Abstract
Objective
This study evaluated how well women from diverse race/ethnic groups were able to take a quantitative cancer risk statistic verbally provided to them and report it in a visual format.
Methods
Cross-sectional survey was administered in English, Spanish or Chinese, to women aged 50 to 80 (n=1,160), recruited from primary care practices. The survey contained breast, colorectal or cervical cancer questions regarding screening and prevention. Women were told cancer-specific lifetime risk then shown a visual display of risk and asked to indicate the specific lifetime risk. Correct indication of risk was the main outcome.
Results
Correct responses on icon arrays were 46% for breast, 55% for colon, and 44% for cervical; only 25% correctly responded to a magnifying glass graphic. Compared to Whites, African American and Latina women were significantly less likely to use the icon arrays correctly. Higher education and higher numeracy were associated with correct responses. Lower education was associated with lower numeracy.
Conclusions
Race/Ethnic differences were associated with women’s ability to take a quantitative cancer risk statistic verbally provided to them and report it in a visual format.
Practice Implications
Systematically considering the complexity of intersecting factors such as race/ethnicity, educational level, poverty, and numeracy in most health communications is needed. (200)
Keywords: risk communication, cancer screening, cancer prevention, ethnic disparities, numeracy, decision making
1. Introduction
Shared decision-making (SDM) has become the “gold standard” [1-3] in delivering patient-centered care [4], particularly in the setting of therapeutic interventions. [5] Effective shared decision-making is complex, dependent on communication skills of the clinician and patient, and the relationship between both of these parties. Clinicians engaging in SDM need to consider both communication issues (e.g., eliciting and offering more information, feelings, and beliefs, reaching explicit closure) and relational issues (e.g. asking patients how they feel about the decision-making process, giving patients permission to reveal any concerns or disagreements about the decision). [6]
Engaging in SDM in the area of cancer risk requires attention to communication and assessment by the clinician as to the patient’s understanding of the risks and benefits of screening, regardless of the relationship, mutual trust and race/ethnicity and gender concordance. [7] An understanding of cancer risk can be affected by both patients’ literacy and numeracy skills. [8] During patient-clinician discussions involving cancer prevention, SDM requires numeracy skills and in turn these skills can have a significant impact on receiving effective health care. [9]
Discussion of cancer screening relies mainly on the clinician’s verbal communication and available printed information. Numerous studies have shown that verbal communication by itself is an ineffective method to present information to patients [8, 10, 11] therefore, utilization of visual displays is used to enhance communication about risk in order to facilitate shared decision-making about screening tests [12] and to assist in processing numerical information [13]. In communicating breast cancer risk, an icon array of female stick figures has been used to illustrate the proportion of women to be diagnosed. For uncommon cancers a log-linear scale using a graphical magnifying glass has been developed [14] for these situations. [15]
Examination of patients’ ability to understand visual displays and how this is affected by numeracy in the area of cancer prevention remains mostly unknown. [8] However, more recent work has shown that those who speak English as a second language may need both numerical and graphical information in communicating medical risks relevant to shared decision-making situations;[16] other analyses of this study have shown differences in perceived risk of cancer by race/ethnicity. [17-19] For example, compared to White women, Latinas had higher perceived risk, whereas Asian women had lower, for cervical and colon cancer after multivariate adjustment. Yet, it is unknown how women from diverse ethnic backgrounds understand visual displays of cancer risk information after accounting for levels of education and numeracy. The purpose of this analysis was to examine whether different visuals displays were useful in assisting ethnically diverse women identify the risk of getting breast, colorectal, or cervical cancer.
2. Methods
2.1 Setting and Participants
Women were recruited from primary care practices at the University of California (UCSF) Medical Center and at community-based clinics. Women were screened by telephone and then invited for face-to-face interviews. Eligibility criteria were: ages 50 to 80 years; ability to speak English, Spanish, or Chinese (Mandarin or Cantonese); self-identified race/ethnicity of African American, Asian, Latina, or non-Latina White (hereafter White); and at least one clinic visit in the previous two years. Women with current cancer or with cognitive impairment, as identified by their physicians, were excluded. All study measures and scripts were translated into Spanish and Chinese using standard forward-backward methods [20] and administered by bicultural and bilingual research assistants in the appropriate language.
2.2 Study Procedures
We obtained permission from primary clinicians to contact their patients by mail from a list of potentially eligible women based on administrative data. For women who did not respond within two weeks, a trained interviewer called, and with verbal consent, completed the baseline survey. Because of limited success in recruiting Chinese-speaking women by telephone, in-person recruitment methods were used at a community-based Chinatown clinic. We aimed to recruit similar numbers of women by race/ethnicity. Women received $20 at the end of the interview. Institutional Review Boards at UCSF and collaborating sites approved this study.
