Abstract
Although cognitive-behavioral treatments for panic disorder have demonstrated efficacy, a considerable number of patients terminate treatment prematurely or remain symtpomatic. Cognitive and biobehavioral coping skills are taught to improve exposure therapy outcomes but evidence for an additive effect is largely lacking. Current methodologies used to study the augmenting effects of coping skills test the degree to which the delivery of coping skills enhances outcomes. However, they do not assess the degree to which acquisition of coping skills and their application during exposure therapy augment outcomes. We examine the extant evidence on the role of traditional coping skills in augmenting exposure for panic disorder, discuss the limitations of existing research, and offer recommendations for methodological advances.
Keywords: acceptance, cognitions, coping skills, exposure, mediation
Panic disorder with or without agoraphobia (PD/A) is a common emotional disorder with a lifetime prevalence estimate of approximately 4.7% in the United States (Kessler, Chiu, Demler, & Walters, 2005). It is associated with high levels of disability (Keller et al., 1994; Klerman, Weissman, Ouellette, Johnson, & Greenwald, 1991), considerable economic costs (Katon et al., 1990; Leon, Portera, & Weissman, 1995; Roy-Byrne et al., 1999), and high medical utilization (Deacon, Lickel, & Abramowitz, 2008).
The most empirically supported psychosocial treatment for PD/A is cognitive behavioral therapy (CBT), of which the central focus is repeated exposure to feared situations and sensations, supported by a set of control-based coping skills (see Craske & Barlow, 2008). These skills typically aim to change catastrophic appraisals and/or somatic symptoms. Patients are encouraged to apply the cognitive skills to control negative thoughts and somatic skills to control dysregulated physiology during exposure to feared sensations or situations. Although CBT for PD has clearly established itself as an effective treatment (Norton & Price, 2007; Westen & Morrison, 2001), effect sizes are smallest among the anxiety disorders (Andrews, Cuijpers, Craske, McEvoy, & Titov, 2010; Hofmann & Smits, 2008 but not Norton & Price, 2007). Also, a large percentage of completers are not panic free or do not reach responder status after treatment (Brown & Barlow, 1995). For example, in the largest randomized-controlled trial for PD to date (Barlow, Gorman, Shear, & Woods, 2000), only 32% assigned to CBT alone demonstrated strong treatment response 12 months after acute treatment. Together, these data indicate that there is room for improvement in PD/A treatment. Therapy optimization calls for a renewed focus on underlying mechanisms (i.e., why treatments work and for whom). The focus of this review is to examine the degree to which active ingredients of CBT (i.e., coping skill techniques) are implemented, augment exposure therapy, and mediate panic symptom reduction. To this end we (a) examine the extant evidence of the role of traditional coping skills in augmenting exposure, (b) discuss the limitations of existing research, and (c) offer recommendations for methodological advances. The latter will be discussed using examples of two emerging therapy approaches, acceptance and cognitive defusion, as employed in acceptance and commitment therapy (Hayes, Strosahl, & Wilson, 1999) and capnometry-assisted respiratory training (Meuret, Wilhelm, Ritz, & Roth, 2008).
Evidence for Additive Effects of Traditional Coping Skills
Coping skills traditionally included in CBT for PD/A are cognitive restructuring and either breathing retraining and/or relaxation. Presumably, the effects of exposure are augmented by applying the skills (e.g., disputing the probability of a harmful outcome while being exposed to a feared situation and showing that dysregulated physiology can be partially regulated). In the following, we review the evidence for the augmenting effects of traditionally taught cognitive and behavioral skills on exposure therapy in PD/A.
Cognitive skill training: description, efficacy, and evidence for augmenting exposure
Background
The cognitive theory of panic disorder (Clark, 1986) posits that panic attacks are caused by catastrophic beliefs about bodily sensations or situational contexts in which such sensations occur. In support, patients with PD/A have strong beliefs and fears of physical or mental harm arising from bodily sensations associated with panic attacks (e.g., Chambless, Caputo, Bright, & Gallagher, 1984; McNally & Lorenz, 1987). They are also more likely to interpret bodily sensations in a catastrophic fashion (Clark et al., 1988), and to allocate more attentional resources to physical sensations presented by words or heart rate feedback (e.g., Ehlers, Margraf, Davies, & Roth, 1988; Hope, Rapee, Heimberg, & Dombeck, 1990; Kroeze & van den Hout, 2000; Maidenberg, Chen, Craske, Bohn, & Bystritsky, 1996; McNally, Riemann, Louro, Lukach, & Kim, 1992). In addition, they are more likely to fear procedures that elicit panic sensations (Antony, Ledley, Liss, & Swinson, 2006; Blechert, Wilhelm, Meuret, Wilhelm, & Roth, 2010; Gorman et al., 1994; Jacob, Furman, Clark, & Durrant, 1992; Perna, Bertani, Arancio, Ronchi, & Bellodi, 1995; Rapee, 1986).
Skill Training
Cognitive skill training (CT) is aimed at recognizing cognitive errors and generating alternative, noncatastrophic explanations for the sensations that are feared during panic attacks. A rationale emphasizing the role of appraisals is followed by consideration of the evidence and logical empiricism to generate more evidence-based appraisals for recent and anticipated panic attacks and contexts that produce panic symptoms. During exposure, patients are encouraged to evaluate the degree to which elicited panic symptoms (via interoceptive or in vivo exposure) are indeed predictive of catastrophic outcome. Whereas bodily sensations are often cited as triggers of panic attacks, according to Clark (1986) and McNally (1994), treatment success depends on the correction of the catastrophic interpretation of these sensations, not the sensations themselves. The extent to which biological factors that may elicit or sustain panic symptoms are without harm to the system remains unknown. As such, claims in either direction (harmful or nonharmful) presently lack an empirical basis.
Evidence for Efficacy From Clinical Trials
CT is often intermingled with behavioral techniques (e.g., “behavioral experiments,” “hypothesis testing,” “instructions” involving exposure), which complicate the direct testing of efficacy of CT in its “pure” form (e.g., Hoffart, Sexton, Hedley, & Martinsen, 2008; Hofmann et al., 2007; Öst, Westling, & Hellström, 1993; Teachman, Marker, & Smith-Janik, 2008). Nonetheless, there is some evidence that training in cognitive procedures in full isolation from exposure and behavioral procedures is efficacious in reducing aspects of panic (Beck, Stanley, Baldwin, Deagle, & Averill, 1994; Meuret, Rosenfield, Seidel, Bhaskara, & Hofmann, 2010; Salkovskis, Clark, & Hackmann, 1991; Van den Hout, Arntz, & Hoekstra, 1994). Similarly, in a study by Bouchard et al. (1996), exposure therapy was as effective in reducing panic symptoms as cognitive restructuring. In comparison to in vivo exposure, some studies have shown that CT alone was less effective for agoraphobia (Williams & Falbo, 1996). Hoffart (1995) found that CT targeting misappraisals of bodily sensations was as effective as guided mastery exposure delivered intensively over 6 weeks for individuals with moderate to severe agoraphobia, although some elements of exposure (e.g., hyperventilation tests to elicit sensations) were included in the CT condition.
Evidence for an Exposure-Augmenting Effect
A few studies have evaluated the effects of CT combined with exposure in comparison to exposure alone or in combination with other coping skills. Most often, CT plus exposure does not yield an additional benefit over exposure in vivo alone (Öst, Thulin, & Ramnero, 2004; van den Hout et al., 1994). One exception was a study by Murphy, Michelson, Marchione, Marchione, and Testa (1998), in which those receiving CT + graded exposure outperformed those receiving graded exposure alone or graded exposure + relaxation training. Furthermore, a recent meta-analysis, albeit across different anxiety disorders, indicated no differences across CT, exposure therapy, or their combination (Norton & Price, 2007). In the only published study to date that has experimentally evaluated initial training in CT followed by in vivo exposure, van den Hout and colleagues randomized clients with moderate to severe agoraphobia to four sessions of CT or attention control followed by eight sessions of exposure therapy. Initial CT resulted in reductions in panic frequency, but not avoidance behavior or other panic-related symptoms. The latter were only reduced with the addition of exposure. Attention control did not change panic symptoms or avoidance, but after adding exposure, avoidance behavior was reduced to the same extent as the CT condition. No differences were observed between CT + exposure or attention control plus exposure during the exposure phase in panic symptoms (behavioral and self-report measures). Hence, CT did not potentiate exposure effects in this study.
Taken together, the extant data indicates that the delivery of CT alone is partially effective for PD/A, but there is little evidence suggesting CT augments the effects of exposure alone. As discussed earlier, the lack of data on successful acquisition and application of cognitive skills renders premature any conclusions regarding their augmenting effect upon exposure. Thus, we can currently conclude that delivery of CT as a part of an exposure-based treatment for PD/A does not confer significantly greater benefit, but conclusions regarding the degree to which actual use of CT during exposure enhances outcome remains unknown.
