Abstract
Objective
The goal of this study was to develop an in-depth understanding of how a health information exchange (HIE) fits into clinical workflow at multiple clinical sites.
Materials and Methods
The ethnographic qualitative study was conducted over a 9-month period in six emergency departments (ED) and eight ambulatory clinics in Memphis, Tennessee, USA. Data were collected using direct observation, informal interviews during observation, and formal semi-structured interviews. The authors observed for over 180 h, during which providers used the exchange 130 times.
Results
HIE-related workflow was modeled for each ED site and ambulatory clinic group and substantial site-to-site workflow differences were identified. Common patterns in HIE-related workflow were also identified across all sites, leading to the development of two role-based workflow models: nurse based and physician based. The workflow elements framework was applied to the two role-based patterns. An in-depth description was developed of how providers integrated HIE into existing clinical workflow, including prompts for HIE use.
Discussion
Workflow differed substantially among sites, but two general role-based HIE usage models were identified. Although providers used HIE to improve continuity of patient care, patient–provider trust played a significant role. Types of information retrieved related to roles, with nurses seeking to retrieve recent hospitalization data and more open-ended usage by nurse practitioners and physicians. User and role-specific customization to accommodate differences in workflow and information needs may increase the adoption and use of HIE.
Conclusion
Understanding end users' perspectives towards HIE technology is crucial to the long-term success of HIE. By applying qualitative methods, an in-depth understanding of HIE usage was developed.
Keywords: Biomedical informatics, clinical informatics, designing usable (responsive) resources and systems, e-prescribing, evaluation studies, health information exchange, human factors, improving healthcare workflow and process efficiency, pediatrics, qualitative/ethnographic field study, qualitative research, social/organizational study, surveys and needs analysis, system implementation and management issues, technology adoption, workflow
Health information exchanges (HIE) support automated sharing of health data across organizational boundaries. Over the past 20 years, various HIE systems have been developed, but many have failed for technological and organizational reasons.1 High-level issues must be addressed to implement an HIE successfully, including disparate health information technology (HIT) infrastructures and vastly different organizational cultures.2 Much previous HIE research focused on these high-level issues and evaluating impacts on healthcare utilization,3 public health tracking,4 return on investment,5 and cost benefits.6 Using survey-based methods, researchers also studied the characteristics of successful HIE efforts.7 8
As HIE efforts moved past initial barriers, research has shifted towards understanding more about the impact of HIE on users. Several studies have surveyed and interviewed providers about HIE, revealing concerns about privacy,9 10 time to disposition of patients,11 productivity,9 workflow,12 and HIE cost.9 10 12 13 Perceived positive impacts balanced these concerns: care quality,10 continuity of care,9 decreasing costs,10 and saving time.9 10 Because of the limited number of functional HIE, much previous research examined provider perceptions before implementation.
As HIE expanded, researchers began to evaluate use in practice, primarily through quantitative data.14 15 Quantitative measures are crucial to the long-term sustainability of HIE, but miss details of other important elements of use. Qualitative evaluation is also needed.16 We examined HIE through new lenses by applying qualitative methods to understand the impact of a HIE on end users in Memphis, Tennessee, USA. In particular, we sought to understand the interaction between HIE and workflow. Our goal was to understand why and how HIE are used. To examine this idea, we proposed three research questions:
How have specific sites integrated HIE into existing approaches?
Are there common HIE-related workflow patterns across sites?
How did providers incorporate HIE into clinical practice?
The knowledge we gained about the interaction between HIE and clinical workflow can be used in future HIE system design and implementation.
Methods
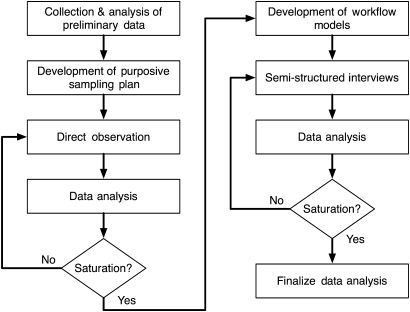
Iterative data collection and analysis occurred from January to August 2009 using direct observation, informal and formal interviews, and the development of workflow models (figure 1).
Figure 1.
Study design.
We conducted fieldwork at multiple sites representing a range of organizational characteristics. Data collection and analysis continued until data saturation, when additional data did not substantially change analytical results.17 Appropriate regulatory groups at all participating organizations approved study procedures before data collection.
Study setting and HIE technology overview
The study took place at sites participating in the MidSouth eHealth Alliance (MSeHA), a regional health information organization formed in 2004 and located in the Memphis, Tennessee region. The majority of large hospitals in the area and two safety net ambulatory clinic systems contribute data to the exchange. Participating institutions contribute varying levels of patient data to the exchange (eg, demographic data, laboratory results, discharge summaries). Throughout this report, we will refer to the Memphis HIE system as the ‘exchange’. The exchange is mainly used in emergency departments (ED) and ambulatory clinics. Across all sites, over 380 individuals had exchange access during the study period. At study initiation, users consulted the exchange for an average of 3% of patient encounters. Each MSeHA-participating organization set its own policies regarding exchange access, within the context of regional health information organization-wide policies. Individuals with exchange access included: registrars, administrative staff, information technology staff, medical assistants, nurses, pharmacists, nurse practitioners and physicians.
The Memphis exchange uses a database structure initially developed at Vanderbilt University Medical Center.18 It applies a data-matching algorithm to connect information maintained in separate organizational vaults. The exchange uses an ‘opt out’ model, with patient data included unless a patient elects not to participate. As of August 2009 the exchange database contained over 41 million documents, corresponding to over 1 million patients. The documents included laboratory reports, imaging reports, pathology reports, discharge summaries, International Classification of Disease version 9 admission codes, and claims records.
