ABSTRACT
In 2009, a novel H1N1 influenza A virus (2009 pH1N1) emerged and caused a pandemic. A human monoclonal antibody (hMAb; EM4C04), highly specific for the 2009 pH1N1 virus hemagglutinin (HA), was isolated from a severely ill 2009 pH1N1 virus-infected patient. We postulated that under immune pressure with EM4C04, the 2009 pH1N1 virus would undergo antigenic drift and mutate at sites that would identify the antibody binding site. To do so, we infected MDCK cells in the presence of EM4C04 and generated 11 escape mutants, displaying 7 distinct amino acid substitutions in the HA. Six substitutions greatly reduced MAb binding (K123N, D131E, K133T, G134S, K157N, and G158E). Residues 131, 133, and 134 are contiguous with residues 157 and 158 in the globular domain structure and contribute to a novel pH1N1 antibody epitope. One mutation near the receptor binding site, S186P, increased the binding affinity of the HA to the receptor. 186P and 131E are present in the highly virulent 1918 virus HA and were recently identified as virulence determinants in a mouse-passaged pH1N1 virus. We found that pH1N1 escape variants expressing these substitutions enhanced replication and lethality in mice compared to wild-type 2009 pH1N1 virus. The increased virulence of these viruses was associated with an increased affinity for α2,3 sialic acid receptors. Our study demonstrates that antibody pressure by an hMAb targeting a novel epitope in the Sa region of 2009 pH1N1 HA is able to inadvertently drive the development of a more virulent virus with altered receptor binding properties. This broadens our understanding of antigenic drift.
IMPORTANCE
Influenza viruses accumulate amino acid substitutions to evade the antibody response in a process known as antigenic drift, making it necessary to vaccinate against influenza annually. Mapping human monoclonal antibody (hMAb) epitopes is a necessary step towards understanding antigenic drift in humans. We defined the specificity of an hMAb that specifically targeted the 2009 pH1N1 virus and describe a novel epitope. In addition, we identified a previously unappreciated potential for antibody escape to enhance the pathogenicity of a virus. The escape mutation that we identified with in vitro immune pressure was independently reported by other investigators using in vivo selection in nonimmune mice. Although in vitro generation of escape mutants is unlikely to recapitulate antigenic drift in its entirety, the data demonstrate that pressure by a human monoclonal antibody targeting a novel epitope in the hemagglutinin of the 2009 pandemic H1N1 virus can inadvertently drive the development of escape mutants, of which a subset have increased virulence and altered receptor binding properties.
Introduction
Hemagglutinin (HA) and neuraminidase (NA), the major envelope glycoproteins of influenza viruses, are the primary targets of the protective immune response to influenza A viruses (1). Protection against influenza virus infection is most efficiently mediated by neutralizing antibodies (Abs), whose induction likely provides the basis for the protective efficacy of licensed vaccines (2-4). While antibodies against HA or NA can impair viral spread, only anti-HA antibodies efficiently neutralize influenza viruses in vitro and in vivo by blocking HA-mediated virus attachment and cell entry, making HA the critical target of the antibody response (5-8).
As influenza viruses evolve in humans, they undergo gradual changes in the HA and NA proteins in a continuous process known as “antigenic drift.” During antigenic drift, influenza viruses accumulate amino acid substitutions in the HA globular domain that select for resistance to neutralization by HA-specific antibodies. This facilitates the continued circulation of influenza viruses in the human population and their ability to cause annual epidemics (9). The H1 HA has five antigenic sites located in the globular domain (Sa, Sb, Ca1, Ca2, and Cb) that are recognized by neutralizing murine monoclonal antibodies (MAbs) (9-11). However, human MAbs (hMAbs) that bind to the influenza virus HA interact with 2 or more of these sites as well as regions between them. Characterization of the antigenic sites is critical for revealing the mechanisms that drive influenza virus evolution.
In addition to antigenic drift, influenza viruses with a novel HA with or without an accompanying novel NA gene from an animal source are periodically introduced into the human population in a process known as “antigenic shift” (12). This can be a consequence of genetic reassortment among influenza viruses or by direct introduction of an animal influenza virus into humans (12-14). Antigenic shift can result in the emergence and pandemic spread of novel influenza viruses in an immunologically naive human population (12-14). The 2009 pandemic H1N1 virus is a reassortant swine influenza virus with genes derived from North American H3N2 and H1N2 swine viruses and Eurasian avian-like swine viruses and quickly established itself as the dominant H1N1 lineage circulating in humans (13). Like previous pandemic influenza viruses, it is expected that the 2009 pH1N1 virus will undergo antigenic drift as it evolves and encounters immune pressure. However, which mutations will arise, their location, and how the mutations may affect viral pathogenesis are not known. For example, a mutation at amino acid residue 222 of the HA protein has been identified in virus isolates from some severely ill patients, though its role in virulence is uncertain (15-19).
Here, we generate escape variants of the 2009 pH1N1 virus with a human monoclonal antibody (hMAb; EM4C04) isolated from a patient who became severely ill from 2009 pH1N1 virus infection. This patient had a primary antibody response that was highly specific for the 2009 pH1N1 virus (20). We identified the binding epitope of the hMAb and found that the escape mutant viruses displayed increased virulence in mice, associated with a change in receptor specificity. Mapping hMAb epitopes is a necessary step towards understanding antigenic drift in humans, and our study identifies the previously unappreciated potential for antibody escape to enhance pathogenicity.
RESULTS
Generation of escape mutants against EM4C04.
Peripheral blood mononuclear cells (PBMCs) were collected from a hospitalized 30-year-old female patient infected with 2009 pH1N1 virus; her course was complicated by acute respiratory distress syndrome (ARDS), bacterial pneumonia, and pulmonary embolism that required prolonged oscillatory ventilator support 31 days after admission (20). The EM4C04 antibody was isolated and purified from sorted IgG antibody-secreting cells (ASCs) as previously described (20). This antibody specifically neutralized the 2009 pH1N1 virus, with no measured cross-reactivity with other influenza viruses, including seasonal H1N1 influenza viruses, while the antibodies isolated from other patients were more broadly cross-reactive (20). Therefore, it was of interest to map the binding epitope of this unique antibody. To do so, escape mutant variants were generated using the 2009 pH1N1 virus.
To map the epitope defined by EM4C04, we sequenced 11 escape mutants that replicated in the presence of EM4C04 (Table 1). The H3 numbering system was used to describe the amino acid residues. Virus (EM18) was isolated from a control well in which cells were inoculated with virus in the absence of EM4C04 antibody. The amino acid sequences of the HA gene of the parental virus and the EM18 virus were identical, and both were used as controls in subsequent assays.
TABLE 1 .
Summary of mutations generated in the presence of EM4C04 antibody
| Mutant name | Mutation(s)a |
|---|---|
| EM18 (parental virus) | None |
| EM30 | K123N |
| EM02 | D131E |
| EM04 | D131E |
| EM10 | D131E |
| EM16 | D131E |
| EM20 | D131E |
| EM26 | K133T |
| EM22 | G134S |
| EM181 | G134S |
| EM27 | K157N, S186P |
| EM06 | G158E |
Amino acid residues are identified using H3 numbering.
A total of 7 different amino acid substitutions were identified in the HAs of 11 mutant viruses (Table 1). No mutations were identified in the NA gene segment. The D131E mutation appeared in 5 of the escape mutant viruses. Two of the substitutions, K157N and G158E, occurred in residues located in the Sa site of the HA globular head (10, 21). While mutations between residues 153 and 157 have been described following passage in cell culture (22), it seems unlikely that this is the case for the K157N and G158E mutations because no mutations were identified in the control wells in which virus was incubated with the cells in the absence of antibody. Also, each virus was amplified in MDCK cells, and no mutations in this region or elsewhere arose due to cell culture passage. Thus, we believe that the antigenic variants arose as a result of antibody pressure from EM4C04.