Breathing training: description, efficacy, and evidence for augmenting exposure
Background
Respiratory abnormalities have been postulated as an important factor in the development or maintenance of PD/A (Gorman et al., 1988; Klein, 1993; see Meuret & Ritz, 2010, for a review) and has led to speculations about a causal relationship between respiratory regulation, in particular PCO2 and panic. According to Ley (1985) panic attacks are caused by acute states of hypocapnia, which may not be limited to the attack itself, but may precede and follow it, giving rise to moderate sustained hypocapnia. Hyperventilation according to Klein is viewed as a compensatory or secondary reaction to an overly sensitive “suffocation alarm system” in these patients. When a patient's PCO2 rises, the system starts firing at an abnormally low threshold and/or responds with greater sensitivity to increments in CO2. This leads to disproportional dyspnea (sensations of air hunger, breathlessness, suffocation), which due to its distressing nature initiates a cascade of panic symptoms. In this context, chronic hyperventilation is interpreted as an adaptation to a lowered suffocation alarm threshold, in that it keeps PCO2 sufficiently low to avoid triggering the suffocation alarm. Evidence for both postulations has been found in a recent ambulatory study tracing cardio respiratory changes in the hour before out-of-the-blue attacks (Meuret et al., in press) and decades of experimental studies (Blechert et al., 2010; Caldirola, Bellodi, Caumo, Migliarese, & Perna, 2004; Dager et al., 1995; Gorman, Martinez, Coplan, Kent, & Kleber, 2004; Gorman et al., 1988; Wilhelm, Gerlach, & Roth, 2001). Consistently, breathing training (BRT), with the purpose of modifying pathogenic breathing, is part of many CBT packages for PD/A (Barlow, Craske, Cerny, & Klosko, 1989; Telch et al., 1993).
Skill Training
The rationale of BRT assumes a central role for hypocapnia in panic symptom production (Ley, 1985), postulating a positive feedback loop between increasing anxiety and increasing hyperventilation. Amelioration of panic symptoms is expected when patients achieve reductions in transient and sustained hypocapnia. The descriptions of the therapeutic strategies and outcomes for BRT are sparse and mixed (see Meuret, Wilhelm, Ritz, & Roth, 2003, for a review). Most manuals and studies describe instructions in abdominal breathing as their central techniques. Other techniques include pacing aids (e.g., recorded audio tones) or breathe counting. Furthermore, target respiratory rates as well as duration and frequency of between-session exercises vary largely across studies. Most surprisingly, the central tenet of BRT, the correction of hypocapnic breathing, is neither measured nor targeted in traditional BRT. Given the lack of such data, bold claims such as, “There is no evidence that breathing therapy works by normalizing pCO2” (Bass, 1997, p. 425) technically are accurate.
Evidence for Efficacy From Clinical Trials
Traditional BRT has rarely been tested in isolation but is intermingled with either cognitive (de Beurs, van Balkom, Lange, Koele, & van Dyck, 1995; de Ruiter, Rijken, Garssen, & Kraaimaat, 1989) or behavioral (de Beurs, Lange, van Dyck, & Koele, 1995) techniques.1 There are only three studies that have tested the effects of traditional BRT in isolation (Clark, Salkovskis, & Chalkley, 1985; Rapee, 1985; Salkovskis, Jones, & Clark, 1986), all of which indicate decreases in panic symptom severity, but also all lack control comparison groups. In-session PCO2 was assessed in only one study (Salkovskis et al., 1986) with evidence of normalization from initial hypocapnic to normocapnic levels at posttreatment.
Evidence for Exposure-Augmenting Effects
Only two controlled studies tested the additive effects of BRT upon exposure. In the study by Hibbert and Chan (1989), PD/A patients were randomly assigned to receive either 2 weeks of BRT or supportive therapy followed by 3 weeks of in vivo exposure. The interventions were equally effective in the first 2-week phase, but BRT yielded greater improvement in clinician (but not self-report) ratings than supportive therapy following the additional exposure training. Bonn, Redhead, and Timmons (1984) alternately allocated patients with agoraphobia to receive either two sessions of BRT followed by 7 weekly sessions of in vivo exposure or in vivo exposure alone for 9 weeks. While BRT plus exposure was equally effective as exposure alone at posttreatment, BRT plus exposure yielded superior outcome 6 months later. Other studies have attempted to identify the degree to which BRT exerts an effect as part of a multicomponent exposure-based protocol using comparative and dismantling designs. For instance, Craske, Rowe, Lewin, and Noriega-Dimitri (1997) compared CT + interoceptive exposure (IE) + in vivo exposure to CT + BRT + in vivo exposure. Group differences at posttreatment suggested that treatments were equally effective on most of the 27 measures related to anxiety and distress, such as panic apprehension, panic fear and avoidance, agoraphobic fear and avoidance, and general distress. A dismantling study by Schmidt and colleagues (2000) examined the differential efficacy of group CBT +/− breathing retraining. No significant condition differences were found, thus questioning the additional additive benefit of BRT to CBT. Although these studies provide an important foundation for studying the additive effect of coping skills, such as BRT, the use of multicomponent treatment protocols for both groups, as well as the lack of outcome assessment after the delivery of each component and/or assessment regarding the degree to which the coping skills are used, limits our ability to fully assess the contribution of BRT over and above other components. As noted by White and Barlow (2002), “An important limitation of this study [Schmidt et al., 2000], however, is the lack of assessment of each patient's true use of each treatment component […] Such evaluation would benefit from a thorough assessment that identifies what treatment techniques were used or not used by patients […]” (p. 371).
Taken together, BRT has been rarely tested in isolation from other therapeutic strategies in the treatment of PD/A, and studies examining the potentiation of BRT upon exposure are limited and yield mixed results. Most problematically, it remains unknown whether traditional BRT actually reverses hypocapnic breathing relative to control conditions.
Relaxation skill training: description, efficacy, and evidence for augmenting exposure
Because traditional relaxation is used less often in recent approaches to treating PD/A, this section will only briefly review the historical significance of this coping skill in the treatment of PD/A, and the research contributions that have furthered our understanding of this technique.
Background
Progressive muscle relaxation (PMR) was first described by Jacobson (1934) and derived from his theory that negative emotional states were caused by “neuromuscular hypertension” (Jacobson, 1938). PMR was later implemented in behavior therapy by Wolpe (1958), who trained patients in this relaxation strategy as part of systematic desensitization. In his protocol, the primary goal was to use relaxation as an antagonistic response to anxiety that would reciprocally inhibit anxiety and eventually become a conditioned inhibitor. Later, Bernstein and Borkovec (1973) formalized and standardized PMR training. PMR as a training for PD/A was typically taught to reduce general tension to achieve a body state that lowers the risk for stressors to elicit panic.
Skill Training
In the most widely studied approach to PMR (Bernstein & Borkovec, 1973), patients learn to tense and relax a series of muscle groups (starting with 16), and gradually reduce the number of muscle groups (typically from 8 to 4). Patients are taught to (a) focus their attention on a specific muscle group, (b) tense that muscle group, (c) maintain the muscle contraction for 5 to 7 seconds, (d) then relax the muscle group upon cue for 20 seconds, and (e) focus on the feelings and sensations of relaxation in the muscle group.
Evidence for Efficacy From Clinical Trials
Evidence for the efficacy of PMR for PD/A is sparse and mixed, which is perhaps why it is infrequently used as a treatment component in modern CBT approaches to PD/A. One study (Marks et al., 1993) compared (a) alprazolam + in vivo exposure (combined treatment), (b) alprazolam + PMR (used as a psychological placebo), (c) pill placebo + in vivo exposure, and (d) pill placebo + PMR (double placebo). All four treatment conditions showed improvement in panic measures, with no differences between them on most panic symptom measures during treatment or throughout the follow-up period. However, percentages of those classified as “much/very much improved” on the Clinical Global Improvement Scale (CGI) at follow-up were lower for PMR + placebo (25%) compared to the other groups (51% for alprazolam + PMR, 71% for alprazolam + exposure, and 71% for placebo + exposure). Thus, PMR (plus placebo) fared less well than the other conditions when using clinician measures. In another study, Öst (1988) found that PMR alone resulted in large reductions of panic symptom severity, although it was less effective than the combination of PMR + interoceptive exposure (i.e., applied relaxation).
Evidence for Exposure-Augmenting Effects
The majority of PMR study designs do not test augmenting effects due to the intermingling effect of additional components. For example, in the study by Öst and Westling (1995), the authors examined the efficacy of applied relaxation (i.e., PMR + in vivo exposure) and CBT (which included “behavioral experiments”). The contribution of either technique over and above exposure only cannot be tested with such design because the inclusion of some exposure strategies prevents the parsing out of components and comparing their effects directly. In another study, Öst and colleagues (1993) assessed differential outcome among three coping skill trainings for patients with PD/A: applied relaxation (AR), in vivo exposure, and CT. Again, CT was intermingled with exposure elements, whereas the in vivo exposure “only” training appeared to be confounded by “instructions for coping with panic during exposure” (p. 387), thus impeding comparative testing. Nonetheless, the results indicated very few differences between in vivo exposure and AR on panic-related measures. On a behavioral measure of fear, AR outperformed CT, whereas in vivo exposure alone did not, suggesting that AR may have augmented exposure to some degree. Other studies have evaluated the effects of applied PMR (i.e., training in PMR combined with instructions to use PMR during in vivo exposure) for PD/A (e.g., Barlow et al., 1989; Milrod et al., 2007), but did not evaluate the additive effects of PMR to in vivo exposure.
