Summary
Background
Thrombolysis is of net benefit in patients with acute ischaemic stroke, who are younger than 80 years of age and are treated within 4·5 h of onset. The third International Stroke Trial (IST-3) sought to determine whether a wider range of patients might benefit up to 6 h from stroke onset.
Methods
In this international, multicentre, randomised, open-treatment trial, patients were allocated to 0·9 mg/kg intravenous recombinant tissue plasminogen activator (rt-PA) or to control. The primary analysis was of the proportion of patients alive and independent, as defined by an Oxford Handicap Score (OHS) of 0–2 at 6 months. The study is registered, ISRCTN25765518.
Findings
3035 patients were enrolled by 156 hospitals in 12 countries. All of these patients were included in the analyses (1515 in the rt-PA group vs 1520 in the control group), of whom 1617 (53%) were older than 80 years of age. At 6 months, 554 (37%) patients in the rt-PA group versus 534 (35%) in the control group were alive and independent (OHS 0–2; adjusted odds ratio [OR] 1·13, 95% CI 0·95–1·35, p=0·181; a non-significant absolute increase of 14/1000, 95% CI −20 to 48). An ordinal analysis showed a significant shift in OHS scores; common OR 1·27 (95% CI 1·10–1·47, p=0·001). Fatal or non-fatal symptomatic intracranial haemorrhage within 7 days occurred in 104 (7%) patients in the rt-PA group versus 16 (1%) in the control group (adjusted OR 6·94, 95% CI 4·07–11·8; absolute excess 58/1000, 95% CI 44–72). More deaths occurred within 7 days in the rt-PA group (163 [11%]) than in the control group (107 [7%], adjusted OR 1·60, 95% CI 1·22–2·08, p=0·001; absolute increase 37/1000, 95% CI 17–57), but between 7 days and 6 months there were fewer deaths in the rt-PA group than in the control group, so that by 6 months, similar numbers, in total, had died (408 [27%] in the rt-PA group vs 407 [27%] in the control group).
Interpretation
For the types of patient recruited in IST-3, despite the early hazards, thrombolysis within 6 h improved functional outcome. Benefit did not seem to be diminished in elderly patients.
Funding
UK Medical Research Council, Health Foundation UK, Stroke Association UK, Research Council of Norway, Arbetsmarknadens Partners Forsakringsbolag (AFA) Insurances Sweden, Swedish Heart Lung Fund, The Foundation of Marianne and Marcus Wallenberg, Polish Ministry of Science and Education, the Australian Heart Foundation, Australian National Health and Medical Research Council (NHMRC), Swiss National Research Foundation, Swiss Heart Foundation, Assessorato alla Sanita, Regione dell'Umbria, Italy, and Danube University.
Introduction
Each year, about 22 million people have a stroke world-wide,1,2 of whom 4 million reside in high-income countries,3,4 where thrombolytic therapy is affordable and feasible. The burden of ischaemic stroke among the elderly is large and increasing;2,5 and we estimate that annually ischaemic stroke affects about a million people older than 80 years of age in high-income countries and about 3 million in low-income and middle-income countries.
Thrombolytic therapy with intravenous recombinant tissue plasminogen activator (rt-PA), when approved in Europe, was restricted to the treatment of patients younger than 80 years of age with acute ischaemic stroke who could be treated within 3 h. A Cochrane systematic review of the 11 completed trials of thrombolysis (including 3977 patients) with intravenous rt-PA for acute ischaemic stroke showed that treatment was associated with a significant increase in survival free of disability, despite an early 3% excess of fatal intracranial haemorrhage.6 The review also suggested that treatment might be beneficial up to 6 h.6 An individual patient data meta-analysis of a subset of intravenous rt-PA trials further showed that the earlier treatment was given, the greater the chance of a favourable outcome.7 Older people have been under-represented in stroke trials in general,8 and in stroke thrombolysis trials in particular (only 79 people aged older than 80 years had been included in trials of rt-PA).6 As a result of the current European Union (EU) approval criteria, treatment is only applicable to a small proportion of patients with acute stroke.9
The Third International Stroke Trial (IST-3), therefore, had the following objectives: to establish the balance of benefits and harms of thrombolytic therapy with rt-PA in patients who did not exactly meet the licence criteria (especially elderly patients); determine whether a wider range of patients might benefit from this treatment; assess which categories of patients were most likely to benefit by investigating possible interactions between treatment effect and various factors (including age, stroke severity, and early brain imaging results); refine current estimates of the duration of the therapeutic time window; and to improve the external validity and precision of the existing estimates of the overall treat-ment effects (benefits and harms). The primary trial hypothesis was that 0·9 mg/kg rt-PA (maximum 90 mg) given to adult patients of all ages with acute ischaemic stroke, within 6 h of symptom onset, increased the proportion of people who were alive and independent at 6 months.
Methods
Study design and patients
IST-3 was a pragmatic10 international, multicentre, randomised-controlled, open-treatment trial. The initial pilot phase was double-blinded and placebo-controlled. At the end of the pilot phase, since the main phase compared treatment with open control, several additional measures were introduced to minimise bias in the assessment of early and late outcomes.11 We have published reports of the rationale for the trial,12 the protocol,13 an update on recruitment, amendments to the protocol and the baseline characteristics of the patients recruited,11 and the statistical analysis plan.14
The eligibility criteria can be summarised in terms of the uncertainty principle.15–17 Inclusion and exclusion criteria are listed in detail in the protocol.13 Briefly, patients were eligible according to the following criteria: they had symp-toms and signs of clinically definite acute stroke; the time of stroke onset was known; treatment could be started within 6 h of onset; and CT or MRI had reliably excluded both intracranial haemorrhage and structural brain lesions, which could mimic stroke (eg, cerebral tumour). Additionally, if the patient had a clear indication for intravenous thrombolysis with rt-PA, they were to be treated in accordance with local guidelines. Equally, if the patient had a clear contraindication to treatment they were not to be entered in the trial. Only if both the clinician and the patient (or a relevant proxy for the patient) felt that the treatment was promising but unproven, could the patient be included in the trial after appropriate informed consent from the patient or a valid proxy. The protocol was approved by the Multi-centre Research Ethics Committees, Scotland (reference MREC/99/0/78), and by local ethical committees.
This study is registered, ISRCTN25765518.
Procedures
Clinicians entered baseline data via a telephone voice-activated or a secure web-based randomisation system. After the system had recorded and checked the data, patients were allocated either immediate thrombolysis with 0·9 mg/kg of intravenous rt-PA to a maximum of 90 mg (10% bolus with the remainder over 1 h) or control treatment. The system would not accept patients with blood pressure or glucose levels outside protocol-defined criteria (appendix pp 4–5) or other data inconsistencies. The system used a minimisation algorithm to achieve optimum balance for key prognostic factors (table 1), and from January, 2006, minimisation was additionally stratified by world region and then minimised on all the other key factors within regions.
Table 1.
