Abstract
Summary
Background and objectives
Experimental acute kidney injury (AKI) activates the HMG–CoA reductase (HMGCR) gene, producing proximal tubule cholesterol loading. AKI also causes sloughing of proximal tubular cell debris into tubular lumina. This study tested whether these two processes culminate in increased urinary pellet cholesterol content, and whether the latter has potential AKI biomarker utility.
Design, setting, participants, & measurements
Urine samples were collected from 29 critically ill patients with (n = 14) or without (n= 15) AKI, 15 patients with chronic kidney disease, and 15 healthy volunteers. Centrifuged urinary pellets underwent lipid extraction, and the extracts were assayed for cholesterol content (factored by membrane phospholipid phosphate content). In vivo HMGCR activation was sought by measuring levels of RNA polymerase II (Pol II), and of a gene activating histone mark (H3K4m3) at exon 1 of the HMGCR gene (chromatin immunoprecipitation assay of urine chromatin samples).
Results
AKI+ patients had an approximate doubling of urinary pellet cholesterol content compared with control urine samples (versus normal; P < 0.001). The values significantly correlated (r, 0.5; P < 0.01) with serum, but not urine, creatinine concentrations. Conversely, neither critical illness without AKI nor chronic kidney disease raised pellet cholesterol levels. Increased HMGCR activity in the AKI+ patients was supported by three- to fourfold increased levels of Pol II, and of H3K4m3, at the HMGCR gene (versus controls or AKI− patients).
Conclusions
(1) Clinical AKI, like experimental AKI, induces HMGCR gene activation; (2) increased urinary pellet cholesterol levels result; and (3) urine pellet cholesterol levels may have potential AKI biomarker utility. The latter will require future testing in a large prospective trial.
Introduction
A seemingly constant consequence of ischemic or toxic acute kidney injury (AKI) is an upregulation of renal cortical HMG–CoA reductase (HMGCR) activity (1–10). Within 12 to 24 hours post-AKI induction, this culminates in an approximately 20% to 40% increase in renal cortical cholesterol content. Furthermore, when cultured human proximal tubular (HK-2) cells are subjected to either toxin or ATP depletion-mediated injury, increased HMGCR activity and cholesterol accumulation result (9). The significance of these in vitro findings is that they imply that injury-induced in vivo cholesterol accumulation reflects, at least in part, a direct proximal tubule cell event. The “downstream” consequences of proximal tubule cholesterol loading remain incompletely defined. However, our prior work indicates that it helps mediate the phenomenon of “ischemic preconditioning” (so-called acquired cytoresistance), whereby previously injured tubular cells become resistant to further ischemic or toxic attack (1–3). Indeed, this sequence of events is analogous to the so-called heat shock response, i.e., whereby a renal stress (i.e., heat shock) upregulates cytoprotective molecules (i.e., heat shock proteins), which then confer a cytoresistant state (11,12). That transient hyperthermia raises both heat shock protein and renal tubular cholesterol levels directly supports this “heat shock” analogy (7).
A morphologic correlate of AKI is sloughing of proximal tubular “brush border” fragments and intact tubular cells into urine (13–16). In light of the above-noted injury-induced cholesterol loading, we hypothesized that an increase in urinary pellet cholesterol content might result. If so, such a finding might have potential value as a “biomarker” of AKI. To gain some initial experimental support for this hypothesis, we collected urine samples from mice that had been subjected to two experimental models of AKI: glycerol induced rhabdomyolyis (17,18) or the maleate model (ATP depletion induced) of ARF (19,20). Urine samples were collected at either 3 or 24 hours post-AKI induction, and, after centrifugation, the pellets were extracted in chloroform: methanol and assayed for cholesterol content (21,22). The results were expressed as a ratio to the total amount of phospholipid phosphate present, used as an internal standard. As early as 3 hours, and persisting for at least 24 hours post-AKI induction, dramatic increases in urinary pellet cholesterol content were observed compared with values observed in normal mouse urine samples (unpublished observations). To assess whether pellet cholesterol assay might be able to differentiate between structural (i.e., tubular necrosis) versus functional (i.e., prerenal) ARF, a prerenal azotemia model was created (indomethacin injection into mice that were simultaneously subjected to surgical stress, induced by abdominal laparotomy). This “prerenal” model induced substantial azotemia, but no increase in urinary pellet cholesterol levels resulted.
