Abstract
Background
Treatment of displaced femoral neck fractures includes internal fixation and arthroplasty. However, whether arthroplasty or internal fixation is the primary treatment for displaced femoral neck fractures in elderly patients remains a subject for debate. The literature contains conflicting evidence regarding rates of mortality, revision surgery, major postoperative complications, and function in elderly patients with displaced femoral neck fractures treated either by internal fixation or arthroplasty (either hemiarthroplasty or THA).
Questions/purpose
We determined mortality, revision surgery rates, major surgical complications (which include infection, nonunion or early redisplacement, avascular necrosis, dislocation, loosening of the prosthesis, acetabular erosion, fracture below or around the implant, and other severe general complications such as deep vein thrombosis and pulmonary embolism), and function in patients treated with either internal fixation or arthroplasty for displaced femoral neck fractures in the elderly.
Methods
We searched PubMed, Embase, and the Cochrane Library for randomized controlled trials (RCTs) comparing internal fixation and arthroplasty. We identified 20 RCTs with 4508 patients meeting all the criteria for eligibility. We performed a meta-analysis of the major complications, reoperations, function, pain, and mortality.
Results
Compared with internal fixation, arthroplasty reduced the risk of the major complications (95% CI, 0.21–0.54 for 1 year; 95% CI, 0.16–0.31 for 5 years) and the incidence of reoperation 1 to 5 years after surgery (95% CI, 0.15–0.34 for 1 year; 95% CI, 0.08–0.24 for 5 years), and provided better pain relief (95% CI, 0.34–0.72). Function was superior (RR = 0.59; 95% CI, 0.44–0.79) for patients treated with arthroplasty than for patients treated by internal fixation. However, mortality 1 to 3 years after surgery was similar (95% CI, 0.96–1.23, p = 0.20 for 1 year; 95% CI, 0.91–1.17, p = 0.63 for 3 years).
Conclusions
Arthroplasty can reduce the risk of major complications and the incidence of reoperation compared with internal fixation, and provide better pain relief and function, but it does not reduce mortality.
Level of Evidence
Level II, prognostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Displaced femoral neck fractures are common in elderly patients [8]. With increases of the geriatric population and average life expectancy, the prevalence of these fractures is steadily increasing worldwide [4].
Operative alternatives for displaced femoral neck fractures differ throughout the world but primarily include arthroplasty and internal fixation. Several factors influence the choice of surgery for displaced femoral neck fractures in elderly patients. Although patients and surgeons need to consider these factors to determine the preferred management, whether arthroplasty or internal fixation is more appropriate for treatment of displaced femoral neck fractures in elderly patients is debatable [20]. A meta-analysis by Lu-Yao et al. [17] concluded that it appears to be a clear trend that arthroplasty — particularly bipolar and total — is associated with fewer secondary major operations than internal fixation. Their results showed an elevated rate of mortality after arthroplasty during the first few months after the fracture, but the mortality rates were similar between the internal fixation and arthroplasty groups afterward. They also suggested that an anterior operative approach for arthroplasty consistently was associated with a lower rate of mortality at 2 months than was a posterior approach. However, the meta-analysis is limited as it is based primarily on observational studies. Clinical studies comparing arthroplasty with internal fixation, including observational studies, RCTs, and systematic reviews, are limited by the lack of independent outcome assessments, variable outcome instruments, limited assessment of possible confounding variables, and possible bias associated with unmeasured or unknown confounders inherent in observational studies.
We therefore conducted a new meta-analysis of RCTs to evaluate mortality, revision surgery rates, major surgical complications, and function in patients treated with either internal fixation or arthroplasty for displaced femoral neck fractures.
Search Strategy and Criteria
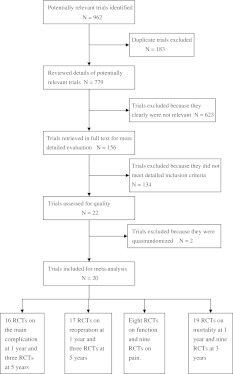
We conducted a literature search of PubMed (1966 to May 2010) and Embase (1974 to May 2010) using the following search strategies: “femoral neck fractures” AND “internal fixation” AND (“prosthetic replacement” OR “arthroplasty”). We used the following search strategies for the Cochrane Central Register of Controlled Trials (The Cochrane Library 2010): (“femoral neck fractures” AND “internal fixation” AND “prosthetic replacement”) OR (“femoral neck fractures” AND “internal fixation” AND “arthroplasty”). The initial searches yielded 962 articles (Fig. 1). We included only studies meeting the following criteria: (1) RCTs comparing internal fixation with arthroplasty, (2) patients 65 years or older with an acute displaced fracture of the femoral neck (Garden Stage III or IV fractures [36]), and (3) patients with normal mental state. No language restriction was applied. Quasirandomized trials were excluded. All studies included patients having surgery for the first time. Reference lists of eligible studies for potentially relevant reports were examined and references in the Cochrane Central Register of Controlled Trials were searched. Additional strategies to identify relevant studies were supplemented with manual searches of primary orthopaedics textbooks and bibliographies of published articles. We also searched conference papers and ongoing trials (for example, the UK National Research Register, Trials Central, Current Controlled Trials) for unpublished articles. Two authors (HW, DG) screened studies for inclusion and retrieved all potentially relevant studies. Two authors (ZH, MZ) independently extracted data for study population, intervention, prespecified outcomes, methodology, and quality from eligible trials. Disagreements were resolved by discussion. Of the 962 citations, 183 were duplicates and were excluded, leaving 779 potentially relevant studies (Fig. 1). Of these, we reviewed 156 retrieved articles for inclusion and data extraction.
