Abstract
Objectives
To explore whether a strategy of more intensive antibiotic therapy leads to emergence or prolongation of renal failure in intensive care patients.
Design
Secondary analysis from a randomised antibiotic strategy trial (the Procalcitonin And Survival Study). The randomised arms were conserved from the primary trial for the main analysis.
Setting
Nine mixed surgical/medical intensive care units across Denmark.
Participants
1200 adult intensive care patients, 18+ years, expected to stay +24 h. Exclusion criteria: bilirubin >40 mg/dl, triglycerides >1000 mg/dl, increased risk from blood sampling, pregnant/breast feeding and psychiatric patients.
Interventions
Patients were randomised to guideline-based therapy (‘standard-exposure’ arm) or to guideline-based therapy supplemented with antibiotic escalation whenever procalcitonin increased on daily measurements (‘high-exposure’ arm).
Main outcome measures
Primary end point: estimated glomerular filtration rate (eGFR) <60 ml/min/1.73 m2. Secondary end points: (1) delta eGFR after starting/stopping a drug and (2) RIFLE criterion Risk ‘R’, Injury ‘I’ and Failure ‘F’. Analysis was by intention to treat.
Results
28-day mortality was 31.8% and comparable (Jensen et al, Crit Care Med 2011). A total of 3672/7634 (48.1%) study days during follow-up in the high-exposure versus 3016/6949 (43.4%) in the ‘standard-exposure arm were spent with eGFR <60 ml/min/1.73 m2, p<0.001. In a multiple effects model, 3 piperacillin/tazobactam was identified as causing the lowest rate of renal recovery of all antibiotics used: 1.0 ml/min/1.73 m2/24 h while exposed to this drug (95% CI 0.7 to 1.3 ml/min/1.73 m2/24 h) vs meropenem: 2.9 ml/min/1.73 m2/24 h (2.5 to 3.3 ml/min/1.73 m2/24 h)); after discontinuing piperacillin/tazobactam, the renal recovery rate increased: 2.7 ml/min/1.73 m2/24 h (2.3 to 3.1 ml/min/1.73 m2 /24 h)). eGFR <60 ml/min/1.73 m2 in the two groups at entry and at last day of follow-up was 57% versus 55% and 41% versus 39%, respectively.
Conclusions
Piperacillin/tazobactam was identified as a cause of delayed renal recovery in critically ill patients. This nephrotoxicity was not observed when using other beta-lactam antibiotics.
Trial registration
ClinicalTrials.gov identifier: NCT00271752.
Article summary
Article focus
To determine whether an increased exposure to broad-spectrum antibiotics causes renal failure in intensive care patients.
To find out whether some of the antibiotics used in the interventional arm were more prone to cause renal failure.
Key messages
More days with renal failure were observed in patients in the highly antibiotic exposed arm.
Administration of piperacillin/tazobactam caused the lowest rate of renal recovery of all analysed drugs and when this drug was discontinued, renal function recovered at a fast rate.
Use of piperacillin/tazobactam in intensive care patients can cause a slow renal recovery and this toxic effect seems at least partially reversible.
Strengths and limitations of this study
The study is a randomised controlled trial with a high sample size and high rate of follow-up and it is the first to systematically investigate the renal toxicity of several of the analysed antibiotics. Existing end points for acute renal failure could not capture renal failure that emerged from baseline and forth, so other end points had to be designed. The study was not designed to detect persistent renal failure and more severe degrees of renal failure.
Introduction
Frequent complications to sepsis are organ failure, especially respiratory failure and renal failure.1–3 Critically ill patients are more vulnerable to organ-related drug toxicities than less severely ill patients.4 Randomised trials assessing safety of broad-spectrum antibiotics in intensive care settings are generally scarce, do not have sufficient statistical power for assessing organ failure end points and do often not include defined kidney organ failure end points.5–7 Data on renal failure end points are also sparse in the published trials from other patient populations, and since the absolute risk of renal failure is low for these patients, analyses may likely have been underpowered.8–12
To our knowledge, randomised trials comparing ‘high exposure’ versus ‘standard exposure to antibiotics’ and specifically addressing whether these interventions affect the occurrence and duration of kidney failure have not been done before in intensive care settings.
In this secondary analysis from a randomised trial, the Procalcitonin And Survival Study,13 we aimed to explore whether a strategy of more intensive antibiotic therapy leads to adverse renal outcomes within 28 days after recruitment.
In our study population (and often in severely infected intensive care unit (ICU) patients), a bacterial hit has resulted in acute onset renal failure, and this bacterial hit (and related organ failure) is often the reason for ICU admittance. In such situations, with the correct treatment of the underlying infection, we expect renal function to recover. ‘Lack of recovery’ is a non-desirable situation, which may be very serious for the patient. We wanted to explore this, and realising, RIFLE/AKIN could not capture this, we have used estimated glomerular filtration rate (eGFR) <60 ml/min/1.73 m2 as the primary end point and examined this from different angles (eGFR <60 ml/min/1.73 m2 at day 7, days with ml/min/1.73 m2). The multiple effects model was built to capture actual estimates of renal function improvement using different antibiotics and adjusting for other known or suspected causes of renal dysfunction.
Second, if renal failure was observed from the high-exposure approach to identify one or several of the antibiotics used in this trial as the cause of such a renal failure.
