Abstract
Objectives
The focus on acute care, time pressure, and lack of resources hamper the delivery of smoking cessation interventions in the emergency department (ED). The aim of this study was to 1) determine the effect of an emergency nurse-initiated intervention on delivery of smoking cessation counseling based on the 5As framework (ask-advise-assess-assist-arrange), and 2) assess ED nurses’ and physicians’ perceptions of smoking cessation counseling.
Methods
The authors conducted a pre-post trial in 789 adult smokers (five or more cigarettes/day) who presented to two EDs. The intervention focused on improving delivery of the 5As by ED nurses and physicians, and included face-to-face training and an online tutorial, use of a charting/reminder tool, fax referral of motivated smokers to the state tobacco quitline for proactive telephone counseling, and group feedback to ED staff. To assess ED performance of cessation counseling, a telephone interview of subjects was conducted shortly after the ED visit. Nurses’ and physicians’ self-efficacy, role satisfaction, and attitudes toward smoking cessation counseling were assessed by survey. Multivariable linear regression was used to assess the effect of the intervention on performance of the 5As, while adjusting for key covariates.
Results
Of 650 smokers who completed the post-ED interview, a greater proportion had been asked about smoking by an ED nurse (68% vs. 53%, adjusted OR = 2.0, 95% CI = 1.3 to 2.9), assessed for willingness to quit (31% vs. 9%, adjusted OR= 4.9, 95% CI = 2.9 to 7.9), assisted in quitting (23% vs. 6%, adjusted OR = 5.1, 95% CI = 2.7 to 9.5), and had arrangements for follow-up cessation counseling (7% vs. 1%, adjusted OR = 7.1, 95% CI = 2.3 to 21) during the intervention compared to the baseline period. A similar increase was observed for emergency physicians. ED nurses’ self-efficacy and role satisfaction in cessation counseling significantly improved following the intervention; however, there was no change in “pros” and “cons” attitudes toward smoking cessation in either ED nurses or physicians.
Conclusions
Emergency department nurses and physicians can effectively deliver smoking cessation counseling to smokers in a time-efficient manner. This trial also provides empirical support for expert recommendations that call for nursing staff to play a larger role in delivering public health interventions in the ED.
INTRODUCTION
Despite increased public awareness of the health hazards of smoking and the availability of evidence-based guidelines for smoking cessation, approximately 21% of U.S. adults still smoke cigarettes.1 The prevalence of smoking tends to be higher among patients treated in the emergency department (ED); 48% of ED patients in three U.S. cities were current smokers in one prospective survey.2 Emergency clinicians are often the main source of primary care and preventive health services for over 50 million uninsured Americans who have limited access to medical care.3 Moreover, many patients in the ED experience a “teachable moment;”4 11% to 49% of ED smokers are willing to make a quit attempt within 30 days,5-9 and many of these patients desire preventive services to be initiated in the ED setting.10 Based on the strength of evidence from primary care settings, use of the U.S. Public Health Service (USPHS) Smoking Cessation Guideline by ED staff was strongly recommended in a position paper commissioned by the Society for Academic Emergency Medicine.11 The USPHS guideline specifically recommends that physicians and nurses should strongly advise their patients who use tobacco to quit, and calls for systems and practice policies to facilitate the delivery of smoking cessation counseling and pharmacotherapy.12
The time available for smoking cessation counseling in the ED may be even less than that reported in primary care.13 The focus on acute care, the lack of an ongoing relationship with the patient, and inadequate reimbursement may also hinder the delivery of cessation counseling. In one survey of emergency physicians (EPs), the most frequently reported barriers to routine implementation of smoking cessation guidelines were time pressures, and perceptions that patients are not interested and that counseling is relatively ineffective.14 In a more recent survey, over half of EPs did not agree that smoking cessation counseling is an appropriate service to offer in their practice.15
One strategy to improve delivery of preventive services in the ED is to integrate smoking cessation into the role of ED nursing staff.16 Nurse-delivered cessation counseling has been associated with higher quit rates compared to usual care in a wide variety of practice settings.17 ED nurses are uniquely positioned to deliver a brief smoking cessation intervention because of their ready access to all patients, and their training in patient education. Moreover, guidance for acute care nurses in applying a brief intervention has been developed18: 1) ask – systematically identify all tobacco users at every visit, 2) advise – strongly urge all tobacco users to quit, 3) assess – determine willingness to make a quit attempt, 4) assist – aid the patient in quitting (provide counseling and medication), and 5) arrange – ensure follow-up contact. This is referred to as the 5As, and this construct has been recommended by the U.S. Preventive Services Task Force as a tool for clinicians to assist patients with behavior change because it was judged to have the highest degree of empiric support for each of its elements, and because of its successful use in prior studies.19 The delivery of smoking cessation advice by nurses is influenced, however, by several professional concerns and practice-related factors, including the perceived ability to offer advice (e.g., time pressure, lack of skills in cessation counseling, lack of available patient education materials),20 perceived support of clinical leadership,21 and perceived autonomy.22
In light of these factors, the primary aim of this study was to evaluate the effectiveness of a pragmatic intervention targeting the delivery of the 5As by ED nurses and physicians (including physician assistants [PAs]). To gain insight into the intervention’s effect, a secondary aim of this study was to determine whether there was any change in ED nurses’ and physicians’ attitudes toward cessation counseling in response to the implementation strategy. In addition, we assessed whether the intervention led to any change in self-efficacy or role satisfaction in cessation counseling.
METHODS
Study Design
We used a pre-post quasi-experimental design at two EDs to determine the effectiveness of the study intervention (Figure 1). This design is appropriate for evaluating an intervention that involves an entire ED system of care, and is compatible with the culture of ongoing quality improvement.23 An advantage of the proposed pre-post design is that each site serves as its own control.24 We monitored the data for secular trends and regularly consulted with ED leaders to identify concurrent changes in practice that might affect our results.
Figure 1.
Schematic of pre-post study design.
The interval between periods corresponds to implementation of the study intervention (approximately two months at each site).
Although a pre-post non-equivalent comparison group design offers certain advantages in facilitating causal inference,25 we chose to evaluate the study intervention at both sites (i.e., without a control site) to determine whether the effect of the implementation intervention is robust across two systems of care (private vs. public), with a different mix of barriers to guideline implementation. During the pre-intervention period, ED staff performed their usual duties and did not receive training in use of the USPHS cessation guideline. At the outset of the intervention period, study personnel trained ED nurses, physicians, and PAs on how to implement the USPHS guideline. Although this investigation was not part of a quality assurance (QA) project or public health initiative, it included several methods commonly used in quality improvement (e.g., staff education, clinical reminder, audit and feedback, practice facilitator). This project was approved by the institutional review boards at both study hospitals.
Study Setting and Population
Study sites
We included one university hospital that has a residency training program in emergency medicine (Hospital 1), and one large community teaching hospital that contracts with a group of private practice physicians to provide emergency medical services (Hospital 2). Both hospitals were selected for this study based on the following criteria: 1) a large annual volume of ED patients, including a substantial proportion of uninsured patients who lack regular access to primary care; 2) an organizational culture that promotes quality improvement; and 3) support from the ED physician directors and nursing leadership for this project. With regard to criterion 1, the annual volumes of adult ED patients in Hospitals 1 and 2 were 39,573 and 29,418 (with 25% and 30% requiring hospitalization), and the proportions of uninsured patients were 10% and 7% at the outset of the study, respectively.
