Abstract
Purpose
We present 120 patients (37 males, 83 females) affected by thoracic lumbar scoliosis, treated by posterior instrumented arthrodesis with the insertion of pedicle screws by “free hand technique”, without any image guided system, radioscopy use during insertion or intraoperative neurophysiological monitoring.
Methods
Seventy-two (60%) patients have been treated by hybrid instrumentation with lumbar and thoracic screws, hooks and wires at thoracic levels, while the remaining 48 (40%) patients have used only lumbar and thoracic pedicle screws. Mean Cobb grades value of the main scoliotic curve was 73° before surgery in patients treated by hybrid instrumentation, reduced to 37.5° after surgery. In patients treated only by screws, mean Cobb grades value of the main scoliotic curve was 65°, reduced to 16° after surgery.
Results
Minimum follow up has been 3 years; mean patient age at surgery was 15 years and 4 months. We placed a total number of 1,004 pedicle screws, 487 of which at thoracic level. In 12 patients (10%) a total number of 20 screws were misplaced at postoperatory exam, without any clinical complication for the patients or consequences on the arthrodesis or on maintaining the correction of the curve.
Conclusions
In our experience pedicle screws is the method that leads to best correction and balance on vertebral bodies, with best results at distance concerning correction maintaining. Our experience shows that even at thoracic level, pedicle screws insertion by free-hand technique is safe and reliable.
Keywords: Scoliosis, Free-hand technique, Pedicle screws, Pedicle violation
Introduction
The use of pedicle screws has become popular during past decade, first in lumbar spine and subsequently in thoracic spine surgery application. Pedicle screws provide various advantages over other methods of spinal fixation: better pull-out strength, greater control in the sagittal, coronal and rotational planes, fewer vertebral motion segments arthrodesed, secure fixation after laminectomy or in presence of incompetent posterior elements and lesser need for postoperative bracing [1].
In patients with spinal deformity segmental pedicle fixation shows enhanced three-dimensional correction with decreased rates of curve progression and higher fusion rates. Pedicle screws fixation has demonstrated the capability to treat severe scoliosis (between 70 and 100 Cobb degrees) without anterior release, with lower total hospital cost, lesser morbidity and an attempt at direct apical vertebral derotation to enhance correction, and to potentially obviate the need for thoracoplasty. The flexibility of multiple screw types allows easier connection to rods, particularly in deformed vertebra [1, 2].
Pedicle screws currently form an integral part of the armamentarium of the spinal surgeon; however, there are still many controversies regarding the use of pedicle screws, and complications are encountered [2].
Complications related to screws use include: screw misplacement, pedicle fracture, screw rupture, bending or loosening, vertebral canal violation, dural tear, vascular or visceral problems and postoperative neurologic symptoms or pain. Complications are potentially more serious at thoracic level as pedicle dimensions are inferior and the close relation of vascular, visceral and neurologic structures with vertebras could lead to severe damage in the case of screw misplacement [1].
Methods that have been used to aid the surgeon in appropriate screw placement included the use of intraoperative fluoroscopy, radiography and image-guided techniques. Multiple sources of error for image-guided systems have been documented: imaging errors, surface-model generation errors, errors in fixing of tracking devices to the patient, registration errors and inaccuracy of surgical tools; the necessary accuracy varies significantly depending on patient anatomy [3]. These accuracy requirements exceed the accuracy of current image-guided surgical systems, based on clinical utility errors reported in the literature.
Free-hand pedicle screw insertion technique relies on tactile feedback of the surgeon and the use of anatomical marks to determine correct screw entry point, without the aid of intraoperative image-guided systems or explorative laminectomy, with no or limited use of intra-operative fluoroscopy. When adopted by a skilled operator, free-hand technique has shorter surgical time, as there is no need of placing guide systems on the spine, or of performing explorative laminectomy or placing pedicle markers and the interruptions of the surgical procedure to let fluoroscopy control of screw placement are reduced to minimum, dramatically reducing exposure of patients and operating room personnel, patient tissues exposition and blood loss. The main shortcoming of free-hand technique is the rather long learning curve, as the successful placement of the screws depends entirely on surgeon ability and a great experience is demanded to obtain good results. In the hands of a skilled and experienced spine surgeon, free-hand technique is a safe and effective procedure.