Interestingly, the K123N and G134S substitutions create a potential glycosylation site (23) defined as an amino acid sequence motif of Asn-Xaa-Ser/Thr, where Xaa can be any amino acid residue except proline (23). A positive score from NetNGlyc at these positions predicted that both of these substitutions would, in fact, create N-linked glycosylation sites. A gel mobility shift assay showed an increase in protein size for HA expressing the K123N or G134S substitutions compared to the wild-type (wt) virus, suggesting that the HA with either of these mutations had acquired an additional glycosylation site that likely blocks the binding epitope of EM4C04. Addition of glycans to the HA globular head has been shown to block neutralization of HA by monoclonal and polyclonal antibodies, as well as altering the receptor binding and fusion properties of the HA (24). While the 2009 pH1N1 virus contained only one glycosylation site on its globular head when it emerged (25), it is likely to accumulate additional glycosylation sites as it evolves.
Binding analysis of escape mutants.
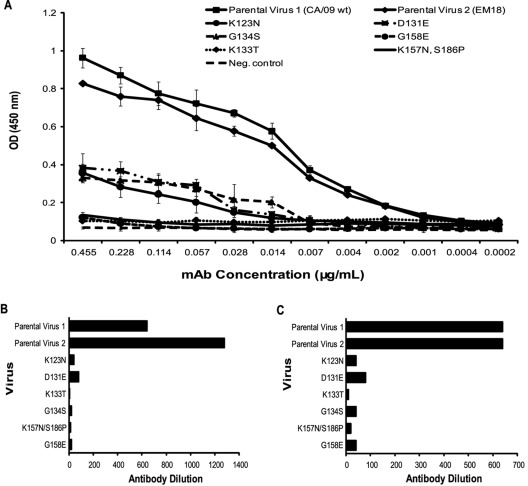
Enzyme-linked immunosorbent assay (ELISA) binding was used to distinguish between escape due to antigenic mutations and that due to adsorptive mutations (Fig. 1). Antigenic mutations significantly reduce antibody binding to the target epitope, while adsorptive mutations increase the binding affinity of the virus to the host cell (9). Antigenic mutants show significantly lower optical density (OD) values than do the wt parental viruses, demonstrating their inability to bind the antibody, while adsorptive mutants show a binding pattern and OD values similar to those of the wt parental viruses because antibody binding is not compromised in these mutants. Figure 1A shows the results from an antibody binding ELISA, in which six viruses with mutations at K123N, D131E, K133T, G134S, K157N/S186P, and G158E, respectively, demonstrated significantly reduced binding to EM4C04 compared to the CA/09 wt parental virus (parental virus 1) and the EM18 control virus (parental virus 2). Recombinant viruses expressing the K157N and S186P mutations both individually and together were generated by reverse genetics to determine the individual effect of each mutation on EM4C04 binding. The K157N mutant showed significantly reduced binding to EM4C04 in an antibody binding ELISA, while the S186P mutant showed a binding pattern similar to that of the parental viruses (see Fig. S1 in the supplemental material). Calculation of the dissociation constant (Kd) values for these recombinant viruses, and the escape mutant viruses, listed in Fig. 1A, showed that the S186P mutant had a higher binding affinity for EM4C04 than did the parental viruses, suggesting that S186P was an adsorptive mutation (see Table S1 in the supplemental material). This was confirmed by treating erythrocytes with Vibrio cholerae neuraminidase receptor-destroying enzyme (RDE), which removes terminal sialic acid (SA), the cellular ligand for HA. Adsorptive mutants exhibit enhanced agglutination of RDE-treated erythrocytes compared to the parental virus (9). In our study, among the escape mutants, only the viruses expressing the S186P mutation agglutinated RDE-treated erythrocytes better than did the wt virus, indicating that S186P is an adsorptive mutation (data not shown).
FIG 1 .
Binding analysis of escape mutants. (A) A binding ELISA was performed using plates coated with each of the indicated viruses in triplicate. Serial dilutions of EM4C04 were added to the wells, followed by the addition of a secondary anti-human antibody conjugated to HRP. OD values were read at 450 nm. The negative control was wells that had PBS alone added without virus. (B) Hemagglutination inhibition (HAI) assay comparing the HAI titers of CA/09 wt and mutant viruses. The HAI titer represents the inverse of the highest MAb dilution at which hemagglutination was inhibited. (C) Neutralization assay of CA/09 wt and mutant viruses. The neutralization titer represents the inverse of the highest MAb dilution at which an infectivity of 100 TCID50 of the virus was neutralized. HAI and neutralization assays were performed in quadruplicate.
Hemagglutination inhibition (HAI) (Fig. 1B) and neutralization (Fig. 1C) assays confirmed the ELISA results. The six mutant viruses expressing the K123N, D131E, K133T, G134S, K157N, and G158E mutations also exhibited significantly reduced neutralization and HAI titers compared to the parental wt viruses. Recombinant viruses expressing the K157N and S186P mutations individually also showed significantly reduced HAI and neutralization titers compared to the wt viruses. Adsorptive mutations decrease HAI and neutralization antibody activities by increasing the viral HA binding avidity for cell surface glycan receptors (9). The reduced HAI and neutralization titers seen with the S186P mutant, in addition to its enhanced agglutination of RDE-treated erythrocytes, were not seen with the other mutant viruses and confirm that S186P is an adsorptive mutation.
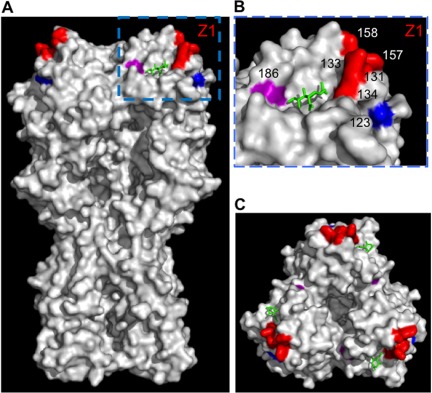
When the mutations were mapped on the crystal structure of the H1 HA, it appeared that the five residues (131, 133, 134, 157, and 158) likely comprise the target epitope for the EM4C04 antibody (Fig. 2). The S186P mutation, which is highlighted in purple, was an adsorptive mutation that was not part of the EM4C04 binding site (Fig. 2). Amino acids 157 and 158 were previously mapped to the H1N1 Sa antigenic site, suggesting that the EM4C04 antibody binds to this antigenic site. Residues 131, 133, and 134, contiguous with residues 157 and 158 in the globular domain structure, have not been previously identified by epitope mapping of escape mutants, suggesting that they contribute to a novel pH1N1 antibody epitope site stretching from residues 157 to 134. Residue 123 is in close proximity to this epitope but is not continuous with the other five residues. The glycosylation site created by the K123N substitution likely interferes with binding to this epitope. It is also possible that the glycosylation site created by the G134S mutation blocks the target epitope in a similar fashion.
FIG 2 .
Map of EM4C04 escape mutations on the HA surface. (A and C) Diagram of the 2009 pH1N1 HA protein with both a side view (A) and a top view (C). (A) The locations of the amino acid residues identified as escape mutations that allow escape from EM4C04 neutralization are highlighted in red (residues 131, 133, 134, 157, and 158), blue (123), and purple (186). (B) A zoomed-in view of the locations of the five amino acid residues that likely comprise the EM4C04 target epitope is shown with the residues labeled. A sialic acid molecule is shown (highlighted in green) to indicate the location of the receptor binding site of the HA protein.
Increased virulence of escape mutants in mice.
Remarkably, the D131E and S186P substitutions were recently shown to increase virulence in mouse-passaged A/California/04/2009 (CA/4/09) viruses compared to the parental virus (26, 27). In one study, these two mutations alone were sufficient to confer virulence in mice (26). In our study, binding analysis identified D131E as an antigenic mutation while S186P was adsorptive.