Fig. 1.
The selection of RCTs comparing arthroplasty with internal fixation for displaced femoral neck fractures in elderly patients is shown.
We extracted information on mortality, revision surgery rates, major surgical complications, and function in patients after intervention. The definition of major surgical complications for internal fixation included deep infection, nonunion, early redisplacement, and avascular necrosis, whereas the major complications of arthroplasty included deep infection, dislocation, acetabular erosion, prosthesis loosening, and femoral shaft fracture adjacent to the prosthesis. The major complications also included severe general complications such as deep vein thrombosis and pulmonary embolism. The definition of reoperations excluded the removal of hardware after fracture healing and closed reduction of prosthesis dislocations. The assessment of function included the ability to walk, reduction of mobility because of hip problems, the need for walking aids, and scales assessing the function, such as the Harris hip score [32], Eq-5d [35], and Barthel index [18, 28]. We extracted the numbers of patients using similar walking aids postoperatively, numbers of patients maintaining their preoperative mobility, or similar scales (ie, Harris hip score, Eq-5d, and Barthel index) obtained postoperatively.
Two authors (HW, DG) independently extracted methodologic information for assessment of quality. We used the following four components [14]: method of randomization, concealment of allocation, number and reasons for patient losses to followup, and blinding. We did a sensitivity analysis for study quality by including only studies with clear methods of randomization and concealment of allocation (high-quality studies). Differences were reconciled by a third reviewer (MZ). We used GRADE [7] to assess the quality of the included studies.
Meta-analysis was performed using RevMan 5.0 software (Cochrane Information Management System; http://ims.cochrane.org/revman). We examined heterogeneity among studies with chi-square and I2 statistics to determine whether the results of various studies and the overall effect were consistent [10]. If the effect was deemed consistent, a fixed-effect model was used; if not, data were analyzed individually to determine the reasons and remove heterogeneity. If we found statistical but not clinical heterogeneity in the data, we used a random effects model. We compared the event rates using relative risks (RR) as summary statistics with corresponding 95% CIs. We used the Mantzel-Haenzel method to calculate the pooled odds ratio. The literature is subject to publication bias: many studies are unpublished because of negative or no statistically significant or no clinically important findings, thereby causing an erroneously high proportion of positive studies and studies with significant findings among published studies. We tested for such bias with funnel plots (standard error (SE) of the log RR). Finally, we performed a sensitivity analysis by excluding low-quality studies.
Nineteen studies with 4237 patients provided mortality rates 1 year after surgery. We found no significant heterogeneity (p = 0.20 > 0.05) among these 19 studies and therefore we used a fixed effects model. Seventeen studies with 3830 patients reported on reoperations 1 year after the index surgery. Because of significant heterogeneity among these 17 studies, we used a random effects model. Three studies reported information on reoperations 5 years after the index surgery. No significant heterogeneity was found so we used the fixed effects model. Sixteen studies including 3221 patients reported information regarding surgical complications occurring within 1 year after surgery. Significant heterogeneity also was observed in these 16 studies and we used the random effects model. Surgical complications 5 years after surgery were reported in only three studies for 789 patients. No significant heterogeneity was observed in these three studies; therefore, the fixed effects model was used. Eight studies with 1982 patients reported detailed data regarding hip function postoperatively. Postoperative hip pain was reported in nine studies with 2121 patients. These nine studies had significant heterogeneity; therefore, the random effects model was used.
A total of 20 trials comparing arthroplasty with internal fixation for displaced femoral neck fracture in the elderly met the eligibility criteria (Fig. 1); we did not find any unpublished trials or articles. All trials compared internal fixation with arthroplasty (Table 1), of which 11 compared internal fixation with hemiarthroplasty, four compared internal fixation with THA, and five compared internal fixation separately with hemiarthroplasty and THA. All included studies described appropriate patient followup. Postoperative followups ranged from 1 to 13 years.
Table 1.
