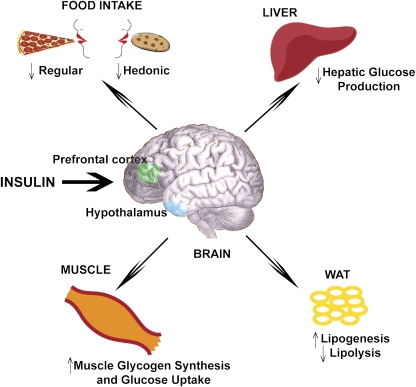
Last year marked the ninetieth anniversary of the discovery of insulin by Nobel Laureates Frederick Banting and John Macleod, as well as Charles Best and James Bertram Collip. The initial success of insulin’s ability to lower glucose levels in type 1 diabetes is now shadowed by the urgent need to characterize insulin resistance and secretion defects in type 2 diabetes and obesity. Insulin triggers signaling pathways in liver, muscle, and fat that inhibit glucose production and increase glucose uptake (1). However, it has only been in recent years that the brain has received attention for being an insulin-sensitive organ that regulates food intake (2) and glucose (3) and lipid (4) homeostasis in animals (Fig. 1).
FIG. 1.
A working hypothesis for insulin action in the brain. Insulin triggers signaling cascades in the brain to regulate food intake and modulate the reward-related hedonic food response. In addition, brain insulin action alters glucose and lipid metabolism. The hypothalamus (blue) is the main effector of the metabolic changes induced by insulin and can coordinate the prefrontal cortex (green) to regulate the hedonic assessment of appetite. WAT, white adipose tissue.
Circulating insulin crosses the blood-brain barrier and acts on its receptor in the hypothalamus to lower food intake and body weight (2). Infusion of insulin into the central nervous system (CNS) lowers food intake in rats (5), mice (6), and baboons (7), whereas hyperphagia is detected in neuronal insulin receptor knockout mice (8). Further, high-fat feeding induces hypothalamic insulin resistance in rodents (9). Although these animal studies expand the role of insulin to regulate appetite and suggest that characterizing insulin signaling pathways may reveal novel targets that reverse brain insulin resistance in obesity, a central question remains, Is insulin action in the brain clinically relevant?
To address this question, an intranasal peptide delivery method was developed in humans (10). This method enables selective elevation of peptide levels in the cerebrospinal fluid without altering plasma peptide levels (10). Using this method, intranasal injection of insulin was found to inhibit food intake in normal fasting men but not women (11). This is consistent with the fact that central insulin lowers food intake in male but not female rats (5); however, hyperphagia is detected in neuronal insulin receptor knockout female but not male mice (8). While CNS insulin does not appear to affect appetite in women, intranasal insulin alters their brain activity under food-stimulated conditions (12). Furthermore, CNS insulin action regulates food reward circuitry in rodents (13). Together, these studies underscore the possibility that the anorectic effect of insulin may be amplified in postprandial conditions in women. In the current issue of Diabetes, Hallschmid et al. (14) carried out well-controlled and designed studies in women to test this hypothesis.
Two sets of experiments permit distinguishing the effects of intranasal insulin administration in postprandial versus fasting conditions. In the first set, the postprandial effects of insulin were assessed in young, lean, healthy women who were given lunch (1230–1245 h) followed by intranasal insulin versus placebo delivery at 1300 h. Appetite rating and blood samples were then collected, and a snack intake test was assessed at 1505 h. In the second set of experiments, women who fasted overnight were given intranasal insulin versus placebo at 1000 h, followed by the same sampling and snack testing protocol. Of note, snack testing involved giving the blinded subjects three types of cookies: butter, coconut, and chocolate chip.
The authors show that intranasal insulin delivery reduced appetite in the postprandial but not the fasted women. In addition, intranasal insulin selectively reduced the intake and the palatability of chocolate cookies among the postprandial women, but failed to alter intake or palatability of other cookies or total calories associated with cookie intake. These interesting findings illustrate the potential clinical relevance in and support the working hypothesis put forward by studies in rodents that CNS insulin action inhibits the hedonic food reward system via dopamine neurons in the ventral tegmental area (13,15). Unfortunately, the current study did not offer mechanistic insights responsible for the differential anorectic responses induced by CNS insulin in women and men (11), as well as in fasting and postprandial conditions. Nonetheless, the data in this report, together with previous literature, highlight a potential role of insulin action in the brain that serves as a physiological satiety factor inhibiting palatable food in postprandial humans. The working hypothesis, of course, remains to be tested.
