Abstract
OBJECTIVE:
Asians have a reduced risk for cerebral palsy (CP) compared with whites. We examined whether individual Asian subgroups have a reduced risk of CP and whether differences in sociodemographic factors explain disparities in CP prevalence.
METHODS:
In a retrospective cohort of 629 542 Asian and 2 109 550 white births in California from 1991 to 2001, we identified all children who qualified for services from the California Department of Health Services on the basis of CP. Asians were categorized as East Asian (Chinese, Japanese, Koreans), Filipino, Indian, Pacific Islander (Guamanians, Hawaiians, and Pacific Islanders), Samoan, or Southeast Asian (Cambodian, Laotian, Thai, Vietnamese).
RESULTS:
Overall, CP prevalence was lower in Asians than whites (1.09 vs 1.36 per 1000; relative risk = 0.80, 95% confidence interval [CI] = 0.74–0.87) and ranged from 0.61/1000 in Thai children to 2.08/1000 in Samoan children. Several Asian subgroups had low risk profiles with respect to maternal age, educational attainment, and birth weight. However, after we adjusted for maternal age and education, infant gender, and birth weight, the adjusted risk of CP remained lower in East Asians (odds ratio [OR] = 0.75, 95% CI = 0.65–0.87), Filipinos (OR = 0.87, 95% CI = 0.75–0.99), Indians (OR = 0.59, 95% CI = 0.44–0.80), Pacific Islanders (OR = 0.62, 95% CI = 0.40–0.97), and Southeast Asians (OR = 0.68, 95% CI = 0.57–0.82) compared with whites.
CONCLUSIONS:
Most Asian national origin subgroups have a lower rate of CP than whites, and this disparity is unexplained. Additional studies that focus on the cause of ethnic disparities in CP may provide new insights into pathogenesis and prevention.
KEY WORDS: cerebral palsy, racial disparity, epidemiology, sociodemographic
What’s Known on This Subject:
Asian Americans have a reduced risk of cerebral palsy (CP) compared with whites. Whether this is true for all Asian ethnic subgroups is unknown. Differences in sociodemographic factors may explain disparities in CP prevalence between Asians and whites.
What This Study Adds:
East Asian, Filipino, Indian, Pacific Islander, and Southeast Asian children were 13% to 38% less likely to have CP than white children. Differences in maternal age and education, gender, and birth weight did not explain these differences in CP rates.
Cerebral palsy (CP) is a clinical syndrome of motor dysfunction due to an intrauterine or perinatal brain lesion1 that occurs in 2 to 3.6 per 1000 births.2–4 The underlying causes of CP are poorly understood. Factors associated with an elevated risk of CP include older maternal age, low educational attainment, male gender, preterm birth, and low birth weight.5–7
CP rates vary significantly by race/ethnicity. Compared with non-Hispanic whites (referred to as “whites”), African Americans demonstrate an increased risk of CP that is largely explained by their increased risk of low birth weight.7 In contrast, Asian Americans (referred to as “Asians”) have a 20% to 30% reduced risk of CP across all birth weight strata.7 Why Asians have a lower risk of CP is unknown. Low maternal educational attainment and young maternal age have been associated with increased risk for CP, and these risk factors occur less commonly in some Asian groups than in whites,8,9 but it is unknown whether such sociodemographic differences account for the reduced risk of CP among Asians.
From 2000 to 2010, the Asian population grew faster (43%) than any other group in the United States.10 Between 2003 and 2006, 30% of all Asian and Pacific Islander births in the United States occurred in California.11 Although Asians are often categorized as a homogeneous group, there is increasing recognition that Asians differ widely in cultural beliefs, socioeconomic status, and health practices according to country of origin. Significant variability in maternal risk factors and perinatal outcomes has been reported among different subgroups of Asians.12–14 For instance, Chinese and Japanese mothers have the highest educational attainment and the lowest infant mortality rates of all Asian subgroups, whereas Cambodian and Laotian mothers have lower educational attainment and higher infant mortality.15,16 Whether the risk of CP varies among different Asian populations has not been studied. Therefore, in a large, multiethnic population in California, we compared the risk of CP in 13 different Asian subgroups and examined whether differences in sociodemographic factors explain the reduced risk of CP among Asians.
