Abstract
Hepatocellular carcinoma (HCC) is one of the most common malignancies worldwide. Although molecular biology of carcinogenesis and tumor progression of HCC has been increasingly understood with intense research in recent years, the molecular and cellular mechanisms of HCC pathogenesis are still poorly understood. In the present study, a case-control study including 390 HCC patients and 431 healthy controls was conducted to investigate the association of HCC susceptibility with the mitochondrial DNA (mtDNA) 9-bp deletion polymorphism in Chinese population. Chi-square testing showed that frequencies of 9-bp one repeat or two repeats were significantly different between HCC and control groups. Carriage of 9-bp one repeat fragment was associated with a significantly increased risk of developing HCC (odds ratio=1.48, 95% confidence interval: 1.03–2.14, p=0.027). Stratification analysis further showed that the differences between cases and controls were more obvious in drinkers than nondrinkers. Computational modeling of the 9-bp deletion polymorphism suggests that the mtDNA sequence without the 9-bp deletion polymorphism lies within a predicted binding site (seed region) for hsa-miR-519c-5p and hsa-miR-526a. Our data suggested that the 9-bp deletion polymorphism in mitochondria may influence HCC risk, likely through specific microRNA-mediated regulation, which was possibly involved in the pathogenesis of HCC. The replication of our studies in other populations with larger sample size is warranted.
Introduction
Hepatocellular carcinoma (HCC) is one of the most common malignancies worldwide, with the highest incidence in Southeast Asia and sub-Saharan Africa (Chen et al., 1997). It has a 5 year natural mortality rate of >95%, and it affects >500,000 people in the world a year, >50% of whom are in China (Wang and Jia, 2011). Apart from genetic factors, the most prominent etiological factors associated with HCC are chronic viral hepatitis B and C (HBV and HCV) infections, exposure to environmental chemicals or alcohol, and metabolic liver diseases (Wang et al., 2002; Moradpour and Blum, 2005). Molecular biology of carcinogenesis and tumor progression of HCC has been increasingly understood with intense research in recent years. However, the molecular and cellular mechanisms of HCC pathogenesis are still poorly understood.
The mitochondrial DNA (mtDNA) mutations that include point mutation, deletion, and duplication that affect transcription and translation of mtDNA are the main etiology factors for most mitochondrial diseases (Basso et al., 2007; Shen et al., 2010). The mtDNA 9-bp deletion polymorphism is caused by the loss of one copy of the 9-bp tandem repeat sequence (CCCCCTCTA) in the intergenic region of cytochrome c oxidase II (COII)/mitochondrial TK2 thymidine kinase 2 (MTTK) (Wrischnik et al., 1987). As one of the phylogenetic markers, the 9-bp deletion polymorphism has been widely used to study evolutionary trends and migration of populations (Soodyall et al., 1996; Yao et al., 2000). However, this polymorphism has also been suggested to be associated with several diseases including cancer (Krishnan and Turnbull, 2010; Zhuo et al., 2010; Komandur et al., 2011). Considering its specific location, the 9-bp deletion polymorphism may have the potential to alter downstream and/or upstream gene expression. For example, some crucial structural components of the respiratory chain, such as ATP synthase 8 (MT-ATP8), ATP synthase 6 (MT-ATP6), cytochrome c oxidase III (MT-CO3), and cytochrome b (MT-CYB) are located in the downstream of 9-bp deletion polymorphism. Abnormal expression of these genes can lead to alterations in oxidative phosphorylation and the level of oxidative stress. It has been proposed that enhanced oxidative stress is one of the most important factors in the carcinogenesis of HCC (Ha et al., 2010; Lawless et al., 2010). Further, some studies have suggested that depletion of the cellular mitochondrial content, impaired mitochondrial biogenesis, and somatic mutations in mtDNA are important events during carcinogenesis of HCC (Cuezva et al., 2002; Yin et al., 2004). However, the genetic contribution of the 9-bp deletion polymorphism to HCC susceptibility is yet to be investigated.
