Abstract
Purpose
EOS 2D/3D is an integrated, low-dose orthopedic digital radioimaging solution, which, due to its groundbreaking properties, has recently shown an increasing application in scoliosis surgery. Its integrated sterEOS 3D software allows creation of patient-specific three-dimensional (3D) lower limb models, and can produce geometrical parameters in 3D. Currently there are a limited number of reports on EOS for lower limb applications.
Methods
Three-dimensional reconstructions of 256 hip and knee joints of 128 healthy subjects, as well as 53 hips and 46 knees of 69 patients with hip or knee arthritis, were evaluated based on orthogonal EOS two-dimensional (2D) images. Measurements for hips included femur and tibia length, total length of the extremity, femoral antetorsion and offset, femoral neck length, neck-shaft and hip-knee-shaft (HKS) angles. Lower limb alignment in both frontal and sagittal planes were determined in normal and arthritic knees. Values were compared with those obtained by standard methods published by others.
Results
Normal hip and knee geometrical parameters were found in our healthy subjects. In osteoarthritic cases, values for neck-shaft angle, femoral antetorsion, femur length and total length of the extremity were shown to decrease non-significantly. Evaluation of lower limb alignment in healthy and arthritic knees showed normal values in healthy subjects apart from three cases with an average six degrees varus. Arthritic knees were most frequently found to have a varus angulation, with the exception of 11 cases with normal or valgus alignment.
Conclusion
EOS 2D/3D with its sterEOS 3D reconstruction is useful for a comprehensive 3D examination of the lower limb. In the near future it may be suitable for daily routine diagnostics of orthopedic lower limb deformities as a primary examination method.
Introduction
Georges Charpak was awarded the Nobel Prize in Physics in 1992 for his invention of a gaseous detector with a multiwire proportional chamber developed in 1968 [1]. This invention helped in the construction of new ultra-sensitive particle detectors for basic research in Physics, and led to the development of a new low-dose radioimaging device in Medicine, called EOS 2D/3D [2]. Typical radiation doses required for standard EOS images are eight to ten times lower than those used by traditional radiodiagnostic devices. Other favourable properties of EOS include fast imaging of the entire body in frontal and sagittal planes. Since a simultaneous capture of spatially calibrated 2D images is performed, 3D surface reconstruction of spine, pelvis, femur and tibia becomes possible. Imaging is performed in standing position, allowing for the examination of bones and joints under normal weight-bearing loads (Figs. 1 and 2).
Fig. 1.
Positioning of the patient in the EOS device
Fig. 2.
Anteroposterior (a) and lateral (b) EOS images of the whole body
Early applications of EOS 2D/3D in orthopedic surgery were mainly targeted at scoliosis diagnostics. Based on sterEOS 3D reconstructions, coronal and sagittal plane spine deformities and the degree of vertebral axial rotation can be precisely determined, along with the groundbreaking possibility of examining the whole spine in 3D from above in the horizontal plane [3–6]. This method also creates the possibility for a new 3D presentation and characterisation of the spinal geometry by vertebra vectors, introduced recently by our Department [7].
Ongoing development of sterEOS 3D software recently has made 3D surface reconstruction and evaluation of lower limbs available. Normal geometrical values of the lower extremity are of crucial importance in everyday practice of orthopedic surgery because they are effectively applied in reconstruction surgery as targets. Completed sterEOS 3D models automatically supply the following lower limb clinical parameters: femur and tibia length, total length of the lower extremity, femoral head diameter, femoral offset (distance of the centre point of the femoral head from the anatomical axis of the femur), femoral neck length, neck-shaft angle, axial angle of the knee joint in varus/valgus (negative values for varus and positive values for valgus position), flexion/recurvatum (positive values for flexion and negative values for recurvatum), hip knee shaft angle (HKS—angle enclosed by the mechanical and anatomical axes of the femur), tibial mechanical angle (angle enclosed by the mechanical axis of the tibia and a tangential line of the tibial plateau), femoral torsion and femoro-tibial rotation. Except for torsional values, most parameters are calculated in both 2D and 3D.
