Abstract
Aims
A growing literature has documented the substantial prevalence of and putative mechanisms underlying co-occurring (i.e., concurrent or simultaneous) cannabis and tobacco use. Greater understanding of the clinical correlates of co-occurring cannabis and tobacco use may suggest how intervention strategies may be refined to improve cessation outcomes and decrease the public health burden associated with cannabis and tobacco use.
Methods
A systematic review of the literature on clinical diagnoses, psychosocial problems, and outcomes associated with co-occurring cannabis and tobacco use. Twenty-eight studies compared clinical correlates in co-occurring cannabis and tobacco users vs. cannabis or tobacco only users. These included studies of treatment-seekers in clinical trials and non-treatment-seekers in cross-sectional or longitudinal epidemiological or non-population-based surveys.
Results
Sixteen studies examined clinical diagnoses, four studies examined psychosocial problems, and 11 studies examined cessation outcomes in co-occurring cannabis and tobacco users (several studies examined multiple clinical correlates). Relative to cannabis use only, co-occurring cannabis and tobacco use was associated with a greater likelihood of cannabis use disorders, more psychosocial problems, and poorer cannabis cessation outcomes. Relative to tobacco use only, co-occurring use did not appear to be consistently associated with a greater likelihood of tobacco use disorders, more psychosocial problems, nor poorer tobacco cessation outcomes.
Conclusions
Cannabis users who also smoke tobacco are more dependent on cannabis, have more psychosocial problems, and have poorer cessation outcomes than those who use cannabis but not tobacco. The converse does not appear to be the case.
Keywords: cannabis, marijuana, tobacco, smoking, co-occurring, outcomes, interventions
Introduction
Concurrent use of cannabis and tobacco (i.e., across the lifespan or in a given time period) has become a prevalent phenomenon worldwide. Between 41% and 94% of adult cannabis users, and half of adult cannabis treatment-seekers, smoke tobacco [1-9]. Cannabis use is also high among tobacco smokers; between 25% and 52% of tobacco smokers use cannabis, and as many as 29% use cannabis at least weekly [10-12]. Simultaneous use of cannabis and tobacco (i.e., at the same time) is an increasingly popular practice [13-17]. Common methods for simultaneous use include rolling cannabis in cigar paper that contains tobacco (“blunts”), adding tobacco to cannabis wrapped in cigarette paper (“spliffs”), or smoking tobacco immediately after cannabis (“chasing”).
Several mechanisms may explain the strong relatedness of cannabis and tobacco use. First, the endocannabinoid system appears involved in addiction to tobacco [18-19]. Preclinical and clinical studies have shown that cannabinoid antagonists decrease the reinforcing effects of nicotine and increase the likelihood of tobacco abstinence [20]. Second, epidemiological evidence indicates that tobacco use often precedes the onset of cannabis use (“gateway theory”; [21]), although in some cases cannabis use may lead to tobacco initiation (“reverse gateway theory”; [22]). Third, shared genetic liability may explain the risk for cannabis dependence and amount of tobacco use, and for early-onset cannabis use and nicotine dependence [23-29]. Fourth, similar environmental or temperamental influences, such as cultural norms [15-16] or personality traits [30-31], may predispose individuals to onset of both cannabis and tobacco use. Fifth, the common route of administration and repeated pairing of cannabis and tobacco during simultaneous use suggest that each may serve as a behavioral cue for the other [1]. Sixth, tobacco may enhance subjective responses to cannabis [32; cf., 33].
One important gap in this growing literature is a comprehensive description of the clinical correlates associated with co-occurring use. Integrating existing data is important to understand the extent to which cannabis use may hinder some individuals’ ability to quit tobacco or vice versa [34-35]. Preliminary evidence indicates that tobacco may substitute for reduced cannabis consumption [36-37], and in some cases, cessation from both cannabis and tobacco may produce more severe withdrawal than cessation from either alone [38]. Furthermore, prior literature with other drug users has suggested that use of two drugs may influence response to treatment [39-44] and thus may have important treatment outcome implications.
This report provides a systematic review of the literature on co-occurring cannabis and tobacco use with particular focus on the association of co-occurring use with clinical severity and outcomes. The broader aims of this review are to highlight the clinical needs of co-occurring users and consider whether future interventions ought to be modified to meet these needs.
Method
This review encompasses studies that compare clinical correlates between co-occurring cannabis and tobacco users (referred to henceforth as “CT”) and users of cannabis or tobacco alone (“C” or “T”). Cannabis use, either alone or co-occurring, was defined as past or current use of cannabis, marijuana, hashish, oral tetrahydrocannabinol, or “joints.” Tobacco use, either alone or co-occurring, was defined as past or current use of cigarettes, cigars, pipes, or smokeless tobacco. Although it is difficult to quantify the amount of tobacco in “blunts” or “spliffs,” these methods were defined as co-occurring use, as was “chasing” cannabis with tobacco. Clinical correlates of interest were: (1) severity of use; (2) psychosocial problems; and (3) clinical outcomes. Severity of use was defined as Diagnostic and Statistical Manual of Mental Disorders (DSM-IV [45]) diagnoses or any individual symptom of cannabis or tobacco use disorders. Although severity of use could be defined in alternative ways (e.g., frequency/amount of use), diagnoses indicate how use interferes with an individual’s functioning and, thus, may be most informative to clinicians. Furthermore, accurately quantifying cannabis use is challenging due to varying quantities in routes of administration and delivery mechanisms [46]. Psychosocial problems were defined as psychiatric (e.g., affect or mood) symptoms or social/interpersonal difficulties. Clinical outcomes were defined as self-reported or biochemically-measured cessation or reduction of cannabis or tobacco.
The Figure outlines the search strategy that located relevant articles [47]. The keywords: “(cannabis or cannabin* or marijuana or marihuana) and (tobacco or cigar* or nicotin*)” were searched in the Ovid MEDLINE, Ovid PsycInfo, and PubMed databases. The search was limited to humans. After removing duplicates and including articles that were located through other sources (e.g., reference lists of relevant articles), 3,029 articles were screened. Articles were included if they examined adults or adolescents who reported any lifetime CT use and compared CT to C or T users. To be as inclusive as possible in this emerging area of research, articles were not excluded based on methodological rigor. The review includes treatment studies because they focus on clinical samples, thereby providing the most direct evidence of the clinical correlates. The review also includes cross-sectional epidemiological surveys, which include large, generalizable samples of co-occurring users, and longitudinal cohort studies, which highlight temporal relations between co-occurring use and clinical correlates [48]. Although not as rigorous, studies with non-population-based samples were included for the sake of completeness. Human laboratory experiments evaluating mechanisms of co-occurring use were not included. Twenty-eight articles were selected for inclusion in the review and are summarized in Table 1. Because the articles are characterized by heterogeneous methods and results, formal meta-analysis was not possible; hence, we provide a systematic rather than quantitative review.
Table 1.
Description of Included Studies.