Once users log on, they can retrieve all matching patient data originating from all contributing sites. A healthcare provider with exchange access can thus review patient data from other hospitals, ED and some ambulatory clinics.
Sampling plan
We collected and analyzed qualitative and quantitative data about potential Memphis research sites including: exchange usage statistics, open-ended interviews with exchange operations team members, open-ended interviews with key informants19 in Memphis, preliminary site visits, and geographical information. We considered all 15 ED sites and all 15 ambulatory clinic sites participating in the exchange for study inclusion. The sampling plan included sites with different exchange usage levels, different geographical areas, and ambulatory and ED contexts (table 1).
Table 1.
Exchange usage
| Site | Geographical area | Average monthly rate (January–April 2009) | |
| Patient visits per month | Percentage of patient visits with eHealth use | ||
| Hospital 1 | Metro–inner | 1938* | 13%* |
| Hospital 2 | Metro–inner | 4425 | 4% |
| Hospital 3 | Suburban | 3848 | 2% |
| Hospital 4 | Metro–outer | 3363 | 13% |
| Hospital 5 | Suburban | 2407 | 10% |
| Hospital 6 | Metro–outer | 4877 | 1% |
| Ambulatory clinic A.1 | Metro–inner | 7085† | 7%† |
| Ambulatory clinic A.2 | Metro–outer | ||
| Ambulatory clinic A.3 | Metro–outer | ||
| Ambulatory clinic A.4 | Metro–inner | ||
| Ambulatory clinic B | Metro–inner | Not available‡ | Not available‡ |
| Ambulatory clinic C.1 | Metro–outer | 6932† | 4%† |
| Ambulatory clinic C.2 | Metro–inner | ||
| Ambulatory clinic C.3 | Metro–inner | ||
Patient visits per month at this site only reflect a portion of the emergency departments (ED) where eHealth is available.
Technology-related design constraints resulted in patient visits per month and percentage of patient visits with exchange use availablity for ambulatory clinic groups only in aggregate form across all sites in each clinic group.
Usage data are not collected for this site as a distinct entity; no data on patient visits per month or per cent of visits with exchange use are available for this clinic. Usage data for this site are incorporated into usage data for an ED site that this clinic was associated with.
We adjusted the sampling plan based on organizational changes at several sites. Site information throughout this report has been anonymized.
Direct observation
We observed workflow for more than 180 h in six ED and eight ambulatory clinics. During 121 h of ED observation, we observed 91 instances of exchange use and six instances of alternative HIE system use. During 66 h of observation in the ambulatory environment, we observed 39 instances of exchange use and 12 instances of alternative HIE system use. Alternative HIE systems included external electronic medical records (EMR) systems, the Tennessee web immunization service,20 and the Tennessee controlled substance monitoring database.21 The total amount of observation time in individual ED ranged from 7 to 38 h and from 4 to 13 h at ambulatory clinic sites (table 2).
Table 2.
Data collection by site
| Site | Hours of observation |
| Hospital 1 | 38 |
| Hospital 2 | 28 |
| Hospital 3 | 14 |
| Hospital 4 | 17 |
| Hospital 5 | 7 |
| Hospital 6 | 7 |
| Ambulatory clinic A.1 | 13 |
| Ambulatory clinic A.2 | 4 |
| Ambulatory clinic A.3 | 6.5 |
| Ambulatory clinic A.4 | 11.5 |
| Ambulatory clinics B | 10 |
| Ambulatory clinics C.1 | 6 |
| Ambulatory clinics C.2 | 7 |
| Ambulatory clinics C.3 | 8 |
We provided a brief project overview and obtained verbal assent from staff, providers, and patients before observation. The researcher followed subjects at each site, observing interactions with the HIE, use of other HIT, and other work activities. All observed subjects had exchange access, but amounts and types of exchange use varied. Subjects were observed in examination rooms, hallways, open work areas such as nurses' stations, and private work areas such as offices. Observation location related to technology usage patterns and patient and context-specific factors. The primary observation location at each site was the main HIE access point. We recorded detailed free-text notes about exchange access, why it was used, interaction between the HIE and other HIT at the site, comments from providers about technology, and how providers used exchange data.
As time allowed, we conducted informal interviews to clarify observations and to understand behavior related to the exchange. Subjects were asked to clarify their rationale for using the exchange, outcomes of obtaining HIE data, and aspects of behavior difficult to understand based solely on observation. For example, subjects logging onto the HIE were asked “Why are you looking this patient up?” As providers wrote patient case notes, they were asked questions to clarify the role, if any, that HIE data played in providing care.
We transcribed notes as soon as possible after observation and stored them in an electronic notebook application22 during fieldwork periods. We used initial notes to focus and refine observation, provide guidance on appropriate approaches for specific contexts, and formulate topics to consider during additional observation. After fieldwork periods, the transcribed notes were transferred to NVivo 8 software23 for further qualitative data analysis.
Analysis of observation data
During data analysis, we applied two approaches to coding: a grounded approach involving open coding and a framework-focused approach involving axial coding.24 25 The grounded, open coding approach consisted of two phases: initial and focused. We organized coding using a combination of the electronic notebook application and NVivo 8. The initial open-ended coding approach allowed theories to emerge from the data rather than imposing pre-set expectations, although influenced by past researcher experiences. We completed initial coding as close as possible to data collection, typically on the same observation day. Specific instances of exchange use provided structure for code assignment. As we collected and analyzed more data, the initial codes indicated areas needing additional data collection. One researcher (KMU) assigned initial codes, but co-authors and a peer debriefer26 reviewed initial coding to ensure the codes fit the data.
