Abstract
We examined the effects of acculturation, depressive symptoms, progesterone, and estriol (E3) as predictors of preterm birth (PTB) in pregnant Hispanic women. This cross-sectional study recruited a sample of 470 Hispanic women between 22- and 24-week gestation from physician practices and community clinics. We used the CES-D to measure maternal depressive symptoms. We measured acculturation by English proficiency on the Bidimensional Acculturation Scale, residence index by years in the USA minus age, nativity, and generational status. Serum progesterone and E3 were analyzed by EIA. Ultrasound and medical records determined gestational age after delivery. In χ2 analysis, there were a significantly greater percentage of women with higher depressive scores if they were born in the USA. In a structural equation model (SEM), acculturation (English proficiency, residence index, and generational status) predicted the estriol/progesterone ratio (E/P), and the interaction of depressive symptoms with the E/P ratio predicted PTB. Undiagnosed depressive symptoms during pregnancy may have biological consequences increasing the risk for PTB.
Keywords: Preterm birth, Depression, Estriol, Progesterone, Acculturation
Hispanics are the fastest growing ethnic minority in the USA (March Of Dimes 2005). This population has a high fertility rate (Martin et al. 2010) and a high rate of preterm birth (PTB). One in eight Hispanic births in the USA in 2006 was preterm. Over the past decade, the PTB rate among Hispanic women has increased by 10% (March of Dimes 2005), with devastating effects on children and families and increasing medical costs. The US economic burden for this major public health issue was estimated to be a minimum of $26.2 billion yearly in 2005 (Behrman and Butler 2007). A growing body of evidence has supported the existence of a “Hispanic paradox”: that healthy pregnancy outcomes have diminished as Hispanic immigrants modify their own culture to adapt to the US culture (Page 2004; McGlade et al. 2004; Brown et al. 2007).
To begin to understand the paradox, it is important to consider if such a paradox occurs with other immigrant groups in other countries. In Taiwan, there is evidence of a healthy immigrant maternal effect on neonatal health both for Chinese and Vietnamese mothers (Hsieh et al. 2011; Xirasagar et al. 2011). In Italy, the paradox does not apply as migrant status is associated with worse infant outcomes, and improvement is attributed to increased accessibility to care (Cacciani et al. 2011). In Canada, research has revealed that selective migration from non-industrialized countries is protective, but migration from industrialized countries is not protective (Urquia et al. 2010). In Thailand, there seems to be no difference in preterm birth between immigrants and native born (Phadungkiatwattana et al. 2011). Therefore, the paradox varies highly with the country and ethnicity studied as to whether the phenomenon is applicable.
In the past 10 years, evidence has shown that acculturation of Hispanics into the US culture has adversely affected the biological mechanisms that maintain pregnancy, particularly the progesterone and estriol balance, thus increasing the risk of PTB (Ruiz et al. 2008). We therefore sought to examine possible explanations for the adverse effects related to acculturation associated with preterm birth.
Predicting preterm birth
There are many considerations when examining causes of PTB as PTB etiologies are believed to be multifactorial (Kamel 2010). One factor is prepregnant body mass index (BMI). A meta-analysis (McDonald et al. 2010) found no increased risk of spontaneous PTB in overweight or obese women, but the risk for medically indicated PTB was increased (Relative risk 1.30; CI 1.23; 1.37). In addition, the risk of spontaneous PTB has been shown to be increased when the maternal BMI is less than 19.6 (Iams 2003). There are many sociodemographic factors that have been examined regarding etiology and risk factors for PTB. Low socioeconomic status has been associated with PTB and is likely caused by factors related to women living in poverty, such as being younger, being single, and using more tobacco and illicit drugs. These factors examined independently have not been shown to be causative for PTB, but it is believed that the combination of these factors contributes to the likelihood of PTB (Reedy 2007). Evidence for a causal role for infection with PTB has been reviewed in detail (Romero et al. 2006), and infection has been implicated as an important factor leading to PTB. One of the most important factors consistently predicting PTB has been a history of PTB, with at least a 1.5- to 2-fold increased risk for a repeat PTB (Iams & Berghella 2010).
Progesterone and estriol are considered essential hormones in pregnancy, and it has been hypothesized that both hormones are part of the process of parturition (Brown et al. 2004; Kamel 2010; Vidaeff and Ramin 2008). There has been much investigation into the idea of functional progesterone withdrawal. When progesterone pathways no longer keep the uterus in a quiescent state, it has been thought that estrogen then counterbalances the effects of progesterone on the uterus and activates contractile pathways. Smith et al. (2009) collected serial blood samples to determine predelivery changes in the ratios of estriol (E3), estradiol (E2), and progesterone. They found that both E3 and E2 increased, and the progesterone/estriol ratio decreased in the month before delivery, e.g., progesterone levels were lower, and E3 levels were higher. Other investigators (Mesiano 2004) have suggested that the receptors of progesterone and estrogen may interact; thus, the receptors may be important in the change of the hormonal balance leading to estrogen activation and functional progesterone withdrawal.
It is important to consider alternative explanations related to acculturation affecting progesterone and estriol levels and increasing the risk of PTB. One study (Nagata et al. 2007) presented data that estriol levels in pregnancy may be regulated by polyunsaturated fatty acids in the diet, mediating the effects on fetal growth. However, a systematic review (Ayala et al. 2008) focusing on the relationship between acculturation and diet revealed several consistent results. First, there was no relationship between acculturation and dietary fat intake, despite the fact that dietary fat intake did vary between the less and more acculturated. The more acculturated individuals consumed more fast food, fatty snacks, and added fats than the less acculturated individuals. Those who were less acculturated used more whole milk and lard to cook with and ate more fruit, rice, and beans. Second, the results of this review found strong evidence that dietary cholesterol intake was not associated with acculturation. Since progesterone and estriol are biochemically broken down from cholesterol in the placenta (Creasy et al. 2009), these data are particularly relevant to refute any competing hypothesis that diet changes related to the acculturation process may explain the changes in progesterone and estriol.
In previous research with Hispanic women (Ruiz et al. 2008), acculturation, as operationalized by English proficiency, predicted a change in the progesterone/estriol ratio, i. e., lower serum progesterone levels and higher serum E3 levels. Thus, factors associated with progesterone and E3 levels may be important in predicting PTB. We included progesterone and E3 measured in the blood as key indicators that have been previously identified (Ruiz et al. 2008) related to the process of parturition. Progesterone and E3 were part of a larger study related to other stress hormones and immune factors in the blood related to parturition.
