Abstract
Erectile dysfunction (ED) has been defined as the persistent inability to attain and maintain an erection sufficient to permit satisfactory sexual performance. By 2025, men with ED will be approximately 322 million, an increase of nearly 170 million men from 1995. The present study was aimed to evaluate the efficacy of Ashwagandha (Withania somnifera) in the management of psychogenic erectile dysfunction. In this study, a total of 95 patients with psychogenic erectile dysfunction satisfying the DSM IV TR diagnostic criteria were selected, out of them 86 patients completed the course of treatment. In Trial Group, Ashwagandha root powder and in Control group, Placebo (Wheat powder) were given for 60 days. Treatment selection and its allocation were done by following computerized randomization plan. Criterion of assessment was based on the scoring of International Index of Erectile Function (IIEF) Scale. Paired and Unpaired t test were used for statistical analysis. In Trial group (n=41), 12.6% and in Control group (n=45), 19.11% of improvement was observed with the significance of (P<0.001). There was no significant difference (P>0.05) found in between the two groups. Both Ashwagandha and Placebo provided no relief (<25% improvement on IIEF) in psychogenic erectile dysfunction.
Keywords: Ashwagandha, International Index of Erectile Function, placebo, psychogenic erectile dysfunction
Introduction
Erectile dysfunction has been defined as the persistent inability to attain and maintain an erection sufficient to permit satisfactory sexual performance. Although ED is a benign disorder, it affects physical and psychosocial health and has a significant impact on the quality of life of sufferers and their partners and families. In the National Health and Social Life Survey (NHSLS), the prevalence of sexual dysfunctions (not specific ED) was 31%.[1] It is estimated that in 1995 there were over 152 million men worldwide who had ED, and in 2025 the number of men with ED will be approximately 322 million, an increase of nearly 170 million men. The greatest increases will be in the developing world, that is, Africa, Asia, and South America.[2]
The erectile difficulties in Psychogenic Male Erectile Disorder are frequently associated with sexual anxiety, fear of failure, concerns about sexual performance, and a decreased subjective sense of sexual excitement and pleasure. ED can disrupt existing marital or sexual relationships and may be the cause of unconsummated marriages and infertility.[3] Although Psychogenic Erectile Dysfunction is a most prevalent condition, only few studies were conducted on this subject in Ayurvedic field.
In Ayurvedic classics, sexual dysfunctions are dealt under the domain of Klaibya. Susruta first described the condition called Manasa Klaibya, which closely resembles with Psychogenic Erectile Dysfunction and for treating this condition Susruta has given priority to Hetu Viparyaya Chikitsa and various Vajeekarana Yogas.[4] For treating Psychogenic Erectile Dysfunction, the drug should possess the qualities of Vajeekarana and at the same time it should be able to pacify the vitiated Manasika Doshas.
Withania somnifera, commonly known as Ashwagandha, is an important medicinal plant that is being used in Ayurvedic and indigenous medicine for over 3000 years. Withania is widely claimed to have potent aphrodisiac, sedative, rejuvenative, and life-prolonging properties. It is also used as a general energy-enhancing tonic known as Medharasayana.[5] Ashwagandha is preferred for adjuvant use in the management of various psychosomatic conditions and it improves tissue vitality, physical and mental endurance, and neuromuscular strength.[6] It is used as a sedative in the treatment of insanity; experimental data prominently label this plant as antistress, anticonvulsant, and tranquilizer. Based on these properties Ashwagandha was selected as a Trial drug in the present study.
Aim and objective
To evaluate the efficacy of Ashwagandha in the management of Psychogenic Erectile Dysfunction.
Materials and Methods
Study design
The present study is a randomized, single-blind, placebo-controlled, parallel-group study.
Selection of the patients
All patients fulfilling the Inclusion Criteria were selected from the OPD of I.P.G.T. and R.A. Hospital, Jamnagar, irrespective of caste, religion, and economic status with their written informed consent.
Inclusion criteria
Patients who are fulfilling the DSM–IV TR Diagnostic. Criteria of Male Erectile Disorder Psychogenic type (302.72).[7]
Belonging to the age group between 18 and 60 years.