Characteristics of the included studies
| Studies | Year | Followup (months) | Interventions | Number of patients | ||
|---|---|---|---|---|---|---|
| Arthroplasty | Internal fixation | Arthroplasty | Internal fixation | |||
| Davison et al. [5] | 2001 | 60 | Hemiarthroplasty | AMBI compression hip screw and two-hole plate | 187 | 93 |
| Frihagen et al. [6] | 2007 | 24 | Hemiarthroplasty | Two parallel cannulated screws | 110 | 112 |
| Johansson et al. [12] | 2000 | 24 | Total hip replacement | Two parallel Olmed screws | 50 | 50 |
| Jónsson et al. [13] | 1996 | 24 | Total hip replacement | Hansson hook pins | 23 | 24 |
| Bjorgul and Reikeras [3] | 2006 | 72 | Hemiarthroplasty | Olmed screws | 455 | 228 |
| Leonardsson et al. [16] | 2010 | 120 | Hemiarthroplasty, Total hip replacement | Hansson hook pins or Olmed screws | 192 | 217 |
| Heetveld et al. [9] | 2007 | 24 | Hemiarthroplasty | screws | 109 | 115 |
| Neander et al. [19] | 1997 | 18 | Total hip replacement | Two parallel Olmed screws | 43 | 57 |
| Parker et al. [21] | 2002 | 12 | Hemiarthroplasty | Three AO screws | 229 | 226 |
| Puolakka et al. [22] | 2001 | 24 | Hemiarthroplasty | Three Ullevaal screws | 15 | 16 |
| Ravikumar and Marsh [23] | 2000 | 156 | Hemiarthroplasty, Total hip replacement | Richards compression screw and plate | 180 | 91 |
| Rödén et al. [24] | 2003 | 60 | Hemiarthroplasty | Two von Bahr screws | 47 | 53 |
| Rogmark et al. [25] | 2002 | 24 | Hemiarthroplasty, Total hip replacement | Hansson hook pins or Olmed screws | 192 | 217 |
| Sikorski and Barrington [30] | 1981 | 12 | Hemiarthroplasty | Garden screws | 114 | 76 |
| Skinner et al. [31] | 1989 | 12 | Hemiarthroplasty, Total Hip Replacement | Sliding compression screws | 180 | 91 |
| Söreide et al. [33] | 1979 | 12 | Hemiarthroplasty | Von Bahr screws | 53 | 51 |
| Svenningsen et al. [34] | 1985 | 36 | Hemiarthroplasty | Compression screw versus McLaughlin nail plate | 59 | 110 |
| Keating et al. [15] | 2006 | 24 | Hemiarthroplasty, Total Hip Replacement | Cancellous screws or sliding hip screw | 180 | 118 |
| Tidermark et al. [37] | 2003 | 24 | Total Hip Replacement | Two cannulated screws | 49 | 53 |
| van Vugt et al. [38] | 1993 | 36 | Hemiarthroplasty | Dynamic hip screw | 22 | 21 |
Documentation of adequate concealment of randomized treatment allocation was reported in only a few studies (Table 2). According to the scale by Schulz et al. [27], only six of 20 trials reported a clearly adequate method of concealment, including two [5, 15] that used computer-generated random numbers and four [6, 12, 16, 25] that used sealed, numbered, opaque envelopes. Five trials [11, 13, 21, 22, 24, 37] reported use of a sealed envelope technique without indicating whether the envelopes were opaque or sequentially numbered, and eight [3, 9, 19, 23, 29, 33, 34, 38] stated only that subjects were randomly allocated or that the study was a randomized trial.
Table 2.
Quality of included studies
| Studies | Randomization | Allocation concealment | Assessor blinding | Loss of followup | Quality grade |
|---|---|---|---|---|---|
| Davison et al. [5] | RCT | Yes | Single blinding | 17.9%, untreated | B |
| Frihagen et al. [6] | RCT | Yes | Unknown | Unknown | B |
| Johansson et al. [12] | RCT | Yes | Unknown | 9%, untreated | B |
| Jónsson et al. [13] | RCT | Yes | Unknown | 4%, untreated | B |
| Bjorgul and Reikeras [3] | RCT | Yes | Unknown | 1%, untreated | B |
| Leonardsson et al. [16] | RCT | Yes | Unknown | 3.9% | B |
| Heetveld et al. [9] | Inadequate | Yes | Double blinding | Unknown | B |
| Neander et al. [19] | RCT | Yes | Unknown | No | B |
| Parker et al. [21] | RCT | Yes | Unknown | No | B |
| Puolakka et al. [22] | RCT | Yes | Unknown | 3% | B |
| Ravikumar and Marsh [23] | RCT | Yes | Unknown | Unknown | B |
| Rödén et al. [24] | RCT | Yes | Unknown | Unknown | B |
| Rogmark et al. [25] | RCT | Yes | Unknown | 10.2%, untreated | B |
| Sikorski and Barrington [30] | RCT | Yes | Unknown | Unknown | B |
| Skinner et al. [31] | Inadequate | Unknown | Unknown | Unknown | C |
| Söreide et al. [35] | Inadequate | Unknown | Unknown | Unknown | C |
| Svenningsen et al. [34] | Inadequate | Yes | Unknown | < 5% | C |
| Keating et al. [15] | RCT | Yes | Double blinding | < 5% | A |
| Tidermark et al. [37] | RCT | Yes | Double blinding | 7.2%, untreated | A |
| van Vugt et al. [38] | RCT | Yes | Unknown | < 5% | B |
Only one trial [30] used a card drawn from a box in the operating theatre. Four studies included information about blinding. Three trials [9, 15, 37] used double blinding and one [5] used single blinding.