Finally, earlier studies (albeit none specifically examining PD/A samples) that compared graduated imaginal exposure with versus without the addition of PMR generally found no differences between the two conditions (e.g., Dawson & McMurray, 1978; Waters, McDonald, & Koresko, 1972; Yates, 1975; see Kazdin & Wilcoxon, 1976; McGlynn, Solomon, & Barrios, 1979, for reviews). These studies provided the basis for abandoning Wolpe's (1958) systematic desensitization approach in favor of more fear-activating approaches to exposure.
In sum, studies that directly test the efficacy of PMR in augmenting are largely absent from the literature. Thus, the degree to which acquisition of PMR skills and their application during exposure therapy augment exposure therapy remains unknown.
Shortcomings in current coping skill research
In light of the reviewed studies, one may conclude that traditional coping skills either bear no augmenting effect over exposure or their effects upon exposure are unknown in the treatment for PD/A. Constructive, dismantling, and component analysis designs have made important contributions to a preliminary understanding of what treatment components are most and least efficacious in the treatment of PD/A. However, despite their strengths, these studies, which typically fail to show that coping skills augment exposure, are limited not only in number, but in the conclusions that can be drawn using these methodologies. Specifically, the methodologies used to study the augmenting effects of coping skills test the degree to which the delivery of coping skills enhances outcomes; they have not assessed the differential degree to which acquisition of coping skills, and/or their application during exposure therapy enhance outcomes. The extant reliance on the delivery of coping skills training detracts from important questions about the degree to which acquisition and application takes place and the validity of their proposed mechanisms.
To advance our understanding on the potent contributors of change in CBT, there is a need for methodological designs that fully evaluate the role of coping skills training above and beyond the effects of exposure therapy alone. Furthermore, successful delivery of coping skills does not guarantee that the recipient successfully acquires and applies the skills. That is, unless we evaluate the degree to which a skill is actually learned and correctly applied during exposure, it is premature to draw conclusions about its potency. Proper testing of augmenting effects warrants a multiphase approach in which a particular skill is first acquired and then tested in the context of exposure therapy. Only if the skill training is administered in a “pure” format (i.e., not mixed with other skill trainings) can the unique contribution of this skill to exposure be determined. Additionally, the combined treatment needs to be contrasted with an “exposure only” treatment, ideally with a preceding placebo to account for time. Up to this point we have reviewed the additive effect of coping skills to exposure (i.e., improved efficacy), which is only part of the question when looking at augmenting effects. Mediational analyses allow us to look at the relationship between changes in psychological constructs of interest (such as catastrophic misinterpretations) and outcomes.
Exploring Mechanism of Therapy Success in PD
Kazdin (2007) cogently outlined the importance of mechanism research, including the potential to optimize the way in which treatment is delivered and thereby enhance outcomes. However, despite the invocation for mechanism research, less than a handful of psychosocial intervention studies have tested mediation properly. In the following we examine the meditational evidence for traditional coping skills in PD.
Mechanistic evidence for cognitive reappraisal strategies
Cognitive strategies are assumed to facilitate exposure by the development of explicit nonthreat appraisals about the mental, physical, or social consequences of panic attacks and related sensations, which in turn encourage approach behavior and lessen distress (e.g., Craske & Barlow, 2008). Thus, both the purported mediator and skill in CT is the ability to reappraise previously feared bodily sensations as nonthreatening.
Most studies of mediation of CT for PD/A merely measure change in purported mediators (i.e., reappraisal) as well as outcomes (i.e., panic symptom reduction) across the same interval of time, from pre- to posttreatment (e.g., Hofmann et al., 2007; Meulenbeek, Spinhoven, Smit, van Balkom, & Cuijpers, 2010; Smits, Powers, Cho, & Telch, 2004; Vögele et al., 2010) or without complete mediation models of analysis (e.g., Clark et al., 1994, 1999; Forman, Herbert, Moitra, Yeomans, & Geller, 2007; Schmidt & Bates, 2003). Among the few studies fulfilling the criteria for mediational analyses is one by Bouchard and colleagues (2007), who found that changes in daily ratings of beliefs about panic preceded and were associated with changes in apprehension about future panic attacks. In another study by Hoffart et al. (2008), fear of bodily sensations influenced catastrophic beliefs, which in turn influenced avoidant behavior. A reduction in the latter decreased the fear of bodily sensations. Finally, evidence for modality-specific pathways was supported in a recent study by Meuret, Rosenfield, et al. (2010). In patients assigned to 4 weeks of exclusive training in cognitive skills, reductions in symptom appraisal mediated improvements in perceived control and panic symptom severity, and vice versa.
These studies, however, relied upon retrospective self-report measures of thoughts and beliefs, which are likely to be confounded by responder biases and demand characteristics, and unlikely to match ongoing, moment-to-moment cognition (Jarrett, Vittengl, Doyle, & Clark, 2007). Additionally, measures such as the Anxiety Sensitivity Index (ASI; Reiss, Peterson, Gursky, & McNally, 1986) capture dispositional characteristics, but not occurrent responding (Fridhandler, 1986). For instance, a person scoring high on the ASI is likely to respond fearfully to bodily sensations and is more likely to catastrophize about them. Notwithstanding, the ASI does not lend evidence to whether such thoughts and feelings are actually occurring in real time. Here, further research on approaches such as the think-aloud paradigm (Davison, Vogel, & Coffman, 1997; Davison, Williams, Nezami, Bice, & DeQuattro, 1991; Williams, Kinney, Harap, & Liebmann, 1997) will allow testing of symptom appraisal in real time. An example for capturing “in-the-moment” appraisals during cognitive skill training and exposure, using the think-aloud technique, is described below (see “Think-Aloud Paradigm”).
Mechanistic evidence for breathing and relaxation strategies
PMR and BRT are presumed to decrease anxiety by reducing heightened physiological arousal observed in PD/A. Specifically, the purported mediator for BRT is PCO2, which serves as an index of the degree of hyperventilation. The commonly used coping skill is slow, deep, and/or abdominal breathing with the purpose of restoring normal levels of PCO2. For PMR, the purported mediator is muscle tonus, and the coping skill is to “physically relax” with the purpose of restoring a “normal” level of muscle tension. These strategies are assumed to facilitate exposure by physical correction of hyperventilation or muscle tension/autonomic arousal that subsequently attenuate disturbing sensations, thereby encouraging further approach behavior and less distress. Given that the proposed mediators for PMR and BRT are physiological indices, they are subject to objective and direct assessment. However, with the exception of one uncontrolled study (Salkovskis et al., 1986), PCO2 has not been assessed in traditional BRT. In addition to speculations of BRT acting as an impediment to treatment success by inhibiting necessary arousal to facilitate learning during exposure (Craske et al., 1997; Schmidt et al., 2000), experimental research suggests an actual hyperventilation-enhancing effect from traditional breathing techniques. That is, the slowing of respiratory rate, one of the core techniques of traditional BRT, can lead to compensatory deeper breathing that perpetuates/exacerbates hyperventilation in persons with PD/A (Conrad et al., 2007; Ley, 1991; Meuret et al., 2003, 2008). Compensatory overventilation is likely attributable to an exaggerated perception of sensations of “air hunger” (i.e., dyspnea) in patients with PD/A (Klein, 1993).
The few studies that have assessed physiological activity as an outcome measure in PMR generally have not found support for the association between decreased physiological arousal and improvement on psychological outcome measures for PD/A (Beck et al., 1994) or chronic anxiety (Leboeuf & Lodge, 1980). Furthermore, although some studies have found PMR to result in decreased physiological arousal, these decreases are not unique to those treated with PMR. For example, Michelson et al. (1990) observed heart rate decrements after both PMR and in vivo exposure for the treatment of agoraphobia, with no differences between the two treatments. The only studies that have actually evaluated muscle tonus throughout exposure therapy utilized imaginal exposure. In those cases, PMR was associated with increased rather than reduced autonomic arousal (Borkovec & Sides, 1979; Levin & Gross, 1985). However, these studies were not conducted in samples with PD/A, and none of the above studies met criteria for proper meditational testing. Taken together, research elucidating the presumed physiological mediators driving symptom reduction is greatly lacking.
In summary, direct evaluation of the degree to which coping skills are acquired and the degree to which they are applied when confronted with feared situations or sensations, or the degree to which such acquisition and application mediate outcomes from exposure therapy is lacking. Furthermore, there are very few studies in which purported mediators are fully assessed. Consequently, extant data may misrepresent the impact of coping skills in the treatment of PD/A, because outcomes from exposure therapy may indeed be augmented as a function of degree of acquisition and/or application of coping skills. Such measurement would permit evaluation of not only the ‘”augmentation potential”’ of coping skills, but also a thorough evaluation of the degree to which individual differences moderate skill acquisition and application, and thereby outcomes. In the following, we introduce strategies aimed at addressing the above-discussed methodological shortcomings.