The diameter of transverse pedicles, the morphology and the angle of the pedicles to vertebral body are the critical anatomical variable on safe placement of the pedicle screw [4–10]. The main shortcoming in using pedicle screws is the risk of iatrogenic damage owing to errors in inserting screws: these errors could cause spinal canal violation, pedicle fracture, nerve root compression and vascular or visceral lesions [11, 12].
In our experience, according to international literature, we began using pedicle screws at lumbar level, with hybrid instrumentation (lumbar screws and sublaminar hooks and wires at thoracic spine level) (Fig. 1); then we started to use screws at every level including thoracic spine, with a selective placement, i.e. not inserting pedicle screws in all thoracic vertebrae in arthrodesis area (Figs. 2, 3).
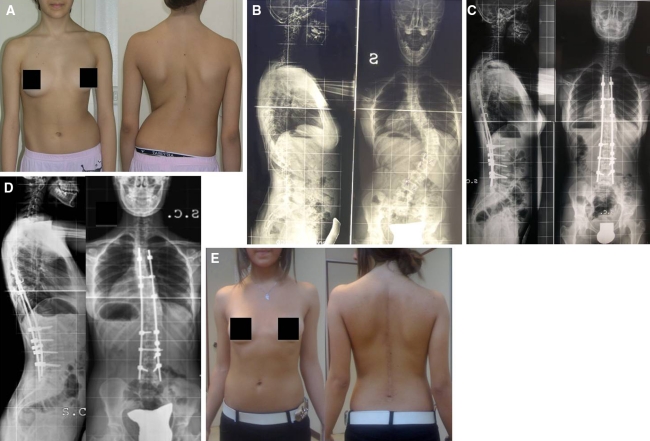
Fig. 1.
E.Y., female, 13-year old, idiopathic scoliosis (a). Main curve 63° Cobb (b). Control after posterior arthrodesis, hybrid instrumentation (c). Control 5 years after surgery, no loss of reduction (d). Clinical result (e)
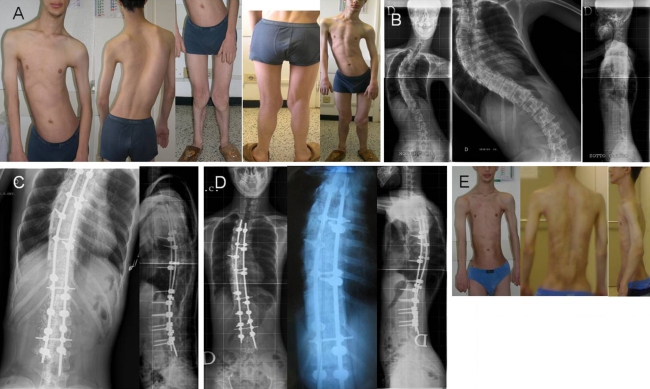
Fig. 2.
A.Q., male, 14-year old, dysmorphic scoliosis, surgical treatment to lower limbs (a). Main curve 78° Cobb (b). Control after posterior arthrodesis, screws instrumentation (c). Control 39 months after surgery, no loss of reduction (d). Clinical result (e)
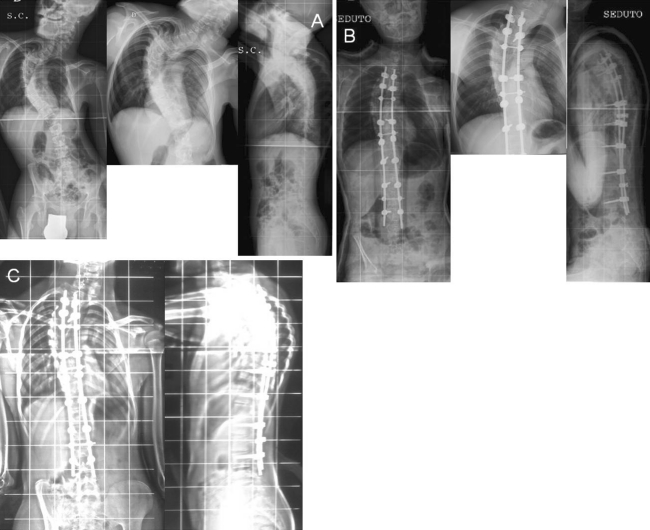
Fig. 3.