| First Author, Year | Sample | Country | Type of Study | Sample Size | Timeframe of Co-Occurring Use | Definition of Cannabis Use | Definition of Tobacco Use | Comparison Group(s) |
|---|---|---|---|---|---|---|---|---|
| Abrantes, 2009 | 9th – 12th grade students | U.S. | Cross-sectional epidemiologic survey | 2033 | Lifetime | Any use | Daily use | T |
| Agrawal, Madden, 2008 | Young adult female twins (aged 18-29) | U.S. | Longitudinal cohort survey | 3787 | Lifetime | Any use | Regular use: history of either 100+ cigarettes, or 2-99 cigarettes but smoking as frequently as once per week | T |
| Agrawal, Pergadia, 2008 | Adults | U.S. | Cross-sectional epidemiologic survey | 1603 | Current | Any use in past 12 months | Any use in past 12 months | M |
| Agrawal & Lynskey, 2009 | Adults | U.S. | Cross-sectional epidemiologic survey | 43093 | Lifetime | Any use | Smoked: >100 cigarettes or >50 cigars or pipe >50 times;Smokeless: snuff >20 times or chewing tobacco >20 times | M |
| Agrawal, Lynskey, Madden, 2009 | Young adult female twins (aged 21-31) | U.S. | Longitudinal cohort survey | 3427 | Lifetime | Any use | Regular use: history of either 100+ cigarettes, or 2-99 cigarettes but smoking as frequently as once per week | C / Co-occurring CT during the lifespan but never simultaneously |
| Bonn-Miller, 2010 | Adults | U.S. | Cross-sectional observational study | 250 | Current | Any use in past 30 days | Any use in past 30 days | C/T |
| Caldeira, 2008 | First-year college students | U.S. | Cross-sectional cohort survey | 1253 | Current | Use ≥5 times in past year | Use ≥1 days in past month | C |
| Coffey, 2003 | Adolescents followed into young adulthood | Australia | Longitudinal cohort survey | 2032 | Current | Use at least “a few times” in past 6 months | Use in past month | C |
| de Dios, 2009 | Adolescents seeking treatment for substance abuse | U.S. | Community-based longitudinal study | 1779 | Current | Relapse between baseline and 12-month follow-up | Use at baseline or 12-month follow-up | Non-T or quit tobacco between baseline and 12-month follow-up |
| Degenhardt, 2001 | Adults | Australia | Cross-sectional epidemiologic survey | 10641 | Current | Use >5 times in past 12 months | Use in past 12 months | C |
| Degenhardt, 2010 | Adolescents followed into young adulthood | Australia | Longitudinal cohort survey | 1943 | Current | Use in past 6 months | Use in past month | T |
| Ford, 2002 | Adults | U.S. | Longitudinal epidemiologic survey | 431 | Current | Use in 30 days pre-baseline | Use in 3 months pre-baseline and usual pattern of smoking ≥ 10 cigarettes/day | T |
| Georgiades, 2007 | Adolescents followed into adulthood | Canada | Longitudinal cohort survey | 1282 | Current | Use in past 6 months | Daily use for continuous 30-day period in past 6 months | C/T |
| Gourlay, 1994 | Adults seeking treatment for tobacco smoking | Australia | Tobacco treatment trial | 1481 | Current | Use in past month | ≥ 15 cigarettes/day for ≥ 3 years | T |
| Gray, 2011 | Adolescents seeking treatment for attention-deficit/hyper-activity disorder and substance use disorders | U.S. | Randomized controlled trial | 303 | Current | Regular use (i.e., > 14 of 28 days) | Regular use (i.e., > 14 of 28 days) | C |
| Haskins, 2010 | Hispanic pregnant women | U.S. | Cross-sectional observational study | 351 | Current | Use in year prior to pregnancy | Use in year prior to pregnancy | T |
| Heffner, 2008 | Adults and adolescents receiving inpatient treatment for bipolar I disorder | U.S. | Cross-sectional observational study | 134 | Lifetime | Regular use (≥3 times/ week for ≥1 month) | Use in past 30 days | C |
| Humfleet, 1999 | Adults seeking treatment for tobacco smoking | U.S. | Tobacco treatment trial | 199 | Current | Use at baseline or during treatment | ≥10 cigarettes/day | T |
| Metrik, in press | Adults seeking treatment for tobacco smoking who were also heavy alcohol drinkers | U.S. | Randomized controlled trial | 236 | Current | Use in past month | >10 cigarettes/day for past year | T |
| Moore, 2001 | Adults seeking outpatient treatment for cannabis dependence | U.S. | Two cannabis treatment trials | 174 | Current | Met DSM-III-R or DSM-IV criteria for cannabis dependence | Any use | C who never smoked tobacco / C who were ex-tobacco smokers |
| Patton, 2005 | Adolescents followed into young adulthood | Australia | Longitudinal cohort survey | 1943 | Current | Use at age 20 | Use but not nicotine dependent at age 20 | T |
| Patton, 2006 | Adolescents followed into young adulthood | Australia | Longitudinal cohort survey | 1943 | Current | Cannabis dependence at age 24 | Daily use between ages 14 and 17 | C |
| Ream, 2008 | Cannabis users who appeared to be 17-35 years old | U.S. | Cross-sectional observational study | 481 | Current | Past year use | Past year “blunt” use, cannabis “chasing” with tobacco, cigar use, cigarette use | C “alone” |
| Stapleton, 2009 | Adults seeking tobacco treatment | United Kingdom | Randomized controlled trial | 100 | Current | Use in past 30 days | [Not described] | T |
| Suris, 2007 | Adolescents | Switzerland | Cross-sectional epidemiologic survey | 5263 | Current | Use in previous 30 days | ≥ 1 cigarette/day | C |
| Swift, 2008 | Adolescents followed into young adulthood | Australia | Longitudinal cohort survey | 1943 | Current | Use during adolescence | Use during adolescence | C |
| Timberlake, 2007 | Adolescents followed into young adulthood | U.S. | Longitudinal cohort survey | 5963 | Lifetime |
|
Use in past 30 days | T |
| Timberlake, 2009 | Adolescents and young adults (aged 12 – 25) | U.S. | Cross-sectional epidemiologic survey | 4348 | Current | Use in past month but never use of “blunts” | “Blunt” only use in past month | C who never used “blunts” |
Note. C = cannabis only users; T = tobacco only users. C/T indicates that two separate comparisons were made.
Results
How is co-occurring cannabis and tobacco use associated with severity of use?
Cannabis Use Disorders
Eleven studies examined the association of CT use with a diagnosis or individual symptoms of DSM-IV [45] cannabis use disorders. Of the 11 studies, seven compared the adjusted odds of having cannabis use disorders (Table 2), two compared the adjusted odds of endorsing symptoms of cannabis use disorders, and two compared unadjusted prevalence estimates of cannabis use disorders between CT and C users. The seven studies that reported adjusted odds ratios used C users as the referent group and adjusted for a range of confounding characteristics (e.g., demographic and psychiatric characteristics), thereby providing a rigorous test of the association of CT use with cannabis use disorders.
Table 2.
Association of Co-Occurring Cannabis and Tobacco vs. Cannabis Only Use with Cannabis Use Disorders.
| Study | Definition of Co-Occurring Use | Diagnosis | Diagnosis Lifetime or Current | Adjusted Odds Ratio |
|---|---|---|---|---|
| Agrawal & Lynskey, 2009 | Lifetime cannabis + smoked and smokeless tobacco | Cannabis abuse/dependence | Lifetime | 1.68* |
| Agrawal & Lynskey, 2009 | Lifetime cannabis + smoked tobacco | Cannabis abuse/dependence | Lifetime | 1.55* |
| Agrawal & Lynskey, 2009 | Lifetime cannabis + smokeless tobacco | Cannabis abuse/dependence | Lifetime | 1.04 |
| Agrawal, Lynskey, Madden, 2009 | Lifetime cannabis + regular cigarette | Cannabis abuse | Lifetime | 2.09* |
| Agrawal, Lynskey, Madden, 2009 | Lifetime cannabis + regular cigarette | Cannabis dependence | Lifetime | 2.30 |
| Coffey, 2003 | Young adult cannabis + adolescent persistent cigarette | Cannabis dependence at age 20 | Current | 1.9* |
| Coffey, 2003 | Young adult cannabis + adolescent daily cigarette | Cannabis dependence at age 20 | Current | 0.71 |
| Degenhardt, 2001 | Current cannabis + current tobacco | Cannabis abuse/dependence | Current | 5.00* |
| Degenhardt, 2001 | Current cannabis + former tobacco | Cannabis abuse/dependence | Current | 4.65* |
| Patton, 2006 | Young adult cannabis + adolescent daily cigarette | Cannabis dependence at age 24 | Current | 27* |
| Swift, 2008 | Adolescent cannabis + persistent cigarette | Cannabis dependence at age 24 | Current | 5.5* |
| Timberlake, 2009 | Current (past month) “blunt” only use | Cannabis abuse | Current (past month) | 2.2* |
| Timberlake, 2009 | Current (past month) “blunt” only use | Cannabis dependence | Current (past month) | 2.4* |
Note. Reference group in each comparison was cannabis only use. Except where noted, “current” refers to past 12 months.
p < .05
Two studies were large (range of N = 3427 – 43,093) U.S. surveys that compared the adjusted odds of a lifetime cannabis use disorder between CT and C users. A cross-sectional epidemiological survey reported that any lifetime use of cannabis plus smoked tobacco, but not smokeless tobacco, was associated with a significantly greater likelihood of cannabis abuse or dependence [1]. A longitudinal cohort study of young adult female twins reported that any lifetime use of cannabis plus regular cigarette smoking was associated with cannabis abuse but not dependence [49]; moreover, simultaneous CT use was associated with significantly greater odds of cannabis abuse but not dependence relative to concurrent CT use.