Future Directions in the Implementation, Assessment, and Evaluation of Current and Novel Coping Skills in Augmenting Exposure
There is a pressing need for both objective and online measurement of purported mediators, and evaluation of the degree to which change in those indices are predictive of change in subsequent symptom outcomes. Below we illustrate the implementation of online assessments using examples of two recently developed therapeutic approaches. The first exemplifies the direct manipulation and assessment of dysfunctional respiration, and the second illustrates a novel approach of assessing online thought processes.
Capnometry-assisted respiratory training: description, efficacy, and evidence for augmenting exposure
Background and Description
In contrast to traditional BRT, capnometry-assisted respiratory training (CART) targets respiratory dysregulation, in particular hypocapnia (Meuret et al., 2008; Meuret, Rosenfield, et al., 2010). CART is a brief, 4-week training that uses immediate feedback of end-tidal PCO2 to teach patients how to raise their subnormal levels of PCO2 (hyperventilation) and thereby gain control over dysfunctional respiratory patterns and associated panic symptoms (e.g., shortness of breath, dizziness). In this respect, CART substantially differs from traditional BRT because it focuses directly on the proposed mediator, PCO2 (see Meuret et al., 2003, for a review). Most importantly for the current review, CART takes advantage of novel technologies that allow the precise assessment and monitoring of core respiratory variables. The device, a portable capnometer, offers breath-by-breath feedback of expired carbon dioxide and rate of breathing (both measured via a nasal canula). Compliance and skill acquisition and application can be assessed by means of electronic data storage. Between-session data are downloaded during the treatment session and presented and discussed with patients. This allows for a unique way to determine whether patients are willing and able to adapt new skills.
Evidence for Efficacy From Clinical Trials
Due to the novelty of CART, randomized controlled trials are limited but promising. In a first randomized controlled study, Meuret and colleagues (2008) tested the efficacy of 4 weeks of CART (n = 20) compared to a delayed wait-list (WL) control group (WL, n = 17). CART, but not WL, led to sustained increases in PCO2 levels and reduced panic severity and frequency. Reductions in panic symptom severity (PDSS; Shear et al., 1997) were comparable to standard CBT and improvements were maintained at 12-month follow-up. In a second study, patients with PD/A were randomly assigned to receive either 4 weeks of CART (n = 21) or CT (n = 20). An initial 4 weeks of skills training was followed by three sessions of in vivo exposure and a fourth session at a 2-month follow-up. Respective skill acquisition trainings led to significant and comparable reductions in panic symptom severity and panic-related cognitions, regardless of modality. However, only CART, but not CT, led to a correction of hypocapnic levels of PCO2 (Meuret, Rosenfield, et al., 2010). Similarly, although improvements in panic severity across exposure sessions were large and independent of previously acquired coping skills, normalization in PCO2 was only observed for patients undergoing prior training CART, but not CT (Seidel, Rosenfield, Bhaskara, Hofmann, & Meuret, 2009). Also, PD/A patients (Meuret et al., 2008) and patients with asthma in another capnometry-assisted study (Meuret, Rosenfield, Hofmann, Suvak, & Roth, 2009) demonstrated high compliance with the assigned 17-min, twice-daily homework exercises. The compliance also moderated improvement in panic symptom reduction (Meuret, Hofmann, & Rosenfield, 2010).
Mechanistic Evidence for CART
Like traditional BRT, PCO2 is presumed to be the primary mediator of CART. Preliminary evidence for this thesis comes from longitudinal mediation analyses indicating that changes in PCO2, measured continuously during between-session exercises, indeed mediated and preceded changes in fear of bodily sensations (Meuret et al., 2009) and cognitive reappraisal of symptoms and perceived control (Meuret et al., 2010) in CART but not CT. Although significantly reduced, reductions in rate of breathing neither mediated reductions in panic fear of bodily sensations (Meuret et al., 2009) nor panic symptom severity or cognitions (including perceived control) (Meuret et al., 2010). Mediation analysis examining changes during exposure showed bidirectional relations for cardiorespiratory changes mediating changes in physical symptom and for cardiac changes mediating changes in cognitive symptoms (Seidel et al., 2009); these pathways were significant and consistent across all exposure sessions. As expected, levels of PCO2 during exposure were significantly greater in CART compared to CT (Seidel et al., 2009).
These findings strengthen the idea that panic symptom reduction can be achieved through different mechanisms. However, an evaluation of the degree to which CART augments exposure therapy (relative to exposure therapy alone) a waits testing. Most importantly, the measurement of changes in PCO2 provides direct, ongoing measurement of purported mechanisms that permits evaluation of the degree to which CART skills are acquired and then applied during in vivo exposure, and the degree to which such acquisition and application mediate symptom outcomes.
Assessment of Cognitive Appraisal/Acceptance Skills: Think-Aloud Paradigm
In a recent pilot study, we tested the feasibility of a modified and extended version of the think-aloud paradigm (Davison et al., 1991, 1997; Williams et al., 1997). The paradigm is aimed at assessing concurrent, situation-specific, and participant representative thoughts both during skill acquisition and application. This online method of recording verbalizations provides a sample of thinking that differs from the constraints of forced-choice formats and retrospective judgments (e.g., questionnaires), and appears to be less susceptible to responder biases inherent to retrospective judgments. Think-aloud methodologies have been used to evaluate thoughts during experimental exposure to feared situations (Williams et al., 1997) and are considered valid indicators of covert verbalizations when derived from instructions to “say in a continuous stream whatever one is saying to oneself at that moment” (vs. report upon what one thinks one has been saying over a past interval) and limited to brief snippets of time.
The clinical application was tested in a small sample of patients undergoing a brief training in acceptance therapy (Hayes et al., 1999; Segal, Williams, & Teasdale, 2002) followed by six sessions of exposure (Meuret, Twohig, Rosenfield, Hayes, & Craske, submitted for publication). Acceptance-based skill training differs to traditional coping skill training as the emphasis is not on control (e.g., of physiology or thoughts) but rather the acceptance of panic-related sensations and cognitions as they occur from moment to moment. Patients are asked to pay nonjudgmental attention to thoughts, feelings, images, and bodily sensations and learn to see thoughts as an ongoing process distinct from self rather than an event with literal meaning (cognitive defusion). Empirical evidence for the efficacy of acceptance approaches for PD/A has been demonstrated (e.g., Forman et al., 2007; Levitt, Brown, Orsillo, & Barlow, 2004); however, as with cognitive and behaviorally based treatments, both acquisition/application and mechanistic validation of acceptance skills is lacking.
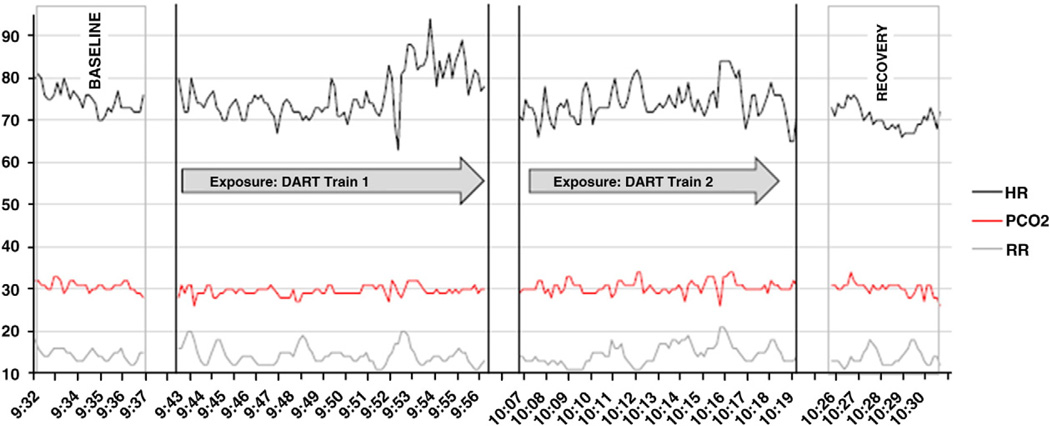
During the first 4 weeks of training, patients were asked to practice willingness to experience internal sensations and apply these techniques using audio-guided exercises. During the twice-daily 15-min between-session exercises, patients recorded whatever was on their mind at prompted, 30-sec intervals (minute: 3, 7, 11), using a digital voice recorder. Recordings, with date and time stamps, were downloaded during the sessions and discussed with the therapist. Think-aloud samples were also recorded, in addition to cardiorespiratory physiology (see Figure 1) during exposures with the instruction to verbalize whatever they were saying to themselves in a continuous stream using a digital voice recorder. The results of this feasibility trial were promising and indicated high compliance with homework exercises and significant improvements in symptom appraisal, mindfulness, and panic symptom severity. The think-aloud paradigm provided valuable data regarding the degree to which patients acquired and applied acceptance-based skills. Notably, the think-aloud paradigm would be equally suitable for cognitive coping skills. In the following, we provide sample data for the physiological and “think-aloud” recordings collected during this pilot trial.
FIGURE 1.
Ambulatory data of heart rate (HR), end-tidal PCO2, and respiration rate (RR) during real-life exposure. Measurement interruptions indicate periods of physical activity.