Antenatal maternal depressive symptoms have been linked to PTB in some, but not all, research studies (Grote et al. 2010). The evidence has revealed a somewhat inconsistent picture (Yonkers et al. 2009). Some evidence has suggested that depression during pregnancy may be associated with PTB (Dayan et al. 2006; Orr et al. 2002). Other studies (Andersson et al. 2004; Copper et al. 1996) have reported no relationships between depressive symptoms and PTB. Explanations for these conflicting findings may be (a) the population studied, (b) the extent to which the control variables are included, such as SES, race/ethnicity, antidepressant use, smoking, substance use, previous PTB, or medical complications, and (c) the study design, methods, sample sizes, and the timing and type of depression measurement (Grote et al. 2010). Grote et al.’s (2010) recent meta-analysis indicated that depression in pregnancy, regardless of categorical or continuous measurement, was associated with a modest but significantly increased risk for PTB. Lower socioeconomic status women had an increased risk of PTB. Another report (Smith et al. 2011) described a study associated with the Healthy Start Initiative. After adjustment for covariates, women with probable depression were one and one-half times more likely to deliver a PTB baby as compared to non-depressed women. Another recent study (Fransson et al. 2011) used the Edinburgh Postnatal Depression Scale to measure depressive symptoms at 16-week gestation in their Swedish sample. Their results also indicated an increased risk of PTB when the cutoff score was 12 or higher (OR 1.56, 95% CI 1.03, 2.35). Thus, the more recent studies have indicated an increased risk for PTB when pregnant women have greater depressive symptoms.
Acculturation is a factor that potentially explains levels of depressive symptoms in pregnant Hispanic women. Acculturation may be defined as the development of new cultural traits when two previously culturally distinct groups interact with one another (Hunt et al. 2004). Several studies (Fortner et al. 2010; Lara et al. 2009) found a high prevalence of prenatal depressive symptoms (30–32% of the sample) among Hispanics. However, the rate of depressive symptoms during pregnancy in the general population varies widely, ranging from 16% (Rich-Edwards et al. 2006) to 53% (Zayas et al. 2003), with highest rates among low socioeconomic status and ethnic minorities. Rates have indicated that Hispanic women with extensive exposure to the US culture (i.e., more acculturated) represent an at-risk population for increased risk of depression (Davila and McFall 2009; Lara et al. 2009) and PTB (March of Dimes 2005). Investigators have used language preference, country of birth, years in the USA, and generational status as proxies for acculturation measures (Fortner et al. 2010). However, there is some controversy related to the Hispanic paradox; some evidence indicates that immigrant women may be at higher risk for depression (Ding and Hargraves 2009). Additionally, investigation into the subgroups of Hispanics has revealed that the paradox holds for Mexicans regarding anxiety and depression, but not to Puerto Ricans, indicating that the phenomenon may vary by Hispanic subgroup (Alegria et al. 2008).
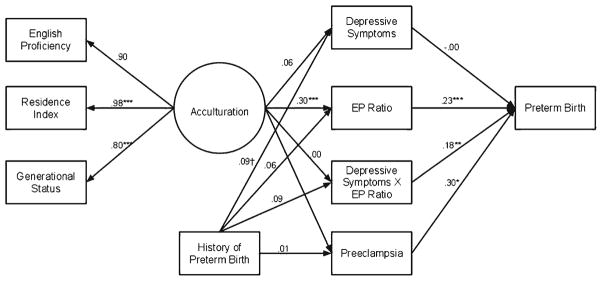
The present study examined interactions between psychological factors and the neuroendocrine system from a psychoneuroimmunological (PNI) perspective. Psychoneuroimmunology (PNI) is the study of the interactions among one’s psychological state (“psycho”), neuroendocrine system (“neuro”), and immune system (“immunology”) (Ader 1981; Nguyen 1991; Kiecolt-Glaser and Kiecolt-Glaser 1991). PNI provided a framework for examining the relationships between psychosocial/cultural and biological phenomena and their influence on health outcomes. The PNI model implemented in the present study examined the impact of interactions between a psychological factor, depression, and the biological factors, E3 and progesterone, on increasing the risk of PTB (see discussion in the “Methods” section for an explanation of the limited number of variables due to low occurrence of PTB in the sample). Depressive symptoms were selected as the psychological variable due to the prevalence in the sample and its prevalence in Hispanic women during pregnancy (Fortner et al. 2010; Rich-Edwards et al. 2006). E3 was selected due its possible links to poor birth outcomes and PTB (Brown et al. 2004; Kamel 2010; Vidaeff and Ramin 2008). Progesterone was chosen as it has a key role in the maintenance of pregnancy (Smith et al. 2009). Our model tested the hypothesis that depressive symptoms, progesterone, and E3 interact and have additive effects in pregnancy, and the combination of changing levels or changes in the ratio with depressive symptoms increases the risk of PTB. We also examined the impact of acculturation as an antecedent of these factors in light of the evidence that greater acculturation in Hispanics is associated with poorer health outcomes (Franzini et al. 2001). In addition, several variables were examined for inclusion in the model due to possible causal relationships with PTB. Figure 1 illustrates the PNI theoretical model with the proposed interactions between acculturation, depressive symptoms, progesterone, E3, and preterm birth.
Fig. 1.
Conceptual model of psychoneuroimmunology (PNI) tested in this study
Purpose and hypotheses
The purpose of the study was to examine the effects of acculturation, depressive symptoms, progesterone, and E3 as predictors of PTB in pregnant Hispanic women. The following hypotheses were tested based on the PNI theoretical framework: (a) There are differences in depressive symptoms by acculturation, (b) depressive symptoms, progesterone, and E3 interact to increase the risk of PTB, and (c) acculturation predicts the interaction of depressive symptoms with the E3/progesterone ratio.
Methods
The study design was cross-sectional. We recruited pregnant women for data collection at 22–24-week gestational age. Twenty-two- to twenty-four-week gestation was chosen because, at that time period in gestation, the fetus is considered viable. In addition, earlier work has established that this is a key time to measure biological factors related to PTB (Ruiz et al. 2002). The inclusion criteria were (a) ability to read and speak English or Spanish, (b) pregnancy with only one fetus, (c) self-identification of Hispanic ethnicity, (d) pregnant less than 22-week gestation, and (e) age 14–40. The exclusion criteria are identified in Table 1. Participants were kept in the study if they were treated with diet only for gestational diabetes or if they were diagnosed with preeclampsia after data collection. Diagnosis for gestational diabetes and preeclampsia was determined by the obstetrical care providers as determined on the prenatal or medical records. The Institutional Review Boards at The University of Texas Medical Branch in Galveston and The University of Texas Health Science Center in San Antonio approved the study. The study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. Informed consent in Spanish or English was obtained from all participants.
Table 1.
Exclusion criteria. If a potential participant reported one or more of the following conditions, she was excluded from the study
| -Identified cervical or intrauterine abnormalities | -Oral steroid use within one month of data collection |
| -Inability to read Spanish or English | -Congenital fetal abnormalities revealed by ultrasound |
| -Kidney disease | -Active placenta previa |
| -Multiple gestation | -Cervico-vaginal bleeding |
| -Immune disorders | -Blood group isoimmunization |
| -Heart disease | -Diagnosis of major mental disorders |
| -Asthma | -Antidepressant use |
| -Diabetes | -Self-identification of non-Hispanic ethnicity |
| -Hypertension | |
| -Identified pre eclampsia |
The study occurred during the years 2003–2007 in several regions in Texas. Participants from the Houston/Gulf Coast area were chosen from a single community clinic in Pasadena, TX (n=68). The majority of these participants were self-pay or had state-funded insurance. The second region was from the San Antonio/South Texas area, coming from five private-practice physicians (n=172) and had primarily Medicaid or private insurance. The third region was from the Austin/Central Texas area, coming from five Austin community clinics (n=279) and were primarily self-pay or had state-funded insurance.