Patient inclusion and exclusion criteria
We enrolled a convenience sample of adult smokers, aged 18 years or older, who presented to the ED by private vehicle or as walk-ins. Although very light smokers can potentially benefit from quitting,26 we excluded those who smoked five or fewer cigarettes per day as these smokers tend not to experience nicotine withdrawal,27 and the proposed intervention was unlikely to be perceived as having much relevance for them. Additional exclusion criteria include acute medical decompensation (e.g., acute respiratory failure requiring intubation, cardiac arrest, cardiogenic or septic shock), life-threatening trauma, altered mental status, dementia, language barrier, incarceration, transfer to another ED, departure from the ED prior to evaluation, inability to be contacted by telephone, uncontrolled psychiatric disorder or psychiatric emergency (including suicide attempt or suicidal ideation, homicidal ideation, acute psychosis), sexual assault, and prior enrollment in this study. No patient was included unless he or she was able to provide informed consent and agreed to be contacted by telephone during follow-up. All eligible patients were invited to participate in the study and interviewed regardless of their willingness to quit.
Clinician inclusion and exclusion criteria
All staff nurses, physicians, and physician assistants (PAs) who provided direct patient care in the ED were eligible. “Float” nurses and nursing assistants were excluded.
Study Protocol
Implementation Intervention
Training of ED staff
The evidence in non-ED settings suggests that counseling by multiple clinicians produces better results than counseling by a single clinician.12,28 Thus, the intervention included training of emergency nurses, EPs, and PAs, to provide brief cessation counseling based on the 5As. ED staff were solely responsible for providing brief smoking cessation counseling – no counseling was provided by members of the research team. Nurses were instructed to perform the smoking assessment and counseling in two to three minutes on average, and to document cessation counseling in the medical record; although brief, this is consistent with the amount of time that is typically available to ED nurses for cessation counseling in practice. Given their other responsibilities, EPs were trained to reinforce nurse counseling (e.g., by providing a tailored stop smoking message) and to prescribe pharmacotherapy for smoking cessation when appropriate. Each ED nurses and EP also received a pocket card showing the study algorithm (Data Supplement, available online), and was instructed on how to recognize and manage resistance to behavior change.29,30 Consistent with principles of motivational interviewing, which has been shown to increase cessation rates,31 staff were encouraged to adopt a directive, client-centered approach in an effort to help patients recognize and resolve ambivalent feelings about cigarette use. Staff were trained to elicit and strengthen motivation and commitment through the use of “change talk,” in which the patient (rather than the nurse or physician) makes his or her own case for quitting smoking. Face-to-face training was supplemented by a 45-minute online tutorial, which provided an overview of the stages of change, key elements of brief cessation counseling12,18,32 and pharmacotherapy, and a demonstration of brief counseling technique.
Training was adapted based on the scheduling constraints and training preferences of both groups. Classroom training was impractical for the nurses, who rarely convened for didactic instruction at each site; in contrast, physicians at both sites met routinely for a departmental staff conference and business meeting and preferred large group training. Thus, a single instructor met with each nurse for approximately 20 minutes, highlighted gaps in performance of the 5As (based on aggregate data collected during the baseline phase), discussed how to deliver a stage-appropriate cessation message (using role-play scenarios), and explained how to prepare a referral to Quitline Iowa (state tobacco quitline) for appropriate patients.33 The same instructor also provided EPs and PAs with a brief didactic lecture, during which he reviewed baseline 5As data, discussed the principles of brief cessation counseling, and provided prescribing instructions for smoking cessation pharmacotherapy (Data Supplement). Physicians and nurses were also trained to complete a prior authorization form for Medicaid patients, who were eligible for one free course of nicotine replacement therapy (NRT) or varenicline annually (a covered benefit at the time of this study).
Charting/reminder tool and quick orders
We worked with each study site to modify the charting tool to include pertinent questions about smoking, and provided hands-on instruction on use of charting and referral tools. One hospital incorporated the charting tool into the electronic medical record (EMR); the other hospital prepared a separate paper worksheet for smoking cessation that was attached to the ED chart. The modified form prompted nurses to assess patients’ willingness to quit and to assist patients in quitting. At repeated ED visits by patients during the intervention period, ED nurses were instructed to ascertain whether there was any interim change in smoking status, willingness to quit, or quit attempts, and to customize their brief counseling message accordingly. Posters that emphasized delivery of the 5As were also displayed prominently throughout the ED (and were adapted for each site). To facilitate prescribing of recommended pharmacotherapy, computerized “quick orders” for these medications (with prefilled dose, duration, and patient instructions) were created at each site.
Organizational support and feedback
To ensure attendance at tutorial sessions, the ED medical director and director of nursing endorsed the goals of the training program and strongly encouraged participation in training.34 Alignment of clinicians and management increases the likelihood that an intervention will be successfully integrated into practice.35 The nurse manager at each site designated a nurse facilitator, who was responsible for serving as a liaison between the study team and nurses (e.g., helping to facilitate scheduling of training and feedback sessions), providing informal coaching to nurses (e.g., use of the charting tool, patient education materials), and troubleshooting. The primary investigator regularly followed up with the nurse facilitator during the intervention period to address any problems that arose and to review feedback on performance of the 5As. Group feedback was presented during the initial training session (pre-intervention data) and periodically throughout the intervention period. Suggestions to improve the implementation strategy were solicited during feedback sessions.
Screening and enrollment
Every adult patient was screened for eligibility by medical record review and brief screening questionnaire by one of several study site research assistants (RAs), who were stationed in the ED for a total of 40 hours per week (between 7 AM to 11 PM), including weekend days. After obtaining informed consent, the RA administered a baseline interview to assess sociodemographic factors, overall health status, alcohol use, and smoking-related variables (e.g., prior diagnosis of smoking-related illnesses, patient’s perceived relatedness of the ED encounter to smoking status36). We assessed the patient’s readiness to quit smoking using the Contemplation Ladder, an 11-point instrument designed to assess a smoker’s readiness to quit on a continuum ranging from having no thoughts about quitting to being actively engaged in quitting (range 0 to 10); it has been shown to independently predict quit attempts,37 and has been previously used in ED patients.38 We assessed nicotine dependence using the Fagerstrom Test for Nicotine Dependence (FTND), a six-item self-report measure that has been shown to predict biochemical measures of smoking (exhaled carbon monoxide, salivary cotinine),39 has fair internal consistency reliability,40 and has been previously used in ED patients.7,41 We used a single item to assess social support for quitting on a five-point Likert scale: “If you were to stop smoking, how helpful would the people closest to you be?”42 We assessed depressed mood using the Patient Health Questionnaire nine question depression module (PHQ-9); a score of ≥10 had a sensitivity of 88% and a specificity of 88% for major depression in a primary care population (when compared to a structured clinical interview by a mental health professional).43 The RA also obtained complete contact information (home and work phone, cell phone, and emergency contact) and asked study patients about the best time to call.
Post-visit survey
Shortly after leaving the ED (or transfer to an inpatient ward), the RAs telephoned study patients to determine whether or not the ED staff had performed the 5As; for those items that were answered affirmatively, patients were asked to specify whether the nurse, physician, or another staff member had performed the 5As. As it was not possible to blind the RAs to the period of the study (pre-intervention vs. intervention), they were trained to administer the post-visit survey verbatim (using a phone script). A telephone checklist was developed to capture data on the 5As. Provision of self-help literature, help in setting a quit date, or discussion of pharmacotherapy was considered to be “assistance.” Arrangement of follow-up was defined as having received a referral for quitline counseling. The site research coordinator also tracked fax referrals to Quitline Iowa during the study. We calculated a 5As composite score for each patient (ranging from 0 to 5), based on the sum of ask, assess, advise, assist, and arrange follow-up (each of which was scored as 0 or 1). To check for any global trends in substance abuse counseling during the pre-intervention and intervention periods, the RAs also questioned patients on whether a member of the ED staff had asked about alcohol drinking.
