Abstract
OBJECTIVE:
The goal was to assess the rate and behavioral methods of nonsuicidal self-injury (NSSI) in a community sample of youth and examine effects of age and sex.
METHODS:
Youth in the third, sixth, and ninth grades (ages 7–16) at schools in the community were invited to participate in a laboratory study. A total of 665 youth (of 1108 contacted; 60% participation rate) were interviewed about NSSI over their lifetime via the Self-Injurious Thoughts and Behaviors Interview.
RESULTS:
Overall, 53 (8.0%) of the 665 youth reported engaging in NSSI; 9.0% of girls and 6.7% of boys reported NSSI engagement; 7.6% of third-graders, 4.0% of sixth-graders, and 12.7% of ninth-graders reported NSSI engagement. There was a significant grade by gender interaction; girls in the ninth grade (19%) reported significantly greater rates of NSSI than ninth-grade boys (5%). Behavioral methods of NSSI differed by gender. Girls reported cutting and carving skin most often, whereas boys reported hitting themselves most often. Finally, 1.5% of youth met some criteria for the proposed fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) diagnosis of NSSI.
CONCLUSIONS:
Children and adolescents engage in NSSI. Ninth-grade girls seem most at risk, as they engage in NSSI at 3 times the rate of boys. Behavioral methods of NSSI also vary by grade and gender. As possible inclusion of an NSSI diagnosis in the fifth edition of the DSM-5 draws near, it is essential to better understand NSSI engagement across development and gender.
Keywords: nonsuicidal self-injury, children, adolescents, self-mutilation, mental health
What’s Known on This Subject:
Known rates of nonsuicidal self-injury, hurting oneself without the intent to die, are between ∼7% and 24% in samples of early adolescents and older adolescents, yet research has not reported rates for youth younger than 11 years old.
What This Study Adds:
Children as young as 7 years old report engaging in nonsuicidal self-injury. There is a grade by gender interaction for nonsuicidal self-injury, such that ninth-grade girls report the greatest rates of engagement and do so by cutting themselves.
Nonsuicidal self-injury (NSSI) is defined as intentionally causing destruction to one’s skin or body without the intent to die.1 This behavior appears to increase across development and affects many youth.2 In community samples, 7.7% of early adolescents (grades 6–8, n = 508) reported engaging in NSSI3 and 13.9% to 21.4% of high school adolescents (grades 9–12, mean age 16) reported NSSI.4 In college-age samples, rates of NSSI can be as high as 38%.2 Research with clinical samples shows even higher rates of ∼40%.5 Engaging in NSSI is a risk factor for suicidal thoughts and behaviors and a precursor to more serious psychopathology.6 In fact, as publication of the new Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V) approaches, it seems likely that NSSI will become a new psychiatric diagnosis.7 Given likely inclusion in the official psychiatric nomenclature, it is important to establish rates and behavioral methods used to self-injure among children and adolescents.
Despite some valuable epidemiologic data on NSSI, there are several important gaps in the knowledge base. First, to our knowledge, there is no research reporting rates of NSSI in children younger than middle school (ie, age 11 or younger). Second, gender differences in NSSI remain to be fully understood.8 Specifically some evidence suggests similar rates among early and late adolescent boys and girls,3,4 whereas other research shows that adolescent girls report higher rates of NSSI than boys.9–11 Third, research with adolescents reveals many different behavioral methods (eg, cutting, burning, hitting oneself) of NSSI,4,10 and shows that girls report cutting themselves more than boys.12–14 Yet, to our knowledge, no research has explored potential age and gender differences in NSSI behavioral methods in youth of different ages.
Given these gaps and the necessity of describing basic age and gender patterns in NSSI, this study aimed to answer the following questions: (1) What are the lifetime rates of NSSI in a general community sample of children and adolescents (ages 7–16)? (2) Are there gender and/or age differences in NSSI rates? (3) What methods are used by youth engaging in NSSI, and do these methods vary by gender or age? (4) What is the rate of youth currently meeting criteria for a diagnosis of NSSI by using DSM-V–proposed diagnostic criteria (see Appendix and ref 15)?