Based on these promising preliminary experimental data, in the present study we sought to determine (1) whether this same phenomenon occurs in AKI patients; (2) whether evidence of increased HMGCR gene activity could be documented in patients by assessing RNA polymerase II binding (the enzyme that drives transcription) to HMGCR gene fragments in pelleted urinary chromatin samples (by chromatin immunoprecipitation, ChIP, assay [10]); and (3) whether pellet cholesterol levels might have potential utility as a clinical AKI biomarker. If positive data were to be obtained in this “proof of concept” study, they would provide a rationale for further testing in a large prospective clinical trial.
Materials and Methods
Patient Samples
Banked, frozen urine samples were obtained from three groups of patients: (1) critically ill patients with AKI (AKI+; n = 14); (2) critically ill patients without AKI (AKI−; n = 15); and (3) patients with chronic kidney disease (CKD; n = 15). The AKI+ and AKI− individuals were subsets of patients who were enrolled in a large, IRB-approved prospective observational study of critically ill adults treated in multiple intensive care (ICU) units at Vanderbilt University (23–25). AKI+ was defined as a ≥50% (or >26.5 μmol/L) increase in serum creatinine concentration from baseline. All AKI+ patients had a presumptive diagnosis of “acute tubular necrosis,” as judged by consulting nephrologists. The AKI− group comprised 15 critically ill ICU-hospitalized patients who had comparable overall illness severity as the AKI+ group (APACHE II scores) but who did not have AKI. The AKI+ and AKI− populations were matched for age, race, gender, and sepsis status. Demographic information for these patients and the specifics of urine sample collection has been previously described (23) (also reviewed and expanded upon in Table 1). The CKD patient population consisted of six individuals with diabetic nephropathy and nine individuals with nondiabetic CKD. These patients were enrolled in the Seattle Kidney Study, a prospective, observational IRB-approved study of subjects with CKD. Subjects are eligible if they have a Modification of Diet in Renal Disease estimated GFR <60 ml/min/1.73m2, are not receiving dialysis, and are at least 18 years of age. The CKD subjects were matched to serum creatinine concentrations that were observed in the AKI+ group at the time of study (AKI+, 2.65 ± 1.16 mg/dl; AKI−, 0.84 ± 0.29 mg/dl; CKD, 2.2 ± 0.3 mg/dl; means ± 1 SD). In addition to these 44 patient urine samples (14 AKI+, 15 AKI−; 15 CKD), additional urine samples were obtained from 15 healthy volunteers.
Table 1.
Patient characteristics of the ICU patient cohorts reported in this study
| Characteristic | Controls (n = 15) | Acute Kidney Injury (n = 14) |
|---|---|---|
| Age (years) | 64 ± 14 | 52 ± 17 |
| Male sex | 7/15 (47%) | 10/14 (71%) |
| Caucasian | 13/15 (87%) | 12/14 (86%) |
| APACHE II score | 27 ± 4 | 33 ± 7 |
| Sepsis | 10/15 (67%) | 11/14 (79%) |
| Prehospital statin use | 2/15 (13%) | 5/14 (36%) |
| Hospital mortality | 0/15 (0%) | 4/14 (29%) |
| Creatinine at enrollment | 0.84 ± 0.29 | 2.65 ± 1.16 |
| AKIN stage at enrollment | 0 | 2.3 ± 0.8 |
Clinical characteristics of the ICU patients with and without AKI at the time of enrollment. The serum creatinine concentrations at enrollment (and AKIN scores) were statistically different between the two groups. The other factors did not manifest statistical significance (overlapping 95% confidence intervals). ICU, intensive care unit; APACHE II, Acute Physiology and Chronic Health Evaluation II score; AKIN, Modified AKIN score based on serum creatinine measurements (ref 32). Continuous variables are given as means ± 1 SD.
