Abstract
Comprehensiveness relates both to scope of services offered and to a whole-person clinical approach. Comprehensive services are defined as “the provision, either directly or indirectly, of a full range of services to meet most patients' healthcare needs”; whole-person care is “the extent to which a provider elicits and considers the physical, emotional and social aspects of a patient's health and considers the community context in their care.” Among instruments that evaluate primary healthcare, two had subscales that mapped to comprehensive services and to the community component of whole-person care: the Primary Care Assessment Tool – Short Form (PCAT-S) and the Components of Primary Care Index (CPCI, a limited measure of whole-person care).
Objective:
To examine how well comprehensiveness is captured in validated instruments that evaluate primary healthcare from the patient's perspective.
Method:
645 adults with at least one healthcare contact in the previous 12 months responded to six instruments that evaluate primary healthcare. Scores were normalized for descriptive comparison. Exploratory and confirmatory (structural equation modelling) factor analysis examined fit to operational definition, and item response theory analysis examined item performance on common constructs.
Results:
Over one-quarter of respondents had missing responses on services offered or doctor's knowledge of the community. The subscales did not load on a single factor; comprehensive services and community orientation were examined separately. The community orientation subscales did not perform satisfactorily. The three comprehensive services subscales fit very modestly onto two factors: (1) most healthcare needs (from one provider) (CPCI Comprehensive Care, PCAT-S First-Contact Utilization) and (2) range of services (PCAT-S Comprehensive Services Available). Individual item performance revealed several problems.
Conclusion:
Measurement of comprehensiveness is problematic, making this attribute a priority for measure development. Range of services offered is best obtained from providers. Whole-person care is not addressed as a separate construct, but some dimensions are covered by attributes such as interpersonal communication and relational continuity.
Abstract
La notion de globalité des soins s'applique tant à l'étendue des services offerts qu' à une approche holistique des soins cliniques. La globalité des services se définit comme « la prestation, directe ou indirecte, d'une gamme complète de services afin de répondre aux besoins des patients en matière de soins de santé »; les soins centrés sur le patient se définissent par « l' étendue selon dans laquelle le fournisseur de soins considère les aspects physiques, émotionnels et sociaux de la santé d'un patient et tient compte du contexte communautaire lors de la prestation de soins. » Deux des instruments d'évaluation des soins primaires comprennent des sous-échelles qui correspondent à la globalité des soins et aux composantes communautaires des soins centrés sur le patient : le Primary Care Assessment Tool – version courte (PCAT-S) et le Components of Primary Care Index (CPCI, mesure limitée des soins centrés sur le patient).
Objectif :
Examiner dans quelle mesure la globalité des soins est captée par les instruments validés qui servent à évaluer les soins de santé primaires du point de vue du patient.
Méthode :
Six cent quarante-cinq adultes, qui ont eu au moins un contact avec les services de santé au cours des 12 mois antérieurs, ont répondu à six instruments d'évaluation des soins primaires. Les résultats ont été normalisés pour permettre des comparaisons descriptives. Les analyses factorielles exploratoires et confirmatoires (modélisation par équation structurelle) ont été employées pour vérifier l'adéquation à la définition opérationnelle, et l'analyse de réponse par item a été utilisée pour examiner la performance en fonction de construits communs.
Résultats :
Plus du quart des répondants ont laissé des questions sans réponse au sujet des services offerts ou des connaissances du médecin sur la communauté. Les sous-échelles ne correspondent pas à un seul facteur; la globalité des services et l'orientation communautaire ont été examinées séparément. Les sous-échelles « orientation communautaire » n'ont pas offert une performance satisfaisante. Les trois sous-échelles « globalité des services » se sont ajustées très modestement à deux facteurs : (1) la plupart des besoins en matière de services de santé [d'un fournisseur] (« globalité des soins » du CPCI et « utilisation de premier contact » du PCAT-S) et (2) étendue des services (« globalité des services disponibles » du PCAT-S). La performance individuelle d'items a révélé plusieurs problèmes.
Conclusion :
La mesure de la globalité des soins est problématique, ce qui en fait une priorité pour le développement de mesures. L' étendue des services offerts s'obtient plus efficacement auprès des fournisseurs. Les soins centrés sur le patient ne sont pas traités comme un construit indépendant, mais certaines dimensions sont couvertes par des caractéristiques telles que la communication interpersonnelle et la continuité relationnelle.
