Abstract
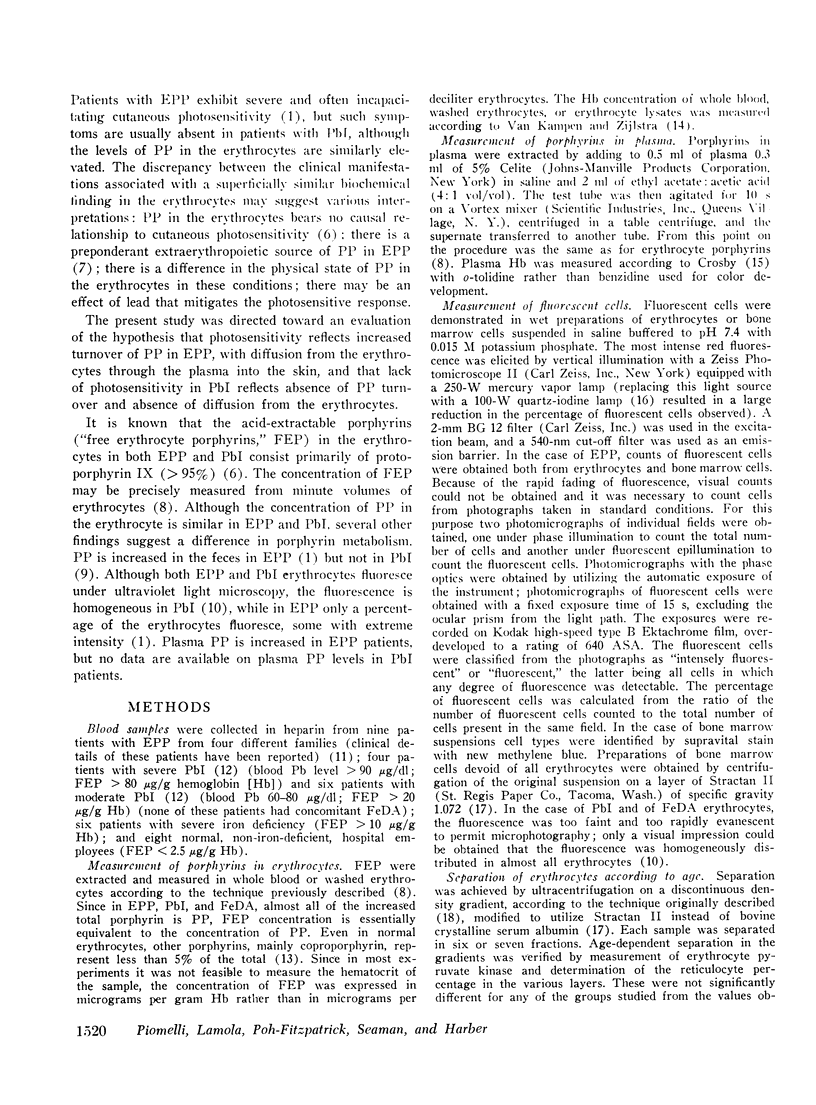
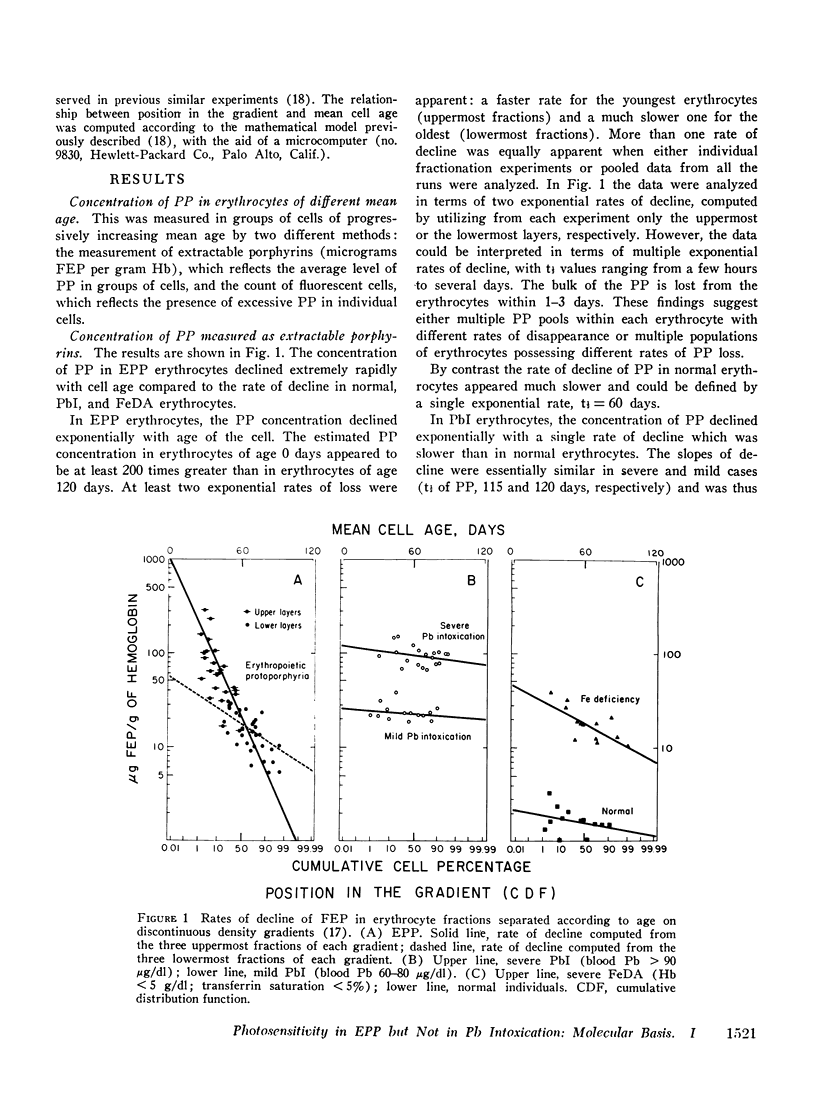
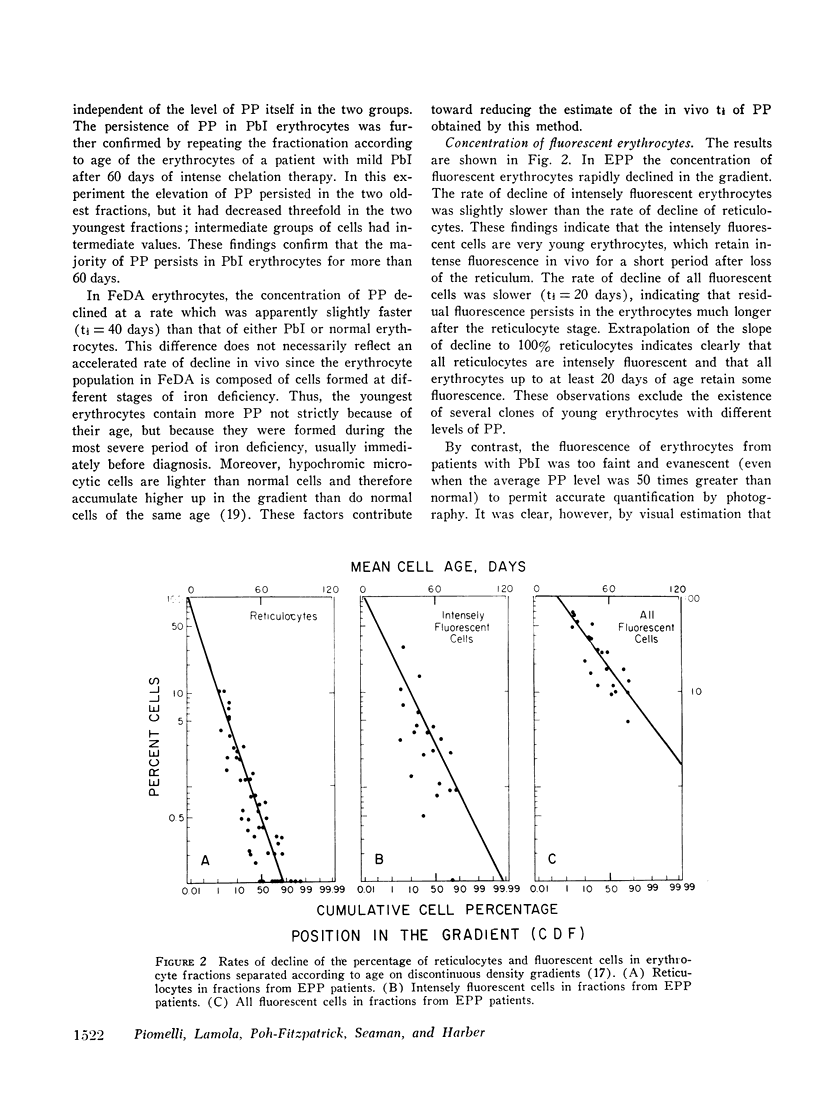
In lead intoxication photosensitivity is usually absent, despite concentrations of protoporphyrin in the erythrocytes equal to or greater than in erythropoietic protoporphyria. Profound differences in the distribution of protoporphyrin in aging erythrocytes were demonstrated by age-dependent fractionation of cells on discontinuous density gradients. In erythropoietic protoporphyria the concentration of protoporphyrin declined extremely rapidly with erythrocyte age; the bulk of the protoporphyrin was lost in less than 3 days and the concentration of fluorescent erythrocytes in the gradient paralleled the decline of protoporphyrin. In lead intoxication the protoporphyrin concentration declined only slightly with cell aging and erythrocytes of all ages fluoresced. In the bone marrow from a patient with erythropoietic protoporphyria all reticulocytes, but only occasional late normoblasts, fluoresced, suggesting a single population. Sterile incubation in plasma (pH 7.5) demonstrated rapid diffusion of protoporphyrin from the erythrocytes in erythropoietic protoporphyria, but not in lead intoxication. Plasma protoporphyrin was elevated in erythropoietic protoporphyria, but not in lead intoxication. Estimates of the daily loss of protoporphyrin from erythropoietic tissue in erythropoietic proporphyria suggested an order of magnitude similar to the total blood protoporphyrin. Therefore, it is not necessary to postulate a preponderant extraerythropoietic source to explain the amount of fecal excretion. A significant amount of the diffused protoporphyrin probably reaches the skin with resulting photosensitivity. In contrast, in lead intoxication protoporphyrin remains within the erythrocyte throughout its life span ; there is no diffusion into the plasma and hence no photosensitivity.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- CROSBY W. H., FURTH F. W. A modification of the benzidine method for measurement of hemoglobin in plasma and urine. Blood. 1956 Apr;11(4):380–383. [PubMed] [Google Scholar]