Serum testosterone levels should be more than 239 ng/dL.
Exclusion criteria
Male Erectile Disorder Organic type.
Sexual dysfunctions that are substance induced.
Age below 18 and above 60 years.
Major Organic and Psychotic disorders.
Serum testosterone levels less than 239 ng/dL.
The study was cleared by the Institutional Ethics Committee. Written consent was taken from each patient willing to participate before the start of the study. Patients were free to withdraw from the study at any time without giving any reason. A detailed proforma was prepared incorporating Ayurvedic as well as Modern points.
A total of 95 patients were registered in the present study. In the Trial Group, 46 patients were registered, among them 41 patients completed the course of treatment and 5 patients discontinued the treatment. In the Control Group, 49 patients were registered, among them 45 patients completed the course of treatment and 4 patients discontinued. A total of 86 patients completed the course of treatment and 9 patients discontinued in both the groups.
Laboratory investigations
Semen analysis including Sperm Count, Volume, Motility, Liquefaction time and Morphology, Routine Hematological tests, such as Hemoglobin, Total RBC Count, Total Leukocyte Count, Differential Leukocyte Count, Erythrocyte Sedimentation Rate, Packed Cell Volume, Platelet Count, Bleeding time, and Clotting time, Biochemical Investigations, such as Random Blood Sugar, Serum Cholesterol, Serum Triglycerides, HDL Cholesterol, Total protein, Albumin, Globulin, Albumin Globulin Ratio, S.G.P.T, S.G.O.T, Serum Bilirubin, Alkaline Phosphatase, Blood Urea, and Serum Creatinine, Urine Physical, Chemical, and Microscopic examination were carried out.
All these investigations were carried out before the treatment to exclude any organic pathology and to assess the general condition of the patient. If any of the abnormalities were found in the investigation reports, those patients were excluded (n=18) from the study.
Serum Testosterone levels were measured for all of the patients before treatment. Those who were having Serum Testosterone levels less than 239 ng/dL were not registered in the study. This is to exclude any organic, endocrinal pathology, and Hypoactive Sexual Desire Disorder.
Grouping
The patients satisfying Inclusion Criteria were selected and randomly divided into two groups by following computerized randomization plan.[8]
Intervention
In Trial Group, Ashwagandha (Withania somnifera) tablets were given in the dose of 4 tablets (500 mg each) thrice a day through oral route after food for 60 days. Placebo (Wheat powder) tablets in the dose of 4 tablets (500 mg each) thrice a day orally after food for 60 days has been given to the Control Group. The follow-up period was 30 days in both groups after the treatment period. Nature of the disease was explained and reassurance was given to all the patients belonging to both the groups.
Method of preparation of Ashwagandha and placebo tablets
Dried roots of Ashwagandha were cleaned and ground into a fine powder of 60 mesh size. Powder was filtered through mesh to remove fibers and coarse particles. Then, this powder was mixed with 10% gum acacia in an end runner for the purpose of binding. After proper addition of binding agent it was subjected to granular machine to convert in to granules. This product was then added with 1%–2% silicate of magnesium and starch before it was made into 500 mg tablets in tablet making machine. Placebo tablets were also prepared with wheat powder by following the same method.
Assessment
Before and after treatment total two assessments were carried out. A criterion of assessment was based on the scoring of International Index of Erectile Function (IIEF).[9] The IIEF is composed of 15 Items (Questions) categorized into 5 dimensions (Domains). The IIEF has been used in clinical trials of men with ED who had been in a stable relationship, so these men had opportunities to engage in sexual activity and sexual intercourse. The 15 Questions of IIEF asks about the erection problems one has had in their sex life over the last 4 weeks.