Methods
We conducted a retrospective cohort study of all infants who were born in California during an 11-year period (January 1, 1991, to December 31, 2001). Data were retrieved from 3 sources: (1) the California Office of Statewide Health Planning and Development’s (OSHPD) Patient Discharge Diagnoses; (2) the California Department of Health Services’ Linked Vital Statistics Birth and Infant Death file; and (3) the California Department of Developmental Services (DDS), a statewide program that provides services to children with CP regardless of income. All study procedures were approved by the California Committee for the Protection of Human Subjects, and by the institutional review boards at the University of California, San Francisco and the University of California, Davis.
The California OSHPD maintains a database of discharge abstracts for all admissions to nonfederal hospitals, which represent 96% (571 of 594) of all hospitals in the state. According to the 1991–1998 California natality figures from the Centers for Disease Control and Prevention, 96.7% of all live births in California were recorded in the OSHPD hospital discharge data set. From the OSHPD hospital discharge data set, we identified all live births in California during the study years, as well as insurance status for each hospital delivery. Women who were uninsured or publicly insured were categorized as having low insurance status, whereas women with private or managed care insurance were categorized as having high insurance status. From linked birth certificate data, we extracted the following variables: maternal age, Asian ethnicity, and years of education; timing of entry to prenatal care; infant gender, birth weight, and gestational age. We defined 4 birth weight categories: high (≥4500 g), normal (2500–4499 g), low (1500–2499 g), and very low (400–1500 g). We identified infants diagnosed with birth asphyxia (International Classification of Diseases, Ninth Revision, Clinical Modification 768.5–768.9) by searching OSHPD hospital discharge abstracts.
Asians were categorized into 13 national origin subgroups, listed according to the number of CP cases: Filipino (N = 211), Chinese (N = 124), Vietnamese (N = 91), Korean (N = 47), Indian (N = 46), Japanese (N = 28), Cambodian (N = 24), Samoan (N = 21), Laotian (N = 18), Pacific Islander (N = 11), Guamanian (N = 5), Hawaiian (N = 4), and Thai (N = 4). Information about Asian national origin subgroup was missing for 63 Asian children with CP; we included these children in the calculation of overall CP prevalence but excluded them from subgroup analyses. Given that several national origin subgroups had very few cases of CP, we grouped Asians into 6 categories that were based on geographic proximity: (1) East Asians (Chinese, Japanese, and Korean); (2) Filipinos; (3) Indians; (4) Pacific Islanders (Guamanian, Hawaiian, and Pacific Islanders); (5) Samoans; and (6) Southeast Asians (Cambodian, Laotian, Thai, and Vietnamese). We analyzed Samoans separately from Pacific Islanders because we found that they had an increased risk of CP in preliminary analyses.
The DDS runs a statewide program that provides occupational and physical therapy, case management, and social services for all residents who have a substantive disability related to CP. CP is defined as follows: (1) a nonprogressive lesion or disorder in the brain occurring during intrauterine life or the perinatal period and characterized by paralysis, spasticity, or abnormal control of movement or posture that is manifest before 2 to 3 years of age; and (2) other significant motor dysfunction appearing before age 18 years. Among infants born in the years 1991–2001 in the California birth cohort, we identified all children who qualified for DDS services for CP before November 30, 2006. Thus, all children in our study were at least 5 years old at the time of CP ascertainment. Because we were interested in prenatal and perinatal risk factors for CP, we excluded children with postnatal causes of CP, including child abuse (n = 272), motor vehicle and other vehicle injuries (n = 213), and near drowning (n = 72), based on available DDS data.
We used Pearson’s χ2 test to compare the frequency of demographic risk factors by Asian subgroup and computed relative risks (RRs) and 95% confidence intervals (95% CIs) to compare CP rates in Asians and whites. We used logistic regression to calculate odds ratios (ORs) and 95% CIs to determine whether CP rates in Asians and whites remained statistically different after adjusting for maternal age, education, infant gender, and birth weight. The logistic model included birth weight but not gestational age because these variables are collinear. Birth asphyxia is a possible mediator of the relationship between ethnicity and CP. We analyzed whether ethnic differences in birth asphyxia prevalence exist, and if so, whether CP rates differ between ethnic groups after excluding all patients with a diagnosis of birth asphyxia.