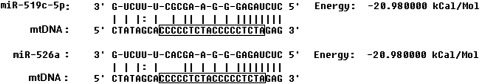
MicroRNAs (miRNAs) are a class of short noncoding RNAs with posttranscriptional regulatory functions (Pillai, 2005). Recently, the presence of pre-miRNA and miRNA in the human mitochondria has been experimentally demonstrated, supporting the hypothesis that some miRNA could be imported and/or processed in the mitochondria for post-transcriptional regulation of mitochondria (Barrey et al., 2011). Thus, polymorphisms residing in the mitochondria may interrupt the binding of miRNA to mRNA with consequences on regulation of target genes thereby affecting the individual's cancer risk (Chen et al., 2008). Based on in silico analysis, we find that the 9-bp deletion polymorphism is located in the hsa-miR-519c-5p and hsa-miR-526a potential target sequence. Deletion of 9-bp repeat sequence (CCCCCTCTA) will disrupt the bindings of hsa-miR-519c-5p and hsa-miR-526a to the target. The aim of the present study is to investigate whether the 9-bp deletion polymorphism would modify the occurrence of HCC in a Chinese population.
Materials and Methods
In silico analysis of miRNA-binding
The mature human miRNA sequences were obtained from the miRNA database (miRBase) (http://microrna.sanger.ac.uk). A region comprising the polymorphism plus 15-bp 5′ and 3′ was used for analyzing hybridization of putative miRNAs. The minimum free energy required for hybridization of putative miRNA and polymorphisms was predicted by miRanda software with default parameters (John et al., 2004).
Study populations
The case-control study was performed on genomic DNA extracted from peripheral blood of newly diagnosed incident HCC cases together with controls after obtaining informed consent. All subjects recruited were unrelated ethnic Han Chinese. The case series comprised 390 HCC patients diagnosed, hospitalized, and treated in the Suzhou municipal hospital and the affiliated hospitals of Soochow University from 2006 to 2009. All the patients had not been given any medical treatment. The diagnosis of the cases, the inclusion and exclusion criteria for the cases and controls, and the definition of smokers and drinkers were previously described in detail (Gao et al., 2009; Chen et al., 2010; He et al., 2010). Briefly, HCC patients were excluded if they had: (a) primary or secondary biliary cirrhosis or Budd-Chiari syndrome; (b) autoimmune hepatitis or toxic hepatitis; (c) recurrence of HCC; (d) tumors other than HCC; or (e) liver disease due to parasitosis, diabetes, fatty liver, metabolism disorders or severe cardiovascular diseases. HCC diagnosis was confirmed by a pathological examination combined with positive results on magnetic resonance imaging and/or computerized tomography. Tumor stages were determined according to a modified American Joint Committee on Cancer and International Union against Cancer standard. A total of 431 controls were cancer-free individuals selected from a community nutritional survey that was conducted in the same regions during the same period as recruitment of cancer patients. Subjects who smoked more than two cigarettes per day for >1 year were classified as smokers; others were defined as nonsmokers. Subjects were considered as alcohol drinkers, if they drank at least once per week; others were considered nondrinkers. All participants were negative for antibodies to hepatitis C virus, hepatitis D virus, and HIV. The design of the study was approved by the Ethical Committee of Suzhou Municipal Hospital and Soochow University.
DNA extraction and genotyping
A Chelex method was used for extracting genomic DNA of blood samples (Walsh et al., 1991). DNA fragments containing the polymorphism were amplified with the forward primer 5′-CGA CCA ACT CAT ACA CCT CC-3′ and reverse primer 5′-GAGAAG TAG ATT GAA GCC AG-3′. Polymerase chain reaction (PCR) was performed in a total volume of 37.5 μL, including 3.75 μL 10× PCR buffer, 1.5 mM MgCl2, 0.25 mM dNTPs, 0.5 mM each primer, 100 ng of genomic DNA, and 1.5U of Taq DNA polymerase. The PCR conditions were 94°C for 5 min, followed by 35 cycles of 40 s at 94°C, 40 s at 58°C, and 40 s at 72°C, with a final elongation at 72°C for 5 min. The PCR products were analyzed by 7% nondenaturing polyacrylamide gel electrophoresis and visualized by silver staining (Allen et al., 1989). A 10% random sample was tested in duplicate by different researchers, and the reproducibility was 100%. The genotype was determined by the number and position of the band on the gels. The 9-bp one repeat, two repeats, and three repeats yielded a 191-bp, a 200-bp band, and a 209-bp, respectively.