Baseline characteristics
| rt-PA (n=1515) | Control(n=1520) | ||
|---|---|---|---|
| Baseline variables collected before treatment allocation* | |||
| Region† | |||
| Northwest Europe (UK, Austria, Belgium, Switzerland) | 792 (52%) | 797 (52%) | |
| Scandinavia (Norway, Sweden) | 251 (17%) | 250 (16%) | |
| Australasia | 89 (6%) | 90 (6%) | |
| Southern Europe (Italy, Portugal) | 204 (13%) | 204 (13%) | |
| Eastern Europe (Poland) | 174 (11%) | 173 (11%) | |
| Americas (Canada, Mexico) | 5 (<1%) | 6 (<1%) | |
| Age (years)‡ | |||
| 18–50 | 59 (4%) | 68 (4%) | |
| 51–60 | 98 (6%) | 104 (7%) | |
| 61–70 | 188 (12%) | 177 (12%) | |
| 71–80 | 353 (23%) | 371 (24%) | |
| 81–90 | 706 (47%) | 701 (46%) | |
| >90 | 111 (7%) | 99 (7%) | |
| Sex† | |||
| Female | 782 (52%) | 788 (52%) | |
| NIHSS† | |||
| 0–5 | 304 (20%) | 308 (20%) | |
| 6–10 | 422 (28%) | 430 (28%) | |
| 11–15 | 306 (20%) | 295 (19%) | |
| 16–20 | 270 (18%) | 273 (18%) | |
| >20 | 213 (14%) | 214 (14%) | |
| Delay in randomisation†‡ | |||
| 0–3·0 h | 431 (28%) | 418 (28%) | |
| 3·0–4·5 h | 577 (38%) | 600 (39%) | |
| 4·5–6·0 h | 507 (33%) | 500 (33%) | |
| >6·0 h | 0 (0%) | 2 (<1%) | |
| Atrial fibrillation | 473 (31%) | 441 (29%) | |
| Systolic blood pressure | |||
| ≤143 mm Hg | 487 (32%) | 492 (32%) | |
| 144–164 mm Hg | 498 (33%) | 518 (34%) | |
| ≥165 mm Hg | 530 (35%) | 510 (34%) | |
| Diastolic blood pressure§ | |||
| ≤74 mm Hg | 462 (31%) | 445 (29%) | |
| 75–89 mm Hg | 541 (36%) | 588 (39%) | |
| ≥90 mm Hg | 500 (33%) | 480 (32%) | |
| Blood glucose¶ | |||
| ≤5 mmol/L | 254 (18%) | 285 (21%) | |
| 6–7 mmol/L | 664 (48%) | 638 (46%) | |
| ≥8 mmol/L | 455 (33%) | 456 (33%) | |
| Treatment with antiplatelet drugs in previous 48 h† | 775 (51%) | 787 (52%) | |
| Predicted probability of poor outcome at 6 months‖ | |||
| <40% | 351 (23%) | 378 (25%) | |
| 40–50% | 169 (11%) | 160 (11%) | |
| 50–75% | 361 (24%) | 357 (23%) | |
| ≥75% | 634 (42%) | 625 (41%) | |
| Stroke clinical syndrome†** | |||
| TACI | 639 (42%) | 666 (44%) | |
| PACI | 596 (39%) | 551 (36%) | |
| LACI | 168 (11%) | 164 (11%) | |
| POCI | 110 (7%) | 136 (9%) | |
| Other | 2 (<1%) | 3 (<1%) | |
| Baseline variables collected from prerandomisation scan | |||
| Expert reader's assessment of acute ischaemic change†† | ‥ | ‥ | |
| Scan completely normal | 140 (9%) | 129 (8%) | |
| Scan not normal but no sign of acute ischaemic change | 743 (49%) | 781 (51%) | |
| Signs of acute ischaemic change | 624 (41%) | 600 (40%) | |
Data are number (%). Percentages exclude missing values from denominators. rt-PA=recombinant tissue plasminogen activator. NIHSS=National Institutes of Health Stroke Scale. TACI=total anterior circulation infarct. PACI=partial anterior circulation infarct. LACI=lacunar infarct. POCI=posterior circulation infarct.
Data for these variables were gathered via the web-based or telephone randomisation system and had to be entered, complete, and have passed range and consistency checks before the system would issue a treatment allocation.
Variables were used in the minimisation algorithm.
Two patients in the control group were randomly assigned at more than 6 h (protocol violation). One of these was recorded as having severe swelling on the randomisation scan, because the stroke had in fact occurred about 24 h earlier.
Diastolic blood pressure missing for 12 patients in the rt-PA group and seven in the control group.
For the first 282 patients, glucose levels were not recorded. After patient 282, glucose levels were measured at randomisation. One further patient had a missing value.
Risk predicted by novel model designed by Konig and colleagues.18 This model predicts outcome (death or Bartel Index <95) at 3 months. If we assume that those who die between 3 months and 6 months were dependent at 3 months, and those who do not die between 3 months and 6 months do not change their dependency status, then the risk estimates are likely to be quite accurate for death or dependency at 6 months.
Stroke clinical syndrome derived from baseline clinical features assigned by an algorithm (algorithm available on request). For the randomisation algorithm TACI, PACI, and POCI were combined as non-lacunar so the process ensured balance in the number of lacunar syndromes in each treatment group.
Expert panel's masked assessment of prerandomisation scan. This assessment was done by members of the expert panel after randomisation and masked to treatment allocation and all clinical details. Prerandomisation scans were unavailable for eight patients in the rt-PA group and ten in the control group.
To be eligible to join the trial, participating hospitals had to have an organised system of stroke care. Acute-care protocols were not specified by the trial, but had to include the components of effective stroke-unit care,19 including, soon after admission, intravenous access, monitoring of physiological variables, correction of any abnormalities, and where clinically appropriate, intravenous-fluid therapy. All patients in the trial were to be treated within that organised system of stroke care, irrespective of treatment allocation. Patients allocated to the control group were to avoid treatment with rt-PA and received stroke care in the same clinical environment as those allocated to the rt-PA group. Both treatment groups had blood pressure monitored closely over the first 24 h. In the double-blinded phase, both groups were to avoid antiplatelet or anticoagulant therapy for 24 h. In the open phase, patients allocated to the control group were to start aspirin immediately. Blood pressure was managed in the same way in both treatment groups, according to local protocol. Additionally, all centres were asked for their pretrial experience of thrombolysis for treatment of stroke, and if the centre had, before joining the trial, a protocol for open-label use of rt-PA and had treated at least three people in the 12 months before joining the trial, the centre was classed as experienced.
All patients had a CT or MRI brain scan before randomisation and a follow-up scan at 24–48 h. A repeat brain scan was required if the patient deteriorated neurologically or intracranial haemorrhage was suspected for any reason. Although CT scanning was preferred, MRI was allowed. All scans were sent to the trial centre in Edinburgh for masked central rating of any signs of visible early ischaemia (presence and extent of hypo-attenuation, swelling, hyperattenuated artery), haemorrhage, and background brain changes (leukoaraiosis, atrophy, prior stroke lesions, non-stroke lesions) with validated rating methods.20–25 Images were assessed with all original identifiers stripped from the record, and then viewed via a secure web-based image viewing system by an international panel of expert radiologists. All assessments were made masked to all patient details and treatment allocation.
The primary outcome specified in version 1·93 of the protocol and in the published statistical analysis plan14 was the proportion of patients alive and independent as measured by the Oxford Handicap Score (OHS),26 a commonly used variant of the modified Rankin score.27 Patients with an OHS of 0, 1, or 2 were classed as independent. The statistical analysis plan specified an ordinal analysis of the OHS score at 6 months. Additional secondary outcomes were to be reported separately.
Events occurring within 7 days of stroke were recorded by the local trial clinician on the 7-day form: deaths subdivided by cause (swelling of the initial infarct, intracranial haemorrhage, other deaths from the initial stroke, recurrent ischaemic stroke, recurrent stroke of unknown type, any other cause); symptomatic intracranial haemorrhage; recurrent ischaemic stroke; recurrent stroke of unknown type; neurological deterioration attributed to swelling of the initial ischaemic stroke; neurological deterioration not attributable to swelling of the initial ischaemic stroke or haemorrhage; and major extracranial haemorrhage (operational definitions of each of these events are provided in the published protocol13 and statistical analysis plan14). Other fatal and non-fatal non-cerebral events were also recorded and coded. Data on potential reports of any of these events were extracted from the trial database and presented to the adjudication committee who were masked to treatment allocation.
Randomisation and masking
To avoid predictable alternation of treatment allocation, and thus potential loss of allocation concealment, patients were allocated with a probability of 0·80 to the treatment group that would minimise the difference between the groups on the key prognostic factors. Additional details of the procedures used in the double-blinded phase of the study are reported elsewhere.11 The randomisation system informed local clinicians of the patients' unique trial identification number, and the weight-adjusted dose of drug or placebo in the double-blinded phase, or of the weight-adjusted drug dose among those allocated thrombolysis in the open phase, to be given as a 10% bolus with the remainder by an infusion over 1 h.
With the exception of the 276 patients treated in the double-blinded phase of the trial, treatment was given openly and neither the patient nor the treating clinicians were masked. Hospital staff completed an early outcome form at 7 days, death, or hospital discharge, whichever occured first, recording details of events occurring in hospital within 7 days, details of background treatments given and functional status. 6 months after randomisation, general practitioners (or hospital coordinators) were contacted by the IST-3 trial office staff to check that the patient was alive and inform them that they might be approached for follow-up. If appropriate, the IST-3 trial office masked staff then mailed a postal questionnaire to patients to assess outcome. Non-responders were contacted by telephone, and follow-up data was obtained by telephone interview. In Italy and Austria, all follow-ups were done as telephone interviews by a clinician, who was masked to treatment allocation and was highly experienced in outcome assessment. In Portugal, patients were followed up in clinic by clinicians not involved in the patients' initial treatment, again, masked to treatment allocation as far as possible. To assess the durability of any treatment benefit beyond 6 months, patients recruited in the UK (and in other countries where appropriate funding had been obtained) were also followed up at 18 months. All follow-up done by patient contact for these analyses ceased on March 31, 2012, but recording of deaths from national registries of deaths continues in UK, Norway, and Sweden.