We identified potential participants through examination of medical charts. Participants whose gestational age was less than 20 weeks or earlier were approached either before or after routine prenatal doctor visits. Convenience sampling was used to recruit all participants who met the criteria. After obtaining informed consent, a research nurse scheduled a separate appointment with the participant for data collection. During the data collection visit, the nurses acquired demographic data, including the participants’ age, number of pregnancies (gravidity), marital status, years in the USA, generational status, and where they were born (foreign born or US born), and administered self-report questionnaires (acculturation and depressive symptoms). The research nurses also noted from the prenatal chart any history of PTB. Height and prepregnancy weight were recorded from the prenatal chart to determine body mass index (BMI). Any incidence of infection during pregnancy was recorded from the prenatal chart. The nurses asked if any medications were taken, and the time those medications were last taken was also recorded based on participant recall. The nurses also drew a venous blood sample and collected a urine sample to be commercially analyzed for cotinine to quantitatively measure smoking. All appointments took place only between 1 p.m. and 3 p.m. to control any potential diurnal variation of E3 and progesterone.
After birth, we obtained maternal and infant outcomes by chart review. We used an ultrasound at less than 20 weeks as preferred dating criteria to establish gestational age at birth. The definition used for PTB was parturition before 37-week 0-day gestational age and included both spontaneous PTB and medically indicated PTB due to preeclampsia.
Acculturation measures
We used a self-report instrument, the Bidimensional Acculturation Scale (BAS) for Hispanics, to measure acculturation (Marin and Gamba 1996). The instrument assesses bidirectional changes in behavior in two cultural areas: Hispanic and non-Hispanic. We chose to administer The Language Proficiency (LPS) subscale out of the BAS as it is a briefer version that provides a rapid and valuable measure of acculturation (Marin and Gamba 1996). Participants with scores above 2.5 on the Language Proficiency subscale were interpreted to be English proficient. Previous testing with the BAS showed high internal consistency and high validity coefficients, working well with Mexican–Americans and with Central Americans (Marin 1992). The LPS subscale of the BAS to measure English proficiency in this study had a high alpha reliability coefficient of 0.89. In addition, we used demographic measures associated with acculturation such as years in the USA, whether the participant had Medicaid or private health insurance, and country of birth (US versus foreign born). In previous studies (Ruiz et al. 2007), greater residence in the USA for more than 10 years indicated a potential greater acculturation. Residence index was calculated by subtracting years spent in the USA from the participant’s age to operationalize exposure to the US culture. Generational status was determined by categorizing the participant as first generation if she was foreign born, second generation if her mother was foreign born and she was born in the USA, and third generation if the participant, her mother, and her grandmother were all born in the USA.
Depressive symptoms
We used the Center of Epidemiological Studies Depression Index (CES-D) (Radloff 1977) to evaluate depressive symptoms. All questionnaires were completed during the same data collection visit as when the blood samples were collected. The CES-D is a 20 item, 4-point Likert scale ranging from never (0) to most of the time (3) and has been used to assess the overall level of depressive symptoms experienced in the past week. Potential scores range from 0–60, with elevated scores indicating greater depressive symptomatology. It is appropriate for use in general populations, as well as pregnant populations, and has strong psychometric properties (α=0.85) (Radloff 1977). We defined depressive symptoms as a CES-D score of >16 as that has been used in many investigations about depression during pregnancy (Lancaster et al. 2010; Ruiz et al. 2007). The CES-D had an alpha reliability coefficient of 0.87 for this sample.
Estriol
We collected 20 ml of blood for the entire large study, and aliquoted 0.5 ml for E3 measurements. Blood samples were centrifuged at 2,000×g (10 min) immediately after being drawn, and the serum decanted into polypropylene tubes and stored on ice until they could be placed in a −80°C freezer no more than 4 h after collection. E3 levels were analyzed by EIA (Labor Diagnostika Nord, Germany) according to the manufacturer’s instructions. The EIA was read spectrophotometrically at 450 nm with a μ-Quant Reader (Bio-Tek Instruments, Inc., Winooski, VT). The interassay coefficient of variation was 10.18%, with the sensitivity of the assay at 0.02 ng/ml. The same laboratory technician conducted the analyses and was blinded to participant names and histories.
Progesterone
Progesterone was also analyzed using an Enzyme Immunoassay technique (MP Biomedicals, Irvine, CA) and read spectrophotometrically at 450 nm using the same μ-Quant Reader as for estriol (Bio-Tek Instruments, Inc. Winooski, VT). The interassay coefficient of variation for progesterone was 9.04%, and the sensitivity of the assay was 0.3 ng/ml.
Statistical analysis
We formed a ratio of E3 to progesterone (henceforth EP ratio) by dividing E3 by progesterone.1 Prior to forming the ratio, we transformed E3 and progesterone into their natural log to improve interpretability as log values approximate proportional change.
Prior to model building, we computed descriptive statistics for demographic and biological measures. We conducted bivariate analyses within the group of PTB’s for relationships with depression, including the EP ratio. Model building was conducted in two phases. In the first phase of model building, we assessed the impact of potentially confounding variables on the outcome variable using guidelines developed by Hosmer and Lemeshow (2000). We used SAS statistical software (version 9.2, Cary, NC,) to fit all models described in this phase of the analysis. There were two variables of clinical interest for our model, EP ratio and depressive symptoms (CES-D), and seven potentially confounding variables that were evaluated for inclusion in the model, including history of PTB, preeclampsia, marital status, infections during pregnancy, age, BMI, and gestational age at which the blood was drawn. We considered epidemiological methods for model fitting that favor all potentially relevant variables added in the model to account for the potential of confounding effects. The combination of several control variables collectively is thought to produce a confounding effect (Greenland 1989). While we favor this approach, it has the potential to overfit the data and thus produces inflated standard errors and numerically unstable results. In addition, there were a limited number of events of PTB’s (n=33). While there are no firm rules on the number of covariates per event, guidelines suggest that there should be ten events per covariate (Hosmer and Lemeshow 2000). Following this guideline, we have the potential to include no more than three covariates, which would only allow us to examine the two variables of interest and their interaction. However, we felt that it was important to consider other potentially confounding variables and examined these variables following recommendations from Hosmer and Lemeshow (2000) in which variables are examined in the following sequence: (1) Univariable analyses are conducted using Pearson’s Chi-square tests between the outcome and each of the categorical variables, and t tests are conducted using the outcome as an independent variable for the continuous variables, (2) non-significant variables are excluded from the model, (3) the importance of each variable is verified in the multivariable model, (4) examine categorical variables for appropriate categories, and examine linearity in continuous variables, and (5) interactions are fit.