Two studies were large (range of N = 4348 - 10,641) cross-sectional epidemiological surveys that compared the adjusted odds of a current cannabis use disorder between CT and C users. Among Australian adults, current (i.e., past-year) cannabis use plus current or former tobacco smoking was associated with cannabis abuse/dependence [50]. Among U.S. adolescents and young adults, past-month smoking of “blunts” was associated with cannabis abuse and dependence [51]. This latter study did not report on non-“blunt” tobacco use (e.g., cigarettes).
Three studies were from the Victorian Adolescent Health Cohort Study, a large (N > 1520) longitudinal cohort of Australian adolescents who were followed into young adulthood. These studies reported that: (a) adolescent CT, relative to C, use was associated with significantly greater odds of cannabis dependence at age 24 [52]; (b) persistent cigarette smoking (i.e., in at least four of six waves of data collection) during adolescence plus cannabis use by age 20 was associated with cannabis dependence at age 20, but daily cigarette smoking in at least one adolescent wave was not [53]; and (c) daily cigarette smoking in at least one adolescent wave plus cannabis use by age 24 was associated with cannabis dependence at age 24 [54]. Thus, the severity or duration of cigarette smoking may play a role in the temporal relation between CT use and development of cannabis use disorders.
Two studies examined the adjusted odds of CT and C users endorsing individual symptoms of cannabis use disorders. Although DSM-IV [45] excludes withdrawal from the diagnostic criteria for cannabis dependence, several studies have documented the existence of the cannabis withdrawal syndrome [55]; thus, this review includes withdrawal as a symptom of cannabis use disorders. A large (N = 1603) cross-sectional epidemiological survey in the U.S. reported that CT, relative to C, users reported experiencing a greater number of cannabis withdrawal symptoms and were more likely to report past-year withdrawal symptoms of depressed mood, unpleasant dreams, headaches, sweating/heart-racing, nausea, and yawning [56]. In a cross-sectional non-population-based sample of 481 U.S. cannabis users aged 17-35, CT use in the form of “blunts” and “chasing” cannabis with tobacco was associated with five symptoms of current cannabis dependence, while C use in the form of “joints” or “pipes” was associated with only one symptom [57]. This study also examined tobacco use in the form of cigarettes and found that the number of days in which cannabis users smoked cigarettes was associated with one symptom of cannabis use disorders, and the number of cigarettes smoked in the prior day with two symptoms. Therefore, in this study the association between CT use and cannabis use disorders appears due to “blunt” use and “chasing” cannabis with tobacco, rather than cigarette use.
Two studies were cross-sectional studies with non-population-based U.S. samples and compared the unadjusted prevalence of cannabis use disorders between CT and C users. Therefore, findings might be better accounted for by other factors. Among 1253 first-year college students, the prevalence of current cannabis dependence was significantly greater in CT than C users (23% vs. 11%), although the prevalence of cannabis abuse did not differ (25% vs. 21%) [58]. Among 134 adolescent and adult patients with bipolar I disorder, the prevalence of lifetime cannabis use disorders was significantly greater in CT than C users (53% vs. 12%) [59].
Tobacco Use Disorders
Five studies assessed the association of CT use with a DSM-IV [45] diagnosis of nicotine dependence. All five studies compared the adjusted odds of having nicotine dependence between CT and T users, with T users as the referent group and adjusting for several confounding characteristics, thereby providing a rigorous test of the association of CT use with tobacco use disorders (Table 3).
Table 3.
Association of Co-Occurring Cannabis and Tobacco vs. Tobacco Only Use with Tobacco Use Disorders.
| Study | Definition of Co-Occurring Use | Diagnosis | Diagnosis Lifetime or Current | Adjusted Odds Ratio |
|---|---|---|---|---|
| Agrawal, Madden, 2008 | Lifetime cannabis + regular cigarette | Nicotine dependence | Lifetime | 2.80* |
| Degenhardt, 2010 | Adolescent weekly cannabis + cigarette at age 24 | Nicotine dependence at age 24 | Current | 1.3 |
| Degenhardt, 2010 | Adolescent occasional cannabis + cigarette at age 24 | Nicotine dependence at age 24 | Current | 1.3 |
| Patton, 2005 | Daily cannabis + cigarette at age 20 | Nicotine dependence at age 24 | Current | 3.6* |
| Patton, 2005 | Weekly cannabis + cigarette at age 20 | Nicotine dependence at age 24 | Current | 1.6 |
| Patton, 2005 | Monthly cannabis + cigarette at age 20 | Nicotine dependence at age 24 | Current | 1.7 |
| Timberlake, 2007 | Adolescent lifetime cannabis > 10 times + cigarette between ages 23 and 27 | Nicotine dependence | Lifetime | 1.89* |
| Timberlake, 2007 | Adolescent lifetime cannabis 1-10 times + cigarette between ages 23 and 27 | Nicotine dependence | Lifetime | 1.12 |
| Timberlake, 2007 | Adolescent lifetime cannabis > 10 times + cigarette between ages 18 and 22 | Nicotine dependence | Lifetime | 0.58 |
| Timberlake, 2007 | Adolescent lifetime cannabis 1-10 times + cigarette between ages 18 and 22 | Nicotine dependence | Lifetime | 1.00 |
| Timberlake, 2007 | Adolescent past-month cannabis + cigarette between ages 23 and 27 | Nicotine dependence | Lifetime | 1.83* |
| Timberlake, 2007 | Adolescent past-month cannabis + cigarette between ages 18 and 22 | Nicotine dependence | Lifetime | 0.64 |
| Timberlake, 2009 | Current (past month) “blunt” only use | Nicotine dependence | Current (past month) | 1.4 |
Note. Reference group in each study was tobacco only use. Except where noted, “current” refers to past 12 months. NS = not significant.
p < .05
Two studies were longitudinal cohort studies with large U.S. samples that compared the adjusted odds of lifetime nicotine dependence between CT and T users. Among 3787 young adult female twins, lifetime cannabis use plus regular cigarette smoking was associated with a significantly greater likelihood of nicotine dependence [60]. Among 5963 adolescents, using cannabis more than ten times in adolescence or in the past month plus cigarette smoking in young adulthood was significantly associated with nicotine dependence for individuals between the ages of 23 and 27, but using cannabis fewer than ten times was not [61]. Adolescent cannabis use plus cigarette smoking in young adulthood was not associated with nicotine dependence for individuals between the ages of 18 and 22 [61].
Four studies compared the adjusted odds of current nicotine dependence between CT and T users. The aforementioned U.S. longitudinal study reported that any frequency of adolescent cannabis use plus young adult cigarette use was not associated with nicotine dependence but did not report statistical results [61]. Two studies from the longitudinal Victorian Adolescent Health Cohort reported that: (1) neither occasional nor weekly cannabis use during adolescence was associated with nicotine dependence at age 24 [62]; and (2) daily, but not monthly or weekly, cannabis use at age 21 was significantly associated with nicotine dependence at age 24 [22]. The aforementioned cross-sectional epidemiological survey with U.S. adolescents and young adults reported no association between “blunt” use and nicotine dependence; however, as discussed earlier, it did not examine the association of cannabis plus other tobacco use with nicotine dependence [51].
How is co-occurring cannabis and tobacco use associated with psychosocial problems?
Four studies compared psychosocial problems between CT and C users. Among a cross-sectional sample of 250 U.S. adults in a laboratory study on emotion, unadjusted univariate analyses indicated that CT users reported more anxiety symptoms but did not differ in negative affectivity, anhedonic depressive symptoms or alcohol consumption from C users [63]. The following studies reported results from adjusted multivariate analyses. Among a sample of 174 U.S. adults seeking treatment for cannabis dependence, CT, relative to C, users reported fewer years of education, greater psychiatric severity, and more legal problems [64]. Among 5263 Swiss adolescents in a cross-sectional epidemiological survey, CT, relative to C, users were less likely to live with both parents and to have good grades, and more likely to have been drunk in the previous 30 days [65]. Among 1282 Canadian adolescents in a longitudinal cohort study, CT, relative to C, users in adolescence reported decreased life satisfaction, fewer years of education, and increased depressive symptoms in adulthood [66].
Two of these studies also compared psychosocial problems between CT and T users. In adjusted analyses among the longitudinal cohort of Canadian adolescents [66], CT users during adolescence did not differ from T users on life satisfaction, years of education, or depressive symptoms during adulthood; interestingly, adolescent T users reported worse physical health during adulthood than did CT users. In unadjusted analyses among the cross-sectional sample of U.S. adults [63], CT users reported consuming more alcohol than T users, but reported less negative affectivity and did not differ in number of anhedonic depressive symptoms.