Only a limited number of international reports are available on normal geometrical parameters of the lower extremity. Toogood et al. calculated femoral antetorsion and neck-shaft angle from normal adult hip geometrical values based on digital pictures of a skeletal collection of several thousand subjects by ImageJ software [8]. Bråten et al. determined the average antetorsion of normal adults by ultrasound [9]. Femoral offset was measured by Lecerf et al. by bidirectional X-rays [10], while femoro-tibial angle was assessed by Massé et al. on radiographs [11]. The femoro-tibial angle and HKS angle were evaluated in lower extremity X-rays with the assistance of a special computer programme at the Mayo Clinic in Rochester [12]. The total length of the extremity and the torsion value were described by considering the axis and the length of the lower extremity at the Ulm University Clinic [13].
The main purpose of this study was to prove that EOS 2D/3D is a useful tool for clinical examination of the lower extremity. A further goal was to calculate normal values of the lower extremity in young adults by this new method and to compare them with values of axis and angle deviations in degenerative hip and knee disorders.
Materials and methods
For our healthy study group, 65 individuals with no major joint pathology of the limb and no clinical complaints or radiological signs of lower extremity joint degeneration went through an EOS 2D/3D examination between 2008 and 2010 at our Department (Figs. 1 and 2). This resulted in 128 normal lower limb 3D reconstructions, with 65 left and 63 right limbs evaluated. Two right limbs were omitted due to inaccurate limb positioning on anteroposterior X-ray images. Gender ratio was 36 females and 29 males. Average patient age at the time of EOS 2D examinations was 26.3 (range, 19–39) years. Based on the radiological grading scale described by Kellegren and Lawrence, these individuals can be assessed as normal, with no indication for arthritis in the hips or in the knees. Therefore, geometrical parameters of lower limbs in this group were considered as normal, which is characteristic for a healthy population.
EOS 2D/3D examination was performed on 37 patients suffering from hip arthritis. Since in 16 cases both hips were affected, a total of 53 hips were included. Gender ratio was 28 females and nine males. The average patient age was 67.8 (range, 45–80) years. Additionally, 32 patients with knee arthritis were also examined by EOS 2D/3D. Since 18 of the 32 patients were affected unilaterally, a total of 46 knees were included. There were 28 female and four male patients in this subgroup; their average age was 67 years (range, 53–80). In all these patients, the grade of arthritis was assessed as grade two or above based on the Kellegren-Lawrence grading scale.
Lower extremity examinations in standing position were performed by EOS 2D/3D (EOS Imaging, Paris, France) at the Department of Radiology, University of Pécs, Hungary. Lower limb surface 3D reconstructions were created using anteroposterior and lateral EOS X-ray images with sterEOS 3D workstation software version 1.4.2 (EOS Imaging, Paris, France), performing the full 3D procedure. The 3D reconstructions were carried out by two individuals with experience in the lower limb sterEOS 3D reconstruction procedure. Clinical parameters were exported to Microsoft Excel and statistical analysis was performed by SPSS version 19 (IBM Corp., USA).
Results
Geometrical parameters of the lower extremity in our normal group representing a healthy population are demonstrated in Table 1.
Table 1.
Normal geometrical parameters of the lower limb detected in our healthy study group
| Parameters | Total mean | SD | Males | Females |
|---|---|---|---|---|
| Femur length (cm) | 42.9 | 3.11 | 44.1 | 41.8 |
| Tibia length (cm) | 37.1 | 2.81 | 38 | 35.3 |
| Total limb length (cm) | 80.5 | 5.82 | 82.5 | 78.5 |
| Proximal femur | ||||
| Femoral head diameter (mm) | 44.5 | 3.78 | 47.1 | 42 |
| Femoral neck length (mm) | 50.5 | 4.65 | 52.7 | 48.8 |
| Neck-shaft angle (°) | 128.4 | 4.93 | 129 | 127.8 |
| Knee | ||||
| Varus/ valgus (°) | −0.8 | 3.13 | −2.3 | 0.7 |
| Flexion/ recurvatum (°) | −1.2 | 7.37 | 1.2 | −3.7 |
| HKS (°) | 4.8 | 1.33 | 4.9 | 4.6 |
| Tibial mechanical angle (°) | 88 | 3.57 | 86.4 | 89.6 |
| Torsion | ||||
| Femoral antetorsion (°) | 17.1 | 11.51 | 15.1 | 19.2 |
| Femorotibial rotation (°) | 2.3 | 7.16 | 0.9 | 2.6 |
| Tibial torsion (°) | 36 | 8.35 | 34.3 | 37.7 |
SD standard deviation, HKS hip knee shaft angle
Length of the femoral mechanical axis was 42.9 cm (range, 37.3–50.8), and the tibial mechanical axis length was 37.1 cm (range, 32.6–44.4). The longest tibia belonged to the longest femur. A pairwise comparison of these values revealed that they were directly proportional with minimal deviations. Femoral head diameter was 44.5 mm (range, 38.6–55.3), while the femoral neck length was 50.5 cm (range, 40.9–63.4). Length and diameter values of males were larger than those of females.