Methods
Trial design and participants
Procalcitonin And Survival Study is a multicentre, randomised controlled trial in Denmark 2006–2009 in 1200 adult critically ill patients, expected to stay in one of the nine participating mixed medical/surgical ICUs ≥24 h; the CONSORT trial diagram is displayed in supplementary figure 1. Patients were randomised 1:1 either to treatment according to international guidelines: ‘standard-exposure arm’, or to same guidelines but supplemented with daily drug-escalation initiated upon procalcitonin increases (high-exposure arm); 28-day mortality was 31.8% and comparable between the two groups, as reported.13
To be eligible, patients had to be ≥18 years, enrolled within 24 h of admission to the ICU and have an expected intensive car admission length of ≥24 h. Patients with known bilirubin >40 mg/dl and triglycerides >1000 mg/dl (not suspensive) were not eligible (interference with procalcitonin measurements), as were patients who were judged to be at an increased risk from blood sampling. The inclusion criteria were broad since infection is frequent and often causes complications in the patient group and to increase the external validity of the results. The person or next of kin gave informed consent. The study protocol was approved by the regional ethics committees in Denmark (H-KF-272-753) and adheres to the Helsinki declaration, revised in Seoul 2008.
In the present analyses, we explored presence and duration of renal failure as well as change in renal function during the observed time. End points are defined in Statistical analysis section below. Patients were followed until day 28. The primary trial protocol and the analysis plan are available in the online supplement. Analysis was by intention to treat: NCT00271752.
Randomisation and masking
Randomisation was performed 1:1 using a computerised algorithm created by the database manager (JK) with concealed block size, pre-stratified for site of recruitment, initial APACHE II and age (entered in an encrypted screening form in a password protected website); investigators were masked to assignment before, but not after, randomisation. All investigators were trained by the coordinating centre and had to register in an investigator database. Investigators, treating physicians and the coordinator were unaware of outcomes during the study, as were they of all procalcitonin measurements in the standard-exposure (control) group.
Antibiotic therapy in the two arms
The investigators enrolled participants and assigned the high-exposure group participants to the intervention. In the standard-exposure group, the antimicrobial treatment was guided according to current clinical guidelines,14 based on clinical assessment, microbiology and radiology among other parameters, as described elsewhere13
In the high-exposure group, the use of antimicrobial interventions was guided by the same clinical guidelines as in the standard-exposure group to ascertain the best standard of care therapy for all patients, and additionally, antimicrobial interventions were initiated whenever procalcitonin levels were not decreasing at a pre-defined pace (supplementary figure 2) and diagram D1 in the online supplement where a site-adjusted local guideline is displayed.
Measurements, data collection and follow-up
Blood samples for biomarker measurement were made daily in the ICU, beginning immediately after randomisation. The assay used was the Kryptor®-PCT. Organ failure and antibiotic exposure were followed up for until 28 days or death, as described.13 Mortality was followed via the National Patient Register in which all deaths in Denmark are registered within 14 days. Good Clinical Practice guidelines were applied. The regional ethics board approved the protocol (H-KF-01-272-753).
Statistical analysis
The primary end point was ‘eGFR <60 ml/min/1.73 m2’ and several analyses were made to explore this: ‘days with eGFR <60 ml/min/1.73 m2’, ‘risk of eGFR <60 ml/min/1.73 m2 on days 1–7’. Secondary end points were (1) delta eGFR after starting/stopping a drug and (2) RIFLE-criteria Risk ‘R’, Injury ‘I’ and Failure ‘F’ http://www.adqi.net. Since we explored exposure of antibiotics from baseline and forth (and not pre-ICU), in the RIFLE definition, the baseline creatinine was used (instead of an ideal eGFR). eGFR was calculated for every day. To not let this be influenced by hydration status, the baseline weight was used and thus the relation between serum-creatinine and eGFR was a first-degree function for every patient. Other end points explored were ‘ever’ blood-urea level ≥20 mmol/l and eGFR <30.
The multiple effects eGFR ‘slope’ analyses were adjusted for the following variables: treatment arm (high exposure vs standard exposure), age (≥65 vs <65 years), gender, baseline APACHE II score (≥20 vs <20), degree of host response/infection at baseline (severe sepsis/septic shock vs milder or no infection as defined15), the eGFR at initiation of the investigated antibiotic and finally, whether the patient at baseline was considered to be ‘surgical’ or ‘medical’.
Comparisons were made between treatment arms using Students t tests (for normal distributed continuous data) and Mann–Whitney U tests (for non-normally distributed continuous data). χ2 tests and logistic regression models were used to test categorical variables. Time-to-event analyses comparing the high-exposure group with the standard-exposure group were performed using Kaplan–Meier plots and Cox proportional hazards models. Interactions were explored whenever an interaction could be rationally expected according to background literature, for the multivariate models performed. Statistical analyses were performed using STATA V.10.2 and SAS V.9.1. All reported p values are two sided using a level of significance of 0.05.
Sample size
A multivariate approach power calculation was made: The summed squared correlations (Σrho2) to the risk of the antibiotic drug investigated were set to 0.3. The frequency of the end point in the standard-exposure group was set to 20%, the sample size was set to 1200 and the frequency of the exposure was set at 30%, which resulted in a detection limit for OR of ≥1.5 (or ≤0.67).