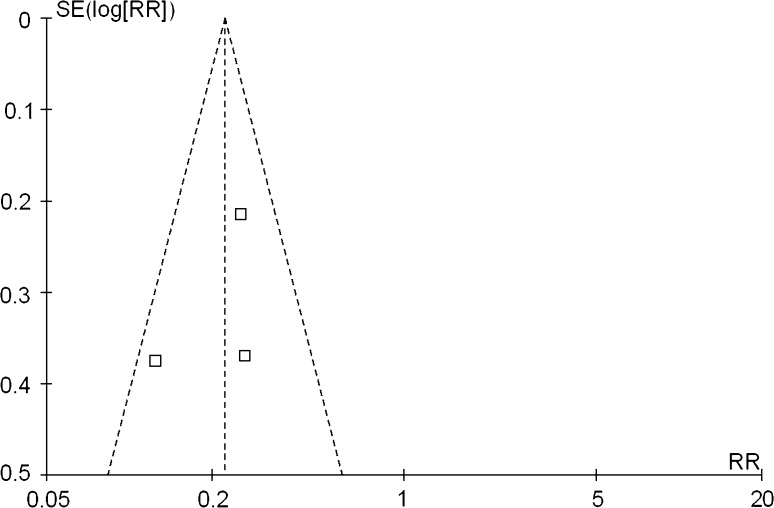
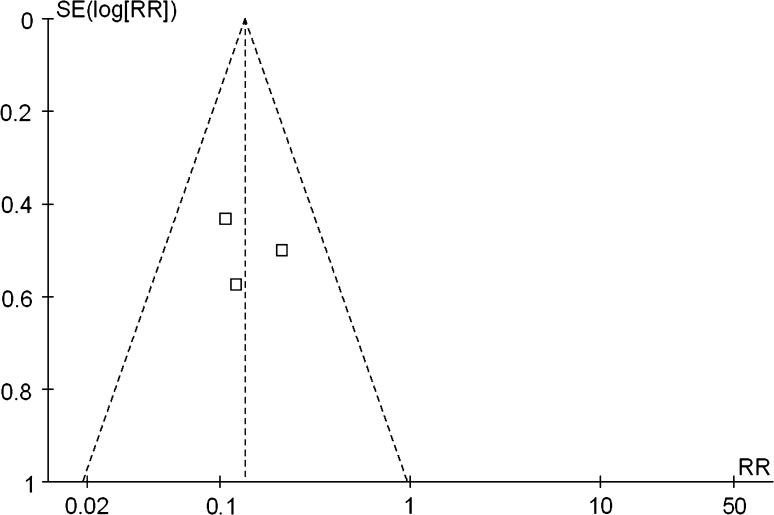
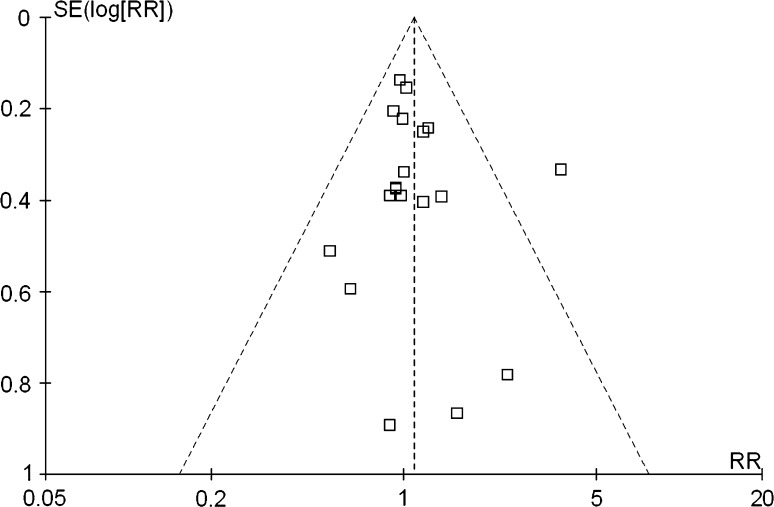
Three trials were judged to be of poor quality and were removed in the sensitivity analysis. We found no influence on the final result. Analysis of publication bias using funnel plots of major complications (Fig. 2), reoperations (Fig. 3), and mortality (Fig. 4) showed no evidence of asymmetry.
Fig. 2.
We used a funnel plot to analyze publication bias of three RCTs that included 789 patients. The major complication at 5 years postoperative showed no evidence of asymmetry, suggesting that there was no statistically significant publication bias.
Fig. 3.
This funnel plot of three RCTs with 655 patients for reoperation at 5 years postoperative shows no evidence of asymmetry suggesting there was no statistically significant publication bias.
Fig. 4.
This funnel plot shows publication bias of 19 RCTs including 4237 patients for mortality at 1 year postoperative. There is no evidence of asymmetry, suggesting there was no statistically significant publication bias in 19 RCTs for mortality at 1 year postoperative.
Results
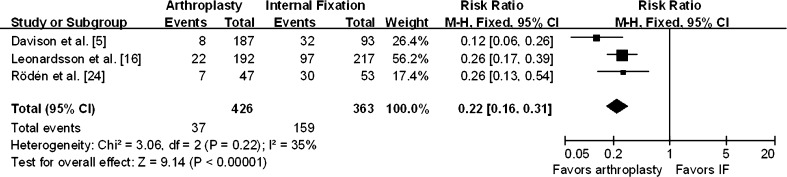
The pooled results showed a lower risk (RR = 0.33; 95% CI, 0.21–0.54) of major surgical complications at 1 year for arthroplasty compared with internal fixation (Fig. 5). There was also a lower risk (RR = 0.22; 95% CI, 0.16–0.31) of major surgical complications for arthroplasty at 5 years postoperatively (Fig. 6).
Fig. 5.
This forest plot shows pooling of RRs of the major complication at 1 year postoperative. It has 16 RCTs including 3221 patients. The 95% CI of the pooled RR is 0.21 to 0.54. This result showed a lower risk of major surgical complications at 1 year for arthroplasty compared with internal fixation. M-H = Mantzel-Haenzel method; df = degrees of freedom; IF = internal fixation.
Fig. 6.
The forest plot compares three RCTs including 789 patients for the major complication at 5 years postoperative. The 95% CI of the pooled RR is 0.16 to 0.31. It showed there was also a lower risk of major surgical complications for arthroplasty at 5 years postoperatively. M-H = Mantzel-Haenzel method; df = degrees of freedom; IF = internal fixation.