In the second phase of model building, we constructed a structural equation model (SEM) by introducing acculturation as an exogenous variable. This model incorporated variables and interactions selected in the first phase of data analysis. Acculturation was considered to be an exogenous variable as it temporally precedes the E/P ratio and CES-D measures that were taken before delivery. We also evaluated covariates retained from the previous phase as being exogenous if they were present prior to pregnancy and endogenous if they were present during pregnancy. All analyses in this phase of model building were implemented using the Mplus software (Muthén and Muthén 2010). We implemented a probit regression model rather than a logistic model because the probit model provides fit indices that are not available for logit models. Mplus implements direct maximum likelihood in model estimation, which makes use of all observed data in model estimation and is a method recommended for the analysis of data with missing values (Graham 2009) under the assumption that data are missing at random and thus allows us to make use of data from all 470 participants in model estimation.
Results
A post-hoc power analysis was conducted using the smallest and largest observed significant effects by using standardized coefficients in a linear regression power analysis. The depression by EP ratio interaction predicting PTB was the smallest standardized coefficient with a value of 0.18 and with a post-hoc power of 0.98, and the largest was the acculturation path to EP ratio with a value of 0.30 and a post-hoc power of >0.99.
Descriptive statistics and results for hypothesis a
There are differences in depressive symptoms by acculturation.
Seven percent of the sample had a PTB. The mean level for EP ratio was 0.29 ng/ml (SD 0.17). The average CES-D score was 14.57 (SD=9.25); 40.3% of the sample exhibited CES-D scores greater than or equal to 16, which is indicative of “mild” to “severe” depressive symptomatology. The range of household yearly income for the sample was $1,500 to $135,000, with a mean of $20,584 (SD=$13,145). Single participants were more acculturated: English proficiency was 2.58 (SD=1.24) for single participants, whereas married participants averaged 2.06 (SD=1.19, t (465)=4.68, p<0.001. Residence index was used as a measure of exposure to the American culture. Years in the USA minus age equaled the residence index (Alegria et al. 2007), with smaller numbers indicating greater acculturation. Therefore, the closer to zero or negative number, the greater was the acculturation. Thus, the residence index had an inverse relationship to acculturation as lesser acculturation equaled larger numbers. Residence index was −11.70 (SD=10.40) for single participants, in contrast to married participants who averaged −16.45 (SD=9.08), t (467)=5.15, p<0.001. For single participants, the mean for generational status was 1.64 (SD=0.64), in contrast to married participants who averaged 1.37 for generational status (SD= 0.73), t (467)=3.68, p<0.001.
Table 2 provides sample characteristics as well as Chi-square analysis demonstrating significant differences in proportions between higher depressive symptom scores in the more acculturated participants as compared to the less acculturated participants. The variables used to operationalize acculturation for Table 2 were years in the USA, English proficiency, presence of medical insurance, and having been born in the USA. Two variables, presence of insurance and having been born in the USA, indicate significant differences in depressive symptoms by acculturation.
Table 2.
Sample characteristics, depressive symptom scores, estriol/progesterone (E/P ratio) levels, and preterm birth percentages
| Demographic, obstetrical, and acculturation variables | Total sample % (n=470) | High depression scores % (dichotomized by CES-D ≥16) | EP ratio levels means and standard deviations (SD) | Preterm % within row (n=33) |
|---|---|---|---|---|
| Age | ||||
| Younger than 18 | 6.0% (n=28) | 50.0% (n=14) | 0.34 (0.15) | 7.1% (n=2) |
| 18–34 | 91.3% (n=429) | 39.6% (n=170) | 0.27 (0.17) | 7.2% (n=31) |
| 35 or older | 2.8% (n=13) | 38.5% (n=5) | 0.34 (0.17) | 0.0% (n=0) |
| Body mass index | ||||
| Normal | 49.4% (n=204) | 40.7% (n=83) | 0.27 (0.17) | 8.3% (n=17) |
| Overweight | 33.2% (n=137) | 42.3% (n=58) | 0.28 (0.17) | 6.6% (n=9) |
| Obese | 17.4% (n=72) | 36.1% (n=26) | 0.26 (0.19) | 2.8% (n=2) |
| Gravida | ||||
| 1 pregnancy | 27.6% (n=128) | 35.9% (n=46) | 0.28 (0.17) | 8.6% (n=11) |
| 2 pregnancies | 30.2% (n=140) | 41.4% (n=58) | 0.27 (0.17) | 3.6% (n=5) |
| 3 pregnancies | 22.9% (n=106) | 44.3% (n=47) | 0.26 (0.16) | 9.4% (n=10) |
| 4 or more pregnancies | 19.2% (n=89) | 40.4% (n=36) | 0.31 (0.18) | 7.9% (n=7) |
| Marital status | ||||
| Currently married | 57.4% (n=269) | 44.2% (n=119) | 0.28 (0.17) | 6.7% (n=18) |
| Not married | 42.6% (n=200) | 35.0% (n=70)a | 0.28 (0.18) | 7.5% (n=15) |
| History of preterm birth | ||||
| No | 92.1% (n=434) | 38.9% (n=169) | 0.28 (0.17) | 6.2% (n=27) |
| Yes | 7.9% (n=37) | 56.8% (n=21)a | 0.29 (0.18) | 16.2% (n=6)a |
| Preeclampsia | ||||
| No | 92.4% (n=400) | 40.0% (n=160) | 0.28 (0.17) | 6.0% (n=24) |
| Yes | 7.6% (n=33) | 45.5% (n=15) | 0.24 (0.15) | 15.2% (n=5)a |
| Infection during pregnancy | ||||
| No | 56.0% (n=247) | 35.6% (n=88) | 0.27 (0.18) | 8.1% (n=20) |
| Yes | 44.0% (n=194) | 45.9% (n=89)a | 0.28 (0.17) | 5.2% (n=10) |
| Acculturation variable: years in the USA | ||||
| Less than 10 | 58.3% (n=274) | 36.9% (n=101) | 0.24 (0.16) | 5.1% (n=14) |
| 10 or more | 41.7% (n=196) | 44.9% (n=88) | 0.33 (0.17) | 9.7% (n=19) |
| Acculturation variable: English proficiency (from the BAS) | ||||
| Low (< 2.5) | 62.0% (n=290) | 38.3% (n=111) | 0.24 (0.16) | 5.2% (n=15) |
| High (≥ 2.5) | 38.0% (n=178) | 43.3% (n=77) | 0.34 (0.17) | 10.1% (n=18)a |
| Acculturation variable: medical insurance (Medicaid or private insurance) | ||||
| No | 65.9% (n=307) | 36.8% (n=113) | 0.24 (0.16) | 5.5% (n=17) |
| Yes | 34.1% (n=159) | 46.5% (n=74)a | 0.36 (0.17) | 10.1% (n=16) |
| Acculturation variable: born in the USA | ||||
| No | 68.2% (n=320) | 37.2% (n=119) | 0.24 (0.15) | 5.6% (n=18) |
| Yes | 31.8% (n=149) | 47.0% (n=70)a | 0.36 (0.17) | 10.1% (n=15) |
Statistically significant at p<0.05 using χ2, analysis of variance, or independent t-tests
Because PTB was a primary outcome variable for the study, we examined characteristics surrounding PTB. Out of 33 PTB’s, there were 28 spontaneous, and five were delivered due to preeclampsia. Thirty-seven participants out of the total sample had a history of PTB, of which six delivered preterm. Nine of the thirty-three preterm infants were less than 34-week gestation. Of the 33 PTB’s, there were no women with sexually transmitted diseases or documented chorioamnionitis on the medical record. Out of the entire sample, there were very few smokers, with only three participants who tested positive for cotinine. One participant reported illegal drug (opiate) use, but this participant did not deliver prematurely.