Statistical analysis
The information gathered on the basis of observations was subjected to statistical analysis in terms of mean difference, standard deviation, standard error, paired t test, and unpaired t test. The obtained results were interpreted as
Overall effect of therapy
Overall effect of therapy on 86 patients of Psychogenic Erectile Dysfunction was calculated by taking the Percentage of Relief based on the scores of IIEF and categorized into
Observations
Maximum number of patients, that is, 64% belong to 21–40 years of age, 43% were Graduates, 65.2% belong to Middle Class, 91.5% were Married, 47.3% of patients were having premature ejaculation as a comorbid condition, 33.6% of patients had chronicity up to 2 years, 80% of patients had recurrent inability to get erections, 74.7% were having inability to attain and maintain the erections, 81% of the patients were having interpersonal difficulties with their partners, 100% of patients had acquired subtype of ED, 89.4% were having situational subtype of ED, 96.8% of patients had ED due to psychological factors subtype. In 56.8% of patients precipitating factors were present and 72.6% of patients were having stressors and problems at work place.
In sexual history, 46.3% of patients were having the frequency of libido twice a week, 78% of patients were having frequency of sexual intercourse 1–2 times per week, 46.3% of patients reported their source of sexual knowledge as their friends, 96.8% of patients were having medium level of knowledge about sex, 67.3% of patients reported their duration of foreplay as less than 5 min, 53.6% of patients had duration of sexual intercourse in between 5–10 min, 88.42% of patients were uncircumcised, and 63.1% of patients were using condoms as a contraceptive measure.
In the present study, 48.42% of patients were having Vata Pitta Prakriti, 51.57% were having Rajasik Tamasika Prakriti, 52.63% of patients were having Avara Satva Sara, 53.68% were having Avara Satva and maximum number of the patients, that is, 53.49%, were coming under high severity of ED followed by moderate severity 38.37%.
Results
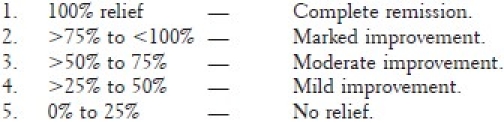
In the present study, in the Trial group (n=41), there was a statistically very significant improvement (P<0.01) was observed in IIEF-2, IIEF-9, and IIEF-12 with the percentage of relief being 12.29, 8.47, and 7.89, respectively. In all other items there was a statistically highly significant improvement (P<0.001) observed except IIEF-14, in which no change was found [Table 1].
Table 1.
Effect of therapy on International Index of Erectile Function in the trial group (n=41)
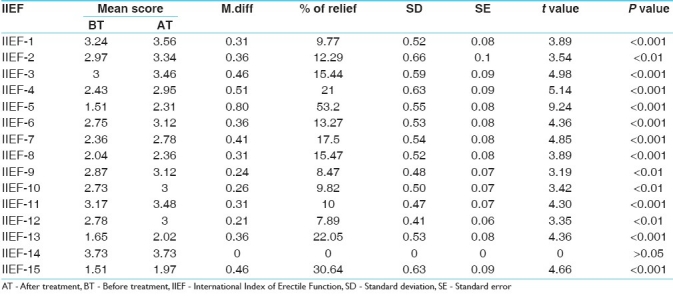
In the control group (n=45), there was a statistically very significant improvement (P<0.01) was observed in IIEF-9, IIEF-10, IIEF-12, and IIEF-13 with the percentage of relief being 8.94, 8.47, 6.29, and 17.85, respectively. In all other items there was a statistically highly significant improvement (P<0.001) observed except IIEF-14, in which there was no significant improvement (P>0.05) found [Table 2].
Table 2.
Effect of therapy on International Index of Erectile Function in control group (n=45)
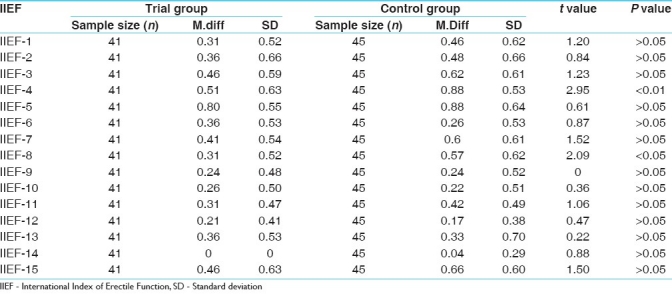
On comparing the effect of therapy on IIEF in between the two groups, there was no statistically significant difference was found in all of the items except IIEF-4 and IIEF-8. In IIEF-4 there was statistically significant (P<0.01) difference was found in between the two groups; In IIEF-8 significant difference (P<0.05) was found. In these two items, that is, IIEF-4 and IIEF-8, Control drug was found better than the Trial drug [Table 3].