The grounded portion of data analysis moved into a focused coding phase as data collection progressed and strong themes emerged. Focused coding synthesized initial codes to develop broader themes. Co-authors and a peer debriefer reviewed the focused coding schemas to ensure the focused codes presented a logical extension of the initial codes and of the data. Gaps in initial data collection, requiring additional data collection, emerged during this phase.
After completing the open coding process, we used axial coding,24 25 applying the workflow elements framework27 to examine the interaction of HIE technology and clinical workflow. The model provided a flexible structure for analysis of workflow-related studies and describes workflow through a specific level and a pervasive level. The specific level is composed of actors performing actions that produce outcomes, with artifacts used to enable actions and characteristics describing actions. Three pervasive components influence the specific attributes of work: temporality, aggregation, and context.
The data, data analysis processes, and outcomes of data analysis were discussed extensively with other members of the research team, formal and informal advisors specializing in ethnographic approaches, and a peer reviewer with extensive qualitative experience.
Workflow modeling
We formalized and standardized a workflow modeling approach described previously.28 Analysis of observation and interview data guided model development using a form of hierarchical task analysis.29 We identified sequences of routine activities related to HIE use across sites, such as who used the exchange and when it was accessed in the care process. The analysis detailed roles and temporal factors related to HIE use and interaction among different roles.
Semistructured interviews
We conducted nine formal semistructured telephone interviews after the completion of observation data analysis. Interviews with observation subjects and other exchange users served as a form of member checking of observation analysis. Interview subjects included six physicians, one nurse practitioner, and two individuals in HIT-related management roles. Whenever possible, we interviewed subjects we had previously observed and sought to represent a range of usage contexts and usage approaches. Limitations at some sites such as work schedules resulted in our interviewing people who were not observed. A set of focused questions guided the interviews; they are available online only as a supplementary appendix. The interview structure allowed us to pose additional questions based on subject responses. These questions clarified observations and addressed research questions raised during data analysis. Interviews were audiotaped and then transcribed.
Analysis of interview data
We imported transcribed interviews into NVivo 8, in which we analyzed data in the context of observation data coding. Data analysis focused on patterns of information-seeking behavior and exchange usage patterns. Analysis of these data resulted in the review and revision of the focused coding schema.
Results
Site-specific HIE-related workflow
The available HIT infrastructure at the sites varied from minimal technology with paper medical records to EMR (table 3). Based on observation and interviews, we developed a model of HIE-related workflow for each ED observation site and a single model of HIE-related workflow for each ambulatory clinic group, as consistent workflow patterns existed across each group (see supplementary appendix, available online only). The workflow diagrams show the timing of HIE use within a patient visit, actors in information retrieval and use, and task sequences. They focus on HIE-related elements of work but include other patient care actions to ground information exchange.
Table 3.
HIT usage patterns
| Hospital | Ambulatory clinic group | ||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | A | B | C | |
| Information access | |||||||||
| Data retrieval from EMR | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Data retrieval from paper chart | ✓ | ✓ | ✓ | ||||||
| Information input | |||||||||
| Entry of documentation into EMR | * | ✓ | ✓ | ||||||
| Computerized order entry | ✓ | ||||||||
| Entry of documentation into ED-specific information system | ✓ | ✓ | |||||||
| Computerized order entry in ED-specific CPOE system | ✓ | ✓ | |||||||
| Entry of documentation on paper form | ✓ | ✓ | ✓ | ✓ | |||||
| Paper-based orders | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Practice management system | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
Scribes input data on attending physicians' behalf in most cases. Nurse practitioners and resident physicians enter their own notes into the electronic medical records (EMR).
CPOE, computerized provider order entry; ED, emergency department; HIT, health information technology.
Hospital 1
Hospital 1 was a standalone site, not affiliated with other hospitals. Their HIT infrastructure included a non-graphical interface EMR system and limited data entry ability. Nurses recorded data in the EMR, while nurse practitioners and physicians charted on paper forms later scanned into the EMR. Providers used paper forms for clinical orders. The environment was interrupt-driven with a rapid patient flow, partly from administrative pressure to maintain a fast pace. One physician described the ED as “fluid, always in motion”. Several physicians expressed concerns about patients visiting the ED for primary care.
A few registrars and nurses had exchange access, but the primary exchange users during the study were physicians. The rapid pace caused initial concerns about exchange use. As one provider stated, “At first I thought it was going to be cumbersome, but it helps me a lot.” The utility of exchange information for the hospital's patient population justified the time needed for data retrieval. The medical director of the ED required that providers document what information was obtained from the exchange.
We discovered an informal data exchange route through residents at hospital 1. Residents in Memphis rotated through multiple regional locations, including several of our research sites. Residents were not eligible for exchange access, but residents often had direct EMR access for several organizations. Residents also described an informal communications network, in which residents contacted colleagues at other hospitals to understand patient medical histories.
Hospital 2
Hospital 2 was part of a larger hospital group, sharing records from all hospitals within the organization through their EMR. The EMR was tightly integrated into routine clinical workflow. Providers extensively used the EMR to retrieve patient data. Nurse practitioners and residents input information into the EMR, but ED physicians worked with scribes for data entry. The scribes closely followed physicians, recording clinical information and entering data in the EMR. Physicians finalized and approved the documentation. Providers used paper forms for clinical orders.
One factor in the HIE usage of hospital 2 was existing access to patient data across the organization through their EMR. Physicians were the primary exchange users at hospital 2, with some exchange use by nurses working in the chest pain center of the ED.
