ABSTRACT
Accelerated formation and accumulation of advanced glycation end-products occur under circumstances of increased supply of substrates such as hyperglycaemic or oxidative stress and in age-related and chronic diseases like diabetes mellitus, chronic renal failure, neurodegenerative diseases, osteoarthritis and also non-diabetic atherosclerosis and chronic heart failure. Advanced glycation end-products accumulation occurs especially on long-lived proteins such as collagen in the skin and in vascular basement membranes leading to vascular damage. Adequate renal clearance capacity is an important factor in the effective removal of advanced glycation end-products. The Autofluorescence Reader was developed as a marker, representative for tissue advanced glycation end-products accumulation, easily applicable in a clinical setting, initially for predicting diabetes related complications. Studies have already shown a relationship between skin autofluorescence and diabetes complications, as well as its predictive value for total and cardiovascular mortality in type 2 diabetes. Moreover skin autofluorescence was demonstrated to be superior to Haemoglobin A1c and other conventional risk factors. Advanced glycation end-products have been proposed as a novel factor involved in the development and progression of chronic heart failure. Assessment of advanced glycation end-products accumulation in end-stage renal disease and undergoing renal replacement therapies patients has become of great importance. Cardiovascular and connective tissue disorders are very common in patients with end-stage renal disease, and the accumulation of advanced glycation end-products is significantly increased in these patients. Mortality is markedly increased in patients with decreased kidney function, particularly in patients with end-stage renal disease. Skin advanced glycation end-products levels are strong predictors of survival in haemodialysis patients independent of other established risk factors. The Autofluorescence Reader may be useful as a clinical tool for rapid assessment of risk for advanced glycation end-products related long-term complications, not only in diabetes, but in other conditions associated with advanced glycation end-products accumulation as well.
Keywords: advanced glycation end-products, skin autofluorescence, metabolic stess, chronic kidney disease
This review focuses on the relationship between advanced glycation end-products (AGEs) accumulation and long-term complications in patients with diabetes and end-stage renal disease (ESRD) treated by dialysis and the clinical relevance of assessing AGEs accumulation in these patients. Recent proof of their involvement in the pathophysiology of chronic heart failure (CHF) and their use as an indirect measure for oxidative stress in a clinical setting is also emphasized.
BACKGROUND
AGEs are a heterogeneous group of compounds derived from non-enzymatic glycation of proteins, lipids and nuclear acids through complex and sequential reactions known as the Maillard reaction (1). Most of the research concerning this topic was done in the last two decades.
These versatile molecules play a major pathogenic role in many chronic diseases related to aging, diabetes, progression of diabetes complications and are of great interest to nephrologists (because of their nephrotoxic potential) and more recently to cardiologists (2,3).
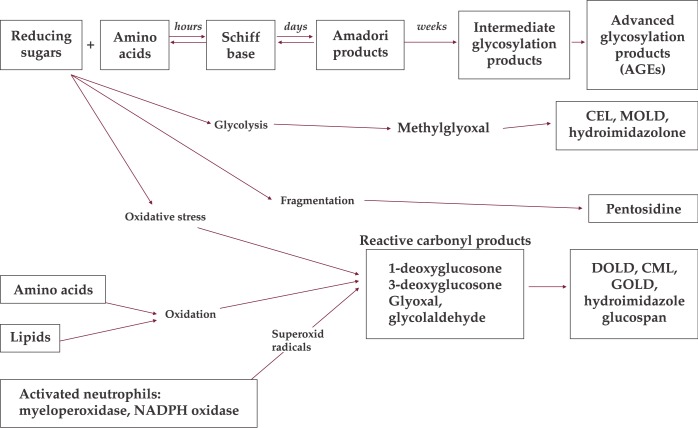
Glycation depends on glucose concentration in the initial stages of the Maillard reaction and this explains its enhancement in diabetes mellitus - due to the availability of high quantities of glucose (4). Baynes and colleagues noted the importance of oxidizing conditions and reactive oxygen species in the formation of glycoxidation products, an important class of AGEs that accumulate in tissues, of which the most studied are CML (carboxymethyl-Lysine) and pentosidine (5). Maillard products are also formed via lipid-derived intermediates, resulting in advanced lipoxidation products (ALEs) (6). Dyslipidemia is a common phenomenon in diabetes and AGEs and ALEs may be formed at the same time in the atherosclerotic plaques of diabetic patients. Lipids are also an important source of protein modifications (Figure 1).
Figure 1. Simplified representation of the complex Maillard reaction and formation of advanced glycation endproducts.
CEL = carboxyethyllysine; MOLD = methylglyoxal lysine dimer; DOLD = 3-deoxyglucosone lysine dimer; CML = carboxymethyllysine; GOLD = glyoxal lysine dimer
Decreased clearance of serum AGEs may further increase tissue AGEs accumulation. Age, the status of oxidative stress, inflammation, liver and kidney function, nutrition and diet also influence AGEs accumulation (7).
In spite of their enormous heterogeneity in terms of structure, all known AGEs lead to a common consequence and that is the crosslinking of proteins (through the formation of specific covalent and translational bonds), with the resultant alteration of protein structure and resistance to proteolysis, in the end leading to tissue remodelling (8).
AGEs can link to any type of proteins and form stable and irreversible bonds. Their bioavailability depends on the half-life time of those proteins. Skin collagen and lens have a very long half-life thus being the most likely sites for AGEs accumulation. Bonds to other types of proteins with shorter half-lives are unstable leading to AGEs degradation followed by renal excretion of AGEs-moieties (9). The accumulation of AGEs (via glycation, glycoxidation, lipoxidation or generation of carbonyl compounds) is known as carbonyl stress, a phenomenon that has been observed in both diabetes and uraemia and has also been proven to play a role in the accelerated atherosclerosis and vascular dysfunction (3,10) even independently of these conditions (11).
AGEs exert their effects via receptors, with a proven pathogenic significance, as they mediate cellular responses through the generation of oxygen-free radicals (12). Previous studies identified several distinct AGEs-specific receptors (RAGE) which include macrophage scavenger receptor and receptors type I and II (13). The relationship between AGEs and their receptors is of great importance as they play both positive and negative roles in the action and fate of AGEs. AGE-R1 (14) and lysozyme (15) receptors are the major degrading mechanism for AGE-modified tissues and cell components. The best characterized proinflammatory AGEs receptor, so far, is a member of the immunoglobulin superfamily, a multiligand receptor called RAGE; it appears to activate a stress response leading to inflammation and cellular dysfunction, promoting multiple signaling pathways that generate reactive oxygen species (ROS).