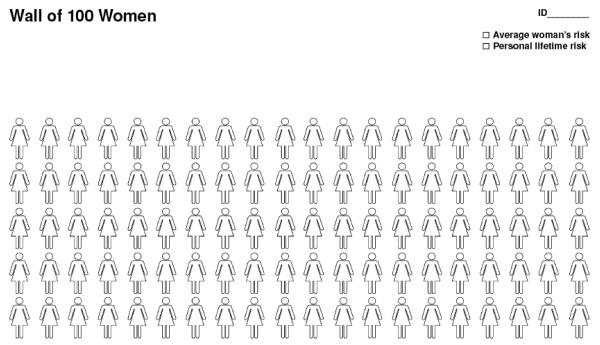
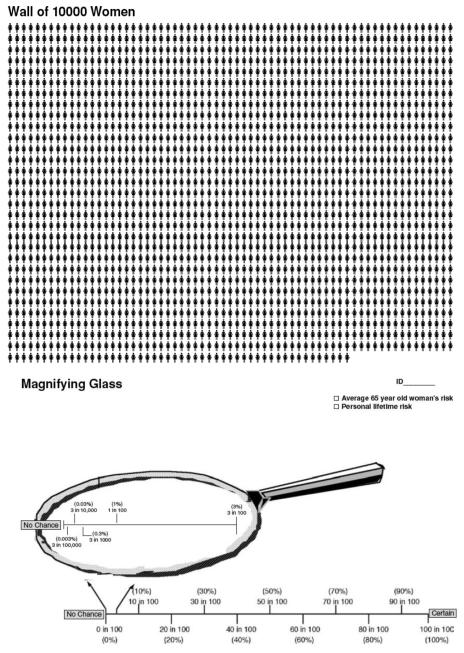
Versions of the survey were developed for each cancer site. Women aged 50-65 years were randomly administered either the breast or colorectal cancer survey that contained the visual icon array of the “wall of 100 women” shown in Figure 1. Those ≥65 years were administered the cervical cancer survey if they had an intact uterus, or if not, were randomly assigned to breast or colorectal survey. Only women aged 65 years and older answered the questions related to risk perceptions about cervical cancer screening since at least two groups, the US Preventive Services Task Force (USPSTF) and the American Cancer Society (ACS) have recommendations that actively discourage women in this age category to continue Pap testing if they have had prior normal Pap testing and who are not otherwise at high risk for cervical cancer.[21] Women answering the cervical cancer survey were administered two visuals, “the wall of 10,000 women” and the “magnifying glass” (Figure 2)
Figure 1.
Wall of 100 Women Scenario for Breast and Colon Cancer Risk
Figure 2.
Wall of 10,000 Women (Five of these Pictures put together)
2.3 Measures and Outcomes
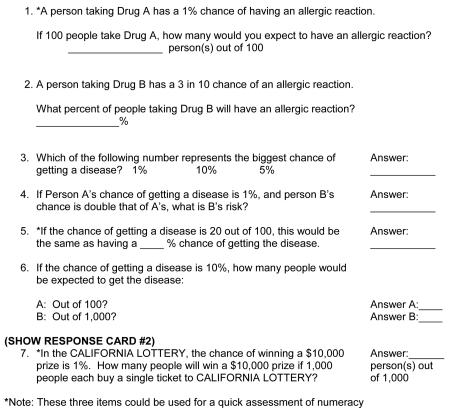
The survey questions were derived from the results obtained through focus groups [22] simultaneously developed in three languages, pre-tested using cognitive interviewing methods [23] in each of the ethnic groups, and then modified. Demographic characteristics included age, years of education, household income, marital status, and employment. Personal or family history of cancer, health status as measured by the SF-12v2, [24] and health insurance coverage were collected. An 8-item numeracy measure to assess how well participants: (a) perform simple arithmetic operations on risk magnitude using percentages and proportions and (b) convert numbers to percentages, proportions to percentages, and probabilities to proportions was administered. This measure was adapted from a published scale and modified items from Lipkus [5, 13] (Appendix 1).
Prior to asking women to use the icon array or magnifying glass graphic to translate the risk of getting cancer, they were shown either the icon array, “wall of 100 women” (for those filling out breast or colon) or the icon array, “wall of 10,000 women” and magnifying glass graphic (for those filling out cervical). Two examples were used to orient women on how the verbal translation of risk was depicted on the icon array or the graphic. The examples were: 1) the chance of being killed by an earthquake and 2) receiving junk mail. Women were asked whether they understood the information presented in the visual; more explanation (in a standardized format) was given, if necessary (<1% of the sample required this). For the icon array of the ‘wall of 100 women,’ participants were then told, “Each woman represents 1 chance in 100 that something will happen. Roughly, 13% (or 6%) of women will develop breast (or colorectal) cancer in their lifetime. This also means that an average woman has a 13% (or 6%) chance of developing breast (or colon) cancer in her lifetime. Please circle how many chances out of 100 would be an average woman’s chance of developing (breast or colon) cancer over her lifetime.” (Figure 1) Women were shown how the percentages would be marked using the visuals before they were asked to mark them.
Women who were administered the cervical cancer survey were also given similar orientations to the icon array of a “wall of 10,000 women” (Figure 2) and a “magnifying glass” graphic (Figure 2).[14] Women were asked, “Using this (wall of 10,000 women/magnifying glass) picture can you mark where 3 in 10,000 is? This is the average 65-year old woman’s risk for getting cervical cancer during the rest of her life if she has had 3 or more normal Pap tests.”
Respondents who circled the correct number of icons in the visual (breast: 13 out of 100, colon: 6 out of 100, and cervical: 3 out of 10,000) were coded as having correctly completed the task. For the magnifying task the correct answer was also 3 out of 10,000. We also examined an outcome describing women’s perceived ease of using the visual aids: after completing the corresponding task and regardless of whether they correctly completed the task, participants were asked, “How easy was the wall of women/magnifying glass to use?” The response choices were, “very easy,” “easy,” “hard,” “very hard.” For ease of interpretation, the variable was dichotomized to “very easy/easy” versus “very hard/hard.”