- Clark K. G., Nicholson D. C. Erythrocyte protoporphyrin and iron uptake in erythropoietic protoporphyria. Clin Sci. 1971 Oct;41(4):363–370. doi: 10.1042/cs0410363. [DOI] [PubMed] [Google Scholar]
- Corash L. M., Piomelli S., Chen H. C., Seaman C., Gross E. Separation of erythrocytes according to age on a simplified density gradient. J Lab Clin Med. 1974 Jul;84(1):147–151. [PubMed] [Google Scholar]
- Cripps D. J., Hawgood R. S., Magnus I. A. Iodine tungsten fluorescence microscopy for porphyrin fluorescence. A study on erythropoietic protoporphyria. Arch Dermatol. 1966 Jan;93(1):129–137. [PubMed] [Google Scholar]
- Donaldson E. M., McCall A. J., Magnus I. A., Simpson J. R., Caldwell R. A., Hargreaves T. Erythropoietic protoporphyria: two deaths from hepatic cirrhosis. Br J Dermatol. 1971 Jan;84(1):14–24. doi: 10.1111/j.1365-2133.1971.tb14191.x. [DOI] [PubMed] [Google Scholar]
- HAEGER-ARONSEN B. Fecal porphyrins in porphyria acuta intermittens, porphyria cutanea tarda and intoxicatio plumbi. Scand J Clin Lab Invest. 1962;14:397–402. doi: 10.3109/00365516209079727. [DOI] [PubMed] [Google Scholar]
- JANDL J. H., INMAN J. K., SIMMONS R. L., ALLEN D. W. Transfer of iron from serum iron-binding protein to human reticulocytes. J Clin Invest. 1959 Jan 1;38(1 Pt 1):161–185. doi: 10.1172/JCI103786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson L. W., Schwartz S. Relation of porphyrin content to red cell age: analysis by fractional hemolysis. Proc Soc Exp Biol Med. 1972 Jan;139(1):191–197. doi: 10.3181/00379727-139-36107. [DOI] [PubMed] [Google Scholar]
- Kaplowitz N., Javitt N., Harber L. C. Isolation of erythrocytes with normal protoporphyrin levels in erythropoietic protoporphyria. N Engl J Med. 1968 May 16;278(20):1077–1081. doi: 10.1056/NEJM196805162782001. [DOI] [PubMed] [Google Scholar]