One of the main exchange-related issues noted at hospital 2 related to passwords. Multiple individuals at the site were initial exchange users, but over time used the system infrequently and forgot their password. A frequent comment when talking to nursing staff at this site was “I have a token, but I haven't used it for a while and forgot my pin.” Providers echoed the concerns expressed at hospital 1 about time for data retrieval. A physician who believed the exchange was more useful for primary care stated, “I need to concentrate on life-threatening illnesses, I don't have time to go looking through the chart looking for records.”
Hospital 3
Hospital 3 was part of a larger hospital group, sharing records from all hospitals within their organization through their EMR. The EMR was tightly integrated into clinical workflow. Nurses, nurse practitioners, and physicians retrieved data from the EMR and entered data directly into the EMR. Hospital 3 also had a computerized order entry system. One physician, describing the role of computers in his clinical work, stated “As this computer stuff progresses, we do less and less patient care and more computer games.”
The existing availability of data from hospitals across the organization limited the utility of exchange data at hospital 3. Providers discussed the usefulness of the exchange for filling in ‘missing details’, but noted that one of the main hospitals visited by some of their patients did not participate. Based on experience with inconsistencies in data availability in their EMR system, providers at hospital 3 were concerned that data in the exchange would not be updated in a timely fashion.
Hospital 4
Hospital 4 was part of a small hospital group that did not support information sharing among their group. The ED at hospital 4 utilized an ED-specific information system including computerized order entry, separate from the hospital's EMR. The separate and non-compatible systems within the same hospital increased the difficulty of accessing data for ED providers. One nurse practitioner, describing frustration with these separate systems, stated “[The EHR] won't let me in. [The EHR] is protected by a password which I have, but if you select a patient and you're not listed as the provider on that patient, you can't look them up.”
The primary exchange users at the site were nurse practitioners and physicians, although some nurses in the chest pain center of the ED had access. Triage nurses expressed interest in exchange access during observation, stating they felt it would be helpful for intake. One triage nurse noted, “Seems like it would be useful, especially in triage. That way, we could look it up and print it out for the doctor, they wouldn't have to look it up.”
Hospital 5
The ED at hospital 5 utilized an ED-specific information system separate from the hospital's EMR and including computerized provider order entry. Physicians used tablet computers to access the EMR while in examination rooms. However, the physicians were instructed not to access the exchange from these tablet computers and to use computers located in a physician workspace area instead.
Providers noted the importance of exchange data due to increases in primary care services in the ED. However, they expressed frustration about the limited amount of ambulatory clinic data in the exchange. One physician stated, “This would be great if all clinics were on it, that's what we really need, where we really need to head.” Providers at hospital 5 were frustrated by requirements to login to multiple separate systems. One physician requested tighter integration between their information system and the exchange, “It would be nice if there was just one program where they had everything, could log on once, and BAM, everything is there without extra log ons.”
Hospital 6
Hospital 6 was part of a larger hospital organization. Providers used a mix of paper and electronic systems. While providers retrieved data from their EMR, patient documentation was entered on paper forms that were later input into the EMR. Providers discussed speed issues with several of their electronic systems and were concerned about disconnects due to multiple approaches to data.
Hospital 6 was an early implementation site for the exchange and began using the exchange when only limited data were available from other sites, resulting in frustration and negative perceptions of the exchange. Initial workflow at this site involved registrars, accessing the exchange for every patient during intake. Registrars printed off a form showing the number of matching external records available in the exchange. As the exchange technology matured and a new screen was implemented to show matching records automatically, administrators removed registrar access. The new intended workflow involved nurse practitioners and physicians directly accessing the exchange to check for matching data. The workflow change led to a dramatic usage decline, from almost all patients to approximately 1% of patients.
Accessing the exchange for providers who did not have access themselves was also discussed at hospital 6. As one nurse practitioner described, “People come to me to login and look information up for them too.”
Ambulatory clinic group A
The clinics within ambulatory clinic group A were the only research sites without any EMR. The clinics utilized a practice management system, but all clinical data were kept in clinic-specific paper charts. We rarely observed physicians or nurse practitioners using computers. Nursing staff accessed the practice management system and also accessed the exchange.
Exchange use at this clinic group was tightly linked to patient reports of recent hospital visits. During patient intake, nursing staff asked the patient if they had recently visited any hospitals. If the patient answered yes, the intake nurse handed the patient information to a nurse with exchange access, who accessed patient data in the exchange, printed off relevant data, and placed the printouts with the paper chart. If patients reported a recent hospital visit during the physician–patient encounter rather than during intake, the physician requested that a nurse access exchange data, typically after the patient visit.
A limited number of physicians used the exchange, typically outside of clinic hours while completing documentation. The pace of patient visits, overall throughput of the clinic, limited number of available computers, and lack computer use for documentation limited the frequency of physician use of the exchange. Several referral nurses also routinely used the exchange to retrieve reports for external procedures, such as ultrasounds following abnormal mammograms.
Due to existing relationships among clinics, providers, and area hospitals, some ambulatory clinic group A staff had direct access to EMR at local hospitals. This direct EMR access consistently provided a higher level of data availability than the exchange, causing one nurse to remark “I can count the times on one hand I have gotten anything like that [eg, discharge summaries, history and physical reports] from this system [the exchange].” A nurse practitioner described the information available in the exchange as ‘kind of vague’. Nurses noted that direct EMR access required multiple steps but data availability made it worthwhile, while a physician stated he would select the level of information available directly from the external EMR ‘in every case’.