Statistical analysis
At the outset of the trial in 2000, we estimated that, among the type of patients likely to be recruited at the time, to detect both an absolute difference of 10% in the proportion of patients alive and independent at 6 months after treatment and to have sufficient power to permit reliable analyses of the prespecified subgroups, a sample of 6000 patients would be needed. A trial of that size could detect a clinically worthwhile net benefit of as little as 3% absolute difference in the primary outcome (80% power, α=0·05). However, it was clear by 2007 that obtaining a sample of 6000 was no longer feasible, and the Steering Committee agreed a revised recruitment target.11 The sample size, re-estimated in 2007 on the basis of event rates in both treatment groups combined, was 3100. This sample size gave 80% power to detect an absolute difference of 4·7% in the primary outcome.11
We monitored the quality and integrity of the accumulating clinical data according to a protocol agreed with the study sponsors, which involved central statistical monitoring according to the principles described by Buyse and colleagues,28 supplemented by onsite monitoring and detailed source data verification in a random sample of 10% of records in centres that had recruited more than 30 patients, or when patterns in the data at a centre seemed anomalous. All IST-3 monitoring procedures were compliant with requirements of all study sponsors, the national ethics committees and regulatory agencies in the 12 participating countries, and they met all appropriate regulatory and Good Clinical Practice requirements. All baseline data, 7-day, and 6-month outcome data were subject to verification checks built into the randomisation and data management system. We monitored all baseline and postrandomisation imaging, which provided additional cross-checks on recruited patients and centre performance. An expert radiologist checked all scans, masked to clinical details and treatment allocation, immediately on receipt at the trial office, for evidence of adverse events and protocol deviations. The independent data monitoring committee met at least annually to review the unmasked data on major outcome events in the trial, on the background stroke-unit care received by trial patients (to ensure it was equal in both treatment groups), relevant external data (including updates of the Cochrane systematic review and reports from large-scale registries of rt-PA use) in strict confidence throughout the course of the trial. The committee judged these data never met the protocol-specified criteria to recommend modification of the protocol or halt recruitment to the study.
The statistical analysis plan was published14 before unmasking of the authors to the data. All randomly assigned patients were included in the analysis. Masked analysis of the patients' baseline characteristics showed clear differences in key prognostic factors (age, stroke severity, degree of ischaemic change on baseline CT or MRI) in patients randomly assigned at different times after stroke onset, which might complicate the estimation of the effect of treatment overall and in subgroups.11 Therefore, the primary analysis of the effect of treatment on the primary outcome was adjusted by logistic regression for linear effects for the following covariates: age; National Institutes of Health stroke scale (NIHSS) score; time from onset of stroke symptoms to randomisation; and presence (vs absence) of ischaemic change on the prerandomisation brain scan according to expert assessment. An unadjusted analysis is also presented.
The trial did not meet its original target of 6000 patients, and so was no longer adequately powered to detect a 3% absolute difference in the primary outcome (with 80% power and α=0·05). The statistical-analysis-plan writing committee, which did not have access to the accumulating data, was therefore expanded to include an independent statistician (Gordon Murray, University of Edinburgh, Edinburgh, UK) to advise on the correct approach. The writing group was persuaded by the recent empirical evidence that the ordinal method was both statistically more efficient (effectively reducing the sample size required in stroke trials29) and robust against substantial deviations from the proportional assumption.30 We therefore specified in the statistical analysis plan an ordinal logistic regression analysis, as a secondary outcome, in which the OHS as a dependent variable had 5 levels: levels 4, 5, and 6 were combined into a single level and levels 0, 1, 2, 3 were retained as distinct.
In this model the treatment odds ratios between one level and the next were assumed to be constant, so a single parameter summarises the shift in outcome distribution between treatment and control groups. For patients known to be alive at 6 months, but with an unknown OHS, we used the level of function recorded on the 7-day form (ie, measured at 7 days or before discharge from hospital) to impute 6-month functional status.14 We chose this simple form of imputation because it effectively classified 6-month outcomes in patients for whom both 7-day and 6-month data were known (data not shown). Analyses were done with SAS (version 9.2).
Role of the funding source
The sponsors of the study had no role in design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Between May, 2000, and July, 2011, 3035 patients were enrolled in 156 centres in 12 countries. Baseline characteristics were well balanced between treatment groups (figure 1, table 1). 1617 (53%) patients were older than 80 years of age. Vital status at 6 months was known for 99% (3011 of 3035) of patients. Overall, 2581 (95%) of 2714 patients with data (data for some relevant variables were not collected in the initial phase) did not meet the prevailing EU-licence-approval criteria. Additional baseline characteristics are shown in appendix pp 2–3.
Figure 1.
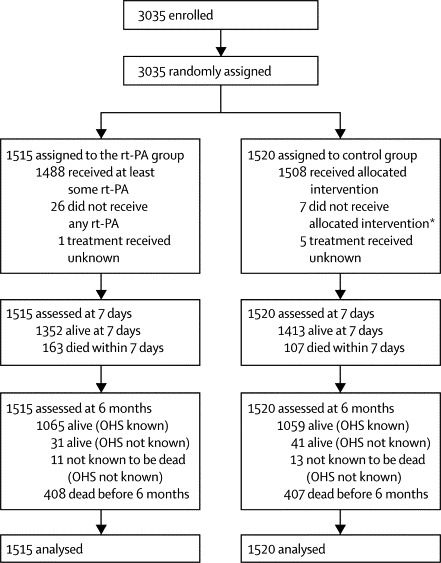
Trial profile
rt-PA=recombinant tissue plasminogen activator. OHS=Oxford Handicap Score. *Of the patients allocated to control, seven actually received some rt-PA. Appendix pp 4–5 gives more detail of treatment actually received and background care.
Of those assigned to the rt-PA group, 26 (2%) did not receive any rt-PA treatment, and of those assigned to the control group, seven (<1%) received at least some rt-PA. Among patients allocated to the rt-PA group, the mean time from randomisation to injection of the bolus was 18 min, the mean time from onset to treatment was 4·2 h (SD 1·2), median 4·2 h (IQR 3·2–5·2). Appendix pp 2–3 documents deviations from the protocol and the background treatments that were given during the first 7 days. Most patients were cared for in a stroke unit, and there was no evidence of a major imbalance in the use of background treatments or place of care (admissions ward, or stroke unit) over the first 7 days; an analysis of blood pressure in patients measured after randomisation showed no significant difference at each timepoint over the first 24 h in either systolic or diastolic blood pressures between the two treatment groups. However, the proportion of those who had spent at least 1 day in a high-dependency area was somewhat higher among patients assigned to the rt-PA group than in the control group (328 [24%] vs 237 [17%]), though in both groups, the median stay in such an area was just 1 day. 76 (49%) centres were classed as experienced in treating stroke with thrombolysis, and 1143 patients were recruited by these centres.
Patients recruited within 1–2 h of onset were significantly more likely to have a more severe neurological deficit did than those recruited at later timepoints after onset (test for linear trend p<0·0001). Similarly, patients recruited at earlier time points were significantly older than those recruited later (test for linear trend p<0·0001). The proportion of patients with a definitely visible ischaemic lesion (vs only possible or no early ischaemic change) on baseline imaging rose with time (test for linear trend p=0·0045).
At 6 months, 554 (37%) in the rt-PA group versus 534 (35%) in the control group were alive and independent in activities of daily living (OHS 0–2; table 2). A secondary ordinal analysis provided evidence of a favourable shift in the distribution of OHS scores at 6 months with treatment (p<0·001; figure 2). More patients died within 7 days in the rt-PA group than in the control group, but between 7 days and 6 months there were correspondingly fewer deaths in the rt-PA group.
Table 2.