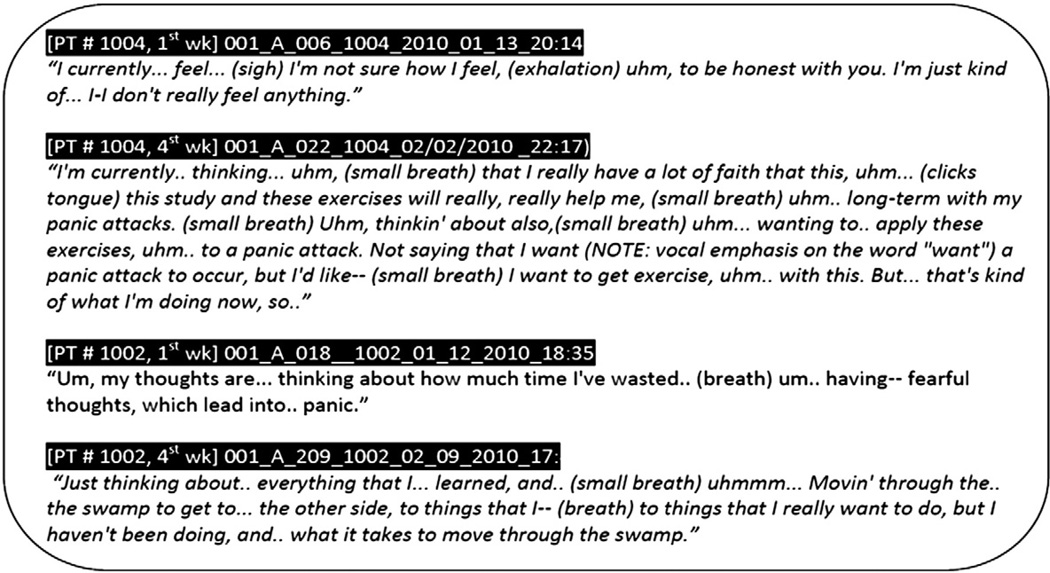
Examples for ongoing recording during skills training and during in vivo eexposure
Overall, patients were very receptive to and compliant with the recording devices for their physiology and their verbalizations. Figure 2 illustrates extracts from the prompted verbalizations during the first 4 weeks of acceptance skills training. Data of this type offers much needed insight into the acquisition and application of coping skills and warrants proper meditational testing. Patient 1 offered some dialogue of increased willingness to experience panic sensations and interest in practicing acceptance while having a panic attack. Patient 2 showed a greater grasp of acceptance as taught in this pilot study. These examples illustrate variation in acceptance skills acquisition (at least as verbalized) across patients. Data such as these will be informative for testing the degree to which coping skills acquisition and subsequent application during exposure actually mediate outcomes. Furthermore, they will permit evaluation of which individual difference variables moderate acceptance skill acquisition, and eventual treatment outcomes.
FIGURE 2.
Sample transcripts from “think-aloud” recordings during the first and last weeks of acceptance skill training.
Conclusion
Empirical support for an augmenting effect of traditional coping skills (cognitive and biobehavioral) on exposure is lacking. However, the extant reliance on delivery of coping skills detracts from examining the degree to which acquisition of coping skills and their application during exposure therapy enhance outcomes. At present, implementation of appraisal techniques (as taught in CT) are largely assessed retrospectively; likewise the assessment of core physiological processes (i.e., PCO2 in BRT and muscle tonus in PMR) both during skill training (i.e., between-session exercises) and application (i.e., exposure) is lacking. Furthermore, concurrent testing of various coping skills clouds the testing of their additive effect on exposure. Thus, it is premature to draw conclusions as to whether they augment exposure alone because it remains unclear whether patients learn and apply the taught skills.
In this review, we advocate improved methodologies for examination of augmenting effects of coping skills. In particular, multiphase intervention designs are warranted, in which skill acquisition training precedes exposure, in order to dissect both the potency of the skill training and its contribution to exposure. Additionally, we posit mediational testing to ascertain that the skill in question indeed exerts its effect by means of its proposed mechanism. We have outlined recently developed methodologies and preliminary evidence for objective, online measurements of cognitive (i.e., think-aloud technique) and physiological processes (i.e., therapeutic capnography) to warrant proper assessment of their mechanism and efficacy testing. Understanding how these strategies work will allow researchers to develop more potent and efficacious treatment protocols for PD/A and will inform practicing clinicians about which coping skill will be most effective for which patient, and thereby improve treatment outcomes.
The findings from this review also offer clinical and applied suggestions. The general cognitive-behavioral treatment package is well supported in the treatment of PD/A, and is considered the first-line psychosocial treatment for PD/A. The choice to focus on cognitive distortions, ineffective breathing patterns, or neither could very reasonably be based on the presentation of the patient. Whatever choice the therapist and patient make, it is also suggested that some method to track the psychological process of change, in addition to outcomes, be utilized. This review suggests that these augmentation techniques are trained, but that their adoption and implementation are generally not tracked. It would behoove therapists to dually focus on what is being learned in the exposure exercises in addition to the outcomes that are being achieved. This can be accomplished with standardized measures, biomedical technology, or by using think-aloud techniques as described herein.
Acknowledgments
The pilot study mentioned is in part funded by the generous support of the Beth and Russell Siegelman Foundation (Meuret).
Footnotes
Studies testing the efficacy of BRT in patients diagnosed with hyperventilation syndrome (HVS; Kraft & Hoogduin, 1984; Folgering, Lenders, & Rosier, 1980; Grossman, de Swart, & Defares, 1985; Han, Stegen, de Valck, Clement, & Van de Woestijne, 1996; van Doorn, Folgering, & Colla, 1982), even though promising, are not included here as the diagnostic entity and relationship of HVS to PD remains debated (Bass, 1997; Spinhoven, Onstein, Sterk, & le Haen-Versteijnen, 1993).
Contributor Information
Alicia E. Meuret, Southern Methodist University
Kate B. Wolitzky-Taylor, University of California, Los Angeles
Michael P. Twohig, Utah State University
Michelle G. Craske, University of California, Los Angeles
References
- Andrews G, Cuijpers P, Craske MG, McEvoy P, Titov N. Computer therapy for anxiety and depressive disorders is effective, acceptable and practice health care: A meta-analysis. PLoS One. 2010;5(10):e13196. doi: 10.1371/journal.pone.0013196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antony MM, Ledley DR, Liss A, Swinson RP. Responses to symptom induction exercises in panic disorder. Behaviour Research and Therapy. 2006;44:85–98. doi: 10.1016/j.brat.2004.12.005. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Craske MG, Cerny JA, Klosko JS. Behavioral treatment of panic disorder. Behavior Therapy. 1989;20:261–282. [Google Scholar]
- Barlow DH, Gorman JM, Shear MK, Woods SW. Cognitive-behavioral therapy, imipramine, or their combination for panic disorder: A randomized controlled trial. Journal of the American Medical Association. 2000;283:2573–2574. doi: 10.1001/jama.283.19.2529. [DOI] [PubMed] [Google Scholar]
- Bass C. Hyperventilation syndrome: A chimera? Journal of Psychosomatic Research. 1997;42:421–426. doi: 10.1016/s0022-3999(96)00365-0. [DOI] [PubMed] [Google Scholar]
- Beck JG, Stanley MA, Baldwin LE, Deagle EA, Averill P. Comparison of cognitive therapy and relaxation training for panic disorder. Journal of Consulting and Clinical Psychology. 1994;62:818–826. doi: 10.1037//0022-006x.62.4.818. [DOI] [PubMed] [Google Scholar]
- Bernstein DA, Borkovec TD. Progressive relaxation training: A manual for the helping professions. Champaign, IL: Research Press; 1973. [Google Scholar]
- Blechert J, Wilhelm FH, Meuret AE, Wilhelm EM, Roth WT. Respiratory, autonomic, and experiential responses to repeated inhalations of 20% CO2 enriched air in panic disorder, social phobia, and healthy controls. Biological Psychology. 2010;84:104–111. doi: 10.1016/j.biopsycho.2010.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonn JA, Readhead CPA, Timmons BH. Enhanced behavioral response in agoraphobic patients pretreated with breathing retraining. Lancet. 1984;2:665–669. doi: 10.1016/s0140-6736(84)91226-1. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Sides JK. Critical procedural variables related to the physiological effects of progressive relaxation: A review. Behaviour Research and Therapy. 1979;17:119–125. doi: 10.1016/0005-7967(79)90020-2. [DOI] [PubMed] [Google Scholar]
- Bouchard S, Gauthier J, Laberge B, French D, Pelletier MH, Godbout C. Exposure versus cognitive restructuring in the treatment of panic disorder with agoraphobia. Behaviour Research and Therapy. 1996;34:213–224. doi: 10.1016/0005-7967(95)00077-1. [DOI] [PubMed] [Google Scholar]
- Bouchard S, Gauthier J, Nouwen A, Ivers H, Vallières A, Simard S, Fournier T. Temporal relationship between dysfunctional beliefs, self-efficacy and panic apprehension in the treatment of panic disorder with agoraphobia. Journal of Behavior Therapy and Experimental Psychiatry. 2007;38:275–292. doi: 10.1016/j.jbtep.2006.08.002. [DOI] [PubMed] [Google Scholar]