The AGE-RAGE interaction could also play a role at the sites of inflammation, as suggested by the evidence that phagocytes in such locations generate CML through myeloperoxidase (16). This pathway, which is independent of glycaemic control, might explain the presence of AGEs in atherosclerotic lesions as well as in patients with inflammatory conditions such as rheumatoid arthritis.
Trying to better understand AGEs involvement in vascular dysfunction, a "two hit" model emerged which involves an initial AGE-RAGE interaction, leading to cell activation and inflammation, followed by lipoprotein accumulation, with the maintenance of the inflammatory status and further acceleration of atherosclerosis (17). Still the complexities of this system are not yet fully understood.
Assessment of AGEs accumulation
Evaluation of AGEs and their accumulation has been difficult because their structure is complex and heterogeneous. Reproducibility of many assays, used so far, is rather poor. Importantly, the sites where chronic complications develop in diabetes and CKD are also those where long-lived proteins are present (e.g. glomerular basement membrane, crystalline lens). It seems therefore appropriate to prefer assays of tissue AGEs accumulation rather than plasma samples.
Meerwaldt et al. reported on a rapid, non-invasive measurement of skin autofluorescence (AF), used to assess AGEs accumulation, based on the fluorescent proprieties of some AGEs called Autoflorencence Reader (AFR) (18). The technique has been validated against measurements of AGEs in skin biopsies, obtained from the same skin spot, taken from healthy subjects, patients with diabetes mellitus as well as haemodialysis patients. Skin AF correlates with skin levels of CML, pentosine, carboxyethyllysine (CEL). It proved to have good reproductibility, to be time efficient and more practical in daily patient care (19).
Mechanisms of cellular damage induced by AGEs
Several mechanisms link AGEs accumulation to cellular dysfunction. AGEs formation leads to structural and functional alterations of intra- and extra-cellular proteins (7,20). This first effect was noticed in a large variety of pathological conditions. Cross-linking of collagen proteins contributes to the rigidity and loss of elasticity of tissues and increased resistance to proteolysis (21,22), inhibition of tissue remodeling and thickening of capillary basement membrane leading to widespread alterations such as glomerular sclerosis. Increased AGEs formation is related to diminished arterial elasticity in diabetics (23). AGEs formed on vascular matrix proteins mediate defective endothelium-dependent vasodilatation by quenching nitric oxide (24). Lipoprotein modifications, induced by AGEs, have an important contribution to the dyslipidaemia, frequently observed in diabetic patients (25). AGEs formed on the matrix components of the vascular wall can trap altered lipoproteins, leading to impaired cholesterol efflux and lipoprotein accumulation (26).
The second important effect of AGEs accumulation is the induction of oxidative stress. AGEs attachment to sites on various cells results in the generation of oxygen free radicals by depletion of cellular antioxidant defense mechanisms, such as vitamin C and glutathione (27, 28). In diabetes, persistent hyperglycaemia causes increased production of free radicals through autoxidation of glucose and non-enzymatic protein glycation and increased flux of glucose through the polyol pathway (29). Oxidation of plasma lipids may stimulate auto-oxidative reactions of sugars, enhancing damage to both lipids and proteins, reinforcing the cycle of oxidative stress. The effect of advanced glycosylation on lipid oxidation was first showed by Bucala et al. (30).
Consequences of AGEs accumulation in atherosclerosis and their clinical implication
A fundamental observation linking AGEs to atherosclerosis is their identification in the atherosclerotic plaques of patients with diabetes or renal disease (31,32) but also in non-diabetic patients with coronary artery disease (33). Vlassara and Bierhaus emphasized, in some of their studies, AGEs' role in accelerating atherosclerosis (34,35). Pathophysiological mechanisms, as described before, include cross-linking of the proteins leading to arterial stiffness; the interaction with AGEs receptors leads to focal adhesion molecules and cytokine expression and atheromatous plaque formation (36). All these actions are of great importance in the promotion of endothelial dysfunction.
Glycoxidation of LDL makes it less recognizable by the native LDL receptor, resulting in delayed clearance and increased LDL-C levels. This promotes LDL uptake by scavenger receptors on macrophages and smooth muscle cells, eventually leading to foam cells formation (37). AGEs may also modify HDL, altering its athero-protective effects (38) and stimulate pro-inflammatory and pro-thrombotic mediators through glycated LDL.
The finding that AGEs have a potential role in atherosclerosis is strengthened by the results of experimental animal studies. It has been shown that direct intravenous infusion of glycated albumin in euglycaemic rabbit's results in enhanced expression of adhesion molecules and thickening of the intima (36) and that local application of AGE – Bovine serum albumin (BSA) to the vessel wall resulted in enhancement of intimal hyperplasia of the carotid artery (39). All these observations are supported by interventional studies on animals proving that by diminishing the AGEs burden with the use of an AGEs inhibitor or cross-link breaker (e.g. aminoguanidine and Alagebrium) the atherosclerotic process can be attenuated (40,41).
Although most of experimental and interventional studies were performed on diabetic models, AGEs have been shown to be involved in atherosclerosis, beyond diabetes and renal disease. Due to the fact that AGE's can now be easily and non-invasively measured by using an AF Reader, in contrast to all other currently available biomarkers for oxidative stress, AGE might become suitable as an indirect measure for oxidative stress in a clinical setting.
Consequences of AGEs accumulation in cardiovascular disease (CVD) and their clinical implication
There are several reasons that point to a link between accumulation of AGEs and CHF, including the high prevalence of heart failure and diastolic dysfunction in those conditions associated with increased AGEs accumulation, such as diabetes and chronic kidney disease (CKD). The involvement of AGE's in diabetic cardiomiopathy has been shown in recent studies (11).
Two pathways involving AGEs may lead to heart failure. One is the interference with matrix proteins (matrix collagen, elastin, laminin) leading to alterations of structure (fibrosis induction) and function (hydrophobicity, charge, elasticity and turnover) (11,42). The second pathway is through AGE–RAGE interactions, leading to multiple vascular and myocardial alterations with negative impact on heart compliance (e.g. via calcium metabolism) (43,44). Accumulation of AGEs also leads, indirectly, to endothelial dysfunction, increased thrombogenicity and accelerated atherosclerosis and, as a result, to coronary perfusion abnormalities. Another potentially important link between AGEs and CHF is the contribution of renal hypoperfusion and function loss as a perpetuating factor in heart failure, through decreased clearance of circulating and renal AGEs.