Analyses were performed by using Stata version 11.1 (Stata Corporation, College Station, TX) and with SAS 9.2 (SAS Institute Inc, Cary, NC).
Results
The overall prevalence of CP in the population was 1.40 per 1000 (8397 CP cases in 6 221 001 births). Asians comprised 10% of all births during the study period, and 8.3% of all cases of CP were Asian. Among 629 542 Asian births during the study period, we identified 697 children with CP, a prevalence of 1.09 per 1000 (95% CI = 1.01–1.17). We identified 2878 white children with CP within a population of 2 109 550, a prevalence of 1.36 per 1000 (95% CI = 1.31–1.41). Overall, the risk of CP was 20% lower in Asians than with whites (RR = 0.80, 95% CI = 0.74–0.87).
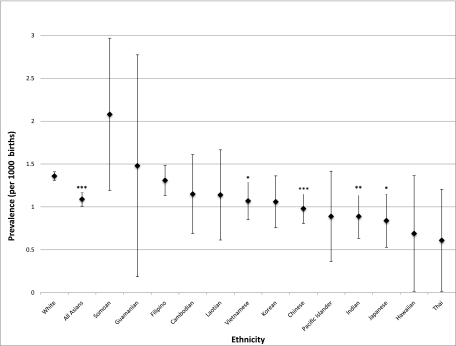
According to national origin subgroup, the prevalence of CP ranged from 0.61 per 1000 in Thai infants to 2.08 per 1000 in Samoans (Fig 1). Individual subgroups that had significantly lower CP rates than whites included Japanese (RR = 0.62, 95% CI = 0.42–0.89), Indian (RR = 0.65, 95% CI = 0.49–0.87), Chinese (RR = 0.72, 95% CI = 0.60–0.86), and Vietnamese (RR = 0.79, 95% CI = 0.64–0.97). Although Samoans had a higher crude rate of CP than whites, the difference was not significant (RR = 1.53, 95% CI = 0.99–2.38). When Asians were combined into 6 geographic categories, 3 groups had a significantly lower risk of CP compared with whites: East Asians (RR = 0.71, 95% CI = 0.63–0.83), Indians (RR = 0.65, 95% CI = 0.48–0.87), and Southeast Asians (RR = 0.79, 95% CI = 0.66–0.93, Table 1).
FIGURE 1.
Prevalence of CP among Asian and white infants born in California, 1991–2001. Asterisks indicate that CP prevalence differs significantly compared with whites (*P < .05, ** P < .01, ***P < .001).
TABLE 1.
Risk of CP in Asian and White Infants Born in California, 1991–2001
| Ethnicity | Births, n | CP, n | Prevalence (per 1000) | RR | 95% CI | P |
|---|---|---|---|---|---|---|
| White | 2 113 749 | 2878 | 1.4 | 1.0 | Ref | Ref |
| Indian | 51 883 | 46 | 0.9 | 0.7 | 0.5–0.9 | .004 |
| Pacific Islander | 21 582 | 20 | 0.9 | 0.7 | 0.4–1.1 | .10 |
| East Asian | 204 547 | 199 | 1.0 | 0.7 | 0.6–0.8 | <.0001 |
| Southeast Asian | 128 382 | 137 | 1.1 | 0.8 | 0.7–0.9 | .006 |
| Filipino | 161 802 | 211 | 1.3 | 1.0 | 0.8–1.1 | .65 |
| Samoan | 10 129 | 21 | 2.1 | 1.5 | 1.0–2.4 | .054 |
Among Asians as a whole, we identified several risk factors for CP (Table 2). Older mothers (>35 years) had a 32% increased risk of having a child with CP. Children born to mothers with less than 6 years of education were 50% more likely to have CP than children born to mothers who had graduated from college. Compared with college graduates, children born to mothers with secondary school education (6–11 years) and mothers who attended some college also experienced significantly higher CP rates (Table 2). Boys were 50% more likely to have CP than girls, as has been described previously.2,7,17 The strongest risk factor for CP was low birth weight (RR = 4.3) and very low birth weight (RR = 25).
