Abstract
Over the last 20 years, there has been extraordinary progress in brain imaging research and its application to the study of Alzheimer's disease (AD). Brain imaging researchers have contributed to the scientific understanding, early detection and tracking of AD. They have set the stage for imaging techniques to play growing roles in the clinical setting, the evaluation of disease-modifying treatments, and the identification of demonstrably effective prevention therapies. They have developed ground-breaking methods, including positron emission tomography (PET) ligands to measure fibrillar amyloid-β (Aβ) deposition, new magnetic resonance imaging (MRI) pulse sequences, and powerful image analysis techniques, to help in these endeavors. Additional work is needed to develop even more powerful imaging methods, to further clarify the relationship and time course of Aβ and other disease processes in the predisposition to AD, to establish the role of brain imaging methods in the clinical setting, and to provide the scientific means and regulatory approval pathway needed to evaluate the range of promising disease-modifying and prevention therapies as quickly as possible. Twenty years from now, AD may not yet be a distant memory, but the best is yet to come.
Keywords: Alzheimer's disease, dementia, mild cognitive impairment, MRI, PET, amyloid, diagnosis, prevention
Introduction
Alzheimer's disease (AD) is the most common cause of cognitive impairment in older people. When one considers the impact of AD on patients and families and the growing number of people living to older ages, there is a need to understand the progressive brain changes associated with the development of AD. There is also an urgent need to find treatments to slow down, stop, reduce the risk of, or completely prevent AD symptoms as soon as possible. Brain imaging techniques have had a profound impact on the scientific study of AD; they are expected to play growing roles in the clinical setting, and they are expected to play critical roles in the effort to find effective AD-modifying and prevention therapies.
In the last 20 years, there has been an explosion of interest in the development and use of brain imaging techniques for the scientific study, early detection, tracking, treatment and prevention of AD. This interest is reflected by the growing proportion of imaging researchers who attend and present their data at the major AD meetings, the development of imaging techniques to measure fibrillar amyloid-β deposition (a cardinal neuropathological feature of AD (Braak and Braak, 1991; Hardy and Selkoe, 2002)) in the living human brain (Klunk et al., 2004), the role that imaging studies have already played in the reconceptualization of AD (Sperling et al., 2011), the extraordinary opportunities researchers have to help in the scientific fight against this devastating disease, and the challenges the field continues to face along the way.
In this article, we review the best established brain imaging measurements for the detection and tracking of AD, and we note several other important imaging measurements, some of which have been less extensively applied or more recently developed. We then consider the how these imaging techniques have contributed to the scientific understanding of AD, their growing roles in the clinical setting, and their emerging roles in the evaluation of treatments to slow down the progression or prevent the onset of AD symptoms. Finally, we consider future research directions and offer a few recommendations. We are indebted to many investigators who have played pioneering roles in the development of brain imaging research, and we apologize in advance for our inability to cite all of the researchers and studies that have had a major impact on the field.
The Best Established Brain Imaging Measurements of AD
Researchers continue to develop a range of brain imaging measurements for the scientific study and clinical evaluation of AD. To date, the best established measurements for the detection and tracking of AD include structural magnetic resonance imaging (sMRI) measurements of regional and whole brain tissue shrinkage, fluorodeoxyglucose positron emission tomography (FDG PET) measurements of decline in the regional cerebral metabolic rate for glucose (CMRgl), and PET measurements of fibrillar amyloid-β (Aβ) burden. The information provided by these and other brain imaging measurements depends not only upon the imaging modality used, but the manner in which the data are acquired and analyzed.
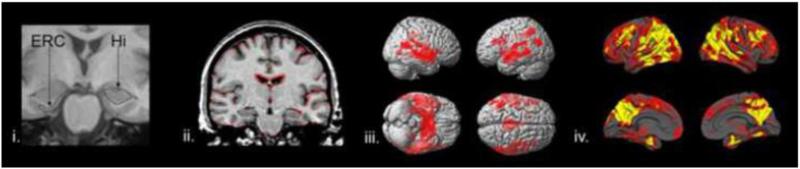
Structural MRI has been the most extensively used brain imaging method in the study of AD. Clinically affected patients have significantly reduced hippocampal and entorhinal cortex volumes, gray matter, and cortical thickness, increased ventricular and sulcal volumes, reduced gray matter or cortical thickness in other cerebral regions, like the precuneus and posterior cingulate, parietal, and temporal cortex, and accelerated rates of decline in these and whole brain measurements over time (Dickerson et al., 2009; Jack, Jr. et al., 2009; Jack, Jr. et al., 2010) (Figure 1). Reductions in hippocampal and entorhinal cortex size appear to correspond to early memory decline and anticipate progression to more severe clinical stages, including mild cognitive impairment (MCI) and Alzheimer's dementia (de Leon et al., 1989; Dickerson et al., 2001; Jack et al., 2004; Jack, Jr. et al., 2005; Kaye et al., 1997). In a few studies, volumetric reductions and accelerated rates of brain tissue loss have been found in cognitively normal people who are at higher genetic risk for AD or who show subsequent evidence of cognitive decline—evidence that may depend in part on the sensitivity of the image analysis technique used (Alexander et al., 2002b; Chen et al., 2007; den Heijer et al., 2002; Espeseth et al., 2008; Jak et al., 2007; Wishart et al., 2006). In the clinical setting, structural MRI is often recommended to help rule out potentially reversible brain abnormalities like tumors or subdural hematomas in patients with dementia and MCI, and it sometimes provides useful information about vascular pathology or the pattern of cortical atrophy. Researchers continue to clarify the extent to which it can be used alone or in combination with other measurements to predict subsequent cognitive decline in MCI patients, but it may not provide sufficient specificity to differentiate AD from other conditions(Knopman et al., 2001).
Figure 1.
Volumetric MRI in the the detection and tracking of AD, including (i) accelerated rates of atrophy in the hippocampus (Hi) and entorhinal cortex (ERC) regions-of-interest (Mike Weiner, with permission); (ii) accelerated rates of whole brain atrophy using sequential MRIs, as shown in red in a symptomatic AD patient (Nick Fox, with permission); (iii) regional gray matter loss, as shown in this statistical brain map comparing symptomatic AD patients and controls. Reprinted from (Baron et al., 2001), Copyright © 2001 with permission from Elsevier. All rights reserved; and (iv) regional thinning in cerebral cortex, as shown in this statistical brain map comparing symptomatic AD patients and controls. Reprinted with permission from (Du et al., 2007), Copyright © 2007 Oxford University Press. All rights reserved. This figure was reproduced with permission from (Reiman and Langbaum, 2009), Copyright © 2009 Oxford University Press. All rights reserved.
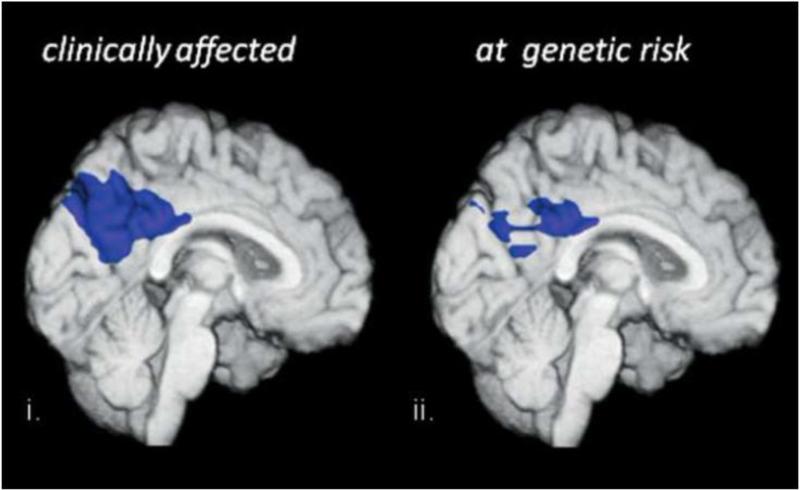
FDG PET is currently the best characterized functional brain imaging method in the study of AD. Studies consistently find reduced CMRgl in the precuneus, in posterior cingulate, parietal, and temporal cortex in clinically affected patients, and in frontal cortex and whole brain as the illness becomes more severe (Alexander et al., 2002a; Chen et al., 2010; Choo et al., 2007; Drzezga et al., 2005b; Foster et al., 1983; Herholz et al., 2002; Hoffman et al., 2000; Langbaum et al., 2009; Li et al., 2008; Minoshima et al., 1997; Mosconi et al., 2009; Reiman et al., 1996). In a smaller number of studies, CMRgl reductions have also been reported in hippocampal and entorhinal cortex regions-of-interest (De Santi et al., 2001; Mosconi et al., 2004b; Mosconi et al., 2005). CMRgl reductions are correlated with clinical severity (Bokde et al., 2005; Choo et al., 2007; Haxby et al., 1990; Landau et al., 2011; Langbaum et al., 2009), and predict subsequent clinical decline and/or the neuropathological diagnosis of AD (Alexander et al., 2002a; Herholz et al., 1999; Hoffman et al., 2000; Jagust et al., 1988; Silverman et al., 2001). Characteristic CMRgl reductions have been demonstrated in the asymptomatic stages of AD (e.g., in people with one or two copies of the apolipoprotein E (APOE) ε4 allele, the major AD susceptibility gene, in those at risk for autosomal dominant early-onset AD, and those with higher rates of subsequent cognitive decline) (Kennedy et al., 1995; Langbaum et al., 2010; Mosconi et al., 2006; Mosconi et al., 2008; Reiman et al., 1996; Reiman et al., 2001; Reiman et al., 2004; Reiman et al., 2005; Rimajova et al., 2008; Scholl et al., 2011; Small et al., 1995; Small et al., 2000; Villemagne et al., 2009) (Figure 2). In the clinical setting, FDG PET is sometimes used to help in the differential diagnosis between AD and frontotemporal lobar degeneration, and researchers continue to clarify the extent to which it can be used alone or in combination with other measurements to predict subsequent cognitive decline in MCI patients. FDG PET has the potential to help in the evaluation of AD-modifying treatments in the clinical and preclinical stages of AD, to further clarify the preclinical stages of AD and a person's risk for subsequent clinical decline, to help evaluate suggested AD risk factors, and to complement other imaging and fluid biomarker measurements in these endeavors, as noted further below (Reiman and Langbaum, 2009; Reiman et al., 2010; Reiman et al., 2011).
Figure 2.
FDG PET in people who are clinically affected by or at increased genetic risk of AD. Characteristic CMRgl reductions (compared to normal controls) are displayed on the medial surface of a brain MRI in clinically affected AD patients and in cognitively normal young adult with one copy of the APOE ε4 allele, the major AD susceptibility gene. Adapted with permission from (Reiman et al., 1996), Copyright © 1996 Massachusetts Medical Society, all rights reserved, and (Reiman et al., 2004), Copyright © 2004 National Academy of Sciences, USA. All rights reserved.
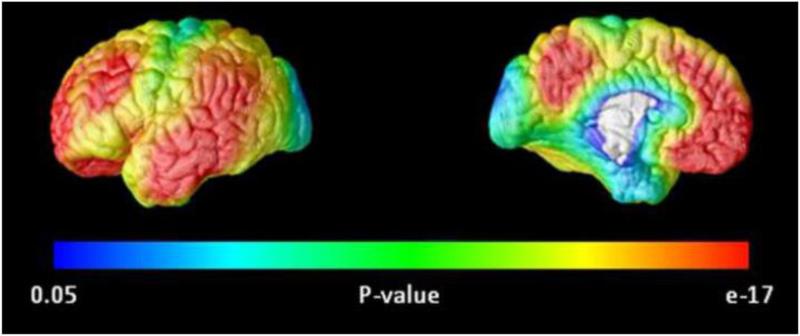
Fibrillar Aβ PET, introduced during the last decade, promises to have a profound impact on the scientific study of AD, the clinical evaluation of patients, and the evaluation of Aβ-modifying treatments. Several PET radioligands have now been shown to provide information about Aβ plaque deposition, a cardinal neuropathological feature of AD, in the living human brain. They include [11C]-labeled “Pittsburgh Compound B (PIB),”(Klunk et al., 2004; Mathis et al., 2002) which has had a major impact on the field and other investigational ligands, including several [F18] ligands that are being developed for the clinical setting due to their longer radioactive half-life and the ability to transport the tracer to different PET Centers from a regional radiopharmacy (Choi et al., 2009; Jureus et al., 2010; Nelissen et al., 2009; Rowe et al., 2008; Tolboom et al., 2009; Vandenberghe et al., 2010). Among other things, fibrillar Aβ PET studies have already confirmed the cortical distribution of fibrillar Aβ in clinically affected patients, with preferential deposition in precuneus, posterior cingulate, parietotemporal, and frontal regions and relative sparing in the hippocampus, and they have suggested that fibrillar Aβ levels are virtually saturated by the time patients have MCI (Doraiswamy et al., 2009; Forsberg et al., 2008; Grimmer et al., 2009; Jack, Jr. et al., 2008; Kemppainen et al., 2007; Klunk et al., 2004; Klunk et al., 2006; Morris et al., 2009; Resnick et al., 2010; Rowe et al., 2007; Rowe et al., 2010; Villemagne et al., 2011; Wolk et al., 2009) (Figure 3). They have suggested significant fibrillar Aβ deposition in about 30% of cognitively normal adults over the age of 70, perhaps 10-15 years before clinical onset, and that the magnitude and spatial extent of fibrillar Aβ is associated with older age and the genetic risk for late-onset AD (Aizenstein et al., 2008; Mintun et al., 2006; Morris et al., 2010; Pike et al., 2007; Reiman et al., 2009; Rowe et al., 2010; Small et al., 2009; Villemagne et al., 2011). They have also suggested a slightly different pattern, with preferential deposition in the striatum in at least some cognitively normal people at genetic risk for early-onset AD (Klunk et al., 2007; Scholl et al., 2011; Villemagne et al., 2009). Initial studies have suggested a close association between PET measurements of fibrillar Aβ at the end of life and subsequent neuropathological measurements of fibrillar Aβ (Clark et al., 2011; Ikonomovic et al., 2008; Sojkova et al., 2011), and the first of these ligands (florbetapir F18) is now being considered for regulatory agency approval to help exclude the diagnosis of AD in patients with dementia or MCI (Clark et al., 2011). Although the technique might increase confidence in the diagnosis of AD, it cannot rule out the possibility that the syndrome is related to mixed pathology. While this technique does not provide direct information about other Aβ species (e.g., soluble oligomers, postulated to have a more toxic effects on neurons), it will now be possible to determine the extent to which cognitively normal people with significant fibrillar Aβ alone or in combination with other measurements predicts subsequent clinical decline, evaluate investigational Aβ-clearing (e.g., immunization) therapies in clinically affected patients, and evaluate the ability of even more investigational Aβ-modifying treatments to slow down the accumulation of fibrillar Aβ in presymptomatic AD (i.e., prevention) trials (Bateman et al., 2011; Reiman and Langbaum, 2009; Reiman et al., 2010; Reiman et al., 2011). Along the way, it will help to provide a key test of the amyloid hypothesis of AD, which suggests that certain amyloid species play a critical and relatively early role in the predisposition to this disease (Hardy and Selkoe, 2002).