Statistical analysis
Chi-square testing was used to analyze the association between the polymorphism and cancer risk. Stratification analyses were also performed based on sex, median of age, HBV infection status, drinking, and smoking status. In all cases, homozygosis for the most common allele was used as the reference category. These statistical analyses were implemented in Statistic Analysis System software (version 8.0, SAS Institute). p<0.05 was used as the criterion of statistical significance.
Results
In silico analysis of miRNA-binding
Computational modeling of the 9-bp deletion polymorphism suggests that the mtDNA sequence without the 9-bp deletion polymorphism lies within a predicted binding site (seed region) for hsa-miR-519c-5p and hsa-miR-526a. Conversely, binding with mtDNA sequence containing the 9-bp insertion allele would be disrupted (Fig. 1). The minimum free energy required for hybridization is calculated as −20.98 kcal/mol.
FIG. 1.
In silico analysis of micro RNA-bindings using miRanda software. The minimum free energy required for hybridization is calculated to be −20.98 kcal/mol.
Association of HCC with the 9-bp deletion polymorphism
The characteristics of the 390 HCC patients and 431 controls included in the analysis were summarized in Table 1. There were no statistically significant differences between cases and controls in terms of the frequency distribution of sex, age, smoking, and drinking status. As expected, HBV infection was a significant risk factor for HCC. About 74.1% of the cases were HBsAg positive, which were significantly higher than that of the controls (11.6%, p<0.0001). In the present study, only one repeat (191-bp) and two repeats (200-bp) were observed in all the case and control samples (n=821). Chi-square testing showed that frequencies of 9-bp one repeat or two repeats were significantly different between HCC and control groups (Table 2). Carriage of 9-bp one repeat fragment was associated with a significantly increased risk of developing HCC (odds ratio=1.48, 95% confidence interval: 1.03–2.14, p=0.027).
Table 1.
Demographic Characteristics Among Hepatocellular Carcinoma Cases and Controls
| |
Case |
Control |
|
||
|---|---|---|---|---|---|
| Characteristics | n=390 | Frequencies (%) | n=431 | Frequencies (%) | p-Value |
| Age (mean±S.D.) | 50.9±8.7 | 51.1±9.2 | 0.89a | ||
| Gender | |||||
| Male | 255 | 65.4 | 289 | 67.1 | 0.61b |
| Female | 135 | 34.6 | 142 | 32.9 | |
| Smoking Status | |||||
| Smokers | 123 | 31.5 | 134 | 31.1 | 0.89b |
| Nonsmokers | 267 | 68.5 | 297 | 68.9 | |
| Drinking status | |||||
| Drinker | 165 | 42.3 | 176 | 40.8 | 0.67b |
| Nondrinker | 225 | 57.7 | 255 | 59.2 | |
| Tumor stages | |||||
| Ia+Ib | 271 | 69.5 | |||
| IIa+IIb | 75 | 19.2 | |||
| IIIa+IIIb | 44 | 11.3 | |||
| HBsAg, N (%) | |||||
| Positive | 289 | 74.1 | 50 | 11.6 | <0.0001b |
| Negative | 101 | 25.9 | 381 | 88.4 | |
Cases indicate patients with HCC and controls are noncancerous patients.
Two-sided two-sample t-test between cases and controls.
χ2 test for differences between cases and controls.
HCC, hepatocellular carcinoma.
Table 2.
Allelic Frequencies of 9-bp Deletion Polymorphism in Cases and Controls, and Risk of Hepatocellular Carcinoma
| Allele | Cases, n (%) | Control, n (%) | OR (95% C.I.) | p-value | ||
|---|---|---|---|---|---|---|
| Two repeats | 304 | 77.9 | 362 | 84.0 | 1.00 (reference) | – |
| One repeat | 86 | 22.1 | 69 | 16.0 | 1.48 (1.03–2.14) | 0.027 |
OR, odds ratio; C.I., confidence interval.