Results
Baseline characteristics
Nine sites included 1200 persons between 9 January 2006 and 2 June 2009. Eighty-three per cent of the patients were assessed by the investigator to have an infection at baseline and 81% of the patients suffered from chronic comorbidity. Supplementary table 1 briefly summarises baseline characteristics. Mortality was comparable between the two groups, as reported.13
Follow-up
Follow-up for renal measures during the 28-day study period was made on 9348 days in the standard-exposure group of 10 755 days alive and admitted to hospital (86.9%) versus 9866 of 11 380 days in the high-exposure group (86.7%). If time after discharge from hospital (where no serum-creatinine values were determined) until day 28 was included, the percentage of days with assessment of renal failure was 71.2% (9348/13 130 days) versus 73.8% (9866/13 377 days).
Use of antibiotics
The antibiotics used most while admitted to the ICU were piperacillin/tazobactam, cefuroxime, meropenem and ciprofloxacin, and there was a substantial higher use of piperacillin/tazobactam and ciprofloxacin in the high-exposure arm (supplementary table 2). Vancomycin was used to a lesser extent in both groups, and aminoglycosides and colistin were used rarely in both groups.
The median length of an antibiotic course was prolonged using the high-exposure algorithm (6 days (IQR 3–11) versus 4 days (IQR 3–10), p=0.004).
Renal failure in the originally randomised study arms
The percentage of days within days 1–28 with eGFR ≤60 ml/min/1.73 m2 was 48% in the high-exposure arm versus 43% in the standard-exposure arm, p<0.0001. Results in table 1 are eGFR values, based on actual measured S-creatinine values; results regarding days with eGFR were comparable if using the ‘last observation carried forward’ approach (not shown). RIFLE-criterion ‘R’ occurred more often within days 1–28 in the high-exposure arm than the standard-exposure arm: 209 patients versus 170 patients, p=0.02, as did blood urea levels exceeding 20 mmol/l: 253 (43.4%) versus 217 (37.4%), p=0.04.
Table 1.
Prevalence and duration of kidney organ failure (‘standard-exposure’ group vs ‘high-exposure’ group)
| Standard-exposure group (N=596) | High-exposure group (N=604) | p Value | |
| eGFR*: number of days (% of days from days 1 to 28 with values): | |||
| Moderately–severely impaired (eGFR: ≤60 ml/min/1.73 m2) | 3016 (43.4) | 3672 (48.1) | <0.0001 |
| Severely impaired (eGFR ≤30 ml/min/1.73 m2) | 1445 (20.8) | 1910 (25.0) | <0.0001 |
| Severely impaired (eGFR ≤30 ml/min/1.73 m2), days from days 1 to 14 | 984 (20.0) | 1253 (23.5) | <0.0001 |
| ‘RIFLE’ criteria, number of patients (%) within days 1–28 | |||
| ’R’ reached | 170 (28.5) | 209 (34.6) | 0.02 |
| ‘I’ reached | 75 (12.6) | 92 (15.2) | 0.19 |
| ‘F’ reached | 121 (20.3) | 150 (24.8) | 0.06 |
| ‘R’ or death | 298 (50.0) | 327 (54.1) | 0.15 |
| ‘I’ or death | 234 (39.3) | 252 (41.7) | 0.39 |
| ‘F’ or death | 270 (45.3) | 287 (47.5) | 0.44 |
| Urea | |||
| Patients with a urea level ever ≥20 mmol/l (days 1–28), n (%) | 217 (37.4) | 253 (43.4) | 0.04 |
eGFR was assessed using the Cockcroft and Gault method (Ref: Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron 1976;16:31–41). Actual measured creatinin values were used. If using the ‘last observation carried forward’ approach regarding creatinin measurement to take into account that patients who died in renal failure should be counted as such did not change the signal or the statistics of these analyses. ‘R’: Risk, ‘I’: Injury, ‘F’: Failure. Presence of renal failure according to ‘RIFLE’ was assessed using the guidelines developed by the acute dialysis quality initiative (http://www.adqi.net).
eGFR, estimated glomerular filtration rate.
The frequency of renal failure on the last day of follow-up was comparable between the arms (table 2), underlining that the results depicted in table 1 reflect a temporary extension of duration of renal failure in the high-exposure group and furthermore that this observation is not explained by premature discharge of renally incompetent patients in the standard-exposure arm.
Table 2.
Prevalence of kidney organ failure on the last day of follow-up (‘standard-exposure’ group vs ‘high-exposure’ group)
| Standard-exposure group | High-exposure group | p Value | |
| Survivors and patients who had last creatinine measured >24 h before death | N=432 | N=438 | |
| Renal failure (*eGFR: ≤60 ml/min/1.73 m2) | 119 (27.6%) | 137 (31.3%) | 0.23 |
| Patients who died (with last creatinine measured within 24 h before death) | N=150 | N=145 | |
| Renal failure (eGFR: ≤60 ml/min/1.73 m2) | 105 (70.0%) | 99 (68.3%) | 0.83 |
| All patients with creatinine measurements | N=582 | N=583 | |
| Renal failure (eGFR: ≤60 ml/min/1.73 m2) | 224 (38.5%) | 236 (40.5%) | 0.51 |
eGFR was assessed using the Cockcroft and Gault method (Ref: Cockcroft DW, Gault MH: Prediction of creatinine clearance from serum creatinine. Nephron 1976;16:31–41). Actual measured creatinin values were used.
eGFR, estimated glomerular filtration rate.