Methods
Sample and Procedures
Youth were recruited by brief information letters sent home directly by the participating school districts to families with a child in third, sixth, or ninth grades. Of the families to whom letters were sent, 1108 parents responded to the letter and called the laboratory for more information. Parent report established that both the parent and child were fluent in English, the child did not have an autism spectrum or psychotic disorder, and the child had an IQ >70. Of the families who initially contacted the laboratory, 665 (60% participation rate) qualified as study participants, as they met criteria and arrived at the laboratory for the assessment. The remaining 460 (40%) are considered nonparticipants for the following reasons: 4 (1%) were excluded because the parents reported that their child had an autism spectrum disorder or low IQ; 13 (3%) were non–English-speaking families; 330 (71%) declined after learning about the study’s requirements; and 113 (25%) were scheduled but did not arrive for assessment.
Participants were 665 youth ranging in age from 7 to 16 years (mean = 11.6, SD = 2.4). Table 1 shows descriptive characteristics. The sample was comparable to the community and school districts from which it was recruited. The sample was also generally comparable to the ethnicity and race characteristics of the overall population of the United States,16 with fewer White participants (80%) and fewer Hispanic participants than the overall population of the United States (18%).
TABLE 1.
Demographic Characteristics of Study Population (n = 665)
| Characteristic | Percent (n) or Median |
|---|---|
| Gender | |
| Female | 55.0 (366) |
| Male | 45.0 (299) |
| Grade | |
| Third | 29.5 (196) |
| Sixth | 37.3 (248) |
| Ninth | 33.2 (221) |
| Race/Ethnicity | |
| White | 62.2 (414) |
| African American | 11.3 (75) |
| Hispanic | 7.5 (50) |
| Asian/Pacific Islander | 9.6 (64) |
| Other/Mixed ethnicity and race | 9.3 (62) |
| Parent marital status | |
| Married | 77.0 (512) |
| Single | 7.0 (46) |
| Divorced or separated | 15.0 (100) |
| Widowed | 1.0 (7) |
| Annual income | |
| Minimum | $0 |
| Median | $86 500 |
| Maximum | $900 000 |
| Free/reduced lunch | 18.3 (122) |
The parent and youth visited the laboratory for the assessment and both youth and parents were compensated $25 each. Parents provided informed written consent for their child’s participation; youth provided written assent. The institutional review board approved all procedures. Participants were reimbursed for participation.
Assessment of NSSI
NSSI was measured by using the Self-Injurious Thoughts and Behaviors Interview (SITBI),17 a structured clinical interview that assesses NSSI engagement and behavioral methods used. This measure was chosen because it is commonly used in research on NSSI engagement with adolescents.18,19 The SITBI has not been used with youth younger than adolescence, and this study is the first to our knowledge to use the SITBI with youth younger than age 12.20 Youth were interviewed via the SITBI in person. Engagement in NSSI was assessed over the youth’s lifetime and in the past year. Behavioral methods of NSSI included “cutting or carving skin,” “hitting oneself,” “inserting sharp objects into the skin or nails,” “burning oneself,” and “picking one’s skin.” The SITBI was also used to measure frequency of NSSI engagement. The SITBI has excellent inter-rater reliability and test-retest reliability (κs = 1.00) and validity (κs ≥ 0.74).17
The Functional Assessment of Self-Mutilation21 was used to measure NSSI functions (ie, purpose). The Functional Assessment of Self-Mutilation measures functions of NSSI along 2 dimensions: interpersonal (eg, to avoid being with people) versus intrapersonal (eg, to give yourself something to do) and negative reinforcement (eg, to stop bad feelings) versus positive reinforcement (eg, to feel something, even if was pain).