Further, based on drinking status stratification analysis, the overall trend is that the differences between cases and controls were more obvious in drinkers than nondrinkers (Table 3). There were no further significant findings for stratification analysis based on sex, median of age, HBV infection status, and smoking status (data not shown).
Table 3.
Logistic Regression Analyses for the Association Between 9-bp Deletion Polymorphism and Risk of Hepatocellular Carcinoma in Drinking and Nondrinking Groups
| |
Drinkers |
Nondrinkers |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Case | % | Control | % | ORa(95% C.I.) | Case | % | Control | % | ORa(95% C.I.) | |
| Two repeats | 120 | 72.7 | 147 | 83.5 | 1.00 (Reference) | 177 | 78.7 | 216 | 84.7 | 1.00 (Reference) |
| One repeat | 45 | 27.3 | 29 | 16.5 | 1.94 (1.11–3.53) | 48 | 21.3 | 39 | 15.3 | 1.51 (0.90–2.56) |
| p-value | p=0.014 | p=0.100 | ||||||||
Adjusted for sex, age, smoking status, and tumor stage.
Discussion
To our knowledge, this is the first molecular epidemiological study to investigate the association of 9-bp with risk of HCC in Chinese population. The genotyping of 390 HCC patients and 431 healthy control individuals showed significant associations with the 9-bp deletion polymorphism with HCC susceptibility. In the current sample set, we did not observe the 9-bp three repeats sequence. One possible reason may relay on its rare frequency in Chinese populations (3 out of 1218) (Yao et al., 2000). On the other hand, the frequency of 9-bp one repeat in our control samples (16.0%) was similar to that of previous reports in Chinese (14.7%). However, this frequency was 22.1% in the HCC groups, indicating a significant association between the 9-bp one repeat and the incidence of HCC.
Human mtDNA is a circular molecule consisting of 16,571-bp that contains 37 genes, including 2 rRNAs, 22 tRNAs, and 13 structural genes of the protein subunits of the oxidative phosphorylation system (Anderson et al., 1981). The mtDNA is highly susceptible to mutations because of its continuous exposure to high levels of reactive oxygen species (ROS) generated during oxidative phosphorylation. Studies have indicated that mtDNA mutation that has a negative effect on mitochondrial function is associated with many types of cancers (Bianchi et al., 2001). Mitochondria are responsible for cellular energy production and oxidative phosphorylation which play a critical role in hepatic cells that are rich in mitochondria. It helps hepatic cells to finish a variety of biological activities, such as glycometabolism, lipid metabolism, and detoxication. It has been demonstrated that miR-122 could regulate mitochondrial metabolism and its loss may be detrimental to sustaining critical liver function and contribute to morbidity and mortality of liver cancer patients (Burchard et al., 2010). Based on bioinformatics prediction, we have ground to hypothesize that miRNAs like hsa-miR-519c-5p and hsa-miR-526a would tightly bind to target transcripts containing the 9-bp two repeats, negatively regulating target genes' expression. Conversely, the binding with target transcripts containing the 9-bp one repeat would be disrupted, allowing upregulated target genes' expression. Therefore, further follow-up functional experiments are still needed for fully clarifying the issues.
Another interesting finding of the present study is that the association between the 9-bp one repeat variation and HCC susceptibility seems more evident in the drinking group. Cirrhosis caused by chronic alcohol consumption is the most common association of HCC in the developed world. Ethanol promotes oxidative stress, both by increasing ROS formation and by decreasing cellular defense mechanisms in the liver, the major site of ethanol metabolism in the body (Hoek et al., 2002). Thus, the prominent association observed in the drinking group implies mitochondria may contribute to the onset or progression of alcohol-induced liver diseases. In line of this, a genetic dimorphism in the mitochondrial targeting sequence of manganese superoxide dismutase has shown to be associated with the risk for developing HCC in cirrhotic patients (Nahon et al., 2005).
Taken together, our data suggest that the 9-bp deletion polymorphism in mitochondria may influence HCC risk, likely through specific miRNAs-mediated regulation, which is possibly involved in the pathogenesis of HCC. The replications of our studies in other populations with larger sample size are warranted.