Attitudes and perceptions of emergency nurses and physicians
We administered a written pre- and post-intervention survey to ED nurses and physicians to collect descriptive information and attitudes toward smoking cessation counseling. We used a 20-item decisional balance questionnaire, which includes 10 items that reflect positive attitudes and 10 items that reflect negative attitudes toward the delivery of smoking cessation assistance; very good internal consistency reliability and discriminative validity of this instrument have been demonstrated.44 We also asked ED staff to rate their self-efficacy and their role satisfaction in helping patients to stop smoking before and after the intervention.45
To explore aspects of the work environment that might impede implementation, we also asked ED nurses about their perceptions of respect from other team members and their ratings of the adequacy of ED personnel and resources to provide high quality patient care. Team respect was measured using a eight-item subscale of the adapted Job Stress scale,46 which has been shown to have acceptable reliability and validity (as supported by its strong correlation with both organizational and professional job satisfaction,47 and prediction of nursing turnover48). The Staff Adequacy subscale of the Nursing Work Index has excellent internal consistency (alpha = 0.80); construct validity of the subscale is supported by the finding of significantly higher nurse scores in “magnet” versus “nonmagnet” hospitals.49
Data management
Using content capture software (Cardiff Enterprise version 10, Cardiff Software, Inc., Vista, CA), each data collection form was scanned, and the scanned data were cross-checked for accuracy. The data were imported into a Microsoft Access database (Microsoft Corp., Redmond, WA), and were subjected to a set of consistency and logic checks.
Data Analysis
Preliminary analysis
Pre-intervention and intervention groups were compared with respect to potential confounding variables using the two-independent-sample t-test, Wilcoxon rank-sum, or chi-square test as appropriate. We used linear regression to test for time trends in the 5As composite score, adjusting for patient covariates. Regression assumptions were checked to ensure that the model was correctly specified; homoscedasticity of errors was verified by examining plots of the residuals versus predicted values.50
Primary analyses
We hypothesized that the performance of each guideline-recommended action (5As) by ED nurses and physicians would be greater during the intervention period compared to the pre-intervention period. In our models of performance outcome (5As), we used logistic regression to compare performance across the two periods while adjusting for a set of prespecified covariates that have been associated with delivery of cessation counseling in the literature: age, sex, race, education, presence of a smoking-related condition, concern that the ED symptoms might be smoking-related, cigarettes per day, contemplation ladder (dichotomized at ≥ 8 versus < 8), and study site.5,6,51-55 Simulation studies have demonstrated that adjustment for prespecified covariates in controlled trials improves statistical power.56 Similarly, we used linear regression to compare the 5As composite score across the two periods.
We hypothesized that ED nurses and physicians would have improved decisional balance scores (higher “pros” and lower “cons” subscale scores), higher ratings of self-efficacy, and higher role satisfaction in providing cessation counseling as a result of the intervention. Thus, we compared pre- and post-intervention values of these measures using a paired t-test (or Wilcoxon signed rank test, if applicable) for those ED staff who completed both surveys.
Secondary analysis
We assessed differences between sites in response to the study intervention by testing for interaction. To avoid multiple testing, we initially evaluated the interaction term for period by site in models of the 5As composite score. If this interaction was statistically significant, we checked the period by site interaction for the individual 5As.
Missing data
Because some patients were unable to recall performance of individual counseling actions (14% of post-visit survey responders), or could not be reached for the post-visit survey (18% of study enrollees), we also conducted a multiple imputation analysis to evaluate the possible effect of missing values of the 5As.57,58 The imputation model for each “A” included the remaining non-missing “As” as well as several other variables that have been associated with smoking cessation counseling in the literature. Five imputed data sets were generated, and parameter estimates were calculated using the MICOMBINE procedure in SAS.
We used PROC GENMOD in SAS for Windows, Version 9.2 (SAS Institute, Cary, NC), and R programming language for all analyses. All models were estimated using generalized estimating equations (GEE) to account for clustering of performance measures at the ED clinician level.59 All tests were two-sided, and a p-value of ≤0.05 was defined as statistically significant; we did not adjust for multiple comparisons.
RESULTS
Patient characteristics
Table 1 summarizes the recruitment and post-visit follow-up of study patients. Approximately 70% of eligible patients during each study period agreed to participate. The proportion of enrolled subjects who completed the post-visit survey was similar during both periods (81% vs. 84%, respectively); there were no significant differences in patient characteristics between those who completed the post-visit survey (n = 650) versus those who did not (n = 139, data not shown). The median time to telephone contact was four days (IQR 1 to 7 days). Compared to pre-intervention patients, intervention patients were more likely to be female, more likely to have a smoking-related condition, and were more concerned that their acute symptoms might be related to smoking, but their smoking history, level of nicotine dependence, and contemplation ladder scores were similar (Table 2).
Table 1.
Recruitment and follow-up of patients in the pre-intervention and intervention periods.
| Variable | Pre-intervention period |
Intervention period |
|---|---|---|
| Patients screened, n | 1707 | 910 |
| Eligible patients, n | 617 | 492 |
| Enrolled, n (% of all eligible patients) | 436 (71) | 353 (72) |
| Completed post-ED interview, n (% of enrollees) |
355 (81) | 295 (84) |
Table 2.
Characteristics of ED study patients.
| Variable* | Pre-intervention (n=436) |
Intervention (n=353) |
|---|---|---|
| Age, mean (±SD) | 35.6 (±11.9) | 37.2 (±13.3) |
| Sex, % male | 49 | 39† |
| Race, % nonwhite | 12 | 11 |
| Highest grade, median (IQR) | 12 (10-13) | 12 (12-14) |
| Marital status, % married or living with companion |
37 | 37 |
| Self-rated health, % excellent-very good | 34 | 36 |
| Alcohol use in past 3 months, % | 62 | 58 |
| PHQ-9 depression score, median (IQR) | 8 (4-13) | 8 (4-13) |
| Smoking-related variables | ||
| Cigarettes per day, median (IQR) | 15 (10-20) | 15 (10-20) |
| Nicotine dependence (FTND), median (IQR)‡ | 5 (3-6) | 5 (3-6) |
| Any smoking-related condition, %§ | 31 | 38† |
| Concern that ED symptoms might be related to smoking, %* |
19 | 26† |
| Prior quit attempts (≥1 full day), median (IQR)^ |
3 (1-4) | 3 (1-5) |
| Contemplation ladder (0-10), mean (±SD) | 5.9 (±2.8) | 6.2 (±2.8) |
| Any other smoker in household, % | 60 | 65 |
p ≤ 0.05
FTND = Fagerstrom Test of Nicotine Dependence. Data were missing for 7 patients.
Prior diagnosis of any of the following conditions: coronary heart disease, congestive heart failure, stroke or transient ischemic attack, chronic obstructive lung disease, peripheral vascular disease, tobacco-related cancer (e.g., lung, oral cavity).
At least “a little bit”
Results shown for 346 and 258 pre-intervention and intervention period patients who reported any prior quit attempt, respectively
ED staff characteristics and survey results
As shown in Table 3, ED nurses had worked in the ED for a median of three years (IQR 1 to 7), and 58% were registered nurses or had attained a bachelor’s degree in nursing (the remainder had obtained an associate’s degree in nursing). Approximately 16% were current smokers (25% were former smokers). Following the intervention, 49% of ED nurses rated themselves as moderately or very effective in cessation counseling (compared to 18% prior to intervention, p = 0.0001). In addition, 47% were satisfied with their role in cessation counseling after the intervention (compared to 28% prior to intervention, p = 0.01). There was no change in nurses’ “pros” and “cons” attitudes delivering smoking cessation interventions, however (Table 4). Physicians had worked in the ED for a median of two years (IQR 1 to 6), and 28% were board certified in emergency medicine; none were current smokers (14% were former smokers). The estimated number of patients seen by EPs was 2.5 to 3.0 per hour at both study sites. EPs showed no significant changes in self-efficacy, role satisfaction in cessation counseling, or attitudes toward smoking cessation (Table 4).
Table 3.