Assessment of Distress
To test if youth meeting proposed criteria for a DSM-V diagnosis of NSSI experienced increased distress, we used The Children’s Depression Inventory (CDI).22 The CDI is a 27-item self-report measure; higher scores indicate greater distress. The CDI has been shown to have good reliability (α ≥ 0.90) and validity.23
Statistical Analyses
All analyses were conducted by using PASW software, version 18 (SPSS Inc, Chicago, IL). Odds ratios were conducted by using binary logistic regression analyses to test main effects of gender and grade, as well as a grade by gender interaction, related to a higher likelihood of engagement in NSSI. For each set of analyses, we began by conducting analyses of frequencies, which are shown in Table 2. To test if there were differences in reported behavioral methods for youth engaging in NSSI, χ2 analyses were conducted for each behavioral method with grade and gender as grouping variables. Odds ratio was used to determine the effect size (small = 1.49, medium = 3.45, large = 9.00) of the regression analysis. Cramer’s V was used to determine the effect size (small = 0.1, medium = 0.3, large = 0.5) of χ2 analyses. Cohen’s d was used to determine the effect size (small = 0.2, medium = 0.5, large = 0.8) of the t test analysis.
TABLE 2.
Rates of NSSI Engagement and Behavioral Methods by Gender and Grade
| n | Rates | Behavioral Method in Lifetime | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lifetime | Cut/carve Skin | Burn Skin | Insert Objects | Pick Skin | Hit Self | Tattoo Self | Other | ||||||||||
| n | % | n | % of | n | % of | n | % of | n | % of | n | % of | n | % of | n | % of | ||
| Overall | 665 | 53 | 8.0 | 24 | 45.3 | 7 | 13.2 | 8 | 15.1 | 4 | 7.5 | 25 | 47.2 | 1 | 2.0 | 10 | 18.9 |
| Girls | 366 | 33 | 9.0 | 21 | 63.6 | 6 | 18.2 | 5 | 15.2 | 3 | 9.1 | 14 | 42.4 | 1 | 3.0 | 5 | 15.2 |
| Third grade | 103 | 7 | 6.8 | ||||||||||||||
| Sixth grade | 141 | 3 | 2.1 | ||||||||||||||
| Ninth grade | 122 | 23 | 18.9 | ||||||||||||||
| Boys | 299 | 20 | 6.7 | 3 | 15.0 | 1 | 5.0 | 3 | 15.0 | 1 | 5.0 | 11 | 55.0 | 0 | 0.0 | 5 | 25.0 |
| Third grade | 94 | 8 | 8.5 | ||||||||||||||
| Sixth grade | 106 | 7 | 6.6 | ||||||||||||||
| Ninth grade | 99 | 5 | 5.1 | ||||||||||||||
| Third grade | 197 | 15 | 7.6 | 2 | 13.3 | 1 | 6.7 | 1 | 6.7 | 1 | 6.7 | 9 | 60.0 | 0 | 0.0 | 5 | 33.3 |
| Sixth grade | 247 | 10 | 4.0 | 3 | 30.0 | 1 | 10.0 | 1 | 10.0 | 0 | 0.0 | 5 | 50.0 | 0 | 0.0 | 1 | 10.0 |
| Ninth grade | 221 | 28 | 12.7 | 19 | 70.4 | 5 | 18.5 | 6 | 22.2 | 3 | 11.1 | 11 | 40.7 | 1 | 3.8 | 4 | 15.4 |
The sum of subgroup numbers may not be equal to the total n for data on behavioral methods because many youth reported multiple methods.
Results
Table 2 provides the rates of NSSI for the overall sample (n = 665) and separately for girls and boys, as well as by grade cohort. In addition, percentages of behavioral methods used for those reporting engagement in NSSI are shown for the sample overall and separated by gender and grade. A total of 53 youth (8.0%) reported engaging in NSSI over their lifetime. Of those 53, a total of 17 youth reported engaging in NSSI only 1 time (2.5% of the total sample; 32.1% of the NSSI sample); the remaining 36 reported multiple instances of NSSI. There were no differences for any results reported between the groups who engaged in NSSI once versus multiple times. Therefore, all results reported are for the larger sample (n = 53).