How is co-occurring cannabis and tobacco use associated with clinical outcomes?
Cannabis Outcomes
Three studies of individuals receiving substance-related treatment in the U.S. examined whether CT users experienced more difficulty quitting cannabis than C users (Table 4). After adjusting for intake level of cannabis, alcohol, and other drug use among 1779 U.S. adolescents in a multisite treatment study, cannabis users who either smoked tobacco persistently or initiated tobacco smoking during treatment reported a greater likelihood of cannabis relapse than those who did not smoke tobacco or quit during treatment [67]. The following studies did not adjust for potential differences between CT and C users. Among 174 adults, CT users reported a significantly lower percent of cannabis-negative urine tests and significantly fewer continuous weeks of cannabis abstinence during treatment than ex-tobacco smokers, but did not differ from never-tobacco smokers [64]. Among 303 adolescents with attention-deficit/hyperactivity disorder in a multisite treatment study targeting non-nicotine substance use disorders, CT users reported a slower rate of change in their cannabis use than C users [68].
Table 4.
Association of Co-Occurring Cannabis and Tobacco vs. Cannabis Only Use with Cannabis Outcomes.
| Study | Group of Co-Occurring Users | Comparison Group | Outcome | Statistic |
|---|---|---|---|---|
| de Dios, 2009 | Cannabis users + persistent tobacco smokers | Cannabis users + tobacco quitters | Adjusted odds ratio of cannabis relapse | 1.71* |
| de Dios, 2009 | Cannabis users + tobacco initiators | Cannabis users + tobacco quitters | Adjusted odds ratio of cannabis relapse | 3.08* |
| Gray, 2011 | Regular cannabis users + regular cigarette smokers | Regular cannabis users | Change in days of cannabis use from baseline to week 1 of treatment | β (slope) = -1.33 vs. -3.17* |
| Gray, 2011 | Regular cannabis users + regular cigarette smokers | Regular cannabis users | Change in cannabis joints/day from baseline to week 1 of treatment | β (slope) = -1.15 vs. -2.34* |
| Moore, 2001 | Current dependent cannabis users + cigarette smokers | Current dependent cannabis users + ex-cigarette smokers | % cannabis-negative urine tests during treatment | 24.4 vs. 49.4* |
| Moore, 2001 | Current dependent cannabis users + cigarette smokers | Current dependent cannabis users + never-cigarette smokers | % cannabis-negative urine tests during treatment | 24.4 vs. 35.0 |
| Moore, 2001 | Current dependent cannabis users + cigarette smokers | Current dependent cannabis users + ex-cigarette smokers | Mean weeks of continuous cannabis abstinence during treatment | 2.8 vs. 5.6* |
| Moore, 2001 | Current dependent cannabis users + cigarette smokers | Current dependent cannabis users + never-cigarette smokers | Mean weeks of continuous cannabis abstinence during treatment | 2.8 vs. 3.7 |
Note. Asterisks indicate that co-occurring users reported significantly poorer outcomes than cannabis only users.
Tobacco Outcomes
Eight studies examined whether CT users experienced more difficulty quitting tobacco use than T users (Table 5). Four of these studies were of adults seeking treatment for tobacco smoking (range of N = 100 – 1481). Two U.S. studies reported no difference in tobacco outcomes between CT and T users [69-70]; one of these studies adjusted for between-group differences [70], although the other did not provide descriptive data or results of statistical tests [69]. In contrast, a study in the United Kingdom reported that a smaller percent of CT than T users achieved biochemically-verified smoking abstinence at the end of treatment [71], and a study in Australia reported that the odds of achieving smoking abstinence were significantly lower for CT than T users; however, results in these two studies were not adjusted for confounders [71-72].
Table 5.
Association of Co-Occurring Cannabis and Tobacco vs. Tobacco Only Use with Tobacco Outcomes.
| Study | Group of Co-Occurring Users | Outcome | Statistic |
|---|---|---|---|
| Abrantes, 2009 | Any lifetime cannabis use + lifetime daily tobacco smoker | Adjusted odds ratio of making tobacco smoking quit attempt in the last year | 0.80 |
| Abrantes, 2009 | Any lifetime cannabis use + lifetime daily tobacco smoker | Adjusted odds ratio of successfully quitting tobacco in the last year | 0.38* |
| Ford, 2002 | Past-month cannabis use (any) + tobacco smoker | Adjusted odds ratio of continued tobacco smoking at 13 years | 1.94* |
| Ford, 2002 | Past-month cannabis use (daily for > 2 weeks) + tobacco smoker | Adjusted odds ratio of continued tobacco smoking at 13 years | 3.09 |
| Gourlay, 1994 | Past-month cannabis users + tobacco smokers | Unadjusted odds ratio of non-smoking for 28 days prior to week 26 follow-up | 0.4* |
| Haskins, 2010 | Daily cannabis users + tobacco smokers | Adjusted odds ratio of quitting smoking during pregnancy | 0.54* |
| Haskins, 2010 | Weekly cannabis users + tobacco smokers | Adjusted odds ratio of quitting smoking during pregnancy | 1.00 |
| Haskins, 2010 | Monthly cannabis users + tobacco smokers | Adjusted odds ratio of quitting smoking during pregnancy | 0.99 |
| Metrik, in press | Weekly cannabis user + tobacco smoker | Adjusted odds ratio of 7-day point prevalence smoking abstinence | 1.13 |
| Metrik, in press | Infrequent cannabis user + tobacco smoker | Adjusted odds ratio of 7-day point prevalence smoking abstinence | 0.96 |
| Patton, 2005 | Daily cannabis use + cigarette smoking at age 20 | Adjusted odds ratio of no tobacco use in month before age 20 assessment | 0.7 |
| Patton, 2005 | Weekly cannabis use + cigarette smoking at age 20 | Adjusted odds ratio of no tobacco use in month before age 20 assessment | 1.0 |
| Patton, 2005 | Monthly cannabis use + cigarette smoking at age 20 | Adjusted odds ratio of no tobacco use in month before age 20 assessment | 0.8 |
| Stapleton, 2009 | Cannabis use in past 30 days + cigarette smoking | Percent in group with biochemically-verified tobacco abstinence for final 2 weeks of treatment | 40% vs. 55.3%* |
Note. Comparison group for all studies was group of tobacco only smokers. Asterisks indicate that co-occurring users reported significantly poorer outcomes than tobacco only smokers.
Four studies involved U.S. non-treatment-seeking tobacco smokers; all four studies reported results from adjusted analyses. In a longitudinal epidemiological survey of 431 adults [73] and a cross-sectional non-population-based study of 351 adult Hispanic pregnant women [74], CT users reported more difficulty quitting tobacco relative to T users. A cross-sectional epidemiological survey of 2033 adolescents reported that CT users were less likely to successfully quit tobacco (i.e., to not smoke tobacco in the last 30 days) than T users but did not differ on initiation of a tobacco quit attempt [75]. The Victorian Adolescent Health Cohort Study reported no differences in tobacco cessation between these groups at age 20 [22].
Four of these studies reported on the association between frequency of cannabis use and tobacco-related outcomes. The study of U.S. Hispanic pregnant women reported that poorer tobacco outcomes were specific to daily cannabis users [74]. The U.S. longitudinal epidemiological survey reported converse findings; poorer tobacco outcomes were specific to past-month users of any cannabis (i.e., past-month daily cannabis users did not report poorer tobacco outcomes than T users) [73]. The two other studies reported that tobacco outcomes did not differ based on frequency of cannabis use [22,70].
Discussion
This systematic review indicates that relative to cannabis only use, co-occurring cannabis and tobacco use was associated with a greater likelihood of cannabis use disorders, more psychosocial problems, and poorer cannabis cessation outcomes. Relative to tobacco only use, co-occurring use did not appear to be consistently associated with a greater likelihood of tobacco use disorders, more psychosocial problems, nor poorer tobacco cessation outcomes. However, the number of studies addressing each of our target questions was small, and comparisons were not consistently adjusted for potential confounders; thus, conclusions should be considered preliminary.