2.4 Statistical Analysis
Race/ethnic group differences in the measures of interest and demographic characteristics were tested by chi-square or t-tests. Using logistic regression, we first examined the relationship between the participants’ ability to correctly complete each of the “wall of women” visual tasks, for the total sample and by cancer sites (breast and colon; cervical), with numeracy and race/ethnicity. Covariates in the model included race/ethnicity, age (per year), education, employment, income level, personal and family history of cancer, health status, numeracy score, cancer scenario, and perceived ease of use of visual display. For most variables there was less than 1% of missing data, with the exception of income, which had 20% missing data. No regression modeled the accuracy of responses to the magnifying glass task because of the overall low number of correct responses. Second, we examined the relationship between race/ethnicity and numeracy using multivariate linear regression in the sub-sample of participants correctly answering the wall of women visuals separately by cancer site (breast and colon; cervical). To account for missing data, each regression model was fit to 20 multiple imputed data sets created using SAS PROC MI [25]. Because PROC MI assumes a multivariate normal distribution, imputed values for binary variables were subsequently rounded to the nearest applicable integer. [26, 27] All parameter estimates and significance tests were calculated by combining results across the imputed data sets. [28, 29] All analyses were conducted using SAS 9.1.3. [25]
3. Results
Of 4,523 letters sent, 906 (20%) of the women were unreachable due to incorrect contact information and 871 (19%) were ineligible due to language, race/ethnicity, illness, or having changed physicians. Of the 2,746 eligible women contacted, 1,319 (48%) completed the baseline screening, 157 declined to participate and two were found ineligible for a final sample of 1,160.
Table 1 shows the characteristics of the sample stratified by race/ethnicity. There were significant differences by race/ethnicity for all variables shown with White women generally having higher income, more private health insurance, and better measure of physical functioning (each difference, p < .001). Race/ethnic minority women had significantly less formal education, especially Latinas and Chinese, and lower numeracy scores with differences ranging from 1.7 for Other Asians to 3.7 for Latinas.
Table 1. Characteristics of 1160 Women Answering Visual Displays of Breast, Colon, and Cervical Cancer Risk, San Francisco Primary Care Clinical Sites, 2004-2006.
| White (n=338) |
African American (n=167) |
Chinese (n=353) |
Latino (n=239) |
Other Asian (n=63) |
|
|---|---|---|---|---|---|
| Variable | |||||
| Age*, years | |||||
| Mean (SD) | 60.7(1.7) | 60.8(1.7) | 60.6(1.6) | 63.6(2.0) | 63.5(2.0) |
| Education *** (%) | |||||
| ≤ high school | 5.6 | 37.1 | 82.2 | 71.4 | 15.9 |
| some college | 26.1 | 35.3 | 6.5 | 17.6 | 20.6 |
| ≥ college | 68.3 | 27.5 | 11.3 | 11.0 | 63.5 |
| Married*** (%) | 52.0 | 30.0 | 73.1 | 38.7 | 57.1 |
| Employment *** (%) | |||||
| Unemployed | 8.5 | 10.9 | 37.6 | 14.8 | 9.7 |
| Disabled | 9.0 | 30.3 | 8.9 | 21.1 | 4.8 |
| Retired | 31.0 | 28.5 | 29.2 | 46.2 | 46.2 |
| Employed | 51.8 | 30.3 | 24.3 | 29.9 | 39.3 |
| Income*** (%) | |||||
| ≤$20,000 | 20.3 | 45.2 | 67.8 | 65.6 | 21.1 |
| $20,001-$50,000 | 22.0 | 29.0 | 21.5 | 22.8 | 29.7 |
| ≥$50,000 | 57.7 | 25.8 | 10.7 | 11.6 | 49.2 |
| Health Insurance*** | |||||
| No insurance | 3.4 | 6.6 | 44.6 | 18.4 | 1.8 |
| Public | 20.8 | 42.0 | 31.5 | 46.0 | 19.3 |
| Private | 75.8 | 51.4 | 23.9 | 34.6 | 78.9 |
| History of Cancer*** (%) | |||||
| No | 74.0 | 81.4 | 92.2 | 79.9 | 78.9 |
| History of Family Cancer*** (%) | |||||
| No | 44.4 | 43.7 | 79.3 | 59.4 | 52.4 |
| Health Status (0-100) | |||||
| Mental Health Functioning* | |||||
| Mean (SD) | 50.0(9.4) | 48.6(12.1) | 49.3(13.2) | 46.1(13.2) | 50.3(8.3) |
| Physical Health Functioning*** | |||||
| Mean (SD) | 47.6(11.5) | 38.9(12.4) | 39.0(11.6) | 41.2(10.7) | 44.3(9.7) |
| Numeracy Score (0-8)*** | |||||
| Mean (SE) | 6.2(0.4) | 3.4(0.5) | 3.6(0.6) | 2.5(0.4) | 4.5(0.5) |
Note.
p<.05
p<.001
Correct Responses to Visual Display Task
Table 2 shows the percent of women who answered the visual display tasks correctly by cancer scenario and race/ethnicity. The icon array of the “wall of 100 women” for the breast and colon cancer surveys was administered to 912 participants. The percentage of women who circled the correct number of icons in this visual ranged from 46% for breast cancer risk to 55% for colon cancer risk. Race/ethnic minority women had significantly lower proportion of correct responses compared to their White counterparts. These were large differences with fewer than half correct responses for the Breast Cancer scenario for African American, Chinese and Latina women.