Figure 3.
Fibrillar amyloid imaging in the study of AD. Increases in Pittsburgh Compound-B PET measurements of fibrillar amyloid-β in symptomatic AD patients. Adapted with permission from (Reiman et al., 2009; Reiman et al., 2010), Copyright © 2009 National Academy of Sciences, USA. All rights reserved.
Other Brain Imaging Measurements
The number of different brain imaging techniques that have been applied to the study of AD is too large to review in a single article. Here we touch on some of the more or less widely used approaches and try to summarize the major findings and applications, fully aware of the incomplete nature of this review.
Functional MRI (fMRI) and Functional Connectivity MRI (fcMRI)
MRI techniques that take advantage of the blood oxygen level dependent (BOLD) signal have been applied to both patients with AD and those at risk. These studies include approaches that utilize cognitive tasks to assess brain activation, and experiments performed during resting states that assess functional connectivity. A primary finding that has emerged is the dysfunction of the default mode network (DMN, see below for more information) in AD (Greicius et al., 2004). This network dysfunction is seen in individuals with PET evidence of Aβ accumulation but no overt symptoms (Hedden et al., 2009) and also predicts decline in patients with MCI (Petrella et al., 2011). fMRI studies that use cognitive paradigms to assess brain activation frequently reveal increased activation in those at risk for dementia (Bookheimer et al., 2000; Quiroz et al., 2010), which appears to decline with disease progression (O'Brien et al., 2010). The reliability of repeated measurements in some studies has suggested the use in clinical trials, although the issues of standardization, compensatory changes, and the ability to distinguish between biological factors and task performance need to be further addressed. Studies of brain activation and the resting state have been informative in application to fundamental questions of disease pathogenesis that are discussed in greater detail below.
Diffusion tensor imaging (DTI)
DTI has been used to study both the integrity and connectivity of white matter in patients with dementia and those at risk. Reduction in white matter integrity, generally measured as decreases in anisotropy (due to reduction in the axonal restrictions on directional diffusion) is now a widely reported finding in patients with AD and preclinical syndromes. Both AD and MCI patients show decreased fractional anisotropy in a wide variety of brain regions including areas known to be affected by AD such as the hippocampus (Sexton et al.); many studies also note relationships between FA and dementia severity. Voxelwise approaches to the analysis of DTI data have also demonstrated regional similarities between patterns of loss of white matter integrity in AD and MCI patients(Medina et al., 2006). The measurement of diffusion changes in the hippocampus may also be predictive of conversion to dementia (Fellgiebel et al., 2006). Through the use of fiber-tracking, or tractography, specific neural tracts of interest such as the cingulate (Zhang et al., 2007) and uncinate fasciculi (Kiuchi et al., 2009) have been shown to be particularly susceptible to white matter changes. The specificity and clinical application of these techniques requires more study.
SPECT Perfusion
Single photon emission computed tomography (SPECT) is a technique that is quite similar to PET and its application to dementia using radiotracers that track cerebral perfusion has produced results that are largely similar to PET scanning of glucose metabolism in clinical diagnostic applications (Bonte et al., 1986; DeKosky et al., 1990; Holman et al., 1992; Miller et al., 1991). SPECT studies have been shown to predict decline in MCI (Johnson et al., 1998) and are related to autopsy findings (Bonte et al., 1997; Jagust et al., 2001). For many years the limited availability of PET resulted in substantial use of SPECT scanning, however the proliferation of PET scanners in conjunction with oncological applications in clinical settings has increased its availability and application to dementia care and research.
Magnetic Resonance Spectroscopy (MRS)
While MRS can acquire data from multiple different atomic nuclei, the largest application has been proton MRS to quantify metabolites such as choline, N-acetyl aspartate (NAA) and myo-inositol (mI) in the brain. These data are usually expressed as normalized values by relating the spectral peaks to those from Creatinine (Cr). Many studies of AD patients have revealed reductions in NAA/Cr that can be found early in the disease prior to frank loss of volume (Adalsteinsson et al., 2000; Schuff et al., 1997). These findings have been taken as evidence of neuronal loss based on the predominant localization of NAA in neurons. A number of studies have also reported increases in mI/Cr which has been interpreted as evidence of gliosis (Kantarci et al., 2004; Valenzuela and Sachdev, 2001).
Other Imaging Techniques
A host of other imaging techniques have proven useful for specific clinical applications or interesting from the perspective of probing the pathology of AD and other dementias. For instance, fluid attenuated inversion recovery (FLAIR) is an MRI pulse sequence that permits researchers to detect the cerebral white matter hyperintensities suggestive of vascular disease, which is commonly found in AD patients (Yoshita et al., 2006) and may contribute to their cognitive decline (Brickman et al., 2008), and which could be used to help characterize a potentially reversible adverse effect of Aβ-modifying immunotherapeutic and medication treatments, now called Amyloid Related Imaging Abnormalities (ARIA). Gradient-recalled echo (GRE) T2* MR images appear to be sensitive to hemosiderin deposits, and as such are capable of detecting microbleeds, which are highly prevalent in dementia samples (Goos et al., 2010) and are particularly related to cerebral amyloid angiopathy (Kimberly et al., 2009). Initial reports suggest that GRE and FLAIR imaging may not only be helpful, but required by regulatory agencies to monitor Aβ-modifying immunotherapeutic and medication treatments.
While PET studies of AD have been largely focused on the assessment of rCMRgl decline and fibrillar Aβ deposition, a wide range of other tracers has been utilized. Studies of inflammation using the tracer PK11195, a ligand that binds to the peripheral benzodiazepine receptor that is expressed on activated microglia, have shown conflicting results, with evidence of both increases (Cagnin et al., 2001; Edison et al., 2008; Okello et al., 2009a) and lack of change in AD and MCI (Wiley et al., 2009); other PET tracers for inflammation that are under development may ultimately yield less ambiguous results. PET tracers have also been applied to dementia to study a wide range of neurotransmitter systems particularly the cholinergic system (Kuhl et al., 1999; Nordberg et al., 1997); these and others are the subject of recent reviews (Kadir and Nordberg, 2010; Nagren et al., 2010; Nordberg et al., 2010; Pappata et al., 2008). In general, neurotransmitter and neuroreceptor studies reveal reductions in a host of different pre- and post-synaptic elements in AD that in some cases are related to symptoms or other disease features. Researchers have suggested the potential of a PET radioligand for the detection of both fibrillar Aβ and tau pathology (Shoghi-Jadid et al., 2002); more recently, other researchers have proposed a PET radioligand with high affinity and selectivity for tau pathology (Fodero-Tavoletti et al., 2009); and researchers continue to explore PET radioligands for the assessment of tau and oligomeric Aβ species.
A growing number of brain imaging methods are available for the study of AD (and, as with the better established methods, they generate images that could be analyzed in a variety of ways). In general, the approaches reviewed here have not received widespread use in the clinic because either the processes being measured have no direct clinical implications or, in some cases because the techniques themselves have not been adequately standardized. These methods can also be expensive and technically demanding. This situation could change if effective therapy becomes available and these measures are shown to affect subject selection or monitoring of treatment.
Contributions to the Early Detection and Tracking of AD
As previously noted, researchers have used brain imaging techniques to detect and track brain changes associated with AD (Jack, Jr. et al., 2009). Several of the reported brain changes are correlated with clinical severity, progressive, predictive of subsequent clinical decline, and predictive of the neuropathological diagnosis of AD. Several of these changes are observed years before the onset of symptoms in persons at increased genetic risk for AD (e.g., APOE ε4 carriers, early-onset AD-causing mutation carriers, and Down syndrome patients) and individuals who subsequently demonstrated accelerated cognitive decline or progression to the clinical stages of AD. Additional studies are needed to determine the extent to which these measurements, alone or in combination with other factors, predict subsequent rates of clinical decline.
Cross-sectional PET studies suggest the onset of significant fibrillar Aβ burden about 10-15 years before the clinical onset of AD—though longitudinal studies are needed to determine the extent to which Aβ burden predicts clinical decline over shorter and longer time frames— and that it may reach a virtual plateau by the time most patients have MCI. It has been suggested that fibrillar Aβ deposition is associated with non-progressive reductions in CSF Aβ42 levels and that it anticipates downstream brain imaging and CSF changes (Fagan et al., 2006), including progressive MRI measurements of brain shrinkage, progressive PET measurements or rCMRgl decline, non-progressive elevations in CSF total tau and phospho-tau levels and, eventually, cognitive decline (Jack, Jr. et al., 2010; Sperling et al., 2011). Imaging studies have raised the possibility of even earlier brain changes, preceding Aβ pathology, in the predisposition to AD (Buckner et al., 2005; Reiman et al., 2004; Shaw et al., 2007; Sheline et al., 2010; Vaishnavi et al., 2010; Vlassenko et al., 2010).
Contributions to the Scientific Understanding of AD
Brain imaging studies have produced insights that have had a profound effect on how we think about the disease. To some extent these findings have come from multimodality approaches that have merged studies of structure, function, and biochemistry, especially those conducted in individuals who have minimal or no symptoms. Here we note some of the key findings in this area.
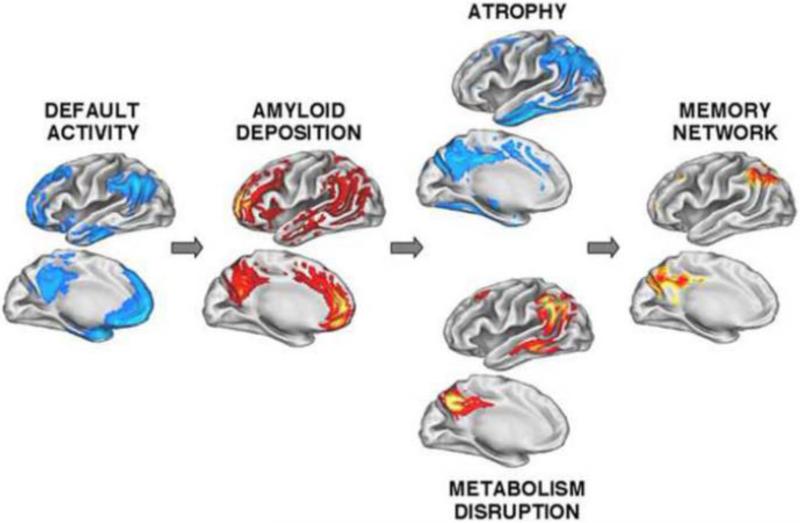
Brain Networks and the Deposition of Fibrillar Aβ
The observation that task induced brain activations are accompanied by clusters of regions that are consistently deactivated has lead to the notion that there is a resting state of the brain, commonly referred to as the default mode network (DMN) (Raichle et al., 2001). Subsequent work has shown that this network anatomically overlaps with both Aβ deposition and the pattern of MRI regional atrophy and PET-FDG hypometabolism (Buckner et al., 2005) (Figure 4). These nodes of the DMN parallel the location of many cortical hubs (Buckner et al., 2009), indicating that they serve as major foci of cortical connections and as key components of multiple networks. As noted, the DMN is disrupted in AD (Greicius et al., 2004) and in resting state connectivity studies in normal older people with asymptomatic fibrillar Aβ deposition (Hedden et al., 2009; Sheline et al., 2010); there is also some evidence that subcomponents of this network show increased connectivity that could represent shifting of the topography of the network perhaps as a compensatory process (Mormino et al., 2011). Failure to deactivate the same regions has been reported in aging and in early stage AD (Lustig et al., 2003), and most recently has been associated with fibrillar Aβ deposition in asymptomatic normal older people performing a memory encoding task (Sperling et al., 2009). The degeneration of this network in AD is paralleled by findings in other disorders in which patterns of neurodegeneration follow the patterns of neural connectivity in a number of different networks, suggesting that intrinsic functional and structural connectivity somehow mediates the regional progression of disorders as disparate as AD, frontotemporal lobar degeneration, and progressive supranuclear palsy (Seeley et al., 2009).
Figure 4.
Spatial relationships (and postulated causal connections) among the brain regions implicated in i and ii) the Default Mode Network and successful episodic memory retrieval in young adults, iii) the regions preferentially associated with fibrillar amyloid-β deposition, and iv and v) the regions preferentially associated with atrophy and CMRgl decline. Reprinted with permission from (Buckner et al., 2005), Copyright © 2005 Society for Neuroscience. All rights reserved.
The DMN is also interesting in another respect; it overlaps with both Aβ deposition and with brain regions that preferentially utilize aerobic glycolysis (Vaishnavi et al., 2010; Vlassenko et al., 2010). This aerobic glycolysis could reflect several different aspects of this brain network including the requirement for rapid production of ATP necessary for glutamate cycling (as aerobic glycolysis generates ATP more quickly than oxidative phosphorylation) or factors associated with neural plasticity including the role of glycolysis in fueling the receptor turnover at the post-synaptic density and activity in biosynthesis through the pentose-phosphate shunt. Why brain regions that preferentially utilize this form of energy metabolism should overlap with both cortical hubs and Aβ deposition is a subject requiring further investigation, but it suggests a relationship between neural metabolism and neuroplasticity and the etiopathogenesis of AD.
In addition to failure to adequately deactivate the DMN, a number of studies have pointed to increased brain activation as a feature of early and pre-symptomatic stages of AD (Bookheimer et al., 2000; Celone et al., 2006; Dickerson et al., 2004; Quiroz et al., 2010). These increases in “task positive” networks (as opposed to brain networks that deactivate during tasks such as the DMN) have been interpreted as attempts at compensation although this remains to be conclusively demonstrated. Alternative explanations include dedifferentiation of cortical function, and aberrant excitation, a finding that has also been seen in vivo in animal models of AD (Palop et al., 2007). In addition, it is possible that lifelong patterns of increased brain activity might themselves predispose to the deposition of β-amyloid(Jagust and Mormino, 2011).
