Abstract
BACKGROUND
Because Medicare Advantage plans must pay for covered services, they may design insurance benefits to appeal to healthier beneficiaries.
METHODS
We identified 11 Medicare Advantage plans that offered new fitness-membership benefits in 2004 or 2005 and matched these plans to 11 Medicare Advantage control plans that did not offer coverage for fitness memberships. Using a difference-in-differences approach, we compared the self-reported health status of persons who enrolled after the fitness benefit was added to the plan with the self-reported health status of persons entering the same plan before the fitness benefit was offered.
RESULTS
The proportion of enrollees reporting excellent or very good health was 6.1 percentage points higher (95% confidence interval [CI], 2.6 to 9.7) among the 755 new enrollees in plans that added fitness benefits than among the 4097 earlier enrollees. The proportion of new enrollees reporting activity limitation was 10.4 percentage points lower (95% CI, 6.6 to 14.3) and the proportion reporting difficulty walking was 8.1 percentage points lower (95% CI, 4.4 to 11.7), as compared with earlier enrollees. Within control plans, the differences between the 1154 new enrollees and the 3910 earlier enrollees were 1.5 percentage points or less for each measure. The adjusted differences between the fitness-benefit plans and the control plans were 4.7 percentage points higher for general health (95% CI, 0.2 to 9.2), 9.2 percentage points lower for activity limitation (95% CI, 5.1 to 13.3), and 7.4 percentage points lower for difficulty walking (95% CI, 4.5 to 10.4). These differences persisted at 2 years for activity limitation and difficulty walking.
CONCLUSIONS
Medicare Advantage plans offering coverage for fitness memberships may attract and retain a healthier subgroup of the Medicare population. (Funded by the National Institute on Aging.)
Because Health Insurers Face the Financial risk of paying for covered health services, they have a strong incentive to enroll people who are healthy rather than those who are sick.1 Health insurers can use several strategies to attract healthier (and thereby less costly) persons to their risk pool. They can deny coverage or increase premiums for high-cost populations, exclude preexisting medical conditions from coverage, or design low-value benefit packages with greater cost-sharing or other restrictions on the use of services. As a consequence of such strategies, less-healthy enrollees may be concentrated in a few plans that have escalating premiums and unstable financial viability (a phenomenon known as the “insurance death spiral”), or such persons may be excluded from purchasing health insurance altogether.1
For these reasons, policymakers have regulated some health insurance markets to mitigate the abilities of health insurance plans to engage in favorable risk selection.1–3 For example, private plans participating in the Medicare Advantage program are not permitted to deny coverage to any Medicare beneficiary and must offer benefits that are equivalent in value to the standard Medicare benefits package. Furthermore, capitated payments to plans participating in the Medicare Advantage program are adjusted for region and demographic and clinical characteristics of enrollees, so that health plans receive larger payments for enrollees with higher-than-average expected costs.4 The 2010 Affordable Care Act extended similar regulations to the individual and small-group health insurance markets.
Despite these policies, favorable selection in plans participating in the Medicare Advantage program continues to occur.5 Medicare Advantage plans, like other private insurance plans, may design and advertise particular benefits to attract a healthier subset of the Medicare population.6 Although deceptive and high-pressure marketing tactics are prohibited, selective marketing is not.7,8 Plans may selectively market their coverage to healthy or active persons by sponsoring community-based events, thereby avoiding persons who are homebound.3 They may also emphasize particular benefits that would appeal to healthier persons, such as sports medicine clinics and dental coverage, while only minimally advertising prescription-drug benefits that would appeal to persons with chronic conditions.3,9,10 Few studies, however, suggest that these strategies are successful in attracting and retaining healthier enrollees.