Estimated group difference for primary and secondary outcomes at 3 months, 8 months, and 12 months, based on intention-to-treat analysis
| rt-PA (n=1515) | Control (n=1520) |
Adjusted analysis* |
Unadjusted analysis† |
|||||
|---|---|---|---|---|---|---|---|---|
| Odds ratio (95% CI) | p value | Odds ratio (95% CI) | p value | Absolute difference per 1000 (95% CI)‡ | ||||
| Died within 7 days | 163 (11%) | 107 (7%) | 1·60 (1·22 to 2·08) | 0·001 | 1·59 (1·23 to 2·07) | 0·0004 | 37 (17 to 57) | |
| Died between 7 days and 6 months | 245 (16%) | 300 (20%) | 0·73 (0·59 to 0·89) | 0·002 | 0·78 (0·65 to 0·95) | 0·011 | −36 (−63 to −8) | |
| Status at 6 months | ||||||||
| Vital status unknown, disability imputed | 11 | 13 | ‥ | ‥ | ‥ | ‥ | ‥ | |
| Alive at 6 months, disability imputed | 31 | 41 | ‥ | ‥ | ‥ | ‥ | ‥ | |
| Known 6 month vital and disability status | 1473 | 1466 | ‥ | ‥ | ‥ | ‥ | ‥ | |
| Number included in analysis (status known or imputed) | 1515 | 1520 | ‥ | ‥ | ‥ | ‥ | ‥ | |
| OHS at 6 months§ | ||||||||
| 0 | 138 (9%) | 116 (8%) | ‥ | ‥ | ‥ | ‥ | ‥ | |
| 1 | 225 (15%) | 204 (13%) | ‥ | ‥ | ‥ | ‥ | ‥ | |
| 2 | 191 (13%) | 214 (14%) | ‥ | ‥ | ‥ | ‥ | ‥ | |
| 3 | 235 (16%) | 193 (13%) | ‥ | ‥ | ‥ | ‥ | ‥ | |
| 4 | 115 (8%) | 140 (9%) | ‥ | ‥ | ‥ | ‥ | ‥ | |
| 5 | 203 (13%) | 246 (16%) | ‥ | ‥ | ‥ | ‥ | ‥ | |
| Died before 6 months | 408 (27%) | 407 (27%) | 0·96 (0·80 to 1·15) | 0·672 | 1·01 (0·86 to1·19) | 0·924 | 2 (−30 to 33) | |
| Alive and favourable outcome (0+1) | 363 (24%) | 320 (21%) | 1·26 (1·04 to 1·53) | 0·018 | 1·18 (0·99 to 1·41) | 0·055 | 29 (−1 to 59) | |
| Alive and independent (0+1+2)¶ | 554 (37%) | 534 (35%) | 1·13 (0·95 to 1·35) | 0·181 | 1·06 (0·92 to1·24) | 0·409 | 14 (−20 to 48) | |
Data are number (%) unless otherwise stated. rt-PA=recombinant tissue plasminogen activator. OHS=Oxford Handicap Scale.
Odds ratios and p values were calculated by logistic regression after adjusting for age (linear), National Institutes of Health Stroke Scale (linear), time (linear), and presence or absence of visible acute ischaemic change on baseline scan as judged by the expert reader.
p value calculated from test of difference between percentages for rt-PA and control, using normal approximation.
Absolute difference calculated as rt-PA–control, so a positive number indicates this outcome was more frequent in the treatment group.
OHS: 0, no symptoms at all; 1, symptoms, but these do not interfere with everyday life; 2, symptoms that have caused some changes in lifestyle but patients are still able to look after themselves; 3, symptoms that have significantly changed lifestyle and patients need some help looking after themselves; 4, severe symptoms requiring help from other people but not so bad as to need attention day and night; 5, severe handicap needing constant attention day and night.
Primary outcomes.
Figure 2.
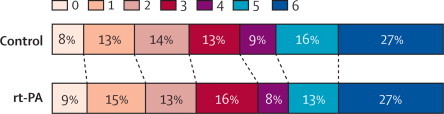
Outcome at 6 months: Oxford Handicap Scale (OHS) by treatment group
For the ordinal analysis, which was adjusted for age, National Institutes of Health Stroke Scale (NIHSS), delay (all linear), and and presence or absence of visible acute ischaemic change on baseline scan as judged by the expert reader, the statistical analysis plan prespecified that OHS levels 4, 5, and 6 were grouped and 0, 1, 2, 3 remained discrete. In that analysis, the common odds ratio was 1·27 (95% CI 1·10–1·47; p=0·001). An ordinal analysis with OHS levels 0, 1, 2, 3, 4, 5, and 6 all discrete, adjusted in the same way, gave an odds ratio of 1·17 (95% CI 1·03–1·33; p=0·016). rt-PA=recombinant tissue plasminogen activator.
Symptomatic intracranial haemorrhage and fatal or non-fatal deterioration due to swelling of the infarct within 7 days occurred in more patients in the rt-PA group than in the control group (table 3). rt-PA was associated with a significant increase in extracranial haemorrhages (table 3).
Table 3.
Fatal and non-fatal cerebral and non-cerebral events within 7 days of randomisation
| rt-PA (n=1515) | Control (n=1520*) |
Adjusted analysis† |
Absolute difference per 1000 (95% CI)‡ | ||||
|---|---|---|---|---|---|---|---|
| Odds ratio (95% CI) | p value | ||||||
| Cerebral events | |||||||
| Symptomatic swelling of original infarct§ | |||||||
| Non-fatal | 21 (1%) | 17 (1%) | 1·23 (0·64 to 2·35) | 0·539 | 3 (−5 to 11) | ||
| Fatal | 47 (3%) | 25 (2%) | 1·89 (1·14 to 3·14) | 0·013 | 15 (4 to 25) | ||
| Total | 68 (4%) | 42 (3%) | 1·66 (1·11 to 2·49) | 0·014 | 17 (4 to 31) | ||
| Symptomatic intracranial haemorrhage¶ | |||||||
| Non-fatal | 49 (3%) | 9 (1%) | 5·56 (2·72 to 11·4) | <0·0001 | 26 (17 to 36) | ||
| Fatal | 55 (4%) | 7 (<1%) | 8·12 (3·68 to 17·9) | <0·0001 | 32 (22 to 42) | ||
| Total | 104 (7%) | 16 (1%) | 6·94 (4·07 to 11·8) | <0·0001 | 58 (44 to 72) | ||
| Neurological deterioration not due to swelling or haemorrhage | |||||||
| Non-fatal | 107 (7%) | 79 (5%) | 1·37 (1·02 to 1·86) | 0·038 | 19 (2 to 36) | ||
| Fatal | 38 (3%) | 49 (3%) | 0·74 (0·48 to 1·14) | 0·167 | −7 (−19 to 5) | ||
| Total | 145 (10%) | 128 (8%) | 1·14 (0·88 to 1·46) | 0·320 | 11 (−9 to 32) | ||
| Recurrent ischaemic stroke | |||||||
| Non-fatal | 18 (1%) | 15 (1%) | 1·21 (0·61 to 2·42) | 0·583 | 2 (−5 to 9) | ||
| Fatal | 3 (0%) | 5 (<1%) | 0·61 (0·14 to 2·57) | 0·499 | −1 (−5 to 2) | ||
| Total | 21 (1%) | 20 (1%) | 1·06 (0·57 to 1·97) | 0·846 | 1 (−8 to 9) | ||
| Recurrent stroke of unknown type | |||||||
| Non-fatal | 1 (<1%) | 2 (<1%) | 0·50 (0·05 to 5·56) | 0·574 | −1 (−3 to 2) | ||
| Fatal | 2 (<1%) | 1 (<1%) | 1·98 (0·18 to 22·3) | 0·581 | 1 (−2 to 3) | ||
| Total | 3 (<1%) | 3 (<1%) | 0·98 (0·20 to 4·89) | 0·981 | 0 (−3 to 3) | ||
| Non-cerebral events‖ | |||||||
| Myocardial infarction | |||||||
| Non-fatal | 18 (1%) | 19 (1%) | 0·89 (0·46 to 1·71) | 0·717 | −1 (−8 to 7) | ||
| Fatal | 5 (<1%) | 4 (<1%) | 1·25 (0·33 to 4·68) | 0·738 | 1 (−3 to 5) | ||
| Total | 23 (2%) | 23 (2%) | 0·95 (0·53 to 1·71) | 0·859 | 0 (−9 to 9) | ||
| Extracranial bleed | |||||||
| Non-fatal | 14 (1%) | 1 (<1%) | 14·5 (1·90 to 110) | 0·010 | 9 (4 to 14) | ||
| Fatal | 2 (<1%) | 2 (<1%) | 0·99 (0·14 to 7·13) | 0·995 | 0 (−3 to 3) | ||
| Total | 16 (1%) | 3 (<1%) | 5·46 (1·59 to 18·8) | 0·007 | 9 (3 to 14) | ||
| Allergic reaction | |||||||
| Non-fatal | 12 (1%) | 0 (0%) | ‥ | ‥ | 8 (3 to 12) | ||
| Fatal | 0 (0%) | 0 (0%) | ‥ | ‥ | 0 (0 to 0) | ||
| Total | 12 (1%) | 0 (0%) | ‥ | ‥ | 8 (3 to 12) | ||
| Total deaths from cerebral causes within 7 days | 145 (10%) | 87 (6%) | 1·76 (1·32 to 2·34) | 0·0001 | 38 (20 to 57) | ||
| Total deaths from non-cerebral causes within 7 days** | 18 (1%) | 20 (1%) | 0·89 (0·47 to 1·69) | 0·717 | −1 (−9 to 7) | ||
| Total deaths within 7 days | 163 (11%) | 107 (7%) | 1·60 (1·22 to 2·08) | 0·001 | 37 (17 to 57) | ||
Data are number (%) unless otherwise stated. rt-PA=recombinant tissue plasminogen activator.
One patient in the control group was missing a 7-day form but did return a 6-month form, so was known to be alive at 7 days. This case has been omitted from the analysis.