Descriptive characteristics of emergency clinicians.*
| Hospital 1 | Hospital 2 | |||
|---|---|---|---|---|
| Characteristic | Nurses (n=55) |
Physicians (n=39) |
Nurses (n=40) |
Physicians (n=22) |
| Age, mean (±SD) | 37.5 (±9.7) | 36.5 (±7.9) | 40.9 (±11.4) | 40.3 (±10.1) |
| Sex, % male | 18 | 62 | 18 | 59 |
| Race, % white | 98 | 85 | 88 | 91 |
| Registered nurse or BSN, % | 56 | NA | 60 | NA |
| Board certified in EM, % | NA | 33 | NA | 18 |
| Total experience (years), median (IQR) | 5 (2-9) | 3 (1-7) | 5 (3-11) | 6 (1-12) |
| ED experience (years), median (IQR) | 3 (1-5) | 2 (1-6) | 4 (2-11) | 1 (1-8) |
| Smoking status, % current smoker | 19 | 0 | 13 | 0 |
BSN = Bachelors of Science in Nursing, NA = not applicable, IQR = interquartile range. The physician category includes a small number of physician assistants at each site.
Table 4.
Emergency clinicians’ attitudes toward smoking cessation counseling before and after the study intervention.*
| Nurses (n=73) | Physicians (N=49) | |||||
|---|---|---|---|---|---|---|
| Clinician variable | Pre- intervention |
Post- Intervention |
p-value† | Pre- intervention |
Post- Intervention |
p-value† |
| Decisional balance – “pros” subscale, mean (SD)‡ |
31.6 (5.6) | 32.1 (5.9) | 0.45 | 32.4 (5.6) | 33.3 (6.1) | 0.29 |
| Decisional balance – “cons” subscale, mean (SD) ‡ |
27.4 (5.1) | 27.4 (5.6) | 0.93 | 28.8 (5.5) | 27.5 (6.2) | 0.15 |
| Self-efficacy in counseling, % moderately-very effective§ |
18 | 49 | 0.0001 | 24 | 3 | 0.15 |
| Satisfaction with counseling role, % satisfied^ |
28 | 47 | 0.01 | 39 | 41 | 0.94 |
Data were missing for those clinicians who were no longer employed at the study sites at the time of the pre- and post-intervention surveys, who did not attend project meetings, or who refused to complete either survey.
Comparisons are based on the signed rank test for ordinal variables (self-efficacy in counseling, satisfaction with counseling role) and the paired t-test for continuous variables (decisional balance subscales).
One or more decisional balance items were missing for 4 and 7 ED nurses on the “pros” and “cons” subscales, respectively.
4-point scale: Very effective=3, Moderately effectively=2, Slightly effective=1, Ineffective=0
5-point scale: Very satisfied=2, Satisfied=1, Neutral=0, Somewhat dissatisfied= −1, Very dissatisfied= −2
Primary analysis
During the pre-intervention period, the majority of study patients were asked by a nurse about smoking (53%), but only 13% received any advice to quit, and less than 10% were asked about their willingness to quit or received any assistance in quitting (Table 5). There was no significant secular trend in the performance of smoking cessation counseling during the pre-intervention period at either site (based on the 5As composite score). In addition, the proportion of ED patients who were asked about alcohol use was similar during the pre-intervention and intervention periods (69.3% and 70.5%, respectively); this argues against any global improvement in substance abuse counseling during the study period.
Table 5.
Proportion of patients who received recommended counseling activities from an ED nurse or physician during the preintervention and intervention periods.
| Received ED nurse Counseling | Received Physician Counseling, % (N)* | |||||
|---|---|---|---|---|---|---|
| Pre- intervention % (N)^ |
Intervention % (N)^ |
Adj OR (95% CI), [N]# |
Pre- intervention % (N)^ |
Intervention % (N)^ |
Adj OR (95% CI), [N] |
|
| Ask about smoking, % | 52.8 (320) | 67.9 (280) | 2.0 (1.3-2.9), [591] | 41.5 (323) | 46.6 (268) | 1.2 (0.87-1.7), [586] |
| Advice to quit, % | 12.6 (341) | 18.1 (287) | 1.5 (0.96-2.4), [618] | 17.9 (341) | 23.7 (287) | 1.4 (0.97-2.0), [607] |
| Assess willingness to quit, % | 8.8 (341) | 31.4 (280) | 4.8 (2.9-7.9), [611] | 9.9 (342) | 21.9 (269) | 2.5 (1.7-3.8), [623] |
| Assist in quitting, % | 5.7 (353) | 22.5 (292) | 5.1 (2.7-9.5), [635] | 5.1 (353) | 18.4 (288) | 4.2 (1.9-9.1), [636] |
| Given self-help literature, % | 2.3 (350) | 14.7 (286) | 8.0 (3.3-19.3), [626] | 0.3 (350) | 4.6 (280) | 17.0 (2.1-136), [628]¥ |
| Discuss pharmacotherapy, % | 4.0 (354) | 16.7 (293) | 4.9 (2.7-9.0), [637] | 4.5 (354) | 17.9 (290) | 4.6 (2.1-9.9), [639] |
| Arrange follow-up, % | 1.1 (354) | 7.2 (293) | 7.1 (2.3-21.4), [637] | 0.9 (353) | 4.5 (292) | 5.5 (1.8-17), [643]¥ |
The physician category includes a small number of physician’s assistants at each site.
The pre- and post-intervention numbers in parentheses are the number of cases available for calculation of 5As results (without multivariable adjustment).
Adj OR = adjusted odds ratio (with 95% confidence interval). Comparisons are based on logistic regression models, estimated using generalized estimating equations. All models were adjusted for age, sex, race, education, presence of a smoking-related condition, concern that the ED symptoms might be smoking-related, cigarettes smoked per day, contemplation ladder score, and study site. The number of cases with complete data in each regression model is shown in brackets; ED nurse and physician could not be identified for 7 and 2 post-visit survey completers, respectively.
Adjusted for site only (fully-adjusted model did not converge).
During the intervention period, more study patients were asked by ED nurses about smoking (adjusted OR = 2.0, 95% CI = 1.3 to 2.9), asked about willingness to quit (adjusted OR = 4.8, 95% CI = 2.9 to 7.9), assisted in quitting (adjusted OR = 5.0, 95% CI = 2.7 to 9.3), and had arrangements for follow-up cessation counseling (adjusted OR =7.1, 95% CI = 2.3 to 21). Patients were not more likely to be advised to quit during the intervention period (adjusted OR = 1.5, 95% CI = 0.96 to 2.4). Assistance in quitting was largely comprised of providing self-help material and discussing pharmacotherapy; few patients received help in setting a quit date (<2%). We observed smaller increments in performance of the 5As across the board for physicians (Table 5), which may reflect the fact that these clinicians received less personalized training and attention than nurses. Nevertheless, significantly more patients reported that a physician assessed their willingness to quit, assisted them with quitting, and arranged follow-up during the intervention period. In our analysis of missing data, the results of multiple imputation were very similar to those obtained using complete case analysis, except that the intervention effect for “Advice to quit (nurses)” attained statistical significance (adjusted OR = 1.6, 95% CI = 1.0 to 2.6).
There was some turnover of emergency nurses and physicians during the study, which could potentially bias estimates of intervention effect if there were significant differences in clinician attributes between the two periods (e.g., job satisfaction, motivation). To minimize the potential effect of unbalanced clinician covariates between study periods, we repeated our analysis of the 5 As in the subsets of nurses and physicians who had treated study patients during both periods. These results were similar to those observed in the full sample of clinicians (data not shown).