Testing the Amyloid Hypothesis
The combined use of multiple imaging modalities has also resulted in new formulations of the sequence of pathological events in AD as proposed in a recent review (Jack, Jr. et al., 2010). By studying groups of individuals with a variety of imaging techniques at different stages of the disease, a picture of the progression of AD is emerging. For example, it has long been known that older individuals can show pronounced deposition of Aβ in the form of neuritic plaques without having evidence of cognitive impairment (Bennett et al., 2006; Tomlinson et al., 1968). PET amyloid imaging has confirmed the finding of substantial Aβ in normal older people, particularly as related to Apolipoprotein E genotype (Morris et al., 2010; Reiman et al., 2009), and it has permitted the simultaneous examination of cognition in great detail. While there remains some debate, most studies show that cognitive function is normal or only mildly affected in older individuals with brain Aβ who are classified as cognitively normal (Aizenstein et al., 2008; Rentz et al., 2010; Villemagne et al., 2011). While such data establish that very early brain abnormalities include Aβ deposits, they cannot definitely rule out the involvement of other pathological processes in the cascade of events leading to cognitive decline and dementia. Indeed, several other studies have noted that Aβ in normal people is accompanied by subtle evidence of brain atrophy that may be even more important than Aβ itself in leading to cognitive decline (Chetelat et al., 2010; Dickerson et al., 2009; Jack, Jr. et al., 2009; Mormino et al., 2009). These findings are echoed by some data from patients with dementia, in whom characteristics of Aβ deposition bear little relationship to clinical syndromes, while functional changes (both in glucose metabolism and brain activation) are more strongly associated with cognitive deficits (Nelissen et al., 2007; Rabinovici et al., 2008). Furthermore, progression from normal cognition through MCI and AD appears to be associated with very slow increases in Aβ accumulation but more rapid atrophy (Chetelat et al., 2010; Jack, Jr. et al., 2009; Villemagne et al., 2011). Accumulating evidence suggests that PET evidence of Aβ deposition is associated with longitudinal cognitive decline in normals (Resnick et al., 2010; Storandt et al., 2009) and conversion to dementia in those with MCI (Forsberg et al., 2008; Okello et al., 2009b; Wolk et al., 2009).
How can we reconcile seemingly contradictory findings wherein Aβ shows minimal relationships to cognitive symptoms but is associated with subsequent decline and dementia? The likely explanation is that there is a long preclinical period during with Aβ produces relatively few clinically observable findings, but is subtly altering both brain structure and function. We can begin to see evidence of Aβ, structural, and functional changes in normal aging. While Aβ appears to increase the probability of subsequent decline, it is not clear to what extent this decline is also predicted by the degree of structural and functional change. As dementia supervenes, structural and functional changes bear a stronger relationship to symptoms, suggesting that Aβ could serve as an initiating event after which “downstream” changes may become uncoupled from amyloid pathology. This has important implications for the early initiation of anti-amyloid therapy, and the potential importance of non-amyloid targets for individuals later in the disease course.
Still, other questions remain: For instance, why do researchers detect some of the earliest fibrillar Aβ deposition in frontal cortex in those at risk for AD (Mintun et al., 2006) (and in the striatum in some of the individuals at risk for autosomal dominant early-onset of AD (Klunk et al., 2007)), while they are unable to detect the declines in executive function (or the extrapyramidal symptoms) until later in the disease? That dissociation may give researchers clues about the differentially harmful or protective effects of Aβ species on neuronal function. Why have some researchers been able to show brain changes in young adults at genetic risk for AD before any evidence of fibrillar or solube Aβ accumulation (Reiman et al., 2004)? They information may give researchers information about the earliest synpaptic or peri-synaptic changes associated with the predisposition to AD, many decades before the progressive biological and cognitive changes observed in the later stages of the disease.? Will presymptomatic treatments shown to slow or even reverse the accumulation of fibrillar Aβ deposition also be associated with a clinical benefit? That might be the best test of the amyloid hypothesis yet—better than a test of the same treatment in clinically affected patients, when there is a concern that those treatments may be too late to exert their most profound benefit.
Relating brain function and structure to behavior
Numerous studies have helped to clarify how brain function and structure are related to behavior. PET studies have shown that the pattern and magnitude of glucose hypometabolism is related to pattern and magnitude of cognitive decline (Foster et al., 1983; Haxby et al., 1985; Landau et al., 2011). MRI studies have shown relationships between patterns of regional atrophy and the pattern of behavioral impairment (e.g., helping to define the relationship between regional atrophy and impaired language domains in patients with primary progressive aphasia (Rogalski et al., 2011). Effects of glucose metabolism and brain atrophy may be disarticulated through careful analysis of precise behavioral correlations. In one study, for example, posterior cingulate hypometabolism was related to deficits in memory retrieval, whereas hippocampal atrophy was related to deficits in both memory encoding and retrieval (Chetelat et al., 2003b).
Emerging Roles in the Clinical Setting
Guidelines for the use of imaging in the clinical evaluation of patients with dementia and pre-dementia syndromes such as MCI are actively being modified. Existing American Academy of Neurology practice parameters for the diagnosis of AD recommend CT or MR imaging only to rule out treatable structural pathology (Knopman et al., 2001) while MCI practice parameters do not address imaging at all (Petersen et al., 2001). These guidelines are 10 years old and outmoded not only because of the development of new imaging modalities, but also because the approach to AD has shifted from a diagnosis largely made by exclusion of other conditions to a diagnosis guided by specific historical, cognitive and, most recently, biomarker findings. This new approach has been reinforced by numerous studies in the clinical arena showing how PET imaging can contribute to the differentiation of AD and other conditions such as fronto-temporal Lobar degeneration (Foster et al., 2007) and how imaging findings may be related to pathology (Gosche et al., 2002).
It is in fact the availability of and increasing amounts of data concerning biomarkers in general that is shifting the thinking about diagnosis to include laboratory assessments that have value in supporting a diagnosis of AD. For instance the “Dubois criteria” propose the use of medial temporal atrophy, temporoparietal hypometabolism, and amyloid imaging (as well as CSF Aβ and tau measurements) as supportive features for a diagnosis of AD in the context of the core diagnostic feature of slowly progressive episodic memory loss (Dubois et al., 2007; Dubois et al., 2010). Notably, these criteria require neither pervasive cognitive loss nor functional impairment, thus including individuals in pre-dementia syndromes in the category of AD. While these criteria have not been widely applied, they have been influential in shifting the thinking about AD diagnosis to involve greater use of biomarkers. This approach has eventuated in a new series of diagnostic criteria developed by the National Institute on Aging and the Alzheimer's Association that cover AD, MCI, and even an asymptomatic, biomarker positive stage referred to as preclinical AD (Albert et al., 2011; McKhann et al., 2011; Sperling et al., 2011). Imaging figures prominently in all 3 diagnostic schemas, largely based upon the amyloid hypothesis and the conceptualization of the pathological sequence of events reviewed above. In these criteria, biomarkers are classified as indicative of Aβ deposition (CSF or PET) or neuronal injury (CSF tau, MRI atrophy, or PET hypometabolism). For both AD and MCI, the presence of both Aβ and neuronal injury confers the highest biomarker evidence of AD, presence of one an intermediate level, conflicting biomarker evidence is considered uninformative, and negative biomarker results lower the likelihood of AD. These criteria thus bring imaging clearly into the diagnostic assessment, largely in the role of supporting a diagnosis of AD. They also raise the possibility of determining which cognitively normal older adults and MCI patients have evidence of the AD pathophysiological process. Conversely, amyloid PET and MRI measurements provide a new opportunity to study the biological and cognitive changes associated with normal aging in the absence of measurable AD or cerebovascular pathology.
The future use of imaging in the clinical evaluation of dementia and MCI is likely related in part to the availability of effective medication treatments. At the present time there is evidence to suggest that amyloid PET imaging can predict decline in both MCI patients and normal older people. There is of course also evidence that FDG-PET and MRI are predictive of decline (Chetelat et al., 2003a; Jack et al., 1999). There are few studies that use multivariate approaches to predict decline in MCI patients but it is possible that markers of neural dysfunction such as FDG-PET and MR atrophy are better indicators of more progressed individuals and, as such, might be more effective than Aβ measures at predicting imminent decline (Chen et al., 2011; Landau et al., 2010). While studies that compare different imaging approaches in prediction will be important from a scientific perspective, the clinical significance of prediction may be more helpful when the information can be related to a clinically effective medication treatment. However, the likely infusion of amyloid PET into the clinical arena through the application of longer-lived F-18 labeled PET tracers (Clark et al., 2011; Rowe et al., 2008; Vandenberghe et al., 2010) could have a major impact on clinical care if effective therapies become available.
We wish to suggest two considerations, as a complement to the inevitable discussion of costs and benefits. First, public policy makers will need to factor in the non-medication treatment issues that have the greatest impact on the welfare of patients and families at this time. For instance, it is possible that amyloid PET findings could help mobilize physicians and families to address the range of distressing non-medication issues (e.g., decisions about driving and retirement, proactive financial, medicolegal, and resource planning) and reduce the family's sense of uncertainty about the underlying diagnosis. Second, a negative fibrillar Aβ PET scan (suggesting that the diagnosis of AD is unlikely) may be more informative than a positive PET scan (since one cannot exclude other contributors to AD, including some of the mixed pathology frequently seen at autopsy). Clinicians, payers and policy makers will have challenging questions to address, starting in the near future.
Emerging Roles in the Evaluation of AD-Modifying Treatments
There is great interest in the role that brain imaging techniques could play in the evaluation of investigational AD-modifying treatments, a major effort to develop the best imaging techniques for this purpose, and an increasing use of MRI, FDG PET and fibrillar amyloid PET in clinical trials. Among other things, imaging techniques have the potential to a) reduce the number of clinically affected AD patients and time needed to evaluate investigational AD-modifying treatments; b) select patients with dementia or MCI based on their estimated likelihood of clinical progression or response to certain treatments; c) differentiate patient subgroups in their response to treatment, helping to minimize attrition in drug development; d) help clarify a treatment's amyloid-modifying and other AD-modifying effects; e) monitor the safety of amyloid-modifying treatments (i.e., evidence of potentially reversible vasogenic edema and microinfarcts using GRE and FLAIR MRI pulse sequences); and f) as noted below, to help evaluate the range of promising presymptomatic AD treatments as quickly as possible (Reiman and Langbaum, 2009; Reiman et al., 2010; Reiman et al., 2011).
For instance, volumetric MRI and FDG PET measurements appear to be better than clinical measurements in their statistical power to track the progression of AD in probable AD and MCI patients and in their estimated statistical power to evaluate AD-modifying treatment effects when used as endpoints in clinical trials (Alexander et al., 2002a; Beckett et al., 2010; Chen et al., 2010; Chen et al., 2011; Fox et al., 2000). Brain imaging and other biomarker measurements have been suggested to help to distinguish those MCI patients most likely to show subsequent clinical progression over the next 12-18 months, providing an enrichment strategy by which to reduce sample size and treatment duration in MCI trials (Chételat et al., 2005a; Chételat et al., 2005b; Drzezga et al., 2005a; Jack, Jr. et al., 2005; Mosconi et al., 2004a). PET or CSF measurements of amyloid burden have been suggested to help distinguish which symptomatic patients have amyloid pathology (Clark et al., 2011), offering the change to identify those candidates who may be most likely to respond to an amyloid-modifying treatment. PET may be too late to assess the ability of an amyloid-modifying treatment to slow down the further fibrillar Aβ accumulation in symptomatic patients, by which time fibrillar Aβ deposition may have reached a plateau (Klunk et al., 2006), but it may be able to detect the extent to which certain (e.g., immunization) treatments actually reverse fibrillar Aβ pathology. Indeed, PiB PET was recently used in a clinical trial to demonstrate greater clearance of amyloid plaques in AD dementia patients treated with an Aβ immunotherapy than those treated with placebo (Rinne et al., 2010). Brain imaging and other biomarker measurements are critically needed to rapidly evaluate disease-modifying treatments in the earliest symptomatic and presymptomatic stages of AD, when investigational treatments may be most likely to exert their most profound effects.
Established in 2004, the United States-based AD Neuroimaging Initiative (ADNI) is primarily intended to help inform the design and performance of multi-center clinical trials of investigational AD-modifying treatments using brain imaging, other biomarker, and clinical measurements in probable AD, MCI and cognitively normal older adults (Mueller et al., 2005), and it has inspired similar initiatives in Europe, Australia, and Japan. It has developed and implemented protocols for the acquisition of MRI, FDG PET, and certain fibrillar Aβ PET measurements, real-time quality-assurance and quality-control procedures and centralized image processing procedures to optimize the quality and comparability of data acquired on different MRI and PET systems. It has demonstrated the feasibility of collecting CSF samples in a high proportion of study participants. It has provided a publicly available resource of data and biological samples for the research community, providing an opportunity to compare new data analysis techniques and biological fluid assays to other measurements in the detection and tracking of AD. Most importantly, it has provided a means to directly compare the different kinds of measurements and different image-analysis techniques in terms of their ability to track the progression of AD, estimate sample sizes needed to detect AD-modifying treatment effects, and the effects of different biomarker enrichment strategies on these estimates.
While brain imaging and other AD biomarker measurements offer great promise in the evaluation of AD-modifying treatments, several uncertainties remain when it comes to the information they will provide in clinical trials. There is a need to embed the most promising biomarkers in clinical trials, determine the extent to which AD-modifying treatments budge the biomarkers, clarify and address potentially confounding effects of the treatment on the biomarkers (e.g., a treatment's effects on brain volume or regional CMRgl unrelated to disease progression), and determine the extent to which the treatment's biomarker effects predict a clinical benefit. While brain imaging and other biomarkers can provide information that may help in the development of promising treatments, regulatory agencies are unlikely to provide an accelerated approval pathway for an AD-modifying treatment based solely on a biomarker (i.e., surrogate) endpoint until there is evidence from clinical trials themselves that a treatment's biomarker effects are reasonably likely to predict a clinical benefit (Reiman and Langbaum, 2009; Reiman et al., 2010; Reiman et al., 2011).
Emerging Roles in the Evaluation of Presymptomatic AD Treatments
When one considers the growing number of clinically affected AD patients, the healthy lifestyle interventions suggested but not proven to reduce the risk of AD symptoms (Haag et al., 2009; Lautenschlager et al., 2008; Peila et al., 2006; Scarmeas et al., 2009; Szekely et al., 2008; Wang et al., 2002; Willis et al., 2006; Zandi et al., 2004), and the possibility that investigational AD treatments may need to be started before the onset of symptoms to have their most profound benefit, there is a need to evaluate these range of “presymptomatic AD treatments” in the most rapid and rigorous way. It currently takes too many healthy volunteers and too many years to evaluate presymptomatic AD treatments in prevention trials using clinical endpoints. There is a growing interest in the role that brain imaging and other biomarker measurements could play in the rapid evaluation of promising presymptomatic AD treatments. Thus, researchers have provided brain imaging evidence of AD progression in cognitively normal late-middle-aged APOE ε4 carriers and the estimated sample sizes needed to evaluate promising presymptomatic AD treatments in two-year proof-of-concept prevention trials.