Insurance coverage for fitness memberships has become more common within the past several years (for both Medicare and non-Medicare plans). Prior studies have shown that physically active elderly persons who are enrolled in such fitness programs have a more favorable health profile and reduced health spending, as compared with elderly persons who do not participate in such programs.11–14 We therefore examined whether Medicare Advantage plans had favorable selection of enrollees after adding coverage for fitness memberships. Using a quasi-experimental design and a nationally representative sample of elderly Medicare beneficiaries, we compared differences in the self-reported health status of persons entering Medicare Advantage plans before and after the plans added a fitness-membership benefit with concurrent differences in matched control plans that did not alter benefit offerings.
METHODS
SOURCES OF DATA AND STUDY POPULATION
We obtained individual-level data from the Medicare Health Outcomes Survey for the years 2006 through 2008 (cohort 9). The Health Outcomes Survey collects data from a random sample of beneficiaries in all participating Medicare Advantage plans during a baseline year and then again in 2 years. The survey includes information on health status, sociodemographic characteristics, and the date each enrollee entered his or her plan. The Centers for Medicare and Medicaid Services (CMS) uses these data for public reporting on the quality of care. For cohort 9 of the Health Outcomes Survey, the survey had a baseline response rate of 69% and a follow-up response rate of 82%. The data-collection process and variables included were published by CMS.15 We also obtained annual information from CMS about each Medicare Advantage plan’s coverage for health services, including coverage for fitness memberships, from 2002 through 2008.
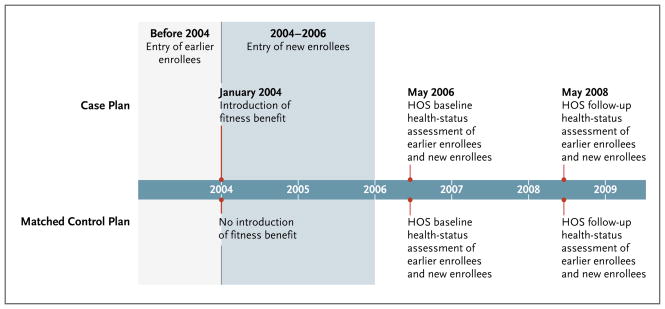
We analyzed the benefit structure of 101 Medicare Advantage plans that had participated in Medicare continuously from 2002 through 2008. We noted that, during that period, the number of plans offering fitness-membership benefits increased by a factor of more than 4 (from 14 plans in 2002 to 58 in 2008) (see Fig. 1 in the Supplementary Appendix, available with the full text of this article at NEJM.org). From this sample, we identified 11 Medicare Advantage plans (hereafter referred to as case plans) that added fitness-membership benefits in either 2004 or 2005 without altering their prescription-drug benefits or ambulatory-care copayments. These 11 case plans were subsequently matched to 11 control plans that offered no fitness-membership benefit from 2002 through 2008 and that did not change prescription-drug benefits or ambulatory-care copayments in the year in which the case plans added coverage for fitness memberships (Fig. 1). The control plans were matched to the case plans on the basis of census division, or if a match was unavailable from the same division, on the basis of census region. If a case plan could be matched to more than one control plan, a control plan was selected at random and without replacement. If a plan served as a control for one case plan, it was not eligible to be matched to any other case plan.
Figure 1. Example of Study Populations and Timelines or a Case Plan That Added a Fitness-Membership Benefit in 2004 and Its Matched Control Plan.
Shown is the study timeline for a case plan that introduced a fitness benefit in 2004 and its matched control plan. For case plans that introduced the fitness benefit in 2005, earlier enrollees were defined as those enrolled before 2005, and new enrollees as those enrolled in 2005 or 2006. All case and control plans participated in Medicare from 2002 through 2008. All beneficiaries were continuously enrolled from the time of entry into the plan until the follow-up health-status assessment in 2008. HOS denotes Health Outcomes Survey.
The analytic sample included 4852 continuously enrolled Medicare Advantage beneficiaries, 65 years of age or older, in 11 plans that added fitness-membership benefits in 2004 or 2005, and 5064 continuously enrolled Medicare Advantage beneficiaries, 65 years of age or older, in 11 matched control plans. All subjects had responded to the 2006 to 2008 Medicare Health Outcomes Survey. The study was approved by the institutional review board of Brown University.