TABLE 2.
Sociodemographic Risk Factors for CP Among 629 542 Asian Births in California, 1991–2001
| CP | Prevalence per 1000 | RR | 95% CI | P | ||
|---|---|---|---|---|---|---|
| n | % | |||||
| Maternal age, y | ||||||
| <18 | 12 | 1.9 | 1.5 | 1.4 | 0.8–2.6 | .21 |
| 18–34 | 464 | 73 | 1.0 | 1.0 | Ref | |
| ≥35 | 158 | 25 | 1.4 | 1.3 | 1.1–1.6 | <.01 |
| Maternal education, y | ||||||
| Primary school or none (0–5) | 32 | 5.1 | 1.5 | 1.5 | 1.1–2.2 | .02 |
| Secondary school (6–11) | 71 | 11 | 1.3 | 1.3 | 1.0–1.7 | .06 |
| High school graduate (12) | 146 | 23 | 1.1 | 1.1 | 0.9–1.4 | .41 |
| Some college (13–15) | 173 | 27 | 1.2 | 1.2 | 1.0–1.5 | .03 |
| College graduate (≥16) | 209 | 33 | 1.0 | 1.0 | Ref | — |
| Onset of prenatal care | ||||||
| First trimester | 527 | 84 | 1.1 | 1.0 | Ref | — |
| Second trimester | 78 | 12 | 1.1 | 1.0 | 0.8–1.2 | .87 |
| Third trimester | 16 | 2.6 | 1.1 | 1.0 | 0.6–1.7 | .96 |
| No prenatal care | 6 | 1.0 | 2.0 | 1.8 | 0.8–4.1 | .14 |
| Low insurance status | 220 | 35 | 1.2 | 1.1 | 0.9–1.3 | .24 |
| Infant gender: boy | 390 | 62 | 1.3 | 1.5 | 1.3–1.8 | <.01 |
| Birth weight, g | ||||||
| Very low (400–1499) | 112 | 18 | 19 | 25 | 20–31 | <.01 |
| Low (1500–2499) | 102 | 16 | 3.3 | 4.3 | 3.4–5.3 | <.01 |
| Normal (2500–4499) | 415 | 65 | 0.8 | 1.0 | Ref | — |
| High (≥4500) | 5 | 0.8 | 1.0 | 1.2 | 0.5–3.0 | .63 |
| Gestational age, wk | ||||||
| <32 | 99 | 16 | 16 | 19 | 16–24 | <.01 |
| 32–36 | 90 | 15 | 2.0 | 2.4 | 1.9–3.0 | <.01 |
| ≥37 | 413 | 69 | 0.8 | 1.0 | Ref | — |
We examined ethnic group differences in the distribution of risk factors that were identified to be associated with CP in Asians (Table 3). Advanced maternal age (>35 years) was less common in Indians (10%) and Pacific Islanders (13%) than in whites (18%). College graduation rates were significantly higher in mothers of East Asian (52%), Indian (51%), and Filipino (36%) descent than among whites (31%), whereas Samoan mothers had a very low rate of college graduation (4%). Low birth weight and very low birth weight infants were more common in Indians, Pacific Islanders and Filipinos than whites.
TABLE 3.
Distribution (%) of Selected Characteristics of Asian and White Infants Born in California, 1991–2001, by Maternal Ethnicity
| Maternal ethnicitya | Maternal Age, y | Maternal Education, y | Birth weight, g | ||||
|---|---|---|---|---|---|---|---|
| <18 | ≥35 | ≤12 | ≥16 | <1500 | 1500−2499 | ≥4500 | |
| White | 2.3 | 18 | 41 | 31 | 1.0 | 4.0 | 2.2 |
| Indian | 0.2 | 10 | 25 | 51 | 1.2 | 7.2 | 0.5 |
| Pacific Islander | 3.1 | 13 | 60 | 14 | 1.3 | 5.0 | 3.2 |
| East Asian | 0.3 | 25 | 27 | 52 | 0.7 | 4.2 | 0.8 |
| Southeast Asian | 2.9 | 17 | 64 | 16 | 1.0 | 5.6 | 0.5 |
| Filipino | 1.8 | 21 | 28 | 36 | 1.3 | 6.3 | 0.9 |
| Samoan | 3.0 | 9.3 | 76 | 4.1 | 1.2 | 3.5 | 5.1 |
Note that all comparisons between Asian groups and whites were statistically significant (P < .01).