Another important finding made by the authors was that within ∼30–40 min of intranasal insulin injection (i.e., time 1345 h), while appetite was yet to be affected, plasma glucose level was lowered by ∼1 mmol/L in the postprandial women. Importantly, this significant reduction in plasma glucose occurred independently of changes in circulating plasma insulin, C-peptide, leptin, and ghrelin levels at this time point. It is not known whether a change in plasma glucagon level was detected. Nonetheless, given that intranasal insulin delivery in 30 min is sufficient to elevate insulin levels in cerebrospinal fluid (10), these findings are in line with previous reports in rats (3) and dogs (16,17), suggesting that direct brain insulin infusion lowers plasma glucose levels independently of changes in food intake.
Only when the liver is removed does central insulin fail to lower glucose levels in dogs (17), suggesting that brain insulin action lowers glucose levels through a modulation of hepatic glucose metabolism. In fact, insulin triggers signaling cascades and activates ATP-sensitive potassium (KATP) channels in the hypothalamus to inhibit glucose production in rodents (3), while activation of hypothalamic KATP channels in humans is implicated to inhibit glucose production (18). Although accumulating evidence indicates that insulin action in the brain of humans and animals reduces plasma glucose levels, it remains to be assessed whether changes in hepatic glucose production induced by CNS lead to the drop in plasma glucose levels. This is due to the fact that insulin action in the brain fails to inhibit hepatic glucose production in dogs while inhibiting net hepatic glucose output and increasing hepatic glycogen synthesis (19). Future comparative studies are warranted in humans, dogs, and rodents to evaluate the ability of insulin action in the brain to regulate hepatic glucose metabolism and glucose homeostasis in various experimental conditions.
Although the drop in plasma glucose induced by intranasal insulin delivery was rapid, the effect was transient and disappeared before a change in appetite was detected. Could a continuous delivery of intranasal insulin sustain the drop in plasma glucose levels and consequently reduce appetite at an earlier time point? Is it because intranasal insulin delivery first delivers insulin to brain regions that are important for glucose regulation and then to other regions for food reward regulation that a drop in plasma glucose levels is first detected? The current study would have benefited from the use of neuroimaging to assess whether different regions of the brain are affected at the time when intranasal insulin delivery reduced appetite and intake of highly palatable snack but not glucose levels and vice versa. In addition, use of a glucose-kinetics clamp technique (18) would be crucial to evaluate whether intranasal insulin delivery inhibits glucose production.
The impact of intranasal insulin delivery on the regulation of lipid homeostasis in humans warrants future investigations. In addition, it has been observed that an enhancement of hypothalamic endoplasmic reticulum stress causes hypothalamic insulin resistance in rodents (6). Given that brain insulin resistance is also detected (20) and delivery of chemical chaperones that reduce endoplasmic reticulum stress improves peripheral insulin sensitivity (21) in obese humans, could the delivery of chemical chaperones enhance brain insulin action?
In summary, although future studies are needed to clarify and evaluate the clinical and metabolic impact of brain insulin action, mounting evidence is beginning to suggest that insulin action in the brain of both animals and humans regulates energy and glucose homeostasis.
ACKNOWLEDGMENTS
P.I.M. is supported by an Ontario graduate scholarship and a Banting and Best Diabetes Centre/University Health Network graduate award. The laboratory of T.K.T.L. is supported by grants from the Canadian Institutes of Health Research (MOP-86554 and -82701), Canadian Diabetes Association (OG-3-10-3048), the Canada Research Chair in Obesity, the John Kitson McIvor Endowed Chair in Diabetes Research, and the Early Researcher Award from the Ontario Ministry of Research and Innovation (ER08-05-141). T.K.T.L. holds the John Kitson McIvor Endowed Chair in Diabetes Research and the Canada Research Chair in Obesity at the Toronto General Research Institute and the University of Toronto.
No potential conflicts of interest relevant to this article were reported.
Footnotes
See accompanying original article, p. 782.