- LICHTMAN H. C., FELDMAN F. In vitro pyrrole and porphyrin synthesis in lead poisoning and iron deficiency. J Clin Invest. 1963 Jun;42:830–839. doi: 10.1172/JCI104775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamola A. A., Piomelli S., Poh-Fitzpatrick M. G., Yamane T., Harber L. C. Erythropoietic protoporphyria and lead intoxication: the molecular basis for difference in cutaneous photosensitivity. II. Different binding of erythrocyte protoporphyrin to hemoglobin. J Clin Invest. 1975 Dec;56(6):1528–1535. doi: 10.1172/JCI108234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langer E. E., Haining R. G., Labbe R. F., Jacobs P., Crosby E. F., Finch C. A. Erythrocyte protoporphyrin. Blood. 1972 Jul;40(1):112–128. [PubMed] [Google Scholar]
- MAGNUS I. A., JARRETT A., PRANKERD T. A., RIMINGTON C. Erythropoietic protoporphyria. A new porphyria syndrome with solar urticaria due to protoporphyrinaemia. Lancet. 1961 Aug 26;2(7200):448–451. doi: 10.1016/s0140-6736(61)92427-8. [DOI] [PubMed] [Google Scholar]
- Medical aspects of childhood lead poisoning. Pediatrics. 1971 Sep;48(3):464–468. [PubMed] [Google Scholar]
- Nakashima K., Oda S., Miwa S. Red cell density in various blood disorders. J Lab Clin Med. 1973 Aug;82(2):297–302. [PubMed] [Google Scholar]
- PORTER F. S. CONGENITAL ERYTHROPOIETIC PROTOPORPHYRIA. II. AN EXPERIMENTAL STUDY. Blood. 1963 Nov;22:532–544. [PubMed] [Google Scholar]
- PORTER F. S., LOWE B. A. CONGENITAL ERYTHROPOIETIC PROTOPORPHYRIA. I. CASE REPORTS, CLINICAL STUDIES AND PORPHYRIN ANALYSES IN TWO BROTHERS. Blood. 1963 Nov;22:521–531. [PubMed] [Google Scholar]
- Piomelli S. A micromethod for free erythrocyte porphyrins: the FEP test. J Lab Clin Med. 1973 Jun;81(6):932–940. [PubMed] [Google Scholar]
- Piomelli S., Corash L. M., Davenport D. D., Miraglia J., Amorosi E. L. In vivo lability of glucose-6-phosphate dehydrogenase in GdA- and GdMediterranean deficiency. J Clin Invest. 1968 Apr;47(4):940–948. doi: 10.1172/JCI105786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piomelli S., Davidow B., Guinee V. F., Young P., Gay G. The FEP (free erythrocyte porphyrins) test: a screening micromethod for lead poisoning. Pediatrics. 1973 Feb;51(2):254–259. [PubMed] [Google Scholar]