To determine whether differences in demographic risk factors accounted for the lower rates of CP among most Asian national origin subgroups, we performed multivariate logistic regression that controlled for maternal age and education, infant gender, and birth weight (Table 4). After adjusting for these sociodemographic and infant factors, we found that children born to women of East Asian, Filipino, Indian, Pacific Islander, and Southeast Asian origins were 13% to 38% less likely to have CP than children born to white women (Table 4). Other independent risk factors for CP included advanced maternal age, less than college education, male gender, and low birth weight (Table 4). Of note, the crude CP risk estimates in Table 1 did not change appreciably after adjusting for confounders in the multivariate analysis, suggesting that the sociodemographic and infant factors we analyzed were not significant confounders. The diagnosis of birth asphyxia was somewhat less common in East Asian than white infants (1.7% vs 2.2%, P = .001). When we excluded infants with birth asphyxia from the analyses, East Asians still had a significantly reduced risk of CP compared with whites (RR = 0.69, 95% CI = 0.59–0.81), which suggests that differences in birth asphyxia do not explain this disparity.
TABLE 4.
Independent Effects of Sociodemographic Factors on Risk of CP in a Multivariable Model
| OR | 95% CI | |
|---|---|---|
| Ethnicitya | ||
| White | 1.0 | Ref |
| Indian | 0.6 | 0.4–0.8 |
| Pacific Islander | 0.6 | 0.4–1.0 |
| East Asian | 0.8 | 0.7–0.9 |
| Southeast Asian | 0.7 | 0.6–0.8 |
| Filipino | 0.9 | 0.8–1.0 |
| Samoan | 1.5 | 0.96–2.3 |
| Maternal age, y | ||
| <18 | 0.9 | 0.7–1.1 |
| 18–34 | 1.0 | Ref |
| ≥35 | 1.3 | 1.2–1.4 |
| Maternal education, y | ||
| Primary school or none (0–5) | 1.4 | 1.0 – 1.8 |
| Secondary school (6–11) | 1.3 | 1.1 – 1.4 |
| High school graduate (12) | 1.2 | 1.1 – 1.3 |
| Some college (13–15) | 1.1 | 1.0 – 1.2 |
| College graduate (≥16) | 1.0 | Ref |
| Boy | 1.4 | 1.3–1.5 |
| Birth weight category | ||
| Very low (400–1499 g) | 27 | 25–30 |
| Moderately low (1500–2499 g) | 5.4 | 4.9–5.9 |
| Normal (2500–4499 g) | 1.0 | Ref |
| High (≥4500 g) | 0.9 | 0.7–1.2 |
Logistic regression model includes all variables in the table.
Discussion
Previous studies have revealed that CP is less common in Asians than in whites6,7; however, it was unknown whether this disparity applies to all Asian subgroups. We found that adjusted CP rates were significantly lower in nearly all Asian subgroups, compared with whites, with the exception of Samoans. Risk factor profiles for CP were similar in Asian and white populations. However, differences in rates of low birth weight, maternal age, and education were insufficient to explain the lower CP rates observed in Asians compared with whites. It is well recognized that perinatal outcomes differ across different Asian subgroups.8,9,13,14,16,18 For instance, neonatal mortality rates in the 1980s were lower in most Asian groups than in whites, except for Thai and Laotian infants, who exhibited increased neonatal mortality.9 Among California births in the 1990s, Cambodian, Japanese, and Korean infants had lower neonatal mortality than white infants, whereas Thai infants experienced increased neonatal mortality.15,16 Birth weight outcomes also vary by ethnic subgroup, with Indians experiencing the highest risk of low birth weight among all Asian subgroups.13,14,19
In this large, population-based study of California births, the risk of CP was consistently low across many Asian groups, with the exception of Samoans. This consistency across most Asian groups was somewhat unexpected, given that Asian subgroups vary in rates of other birth outcomes such as neonatal mortality. Thai infants exhibited the lowest CP rate in our study, even though Thai infants have the highest reported neonatal mortality among Asian subgroups.9,16 It is possible that higher neonatal mortality rates with reduced survival to age 2, the age at which CP is typically diagnosed, could account for lower CP rates in specific subpopulations. However, neonatal mortality rates among many Asian groups in California have been lower than the rate seen in whites,9,15,16 which would argue against differential survival as an explanation for the lower CP rates observed in Asians.