GFR changes and exposure to certain antibiotics
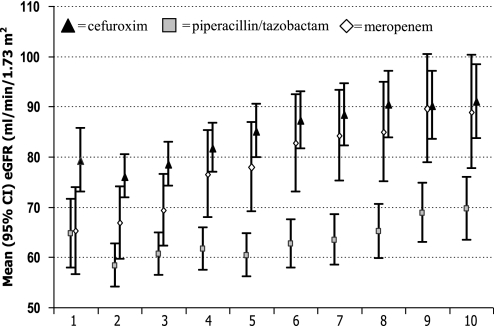
Comparison of the eGFR of all patients (both study arms) for the first 10 days after starting on the most frequently used beta-lactam antibiotics showed that the slowest recovery of renal function was observed in patients on piperacillin/tazobactam as compared with patients on meropenem or cefuroxim (figure 1). A multiple effects model investigating the eGFR regression coefficient (‘increase in eGFR’) per day on these drugs confirmed that renal recovery was lowest in patients on piperacillin/tazobactam (table 3). Of note, renal recovery seems to be low in patients exposed to cefuroxim, but as displayed in figure 1, this drug is given to patients with a relatively normal renal function (leaving few possibilities for ‘recovery’).
Figure 1.
Estimated glomerular filtration rate (eGFR) during 10 days on cefuroxim, piperacillin/tazobactam and meropenem. Difference between eGFR in patients receiving piperacillin/tazobactam versus meropenem: day 1 (p=0.78), day 2 (p=0.18), day 3 (p=0.09), day 4 (p=0.008), day 5 (p=0.001), day 6 (p=0.001), day 7 (p=0.0004), day 8 (p=0.005), day 9 (p=0.006) and day 10 (p=0.02).
Table 3.
Multiple effects models investigating eGFR changes after starting and stopping beta-lactam antibiotics
| Variable | Unadjusted analysis |
Multivariable analysis |
|||
| Regression coefficient (95% CI) | p Value | Regression coefficient (95% CI) | p Value | ||
| After starting the drug | |||||
| Piperacillin/tazobactam | Per day more on piperacillin/tazobactam | 1.39 (1.17 to 1.60) | <0.0001 | 0.99 (0.71 to 1.27) | <0.0001 |
| Meropenem | Per day more on meropenem | 2.74 (2.39 to 3.09) | <0.0001 | 2.86 (2.45 to 3.28) | <0.0001 |
| Cefuroxim | Per day more on cefuroxim | 1.91 (1.67 to 2.16) | <0.0001 | 1.27 (0.90 to 1.64) | <0.0001 |
| After stopping the drug | |||||
| Piperacillin/tazobactam | Per day after stopping piperacillin/tazobactam | 2.79 (2.35 to 3.24) | <0.0001 | 2.70 (2.26 to 3.14) | <0.0001 |
| Meropenem | Per day after stopping meropenem | 0.20 (−0.51 to 0.91) | 0.59 | 0.17 (−0.52 to 0.86) | 0.63 |
| Cefuroxim | Per day after stopping cefuroxim | 0.13 (−0.25 to 0.50) | 0.51 | 0.01 (−0.35 to 0.37) | 0.96 |
All multivariable analyses were adjusted for: treatment arm (‘low exposure’ vs ‘high exposure’), gender, age (≥65 vs <65 years), APACHE II score (≥20 vs <20), clinically judged infection (severe sepsis/septic shock vs milder or no infection), patient category (surgical vs medical) and eGFR level at administration of the antibiotic (1: <30 ml/min/1.73 m2, 2: 31–60 ml/min/1.73 m2, 3: >60 ml/min/1.73 m2).
eGFR, estimated glomerular filtration rate.
For the first 5 days following discontinuation of these drugs, adjusting for the same variables, eGFR increased at the highest rate in patients receiving piperacillin/tazobactam (table 3).
The frequency of eGFR<60 ml/min/1.73 m2 on day 7 (or at death or last follow-up day) in the trial was 523/1200=43.6%. This end point was investigated in a forward censored (p<0.1) logistic regression. Use of piperacillin/tazobactam and other frequently used beta-lactam drugs for at least 3 days within these first 7 days as well as known and suspected predictors of renal failure were explored in a multivariable logistic regression analysis. Five independent predictors of renal failure on day 7 were identified: age above 65 years, APACHE II score >20, Charlson's comorbidity score ≥2, eGFR at baseline and use of piperacillin/tazobactam for at least 3 days within the first 7 days (table 4). Excluding all patients who died within the first 7 days, excluding all patients with invasive fungal infection on days 1–28, combining the beta-lactam exposure with exposure to flour-quinolone exposure (data not shown) or adding ‘Alert-procalcitonin’ at baseline as a variable did not alter the signal (data not shown). To validate the end point as a predictor of mortality, a Cox regression was done; eGFR <60 ml/min/1.73 m2 on day 7 was found to be the strongest predictor of ‘all-cause mortality days 7–28’ of all tested variables (table T1, supplementary material).
Table 4.