Preliminary evidence for AGEs involvement in the development of cardiac dysfunction originates from two trials in heart failure patients - DIAMOND (45) and PEDESTAL (46), trials confirming an improvement in diastolic function and a significant reduction of the left ventricular mass following treatment with Alagebrium (ALT-711) an AGEs cross-link breaker.
Clinical data on circulating AGEs levels remain limited and have not provided yet convincing proofs. Latest studies have revealed that patients with type 2 diabetes and coronary heart disease have higher AGEs levels than patients with diabetes alone (47). It is known that plasma AGEs are related to severity and prognosis of CHF, but it is the tissue levels of AGEs that directly reflect the cross-linking of interstitial and intracellular proteins and the receptor interactions. Thus skin AF, as a marker of tissue AGEs, can better represent tissue function and the overall negative impact of AGEs accumulation (11). Additionally strong associations between tissue accumulation of AGEs and collagen specific fluorescence in skin, myocardium, aortic plaques, and also with carotid to femoral pulse wave velocity was described in diabetic patients (48).
Up to date studies highlighted AGEs involvement and the implication of their evaluation in patients with coronary heart disease, either in acute clinical circumstances or in every day practice. It has been recently demonstrated that skin AF is elevated in patients with coronary artery disease and is associated with serum levels of neopterin (a monocyte activation marker), and with the soluble isoform of the receptor for AGEs (49). Skin AF is a predictor of 5-year coronary heart disease and mortality in diabetes (12). Indeed, tissue AGEs measured with the AFR independently predict future CVD in patients with diabetes and renal failure (47,50). More recent studies focused on searching an association between AF and carotid intima-media thickness (IMT), independently of traditional vascular risk factors and diabetes. Results showed that skin AF provided additional information for identifying subjects with the highest IMT, beyond risk stratification based on commonly used risk scores alone. IMT is positively related to skin AF, independently of clinical factors, (apo)lipoproteins and metabolic syndrome, suggesting that skin AF reflects subclinical atherosclerosis. Increased skin AF may be a marker for early abnormalities involved in atherosclerosis development (51). In patients with acute ST-elevation myocardial infarction (STEMI), skin AF is significantly higher compared with patients with stable coronary artery disease, independent of diabetes and smoking. Recently published results show that elevated skin AF observed in STEMI patients is associated with inflammation and glycaemic stress, and predicts future major adverse cardiac events (52).
Additionally, skin AF was associated with inflammatory markers, including C reactive protein (CRP) (53) and leukocyte count, suggesting a possible role in the process of plaque rupture. This is further supported by previous reports from the same authors, showing that skin AF is strongly related to skin accumulation of primary oxidative stress derived AGEs (54) and inversely correlated with plasma vitamin C levels, in subjects with renal failure (55).
These results highlight that skin AF is a measure of (long-term) metabolic burden and is strongly associated with the presence of CHF and cardiac mortality, superior to other measures of metabolic stress (e.g. HbA1C) (56). To better highlight this a table with the most relevant studies is presented below (Table 1). Skin AF and AGEs/ALEs accumulation may underline the effect of a common pathway and was more strongly associated with CHF and mortality compared with traditional risk factors, including smoking, already proven to be a marker of exogenous AGEs accumulation (57).
Table 1.
Most relevant studies on the role of AGEs and skin-AF in cardiovascular disease
| Study | Population investigated | Measurements | End-point | Results |
|---|---|---|---|---|
| Little et al. (45) DIAMOND study | 23 Patients with DHF | Interventional ALT-711 | LVM DF | ALT-711 improved DF (echo); decreased LVM |
| Thohan et al. (46) PEDESTAL study | 22 Patients with SHF and DHF | Interventional ALT-711 | LVM DF | ALT-711 improved DF (echo); decreased LV mass (echo) Trend to improved SF |
| Meerwaldt et al. (47) | 16 patients with DM type 1 and type 2 | Skin-AF | CVD mortality | Skin-AF is associated with CV mortality |
| Meerwaldt et al. (50) | 109 HD patients | Skin-AF | Overall CV mortality | Skin-AF is a strong predictor of mortality in ESRD patients |
| Mulder et al (52) | 169 patients with STEMI and stable CHD | Skin-AF | 1 year incidence of all cause mortality | Skin-AF is higher in STEMI and is predictive of future cardiovascular events |
| Gerrits et al. (57) | 973 type 2 DM patients | Skin-AF | Development of DM complications | Skin-AF is an independent predictor for the development of microvascular complications |
| Mulder et al. (49) | 63 patients with stable CHD | Skin-AF | Skin-AF is higher in patients with CHD and is associated with sRAGE and neopterin levels |
DHF = dyastolic heart function; ALT-711 = Alagebrium; LVM = left ventricular mass; DF = diastolic function; SHF = systolic heaert function; SF = systolic function; DM = diabetes mellitus; Skin-AF = skin autofluorescence; CVD = cardiovascular disease; CV = cardio-vascular; HD= heart disease; ESRD = end stage renal disease; STEMI = ST-elevation myocardial infarction; CHD = coronary heart disease; sRAGE = serum AGE specific receptors.
Consequences of AGEs accumulation in diabetes and in the development of nephropathy and their clinical implication
Patients with diabetes have significantly higher AGEs levels than the normal population, as a result of glycaemic stress. AGEs have a well established role in the pathogenesis of diabetic macro as well as microvascular complications. The relationship between hyperglycaemia and AGEs is confirmed by the tissue content of AGEs and the serum level of haemoglobin A1c (HbA1c) and fructosamine - biomarkers of time-integrated glucose concentration (58,59). Serum AGEs levels are higher in both type 1 and type 2 DM, are already increased early in the disease by approximately 1.5 fold, and are associated with the severity of retinopathy and nephropathy and also with coronary heart disease in type 2 diabetes mellitus patients (60).