Therefore, we tested the in vitro replication and virulence of mutants expressing either the D131E mutation (EM02) or the S186P mutation (EM27) in mice, relative to the parental CA/09 wt virus. The escape mutant viruses generated by passage of the parental CA/09 wt virus in the presence of EM4C04 are referred to as “biological viruses.” The recombinant K157N and S186P viruses were used in order to distinguish the individual effects of each mutation on influenza virus virulence. In addition, we generated a recombinant CA/09 wt virus and recombinant viruses expressing the D131E mutation alone and the D131E and S186P mutations together. The binding analyses used to characterize the escape mutants, such as ELISA, HAI, neutralization, and RDE avidity assays, were performed with the recombinant mutants to determine whether they behaved similarly to their biological counterparts.
Initially, the biological and recombinant viruses were compared to the wt viruses in vitro in MDCK cells inoculated at a multiplicity of infection (MOI) of 0.1 (see Fig. S2 in the supplemental material). Virus titers peaked at about 24 h postinfection. The K157N/S186P recombinant, S186P recombinant, and D131E recombinant viruses showed higher titers than did the CA/09 wt virus at 24 h postinfection, and the K157N/S186P and D131E recombinant viruses maintained a 10-fold-higher titer than did the CA/09 wt virus at 48 and 72 h postinfection, suggesting that these viruses may grow more efficiently in cell culture than the CA/09 wt virus. Overall, the data suggest that there are only minor differences in viral fitness in vitro between the CA/09 wt and most of the mutant viruses.
To compare the virulence of the mutant viruses and that of the wt viruses in vivo, we first evaluated the response to a dose of 105 50% tissue culture infectious doses (TCID50) of each virus in mice. Consistent with previous results, the biological and recombinant CA/09 wt viruses caused >15% weight loss but were not lethal for BALB/c mice (100% survival) (Fig. 3A and 3B) (26). In contrast, the biological and recombinant viruses expressing either the D131E or S186P mutation or both mutations were lethal at this dose (Fig. 3A and 3B), with mice dying between 5 and 7 days postinfection (dpi) (Fig. 3B); 20% to 40% of the mice infected with the D131E and S186P mutant viruses were found dead, while the rest were euthanized after a >25% loss in body weight. None of the mice infected with viruses expressing the D131E mutation survived, and only 20% of the mice infected with the S186P recombinant virus survived. The recombinant K157N virus was not lethal (100% survival) and produced a pattern of weight loss similar to that of the parental viruses (Fig. 3A and 3B), implicating S186P in the lethality of the double mutant K157N/S186P virus. The remaining escape variants (K123N, K133T, G134S, and G158E) were not lethal for mice at a dose of 105 TCID50, with 100% of the mice surviving. Thus, the D131E and S186P mutations specifically alter the virulence of the 2009 pH1N1 virus in mice (see Fig. S3 in the supplemental material).
FIG 3 .
Weight loss and lethality in mice infected with the D131E and S186P CA/09 mutants. Weight loss (A) and mortality (B) were monitored for 14 days after intranasal inoculation with 105 TCID50 of biological and recombinant CA/09 wt and mutant viruses in groups of five mice. Mice were euthanized if they lost at least 25% of their original body weight. In panel A, the numbers beside each line represent the number of mice that survived per group of five mice. Numbers in parentheses represent results from multiple groups.
We next determined the 50% mouse lethal dose (MLD50) for the wt virus and escape mutants (Table 2). Lethality was observed only at very high doses of the CA/09 wt virus. The D131E substitution decreased the MLD50 by >10-fold, and together, the D131E and S186P mutations decreased the MLD50 by >100-fold (Table 2). Because we sequenced only the HA and NA genes of the escape mutant viruses, we cannot exclude the possibility that mutations in other viral genes of the biologically derived mutant viruses that affect the pathogenicity phenotype may be present.
TABLE 2 .
Virulence of CA/09 wt and mutant viruses in mice
| Virus | >MLD50 (log10 TCID50) |
|---|---|
| CA/09 wt biological | 5.8 |
| CA/09 wt recombinant | 5.5a |
| D131E recombinant | 4.2 |
| D131E biological | 3.8 |
| K157N/S186P recombinant | 4.4 |
| K157N/S186P biological | 3.6 |
| D131E/S186P recombinant | 3.2 |
CA/09 wt recombinant virus MLD50 was determined in a separate experiment.
The effect of the mutations on viral replication in the respiratory tract of mice was assessed by measuring titers in the lungs and nasal turbinates at days 2 and 4 postinfection (see Fig. S4 in the supplemental material). Mice infected with the K157N mutant virus displayed lung virus titers similar to those of the wt viruses (see Fig. S4A and S4B). Modestly higher (~2.5- to 6-fold) titers were observed on both days in mice infected with viruses expressing the D131E or S186P mutation than in those infected with the wt viruses (see Fig. S4A and S4B). Mice infected with recombinant D131E/S186P virus showed significantly higher viral titers in the lungs on both days than did the wt viruses (~13- to 27-fold at days 2 and 4, respectively) and viruses expressing only a single mutation (see Fig. S4A and S4B). Overall, the differences were modest, and although they achieved statistical significance, their biological significance is questionable.
In the nasal turbinates, as in the lungs, mice infected with the K157N mutant showed titers similar to those of the wt viruses (see Fig. S4C and S4D in the supplemental material). However, mice infected with viruses expressing the D131E or S186P mutation showed significantly higher titers in the upper respiratory tract only at day 4 compared to the wt viruses, with about a 5- to 10-fold increase in titer (see Fig. S4D). The D131E/S186P recombinant mutant virus achieved significantly higher titers on both days than did the wt viruses, with a 6- to 10-fold-higher titer on days 2 and 4, respectively (see Fig. S4C and S4D). However, a significant difference in titer was not seen between the D131E/S186P mutant and viruses expressing the individual mutations (see Fig. S4C and S4D).
SA receptor specificity.
HA binds to sialic acid (SA) linked to oligosaccharide side chains with α(2,3)-Gal or α(2,6)-Gal residues (28). The HA from human isolates typically preferentially binds α(2,6)-Gal-linked SA, while avian HAs preferentially bind α(2,3)-Gal-linked SA (29, 30). In the lower respiratory tract of mice, α(2,3)-Gal-linked SA predominates over α(2,6)-Gal-linked SA (31, 32). Mouse-adapted human influenza viruses with increased virulence can display a change in receptor specificity with enhanced binding to α(2,3)-Gal-linked SA (9, 33). Therefore, we tested the receptor specificity of the D131E and S186P mutant viruses in an assay using de-/resialylated chicken red blood cells (cRBCs) (Table 3). Chicken erythrocytes typically express both α(2,3)- and α(2,6)-Gal-linked SA but can be desialylated and resialylated to express only α(2,3)- or α(2,6)-Gal-linked SA. The CA/09 wt viruses bound α(2,6)-Gal-linked SA but not α(2,3)-Gal-linked SA cRBCs. In contrast, mutant viruses expressing either the D131E or S186P mutation bound α(2,6)-Gal-linked SA and showed some binding to α(2,3)-Gal-linked SA cRBCs. These results were confirmed in hemagglutination assays using turkey erythrocytes that express both α(2,3)- and α(2,6)-Gal-linked SA and horse red blood cells (hRBCs) that express only α(2,3)-Gal-linked SA (Table 3). Thus, the CA/09 wt viruses failed to bind horse red blood cells while viruses expressing either the D131E or S186P mutation showed some binding to these cells (Table 3). Together, these results demonstrate that the D131E and S186P mutations modulate receptor binding specificity, resulting in a virus that is able to bind both α(2,3)-Gal-linked SA and α(2,6)-Gal-linked SA.