Lifetime Rates of NSSI
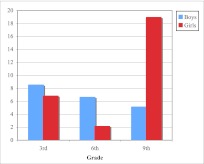
Tests of these 6 analyses assessing differences in reported rates of NSSI were corrected by using Bonferroni familywise adjusted α levels of 0.0083 per test (0.05/6). Analyses revealed a significant interaction effect of grade by gender (b1 = 0.382, P < .001, Wald = 8.279, odds ratio = 1.466) on NSSI engagement. Planned follow-up χ2 analyses were conducted to decompose this grade by gender interaction. For ninth-graders, girls reported significantly greater rates of NSSI engagement than boys (χ21 = 9.409, P = .002, Cramer’s V = 0.206). Neither third- (χ21 = 0.205, P = .650, Cramer’s V = 0.032) nor sixth- (χ21 = 3.164, P = .075, Cramer’s V = 0.113) graders differed by gender in report of NSSI engagement. In addition, for girls, there was a significant difference across grades in report of NSSI engagement (χ22 = 23.314, P < .001, Cramer’s V = 0.252). For boys, there was no significant difference across grades (χ22 = 0.927, P = .639, Cramer’s V = 0.056). Figure 1 shows rates of NSSI for girls and boys in third, sixth, and ninth grade separately.
FIGURE 1.
Grade by gender interaction of lifetime rates of NSSI engagement. Y axis designates percent of each group of youth, or the rate for each group.
Behavioral Methods
Trends in behavioral methods of NSSI engagement differed for boys and girls, as well as by grade (Table 2). For girls, most of those reporting NSSI stated that they cut or carved skin (63.6%). For boys, 55% reporting NSSI stated that they hit themselves (55.0%). For third- (60%) and sixth- (50%) graders, most reported hitting themselves. Most ninth-graders reported cutting and carving skin (70.4%). Overall, many youth (18.9%) reported other behavioral methods of NSSI as well (eg, biting, pulling hair to cause pain, running into walls, throwing body into sharp objects).
Tests of the 14 analyses assessing differences in behavioral methods by grade and gender were Bonferroni corrected by using α of 0.0036 per test (0.05/14). Girls and boys significantly differed in reporting cutting and carving skin (χ21 = 11.884, P = .001, Cramer’s V = 0.483). There were significant grade differences in reporting cutting and carving skin (χ21 = 13.418, P = .001, Cramer’s V = 0.513). The grade by gender interaction for cutting/carving skin was nonsignificant. No other differences (ie, by grade, by gender) were significant.
DSM-V NSSI Diagnosis
This study was able to address criteria A, B.4., and C of the proposed DSM-V diagnosis of NSSI (see Appendix and ref 15). Regarding criterion A, 1.5% youth (n = 10) reported engaging in NSSI on at least 5 occasions in the past year. For criterion B.4, each of these youth also reported engaging in NSSI with a purpose (eg, to stop bad feelings, get help). For criterion C, youth who engaged in NSSI at least 5 times this past (mean = 17.2, SD = 11.5) year reported significantly higher levels of distress on CDI than other youth (mean = 6.9, SD = 5.6, t[9.1] = 2.84, P = .019, Cohen’s d = 1.142).
Discussion
Research has established that adolescents engage in NSSI,3,4 yet no study had examined rates of NSSI in children (ie, younger than age 11). Furthermore, we located no study reporting grade and gender influences on rates of NSSI or behavioral methods in a sample of this age. This study was the first to address these important questions regarding NSSI in a general community sample of children and adolescents from grade school through high school. As scientific, clinical, and public interest in NSSI has increased, results from this study provide novel and essential information on rates of NSSI and methods used by children and adolescents.
One unique aspect of this study is that we assessed NSSI across different ages. We found that 8.0% of youth, overall, reported NSSI engagement in their lifetime. Prior research revealed rates of 7.0% to 8.0% for youth in middle school1,24 and between 17.0% and 23.2% for older youth.4,25 Rates obtained in this study are comparable, albeit somewhat lower. Prior research has used relatively wide age ranges (eg, all adolescents in grades 9–12, ages 15–19), whereas we sampled from specific grades across salient developmental periods. Our sample included youth at the younger end of prior studies. That our rates are generally equivalent when compared with studies with youth of similar ages enhances confidence in findings from this study. Results suggest developmental trends exist in rates of NSSI. It has commonly been thought that NSSI is a behavior characteristic of adolescence and young adulthood.2 Although adolescents (ie, ninth-graders) in this study reported greater lifetime rates of NSSI than younger children (ie, third- and sixth-graders), results show that NSSI is a behavior that children engage in as well.
