doi: 10.1023/a:1023498629385. [DOI] [PubMed] [Google Scholar]
- Farb NAS, Anderson AK, Bloch R, Segal ZV. Mood-linked Responses in Medial Prefrontal Cortex Predict Relapse in Patients with Recurrent Unipolar Depression. Biological Psychiatry. 2011 doi: 10.1016/j.biopsych.2011.03.009. E-pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farb NAS, Anderson AK, Mayberg H, et al. Minding one's emotions: Mindfulness training alters the neural expression of sadness. Emotion. 2010;10(1):25–33. doi: 10.1037/a0017151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farb NAS, Segal ZV, Mayberg H, et al. Attending to the present: mindfulness meditation reveals distinct neural modes of self-reference. Social Cognitive and Affective Neuroscience. 2007;2(4):313–122. doi: 10.1093/scan/nsm030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin P, Gross J. Effects of Mindfulness-Based Stress Reduction (MBSR) on Emotion Regulation in Social Anxiety Disorder. Emotion. 2010;10:83–91. doi: 10.1037/a0018441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin P, McRae K, Ramel W, Gross J. The neural basis of emotion regulation: Reappraisal and suppression of negative emotion. Biological Psychiatry. 2008;63:577–586. doi: 10.1016/j.biopsych.2007.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin P, Ramel W, Gross J. Mindfulness Meditation Training and Self-Referential Processing in Social Anxiety Disorder: Behavioral and Neural Effects. Journal of Cognitive Psychotherapy. 2009;23(3):242–257. doi: 10.1891/0889-8391.23.3.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant JA, Courtemanche J, Rainville P. A non-elaborative mental stance and decoupling of executive and pain-related cortices predicts low pain sensitivity in Zen meditators. Pain. 2011;152:150–156. doi: 10.1016/j.pain.2010.10.006. [DOI] [PubMed] [Google Scholar]
- Grimm S, Ernst J, Boesiger P, et al. Increased self-focus in major depressive disorder is related to neural abnormalities in subcortical-cortical midline structures. Human Brain Mapping. 2008;30(8):2617–2627. doi: 10.1002/hbm.20693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross J. Emotion regulation: Affective, cognitive, and social consequences. Psychophysiology. 2002;39:281–291. doi: 10.1017/s0048577201393198. [DOI] [PubMed] [Google Scholar]
- Grossman P, Kappos L, Gensicke H, et al. MS quality of life, depression, and fatigue improve after mindfulness training: a randomized trial. Neurology. 2010;75:1141–1149. doi: 10.1212/WNL.0b013e3181f4d80d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holzel B, Carmody J, Evans K, et al. Stress reduction correlates with structural changes in the amydgala. Social Cognitive and Affective Neurosci. 2010;5:11–17. doi: 10.1093/scan/nsp034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holzel B, Carmody J, Vangel M, et al. Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Research: Neuroimaging. 2011;191:36–42. doi: 10.1016/j.pscychresns.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holzel BK, Ott U, Hempel H, et al. Differential engagement of anterior cingulate and adjacent medial prefrontal cortex in adept meditators and non-meditators. Neuroscience letters. 2007;421:16–21. doi: 10.1016/j.neulet.2007.04.074. [DOI] [PubMed] [Google Scholar]
- Immordino-Yang MH, McColl A, Damasio A, et al. Neural correlates of admiration and compassion. Proc Natl Acad Sci U S A. 2009;106:7687–8. doi: 10.1073/pnas.0810363106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ives-Deliperi VL, Solms M, Meintjes EM. The neural substrates of mindfulness: An fMRI investigation. Social Neuroscience. 2011;6(3):231–242. doi: 10.1080/17470919.2010.513495. [DOI] [PubMed] [Google Scholar]
- Jha AP, Krompinger J, Baime MJ. Mindfulenss training modifies subsystems of attention. Cognitive, Affective, & Behavioral Neuroscience. 2007;7(2):109–119. doi: 10.3758/cabn.7.2.109. [DOI] [PubMed] [Google Scholar]
- Johnstone T, van Reekum C, Urry H, et al. Failure to regulate: Counterproductive recruitment of top-down prefrontal subcortical circuitry in major depression. J Neurosci. 2007;27:8877–8884. doi: 10.1523/JNEUROSCI.2063-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain and Illness. New York: Delacorte; 1990. pp. 47–93. [Google Scholar]