Meantime, several groups have proposed the evaluation of investigational Aβ-modifying treatments in prevention trials. For instance, researchers from the Alzheimer's Prevention Initiative have proposed a trial using brain imaging, CSF biomarker and cognitive endpoints in cognitively normal people who, based on their age and genetic background, are at the highest imminent risk of early- or late-onset AD symptoms and to provide the evidence needed to show that the treatment's biomarker effects are reasonably likely to predict a clinical benefit so that these biomarkers may receive regulatory agency qualification for use in AD prevention trials (Reiman et al., 2010; Reiman et al., 2011). It is also intended to provide a better test of the amyloid hypothesis than trials in symptomatic patients, when the treatment may be too little too late to have the most profound effect. Researchers from the Dominantly Inherited Alzheimer's Network (DIAN) have proposed proof-of-concept prevention in early-onset AD causing mutation carriers, and to use other biomarker data to help provide the pharmacodynamic data needed to inform these studies (Bateman et al., 2011). Researchers from the AD Cooperative Study have proposed a prevention trial in cognitively normal people with PET evidence of significant fibrillar Aβ burden. These and other trials are needed to not only provide information about the effects of promising presymptomatic treatments on measurements on AD pathophysiology, but to help find the best biomarkers for use in other prevention trials and to help qualify the most suitable biomarkers for use as reasonably likely surrogate endpoints in prevention trials. In this way, AD biomarkers, alone or in combination (e.g., PET fibrillar Aβ measurements along with volumetric MRI, FDG PET or other downstream measures of disease more closely related to clinical outcome), could provide both the scientific means and accelerated regulatory approval pathway to galvanize the evaluation of promising presymptomatic treatments.
Future Directions and a Few Recommendations
There has been has great progress in the scientific discovery of AD, the discovery of promising disease-modifying and presymptomatic treatments, and the development of brain imaging and biomarker techniques to help advance the scientific understanding, detection, tracking, treatment and prevention of AD. But more work remains to be done. A few recommendations:
Continue to develop the brain imaging measurements needed to assess relevant biological processes, including but not limited to brain imaging and fluid biomarker measurements to assess other, potentially more toxic (e.g., oligomeric) Aβ species and neurofibrillary pathology.
Continue to develop, test and compare new image analysis algorithms, including voxel-based algorithms that can capitalize on the wealth of data available in complementary data sets from the same person, and those that can summarize the pattern of measurements or time-dependent changes in a single measurement.
Further characterize the extent to which brain imaging measurements, alone but especially in combination, predict subsequent clinical decline. These imaging biomarkers must also be compared with inexpensive potentially cost-effective measures such as brief cognitive evaluations and fluid biomarkers.
Further characterize the relationship and time course of biomarker and cognitive changes associated with the preclinical and increasingly severe clinical stages of AD—include those changes that may precede the earliest evidence of Aβ accumulation.
Further development and leverage animal imaging resources in the scientific study of AD and the preclinical evaluation of promising AD-modifying treatments.
Work with researchers from other disciplines (e.g., genomics, proteomics, and the basic neurosciences) to leverage each others’ resources in a more effective way.
Embed the range of promising biomarker measurements (including volumetric MRI, FDG PET, fibrillar Aβ PET, CSF assays) and store the biological fluid samples in clinical trials of disease-modifying treatments and presymptomatic AD treatments, providing the evidence needed to inform the use of biomarkers in the evaluation of these treatments and to qualify the relevant biomarkers for use as endpoints in pivotal trials.
Develop, test, and apply PET tracers that can better characterize other neuropathological features of AD, such as those for the assessment of tau pathology (Fodero-Tavoletti et al., 2009), neuroinflammation, and other potentially neurotoxic (e.g., oligomeric) Aβ species.
Provide the federal funding and financial incentives needed to evaluate the range of promising presymptomatic treatments in prevention trials. It is time to advance AD prevention research, and imaging techniques are needed to help evaluate the range of promising treatments in the most rapid and rigorous way.
There is no guarantee that any of the treatments now in clinical and preclinical development will work. But the brain imaging research community is well positioned to help evaluate these treatments, extend them to the presymptomatic stages of AD when they might have their most profound effect, and improve the clinical management of AD as better treatments become available. A sense of urgency among all of the stakeholders is needed to address the problem of AD as quickly as possible.
Acknowledgements
The authors received relevant support from National Institute on Aging grants R01 AG031581, R01 AG034570, P30 AG19610, U01 AG024904 and RC AG036535. They thank Dr. Jessica Langbaum for her assistance in the editing of this article.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- Adalsteinsson E, Sullivan EV, Kleinhans N, Spielman DM, Pfefferbaum A. Longitudinal decline of the neuronal marker N-acetyl aspartate in Alzheimer's disease. Lancet. 2000;355:1696–1697. doi: 10.1016/s0140-6736(00)02246-7. [DOI] [PubMed] [Google Scholar]
- Aizenstein HJ, Nebes RD, Saxton JA, Price JC, Mathis CA, Tsopelas ND, Ziolko SK, James JA, Snitz BE, Houck PR, Bi W, Cohen AD, Lopresti BJ, DeKosky ST, Halligan EM, Klunk WE. Frequent Amyloid Deposition Without Significant Cognitive Impairment Among the Elderly. Archives of Neurology. 2008;65:1509–1517. doi: 10.1001/archneur.65.11.1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, Gamst A, Holtzman DM, Jagust WJ, Petersen RC, Snyder PJ, Phelps CH. The diagnosis of mild cognitive impairment due to Alzheimer‚Ã,,Ã's Disease: Recommendations from the National Institute on Aging and Alzheimer‚Ã,,Ã's Association Workgroup. Alzheimer's & Dementia. 2011 doi: 10.1016/j.jalz.2011.03.008. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander GE, Chen K, Pietrini P, Rapoport SI, Reiman EM. Longitudinal PET evaluation of cerebral metabolic decline in dementia: A potential outcome measure in Alzheimer's disease treatment studies. Am.J.Psychiatry. 2002a;159:738–745. doi: 10.1176/appi.ajp.159.5.738. [DOI] [PubMed] [Google Scholar]
- Alexander GE, Chen K, Reiman EM, Caselli RJ, Lewis D, Bandy D, Prouty A. Longitudinal declines of gray matter in cognitively normal apolopoprotein E ε4 homozygotes and heterozygotes evaluated by voxel-based MRI morphometry. Neurobiol.Aging. 2002b:s363. [Google Scholar]
- Baron JC, Chetelat G, Desgranges B, Perchey G, Landeau B, de, l.S. V, Eustache F. In vivo mapping of gray matter loss with voxel-based morphometry in mild Alzheimer's disease. Neuroimage. 2001;14:298–309. doi: 10.1006/nimg.2001.0848. [DOI] [PubMed] [Google Scholar]
- Bateman RJ, Aisen PS, De Strooper B, Fox NC, Lemere CA, Ringman JM, Salloway S, Sperling RA, Windisch M, Xiong C. Autosomal-dominant Alzheimer's disease: a review and proposal for the prevention of Alzheimer's disease. Alzheimers Res.Ther. 2011;2:35. doi: 10.1186/alzrt59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckett LA, Harvey DJ, Gamst A, Donohue M, Kornak J, Zhang H, Kuo JH. The Alzheimer's Disease Neuroimaging Initiative: Annual change in biomarkers and clinical outcomes. Alzheimers.Dement. 2010;6:257–264. doi: 10.1016/j.jalz.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett DA, Schneider JA, Arvanitakis Z, Kelly JF, Aggarwal NT, Shah RC, Wilson RS. Neuropathology of older persons without cognitive impairment from two community-based studies. Neurology. 2006;66:1837–1844. doi: 10.1212/01.wnl.0000219668.47116.e6. [DOI] [PubMed] [Google Scholar]
- Bokde AL, Teipel SJ, Drzezga A, Thissen J, Bartenstein P, Dong W, Leinsinger G, Born C, Schwaiger M, Moeller HJ, Hampel H. Association between cognitive performance and cortical glucose metabolism in patients with mild Alzheimer's disease. Dement.Geriatr.Cogn Disord. 2005;20:352–357. doi: 10.1159/000088558. [DOI] [PubMed] [Google Scholar]
- Bonte FJ, Ross ED, Chehabi HH, Devous MD. SPECT study of regional cerebral blood flow in Alzheimer disease. J Comput Assist Tomogr. 1986;10:579–583. doi: 10.1097/00004728-198607000-00005. [DOI] [PubMed] [Google Scholar]
- Bonte FJ, Weiner MF, Bigio EH, White CL. Brian blood flow in the dementias: SPECT with histopathologic correlation in 54 patients. Radiology. 1997;202:793–797. doi: 10.1148/radiology.202.3.9051035. [DOI] [PubMed] [Google Scholar]
- Bookheimer SY, Strojwas MH, Cohen MS, Saunders AM, Pericak-Vance MA, Mazziotta JC, Small GW. Patterns of brain activation in people at risk for Alzheimer's disease. N Engl J Med. 2000;343:450–456. doi: 10.1056/NEJM200008173430701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braak H, Braak E. Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol.(Berl) 1991;82:239–259. doi: 10.1007/BF00308809. [DOI] [PubMed] [Google Scholar]
- Brickman AM, Honig LS, Scarmeas N, Tatarina O, Sanders L, Albert MS, Brandt J, Blacker D, Stern Y. Measuring Cerebral Atrophy and White Matter Hyperintensity Burden to Predict the Rate of Cognitive Decline in Alzheimer Disease. Archives of Neurology. 2008;65:1202–1208. doi: 10.1001/archneur.65.9.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner RL, Sepulcre J, Talukdar T, Krienen FM, Liu H, Hedden T, Andrews-Hanna JR, Sperling RA, Johnson KA. Cortical hubs revealed by intrinsic functional connectivity: mapping, assessment of stability, and relation to Alzheimer's disease. J Neurosci. 2009;29:1860–1873. doi: 10.1523/JNEUROSCI.5062-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner RL, Snyder AZ, Shannon BJ, LaRossa G, Sachs R, Fotenos AF, Sheline YI, Klunk WE, Mathis CA, Morris JC, Mintun MA. Molecular, structural, and functional characterization of Alzheimer's disease: evidence for a relationship between default activity, amyloid, and memory. J.Neurosci. 2005;25:7709–7717. doi: 10.1523/JNEUROSCI.2177-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cagnin A, Brooks DJ, Kennedy AM, Gunn RN, Myers R, Turkheimer FE, Jones T, Banati RB. In-vivo measurement of activated microglia in dementia. Lancet. 2001;358:461–467. doi: 10.1016/S0140-6736(01)05625-2. [DOI] [PubMed] [Google Scholar]
- Celone KA, Calhoun VD, Dickerson BC, Atri A, Chua EF, Miller SL, DePeau K, Rentz DM, Selkoe DJ, Blacker D, Albert MS, Sperling RA. Alterations in memory networks in mild cognitive impairment and Alzheimer's disease: an independent component analysis. J Neurosci. 2006;26:10222–10231. doi: 10.1523/JNEUROSCI.2250-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen K, Ayutyanont N, Langbaum JBS, Fleisher AS, Reschke C, Lee W, Liu X, Bandy D, Alexander GE, Thompson PM, Shaw L, Trojanowki JQ, Jack CR, Jr., Landau SM, Foster NL, Harvey DJ, Weiner MW, Koeppe RA, Jagust WJ, Reiman EM, Alzheimer's Disease Neuroimaging Initiative Characterizing Alzheimer's disease using a hypometabolic convergence index. Neuroimage. 2011;56:52–60. doi: 10.1016/j.neuroimage.2011.01.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen K, Langbaum JBS, Fleisher AS, Ayutyanont N, Reschke C, Lee W, Liu X, Bandy D, Alexander GE, Thompson PM, Foster NL, Harvey DJ, de Leon MJ, Koeppe RA, Jagust WJ, Weiner MW, Reiman EM, the Alzheimer's Disease Neuroimaging Initiative Twelve-month metabolic declines in probable Alzheimer's disease and amnestic mild cognitive impairment assessed using an empirically pre-defined statistical region-of-interest: Findings from the Alzheimer's Disease Neuroimaging Initiative. Neuroimage. 2010;51:654–664. doi: 10.1016/j.neuroimage.2010.02.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen K, Reiman EM, Alexander GE, Caselli RJ, Gerkin R, Bandy D, Domb A, Osborne D, Fox N, Crum WR, Saunders AM, Hardy J. Correlations between apolipoprotein E ε4 gene dose and whole brain atrophy rates. Am.J Psychiatry. 2007;164:916–921. doi: 10.1176/ajp.2007.164.6.916. [DOI] [PubMed] [Google Scholar]