- Brown TA, Barlow DH. Long-term outcome in cognitive-behavioral treatment of panic disorder: Clinical predictors and alternative strategies for assessment. Journal of Consulting and Clinical Psychology. 1995;63:754–765. doi: 10.1037//0022-006x.63.5.754. [DOI] [PubMed] [Google Scholar]
- Caldirola D, Bellodi L, Caumo A, Migliarese G, Perna G. Approximate entropy of respiratory patterns in panic disorder. American Journal of Psychiatry. 2004;161:79–87. doi: 10.1176/appi.ajp.161.1.79. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Caputo GC, Bright P, Gallagher R. Assessment of fear of fear in agoraphobics: The Body Sensations Questionnaire and the Agoraphobic Cognitions Questionnaire. Journal of Consulting and Clinical Psychology. 1984;52:1090–1097. doi: 10.1037//0022-006x.52.6.1090. [DOI] [PubMed] [Google Scholar]
- Clark DM. A cognitive approach to panic. Behaviour Research and Therapy. 1986;24:461–470. doi: 10.1016/0005-7967(86)90011-2. [DOI] [PubMed] [Google Scholar]
- Clark DM, Salkovskis PM, Chalkley AJ. Respiratory control as a treatment for panic attacks. Journal of Behavior Therapy and Experimental Psychiatry. 1985;16:23–30. doi: 10.1016/0005-7916(85)90026-6. [DOI] [PubMed] [Google Scholar]
- Clark DM, Salkovskis PM, Gelder M, Koehler C, Martin M, Anastasiades P, Jeavons A. Tests of a cognitive theory of panic. In: Hand I, Wittchen H, editors. Panic and phobias II. Berlin: Springer-Verlag; 1988. [Google Scholar]
- Clark DM, Salkovskis PM, Hackmann A, Middleton H, Anastasiades P, Gelder M. A comparison of cognitive therapy, applied relaxation and imipramine in the treatment of panic disorder. British Journal of Psychiatry. 1994;164:759–769. doi: 10.1192/bjp.164.6.759. [DOI] [PubMed] [Google Scholar]
- Clark DM, Salkovskis PM, Hackmann A, Wells A, Ludgate J, Gelder M. Brief cognitive therapy for panic disorder: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 1999;67:583–589. doi: 10.1037//0022-006x.67.4.583. [DOI] [PubMed] [Google Scholar]
- Conrad A, Müller A, Doberenz S, Kim S, Meuret AE, Wollburg E, Roth WT. Psychophysiological effects of breathing instructions for stress management. Applied Psychophysiology and Biofeedback. 2007;32:89–98. doi: 10.1007/s10484-007-9034-x. [DOI] [PubMed] [Google Scholar]
- Craske MG, Barlow DH. Panic disorder and agoraphobia. In: Barlow DH, editor. Clinical handbook of psychological disorders: A step-by-step treatment manual. 4th ed. New York: Guildford Press; 2008. pp. 1–64. [Google Scholar]
- Craske MG, Rowe M, Lewin M, Noriega-Dimitri R. Interoceptive exposure versus breathing retraining within cognitive-behavioural therapy for panic disorder with agoraphobia. British Journal of Clinical Psychology. 1997;36:85–99. doi: 10.1111/j.2044-8260.1997.tb01233.x. [DOI] [PubMed] [Google Scholar]
- Dager SR, Strauss WL, Marro KI, Richards TL, Metzger GD, Artru AA. Proton magnetic resonance spectroscopy investigation of hyperventilation in subjects with panic disorder and comparison subjects. American Journal of Psychiatry. 1995;152:666–672. doi: 10.1176/ajp.152.5.666. [DOI] [PubMed] [Google Scholar]
- Davison GC, Vogel RS, Coffman SG. Think-aloud approaches to cognitive assessment and the articulated thoughts in simulated situations paradigm. Journal of Consulting and Clinical Psychology. 1997;65:950–958. doi: 10.1037//0022-006x.65.6.950. [DOI] [PubMed] [Google Scholar]
- Davison GC, Williams ME, Nezami E, Bice TL, DeQuattro VL. Relaxation, reduction in angry articulated thoughts, and improvements in borderline hypertension and heart rate. Journal of Behavioral Medicine. 1991;14:453–468. doi: 10.1007/BF00845104. [DOI] [PubMed] [Google Scholar]
- Dawson RW, McMurray NE. Desensitization without hierarchical presentation and concomitant relaxation. Australian Journal of Psychology. 1978;30:119–132. [Google Scholar]
- Deacon B, Lickel J, Abramowitz JS. Medical utilization across the anxiety disorders. Journal of Anxiety Disorders. 2008;22:344–350. doi: 10.1016/j.janxdis.2007.03.004. [DOI] [PubMed] [Google Scholar]
- de Beurs E, Lange A, van Dyck R, Koele P. Respiratory training prior to exposure in vivo in the treatment of panic disorder with agoraphobia: Efficacy and predictors of outcome. Australian and New Zealand Journal of Psychiatry. 1995;29:104–113. doi: 10.3109/00048679509075898. [DOI] [PubMed] [Google Scholar]
- de Beurs E, van Balkom AJ, Lange A, Koele P, van Dyck R. Treatment of panic disorder with agoraphobia: Comparison of fluvoxamine, placebo, and psychological panic management combined with exposure and of exposure in vivo alone. American Journal of Psychiatry. 1995;152:683–691. doi: 10.1176/ajp.152.5.683. [DOI] [PubMed] [Google Scholar]
- de Ruiter C, Rijken H, Garssen B, Kraaimaat F. Breathing retraining, exposure and a combination of both, in the treatment of panic disorder with agoraphobia. Behaviour Research and Therapy. 1989;27:647–655. doi: 10.1016/0005-7967(89)90148-4. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Margraf J, Davies S, Roth W. Selective processing of threat cues in subjects with panic attacks. Cognition and Emotion. 1988;2:201–219. [Google Scholar]
- Folgering H, Lenders J, Rosier I. Biofeedback control of PaCO2, a prospective therapy in hyperventilation. In: Herzog H, editor. Asthma: Progress in respiratory research. Vol. 14. Basle, Switzerland: Karger; 1980. pp. 26–30. [Google Scholar]
- Forman EM, Herbert JD, Moitra E, Yeomans PD, Geller PA. A randomized controlled effectiveness trial of acceptance and commitment therapy and cognitive therapy for anxiety and depression. Behavior Modification. 2007;31:772–799. doi: 10.1177/0145445507302202. [DOI] [PubMed] [Google Scholar]
- Fridhandler BM. Conceptual note on state, trait, and the state-trait distinction. Journal of Personality and Social Psychology. 1986;50(1):169–174. [Google Scholar]
- Gorman JM, Fyer MR, Goetz R, Askanazi J, Liebowitz MR, Fyer AJ, Klein DF. Ventilatory physiology of patients with panic disorder. Archives of General Psychiatry. 1988;45:31–39. doi: 10.1001/archpsyc.1988.01800250035006. [DOI] [PubMed] [Google Scholar]
- Gorman JM, Martinez J, Coplan JD, Kent J, Kleber M. The effect of successful treatment on the emotional and physiological response to carbon dioxide inhalation in patients with panic disorder. Biological Psychiatry. 2004;56:862–867. doi: 10.1016/j.biopsych.2004.08.016. [DOI] [PubMed] [Google Scholar]
- Gorman JM, Papp LA, Coplan JD, Martinez JM, Lennon S, Goetz RR, Klein DF. Anxiogenic effects of CO2 and hyperventilation in patients with panic disorder. American Journal of Psychiatry. 1994;151:547–553. doi: 10.1176/ajp.151.4.547. [DOI] [PubMed] [Google Scholar]
- Grossman P, de Swart JC, Defares PB. A controlled study of a breathing therapy for treatment of hyperventilation syndrome. Journal of Psychosomatic Research. 1985;29:49–58. doi: 10.1016/0022-3999(85)90008-x. [DOI] [PubMed] [Google Scholar]
- Han JN, Stegen K, de Valck C, Clement J, Van de Woestijne KP. Influence of breathing therapy on complaints, anxiety and breathing pattern in patients with hyperventilation syndrome and anxiety disorders. Journal of Psychosomatic Research. 1996;41:481–493. doi: 10.1016/s0022-3999(96)00220-6. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York: Guilford Press; 1999. [Google Scholar]
- Hibbert GA, Chan M. Respiratory control: Its contribution to the treatment of panic attacks: A controlled study. British Journal of Psychiatry. 1989;154:232–236. doi: 10.1192/bjp.154.2.232. [DOI] [PubMed] [Google Scholar]
- Hoffart A. A comparison of cognitive and guided mastery therapy of agoraphobia. Behaviour Research and Therapy. 1995;33:423–434. doi: 10.1016/0005-7967(94)00056-p. [DOI] [PubMed] [Google Scholar]
- Hoffart A, Sexton H, Hedley LM, Martinsen E. Mechanisms of change in cognitive therapy for panic disorder with agoraphobia. Journal of Behavior Therapy and Experimental Psychiatry. 2008;39:262–275. doi: 10.1016/j.jbtep.2007.07.006. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Meuret AE, Rosenfield D, Suvak MK, Barlow DH, Gorman JM, Woods SW. Preliminary evidence for cognitive mediation during cognitive behavioral therapy of panic disorder. Journal of Consulting and Clinical Psychology. 2007;75:374–379. doi: 10.1037/0022-006X.75.3.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: A meta-analysis of randomized placebo-controlled trials. Journal of Clinical Psychiatry. 2008;69:621–632. doi: 10.4088/jcp.v69n0415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hope DA, Rapee RM, Heimberg RG, Dombeck MJ. Representations of the self in social phobia: Vulnerability to social threat. Cognitive Therapy and Research. 1990;14:177–189. [Google Scholar]