At 1 year there were fewer (RR = 0.22; 95% CI, 0.15–0.34) reoperations in patients treated by arthroplasty than by internal fixation (Fig. 7). There also were fewer (RR = 0.13; 95% CI, 0.08–0.24) reoperations in patients treated by arthroplasty at 5 years (Fig. 8). Taking the inverse RR, patients who underwent internal fixation were approximately four times more likely to need a second operation.
Fig. 7.
This forest plot shows pooling of RRs for reoperation at 1 year postoperative. Seventeen RCTs are included with 3830 patients. The 95% CI of the pooled RR is 0.15 to 0.34, suggesting there were fewer reoperations in patients treated by arthroplasty than by internal fixation. M-H = Mantzel-Haenzel method; df = degrees of freedom; IF = internal fixation.
Fig. 8.
This forest plot shows pooling of RRs for reoperation at 5 years postoperative. The three RCTs include 655 patients. The 95% CI of the pooled RR is 0.08 to 0.24 suggesting there also were fewer reoperations in patients treated by arthroplasty at 5 years. M-H = Mantzel-Haenzel method; df = degrees of freedom; IF = internal fixation.
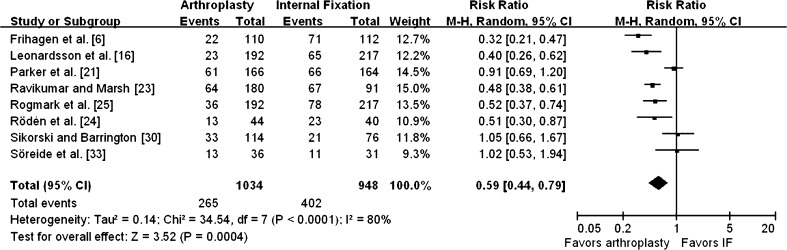
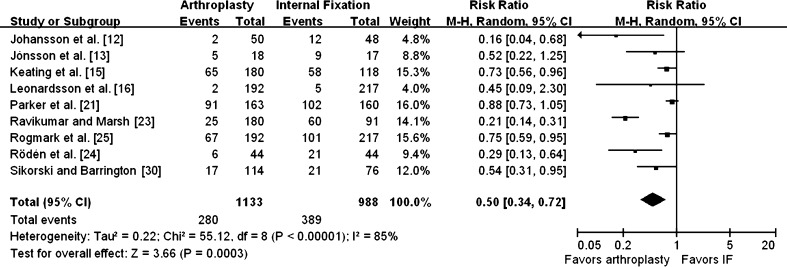
Function was superior (RR = 0.59; 95% CI, 0.44–0.79) in patients treated with arthroplasty than for patients treated by internal fixation (Fig. 9). Patients treated with arthroplasty reported less pain (RR = 0.50; 95% CI, 0.34–0.72) than patients treated with internal fixation (Fig. 10).
Fig. 9.
Eight RCTs including 1982 patients were compared for postoperative function. The 95% CI of the pooled RR is 0.44 to 0.79, suggesting function was better for patients treated with arthroplasty than for patients treated by internal fixation. M-H = Mantzel-Haenzel method; df = degrees of freedom; IF = internal fixation.
Fig. 10.
Nine RCTs including 2121 patients were compared for postoperative pain. The 95% CI of the pooled RR is 0.34 to 0.72 showing patients treated with arthroplasty reported less pain than patients treated with internal fixation. M-H = Mantzel-Haenzel method; df = degrees of freedom; IF = internal fixation.
Nineteen reports with 4237 patients provided mortality rates 1 year after surgery. These studies did not change the overall pooled effect of internal fixation compared with arthroplasty (RR = 1.09, 95% CI, 0.96–1.23; p = 0.20) (Fig. 11). Nine studies reported mortality at 3 years, but there still was no difference in mortality after internal fixation and arthroplasty (RR = 1.03; 95% CI, 0.91–1.17; p = 0.63) (Fig. 12).
Fig. 11.
Pooling of RRs for mortality at 1 year postoperative is shown in this forest plot. Nineteen RCTs including 4237 patients were compared. The 95% CI of the pooled RR is 0.96 to 1.23. The result showed these studies did not significantly change the overall pooled effect of internal fixation compared with arthroplasty. M-H = Mantzel-Haenzel method; df = degrees of freedom; IF = internal fixation.
Fig. 12.
This forest plot shows pooling of RRs for mortality at 5 years postoperative. Nine RCTs were included with 2170 patients. The 95% CI of the pooled RR is 0.91 to 1.17 suggesting there still was no difference in mortality after internal fixation and arthroplasty. M-H = Mantzel-Haenzel method; df = degrees of freedom; IF = internal fixation.
Discussion
Whether arthroplasty or internal fixation is the primary treatment for displaced femoral neck fractures in elderly patients remains a subject for debate [20]. We therefore conducted a meta-analysis of RCTs to evaluate mortality, revision surgery rates, major surgical complications, and function in patients treated with either internal fixation or arthroplasty for displaced femoral neck fractures in the elderly.