TABLE 3 .
Comparison of sialic acid binding specificities
| Virus | HA titer with indicated RBCs |
|||||
|---|---|---|---|---|---|---|
| De-/resialylation assay |
tRBCs | hRBCs | ||||
| SAα2,3 resialylated cRBCs | SAα2,6 resialylated cRBCs | Desialylated cRBCs | Untreated cRBCs | |||
| CA/09 wt biological | <1a | 128 | <1 | 128 | 64b | <1 |
| CA/09 wt recombinant | <1 | 128 | <1 | 128 | 64 | <1 |
| D131E biological | 4 | 128 | <1 | 128 | 64 | 4 |
| D131E recombinant | 4 | 128 | <1 | 128 | 64 | 4 |
| K157N/S186P biological | 8 | 128 | <1 | 128 | 64 | 4 |
| K157N/S186P recombinant | 4 | 128 | <1 | 128 | 64 | 8 |
| S186P recombinant | 8 | 128 | <1 | 128 | 64 | 8 |
| D131E/S186P recombinant | 8 | 128 | <1 | 128 | 64 | 4 |
| H2 SAα2,6 controlc | <1 | 128 | <1 | 128 | 64 | <1 |
| H2 SAα2,3 control | 128 | <1 | <1 | 128 | 64 | 64 |
For assay with cRBCs, HA titers ranged from 1 to 128.
For assay with tRBCs and hRBCs, viruses were standardized to an HA titer of 64.
Controls were recombinant A/Japan/57 (H2N2) viruses with either the 226L/228S amino acid combination (H2 SAα2,6 control) or the 226Q/228G amino acid combination (H2 SAα2,3 control).
DISCUSSION
The purpose of this study was to map the epitope of an hMAb generated in response to a primary infection with 2009 pH1N1 virus to broaden our understanding of antigenic drift with the 2009 pH1N1 virus. We postulated that under immune pressure with the hMAb EM4C04, the 2009 pH1N1 virus would undergo antigenic drift and mutate at sites that would identify the binding site of the antibody. The binding site was identified and mapped by generating escape mutant viruses. Surprisingly, we found that some of the escape mutants displayed increased virulence in mice that was likely the result of altered receptor specificity that allowed the viruses to bind both α(2,3)-Gal-linked SA and α(2,6)-Gal-linked SA.
Although the in vitro generation of escape mutants is unlikely to recapitulate drift in its entirety, this is largely due to the stochastic nature of drift and the very large mutational space available. However, mapping hMAb epitopes is a necessary step towards understanding antigenic drift in humans, and our study identifies the previously unappreciated potential for antibody escape to enhance pathogenicity. Our novel finding of the emergence of escape variants with increased pathogenicity makes us rethink pathogenesis, as we directly show that antibody escape can inadvertently increase pathogenesis. While the D131E and S186P mutations specifically identified in this study may not necessarily increase virulence in humans, our study definitively establishes the potential for this to occur.
Additionally, we defined the specificity of an hMAb that specifically targeted the 2009 pH1N1 virus, defining a novel epitope with residues previously believed to be nonantigenic. We mapped the EM4C04 binding site to a novel epitope that includes residues from the Sa antigenic site of the HA protein. Other hMAbs have been mapped to nearby epitopes on the globular head of the HA close to the receptor binding pocket, including a study that identified escape mutants at amino acid residue 133 on the pH1N1 virus (34, 35). It is difficult to judge to what extent hMAb EM4C04 is representative, especially considering that the majority of antibodies induced after infection with pandemic H1N1 viruses were cross-reactive. However, while cross-reactive Abs may predominate in adults with many prior infections/vaccination, it is likely that more strain-specific Abs predominate in children, particularly after their first infection. This population may be largely responsible for antigenic drift. The EM4C04 antibody was isolated from a severely ill 30-year-old female patient with complications of ARDS, bacterial pneumonia, and pulmonary embolism (20). Her antibody response was concluded to be characteristic of a primary antibody response, presumably due to lack of previous exposure to related influenza viruses, based on the high specificity against 2009 pH1N1, the low levels of somatic mutation in the variable genes from the plasmablasts, and the severe disease in the absence of predisposing conditions (20). At least two other studies have shown that antibodies generated following pH1N1 infection target the Sa region, as does EM4C04 (36, 37). Taken together, the studies suggest that the Sa region is an immunodominant antigenic site on the 2009 pH1N1 virus, which may drift as the 2009 pH1N1 virus evolves (36, 37).
Escape mutant variants expressing the D131E or S186P mutation exhibited increased virulence in mice compared to the wt parental virus, suggesting that these two residues are virulence determinants for the 2009 pH1N1 virus. These viruses caused greater morbidity in mice, showed increased viral replication in the lower respiratory tract, and were lethal at lower doses. Either mutation alone was sufficient to confer increased virulence, with the expression of both mutations resulting in a minor enhancement in virulence. To our knowledge, this is the first study to use an hMAb to generate 2009 pH1N1 escape mutant variants in vitro. Previous studies have identified virulent viruses expressing similar mutations following an alternative selection method of serial passage in mice in the absence of preexisting immune responses (26, 27). Mutations generated using hMAbs, however, are likely to more accurately predict mutations that could arise as influenza viruses circulate in humans. The generation of more-virulent viruses expressing the D131E and S186P mutations extends results from passage in mice using the closely related A/California/04/2009 pH1N1 virus and argues that these residues are virulence determinants that may emerge in humans as a result of antigenic drift. However, the scenario in natural infection associated with a polyclonal antibody response is undoubtedly more complex than selection pressure placed on a virus by a single monoclonal antibody. Thus, the implications of our findings cannot be directly extrapolated to humans.
The enhanced virulence of the mutant viruses is probably related to a change in SA receptor specificity. While CA/09 wt viruses specifically bind to only α(2,6)-Gal-linked SA, viruses expressing either the D131E or S186P mutation bound both α(2,6)-Gal-linked SA and α(2,3)-Gal-linked SA. The close proximity of these residues to the receptor binding site (RBS) likely contributes to their ability to alter SA binding. The predominance of α(2,3)-Gal-linked SA in the lower respiratory tract of mice (31, 32) and the fact that mouse-adapted human influenza viruses, which show increased virulence compared to the parental viruses, can display enhanced binding to α(2,3)-Gal-linked SA (9, 33) suggest that the D131E and S186P mutants display increased viral replication in the lungs and enhanced virulence in mice because of their ability to bind α(2,3)-Gal-linked SA. Interestingly, the D222G mutation, which may be associated with increased virulence in the 2009 pH1N1 virus in humans (15-19), also alters receptor specificity (38, 39). Notably, while the D131E and S186P mutations were found to increase binding affinity for α(2,3)-Gal-linked SA, the viruses did not lose their ability to bind α(2,6)-Gal-linked SA. Together, these results suggest that the acquired ability to bind both α(2,3)- and α(2,6)-Gal-linked SA may be associated with increased virulence for the 2009 pH1N1 virus.