Table 2. Number and percent of women who answered visual display task correctly by cancer scenario and stratified by race/ethnicity, San Francisco Primary Care Clinical Sites, 2004-2006.
| Breast/Colon Cancer Scenario: |
Total N (% Correct) |
White (% Correct) |
African American (% Correct) |
Chinese (% Correct) |
Latino (% Correct) |
Other Asian (% Correct) |
|---|---|---|---|---|---|---|
|
Wall of 100 women |
||||||
| Breast | 420 (46%) | 121 (80%) | 61 (32%)*** | 124 (35%)*** | 87 (24%)*** | 27 (57%)* |
| Colon | 492 (55%) | 153 (86%) | 77 (37%)*** | 140 (48%)*** | 105 (32%)*** | 17 (55%)** |
|
Cervical Cancer Scenario |
||||||
|
Wall of 10,000 women |
248 (44%) | 64 (67%) | 29 (36%)* | 89 (41%)** | 47 (16%)*** | 19 (62%) |
| Magnifying | 248 (13%) | 64 (22%) | 29 (6%) | 89 (7%) | 47 (17%) | 19 (17%) |
| glass | 25% | 53% | 17% | 13% | 8% | 42% |
The remaining 248 women were administered both the icon array of the “wall of 10,000 women” and the graphic magnifying glass visuals corresponding to risk of cervical cancer. Only 25% of women who were administered the cervical cancer survey correctly responded to the magnifying glass task and no significant differences were found by race/ethnicity groups. Similar results were found for the correct responses to the Wall of 10,000 women with significantly fewer correct responses for African Americans, Chinese and Latina women.
The “wall of 100 women” was rated the easiest to use among the two icon arrays and graphic; most Whites (92%), Chinese (92%), Other Asians (80%), Latinas (75%) and African Americans (72%) reported it was easy to use. The magnifying glass visual was rated as the second easiest to use by 81% of Whites, 72% of Other Asians, 66% of Latinas, 61% of African Americans, and 55% of Chinese women. Half of the participants (52%) completing the cervical cancer visual rated the “wall of 10,000 women” easy to use. There was poor concordance between women’s rated ease of use and correct completion of the icon arrays and graphic (data not shown). For example, in the “wall of 100 women”, 92% of both White and Chinese women reported this icon array was easy to use. Yet, 87% of White women answered correctly and less than half (42%) of Chinese women answered correctly. About three-quarters (76%) of Latina participants reported that the “wall of 100 women” was easy to use, but only a third (32%) answered correctly. Among 76% of African American women reporting ease of use, 42% answered correctly. Of the 90% of women who reported the “wall of 10,000 women” easy to use, 67% answered correctly.
Predictors of Correct Responses to Visual Display Tasks
The first set of regression models examined the effects of race/ethnicity after adjusting for all covariates on three different “wall of women” visual task outcomes: Three combined “wall of women scenarios”, “wall of 100 women scenarios” for breast and colon cancer, and “wall of 10,000 women scenario” for cervical cancer (Table 3). In the overall model, African American and Latino women were significantly less likely to translate the verbal provision of cancer risk to a visual format correctly, compared to Whites. Those with less than a high school education were less likely to use the icon arrays correctly but women who had a higher numeracy score or reported the icon arrays easier to use were more likely to use them correctly.
Table 3. Logistic regression models of correct/incorrect use of wall of women visuals, San Francisco Primary Care Clinical Sites, 2004-2006.
| Total wall of women: Breast, Colon, and Cervical Scenarios |
Wall of 100 women: Breast or Colon Scenarios |
Wall of 10,000 women: Cervical Scenario |
|
|---|---|---|---|
| Variable | Odds Ratio (95% CI) | Odds Ratio (95% CI) | Odds Ratio (95% CI) |
| Age (per year) | 1.00 (0.98-1.03) | 1.00 (0.96-1.03) | 1.07 (0.97-1.17) |
| Ethnicity (White-ref) | |||
| African American | 0.36(0.22-0.61)** | 0.30(0.17-0.54)*** | 0.62(0.18-2.11) |
| Chinese | 0.68(0.41-1.13) | 0.49(0.27-0.89)* | 1.54(0.55-4.31) |
| Latino | 0.36(0.22-0.60)*** | 0.34(0.19-0.61)** | 0.25(0.07-0.83)* |
| Other Asian | 0.63(0.33-1.20) | 0.48(0.21-1.06) | 1.04(0.29-3.66) |
| Education (≥ college, ref) | |||
| Less than, equal to High school | 0.68 (0.51-0.90)** | 0.44 (0.25-0.78)* | 0.52 (0.16-1.69) |
| Some college | 0.92 (0.71-1.17) | 0.56 (0.34-0.91)* | 0.64 (0.25-1.64) |
| Employment (Employed, ref) | |||
| Unemployed | 0.55(0.35-0.86)* | 0.57(0.36-0.92)* | 0.91(0.12-6.81) |
| Disabled | 0.91(0.53-1.58) | 0.89(0.49-1.60) | 0.68(0.07-6.75) |
| Retired | 0.72(0.44-1.16) | 0.73(0.41-1.30) | 0.62(0.19-1.98) |
| Annual Income (>$50,000, ref) | |||
| $20,000 or less | 0.82(0.51-1.34) | 0.71(0.41-1.24) | 1.67(0.51-5.38) |
| $20,001-$50,000 | 0.82(0.49-1.34) | 0.72(0.41-1.27) | 1.49(0.47-4.67) |
| History of Cancer | |||
| No | 0.74(0.50-1.11) | 0.69(0.43-1.10) | 1.04(0.43-2.51) |
| History of Family Cancer | |||
| No | 1.20(0.87-1.64) | 1.36(0.95-1.95) | 0.79(0.36-1.75) |
| Health Status (SF-36) | |||
| Mental Health Function | 1.00(0.91-1.08) | 1.03(0.93-1.14) | 0.94(0.75-1.16) |
| Physical Health Function | 1.09(0.96-1.24) | 1.02(0.88-1.18) | 1.35 (1.03-1.76)* |
| Numeracy Score | 1.30 (1.21-1.40)*** | 1.29(1.18-1.41)*** | 1.37(1.15-1.64)** |
| Perceived Ease of Use | |||
| Easy/very easy | 2.09 (1.38-3.17)** | 2.31(1.36-3.92)** | 1.96(0.93-4.12) |
Note. All final data were imputed.
p<.05
p<.01
p<.001
CI indicates confidence interval.