Multivariable logistic regression: beta-lactam antibiotics and other risk variables versus binary end point eGFR <60 ml/min/1.73 m2 on day 7
| Unadjusted analysis |
Multivariable analysis |
|||
| Odds ratio (95% CI) | p Value | Odds ratio (95% CI) | p Value | |
| Other variables | ||||
| Age (≥65 vs <65 years) | 2.36 (1.86 to 3.00) | <0.0001 | 1.85 (1.31 to 2.60) | <0.0001 |
| APACHE II score (≥20 vs <20) | 2.49 (1.90 to 3.25) | <0.0001 | 1.64 (1.12 to 2.41) | 0.01 |
| Severe sepsis/septic shock versus milder or no infection | 2.02 (1.59 to 2.56) | <0.0001 | 1.16 (0.82 to 1.66) | 0.40 |
| Autoimmune disease (Y vs N) | 1.31 (0.73 to 2.33) | 0.36 | NI | – |
| Cancer (Y vs N) | 1.26 (0.88 to 1.79) | 0.21 | NI | – |
| Charlson score (≥2 vs <2) | 1.72 (1.35 to 2.18) | <0.0001 | 1.70 (1.21 to 2.40) | 0.002 |
| Surgical (Y vs N) | 1.16 (0.90 to 1.50) | 0.24 | NI | – |
| Body mass index (≥25 vs <25) | 1.57 (1.17 to 2.12) | 0.003 | 1.19 (0.78 to 1.82) | 0.41 |
| Gender (male vs female) | 1.25 (0.99 to 1.57) | 0.06 | 1.28 (0.92 to 1.78) | 0.14 |
| eGFR level at baseline | ||||
| >60 ml/min/1.73 m2 | Ref | – | Ref | – |
| 31–60 ml/min/1.73 m2 | 14.6 (10.2 to 21.0) | <0.0001 | 11.7 (8.0 to 17.0) | <0.0001 |
| <30 ml/min/1.73 m2 | 81.1 (51.2 to 128.5) | <0.0001 | 65.9 (40.7 to 106.6) | <0.0001 |
| Beta-lactam antibiotics | ||||
| Piperacillin/tazobactam (≥3 vs <3 days)* | 2.32 (1.82 to 2.96) | <0.0001 | 1.70 (1.18 to 2.43) | 0.004 |
| Meropenem (≥3 vs <3 days)* | 0.99 (0.71 to 1.37) | 0.94 | NI | – |
| Cefuroxim (≥3 vs <3 days)* | 0.73 (0.57 to 0.94) | 0.01 | 1.24 (0.85 to 1.80) | 0.26 |
All variables entered in the multivariable analysis were adjusted for the other variables in this model.
All beta-lactam drug exposures are 3 vs <3 days. eGFR was measured on day 7. If a day 7 measurement was not available, the last measurement before this day was used. All variables with a p value <0.2 were included in the multivariable model.
eGFR, estimated glomerular filtration rate; N, no; NI, not included; Y, yes.
Discussion
Principal findings
We observed that the duration of renal failure is prolonged in critically ill patients randomised to receive high exposure to broad-spectrum antibiotics and escalated diagnostic work-up according to a biomarker-strategy compared with patients randomised to receive standard care according to guidelines regarding use of antibiotics and diagnostics. This difference in renal function was mainly confined to a prolongation of existing renal dysfunction since there was only a moderate, although significant, difference in de novo acute renal failure.
To our knowledge, this study provides the first clinical report to inform this critical issue within ICU medicine. First, the study was a randomised, good clinical practice controlled trial with a high sample size for comparison of organ failure, and the patients' baseline characteristics in general and specifically regarding renal parameters were comparable. Second, the rate of follow-up, although not complete for the entire period, was high and equal among the groups and the rate of renal failure on the last day of follow-up in the two groups was comparable. Thus, the observed increased risk of persistent renal failure in the high-exposure group is attributable to this intervention in some way.
The intervention consisted of an increased number of culture samples, a proposed initiative to do further diagnostic imaging (no observed difference) and a rapid and aggressive antibiotic escalation with certain drugs, which was documented to be of substantial extent (supplementary table 2). As a moderate increase in microbiologic sampling would not cause renal failure and since there was no observed increase in diagnostic imaging, these interventions seems implausible reasons to explain the observations depicted in table 1.
This leaves us with the documented escalation in use of piperacillin/tazobactam and ciprofloxacin as possible explanations. Before concluding that the observed renal dysfunction was caused directly by one (or both) of these drugs, we wanted to exclude the possibility that the results had appeared because of a derived effect of an increase in fungal infections. Fungal infections have been linked to broad-spectrum antibiotics,16 and renal failure is a well-known complication to some antifungals.17 However, excluding all patients with invasive fungal infections did not alter the results.
Based on these results and after having excluded other potential explanations, we realised that nephrotoxicity from piperacillin/tazobactam and/or ciprofloxacin was the most plausible explanation of the observed renal dysfunction. To further substantiate this, several analyses were conducted. A multiple effects model was built to examine the GFR in the days after administration of different frequently used drugs. This model included the five most often administered antibiotics, including piperacillin/tazobactam, meropenem, cefuroxim, ciprofloxacin and vancomycin along with other known and suspected causes of renal failure. In this model, the use of piperacillin/tazobactam was associated with a striking low rate of GFR improvement compared with the other drugs investigated. Intriguingly, this adverse effect appears to be reversible since patients in whom piperacillin/tazobactam was discontinued had the fastest improvement in renal function as compared with patients on other antibiotic courses. Several sensitivity analyses were performed with findings consistent with this observation.