The relatively consistent finding that, in comparison to cannabis only users, co-occurring cannabis and tobacco users were more likely to report cannabis use disorders and higher levels of psychosocial problems is of clinical relevance for several reasons. First, consistent with findings in alcohol users [76], tobacco use in cannabis users seems to serve as an indicator of more severe clinical problems and, thus, greater need for treatment. As a result of greater cannabis-related problems, co-occurring users may find it more difficult to stop using cannabis (i.e., due to interference with multiple domains of functioning). Second, assessment of tobacco use among cannabis treatment-seekers should become more routine. Assessment of tobacco is standardized and brief, and would be consistent with current clinical guidelines recommended for health care settings [77]. Third, co-occurring users having more severe clinical problems underscores the need to appropriately match type and intensity of treatment to individuals’ presenting problems.
In contrast, this group of studies did not suggest that co-occurring cannabis and tobacco users are more likely than tobacco users to report nicotine dependence or psychosocial problems. A likely explanation is the strong relationship between tobacco use and nicotine dependence/psychosocial problems, i.e., the majority of cigarette smokers are nicotine dependent [78], and tobacco smoking is prevalent among individuals with psychosocial difficulties [79-82]. Therefore, cannabis use may not significantly add to the association between tobacco smoking and related problems. Another explanation for the mixed evidence concerns the frequency of cannabis use. In the reviewed studies where any cannabis use was examined, there was not a consistent association with nicotine dependence; however, two of the three studies that examined more frequent cannabis use did report a positive association [22,61-62]. Thus, contribution to tobacco-related problems may be seen only at higher levels of cannabis use. To better understand how the association between CT use and tobacco-related problems relates to the intensity of cannabis use, future studies might incorporate recently-developed methods of assessing frequency and quantity of cannabis use [83], rather than rely on “ever vs. never” distinctions of use.
The third conclusion is that co-occurring tobacco use may contribute to poorer cannabis cessation outcomes. Empirically-based interventions for cannabis use [84] have yet to evaluate interventions also targeting tobacco; therefore, it is unclear whether targeting both would improve outcomes for co-occurring users. Historically, tobacco smoking has not been addressed in interventions for alcohol or illicit drugs out of concern that it might negatively affect compliance or compromise recovery from alcohol or drugs. More recently, however, studies have not shown a negative effect of tobacco-related interventions on outcomes in substance abusing patients [85-86]. It should be noted that the three reviewed studies on the effect of tobacco on cannabis outcomes [64, 67-68] reported different outcome indices and did not consistently control for possibly confounding factors, making it difficult to confidently synthesize results and rendering our conclusion tentative. To better evaluate the potential causal nature of tobacco smoking on cannabis cessation outcomes, future prospective comparative clinical trials that test the effect of simultaneously treating cannabis and tobacco on cannabis cessation outcomes are needed; such studies should be consistent in their reporting of cannabis-related outcomes [87] and statistically adjust for potential population differences.
Evidence on the association of co-occurring cannabis and tobacco use with tobacco cessation outcomes was less consistent. The majority of the reviewed studies utilized sound methodologies, in that outcome measures were usually adjusted for confounders, were similar across studies, and followed recommendations for the reporting of tobacco outcomes [88]. Given the current literature, it is unclear whether addressing cannabis use in the context of tobacco interventions may improve tobacco cessation outcomes. However, the fact that reviewed studies detected either no effect or a negative effect of cannabis use on tobacco outcomes, plus the illicit status of cannabis, would suggest that cannabis use be addressed in tobacco interventions.
Strengths of this review include its focused scope, systematic search for relevant articles, and inclusion of international and large, population-based samples. Limitations include variability in how CT use and clinical correlates were measured, and inclusion of studies with potential methodological weaknesses. However, some evidence suggests scales of methodological rigor are problematic [89], and given this nascent area of research, we aimed to be inclusive with studies. To mitigate limitations, we have highlighted studies’ weaknesses when appropriate. Another limitation is the lack of findings regarding alternative indices of severity of cannabis and tobacco use (e.g., quantity of cannabis use); however, given variability in the measurement of alternative indices, we have focused on the standardized index of substance abuse/dependence diagnosis as the main indicator of severity of use.
Because this is a relatively new area of research, the literature has not yet addressed several important clinical questions, such as:
How should future interventions address use of both cannabis and tobacco? The reviewed literature suggests that future interventions for co-occurring users might address both cannabis and tobacco to improve cessation outcomes. As a first test of the benefit of a combined intervention, treatment-seeking cannabis users who smoke tobacco could be randomized to receive a psychosocial intervention that addresses both cannabis and tobacco use vs. cannabis use only. Outcomes to measure the intervention’s impact could include treatment acceptability and biochemically-confirmed cannabis and tobacco abstinence at the end of treatment and during follow-up. If a combined intervention is found to be efficacious and acceptable to patients, a subsequent test could compare a concurrent cannabis and tobacco intervention vs. a delayed tobacco intervention; this type of design would be similar to that utilized by Joseph et al. [90] with alcohol-dependent smokers.
How is co-occurring cannabis and tobacco use associated with other indices of clinical severity? The reviewed studies examined the severity of co-occurring use by comparing rates of cannabis and tobacco use disorders in co-occurring vs. single substance users, and some also compared the amount/frequency of use [49,63-65,67-70]. However, the literature lacks data on other indices of severity of use, such as scores on self-report assessments of substance-related problems (e.g., Marijuana Problems Scale [91]) and biological measures of use (e.g., cotinine). The reviewed studies also examined the severity of co-occurring use by comparing psychiatric symptoms, but future studies might examine psychiatric disorders and a wider variety of psychosocial problems (e.g., unemployment). Comparisons of multiple indices of severity of use, beyond diagnostic criteria alone, can provide a more complete picture of the severity of co-occurring use and better highlight the treatment needs of co-occurring users.
Other potentially valuable areas of future research include examination of other clinically-relevant outcomes (e.g., cognition); tests of the specificity of the association of cannabis and tobacco use with clinical correlates; and evaluation of mechanisms of cessation outcomes. Ultimately, more complete understanding of the clinical impact of cannabis and tobacco use will assist in the refinement of intervention strategies that may aid in decreasing the public health burden associated with cannabis and tobacco use.
Figure 1.
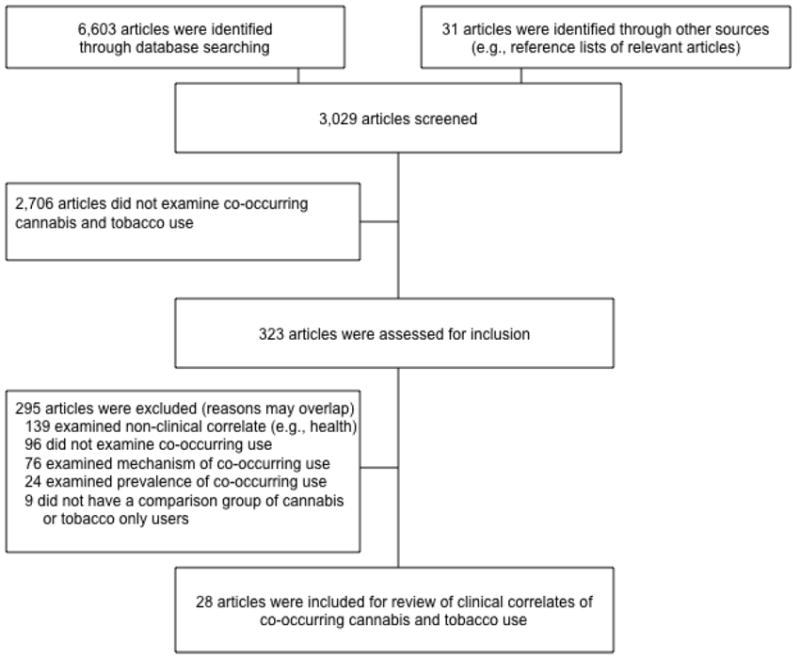
Summary of the article selection process as recommended by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement.
Acknowledgments
Funding for this research was provided by National Institute on Drug Abuse grants T32-DA007238 (ENP), R01-DA023526 (AJB), R01-DA015186 (AJB), and P50-DA009241 (KMC). Dr. Budney has consulted with GW Pharmaceuticals. The authors are under no contractual constraints on publishing imposed by the funders.
Footnotes
Declaration of Interest: Drs. Peters and Carroll have no conflicts to declare.