Skin AF seems to be related to microvascular complications in diabetes (60) as well. Multiple regression analysis showed significant correlation of skin AF with age, sex, diabetes duration, body mass index (BMI), smoking, HbA1c, plasma creatinine, HDL cholesterol, and albumin-to-creatinine ratio (62). Recent studies focused on the relationship between skin AF and the outcome of type 2 diabetes patients. Lutgers et al. were the first showing evidence that skin AF is an independent predictor of the development of microvascular complications in a well-controlled type 2 diabetes population (57). Increased AF values were associated with the presence of microalbuminuria even after correction for age, A1C, triglycerides, and LDL. Thus, skin AF is superior to many other commonly used risk predictors - like diabetes duration and HbA1c in type 2 diabetes.
Multiple studies have shown that AGEs are important factors in the pathogenesis of nephropathy. CML, pyrraline and pentosidine have all been found in increased quantities in kidneys of patients with diabetes mellitus with or without CKD (63). AGEs accumulation is related to the severity of diabetic nephropathy - this was first described by Monnier at al. (64). Beisswenger et al. have shown that AGEs accumulation precedes and correlates with early manifestations of renal disease (56).
In both type 1 and type 2 diabetic populations, studies showed correlations with creatinine levels. The highest AF values were observed in diabetic patients on haemodialysis treatment. In this group of patients, AF values correlated with age, markers of metabolic burden like A1C, triglycerides, LDL and dialysis vintage.
Consequences of AGEs accumulation in ESRD and their clinical implication
Since AGEs levels are increased in plasma and collagen of normoglycaemic uremic patients, this abnormality cannot be credited as a result of only the increased glycation of proteins. Four sources are incriminated for AGEs accumulation in ESRD patients without diabetes:
-
1.
Oxidative stress, having as contributors: age, inflammation, infections, bio-incompatibility of the dialysis membrane (65) or reduced antioxidant activity. ESRD is a condition of increased (intracellular) oxidative stress, indicated by increased lipid peroxidation and a decrease in the ratio of oxidized glutathione to reduced glutathione (66) even before the start of renal replacement therapy (67). Patients with CKD, and in particular those on renal replacement therapy, are subject to a tremendous degree of metabolic stress (68).
-
2.
Carbonyl stress derived from the oxidation of sugars and lipids or reduced detoxification of carbonyl compounds such as glyoxalase 1 or aldose reductase.
-
3.
Reduced kidney excretion of AGEs precursors, due to a decrease in glomerular filtration, leading to AGEs accumulation and decreased tubular catabolism. This occurs yet before actual nephron loss, as it is demonstrated by kidney tubular accumulation of AGEs in experimental proteinuria, despite relatively well-preserved kidney function (69).
-
4.
Metabolic burden, due to reduced lipid clearance and/or insulin resistance; this stimulates de novo AGEs formation (70).
Incresed AGEs levels have been attributed to both impaired renal clearance and increased endogenous AGEs formation, but recent data, show that diet, as well, has an important role in AGEs accumulation, acting as a source of AGEs. Dietary AGEs are believed to sustain circulating levels and toxicity in proinflammatory and pro-oxidative conditions of CKD and dyalisis patients (71). Dietary AGEs content is an important contributor to excess serum AGEs levels in patients with renal failure, independently of other diet constituents, as some studies have shown. Interventional studies illustrate indicates that a reduction in dietary AGEs content can be obtained safely without compromising the content of obligatory nutrients as no correlation between serum AGEs levels and dietary protein, fat, and carbohydrate intake was observed (72). Other studies investigated the role of dietary AGEs in inflammation and potentially CVD in CKD, highlighted that restriction of AGEs in the diet reduces kidney lesions in aging and some of them even proposed dietary modifications as part of the multifactorial approach needed to improve CKD patients' life quality (73).
The mechanisms by which AGEs may induce tissue damage and long-term complications are those involved in the development of accelerated atherosclerosis and CHF in patients without renal failure.
Cardiovascular mortality is grossly elevated in patients with CKD, and is associated with a wide variety of structural and functional abnormalities. Mortality rates in haemodialysis patients are also markedly increased, despite current measures to improve survival (74), thus, assessment of AGEs accumulation in patients with CKD and in those undergoing renal replacement therapies has become of great importance. Several edifying studies have been recently published. Skin AF levels are strong predictors of survival in haemodialysis patients independent of other established risk factors. Multivariate analysis of the results of recent studies showed that skin AF is a stronger predictor of mortality than traditional risk factors, such as smoking and lipid profile. Skin AF was an independent and strong predictor of 3-year overall and cardiovascular mortality (49). In contrast to the data we have on tissue AGEs, the relationship between serum AGEs and mortality, in haemodialysis patients, is not that obvious, mostly because serum AGEs measurement needs different, and more complex methods (70), and their levels fluctuate considerably, under the influence of dialysis timing, and exogenous sources such as absorption from food, and smoking (75,76). A more recent study found that skin AF and not serum levels of specific AGEs, predicts composite cardiovascular outcome (combination of cardiovascular death and events) in haemodialysis patients (11).
High serum AGEs levels might even reflect better nutritional support, associated with improved survival (76). Patients with low serum AGEs levels were found to have high CRP and low serum albumin levels (known predictors of mortality in haemodialysis patients).
In peritoneal dialysis patients, on the other hand, the causes of peritoneal membrane dysfunction, over time, are still vague; however, the main trigger is thought to be the unphysiological exposure of the peritoneal membrane to glucose-containing dialysis fluids. The peritoneal membrane dysfunction is characterized by vascular proliferation and extra-cellular structural changes (77). AGEs-RAGE interaction in human peritoneal mesothelium cells results in overexpression of vascular and intercellular cell adhesion molecules which may promote local inflammation and injury (78).
Although AGEs accumulation has been found to be an independent and strong predictor of total and cardiovascular mortality in dialysis patients, larger studies on dialysis patients are still needed to evaluate to what extent they contribute to the development of ESRD cardiovascular morbidity and other complications. In ESRD patients, not only cardiovascular complications are important to prognosis but also a series of connective tissue complications such as destructive spondyl-arthropathy, carpal tunnel syndrome, and lytic bone cysts. Accumulation of amyloid deposits has been linked to ESRD-related connective tissue disease, and beta2-microglobulin is a major component in amyloid deposits (79,80). Serum AGEs levels increase in dialysis patients with connective tissue disorders. Interestingly, increased AGEs levels have also been found on collagen samples from carpal tunnel connective tissue in the absence of amyloid deposits (81).