Comparison with other studies
Although clinical evidence regarding renal failure according to use of piperacillin/tazobactam in ICU patients has been limited, the influence of piperacillin on renal function has been investigated in healthy volunteers in laboratory experiments. In a cross-over experiment, the influence on drug clearance from concurrent administration of piperacillin and flucloxacillin was estimated.18 The authors observed that flucloxacillin clearance was reduced to 45% (90% CI 40 to 50%) when piperacillin was administered simultaneously, whereas piperacillin clearance was unaffected by concurrent flucloxacillin administration. Time–clearance slope modelling identified competitive inhibition of renal tubular secretion as the most likely explanation. Piperacillin-induced reduction of imipenem clearance19 and of tazobactam clearance has also been found,20 and a high correlation between creatinin clearance and piperacillin clearance has been documented,21 and thus, it is plausible that piperacillin specifically causes nephrotoxicity.
Additionally, the published randomised trials comparing piperacillin/tazobactam with other beta-lactam drugs in ICU settings are scarce, underpowered for assessment of renal failure end points and do generally not address renal end points.5–7 Trials from other settings: haematological patients, diabetes patients and surgical settings do generally not investigate renal failure end points, and in the few (non-ICU) trials that do report kidney end points, the total frequency of these makes the power to avoid type II error very low (diagram D2, online supplement).
Strengths and weaknesses of the study
Although our study is performed on analyses from a large, randomised, good clinical practice controlled trial with a stringent methodology and a high level of follow-up, there are limitations that deserve mentioning: first, follow-up for organ-related measures was not complete, although we followed patients for all blood samples done in (1) the hospital, at which they were initially recruited and (2) other hospitals in Denmark, where we had electronic access to blood samples. However, patients who continued to suffer from renal failure when discharged from hospital were out of reach for follow-up for their renal function. Of note, the fraction of patients with remaining renal failure at time of discharge was comparable between the two groups (table 2), and hence, it is unlikely that this lack of ability to ascertain renal outcome contributed to our main findings.
Second, eGFR may not be an accurate measure of creatinine clearance, as recently documented by Martin et al.22 However, even though this measure is not accurate to describe the creatinine clearance, changes in eGFR reflect changes in renal function, as validated, and is closely correlated to outcome.23 Additionally, since hydration can be a source of error, we used the baseline weight in the eGFR equation. Additionally, we found that eGFR <60 ml/min/1.73 m2 on day 7 is a strong independent predictor of mortality.
Third, the RIFLE criteria used as secondary end point measures are not suitable to detect renal failure from baseline and forth since the reference is defined as the pre-morbid creatinine. Hence, renal failure caused by exposure to antibiotics beginning at baseline will not necessarily be captured using these criteria. This was the reason for not using these as primary end points.
Forth, the study was a post hoc analysis using a previously published trial as material. We have tried to compensate for this by writing a detailed analysis plan based on the hypotheses, we wanted to test, before analysis. Fifth, although the sample size was relatively large compared with most other randomised trials in this setting, the sample size for these secondary analyses were based on the assumption of 25% renal failure in the standard-exposure group and a RR of 1.25 in the high-exposure group. The observed numbers were 21% and 1.22 of which calls for a slightly higher sample size. However, the sample size needed to show the differences observed in the multivariable analyses was far smaller, and since these analyses confirmed the main findings, we do not think the results are due to chance.
In this trial, for the first time ever to our knowledge, random allocation to high exposure to broad-spectrum antibiotics in the ICU has been systematically applied according to a systematic algorithm and this resulted in prolongation of renal failure. The results were confirmed when excluding patients with fungal infections, and a multiple effects model revealed a particularly low renal recovery in patients while piperacillin/tazobactam was administered and a remarkable recovery when discontinuing this drug, a finding that was specific for this drug. Several other crude and adjusted models likewise confirmed the findings. Finally, the results from this trial are supported by human experimental studies.
Conclusions
In conclusion, the use of piperacillin/tazobactam caused a delayed renal recovery in critically ill patients and renal function improved after discontinuation of the drug. However, the study is not designed to investigate de novo emergence of renal failure since the lowest renal function is at baseline in most patients. The study was not designed to establish whether the use of piperacillin/tazobactam or other of the interventional drugs, in some cases, cause persistent renal failure, and thus, further research to explore this is warranted. We think this impact on renal function is more likely caused by a—at least partially reversible—toxic effect on the renal tubule than by a lack of effect towards the infection since this drug is independently associated with a high chance of survival in other infected populations,8 and we must emphasise that our findings are strictly confined to critically ill patients.
Supplementary Material
Appendix 1.