This study contributes to understanding the emergence of gender differences in NSSI. Past studies reporting effects of gender on NSSI engagement have focused on early and middle adolescents,10,11 but not children, and they did not test for a gender by age interaction for NSSI engagement. Research on this topic has been mixed.8 Although some research has found that more girls than boys report NSSI,9,11 other research has shown no gender difference.4,12,26 Results from the current study showed a grade by gender interaction for lifetime NSSI. For younger youth (ie, third- and sixth-graders), rates of NSSI did not differ for girls and boys. Older girls (ie, ninth grade) were more likely to engage in NSSI than same-aged boys. This study suggests that it is not until the transition to adolescence that the gender difference in NSSI engagement emerges.
Three times as many adolescent girls engaged in NSSI compared with boys. Similar trends have been found in other epidemiologic studies of mental health outcomes in youth. For example, clinical depression rates are similar for girls and boys until age 13, and thereafter girls experience depression at twice the rate of boys.27,28 The broader developmental epidemiologic literature shows a greater preponderance of emotional disorders for girls, compared with boys, starting with the adolescent transition.29,30
Youth reported using different behavioral methods of NSSI across different developmental periods and gender. Past research shows that adolescent and young adult girls report cutting their skin at higher rates than boys of the same age.12,25,30 In the current sample, girls reported cutting or carving their skin most often; boys reported hitting themselves. Older youth (ie, ninth-graders) reported cutting/carving their skin most often; younger youth (ie, third-graders) reported hitting themselves most often. Based on these findings, it seems important to take into account developmental trends and gender when assessing NSSI behaviors and to assess a greater breadth of NSSI behavioral methods.
Finally, we investigated how many youth might meet proposed criteria for a DSM-V NSSI diagnosis.15 We assessed several, although not all, of the proposed criteria. In this sample, 1.5% of youth met some criteria for the proposed NSSI diagnosis because they reported (1) engaging in NSSI at least 5 times in the past year, (2) engaging in NSSI for a purpose, and (3) high levels of distress.
This study has several implications. Knowing that a substantial percentage of youth overall report engaging in NSSI suggests it is a mental health outcome that needs medical evaluation, especially as NSSI might be a precursor for suicidal behaviors.6 Hospital emergency rooms discharge nearly 60% of patients who report self-harm without a mental health evaluation.31 Psychiatric problems with childhood and adolescence ontogeny are among the most burdensome globally,32 and can lead to chronic obesity33,34 and substance use and abuse.35,36 Therefore, early identification of NSSI engagement could help prevent these negative physical and mental health outcomes.
Beginning to explore NSSI in youth and the various behavioral methods reported by youth engaging in NSSI leads to other unanswered questions. Do commonly used assessment measures of NSSI capture all behavioral methods? Although the SITBI is the gold standard clinical interview to assess NSSI, a proportion (18.9%) of youth reporting NSSI engaged in other behaviors not directly assessed by the SITBI. When evaluating NSSI in youth, solely asking about cutting or carving skin, or hitting oneself, may not be adequate. A more thorough assessment should include asking open-ended questions about other behavioral methods.
It is important to consider strengths and limitations of this study. This is the first study to assess NSSI from middle childhood through adolescence, establish that children engage in NSSI, examine behavioral method differences by gender and grade, and begin to explore rates of a potential DSM-V NSSI diagnosis. We assessed NSSI engagement by using a reliable and valid structured clinical interview in a general community sample, which allowed for accurate rates for the overall sample and separately for grade and gender; however, limitations include having only 53 (8.0%) youth reporting engaging in NSSI. Although this rate is similar to that reported in other studies using samples of similar-aged youth, replication of rates and behavioral methods are needed with larger, representative epidemiologic samples. In addition, findings from this study on gender differences in methods of NSSI should be taken with caution given the low base rate of NSSI engagement. Another limitation is that we combined together youth engaging in NSSI once and those reporting multiple occasions, and some research suggests these groups differ.37,38 The study lacked full assessment of psychiatric diagnoses. Our classification of a potential DSM-V NSSI diagnosis has weaknesses. We used the CDI as a measure of distress, and the CDI asks about distress in the past week but not acute distress occurring more proximally to NSSI engagement. Finally, youth in this study, although ethnically diverse and representative of the larger areas from which the sample was drawn, were from families with relatively high socioeconomic status. It is possible that findings from this study may not generalize to youth with lower socioeconomic status or to those in other countries.