STUDY VARIABLES
The primary outcome variables were three self-reported measures of enrollees’ health: general health (excellent, very good, good, fair, or poor), limitation in moderate activity (no limitation, some limitation, or unable to engage in moderate activity), and difficulty walking (no difficulty, some difficulty, or unable to walk). We also examined the Physical Component Summary (PCS) score — a measure of general health based on enrollees’ responses to 12 survey items. The PCS score is derived from the Veterans RAND 12-Item Health Survey (VR-12), a validated instrument developed as a shortened version of the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36).16 The VR-12 spans eight dimensions of physical and mental health and is used to measure disease burden and health-related quality of life.16,17 PCS scores range from 0 to 100, with higher scores indicating better physical health. Prior validation studies have shown that hypertension, angina, and diabetes are associated with declines in PCS scores of 0.6, 2.5, and 3.4 points, respectively, suggesting that differences of these magnitudes are clinically meaningful.18,19
Self-reports of physical health and functional status have been shown to predict mortality, health care costs, and use of health care services, even after adjustment for the presence of coexisting conditions.20–24 The addition of such self-reports of health and functional status to claims-based diagnostic models can significantly improve predictions of future health care spending, particularly for frail, elderly persons.25,26
The independent variables were an indicator for whether the plan added a fitness-membership benefit, an indicator for time of an enrollee’s entry into the plan (0 signifying an enrollment date before the benefit change, and 1 indicating an enrollment date afterward), and a term for the interaction of these two variables. Covariates included enrollee age (as a continuous variable) and sex and the year in which the fitness benefit was added.
STATISTICAL ANALYSIS
We used a difference-in-differences approach to compare the self-reported health status of enrollees who entered the plan after the fitness-membership benefit was instituted with the health status of enrollees who entered before the addition of the fitness benefit. We subtracted the difference in the proportion of enrollees reporting a given health status within control plans from the concurrent difference reported by enrollees within case plans, yielding a difference-in-differences estimate. We chose to use a difference-in-differences design because it accounts for secular trends as well as for unobserved characteristics of health plans that are independent of time.
We used generalized linear models that included the independent variables and covariates listed above, with generalized estimating equations to adjust for clustering by health plans. The models estimate the mean within-plan effect of the addition of a fitness-membership benefit on enrollee self-reported health measures. To assess whether differences in health status persisted at 2 years, we repeated the analyses using the follow-up responses to the Health Outcomes Survey. In these analyses, we used generalized estimating equations to account for clustering within health plans and repeated measurements of enrollees in the baseline and follow-up periods.
All analyses were performed with SAS software, version 9.2 (SAS Institute). Results are reported with 95% confidence intervals.
RESULTS
CHARACTERISTICS OF PLANS AND ENROLLEES
Matched pairs of case and control plans were located in all but one of the nine U.S. Census divisions (none were matched in the Pacific division). Case plans had a median Medicare contract duration of 11.0 years, and control plans had a median Medicare contract duration of 10.6 years. During the study period, case plans served a median population of 31,540 Medicare beneficiaries, and control plans served a median population of 18,241. The case and control plans were predominantly nonstaff and nongroup models; two case plans were designated group or staff model types (see the table in the Supplementary Appendix).
Enrollees in case plans were similar to enrollees in control plans with respect to age, sex, and marital status (Table 1). For the period after the benefit change, control plans had a greater proportion of black enrollees than case plans did. Enrollees in case plans, as compared with those in control plans, reported slightly higher combined family income and were more likely to report college attendance. New entrants in case plans had an increase of 5 percentage points in reported college attendance, relative to prior enrollees (P = 0.01). There was no significant difference in rates of college attendance between new enrollees and earlier enrollees in control plans. Enrollees in the case and control plans were also similar with respect to the prevalence of six common clinical diagnoses, and they had nearly identical mean numbers of coexisting conditions.