The members of the Procalcitonin And Survival Study (PASS) study group are as follows: Central Coordinating Center: J U Jensen, B Lundgren, J Grarup, M L Jakobsen, S S Reilev, M Kofoed-Djursner, J D Lundgren; Regional Coordinating Centres: Hvidovre: J Løken, M Steensen; Gentofte: T Mohr, K Thornberg, K Thormar; Hillerød: L Hein, M Bestle; Glostrup: D Strange, A Ø Lauritsen; Herlev: H Tousi, P Søe-Jensen; Roskilde: N Reiter, N E Drenck; Skejby: M H Andersen, P Fjeldborg; Århus: K M Larsen; Data Management & Statistical Centre: Z Fox, J Kjær, D Kristensen; Procalcitonin Analysis & Logistics Centre: J U Jensen, B Lundgren, M B Rasmussen, C S v Hallas, M Zacho, J Iversen, T Leerbeck, M Jeppesen, K S Hansen, K B Jensen; Data and Safety Monitoring Board: H Masur (Chair), J Chastre, H Schønheyder, C Pedersen; Clinical Microbiology Management: B Lundgren, J D Knudsen, A Friis-Møller, K Schønning, A Lester, H Westh, G Lisby, J K Møller, B Bruun, J J Christensen, C Østergaard, M Arpi, K Astvad, M D Bartels, J Engberg, H Fjeldsøe-Nielsen, U S Jensen; PASS Site Clinical Investigators (numbers of recruited persons are in parentheses): Glostrup (290): L Hein, T Mohr, D G Strange, P L Petersen, A Ø Lauritsen, S Hougaard, T Mantoni, L Nebrich, A Bendtsen, L H Andersen, F Bærentzen, Andreas Eversbusch, B Bømler, R Martusevicius, T Nielsen. P M Bådstøløkken, C Maschmann, U Grevstad, P Hallas, A Lindhardt, T Galle, K Graeser, E Hohwu-Christensen, P Gregersen, H C Boesen, L M Pedersen, K Thiesen, L C Hallengreen, I Rye, J Cordtz, K R Madsen, P R C Kirkegaard, L Findsen, L H Nielsen, D H Pedersen, J H Andersen, C Albrechtsen, A Jacobsen, T Jansen, A G Jensen, H H Jørgensen, M Vazin; Gentofte (209): L Lipsius, K Thornberg, J Nielsen, K Thormar, M Skielboe, B Thage, C Thoft, M Uldbjerg, E Anderlo, M Engsig, F Hani, R B Jacobsen. L Mulla, U Skram; Herlev (154): H Tousi, P Søe-Jensen, T Waldau, T Faber, B Andersen, I Gillesberg, A Christensen, C Hartmann, R Albret, D S Dinesen, K Gani, M Ibsen; Hvidovre (148): J Løken, M Steensen, J A Petersen, P Carl, E Gade, D Solevad, C Heiring, M Jørgensen, K Ekelund, A Afshari, N Hammer, M Bitsch, J S Hansen, C Wamberg, T D Clausen, R Winkel, J Huusom, D L Buck, U Grevstad, E Aasvang, K Lenz, P Mellado, H Karacan, J Hidestål, J Høgagard, J Højbjerg, J Højlund, M Johansen, S Strande; Hillerød (138): M Bestle, S Hestad, M Østergaard, N Wesche, S A Nielsen, H Christensen, H Blom, C H Jensen K Nielsen, N G Holler, K A Jeppesen; Århus-Skejby (94): M H Andersen, P Fjeldborg, A Vestergaard, O Viborg, C D Rossau; Roskilde (90): N Reiter, M Glæemose, M B Wranér, C B Thomsen, B Rasmussen, C Lund-Rasmussen, B Bech, K Bjerregaard, L Spliid, L L W Nielsen, N E Drenck; Århus-Centre (63): K M Larsen, M Goldinger, D Illum, C Jessen, A Christiansen, A Berg, T Elkmann, J A K Pedersen, M Simonsen; Bispebjerg (14) H Joensen, H Alstrøm, C Svane, A Engquist.
Footnotes
To cite: Jensen J-US, Hein L, Lundgren B, et al. Kidney failure related to broad-spectrum antibiotics in critically ill patients: secondary end point results from a 1200 patient randomised trial. BMJ Open 2012;2:e000635. doi:10.1136/bmjopen-2011-000635
Contributors: J-USJ designed the study, made the data collection tools, monitored data collection for the whole trial, wrote the statistical analysis plan and drafted the paper. He is guarantor. J-USJ, ZF and JK cleaned and analysed the data. JL, BL, LH, MHB, TM, MHA, KJT, JL, MS, HT, PS-J, AØL, DGS, NR, KT, PCF, KML, N-ED, MEJ, LRN, CØ, ZF, JK and JG made input study design, data collection tools and analysis plan on the manuscript. J-USJ implemented the trial at the centres. All members of the Procalcitonin And Survival Study Group assisted in designing the trial.
Funding: This study was supported by grants from the Danish Research Council, The Lundbeck Foundation, Research Foundation for the Capitol Region of Denmark, The Toyota Foundation, Brahms Diagnostica (un-restricted grant), The Harboe Foundation, The A.P. Møller Foundation and the Idella Foundation. None of these had any influence on the design or conduct of the study; collection, management, analysis and interpretation of the data or the preparation or approval of the manuscript. All authors had full access to all the data in the study and conjointly take responsibility for the integrity of the data and the accuracy of the data analysis.
Competing interests: All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare that the trial was funded mainly by the Danish State (Danish Research Council), and all authors state that they have no relationships with companies that might have an interest in the submitted work in the previous 3 years; their spouses, partners or children have no financial relationships that may be relevant to the submitted work, and all authors have no non-financial interests that may be relevant to the submitted work.
Patient consent: We received written consent from the patient or the next of kin for trial inclusion.
Ethics approval: Ethical approval was provided by the ethics committee for Copenhagen and Frederiksberg Community (now Ethics Committee for the Capitol Region): H-KF-01-272-753.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data available.