References
*Studies included in the review are marked with an asterisk
- 1*.Agrawal A, Lynskey MT. Tobacco and cannabis co-occurrence: Does route of administration matter? Drug Alcohol Depend. 2009;99:240–7. doi: 10.1016/j.drugalcdep.2008.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clough AR, D’Abbs P, Cairney S, Gray D, Maruff P, Parker R, et al. Emerging patterns of cannabis and other substance use in Aboriginal communities in Arnhem Land, Northern Territory: A study of two communities. Drug Alcohol Rev. 2004;23:381–90. doi: 10.1080/09595230412331324509. [DOI] [PubMed] [Google Scholar]
- 3.Martin CS, Clifford PR, Clapper RL. Patterns and predictors of simultaneous and concurrent use of alcohol, tobacco, marijuana, and hallucinogens in first-year college students. J Subst Abuse. 1992;4:319–26. doi: 10.1016/0899-3289(92)90039-z. [DOI] [PubMed] [Google Scholar]
- 4.Richter KP, Kaur H, Resnicow K, Nazir N, Mosier MC, Ahluwalia JS. Cigarette smoking among marijuana users in the United States. Subst Abuse. 2005;25:35–43. doi: 10.1300/j465v25n02_06. [DOI] [PubMed] [Google Scholar]
- 5.Rigotti NA, Lee JE, Wechsler H. US college students’ use of tobacco products: Results of a national survey. JAMA. 2000;284:699–705. doi: 10.1001/jama.284.6.699. [DOI] [PubMed] [Google Scholar]
- 6.Tullis LM, Dupont R, Frost-Pineda K, Gold MS. Marijuana and tobacco: A major connection? J Addict Dis. 2003;22:51–62. doi: 10.1300/J069v22n03_05. [DOI] [PubMed] [Google Scholar]
- 7.Budney AJ, Higgins ST, Radonovich KJ, Novy PL. Adding voucher-based incentives to coping skills and motivational enhancement improves outcomes during treatment for marijuana dependence. J Consult Clin Psychol. 2000;68:1051–61. doi: 10.1037//0022-006x.68.6.1051. [DOI] [PubMed] [Google Scholar]
- 8.Budney AJ, Moore BA, Rocha HL, Higgins ST. Clinical trial of abstinence-based vouchers and cognitive-behavioral therapy for cannabis dependence. J Consult Clin Psychol. 2006;74:307–16. doi: 10.1037/0022-006X.4.2.307. [DOI] [PubMed] [Google Scholar]
- 9.Kadden RM, Litt MD, Kabela-Cormier E, Petry NM. Abstinence rates following behavioral treatments for marijuana dependence. Addict Behav. 2007;32:1220–36. doi: 10.1016/j.addbeh.2006.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leatherdale ST, Ahmed R, Kaiserman M. Marijuana use by tobacco smokers and nonsmokers: Who is smoking what? CMAJ. 2006;174:1399. doi: 10.1503/cmaj.051614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leatherdale ST, Hammond DG, Kaiserman M, Ahmed R. Marijuana and tobacco use among young adults in Canada: Are they smoking what we think they are smoking? Cancer Causes Control. 2007;18:391–7. doi: 10.1007/s10552-006-0103-x. [DOI] [PubMed] [Google Scholar]
- 12.Substance Abuse and Mental Health Services Administration. Results from the 2004 National Survey on Drug Use and Health: National Findings. Rockville, MD: NSDUH Series H-28. DHHS Pub. No. (SMA) 05-4062; 2005. [Google Scholar]
- 13.Akre C, Michaud P-A, Berchtold A, Suris J-C. Cannabis and tobacco use: Where are the boundaries? A qualitative study on cannabis consumption modes among adolescents. Health Educ Res. 2010;25:74–82. doi: 10.1093/her/cyp027. [DOI] [PubMed] [Google Scholar]
- 14.Barrett SP, Darredeau C, Pihl RO. Patterns of simultaneous polysubstance use in drug using university students. Hum Psychopharmacol. 2006;21:255–63. doi: 10.1002/hup.766. [DOI] [PubMed] [Google Scholar]
- 15.Golub A, Johnson BD, Dunlap E. The growth in marijuana use among American youths during the 1990s and the extent of blunt smoking. J Ethn Subst Abuse. 2005;4:1–21. doi: 10.1300/J233v04n03_01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kelly BC. Bongs and blunts: Notes from a suburban marijuana subculture. J Ethn Subst Abuse. 2005;4:81–97. doi: 10.1300/J233v04n03_04. [DOI] [PubMed] [Google Scholar]
- 17.Soldz S, Huyser DJ, Dorsey E. The cigar as a drug delivery device: Youth use of blunts. Addiction. 2003;98:1379–86. doi: 10.1046/j.1360-0443.2003.00492.x. [DOI] [PubMed] [Google Scholar]
- 18.Castañe A, Berrendero F, Maldonado R. The role of the cannabinoid system in nicotine addiction. Pharmacol Biochem Be. 2005;81:381–6. doi: 10.1016/j.pbb.2005.01.025. [DOI] [PubMed] [Google Scholar]
- 19.Maldonado R, Valverde O, Berrendero F. Involvement of the endocannabinoid system in drug addiction. Trends Neurosci. 2006;29:225–32. doi: 10.1016/j.tins.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 20.Le Foll B, Forget B, Aubin H-J, Goldberg SR. Blocking cannabinoid CB1 receptors for the treatment of nicotine dependence: Insights from pre-clinical and clinical studies. Addict Biol. 2008;13:239–52. doi: 10.1111/j.1369-1600.2008.00113.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kandel DB, editor. Stages and pathways of drug involvement: Examining the gateway hypothesis. Cambridge, UK: Cambridge University Press; 2002. [Google Scholar]
- 22*.Patton GC, Coffey C, Carlin JB, Sawyer SM, Lynskey M. Reverse gateways? Frequent cannabis use as a predictor of tobacco initiation and nicotine dependence. Addiction. 2005;100:1518–25. doi: 10.1111/j.1360-0443.2005.01220.x. [DOI] [PubMed] [Google Scholar]
- 23.Agrawal A, Silberg JL, Lynskey MT, Maes HH, Eaves LJ. Mechanisms underlying the lifetime co-occurrence of tobacco and cannabis use in adolescent and young adult twins. Drug Alcohol Depend. 2010;108:49–55. doi: 10.1016/j.drugalcdep.2009.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen X, Williamson VS, An S-S, Hettema JM, Aggen SH, Neale MC, et al. Cannabinoid receptor 1 gene association with nicotine dependence. Arch Gen Psychiat. 2008;65:816–24. doi: 10.1001/archpsyc.65.7.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Neale MC, Harvey E, Maes HHM, Sullivan PF, Kendler KS. Extensions to the modeling of initiation and progression: Applications to substance use and abuse. Behav Genet. 2006;36:507–24. doi: 10.1007/s10519-006-9063-x. [DOI] [PubMed] [Google Scholar]
- 26.Xian H, Scherrer JF, Grant JD, Eisen SA, True WR, Jacob T, et al. Genetic and environmental contributions to nicotine, alcohol and cannabis dependence in male twins. Addiction. 2008;103:1391–8. doi: 10.1111/j.1360-0443.2008.02243.x. [DOI] [PubMed] [Google Scholar]
- 27.Young SE, Rhee SH, Stallings MC, Corley RP, Hewitt JK. Genetic and environmental vulnerabilities underlying adolescent substance use and problem use: General or specific? Behav Genet. 2006;36:603–15. doi: 10.1007/s10519-006-9066-7. [DOI] [PubMed] [Google Scholar]