We encountered limitations in the literature, and our specific study is limited by specific aspects of our searches and inclusion and exclusion criteria. First, potential sources of bias in these trials included failure of most trials to report clearly adequate methods to conceal random allocation, postrandomization exclusion of study participants from analyses in several trials, lack of blinding to type of surgical treatment by outcomes assessors, and high loss to followup. Second, our review has insufficient power to clarify whether the possible early excess in mortality after arthroplasty relative to internal fixation is real or a statistical artifact. Third, although it was not the purpose of this review to evaluate economic outcomes, only two eligible trials [15, 21] reported any cost data, limiting the potential to compare cost outcomes for arthroplasty versus internal fixation in patients with displaced femoral neck fractures. Fourth, the type of arthroplasty (hemiarthroplasty versus total arthroplasty), approach (anterior, anterolateral, posterior), and method of fixation (open versus closed), fixation method (screws versus other), may have an impact on the final treatment effect. We did not assess the relative outcomes of internal fixation and arthroplasty in important subgroups for stratified analysis. Fifth, many of the studies are likely older and may not provide contemporary estimates of the four key parameters. Since few meta-analyses and RCTs have been reported in recent years we presumed more RCTs would be important for the meta-analysis and therefore included some older RCTs. Finally, we excluded mostly quasirandomized trials in this review, which are prone to bias. Two more recent meta-analyses [2, 26] comprising randomized and quasirandomized trials have reported similar findings for mortality, reoperations, major complications, and function.
Our meta-analysis suggests similar mortality for internal fixation and arthroplasty for treating displaced femoral neck fractures at 1 and 5 years after surgery. In their meta-analysis of nine studies comprising 1162 patients, Bhandari et al. [2] reported that an incremental trend in the RR of death occurs during the first 4 months after arthroplasty compared with the risk during the same period after internal fixation. Leonardsson et al. [16] reported higher mortality 4 months after arthroplasty than after internal fixation, but not during the long-term followup. Conversely, Hudson et al. [11] reported a higher mortality after internal fixation compared with hemiarthroplasty when adjusted for age, gender, and comorbidities.
We found the use of arthroplasty rather than internal fixation decreased the incidence of revision surgery. Because the followup period in most of the studies is 1 to 3 years, the overall reoperation rate is lower than that in clinical practice. We thought this may be particularly relevant for the long-term revision rate of arthroplasty, which has not been well documented. Ravikumar and Marsh [23] conducted the study with the longest followup of 13 years, reporting a reoperation rate of only 7% after arthroplasty. They found that arthroplasty reduces long-term risks, which is likely attributable to the higher mortality in patients 65 years or older with femoral neck fractures.
Our meta-analysis shows the RR for the major complications for arthroplasty versus those for internal fixation is 0.22 to 0.33, supporting primary arthroplasty. Arthroplasty, including hemiarthroplasty and THA, is a more complicated surgery, often requiring a longer operative time compared with internal fixation. Arthroplasty is associated with a greater risk of hip dislocation and wound infection. According to the best estimates from previous meta-analyses [2, 39], an average of 17 revision surgeries can be avoided for every 100 patients treated with arthroplasty instead of internal fixation, at the expense of one hip dislocation and four additional wound infections. Regarding what influences the rate of dislocation, Sierra et al. [29] reported the value of the anterior approach as capable of dramatically reducing the risk of dislocations in patients undergoing THA. They suggested that capsular repair is the most important predictive factor for reducing dislocation when using a posterior approach for THA in patients older than 80 years. Lu-Yao et al. [17] suggested that the short-term mortality rate is lower with an anterior approach, indicating a trend for lower dislocation rates with the anterior approach as well. Berry et al. [1] analyzed their institution’s large THA database and confirmed that the use of a 32-mm diameter femoral head is associated with a lower cumulative risk of dislocation compared with smaller diameter heads. Otherwise, complications of arthroplasty, such as acetabular erosion, often occur long after the operation, thereby influencing the result. However, Ravikumar and Marsh [23] reported that arthroplasty reduces the major complications compared with internal fixation.
The important final measure of pain has not been adequately reported or has not been mentioned in many studies. We found only nine studies with 2121 patients reported data for residual pain and eight studies with 1982 patients reported data for postoperative function. The pooled results of these data showed less pain and better function after arthroplasty compared with internal fixation. We suspect patients who had internal fixation are more likely to be receiving analgesics, less likely to be mobile on long-term followup, and have a higher likelihood of undergoing revision surgery. In contrast, cemented arthroplasty provides skeletal stability immediately, and allows patients to move more freely.
Our meta-analysis suggests, for a relatively healthy, independent, elderly patient with a displaced femoral neck fracture, primary arthroplasty is superior to internal fixation; it reduced the risk of major complications (95% CI, 0.21–0.54 for 1 year; 95% CI, 0.16–0.31 for 5 years) and the incidence of reoperation 1 to 5 years after surgery (95% CI, 0.15–0.34 for 1 year; 95% CI, 0.08–0.24 for 5 years), and provided better pain relief (95% CI, 0.34–0.72) and function (95% CI, 0.44–0.79). However, mortality 1 to 3 years after surgery was similar (95% CI, 0.96–1.23, p = 0.20 for 1 year; 95% CI, 0.91–1.17, p = 0.63 for 3 years). Our data suggest no difference has been established. Moreover, arthroplasty obviously is conducive to the quality of life of patients. Future RCTs and meta-analyses should focus on the types of arthroplasties, with RCTs using studies that have greater long-term followups.