References
- 1.Levy MM, Macias WL, Vincent JL, et al. Early changes in organ function predict eventual survival in severe sepsis. Crit Care Med 2005;33:2194–201 [DOI] [PubMed] [Google Scholar]
- 2.Jia X, Malhotra A, Saeed M, et al. Risk factors for ARDS in patients receiving mechanical ventilation for > 48 h. Chest 2008;133:853–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rubenfeld GD, Caldwell E, Peabody E, et al. Incidence and outcomes of acute lung injury. N Engl J Med 2005;353:1685–93 [DOI] [PubMed] [Google Scholar]
- 4.Kane-Gill SL, Jacobi J, Rothschild JM. Adverse drug events in intensive care units: risk factors, impact, and the role of team care. Crit Care Med 2010;38(Suppl 6):S83–9 [DOI] [PubMed] [Google Scholar]
- 5.Brun-Buisson C, Sollet JP, Schweich H, et al. Treatment of ventilator-associated pneumonia with piperacillin-tazobactam/amikacin versus ceftazidime/amikacin: a multicenter, randomized controlled trial. VAP Study Group. Clin Infect Dis 1998;26:346–54 [DOI] [PubMed] [Google Scholar]
- 6.Alvarez-Lerma F, Insausti-Ordenana J, Jorda-Marcos R, et al. Efficacy and tolerability of piperacillin/tazobactam versus ceftazidime in association with amikacin for treating nosocomial pneumonia in intensive care patients: a prospective randomized multicenter trial. Intensive Care Med 2001;27:493–502 [DOI] [PubMed] [Google Scholar]
- 7.Marra F, Reynolds R, Stiver G, et al. Piperacillin/tazobactam versus imipenem: a double-blind, randomized formulary feasibility study at a major teaching hospital. Diagn Microbiol Infect Dis 1998;31:355–68 [DOI] [PubMed] [Google Scholar]
- 8.Paul M, Yahav D, Bivas A, et al. Anti-pseudomonal beta-lactams for the initial, empirical, treatment of febrile neutropenia: comparison of beta-lactams. Cochrane Database Syst Rev 2010;11:CD005197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reich G, Cornely OA, Sandherr M, et al. Empirical antimicrobial monotherapy in patients after high-dose chemotherapy and autologous stem cell transplantation: a randomised, multicentre trial. Br J Haematol 2005;130:265–70 [DOI] [PubMed] [Google Scholar]
- 10.Gomez L, Estrada C, Gomez I, et al. Low-dose beta-lactam plus amikacin in febrile neutropenia: cefepime vs. piperacillin/tazobactam, a randomized trial. Eur J Clin Microbiol Infect Dis 2010;29:417–27 [DOI] [PubMed] [Google Scholar]
- 11.Sato T, Kobayashi R, Yasuda K, et al. A prospective, randomized study comparing cefozopran with piperacillin-tazobactam plus ceftazidime as empirical therapy for febrile neutropenia in children with hematological disorders. Pediatr Blood Cancer 2008;51:774–7 [DOI] [PubMed] [Google Scholar]
- 12.Bow EJ, Rotstein C, Noskin GA, et al. A randomized, open-label, multicenter comparative study of the efficacy and safety of piperacillin-tazobactam and cefepime for the empirical treatment of febrile neutropenic episodes in patients with hematologic malignancies. Clin Infect Dis 2006;43:447–59 [DOI] [PubMed] [Google Scholar]
- 13.Jensen JU, Hein L, Lundgren B, et al. Procalcitonin-guided interventions against infections to increase early appropriate antibiotics and improve survival in the intensive care unit: a randomized trial. Crit Care Med 2011;39:2048–58 [DOI] [PubMed] [Google Scholar]
- 14.Dellinger RP, Levy MM, Carlet JM, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med 2008;36:296–327 [DOI] [PubMed] [Google Scholar]
- 15.Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Crit Care Med 2003;31:1250–6 [DOI] [PubMed] [Google Scholar]
- 16.Hebert C, Villaran R, Tolentino J, et al. Prior antimicrobial exposure and the risk for bloodstream infection with fluconazole-non-susceptible Candida strains. Scand J Infect Dis 2010;42:506–9 [DOI] [PubMed] [Google Scholar]
- 17.Sorkine P, Nagar H, Weinbroum A, et al. Administration of amphotericin B in lipid emulsion decreases nephrotoxicity: results of a prospective, randomized, controlled study in critically ill patients. Crit Care Med 1996;24:1311–15 [DOI] [PubMed] [Google Scholar]
- 18.Landersdorfer CB, Kirkpatrick CM, Kinzig M, et al. Inhibition of flucloxacillin tubular renal secretion by piperacillin. Br J Clin Pharmacol 2008;66:648–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saitoh H, Oda M, Gyotoku T, et al. A beneficial interaction between imipenem and piperacillin possibly through their renal excretory process. Biol Pharm Bull 2006;29:2519–22 [DOI] [PubMed] [Google Scholar]
- 20.Komuro M, Maeda T, Kakuo H, et al. Inhibition of the renal excretion of tazobactam by piperacillin. J Antimicrob Chemother 1994;34:555–64 [DOI] [PubMed] [Google Scholar]
- 21.Aronoff GR, Sloan RS, Brier ME, et al. The effect of piperacillin dose on elimination kinetics in renal impairment. Eur J Clin Pharmacol 1983;24:543–7 [DOI] [PubMed] [Google Scholar]
- 22.Martin JH, Fay MF, Udy A, et al. Pitfalls of using estimations of glomerular filtration rate in an intensive care population. Intern Med J 2011;41:537–43 [DOI] [PubMed] [Google Scholar]
- 23.Bagshaw SM, George C, Dinu I, et al. A multi-centre evaluation of the RIFLE criteria for early acute kidney injury in critically ill patients. Nephrol Dial Transpl 2008;23:1203–10 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.