- Chetelat G, Desgranges B, De La Sayette V, Viader F, Eustache F, Baron JC. Mild cognitive impairment: Can FDG-PET predict who is to rapidly convert to Alzheimer's disease? Neurology. 2003a;60:1374–1377. doi: 10.1212/01.wnl.0000055847.17752.e6. [DOI] [PubMed] [Google Scholar]
- Chetelat G, Desgranges B, de, l.S. V, Viader F, Berkouk K, Landeau B, Lalevee C, Le DF, Dupuy B, Hannequin D, Baron JC, Eustache F. Dissociating atrophy and hypometabolism impact on episodic memory in mild cognitive impairment. Brain. 2003b;126:1955–1967. doi: 10.1093/brain/awg196. [DOI] [PubMed] [Google Scholar]
- Chételat G, Eustache F, Viader F, de la Sayette V, Pélerin A, Mézenge F, Hannequin D, Dupuy B, Baron JC, Desgranges B. FDG-PET measurement is more accurate than neuropsychological assessments to predict global cognitive deterioration in patients with mild cognitive impairment. Neurocase. 2005a;11:14–25. doi: 10.1080/13554790490896938. [DOI] [PubMed] [Google Scholar]
- Chételat G, Landeau B, Eustache F, Mézenge F, Viader F, de, l.S. V, Desgranges B, Baron JC. Using voxel-based morphometry to map the structural changes associated with rapid conversion in MCI: a longitudinal MRI study. Neuroimage. 2005b;27:934–946. doi: 10.1016/j.neuroimage.2005.05.015. [DOI] [PubMed] [Google Scholar]
- Chetelat G, Villemagne VL, Bourgeat P, Pike KE, Jones G, Ames D, Ellis KA, Szoeke C, Martins RN, O'Keefe GJ, Salvado O, Masters CL, Rowe CC. Relationship between atrophy and beta-amyloid deposition in Alzheimer disease. Ann Neurol. 2010;67:317–324. doi: 10.1002/ana.21955. [DOI] [PubMed] [Google Scholar]
- Choi SR, Golding G, Zhuang Z, Zhang W, Lim N, Hefti F, Benedum TE, Kilbourn MR, Skovronsky D, Kung HF. Preclinical properties of 18F-AV-45: a PET agent for Abeta plaques in the brain. J Nucl.Med. 2009;50:1887–1894. doi: 10.2967/jnumed.109.065284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choo IH, Lee DY, Youn JC, Jhoo JH, Kim KW, Lee DS, Lee JS, Woo JI. Topographic patterns of brain functional impairment progression according to clinical severity staging in 116 Alzheimer disease patients: FDG-PET study. Alzheimer Dis.Assoc.Disord. 2007;21:77–84. doi: 10.1097/WAD.0b013e3180687418. [DOI] [PubMed] [Google Scholar]
- Clark CM, Schneider JA, Bedell BJ, Beach TG, Bilker WB, Mintun MA, Pontecorvo MJ, Hefti F, Carpenter AP, Flitter ML, Krautkramer MJ, Kung HF, Coleman RE, Doraiswamy PM, Fleisher AS, Sabbagh MN, Sadowsky CH, Reiman PE, Zehntner SP, Skovronsky DM. Use of florbetapir-PET for imaging beta-amyloid pathology. JAMA. 2011;305:275–283. doi: 10.1001/jama.2010.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Leon MJ, George AE, Stylopoulos LA, Smith G, Miller DC. Early marker for Alzheimer's disease: the atrophic hippocampus. Lancet. 1989;2:672–673. doi: 10.1016/s0140-6736(89)90911-2. [DOI] [PubMed] [Google Scholar]
- De Santi S, de Leon MJ, Rusinek H, Convit A, Tarshish CY, Roche A, Tsui WH, Kandil E, Boppana M, Daisley K, Wang GJ, Schlyer D, Fowler J. Hippocampal formation glucose metabolism and volume losses in MCI and AD. Neurobiol.Aging. 2001;22:529–539. doi: 10.1016/s0197-4580(01)00230-5. [DOI] [PubMed] [Google Scholar]
- DeKosky ST, Shih WJ, Schmitt FA, Coupal J, Kirkpatrick C. Assessing utility of single photon emission computed tomography (SPECT) scan in Alzheimer disease: correlation with cognitive severity. Alzheimer disease and Assoc Disorders. 1990;4:14–23. doi: 10.1097/00002093-199040100-00002. [DOI] [PubMed] [Google Scholar]
- den Heijer T, Oudkerk M, Launer LJ, Van Duijn CM, Hofman A, Breteler MM. Hippocampal, amygdalar, and global brain atrophy in different apolipoprotein E genotypes. Neurology. 2002;59:746–748. doi: 10.1212/wnl.59.5.746. [DOI] [PubMed] [Google Scholar]
- Dickerson BC, Bakkour A, Salat DH, Feczko E, Pacheco J, Greve DN, Grodstein F, Wright CI, Blacker D, Rosas HD, Sperling RA, Atri A, Growdon JH, Hyman BT, Morris JC, Fischl B, Buckner RL. The cortical signature of Alzheimer's disease: regionally specific cortical thinning relates to symptom severity in very mild to mild AD dementia and is detectable in asymptomatic amyloid-positive individuals. Cereb Cortex. 2009;19:497–510. doi: 10.1093/cercor/bhn113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson BC, Goncharova I, Sullivan MP, Forchetti C, Wilson RS, Bennett DA, Beckett LA, Toledo-Morrell L. MRI-derived entorhinal and hippocampal atrophy in incipient and very mild Alzheimer's disease. Neurobiol.Aging. 2001;22:747–754. doi: 10.1016/s0197-4580(01)00271-8. [DOI] [PubMed] [Google Scholar]
- Dickerson BC, Salat DH, Bates JF, Atiya M, Killiany RJ, Greve DN, Dale AM, Stern CE, Blacker D, Albert MS, Sperling RA. Medial temporal lobe function and structure in mild cognitive impairment. Ann Neurol. 2004;56:27–35. doi: 10.1002/ana.20163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doraiswamy PM, Farmer M, Holub R, Johnson K, Reiman EM, Sadowsky C, Safirstein B, Spicer K, Carpenter A, Clark CM, Joshi A, Veeraraj C, Pontecorvo MJ, Skovronsky D. Relationship between regional amyloid levels and cognitive performance in healthy controls, MCI subjects, and patients with AD: Phase II results from a florpiramine F18 PET imaging study. Alzheimer's and Dementia. 2009;5:P77. [Google Scholar]
- Drzezga A, Grimmer T, Riemenschneider M, Lautenschlager N, Siebner H, Alexopoulus P, Minoshima S, Schwaiger M, Kurz A. Prediction of individual clinical outcome in MCI by means of genetic assessment and (18)F-FDG PET. J.Nucl.Med. 2005a;46:1625–1632. [PubMed] [Google Scholar]
- Drzezga A, Riemenschneider M, Strassner B, Grimmer T, Peller M, Knoll A, Wagenpfeil S, Minoshima S, Schwaiger M, Kurz A. Cerebral glucose metabolism in patients with AD and different APOE genotypes. Neurology. 2005b;64:102–107. doi: 10.1212/01.WNL.0000148478.39691.D3. [DOI] [PubMed] [Google Scholar]
- Du AT, Schuff N, Kramer JH, Rosen HJ, Gorno-Tempini ML, Rankin K, Miller BL, Weiner MW. Different regional patterns of cortical thinning in Alzheimer's disease and frontotemporal dementia. Brain. 2007;130:1159–1166. doi: 10.1093/brain/awm016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubois B, Feldman HH, Jacova C, Cummings JL, DeKosky ST, Barberger-Gateau P, Delacourte A, Frisoni G, Fox NC, Galasko D, Gauthier S, Hampel H, Jicha GA, Meguro K, O'Brien J, Pasquier F, Robert P, Rossor M, Salloway S, Sarazin M, de Souza LC, Stern Y, Visser PJ, Scheltens P. Revising the definition of Alzheimer's disease: a new lexicon. Lancet Neurol. 2010;9:1118–1127. doi: 10.1016/S1474-4422(10)70223-4. [DOI] [PubMed] [Google Scholar]
- Dubois B, Feldman HH, Jacova C, DeKosky ST, Barberger-Gateau P, Cummings J, Delacourte A, Galasko D, Gauthier S, Jicha G, Meguro K, O'Brien J, Pasquier F, Robert P, Rossor M, Salloway S, Stern Y, Visser PJ, Scheltens P. Research criteria for the diagnosis of Alzheimer's disease: revising the NINCDS-ADRDA criteria. Lancet Neurol. 2007;6:734–746. doi: 10.1016/S1474-4422(07)70178-3. [DOI] [PubMed] [Google Scholar]
- Edison P, Archer HA, Gerhard A, Hinz R, Pavese N, Turkheimer FE, Hammers A, Tai YF, Fox N, Kennedy A, Rossor M, Brooks DJ. Microglia, amyloid, and cognition in Alzheimer's disease: An [11C](R)PK11195-PET and [11C]PIB-PET study. Neurobiol Dis. 2008;32:412–419. doi: 10.1016/j.nbd.2008.08.001. [DOI] [PubMed] [Google Scholar]
- Espeseth T, Westlye LT, Fjell AM, Walhovd KB, Rootwelt H, Reinvang I. Accelerated age-related cortical thinning in healthy carriers of apolipoprotein E epsilon 4. Neurobiol.Aging. 2008;29:329–340. doi: 10.1016/j.neurobiolaging.2006.10.030. [DOI] [PubMed] [Google Scholar]
- Fagan AM, Mintun MA, Mach RH, Lee SY, Dence CS, Shah AR, LaRossa GN, Spinner ML, Klunk WE, Mathis CA, DeKosky ST, Morris JC, Holtzman DM. Inverse relation between in vivo amyloid imaging load and cerebrospinal fluid Aβ42 in humans. Annals of Neurology. 2006;59:512–519. doi: 10.1002/ana.20730. [DOI] [PubMed] [Google Scholar]
- Fellgiebel A, Dellani PR, Greverus D, Scheurich A, Stoeter P, Muller MJ. Predicting conversion to dementia in mild cognitive impairment by volumetric and diffusivity measurements of the hippocampus. Psychiatry Res. 2006;146:283–287. doi: 10.1016/j.pscychresns.2006.01.006. [DOI] [PubMed] [Google Scholar]
- Fodero-Tavoletti MT, Rowe CC, McLean CA, Leone L, Li QX, Masters CL, Cappai R, Villemagne VL. Characterization of PiB Binding to White Matter in Alzheimer Disease and Other Dementias. The Journal of Nuclear Medicine. 2009;50:198–204. doi: 10.2967/jnumed.108.057984. [DOI] [PubMed] [Google Scholar]
- Forsberg A, Engler H, Almkvist O, Blomquist G, Hagman G, Wall A, Ringheim A, Långstrom B, Nordberg A. PET imaging of amyloid deposition in patients with mild cognitive impairment. Neurobiology of aging. 2008;29:1456–1465. doi: 10.1016/j.neurobiolaging.2007.03.029. [DOI] [PubMed] [Google Scholar]
- Foster NL, Chase TN, Fedio P, Patronas NJ, Brooks RA, Di Chiro G. Alzheimer's disease: focal cortical changes shown by positron emission tomography. Neurology. 1983;33:961–965. doi: 10.1212/wnl.33.8.961. [DOI] [PubMed] [Google Scholar]
- Foster NL, Heidebrink JL, Clark CM, Jagust WJ, Arnold SE, Barbas NR, DeCarli CS, Turner RS, Koeppe RA, Higdon R, Minoshima S. FDG-PET improves accuracy in distinguishing frontotemporal dementia and Alzheimer's disease. Brain. 2007;130:2616–2635. doi: 10.1093/brain/awm177. [DOI] [PubMed] [Google Scholar]
- Fox NC, Cousens S, Scahill R, Harvey RJ, Rossor MN. Using serial registered brain magnetic resonance imaging to measure disease progression in Alzheimer disease: power calculations and estimates of sample size to detect treatment effects. Arch.Neurol. 2000;57:339–344. doi: 10.1001/archneur.57.3.339. [DOI] [PubMed] [Google Scholar]
- Goos JD, Henneman WJ, Sluimer JD, Vrenken H, Sluimer IC, Barkhof F, Blankenstein MA, Scheltens PH, van der Flier WM. Incidence of cerebral microbleeds: a longitudinal study in a memory clinic population. Neurology. 2010;74:1954–1960. doi: 10.1212/WNL.0b013e3181e396ea. [DOI] [PubMed] [Google Scholar]
- Gosche KM, Mortimer JA, Smith CD, Markesbery WR, Snowdon DA. Hippocampal volume as an index of Alzheimer neuropathology: findings from the Nun Study. Neurology. 2002;58:1476–1482. doi: 10.1212/wnl.58.10.1476. [DOI] [PubMed] [Google Scholar]
- Greicius MD, Srivastava G, Reiss AL, Menon V. Default-mode network activity distinguishes Alzheimer's disease from healthy aging: evidence from functional MRI. Proc Natl Acad Sci U S A. 2004;101:4637–4642. doi: 10.1073/pnas.0308627101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimmer T, Henriksen G, Wester H, Förstl H, Klunk WE, Mathis CA, Kurz A, Drzezga A. Clinical severity of Alzheimer's disease is associated with PIB uptake in PET. Neurobiology of aging. 2009;30:1902–1909. doi: 10.1016/j.neurobiolaging.2008.01.016. [DOI] [PubMed] [Google Scholar]
- Haag MDM, Hofman A, Koudstaal PJ, Stricker BHC, Breteler MMB. Statins are associated with a reduced risk of Alzheimer disease regardless of lipophilicity. The Rotterdam Study. Journal of Neurology, Neurosurgery, and Psychiatry. 2009;80:13–17. doi: 10.1136/jnnp.2008.150433. [DOI] [PubMed] [Google Scholar]
- Hardy J, Selkoe DJ. The amyloid hypothesis of Alzheimer's disease: progress and problems on the road to therapeutics. Science. 2002;297:353–356. doi: 10.1126/science.1072994. [DOI] [PubMed] [Google Scholar]
- Haxby JV, Duara R, Grady CL, Cutler NR, Rapoport SI. Relations between neuropsychological and cerebral metabolic asymmetries in early Alzheimer's disease. J Cereb Blood Flow Metab. 1985;5:193–200. doi: 10.1038/jcbfm.1985.25. [DOI] [PubMed] [Google Scholar]
- Haxby JV, Grady CL, Koss E, Horwitz B, Heston L, Schapiro M, Friedland RP, Rapoport SI. Longitudinal study of cerebral metabolic asymmetries and associated neuropsychological patterns in early dementia of the Alzheimer type. Arch.Neurol. 1990;47:753–760. doi: 10.1001/archneur.1990.00530070043010. [DOI] [PubMed] [Google Scholar]
- Hedden T, Van Dijk KR, Becker JA, Mehta A, Sperling RA, Johnson KA, Buckner RL. Disruption of functional connectivity in clinically normal older adults harboring amyloid burden. J Neurosci. 2009;29:12686–12694. doi: 10.1523/JNEUROSCI.3189-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herholz K, Nordberg A, Salmon E, Perani D, Kessler J, Mielke R, Halber M, Jelic V, Almkvist O, Collette F, Alberoni M, Kennedy A, Hasselbalch S, Fazio F, Heiss WD. Impairment of neocortical metabolism predicts progression in Alzheimer's disease. Dement.Geriatr.Cogn Disord. 1999;10:494–504. doi: 10.1159/000017196. [DOI] [PubMed] [Google Scholar]