While others have speculated as to why these mutations result in increased virulence (26), our study suggests that it results from altered receptor specificity. In humans, α(2,6)-Gal-linked SA is predominantly found in the upper respiratory tract while α(2,3)-Gal-linked SA is predominantly present in the lower respiratory tract (40-42). Human influenza viruses are generally characterized by their binding preference for α(2,6)-Gal-linked SA, while avian influenza viruses preferentially bind α(2,3)-Gal-linked SA (40-42), though the virus-host interactions that lead to disease pathogenesis in intact animals and humans are likely to be much more complex than the receptor binding preference paradigm suggests. The 131E and 186P mutations have previously been characterized as avian-type mutations because of their presence in the 1918 H1N1 viruses of avian origin (26). Thus, it is not surprising that we found that mutant viruses expressing the D131E or S186P mutation acquired the ability to bind α(2,3)-Gal-linked SA. This new phenotype could have significant consequences if the viruses are able to replicate more efficiently in the human lower respiratory tract. Highly pathogenic avian influenza (HPAI) H5N1 viruses, which preferentially bind α(2,3)-Gal-linked SA, are associated with a case fatality rate of ~60% in laboratory-confirmed cases that meet the World Health Organization definition (43, 44). However, the actual case fatality rate may be significantly lower (45, 46). The severe disease caused by HPAI H5N1 is believed to be at least in part due to preferential infection of the human lower respiratory tract (41, 42, 47, 48). This emphasizes the role of influenza virus infection of the human lower respiratory tract as a key event in the pathogenesis of severe disease and/or death. Ye et al. (26) examined the transmissibility of viruses expressing the D131E and S186P mutations in ferrets, which have an SA receptor distribution similar to that of humans, and concluded that viruses expressing these mutations are transmitted to levels similar to those of the parental viruses, suggesting that these mutations do not negatively affect viral growth or transmissibility (26).
A comparison of 4,200 published 2009 pH1N1 HA sequences in the Influenza Research Database (IRB) revealed that the 131E and 186P residues are infrequent among currently circulating 2009 pH1N1 viruses. Only 12 (0.29%) isolates expressed 131E, while 13 (0.30%) expressed 186P. In some instances, a mixed population of sequences with 131D or 186S was present, suggesting that the variants may exist as a minor quasispecies that could be selected under immune pressure. However, the number of 2009 pH1N1 human isolates expressing the S186P mutation has increased from 2009 to 2011, and it is possible that this trend may continue. Information was not available regarding the severity of disease in patients from whom these viruses were isolated. Our data show that there is the potential for escape mutants that arise as a result of antigenic drift to be more virulent than the parental virus in mice.
The 131E and 186P residues are common among classical swine influenza viruses. For instance, the 131E residue was identified in viruses such as A/swine/Iowa/1930 and A/New Jersey/8/1976, while the 186P residue was identified in A/Alaska/1935 and A/New Jersey/8/1976. Both residues were also conserved in the 1918 H1N1 influenza viruses, which caused a pandemic that was responsible for as many as 50 million deaths worldwide (49). If expression of the 131E and 186P residues in the 1918 influenza virus contributed to its highly virulent phenotype, then the emergence of these residues in the 2009 pH1N1 virus and their effect on virulence should be closely monitored. Interestingly, the 186P residue is also conserved among most seasonal H1N1 influenza viruses isolated from 1998 to 2007. If the 186P residue does contribute to increased virulence, it seems likely that additional genomic changes decrease the pathogenic potential of 186P in seasonal H1N1 influenza viruses. And while it is possible that the 186P residue does not have an effect on virulence in humans, the increase in 2009 pH1N1 isolates expressing the S186P mutation from 2009 to 2011 still suggests that this mutation is being selected for in humans.
Our analysis of available sequences shows that 2009 pH1N1 viruses have acquired mutations at all 13 residues previously mapped to the Sa antigenic site while changes in the other antigenic sites have been much more limited. This supports the conclusion that the Sa antigenic site is the immunodominant antigenic site (36, 37). However, it is not known if these mutations arose as a result of pressure from EM4C04-like antibodies in vivo. For the mutations specifically identified in this study, the 133T, 134S, and 157N mutations were not reported in H1N1 isolates prior to 2009, suggesting that these residues are specific features of the 2009 pH1N1 HA. The 158E residue is present in some H1N1 viruses isolated in the early 1930s, including A/PR/8/34 and A/swine/Iowa/30. The G158E mutation was detected as a quasispecies in viral RNA extracted from the lung tissue of a 2009 pH1N1 virus-infected patient who died of viral pneumonia (50). The K123N and G134S mutations likely generate glycosylation sites on the HA globular head. The K123N mutation was also seen in a 2009 pH1N1 mouse-adapted virus (27). In the past, there has been a tendency towards the accumulation of glycosylation sites on the globular head of the HA as pandemic influenza viruses evolve in humans (23, 25). The functional importance of these sites lies in their ability to mask antigenic regions and prevent neutralization by antibodies (25). Detection of the K123N and G134S substitutions in our study has identified the positions of two potential glycosylation sites that may emerge as a result of antigenic drift as the 2009 pH1N1 virus circulates in humans.
In conclusion, we have shown that 2009 pH1N1 escape mutant viruses generated in vitro under immunological pressure with an hMAb specific for a novel epitope in the Sa antigenic site of the HA protein can inadvertently lead to the generation of viruses with altered receptor specificity and enhanced virulence. These novel findings broaden our understanding of influenza antigenic drift and its possible consequences on pathogenicity. The emergence of mutations in the 2009 pH1N1 virus and their effect on viral pathogenicity should be closely monitored.
MATERIALS AND METHODS
Viruses.
The wild-type (wt) 2009 pH1N1 virus, A/California/07/2009 (CA/09), was kindly provided by Ruben Donis and Alexander Klimov from the Influenza Division, Centers for Disease Control and Prevention, Atlanta, GA. Recombinant CA/09 viruses were generated by reverse genetics as described previously (51). In accordance with the manufacturer’s protocol, site-directed mutagenesis (Agilent Technologies) was used to introduce mutations into HA to create CA/09 recombinant viruses for in vivo studies. The wt and recombinant viruses were propagated in the allantoic cavity of 9- to 11-day-old embryonated specific-pathogen-free hen’s eggs. Eggs inoculated with the viruses were incubated at 35°C, and allantoic fluid was harvested 48 to 72 h later, tested for hemagglutinating activity, and stored at −80°C until use. The 50% tissue culture infectious dose (TCID50) for each virus was determined by serial titration of virus in MDCK cells and calculated by the method developed by Reed and Muench (52). For the receptor specificity assays, influenza viruses with known binding preferences for either SAα2,3 or SAα2,6 were used as controls.
Antibody.
The generation of the human monoclonal antibody EM4C04 was described by Wrammert et al. (20). This antibody was purified from IgG antibody-secreting cells (ASCs) from the peripheral blood mononuclear cells (PBMCs) of a patient infected with the 2009 pH1N1 virus as described elsewhere (20).
Animals.
Six- to 8-week-old female BALB/c mice (Taconic Farms, Inc., Germantown, NY) were used to evaluate the lethality and replication of the wt and mutant CA/09 viruses. Postinfection polyclonal serum against the CA/09 wt virus was generated in 6-month-old female BALB/c mice. The National Institutes of Health Animal Care and Use Committee approved all animal experiments.
Generation of escape mutants.
CA/09 wt virus was serially diluted 2-fold in minimum essential medium (MEM) in round-bottomed 96-well plates. EM4C04 antibody with an original concentration of 600 µg/milliliter was diluted 1:1,000 and added to the virus. The virus-antibody mixture was incubated for 30 min at room temperature and then transferred to MDCK cells cultured in 96-well plates. The virus-antibody mixture was incubated with the cells for 2 h at 37°C, after which the mixture was removed, and fresh MEM [supplemented with 4 mM l-glutamine, 1× antibiotic-antimycotic (Gibco Ant-Anti, Invitrogen), and 1 µg/milliliter l-(tosylamido-2-phenyl) ethyl chloromethyl ketone (TPCK)] containing EM4C04 (diluted 1:10,000) was added. Control cells were inoculated with virus alone in the absence of EM4C04. Cells were incubated at 37°C for 4 days and checked for the presence of cytopathic effect (CPE). The antibody dilutions used provided concentrations of EM4C04 that were optimal for driving the emergence of escape mutants for this particular antibody.
Sequencing of escape mutants.