Although the percentage of PTB from this sample was low (7%), this was due to a large number (290) of participants in the sample being primarily proficient in Spanish or born in Mexico (320) and were new immigrants here (less than 5 years in the USA). These women had a 5% PTB rate, compared to the 10% rate of the women who spoke English (n=178) or were born in the USA (n=149), of which the sample had a smaller number. The majority of the women were new immigrants with better birth outcomes; thus, the total percentage of PTBs was smaller overall.
We also examined factors that possibly could have had an effect on estriol and thus the EP ratio levels. There was only one participant, of those who had preterm birth, who was on antibiotics 2 weeks before data collection. The rest of the preterm births were not on antibiotic therapy, steroids, or antidepressant medications. We used gestational age at time of blood draw to control for variations in EP ratio by gestational age. Importantly, all of the different measures related to increased acculturation had similar rates of preterm birth. Three variables were significantly different in the rate of preterm birth: history of preterm birth, preeclampsia, and English proficiency.
Hypotheses b
Depressive symptoms, progesterone, and estriol interact to increase the risk of PTB.
Hypothesis c
Acculturation impacts the EP ratio and depressive symptoms.
Steps in model building
Following the variable selection steps outlined previously, we first examined univariable relationships with the outcome, PTB. Among the categorical variables, we observed a significant effect for the history of preterm birth (χ2=5.20, p=0.02) and preeclampsia (χ2=4.09, p=0.04), whereas there was no significant effect for marital status and preterm birth (χ2=0.11, p=0.73) or infections during pregnancy and preterm birth (χ2=1.48, p=0.22). Examining the differences between preterm and full-term infants for the continuous variables, there were no differences in age (t (468)=0.79, p=0.43), BMI (t (457)=0.66, p=0.51), gravida (t (461)= −0.55, p=0.58), or gestational age at which the blood was drawn (t (468)=−0.31, p=0.76). Second, we determined which variables to include in subsequent phases. After evaluating each of the possible potentially confounding variables in the model, there were five variables that we were clearly able to exclude: age, BMI, gravida, and gestational age at time of blood draw. History of preterm birth and preeclampsia were retained in all subsequent analyses. Third, in a multiple variable model that contained the two variables of primary interest, depression and EP ratio, we verified the importance of history of preterm birth which remained marginally significant (χ2=2.85, p=0.092), and preeclampsia was also marginally significant (χ2=3.82, p= 0.051). Fourth, we examined the linearity of continuous variables in logistic regression models with linear and quadratic trends. In models containing the variables entered in previous steps with the addition of a quadratic effect, neither the EP ratio quadratic effect (χ=2.18, p=0.14) nor the CES-D quadratic effect (χ2=0.30, p=0.586) was significant. Fifth, we examined interactions for each of the variables in the model. The interaction between EP ratio and history of PTB birth (χ2=0.43, p=0.513) and the interaction between CES-D and history of PTB (χ2=0.68, p=0.408) were not significant. The interaction between EP ratio and preeclampsia (χ2=0.249, p=0.618) and the interaction between CES-D and preeclampsia (χ2 =0.01, p=0.915) were not significant. The interaction between E3 and CES-D was significant (χ2=6.93, p=0.009), resulting in the interaction between EP ratio and CES-D being significant (χ2=5.33, p=0.021).
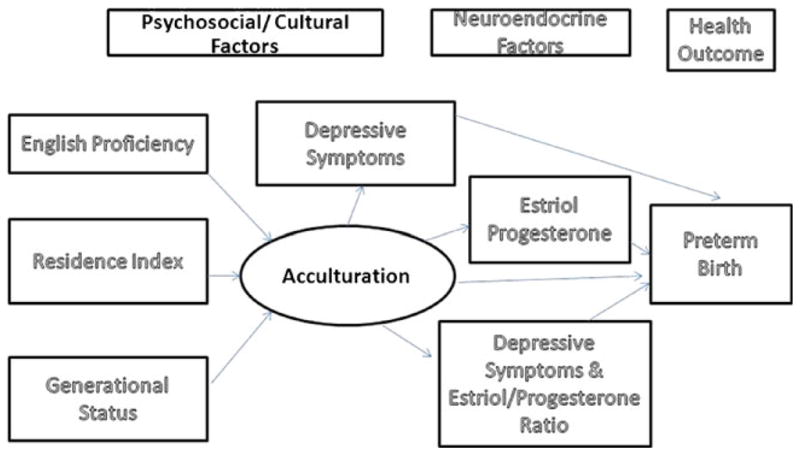
In the second phase of model building, we constructed the SEM model displayed in Fig. 2. Model fit was good for each of the fit indices: The χ2 test of model fit was not significant (χ2=23.75 (21), p=0.306), and all model fit indices exhibited good fit: Tucker–Lewis index=0.97, root mean square error of approximation=0.02 (95% CI=0.00, 0.04), and weighted root mean square residual=0.58. R2 for preterm birth was 0.18. The direct path from acculturation to EP ratio was significant. The direct path from history of PTB to depression was marginally significant (p=0.08). EP ratio, preeclampsia, and the EP ratio by CES-D interaction were significant predictors of PTB.
Fig. 2.
Structural equation model with standardized coefficients predicting PTB
Discussion
Hypothesis a tested for differences in depressive symptoms by acculturation and was clearly supported in the results presented in Table 2. Hypothesis b predicted an interaction of depressive symptoms, progesterone, and E3 that would increase the risk of PTB; this hypothesis was also supported. Hypothesis c predicted that acculturation would directly affect the E/P ratio and depressive symptoms. The third hypothesis was partially supported in that acculturation directly predicted the E/P ratio, e.g., higher estriol, lower progesterone. But, acculturation did not directly significantly predict depressive symptoms. Only when E3, and thus the E/P ratio, interacted with depressive symptoms was the risk of PTB increased. This analysis possibly indicates the additive effect of depressive symptoms with E3 and progesterone, moderating the effect on PTB. Thus, these results may partially explain the finding that acculturation affects progesterone and estriol in Mexican origin Hispanic women to predict PTB (Ruiz et al 2008).
Acculturation was modeled as a latent variable using three indicators: English proficiency, residence index (years in the USA minus age), and generational status. These measures for acculturation are consistent with how acculturation was measured in other studies (Fuentes-Afflick and Hessol 2008; Himmelgreen et al. 2004). English proficiency and residence index could be easily assessed in a clinical setting. Within several minutes of initial greeting, care providers can establish the English proficiency of a woman. Providers may also quickly ask how long the woman has been in the USA, as well as her age. Closer matches between years in the USA and a woman’s age are associated with greater levels of acculturation. Thus, these data give indicators of how the risk of acculturation may be easily screened clinically.