- Herholz K, Salmon E, Perani D, Baron JC, Holthoff V, Frolich L, Schonknecht P, Ito K, Mielke R, Kalbe E, Zundorf G, Delbeuck X, Pelati O, Anchisi D, Fazio F, Kerrouche N, Desgranges B, Eustache F, Beuthien-Baumann B, Menzel C, Schroder J, Kato T, Arahata Y, Henze M, Heiss WD. Discrimination between Alzheimer dementia and controls by automated analysis of multicenter FDG PET. Neuroimage. 2002;17:302–316. doi: 10.1006/nimg.2002.1208. [DOI] [PubMed] [Google Scholar]
- Hoffman JM, Welsh-Bohmer KA, Hanson M, Crain B, Hulette C, Earl N, Coleman RE. FDG PET imaging in patients with pathologically verified dementia. J.Nucl.Med. 2000;41:1920–1928. [PubMed] [Google Scholar]
- Holman BL, Johnson KA, Gerada B, Carvalho PA, Satlin A. The scintigraphic appearance of Alzheimer's disease: a prospective study using technetium-99m-HMPAO SPECT. J Nucl Med. 1992;33:181–185. [PubMed] [Google Scholar]
- Ikonomovic MD, Klunk WE, Abrahamson EE, Mathis CA, Price JC, Tsopelas ND, Lopresti BJ, Ziolko S, Bi W, Paljug WR, Debnath ML, Hope CE, Isanski BA, Hamilton RL, DeKosky ST. Post-mortem correlates of in vivo PiB-PET amyloid imaging in a typical case of Alzheimer's disease. Brain. 2008;131:1630–1645. doi: 10.1093/brain/awn016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jack CR, Jr., Knopman DS, Jagust WJ, Shaw LM, Aisen PS, Weiner MW, Petersen RC, Trojanowski JQ. Hypothetical model of dynamic biomarkers of the Alzheimer's pathological cascade. Lancet Neurol. 2010;9:119–128. doi: 10.1016/S1474-4422(09)70299-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jack CR, Jr., Lowe VJ, Senjem ML, Weigand SD, Kemp BJ, Shiung MM, Knopman DS, Boeve BF, Klunk WE, Mathis CA, Petersen RC. 11C PiB and structural MRI provide complementary information in imaging of Alzheimer's disease and amnestic mild cognitive impairment. Brain. 2008;131:665–680. doi: 10.1093/brain/awm336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jack CR, Jr., Lowe VJ, Weigand SD, Wiste HJ, Senjem ML, Knopman DS, Shiung MM, Gunter JL, Boeve BF, Kemp BJ, Weiner M, Petersen RC, the Alzheimer's Disease Neuroimaging Initiative Serial PIB and MRI in normal, mild cognitive impairment and Alzheimer's disease: implications for sequence of pathological events in Alzheimer's disease. Brain. 2009;132:1355–1365. doi: 10.1093/brain/awp062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jack CR, Petersen RC, Xu YC, O'Brien PC, Smith GE, Ivnik RJ, Boeve BF, Waring SC, Tangalos E. Prediction of AD with MRI-based hippocampal volume in mild cognitive impairment. Neurology. 1999;52:1397–1403. doi: 10.1212/wnl.52.7.1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jack CR, Shiung MM, Gunter JL, O'Brien PC, Weigand SD, Knopman DS, Boeve BF, Ivnik RJ, Smith GE, Cha RH, Tangalos EG, Petersen RC. Comparison of different MRI brain atrophy rate measures with clinical disease progression in AD. Neurology. 2004;62:591–600. doi: 10.1212/01.wnl.0000110315.26026.ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jack CR, Jr., Shiung MM, Weigand SD, O'Brien PC, Gunter JL, Boeve BF, Knopman DS, Smith GE, Ivnik RJ, Tangalos EG, Petersen RC. Brain atrophy rates predict subsequent clinical conversion in normal elderly and amnestic MCI. Neurology. 2005;65:1227–1231. doi: 10.1212/01.wnl.0000180958.22678.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagust W, Thisted R, Devous MD, Sr., Van Heertum R, Mayberg H, Jobst K, Smith AD, Borys N. SPECT perfusion imaging in the diagnosis of Alzheimer's disease: a clinical-pathologic study. Neurology. 2001;56:950–956. doi: 10.1212/wnl.56.7.950. [DOI] [PubMed] [Google Scholar]
- Jagust WJ, Friedland RP, Budinger TF, Koss E, Ober B. Longitudinal studies of regional cerebral metabolism in Alzheimer's disease. Neurology. 1988;38:909–912. doi: 10.1212/wnl.38.6.909. [DOI] [PubMed] [Google Scholar]
- Jagust WJ, Mormino EC. Lifespan brain activity, beta-amyloid, and Alzheimer's disease. Trends Cogn Sci. 2011;15:520–526. doi: 10.1016/j.tics.2011.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jak AJ, Houston WS, Nagel BJ, Corey-Bloom J, Bondi MW. Differential cross-sectional and longitudinal impact of APOE genotype on hippocampal volumes in nondemented older adults. Dement.Geriatr Cogn Disord. 2007;23:382–389. doi: 10.1159/000101340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson KA, Jones K, Holman BL, Becker JA, Spiers PA, Satlin A, Albert MS. Preclinical prediction of Alzheimer's disease using SPECT. Neurology. 1998;50:1563–1571. doi: 10.1212/wnl.50.6.1563. [DOI] [PubMed] [Google Scholar]
- Jureus A, Swahn BM, Sandell J, Jeppsson F, Johnson AE, Johnstrom P, Neelissen JA, Sunnemark D, Farde L, Svensson SP. Characterization of AZD4694, a novel fluorinated Abeta plaque neuroimaging PET radioligand. J.Neurochem. 2010;114:784–794. doi: 10.1111/j.1471-4159.2010.06812.x. [DOI] [PubMed] [Google Scholar]
- Kadir A, Nordberg A. Target-specific PET probes for neurodegenerative disorders related to dementia. J Nucl Med. 2010;51:1418–1430. doi: 10.2967/jnumed.110.077164. [DOI] [PubMed] [Google Scholar]
- Kantarci K, Petersen RC, Boeve BF, Knopman DS, Tang-Wai DF, O'Brien PC, Weigand SD, Edland SD, Smith GE, Ivnik RJ, Ferman TJ, Tangalos EG, Jack CR., Jr. 1H MR spectroscopy in common dementias. Neurology. 2004;63:1393–1398. doi: 10.1212/01.wnl.0000141849.21256.ac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaye JA, Swihart T, Howieson D, Dame A, Moore MM, Karnos T, Camicioli R, Ball M, Oken B, Sexton G. Volume loss of the hippocampus and temporal lobe in healthy elderly persons destined to develop dementia. Neurology. 1997;48:1297–1304. doi: 10.1212/wnl.48.5.1297. [DOI] [PubMed] [Google Scholar]
- Kemppainen NM, Aalto S, Wilson IA, Nagren K, Helin S, Bruck A, Oikonen V, Kailajarvi M, Scheinin M, Viitanen M, Parkkola R, Rinne JO. PET amyloid ligand [11C]PIB uptake is increased in mild cognitive impairment. Neurology. 2007;68:1603–1606. doi: 10.1212/01.wnl.0000260969.94695.56. [DOI] [PubMed] [Google Scholar]
- Kennedy AM, Frackowiak RS, Newman SK, Bloomfield PM, Seaward J, Roques P, Lewington G, Cunningham VJ, Rossor MN. Deficits in cerebral glucose metabolism demonstrated by positron emission tomography in individuals at risk of familial Alzheimer's disease. Neurosci.Lett. 1995;186:17–20. doi: 10.1016/0304-3940(95)11270-7. [DOI] [PubMed] [Google Scholar]
- Kimberly WT, Gilson A, Rost NS, Rosand J, Viswanathan A, Smith EE, Greenberg SM. Silent ischemic infarcts are associated with hemorrhage burden in cerebral amyloid angiopathy. Neurology. 2009;72:1230–1235. doi: 10.1212/01.wnl.0000345666.83318.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiuchi K, Morikawa M, Taoka T, Nagashima T, Yamauchi T, Makinodan M, Norimoto K, Hashimoto K, Kosaka J, Inoue Y, Inoue M, Kichikawa K, Kishimoto T. Abnormalities of the uncinate fasciculus and posterior cingulate fasciculus in mild cognitive impairment and early Alzheimer's disease: a diffusion tensor tractography study. Brain Res. 2009;1287:184–191. doi: 10.1016/j.brainres.2009.06.052. [DOI] [PubMed] [Google Scholar]
- Klunk WE, Engler H, Nordberg A, Wang Y, Blomqvist G, Holt DP, Bergstrom M, Savitcheva I, Huang GF, Estrada S, Ausen B, Debnath ML, Barletta J, Price JC, Sandell J, Lopresti BJ, Wall A, Koivisto P, Antoni G, Mathis CA, Langstrom B. Imaging brain amyloid in Alzheimer's disease with Pittsburgh Compound-B. Ann.Neurol. 2004;55:306–319. doi: 10.1002/ana.20009. [DOI] [PubMed] [Google Scholar]
- Klunk WE, Mathis CA, Price JC, Lopresti BJ, DeKosky ST. Two-year follow-up of amyloid deposition in patients with Alzheimer's disease. Brain. 2006;129:2805–2807. doi: 10.1093/brain/awl281. [DOI] [PubMed] [Google Scholar]
- Klunk WE, Price JC, Mathis CA, Tsopelas ND, Lopresti BJ, Ziolko SK, Bi W, Hoge JA, Cohen AD, Ikonomovic MD, Saxton JA, Snitz BE, Pollen DA, Moonis M, Lippa CF, Swearer JM, Johnson KA, Rentz DM, Fischman AJ, Aizenstein HJ, DeKosky ST. Amyloid deposition begins in the striatum of presenilin-1 mutation carriers from two unrelated pedigrees. J Neurosci. 2007;27:6174–6184. doi: 10.1523/JNEUROSCI.0730-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knopman DS, DeKosky ST, Cummings JL, Chui H, Corey-Bloom J, Relkin N, Small GW, Miller B, Stevens JC. Practice parameter: diagnosis of dementia (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2001;56:1143–1153. doi: 10.1212/wnl.56.9.1143. [DOI] [PubMed] [Google Scholar]
- Kuhl DE, Koeppe RA, Minoshima S, Snyder SE, Ficaro EP, Foster NL, Frey KA, Kilbourn MR. In vivo mapping of cerebral acetylcholinesterase activity in aging and Alzheimer's disease. Neurology. 1999;52:691–699. doi: 10.1212/wnl.52.4.691. [DOI] [PubMed] [Google Scholar]
- Landau SM, Harvey D, Madison CM, Koeppe RA, Reiman EM, Foster NL, Weiner MW, Jagust WJ. Associations between cognitive, functional, and FDG-PET measures of decline in AD and MCI. Neurobiology of aging. 2011;32:1207–1218. doi: 10.1016/j.neurobiolaging.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landau SM, Harvey D, Madison CM, Reiman EM, Foster NL, Aisen PS, Petersen RC, Shaw LM, Trojanowski JQ, Jack CR, Jr., Weiner MW, Jagust WJ. Comparing predictors of conversion and decline in mild cognitive impairment. Neurology. 2010;75:230–238. doi: 10.1212/WNL.0b013e3181e8e8b8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langbaum JB, Chen K, Caselli RJ, Lee W, Reschke C, Bandy D, Alexander GE, Burns CM, Kaszniak AW, Reeder SA, Corneveaux JJ, Allen AN, Pruzin J, Huentelman MJ, Fleisher AS, Reiman EM. Hypometabolism in Alzheimer-affected brain regions in cognitively healthy Latino individuals carrying the apolipoprotein E epsilon4 allele. Arch.Neurol. 2010;67:462–468. doi: 10.1001/archneurol.2010.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langbaum JBS, Chen K, Lee W, Reschke C, Bandy D, Fleisher AS, Alexander GE, Foster NL, Weiner MW, Koeppe RA, Jagust WJ, Reiman EM. Categorical and correlational analyses of baseline fluorodeoxyglucose positron emission tomography images from the Alzheimer's Disease Neuroimaging Initiative (ADNI). Neuroimage. 2009;45:1107–1116. doi: 10.1016/j.neuroimage.2008.12.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lautenschlager NT, Cox KL, Flicker L, Foster JK, van Bockxmeer FM, Xiao J, Greenop KR, Almeida OP. Effect of Physical Activity on Cognitive Function in Older Adults at Risk for Alzheimer Disease: A Randomized Trial. JAMA: The Journal of the American Medical Association. 2008;300:1027–1037. doi: 10.1001/jama.300.9.1027. [DOI] [PubMed] [Google Scholar]
- Li Y, Rinne JO, Mosconi L, Pirraglia E, Rusinek H, DeSanti S, Kemppainen N, Nagren K, Kim BC, Tsui W, de Leon MJ. Regional analysis of FDG and PIB-PET images in normal aging, mild cognitive impairment, and Alzheimer's disease. Eur.J.Nucl.Med.Mol.Imaging. 2008;35:2169–2181. doi: 10.1007/s00259-008-0833-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lustig C, Snyder AZ, Bhakta M, O'Brien KC, McAvoy M, Raichle ME, Morris JC, Buckner RL. Functional deactivations: change with age and dementia of the Alzheimer type. Proc Natl Acad Sci U S A. 2003;100:14504–14509. doi: 10.1073/pnas.2235925100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathis CA, Bacskai BJ, Kajdasz ST, McLellan ME, Frosch MP, Hyman BT, Holt DP, Wang Y, Huang GF, Debnath ML, Klunk WE. A lipophilic thioflavin-T derivative for positron emission tomography (PET) imaging of amyloid in brain. Bioorg.Med.Chem.Lett. 2002;12:295–298. doi: 10.1016/s0960-894x(01)00734-x. [DOI] [PubMed] [Google Scholar]
- McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR, Kawas CH, Klunk WE, Koroshetz WJ, Manly JJ, Mayeux R, Mohs RC, Morris JC, Rossor MN, Scheltens P, Thies W, Weintraub S, Phelps CH. The diagnosis of dementia due to Alzheimer's disease: Recommendations from the National Institute on Aging and the Alzheimer's Association Workgroup. Alzheimer's & Dementia. 2011 doi: 10.1016/j.jalz.2011.03.005. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medina D, Detoledo-Morrell L, Urresta F, Gabrieli JD, Moseley M, Fleischman D, Bennett DA, Leurgans S, Turner DA, Stebbins GT. White matter changes in mild cognitive impairment and AD: A diffusion tensor imaging study. Neurobiology of aging. 2006;27:663–672. doi: 10.1016/j.neurobiolaging.2005.03.026. [DOI] [PubMed] [Google Scholar]
- Miller BL, Cummings JL, Villaneuva-Meyer J, Boone K, Mehringer CM, Lesser IM, Mena I. Frontal lobe degeneration: clinical, neuropsychological, and SPECT characteristics. Neurology. 1991;41:1374–1382. doi: 10.1212/wnl.41.9.1374. [DOI] [PubMed] [Google Scholar]