Comprehensiveness is enshrined as one of the five principles of the Canada Health Act (Madore 2005) and is often applied as a qualifier of primary healthcare (PHC) (Macinko et al. 2007; Romanow 2002), distinguishing the ideal from the merely functional or, at worst, “selective” (Cueto 2004) forms of care. While this attribute evokes a sense of “good,” the generality of its invocation obscures precision about its meaning, posing a major challenge for its assessment.
Background
Conceptualizing comprehensiveness
One objective of PHC reform in Canada is to expand the comprehensiveness of services, especially in health promotion and chronic disease management (Health Canada 2007). Most PHC renewal interventions include introducing team-based care and alternative payment mechanisms. Consequently, evaluating comprehensiveness of care is vital to evaluating the renewal of PHC in Canada.
The dictionary definition of comprehensiveness – “covering completely or broadly” (Merriam-Webster 1998) – is applied in PHC to the mandate to resolve and manage the most prevalent health conditions, undifferentiated by age, sex or disease (CFPC 2006). However, comprehensiveness sometimes refers to the bio-psycho-social or whole-person approach, which sees the patient as body and soul within a specific social context (CFPC 2006). The closest French equivalent of “comprehensiveness,” globalité, invokes an image of both scope and whole-person approach.
Evaluating the comprehensiveness of primary healthcare
A clear operational definition of comprehensiveness is a first step in any measurement. Our consensus consultation of PHC experts (Haggerty et al. 2007) unanimously identified comprehensiveness as a core attribute of PHC, but two distinct definitions emerged. The first, comprehensive services, corresponds to scope: “The provision, either directly or indirectly, of a full range of services to meet patients' healthcare needs. This includes health promotion, prevention, diagnosis and treatment of common conditions, referral to other providers, management of chronic conditions, rehabilitation, palliative care and, in some models, social services.” The second definition, whole-person care, is: “The extent to which a provider elicits and considers the physical, emotional and social aspects of a patient's health and considers the community context in their care.” Most experts agreed that providers and utilization data were the best data sources for comprehensive services, and the patient for whole-person care.
Our objective was to compare subscales from different validated instruments that purport to measure comprehensiveness. We compare scores and examine (a) whether comprehensiveness subscales from different instruments seem to measure the same underlying construct, or how emerging factors relate to both operational definitions and (b) how well individual items perform. Our intent is not to recommend one instrument over another, but to provide evaluators with insight into how well different subscales fit the experts' operational definitions.
Method
The method and analytic strategy are described in detail elsewhere in this special issue of the journal (Haggerty, Burge et al. 2011; Santor et al. 2011). Briefly: six instruments that evaluate PHC from the patient's perspective were administered to 645 healthcare users balanced by English/French language, rural/urban location, low/high level of education and poor/average/excellent overall PHC experience. The analysis consisted of examining the distributional statistics and subscale correlations, followed by common factor and confirmatory factor analysis (structural equation modelling) to identify dimensions common to the entire set of items. Finally, we examined the performance of individual items and response scales against constructs emerging across instruments using item response theory analysis.
Measure description
Among the six validated instruments in our study that assess PHC services from the patient's perspective, two contain subscales that mapped to our operational definitions of comprehensiveness. No subscales mapped specifically to whole-person care except for subscales for community-oriented clinical care that address one element in our definition of whole-person care: “elicits and considers the social aspects of a patient's health and considers the community context in their care.”
The Components of Primary Care Index (CPCI) (Flocke 1997) has a six-item Comprehensive Care and a two-item Community Context subscale. Both elicit degree of agreement with statements about the “regular doctor” using a six-point semantic differential response scale with “1=strongly disagree” and “6=strongly agree” as anchors at each extremity.
The Primary Care Assessment Tool – Short Form, adult (PCAT-S) (Shi et al. 2001) has a four-item Services Available and a three-item Community Orientation subscale. The subscale assessing comprehensiveness with a Services Received subscale was not retained in our study because we mapped it to health promotion. The three-item subscale on First-Contact Utilization, initially mapped to accessibility, was included in the comprehensiveness attribute based on best psychometric fit (Haggerty, Lévesque et al. 2011). Questions about different aspects of care from the “primary care provider” are answered using a four-point Likert scale (“1=definitely not,” “2=probably not,” “3=probably,” “4=definitely”).