Urine Cholesterol Assay
Urine samples were thawed at room temperature and centrifuged (12,000 rpm × 5 minutes). Immediately after thawing, the pellets underwent lipid extraction in chloroform: methanol, as described previously (1–3). The extracts were then assayed for cholesterol by the Amplex Red method (21,22). In addition, total phospholipid phosphate content was assessed, serving as an internal standard of total membrane lipid extracted (1). The cholesterol results were expressed as ratios to phospholipid phosphate content (1–3).
Assessment of HMGCR Gene Activation
We have recently demonstrated that in vivo gene activation can be noninvasively monitored in patients by measuring RNA polymerase II (Pol II) binding to target gene fragments in urinary pellets (23,25). Three principles underlie this approach: first, Pol II is the enzyme that drives transcription (30); second, degrees of Pol II binding to target genes is an indirect gauge of gene transcription (30,31); and third, chromatin immunoprecipitation assay (ChIP) can be successfully deployed for measuring Pol II gene binding using sheared, formalin-fixed urinary chromatin samples (23,25). Using this approach, we as sessed degrees of Pol II binding to exon 1 of the HMGCR gene in urinary pellets obtained from the AKI− and AKI+ patients and from normal volunteers. In brief, the urine samples were centrifuged and the pellets were fixed in formalin. The chromatin was then sheared, and RNA polymerase II binding to the start exon (exon 1) of the HMGCR gene was assessed by ChIP assay (23,25). The results were factored by the amount of Pol II binding to exon 1 of the β actin “housekeeping” gene.
Assessment of Chromatin Remodeling at the HMGCR Gene
We have previously demonstrated that one potential reason for increased HMGCR gene activity in response to AKI is the induction of “gene activating” histone modifications at the HMGCR gene (10). This allows for enhanced Pol II-gene binding and, hence, increased transcription. One notable example of this altered histone profile is an increase in the amount of trimethylated histone H3 at the lysine 4 position, yielding H3K4m3 (10). Thus, we sought clinical confirmation of our previous experimental findings by applying ChIP assay to urinary pellet chromatin fragments. To this end, the chromatin fragments generated for the above Pol II binding experiments were probed for H3K4m3 levels at HMGCR exon 1 by ChIP assay. The results were factored by H3K4m3 levels at the β actin gene.
Calculations and Statistics
All values are presented as means ± 1 SEM, unless stated otherwise. Comparisons were made by unpaired t test with Bonferroni corrections for multiple comparisons. Statistical significance was judged at a P value of <0.05.
Results
Clinical Characteristics of ICU Patient Cohorts
Clinical characteristics of the patients who formed the ICU/AKI− and ICU/AKI+ cohorts are presented in Table 1. Other than significantly higher serum creatinine levels and AKIN scores at enrollment for the AKI+ versus AKI− group, no other statistically significant differences existed between these two groups (overlapping 95% confidence intervals). Of particular note, the overall illness severity (as assessed by APACHE II scores) and the frequency of sepsis syndrome for the two groups were highly comparable.
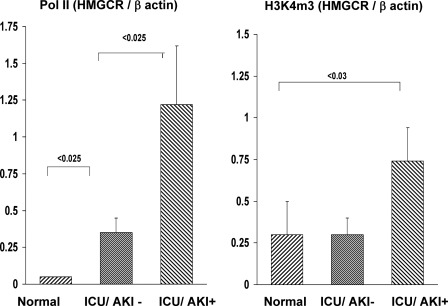
Pol II Binding and Histone 3 Lysine 4 Trimethylation at Exon 1 of the HMGCR Gene
The results of the urine pellet chromatin assessments are presented in Figure 1. As shown in the left-hand panel, Pol II binding to exon 1 of the HMGCR gene was approximately fourfold higher in the AKI+ versus the AKI− group (P < 0.025). However, even the AKI− group had a modest increase in Pol II-HMGCR binding (P < 0.025) compared with control urine chromatin samples (consistent with sepsis-induced activation of the HMGCR gene, as previously shown in experimental sepsis (7).