Conclusions
This study found that children engage in NSSI at a rate that is similar to early adolescents. As possible inclusion of a NSSI diagnosis in the DSM-V draws near, it is essential to better understand rates and methods of NSSI engagement across development and gender. Rates of NSSI surged dramatically from childhood into adolescence, especially for girls. Specifically, 3 times as many ninth-grade girls reported engaging in NSSI compared with ninth-grade boys. In addition, there were grade and gender differences in behavioral methods of NSSI engagement; older youth and girls report higher rates of cutting or carving their skin. Last, we obtained a point prevalence rate of 1.5% for a psychiatric diagnosis of NSSI given proposed DSM-V criteria. In light of this evidence, routine health examinations including assessment of NSSI may be warranted.
Glossary
- CDI
Children’s Depression Inventory
- DSM-V
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
- NSSI
nonsuicidal self-injury
- SITBI
Self-Injurious Thoughts and Behaviors Interview
Appendix: DSM-V Proposed Diagnostic Criteria for NSSI Diagnosis
In the past year, the individual has, on 5 or more days, engaged in intentional self-inflicted damage to the surface of his or her body, of a sort likely to induce bleeding or bruising or pain (eg, cutting, burning, stabbing, hitting, excessive rubbing), for purposes not socially sanctioned (eg, body piercing, tattooing, and so forth), but performed with the expectation that the injury will lead to only minor or moderate physical harm. The absence of suicidal intent is either reported by the patient or can be inferred by frequent use of methods that the patient knows, by experience, not to have lethal potential. (When uncertain, code with NOS 2.) The behavior is not of a common and trivial nature, such as picking at a wound or nail biting.
-
The intentional injury is associated with at least 2 of the following:
Negative feelings or thoughts, such as depression, anxiety, tension, anger, generalized distress, or self-criticism, occurring in the period immediately before the self-injurious act.
Before engaging in the act, a period of preoccupation with the intended behavior that is difficult to resist.
The urge to engage in self-injury occurs frequently, although it might not be acted on.
The activity is engaged in with a purpose; this might be relief from a negative feeling/cognitive state or interpersonal difficulty or induction of a positive feeling state. The patient anticipates these will occur either during or immediately after the self-injury.
The behavior and its consequences cause clinically significant distress or impairment in interpersonal, academic, or other important areas of functioning.
The behavior does not occur exclusively during states of psychosis, delirium, or intoxication. In individuals with a developmental disorder, the behavior is not part of a pattern of repetitive stereotypies. The behavior cannot be accounted for by another mental or medical disorder (ie, psychotic disorder, pervasive developmental disorder, mental retardation, Lesch-Nyhan Syndrome).
Footnotes
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or National Institutes of Health.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by NIMH grant R01-MH 077195 to Drs Hankin and Young. Funded by the National Institutes of Health (NIH).