- Kelley WM, Macrae CN, Wyland CL, et al. Finding the self? An event-related fMRI study. Journal of Cognitive Neuroscience. 2002;14:785–94. doi: 10.1162/08989290260138672. [DOI] [PubMed] [Google Scholar]
- Kilpatrick LA, Suyenobu BY, Smith SR, et al. Impact of mindfulness-based stress reduction training on intrinsic brain connectivity. Neuroimage. 2011;56(1):290–298. doi: 10.1016/j.neuroimage.2011.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane RD, Fink GR, Chau PM-L, Dolan R. Neural activation during selective attention to subjective emotional responses. Neuroreport. 1997;8(18):3969–3972. doi: 10.1097/00001756-199712220-00024. [DOI] [PubMed] [Google Scholar]
- Lazar SW, Bush G, Gollub RL, et al. Functional brain mapping of the relaxation response and meditation. NeuroReport. 2000;11(7):1581–1585. [PubMed] [Google Scholar]
- Lazar SW, Kerr CE, Wasserman RH, et al. Meditation experience is associated with increased cortical thickness. NeuroReport. 2005;16(17):1893–1897. doi: 10.1097/01.wnr.0000186598.66243.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leary MR, Tate EB, Adams CE, et al. Self-compassion and reactions to unpleasant self-relevant events: the implications of treating oneself kindly. J Pers Soc Psychol. 2007;92:887–904. doi: 10.1037/0022-3514.92.5.887. [DOI] [PubMed] [Google Scholar]
- Longe O, Maratos FA, Glibert P, et al. Having a word with yourself: neural correlates of self-criticism and self-reassurance. Neuroimage. 2010;49(2):1849–56. doi: 10.1016/j.neuroimage.2009.09.019. [DOI] [PubMed] [Google Scholar]
- Lou HC, Kjaer TW, Friberg L, et al. A 15O-H20 PET Study of Meditation and the Resting State of Normal Consciousness. Human Brain Mapping. 1999;7:98–105. doi: 10.1002/(SICI)1097-0193(1999)7:2<98::AID-HBM3>3.0.CO;2-M. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludwig DS, Kabat-Zinn J. Mindfulness in Medicine. JAMA. 2008;300(11):1350–1352. doi: 10.1001/jama.300.11.1350. [DOI] [PubMed] [Google Scholar]
- Lutz A, Breczynski-Lewis J, Johnstone T, Davidson RJ. Regulation of the Neural Circuitry of Emotio by Compassion Meditation: Effects of Meditative Expertise. PLoS ONE. 2008b;3(3):e1897. doi: 10.1371/journal.pone.0001897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutz A, Slagter HA, Dunne JD, Davidson RJ. Attention regulation and monitoring in meditation. Trends Cogn Sci. 2008a;12(4):163–169. doi: 10.1016/j.tics.2008.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayberg HS, Liotti M, Brannan SK, et al. Reciprocal Limbic-Cortical Function and Negative Mood: Converging PET Findings in Depression and Normal Sadness. Am J Psychiatry. 1999;156:675–682. doi: 10.1176/ajp.156.5.675. [DOI] [PubMed] [Google Scholar]
- Murphy ST, Zajonc RB. Affect, cognition, and awareness: Affective priming with optimal and suboptimal stimulus exposures. Journal of Personality and Social Psychology. 1993;64(5):723–739. doi: 10.1037//0022-3514.64.5.723. [DOI] [PubMed] [Google Scholar]
- Newberg AB, Alavi A, Baime MJ, et al. The measurement of regional cerebral blood flow during the complex cognitive task of meditation: a preliminary SPECT study. Psychiatry Research: Neuroimaging. 2001;106(2):113–122. doi: 10.1016/s0925-4927(01)00074-9. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. Journal of Abnormal Psychology. 2000;109:504–511. [PubMed] [Google Scholar]
- Northoff G, Bermpohl F. Cortical midline structure and the self. Trends in Cognitive Science. 2004;8:102–107. doi: 10.1016/j.tics.2004.01.004. [DOI] [PubMed] [Google Scholar]
- Ochsner KN, Bunge SA, Gross JJ, Gabrieli JD. Rethinking feelings: an FMRI study of the cognitive regulation of emotion. J Cogn Neurosci. 2002;14:1215–1229. doi: 10.1162/089892902760807212. [DOI] [PubMed] [Google Scholar]
- Ochsner KN, Ray RD, Cooper JC, et al. For better or for worse: Neural systems supporting the cognitive down- and up-regulation of negative emotion. Neuroimage. 2004;23:483, 499. doi: 10.1016/j.neuroimage.2004.06.030. [DOI] [PubMed] [Google Scholar]
- Opsina MB, Bond TK, Karkhaneh M, et al. Meditation practices for health: state of the research. Evid Rep Technol Assess. 2007;155:1–263. [PMC free article] [PubMed] [Google Scholar]