Head-neck angle in males was 129° (116–142), which was significantly greater than in females 127.8° (range, 114–141.6). HKS angle was 4.8° (range, 1–8.6), with 4.6° in females and 4.9° in males.
The angle of the femoro-tibial axis enclosed by the femoral and tibial mechanical angles in the frontal plane was −0.8° (range, −7.5−5.5), i.e. a small varus position. In males this parameter was −2.3° (i.e., varus), while in females it was 0.7° (i.e., valgus). Flexion/recurvatum is the angle enclosed by the femoral and tibial mechanical angles measured in the sagittal plane. Positive values are called flexion, while negative values are called recurvatum. A representative case with a moderate −1.2° recurvatum is shown in Fig. 3. A difference based on sex was found to be nearly 5° (females, −3.7°; males, 1.2°) and it could be considered significant.
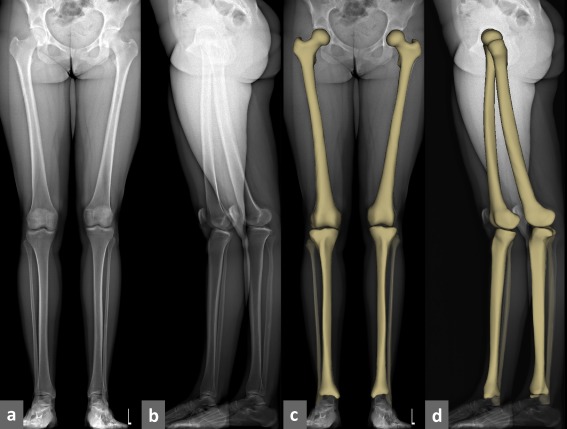
Fig. 3.
Anterioposterior and lateral EOS 2D images (a,b); frontal and lateral views of a corresponding sterEOS 3D model overlayed on EOS 2D images (c,d) of a normal lower limb
When the healthy group was analysed based on their varus and valgus values, the following observations were made: 125 knees belonged to a subgroup with normal axis position (a “normal” axis position was considered when, in accordance with published reports, it did not deviate more than 5° from zero), only three knees were found with varus showing an average four degrees and none was found with valgus. Mean values of clinical parameters within the “normal” subgroup were: 1° valgus, −3° recurvatum and 5° HKS. The same values for the three cases with varus alignment were 6° varus, 0.6° flessum, and 4.6° HKS.
The 3D values for torsion were remarkably diverse. The average value of femoral torsion was 17.1° (range, −4.4 to 39.1) with a standard deviation of 11.51°. Its value was positive in antetorsion and negative in retrotorsion. Antetorsion in females was 19.2°, 4.1° greater than in males. Average tibial torsion was 36° (range, 16.6–52.3), indicating a significant outwards rotation (negative values would indicate inwards rotation). The average value in females was higher than in males (37.6° and 34.2°, respectively). sterEOS 3D software calculates femoro-tibial rotation between a tangent line drawn along the two most posterior points of the tibia plateau and the bimalleolar line, in a plane perpendicular to the mechanical axis of the femur. Its value is positive when the tibia is rotated outwards and negative when rotated inwards. Total mean value was 2.3° (range, −10.7 to 14.8), with a standard deviation of 7.16°. Similarly to the other torsion parameters, the mean value in females (3.6°) exceeded the one in males (0.9°).
All the above parameters were evaluated in our group of 37 hip arthritis patients and 32 knee arthritis patients. Results are summarised in Table 2, demonstrating that in patients suffering from hip joint degeneration the mean neck-shaft angle, femoral antetorsion, femoral and tibial length, as well as the total length of the extremity showed reduced values compared to those in the healthy population. Higher values were found for femoral offset compared to normals.
Table 2.