Odds ratio and p value calculated from logistic regression after adjusting for age (linear), National Institutes of Health Stroke Scale (linear), time (linear), and presence or absence of visible acute ischaemic change on baseline scan. When no events occurred in one treatment group the logistic model was not applied.
Absolute difference was calculated as rt-PA–control, so a positive number indicates this outcome was more frequent in the treatment group.
Symptomatic swelling of the original infarct was defined as significant neurological deterioration accompanied by evidence of significant brain swelling as determined by the independent masked expert assessment of the scan defined as: shift of the midline away from the side of the ventricle or effacement of the basal cisterns or uncal herniation on a postrandomisation scan (or autopsy if not rescanned before death). The presence of some degree of haemorrhagic transformation was permitted, provided it was not identified by the expert CT reader to be a major contributor to the mass effect.
Symptomatic intracranial haemorrhage was defined as significant neurological deterioration accompanied by clear evidence of significant intracranial haemorrhage on the postrandomisation scan (or autopsy if not rescanned and death occurs after 7 days). Significant haemorrhage was present on any postrandomisation scan if the expert reader both noted the presence of significant haemorrhagic transformation of the infarct or parenchymal haematoma and indicated that haemorrhage was a major component of the lesion (or was remote from the lesion and likely to have contributed significantly to the burden of brain damage). This event included clinical events described as a recurrent stroke within 7 days, in which the recurrent stroke was confirmed to be caused by an intracranial haemorrhage.
Non-fatal cerebral events are exclusive. However, non-fatal non-cerebral events are not exclusive. A given patient could have one or more non-fatal non-cerebral events and a non-fatal cerebral event.
The deaths in the fatal rows are exclusive (a patient can only contribute to one of the fatal rows). Total deaths from non-cerebral causes include deaths not attributed to myocardial infarction, extracranial bleed, or allergic reaction.
To assess the effect of treatment on the primary outcome, the statistical analysis plan predefined a small subset of key prognostic subgroups (figure 3). The subgroup analyses are of the adjusted effects and take account of the fact that, for a specific prognostic factor, the distribution of other factors might differ between subcategories. For example, in older patients the time to randomisation was shorter. The subgroup analyses for a specific factor provide estimated effects within sub-categories that adjust for such imbalances. Overall, little variation occurred in the adjusted effects of treatment in different subgroups. However, a significant difference did occur in the adjusted effect of treatment between patients older than 80 years and in patients 80 years or younger (p=0·027), suggesting greater benefit in those older than 80 years of age; contrary to expectations.14 Treatment appeared at least as effective in this age group as in younger patients. Significant trends towards larger effects of treatment in more severe strokes were also seen (as assessed by the NIHSS and by the predicted probability of a poor outcome18). Benefit was greatest in patients treated within 3 h, but there was insufficient power to examine decay of benefit with time. An analysis of the treatment effect in each of three equal-sized cohorts of patients (ie, those recruited in 2000–06, 2007–08, 2009–11) did not provide any evidence of period effects (data not shown). We also undertook a sensitivity analysis restricted to the 2939 (96%) patients with known 6-month vital and disability status (appendix pp 4–5), and the results were not qualitatively different from those in table 2.
Figure 3.
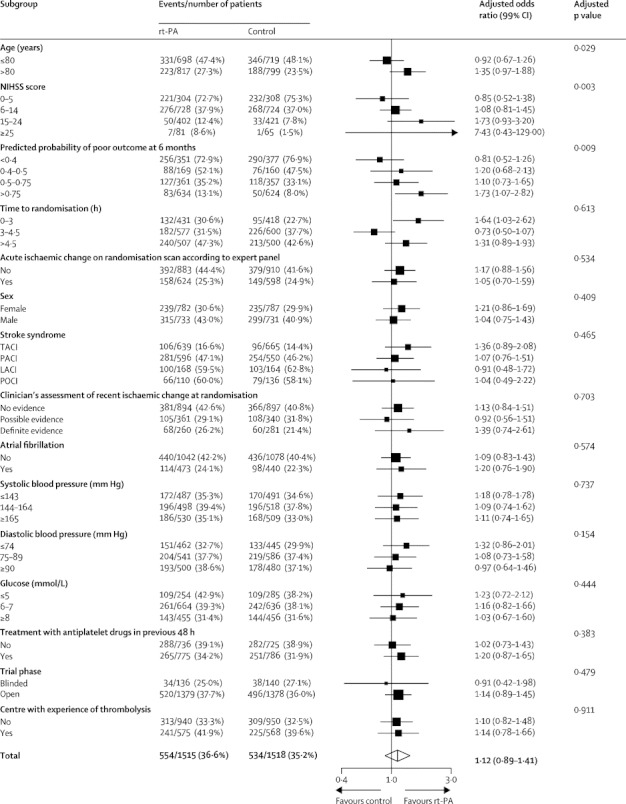
Adjusted effect of treatment on the primary outcome (alive and independent, Oxford Handicap Score 0, 1, or 2) in subgroups
The key predefined subgroups were age 80 years or younger, age older than 80 years, time from stroke onset to randomisation (0–3·0 h, 3·0–4·5 h, 4·5–6·0 h), initial stroke severity as measured by National Institutes of Health stroke score, and the appearance of the baseline brain scan on expert read for each subgroup (whether ischaemic change is visible or not). The treatment odds ratio in each subgroup has been adjusted for the linear effects of the other key variables (age, NIHSS, and delay) but not for the presence or absence visible ischaemic change. It is for this reason that the adjusted odds ratio in the “Total” row at the bottom of the table does not exactly agree with the odds ratio in table 2. The choice of cut-points to define certain subgroups is slightly different to those given in table 1.14 On the graph, for each subgroup, the horizontal line represents the 99% CI, the diamond is centred on the overall estimate and it represents the 95% CI. The graph was generated with R (version 2.11.1). rt-PA=recombinant tissue plasminogen activator. NIHSS=National Institutes of Health Stroke Scale. TACI=total anterior circulation infarct. PACI=partial anterior circulation infarct. LACI=lacunar infarct. POCI=posterior circulation infarct.
Discussion
Although the increase in the number of patients treated with rt-PA who were alive and independent at 6 months was smaller than originally anticipated and was not significant, the secondary analysis provides supportive evidence of benefit. The ordinal analysis provided evidence that on average, patients treated with intravenous thrombolysis up to 6 h after stroke survived with less disability. At 6 months, vital status was known for most patients and there was no evidence of any difference in the number of deaths, despite the excess of deaths within 7 days of stroke (mainly due to intracranial haemorrhage). Since mortality at 6 months was equal in the two groups, and in view of the evidence that the lower the patients' degree of disability at 6 months, the greater their subsequent survival,31 long-term follow-up beyond 6 months is important. Follow-up for survival, therefore, continues in the UK, Norway, and Sweden to assess whether an overall survival advantage from rt-PA after 6 months emerges.
Since we sought to recruit older patients and patients who did not strictly meet prevailing licence criteria for thrombolytic therapy with rt-PA, we anticipated a higher risk of adverse events, chiefly symptomatic intracranial haemorrhage. The patient information leaflet stated that rt-PA treatment might be associated with an increased risk of fatal intracranial haemorrhage of 4%, which indeed was the rate reported in the trial. Furthermore, applying a similar definition of symptomatic intra-cerebral haemorrhage as in the Cochrane systematic review, the frequency of this disorder within 7 days in IST-3 patients treated with rt-PA (6·8%) was comparable with the 7·3% reported in the Safe Implementation of Thrombolysis in Stroke (SITS) registry of 6483 patients treated within licence in routine clinical practice.32 We also expected a higher risk of death in the control group, and a smaller proportion alive and independent than in previous trials. Reassuringly, despite the different event rates in the control group, for most of the outcomes, there was no clear evidence that the effects of treatment were qualitatively different in IST-3 to those seen in earlier randomised trials, with two exceptions. We identified significant trends towards larger effects of treatment in patients with more severe strokes. We also anticipated a reduction in fatal and non-fatal neurological deterioration due to swelling of the initial infarct,6 so the clear 17 per 1000 excess was unexpected, and inconsistent with data from previous trials.6
As proposed by Kent and colleagues,33 we reported the effect of treatment on the primary outcome in several prespecified subgroups and included the effects sub-divided by the result of a prognostic score. Benefit with treatment was greatest within 3 h, but the analyses did not have sufficient power to define the shape of the relation between benefit and time beyond 3 h. The effect of treatment in patients older than 80 years of age was at least as large as in patients younger than 80 years of age. A formal test for trend showed a significant difference for greater benefit of rt-PA in patients with increasingly severe strokes. However, in view of the overall non-significant benefit for the primary outcome, the significant interactions across subgroups in these analyses should be interpreted with caution. As specified in the statistical analysis plan, we planned additional secondary analyses to explore these apparent effects on the primary outcome (and on other outcomes, such as symptomatic intracranial haemorrhage) and to decide if these effects were due to chance.