L.R., male, 15-year old, neurologic scoliosis in cerebral palsy from hydrocephalus (a). Control after posterior arthrodesis, screws instrumentation (b). Control 5 years after surgery, no loss of reduction (c)
Materials and methods
From 1997 to 2007 we treated 120 patients (83 females, 37 males) affected by thoracic lumbar scoliosis by free-hand technique pedicle screws insertion instrumentation. Mean patient age at the time of the procedure was 15 years and 4 months. Our patients comprise:
– 96 idiopathic scoliosis
– 10 neurologic scoliosis
– 6 scoliosis associated to dismorphic syndrome
– 8 congenital scoliosis.
In 72 patients (60%) we used hybrid instrumentation with pedicle screws at lumbar and thoracic level and hooks and sublaminar wires at thoracic level, while in the remaining 48 patients (40%) we used only pedicle screws at thoracic and lumbar level. We inserted a total of 1,004 screws, 487 at thoracic level (arriving to T11), 517 at lumbar level.
All operations were performed by the same surgeon. During procedure there was no use of navigator or explorative laminectomy, and intra-operative radioscopic controls were reduced at minimum. We performed wake-up test in all patients with negative results. We did not use intraoperative neurophysiologic monitoring during procedures. All patients were studied before surgery by standard X-rays exam of the spine in anterior–posterior and lateral projections plus lateral bendings in anterior–posterior projection, and by MRI of the cord to assess the presence of neural abnormalities. In some selected cases patients have been studied by traction whole spine anterior posterior view (Stagnara suspension test). Some patients were studied by CT scan for viewing vertebral abnormalities (as in congenital scoliosis cases), but CT scan was not used routinely to assess diameter and orientation of the deformed pedicles.
All patients were evaluated after surgery with clinical exam and anterior–posterior and lateral X-rays at 1, 3, 6 months and 1 year, and then every other year. Minimum follow-up was 3 years.
The free-hand technique for placement of pedicle instrumentation relies completely on the use of visible and palpable anatomic landmarks for accurate pedicle screws placement. It depends on a clear exposition and identification of the posterior elements bony landmarks, including the entire transverse process and the caudal and cephalic facet joints [13]. In the lumbar spine an osteotomy (partial facetectomy) of the inferior–lateral one-third of the inferior articular process of the superior vertebra is performed for three reasons: it enables the identification of the exact limit between the superior and inferior articular processes; it facilitates the correct identification of the initial perforation site; it decreases the amount of cortical bone, which may make the initial perforation difficult, specially in the presence of hypertrophic facets, and is the first step toward arthrodesis. In our practice we perform an accurate anatomic exposition of posterior bone structure of the spine, beginning with subperiosteal dissection, to remove muscles insertion with minimal hemorrhage; hemostasis is meticulous, as to reduce blood loss and maintain a clear operating field, determining correct insertion point for screws. The entry point is the intersection between a line that passes just laterally to the inferior articular process and a line, which bisects the transverse process [14]. The direction of the screws follows the axis of the pedicle. It is slightly oblique toward the midline. After initial perforation, an internal pedicle palpation by ball tip probe is used to verify the presence of possible pedicle violations. The optimal anatomic location for screw entry in the thoracic spine is much more difficult to be determined in comparison to lumbar level [3, 15, 16]. In our opinion in the thoracic spine the best way is to identify lateral and medial limits of upper articular facet, as these landmarks sign the origin of the pedicle from vertebra, as pedicle is always perpendicular to facet. In our practice we use variable insertion points in high, middle and low thoracic spine and in lumbar spine, based on anatomic landmarks, and, after removing cortical bone in insertion point, we proceed with cautious progressive insertion. We continuously assess the integrity of screw bone path using a ballpoint probe, always searching for eventual pedicle violation by probing the presence of four intact bone walls inside the pedicle. Radiologic controls have been reduced to a minimum; we used radioscopy only to assess correct position on the spine, and as final control of the screws insertion, usually in lateral view. For single patient mean X-rays exposition has been 1.3 s (range 0.5–2 s exposition). In spines affected by severe deformity it is more often necessary to use more views with fluoroscopy in transverse position to assess pedicle screws paths: so in these patients X-rays exposition is longer than in patients affected by lesser deformity.