Our results are consistent with recent findings demonstrating that depressive symptoms predict an increased risk of PTB (Grote et al. 2010; Smith et al. 2011). The current study focused specifically on the Hispanic Mexican origin population, and therefore, it is particularly applicable to that ethnicity. In the SEM model, depressive symptoms had a significant statistical interaction with the E/P ratio to predict PTB. While the direct path between acculturation and depressive symptoms wasn’t statistically significant in the SEM, it was apparent when examining the descriptive statistics that depressive symptoms were significantly higher in the more acculturated women. This finding suggested that the more acculturated women (those who have medical insurance and were born in the USA) have more risk of depressive symptoms.
It may also be important to consider other explanations for the acculturation effect on E3 and the E/P ratio. The most apparent possible explanation is the effect of acculturation on diet, which was discussed in the introduction. Other possible effects of acculturation related to estriol and PTB might be that as the women acculturate, they tend to be younger when they get pregnant and tend to be single, with the E/P ratios slightly higher (though not statistically significant).
It is significant to note that in this study, none of the participants were on medications for depression as that was an exclusion criterion. We were trying to avoid confounders, such as the use of antidepressants, which could affect the etiology of PTB. Some studies (Suri et al. 2007; Lund et al. 2009) have implicated the use of antidepressant medications, specifically selective serotonin reuptake inhibitors (SSRI’s), as increasing the risk of PTB. The evidence from this study suggests that it may be the pathophysiology resulting from depressive symptoms that is related to PTB, which, in this case, is specifically related to E3 and the E/P ratio.
The data presented related to history of PTB and preeclampsia predicting PTB are consistent with risk factors that are well established for PTB (Iams and Berghella 2010). Preeclampsia often correlates with PTB significantly as oftentimes early delivery is the only real cure to prevent severe complications from preeclampsia in both mother and infant. History of PTB is one of the strongest known risk factors for PTB (Iams and Berghella 2010), and the results from this study are consistent with earlier work.
The rates of depressive symptomatology reported from this study are congruent with the literature on the prevalence of depression in Hispanic women (Davila and McFall 2009; Lara et al. 2009). The findings reported from this study are also consistent with higher depressive symptoms during pregnancy (Zayas et al. 2003). In another study (Yonkers et al. 2001), the investigators reported that half of the Hispanic and African–American women suffered the beginnings of a major depressive disorder in their pregnancy. These findings underscore the vital need to screen for depressive symptoms during pregnancy.
The model from the PNI framework suggests that psychosocial factors, e.g., depressive symptoms, would interact in a bidirectional manner with the neuroendocrine factors or hormones, e.g., E3 and progesterone, thus suggesting an interaction between psychological and biological factors impacting health outcomes. Depressive symptoms did not directly predict PTB in the model; however, the combination of depressive symptoms with progesterone and E3 predicted PTB, indicating that the combined impact of these factors produced the greatest risk. It may be that the effects of the steroid hormone changes interact with the central nervous system and result in depressive symptoms, or it may be that the central nervous system response (manifested as depressive symptoms) affects the steroid hormones. These findings potentially have clinical significance in that it may be beneficial to screen for depressive symptoms, E3, and progesterone concurrently to better determine risk, for example, at the time of the multiple marker screen when E3 is normally included in testing. Acculturation directly impacted E3 and thus the E/P ratio, indicating that more acculturated women had higher levels of this risk factor for PTB. This finding is consistent with the Hispanic paradox, whereby more acculturated individuals exhibit poorer health outcomes (Franzini et al. 2001). The data presented here provide further evidence that acculturation of Mexican origin pregnant women may be part of an evolving risk profile to predict PTB. The risk profile holds promise to identify clinically those Hispanic pregnant women who are more acculturated, may score higher than 16 on the CES-D for depressive symptoms, and have a higher estriol level and a lower progesterone level. Further research will need to identify the accuracy of such predictions for clinical practice.
There are at least three limitations in the study of which we are aware. First, the cross-sectional design limited ability to determine when depressive symptoms might have a worse effect on PTB over different times in pregnancy. Second, the sample was a convenience sample, which possibly could have introduced bias in the results. Use of a self-report measure of depressive symptoms was another limitation as some of the questions ask about fatigue, changes in sleep, and changes in appetite that may have an overlap with symptoms in pregnancy. We recommend using a secondary measure of depression with the CES-D for validation of the results in this study.
The data presented from this study suggest that it is vital to screen for depressive symptoms early and often in pregnancy. The linkages of depressive symptoms to acculturation need further exploration in relationship to acculturative stress and discrimination, as well as to critical periods in pregnancy when depressive symptoms may have the most deleterious effect on pregnancy outcomes. We speculate that depressive symptoms may be worse in different stages of the acculturation process and that knowledge may be important for an evolving risk profile to prevent PTB. It will be important to develop innovative interventions to help facilitate the acculturation process and protect against depressive symptoms.
Acknowledgments
The authors would like to acknowledge the National Institute of Health National Institute of Nursing Research for funding this study, grant number: NINRR0107891
Footnotes
We elected to use an estriol to progesterone ratio, rather than the progesterone to estriol ratio used in Ruiz et al. (2008), so that the effects of the ratio and depressive symptoms, the other focal variable, were in the same direction, which facilitates interpretation (e.g., higher estriol to progesterone ratio and higher levels of depressive symptoms are considered to be unhealthy and thus more likely to lead to PTB).
Conflicts of interest The authors declare there are no conflicts of interest.
Contributor Information
R. Jeanne Ruiz, Email: jruiz@austin.utexas.edu, The School of Nursing, The University of Texas at Austin, 1700 Red River, Austin, TX 78701-1499, USA.
C. Nathan Marti, Consulting Services Division of Statistics and Scientific Computation, The University of Texas at Austin, Austin, TX, USA.
Rita Pickler, Cincinnati Children’s Hospital, Cincinnati, OH, USA.
Christina Murphey, The School of Nursing, The University of Texas at Austin, 1700 Red River, Austin, TX 78701-1499, USA.
Joel Wommack, The School of Nursing, The University of Texas at Austin, 1700 Red River, Austin, TX 78701-1499, USA.