Table 3.
Comparison of effect of therapy on International Index of Erectile Function
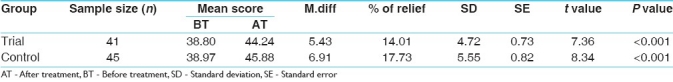
There was statistically highly significant improvement (P<0.001) observed in total score of the IIEF Scale in both the groups. In the Trial group (n = 41), 14.01% improvement was noticed (95% CI for difference of means 6.9-3.9), whereas in the control group (n = 45), 17.73% (95% CI for difference of means 8.5-5.2) of improvement was observed. On comparing the effect of therapy on total score of the IIEF Scale in between the two groups, it was found that there was no statistically significant difference (P.>0.05) [Table 4].
Table 4.
Effect of therapy on total score of International Index of Erectile Function
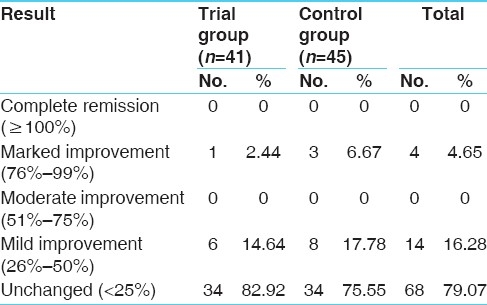
Overall effect of therapy
Effect of therapy on total score of International Index of Erectile Function is shown in Table 4. The overall effect of therapy on IIEF, in the Trial group, none of them got complete cure and moderate improvement, 14.64% showed mild improvement, 2.44% got marked improvement, whereas 82.9% were unchanged. In the control group 6.67% showed marked improvement, none of them got complete remission and moderate improvement, 17.78% got mild improvement, whereas 75.55% were unchanged. The overall maximum number of the patients, that is, 79.07% was coming under Unchanged or No relief category followed by 16.28% Mild improvement, 4.65% Marked improvement, none of them got Complete remission and Moderate improvement [Table 5].
Table 5.
Overall effect of the therapy based on International Index of Erectile Function
Discussion
Age
In the present study maximum number of the patients, that is, 64% were 21–40 years of age. The ratio of organic to psychogenic male sexual dysfunction has been reported to be directly proportional to age, 70% of men under 35 years of age having Psychogenic Erectile Dysfunction and 85% of men over 50 years of age having Organic Erectile Dysfunction.[10]
Education
An association between education and ED is not well established. Education has been shown to be inversely related to ED in some studies. Low level of education is also a marker of the high prevalence of nondiagnosed diseases.[11] In the present study 43% of the patients were graduates. This observation supports the inconsistent association between education and ED.
Socioeconomic status
Men with lower socioeconomic status tend to have lower sexual function. The effect of socioeconomic status on ED is partly mediated by life style factors and medical conditions. Low income is related to higher levels of stress.[12] In the present study 65.2% of the patients belong to middle class, which contains most of the patients in lower middle class. This observation of the present study supports the observations of the previous works.
Marital status
Some studies have reported that men who were unmarried have a low prevalence of ED than married men.[13] In the present study 91.5% of the patients were married. The present study supports the previous works.
Co-morbidity
Sexual dysfunctions, such as reduced libido, ejaculatory disturbances, such as premature ejaculation, reduced orgasmic sensation, and infertility, may accompany ED.[14] In the present study also 47.3% of the patients were having premature ejaculation as a co-morbid condition.
Subtype of erectile dysfunction
Psychogenic Erectile Dysfunction is characterized by sudden onset, situational inability to get erections, varying course, long history of psychosexual problems, and interpersonal difficulties with partner at onset of the disease.[15] In the present study also similar findings were observed, that is, 89.4% were having situational subtype and 96.8% of patients had ED due to psychological factors subtype, 80% of the patients having recurrent or situational inability to get erections, and 81% of the patients were having interpersonal difficulties with their partners.