There is no clear explanation for the lower rate of CP among Asian children than white children. Although Chinese, Japanese, Korean, and Vietnamese mothers have lower rates of very low birth weight infants than white women,16 controlling for birth weight did not close the gap in CP rates between Asians and whites in our study. Similarly, differences in frequency of birth asphyxia did not explain lower Asian CP rates. Low maternal educational attainment was less common in East Asians and Indians and more common in Pacific Islanders and Samoans, as has been previously described.8 However, CP rates remained lower in most Asian groups than whites after adjusting for maternal education.
In contrast to other Asian groups, Samoans had a 50% higher adjusted CP rate than whites, though this difference was of borderline statistical significance. Consistent with previous reports,13,14 macrosomia was relatively common in Samoan infants, but birth weight did not explain the trend for increased CP among Samoans. Further studies with larger numbers of Samoans are needed to determine whether CP is truly more common in this population. Obesity is common among Samoan women,20 and maternal obesity has been associated with a threefold increased risk of CP.21 Studies of maternal obesity and CP may also provide additional insight into ethnic disparities in CP.
Racial and ethnic data obtained from California birth certificates are highly reliable and exhibit over 96% predictive value for maternal race/ethnicity, as classified by postpartum interview.22 However, we lacked ethnic subgroup information for a small number of Asian infants, and we could not adjust for mixed maternal heritage. Our study was limited by the small number of CP cases in several Asian subgroups and also by ascertainment bias. Because children with mild CP may not seek or qualify for services from the DDS, patients identified from the DDS data set are probably more severely impaired than the general population of children with CP. Children with CP who moved to another state would have been excluded, and there is no way to know if there were ethnic differences in relocation. The overall CP rate in our study (1.4 per 1000) is lower than most reported population prevalence rates (1.9–3.6 per 1000).2,23–25 This is likely because our study includes only more severely affected children with CP.
It is also possible that Asians are less likely to seek services from DDS than whites, which could result in an ascertainment bias that could contribute to ethnic differences in risk of CP. Although DDS services are not dependent upon financial income, there may be cultural reasons for Asians to be more reluctant to seek assistance from DDS. Given the widely disparate cultures, health practices, and beliefs represented by the different Asian subgroups in this study, however, it would be difficult to attribute the consistently lower CP rates seen across Asian subgroups to lower DDS enrollment, though this possibility cannot be completely excluded. Another California population-based study of children with CP in a large health maintenance organization who were identified through medical record review (rather than use of services) also revealed a reduced risk of CP among Asians compared with whites (RR = 0.7, 95% CI = 0.5–1.0).6
Potential explanations for the reduced risk of CP seen in Asians could include differences in rates of maternal infection, congenital anomalies, or delivery complications other than birth asphyxia. On-going data analyses of complications occurring during pregnancy and delivery may shed further light on ethnic differences in CP. Maternal nativity could also play a role in explaining the reduced risk of CP in Asians. Infants of mothers who were born outside the United States exhibit improved birth outcomes compared with US-born mothers.26,27 Among several Asian groups, preterm delivery and low birth weight were less common among foreign-born mothers than US-born mothers.18,19,28 From 1992 to 1997 and 1999 to 2003, 88% of all Asian births in California were to foreign-born mothers.18 Therefore, future studies of CP that take into account the role of maternal birth place may uncover additional insights regarding CP disparities between Asians and whites. By examining the reasons behind the disparity in CP rates between Asians and whites, we may obtain a better understanding of the underlying causes of CP and come closer to developing effective interventions to reduce the prevalence of CP in all racial/ethnic groups.