Ambulatory clinic B
Ambulatory clinic B was affiliated with a hospital. The clinic utilized an EMR for documentation. Physicians actively pursued exchange access and obtained it through their hospital affiliation. However, the exchange was not part of their routine workflow. Exchange use was limited to special circumstances, such as gathering documentation for a specialty care referral or retrieving data on recent hospitalizations.
Like ambulatory clinic group A, physicians at this clinic had direct access to external EMR, primarily through residents. Although physicians expressed support for the exchange, they were uncertain how to incorporate it into routine clinical workflow and expressed concern about residents not having access.
Ambulatory clinic group C
Of the three ambulatory clinic groups, ambulatory clinic group C had the most developed HIT infrastructure. We observed physicians and nurse practitioners using their EMR for a variety of purposes in different contexts, including examination rooms. The clinics maintained paper charts to retain referral reports. Computer use was a routine part of clinical workflow.
Several providers noted the lack of time for additional activities such as consulting the exchange for data. In particular, one physician noted that “sometimes it means I have to go through a lot of information” when consulting the exchange, a challenge given limited time. Another physician in this clinic group described the workflow aspects of exchange use as ‘tricky’, especially for providers not using computers in examination rooms. Looking up referral results and data on recent hospitalizations were major reasons for exchange access at these sites.
Cross-organizational HIE-related workflow patterns
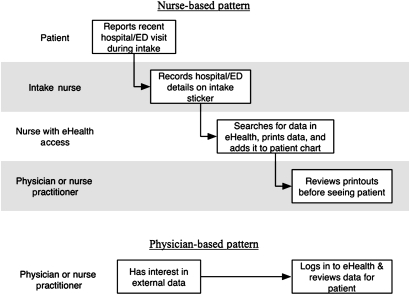
We analyzed the site-specific workflow models for common patterns of HIE-related workflow. Two main role-based workflow patterns emerged: nurse based and physician based (figure 2). We observed the nurse-based workflow pattern at sites where medical assistants and nurses were primary exchange users. The physician-based workflow pattern occurred at sites where nurse practitioners and physicians were primary exchange users. See table 4 for primary and secondary workflow patterns at each site.
Figure 2.
Health information exchange-related common workflow patterns. ED, emergency department.
Table 4.
Exchange usage models, by site
| Hospital | Ambulatory clinic group | ||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | A | B | C | |
| Primary usage model | MD | MD | MD | MD | MD | MD | RN | MD | MD |
| Secondary usage model | – | RN | – | RN | – | – | MD | – | RN |
MD, physicians; RN, nurse practitioners.
Several factors differentiated the two patterns in addition to roles: timing of exchange use, types of exchange data retrieved, and information transfer modalities. Both workflow patterns shared a common element: the information consumer. Regardless of who retrieved exchange data or the data retrieval process, a nurse practitioner or physician reviewed it and applied it to patient care.
Nurse-based workflow pattern
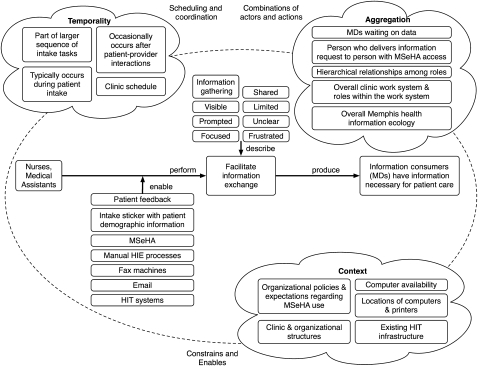
Nurses typically accessed the exchange if a patient mentioned recent hospital visits during triage, although later access also occurred. The medical assistant or nurse printed information from the exchange so nurse practitioners or physicians could review it. We also applied the workflow elements framework to the nurse-based workflow pattern (figure 3).
Figure 3.
Nurse-based workflow elements. HIE, health information exchange; HIT, health information technology; MD, physician; MSeHA, MidSouth eHealth Alliance.
A key artifact enabling the information exchange process was an intake sticker with patient demographic information. When patients reported a recent hospital visit, the intake nurse recorded details on this sticker and gave it to a nurse with exchange access. Nurses' exchange use was highly focused on recent hospital visits and they rarely browsed medical history. If a summary document such as a discharge summary was available, they printed it in preference to raw data such as laboratory reports. Because some sites limited data types contributed to the exchange, nurse access to the exchange was often frustrated by summary data unavailability. The nurse-based workflow pattern highlighted hierarchical relationships among healthcare professionals, as nurses typically accessed the exchange to obtain information for use by physicians.
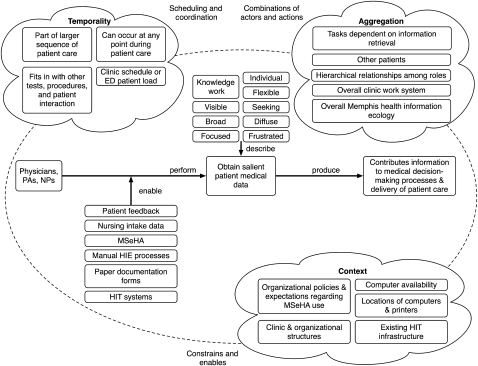
Physician-based workflow pattern
Nurse practitioners and physicians accessed the exchange for a wider range of reasons than nurses. Access occurred at different points during patient care, depending on triage information and patient interaction. Physicians retrieved information for their own use. We applied the workflow elements framework to the physician-based workflow pattern (figure 4).
Figure 4.