Acknowledgments
This study is supported by grants from the Natural Science Foundation of China (No. 30800621) and the China Postdoctoral Science Foundation (No. 20080431121, No. 200902530).
Disclosure Statement
No competing financial interests exist.
References
- Allen RC. Graves G. Budowle B. Polymerase chain reaction amplification products separated on rehydratable polyacrylamide gels and stained with silver. Biotechniques. 1989;7:736–744. [PubMed] [Google Scholar]
- Anderson S. Bankier AT. Barrell BG, et al. Sequence and organization of the human mitochondrial genome. Nature. 1981;290:457–465. doi: 10.1038/290457a0. [DOI] [PubMed] [Google Scholar]
- Barrey E. Saint-Auret G. Bonnamy B, et al. Pre-microRNA and mature microRNA in human mitochondria. PLoS One. 2011;6:e20220. doi: 10.1371/journal.pone.0020220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basso D. Navaglia F. Fogar P, et al. DNA repair pathways and mitochondrial DNA mutations in gastrointestinal carcinogenesis. Clin Chim Acta. 2007;381:50–55. doi: 10.1016/j.cca.2007.02.020. [DOI] [PubMed] [Google Scholar]
- Bianchi NO. Bianchi MS. Richard SM. Mitochondrial genome instability in human cancers. Mutat Res. 2001;488:9–23. doi: 10.1016/s1383-5742(00)00063-6. [DOI] [PubMed] [Google Scholar]
- Burchard J. Zhang C. Liu AM, et al. microRNA-122 as a regulator of mitochondrial metabolic gene network in hepatocellular carcinoma. Mol Syst Biol. 2010;6:402. doi: 10.1038/msb.2010.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen CJ. Yu MW. Liaw YF. Epidemiological characteristics and risk factors of hepatocellular carcinoma. J Gastroenterol Hepatol. 1997;12:S294–S308. doi: 10.1111/j.1440-1746.1997.tb00513.x. [DOI] [PubMed] [Google Scholar]
- Chen K. Song F. Calin GA, et al. Polymorphisms in microRNA targets: a gold mine for molecular epidemiology. Carcinogenesis. 2008;29:1306–1311. doi: 10.1093/carcin/bgn116. [DOI] [PubMed] [Google Scholar]
- Chen S. He Y. Ding J, et al. An insertion/deletion polymorphism in the 3′ untranslated region of beta-transducin repeat-containing protein (betaTrCP) is associated with susceptibility for hepatocellular carcinoma in Chinese. Biochem Biophys Res Commun. 2010;391:552–556. doi: 10.1016/j.bbrc.2009.11.096. [DOI] [PubMed] [Google Scholar]
- Cuezva JM. Krajewska M. de Heredia ML, et al. The bioenergetic signature of cancer: a marker of tumor progression. Cancer Res. 2002;62:6674–6681. [PubMed] [Google Scholar]
- Gao Y. He Y. Ding J, et al. An insertion/deletion polymorphism at miRNA-122-binding site in the interleukin-1alpha 3′ untranslated region confers risk for hepatocellular carcinoma. Carcinogenesis. 2009;30:2064–2069. doi: 10.1093/carcin/bgp283. [DOI] [PubMed] [Google Scholar]
- Ha HL. Shin HJ. Feitelson MA, et al. Oxidative stress and antioxidants in hepatic pathogenesis. World J Gastroenterol. 2010;16:6035–6043. doi: 10.3748/wjg.v16.i48.6035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He Y. Ni J. Chen S, et al. The vascular endothelial growth factor-2549 insertion/deletion polymorphism is not associated with susceptibility to hepatocellular carcinoma in Chinese. DNA Cell Biol. 2010;29:393–396. doi: 10.1089/dna.2009.1015. [DOI] [PubMed] [Google Scholar]