Results of our hip arthritis group
| All hips (n = 53) | Mean | SD |
|---|---|---|
| Age (years) | 67.8 | 29.5 |
| Femoral length (cm) | 40.8 | 2.6 |
| Tibial length (cm) | 35.2 | 2.6 |
| Total length of the limb (cm) | 76 | 56.2 |
| Femoral head diameter (mm) | 46 | 4.1 |
| Femoral neck length (mm) | 50.8 | 4.8 |
| Neck-shaft angle (°) | 122.8 | 6.0 |
| Femoral antetorsion (°) | 15.6 | 11.2 |
| Femoro-tibial rotation (°) | 2.2 | 7.2 |
| Tibial torsion (°) | 26.8 | 9.4 |
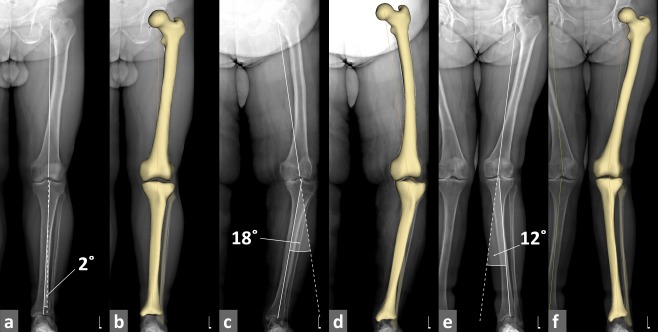
When our group of patients suffering from knee joint degeneration was analysed based on their lower extremity varus/valgus alignment, seven knees were found showing normal axis position with an average value of −0.9° (range, 4 to 5), 35 knees exhibiting varus position with an average of −8.8° (range, −16 to 5), and four knees with a valgus position with an average of 9.6° (range, 5–20) (results shown in Table 3). Our results demonstrate that the arthritic knee varus position was the most typical knee axis alignment. Its value, however, was much more pronounced compared to the value found in our healthy subgroup with varus alignment (−6.0° versus −0.8°, shown in Fig. 4).
Table 3.
Results of our knee arthritis group
| All knees (n = 46) | Mean | SD |
|---|---|---|
| Age (years) | 67.0 | 12.73 |
| Valgus/Varus (°) | −6.0 | 2.55 |
| Flexion/Recurvatum (°) | 7.0 | 6.44 |
| HKS (°) | 7.0 | 2.25 |
| Tibial mechanical angle (°) | 85.2 | 3.41 |
| Normal axis (n = 7) | ||
| Age (years) | 70.3 | 11.7 |
| Valgus/Varus (°) | −0.9 | 1.86 |
| Flexion/Recurvatum (°) | 7.0 | 4.71 |
| HKS (°) | 6.4 | 2.38 |
| Tibial mechanical angle (°) | 85.7 | 4.31 |
| Varus axis (n = 35) | ||
| Age (years) | 69.1 | 29.9 |
| Valgus/Varus (°) | −8.8 | 4.19 |
| Flexion/Recurvatum (°) | 8.8 | 7.52 |
| HKS (°) | 7.0 | 2.34 |
| Tibial mechanical angle (°) | 85.0 | 3.31 |
| Valgus axis (n = 4) | ||
| Age (years) | 67.0 | 29.6 |
| Valgus/Varus (°) | 9.6 | 1.61 |
| Flexion/Recurvatum (°) | 5.2 | 7.09 |
| HKS (°) | 7.0 | 2.05 |
| Tibial mechanical angle (°) | 93.9 | 2.96 |
SD standard deviation, HKS hip knee shaft angle
Fig. 4.
Anterioposterior EOS 2D images and frontal views of sterEOS 3D models of representative knee arthritis cases with normal, (a-b) varus (c-d), and valgus (e-f) knee alignment
Discussion
There have been few reports of the EOS imaging system for the lower extremity. Lazennec et al. presented a case report about a patellofemoral disorder following total hip replacement. In another publication the same authors evaluated acetabular component orientation with EOS 2D/3D after total hip replacement in sitting and standing positions and compared the results with conventional radiographs. They stated that methods based on the EOS imaging system played an important diagnostic role when length differences persisted postoperatively but were concealed by compensatory mechanisms. Further importance of EOS 2D/3D was also highlighted in preoperative planning [14, 15]. To our knowledge, there are no reports published presenting normal geometrical values of the major joints of the lower limb evaluated by EOS 2D/3D; therefore, our results were compared with those obtained by other examination methods. Values for neck-shaft angle, femoral antetorsion, the femoral and tibial length, as well as the total length of the extremity in our healthy group are in good accord with normal values presented in the international literature. The mean value of neck-shaft angle for the healthy population was identical to the value of 128.23° reported by Toogood et al. [8].