Lyden34 has identified limitations in these data, chiefly that IST-3 recruited only half the number of patients originally intended and so was underpowered for the primary outcome (and more so for the subgroup analyses). The many changes in the regulatory environment over the course of the trial delayed the approval of the trial in many centres and precluded the participation of several countries and hence was a significant factor in our failing to achieve our original target.11 Nonetheless, the trial was the largest-ever trial of thrombolysis therapy for stroke34 (over three times larger than any previous trial) and included more patients treated within 3 h of stroke (n=849) than were included in the National Institute of Neurological Disorders and Stroke (NINDS) trial (n=624), the only previous trial examining specifically treatment within 3 h (panel). The fact that most of the IST-3 patients treated within 3 h were older than 80 years of age (n=726), yet achieved similar benefit to younger patients in NINDS trial, adds to the NINDS trial.
Panel. Research in context.
Systematic review
To update the published systematic review of randomised-controlled trials of recombinant tissue plasminogen activator (rt-PA) in patients with acute ischaemic stroke and incorporate the third International Stroke Trial (IST-3) results,6 we searched for additional randomised trials of intravenous rt-PA versus control within 6 h of onset of acute ischaemic stroke up to March 30, 2012, in the Cochrane Stroke Trials Registry (November, 2011), Internet Stroke Trials Centre (March, 2011), Medline and Embase (search strategy available on request), and references lists in review articles and conference abstracts. The primary analysis was for all patients treated up to 6 h after stroke. Data were available for 7012 patients in 12 trials. We tested for heterogeneity between the estimates of effect for key outcomes from two strata: all trials before IST-3 and IST-3. The tests for heterogeneity in the proportional effects of treatment across these two strata were not significant for symptomatic intracranial haemorrhage (χ2 2·13, p=0·1), deaths within 7 days (χ2 1·44, p=0·2), deaths by the end of follow-up (χ2 1·0, p=0·3) and, the proportion alive and independent (modified Rankin score 0–2: χ2 3·08, p=0·08). Similarly, no heterogeneity occurred across the two strata for patients of all ages treated within 3 h (χ2 0·25, p=0·6). The review established that the effects of treatment reported in IST-3—in this wider range of patients (generally outside the current approvals)—were consistent with those seen in previous trials.
Interpretation
By providing estimates on the benefits and harms of treating patients with acute ischaemic stroke outside the current approvals, IST-3 enables clinicians to consider thrombolytic treatment for a wider range of patients, especially those older than 80 years of age. The data reinforce the need for further efforts to increase the proportion of all ischaemic strokes treated within 3 h. The additional data from IST-3 give greater confidence that mortality is not increased by treatment. The implications for ongoing research are that the data strengthen the rationale for the ongoing trials of thrombolysis in patients presenting more than 4·5 h after onset of stroke, and suggest that the imposition of upper age limits on future trials in acute stroke will become harder to justify.
The absence of masking is most relevant for the assessment of the events within 7 days. However, every possible precaution was taken to ensure masking of the expert panel assessing the scans, and the adjudication committee, who also assessed clinical data on all potential cerebral events. The proportional effect of treatment on fatal and non-fatal events within 7 days was very similar, which perhaps suggest that masking of the assessors was successful. The self-assessment at 6 months by patients or their carer by postal questionnaire or masked telephone interview was unmasked and so could be subject to reporting bias.34 However, self-reported outcome by patients is necessarily subjective and affected by many things besides knowledge of treatment allocation. The subgroup analysis subdivided by trial phase provides some reassurance in that no significant difference was seen in the effect of treatment on the primary outcome in the double-blind phase and the open phase (figure 3). The measurement of outcome with OHS at 6 months is different from previous trials that measured the modified Rankin score at 3 months. When we planned IST-3 in 1998, the modified Rankin score and OHS were judged to be equivalent. Both are derivatives of the original Rankin scale, developed by members of our group. While the proportion of patients recorded as dependent might be slightly different with each scale, the choice of outcome scale would not bias the assessment of treatment effect between treatment and control groups.
The outcome was recorded at 6 months and 18 months, to assess the effects on survival free of disability after a few months and also in the long term (the longer the benefit persists, the greater the cost-effectiveness). The longer time to follow-up allowed any differential effect of rt-PA on early and late death to become clearer. Outcome (other than survival) was not recorded at 3 months, although the proportional effects on death and disability seen at 6 months in IST-3 are comparable with those seen at 3 months in previous trials.
Lyden also comments that the sampling approach to monitoring in IST-3 was less intense than in many commercial studies, and is a potential concern, but also states: “many clinical trialists believe that source verification of some clinical trial data assures safety, accuracy, and validity of the trial data. Authorities do not agree on the minimum quantity of verified data to assure validity (100%, half, 10% sample)…but there is no evidence to suggest any problems with the [IST-3] data set due to limited monitoring.”34
When the results of IST-3 are incorporated into an updated systematic review,35 the estimates of relative treatment effect are broadly compatible with the previous rt-PA trials for each of the main outcomes: alive and independent; death at final follow-up; and fatal intracranial haemorrhage.
Our trial was underpowered to reliably detect important subgroup effects, and so a collaborative individual patient data meta-analysis (the Stroke Thrombolysis Trialists Collaboration [STTC]) has been established, which will include data from all the completed intravenous rt-PA trials and will update the previous pooled analysis.7 The meta-analysis will explore which baseline factors, other than time, might modify the effects of treatment on major outcomes (such as death, functional outcome, and intracerebral haemorrhage), and so provide better guidance for clinicians and patients to apply this treatment as effectively as possible in routine practice.
For the types of patient recruited in IST-3 (about three quarters of whom were randomised after 3 h, and half of all patients were older than 80 years of age), by 6 months there was evidence that rt-PA improved functional outcome. The data add weight to the policy of treating patients as soon as possible, and also justify extending treatment to patients older than 80 years of age. The data do not support any restriction of treatment on the basis of stroke severity or the presence of early ischaemic change on the baseline brain scan. The data support the need for randomised trials of thrombolysis in selected patients more than 4·5 h after stroke.
Correspondence to: Prof Peter Sandercock, Division of Clinical Neurosciences, University of Edinburgh, Western General Hospital, Crewe Road, Edinburgh EH4 2XU, UK
Acknowledgments
Acknowledgments
The IST-3 collaborative group thanks all the patients who participated in the study, and the many individuals not specifically mentioned in the paper who have supported the study. IST-3 is an investigator led trial. The University of Edinburgh and the Lothian Health Board are cosponsors. The start-up phase was supported by a grant from the Stroke Association, UK. The expansion phase was funded by The Health Foundation UK. The main phase of the trial is funded by the following organisations: UK MRC (grant numbers G0400069 and EME 09-800-15) and managed by NIHR on behalf of the MRC-NIHR partnership; The Research Council of Norway; AFA Insurances (Sweden); the Swedish Heart Lung Fund; The Foundation of Marianne and Marcus Wallenberg; Stockholm County Council and Karolinska Institute Joint ALF-project grants (Sweden); the Government of Poland (grant number 2PO5B10928); the Australian Heart Foundation (grant number G 04S 1638); Australian NHMRC (grant number 457343); the Swiss National Research Foundation; the Swiss Heart Foundation; Foundation for health and cardio-/neurovascular research, Basel, Switzerland; the Assessorato alla Sanita, Regione dell'Umbria; Danube University, Krems, Austria. Drug and placebo for the 300 patients in the double-blind component of the start-up phase were supplied by Boehringer Ingelheim. We thank the NIHR Stroke Research Network, NHS Research Scotland, through the Scottish Stroke Research Network, and the National Institute for Social Care and Health Research Clinical Research Centre for their support. The imaging work was undertaken at the Brain Imaging Research Centre, a member of the SINAPSE collaboration, at the Division of Clinical Neurosciences, University of Edinburgh. SINAPSE is funded by the Scottish Funding Council and the Chief Scientist Office of the Scottish Executive. Additional support was received from Chest Heart and Stroke Scotland, DesAcc, University of Edinburgh, Danderyd Hospital R&D Department, Karolinska Institutet, Oslo University Hospital, and the Dalhousie University Internal Medicine Research Fund. This report presents independent research supported by the NIHR through the UK Stroke Research Network. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health.