- Hoek JB. Cahill A. Pastorino JG. Alcohol and mitochondria: a dysfunctional relationship. Gastroenterology. 2002;122:2049–2063. doi: 10.1053/gast.2002.33613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John B. Enright AJ. Aravin A, et al. Human MicroRNA targets. PLoS Biol. 2004;2:e363. doi: 10.1371/journal.pbio.0020363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komandur S. Venkatasubramanian S. Alluri RV, et al. Mitochondrial insertion-deletion polymorphism: role in disease pathology. Genet Test Mol Biomarkers. 2011;15:361–364. doi: 10.1089/gtmb.2010.0205. [DOI] [PubMed] [Google Scholar]
- Krishnan KJ. Turnbull DM. Mitochondrial DNA and genetic disease. Essays Biochem. 2010;47:139–151. doi: 10.1042/bse0470139. [DOI] [PubMed] [Google Scholar]
- Lawless MW. O'Byrne KJ. Gray SG. Targeting oxidative stress in cancer. Expert Opin Ther Targets. 2010;14:1225–1245. doi: 10.1517/14728222.2010.526933. [DOI] [PubMed] [Google Scholar]
- Moradpour D. Blum HE. Pathogenesis of hepatocellular carcinoma. Eur J Gastroenterol Hepatol. 2005;17:477–483. doi: 10.1097/00042737-200505000-00002. [DOI] [PubMed] [Google Scholar]
- Nahon P. Sutton A. Pessayre D, et al. Genetic dimorphism in superoxide dismutase and susceptibility to alcoholic cirrhosis, hepatocellular carcinoma, and death. Clin Gastroenterol Hepatol. 2005;3:292–298. doi: 10.1016/s1542-3565(04)00718-9. [DOI] [PubMed] [Google Scholar]
- Pillai R.S. MicroRNA function: multiple mechanisms for a tiny RNA? RNA. 2005;12:1753–1761. doi: 10.1261/rna.2248605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen L. Fang H. Chen T, et al. Evaluating mitochondrial DNA in cancer occurrence and development. Ann NY Acad Sci. 2010;1201:26–33. doi: 10.1111/j.1749-6632.2010.05635.x. [DOI] [PubMed] [Google Scholar]
- Soodyall H. Vigilant L. Hill AV, et al. mtDNA control-region sequence variation suggests multiple independent origins of an “Asian-specific” 9-bp deletion in sub-Saharan Africans. Am J Hum Genet. 1996;58:595–608. [PMC free article] [PubMed] [Google Scholar]
- Walsh PS. Metzger DA. Higuchi R. Chelex 100 as a medium for simple extraction of DNA for PCR-based typing from forensic material. Biotechniques. 1991;10:506–513. [PubMed] [Google Scholar]
- Wang XW. Hussain SP. Huo TI, et al. Molecular pathogenesis of human hepatocellular carcinoma. Toxicology. 2002;181–182:43–47. doi: 10.1016/s0300-483x(02)00253-6. [DOI] [PubMed] [Google Scholar]
- Wang Y. Jia J. Control of hepatitis B in China: prevention and treatment. Expert Rev Anti Infect Ther. 2011;9:21–25. doi: 10.1586/eri.10.143. [DOI] [PubMed] [Google Scholar]
- Wrischnik LA. Higuchi RG. Stoneking M, et al. Length mutations in human mitochondrial DNA: direct sequencing of enzymatically amplified DNA. Nucleic Acids Res. 1987;15:529–542. doi: 10.1093/nar/15.2.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao YG. Watkins WS. Zhang YP. Evolutionary history of the mtDNA 9-bp deletion in Chinese populations and its relevance to the peopling of east and southeast Asia. Hum Genet. 2000;107:504–512. doi: 10.1007/s004390000403. [DOI] [PubMed] [Google Scholar]
- Yin PH. Lee HC. Chau GY, et al. Alteration of the copy number and deletion of mitochondrial DNA in human hepatocellular carcinoma. Br J Cancer. 2004;90:2390–2396. doi: 10.1038/sj.bjc.6601838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhuo G. Feng G. Leng J, et al. A 9-bp deletion homoplasmy in women with polycystic ovary syndrome revealed by mitochondrial genome-mutation screen. Biochem Genet. 2010;48:157–163. doi: 10.1007/s10528-009-9308-5. [DOI] [PubMed] [Google Scholar]