Figure 1.
Patients with AKI manifest increased levels of RNA polymerase II (Pol II) and of histone H3 lysine 4 trimethylation (H3K4m3) at exon 1 of HMG–CoA (HMGCR) gene in urine chromatin samples. Urine pellet samples from normal subjects, intensive care unit/acute kidney injury (ICU/AKI)+ patients, and ICU/AKI− patients were probed for Pol II and H3K4m3 at exon 1 of the HMGCR gene (ChIP assay; all results factored by amounts of Pol II and H3K4m3 at exon 1 of the house keeping gene β-actin). Increased Pol II levels were observed in both ICU cohorts, versus normal controls, but the levels were approximately fourfold greater in the AKI+ patients versus the AKI− controls. The AKI+ patients had a twofold increase in H3K4m3 levels at the HMGCR gene, whereas no increase was seen in the ICU/AKI− population. Thus, these data support the concept that AKI causes increased expression of the HMGCR gene. Values are presented as means ± 1 SEM.
In addition to increased AKI induced Pol II binding, a doubling of the gene-activating mark, H3K4m3, was observed at exon 1 of the HMGCR gene compared with that observed in either the control or AKI− patient urine samples (Figure 1, right panel; P < 0.03). Indeed, the H3K4m3 levels were essentially identical for the control and ICU / AKI− groups.
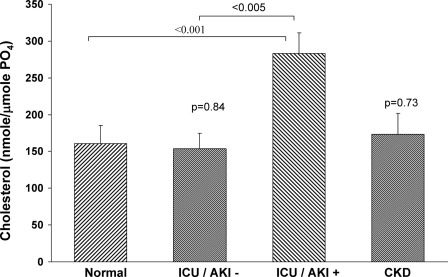
Urine Pellet Cholesterol Levels
As shown in Figure 2, the ICU/AKI– patient population had essentially the same urinary pellet cholesterol/phospholipid phosphate ratios to those observed in the control urine samples. Conversely, the ICU/AKI+ patients had an approximate doubling of pellet cholesterol levels (P < 0.005). The urine creatinine concentrations for the AKI− and AKI+ groups did not statistically differ (100 ± 16 mg/dl and 137 ± 26 mg/dl, respectively, P = 0.23). There was no significant relationship between the urine creatinine concentrations and the pellet cholesterol/phospholipid ratios in the AKI+ group (r = 0.14). This is consistent with the fact that creatinine excretion reflects GFR, whereas pellet cholesterol levels reflect tubular cell cholesterol loading and tubular cell membrane sloughing. Of note, however, the urine pellet cholesterol levels did significantly correlate with the serum creatinine concentrations (r = 0.5; P < 0.01), suggesting that it could potentially be a reflection of tubular injury severity.
Figure 2.
Urinary pellet cholesterol levels are elevated in patients with acute kidney injury (AKI) but not in critically ill intensive care unit (ICU) patients without AKI or in patients with chronic kidney disease (CKD). Urine samples from 15 normal volunteers, 15 ICU patients without AKI, 14 ICU patients with AKI, and 15 patients with CKD were assayed for urinary pellet cholesterol levels. The results were factored for lipid extract phospholipid phosphate levels. The AKI+ patients had an approximate doubling of pellet cholesterol levels, whereas the AKI− and CKD patients manifested normal levels (versus normal values).
As shown in Figure 2, the CKD patients did not manifest any increase in urinary pellet cholesterol content compared with control urine pellet values. Of interest, eight of the 15 CKD patients were receiving statin treatment, and yet their urinary pellet cholesterol levels were slightly, but not statistically, higher than values observed in non-statin-treated CKD patients (206 ± 40 versus 128 ± 34, respectively; P = 0.17).