Contributors
The study was conceived by the co-chief investigators, PS, RIL, and JMW. JMW led the development of all of the imaging aspects of the study. The study was designed by PS, RIL, and JMW, with input from all the other listed contributors who act as coordinators of the trial in their own country. PS, RIL, JMW, MD, and KI designed the study and wrote the protocol. KI is the study coordinator. GC is the study statistician who prepared the analyses for this paper. PS, RIL, MD, GV, AC, AK, EB, KBS, VM, AP, GJH, KM, MB, SR, GG, SJP, AA, MC, and PL recruited patients to the study. GV, AC, AK, EB, KBS, VM, AP, GJH, KM, MB, SR, GG, SJP, AA, MC, and PL acted as National Coordinators. PS drafted the Article and all authors commented on drafts and approved the final version.
IST-3 collaborative group
The members of the collaborative group are listed in full in the appendix.
Writing committee
Peter Sandercock (University of Edinburgh, Edinburgh, Scotland), Joanna M Wardlaw (University of Edinburgh, Edinburgh, Scotland), Richard I Lindley (Sydney Medical School – Westmead Hospital and The George Institute for Global Health, University of Sydney, Australia), Martin Dennis (University of Edinburgh, Edinburgh, Scotland), Geoff Cohen, Gordon Murray, Karen Innes (University of Edinburgh, Edinburgh, Scotland), Graham Venables (Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, UK), Anna Czlonkowska (Medical University of Warsaw, Warsaw, Poland), Adam Kobayashi (Medical University of Warsaw, Warsaw, Poland), Stefano Ricci (Department of Neurology ASL1, Ospedale, Citta' di Castello, Italy), Veronica Murray (Karolinska Institutet, Stockholm, Sweden), Eivind Berge (Oslo University Hospital, Oslo, Norway), Karsten Bruins Slot (Oslo University Hospital, Oslo, Norway), Graeme J Hankey (Royal Perth Hospital, Perth, Australia), Manuel Correia (Hospital Geral de Santo Antonio, Porto, Portugal), Andre Peeters (Cliniques Universitaires Saint-Luc, Bruxelles, Belgium), Karl Matz (Landesklinikum Donauregion Tulln, Tulln, Austria), Phillippe Lyrer (University Hospital Basel, Basel, Switzerland), Gord Gubitz (Dalhousie University and Queen Elizabeth II Health Sciences Centre, Halifax, Canada), Stephen J Phillips (Dalhousie University and Queen Elizabeth II Health Sciences Centre, Halifax, Canada), Antonio Arauz (Instituto Nacional de Neurologia, Mexico City, Mexico).
Trial steering committee
Independent chairmen: Colin Baigent (University of Oxford, Oxford UK); David Chadwick (University of Liverpool, Liverpool UK). Independent member: Pippa Tyrrell (University of Manchester, Manchester, UK); Gordon Lowe (University of Glasgow, Glasgow, UK). Co-principal investigators: PS; RIL. Chief investigator for neuroradiology: JMW; MD. Statistician: GC. Trial Co-ordinator: KI. Lay representative: Heather Goodare.
CT and MRI reading panel
JMW, Andrew Farrall, Rüdiger von Kummer, Lesley Cala, Anders von Heijne, Zoe Morris, Alessandro Adami, AP, Gillian Potter, Nick Brady.
Data monitoring committee
Rory Collins (Oxford University, Oxford, UK; Chairman), Philip Bath (Nottingham University, Nottingham, UK), Jan van Gijn (University of Utrecht, Utrecht, Netherlands), Richard Gray (University of Oxford, Oxford, UK), Robert Hart (McMaster University, ON, Canada), Salim Yusuf (McMaster University, ON, Canada).
Event adjudication committee
Keith Muir (Institute of Neurological Science, University of Glasgow, Glasgow, UK), PS, RIL.
National coordinators and associate national coordinators
Australia: RIL, GJH. Austria: KM, Michael Brainin. Belgium: AP. Canada: GG, SJP. Italy: SR. Mexico: AA. Norway: EB, KBS. Poland: AC, AK. Portugal: MC. Switzerland: PL; Stefan Engelter. Sweden: VM, Andreas Terent, Bo Norrving, Per Wester: UK: GV.
Trial coordinating centres
Division of Clinical Neuroscience, University of Edinburgh, Edinburgh, Scotland: KI, Alison Clark, David Perry, Vera Soosay, David Buchanan, Sheila Grant, Eleni Sakka, Jonathan Drever, Pauli Walker, Indee Herath, Ann Leigh Brown, Paul Chmielnik, Christopher Armit, Andrea Walton, Mischa Hautvast, Steff Lewis, Graeme Heron, Sylvia Odusanya, Pam Linksted, Ingrid Kane, Will Whiteley, Robin Sellar, Philip White, Peter Keston, Andrew Farrell, Zoe Morris, Hector Miranda. Clinical Trials Service Unit, Oxford, UK: Lisa Blackwell.
National coordinating centres
Italy (up to Sept, 2008): Maria Grazia Celani; Enrico Righetti. Italy (after Sept, 2008): Silvia Cenciarelli; Tatiana Mazzoli. Central follow-up for Italy: Teresa Anna Cantisani. Poland: Jan Bembenek. Sweden: Eva Isaakson. Norway: EB, KBS. Australia: Genevieve Freys. The list of participating hospitals in each country is in the appendix.
Conflicts of interest
EB has received honoraria for lectures at meetings arranged by Boehringer Ingelheim, and reimbursement for costs for attending these meetings. AC has received lecture fees and conference travel costs from Boehringer Ingelheim. GB has received honoraria and speaker fees from Boehringer Ingelheim, Sanofi Synthlabo Aventis, Hoffman La Roche, and Novo Nordisk. AK has received lecture fees and conference travel costs from Boehringer Ingelheim. RIL has received payment in his role as conference scientific committee member and for occasional lectures from Boehringer Ingelheim; has attended national stroke meetings organised and funded by Boehringer Ingelheim; and is not a member of any industry advisory boards. PS has received lecture fees (paid to the Division of Clinical Neurosciences, University of Edinburgh) and travel expenses from Boehringer Ingelheim for occasional lectures given at international conferences; and was a member of the Independent Data and Safety Monitoring Board (DSMB) of the Randomized Evaluation of Long-Term Anticoagulation Therapy (RE-LY) trial funded by Boehringer Ingelheim and received attendance fees and travel expenses for attending DSMB meetings (paid to the Division of Clinical Neurosciences, University of Edinburgh). KBS has received an honorarium for a lecture from Boehringer Ingelheim and had costs for participating in scientific meetings reimbursed; is a member of the European Medicines Agency's Committee for Medicinal Products for Human Use (CHMP) and the Cardiovascular Working Party. The views expressed in this article are the personal views of KBS and should not be understood or quoted as being made on behalf of or reflecting the position of the European Medicines Agency or one of its committees or working parties. VM has received an unrestricted educational grant for a meeting on thrombolysis in stroke at which IST-3 was discussed. JMW received reimbursement for reading CT scans for European Cooperative Acute Stroke Study III (ECASS III) from Boehringer Ingelheim in the form of funding to her department, the Division of Clinical Neurosciences, University of Edinburgh; is the contact reviewer for the Cochrane systematic reviews of thrombolytic treatment for acute stroke; has attended meetings held by Boehringer Ingelheim as an unpaid independent external adviser during the licensing of rt-PA, but was refunded her travel expenses and the time away from work; has attended and spoken at national and international stroke meetings organised and funded by Boehringer Ingelheim for which she received honoraria and travel expenses; and is director of the Brain Research Imaging Centre for Scotland, which is located within the Department of Clinical Neurosciences at the University of Edinburgh, Edinburgh, Scotland and houses a research MRI scanner, which was funded by the UK Research Councils Joint Research Equipment Initiative, supplemented by grants and donations from various other sources including Novartis, Schering, General Electric, and Boehringer Ingelheim. These commercial sources contributed to the purchase of the scanner, but not the running costs or any individual studies. All other members of the writing committee declare that they have no conflicts of interest.