Viral RNA was purified from aliquots of supernatant taken from wells showing evidence of CPE using the QIAmp viral RNA minikit (Qiagen). To generate cDNA, reverse transcriptase PCR (RT-PCR) was performed, according to the manufacturer’s protocol, using the Qiagen One Step RT-PCR kit. The HA and NA gene segments were amplified and PCR products were purified using the QIAquick PCR purification kit. DNA sequencing was performed on an Applied Biosystems 3730 DNA analyzer.
Monoclonal antibody binding analysis.
As previously described (9), wt and mutant CA/09 viruses diluted in phosphate-buffered saline (PBS) were added in triplicate to 96-well flat-bottomed ELISA plates. After incubation at 4°C for at least 16 h, wells were blocked with PBS-5% fetal bovine serum (FBS) for 1 h at room temperature. A nonsaturating concentration of the human EM4C04 antibody (diluted 1:1,000) in the linear portion of the antibody titration curve determined previously was added to each well, serially diluted 2-fold, and incubated with the virus-coated plates for 1 h at room temperature. After washing, anti-human horseradish peroxidase (HRP)-conjugated antibody was added to the plates, and they were incubated for 1 h at room temperature. After another round of washing, TMB (3,3′,5,5′-tetramethylbenzidine) substrate (KPL Biomedical) was added, and HCl was used to stop the reaction. The amount of HRP product was determined using a plate reader at 450 nm. Antibody binding to the M2 protein was also measured to verify that the plates were coated with similar amounts of virus. Based on these antibody titrations, dissociation constants (Kds) were calculated using GraphPad Prism.
HAI assay.
As previously described (53), HAI assays were performed in 96-well V-bottomed plates. The EM4C04 antibody was 2-fold serially diluted starting at a dilution of 1:10, and 4 hemagglutinating units of virus was added. Control wells received PBS alone or PBS with virus in the absence of antibody. Virus and EM4C04 antibody were incubated together for 30 min at room temperature. Next, 50 µl of a 0.5% (vol/vol) turkey erythrocyte solution was added. The antibody, virus, and erythrocytes were gently mixed, and the results were recorded after incubation for 45 to 60 min at room temperature. HAI titers were recorded as the inverse of the highest antibody dilution that inhibited the agglutination of red blood cells.
In vitro neutralization assay.
As previously described (54), wt and mutant viruses were diluted to a concentration of 100 TCID50 per 50 µl (103.3 TCID50/ml) in MEM-0.5% bovine serum albumin (BSA). Serial dilutions of the EM4C04 antibody or mouse sera were mixed with each of the viruses and incubated at room temperature for 1 h. After 1 h, the virus-antibody mixture was added in quadruplicate to MDCK cells cultured in 96-well plates. Cells were incubated at 37°C, and virus growth was scored 4 days later by CPE. The neutralization titer is the inverse of the highest EM4C04 dilution where infectivity was neutralized.
Assessment of lethality in mice.
We administered 50 µl containing 105 TCID50 of the biological and recombinant CA/09 wt and mutant viruses intranasally (i.n.) to groups of 5 lightly anesthetized 6- to 8-week-old female BALB/c mice. Body weights were recorded daily for a period of 14 days following infection. Mice that lost ≥25% of their initial body weight were sacrificed according to the institutional animal care and use committee guidelines.
To determine the 50% mouse lethal doses (MLD50s) of selected viruses, groups of five 6- to 8-week-old female BALB/c mice were lightly anesthetized and infected with 50 µl of 10-fold serial dilutions containing 101 to 106 TCID50 of the viruses. Mice were monitored daily for 14 days postinfection (dpi) for changes in body weight and mortality.
RDE avidity assay.
As previously described (9), a 10% (vol/vol) turkey erythrocyte solution was treated with various concentrations (1 U, 500 mU, 50 mU, 25 mU, 10 mU, 5 mU, and 0 U) of V. cholerae neuraminidase receptor-destroying enzyme (RDE) for 1 h at 37°C. The cells were washed, diluted to 2% (vol/vol) in PBS, and added to 96-well V-bottomed plates containing 4 HA units of the biological and recombinant viruses. The plates were gently shaken, and the results were recorded after incubation for 45 to 60 min at room temperature.
Assessment of viral replication in mice.
To assess the ability of the biological and recombinant CA/09 wt and mutant viruses to replicate in the respiratory tract, groups of 8 lightly anesthetized female BALB/c mice were inoculated with 50 µl containing 105 TCID50 of the different viruses. On days 2 and 4 postinfection, the lungs and nasal turbinates were harvested. Organs were weighed and homogenized in L-15 medium containing antibiotic-antimycotic (Invitrogen-Gibco) to make 10% (wt/vol) tissue homogenates. Tissue homogenates were clarified by low-speed centrifugation and titrated in 24- and 96-well culture plates containing MDCK cells. Titers are expressed as log10 TCID50/g of tissue.
Hemagglutination assay.
CA/09 wt and mutant viruses standardized to an HA titer of 64 were 2-fold serially diluted in PBS in 96-well V-bottomed plates. Next, 50 µl of a 0.5% (vol/vol) erythrocyte solution of either turkey red blood cells (tRBCs) or horse red blood cells (hRBCs) was added. The virus and erythrocytes were gently mixed, and the results were recorded after incubation for 30 to 60 min at room temperature.
De-/resialylation assay.
Chicken red blood cells (cRBCs) (10%) (HEMA Resource and Supply Inc.) were desialylated by incubation with 250 mU/µl Clostridium perfringens neuraminidase (Sigma) for 1 h at 37°C. The cells were then washed twice in PBS and resuspended in PBS-1% BSA. The cells were resialylated by incubating aliquots of cRBCs with CMP-sialic acid (Sigma) and either α2,3-sialyltransferase (Sigma) or α2,6-sialyltransferase (Calbiochem) for 1.5 h at 37°C. The resialylated cRBCs were then washed 3 times in PBS and resuspended in PBS at a 1% concentration, and a hemagglutination assay was performed as described above. H2N2 Japan/57 (JP/57) recombinant viruses with known receptor specificities were used as controls. H2N2 JP/57 L-S with the 226L/228S amino acid combination preferentially binds α2,6-sialic acid, while H2N2 JP/57 Q-G with the 226Q/228G amino acid combination specifically binds α2,3-sialic acid. Each virus was also tested against untreated cRBCs and desialylated cRBCs.
In vitro viral replication kinetics.
MDCK cells cultured in 24-well plates were inoculated in triplicate with CA/09 wt and mutant viruses for 1 h at 37°C at an MOI of 0.1. The supernatant was collected 0, 8, 24, 36, 48, and 72 h later and stored at −80°C until the samples were titrated on MDCK cells.
Statistical analysis.
The significance of difference between any two different groups was assessed by a nonparametric Mann-Whitney test using Prism (GraphPad Software). P values of <0.05 are considered significantly different.
SUPPLEMENTAL MATERIAL
ELISA of recombinant viruses. ELISA binding was performed using plates coated with each of the indicated recombinant viruses in triplicate. Serial dilutions of EM4C04 were added to the wells, followed by the addition of a secondary anti-human antibody conjugated to HRP. OD values were read at 450 nm. The negative control was wells that had PBS alone added without virus. Download Figure S1, PDF file, 0.4 MB.
In vitro replication kinetics of CA/09 wt and mutant viruses. CA/09 wt and mutant viruses were added in triplicate to MDCK cells cultured in 24-well plates for 1 h at 37°C at an MOI of 0.1. Supernatant was harvested at 0, 8, 24, 36, 48, and 72 h postinfection, and virus titers were determined in MDCK cells cultured in 96-well plates in quadruplicate. Viral titer is expressed as TCID50/ml. Download Figure S2, PDF file, 0.5 MB.