Table 1.
Characteristics of Enrollees in Medicare Advantage Case Plans, Which Added Fitness Benefits, and Medicare Advantage Control Plans.*
| Characteristic | Case Plans | Control Plans | ||||
|---|---|---|---|---|---|---|
| Earlier Enrollees (N = 4097) | New Enrollees (N = 755) | P Value | Earlier Enrollees (N = 3910) | New Enrollees (N = 1154) | P Value | |
| Age (yr) | 74.7±8.2 | 69.7±8.6 | <0.001 | 74.4±8.7 | 70.5±8.5 | <0.001 |
| Female sex (%)† | 55 | 56 | 0.41 | 55 | 55 | 0.73 |
| Race (%)† | ||||||
| White | 87 | 85 | 0.23 | 86 | 81 | <0.001 |
| Black | 9 | 11 | 11 | 16 | ||
| Other | 3 | 4 | 4 | 3 | ||
| Married (%) | 61 | 63 | 0.22 | 57 | 61 | 0.02 |
| Combined annual family income <$10,000 (%) | 10 | 10 | 0.93 | 13 | 14 | 0.26 |
| Attended college (%) | 35 | 40 | 0.03 | 32 | 32 | 0.77 |
| Coexisting conditions (no.) | 3.0±2.0 | 2.9±2.1 | 0.09 | 3.0±2.1 | 3.0±2.1 | 0.54 |
| Hypertension (%) | 65 | 62 | 0.09 | 63 | 63 | 0.74 |
| Congestive heart failure (%) | 9 | 7 | 0.21 | 8 | 7 | 0.09 |
| Myocardial infarction (%) | 12 | 11 | 0.61 | 12 | 10 | 0.27 |
| Arthritis of hip or knee (%) | 41 | 39 | 0.26 | 40 | 42 | 0.28 |
| Diabetes (%) | 22 | 25 | 0.13 | 22 | 24 | 0.07 |
| Cancer (%) | 16 | 15 | 0.77 | 14 | 13 | 0.39 |
Plus–minus values are means ±SD. Earlier enrollees were defined as those enrolled in case or control plans before the year in which the case plans introduced the fitness benefit (2004 or 2005). New enrollees were defined as those enrolled in case or control plans in the period from 2004 through 2006 (for case plans that introduced the benefit in 2004) or in the period from 2005 through 2006 (for case plans that introduced the benefit in 2005). Because of rounding, percentages may not add up to 100.
Information on sex and race was obtained from Medicare enrollment data.
SELF-REPORTED HEALTH RATINGS
In case plans, enrollees who entered after the addition of a fitness-membership benefit reported better health (proportion reporting excellent or very good health, 35.3% for new enrollees vs. 29.1% for earlier enrollees; difference, 6.1 percentage points; 95% confidence interval [CI], 2.6 to 9.7). Similarly, new enrollees in case plans were less likely than earlier enrollees to report limitations in moderate activities (proportion reporting any limitation, 45.7% vs. 56.1%; difference, −10.4 percentage points; 95% CI, −14.3 to −6.6) and difficulty walking (proportion reporting any difficulty, 25.1% vs. 33.1%; difference, −8.1 percentage points; 95% CI, −11.7 to −4.4), and they had a higher mean PCS score (41.3 vs. 39.2; difference, 2.1 points; 95% CI, 1.2 to 3.1) (Table 2). Among the 11 control plans, the differences for self-reported health, limitations in moderate activity, and difficulty in walking were 1.5 percentage points or less. The difference in PCS scores among new enrollees and earlier enrollees in control plans was 0.2 points (95% CI, −0.7 to 1.0).
Table 2.