Results
Comparative descriptive statistics
Table 1 summarizes the item content and behaviour in the five subscales; the detailed content and distributions are available online at http://www.longwoods.com/content/22639. Several items have more than 5% missing values, especially items about available service by the doctor or clinic. Most problematically, a large proportion selected the “not sure” option for items in the PCAT-S Services Available and Community Orientation subscales, interpreted as missing values. Indeed, this was the model response for two items in the three-item PCAT-S Community Orientation subscale. Ceiling effects were present with a large proportion endorsing the maximum value, especially for the CPCI Comprehensive Care and the PCAT-S First-Contact Utilization items. The discriminability of items indicates good capacity to discriminate between different levels of the subscale score.
TABLE 1.
Summary of comprehensiveness of services subscale content and distribution of item responses. (Detailed distribution available at http://www.longwoods.com/content/22639)
| Subscale and Item Description | Response Scale | Range Missing Values | Overall Modal Response | Range Item Discriminability | Comments on Distribution |
|---|---|---|---|---|---|
| Comprehensive Services | |||||
|
CPCI Comprehensive Care (6 items) Agreement with statements about regular doctor: I go to this doctor for almost all my medical care; doctor handles emergencies; can take care of almost any medical problem I could go to this doctor: for help with an emotional problem; for care of an ongoing problem; for a check-up to prevent illness |
Semantic differential opinion, 1=strongly disagree, 6=strongly agree | 2%–6% | 6 (strongly agree) | 1.32 (emergencies) to 3.00 (ongoing problem) | 30%–67% of respondents select most positive opinion; 3%–10% most negative |
|
PCAT-S Comprehensiveness – Services Available (4 items) Likelihood of reporting of availability of service at the clinic… Immunizations; family planning or birth control; counselling for mental health problems; sewing up a cut that needs stitches |
Likert evaluative, 1=definitely not to 4=definitely | 2%–7% (true missing), 8%–24% not sure | 4 (definitely) | 1.84 (sewing) to 2.10 (family planning) | Approximately 15%–24% of respondents “not sure” (exception for Immunizations) |
|
PCAT-S First-Contact Utilization (3 items) Likelihood of seeking care first from primary care provider for routine care; for a new problem; need for referral to see a specialist |
Likert evaluative, 1=definitely not to 4=definitely | 1%–2% (true missing), 0%–4% not sure | 4 (definitely) | 0.87 (referral by PCP) to 4.7 (clinic=first place for routine care) | ∼85% of responses in the most positive category for seeking care first with primary care provider |
| Community Oriented (Whole-Person Care) | |||||
|
CPCI Community Context (2 items) Agreement with statements about regular doctor: This doctor knows a lot about my community; uses her/his knowledge of my community to take care of me |
Semantic differential opinion, 1=strongly disagree, 6=strongly agree | 4%–5% | 6 (strongly agree) | Inappropriate in a two-item scale services | Responses relatively evenly distributed among options; ∼32% in most positive category |
|
PCAT-S Community Orientation (3 items) Likelihood of primary care provider… Making home visit; knowing about health problems in neighbourhood; getting opinions from people to provide better healthcare |
Likert evaluative, 1=definitely not to 4=definitely | 2% (true missing), 27%–32% not sure | 3 (probably) | 1.18 (get opinions) to 2.61 (neighbourhood) | Responses relatively evenly distributed among options. High missing values due to “not sure” response. |
TABLE 1.