- Ottenbreit ND, Dobson KS. Avoidance and depression: the construction of the Cognitive-Behavioral Avoidance Scale. Behaviour Research and Therapy. 2004;42(3):293–313. doi: 10.1016/S0005-7967(03)00140-2. [DOI] [PubMed] [Google Scholar]
- Pauley G, McPherson S. The experience and meaning of compassion and self-compassion for individuals with depression and anxiety. Psychology & Psychotherapy. 2010;83:129–43. doi: 10.1348/147608309X471000. [DOI] [PubMed] [Google Scholar]
- Perlman D, Salomons T, Davidson R, et al. Differential effects on Pain Intensity and Unpleasantness of Two Meditation Practices. Emotion. 2010;10:65–71. doi: 10.1037/a0018440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phan KL, Fitzgerald DA, Nathan PJ, et al. Neural substrates for voluntary suppression of negative affect: a functional magnetic resonance imaging study. Biol Psychiatry. 2005;57:210–219. doi: 10.1016/j.biopsych.2004.10.030. [DOI] [PubMed] [Google Scholar]
- Pizzagalli DA. Frontocingulate Dysfunction in Depression: Toward Biomarkers of Treatment Response. Neuropsychopharmacology Reviews. 2011;36:183–206. doi: 10.1038/npp.2010.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramel W, Goldin P, Carmona P, et al. The effects of mindfulness meditation on cognitive processes and affect in patients with past depression. Cognitive Therapy and Research. 2004;28:433–455. [Google Scholar]
- Ressler K, Mayberg H. Targeting abnormal neural circuits in mood and anxiety disorders: From the laboratory to the clinic. Nature Neuroscience. 2007;10:1116–1124. doi: 10.1038/nn1944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scherer KR, Schorr A, Johnstone T. Appraisal processes in emotion: theory, methods, and research. Canary, NC: Oxford University Press; 2001. [Google Scholar]
- Seeley WW, Menon V, Schatzberg AF, et al. Dissociable intrinsic connectivity networks for salience processing and executive control. J Neurosci. 2007;27:2349–56. doi: 10.1523/JNEUROSCI.5587-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal ZV, Williams JMG, Teasdale J. Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse. New York: Guilford Press; 2002. [Google Scholar]
- Sheline YI, Barch DM, Price JL, et al. The default mode network and self-referential processes in depression. Proc Natl Acam Sci U S A. 2009;106(6):1942–1947. doi: 10.1073/pnas.0812686106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheline YI, Price JL, Yan Z, Mintun MA. Resting-state functional MRI in depression unmasks increased connectivity between networks via the dorsal nexus. Proc Natl Acad Sci U S A. 2010;107(24):11020–11025. doi: 10.1073/pnas.1000446107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegle D. Mindfulness training and neural integration: differentiation of distinct streams of awareness and the cultivation of well-being. Social Cognitive and Affective Neuroscience. 2007;2:259, 263. [Google Scholar]
- Singer T, Seymour B, O’Doherty J, et al. Empathy for pain involves the Affective but not Sensory Components for Pain. Science. 2004;303(5561):1157–1162. doi: 10.1126/science.1093535. [DOI] [PubMed] [Google Scholar]
- Sridharan D, Levitin DJ, Menon V. A critical role for the right fronto-insular cortex in switching between central-executive and default-mode networks. Proc Natl Acad U S A. 2008;105(34):12569–12574. doi: 10.1073/pnas.0800005105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins E, Moberly NJ, Moulds ML. Processing mode causally influences emotional reactivity: Distinct effects of abstract versus concrete construal on emotional response. Emotion. 2008;8:364–378. doi: 10.1037/1528-3542.8.3.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Way BM, Creswell JD, Eisenberger NI, Lieberman MD. Dispositional Mindfulness and Depressive Symptomatology: Correlations With Limbic and Self-Referential Neural Activity During Rest. Emotion. 2010;10(1):12–24. doi: 10.1037/a0018312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeidan F, Martucci KT, Kraft RA, et al. Brain Mechanisms Supporting the Modulation of Pain by Mindfulness Meditation. J Neurosci. 2011;31(14):5540–5548. doi: 10.1523/JNEUROSCI.5791-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]