Covariates in the model include scenario presented, ethnicity, age (per year), education, employment, income level, personal and family history of cancer, health status, numeracy score (one-point increase) and perceived use of visual display.
Among the participants who completed the “wall of 100 women” task, African American, Chinese, and Latino women were significantly less likely to translate the verbal provision of cancer risk to a visual format correctly, compared to Whites. In this model, women with less than high school education or even high school graduates were less likely to use this icon array correctly compared to those with some college or more. Correct risk translation to the visual format was more likely among women with a higher numeracy score or who rated this visual display task easy to use. Among those who completed the “wall of 10,000 women” task, only Latinas were significantly less likely to use the visual correctly, compared to Whites. Women who had a higher numeracy score were again significantly more likely to use this visual display correctly.
Correlates of Numeracy
Because numeracy was significantly associated with correct responses on “wall of women” outcomes, in addition to the independent association of race/ethnicity, we examined correlates of numeracy. Table 4 presents results of linear models regressing numeracy scores onto race/ethnicity after controlling for age, education, occupational status, and income. Compared to Whites, women from other race/ethnic backgrounds had significantly lower numeracy scores. In the total sample, average numeracy scores of race/ethnic groups ranged from 0.51 to 1.72 points lower than that of Whites (out of a possible total of 8 points). Similar findings were noted among the women who were administered the “wall of 100 women” visual display task. Among those administered the “wall of 10,000 women” task, only African American (1.62 points) and other Asian (1.04 points) women’s average numeracy scores were significantly lower than that for Whites. Across all regression models, less than high school education and even high school graduates were significantly associated with lower numeracy ranging from 0.71 to 3.10 points. Similar but smaller differences were found by income.
Table 4. Correlates of Numeracy in 1160 Women, San Francisco Primary Care Clinical Sites, 2004-2006.
| Total Wall of women: Breast, Colon, and Cervical Scenarios |
Wall of 100 women: Breast/Colon Scenarios |
Numeracy among Wall of 10,000 women: Cervical Scenario |
|
|---|---|---|---|
| Variable | B(SE) | B(SE) | B (SE) |
| Age | −0.02(0.01)* | −0.02 (0.01) | −0.05 (0.03) |
| Ethnicity (White-ref) | |||
| African American | −1.72(0.20)*** | −1.74 (0.22)*** | −1.62(0.46)** |
| Chinese | −0.51(0.19)* | −0.51 (0.22)* | −0.44(0.40) |
| Latino | −1.72(0.20)*** | −1.95 (0.22)*** | −0.70 (0.45) |
| Other Asian | −1.42(0.27)*** | −1.60 (0.31)*** | −1.04 (0.53)* |
| Education (> high school, ref) | |||
| < high school | −2.32(0.19)*** | −2.12 (0.22)*** | −3.10 (0.40)*** |
| high school | −0.80(0.17)*** | −0.71 (0.19)** | −1.05 (0.38)* |
| Employment (Employed, ref) | |||
| Unemployed | 0.09(0.18) | 0.10 (0.19) | −0.93 (0.59) |
| Disabled | −0.12(0.20) | −0.14 (0.21) | −0.35 (0.68) |
| Retired | 0.07(0.18) | 0.10 (0.22) | −0.07 (0.42) |
| Income (>$50,000, ref) | |||
| ≤$20,000 | −1.06(0.20)*** | −1.06 (0.22)*** | −1.00 (0.44)* |
| $20,001-$50,000 | −0.72(0.19)*** | −0.73 (0.20)** | −0.74 (0.42) |
Note. All final data are imputed.
p<.05
p<.01
p<.001
4. Discussion and Conclusion
4.1 Discussion
The goal of this study was to evaluate how well women from diverse race/ethnic groups were able to take a quantitative cancer risk statistic verbally provided to them and report it in a visual format using either an icon array or a graphic of a magnifying glass. While there has been increasingly widespread use of probabilistic information in health communication in numeric and visual formats,[5] the results from this study adds new information on the use of graphic formats to communicate cancer risk to women from diverse race/ethnic backgrounds. The observation that minority women, particularly African American and Latino, were significantly less likely to correctly circle the number of icons that representing lifetime risk of getting cancer (breast, colon, or cervical), even after adjusting for formal education and numeracy, was striking.
We offer several explanations for this finding. First, it could be that African American and Chinese (“wall of 100 women” only) and Latino women do not understand the number provided. Yet, when the women were first oriented to how the visuals represented a quantitative risk, few asked for further explanation, and all participants indicated they understood both the number and the visual. Indeed, those who had a higher numeracy score were more likely to circle the correct number of icons. Second, these same minority women may not have understood the graphic(s) presented. Even though other research has shown that large improvements in accuracy of comprehension can be achieved in using both visual aids such as icon arrays and numerical information, the race/ethnicity of the US sample in that study was not reported. [30] Third, it could be that these women were unable to translate the verbal information into the appropriate marks on the graphic. Fourth, the substantial ethnic differences may be due to the fact that exposure to these types of health risk depictions or exposure to health information in general differs by race/ethnicity. Adjustment for education and numeracy may not have adequately addressed this difference; in addition, we do not have a measure of prior media exposure or familiarity with graphic presentation of information. Finally, it could be that women from diverse backgrounds may consider the risk of cancer to be pre-determined or as a qualitative event and therefore do not conceptualize cancer risk in similar ways to Whites.