Supplementary Material
References
- 1.Strong K, Mathers C, Bonita R. Preventing stroke: saving lives around the world. Lancet Neurol. 2007;6:182–187. doi: 10.1016/S1474-4422(07)70031-5. [DOI] [PubMed] [Google Scholar]
- 2.Rothwell PM, Coull AJ, Giles MF, the Oxford Vascular Study Change in stroke incidence, mortality, case-fatality, severity, and risk factors in Oxfordshire, UK from 1981 to 2004 (Oxford Vascular Study) Lancet. 2004;363:1925–1933. doi: 10.1016/S0140-6736(04)16405-2. [DOI] [PubMed] [Google Scholar]
- 3.Feigin VL, Lawes CM, Bennett DA, Barker-Collo SL, Parag V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol. 2009;8:355–369. doi: 10.1016/S1474-4422(09)70025-0. [DOI] [PubMed] [Google Scholar]
- 4.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367:1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 5.Islam MS, Anderson CS, Hankey GJ. Trends in incidence and outcome of stroke in Perth, Western Australia during 1989 to 2001: the Perth Community Stroke Study. Stroke. 2008;39:776–782. doi: 10.1161/STROKEAHA.107.493643. [DOI] [PubMed] [Google Scholar]
- 6.Wardlaw JM, Murray V, Berge E, Del Zoppo GJ. Thrombolysis for acute ischaemic stroke. Cochrane Database Syst Rev. 2009;4 doi: 10.1002/14651858.CD000213.pub2. CD000213. [DOI] [PubMed] [Google Scholar]
- 7.Lees KR, Bluhmki E, von Kummer R, the ECASS, ATLANTIS, NINDS and EPITHET rt-PA Study Group Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet. 2010;375:1695–1703. doi: 10.1016/S0140-6736(10)60491-6. [DOI] [PubMed] [Google Scholar]
- 8.Sanossian N, Ovbiagele B. Prevention and management of stroke in very elderly patients. Lancet Neurol. 2009;8:1031–1041. doi: 10.1016/S1474-4422(09)70259-5. [DOI] [PubMed] [Google Scholar]
- 9.Bembenek J, Kobayashi A, Sandercock P, Czlonkowska A. How many patients might receive thrombolytic therapy in the light of the ECASS-3 and IST-3 data? Int J Stroke. 2010;5:430–431. doi: 10.1111/j.1747-4949.2010.00479.x. [DOI] [PubMed] [Google Scholar]
- 10.Ware JH, Hamel MB. Pragmatic trials–guides to better patient care? N Engl J Med. 2011;364:1685–1687. doi: 10.1056/NEJMp1103502. [DOI] [PubMed] [Google Scholar]
- 11.Sandercock P, Lindley R, Wardlaw J, the IST-3 collaborative group Update on the third international stroke trial (IST-3) of thrombolysis for acute ischaemic stroke and baseline features of the 3035 patients recruited. Trials. 2011;12:252. doi: 10.1186/1745-6215-12-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Whiteley W, Lindley R, Wardlaw J, Sandercock P, the IST-3 Collaborative Group Third international stroke trial. Int J Stroke. 2006;1:172–176. doi: 10.1111/j.1747-4949.2006.00043.x. [DOI] [PubMed] [Google Scholar]
- 13.Sandercock P, Lindley R, Wardlaw J. Third international stroke trial (IST-3) of thrombolysis for acute ischaemic stroke. Trials. 2008;9:37. doi: 10.1186/1745-6215-9-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sandercock P, Lindley R, Wardlaw J, Whiteley W, Murray G, the ST-3 collaborative group Statistical analysis plan for the third International Stroke Trial (IST-3); part of a ‘thread’ of reports of the trial. Int J Stroke. 2012;7:186–187. doi: 10.1111/j.1747-4949.2012.00782.x. [DOI] [PubMed] [Google Scholar]
- 15.Warlow C, D'Hooghe M, Joos F. MRC European Carotid Surgery Trial: interim results for symptomatic patients with severe (70–99%) or with mild (0–29%) carotid stenosis. Lancet. 1991;337:1235–1243. [PubMed] [Google Scholar]
- 16.Peto R, Baigent C. Trials: the next 50 years. Large scale randomised evidence of moderate benefits. BMJ. 1998;317:1170–1171. doi: 10.1136/bmj.317.7167.1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Collins R, MacMahon S. Reliable assessment of the effects of treatment on mortality and major morbidity, I: clinical trials. Lancet. 2001;357:373–380. doi: 10.1016/S0140-6736(00)03651-5. [DOI] [PubMed] [Google Scholar]
- 18.König IR, Ziegler A, Bluhmki E, the Virtual International Stroke Trials Archive (VISTA) Investigators Predicting long-term outcome after acute ischemic stroke: a simple index works in patients from controlled clinical trials. Stroke. 2008;39:1821–1826. doi: 10.1161/STROKEAHA.107.505867. [DOI] [PubMed] [Google Scholar]
- 19.Langhorne P, Pollock A, the Stroke Unit Trialists' Collaboration What are the components of effective stroke unit care? Age Ageing. 2002;31:365–371. doi: 10.1093/ageing/31.5.365. [DOI] [PubMed] [Google Scholar]
- 20.Barber PA, Demchuk AM, Zhang J, Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score. Lancet. 2000;355:1670–1674. doi: 10.1016/s0140-6736(00)02237-6. [DOI] [PubMed] [Google Scholar]
- 21.Wardlaw JM, Sellar RJ. A simple practical classification of cerebral infarcts on CT and its interobserver reliability. AJNR Am J Neuroradiol. 1994;15:1933–1939. [PMC free article] [PubMed] [Google Scholar]
- 22.Wardlaw JM, Farrall AJ, Perry D, the Acute Cerebral CT Evaluation of Stroke Study (ACCESS) Study Group Factors influencing the detection of early CT signs of cerebral ischemia: an internet-based, international multiobserver study. Stroke. 2007;38:1250–1256. doi: 10.1161/01.STR.0000259715.53166.25. [DOI] [PubMed] [Google Scholar]
- 23.van Swieten JC, Hijdra A, Koudstaal PJ, van Gijn J. Grading white matter lesions on CT and MRI: a simple scale. J Neurol Neurosurg Psychiatry. 1990;53:1080–1083. doi: 10.1136/jnnp.53.12.1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cordonnier C, Potter GM, Jackson CA. Improving inter-rater agreement about brain microbleeds. Development of the Brain Observer MicroBleed Scales (BOMBS) Stroke. 2009;49:94–99. doi: 10.1161/STROKEAHA.108.526996. [DOI] [PubMed] [Google Scholar]
- 25.Farrell C, Chappell F, Armitage PA. Development and initial testing of normal reference MR images for the brain at ages 65–70 and 75–80 years. Eur Radiol. 2009;19:177–183. doi: 10.1007/s00330-008-1119-2. [DOI] [PubMed] [Google Scholar]
- 26.Bamford J, Sandercock P, Dennis M, Burn J, Warlow C. A prospective study of acute cerebrovascular disease in the community: the Oxfordshire Community Stroke Project—1981–86. 2. Incidence, case fatality rates and overall outcome at one year of cerebral infarction, primary intracerebral and subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry. 1990;53:16–22. doi: 10.1136/jnnp.53.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19:604–607. doi: 10.1161/01.str.19.5.604. [DOI] [PubMed] [Google Scholar]
- 28.Buyse M, George SL, Evans S. The role of biostatistics in the prevention, detection and treatment of fraud in clinical trials. Stat Med. 1999;18:3435–3451. doi: 10.1002/(sici)1097-0258(19991230)18:24<3435::aid-sim365>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 29.Bath PM, Gray LJ, Collier T, Pocock S, Carpenter J, the Optimising Analysis of Stroke Trials (OAST) Collaboration Can we improve the statistical analysis of stroke trials? Statistical reanalysis of functional outcomes in stroke trials. Stroke. 2007;38:1911–1915. doi: 10.1161/STROKEAHA.106.474080. [DOI] [PubMed] [Google Scholar]
- 30.McHugh GS, Butcher I, Steyerberg EW. A simulation study evaluating approaches to the analysis of ordinal outcome data in randomized controlled trials in traumatic brain injury: results from the IMPACT Project. Clin Trials. 2010;7:44–57. doi: 10.1177/1740774509356580. [DOI] [PubMed] [Google Scholar]
- 31.Slot KB, Berge E, Dorman P, Lewis S, Dennis M, Sandercock P, the Oxfordshire Community Stroke Project, the International Stroke Trial (UK), and the Lothian Stroke Register Impact of functional status at six months on long term survival in patients with ischaemic stroke: prospective cohort studies. BMJ. 2008;336:376–379. doi: 10.1136/bmj.39456.688333.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wahlgren N, Ahmed N, Dávalos A, the SITS-MOST investigators Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke-Monitoring Study (SITS-MOST): an observational study. Lancet. 2007;369:275–282. doi: 10.1016/S0140-6736(07)60149-4. [DOI] [PubMed] [Google Scholar]
- 33.Kent DM, Rothwell PM, Ioannidis JP, Altman DG, Hayward RA. Assessing and reporting heterogeneity in treatment effects in clinical trials: a proposal. Trials. 2010;11:85. doi: 10.1186/1745-6215-11-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lyden PD. In Anticipation of International Stroke Trial-3 (IST-3) Stroke. 2012 doi: 10.1161/STROKEAHA.112.656876. published online May 3. [DOI] [PubMed] [Google Scholar]
- 35.Wardlaw JM, Murray V, Berge E. Recombinant tissue plasminogen activator for acute ischaemic stroke: an updated systematic review and meta-analysis. Lancet. 2012 doi: 10.1016/S0140-6736(12)60738-7. published online May 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