Stressors and problems
In the concept of an adequate model of psychogenic ED, Hartmann proposed a model of psychogenic ED. According to this model a level of dispositional factors account for the specific vulnerability of the sexual response system to stress and the associated liability of erection.[16] In the present study 72.6% of the patients were having various stressors and problems at work place. These stressors may precipitate the erectile problems.
Sexual history
Inadequate sexual information, unreasonable expectations, demanding partner, little foreplay, psychosexual skills deficit, and sexual knowledge from improper source, and so on, were considered as causative factors in the manifestation of Psychogenic Erectile Dysfunction.[17] In the present study also similar observations were made, that is, 46.3% of the patients reported their source of sexual knowledge as their friends, 96.8% of the patients were having medium level of knowledge about sex, 67.3% of the patients reported their duration of foreplay as less than 5 min and 53.6% of the patients had duration of sexual intercourse in between 5 and 10 min.
Prakriti and Satva
In the present study, 48.42% of the patients were having Vata Pitta Prakriti, 51.57% were having Rajasik Tamasika Prakriti, and 53.68% were having Avara Satva. Similar observations were found in the studies conducted previously on sexual dysfunctions (54% Vata Pitta Prakriti, 72.2% Rajasika Prakriti, and 48.6% Avara Satva).[18] According to Ayurvedic classics, Vata and Pitta Prakriti individuals both are prone to be suffered with Alpa Shukra.[19] Avara Satva people are more prone to get various psychiatric diseases.[20]
Probable mode of action of Ashwagandha
Ashwagandha is proved anxiolytic, antidepressant, and antistress adaptogen. It was found effective in stress-induced sexual dysfunctions in rat models.[21] Ashwagandha produces gamma-aminobutyric acid (GABA)-like activity, which may account for the herb's antianxiety effects. GABA is an inhibitory neurotransmitter in the brain. Its function is to decrease neuron activity and inhibit nerve cells from over firing. This action produces a calming effect. Excessive neuronal activity can lead to restlessness and insomnia, but GABA inhibits the number of nerve cells that fire in the brain, and helps to induce sleep, uplift mood, and reduce anxiety.[22] The standardized extract of Ashwagandha was proved effective on the negative effects of stress; it increases energy, reduced fatigue, better sleep, enhanced sense of well-being, and reduction of cortisol levels up to 26%. Ashwagandha can address many of the health and psychological issues that plague today's society.[23] By considering these facts, Ashwagandha was selected as a Trial drug in the present study.
Probable mode of action of placebo
In the present study wheat powder was selected as placebo in control group. The placebo can be any clinical intervention, including words, gestures, pills, devices, and surgery. In clinical trials, substances or procedures that are designed to serve merely as control conditions may actually produce an effect on subjective or biomarker outcomes. These indirect effects of biologically inert substances or inactive procedures will be considered under the umbrella term placebo effects.
Placebo effects presumably have different mediators depending on the specific learned association and whether referring to acquisition of the association or the placebo response. The central nervous system is the primary location and mediator of the physiological basis of the placebo effects through its role in learning and memory and its outputs on sensory, motor, and autonomic pathways as well as the immune and endocrine systems. People have individual traits that predispose them to be more or less responsive to certain stimuli; the interaction between the learned associations of the clinical situation and the person's particular biology produces a response. The response could be a basic physiological process, such as modulation of sensory processing, release of neurotransmitters or alterations in hypothalamic–pituitary–adrenal axis or immune system activity. The placebo response could also be some more complex physiological process, including change in mood, change in motivation/effort, or cognitive set-shifting.
Many aspects of placebo effects, including verbal communication, interactions between person and health care provider, health care setting, practitioner characteristics, physical characteristics of a pill, type of treatment, and pill administration frequency. Additionally, anticipation or expectancy can refer to a response expectancy or self-efficacy expectancy, that is, one's sense of being able to achieve an outcome. Desire or motivation for improvement is another aspect of the placebo effect. These placebo effects are mediated through changes in neocortical and subcortical systems.[24]
Discussion on the effect of therapy
In Trial group (n=41), 53.2% relief was found (P<0.001) in the item IIEF-5 (difficulty to maintain the erections until completion of intercourse) and 30.64% relief was found (P<0.001) in IIEF-15 (confidence of getting and maintaining erections). In all other 13 items of IIEF, there was no relief (less than 25%) [Table 1].