Physician-based workflow elements. ED, emergency department; HIE, health information exchange; HIT, health information technology; MD, physician; MSeHA, MidSouth eHealth Alliance; NP, nurse practitioner; PA, physician assistant.
Physicians accessed a broader scope of information and browsed more of a patient's medical history. Although physicians and nurse practitioners at some sites used paper-based documentation, they typically reviewed exchange data online. If a provider planned to admit a patient, they sometimes printed data for use by inpatient physicians without exchange access. Physician and nurse practitioner use of the exchange was applied directly to decision-making (eg, about tests and procedures).
Less common HIE-related workflow patterns
We observed other less common site-specific workflow patterns. For example, at one ambulatory clinic, referral clerks used the exchange to track the completion of external procedures such as biopsies. They retrieved procedure reports from the exchange and contacted patients to communicate results or schedule follow-up appointments. The exchange served an auxiliary role to other methods of referral-related communication such as faxes.
Evolution of workflow patterns
Workflow patterns across all sites changed over time based on multiple individual, organizational, and contextual factors. For example, as we discussed earlier, administrators at hospital 6 selected registrars as the primary exchange users during initial system implementation. Once a screen showing the number of matching exchange records for patients recently registered at the hospital became available, administrators removed access for registrars and expanded access for clinical staff. This led to a precipitous usage drop at hospital 6 and fundamentally changed HIE-related workflow at the site. Staff changes also resulted in HIE-related workflow changes. For example, a nurse served as the primary exchange user in the chest pain center of one ED, using it to find cardiac-related data during triage. After the nurse resigned, usage shifted to physicians and access occurred later in patient care. Although the workflow diagrams represent a snapshot of HIE-related workflow at sites, based on observation overall patterns of HIE-related work had stabilized by the time of the study.
Incorporating HIE into clinical practice
Prompts for HIE use
We used workflow models to assess how clinicians incorporated the exchange into clinical practice. Our data led to further examination of what prompted providers to add exchange use to their clinical workflow. Based on observation and interviews, we identified five categories describing reasons for exchange use: other hospital visits, lack of trust in a patient's narrative, communication challenges, referrals and consultations, and technology problems.
One of the most commonly observed reasons for exchange use was a patient reporting a visit to another hospital. Providers in ambulatory and ED settings viewed laboratory, radiology, and other procedure reports as important, but stated that discharge summaries were the most helpful type of data. When summaries were available, providers stated that they did not have to ‘piece together’ data to formulate a comprehensive view of a visit.
An unanticipated but frequently encountered reason for exchange use involved issues of trusting patients. Physicians at different ED sites described patient behaviors that acted as ‘red flags’. For example, physicians at several sites routinely consulted the exchange about patients with chief complaints of headache or back pain in the absence of trauma, due to concerns about chronic pain medication abuse. As one physician stated,
“Sometimes, like it or not, we have patients that we feel are drug seeking, especially if they come in talking about chronic pain issues. This way [with the exchange] we can see how many facilities they have been to recently. You would be surprised, sometimes, you look up a patient and they've been to just about every hospital in Memphis, at least that the eHealth system will show us, over the past month. So that kind of sends a red flag to you about, ‘What's really going on?’”
One ED physician discussed her reasons for accessing the exchange, “The two biggest groups I use it for are [people with] multiple medical problems using multiple facilities and people who are trying to BS.” For the first group, the goal was to ensure continuity of patient care. For the second group, the goal was to verify the patient's narrative.
Some physicians disagreed with classifying some exchange access as trust related. One ambulatory physician stated, “It's not that I don't trust them, it's just that maybe the patient doesn't know or maybe doesn't have a high medical literacy or something like that.” Trust-related issues were more openly described in ED contexts.
Another major reason for consulting the exchange was communication. We observed multiple types of communication challenges. Some patients could not communicate clearly due to physical problems, making it difficult to understand the patient's medical history. For example, a nurse practitioner could not understand a patient with stroke-related aphasia and used the exchange to obtain medical history data. Language-related issues also posed a communication challenge even when medical interpreters were available. As one physician stated, “Even with an interpreter, I just feel like communication isn't as clear.” There were also challenges related to medical literacy. Physicians noted a gap between a layperson's knowledge and the level of information useful for medical decision-making. Exchange data helped bridge this gap by providing information patients could not clearly communicate.
Both ambulatory and ED care teams used exchange data to facilitate referrals and consultations. In the ambulatory environment, staff and physicians used the exchange to obtain information required for a specialist referral and to retrieve reports. While only a few specialty provider sites contributed data to the exchange, this included the main specialty clinics used by participating ambulatory clinics. Ambulatory care providers noted delays in obtaining referral reports and stated that the exchange reduced time and effort involved to retrieve reports. In the ED environment, providers presented exchange data during consultations with specialists. Hospitals typically provided exchange access to ED providers, not to hospitalists or specialists. ED providers, as a result, provided exchange data to inpatient providers.
Providers at some sites, especially hospital 2 and hospital 3, used the exchange as a workaround to their site's HIT for reasons such as: usability issues, difficult login procedures, delays in laboratory data availability, and EMR downtime. For example, one provider described using the exchange due to difficulty navigating the site's EMR,
“I use it [the exchange] a lot. Now that we [the current hospital] have discharge summaries in there, I use it to pull up our discharge summaries. I can login to MSeHA faster than I can login to our system [EMR].”
Exchange use for this purpose varied, with providers at several sites reporting limited or no use of the exchange for this purpose.