Self-Reported Health Status of Enrollees in Medicare Advantage Case and Control Plans.
| Health Status | Case Plans | Control Plans | Difference between Case and Control Plans (95% CI)* | |||||
|---|---|---|---|---|---|---|---|---|
| Earlier Enrollees | New Enrollees | Difference (95% CI)* | Earlier Enrollees | New Enrollees | Difference (95% CI)* | Unadjusted | Adjusted | |
| Excellent or very good health | 29.1% | 35.3% | 6.1 (2.6 to 9.7) | 28.5% | 30.0% | 1.5 (−1.5 to 4.5) | 4.7 (0.2 to 9.1) | 4.7 (0.2 to 9.2) |
| Any limitation in moderate activities | 56.1% | 45.7% | −10.4 (−14.3 to −6.6) | 56.2% | 55.1% | −1.1 (−4.4 to 2.2) | −9.3 (−13.4 to −5.2) | −9.2 (−13.3 to −5.1) |
| Any difficulty walking | 33.1% | 25.1% | −8.1 (−11.7 to −4.4) | 32.4% | 31.7% | −0.8 (−3.9 to 2.4) | −7.4 (−10.3 to −4.5) | −7.4 (−10.4 to −4.5) |
| Physical Component Summary score† | 39.2 | 41.3 | 2.1 (1.2 to 3.1) | 39.2 | 39.4 | 0.2 (−0.7 to 1.0) | 2.0 (0.8 to 3.2) | 2.0 (1.0 to 3.1) |
Differences in self-reported excellent or very good health, limitation in moderate activities, or difficulty walking are expressed in percentage points. Differences in Physical Component Summary scores are expressed in points.
Scores range from 0 to 100, with higher scores indicating better physical health.
In analyses adjusted for age, sex, and the year in which case plans added the fitness benefit, the difference-in-differences estimates remained significant for all outcomes of interest. Relative to the differences in self-reported health between new enrollees and earlier enrollees in matched control plans, 8 of the 11 case plans had larger proportions of enrollees reporting excellent or very good health, 10 of the 11 had larger proportions of enrollees reporting no activity limitations, and 9 of the 11 had larger proportions of enrollees reporting that they had no difficulty walking (Fig. 2 in the Supplementary Appendix).
These patterns persisted in 2-year follow-up responses for PCS score (increase of 1.8 points [95% CI, 0.4 to 3.3] for new enrollees vs. earlier enrollees), activity limitation (decrease of 6.7 percentage points; 95% CI, −10.9 to −2.5), and difficulty walking (decrease of 10.0 percentage points; 95% CI, −14.9 to −5.1), but not for self-rated general health (increase of 1.9 percentage points; 95% CI, −3.7 to 7.5) (Table 3).
Table 3.
Self-Reported Health Status of Enrollees in Medicare Advantage Case and Control Plans at a 2-Year Follow-up Assessment.
| Health Status | Case Plans | Control Plans | Difference between Case and Control Plans (95% CI)* | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Earlier Enrollees | New Enrollees | Difference (95% CI)* | Earlier Enrollees | New Enrollees | Difference (95% CI)* | Unadjusted | Adjusted | ||
| Excellent or very good health | 29.2% | 33.5% | 4.3 (0.2 to 8.4) | 27.9% | 30.2% | 2.3 (−1.1 to 5.7) | 2.0 (−3.7 to 7.6) | 1.9 (−3.7 to 7.5) | |
| Any limitation in moderate activities | 58.5% | 49.3% | −9.5 (−13.9 to −5.0) | 60.3% | 57.6% | −2.7 (−6.4 to 1.0) | −6.8 (−11.1 to −2.6) | −6.7 (−10.9 to −2.5) | |
| Any difficulty walking | 34.9% | 23.6% | −11.2 (−15.5 to −7.0) | 34.9% | 33.7% | −1.2 (−4.8 to 2.4) | −10.1 (−14.9 to −5.3) | −10.0 (−14.9 to −5.1) | |
| Physical Component Summary score | 38.8 | 40.9 | 2.1 (1.0 to 3.2) | 38.6 | 38.9 | 0.3 (−0.6 to 1.2) | 1.8 (0.4 to 3.3) | 1.8 (0.4 to 3.3) | |
Differences in self-reported excellent or very good health, limitation in moderate activities, or difficulty walking are expressed in percentage points. Differences in Physical Component Summary scores are expressed in points.