Charles E. L. Brown, The University of Texas Southwestern Medical School, Austin, TX, USA
References
- Ader R. Psychoneuroimmunology. 1. Academic; Orlando: 1981. [Google Scholar]
- Alegria M, Shrout PE, Woo M, Guarnaccia P, Sribney W, Vila D, Polo A, Cao Z, Mulvaney N, Torres M, Canino G. Understanding differences in past year psychiatric disorders for Latinos living in the U.S. Soc Sci Med. 2007;65(2):214–230. doi: 10.1016/j.socscimed.2007.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Canino G, Shrout PE, Woo M, Duan N, Villa D, Torres M, Chen CN, Meng XL. Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. Am J Psychiatry. 2008;165(3):359–369. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson L, Sundstrom-Poromaa I, Wulff M, Astrom M, Bixo M. Neonatal outcome following maternal antenatal depression and anxiety: a population based study. Am J Epidemiol. 2004;159 (9):872–881. doi: 10.1093/aje/kwh122. [DOI] [PubMed] [Google Scholar]
- Ayala GX, Baquero B, Klinger S. A systematic review of the relationship between acculturation and diet among Latinos in the United States: implications for future research. J Am Diet Assoc. 2008;108:1330–1344. doi: 10.1016/j.jada.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behrman RE, Butler AS, editors. Preterm birth: causes, consequences, and prevention. Washington D.C: 2007. [PubMed] [Google Scholar]
- Brown AG, Leite RS, Strauss JF. Mechanisms underlying functional progesterone withdrawal at parturition. Ann N Y Acad Sci. 2004;1034:36–49. doi: 10.1196/annals.1335.004. [DOI] [PubMed] [Google Scholar]
- Brown HL, Chireau MV, Jallah Y, Howard D. The “Hispanic paradox”: an investigation of racial disparity in pregnancy outcomes at a tertiary care medical center. Am J Obstet Gynecol. 2007;197:e1–e9. doi: 10.1016/j.ajog.2007.04.036. [DOI] [PubMed] [Google Scholar]
- Cacciani L, Asole S, Polo A, Franco F, Lucchini R, DeCurtis M, DiLallo D, Guasticchi G. Perinatal outcomes among immigrant mothers over two periods in a region of central Italy. BMC Publ Health. 2011;11:294. doi: 10.1186/1471-2458-11-294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copper RL, Goldenberg RL, Das A, Elder N, Swain M, Norman G, Ramsey R, Cotroneo P, Collins BA, Johnson F, Jones P, Meier AM National Institute of Child Health and Human Development Units Network . The preterm prediction study: maternal stress is associated with spontaneous preterm birth at less than thirty-five weeks’ gestation. Am J Obstet Gynecol. 1996;175(5):1282–1286. doi: 10.1016/s0002-9378(96)70042-x. [DOI] [PubMed] [Google Scholar]
- Creasy RK, Resnik R, Iams JD. Creasy and Resnik’s maternal–fetal medicine: principles and practice. Saunders Elsevier; Philadelphia: 2009. [Google Scholar]
- Davila M, McFall SL. Acculturation and depressive symptoms among pregnant and postpartum Latinas. Matern Child Health J. 2009;13:318–325. doi: 10.1007/s10995-008-0385-6. [DOI] [PubMed] [Google Scholar]
- Dayan J, Creveuil C, Marks MN, Conroy S, Herlicoviez M, Dreyfus M, Tordjman S. Prenatal depression, prenatal anxiety, and spontaneous preterm birth: a prospective cohort study among women with early and regular care. Psychosom Med. 2006;68(6):938–946. doi: 10.1097/01.psy.0000244025.20549.bd. [DOI] [PubMed] [Google Scholar]
- Ding H, Hargraves L. Stress-associated poor health among adult immigrants with a language barrier in the United States. J Immigr Minority Health. 2009;11:446–452. doi: 10.1007/s10903-008-9200-0. [DOI] [PubMed] [Google Scholar]
- Fortner RT, Pekow P, Dole N, Markenson G, Chasan-Taber L. Risk factors for prenatal depressive symptoms among Hispanic women. Matern Child Health J. 2010 doi: 10.1007/s10995-010-0673-9. Online First. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fransson E, Ortenstrand A, Hjelmstedt A. Antenatal depressive symptoms and preterm birth: a prospective study of a Swedish national sample. Birth. 2011;38(1):10–16. doi: 10.1111/j.1523-536X.2010.00441.x. [DOI] [PubMed] [Google Scholar]
- Franzini L, Ribble JC, Keddie AM. Understanding the Hispanic paradox. Ethn Dis. 2001;11(3):496–518. [PubMed] [Google Scholar]
- Fuentes-Afflick E, Hessol NA. Acculturation and body mass among Latina women. J Women’s Health. 2008;17(1):67–73. doi: 10.1089/jwh.2007.0389. [DOI] [PubMed] [Google Scholar]
- Graham JW. Missing data analysis: making it work in the real world. Annu Rev Psychol. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Greenland S. Modeling and variable selection in epidemiologic analysis. Am J Public Health. 1989;79(3):340–349. doi: 10.2105/ajph.79.3.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grote N, Bridge JA, Gavin AR, Melville J, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012–1024. doi: 10.1001/archgenpsychiatry.2010.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himmelgreen DA, Perez-Escamilla R, Martinez D, Bretnall A, Eeells B, Peng Y, Bermudez A. The longer you stay, the bigger you get: length of time and language use in the U.S. are associated with obesity in Puerto Rican women. Am J Phys Anthropol. 2004;125 (1):90–96. doi: 10.1002/ajpa.10367. [DOI] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Appl logistic regression. 2. Vol. 354. Wiley; New York: 2000. Probability and statistics series. [Google Scholar]
- Hsieh WS, Hsieh CJ, Jeng SF, Liao HF, Su YN, Lin SJ, Chang PJ, Chen PC. Favorable neonatal outcomes among immigrants in Taiwan: evidence of a healthy immigrant mother effect. J Women’s Health. 2011;20(7):1083–1090. doi: 10.1089/jwh.2011.2809. [DOI] [PubMed] [Google Scholar]
- Hunt L, Schneider S, Corner B. Should “acculturation” be a variable in health research? A critical review of research on U.S. Hispanics. Soc Sci Med. 2004;59:973–986. doi: 10.1016/j.socscimed.2003.12.009. [DOI] [PubMed] [Google Scholar]
- Iams JD. The epidemiology of preterm birth. Clin Perinatol. 2003;30:651–664. doi: 10.1016/s0095-5108(03)00101-5. [DOI] [PubMed] [Google Scholar]
- Iams JD, Berghella V. Care for women with prior preterm birth. Am J Obstet Gynecol. 2010;203(2):89–100. doi: 10.1016/j.ajog.2010.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamel RM. The onset of human parturition. Arch Gynecol Obstet. 2010;281:975–982. doi: 10.1007/s00404-010-1365-9. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JKG, Kiecolt-Glaser R. Psychoneuroimmunology. 2. Academic; San Diego: 1991. [Google Scholar]
- Lancaster CA, Gold KJ, FlynnHA YH, Marcus SM, Davis MM. Risk factors for depressive symptoms during pregnancy: a systematic review. Am J Obstet Gynecol. 2010;202:5–14. doi: 10.1016/j.ajog.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara A, Le H, Letechipia G, Hochausen L. Prenatal depression in Latinas in the U.S. and Mexico. Matern Child Health J. 2009;13:567–576. doi: 10.1007/s10995-008-0379-4. [DOI] [PubMed] [Google Scholar]
- Lund N, Pedersen LH, Henriksen TB. Selective serotonin reuptake inhibitor exposure in utero and pregnancy outcomes. Arch Pediatr Adolesc Med. 2009;163(10):949–954. doi: 10.1001/archpediatrics.2009.164. [DOI] [PubMed] [Google Scholar]
- March of Dimes Special Report. Born Too Soon: Prematurity in the Hispanic Population. [www] 2005 www.marchofdimes.com.