Workflow-related challenges of data exchange with and without HIE
A significant workflow challenge of data exchange before HIE availability involved time and effort involved in external record retrieval. In the ambulatory setting, a patient would arrive, report a recent hospital visit, and staff would begin attempting to retrieve records. One nurse at an ambulatory clinic described a scenario in which a hospital stated files would be faxed ‘shortly’. Based on her past experience, she commented, “Shortly means three hours from now.” A patient visit could already be completed by the time records arrived, leading to information being unavailable during the patient–provider encounter and additional work after the encounter. Depending on the hospital, delays could be extensive with one provider noting, “Usually it takes a couple of days [from a specific hospital], definitely not the same day.” The rapid pace of emergency care meant retrieval delays could impact patient outcomes. As ED operate continuously, one provider pointed out “Before we could call between 8 and 4 to get records from other sites, but eHealth is 24 h.”
Even with HIE technology in place, events such as downtime or other technological issues led to delays. For example, we observed one site where the exchange was unavailable after their information technology group reconfigured proxy servers. Even brief delays using the exchange resulted in providers proceeding to other tasks, especially in the ED. We observed an exchange user encouraging a colleague frustrated with exchange performance by saying, “It's loading, it just takes a second.”
There were also challenges that the exchange could not fully resolve, especially related to the fragmentation of information and medication management. Providers with access to multiple sources of information had to sort through their site's EMR, EMR of other sites, the exchange, and paper forms to understand a patient's medical history fully. The additional work of resolving questions caused by fragmented or unclear information was difficult, even with the exchange.
Discussion
The research described in this report examined HIE usage from the perspective of its end users, an important and under-evaluated area. We focused on how and why clinicians used a functional HIE system and how it impacted patient care. The Memphis exchange achieved significant organizational and technological accomplishments, but overall usage was lower than anticipated. We previously explored quantitative data on exchange usage.14 Examining how the HIE technology fits into workflow using qualitative methods helped develop a deeper understanding of usage data.
Our ethnographic approach assessed how the exchange fit into existing work patterns and what prompted individuals to use the system. Sites participating in the exchange differed significantly on multiple characteristics including geographical location, organizational affiliation and structure, and HIT infrastructure. Not surprisingly, these different site characteristics led to different approaches towards HIE. Users adapted the HIE technology to meet the information and workflow needs appropriate to their context, with varying degrees of success. Our results suggest that users may need assistance with integrating HIE into clinical workflow and with understanding how HIE can directly benefit healthcare delivery.
Although every context has unique characteristics, two main workflow patterns emerged across all sites. System use by nurses was typically driven by recent hospital visits with a goal of retrieving specific data for physicians' use. Nurse practitioner and physician exchange use was more open-ended. These findings can assist efforts to understand HIE benefits for different user types and to improve HIE adoption. Supporting the needs of different user roles involves several key components: providing a range of functionality, supporting different approaches to data, and presenting different levels of data. A major barrier to some users is a low expectation that needed information is available through the exchange, highlighting the crucial role of understanding information needs and user expectations. The current design of the exchange is a ‘one size fits all’ model; allowing for user and role-specific customization may increase adoption and use.
The identified prompts for exchange use highlight concerns about the reliability and accuracy of patient medical history reports, illustrating the dichotomous nature of HIE. A system designed to improve care delivery across the healthcare continuum was also used to verify patient narratives and significantly impacted patient–provider trust. Understanding why and how clinicians use HIE data can assist with designing for user needs and with targeting implementation strategies. In addition, information about clinician perceptions of HIE is a powerful outreach tool to other clinicians unsure about the benefits of this technology. Knowing how clinicians have benefited from HIE data may provide reasons for individuals to adopt this technology.
Study limitations
A single researcher collected the study data, introducing the potential for observer bias. Before entering the field, the researcher considered potential sources of bias to assist in identifying and avoiding methodological and analysis approaches based on past experience rather than the current research experience. As with any observational study, the Hawthorne effect30 was a potential data confounder. In order to mediate for this potential problem, the researcher asked probing questions throughout observation and interviews to evaluate potential observer effects on exchange use.
Conclusion
This study focused on the application of HIE technology to patient care. We examined why providers accessed an HIE, what types of information they gathered, and how they used this information in patient care. We identified factors that prompted exchange use and outcomes of use. The main study outcomes were in-depth descriptions of how HIE fit into clinical workflow at each site, the identification of general HIE-related workflow patterns, and an exploration of exchange use across clinical contexts.
Our research addressed a significant gap in the knowledge about the front-line impact of HIE on patient care delivery. Previous HIE evaluation efforts have focused on demonstrating return on investment through analysis of quantitative data such as duplicate test rates. The actual impacts of a HIE system on patient care we observed were nuanced and rarely delivered clear-cut financial benefits. We demonstrated the importance of evaluating and understanding the information needs and work practices of intended consumers of HIE.
Our next steps include applying workflow research to other HIE projects in project design and implementation stages. We are also interested in applying the workflow elements model to other settings, to continue testing and expanding the model.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge the assistance of Dr Cynthia Gadd, Dr Madhu Reddy, Dr Bruce Barry and Dr Mark Frisse.
Footnotes
Funding: Early stages of this research were supported by a National Library of Medicine Training Grant, #T15 LM007450. Later stages of the project, including travel support for data collection trips to Memphis, were supported by AHRQ contract 290-04-0006 and the State of Tennessee. This report has not been approved by the Agency for Healthcare Research and Quality.
Competing interests: None.
Patient consent: Subjects of the study were healthcare providers, not patients. Proper consent was obtained from research subjects, as approved by the Vanderbilt Institutional Review Board.