Discussion
The results of this study provide clinical support for a sequence of events that has been noted in experimental studies of AKI, namely, that (1) acute tubular injury activates the HMGCR gene; (2) this results in increased cholesterol synthesis and proximal tubular cell cholesterol loading; and (3) upon release of tubular cells and tubular cell debris into the urinary space, increases in urinary pellet cholesterol content result. We have previously demonstrated that, unlike AKI, experimental chronic nephropathy does not activate these pathways (29). Thus, we hypothesized that an increase in urinary pellet cholesterol might have utility as an AKI biomarker.
To test these hypotheses, we sought evidence for increased HMGCR activity in patients with AKI by measuring degrees of RNA polymerase II binding to urinary chromatin fragments of the HMGCR gene. As shown in the left-hand panel of Figure 1, a marked increase in Pol II binding was observed in the AKI+ patients compared with that observed in either the control or ICU/AKI− urine samples. Because the degree of Pol II-gene binding correlates with rates of gene transcription, this finding provides clinical support for the experimental observation that AKI increases HMGCR gene activity. That a gene activating histone mark, H3K4m3, was also elevated at the HMGCR gene in the AKI+, but not in the AKI−, patient urine samples further supports the concept that AKI increases HMGCR gene transcription.
With this information in hand, we directly tested the hypothesis that an increase in urinary pellet cholesterol levels might be found in clinical AKI and that these values would be able to differentiate AKI versus critical illness without AKI, and versus CKD. As shown in Figure 2, this appears to be the case. Patients with AKI had an approximate doubling of urinary pellet cholesterol content compared with values observed in control urine samples. Conversely, critically ill patients without AKI manifested normal pellet cholesterol levels. Furthermore, urine pellet cholesterol values were normal in the patients with CKD. Noteworthy in regard to this latter finding is that many urinary protein AKI biomarkers, e.g., NGAL, KIM-1, and MCP-1, are typically elevated with both acute as well as chronic kidney disease (26–28). That pellet cholesterol levels were elevated in the AKI+, but not in the CKD, cohort suggests potential differential diagnostic utility in this regard.
Of note, statin therapy, which is common in patients with CKD, could theoretically be a confounding variable in interpreting urinary pellet cholesterol levels. However, we have previously demonstrated that statins do not alter renal cortical cholesterol content (8). Indeed, eight of the 15 CKD patients in the present study received statin therapy, and yet their urinary pellet cholesterol levels tended to somewhat higher (albeit nonsignificantly), not lower, than those found in the non-statin-treated CKD patients (see Results). Thus, it appears most unlikely that statin treatment would negate the potential utility of pellet cholesterol levels as a useful AKI biomarker.
Conclusions
In sum, these studies provide clinical support for a novel concept that has emerged from our experimental studies of AKI: that AKI activates the HMGCR/cholesterol axis and that, with release of tubular cells and tubular cell debris into urine, increases in urinary pellet cholesterol levels result. Particularly noteworthy in this regard are the following: (1) prior experimental data demonstrate that pellet cholesterol levels rise within 3 hours post-AKI induction, indicating potential utility in detecting early AKI; (2) pellet cholesterol levels remain normal with experimental prerenal azotemia; and (3) pellet cholesterol levels appear to be able to differentiate patients with acute versus chronic renal disease. Of note, the current emphasis in AKI biomarker research is to develop a panel of biomarkers that reflect differing injury-induced pathways. Thus, the addition of a lipid biomarker to a variety of urinary protein biomarkers might be quite useful in this regard. It is premature to draw conclusions as to the clinical utility of measuring urinary pellet cholesterol levels. Clearly, this will require a large prospective clinical trial to assess. However, this study does provide clinical support for conclusions derived from our previous experimental AKI studies, i.e., that AKI activates the HMG–CoA reductase gene and that renal tubular cholesterol loading results. Whether these “bench to bedside” observations will ultimately find clinical application, either in terms of deploying a new biomarker or in terms of better understanding AKI pathogenesis, remains to be defined.
Disclosures
None.