References
- 1.Nock MK, Favazza AR. Nonsuicidal self-injury: definition and classification. In: Nock ML, ed. Understanding Non-Suicidal Self-Injury: Origins, Assessment, and Treatment. Washington, DC: American Psychological Association; 2009:9–18 [Google Scholar]
- 2.Rodham K, Hawton K. Epidemiology and phenomenology of nonsuicidal self-injury. In: Nock ML, ed. Understanding Non-Suicidal Self-Injury: Origins, Assessment, and Treatment. Washington, DC: American Psychological Association; 2009:37–62 [Google Scholar]
- 3.Hilt LM, Nock MK, Lloyd-Richardson EE, Prinstein MJ. Longitudinal study of nonsuicidal self-injury among young adolescents. J Early Adolesc. 2008;28(3):455–469 [Google Scholar]
- 4.Muehlenkamp JJ, Gutierrez PM. An investigation of differences between self-injurious behavior and suicide attempts in a sample of adolescents. Suicide Life Threat Behav. 2004;34(1):12–23 [DOI] [PubMed] [Google Scholar]
- 5.Jacobson CM, Muehlenkamp JJ, Miller AL, Turner JB. Psychiatric impairment among adolescents engaging in different types of deliberate self-harm. J Clin Child Adolesc Psychol. 2008;37(2):363–375 [DOI] [PubMed] [Google Scholar]
- 6.Nock MK, Joiner TE, Jr, Gordon KH, Lloyd-Richardson E, Prinstein MJ. Non-suicidal self-injury among adolescents: diagnostic correlates and relation to suicide attempts. Psychiatry Res. 2006;144(1):65–72 [DOI] [PubMed] [Google Scholar]
- 7.Selby EA, Bender TW, Gordon KH, Nock MK, Joiner TE. Non-suicidal self-injury (NSSI) disorder: a preliminary study. Personality Disorders: Theory, Research, & Treatment. (in press) [DOI] [PubMed] [Google Scholar]
- 8.Barrocas AL, Jenness JL, Davis TS, et al. Developmental perspectives on vulnerability to nonsuicidal self-injury in youth. In: Benson J, ed. Advances in Child Development and Behavior. 40th ed. London: Elsevier; 2011:301–336 [DOI] [PubMed] [Google Scholar]
- 9.Laye-Gindhu A, Schonert-Reichl KA. Nonsuicidal self-harm among community adolescents: understanding the “whats” and “whys” of self-harm. J Youth Adolesc. 2005;34(5):447–457 [Google Scholar]
- 10.Muehlenkamp JJ, Gutierrez PM. Risk for suicide attempts among adolescents who engage in non-suicidal self-injury. Arch Suicide Res. 2007;11(1):69–82 [DOI] [PubMed] [Google Scholar]
- 11.Ross S, Heath N. A study of the frequency of self-mutilation in a community sample of adolescents. J Youth Adolesc. 2002;31(1):67–77 [Google Scholar]
- 12.Gratz KL, Latzman RD, Young J, et al. Deliberate self-harm among underserved adolescents: the moderating roles of gender, race, and school-level and association with borderline personality features. Personality Disorders: Theory, Research, and Treatment. (in press) [DOI] [PubMed] [Google Scholar]
- 13.Izutsu T, Shimotsu S, Matsumoto T, et al. Deliberate self-harm and childhood hyperactivity in junior high school students. Eur Child Adolesc Psychiatry. 2006;15(3):172–176 [DOI] [PubMed] [Google Scholar]
- 14.Lundh LG, Karim J, Quilisch E. Deliberate self-harm in 15-year-old adolescents: a pilot study with a modified version of the Deliberate Self-Harm Inventory. Scand J Psychol. 2007;48(1):33–41 [DOI] [PubMed] [Google Scholar]
- 15.American Psychiatric Association. V 01 non-suicidal self-injury. DSM-5 Web site. Available at: www.dsm5.org/ProposedRevisions/Pages/proposedrevision.aspx?rid=443. Accessed December 11, 2011
- 16.US Census Bureau Population Division. Table 3. Annual Estimates of the Resident Population by Sex, Race, and Hispanic Origin for the United States: April 1, 2000 to July 1, 2009 (NC-EST-2009-03).” June 2010. Available at: www.census.gov.popest/national/asrh/NC-EST2009/NC-EST2009-03.xls. Accessed April 8, 2012
- 17.Nock MK, Holmberg EB, Photos VI, Michel BD. Self-Injurious Thoughts and Behaviors Interview: development, reliability, and validity in an adolescent sample. Psychol Assess. 2007;19(3):309–317 [DOI] [PubMed] [Google Scholar]
- 18.Glassman LH, Weierich MR, Hooley JM, Deliberto TL, Nock MK. Child maltreatment, non-suicidal self-injury, and the mediation role of self-criticism. Behav Res Ther. 2008;45(10):2483–2490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Janis IB, Nock MK. Behavioral forecasts do not improve the prediction of future behavior: a prospective study of self-injury. J Clin Psychol. 2008;64(10):1164–1174 [DOI] [PubMed] [Google Scholar]