- 28.Anney RJL, Lotfi-Miri M, Olsson CA, Reid SC, Hemphill SA, Patton GC. Variation in the gene coding for the M5 Muscarinic receptor (CHRM5) influences cigarette dose but is not associated with dependence to drugs of addiction: Evidence from a prospective population based cohort study of young adults. BMC Genet. 2007;8:46–54. doi: 10.1186/1471-2156-8-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Agrawal A, Lynskey MT, Pergadia ML, Bucholz KK, Heath AC, Martin NG, et al. Early cannabis use and DSM-IV nicotine dependence: A twin study. Addiction. 2008;103:1896–1904. doi: 10.1111/j.1360-0443.2008.02354.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brook JS, Lee JY, Finch SJ, Brown EN. Course of comorbidity of tobacco and marijuana use: Psychosocial risk factors. Nicotine Tob Res. 2010;12:474–82. doi: 10.1093/ntr/ntq027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Creemers HE, Korhonen T, Kaprio J, Vollebergh WAM, Ormel J, Verhulst FC, et al. The role of temperament in the relationship between early onset of tobacco and cannabis use: The TRAILS study. Drug Alcohol Depend. 2009;104:113–8. doi: 10.1016/j.drugalcdep.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 32.Penetar DM, Kouri EM, Gross MM, McCarthy EM, Rhee CK, Peters EN, et al. Transdermal nicotine alters some of marihuana’s effects in male and female volunteers. Drug Alcohol Depend. 2005;79:211–23. doi: 10.1016/j.drugalcdep.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 33.Cooper ZD, Haney M. Comparison of subjective, pharmacokinetic, and physiological effects of marijuana smoked as joints and blunts. Drug Alcohol Depend. 2009;103:107–13. doi: 10.1016/j.drugalcdep.2009.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Amos A, Wiltshire S, Bostock Y, Haw S, McNeill A. ‘You can’t go without a fag…you need it for your hash’ – A qualitative exploration of smoking, cannabis and young people. Addiction. 2004;99:77–81. doi: 10.1111/j.1360-0443.2004.00531.x. [DOI] [PubMed] [Google Scholar]
- 35.Highet G. The role of cannabis in supporting young people’s cigarette smoking: A qualitative exploration. Health Educ Res. 2004;19:635–43. doi: 10.1093/her/cyg089. [DOI] [PubMed] [Google Scholar]
- 36.Copersino ML, Boyd SJ, Tashkin DP, Huestis MA, Heishman SJ, Dermand JC, et al. Cannabis withdrawal among non-treatment-seeking adult cannabis users. Am J Addiction. 2006;15:8–14. doi: 10.1080/10550490500418997. [DOI] [PubMed] [Google Scholar]
- 37.Schaub M, Gmel G, Annaheim B, Mueller M, Schwappach D. Leisure time activities that predict initiation, progression and reduction of cannabis use: A prospective, population-based panel survey. Drug Alcohol Rev. 2010;29:378–84. doi: 10.1111/j.1465-3362.2009.00156.x. [DOI] [PubMed] [Google Scholar]
- 38.Vandrey RG, Budney AJ, Hughes JR, Liguori A. A within-subject comparison of withdrawal symptoms during abstinence from cannabis, tobacco, and both substances. Drug Alcohol Depend. 2008;92:48–54. doi: 10.1016/j.drugalcdep.2007.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bobo JK, Gilchrist LD, Schilling RF, Noach B, Schinke SP. Cigarette smoking cessation attempts by recovering alcoholics. Addict Behav. 1987;12:209–15. doi: 10.1016/0306-4603(87)90030-x. [DOI] [PubMed] [Google Scholar]
- 40.Budney AJ, Higgins ST, Bickel WK. Nicotine and caffeine use in cocaine dependent individuals. J Subst Abuse Treat. 1993;5:117–30. doi: 10.1016/0899-3289(93)90056-h. [DOI] [PubMed] [Google Scholar]
- 41.Daeppen JB, Smith TL, Danko GP, Gordon L, Landi NA, Nurnberger J, et al. Clinical correlates of cigarette smoking and nicotine dependence in alcohol-dependent men and women. Alcohol Alcohol. 2000;35:171–5. doi: 10.1093/alcalc/35.2.171. [DOI] [PubMed] [Google Scholar]
- 42.Joseph AM, Nichols KL, Anderson H. Effect of treatment for nicotine dependence on alcohol and drug treatment outcomes. Addict Behav. 1993;18:635–44. doi: 10.1016/0306-4603(93)90017-4. [DOI] [PubMed] [Google Scholar]
- 43.Roll JM, Higgins ST, Budney AJ, Bickel WK, Badger G. A comparison of cocaine-dependent cigarette smokers and non-smokers on demographic, drug use, and other characteristics. Drug Alcohol Depend. 1996;40:195–201. doi: 10.1016/0376-8716(96)01219-7. [DOI] [PubMed] [Google Scholar]
- 44.Stuyt EB. Recovery rates after treatment for alcohol/drug dependence: Tobacco users vs. non-tobacco users. Am J Addiction. 1997;6:159–67. [PubMed] [Google Scholar]
- 45.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. Washington, DC: American Psychiatric Association; 2000. Text Revision. [Google Scholar]
- 46.McLaren J, Swift W, Dillon P, Allsop S. Cannabis potency and contamination. Addiction. 2008;103:1100–1109. doi: 10.1111/j.1360-0443.2008.02230.x. [DOI] [PubMed] [Google Scholar]
- 47.Moher D, Liberati A, Tetzlaff J, Altman DG The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. PLoS Med. 2009;6:1–6. [PMC free article] [PubMed] [Google Scholar]
- 48.Gordis L. Epidemiology. 3. Philadelphia, PA: Elsevier Saunders; 2004. [Google Scholar]
- 49*.Agrawal A, Lynskey MT, Madden PAF, Pergadia ML, Bucholz KK, Heath AC. Simultaneous cannabis and tobacco use and cannabis-related outcomes in young women. Drug Alcohol Depend. 2009;101:8–12. doi: 10.1016/j.drugalcdep.2008.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50*.Degenhardt L, Hall W. The relationship between tobacco use, substance-use disorders and mental health: Results from the National Survey of Mental Health and Well-being. Nicotine Tob Res. 2001;3:225–34. doi: 10.1080/14622200110050457. [DOI] [PubMed] [Google Scholar]
- 51*.Timberlake DS. A comparison of drug use and dependence between blunt smokers and other cannabis users. Subst Use Misuse. 2009;44:401–15. doi: 10.1080/10826080802347651. [DOI] [PubMed] [Google Scholar]
- 52*.Swift W, Coffey C, Carlin JB, Degenhardt L, Patton GC. Adolescent cannabis users at 24 years: Trajectories to regular weekly use and dependence in young adulthood. Addiction. 2008;103:1361–70. doi: 10.1111/j.1360-0443.2008.02246.x. [DOI] [PubMed] [Google Scholar]
- 53*.Coffey C, Carlin JB, Lynskey M, Li N, Patton GC. Adolescent precursors of cannabis dependence: Findings from the Victorian Adolescent Health Cohort Study. Br J Psychiatry. 2003;182:330–6. doi: 10.1192/bjp.182.4.330. [DOI] [PubMed] [Google Scholar]
- 54*.Patton GC, Coffey C, Carlin JB, Sawyer SM, Wakefield M. Teen smokers reach their mid twenties. J Adolesc Health. 2006;39:214–20. doi: 10.1016/j.jadohealth.2005.11.027. [DOI] [PubMed] [Google Scholar]
- 55.Budney AJ, Hughes JR. The cannabis withdrawal syndrome. Curr Opin Psychiatry. 2006;19:233–8. doi: 10.1097/01.yco.0000218592.00689.e5. [DOI] [PubMed] [Google Scholar]
- 56*.Agrawal A, Pergadia ML, Lynskey MT. Is there evidence for symptoms of cannabis withdrawal in the National Epidemiologic Survey of Alcohol and Related Conditions? Am J Addiction. 2008;17:199–208. doi: 10.1080/10550490802019519. [DOI] [PubMed] [Google Scholar]
- 57*.Ream GL, Benoit E, Johnson BD, Dunlap E. Smoking tobacco along with marijuana increases symptoms of cannabis dependence. Drug Alcohol Depend. 2008;95:199–208. doi: 10.1016/j.drugalcdep.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58*.Caldeira KM, Arria AM, O’Grady KE, Vincent KB, Wish ED. The occurrence of cannabis use disorders and other cannabis-related problems among first-year college students. Addict Behav. 2008;33:397–411. doi: 10.1016/j.addbeh.2007.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59*.Heffner JL, DelBello MP, Fleck DE, Anthenelli RM, Strakowski SM. Cigarette smoking in the early course of bipolar disorder: Associations with ages-at-onset of alcohol and marijuana use. Bipolar Disord. 2008;10:838–45. doi: 10.1111/j.1399-5618.2008.00630.x. [DOI] [PubMed] [Google Scholar]
- 60*.Agrawal A, Madden PAF, Bucholz KK, Heath AC, Lynskey MT. Transitions to regular smoking and to nicotine dependence in women using cannabis. Drug Alcohol Depend. 2008;95:107–14. doi: 10.1016/j.drugalcdep.2007.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61*.Timberlake DS, Haberstick BC, Hopfer CJ, Bricker J, Sakai JT, Lessem JM, et al. Progression from marijuana use to daily smoking and nicotine dependence in a national sample of U.S. adolescence. Drug Alcohol Depend. 2007;88:272–81. doi: 10.1016/j.drugalcdep.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 62*.Degenhardt L, Coffey C, Carlin JB, Swift W, Moore E, Patton GC. Outcomes of occasional cannabis use in adolescence: 10-year follow-up study in Victoria, Australia. Br J Psychiatry. 2010;196:290–5. doi: 10.1192/bjp.bp.108.056952. [DOI] [PubMed] [Google Scholar]