- Marin G. Issues in the measurement of acculturation among Hispanics. In: Geisinger KF, editor. Psychological testing of Hispanics. American Psychological Association; Washington: 1992. pp. 23–51. [Google Scholar]
- Marin G, Gamba RJ. A new measurement of acculturation for Hispanics: the Bidimensional Acculturation Scale for Hispanics (BAS) Hisp J Behav Sci. 1996;18:297–316. [Google Scholar]
- Martin JA, Hamilton BE, Sutton PD, et al. Births: final data for 2007. National Vital Statistics Report. 2010;58(24):1–85. Retrieved Aug 9 2010. [PubMed] [Google Scholar]
- McDonald SD, Han Z, Mulla S, Beyene J. Overweight and obesity and risk of preterm birth and low birth weight infants: systematic review and metaanalysis. Br Med J. 2010;341c:3428. [Google Scholar]
- McGlade MS, Saha S, Dahlstrom ME. The Latina paradox: an opportunity for restructuring prenatal care delivery. Am J Public Health. 2004;94:2062–2065. doi: 10.2105/ajph.94.12.2062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesiano S. Myometrial progesterone responsiveness and the control of human parturition. J Gynecol Invest. 2004;11(4):193–202. doi: 10.1016/j.jsgi.2003.12.004. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 6. Muthén & Muthén; Los Angeles: 1998–2010. [Google Scholar]
- Nagata C, Iwasa S, Shiraki M, Sahashi Y, Shimizu H. Association of maternal fat and alcohol intake with maternal and umbilical hormone levels and birth weight. Cancer Sci. 2007;98(6):869–873. doi: 10.1111/j.1349-7006.2007.00464.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen TV. Mind, brain, and immunity: a critical review. Holist Nurs Pract. 1991;5(4):1–9. doi: 10.1097/00004650-199107000-00003. [DOI] [PubMed] [Google Scholar]
- Orr ST, James SA, Blackmore Prince C. Maternal prenatal depressive symptoms and spontaneous preterm births among African–American women in Baltimore, Maryland. Am J Epidemiol. 2002;156(9):797–802. doi: 10.1093/aje/kwf131. [DOI] [PubMed] [Google Scholar]
- Page RL. Positive pregnancy outcomes in Mexican immigrants: what can we learn? J Obstet Gynecol Nurs. 2004;33(6):783–790. doi: 10.1177/0884217504270595. [DOI] [PubMed] [Google Scholar]
- Phadungkiatwattana P, Rujiwetpongstorn J, Tansathit T, Srisantiroj N. Pregnancy outcomes of Southeast Asian immigrant pregnant women compared with Thai pregnant women in Rajavithi Hospital. J Med Assoc Thailand. 2011;94(2):147–151. [PubMed] [Google Scholar]
- Radloff LS. The center for epidemiologic studies depression index. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- Reedy N. Born too soon: the continuing challenge of preterm labor and birth in the United States. J Nurs Midwif. 2007;52(3):281–290. doi: 10.1016/j.jmwh.2007.02.022. [DOI] [PubMed] [Google Scholar]
- Rich-Edwards JW, Kleinman K, Abrams A, et al. Sociodemographic predictors of antenatal and postpartum depressive symptoms among women in a medical group practice. J Epidemiol Community Health. 2006;60:221–227. doi: 10.1136/jech.2005.039370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romero R, Espinoza J, Kusanovic JP, Gotsch F, Hassan S, Erez O, Chaiworapongsa T, Mazor M. The preterm parturition syndrome. Br J Obstet Gynecol. 2006;113(Suppl 3):17–42. doi: 10.1111/j.1471-0528.2006.01120.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz RJ, Dudley D, Brown CEL, Fullerton J. Predicting risk of preterm birth: the roles of stress, corticotrophin releasing hormone, traditional clinical risk factors. Bio Res Nurs. 2002;4(1):54–65. doi: 10.1177/1099800402004001007. [DOI] [PubMed] [Google Scholar]
- Ruiz RJ, Stowe RP, Goluszko E, Clark M, Tan A. The relationships among acculturation, body mass index, depression, and interleukin 1-receptor antagonist in Hispanic pregnant women. Ethn Dis. 2007;17:338–343. [PubMed] [Google Scholar]
- Ruiz RJ, Saade GR, Brown CE, et al. The effect of acculturation on progesterone/estriol ratios and preterm birth in Hispanics. Obstet Gynecol. 2008;111(2 Pt 1):309–316. doi: 10.1097/01.AOG.0000297896.00491.2c. [DOI] [PubMed] [Google Scholar]
- Smith R, Smith J, Shen X, Engel P, Bowman ME, McGrath SA, Bisits AM, McElduff P, Giles WB, Smith D. Patterns of plasma corticotropin releasing hormone, progesterone, estradiol, and estriol change and the onset of human labor. J Clin Endocrin Metabol. 2009;94:2066–2074. doi: 10.1210/jc.2008-2257. [DOI] [PubMed] [Google Scholar]
- Smith MV, Shao L, Howell H, Lin H, Yonkers KA. Perinatal depression and birth outcomes in a healthy start project. Matern Child Health J. 2011;15:401–409. doi: 10.1007/s10995-010-0595-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suri R, Altshuler L, Hellemann G, Burt VK, Aquino A, Mintz J. Effects of antenatal depression and antidepressant treatment on gestational age at birth and risk of preterm birth. Am J Psychiatr. 2007;164:1206–1213. doi: 10.1176/appi.ajp.2007.06071172. [DOI] [PubMed] [Google Scholar]
- Urquia ML, Frank JW, Glazier RH. From places to flows. International secondary migration and birth outcomes. Soc Sci Med. 2010;71(9):1620–1626. doi: 10.1016/j.socscimed.2010.08.006. [DOI] [PubMed] [Google Scholar]
- Vidaeff AC, Ramin SM. Potential bichemical events associated with initiation of labor. Curr Med Chem. 2008;15:614–619. doi: 10.2174/092986708783769786. [DOI] [PubMed] [Google Scholar]
- Xirasagar S, Fu JC, Liu J, Probst JC, Lin DP. Neonatal outcomes for immigrant vs. native-born mothers in Taiwan: an epidemiological paradox. Matern Child Health. 2011;15(2):269–279. doi: 10.1007/s10995-010-0612-9. [DOI] [PubMed] [Google Scholar]
- Yonkers KA, Ramin SM, Rush AJ, Navarette CA, Carmody MD, et al. Onset and persistence of postpartum depression in an inner-city maternal health clinic system. Am J Psychiatr. 2001;158 (11):1856–1863. doi: 10.1176/appi.ajp.158.11.1856. [DOI] [PubMed] [Google Scholar]
- Yonkers KA, Wisner KL, Stewart DE, Oberlander TF, Dell DL, Stotland N, Ramin S, Chaudron L, Lockwood CL. The management of depression during pregnancy: a report from the American Psychiatric Association and the American College of Obstetricians and Gynecologists. Gen Hosp Psychiatry. 2009;31 (5):401–413. doi: 10.1016/j.genhosppsych.2009.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zayas LH, Jankowski KAR, McKee MD. Prenatal and postpartum depression among low-income Dominican and Puerto Rican women. Hispanic J Behav Sci. 2003;25:370–385. [Google Scholar]