- 20.Dour HJ, Cha CB, Nock MK. Evidence for an emotion-cognition interaction in the statistical prediction of suicide attempts. Behav Res Ther. 2011;49(4):294–298 [DOI] [PubMed] [Google Scholar]
- 21.Lloyd EE, Kelley ML, Hope T. Self-mutilation in a community sample of adolescents: descriptive characteristics and provisional prevalence rates. Poster presented at: Annual meeting of the Society for Behavioral Medicine; April 1997; New Orleans, LA [Google Scholar]
- 22.Kovacs M. Rating scales to assess depression in school-aged children. Acta Paedopsychiatr. 1981;46(5-6):305–315 [PubMed] [Google Scholar]
- 23.Kazdin AE, French NH, Unis AS. Child, mother, and father evaluations of depression in psychiatric inpatient children. J Abnorm Child Psychol. 1983;11(2):167–179 [DOI] [PubMed] [Google Scholar]
- 24.Hankin BL, Abela JRZ. Nonsuicidal self-injury in adolescence: prospective rates and risk factors in a 2½ year longitudinal study. Psychiatry Res. 2011;186(1):65–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Whitlock J, Eckenrode J, Silverman D. Self-injurious behaviors in a college population. Pediatrics. 2006;117(6):1939–1948 [DOI] [PubMed] [Google Scholar]
- 26.Lloyd-Richardson EE, Perrine N, Dierker L, Kelley ML. Characteristics and functions of non-suicidal self-injury in a community sample of adolescents. Psychol Med. 2007;37(8):1183–1192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ge X, Lorenz FO, Conger RD, Elder GH, Simons RL. Trajectories of stressful life events and depressive symptoms during adolescence. Dev Psychol. 1994;30(4):467–483 [Google Scholar]
- 28.Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: emerging gender differences in a 10-year longitudinal study. J Abnorm Psychol. 1998;107(1):128–140 [DOI] [PubMed] [Google Scholar]
- 29.Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74(1):5–13 [DOI] [PubMed] [Google Scholar]
- 30.Rodham K, Hawton K, Evans E. Reasons for deliberate self-harm: comparison of self-poisoners and self-cutters in a community sample of adolescents. J Am Acad Child Adolesc Psychiatry. 2004;43(1):80–87 [DOI] [PubMed] [Google Scholar]
- 31.Hickey L, Hawton K, Fagg J, Weitzel H. Deliberate self-harm patients who leave the accident and emergency department without a psychiatric assessment: a neglected population at risk of suicide. J Psychosom Res. 2001;50(2):87–93 [DOI] [PubMed] [Google Scholar]
- 32.Costello EJ, Egger H, Angold A. 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. J Am Acad Child Adolesc Psychiatry. 2005;44(10):972–986 [DOI] [PubMed] [Google Scholar]
- 33.Mustillo S, Worthman C, Erkanli A, Keeler G, Angold A, Costello EJ. Obesity and psychiatric disorder: developmental trajectories. Pediatrics. 2003;111(4 pt 1):851–859 [DOI] [PubMed] [Google Scholar]
- 34.Pine DS, Cohen P, Brook J, Coplan JD. Psychiatric symptoms in adolescence as predictors of obesity in early adulthood: a longitudinal study. Am J Public Health. 1997;87(8):1303–1310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bardone AM, Moffitt TE, Caspi A, Dickson N, Stanton WR, Silva PA. Adult physical health outcomes of adolescent girls with conduct disorder, depression, and anxiety. J Am Acad Child Adolesc Psychiatry. 1998;37(6):594–601 [DOI] [PubMed] [Google Scholar]
- 36.Costello EJ, Erkanli A, Federman E, Angold A. Development of psychiatric comorbidity with substance abuse in adolescents: effects of timing and sex. J Clin Child Psychol. 1999;28(3):298–311 [DOI] [PubMed] [Google Scholar]
- 37.Klonsky ED, Olino TM. Identifying clinically distinct subgroups of self-injurers among young adults: a latent class analysis. J Consult Clin Psychol. 2008;76(1):22–27 [DOI] [PubMed] [Google Scholar]
- 38.Whitlock J, Muehlenkamp JJ, Eckenrode J. Variation in nonsuicidal self-injury: identification and features of latent classes in a college population of emerging adults. J Clin Child Adolesc Psychol. 2008;37(4):725–735 [DOI] [PubMed] [Google Scholar]