In the control group (n=45), 37.73% of relief was found (P<0.001) in the item IIEF-4 (ability to maintain the erection after penetration), 58.82% of relief (P<0.001) in item IIEF-5 (difficulty to maintain the erections until completion of intercourse), 25.96% of relief (P<0.001) in the item IIEF-7 (satisfaction in sexual intercourse), 29.21% of relief was found (P<0.001) in the item IIEF-8 (enjoyment in sexual intercourse), and 39.47% of relief found (P<0.001) in the item IIEF-15 (confidence of getting and maintaining erections). In all other 10 items of IIEF, there was no relief (less than 25%) [Table 2].
Although both Trial drug and Control drug provided relief in IIEF-5 and IIEF-15, the difference between these two groups in IIEF-5 and IIEF-15 was statistically insignificant (P>0.05) [Table 3].
Based on the total score of IIEF, in Trial group 14.01% improvement was noticed, whereas in control group 17.73% of improvement was observed (P<0.001) [Table 4]. The difference between the two groups on total score of IIEF was statistically insignificant (P>0.05).
Overall effect of therapy
The overall effect of therapy on IIEF, in Trial group, 82.9% were unchanged and in the Control group, 75.55% were unchanged. Overall 79.07% of patients were coming under the unchanged or no relief category [Table 5].
Both Trial drug (Ashwagandha) and Control drug (Placebo) were proved ineffective in providing relief in Psychogenic Erectile Dysfunction.
The reasons for the negative results may be as follows:
Maximum number of the patients, that is, 53.49% were having a high severity of ED followed by moderate severity 38.37%.
Maximum number of patients, that is, 51.57% were having Rajasik Tamasika Prakriti and 53.68% were having Avara Satva.
In the present study, 81% of the patients were having interpersonal difficulties with their partners. To treat Psychogenic Erectile Dysfunction various techniques can be used, which decrease the anxiety associated with intercourse. The patient's partner can help with the techniques, which include gradual development of intimacy and stimulation.[25]
So, maximum number of patients having Rajasika tamasika Prakriti and Alpa Satva (having less Roga bala) with severe ED (having more Roga bala) without having the support from their partners didn’t get the sufficient relief in the present study.
Conclusion
Ashwagandha was not effective in the management of Psychogenic Erectile Dysfunction when compared with placebo.
References
- 1.Hatzimouratidis K, Amar E, Eardley I, Giuliano F, Hatzichristou D, Montorsi F, et al. Guidelines on male sexual dysfunction: Erectile dysfunction and premature ejaculation. Eur Urol. 2010;57:804–14. doi: 10.1016/j.eururo.2010.02.020. [DOI] [PubMed] [Google Scholar]
- 2.Rehman S. Erectile dysfunction: Prevalence, incidence and risk factors, Academic Dissertation. University of Tampere; 2004. [Google Scholar]
- 3.Diagnostic and Statistical Manual of Mental Disorders – Text Revision (DSM-IV-TR) 4th ed. New Delhi: Jaypee Publications; 2000. American Psychiatric Association; p. 545. [Google Scholar]
- 4.Acharya Vaidya Yadavji Trikamji , Acharya Kavyatirtha Narayan Ram. Susruta Samhita of Susruta with Nibandha Sangraha Commentary. 9-10. Vol. 26. Varanasi: Chaukhambha Orientalia; 2005. p. 497. Su.Chi. [Google Scholar]
- 5.Mirjalili MH, Moyano E, Bonfill M, Cusido RM, Palazon J. Steroidal lactones from Withania somnifera, an Ancient plant for Novel medicine. Molecules. 2009;14:2373–93. doi: 10.3390/molecules14072373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anonymous. Monograph on Popular and Effective Select Traditional Home Remedies. Department of Ayush, Ministry of Health and Family Welfare, New Delhi, In collaboration with WHO Country office for India. 2006-2007:30. [Google Scholar]