- Minoshima S, Giordani B, Berent S, Frey KA, Foster NL, Kuhl DE. Metabolic reduction in the posterior cingulate cortex in very early Alzheimer's disease. Ann.Neurol. 1997;42:85–94. doi: 10.1002/ana.410420114. [DOI] [PubMed] [Google Scholar]
- Mintun MA, Larossa GN, Sheline YI, Dence CS, Lee SY, Mach RH, Klunk WE, Mathis CA, DeKosky ST, Morris JC. [11C]PIB in a nondemented population: potential antecedent marker of Alzheimer disease. Neurology. 2006;67:446–452. doi: 10.1212/01.wnl.0000228230.26044.a4. [DOI] [PubMed] [Google Scholar]
- Mormino EC, Kluth JT, Madison CM, Rabinovici GD, Baker SL, Miller BL, Koeppe RA, Mathis CA, Weiner MW, Jagust WJ. Episodic memory loss is related to hippocampal-mediated beta-amyloid deposition in elderly subjects. Brain. 2009;132:1310–1323. doi: 10.1093/brain/awn320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mormino EC, Smiljic A, Hayenga AO, Onami H, Greicius MD, Rabinovici GD, Janabi M, Baker SL, Yen V, Madison CM, Miller BL, Jagust WJ. Relationships between Beta-Amyloid and Functional Connectivity in Different Components of the Default Mode Network in Aging. Cereb Cortex. 2011 doi: 10.1093/cercor/bhr025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris JC, Roe CM, Grant EA, Head D, Storandt M, Goate AM, Fagan AM, Holtzman DM, Mintun MA. Pittsburgh Compound B imaging and prediction of progression from cognitive normality to symptomatic Alzheimer disease. Arch Neurol. 2009;66:1469–1475. doi: 10.1001/archneurol.2009.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris JC, Roe CM, Xiong C, Fagan AM, Goate AM, Holtzman DM, Mintun MA. APOE predicts amyloid-beta but not tau Alzheimer pathology in cognitively normal aging. Ann.Neurol. 2010;67:122–131. doi: 10.1002/ana.21843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosconi L, De SS, Brys M, Tsui WH, Pirraglia E, Glodzik-Sobanska L, Rich KE, Switalski R, Mehta PD, Pratico D, Zinkowski R, Blennow K, de Leon MJ. Hypometabolism and altered cerebrospinal fluid markers in normal apolipoprotein E E4 carriers with subjective memory complaints. Biol.Psychiatry. 2008;63:609–618. doi: 10.1016/j.biopsych.2007.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosconi L, Mistur R, Switalski R, Tsui WH, Glodzik L, Li Y, Pirraglia E, De SS, Reisberg B, Wisniewski T, de Leon MJ. FDG-PET changes in brain glucose metabolism from normal cognition to pathologically verified Alzheimer's disease. Eur.J Nucl.Med.Mol.Imaging. 2009;36:811–822. doi: 10.1007/s00259-008-1039-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosconi L, Perani D, Sorbi S, Herholz K, Nacmias B, Holthoff V, Salmon E, Baron JC, De Cristofaro MT, Padovani A, Borroni B, Franceschi M, Bracco L, Pupi A. MCI conversion to dementia and the APOE genotype: a prediction study with FDG-PET. Neurology. 2004a;63:2332–2340. doi: 10.1212/01.wnl.0000147469.18313.3b. [DOI] [PubMed] [Google Scholar]
- Mosconi L, Pupi A, De Cristofaro MT, Fayyaz M, Sorbi S, Herholz K. Functional interactions of the entorhinal cortex: an 18F-FDG PET study on normal aging and Alzheimer's disease. J.Nucl.Med. 2004b;45:382–392. [PubMed] [Google Scholar]
- Mosconi L, Sorbi S, de Leon MJ, Li Y, Nacmias B, Myoung PS, Tsui W, Ginestroni A, Bessi V, Fayyazz M, Caffarra P, Pupi A. Hypometabolism exceeds atrophy in presymptomatic early-onset familial Alzheimer's disease. The Journal of Nuclear Medicine. 2006;47:1778–1786. [PubMed] [Google Scholar]
- Mosconi L, Tsui WH, De Santi S, Li J, Rusinek H, Convit A, Li Y, Boppana M, de Leon MJ. Reduced hippocampal metabolism in MCI and AD: automated FDG-PET image analysis. Neurology. 2005;64:1860–1867. doi: 10.1212/01.WNL.0000163856.13524.08. [DOI] [PubMed] [Google Scholar]
- Mueller SG, Weiner MW, Thal LJ, Petersen RC, Jack CR, Jagust W, Trojanowski JQ, Toga AW, Beckett L. Ways toward an early diagnosis in Alzheimer's disease: The Alzheimer's Disease Neuroimaging Initiative (ADNI). Alzheimers.Dement. 2005;1:55–66. doi: 10.1016/j.jalz.2005.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagren K, Halldin C, Rinne JO. Radiopharmaceuticals for positron emission tomography investigations of Alzheimer's disease. Eur J Nucl Med Mol Imaging. 2010;37:1575–1593. doi: 10.1007/s00259-009-1301-z. [DOI] [PubMed] [Google Scholar]
- Nelissen N, Van LK, Thurfjell L, Owenius R, Vandenbulcke M, Koole M, Bormans G, Brooks DJ, Vandenberghe R. Phase 1 study of the Pittsburgh compound B derivative 18F-flutemetamol in healthy volunteers and patients with probable Alzheimer disease. J.Nucl.Med. 2009;50:1251–1259. doi: 10.2967/jnumed.109.063305. [DOI] [PubMed] [Google Scholar]
- Nelissen N, Vandenbulcke M, Fannes K, Verbruggen A, Peeters R, Dupont P, Van Laere K, Bormans G, Vandenberghe R. Abeta amyloid deposition in the language system and how the brain responds. Brain. 2007;130:2055–2069. doi: 10.1093/brain/awm133. [DOI] [PubMed] [Google Scholar]
- Nordberg A, Lundqvist H, Hartvig P, Andersson J, Johansson M, Hellstrom-Lindahi E, Langstrom B. Imaging of nicotinic and muscarinic receptors in Alzheimer's disease: effect of tacrine treatment. Dementia and Geriatric Cognitive Disorders. 1997;8:78–84. doi: 10.1159/000106611. [DOI] [PubMed] [Google Scholar]
- Nordberg A, Rinne JO, Kadir A, Langstrom B. The use of PET in Alzheimer disease. Nat Rev Neurol. 2010;6:78–87. doi: 10.1038/nrneurol.2009.217. [DOI] [PubMed] [Google Scholar]
- O'Brien JL, O'Keefe KM, LaViolette PS, DeLuca AN, Blacker D, Dickerson BC, Sperling RA. Longitudinal fMRI in elderly reveals loss of hippocampal activation with clinical decline. Neurology. 2010;74:1969–1976. doi: 10.1212/WNL.0b013e3181e3966e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okello A, Edison P, Archer HA, Turkheimer FE, Kennedy J, Bullock R, Walker Z, Kennedy A, Fox N, Rossor M, Brooks DJ. Microglial activation and amyloid deposition in mild cognitive impairment: A PET study. Neurology. 2009a;72:56–62. doi: 10.1212/01.wnl.0000338622.27876.0d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okello A, Koivunen J, Edison P, Archer HA, Turkheimer FE, Nagren K, Bullock R, Walker Z, Kennedy A, Fox NC, Rossor MN, Rinne JO, Brooks DJ. Conversion of amyloid positive and negative MCI to AD over 3 years: An 11C-PIB PET study. Neurology. 2009b;73:754–760. doi: 10.1212/WNL.0b013e3181b23564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palop JJ, Chin J, Roberson ED, Wang J, Thwin MT, Bien-Ly N, Yoo J, Ho KO, Yu GQ, Kreitzer A, Finkbeiner S, Noebels JL, Mucke L. Aberrant excitatory neuronal activity and compensatory remodeling of inhibitory hippocampal circuits in mouse models of Alzheimer's disease. Neuron. 2007;55:697–711. doi: 10.1016/j.neuron.2007.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappata S, Salvatore E, Postiglione A. In vivo imaging of neurotransmission and brain receptors in dementia. J Neuroimaging. 2008;18:111–124. doi: 10.1111/j.1552-6569.2007.00194.x. [DOI] [PubMed] [Google Scholar]
- Peila R, White LR, Masaki K, Petrovitch H, Launer LJ. Reducing the risk of dementia: efficacy of long-term treatment of hypertension. Stroke. 2006;37:1165–1170. doi: 10.1161/01.STR.0000217653.01615.93. [DOI] [PubMed] [Google Scholar]
- Petersen RC, Stevens JC, Ganguli M, Tangalos EG, Cummings JL, DeKosky ST. Practice parameter: early detection of dementia: mild cognitive impairment (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2001;56:1133–1142. doi: 10.1212/wnl.56.9.1133. [Comment In: Neurology. 2001 May 8;56(9):1131-2 UI: 21241015].
- Petrella JR, Sheldon FC, Prince SE, Calhoun VD, Doraiswamy PM. Default mode network connectivity in stable vs progressive mild cognitive impairment. Neurology. 2011;76:511–517. doi: 10.1212/WNL.0b013e31820af94e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pike KE, Savage G, Villemagne VL, Ng S, Moss SA, Maruff P, Mathis CA, Klunk WE, Masters CL, Rowe CC. β-amyloid imaging and memory in non-demented individuals: evidence for preclinical Alzheimer's disease. Brain. 2007;130:2837–2844. doi: 10.1093/brain/awm238. [DOI] [PubMed] [Google Scholar]
- Quiroz YT, Budson AE, Celone K, Ruiz A, Newmark R, Castrillon G, Lopera F, Stern CE. Hippocampal hyperactivation in presymptomatic familial Alzheimer's disease. Ann Neurol. 2010;68:865–875. doi: 10.1002/ana.22105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabinovici GD, Jagust WJ, Furst AJ, Ogar JM, Racine CA, Mormino EC, O'Neil JP, Lal RA, Dronkers NF, Miller BL, Gorno-Tempini ML. Abeta amyloid and glucose metabolism in three variants of primary progressive aphasia. Ann Neurol. 2008;64:388–401. doi: 10.1002/ana.21451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raichle ME, MacLeod AM, Snyder AZ, Powers WJ, Gusnard DA, Shulman GL. A default mode of brain function. Proc Natl Acad Sci U S A. 2001;98:676–682. doi: 10.1073/pnas.98.2.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiman EM, Langbaum JBS. Brain imaging in the evaluation of putative Alzheimer's disease slowing, risk-reducing and prevention therapies. In: Jagust WJ, D'Esposito M, editors. Imaging the Aging Brain. Oxford University Press; New York: 2009. pp. 319–350. [Google Scholar]
- Reiman EM, Caselli RJ, Chen K, Alexander GE, Bandy D, Frost J. Declining brain activity in cognitively normal apolipoprotein E ε4 heterozygotes: A foundation for using positron emission tomography to efficiently test treatments to prevent Alzheimer's disease. Proc.Natl.Acad.Sci.U.S.A. 2001;98:3334–3339. doi: 10.1073/pnas.061509598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiman EM, Caselli RJ, Yun LS, Chen K, Bandy D, Minoshima S, Thibodeau SN, Osborne D. Preclinical evidence of Alzheimer's disease in persons homozygous for the ε4 allele for apolipoprotein E. N.Engl.J.Med. 1996;334:752–758. doi: 10.1056/NEJM199603213341202. [DOI] [PubMed] [Google Scholar]
- Reiman EM, Chen K, Alexander GE, Caselli RJ, Bandy D, Osborne D, Saunders AM, Hardy J. Functional brain abnormalities in young adults at genetic risk for late-onset Alzheimer's dementia. Proc.Natl.Acad.Sci.U.S.A. 2004;101:284–289. doi: 10.1073/pnas.2635903100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiman EM, Chen K, Alexander GE, Caselli RJ, Bandy D, Osborne D, Saunders AM, Hardy J. Correlations between apolipoprotein E ε4 gene dose and brain-imaging measurements of regional hypometabolism. Proc.Natl.Acad.Sci.U.S.A. 2005;102:8299–8302. doi: 10.1073/pnas.0500579102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiman EM, Chen K, Liu X, Bandy D, Yu M, Lee W, Ayutyanont N, Keppler J, Reeder SA, Langbaum JBS, Alexander GE, Klunk WE, Mathis CA, Price JC, Aizenstein HJ, DeKosky ST, Caselli RJ. Fibrillar amyloid-β burden in cognitively normal people at three levels of genetic risk for Alzheimer's disease. Proc.Natl.Acad.Sci.U.S.A. 2009;106:6820–6825. doi: 10.1073/pnas.0900345106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiman EM, Langbaum JBS, Fleisher AS, Caselli RJ, Chen K, Ayutyanont N, Quiroz YT, Kosik KS, Lopera F, Tariot PN. Alzheimer's Prevention Initiative: a plan to accelerate the evaluation of presymptomatic treatments. J Alzheimers Dis. 2011;25:293–301. doi: 10.3233/JAD-2011-0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiman EM, Langbaum JBS, Tariot PN. Alzheimer's Prevention Initiative: a proposal to evaluate presymptomatic treatments as quickly as possible. Biomarkers in Medicine. 2010;4:3–14. doi: 10.2217/bmm.09.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rentz DM, Locascio JJ, Becker JA, Moran EK, Eng E, Buckner RL, Sperling RA, Johnson KA. Cognition, reserve, and amyloid deposition in normal aging. Ann Neurol. 2010;67:353–364. doi: 10.1002/ana.21904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick SM, Sojkova J, Zhou Y, An Y, Ye W, Holt DP, Dannals RF, Mathis CA, Klunk WE, Ferrucci L, Kraut MA, Wong DF. Longitudinal cognitive decline is associated with fibrillar amyloid-beta measured by [11C]PiB. Neurology. 2010;74:807–815. doi: 10.1212/WNL.0b013e3181d3e3e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimajova M, Lenzo NP, Wu JS, Bates KA, Campbell A, Dhaliwal SS, McCarthy M, Rodrigues M, Paton A, Rowe C, Foster JK, Martins RN. Fluoro-2-deoxy-D-glucose (FDG)-PET in APOE epsilon4 carriers in the Australian population. J Alzheimers Dis. 2008;13:137–146. doi: 10.3233/jad-2008-13203. [DOI] [PubMed] [Google Scholar]
- Rinne JO, Brooks DJ, Rossor MN, Fox NC, Bullock R, Klunk WE, Mathis CA, Blennow K, Barakos J, Okello AA, de LIano SRM, Liu E, Koller M, Gregg KM, Schenk D, Black R, Grundman M. 11C-PiB PET assessment of change in fibrillar amyloid-β load in patients with Alzheimer's disease treated with bapineuzumab: a phase 2, double-blind, placebo-controlled, ascending-dose study. The Lancet Neurology. 2010;9:363–372. doi: 10.1016/S1474-4422(10)70043-0. [DOI] [PubMed] [Google Scholar]