- REDEKER A. G., BRONOW R. S., STERLING R. E. ERYTHROPOIETIC PROTOPORPHYRIA. S Afr J Lab Clin Med. 1963 Dec;14:235–238. [PubMed] [Google Scholar]
- Scholnick P., Marver H. S., Schmid R. Erythropoietic protoporphyria: evidence for multiple sites of excess protoporphyrin formation. J Clin Invest. 1971 Jan;50(1):203–207. doi: 10.1172/JCI106474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schothorst A. A., Van Steveninck J., Went L. N., Suurmond D. Protoporphyrin-induced photohemolysis in protoporphyria and in normal red blood cells. Clin Chim Acta. 1970 Apr;28(1):41–49. doi: 10.1016/0009-8981(70)90158-0. [DOI] [PubMed] [Google Scholar]
- Schwartz S., Johnson J. A., Stephenson B. D., Anderson A. S., Edmondson P. R., Fusaro R. M. Erythropoietic defects in protoporphyria: a study of factors involved in labelling of porphyrins and bile pigments from ALA- 3 H and glycine- 14 C. J Lab Clin Med. 1971 Sep;78(3):411–434. [PubMed] [Google Scholar]
- WATSON C. J. The erythrocyte coproporphyrin; variation in respect to erythrocyte protoporphyrin and reticulocytes in certain of the anemias. AMA Arch Intern Med. 1950 Dec;86(6):797–809. doi: 10.1001/archinte.1950.00230180002001. [DOI] [PubMed] [Google Scholar]
- WHITAKER J. A., VIETTI T. J. Fluorescence of the erythrocytes in lead poisoning in children: an aid to rapid diagnosis. Pediatrics. 1959 Nov;24:734–738. [PubMed] [Google Scholar]
- WRANNE L. Free erythrocyte copro-and protoporphyrin. A methodoogical and clinical study. Acta Paediatr Suppl. 1960 May;49(Suppl 124):1–78. [PubMed] [Google Scholar]
- van KAMPEN E., ZIJLSTRA W. G. Standardization of hemoglobinometry. II. The hemiglobincyanide method. Clin Chim Acta. 1961 Jul;6:538–544. doi: 10.1016/0009-8981(61)90145-0. [DOI] [PubMed] [Google Scholar]