Although there has been past work completed examining numeracy and graphical literacy in “cross-cultural studies”, those samples were presumably predominantly White men and women from the US, Germany and Polish immigrants to the United Kingdom [31, 32]. This study is the only one to conduct analyses of risk translation by race/ethnic groups in the US with adjustments for formal education and numeracy. However, our study should be interpreted with caution. Instructions for the numeracy scale could have affected the women’s ability to provide the correct answer. Respondents could have ignored the instructions and believed they were in a test situation feeling evaluated or heeded the instructions and put little effort into obtaining the correct answers because there was no consequence of having wrong information. Additionally, we used average lifetime risk estimates independent of the participant’s age, rather than risk estimates based on remaining expected life expectancy. Although this may be a subtle difference, it may have affected participants’ understanding of the risk information and led to incorrect responses. The fact that age was not a significant predictor in the regression analyses is reassuring that this would not explain our results.
This was a cross-sectional study and does not track decision-making in real-time cancer screening decisions. We asked participants to learn a quantitative fact verbally and then transcribe this on the visual display. Completion of this task varied significantly by race/ethnicity, educational level and numeracy. The extent to which the distribution in numeracy scores applies to others is unknown since low numeracy is common among primary care patients, ranging from 66% [33] to 84% [34]. Although some recent work with Swiss participants has shown that people with low numeracy do not rely on numbers even when displayed in a graphic form [35], clearly, more work is needed in examining risk translation and graphical literacy in the area of cancer and amongst diverse ethnic groups.
This study is unique in that we asked participants to move beyond examining a visual aide to translating their knowledge of cancer risk from a verbal format to a visual one. Although it could be argued that there is little need for patients to translate verbal information to a visual format, health educational theory posits that 90% of information can be retained by “hearing, seeing, talking, and doing” compared to retaining only 50% of information from “hearing and seeing.” [36] That we found poor concordance between women’s ratings in ease of use and circling the correct number of icons or correctly using the magnifying glass graphic could suggest that there is a need to elicit accuracy of understanding, especially within the context of cancer risk prevention and treatment decision-making. Importantly, having individuals report that a visual aid is easy to use but then provide an incorrect response to a knowledge translation of cancer risk task suggests a lack of comprehension at some stages of task completion.
It is well known that many people have challenges grasping numerical concepts even with the additional benefits of using one or more visual aids [30, 37, 38] or using a sequentially ordered presentation of visual aids. [39] Our results suggest that more work is needed in the facilitation of translating small risks (e.g. cervical cancer risk) from a verbal to a visual format. Although age was not significantly associated with circling the icons on the “wall of 10,000” women, it could be that use of a graphic such as the “magnifying glass” is more challenging as age increases over 65 years due to visual impairments.
These results suggest that race/ethnic minority women, in particular, may appear to understand treatment risk or screening benefits but in fact have more difficulty than their White counterparts. In part, this could be due to their lower numeracy and the intersecting effects of lower educational attainment, more poverty, and perceived discrimination (not measured in this study). What is concerning is that race/ethnic minority patients’ numeracy, in particular, can affect their ability to be involved in shared decision-making and understanding of cancer screening and treatment options, even if cancer risk information is discussed using both numerical formats and visual aids.
4.2 Conclusion
Women with low numeracy scores can have difficulty responding correctly to the visual display tasks, consistent with other studies [33, 40] Low numeracy can pose a barrier to processing, computation, interpretation, and correct use of risk information, even if presented with a visual aid. [9, 41] More recent work provides evidence that visual aids can improve communication of risk [16, 30]. Regardless, without diligent use of presenting the numerical and visual format and eliciting patients’ comprehension of the risk being communicated, shared decision-making may not occur. Clinicians have an obligation to provide patients information in a way they can understand, whereas patients are responsible for understanding information in order to actively participate in decision making about their health [42]. For cancer patients this is an especially relevant problem due to the fact that screening and treatment decision-making requires a clear assessment and understanding of the risks involved [41]. In sum, our study sought active participation from women in translating their knowledge of verbal numerical information to a visual format. Ethnic differences were associated with women’s ability to translate this knowledge.
4.3 Practice Implications
Clinicians need to systematically consider the complexity of intersecting factors such as race/ethnicity, educational level, poverty, and numeracy in most health communications, but especially in discussions about risk of disease. Numeracy assessment of patients may assist providers in tailoring risk communication for optimal shared decision-making and patient-centered care. Although verbal terms (not studied here) are known to cause problems with communication due to inconsistent interpretation and vagueness, for some patients, use of words and verbal descriptors of risk, in addition to numerical information, may be more helpful in explaining cancer risk to patients. For other patients, the use of a visual aid with numerical information in eliciting their knowledge of the cancer risk may be more helpful. Further research is needed on understanding the complex intersecting factors that affect individuals from diverse ethnic backgrounds’ use of cancer risk information.
Acknowledgements
The authors thank Gregory Nah for conducting the data analyses, the women who participated in this study, and the research assistants who collected data. Miriam Kuppermann, PhD, and Anita Stewart, PhD, provided helpful feedback in the development of the study questionnaires. We also thank the anonymous reviewers for their helpful feedback on this manuscript.