Glossary
- CI
confidence interval
- CP
cerebral palsy
- DDS
Department of Developmental Services
- OR
odds ratio
- OSHPD
Office of Statewide Health Planning and Development
- RR
relative risk
Footnotes
All authors provided substantial contributions to conception and design, acquisition of data, analysis and interpretation of data, and to drafting the article or revising it critically for intellectual content; and all authors provided final approval of version being submitted. Each author participated sufficiently in the work to take public responsibility for appropriate portions of the content.
FINANCIAL DISCLOSURE: Drs Wu and Gilbert have provided expert testimony on cases related to cerebral palsy; the other authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by the Cerebral Palsy International Research Foundation, the National Institutes of Health grant R03-HD050575, and the National Institutes of Health Pathways to Careers in Clinical and Translational Research grant 5 TL1 RR 24129-5. Funded by the National Institutes of Health (NIH).
References
- 1.Bax M, Goldstein M, Rosenbaum P, et al. Executive Committee for the Definition of Cerebral Palsy . Proposed definition and classification of cerebral palsy, April 2005. Dev Med Child Neurol. 2005;47(8):571–576 [DOI] [PubMed] [Google Scholar]
- 2.Yeargin-Allsopp M, Van Naarden Braun K, Doernberg NS, Benedict RE, Kirby RS, Durkin MS. Prevalence of cerebral palsy in 8-year-old children in three areas of the United States in 2002: a multisite collaboration. Pediatrics. 2008;121(3):547–554 [DOI] [PubMed] [Google Scholar]
- 3.Topp M, Uldall P, Greisen G. Cerebral palsy births in eastern Denmark, 1987--90: implications for neonatal care. Paediatr Perinat Epidemiol. 2001;15(3):271–277 [DOI] [PubMed] [Google Scholar]
- 4.Colver AF, Gibson M, Hey EN, Jarvis SN, Mackie PC, Richmond S, The North of England Collaborative Cerebral Palsy Survey . Increasing rates of cerebral palsy across the severity spectrum in north-east England 1964-1993. Arch Dis Child Fetal Neonatal Ed. 2000;83(1):F7–F12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nelson KB. Causative factors in cerebral palsy. Clin Obstet Gynecol. 2008;51(4):749–762 [DOI] [PubMed] [Google Scholar]
- 6.Wu YW, Croen LA, Shah SJ, Newman TB, Najjar DV. Cerebral palsy in a term population: risk factors and neuroimaging findings. Pediatrics. 2006;118(2):690–697 [DOI] [PubMed] [Google Scholar]
- 7.Wu YW, Xing G, Fuentes-Afflick E, Danielson B, Smith LH, Gilbert WM. Racial, ethnic, and socioeconomic disparities in the prevalence of cerebral palsy. Pediatrics. 2011;127(3). Available at: www.pediatrics.org/cgi/content/full/127/3/e674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Le LT, Kiely JL, Schoendorf KC. Birthweight outcomes among Asian American and Pacific Islander subgroups in the United States. Int J Epidemiol. 1996;25(5):973–979 [DOI] [PubMed] [Google Scholar]
- 9.Morrow HW, Chávez GF, Giannoni PP, Shah RS. Infant mortality and related risk factors among Asian Americans. Am J Public Health. 1994;84(9):1497–1500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.United States Census. 2010 Census shows America’s diversity. 2010. Available at: http://2010.census.gov/news/releases/operations/cb11-cn125.html. Accessed July 7, 2011
- 11.United States Department of Health and Human Services (US DHHS), Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS), Division of Vital Statistics, Natality public-use data 2003-2006, on CDC WONDER Online Database, March 2009. Available at: http://wonder.cdc.gov/natality-current.html. Accessed February 8, 2012