Results
In our patients mean Cobb angle value of main scoliosis curve was 65° (45°–99°) in cases treated by screws only, with mean 39% reduction at bending test and 73° (63°–96°) in cases treated by hybrid instrumentation, with mean 43% reduction at bending test. After surgery these values have been reduced to 16° (9°–42°) with mean 61% improvement in patients treated by screws only and to 37.5° (16°–45°) with mean 49% improvement in patients treated by hybrid instrumentation. In 12 patients (10%) a total number of 20 screws were misplaced at a standard X-ray examination after surgery.
The overall reported rates of correct pedicle screw placement is extremely variable in the literature [12, 17–19]. The studies on the complication associated with the use of pedicle screws varied greatly with respect to the number of patients and devices; Liljenqvist et al. [20] and Weinstein et al. [21] found an overall missing rate of 20%. In these studies it seems that the addition of fluoroscopy during screws insertion little improves the accuracy of screw placement, especially in the upper and middle thoracic spine. In our patients we limited the use of fluoroscopy only to assess correct position of the screws after insertion, and we experienced no major pedicle wall violation. However, the increased rates of radiographic cortical violations do not necessarily correlate with poorer clinical outcome [15, 22]. In our patients we had no cases of major complication (infection, neurologic lesion, major or minor, vascular lesion or other visceral lesion).The 12 patients that presented misplaced screws had no complications at follow up. We had three cases of broken lumbar screws and one case of loosening of the rod from the lumbar screw at follow up, all without loss of correction. Our results are in accordance with international literature, and our experience is similar to Weinstein, as X-rays exposition in our patients has been reduced to control at the end of screws placement, with surgical team away from patient during radiologic exam.
Discussion
Pedicle screw fixation is potentially dangerous as screw misplacement can cause damages to near structures. These dangers are much more evident in thoracic spine, because of maximum permissible translational error of less than 1 mm and rotational error of less than 5° at the normal midthoracic spine due to small pedicle diameter and little space between the spinal cord and medial pedicle. Although many studies reported medial wall violation of the thoracic pedicle, the incidence of neurologic, cardiovascular or visceral complication associated to medial wall violation is rather low [23, 24]. The anatomic characteristic of the thoracic pedicle demonstrates a thicker medial cortical wall compared to the lateral wall. Compared to the lumbar spine, the pedicle entry point is more ventral. The convex and ventral sides of the scoliotic spine usually have room because the dural sac and cord shift toward the concave, dorsal side. Rotation of the concave pedicle toward the convex side increases the angle of convergence relative to sagittal plane. Because of these anatomic characteristic and possible plastic deformation of the pedicle wall the fixation may be performed in a safe way. Lateral perforation of the pedicular cortex is potential threat to the pleural cavity, great vessels and esophagus, mainly in the upper and middle thoracic level. In the case of inferior violations, in the thoracic spine the most feared consequence is refractory neuropathic pain, whereas in the lumbar spine injury to the emerging nerve roots may lead to unacceptable motor deficits [25]. Risk is higher over T10 level as between T10 and L4 a “safety zone” exists, which tolerates medial violations up to 4 mm without significative clinical symptoms. This was attributed to the larger diameter of the pedicle at this region as well as larger diameter of the spine canal. Anterior violations in the lumbar spine are much less dangerous once abdominal viscera are usually not fixed to the anterior longitudinal ligament. In 12 of our patients (10%) at X-ray control after surgery we found misplaced screws: we had a total number of 20 misplaced screws, 7 at thoracic level out of 487 thoracic pedicle screws inserted and 13 at lumbar level out of 517 lumbar pedicle screws. All these misplaced screws were laterally placed and none impinged into vertebral canal. As none of these 12 patients experienced any symptoms such as pain, muscular weakness or other neurologic adverse effects and no visceral adverse effect, we did not see the opportunity to perform CT scan postoperatory exam. At follow up none of this patient group displayed any loss of correction of treated deformity. Wake up test, as well as intraoperative neurophysiologic monitoring is useful in avoiding major pedicle wall violation but do not improve significantly the reliability of the safe screw placement without pedicle wall minor violation (2 mm or lesser) in upper and middle thoracic spine, because of poor sensitivity and positive predictive values [25]. In our experience we have never used intraoperative neurophysiologic monitoring during procedure, without experiencing any neurological impairment in our patients after surgery.