This study was supported by the Agency for Healthcare Research and Quality (5P01 HS10856) for an Excellence Center to Eliminate Ethnic/Racial Disparities (EXCEED), by grant P30-AG15272 for the Center for Aging in Diverse Communities (CADC) under the Resource Centers for Minority Aging Research program by the National Institute on Aging, National Institutes of Health, and by grant Redes En Acción, U01-CA86117 from the National Cancer Institute. A Diversity Supplement to the CADC grant, a Michael Smith Scholar Award (CI-SCH-051), and CIHR New Investigator award supported Dr. Wong.
Appendix 1
These next set of questions are about how people might use numbers to think about their health. These questions are not to test you or make you feel that you must give me the right answer. I am not interested in whether you know the right or wrong answer. These questions will be used to help doctors communicate better with their patients about medical information that involves numbers.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
None of the authors have any potential conflict of interest related to this work.
References
- [1].Elwyn G, Edwards A, Gwyn R, Grol R. Towards a feasible model for shared decision making: focus group study with general practice registrars. Bmj. 1999;319(7212):753–6. doi: 10.1136/bmj.319.7212.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Elwyn G, Edwards A, Wensing M, Hood K, Atwell CRG. Shared decision-making: developing the OPTION scale for measuring patient involvement. Quality and Safety in Health Care. 2003;12:93–9. doi: 10.1136/qhc.12.2.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango) Soc Sci Med. 1997;44(5):681–92. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- [4].Davis K, Schoenbaum SC, Audet A-M. A 2020 Vision of Patient-Centered Primary Care. JGIM: Journal of General Internal Medicine. 2005;20(10):953–7. doi: 10.1111/j.1525-1497.2005.0178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Lipkus I. Numeric, verbal, and visual formats of conveying health risks: suggested best practices and future recommendations. Medical Decision Making. 2007;27:696–713. doi: 10.1177/0272989X07307271. [DOI] [PubMed] [Google Scholar]
- [6].Saba G, Wong S, Schillinger D, Fernandez A, Somkin C, Wilson C, et al. Shared decision making and the experience of partnership in primary care. Ann Fam Med. 2006;4:54–62. doi: 10.1370/afm.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Garcia JA, Paterniti DA, Romano PS, Kravitz RL. Patient preferences for physician characteristics in university-based primary care clinics. Ethnicity and Disease. 2003;13:259–67. [PubMed] [Google Scholar]
- [8].Gigerenzer G, Gaissmaier W, Kurz-Milcke E, Schwartz LM, Woloshin S. Helping Doctors and Patients Make Sense of Health Statistics. Psychological Science in the Public Interest (Wiley-Blackwell) 2007;8(2):53–96. doi: 10.1111/j.1539-6053.2008.00033.x. [DOI] [PubMed] [Google Scholar]
- [9].Fagerlin A, Ubel PA, Smith DM, Zikmund-Fisher BJ. Making Numbers Matter: Present and Future Research in Risk Communication. American Journal of Health Behavior. 2007;31(Supplement 1):S47–S56. doi: 10.5555/ajhb.2007.31.supp.S47. [DOI] [PubMed] [Google Scholar]
- [10].Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J. Health Literacy and Mortality Among Elderly Persons. Archives of Internal Medicine. 2007 Jul 23;167(14):1503–9. doi: 10.1001/archinte.167.14.1503. 2007. [DOI] [PubMed] [Google Scholar]
- [11].Kutner M, Greenberg E, Jin Y, Paulsen C. The health literacy of America’s adults: Results from the 2003 national assessment of adult literacy (NCES 2006-483) National Center for Education Statistics; Washington, DC: 2006. [Google Scholar]
- [12].Gigerenzer G. Reckoning with risk: learning to live with uncertainty. Penguin; London, EN: 2002. [Google Scholar]
- [13].Lipkus I, Hollands J. The visual communication of risk. Journal of National Cancer Institute Monograph. 1999;25:149–63. doi: 10.1093/oxfordjournals.jncimonographs.a024191. [DOI] [PubMed] [Google Scholar]
- [14].Woloshin S, Schwartz L, Byram S, Fischhoff B, Welch H. A new scale for asessing perceptions of chance: a validation study. Medical Decision Making. 2000;20(3):298–307. doi: 10.1177/0272989X0002000306. [DOI] [PubMed] [Google Scholar]
- [15].Shaheen N, Green B, Medapalli R. The perception of cancer risk in patients with prevalent Barrett’s esophagus enrolled in an endoscopice surveillance program. Gastroenterology. 2005;129(2):429–36. doi: 10.1016/j.gastro.2005.05.055. al e. [DOI] [PubMed] [Google Scholar]