- 7.Diagnostic and Statistical Manual of Mental Disorders-Text Revision (DSM-IV-TR) 4th ed. New Delhi: Jaypee Publications; 2000. American Psychiatric Association; p. 547. [Google Scholar]
- 8.Randomization.com [homepage on the Internet]. 100 subjects randomized in to two blocks, to reproduce the plan use the seed 8200. [Last accessed on 2009 Jan 2]. Available from: http://www.randomization.com/
- 9.Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): A multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–30. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 10.Rehman S. Erectile dysfunction: Prevalence, incidence and risk factors, Academic Dissertation. University of Tampere; 2004. p. 20. [Google Scholar]
- 11.Rehman S. Erectile dysfunction: Prevalence, incidence and risk factors, Academic Dissertation. University of Tampere; 2004. p. 18. [Google Scholar]
- 12.Rehman S. Erectile dysfunction: Prevalence, incidence and risk factors, Academic Dissertation. University of Tampere; 2004. p. 19. [Google Scholar]
- 13.Rehman S. Erectile dysfunction: Prevalence, incidence and risk factors, Academic Dissertation. University of Tampere; 2004. p. 17. [Google Scholar]
- 14.Fabbri A, Aversa A, Isidori A. Erectile dysfunction: An overview. Hum Reprod Update. 1997;3:455–66. doi: 10.1093/humupd/3.5.455. [DOI] [PubMed] [Google Scholar]
- 15.Singh JC, Devasia A, Gnanaraj L, Chacko KN. Erectile dysfunction. Natl Med J India. 2005;18:139–43. [PubMed] [Google Scholar]
- 16.Stief CG. Is there a common pathophysiology of erectile dysfunction and how does this relate to new pharmacotherapies? Int J Impot Res. 2002;14(Suppl 1):S11–6. doi: 10.1038/sj.ijir.3900791. [DOI] [PubMed] [Google Scholar]
- 17.Borras-Valls JJ, Gonzalez-Correales R. Specific aspects of erectile dysfunction in sexology. Int J Impot Res. 2004;16(Suppl 2):S3–6. doi: 10.1038/sj.ijir.3901235. [DOI] [PubMed] [Google Scholar]
- 18.Bhatt NN. A Role of Manas in Klaibya (Male Sexual Dysfunctions) and its management, Department of Kayachikitsa, Institute of Post Graduate Teaching and Research in Ayurveda. Jamnagar: Gujarat Ayurved University; 2000. pp. 137–8. [Google Scholar]
- 19.Aacharya Vaidya Jadavaji Trikamji., editor. Charaka samhita, Vimana Sthana, Roga Bishagjitiyam Adhyaya. 2nd ed. 97-98. Vol. 8. Varanasi: Chaukhamba Surabharati Prakashan; 2008. Agnivesha, Charaka, Dridhabala; p. 277. [Google Scholar]
- 20.Aacharya Vaidya Jadavaji Trikamji., editor. Charaka samhita, Vimana Sthana, Roga Bishagjitiyam Adhyaya. 2nd ed. 119. Vol. 8. Varanasi: Chaukhamba Surabharati Prakashan; 2008. Agnivesha, Charaka, Dridhabala; p. 280. [Google Scholar]
- 21.Monograph. Withania somnifera. Altern Med Rev. 2004;9:211–4. [PubMed] [Google Scholar]
- 22.Mehta AK, Binkley P, Gandhi SS, Ticku MK. Pharmacological effects of Withania somnifera root extract on GABAA receptor complex. Indian J Med Res. 1991;94:312–5. [PubMed] [Google Scholar]
- 23.Kiefer D. Report, stress reduction, neural protection, and a lot more from an ancient herb. Life Extension Magazine. 2006:1–3. [Google Scholar]
- 24.Oken BS. Placebo effects: Clinical aspects and neurobiology. Brain. 2008;131:2812–23. doi: 10.1093/brain/awn116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Kidney and Urologic Disease Information Clearing house. Erectile Dysfunction. U.S. Department of Health and Human Services: NIH Publication. 2009:2–3. [Google Scholar]