Weight loss and lethality in mice infected with the EM4C04 escape mutants. Weight loss (A) and percent survival (B) were monitored for 14 days after intranasal inoculation with 105 TCID50 of CA/09 escape mutants generated against EM4C04 in groups of five mice. Mice were euthanized if they lost at least 25% of their original body weight. In panel B, the viruses that caused no lethality are superimposed; this includes mock, EM30 (K123N), EM26 (K133T), EM22 (G134S), and EM06 (G158E). Only EM02 (D131E) and EM27 (K157N/S186P) caused lethality. Download Figure S3, PDF file, 4.5 MB.
Replication of CA/09 D131E and S186P mutant viruses in mice. The lungs (A and B) and nasal turbinates (C and D) from groups of four mice infected with biological and recombinant CA/09 wt and mutant viruses were harvested at days 2 and 4 postinfection. Tissues were homogenized, and titers were determined. Titers are expressed as log10 TCID50/g tissue. Each sample titer was determined in quadruplicate. The limit of detection for this assay was 1.8 log10 TCID50/g tissue and is highlighted by the broken black bar in each graph (*, P < 0.05). Download Figure S4, PDF file, 2.9 MB.
Comparison of dissociation constant (Kd) values.
ACKNOWLEDGMENTS
We thank Hong Jin, Zhongying Chen, Weijia Wang, and Amorsolo Suguitan, Jr., for providing H1N1 plasmids for virus rescue. We thank the staff of the Comparative Medicine Branch, NIAID, for technical support for animal studies performed at the NIH.
This work was conducted in part under a CRADA between MedImmune and NIAID/NIH. This research was supported in part by the Intramural Research Program of the NIH, NIAID. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Citation O’Donnell CD, et al. 2012. Antibody pressure by a human monoclonal antibody targeting the 2009 pandemic H1N1 virus hemagglutinin drives the emergence of a virus with increased virulence in mice. mBio 3(3):e00120-12. doi:10.1128/mBio.00120-12.
REFERENCES
- 1. Wright PF, Neumann G, Kawaoka Y. 2007. Orthomyxoviruses, p 1691–1740 In Knipe DM, Fields virology, 5th ed. Lippincott Williams & Wilkins, Philadelphia, PA. [Google Scholar]
- 2. Couch RB, Kasel JA. 1983. Immunity to influenza in man. Annu. Rev. Microbiol. 37:529–549 [DOI] [PubMed] [Google Scholar]
- 3. Potter CW, Oxford JS. 1979. Determinants of immunity to influenza infection in man. Br. Med. Bull. 35:69–75 [DOI] [PubMed] [Google Scholar]
- 4. Epstein SL, et al. 1993. Beta 2-microglobulin-deficient mice can be protected against influenza A infection by vaccination with vaccinia-influenza recombinants expressing hemagglutinin and neuraminidase. J. Immunol. 150:5484–5493 [PubMed] [Google Scholar]
- 5. Martinez O, Tsibane T, Basler CF. 2009. Neutralizing anti-influenza virus monoclonal antibodies: therapeutics and tools for discovery. Int. Rev. Immunol. 28:69–92 [DOI] [PubMed] [Google Scholar]
- 6. Gerhard W. 2001. The role of the antibody response in influenza virus infection. Curr. Top. Microbiol. Immunol. 260:171–190 [DOI] [PubMed] [Google Scholar]
- 7. Gerhard W. 1976. The analysis of the monoclonal immune response to influenza virus. II. The antigenicity of the viral hemagglutinin. J. Exp. Med. 144:985–995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Palese P, Shaw ML. 2007. Orthomyxoviridae: the viruses and their replication, p 1647–1689 In Knipe DM, Fields virology, vol 2, 5th ed. Lippincott Williams & Wilkins, Philadelphia, PA. [Google Scholar]
- 9. Hensley SE, et al. 2009. Hemagglutinin receptor binding avidity drives influenza A virus antigenic drift. Science 326:734–736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Caton AJ, Brownlee GG, Yewdell JW, Gerhard W. 1982. The antigenic structure of the influenza virus A/PR/8/34 hemagglutinin (H1 subtype). Cell 31:417–427 [DOI] [PubMed] [Google Scholar]
- 11. Raymond FL, Caton AJ, Cox NJ, Kendal AP, Brownlee GG. 1983. Antigenicity and evolution amongst recent influenza viruses of H1N1 subtype. Nucleic Acids Res. 11:7191–7203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Horimoto T, Kawaoka Y. 2005. Influenza: lessons from past pandemics, warnings from current incidents. Nat. Rev. Microbiol. 3:591–600 [DOI] [PubMed] [Google Scholar]
- 13. Kawaoka Y, Krauss S, Webster RG. 1989. Avian-to-human transmission of the PB1 gene of influenza A viruses in the 1957 and 1968 pandemics. J. Virol. 63:4603–4608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Garten RJ, et al. 2009. Antigenic and genetic characteristics of swine-origin 2009 A(H1N1) influenza viruses circulating in humans. Science 325:197–201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mak GC, et al. 2010. Association of D222G substitution in haemagglutinin of 2009 pandemic influenza A (H1N1) with severe disease. Euro Surveill. 15:19534 http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19534 [PubMed] [Google Scholar]
- 16. Kilander A, Rykkvin R, Dudman SG, Hungnes O. 2010. Observed association between the HA1 mutation D222G in the 2009 pandemic influenza A(H1N1) virus and severe clinical outcome, Norway 2009–2010. Euro Surveill. 15:19498 http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19498 [DOI] [PubMed] [Google Scholar]
- 17. World Health Organization 2009. Public health significance of virus mutation detected in Norway pandemic (H1N1) 2009. Pandemic (H1N1) 2009 briefing note 17. http://www.who.int/csr/disease/swineflu/notes/briefing_20091120/en/ [Google Scholar]
- 18. Chen H, et al. 2010. Quasispecies of the D225G substitution in the hemagglutinin of pandemic influenza A(H1N1) 2009 virus from patients with severe disease in Hong Kong, China. J. Infect. Dis. 201:1517–1521 [DOI] [PubMed] [Google Scholar]
- 19. Ikonen N, et al. 2010. Genetic diversity of the 2009 pandemic influenza A(H1N1) viruses in Finland. PLoS One 5:e13329 http://dx.doi.org/10.1371/journal.pone.0013329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wrammert J, et al. 2011. Broadly cross-reactive antibodies dominate the human B cell response against 2009 pandemic H1N1 influenza virus infection. J. Exp. Med. 208:181–193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Brownlee GG, Fodor E. 2001. The predicted antigenicity of the haemagglutinin of the 1918 Spanish influenza pandemic suggests an avian origin. Philos. Trans. R. Soc. Lond. B Biol. Sci. 356:1871–1876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yang H, Carney P, Stevens J. 2010. Structure and receptor binding properties of a pandemic H1N1 virus hemagglutinin. PLoS Curr. 2:RRN1152 http://dx.doi.org/10.1371/currents.RRN1152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Das SR, et al. 2010. Glycosylation focuses sequence variation in the influenza A virus H1 hemagglutinin globular domain. PLoS Pathog. 6:e1001211 http://dx.doi.org/10.1371/journal.ppat.1001211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tsuchiya E, et al. 2002. Effect of addition of new oligosaccharide chains to the globular head of influenza A/H2N2 virus haemagglutinin on the intracellular transport and biological activities of the molecule. J. Gen. Virol. 83:1137–1146 [DOI] [PubMed] [Google Scholar]
- 25. Wei CJ, et al. 2010. Cross-neutralization of 1918 and 2009 influenza viruses: role of glycans in viral evolution and vaccine design. Sci. Transl. Med. 2:24ra21 http://dx.doi.org/10.1126/scitranslmed.3000799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ye J, et al. 2010. Variations in the hemagglutinin of the 2009 H1N1 pandemic virus: potential for strains with altered virulence phenotype? PLoS Pathog. 6:e1001145 http://dx.doi.org/10.1371/journal.ppat.1001145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ilyushina NA, et al. 2010. Adaptation of pandemic H1N1 influenza viruses in mice. J. Virol. 84:8607–8616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Skehel JJ, Wiley DC. 2000. Receptor binding and membrane fusion in virus entry: the influenza hemagglutinin. Annu. Rev. Biochem. 69:531–569 [DOI] [PubMed] [Google Scholar]