It is possible that AGEs may represent an important component of uremic toxicity contributing to accelerated atherosclerosis and connective tissue disease in patients with ESRD. Assessment of AGEs accumulation may help tailor and monitor treatment and identify patients at risk of long-term complications. ❑
CONCLUSIONS
AGEs may have a vital role in the normal aging process and in the evolution of the complications of diabetes and CKD. They have been implicated in the pathogenesis of long term complications in diabetes. AGEs accumulation is increased in patients with ESRD and may, through several biochemical reactions, add to the development of ESRD complications.
Skin AGEs accumulation can now be rapidly noninvasively assessed using an AFR which proved to be a strong and independent determinant of total and cardiovascular morbidity and mortality, both in patients on dialysis and in diabetic patients. Assessment of AGEs accumulation may facilitate treatment management and further identify patients at risk of long-term complications.
More and more, measuring skin AF provides an easily applicable and reproducible tool to investigate the pathogenic effects of AGEs in larger populations. Due to the fact that AGEs can now be easily measured using the AFR, in contrast to all other currently available biomarkers for oxidative stress, they might become suitable as an indirect measure for oxidative stress in a clinical setting. ❑
COMMENTS
Abbreviations:
ESRD = end-stage renal disease
CHF = congestive heart failure
CML = carboxymethyl-Lysine
ALEs = advanced lipoxidation products
RAGE = AGE specific receptors
ROS = reactive oxygen species
AFR = Autofluorescence Reader
AF = autofluorescence
CEL = carboxyethyllysine
BSA = bovine serum albumin
CKD = chronic kidney disease
ALT-711 = Alagebrium
CVD = cardiovascular disease
IMT = carotid intima-media thickness
STEMI = ST-elevation myocardial infarction
HbA1c = haemoglobin A1c
CRP = C-reactive protein
LVM = left ventricular mass
DHF = diastolic heart failure
DM = diabetes mellitus
HD = haemodialysis
CHD = coronary heart disease
References
- 1.John WG, Lamb EJ. The maillard or browning reaction in diabetes. Eye. 1993;7:230–237. doi: 10.1038/eye.1993.55. [DOI] [PubMed] [Google Scholar]
- 2.Singh R, Barden A, Mori T, et al. Advanced glycation end-products: a review. Diabetologia. 2001;44:129–146. doi: 10.1007/s001250051591. [DOI] [PubMed] [Google Scholar]
- 3.Raj DS, Choudhury D, Welbourne TC, et al. AGE: a nephrologist`s perspective. Am J Kidney Dis. 2000;35:365–380. doi: 10.1016/s0272-6386(00)70189-2. [DOI] [PubMed] [Google Scholar]
- 4.Furth A. Glycated proteins in diabetes. Br J Bio-medSci. 1997;54:192–200. [PubMed] [Google Scholar]
- 5.Miyata T, Maeda K, Kurokawa K, et al. Oxidation conspires with glycation to generate noxious advanced glycation end-products in renal failure. Nephrol Dial Transplant. 1997;12:255–258. doi: 10.1093/ndt/12.2.255. [DOI] [PubMed] [Google Scholar]
- 6.Smith MA, Taneda S, Richey PL, et al. Advanced Maillard reaction end products are associated with Alzheimer disease pathology. Proc Natl Acad Sci USA. 1994;91:5710–5714. doi: 10.1073/pnas.91.12.5710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fu MX, Wells-Knecht KJ, Blackledge JA, et al. Glycation, glycoxidation, and crosslinking of collagen by glucose. Kinetics, mechanisms, and inhibition of late stages of the Maillard reaction. Diabetes. 1994;43:676–683. doi: 10.2337/diab.43.5.676. [DOI] [PubMed] [Google Scholar]
- 8.Ienaga K, Nakamura K, Hochi T, et al. Crosslines, fluorophores in the AGE-related cross-linked proteins. Contrib Nephrol. 1995;112:42–51. doi: 10.1159/000424091. [DOI] [PubMed] [Google Scholar]
- 9.Miyata T, Ueda Y, Yamada Y, et al. Accumulation of carbonyls accelerates the formation of pentosidine, an advanced glycation end product: carbonyl stress in uremia. J Am Soc Nephrol. 1998;9:2349–2356. doi: 10.1681/ASN.V9122349. [DOI] [PubMed] [Google Scholar]
- 10.Miyata T, van Ypersele de Strihou C, Kurawaka K, et al. Alteration in non enzymatic biochemistry in uraemia: origin and significance of "carbonyl stress" in long term uraemic complications. Kidney Int. 1999;55:389–399. doi: 10.1046/j.1523-1755.1999.00302.x. [DOI] [PubMed] [Google Scholar]
- 11.Hartog JWL, Voors AA, Bakker SJL, et al. Advanced Glycation end-products (AGEs) and heart failure: pathophysiology and clinical implications. Eur J Heart Fail. 2007;9:1146–1155. doi: 10.1016/j.ejheart.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 12.Brownlee M. Biochemistry and molecular cell biology of diabetic complications. Nature. 2001;414:813–820. doi: 10.1038/414813a. [DOI] [PubMed] [Google Scholar]
- 13.Brett J, Schmidt AM, Yan SD, et al. Survey of the distribution of a newly characterized receptor for advanced glycation end products in tissues. Am J Pathol. 1993;143:1699–1712. [PMC free article] [PubMed] [Google Scholar]
- 14.He CJ, Koschinsky T, Buenting C, et al. Presence of diabetic complications in type 1 diabetic patients correlates with low expression of mononuclear cell AGE-receptor-1 and elevated serum AGE. Mol Med. 2001;7:159–168. [PMC free article] [PubMed] [Google Scholar]
- 15.Zheng F, Cai W, Mitsuhashi T, et al. Lysozyme enhances renal excretion of advanced glycation endproducts in vivo and suppresses adverse age-mediated cellular effects in vitro: a potential AGE sequestration therapy for diabetic nephropathy? Mol Med. 2001;7:737–747. [PMC free article] [PubMed] [Google Scholar]