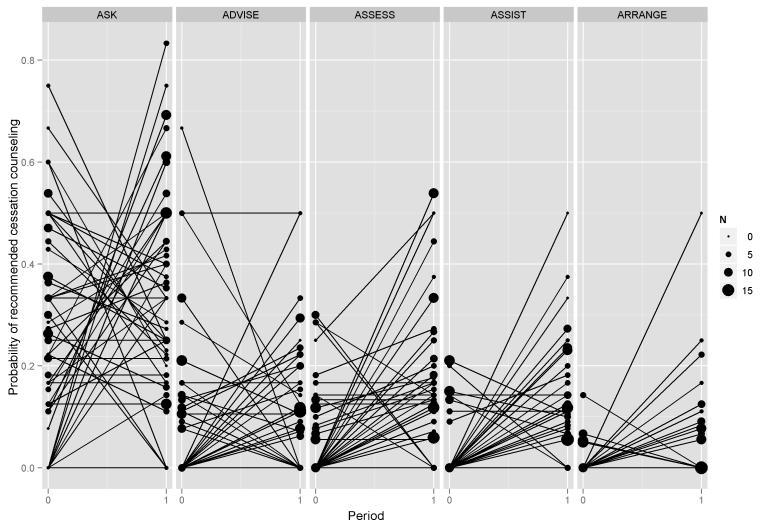
Closer inspection of the data for individual nurses revealed considerable variability in delivery of cessation counseling (Figure 2). In a post-hoc comparison of those nurses whose 5 As composite score increased versus those whose score decreased, we did not identify any significant differences in age, experience, or attitudes toward smoking cessation between these two groups (data not shown). Similar results were observed for physicians.
Figure 2.
Change in nurse performance of the 5As.
Results are shown for each ED nurse with evaluable study patients during both pre-intervention (0) and intervention (1) periods (N = 60 for Ask, N = 61 for all other As). The size of each data point corresponds to the number of patients seen by each ED nurse during each period.
Secondary analysis
Another source of variability in response to the intervention was study site. We observed a larger improvement in the mean 5As composite score for nurses at Hospital 2 versus Hospital 1 (1.14 vs. 0.26, p < 0.0001 for the period × site interaction). The change in composite score for physicians was not different between hospitals (0.60 vs. 0.19, p=0.07 for the period × site interaction). Closer evaluation of the individual “As” for nurses showed greater improvements in “ask” and “assess” during the intervention phase at Hospital 2 compared to Hospital 1: 22% vs. 8% for “ask” (p = 0.019, for period × site interaction), and 41% vs. 9% for “assess” (p < 0.0001, for period × site interaction). Additional analyses showed similar improvements in nurses’ self-efficacy and role satisfaction at both sites. Nurses’ perceptions of the adequacy of staffing and resources and professional respect from other team members were also similar at both sites. There were no significant differences between study sites in nurses’ or physicians’ future intentions to change cessation practices.
DISCUSSION
Despite recommendations for ED clinicians to follow national smoking cessation guidelines,11,60 only a minority of ED patients who smoke receive advice to quit or any assistance in quitting.61 The effectiveness of an ED-based smoking cessation program depends on the well-coordinated delivery of brief yet personalized cessation counseling by trained ED personnel to appropriately selected patients under certain conditions,62 but there is relatively little guidance on how to implement “best evidence” on smoking cessation in the ED. There is also some debate about the scope of cessation counseling in the ED, with some experts advocating an abbreviated “Ask-Advise-Refer” model as an alternative to the 5As.63
This quasi-experimental trial provides empirical support for the use of a nurse-initiated strategy (based on the 5As framework) to deliver brief cessation counseling to all smokers in the ED, and is consistent with expert recommendations that call for nursing staff to play a larger role in delivering public health interventions in the ED.64 Compared to the pre-intervention period, a significantly greater proportion of ED patients received recommended counseling activities during the intervention. The availability of context-specific training and smoking cessation resources enabled ED nurses to take a more active role in cessation counseling (and to operate within the time constraints of the ED). Following the intervention, ED nurses reported greater self-efficacy and role satisfaction in cessation counseling, both of which relate to the staff member’s beliefs about his or her ability to perform the behavior (perceived behavioral control).65,66 In contrast, EPs showed little change in their attitudes during the intervention period.
There was substantial variability in the responses of ED nurses and physicians to the intervention. In both periods, we observed that ED staff were more likely to ask about smoking and to assess willingness to quit than to advise or assist with quitting. The apparent reluctance of clinicians to advise patients to quit has been reported previously,55,67 and may be related to lack of training and self-confidence in cessation counseling. The substantial falloff in performance between “assess” and “assist” may reflect the fact that emergency clinicians are reserving their time and effort for selected patients (e.g., those with tobacco-related conditions) who are most likely to benefit from cessation in their judgment, or whom they perceive to be more ready to quit. In many cases, however, patients expressed an interest in quitting, but were not offered a referral for cessation counseling or pharmacotherapy; rather, the dialogue tended to focus on reinforcing smoking-related health risks and gathering data.
A possible reason for the gap in prescribing medication is physicians’ discomfort in prescribing long-term psychoactive medications that they believe would be more appropriately prescribed by a primary care provider who has an established relationship with the patient. Unfortunately, many ED patients do not have an established relationship with a primary care provider. Providing emergency medicine residents and staff with more formal training on use of pharmacotherapy for smoking cessation, implementing ED “quick orders” for these medications, and improved communication with primary care68 may help to change the mindset of EPs with regard to prescribing recommended smoking cessation medications.
We also observed differential effects of the intervention for two of the 5As. Although our survey data did not reveal a specific explanation for this site-by-period interaction, several factors may account for this finding: 1) competing interventions in the ED – one site was preparing for deployment of a new electronic medical record during the intervention period (and thus may have had less “adaptive reserve” for change), 2) variable involvement of nurse facilitators – at one site, the nurse facilitator appeared to take greater responsibility for implementation of the study intervention, and 3) EM residents provided a large proportion of ED care at one of the two sites – participation of the residents in smoking cessation training was variable on account of work/rotation schedules. Contextual factors related to the practice environment exert an important influence on the response of clinical staff to implementation of evidence-based care strategies.69,70
Few published studies have addressed the delivery of smoking cessation interventions by ED nurses and physicians. Two randomized controlled trials showed no benefit of brief physician advice coupled with referral for outpatient (face-to-face) tobacco use counseling;41,71 however, neither of these studies provided sufficient detail to judge whether the cessation intervention was implemented with high fidelity, nor did they report the characteristics of those delivering the intervention.24 A recent pre-post study in eight EDs evaluated the effect of an educational intervention (1-hour didactic session on use of the “Ask-Advise-Refer” model, coupled with quit line referral cards), and reported significant improvement in physicians’ counseling and referral of tobacco users.55 In another intervention study, a gift incentive for ED staff significantly increased referrals of smokers to an onsite counseling intervention, but staff performance of other cessation counseling activities was not reported.72 Several additional studies have investigated the feasibility and effectiveness of ED-based smoking cessation interventions delivered by non-clinical personnel with varying levels of success.38,73-75 None of the above intervention studies included ED prescribing of smoking cessation pharmacotherapy, which may have limited their effect on cessation rates. Future research should determine how to adapt smoking cessation strategies for different EDs based on their organizational readiness and adaptive reserve,35,76 and how to promote teamwork between ED nurses and physicians in delivering cessation counseling.77 We are currently evaluating whether improvements in delivery of the 5As translate into meaningful improvements in cessation rates.
LIMITATIONS
Several limitations of this study deserve further comment. First, lack of a concomitant control group makes it difficult to rule out secular trends (e.g., the release of new smoking cessation aids or hospital policies) or maturation effects (changes in staff performance related to the evolution of clinical skills) as an explanation for improvements in the 5As during this study.25 We note, however, that there were no secular changes in patient volume, patient acuity (as measured by the proportion of ED patients requiring admission), patient load (as measured by the ratio of ED patients to physicians), or concurrent quality improvement directives that might account for the increase in cessation counseling during the intervention period. In addition, delivery of the 5As and assessment of alcohol use (a marker of substance abuse counseling) remained stable during the pre-intervention period at each site.
Second, performance of the 5As may have been greater if we had provided more intensive training to physicians, and had focused on improving communication and teamwork between ED nurses and physicians.