REFERENCES
- 1.Saltiel AR, Kahn CR. Insulin signalling and the regulation of glucose and lipid metabolism. Nature 2001;414:799–806 [DOI] [PubMed] [Google Scholar]
- 2.Schwartz MW, Woods SC, Porte D, Jr, Seeley RJ, Baskin DG. Central nervous system control of food intake. Nature 2000;404:661–671 [DOI] [PubMed] [Google Scholar]
- 3.Pocai A, Lam TK, Gutierrez-Juarez R, et al. Hypothalamic K(ATP) channels control hepatic glucose production. Nature 2005;434:1026–1031 [DOI] [PubMed] [Google Scholar]
- 4.Scherer T, O’Hare J, Diggs-Andrews K, et al. Brain insulin controls adipose tissue lipolysis and lipogenesis. Cell Metab 2011;13:183–194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clegg DJ, Riedy CA, Smith KA, Benoit SC, Woods SC. Differential sensitivity to central leptin and insulin in male and female rats. Diabetes 2003;52:682–687 [DOI] [PubMed] [Google Scholar]
- 6.Zhang X, Zhang G, Zhang H, Karin M, Bai H, Cai D. Hypothalamic IKKbeta/NF-kappaB and ER stress link overnutrition to energy imbalance and obesity. Cell 2008;135:61–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Woods SC, Lotter EC, McKay LD, Porte D., Jr Chronic intracerebroventricular infusion of insulin reduces food intake and body weight of baboons. Nature 1979;282:503–505 [DOI] [PubMed] [Google Scholar]
- 8.Brüning JC, Gautam D, Burks DJ, et al. Role of brain insulin receptor in control of body weight and reproduction. Science 2000;289:2122–2125 [DOI] [PubMed] [Google Scholar]
- 9.Clegg DJ, Gotoh K, Kemp C, et al. Consumption of a high-fat diet induces central insulin resistance independent of adiposity. Physiol Behav 2011;103:10–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Born J, Lange T, Kern W, McGregor GP, Bickel U, Fehm HL. Sniffing neuropeptides: a transnasal approach to the human brain. Nat Neurosci 2002;5:514–516 [DOI] [PubMed] [Google Scholar]
- 11.Benedict C, Kern W, Schultes B, Born J, Hallschmid M. Differential sensitivity of men and women to anorexigenic and memory-improving effects of intranasal insulin. J Clin Endocrinol Metab 2008;93:1339–1344 [DOI] [PubMed] [Google Scholar]
- 12.Guthoff M, Grichisch Y, Canova C, et al. Insulin modulates food-related activity in the central nervous system. J Clin Endocrinol Metab 2010;95:748–755 [DOI] [PubMed] [Google Scholar]
- 13.Figlewicz DP, Sipols AJ. Energy regulatory signals and food reward. Pharmacol Biochem Behav 2010;97:15–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hallschmid M, Higgs S, Thienel M, Ott V, Lehnert H. Postprandial administration of intranasal insulin intensifies satiety and reduces intake of palatable snacks in women. Diabetes 2012;61:782–789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Könner AC, Hess S, Tovar S, et al. Role for insulin signaling in catecholaminergic neurons in control of energy homeostasis. Cell Metab 2011;13:720–728 [DOI] [PubMed] [Google Scholar]
- 16.Chowers I, Lavy S, Halpern L. Effect of insulin administered intracisternally on the glucose level of the blood and the cerebrospinal fluid in vagotomized dogs. Exp Neurol 1966;14:383–389 [DOI] [PubMed] [Google Scholar]
- 17.Agarwala GC, Mittal RK, Bapat SK, Bhardwaj UR. Effect of centrally administered insulin on blood glucose levels in dogs. Indian J Physiol Pharmacol 1977;21:11–18 [PubMed] [Google Scholar]
- 18.Kishore P, Boucai L, Zhang K, et al. Activation of K(ATP) channels suppresses glucose production in humans. J Clin Invest 2011;121:4916–4920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramnanan CJ, Saraswathi V, Smith MS, et al. Brain insulin action augments hepatic glycogen synthesis without suppressing glucose production or gluconeogenesis in dogs. J Clin Invest 2011;121:3713–3723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guthoff M, Stingl KT, Tschritter O, et al. The insulin-mediated modulation of visually evoked magnetic fields is reduced in obese subjects. PLoS ONE 2011;6:e19482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Engin F, Hotamisligil GS. Restoring endoplasmic reticulum function by chemical chaperones: an emerging therapeutic approach for metabolic diseases. Diabetes Obes Metab 2010;12(Suppl. 2):108–115 [DOI] [PubMed] [Google Scholar]