- 16.Yoshihara K, Nakamura K, Kanai M, et al. Determination of urinary and serum penosidine and its application to older patients. Biol Pharm Bull. 1998;21:1005–1008. doi: 10.1248/bpb.21.1005. [DOI] [PubMed] [Google Scholar]
- 17.Schmidt AM, Yan SD, Wautier J-L, et al. Activation of receptor for advanced glycation end-products: a mechanism for chronic vascular dysfunction in diabetic vasculopathy and atherosclerosis. Circ Res. 1999;84:489–497. doi: 10.1161/01.res.84.5.489. [DOI] [PubMed] [Google Scholar]
- 18.Meerwaldt R, Smit AJ, Navis GJ, et al. Increased skinautofluorescence in diabetes mellitus and renal failure. Diabetologia. 2000;44(supplA):1046–1046. [Google Scholar]
- 19.Meerwaldt R, Links T, Graaff R, et al. Simple noninvasive measurement of skin autofluorescence. Ann NY Acad Sci. 2005;1043:290–29. doi: 10.1196/annals.1333.036. [DOI] [PubMed] [Google Scholar]
- 20.Aronson D. Cross-linking of glycated collagen in the pathogenesis of arterial and myocardial stiffening of aging and diabetes. . J Hypertens. 2003;21:3–12. doi: 10.1097/00004872-200301000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Dyer DG, Dunn JA, Thorpe SR, et al. Accumulation of Maillard reaction products in skin collagen in diabetes and aging. J Clin Invest. 1993;91:2463–2469. doi: 10.1172/JCI116481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kent MJ, Light ND, Bailey AJ. Evidence for glucose-mediated covalent cross-linking of collagen after glycosylation in vitro. Biochem J. 1985;225:745–752. doi: 10.1042/bj2250745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Airaksinen KE, Salmela PI, Linnaluoto MK, et al. Diminished arterial elasticity in diabetes: association with fluorescent advanced glycosylation end products in collagen. Cardiovasc Res. 1993;27:942–945. doi: 10.1093/cvr/27.6.942. [DOI] [PubMed] [Google Scholar]
- 24.Bucala R, Tracey KJ, Cerami A. Advanced glycosylation products quench nitric oxide and mediate defective endothelium-dependent vasodilatation in experimental diabetes. J Clin Invest. 1991;87:432–438. doi: 10.1172/JCI115014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bucala R, Makita Z, Vega G, et al. Modification of low density lipoprotein by advanced glycation end products contributes to the dyslipidemia of diabetes and renal insufficiency. Proc Natl Acad Sci USA. 1994;91:9441–9445. doi: 10.1073/pnas.91.20.9441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ohgami N, Nagai R, Miyazaki A, et al. Scavenger receptor class B type I-mediated reverse cholesterol transport is inhibited by advanced glycation end products. J Biol Chem. 2001;276:13348–13355. doi: 10.1074/jbc.M011613200. [DOI] [PubMed] [Google Scholar]
- 27.Schmidt AM, Hori O, Brett J, et al. Cellular receptors for advanced glycation end products. Implications for induction of oxidant stress and cellular dysfunction in the pathogenesis of vascular lesions. Arterioscler Thromb. 1994;14:1521–1528. doi: 10.1161/01.atv.14.10.1521. [DOI] [PubMed] [Google Scholar]
- 28.Bierhaus A, Illmer T, Kasper M, et al. Advanced glycation end product (AGE)- mediated induction of tissue factor in cultured endothelial cells is dependent on RAGE. Circulation. 1997;96:2262–2271. doi: 10.1161/01.cir.96.7.2262. [DOI] [PubMed] [Google Scholar]
- 29.Giugliano D, Ceriello A, Paolisso G. Oxidative stress and diabetic vascular complications. Diabetes Care. 1996;19:257–267. doi: 10.2337/diacare.19.3.257. [DOI] [PubMed] [Google Scholar]
- 30.Bucala R, Makita Z, Koschinsky T, et al. Lipid advanced glycosylation: pathway for lipid oxidation in vivo. Proc Natl Acad Sci USA. 1993;90:6434–6438. doi: 10.1073/pnas.90.14.6434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nishino T. Immunohistochemical detection of advanced glycosylation end products within the vascular lesions and glomeruli in diabetic nephropathy. Human Pathology. 1995;26(3):308–313. doi: 10.1016/0046-8177(95)90063-2. [DOI] [PubMed] [Google Scholar]
- 32.Sakata N, Imanaga Y, Meng J, et al. Increased advanced glycation end products in atherosclerotic lesions of patients with end-stage renal disease. Atherosclerosis. 1999;142:67–77. doi: 10.1016/s0021-9150(98)00192-0. [DOI] [PubMed] [Google Scholar]
- 33.Stitt AW. Elevated AGE-modified ApoB in sera of euglycemic, normolipidemic patients with atherosclerosis: relationship to tissue AGEs. Mol Med. 1997;3:617–627. [PMC free article] [PubMed] [Google Scholar]
- 34.Vlassara H. Advanced glycation end-products and atherosclerosis. Ann Med. 1996;28:419–426. doi: 10.3109/07853899608999102. [DOI] [PubMed] [Google Scholar]
- 35.Bierhaus A, Hofmann MA, Ziegler R, et al. AGEs and their interaction with AGE-receptors in vascular disease and diabetes mellitus. I. The AGE concept. Cardiovasc Res. 1998;37:586–600. doi: 10.1016/s0008-6363(97)00233-2. [DOI] [PubMed] [Google Scholar]
- 36.Vlassara H, Fuh H, Donnelly T, et al. Advanced glycation endproducts promote adhesion molecule (VCAM-1, ICAM-1) expression and atheroma formation in normal rabbits. Mol Med. 1995;1:447–456. [PMC free article] [PubMed] [Google Scholar]
- 37.Bucala R, Mitchell R, Arnold K, et al. Identification of the major site of apolipoprotein B modification by advanced glycosylation end products blocking uptake by the low density lipoprotein receptor. J Biol Chem. 1995;270:10828–10832. doi: 10.1074/jbc.270.18.10828. [DOI] [PubMed] [Google Scholar]