- Rogalski E, Cobia D, Harrison TM, Wieneke C, Thompson CK, Weintraub S, Mesulam MM. Anatomy of language impairments in primary progressive aphasia. J Neurosci. 2011;31:3344–3350. doi: 10.1523/JNEUROSCI.5544-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe CC, Ackerman U, Browne W, Mulligan R, Pike KL, O'Keefe G, Tochon-Danguy H, Chan G, Berlangieri SU, Jones G, ckinson-Rowe KL, Kung HP, Zhang W, Kung MP, Skovronsky D, Dyrks T, Holl G, Krause S, Friebe M, Lehman L, Lindemann S, Dinkelborg LM, Masters CL, Villemagne VL. Imaging of amyloid beta in Alzheimer's disease with (18)F-BAY94-9172, a novel PET tracer: proof of mechanism. Lancet Neurol. 2008;7:129–135. doi: 10.1016/S1474-4422(08)70001-2. [DOI] [PubMed] [Google Scholar]
- Rowe CC, Ellis KA, Rimajova M, Bourgeat P, Pike KE, Jones G, Fripp J, Tochon-Danguy H, Morandeau L, O'Keefe G, Price R, Raniga P, Robins P, Acosta O, Lenzo N, Szoeke C, Salvado O, Head R, Martins R, Masters CL, Ames D, Villemagne VL. Amyloid imaging results from the Australian Imaging, Biomarkers and Lifestyle (AIBL) study of aging. Neurobiol.Aging. 2010;31:1275–1283. doi: 10.1016/j.neurobiolaging.2010.04.007. [DOI] [PubMed] [Google Scholar]
- Rowe CC, Ng S, Ackermann U, Gong SJ, Pike K, Savage G, Cowie TF, Dickinson KL, Maruff P, Darby D, Smith C, Woodward M, Merory J, Tochon-Danguy H, O'Keefe G, Klunk WE, Mathis CA, Price JC, Masters CL, Villemagne VL. Imaging beta-amyloid burden in aging and dementia. Neurology. 2007;68:1718–1725. doi: 10.1212/01.wnl.0000261919.22630.ea. [DOI] [PubMed] [Google Scholar]
- Scarmeas N, Luchsinger JA, Schupf N, Brickman AM, Cosentino S, Tang MX, Stern Y. Physical activity, diet, and risk of Alzheimer disease. JAMA: The Journal of the American Medical Association. 2009;302:627–637. doi: 10.1001/jama.2009.1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholl M, Almkvist O, Axelman K, Stefanova E, Wall A, Westman E, Langstrom B, Lannfelt L, Graff C, Nordberg A. Glucose metabolism and PIB binding in carriers of a His163Tyr presenilin 1 mutation. Neurobiol Aging. 2011;32:1388–1399. doi: 10.1016/j.neurobiolaging.2009.08.016. [DOI] [PubMed] [Google Scholar]
- Schuff N, Amend D, Ezekiel F, Steinman SK, Tanabe J, Norman D, Jagust W, Kramer JH, Mastrianni JA, Fein G, Weiner MW. Changes of hippocampal N-acetyl aspartate and volume in Alzheimer's disease. A proton MR spectroscopic imaging and MRI study. Neurology. 1997;49:1513–1521. doi: 10.1212/wnl.49.6.1513. [DOI] [PubMed] [Google Scholar]
- Seeley WW, Crawford RK, Zhou J, Miller BL, Greicius MD. Neurodegenerative diseases target large-scale human brain networks. Neuron. 2009;62:42–52. doi: 10.1016/j.neuron.2009.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sexton CE, Kalu UG, Filippini N, Mackay CE, Ebmeier KP. A meta-analysis of diffusion tensor imaging in mild cognitive impairment and Alzheimer's disease. Neurobiol Aging. doi: 10.1016/j.neurobiolaging.2010.05.019. [DOI] [PubMed] [Google Scholar]
- Shaw P, Lerch JP, Pruessner JC, Taylor KN, Rose AB, Greenstein D, Clasen L, Evans A, Rapoport JL, Giedd JN. Cortical morphology in children and adolescents with different apolipoprotein E gene polymorphisms: an observational study. Lancet Neurol. 2007;6:494–500. doi: 10.1016/S1474-4422(07)70106-0. [DOI] [PubMed] [Google Scholar]
- Sheline YI, Raichle ME, Snyder AZ, Morris JC, Head D, Wang S, Mintun MA. Amyloid plaques disrupt resting state default mode network connectivity in cognitively normal elderly. Biol Psychiatry. 2010;67:584–587. doi: 10.1016/j.biopsych.2009.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoghi-Jadid K, Small GW, Agdeppa ED, Kepe V, Ercoli LM, Siddarth P, Read S, Satyamurthy N, Petric A, Huang SC, Barrio JR. Localization of neurofibrillary tangles and beta-amyloid plaques in the brains of living patients with Alzheimer disease. Am J Geriatr Psychiatry. 2002;10:24–35. [PubMed] [Google Scholar]
- Silverman DH, Small GW, Chang CY, Lu CS, Kung De Aburto MA, Chen W, Czernin J, Rapoport SI, Pietrini P, Alexander GE, Schapiro MB, Jagust WJ, Hoffman JM, Welsh-Bohmer KA, Alavi A, Clark CM, Salmon E, de Leon MJ, Mielke R, Cummings JL, Kowell AP, Gambhir SS, Hoh CK, Phelps ME. Positron emission tomography in evaluation of dementia: regional brain metabolism and long-term outcome. JAMA. 2001;286:2120–2127. doi: 10.1001/jama.286.17.2120. [DOI] [PubMed] [Google Scholar]
- Small GW, Ercoli LM, Silverman DH, Huang SC, Komo S, Bookheimer SY, Lavretsky H, Miller K, Siddarth P, Rasgon NL, Mazziotta JC, Saxena S, Wu HM, Mega MS, Cummings JL, Saunders AM, Pericak-Vance MA, Roses AD, Barrio JR, Phelps ME. Cerebral metabolic and cognitive decline in persons at genetic risk for Alzheimer's disease. Proc.Natl.Acad.Sci.U.S.A. 2000;97:6037–6042. doi: 10.1073/pnas.090106797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Small GW, Mazziotta JC, Collins MT, Baxter LR, Phelps ME, Mandelkern MA, Kaplan A, La Rue A, Adamson CF, Chang L. Apolipoprotein E type 4 allele and cerebral glucose metabolism in relatives at risk for familial Alzheimer disease. JAMA. 1995;273:942–947. [PubMed] [Google Scholar]
- Small GW, Siddarth P, Burggren AC, Kepe V, Ercoli LM, Miller KJ, Lavretsky H, Thompson PM, Cole GM, Huang SC, Phelps ME, Bookheimer SY, Barrio JR. Influence of cognitive status, age, and APOE-4 genetic risk on brain FDDNP positron-emission tomography imaging in persons without dementia. Arch.Gen.Psychiatry. 2009;66:81–87. doi: 10.1001/archgenpsychiatry.2008.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sojkova J, Driscoll I, Iacono D, Zhou Y, Codispoti KE, Kraut MA, Ferrucci L, Pletnikova O, Mathis CA, Klunk WE, O'Brien RJ, Wong DF, Troncoso JC, Resnick SM. In Vivo Fibrillar {beta}-Amyloid Detected Using [11C]PiB Positron Emission Tomography and Neuropathologic Assessment in Older Adults. Archives of Neurology. 2011;68:232–240. doi: 10.1001/archneurol.2010.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sperling RA, Aisen PS, Beckett LA, Bennett DA, Craft S, Fagan AM, Iwatsubo T, Jack CR, Kaye J, Montine TJ, Park DC, Reiman EM, Rowe CC, Siemers E, Stern Y, Yaffe K, Carrillo MC, Thies B, Morrison-Bogorad M, Wagster MV, Phelps CH. Toward defining the preclinical stages of Alzheimer's disease: Recommendations from the National Institute on Aging and the Alzheimer's Association workgroup. Alzheimer's & dementia : the journal of the Alzheimer's Association. 2011;7:280–292. doi: 10.1016/j.jalz.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sperling RA, LaViolette PS, O'Keefe K, O'Brien J, Rentz DM, Pihlajamaki M, Marshall G, Hyman BT, Selkoe DJ, Hedden T, Buckner RL, Becker JA, Johnson KA. Amyloid deposition is associated with impaired default network function in older persons without dementia. Neuron. 2009;63:178–188. doi: 10.1016/j.neuron.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storandt M, Mintun MA, Head D, Morris JC. Cognitive decline and brain volume loss as signatures of cerebral amyloid-beta peptide deposition identified with Pittsburgh compound B: cognitive decline associated with Abeta deposition. Arch Neurol. 2009;66:1476–1481. doi: 10.1001/archneurol.2009.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szekely CA, Green RC, Breitner JCS, Ostbye T, Beiser AS, Corrada MM, Dodge HH, Ganguli M, Kawas CH, Kuller LH, Psaty BM, Resnick SM, Wolf PA, Zonderman AB, Welsh-Bohmer KA, Zandi PP. No advantage of Aβ42-lowering NSAIDs for prevention of Alzheimer dementia in six pooled cohort studies. Neurology. 2008;70:2291–2298. doi: 10.1212/01.wnl.0000313933.17796.f6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolboom N, Yaqub M, van der Flier WM, Boellaard R, Luurtsema G, Windhorst AD, Barkhof F, Scheltens P, Lammertsma AA, van Berckel BNM. Detection of Alzheimer Pathology In Vivo Using Both 11C-PIB and 18F-FDDNP PET. The Journal of Nuclear Medicine. 2009;50:191–197. doi: 10.2967/jnumed.108.056499. [DOI] [PubMed] [Google Scholar]
- Tomlinson BE, Blessed G, Roth M. Observations on the brains of non-demented old people. J Neurol Sci. 1968;7:331–336. doi: 10.1016/0022-510x(68)90154-8. [DOI] [PubMed] [Google Scholar]
- Vaishnavi SN, Vlassenko AG, Rundle MM, Snyder AZ, Mintun MA, Raichle ME. Regional aerobic glycolysis in the human brain. Proc.Natl.Acad.Sci.U.S.A. 2010;107:17757–17762. doi: 10.1073/pnas.1010459107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valenzuela MJ, Sachdev P. Magnetic resonance spectroscopy in AD. Neurology. 2001;56:592–598. doi: 10.1212/wnl.56.5.592. [DOI] [PubMed] [Google Scholar]
- Vandenberghe R, Van LK, Ivanoiu A, Salmon E, Bastin C, Triau E, Hasselbalch S, Law I, Andersen A, Korner A, Minthon L, Garraux G, Nelissen N, Bormans G, Buckley C, Owenius R, Thurfjell L, Farrar G, Brooks DJ. 18F-flutemetamol amyloid imaging in Alzheimer disease and mild cognitive impairment: a phase 2 trial. Ann.Neurol. 2010;68:319–329. doi: 10.1002/ana.22068. [DOI] [PubMed] [Google Scholar]
- Villemagne VL, Ataka S, Mizuno T, Brooks WS, Wada Y, Kondo M, Jones G, Watanabe Y, Mulligan R, Nakagawa M, Miki T, Shimada H, O'Keefe GJ, Masters CL, Mori H, Rowe CC. High striatal amyloid beta-peptide deposition across different autosomal Alzheimer disease mutation types. Arch Neurol. 2009;66:1537–1544. doi: 10.1001/archneurol.2009.285. [DOI] [PubMed] [Google Scholar]
- Villemagne VL, Pike KE, Chetelat G, Ellis KA, Mulligan RS, Bourgeat P, Ackermann U, Jones G, Szoeke C, Salvado O, Martins R, O'Keefe G, Mathis CA, Klunk WE, Ames D, Masters CL, Rowe CC. Longitudinal assessment of Abeta and cognition in aging and Alzheimer disease. Ann Neurol. 2011;69:181–192. doi: 10.1002/ana.22248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vlassenko AG, Vaishnavi SN, Couture L, Sacco D, Shannon BJ, Mach RH, Morris JC, Raichle ME, Mintun MA. Spatial correlation between brain aerobic glycolysis and amyloid-beta (Abeta ) deposition. Proc.Natl.Acad.Sci.U.S.A. 2010;107:17763–17767. doi: 10.1073/pnas.1010461107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang HX, Karp A, Winblad B, Fratiglioni L. Late-life engagement in social and leisure activities is associated with a decreased risk of dementia: a longitudinal study from the Kungsholmen project. Am J Epidemiol. 2002;155:1081–1087. doi: 10.1093/aje/155.12.1081. [DOI] [PubMed] [Google Scholar]
- Wiley CA, Lopresti BJ, Venneti S, Price J, Klunk WE, DeKosky ST, Mathis CA. Carbon 11-labeled Pittsburgh Compound B and carbon 11-labeled (R)-PK11195 positron emission tomographic imaging in Alzheimer disease. Arch Neurol. 2009;66:60–67. doi: 10.1001/archneurol.2008.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willis SL, Tennstedt SL, Marsiske M, Ball K, Elias J, Koepke KM, Morris JN, Rebok GW, Unverzagt FW, Stoddard AM, Wright E. Long-term effects of cognitive training on everyday functional outcomes in older adults. JAMA. 2006;296:2805–2814. doi: 10.1001/jama.296.23.2805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wishart HA, Saykin AJ, McAllister TW, Rabin LA, McDonald BC, Flashman LA, Roth RM, Mamourian AC, Tsongalis GJ, Rhodes CH. Regional brain atrophy in cognitively intact adults with a single APOE ε4 allele. Neurology. 2006;67:1221–1224. doi: 10.1212/01.wnl.0000238079.00472.3a. [DOI] [PubMed] [Google Scholar]
- Wolk DA, Price JC, Saxton JA, Snitz BE, James JA, Lopez OL, Aizenstein HJ, Cohen AD, Weissfeld LA, Mathis CA, Klunk WE, Dekoskym ST. Amyloid imaging in mild cognitive impairment subtypes. Ann Neurol. 2009;65:557–568. doi: 10.1002/ana.21598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshita M, Fletcher E, Harvey D, Ortega M, Martinez O, Mungas DM, Reed BR, DeCarli CS. Extent and distribution of white matter hyperintensities in normal aging, MCI, and AD. Neurology. 2006;67:2192–2198. doi: 10.1212/01.wnl.0000249119.95747.1f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandi PP, Anthony JC, Khachaturian AS, Stone SV, Gustafson D, Tschanz JT, Norton MC, Welsh-Bohmer KA, Breitner JC. Reduced risk of Alzheimer disease in users of antioxidant vitamin supplements: the Cache County Study. Arch Neurol. 2004;61:82–88. doi: 10.1001/archneur.61.1.82. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Schuff N, Jahng GH, Bayne W, Mori S, Schad L, Mueller S, Du AT, Kramer JH, Yaffe K, Chui H, Jagust WJ, Miller BL, Weiner MW. Diffusion tensor imaging of cingulum fibers in mild cognitive impairment and Alzheimer disease. Neurology. 2007;68:13–19. doi: 10.1212/01.wnl.0000250326.77323.01. [DOI] [PMC free article] [PubMed] [Google Scholar]