- Jacob RG, Furman JM, Clark DB, Durrant JD. Vestibular symptoms, panic, and phobia: Overlap and possible relationships. Annals of Clinical Psychiatry. 1992;4:163–174. [Google Scholar]
- Jacobson E. Electrical measurements concerning muscular contraction (tonus) and the cultivation of relaxation in man: Relaxation times of individuals. American Journal of Physiology. 1934;108:573–580. [Google Scholar]
- Jacobson E. Progressive relaxation. 2nd ed. Chicago: University of Chicago Press; 1938. [Google Scholar]
- Jarrett RB, Vittengl JR, Doyle K, Clark LA. Changes in cognitive content during and following cognitive therapy for recurrent depression: Substantial and enduring, but not predictive of change in depressive symptoms. Journal of Consulting and Clinical Psychology. 2007;75:432–446. doi: 10.1037/0022-006X.75.3.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katon W, Von Korff M, Lin E, Lipscomb P, Russo J, Wagner E, Polk E. Distressed high utilizers of medical care. DSM-III-R diagnoses and treatment needs. General Hospital Psychiatry. 1990;12:355–362. doi: 10.1016/0163-8343(90)90002-t. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology. 2007;3:1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Wilcoxon LA. Systematic desensitization and nonspecific treatment effects: A methodological evaluation. Psychological Bulletin. 1976;83:729–758. [PubMed] [Google Scholar]
- Keller MB, Yonkers KA, Warshaw MG, Pratt LA, Gollan JK, Massion AO, Lavori PW. Remission and relapse in subjects with panic disorder and panic with agoraphobia: A prospective short-interval naturalistic follow-up. Journal of Nervous and Mental Disease. 1994;182:290–296. doi: 10.1097/00005053-199405000-00007. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein DF. Panic disorder with agoraphobia. British Journal of Psychiatry. 1993;163:835–837. doi: 10.1192/bjp.163.6.835a. [DOI] [PubMed] [Google Scholar]
- Klerman GL, Weissman MM, Ouellette R, Johnson J, Greenwald S. Panic attacks in the community. Social morbidity and health care utilization. Journal of the American Medical Association. 1991;265:742–746. [PubMed] [Google Scholar]
- Kraft AR, Hoogduin CA. The hyperventilation syndrome: A pilot study on the effectiveness of treatment. British Journal of Psychiatry. 1984;145:538–542. doi: 10.1192/bjp.145.5.538. [DOI] [PubMed] [Google Scholar]
- Kroeze S, van den Hout MA. Selective attention for cardiac information in panic patients. Behaviour Research and Therapy. 2000;38:63–72. doi: 10.1016/s0005-7967(99)00023-6. [DOI] [PubMed] [Google Scholar]
- Leboeuf A, Lodge J. A comparison of frontalis EMG feedback training and progressive relaxation in the treatment of chronic anxiety. British Journal of Psychiatry. 1980;137:279–284. doi: 10.1192/bjp.137.3.279. [DOI] [PubMed] [Google Scholar]
- Leon AC, Portera L, Weissman MM. The social costs of anxiety disorders. [Supplemental material] British Journal of Psychiatry. 1995;27:19–22. [PubMed] [Google Scholar]
- Levin RB, Gross AM. The role of relaxation in systematic desensitization. Behaviour Research and Therapy. 1985;23:187–196. doi: 10.1016/0005-7967(85)90027-0. [DOI] [PubMed] [Google Scholar]
- Levitt JT, Brown TA, Orsillo SM, Barlow DH. The effects of acceptance versus suppression of emotion on subjective and psychophysiological response to carbon dioxide challenge in patients with panic disorder. Behavior Therapy. 2004;35:747–766. [Google Scholar]
- Ley RA. Blood, breath and fears: A hyperventilation theory of panic attacks and agoraphobia. Clinical Psychology Review. 1985;5:271–285. [Google Scholar]
- Ley RA. The efficacy of breathing retraining and the centrality of hyperventilation in panic disorder: A reinterpretation of experimental findings. Behaviour Research and Therapy. 1991;29:301–304. doi: 10.1016/0005-7967(91)90121-i. [DOI] [PubMed] [Google Scholar]
- Maidenberg E, Chen E, Craske M, Bohn P, Bystritsky A. Specificity of attentional bias in panic disorder and social phobia. Journal of Anxiety Disorders. 1996;10:529–541. [Google Scholar]
- Marks IM, Swinson RP, Basoglu M, Kuch K, Noshirvani H, O'Sullivan G, Wickwire K. Alprazolam and exposure alone and combined in panic disorder with agoraphobia: A controlled study in London and Toronto. British Journal of Psychiatry. 1993;162:776–782. doi: 10.1192/bjp.162.6.776. [DOI] [PubMed] [Google Scholar]
- McGlynn FD, Solomon GS, Barrios BA. Graded imagination and relaxation as components of experimental desensitization: A psychophysiological evaluation. Journal of Clinical Psychology. 1979;35:542–546. doi: 10.1002/1097-4679(197907)35:3<542::aid-jclp2270350313>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- McNally RJ. Panic disorder: A critical analysis. New York: Guilford Press; 1994. [Google Scholar]
- McNally RJ, Lorenz M. Anxiety sensitivity in agoraphobics. Journal of Behavior Therapy and Experimental Psychiatry. 1987;18:3–11. doi: 10.1016/0005-7916(87)90065-6. [DOI] [PubMed] [Google Scholar]
- McNally RJ, Riemann BC, Louro CE, Lukach BM, Kim E. Cognitive processing of emotional information in panic disorder. Behaviour Research and Therapy. 1992;30:143–149. doi: 10.1016/0005-7967(92)90137-6. [DOI] [PubMed] [Google Scholar]
- Meulenbeek P, Spinhoven P, Smit F, van Balkom A, Cuijpers P. Cognitive mediation of panic reduction during an early intervention for panic. Acta Psychiatrica Scandinavica. 2010;122:20–29. doi: 10.1111/j.1600-0447.2009.01530.x. [DOI] [PubMed] [Google Scholar]
- Meuret AE, Hofmann SG, Rosenfield D. Catastrophic appraisal and perceived control as moderators of treatment response in panic disorder. International Journal of Cognitive Therapy. 2010;3:262–277. doi: 10.1521/ijct.2010.3.3.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meuret AE, Ritz T. Hyperventilation in panic disorder and asthma: Empirical evidence and clinical strategies. International Journal of Psychophysiology. 2010;78:68–79. doi: 10.1016/j.ijpsycho.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meuret AE, Rosenfield D, Hofmann SG, Suvak MK, Roth WT. Changes in respiration mediate changes in fear of bodily sensations in panic disorder. Journal of Psychiatric Research. 2009;43:634–641. doi: 10.1016/j.jpsychires.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meuret AE, Rosenfield D, Seidel A, Bhaskara L, Hofmann SG. Respiratory and cognitive mediators of treatment change in panic disorder: Evidence for intervention specificity. Journal of Consulting and Clinical Psychology. 2010;78:691–704. doi: 10.1037/a0019552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meuret AE, Rosenfield D, Wilhelm FH, Zhou E, Conrad A, Ritz T, Roth WT. Biological Psychiatry. Do unexpected panic attacks occur spontaneously? (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meuret AE, Twohig M, Rosenfield D, Hayes S, Craske MG. Brief acceptance and exposure therapy for panic disorder: A pilot study. (submitted for publication) [Google Scholar]
- Meuret AE, Wilhelm FH, Ritz T, Roth WT. Breathing training for treating panic disorder. Useful intervention or impediment? Behavior Modification. 2003;27:731–754. doi: 10.1177/0145445503256324. [DOI] [PubMed] [Google Scholar]
- Meuret AE, Wilhelm FH, Ritz T, Roth WT. Feedback of end-tidal pCO2 as a therapeutic approach for panic disorder. Journal of Psychiatric Research. 2008;42:560–568. doi: 10.1016/j.jpsychires.2007.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michelson LK, Mavissakalian M, Marchione K, Ulrich RF, Marchione N, Testa S. Psychophysiological outcome of cognitive, behavioral and psychophysiologically-based treatments of agoraphobia. Behavior Research and Therapy. 1990;28:127–139. doi: 10.1016/0005-7967(90)90025-e. [DOI] [PubMed] [Google Scholar]