DISCUSSION
This study examined the consequences of adding a fitness-membership benefit on the self-reported health status of enrollees in Medicare Advantage plans. Using a quasi-experimental design, we found that persons enrolling in plans after the addition of a fitness-membership benefit reported significantly better general health, fewer limitations in moderate activities, less difficulty walking, and higher PCS scores than did persons who enrolled in the same plan before the fitness benefit was added and in matched control plans that never offered a fitness benefit. These patterns persisted in the analyses of 2-year follow-up responses for all measures except self-reported general health. Our findings suggest that there is an association between the adoption of fitness-membership benefits in Medicare Advantage plans and the enrollment of healthier Medicare beneficiaries.
Our findings are consistent with the results of cross-sectional studies of benefit offerings and risk selection. Atherly et al. reported that prescription-drug benefits and vision benefits were strong predictors of the selective enrollment of less-healthy persons in Medicare+Choice (now Medicare Advantage) plans.27 Likewise, Feldman et al. found that dental benefits were associated with favorable selection in the same population.28 In contrast, hearing benefits were not associated with selective enrollment in Medicare Advantage plans.27 In a study of disenrollment from Medicare managed-care plans, Ng et al. reported that combinations of benefits can balance such selection factors; for instance, plans that offer both prescription-drug coverage and dental benefits may have a more diverse risk pool than plans that offer either of these benefits alone.29 In our study, case plans that added a fitness-membership benefit did not institute other changes to their benefit design. Therefore, it is unlikely that such competing forces influenced our findings.
These studies examined data before the Medicare program instituted an enhanced risk-adjustment payment system in 2004. Risk-adjusted payments are designed to reduce incentives for plans to avoid high-cost patients.2,4 However, the enhanced Medicare risk-adjustment model has the power to explain only 11% of the total variation in health spending. Furthermore, the model over-predicts costs for persons in good health and underpredicts costs for persons in poor health, yielding overpayments for healthy enrollees and underpayments for less-healthy enrollees.25,30 Therefore, the continued limitations of the CMS payment model may not discourage Medicare Advantage plans from engaging in risk-selective activities.6,9 Our findings are consistent with the notion that Medicare managed-care plans have continued to selectively market their benefits to healthier beneficiaries, even after the improved risk-adjustment program was instituted.
The primary limitation of our study is that Medicare beneficiaries were not randomly assigned to the case and control plans. Before the fitness-membership benefit was added to the case plans, enrollees in the case and control plans reported similar health status, and we used a quasi-experimental approach that can account for time-invariant characteristics of health plans. However, we cannot exclude the possibility that unmeasured differences between the case and control plans influenced our study findings, nor can we definitively infer causality.
Our study cannot establish the rationale underlying the decisions of Medicare Advantage plans to offer coverage for fitness memberships. The plans may have adopted such benefits for reasons that are unrelated to enrollment or retention of less costly patients. For example, offering coverage for fitness memberships may increase total market share, irrespective of the health profile of the plan’s population. Alternatively, plans may have instituted fitness-membership benefits to improve the health status or reduce the health spending of their current beneficiaries. These motives are not mutually exclusive.
We were limited to self-reported measures of health and were unable to examine health service utilization and spending. However, other studies have shown that self-reported health measures are reliable predictors of patients’ future health care use and costs.21,22,24 We did not have information relating to the enrollees’ Hierarchical Condition Category risk scores. The CMS uses these scores to calculate risk-adjusted payments to Medicare Advantage plans. However, we observed a similar prevalence of clinical conditions and a nearly identical mean number of coexisting conditions among enrollees in the case plans and those in the control plans. Our study was also limited to plans participating in the Medicare Advantage program and did not compare selective enrollment between the Medicare Advantage program and the traditional Medicare fee-for-service program.