Footnotes
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
References
- 1.Berry DJ, Knoch M, Schleck CD, Harmsen WS. Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am. 2005;87:2456–2463. doi: 10.2106/JBJS.D.02860. [DOI] [PubMed] [Google Scholar]
- 2.Bhandari M, Devereaux PJ, Swiontkowski MF, Tornetta P, 3rd, Obremskey W, Koval KJ, Nork S, Sprague S, Schemitsch EH, Guyatt GH. Internal fixation compared with arthroplasty for displaced fractures of the femoral neck: a meta-analysis. J Bone Joint Surg Am. 2003;85:1673–1681. doi: 10.2106/00004623-200309000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Bjorgul K, Reikeras O. Hemiarthroplasty in worst cases is better than internal fixation in best cases of displaced femoral neck fractures: a prospective study of 683 patients treated with hemiarthroplasty or internal fixation. Acta Orthop. 2006;77:368–374. doi: 10.1080/17453670610046271. [DOI] [PubMed] [Google Scholar]
- 4.Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:1761–1767. doi: 10.1016/S0140-6736(02)08657-9. [DOI] [PubMed] [Google Scholar]
- 5.Davison JN, Calder SJ, Anderson GH, Ward G, Jagger C, Harper WM, Gregg PJ. Treatment for displaced intracapsular fracture of the proximal femur: a prospective randomised trial in patients aged 65 to 79 years. J Bone Joint Surg Br. 2001;83:206–212. doi: 10.1302/0301-620X.83B2.11128. [DOI] [PubMed] [Google Scholar]
- 6.Frihagen F, Nordsletten L, Madsen JE. Hemiarthroplasty or internal fixation for intracapsular displaced femoral neck fractures: randomised controlled trial. BMJ. 2007;335:1251–1254. doi: 10.1136/bmj.39399.456551.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P. GRADE Working Group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hedlund R, Lindgren U, Ahlbom A. Age- and sex-specific incidence of femoral neck and trochanteric fractures: an analysis based on 20,538 fractures in Stockholm County, Sweden, 1972–1981. Clin Orthop Relat Res. 1987;222:132–139. [PubMed] [Google Scholar]
- 9.Heetveld MJ, Raaymakers EL, Luitse JS, Nijhof M, Gouma DJ. Femoral neck fractures: can physiologic status determine treatment choice? Clin Orthop Relat Res. 2007;461:203–212. doi: 10.1097/BLO.0b013e3180574aca. [DOI] [PubMed] [Google Scholar]
- 10.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hudson JI, Kenzora JE, Hebel JR, Gardner JF, Scherlis L, Epstein RS, Magaziner JS. Eight-year outcome associated with clinical options in the management of femoral neck fractures. Clin Orthop Relat Res. 1998;348:59–66. doi: 10.1097/00003086-199803000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Johansson T, Jacobsson SA, Ivarsson I, Knutsson A, Wahlström O. Internal fixation versus total hip arthroplasty in the treatment of displaced femoral neck fractures: a prospective randomized study of 100 hips. Acta Orthop Scand. 2000;71:597–602. doi: 10.1080/000164700317362235. [DOI] [PubMed] [Google Scholar]
- 13.Jónsson B, Sernbo I, Carlsson A, Fredin H, Johnell O. Social function after cervical hip fracture: a comparison of hook-pins and total hip replacement in 47 patients. Acta Orthop Scand. 1996;67:431–434. doi: 10.3109/17453679608996662. [DOI] [PubMed] [Google Scholar]
- 14.Jüni P, Altman DG, Egger M. Systematic reviews in health care: assessing the quality of controlled clinical trials. BMJ. 2001;323:42–46. doi: 10.1136/bmj.323.7303.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Keating JF, Grant A, Masson M, Scott NW, Forbes JF. Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty: treatment of displaced intracapsular hip fractures in healthy older people. J Bone Joint Surg Am. 2006;88:249–260. doi: 10.2106/JBJS.E.00215. [DOI] [PubMed] [Google Scholar]
- 16.Leonardsson O, Sernbo I, Carlsson A, Akesson K, Rogmark C. Long-term follow-up of replacement compared with internal fixation for displaced femoral neck fractures: results at ten years in a randomised study of 450 patients. J Bone Joint Surg Br. 2010;92:406–412. doi: 10.1302/0301-620X.92B3.23036. [DOI] [PubMed] [Google Scholar]
- 17.Lu-Yao GL, Keller RB, Littenberg B, Wennberg JE. Outcomes after displaced fractures of the femoral neck: a meta analysis of one hundred and six published reports. J Bone Joint Surg Am. 1994;76:15–25. doi: 10.2106/00004623-199401000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J. 1965;14:61–65. [PubMed] [Google Scholar]
- 19.Neander G, Adolphson P, Sivers K, Dahlborn M, Dalén N. Bone and muscle mass after femoral neck fracture: a controlled quantitative computed tomography study of osteosynthesis versus primary total hip arthroplasty. Arch Orthop Trauma Surg. 1997;116:470–474. doi: 10.1007/BF00387579. [DOI] [PubMed] [Google Scholar]
- 20.Parker M, Johansen A. Hip fracture. BMJ. 2006;333:27–30. doi: 10.1136/bmj.333.7557.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parker MJ, Khan RJ, Crawford J, Pryor GA. Hemiarthroplasty versus internal fixation for displaced intracapsular hip fractures in the elderly: a randomized trial of 455 patients. J Bone Joint Surg Br. 2002;84:1150–1155. doi: 10.1302/0301-620X.84B8.13522. [DOI] [PubMed] [Google Scholar]