Our results for femoral antetorsion are comparable to those described by Bråten et al., with 18° antetorsion in males and 14° in females [9]. Femoral and tibial length and the total length of the extremity correspond very well with the values 46.3 ± 6.4 cm, 36.9 ± 5.6 cm and 83.2 ± 11.4 cm, respectively, published earlier by the University Clinic in Ulm [13]. Comparing results for our healthy knee group with those presented by Massé et al., it is concluded that our value of femoro-tibial angle of −0.8° varus is in very good agreement with the value of 0° reported [11]. Our observation, however, of the value of femoro-tibial angle in normals with an average 2.3° varus in males and 0.7° valgus in females was not supported by their results [11].
Compared to our healthy subjects, a decreased mean neck-shaft angle value was found in our patients with hip arthritis. Considering that the average age of our healthy group was 26.3 years (range, 19–39), whereas it was 67 years (range, 53–80) in our arthritic group, it can be concluded that aging may have an influence on the reduction of neck-shaft angle. This observation seems to be supported by other published reports documenting the neck-shaft angle value to constantly decrease with age [16]. Femoral antetorsion in our arthritic group was found to be 2.7° smaller than in our healthy group, which value still falls within the normal range and corresponds to normal values described by Byrne and Tönnis [16]. The decrease in values for femoral offset and total length of lower extremity presented in our study correspond to results reported by Sariali et al., who detected a value of 42.2 mm in idiopathic hip osteoarthritis [17]. Comparing our arthritic and healthy groups, an average 1.5-mm difference was found in values of femoral head diameter, a discrepancy which may be caused by osteophytes deposited on the femoral head. No significant difference was found in femoral neck length between our two patient groups, indicating that hip arthritis has no influence on its value.
In our group with knee arthritis 35 knees were shown in varus position and four in valgus position. This corresponds well to observations by Chitnavis et al., who demonstrated that the varus position is more common than valgus for knee alignment [18]. Knee degeneration is usually accompanied by axis deviation, although a prevalent role in this is played by alteration of the tibial mechanical angle. Our study revealed the tibial mechanical angle in our knee arthritis group showing a significant difference compared to normal values within our healthy study group (85° in the varus subgroup and 94° in the valgus subgroup), or a similar difference to normal values reported by Derek et al. [19]. With regards to HKS, our results correspond to those published by Kraus et al., reporting a value of 6.4° in males and 3.5° in females [20].
Our study demonstrated that EOS imaging is a satisfactory method for lower limb examinations. Hip and knee geometrical parameters can be evaluated at a significantly lower radiation dose compared to conventional X-ray techniques. More importantly, reported clinical parameters reflect results of real 3D measurements, rather than representing conventional projected 2D values. In addition, examination of the whole lower extremity as a complex biomechanical system becomes possible. Furthermore, evaluation of torsional parameters (e.g. femur antetorsion, femorotibial rotation) are also easily performed. Earlier, these were only possible based on 3D reconstructions from computed tomography.
We believe that due to an ongoing development of the EOS system, the scope of its applications can be expected to expand and soon to be regarded as a primary diagnostic examination method.
Acknowledgement
Part of this work was supported by grant ETT287-10/2009 from the Health Science Council of Hungary (Dr. P. Than).