Third, data on receipt of smoking cessation counseling were based on self-report. Although direct observation of patient encounters is often considered the “gold standard,” patient recall has been shown to be reasonably accurate in clinical practice (sensitivity 92%, specificity 82% for advice to quit).78
Fourth, approximately 20% of study enrollees did not provide data for the post-visit survey, despite efforts to obtain complete contact information from subjects (home and work phone, cell phone, and emergency contact) at the time of enrollment.79,80 High attrition has been well documented in ED populations on account of subjects providing inaccurate phone numbers, disconnecting their phones, or refusing to answer phone calls.33,81 To enhance follow-up, a member of the research team (JH) used multiple search strategies to track down study patients with non-working telephone numbers, including a paid search service (Intellius, Inc., Bellevue, WA).82
Fifth, we did not collect data on the actual amount of time that nurses or physicians spent on smoking cessation counseling. Finally, it is not clear whether the intervention would have been as effective in unselected EDs that had less interest in smoking cessation or less support from ED leadership.
CONCLUSIONS
The approximately 25 million visits by smokers to U.S. EDs annually83 represent an under-utilized opportunity to encourage patients to stop smoking and to provide them with assistance in quitting. We found that ED staff can effectively deliver smoking cessation counseling in a time-efficient manner, and in so doing, can help attain the public health goal of reducing the prevalence of smoking in the United States to 12% by 2020.84
Supplementary Material
Acknowledgments
The authors thank those who provided research assistance throughout the study: Sheryl Eastin, RN, Margaret Graham, MS, Rose Kim, MPH, Cassie Cunningham, Jennifer Carroll, RN, Yara Dahud, MS, Kadian Mijic, RN, and Maureen Myshock, MPH, MHA. We also thank George Bailey, MS, for assisting with database design, and Erin Greve for assisting with data entry. We are especially grateful for the assistance of the nurse and physician assistant facilitators and nurse managers who served as liaisons to the study team: Shukrije Arifi, RN, Wendy Gerard, RN, Pat Bott, RN, Alfred Belinsky, RN, Elizabeth Finch, RN, and Rebecca Copeland, PA. We also thank Lori Wright for administrative support and Alicia Denman for assistance with manuscript preparation.
Sources of support: National Institute of Drug Abuse (R21 DA021607), Holden Comprehensive Cancer Center (Population Science Pilot Grant)
Footnotes
Presentations: Society for Medical Decision Making Annual Meeting, October 2010, Toronto, Ontario, Canada
REFERENCES
- 1.Center for Disease Control Vital Signs: current cigarette smoking among adults aged > 18 years -- United States, 2009. MMWR Morb Mortal Wly Rep. 2010;59(35):1135–40. [PubMed] [Google Scholar]
- 2.Lowenstein S, Koziol-McLain J, Thompson M, et al. Behavioral risk factors in emergency department patients: a multisite survey. Acad Emerg Med. 1998;5:781–7. doi: 10.1111/j.1553-2712.1998.tb02504.x. [DOI] [PubMed] [Google Scholar]
- 3.Rhodes K, Gordon J, Lowe R, for the Society for Academic Emergency Medicine Public Health and Education Task Force Preventive Services Work Group Preventive care in the emergency department, Part I: clinical preventive services--are they relevant to emergency medicine? Acad Emerg Med. 2000;7:1036–41. doi: 10.1111/j.1553-2712.2000.tb02097.x. [DOI] [PubMed] [Google Scholar]
- 4.McBride C, Emmons K, Lipkus I. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res. 2003;18(2):156–70. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- 5.Bock BC, Becker B, Niaura R, Partridge R. Smoking among emergency chest pain patients: motivation to quit, risk perception and physician intervention. Nicotine Tob Res. 2000;2:93–6. doi: 10.1080/14622200050011358. [DOI] [PubMed] [Google Scholar]
- 6.Bock BC, Becker B, Monteiro R, Partridge R, Fisher S, Spencer J. Physician intervention and patient risk perception among smokers with acute respiratory illness in the emergency department. Prev Med. 2001;32(2):175–81. doi: 10.1006/pmed.2000.0799. [DOI] [PubMed] [Google Scholar]
- 7.Boudreaux ED, Hunter GC, Bos K, Clark S, Carmago CA., Jr. Predicting smoking stage of change among emergency department patients and visitors. Acad Emerg Med. 2006;13:39–47. doi: 10.1197/j.aem.2005.07.030. [DOI] [PubMed] [Google Scholar]
- 8.Lowenstein S, Tomlinson D, Koziol-McLain J, Prochazka A. Smoking habits of emergency department patients: an opportunity for disease prevention. Acad Emerg Med. 1995;2:165–71. doi: 10.1111/j.1553-2712.1995.tb03189.x. [DOI] [PubMed] [Google Scholar]
- 9.Klinkhammer M, Patten C, Sadosty A, Stevens S, Ebbert J. Motivation for stopping tobacco use among emergency department patients. Acad Emerg Med. 2005;12:568–71. doi: 10.1197/j.aem.2004.11.027. [DOI] [PubMed] [Google Scholar]
- 10.Rodrigues R, Kreider W, Baraff L. Need and desire for preventive care measures in emergency department patients. Ann Emerg Med. 1995;26(5):615–20. doi: 10.1016/s0196-0644(95)70014-5. [DOI] [PubMed] [Google Scholar]
- 11.Bernstein S, Becker B. Preventive care in the emergency department: diagnosis and management of smoking and smoking-related illness in the emergency department: a systematic review. Acad Emerg Med. 2002;9:720–9. doi: 10.1111/j.1553-2712.2002.tb02153.x. [DOI] [PubMed] [Google Scholar]
- 12.Fiore M, Bailey W, Cohen S, et al. Clinical Practice Guideline. US Department of Health and Human Services, US Public Health Service; Rockville, MD: 2008. Treating tobacco use and dependence. [Google Scholar]
- 13.Jaen CR, Crabtree BF, Zyzanski SJ, Goodwin MA, Stange KC. Making time for tobacco cessation counseling. J Fam Pract. 1998;46(5):425–8. [PubMed] [Google Scholar]
- 14.Prochaska JO, Koziol-McLain J, Tomlinson D, Lowenstein S. Smoking cessation counseling by emergency physicians: opinions, knowledge, and training needs. Acad Emerg Med. 1995;2:211–6. doi: 10.1111/j.1553-2712.1995.tb03201.x. [DOI] [PubMed] [Google Scholar]
- 15.Tong EK, Strouse R, Hall J, Kovac M, Schroeder SA. National survey of U.S. health professionals’ smoking prevalence, cessation practices, and beliefs. Nicotine Tob Res. 2010;12(7):724–32. doi: 10.1093/ntr/ntq071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stone EG, Morton SC, Hulscher ME, et al. Interventions that increase use of adult immunization and cancer screening services: a meta-analysis. Ann Intern Med. 2002;136(9):641–51. doi: 10.7326/0003-4819-136-9-200205070-00006. [DOI] [PubMed] [Google Scholar]
- 17.Mojica WA, Suttorp MJ, Sherman SE, et al. Smoking-cessation interventions by type of provider: a meta-analysis. Am J Prev Med. 2004;26(5):391–401. doi: 10.1016/j.amepre.2004.02.014. [DOI] [PubMed] [Google Scholar]
- 18.Green JS, Briggs L. Tobacco cessation in acute and critical care nursing practice: challenges and approaches. Crit Care Nurs Clin North Am. 2006;18:81–93. doi: 10.1016/j.ccell.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 19.Whitlock EP, Orleans CT, Pender N, Allan J. Evaluating primary care behavioral counseling interventions: an evidence-based approach. Am J Prev Med. 2002;22(4):267–84. doi: 10.1016/s0749-3797(02)00415-4. [DOI] [PubMed] [Google Scholar]