Conclusion
“Free hand pedicle screw insertion technique” without radiographic guidance, intraoperative tracking devices use and intraoperative neurophysiologic monitoring appears to be a safe and reliable procedure. The operating surgeon must have a thorough knowledge of spine and vertebral anatomy, he must follow and use diligent and repetitive confirmatory steps to compulsively assure intra osseous placement. Even if pedicle wall violations are possible, if the technique is correct and the misplacement not redundant, permanent complications are rather rare. The incidence of pedicle violation in the literature is inversely correlated with the size of the pedicle, so technique must be particular accurate in the thoracic spine. In our experience an accurate anatomic landmark preparation during surgery allows a safe positioning of thoracic pedicle screws, and we do not use routinely CT scan to assess pedicles morphology before surgery. We performed free-hand procedure without intraoperative neurophysiologic monitoring and in our series we experienced no neurologic impairment; our opinion is that these technical supports are useful, but in no way mandatory to obtain a safe and successful pedicles screws insertion at all levels, even in thoracic spine. Our past successful experience guided us in expanding screws use at all vertebral level in our surgical routine, eliminating hybrid instrumentation. The authors have operated other 150 patients from 2007 to 2011 for a total of 1,048 screws inserted with free-hand technique at all vertebral level, included thoracic spine, with all-screws instrumentation (just using hooks at upper foundation); these cases have not been reported, but at present none of the 150 mentioned patient presented any neurologic impairment or other adverse effect.
Conflict of interest
None.
References
- 1.Xu R, Ebraheim NA, Ou Y, Yeasting RA. Anatomic consideration of pedicle screw placement in the thoracic spine: Roy-Camille technique versus open-lamina technique. Spine. 1998;23(9):1065–1068. doi: 10.1097/00007632-199805010-00021. [DOI] [PubMed] [Google Scholar]
- 2.Yongjung JK, Lenke LG. Thoracic pedicle screw placement: free-hand technique. Neurol India. 2005;53(4):512–519. doi: 10.4103/0028-3886.22622. [DOI] [PubMed] [Google Scholar]
- 3.Rampersaud RR, Simon DA, Foley KT. Accuracy requirements for image-guided spinal pedicle screw placement. Spine. 2001;26(4):352–359. doi: 10.1097/00007632-200102150-00010. [DOI] [PubMed] [Google Scholar]
- 4.Parent S, Labelle H, Skalli W, Guise J. Thoracic pedicle morphometry in vertebrae from scoliotic spines. Spine. 2004;29:239–248. doi: 10.1097/01.BRS.0000109995.64028.FE. [DOI] [PubMed] [Google Scholar]
- 5.Misenheimer GR, Peek RD, Wiltse LL, Rothman SL, Widell EH. Anatomic analysis of pedicle cortical and cancellous diameter as related to screw size. Spine. 1989;14:367–372. doi: 10.1097/00007632-198904000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Kothe R, O’Holleran JD, Liu W, Panjabi MM. Internal architecture of the thoracic pedicle. An anatomic study. Spine. 1996;21:264–270. doi: 10.1097/00007632-199602010-00002. [DOI] [PubMed] [Google Scholar]
- 7.Hou S, Hu R, Shi Y. Pedicle morphology of the lower thoracic and lumbar spine in a Chinese population. Spine. 1993;18:1850–1855. doi: 10.1097/00007632-199310000-00021. [DOI] [PubMed] [Google Scholar]
- 8.Panjabi MM, O’Holleran JD, Crisco JJ, Kothe R. Compexity of the thoracic spine pedicle anatomy. Eur Spine J. 1997;6:19–24. doi: 10.1007/BF01676570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zindrick MR, Knight GW, Sartori MJ, Carnevale TJ, Patwardhan AG, Lorentz MA. Pedicle morphology in the immature thoracolumbar spine. Spine. 2000;25:2726–2735. doi: 10.1097/00007632-200011010-00003. [DOI] [PubMed] [Google Scholar]