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Charpak G. La detection des particules. Recherche. 1981;128:1384–1396. [Google Scholar]
- 2.Kalifa G, Charpak G, Maccia C, Fery-Lemonnier E, Bloch J, Boussard JM, Attal M, Dubousset J, Adamsbaum C. Evaluation of a new low-dose digital x-ray device: first dosimertric and clinical result in children. Pediatr Radiol. 1998;28:557–561. doi: 10.1007/s002470050413. [DOI] [PubMed] [Google Scholar]
- 3.Aubin C-É, Dansereau J, Petit Y, Parent F, Guise JA, Labelle H. 3D measurement of wedge scoliotic vertebrae and intervertebral disks. Eur Spine J. 1998;7:59–65. doi: 10.1007/s005860050029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Delorme S, Labelle H, Aubin C-É, Guise JA, Rivard C, Poitras B, Dansereau J. A three-dimensional radiographic comparison of Cotrel-Dubousset and Colorado Instrumentations for the correction of idiopathic scoliosis. Spine. 2000;25:205–210. doi: 10.1097/00007632-200001150-00010. [DOI] [PubMed] [Google Scholar]
- 5.Liljenqvist UR, Link TM, Halm HF. Morphometric analysis of thoracic and lumbar vertebrae in idiopathic scoliosis. Spine. 2000;25:1247–1253. doi: 10.1097/00007632-200005150-00008. [DOI] [PubMed] [Google Scholar]
- 6.Petit Y, Aubin C-É, Labelle H. Three-dimensional imaging for the surgical treatment of idiopathic scoliosis in adolescents. Can J Surg. 2002;45:453–458. [PMC free article] [PubMed] [Google Scholar]
- 7.Illés T, Tunyogi-Csapó M, Somoskeöy S. Breakthrough in three-dimensional scoliosis diagnosis: significance of horizontal plane view and vertebra vectors. Eur Spine J. 2011;20:135–143. doi: 10.1007/s00586-010-1566-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Toogood BS, Skalak A, Cooperman DR. Proximal femoral anatomy in the normal human population. Clin Orthop Relat Res. 2009;467:876–885. doi: 10.1007/s11999-008-0473-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bråten M, Terjesen T, Rossvoll I. Femoral anteversion in normal adults. Ultrasound measurements in 50 men and 50 women. Acta Orthop Scand. 1992;63:29–32. doi: 10.3109/17453679209154844. [DOI] [PubMed] [Google Scholar]
- 10.Lecerf G, Fessy MH, Philippot R, Massin P, Giraud F, Flecher X, Girard J, Mertl P, Marchetti E, Stindel E. Femoral offset: Anatomical concept, definition, assessment, implications for preoperative templating and hip arthroplasty. Orthop Traumatol Surg Res. 2009;95:210–219. doi: 10.1016/j.otsr.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 11.Massé JP, Glimet T, Alpérovitch A, Kuntz D. Value of the femorotibial angle in 244 patients without knee arthritis. Rev Rheum Mal Osteoartic. 1985;52:91–94. [PubMed] [Google Scholar]
- 12.Hsu RW, Himeno S, Coventry MB, Chao EY. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res. 1990;255:215–227. [PubMed] [Google Scholar]
- 13.Strecker W, Keppler P, Gebhard F, Kinzl L. Length and torsion of the lower limb. J Bone Joint Surg Br. 1997;79:1019–1023. doi: 10.1302/0301-620X.79B6.7701. [DOI] [PubMed] [Google Scholar]
- 14.Lazennec J-Y, Rangel A, Baudoin A, Skalli W, Catonne Y, Rousseau MA. The EOS imaging system for understanding a patellofemoral disorder following THR. Orthop Traumatol Surg Res. 2011;97:98–101. doi: 10.1016/j.otsr.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 15.Lazennec J-Y, Rousseau MA, Rangel A, Gorin M, Belicourt A, Brusson A, Catonné Y. Pelvis and total hip arthroplasty acetabular component orientations in sitting and standing positions: Measurements reproductibility with EOS imaging system versus conventional radiographies. Orthop Traumatol Surg Res. 2011;97:373–380. doi: 10.1016/j.otsr.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 16.Byrne DP, Mulhall KJ, Baker JF. Anatomy & biomechanics of the hip. The Open Sports Med J. 2010;4:44–50. [Google Scholar]
- 17.Sariali E, Mouttet A, Pasquier G, Durante E. Three-dimensional hip anatomy in osteoarthritis. Analysis of the femoral offset. J Arthroplasy. 2009;24:990–997. doi: 10.1016/j.arth.2008.04.031. [DOI] [PubMed] [Google Scholar]
- 18.Chitnavis J, Sinsheimer JS, Suchard MA, Clipsham K, Carr AJ. End-stage coxarthritis and gonarthritis. Aetiology, clinical patterns and radiological features of idiopathic osteoarthritis. Rheumatol (Oxford) 2000;39:612–619. doi: 10.1093/rheumatology/39.6.612. [DOI] [PubMed] [Google Scholar]
- 19.Derek T, Cooke V, Kelly B, Li J. Prosthetic reconstruction of the arthritic knee: considerations for limb alignment, geometry and soft tissue reconstruction. Knee. 1998;5:165–174. doi: 10.1016/S0968-0160(97)10014-X. [DOI] [Google Scholar]
- 20.Kraus VB, Vail TP, Worrell T, McDaniel G. A comparative assessment of alignment angle of the knee by radiographic and physical examination methods. Arth Rheum. 2005;52:1730–1735. doi: 10.1002/art.21100. [DOI] [PubMed] [Google Scholar]