In conclusion, we found that plans offering coverage for fitness memberships may attract and retain a healthier subset of the Medicare population. Even with important components in place to promote more balanced risk pools — standard benefits packages, risk-adjusted payment, and guaranteed coverage — some Medicare Advantage plans may engage in favorable selection by designing insurance benefits that selectively appeal to healthy persons.
Supplementary Material
Acknowledgments
Supported by grants (5RC1AG036158 and 5T32AG023482-07) from the National Institute on Aging.
We thank Vincent Mor and Ira Wilson for helpful comments on an earlier version of the manuscript.
Footnotes
The views expressed are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the U.S. government.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Cutler DM, Zeckhauser RJ. Adverse selection in health insurance. Forum Health Econ Pol. 1998;1:1–31. [Google Scholar]
- 2.Iezzoni LI, Ayanian JZ, Bates DW, Burstin HR. Paying more fairly for Medicare capitated care. N Engl J Med. 1998;339:1933–8. doi: 10.1056/NEJM199812243392613. [DOI] [PubMed] [Google Scholar]
- 3.Luft HS, Miller RH. Patient selection in a competitive health care system. Health Aff (Millwood) 1988;7(3):97–119. doi: 10.1377/hlthaff.7.3.97. [DOI] [PubMed] [Google Scholar]
- 4.Pope GC, Kautter J, Ellis RP, et al. Risk adjustment of Medicare capitation payments using the CMS-HCC model. Health Care Financ Rev. 2004;25:119–41. [PMC free article] [PubMed] [Google Scholar]
- 5.Berenson RA. Medicare disadvantaged and the search for the elusive ‘level playing field.’. Health Aff (Millwood) 2004;(Suppl Web Exclusives):W4-572–W4-585. doi: 10.1377/hlthaff.w4.572. [DOI] [PubMed] [Google Scholar]
- 6.Brown J, Duggan M, Kuziemko I, Woolston W. New evidence from the Medicare Advantage Program. College Park: University of Maryland; 2010. Can risk adjustment reduce selection in the private health insurance market? [Google Scholar]
- 7.Medicare Advantage. CMS assists beneficiaries affected by inappropriate marketing but has limited data on scope of issue. Washington, DC: Government Accountability Office; 2009. [Google Scholar]
- 8.O’Brien E, Hoadley J. Medicare Advantage: options for standardizing benefits and information to improve consumer choice. New York: The Commonwealth Fund; 2008. [PubMed] [Google Scholar]
- 9.Chandra A, Gruber J, McKnight R. Patient cost-sharing, hospitalization offsets, and the design of optimal health insurance for the elderly. Cambridge, MA: National Bureau of Economic Research; 2007. [Google Scholar]
- 10.Pizer SD, Frakt AB, Feldman R. Predicting risk selection following major changes in Medicare. Health Econ. 2008;17:453–68. doi: 10.1002/hec.1252. [DOI] [PubMed] [Google Scholar]
- 11.Benzo RP, Chang C-CH, Farrell MH, et al. Physical activity, health status and risk of hospitalization in patients with severe chronic obstructive pulmonary disease. Respiration. 2010;80:10–8. doi: 10.1159/000296504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chard SE, Stuart M. An ecological perspective on the community translation of exercise research for older adults. J Appl Gerontol. 2010 Oct 25; (Epub ahead of print) [Google Scholar]
- 13.Nguyen HQ, Ackermann RT, Maciejewski M, et al. Managed-Medicare health club benefits and reduced health care costs among older adults. Prev Chronic Dis. 2008;5(1):A14. [PMC free article] [PubMed] [Google Scholar]