- 22.Puolakka TJ, Laine HJ, Tarvainen T, Aho H. Thompson hemiarthroplasty is superior to Ullevaal screws in treating displaced femoral neck fractures in patient over 75 years: a prospective randomized study with two-year follow-up. Ann Chir Gynaecol. 2001;90:225–228. [PubMed] [Google Scholar]
- 23.Ravikumar KJ, Marsh G. Internal fixation versus hemiarthroplasty versus total hip arthroplasty for displaced subcapital fractures of femur: 13 year results of a prospective randomised study. Injury. 2000;31:793–797. doi: 10.1016/S0020-1383(00)00125-X. [DOI] [PubMed] [Google Scholar]
- 24.Rödén M, Schön M, Fredin H. Treatment of displaced femoral neck fractures: a randomized minimum 5-year follow-up study of screws and bipolar hemiprostheses in l00 patients. Acta Orthop Scand. 2003;74:42–44. doi: 10.1080/00016470310013635. [DOI] [PubMed] [Google Scholar]
- 25.Rogmark C, Carlsson A, Johnell O, Sernbo I. A prospective randomised trial of internal fixation versus arthroplasty for displaced fractures of the neck of the femur: functional outcome for 450 patients at two years. J Bone Joint Surg Br. 2002;84:183–188. doi: 10.1302/0301-620X.84B2.11923. [DOI] [PubMed] [Google Scholar]
- 26.Rogmark C, Johnell O. Primary arthroplasty is better than internal fixation of displaced femoral neck fractures: a meta-analysis of 14 randomized studies with 2,289 patients. Acta Orthop. 2006;77:359–367. doi: 10.1080/17453670610046262. [DOI] [PubMed] [Google Scholar]
- 27.Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias: dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. 1995;273:408–412. doi: 10.1001/jama.1995.03520290060030. [DOI] [PubMed] [Google Scholar]
- 28.Shepherd SM, Prescott RJ. Use of standardised assessment scales in elderly hip fracture patients. J R Coll Physicians Lond. 1996;30:335–343. [PMC free article] [PubMed] [Google Scholar]
- 29.Sierra RJ, Raposo JM, Trousdale RT, Cabanela ME. Dislocation of primary THA done through a posterolateral approach in the elderly. Clin Orthop Relat Res. 2005;441:262–267. doi: 10.1097/01.blo.0000194308.23105.f4. [DOI] [PubMed] [Google Scholar]
- 30.Sikorski JM, Barrington R. Internal fixation versus hemiarthroplasty for the displaced subcapital fracture of the femur: a prospective randomised study. J Bone Joint Surg Br. 1981;63:357–361. doi: 10.1302/0301-620X.63B3.7263746. [DOI] [PubMed] [Google Scholar]
- 31.Skinner P, Riley D, Ellery J, Beaumont A, Coumine R, Shafighian B. Displaced subcapital fractures of the femur: a prospective randomized comparison of internal fixation, hemiarthroplasty and total hip replacement. Injury. 1989;20:291–293. doi: 10.1016/0020-1383(89)90171-X. [DOI] [PubMed] [Google Scholar]
- 32.Söderman P, Malchau H. Is the Harris hip score system useful to study the outcome of total hip replacement? Clin Orthop Relat Res. 2001;384:189–197. doi: 10.1097/00003086-200103000-00022. [DOI] [PubMed] [Google Scholar]
- 33.Söreide O, Mölster A, Raugstad TS. Internal fixation versus primary prosthetic replacement in acute femoral neck fractures: a prospective, randomized clinical study. Br J Surg. 1979;66:56–60. doi: 10.1002/bjs.1800660118. [DOI] [PubMed] [Google Scholar]
- 34.Svenningsen S, Benum P, Nesse O, Furset OI. [Femoral neck fractures in the elderly: a comparison of 3 methods of treatment] [in Norwegian. Nord Med. 1985;100:256–259. [PubMed] [Google Scholar]
- 35.The EuroQol Group EuroQol: a new facility for the measurement of health-related quality of life. The EuroQol Group. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 36.Thomsen NO, Jensen CM, Skovgaard N, Pedersen MS, Pallesen P, Soe-Nielsen NH, Rosenklint A. Observer variation in the radiographic classification of fractures of the neck of the femur using Garden’s system. Int Orthop. 1996;20:326–329. doi: 10.1007/s002640050087. [DOI] [PubMed] [Google Scholar]
- 37.Tidermark J, Ponzer S, Svensson O, Söderqvist A, Törnkvist H. Internal fixation compared with total hip replacement for displaced femoral neck fractures in the elderly: a randomised, controlled trial. J Bone Joint Surg Br. 2003;85:380–388. doi: 10.1302/0301-620X.85B3.13609. [DOI] [PubMed] [Google Scholar]
- 38.Vugt AB, Oosterwijk WM, Goris RJ. Osteosynthesis versus endoprosthesis in the treatment of unstable intracapsular hip fractures in the elderly: a randomised clinical trial. Arch Orthop Trauma Surg. 1993;113:39–45. doi: 10.1007/BF00440593. [DOI] [PubMed] [Google Scholar]
- 39.Wang J, Jiang B, Marshall RJ, Zhang P. Arthroplasty or internal fixation for displaced femoral neck fractures: which is the optimal alternative for elderly patients? A meta-analysis. Int Orthop. 2009;33:1179–1187. doi: 10.1007/s00264-009-0763-8. [DOI] [PMC free article] [PubMed] [Google Scholar]