- 38.Ferretti G, Bacchetti T, Negre-Salvayre A, et al. Structural modifications of HDL and functional consequences. Atherosclerosis. 2006;184:1–7. doi: 10.1016/j.atherosclerosis.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 39.Crauwels HM, Herman AG, Bult H. Local application of advanced glycation end products and intimal hyperplasia in the rabbit collared carotid artery. Cardiovasc Res. 2000;47:173–182. doi: 10.1016/s0008-6363(00)00090-0. [DOI] [PubMed] [Google Scholar]
- 40.Forbes J, Yee L, Thallas V, et al. Advanced glycation end product interventions reduce diabetes accelerated atherosclerosis. Diabetes. 2004;53:1813–1823. doi: 10.2337/diabetes.53.7.1813. [DOI] [PubMed] [Google Scholar]
- 41.Wolffenbuttel BH. Breakers of advanced glycation end products restore large artery properties in experimental diabetes. Proc NatlAcadSci USA. 1998;95:4630–4634. doi: 10.1073/pnas.95.8.4630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Smit AJ, Lutgers HL. The clinical relevance of advanced glycation endproducts and recent developments in pharmaceutics to reduce AGE accumulation. Curr Med Chem. 2004;11:2767–2784. doi: 10.2174/0929867043364342. [DOI] [PubMed] [Google Scholar]
- 43.Striler LJ, Striker GE. Administration of AGEs in vivo induces extracellular matrix gene expression. Nephrol. Dial. Transpl. 1996;11:S62–S65. doi: 10.1093/ndt/11.supp5.62. [DOI] [PubMed] [Google Scholar]
- 44.Petrova R, Yamamoto Y, Muraki K, et al. Advanced glycation endproductinduced calcium handling impairment in mouse cardiacmyocytes. J. Mol. Cell Card. 2002;34:1425–1431. doi: 10.1006/jmcc.2002.2084. [DOI] [PubMed] [Google Scholar]
- 45.Little WC, Zile MR, Kitzman DW, et al. The effect of alagebrium chloride (ALT-711), a novel glucose cross-link breaker, in the treatment of elderly patients with diastolic heart failure. . J Card Fail. 2005;11:191–195. doi: 10.1016/j.cardfail.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 46.Thohan V, Koerner MM, Pratt CM, et al. Improvements in diastolic function among patients with advanced systolic heart failure utilizing alagebrium (an oral advanced glycation endproduct cross-link breaker). . Circulation. 2005;112(Suppl2):2647–2647. [Google Scholar]
- 47.Meerwaldt R, Lutgers HL, Links TP, et al. Skin autofluorescence is a strong predictor of cardiac mortality in diabetes. . Diabetes Care. 2007;30:107–112. doi: 10.2337/dc06-1391. [DOI] [PubMed] [Google Scholar]
- 48.Lutgers HL, Graaff R, Links TP, et al. Skin autofluorescence as a noninvasive marker of vascular damage in patients with type 2 diabetes. . Diabetes Care. 2006;29:2654–9. doi: 10.2337/dc05-2173. [DOI] [PubMed] [Google Scholar]
- 49.Mulder DJ, van Haelst PL, Gross S, et al. Skin autofluorescence is elevated in patients with stable coronary artery disease and is associated with serum levels of neopterin and the soluble re ce ptor for advanced glycation end pro ducts. Atherosclerosis. 2008;197:217–23. doi: 10.1016/j.atherosclerosis.2007.03.027. [DOI] [PubMed] [Google Scholar]
- 50.Meerwaldt R, Hartog JW, Graaff R, et al. Skin autofluorescence, a measure of cumulative metabolic stress and advanced glycation end products, predicts mortality in hemodialysis patients. . J Am Soc Nephrol. 2005;16:3687–3693. doi: 10.1681/ASN.2005020144. [DOI] [PubMed] [Google Scholar]
- 51.Lutgers HL, Graaff R, De Vries R, et al. Carotid artery intima media thickness associates with skin autofluoresence in non-diabetic subjects without clinically manifest cardiovascular disease. . Eur J Clin Invest. 2010;40:812–817. doi: 10.1111/j.1365-2362.2010.02329.x. [DOI] [PubMed] [Google Scholar]
- 52.Mulder DJ, van Haelst PL, Graaff R, et al. Skin autofluorescence is elevated in acute myocardial infarction and is associated with the one-year incidence of major adverse cardiac events. . Neth Heart J. 2009;17:162–168. doi: 10.1007/BF03086239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ridker PM, Cannon CP, Morrow D, et al. C-reactive protein levels and outcomes after statin therapy. . N Engl J Med. 2005;352:20–28. doi: 10.1056/NEJMoa042378. [DOI] [PubMed] [Google Scholar]
- 54.Meerwaldt R, Oomen PHN, Links TP, et al. Simple non-invasive assessment of advanced glycation endproduct accumulation. . Diabetologia. 2004;47:1324–1330. doi: 10.1007/s00125-004-1451-2. [DOI] [PubMed] [Google Scholar]
- 55.Hartog JW, de Vries AP, Bakker SJ, et al. Risk factors for chronic transplant dysfunction and cardiovascular disease are related to accumulation of advanced glycationend-products in renal transplant recipients. Nephrol Dial Transplant. 2006 doi: 10.1093/ndt/gfl132. [DOI] [PubMed] [Google Scholar]
- 56.Beisswenger PJ, Makita Z, Curphey TJ, et al. Formation of immunochemical advanced glycosylationend products precedes and correlates with earlymanifestations of renal and retinal disease in diabetes. . Diabetes. 1995;44:824–829. doi: 10.2337/diab.44.7.824. [DOI] [PubMed] [Google Scholar]
- 57.Gerrits EG, Lutgers HL, Kleefstra N, et al. Skin autofluorescence: a tool to identify type 2 diabetic patients at risk for developing microvascular complications. Diabetes Care. 2008;31:517–21. doi: 10.2337/dc07-1755. [DOI] [PubMed] [Google Scholar]
- 58.Friedman EA. Avanced glycosylated end-products and hyperglycaemia in the pathogenesis of diabetic complications. Diabetes Care. 1999;22:B65–B71. [PubMed] [Google Scholar]
- 59.Dyer DG, Dunn JA, Thorpe SR, et al. Accumulation of Maillard reaction products in skin collagen in diabetes and aging. . J Clin Invest. 1993;91:2463–2469. doi: 10.1172/JCI116481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Aso Y, Inukai T, Tayama K, et al. Serum concentrations of advanced glycation endproducts are associated with the development of atherosclerosis as well as diabetic microangiopathy in patients with type 2 diabetes. Acta Diabetol. 2000;37:87–92. doi: 10.1007/s005920070025. [DOI] [PubMed] [Google Scholar]