- [16].Garcia-Retamero R, Dhami MK. Pictures speak louder than numbers: on communicating medical risks to immigrants with limited non-native language proficiency. Health Expectations. 2011;14:46–57. doi: 10.1111/j.1369-7625.2011.00670.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Huang A, Pérez-Stable E, Kim S, Wong S, Kaplan C, Walsh J, et al. Preferences for Human Papillomavirus Testing with Routine Cervical Cancer Screening in Diverse Older Women. JGIM: Journal of General Internal Medicine. 2008;23(9):1324–9. doi: 10.1007/s11606-008-0633-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Kim SE, Perez-Stable EJ, Wong S, Gregorich S, Sawaya GF, Walsh JME, et al. Association Between Cancer Risk Perception and Screening Behavior Among Diverse Women. Archives of Internal Medicine. 2008 Apr 14;168(7):728–34. doi: 10.1001/archinte.168.7.728. 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Sawaya GF, Iwaoka-Scott AY, Kim S, Wong ST, Huang AJ, Washington AE, et al. Ending cervical cancer screening: attitudes and beliefs from ethnically diverse older women. American Journal of Obstetrics and Gynecology. 2009;200(1):40.e1–.e7. doi: 10.1016/j.ajog.2008.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Marìn G, Marìn BV. Research with Hispanic populations. Sage Publications; Newbury Park, California: 1991. [Google Scholar]
- [21].Saslow D, Runowicz C, Solomon D, et al. American Cancer Society guideline for the early detection of cervical neoplasia and cancer. CA Cancer J Clin. 2002;52(6):342–62. doi: 10.3322/canjclin.52.6.342. [DOI] [PubMed] [Google Scholar]
- [22].Denberg TD, Wong S, Beattie A. Women’s misconceptions about cancer screening: implications for informed decision-making. Patient Education and Counseling. 2005;57(3):280–5. doi: 10.1016/j.pec.2004.07.015. [DOI] [PubMed] [Google Scholar]
- [23].Harris-Kojetin LDP, Fowler FJJP, Brown JABA, Schnaier JAMA, Sweeny SFMA. The Use of Cognitive Testing to Develop and Evaluate CAHPS(TM) 1.0 Core Survey Items. Medical Care. 1999;37(3):MS10–MS21. doi: 10.1097/00005650-199903001-00002. SUPPLEMENT. [DOI] [PubMed] [Google Scholar]
- [24].Ware J, Kosinski M, Turner-Bowker D, Gandek B. How to score version 2 of the SF12 Health Survey. QualityMetric; Lincoln, RI: 2002. [Google Scholar]
- [25].Sas Institute . SAS Online Doc 9.1.3. SAS Institute Inc; Cary, NC: 2007. [Google Scholar]
- [26].Allison P. Missing Data. Sage University; Thousand Oaks, CA: 2001. [Google Scholar]
- [27].Schaefer J. Analysis of incomplete multivariate data. Chapman and Hall; London, NY: 1997. [Google Scholar]
- [28].Meng X, Rubin D. Performing likelihood ratio tests with multiply-imputed data sets. Biometrika. 1992:103–11. [Google Scholar]
- [29].Rubin D. Multiple Imputation for Nonresponse in Surveys. Wiley; New York, NY: 1987. [Google Scholar]
- [30].Garcia-Retamero R, Galesic M. Who profits from visual aids: Overcoming challenges in people’s understanding of risks. Social Science & Medicine. 2010 Apr;70(7):1019–25. doi: 10.1016/j.socscimed.2009.11.031. 2010. [DOI] [PubMed] [Google Scholar]
- [31].Galesic M, Garcia-Retamero R. Statistical Numeracy for Health: A Cross-cultural Comparison With Probabilistic National Samples. Archives of Internal Medicine. 2010 Mar 8;170(5):462–8. doi: 10.1001/archinternmed.2009.481. 2010. [DOI] [PubMed] [Google Scholar]
- [32].Galesic M, Garcia-Retamero R. Graph Literacy. Medical Decision Making. 2011 May-Jun;31(3):444–57. doi: 10.1177/0272989X10373805. 2011. [DOI] [PubMed] [Google Scholar]
- [33].Woloshin S, Schwartz L, Moncur M, Gabriel S, Tosteson A. Assessing values for health: numeracy matters. Medical Decision Making. 2001;21:380–8. doi: 10.1177/0272989X0102100505. [DOI] [PubMed] [Google Scholar]
- [34].Schwartz L, Woloshin S, Black W, Welch H. The role of numeracy in understanding the benefit of screening mammography. Annals of Internal Medicine. 1997;127:966–72. doi: 10.7326/0003-4819-127-11-199712010-00003. [DOI] [PubMed] [Google Scholar]
- [35].Hess R, Visschers V, Siegrist M. How do people perceive graphical risk communication? The role of subjective numeracy. Journal of Risk Research. 2011;14(1):47–61. [Google Scholar]
- [36].University of British Columbia Centre for Teaching, Learning, and Technology. 2011 [cited 2011 Aug. 2011]; Available from: http://ctlt.ubc.ca/
- [37].Edwards A, Elwyn G, Mulley A. Explaining risks: turning numerical data into meaningful pictures. British Medical Journal. 2002 Apr 6;324(7341):827–30. doi: 10.1136/bmj.324.7341.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Galesic M, Garcia-Retamero R, Gigerenzer G. Using icon arrays to communicate medical risks: Overcoming low numeracy. Health Psychol. 2009;28(2):210–6. doi: 10.1037/a0014474. [DOI] [PubMed] [Google Scholar]
- [39].Zikmund-Fisher B, Angott A, Ubel P. The benefits of discussing adjuvant therapies one at a time instead of all at once. Breast Cancer Research Treatment. 2011;129(1):79–87. doi: 10.1007/s10549-010-1193-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Woloshin S, Schwartz L, Black W, Welch G. Women’s perceptions of breast cancer risk: how you ask matters. Medical Decision Making. 1999;19:221–9. doi: 10.1177/0272989X9901900301. [DOI] [PubMed] [Google Scholar]
- [41].Nelson W, Reyna VF, Fagerlin A, Lipkus I, Peters E. Clinical Implications of Numeracy: Theory and Practice. Annals of Behavioral Medicine. 2008;35(3):261–74. doi: 10.1007/s12160-008-9037-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Hanson JL. Shared Decision Making: Have We Missed the Obvious? Archives of Internal Medicine. 2008 Jul 14;168(13):1368–70. doi: 10.1001/archinte.168.13.1368. 2008. [DOI] [PubMed] [Google Scholar]