- 10.Vaccaro AR, Rizzolo SJ, Allardyce TJ, Ramsey M, Salvo J, Balderston RA, Cotler JM. Placement of pedicle screws in the thoracic spine. Part I: morphometric analysis of the thoracic vertebrae. J Bone Joint Surg Am. 1995;77:1193–1199. doi: 10.2106/00004623-199508000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Ebraheim NA, Jabaly G, Xu R, Yeasting RA. Anatomic relations of the thoracic pedicle to the adjacent neural structures. Spine. 1997;22:1553–1557. doi: 10.1097/00007632-199707150-00002. [DOI] [PubMed] [Google Scholar]
- 12.Vaccaro AR, Rizzolo SJ, Baldestron RA, Allardyce TJ, Garfin SR, Dolinskas C, An HS. Placement of pedicle screws in the thoracic spine. Part II: an anatomical and radiographic assessment. J Bone Joint Surg Am. 1995;77:1200–1206. doi: 10.2106/00004623-199508000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Cinotti G, Gumina S, Ripani M, Postacchini F. Pedicle instrumentation in the thoracic spine. A morphometric and cadaveric study for placement of screws. Spine. 1999;24:114–119. doi: 10.1097/00007632-199901150-00003. [DOI] [PubMed] [Google Scholar]
- 14.Mattei TA, Meneses MS, Milano JB, Ramina R. Free hand technique for thoracolumbar pedicle screw instrumentation: critical appraisal of current “State of Art”. Neurol India. 2009;57:715–721. doi: 10.4103/0028-3886.59465. [DOI] [PubMed] [Google Scholar]
- 15.Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD. Free hand pedicle screw placement in the thoracic spine: is it safe? Spine. 2004;29(3):333–342. doi: 10.1097/01.BRS.0000109983.12113.9B. [DOI] [PubMed] [Google Scholar]
- 16.Chung KJ, Shu SW, Desai S, Song HR. Ideal entry point for the thoracic pedicle screw during the free hand technique. Int Orthop. 2008;32:657–662. doi: 10.1007/s00264-007-0363-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Castro WH, Halm H, Jerosch J, Malms J, Steinbeck J, Blasius S. Accuracy of pedicle screw placement in lumbar vertebrae. Spine. 2006;21:1320–1324. doi: 10.1097/00007632-199606010-00008. [DOI] [PubMed] [Google Scholar]
- 18.Farber GL, Place HM, Mazur RA, Jones DE, Damiano TR. Accuracy of pedicle screw placement in lumbar fusions by plain radiographs and computed tomography. Spine. 1995;20:1494–1499. doi: 10.1097/00007632-199507000-00010. [DOI] [PubMed] [Google Scholar]
- 19.Berlemann U, Heini P, Muller U, Stoupis C, Schwarzenbach O. Reliability of pedicle screw assessment utilizing plain radiographs versus CT reconstruction. Eur Spine J. 1997;6:406–410. doi: 10.1007/BF01834069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liljenqvist UR, Halm HF, Link TM. Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine. 1997;22:2239–2245. doi: 10.1097/00007632-199710010-00008. [DOI] [PubMed] [Google Scholar]
- 21.Weinstein JN, Spratt KF, Spengler D, Brick C, Reid S. Spinal pedicle fixation: reliability and validity of roentgenogram-based assessment and surgical factors on successful screw placement. Spine. 1988;13:1012–1018. doi: 10.1097/00007632-198809000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Lonstein JE, Denis F, Perra JH, Pinto MR, Smith MD, Winter RB. Complications associated with pedicle screws. J Bone Joint Surg Am. 2001;81(11):1519–1528. doi: 10.2106/00004623-199911000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Halm HF, Niemer T, Link TM. Segmental pedicle screw instrumentation in idiopathic thoracolumbar and lumbar scoliosis. Eur Spine J. 2000;9:192–197. doi: 10.1007/s005860000139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Belmont PJ, Klemme WR, Dhawan A. In vivo accuracy of thoracic pedicle screws. Spine. 2001;26:2340–2346. doi: 10.1097/00007632-200111010-00010. [DOI] [PubMed] [Google Scholar]
- 25.Papin P, Arlet V, Marchesi D, Rosenblatt B, Aebi M. Unusual presentation of spinal cord compression related to misplaced pedicle screws in thoracic scoliosis. Eur Spine J. 1999;8:156–160. doi: 10.1007/s005860050147. [DOI] [PMC free article] [PubMed] [Google Scholar]