Ethics approval: Ethics approval was granted by the Vanderbilt University Institutional Review Board.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Lorenzi NM. Strategies for creating successful local health information infrastructure initiatives. 2003. http://aspe.hhs.gov/sp/nhii/lhii-lorenzi-12.16.03.pdf (accessed 26 Aug 2011). [Google Scholar]
- 2.Vest JR, Gamm LD. Health information exchange: persistent challenges and new strategies. J Am Med Inform Assoc 2010;17:288–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vest JR. Health information exchange and healthcare utilization. J Med Syst 2009;33:223–31 [DOI] [PubMed] [Google Scholar]
- 4.Kho A, Lemmon L, Commiskey M, et al. Use of a regional health information exchange to detect crossover of patients with MRSA between urban hospitals. J Am Med Inform Assoc 2008;15:212–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frisse ME, Holmes R. Estimated financial savings associated with health information exchange and ambulatory care referral. J Biomed Inform 2007;40(6 Suppl):S27–32 [DOI] [PubMed] [Google Scholar]
- 6.Walker J, Pan E, Johnston D, et al. The value of health care information exchange and interoperability. Health Aff (Millwood) 2005;Suppl Web Exclusive:W5-10–W5-18 http://www.ncbi.nlm.nih.gov/pubmed/15659453/ [DOI] [PubMed] [Google Scholar]
- 7.Adler-Milstein J, Bates DW, Jha AK. A survey of health information exchange organizations in the United States: implications for meaningful use. Ann Intern Med 2011;154:666–71 [DOI] [PubMed] [Google Scholar]
- 8.Adler-Milstein J, Landefeld J, Jha AK. Characteristics associated with regional health information organization viability. J Am Med Inform Assoc 2010;17:61–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patel V, Abramson EL, Edwards A, et al. Physicians' potential use and preferences related to health information exchange. Int J Med Inform 2011;80:171–80 [DOI] [PubMed] [Google Scholar]
- 10.Wright A, Soran C, Jenter CA, et al. Physician attitudes toward health information exchange: results of a statewide survey. J Am Med Inform Assoc 2010;17:66–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shapiro J, Kannry J, Kushniruk A, et al. Emergency physicians' perceptions of health information exchange. J Am Med Inform Assoc 2007;14:700–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ross SE, Schilling LM, Fernald DH, et al. Health information exchange in small-to-medium sized family medicine practices: motivators, barriers, and potential facilitators of adoption. Int J Med Inform 2010;79:123–9 [DOI] [PubMed] [Google Scholar]
- 13.Fontaine P, Zink T, Boyle RG, et al. Health information exchange: participation by Minnesota primary care practices. Arch Intern Med 2010;170:622–9 [DOI] [PubMed] [Google Scholar]
- 14.Johnson K, Unertl K, Chen Q, et al. Health information exchange usage in emergency departments and clinics: the who, what, and why. J Am Med Inform Assoc 2011;18:690–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vest JR, Zhao H, Jaspserson J, et al. Factors motivating and affecting health information exchange usage. J Am Med Inform Assoc 2011;18:143–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johnson K, Gadd C. Playing smallball: approaches to evaluating pilot health information exchange systems. J Biomed Inform 2007;40(6 Suppl):S21–6 [DOI] [PubMed] [Google Scholar]
- 17.Tuckett A. Qualitative research sampling: the very real complexities. Nurse Res 2004;12:47–61 [DOI] [PubMed] [Google Scholar]
- 18.Frisse M, King J, Rice W, et al. A regional health information exchange: architecture and implementation. AMIA Annu Symp Proc 2008:212–16 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2655967/ [PMC free article] [PubMed] [Google Scholar]
- 19.Marshall M. The key informant technique. Fam Pract 1996;13:92–7 [DOI] [PubMed] [Google Scholar]
- 20.Tennessee Web Immunization Service (TWIS) Tennessee Department of Health: Tennessee Web Immunization System. 2011. http://health.state.tn.us/twis/ (accessed 25 Oct 2009).
- 21.Tennessee Controlled Substance Monitoring Database Tennessee Department of Health: Controlled Substance Database Program. 2011. http://health.state.tn.us/boards/Controlledsubstance/ (accessed 25 Oct 2009).
- 22.Circus Ponies, Inc NoteBook by Circus Ponies Software. 2011. http://www.circusponies.com/ (accessed 26 Aug 2011).
- 23.NVivo 8 by QSR International. QSR International Pty Ltd, 2011. http://www.qsrinternational.com/products_nvivo.aspx (accessed 26 Aug 2011).
- 24.Charmaz K. Constructing Grounded Theory: A Practical Guide Through Qualitative Analysis. Thousand Oaks, CA: Sage Publications Ltd, 2006 [Google Scholar]
- 25.Charmaz KC. Coding in grounded theory practice. In: Constructing Grounded Theory: A Practical Guide Through Qualitative Analysis. Thousand Oaks, CA: Sage, 2006:42–71 [Google Scholar]
- 26.Lincoln Y, Guba E. Establishing trustworthiness. In: Naturalistic Inquiry. Beverly Hills, CA: Sage Publications, 1985:289–331 [Google Scholar]
- 27.Unertl K, Novak L, Johnson K, et al. Traversing the many paths of workflow research: Developing a conceptual framework of workflow terminology through a systematic literature review. J Am Med Inform Assoc 2010;17:265–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Unertl K, Weinger M, Johnson K, et al. Describing and modeling workflow and information flow in chronic disease care. J Am Med Inform Assoc 2009;16:826–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shepherd A. Hierarchical Task Analysis. London: CRC Press, 2001 [Google Scholar]
- 30.Sonnenfeld JA. Shedding light on the Hawthorne studies. J Occup Behav 1985;6:111–30 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.