- 29. Connor RJ, Kawaoka Y, Webster RG, Paulson JC. 1994. Receptor specificity in human, avian, and equine H2 and H3 influenza virus isolates. Virology 205:17–23 [DOI] [PubMed] [Google Scholar]
- 30. Rogers GN, Paulson JC. 1983. Receptor determinants of human and animal influenza virus isolates: differences in receptor specificity of the H3 hemagglutinin based on species of origin. Virology 127:361–373 [DOI] [PubMed] [Google Scholar]
- 31. Glaser L, Conenello G, Paulson J, Palese P. 2007. Effective replication of human influenza viruses in mice lacking a major alpha2,6 sialyltransferase. Virus Res. 126:9–18 [DOI] [PubMed] [Google Scholar]
- 32. Ning ZY, et al. 2009. Detection of expression of influenza virus receptors in tissues of BALB/c mice by histochemistry. Vet. Res. Commun. 33:895–903 [DOI] [PubMed] [Google Scholar]
- 33. Keleta L, Ibricevic A, Bovin NV, Brody SL, Brown EG. 2008. Experimental evolution of human influenza virus H3 hemagglutinin in the mouse lung identifies adaptive regions in HA1 and HA2. J. Virol. 82:11599–11608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Krause JC, et al. 2011. A broadly neutralizing human monoclonal antibody that recognizes a conserved, novel epitope on the globular head of the influenza H1N1 virus hemagglutinin. J. Virol. 85:10905–10908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Whittle JR, et al. 2011. Broadly neutralizing human antibody that recognizes the receptor-binding pocket of influenza virus hemagglutinin. Proc. Natl. Acad. Sci. U. S. A. 108:14216–14221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Manicassamy B, et al. 2010. Protection of mice against lethal challenge with 2009 H1N1 influenza A virus by 1918-like and classical swine H1N1 based vaccines. PLoS Pathog. 6:e1000745 http://dx.doi.org/10.1371/journal.ppat.1000745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Krause JC, et al. 2010. Naturally occurring human monoclonal antibodies neutralize both 1918 and 2009 pandemic influenza A (H1N1) viruses. J. Virol. 84:3127–3130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Chutinimitkul S, et al. 2010. Virulence-associated substitution D222G in the hemagglutinin of 2009 pandemic influenza A(H1N1) virus affects receptor binding. J. Virol. 84:11802–11813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Liu Y, et al. 2010. Altered receptor specificity and cell tropism of D222G hemagglutinin mutants isolated from fatal cases of pandemic A(H1N1) 2009 influenza virus. J. Virol. 84:12069–12074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Korteweg C, Gu J. 2008. Pathology, molecular biology, and pathogenesis of avian influenza A (H5N1) infection in humans. Am. J. Pathol. 172:1155–1170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. van Riel D, et al. 2006. H5N1 virus attachment to lower respiratory tract. Science 312:399. [DOI] [PubMed] [Google Scholar]
- 42. Shinya K, et al. 2006. Avian flu: influenza virus receptors in the human airway. Nature 440:435–436 [DOI] [PubMed] [Google Scholar]
- 43. Beigel JH, et al. 2005. Avian influenza A (H5N1) infection in humans. N. Engl. J. Med. 353:1374–1385 [DOI] [PubMed] [Google Scholar]
- 44. Writing Committee of the Second World Health Organization Consultation on Clinical Aspects of Human Infection with Avian Influenza A (H5N1) Virus 2008. Update on avian influenza A (H5N1) virus infection in humans. N. Engl. J. Med. 358:261–273 [DOI] [PubMed] [Google Scholar]
- 45. Wang TT, Parides MK, Palese P. 2012. Seroevidence for H5N1 influenza infections in humans: meta-analysis. Science 335:1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Powell TJ, et al. 2012. Identification of H5N1-specific T-cell responses in a high-risk cohort in Vietnam indicates the existence of potential asymptomatic infections. J. Infect. Dis. 205:20–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Nicholls JM, et al. 2007. Tropism of avian influenza A (H5N1) in the upper and lower respiratory tract. Nat. Med. 13:147–149 [DOI] [PubMed] [Google Scholar]
- 48. Uiprasertkul M, et al. 2005. Influenza A H5N1 replication sites in humans. Emerg. Infect. Dis. 11:1036–1041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Taubenberger JK, Morens DM. 2006. 1918 Influenza: the mother of all pandemics. Emerg. Infect. Dis. 12:15–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Kuroda M, et al. 2010. Characterization of quasispecies of pandemic 2009 influenza A virus (A/H1N1/2009) by de novo sequencing using a next-generation DNA sequencer. PLoS One 5:e10256 http://dx.doi.org/10.1371/journal.pone.0010256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Suguitan AL, et al. 2006. Live, attenuated influenza A H5N1 candidate vaccines provide broad cross-protection in mice and ferrets. PLoS Med. 3:e360 http://dx.doi.org/10.1371/journal.pmed.0030360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Reed LJ, Muench H. 1938. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 27:493–497 [Google Scholar]
- 53. Chen GL, et al. 2011. Comparison of a live attenuated 2009 H1N1 vaccine with seasonal influenza vaccines against 2009 pandemic H1N1 virus infection in mice and ferrets. J. Infect. Dis. 203:930–936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Lau YF, Tang LH, McCall AW, Ooi EE, Subbarao K. 2010. An adjuvant for the induction of potent, protective humoral responses to an H5N1 influenza virus vaccine with antigen-sparing effect in mice. J. Virol. 84:8639–8649 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
ELISA of recombinant viruses. ELISA binding was performed using plates coated with each of the indicated recombinant viruses in triplicate. Serial dilutions of EM4C04 were added to the wells, followed by the addition of a secondary anti-human antibody conjugated to HRP. OD values were read at 450 nm. The negative control was wells that had PBS alone added without virus. Download Figure S1, PDF file, 0.4 MB.
In vitro replication kinetics of CA/09 wt and mutant viruses. CA/09 wt and mutant viruses were added in triplicate to MDCK cells cultured in 24-well plates for 1 h at 37°C at an MOI of 0.1. Supernatant was harvested at 0, 8, 24, 36, 48, and 72 h postinfection, and virus titers were determined in MDCK cells cultured in 96-well plates in quadruplicate. Viral titer is expressed as TCID50/ml. Download Figure S2, PDF file, 0.5 MB.
Weight loss and lethality in mice infected with the EM4C04 escape mutants. Weight loss (A) and percent survival (B) were monitored for 14 days after intranasal inoculation with 105 TCID50 of CA/09 escape mutants generated against EM4C04 in groups of five mice. Mice were euthanized if they lost at least 25% of their original body weight. In panel B, the viruses that caused no lethality are superimposed; this includes mock, EM30 (K123N), EM26 (K133T), EM22 (G134S), and EM06 (G158E). Only EM02 (D131E) and EM27 (K157N/S186P) caused lethality. Download Figure S3, PDF file, 4.5 MB.
Replication of CA/09 D131E and S186P mutant viruses in mice. The lungs (A and B) and nasal turbinates (C and D) from groups of four mice infected with biological and recombinant CA/09 wt and mutant viruses were harvested at days 2 and 4 postinfection. Tissues were homogenized, and titers were determined. Titers are expressed as log10 TCID50/g tissue. Each sample titer was determined in quadruplicate. The limit of detection for this assay was 1.8 log10 TCID50/g tissue and is highlighted by the broken black bar in each graph (*, P < 0.05). Download Figure S4, PDF file, 2.9 MB.
Comparison of dissociation constant (Kd) values.