Acknowledgments
We thank Mr. John Ruzinski and Mr. Ernie Ayers, Kidney Research Institute, Seattle; Ms. Nancy Wickersham, Vanderbilt University; and Ms. Jill Corson, Puget Sound Blood Center, Seattle, for their assistance with acquiring test urine samples. We also thank Ms. Kirsten Becker for her technical assistance. This work was supported by grants from the National Institutes of Health (DK384342; R21-DK083315; HL081332; HL-103836; DK082192, and HL 070938), and from nonrestricted research funds from the Kidney Research Institute, Seattle.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1. Zager RA, Burkhart KM, Johnson A, Sacks B: Increased proximal tubular cholesterol content: Implications for cell injury and the emergence of “acquired cytoresistance.” Kidney Int 56: 1788–1797, 1999 [DOI] [PubMed] [Google Scholar]
- 2. Zager RA: Plasma membrane cholesterol: A critical determinant of cellular energetics and tubular resistance to attack. Kidney Int 58: 193–205, 2000 [DOI] [PubMed] [Google Scholar]
- 3. Zager RA, Kalhorn T: Changes in free and esterified cholesterol: Hallmarks of acute tubular injury and acquired cytoresistance. Am J Pathol 157: 1007–1016, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zager RA, Johnson A, Anderson K, Wright S: Cholesterol ester accumulation: An immediate consequence of acute ischemic renal injury. Kidney Int 59: 1750–1761, 2001 [DOI] [PubMed] [Google Scholar]
- 5. Zager RA: P glycoprotein-mediated cholesterol cycling: A potentially important determinant of proximal tubular cell viability. Kidney Int 60: 944–956, 2001 [DOI] [PubMed] [Google Scholar]
- 6. Zager RA, Andoh T, Bennett WM: Renal cholesterol accumulation: A durable response following acute and subacute renal insults. Am J Pathol 159: 743–752, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zager RA, Johnson AC: Renal cortical cholesterol accumulation: An integral component of the systemic stress response. Kidney Int 60: 2229–2310, 2001 [DOI] [PubMed] [Google Scholar]
- 8. Zager RA, Shah VO, Shah HV, Zager PG, Johnson ACM, Hanson S: The mevalonate pathway during acute tubular injury: Selected determinants and consequences. Am J Pathol 161: 681–692, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zager RA, Johnson ACM, Hanson SY: Proximal tubular cholesterol loading following mitochondrial, but not glycolytic blockade. Am J Physiol: 285: F1092–F1099, 2003 [DOI] [PubMed] [Google Scholar]
- 10. Naito M, Bomstzyk K, Zager RA: Renal ischemia- induced cholesterol loading: Transcription factor recruitment and chromatin remodeling along the HMG CoA reductase gene. Am J Pathol 174: 54–62, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gaudio KM, Thulin G, Mann A, Kashgarian M, Siegel NJ: Role of heat stress response in the tolerance of immature renal tubules to anoxia. Am J Physiol 274: F1029–F1036, 1998 [DOI] [PubMed] [Google Scholar]
- 12. Van Why SK, Siegel NJ: Heat shock proteins in renal injury and recovery. Curr Opin Nephrol Hypertens 7: 407–412, 1998 [DOI] [PubMed] [Google Scholar]
- 13. Venkatachalam MA, Bernard DB, Donohoe JF, Levinsky NG: Ischemic damage and repair in the rat proximal tubule: Differences among the S1, S2, and S3 segments. Kidney Int 14: 31–49, 1978 [DOI] [PubMed] [Google Scholar]
- 14. Donohoe JF, Venkatachalam MA, Bernard DB, Levinsky NG: Tubular leakage and obstruction after renal ischemia: Structural-functional correlations. Kidney Int 13: 208–222, 1978 [DOI] [PubMed] [Google Scholar]
- 15. Racusen LC, Fivush BA, Li YL, Slatnik I, Solez K: Dissociation of tubular cell detachment and tubular cell death in clinical and experimental “acute tubular necrosis.” Lab Invest 64: 546–556, 1991 [PubMed] [Google Scholar]