- 12.Fuentes-Afflick E, Hessol NA. Impact of Asian ethnicity and national origin on infant birth weight. Am J Epidemiol. 1997;145(2):148–155 [DOI] [PubMed] [Google Scholar]
- 13. Wong LF, Caughey AB, Nakagawa S, Kaimal AJ, Tran SH, Cheng YW. Perinatal outcomes among different Asian-American subgroups. Am J Obstet Gynecol. 2008;199(4):382; e381–e386 [DOI] [PubMed] [Google Scholar]
- 14.Rao AK, Daniels K, El-Sayed YY, Moshesh MK, Caughey AB. Perinatal outcomes among Asian American and Pacific Islander women. Am J Obstet Gynecol. 2006;195(3):834–838 [DOI] [PubMed] [Google Scholar]
- 15.Qin C, Gould JB. The Asian birth outcome gap. Paediatr Perinat Epidemiol. 2006;20(4):279–289 [DOI] [PubMed] [Google Scholar]
- 16.Baker LC, Afendulis CC, Chandra A, McConville S, Phibbs CS, Fuentes-Afflick E. Differences in neonatal mortality among whites and Asian American subgroups: evidence from California. Arch Pediatr Adolesc Med. 2007;161(1):69–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnston MV, Hagberg H. Sex and the pathogenesis of cerebral palsy. Dev Med Child Neurol. 2007;49(1):74–78 [DOI] [PubMed] [Google Scholar]
- 18.Qin C, Gould JB. Maternal nativity status and birth outcomes in Asian immigrants. J Immigr Minor Health. 2010;12(5):798–805 [DOI] [PubMed] [Google Scholar]
- 19.Hayes DK, Lukacs SL, Schoendorf KC. Heterogeneity within Asian subgroups: a comparison of birthweight between infants of US and non-US born Asian Indian and Chinese mothers. Matern Child Health J. 2008;12(5):549–556 [DOI] [PubMed] [Google Scholar]
- 20.Sundborn G, Metcalf PA, Gentles D, et al. Overweight and obesity prevalence among adult Pacific peoples and Europeans in the Diabetes Heart and Health Study (DHAHS) 2002-2003, Auckland New Zealand. N Z Med J. 2010;123(1311):30–42 [PubMed] [Google Scholar]
- 21.Walstab J, Bell R, Reddihough D, Brennecke S, Bessell C, Beischer N. Antenatal and intrapartum antecedents of cerebral palsy: a case-control study. Aust N Z J Obstet Gynaecol. 2002;42(2):138–146 [DOI] [PubMed] [Google Scholar]
- 22.Baumeister L, Marchi K, Pearl M, Williams R, Braveman P. The validity of information on “race” and “Hispanic ethnicity” in California birth certificate data. Health Serv Res. 2000;35(4):869–883 [PMC free article] [PubMed] [Google Scholar]
- 23.Nelson KB. The epidemiology of cerebral palsy in term infants. Ment Retard Dev Disabil Res Rev. 2002;8(3):146–150 [DOI] [PubMed] [Google Scholar]
- 24.Wu YW, Swaiman KF. Cerebral palsy. In: Swaiman A, Ferriero, eds. Pediatric Neurology: Principles and Practice. Vol 1. Philadelphia, PA: Mosby Elsevier; 2006:491 [Google Scholar]
- 25.ACPR Group. Report of the Australian Cerebral Palsy Register. Birth years, 1993–2003, Dec 2009. Available at: https://secure.cpregister-aus.com.au/. Accessed February 8, 2012
- 26.Guendelman S, English PB. Effect of United States residence on birth outcomes among Mexican immigrants: an exploratory study. Am J Epidemiol. 1995;142(suppl 9):S30–S38 [DOI] [PubMed] [Google Scholar]
- 27.David RJ, Collins JW, Jr. Differing birth weight among infants of U.S.-born blacks, African-born blacks, and U.S.-born whites. N Engl J Med. 1997;337(17):1209–1214 [DOI] [PubMed] [Google Scholar]
- 28.Singh GK, Yu SM. Adverse pregnancy outcomes: differences between US- and foreign-born women in major US racial and ethnic groups. Am J Public Health. 1996;86(6):837–843 [DOI] [PMC free article] [PubMed] [Google Scholar]