- 63*.Bonn-Miller MO, Zvolensky MJ, Johnson KA. Uni-morbid and co-occurring marijuana and tobacco use: Examination of concurrent associations with negative mood states. J Addict Dis. 2010;29:68–77. doi: 10.1080/10550880903435996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64*.Moore BA, Budney AJ. Tobacco smoking in marijuana-dependent outpatients. J Subst Abuse. 2001;13:583–96. doi: 10.1016/s0899-3289(01)00093-1. [DOI] [PubMed] [Google Scholar]
- 65*.Suris JC, Akre C, Berchtold A, Jeannin A, Michaud P-A. Some go without a cigarette: Characteristics of cannabis users who have never smoked tobacco. Arch Pediat Adol Med. 2007;161:1042–7. doi: 10.1001/archpedi.161.11.1042. [DOI] [PubMed] [Google Scholar]
- 66*.Georgiades K, Boyle MH. Adolescent tobacco and cannabis use: Young adult outcomes from the Ontario Child Health Study. J Child Psychol Psyc. 2007;48:724–31. doi: 10.1111/j.1469-7610.2007.01740.x. [DOI] [PubMed] [Google Scholar]
- 67*.de Dios MA, Vaughan EL, Stanton CA, Niaura R. Adolescent tobacco use and substance abuse treatment outcomes. J Subst Abuse Treat. 2009;37:17–24. doi: 10.1016/j.jsat.2008.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68*.Gray KM, Riggs PD, Min S-J, Mikulich-Gilbertson SK, Bandyopadhyay D, Winhausen T. Cigarette and cannabis use trajectories among adolescents in treatment for attention-deficit/hyperactivity disorder and substance use disorders. Drug Alcohol Depend. 2011;117:242–7. doi: 10.1016/j.drugalcdep.2011.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69*.Humfleet G, Muñoz R, Sees K, Reus V, Hall S. History of alcohol or drug problems, current use of alcohol or marijuana, and success in quitting smoking. Addict Behav. 1999;24:149–54. doi: 10.1016/s0306-4603(98)00057-4. [DOI] [PubMed] [Google Scholar]
- 70*.Metrik J, Spillane NS, Leventhal AM, Kahler CW. Marijuana use and tobacco smoking cessation among heavy alcohol drinkers. Drug Alcohol Depend. doi: 10.1016/j.drugalcdep.2011.06.004. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71*.Stapleton JA, Keaney F, Sutherland G. Illicit drug use as a predictor of smoking cessation treatment outcome. Nicotine Tob Res. 2009;11:685–9. doi: 10.1093/ntr/ntp050. [DOI] [PubMed] [Google Scholar]
- 72*.Gourlay SG, Forbes A, Marriner T, Pethica D, McNeil JJ. Prospective study of factors predicting outcome of transdermal nicotine treatment in smoking cessation. BMJ. 1994;309:842–6. doi: 10.1136/bmj.309.6958.842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73*.Ford DE, Vu HT, Anthony JC. Marijuana use and cessation of tobacco smoking in adults from a community sample. Drug Alcohol Depend. 2002;67:242–8. doi: 10.1016/s0376-8716(02)00066-2. [DOI] [PubMed] [Google Scholar]
- 74*.Haskins A, Bertone-Johnson E, Pekow P, Carbone E, Chasan-Taber L. Correlates of smoking cessation at pregnancy onset among Hispanic women in Massachusetts. Am J Health Promot. 2010;25:100–8. doi: 10.4278/ajhp.090223-QUAN-77. [DOI] [PubMed] [Google Scholar]
- 75*.Abrantes AM, Lee CS, MacPherson L, Strong DR, Borrelli B, Brown RA. Health risk behaviors in relation to making a smoking quit attempt among adolescents. J Behav Med. 2009;32:142–9. doi: 10.1007/s10865-008-9184-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.McKee SA, Falba T, O’Malley SS, Sindelar J, O’Connor PG. Smoking status as a clinical indicator for alcohol misuse in US adults. Arch Intern Med. 2007;167:716–21. doi: 10.1001/archinte.167.7.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Fiore MC, Jaen CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, et al. Treating Tobacco Use and Dependence: 2008 Update. Rockville, MD: U.S. Department of Health and Human Services Public Health Service; 2008. [Google Scholar]
- 78.Substance Abuse and Mental Health Services Administration. Results from the 2006 National Survey on Drug Use and Health: National Findings. Rockville, MD: Office of Applied Studies, NSDUH Series H-32, DHHS Publication No. SMA 07-4293); 2007. [Google Scholar]
- 79.Tyas S, Pederson L. Psychosocial factors related to adolescent smoking: A critical review of the literature. Tob Control. 1998;7:409–20. doi: 10.1136/tc.7.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Morissette SB, Tull MT, Gulliver SB, Kamholz BW, Zimering RT. Anxiety, anxiety disorders, tobacco use and nicotine: A critical review of interrelationships. Psychol Bull. 2007;133:245–72. doi: 10.1037/0033-2909.133.2.245. [DOI] [PubMed] [Google Scholar]
- 81.Wagenknecht LE, Perkins LL, Cutter GR, Sidney S, Burke GL, Manolio TA, et al. Cigarette smoking behavior is strongly related to educational status: The cardia study. Prev Med. 1990;19:158–69. doi: 10.1016/0091-7435(90)90017-e. [DOI] [PubMed] [Google Scholar]
- 82.Flint AJ, Novotny TE. Poverty status and cigarette smoking prevalence and cessation in the United States, 1983-1993: The independent risk of being poor. Tob Control. 1997;6:14–8. doi: 10.1136/tc.6.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Norberg MM, Mackenzie J, Copeland J. Quantifying cannabis use with the Timeline Followback approach: A psychometric evaluation. Drug Alcohol Depend. doi: 10.1016/j.drugalcdep.2011.09.007. in press. [DOI] [PubMed] [Google Scholar]
- 84.Budney AJ, Roffman R, Stephens SS, Walker D. Marijuana dependence and its treatment. Addict Sci Clin Pract. 2007;4:4–16. doi: 10.1151/ascp07414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kalman D, Kim S, DiGirolamo G, Smelson D, Ziedonis D. Addressing tobacco use disorder in smokers in early remission from alcohol dependence: The case for integrating smoking cessation services in substance use disorder treatment programs. Clin Psychol Rev. 2010;30:12–24. doi: 10.1016/j.cpr.2009.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Prochaska JJ, Delucchi K, Hall SM. A meta-analysis of smoking cessation interventions with individuals in substance abuse treatment or recovery. J Consult Clin Psychol. 2004;72:1144–56. doi: 10.1037/0022-006X.72.6.1144. [DOI] [PubMed] [Google Scholar]
- 87.Peters EN, Nich C, Carroll KM. Primary outcomes in two randomized controlled trials of treatments for cannabis use disorders. Drug Alcohol Depend. 2011;118:408–416. doi: 10.1016/j.drugalcdep.2011.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hughes JR, Keely JP, Niaura RS, Ossip-Klein DJ, Richmond RL, Swan GE. Measures of abstinence in clinical trials: Issues and recommendations. Nicotine Tob Res. 2003;5:13–25. [PubMed] [Google Scholar]
- 89.Jüni P, Witschi A, Bloch R, Egger M. The hazards of scoring the quality of clinical trials for meta-analysis. JAMA. 1999;282:1054–60. doi: 10.1001/jama.282.11.1054. [DOI] [PubMed] [Google Scholar]
- 90.Joseph AM, Willenbring ML, Nugent SM, Nelson DB. A randomized trial of concurrent versus delayed smoking intervention for patients in alcohol dependence treatment. J Stud Alcohol. 2004;65:681–691. doi: 10.15288/jsa.2004.65.681. [DOI] [PubMed] [Google Scholar]
- 91*.Stephens RS, Roffman RA, Curtin L. Comparison of extended versus brief treatments for marijuana use. J Consult Clin Psychol. 2000;68:898–908. [PubMed] [Google Scholar]