- 16. Racusen LC: Epithelial cell shedding in acute renal injury. Clin Exp Pharmacol Physiol 25: 273–275, 1998 [DOI] [PubMed] [Google Scholar]
- 17. Nath KA, Balla G, Vercellotti GM, Balla J, Jacob HS, Levitt MD, Rosenberg ME: Induction of heme oxygenase is a rapid, protective response in rhabdomyolysis in the rat. J Clin Invest 90: 267–270, 1992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nath KA, Croatt AJ, Haggard JJ, Grande JP: Renal response to repetitive exposure to heme proteins: Chronic injury induced by an acute insult. Kidney Int 57: 2423–2433, 2000 [DOI] [PubMed] [Google Scholar]
- 19. Kellerman PS: Exogenous adenosine triphosphate (ATP) preserves proximal tubule microfilament structure and function in vivo in a maleic acid model of ATP depletion. J Clin Invest 92: 1940–1949, 1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zager RA, Johnson ACM, Naito M, Bomsztyk K: Maleate nephrotoxicity: Mechanisms of injury and correlates with ischemic/hypoxic tubular cell death. Am J Physiol 294: F187–F197, 2008 [DOI] [PubMed] [Google Scholar]
- 21. Stirewalt DL, Appelbaum FR, Willman CL, Zager RA, Banker DE: Mevastatin can increase toxicity in primary AMLs exposed to standard therapeutic agents, but statin efficacy is not simply associated with ras hotspot mutations or overexpression. Leuk Res 27: 133–145, 2003 [DOI] [PubMed] [Google Scholar]
- 22. Li HY, Appelbaum FR, Willman CL, Zager RA, Banker DE: Cholesterol-modulating agents kill acute myeloid leukemia cells and sensitize them to therapeutics by blocking adaptive cholesterol responses. Blood 101: 3628–3634, 2003 [DOI] [PubMed] [Google Scholar]
- 23. Ware LB, Johnson AC, Zager RA: Renal cortical albumin gene induction and urinary albumin excretion in responses to acute kidney injury. Am J Physiol Renal Physiol 300: F628–F638, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Siew ED, Ware LB, Gebretsadik T, Shintani A, Moons KG, Wickersham N, Bossert F, Ikizler TA: Urine neutrophil gelatinase-associated lipocalin moderately predicts acute kidney injury in critically ill adults. J Am Soc Nephrol 20: 1823–1832, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Munshi R, Johnson A, Siew ED, Ikizler TA, Ware LB, Wurfel MM, Himmelfarb J, Zager RA: MCP-1 gene activation marks acute kidney injury. J Am Soc Nephrol 22: 165–175, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Devarajan P: The use of targeted biomarkers for chronic kidney disease. Adv Chronic Kidney Dis 17: 469–479, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Perico N, Cattanio D, Remuzzi G: Kidney injury molecule 1: In search of biomarkers of chronic tubulointerstitial damage and disease progression. Am J Kidney Dis 53: 1–4, 2009 [DOI] [PubMed] [Google Scholar]
- 28. Rovin BH, Song H, Birmingham DJ, Hebert LA, Yu CY, Nagaraja HN: Urine chemokines as biomarkers of human systemic lupus erythematosus activity. J Am Soc Nephrol 16: 467–473, 2005 [DOI] [PubMed] [Google Scholar]
- 29. Johnson AC, Yabu JM, Hanson S, Shah VO, Zager RA: Experimental glomerulopathy alters renal cortical cholesterol, SR-B1, ABCA1, and HMG CoA reductase expression. Am J Pathol 162: 283–291, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kornberg RD: The molecular basis of eukaryotic transcription. Proc Natl Acad Sci U S A 104: 12955–12961, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nikolov DB, Burley SK: RNA polymerase II transcription initiation: A structural view. Proc Natl Acad Sci U S A 94: 15–22, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ricci Z, Cruz DN, Ronco C: Classification and staging of acute kidney injury: beyond the RIFLE and AKIN criteria. Nature Reviews Nephrology 7: 201–208, 2011 [DOI] [PubMed] [Google Scholar]