- 20.McCarty M, Hennrikus D, Lando H, Vessey J. Nurses’ attitudes concerning the delivery of brief cessation advice to hospitalized smokers. Prev Med. 2001;33:674–81. doi: 10.1006/pmed.2001.0944. [DOI] [PubMed] [Google Scholar]
- 21.Solberg L, Brekke M, Kottke T. How important are clinician and nurse attitudes to the delivery of clinical preventive services? J Fam Pract. 1997;44:451–61. [PubMed] [Google Scholar]
- 22.Williams GC, Levesque C, Zeldman A, Wright S, Deci EL. Health care practitioners’ motivation for tobacco-dependence counseling. Health Educ Res. 2003;18(5):538–53. doi: 10.1093/her/cyf042. [DOI] [PubMed] [Google Scholar]
- 23.Berwick D. Disseminating innovations in health care. JAMA. 2003;289(15):1969–75. doi: 10.1001/jama.289.15.1969. [DOI] [PubMed] [Google Scholar]
- 24.Glasgow RE, Magid DJ, Beck A, Ritzwoller D, Estabrooks PA. Practical clinical trials for translating research to practice: design and measurement recommendations. Med Care. 2005;43(6):551–7. doi: 10.1097/01.mlr.0000163645.41407.09. [DOI] [PubMed] [Google Scholar]
- 25.Shadish W, Cook T, Campbell D. Experimental and quasi-experimental designs for generalized causal inference. Houghton Mifflin; Boston, MA: 2002. [Google Scholar]
- 26.Vollset SE, Tverdal A, Gjessing HK. Smoking and deaths between 40 and 70 years of age in women and men. Ann Intern Med. 2006;144:381–9. doi: 10.7326/0003-4819-144-6-200603210-00004. [DOI] [PubMed] [Google Scholar]
- 27.Shiffman S, Paty JA, Gnys M, Kassel JD, Elash C. Nicotine withdrawal in chippers and regular smokers: subjective and cognitive effects. Health Psychol. 1995;14:301–9. doi: 10.1037//0278-6133.14.4.301. [DOI] [PubMed] [Google Scholar]
- 28.An LC, Foldes SS, Alesci NL, et al. The impact of smoking-cessation intervention by multiple health professionals. Am J Prev Med. 2008;34:54–60. doi: 10.1016/j.amepre.2007.09.019. [DOI] [PubMed] [Google Scholar]
- 29.Miller W, Rollnick S. Motivational interviewing. Guilford Press; New York, NY: 1991. [Google Scholar]
- 30.Rollnick S, Mason P, Butler C. Health behavior change: a guide for practitioners. Churchill Livingstone; New York, NY: 2000. [Google Scholar]
- 31.Lai DT, Cahill K, Qin Y, Tang JL. Motivational interviewing for smoking cessation. Cochrane Database Syst Rev. 2010;20(1):CD006936. doi: 10.1002/14651858.CD006936.pub2. [DOI] [PubMed] [Google Scholar]
- 32.Goldberg D, Hoffman A, Anel D. Understanding people who smoke and how they change: a foundation for smoking cessation in primary care, part 2. Dis Mon. 2002;48(7):445–85. doi: 10.1067/mda.2002.129141. [DOI] [PubMed] [Google Scholar]
- 33.Schiebel NEE, Ebbert JO. Quitline referral vs. self-help manual for tobacco use cessation in the emergency department: a feasibility study. BMC Emerg Med. 2007;7:e15. doi: 10.1186/1471-227X-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wise C, Billi J. A model for practice guideline adaptation and implementation: empowerment of the physician. Jt Comm J Qual Improv. 1995;21:465–76. doi: 10.1016/s1070-3241(16)30173-0. [DOI] [PubMed] [Google Scholar]
- 35.Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidu O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82(4):581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boudreaux ED, Baumann BM, Friedman K, Ziedonis DM. Smoking stage of change and interest in an emergency department-based intervention. Acad Emerg Med. 2005;12:211–8. doi: 10.1197/j.aem.2004.09.022. [DOI] [PubMed] [Google Scholar]
- 37.Biener L, Abrams D. The contemplation ladder: validation of a measure of readiness to consider smoking cessation. Health Psychol. 1991;10(5):360–5. doi: 10.1037//0278-6133.10.5.360. [DOI] [PubMed] [Google Scholar]
- 38.Bock B, Becker B, Niaura R, Partridge R, Fava J, Trask P. Smoking cessation among patients in an emergency chest pain observation unit: outcomes of the Chest Pain Smoking Study (CPSS) Nicotine Tob Res. 2008;10(10):1523–31. doi: 10.1080/14622200802326343. [DOI] [PubMed] [Google Scholar]
- 39.Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom test for nicotine dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict. 1991;86:1119–27. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 40.Piper ME, McCarthy D, Baker T. Assessing tobacco dependence: a guide to measure evaluation and selection. Nicotine Tob Res. 2006;8(3):339–51. doi: 10.1080/14622200600672765. [DOI] [PubMed] [Google Scholar]
- 41.Richman P, Dinowitz S, Nashed A, et al. The emergency department as a potential site for smoking cessation intervention: a randomized, controlled trial. Acad Emerg Med. 2000;7:348–53. doi: 10.1111/j.1553-2712.2000.tb02235.x. [DOI] [PubMed] [Google Scholar]
- 42.Rigotti NA, Arnsten JH, McKool KM, Wood-Reid KM, Pasternak R, Singer DE. Efficacy of a smoking cessation program for hospital patients. Arch Intern Med. 1997;157:2653–60. [PubMed] [Google Scholar]
- 43.Kroenke K, Spitzer R, Williams J. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Park E, Eaton CA, Goldstein MG, et al. The development of a decisional balance measure of physician smoking cessation interventions. Prev Med. 2001;33:261–7. doi: 10.1006/pmed.2001.0879. [DOI] [PubMed] [Google Scholar]
- 45.Katz D, Muehlenbruch D, Brown R, Fiore M, Baker T. Effectiveness of implementing the Agency for Healthcare Research and Quality Smoking Cessation clinical practice guideline: a randomized controlled trial. J Nat Cancer Inst. 2004;96:594–603. doi: 10.1093/jnci/djh103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hinshaw A, Atwood J. Final report: National Institute of Health. National Center for Nursing Research; Bethesda MD: 1985. Anticipated turnover among nursing staff study. No. R01NU00908. [Google Scholar]
- 47.Leveck M, Jones C. The nursing practice environment, staff retention, and quality of care. Res Nurs Health. 1996;19:331–43. doi: 10.1002/(SICI)1098-240X(199608)19:4<331::AID-NUR7>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 48.Shader K, Broome ME, Broome CD, West ME, Nash M. Factors influencing satisfaction and anticipated turnover for nurses in an academic medical center. JONA. 2001;31(4):210–6. doi: 10.1097/00005110-200104000-00010. [DOI] [PubMed] [Google Scholar]
- 49.Lake ET. Development of the Practice Environment Scale of the Nursing Work Index. Res Nurs Health. 2002;25:176–88. doi: 10.1002/nur.10032. [DOI] [PubMed] [Google Scholar]
- 50.Neter J, Kutner M, Nachtsheim C, Wasserman W. Applied Linear Statistical Models. 4th ed Irwin; Homewood, IL: 1996. [Google Scholar]
- 51.Goldstein M, Niaura R, Willeylessne C, et al. Physicians counseling smokers-a population-based survey of patients perceptions of health care provider-delivered smoking cessation interventions. Arch Intern Med. 1997;157:1313–9. doi: 10.1001/archinte.157.12.1313. [DOI] [PubMed] [Google Scholar]
- 52.McBride P, Plane M, Underbakke G, Brown R, Solberg L. Smoking screening and management in primary care practices. Arch Fam Med. 1997;6:165–72. doi: 10.1001/archfami.6.2.165. [DOI] [PubMed] [Google Scholar]