- 61.Genuth S, Sun W, Cleary P, et al. Glycationand carboxymethyllysine levels in skin collagen predictthe risk of future 10-year progression of diabeticretinopathy and nephropathy in the diabetes control and complications trial and epidemiology of diabetes interventions and complications participants with type 1 diabetes. Diabetes. 2005;54:3103–3111. doi: 10.2337/diabetes.54.11.3103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Schleicher ED, Wagner E, Nerlich AG. Increased accumulation of the glycoxidation product N(epsilon)- (carboxymethyl)lysine in human tissues in diabetes and aging. J Clin Invest. 1997;99:457–468. doi: 10.1172/JCI119180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wagner Z, Wittmann I, Mazak I, et al. N(epsilon)-(carboxymethyl)lysine levels in patients with type 2 diabetes: role of renal function. . Am J Kidney Dis. 2001;38:785–791. doi: 10.1053/ajkd.2001.27695. [DOI] [PubMed] [Google Scholar]
- 64.Sell DR, Lapolla A, Odetti P, et al. Pentosidine formation in skin correlates with severity of complications in individuals with long-standing IDDM. . Diabetes. 1992;41:1286–1292. doi: 10.2337/diab.41.10.1286. [DOI] [PubMed] [Google Scholar]
- 65.Kosch M, Levers A, Fobker M, et al. Dialysis filter type determines the acute effect of haemodialysis on endothelial function and oxidative stress. . Nephrol Dial Transplant. 2003;18:1370–1375. doi: 10.1093/ndt/gfg169. [DOI] [PubMed] [Google Scholar]
- 66.Vaziri ND. Oxidative stress in uremia: Nature, mechanisms, and potential consequences. . Semin Nephrol. 2004;24:469–473. doi: 10.1016/j.semnephrol.2004.06.026. [DOI] [PubMed] [Google Scholar]
- 67.Diepeveen SH, Verhoeven GH, van der PJ, et al. Oxidative stress in patients with end-stage renal disease prior to the start of renal replacement therapy. . Nephron Clin Pract. 2004;98:c3–c7. doi: 10.1159/000079921. [DOI] [PubMed] [Google Scholar]
- 68.Locatelli F, Canaud B, Eckardt KU, et al. Oxidative stress in endstage renal disease: an emerging threat to patient outcome. . Nephrol Dial Transplant. 2003;18:1272–1280. doi: 10.1093/ndt/gfg074. [DOI] [PubMed] [Google Scholar]
- 69.Waanders F, Greven WL, Baynes JW, et al. Renal accumulation of pentosidine in non-diabetic proteinuria induced renal damage in rats. . Nephrol Dial Transplant. 2005;20:2060–2070. doi: 10.1093/ndt/gfh939. [DOI] [PubMed] [Google Scholar]
- 70.Meerwaldt R, Zeebregts C, Navis G, et al. Accumulation of Advanced Glycation End Products and Chronic Complications in ESRD Treated by Dialysis . Am J Kidney Dis. 2008;53:138–150. doi: 10.1053/j.ajkd.2008.08.031. [DOI] [PubMed] [Google Scholar]
- 71.Vlassara H, Uribarri J, Ferrucci L, et al. Identifying Advanced Glycation End Products as a Major Source of Oxidants in Aging: Implications for the Management and/or Prevention of Reduced Renal Function in Elderly Persons. Seminars in Nephrology. 2009;29:594–602. doi: 10.1016/j.semnephrol.2009.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Uribarri J, Peppa M, Cai W, et al. Dietary glycotoxins correlate with circulating advanced glycation end product levels in renal failure patients. . AJKD. 2003;42:532–538. doi: 10.1016/s0272-6386(03)00779-0. [DOI] [PubMed] [Google Scholar]
- 73.Neade T, Uribarri J. Diet, Inflammation, and Chronic Kidney Disease: Getting to the Heart of the Matter. . Seminars in Dialysis. 2008;21:331–337. doi: 10.1111/j.1525-139X.2008.00445.x. [DOI] [PubMed] [Google Scholar]
- 74.Foley RN, Parfrey PS, Sarnak MJ. Epidemiology of cardiovascular disease in chronic renal disease. . J Am Soc Nephrol. 1998;9(suppl12):S16–S23. [PubMed] [Google Scholar]
- 75.He C, Sabol J, Mitsuhashi T, et al. Dietary glycotoxins: Inhibition of reactive products by aminoguanidine facilitates renal clearance and reduces tissue sequestration. Diabetes. 1999;48:1308–1315. doi: 10.2337/diabetes.48.6.1308. [DOI] [PubMed] [Google Scholar]
- 76.Schwedler SB, Metzger T, Schinzel R, et al. Advanced glycation end products and mortality in hemodialysis patients. Kidney Int. 2002;62:301–310. doi: 10.1046/j.1523-1755.2002.00423.x. [DOI] [PubMed] [Google Scholar]
- 77.Combet S, Ferrier ML, Van Landschoot M, et al. Chronic uremia induces permeability changes, increased nitric oxide synthase expression, and structural modifications in the peritoneum. J Am Soc Nephrol. 2001;12:2146–2157. doi: 10.1681/ASN.V12102146. [DOI] [PubMed] [Google Scholar]
- 78.De Vries AS, Flyvbjerg A, Mortier S, et al. Inhibition of the interaction of AGE-RAGE prevents hyperglycemiainduced fibrosis of the peritoneal membrane. J Am Soc Nephrol. 2003;14:2109–2118. doi: 10.1681/ASN.V1482109. [DOI] [PubMed] [Google Scholar]
- 79.Gejyo F, Odani S, Yamada T, et al. Beta 2-microglobulin: A new form of amyloid protein associated with chronic hemodialysis. Kidney Int. 1986;30:385–390. doi: 10.1038/ki.1986.196. [DOI] [PubMed] [Google Scholar]
- 80.Gejyo F, Narita I. Current clinical and pathogenetic understanding of beta2-m amyloidosis in long-term haemodialysis patients. Nephrology. 2003;8:S45–S49. doi: 10.1046/j.1440-1797.8.s.10.x. [DOI] [PubMed] [Google Scholar]
- 81.Brancaccio D, Gallieni M, Niwa T, et al. Ultrastructural localization of advanced glycation end products and beta2-microglobulin in dialysis amyloidosis. J Nephrol. 2000;13:129–136. [PubMed] [Google Scholar]