- Milrod B, Leon AC, Busch F, Rudden M, Schwalberg M, Clarkin J, Shear MK. A randomized controlled clinical trial of psychoanalytic psychotherapy for panic disorder. American Journal of Psychiatry. 2007;164:265–272. doi: 10.1176/ajp.2007.164.2.265. [DOI] [PubMed] [Google Scholar]
- Murphy MT, Michelson LK, Marchione K, Marchione N, Testa S. The role of self-directed in vivo exposure in combination with cognitive therapy, relaxation training, or therapist-assisted exposure in the treatment of panic disorder with agoraphobia. Journal of Anxiety Disorders. 1998;12:117–138. doi: 10.1016/s0887-6185(98)00003-6. [DOI] [PubMed] [Google Scholar]
- Norton PJ, Price EC. A meta-analytic review of adult cognitive-behavioral treatment outcome across the anxiety disorders. Journal of Nervous and Mental Disease. 2007;195:521–531. doi: 10.1097/01.nmd.0000253843.70149.9a. [DOI] [PubMed] [Google Scholar]
- Öst L-G. Applied relaxation vs. progressive relaxation in the treatment of panic disorder. Behaviour Research and Therapy. 1988;26:13–22. doi: 10.1016/0005-7967(88)90029-0. [DOI] [PubMed] [Google Scholar]
- Öst L-G, Thulin U, Ramneroe J. Cognitive behavior therapy vs. exposure in vivo in the treatment of panic disorder with agoraphobia. Behaviour Research and Therapy. 2004;42:1105–1127. doi: 10.1016/j.brat.2003.07.004. [DOI] [PubMed] [Google Scholar]
- Öst L-G, Westling BE. Applied relaxation vs. cognitive behavior therapy in the treatment of panic disorder. Behaviour Research and Therapy. 1995;33:145–158. doi: 10.1016/0005-7967(94)e0026-f. [DOI] [PubMed] [Google Scholar]
- Öst L-G, Westling BE, Hellström K. Applied relaxation, exposure in vivo and cognitive methods in the treatment of panic disorder with agoraphobia. Behaviour Research and Therapy. 1993;31:383–394. doi: 10.1016/0005-7967(93)90095-c. [DOI] [PubMed] [Google Scholar]
- Perna G, Bertani A, Arancio C, Ronchi P, Bellodi L. Laboratory response of patients with panic and obsessive-compulsive disorders to 35% CO2 challenges. American Journal of Psychiatry. 1995;152:85–89. doi: 10.1176/ajp.152.1.85. [DOI] [PubMed] [Google Scholar]
- Rapee RM. A case of panic disorder treated with breathing retraining. Journal of Behavior Therapy and Experimental Psychiatry. 1985;16:63–65. doi: 10.1016/0005-7916(85)90032-1. [DOI] [PubMed] [Google Scholar]
- Rapee RM. Differential response to hyperventilation in panic disorder and generalized anxiety disorder. Journal of Abnormal Psychology. 1986;95:24–28. doi: 10.1037//0021-843x.95.1.24. [DOI] [PubMed] [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne PP, Stein MB, Russo J, Craske MG, Katon W, Sullivan G, Sherbourne C. Medical illness and response to treatment in primary care panic disorder. General Hospital Psychiatry. 1999;27:237–243. doi: 10.1016/j.genhosppsych.2005.03.007. [DOI] [PubMed] [Google Scholar]
- Salkovskis PM, Clark DM, Hackmann A. Treatment of panic attacks using cognitive therapy without exposure or breathing retraining. Behaviour Research and Therapy. 1991;29:161–166. doi: 10.1016/0005-7967(91)90044-4. [DOI] [PubMed] [Google Scholar]
- Salkovskis PM, Jones DR, Clark DM. Respiratory control in the treatment of panic attacks: Replication and extension with concurrent measurement of behaviour and pCO2. British Journal of Psychiatry. 1986;148:526–532. doi: 10.1192/bjp.148.5.526. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Bates MJ. Evaluation of a pathoplastic relationship between anxiety sensitivity and panic disorder. Anxiety, Stress, and Coping. 2003;16:17–30. [Google Scholar]
- Schmidt NB, Woolaway-Bickel K, Trakowski J, Santiago H, Storey J, Koselka M, Cook J. Dismantling cognitive-behavioral treatment for panic disorder: Questioning the utility of breathing retraining. Journal of Consulting and Clinical Psychology. 2000;68:417–424. doi: 10.1037//0022-006x.68.3.417. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Williams JM, Teasdale JD. Mindfulness-based cognitive therapy for depression. New York: Guilford Press; 2002. [Google Scholar]
- Seidel A, Rosenfield D, Bhaskara L, Hofmann SG, Meuret AE. Pathways of biobehavioral change in exposure therapy of panic disorder. Paper presented at the 43rd Annual Convention of the Association of Advancement of Behavior and Cognitive Therapy; New York, NY. 2009. Nov, [Google Scholar]
- Shear MK, Brown TA, Barlow DH, Money R, Sholomskas DE, Woods SW, Laszlo A. Multicenter Collaborative Panic Disorder Severity Scale. American Journal of Psychiatry. 1997;154:1571–1575. doi: 10.1176/ajp.154.11.1571. [DOI] [PubMed] [Google Scholar]
- Smits JAJ, Powers MB, Cho Y, Telch MJ. Mechanism of change in cognitive-behavioral treatment of panic disorder: Evidence for the fear of fear mediational hypothesis. Journal of Consulting and Clinical Psychology. 2004;72:646–652. doi: 10.1037/0022-006X.72.4.646. [DOI] [PubMed] [Google Scholar]
- Spinhoven P, Onstein EJ, Sterk PJ, le Haen-Versteijnen D. Discordance between symptom and physiological criteria for the hyperventilation syndrome. Journal of Psychosomatic Research. 1993;37:281–289. doi: 10.1016/0022-3999(93)90037-g. [DOI] [PubMed] [Google Scholar]
- Teachman BA, Marker CD, Smith-Janik SB. Automatic associations and panic disorder: Trajectories of change over the course of treatment. Journal of Consulting and Clinical Psychology. 2008;76:988–1002. doi: 10.1037/a0013113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telch MJ, Lucas JA, Schmidt NB, Hanna HH, Jaimez TL, Lucas R. Group cognitive-behavioral treatment of panic disorder. Behaviour Research and Therapy. 1993;31:279–287. doi: 10.1016/0005-7967(93)90026-q. [DOI] [PubMed] [Google Scholar]
- Van den Hout M, Arntz A, Hoekstra R. Exposure reduced agoraphobia but not panic, and cognitive therapy reduced panic but not agoraphobia. Behaviour Research and Therapy. 1994;32:447–451. doi: 10.1016/0005-7967(94)90008-6. [DOI] [PubMed] [Google Scholar]
- van Doorn P, Folgering H, Colla P. Control of the end-tidal PCO2 in the hyperventilation syndrome: Effects of biofeedback and breathing instructions compared. Bulletin of European Physiopathological Respiration. 1982;18:829–836. [PubMed] [Google Scholar]
- Vögele C, Ehlers A, Meyer AH, Frank M, Hahlweg K, Margraf J. Cognitive mediation of clinical improvement after intensive exposure therapy of agoraphobia and social phobia. Depression and Anxiety. 2010;27:294–301. doi: 10.1002/da.20651. [DOI] [PubMed] [Google Scholar]
- Waters WF, McDonald DG, Koresko RL. Psychophysiological responses during analogue systematic desensitization and non-relaxation control procedures. Behaviour Research and Therapy. 1972;10:381–393. doi: 10.1016/0005-7967(72)90061-7. [DOI] [PubMed] [Google Scholar]
- Westen D, Morrison K. A multidimensional meta-analysis of treatments for depression, panic, and generalized anxiety disorder: An empirical examination of the status of empirically supported therapies. Journal of Consulting and Clinical Psychology. 2001;69:875–899. [PubMed] [Google Scholar]
- White K, Barlow DH. Panic disorder and agoraphobia. In: Barlow DH, editor. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2nd ed. New York: Guilford Press; 2002. pp. 292–327. [Google Scholar]
- Wilhelm FH, Gerlach AL, Roth WT. Slow recovery from voluntary hyperventilation in panic disorder. Psychosomatic Medicine. 2001;63:638–649. doi: 10.1097/00006842-200107000-00017. [DOI] [PubMed] [Google Scholar]
- Williams SL, Falbo J. Cognitive and performance-based treatments for panic attacks in people with varying degrees of agoraphobic disability. Behaviour Research and Therapy. 1996;34:253–264. doi: 10.1016/0005-7967(95)00063-1. [DOI] [PubMed] [Google Scholar]
- Williams SL, Kinney PJ, Harap ST, Liebmann M. Thoughts of agoraphobic people during scary tasks. Journal of Abnormal Psychology. 1997;106:511–520. doi: 10.1037//0021-843x.106.4.511. [DOI] [PubMed] [Google Scholar]
- Wolpe W. Psychotherapy by reciprocal inhibition. Stanford, CA: Stanford University Press; 1958. [Google Scholar]
- Yates A. Theory and practice in behavior therapy. New York: Wiley-Interscience; 1975. [Google Scholar]