- 14.Nguyen HQ, Maciejewski ML, Gao S, Lin E, Williams B, LoGerfo JP. Health care use and costs associated with use of a health club membership benefit in older adults with diabetes. Diabetes Care. 2008;31:1562–7. doi: 10.2337/dc08-0624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Medicare Health Outcomes Survey: 2006–2008 cohort 9 performance measurement data user’s guide. Baltimore: Centers for Medicare and Medicaid Services; 2008. [Google Scholar]
- 16.Kazis LE, Selim A, Rogers W, Ren XS, Lee A, Miller DR. Dissemination of methods and results from the Veterans Health Study: final comments and implications for future monitoring strategies within and outside the Veterans Healthcare System. J Ambul Care Manage. 2006;29:310–9. doi: 10.1097/00004479-200610000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Kazis LE, Miller DR, Skinner KM, et al. Applications of methodologies of the Veterans Health Study in the VA Health-care System. J Ambul Care Manage. 2006;29:182–8. doi: 10.1097/00004479-200604000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Iqbal SU, Rogers W, Selim A, et al. The Veterans RAND 12 Item Health Survey (VR-12): what it is and how it is used. Washington, DC: Veterans Health Administration; 2009. [Google Scholar]
- 19.Kazis LE, Miller DR, Skinner KM, et al. Patient-reported measures of health: the Veterans Health Study. J Ambul Care Manage. 2004;27:70–83. doi: 10.1097/00004479-200401000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Barengo NC, Hu G, Lakka TA, Pekkarinen H, Nissinen A, Tuomilehto J. Low physical activity as a predictor for total and cardiovascular disease mortality in middle-aged men and women in Finland. Eur Heart J. 2004;25:2204–11. doi: 10.1016/j.ehj.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 21.DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question. J Gen Intern Med. 2006;21:267–75. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DeSalvo KB, Jones TM, Peabody J, et al. Health care expenditure prediction with a single item, self-rated health measure. Med Care. 2009;47:440–7. doi: 10.1097/MLR.0b013e318190b716. [DOI] [PubMed] [Google Scholar]
- 23.Fried TR, Bradley EH, Williams CS, Tinetti ME. Functional disability and health care expenditures for older persons. Arch Intern Med. 2001;161:2602–7. doi: 10.1001/archinte.161.21.2602. [DOI] [PubMed] [Google Scholar]
- 24.Miilunpalo S, Vuori I, Oja P, Pasanen M, Urponen H. Self-rated health status as a health measure: the predictive value of self-reported health status on the use of physician services and on mortality in the working-age population. J Clin Epidemiol. 1997;50:517–28. doi: 10.1016/s0895-4356(97)00045-0. [DOI] [PubMed] [Google Scholar]
- 25.Newhouse JP, Buntin MB, Chapman JD. Risk adjustment and Medicare. Washington, DC: The Commonwealth Fund; 1999. [Google Scholar]
- 26.Pope GC, Adamache KW, Walsh EG, Khandker RK. Evaluating alternative risk adjusters for Medicare. Health Care Financ Rev. 1998;20:109–29. [PMC free article] [PubMed] [Google Scholar]
- 27.Atherly A, Dowd BE, Feldman R. The effect of benefits, premiums, and health risk on health plan choice in the Medicare program. Health Serv Res. 2004;39:847–64. doi: 10.1111/j.1475-6773.2004.00261.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Feldman R, Dowd B, Wrobel M. Risk selection and benefits in the Medicare+Choice program. Health Care Financ Rev. 2003;25:23–36. [PMC free article] [PubMed] [Google Scholar]
- 29.Ng JH, Kasper JD, Forrest CB, Bierman AS. Predictors of voluntary disenrollment from Medicare managed care. Med Care. 2007;45:513–20. doi: 10.1097/MLR.0b013e31802f91a5. [DOI] [PubMed] [Google Scholar]
- 30.Report to the Congress: issues in a modernized Medicare program. Washington, DC: Medicare Payment Advisory Commission; 2005. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.