- 53.Thorndike AN, Rigotti NA, Stafford RS, Singer DE. National patterns in the treatment of smokers by physicians. JAMA. 1998;279(8):604–8. doi: 10.1001/jama.279.8.604. [DOI] [PubMed] [Google Scholar]
- 54.Wilson A, Hippisley-Cox J, Coupland C, Coleman T, Britton J, Barrett S. Smoking cessation treatment in primary care: prospective cohort study. Tob Control. 2005;14(4):242–6. doi: 10.1136/tc.2004.010090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bernstein SL, Boudreaux ED, Cabral L, et al. Efficacy of a brief intervention to improve emergency physicians’ smoking cessation counseling skills, knowledge, and attitudes. Subst Abuse. 2009;30:158–81. doi: 10.1080/08897070902802117. [DOI] [PubMed] [Google Scholar]
- 56.Hernández AV, Steyerberg EW, Habbema DF. Covariate adjustment in randomized controlled trials with dichotomous outcomes increases statistical power and reduces sample size requirements. J Clin Epidemiol. 2004;57:454–60. doi: 10.1016/j.jclinepi.2003.09.014. [DOI] [PubMed] [Google Scholar]
- 57.Newgard CD, Haukoos JS. Advanced Statistics: missing data in clinical research--part 2: multiple imputation. Acad Emerg Med. 2007;14:669–78. doi: 10.1197/j.aem.2006.11.038. [DOI] [PubMed] [Google Scholar]
- 58.Raghunathan TE. What do we do with missing data? Some options for analysis of incomplete data. Annu Rev Public Health. 2004;25:99–117. doi: 10.1146/annurev.publhealth.25.102802.124410. [DOI] [PubMed] [Google Scholar]
- 59.Zeger S, Liang K. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–30. [PubMed] [Google Scholar]
- 60.Bernstein S, Boudreaux ED, Cydulka RK, et al. Tobacco control interventions in the emergency department: a joint statement of emergency medicine organizations. Ann Emerg Med. 2006;48:e417–25. doi: 10.1016/j.annemergmed.2006.02.018. [DOI] [PubMed] [Google Scholar]
- 61.Vokes NI, Bailey JM, Rhodes KV. “Should I give you my smoking lecture now or later?” Characterizing emergency physician smoking discussions and cessation counseling. Ann Emerg Med. 2006;48(4):406–14. doi: 10.1016/j.annemergmed.2006.03.037. [DOI] [PubMed] [Google Scholar]
- 62.Flay B, Best J. Overcoming design problems in evaluating health behavior programs. Eval Health Prof. 1982;5:43–69. doi: 10.1177/016327878200500104. [DOI] [PubMed] [Google Scholar]
- 63.Schroeder SA. Should emergency physicians help smokers quit? Ann Emerg Med. 2006;48(4):415–6. doi: 10.1016/j.annemergmed.2006.05.023. [DOI] [PubMed] [Google Scholar]
- 64.Bernstein SL, Bernstein E, Boudreaux ED, et al. Public health considerations in knowledge translation in the emergency department. Acad Emerg Med. 2007;14:1036–41. doi: 10.1197/j.aem.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 65.Ajzen I, Fishbein M. Understanding attitudes and predicting social behavior. Prentice Hall; Englewood Cliffs, NJ: 1980. [Google Scholar]
- 66.Godin G, Belanger-Gravel A, Eccles M, Grimshaw J. Healthcare professionals’ intentions and behaviours: a systematic review of studies based on social cognitive theories. Implement Sci. 2008;3:e36. doi: 10.1186/1748-5908-3-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pipe A, Sorensen M, Reid R. Physician smoking status, attitudes toward smoking, and cessation advice to patients: an international survey. Patient Educ Couns. 2009;74(1):118–23. doi: 10.1016/j.pec.2008.07.042. [DOI] [PubMed] [Google Scholar]
- 68.Carrier E, Tracy Y, Holzwart R. [Accessed Jan 15, 2012];Coordination between emergency and primary care physicians. Research Brief No. 3: National Institute for Health Care Reform. Available at: http://www.nihcr.org/ED-Coordination.pdf.
- 69.Solberg LI. Guideline implementation: what the literature doesn’t tell us. Jt Comm J Qual Improv. 2000;26(9):525–37. doi: 10.1016/s1070-3241(00)26044-6. [DOI] [PubMed] [Google Scholar]
- 70.Rycroft-Malone J, Kitson A, Harvey G, et al. Ingredients for change: revisiting a conceptual framework. Qual Saf Health Care. 2002;11:174–80. doi: 10.1136/qhc.11.2.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Antonacci M, Eyck R. Utilization and effectiveness of an emergency department initiated smoking cessation program [abstract] Acad Emerg Med. 2000;7:1166. [PubMed] [Google Scholar]
- 72.Greenberg MR, Weinstock M, Fenimore DG, Sierzega GM. Emergency department tobacco cessation program: staff participation and intervention success among patients. J Am Osteopath Assoc. 2008;108(8):391–6. [PubMed] [Google Scholar]
- 73.Boudreaux ED, Baumann BM, Perry J, et al. Emergency department initiated treatments for tobacco (EDITT): a pilot study. Ann Behav Med. 2008;36(3):314–25. doi: 10.1007/s12160-008-9066-3. [DOI] [PubMed] [Google Scholar]
- 74.Ersel M, Kitapcioglu G, Solak ZA, Yuruktumen A, Karahalli E, Cevrim O. Are emergency department visits really a teachable moment? Smoking cessation promotion in emergency department. Eur J Emerg Med. 2010;17:73–9. doi: 10.1097/MEJ.0b013e32832e67d6. [DOI] [PubMed] [Google Scholar]
- 75.Neuner B, Weiss-Gerlach E, Miller P, Martus P, Hesse D, Spies C. Emergency department-initiated tobacco control: a randomised controlled trial in an intercity university hospital. Tob Control. 2009;18(4):283–93. doi: 10.1136/tc.2008.028753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Jaén C, Crabtree B, Palmer R, et al. Methods for evaluating practice change toward a patient-centered medical home. Ann Fam Med. 2010;8(Suppl 1):S9–20. doi: 10.1370/afm.1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Williams JM, Chinnis AC, Gutman D. Health promotion practices of emergency physicians. Am J Emerg Med. 2000;18:17–21. doi: 10.1016/s0735-6757(00)90041-x. [DOI] [PubMed] [Google Scholar]
- 78.Ward J, Sanson-Fisher R. Accuracy of patient recall of opportunistic smoking cessation advice in general practice. Tob Control. 1996;5(2):110–3. doi: 10.1136/tc.5.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Thibodeau LG, Chan L, Reilly KM, Reyes VM. Improving telephone contract rates of patients discharged from the emergency department. Ann Emerg Med. 2000;35(6):564–7. [PubMed] [Google Scholar]
- 80.Woolard RH, Carty K, Wirtz P, et al. Research fundamentals: follow-up of subjects in clinical trials: addressing subject attrition. Acad Emerg Med. 2004;11:859–66. doi: 10.1111/j.1553-2712.2004.tb00769.x. [DOI] [PubMed] [Google Scholar]
- 81.Boudreaux ED, Ary RD, St. John B, Mandry CV. Telephone contact of patients visiting a large, municipal emergency department: can we rely on numbers given during routine registration? J Emerg Med. 2000;18(4):409–15. doi: 10.1016/s0736-4679(00)00155-4. [DOI] [PubMed] [Google Scholar]
- 82.Lovell ME, Morcuende JA. Patient location strategies for pediatric long-term follow-up studies. Iowa Orthop J. 2006;26:91–5. [PMC free article] [PubMed] [Google Scholar]
- 83.McCaig L. Advance data from vital and health statistics, no. 313. National Center for Health Statistics; Hyattsville, MD: 2000. National Hospital Ambulatory Medical Care Survey: 1998 emergency department summary. [PubMed] [Google Scholar]
- 84.Center for Disease Control and Prevention [Accessed Jan 15, 2012];Healthy People 2020. Available at: http://www.healthypeople.gov/2020/default.aspx.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.