Distribution of responses to items in subscales mapped to comprehensiveness of services and whole-person care, grouped within instrument subscale (n=645)
| Item Code | Item Statement | Missing % (n) | Percentage (Number) by Response Option | Item Discrimination* | |||||
|---|---|---|---|---|---|---|---|---|---|
| Comprehensiveness of Services | |||||||||
| CPCI Comprehensive Care | |||||||||
| 1=Strongly disagree | 2 | 3 | 4 | 5 | 6=Strongly agree | ||||
| CP_cc1 | I go to this doctor for almost all my medical care. | 2 (10) | 3 (18) | 1 (8) | 7 (42) | 6 (41) | 15 (96) | 67 (430) | 2.30 (0.21) |
| CP_cc2 | This doctor handles emergencies. | 6 (36) | 10 (63) | 8 (52) | 17 (109) | 12 (80) | 17 (111) | 30 (194) | 1.32 (0.13) |
| CP_cc3 | This doctor can take care of almost any medical problem I might have. | 3 (19) | 6 (40) | 6 (40) | 10 (64) | 19 (122) | 23 (148) | 33 (212) | 2.50 (0.18) |
| CP_cc4 | I could go to this doctor for help with a personal or emotional problem. | 3 (22) | 7 (43) | 7 (43) | 9 (58) | 13 (83) | 19 (122) | 42 (274) | 2.51 (0.19) |
| CP_cc5 | I could go to this doctor for care of an ongoing problem such as high blood pressure. | 2 (11) | 3 (17) | 2 (11) | 5 (33) | 7 (42) | 16 (102) | 67 (429) | 3.00 (0.26) |
| CP_cc6 | I could go to this doctor for a check-up to prevent illness. | 2 (11) | 4 (24) | 3 (22) | 5 (30) | 8 (52) | 21 (134) | 58 (372) | 1.90 (0.16) |
| PCAT-S Comprehensiveness – Services Available | |||||||||
| Following is a list of services that you or your family might need at some time. For each one, please indicate whether it is available at your Primary Care Provider's office. | 1=Definitely not | 2=Probably not | 3= Probably | 4= Definitely | Not sure / Don't remember | ||||
| PT_csa1 | Immunizations (shots) | 2 (15) | 5 (33) | 3 (22) | 13 (82) | 68 (441) | 8 (52) | 2.07 (0.21) | |
| PT_csa2 | Family planning or birth control methods | 7 (45) | 5 (32) | 2 (15) | 17 (110) | 55 (352) | 14 (91) | 2.10 (0.21) | |
| PT_csa3 | Counselling for mental health problems | 6 (38) | 9 (57) | 12 (79) | 23 (146) | 29 (188) | 21 (137) | 2.00 (0.19) | |
| PT_csa4 | Sewing up a cut that needs stitches | 5 (29) | 11 (71) | 12 (77) | 18 (118) | 30 (194) | 24 (156) | 1.84 (0.19) | |
| PCAT-S First-Contact Utilization | |||||||||
| 1=Definitely not | 2=Probably not | 3= Probably | 4= Definitely | Not sure / Don't remember | |||||
| PT_fcu1 | When you need a regular general checkup, do you go to your Primary Care Provider before going somewhere else? | 1 (7) | 2 (12) | 1 (6) | 10 (64) | 86 (554) | 0 (2) | 4.70 (0.60) | |
| PT_fcu2 | When you have a new health problem, do you go to your Primary Care Provider before going somewhere else? | 1 (8) | 2 (13) | 2 (15) | 12 (79) | 82 (528) | 0 (2) | 4.59 (0.54) | |
| PT_fcu3 | When you have to see a specialist, does your Primary Care Provider have to approve or give you a referral? | 2 (10) | 2 (16) | 4 (27) | 23 (151) | 65 (418) | 4 (23) | 0.87 (0.13) | |
| Whole Person Care (community aspect only) | |||||||||
| CPCI Community Context | |||||||||
| 1=Strongly disagree | 2 | 3 | 4 | 5 | 6=Strongly agree | ||||
| CP_com1 | This doctor knows a lot about my community. | 4 (24) | 8 (51) | 9 (59) | 13 (84) | 15 (94) | 20 (132) | 31 (201) | ** |
| CP_com2 | This doctor uses her/his knowledge of my community to take care of me. | 5 (30) | 11 (69) | 10 (67) | 11 (71) | 14 (92) | 16 (105) | 33 (211) | ** |
| PCAT-S Community Orientation | |||||||||
| 1=Definitely not | 2=Probably not | 3= Probably | 4= Definitely | Not sure / Don't remember | |||||
| PT_co1 | Does anyone at your Primary Care Provider's office ever make home visits? | 2 (12) | 30 (193) | 18 (118) | 9 (61) | 9 (57) | 32 (204) | 1.54 (0.18) | |
| PT_co2 | Does your Primary Care Provider know about the important health problems of your neighborhood? | 2 (14) | 20 (128) | 18 (114) | 23 (149) | 11 (69) | 27 (171) | 2.61 (0.23) | |
| PT_co3 | Does your Primary Care Provider get opinions and ideas from people that will help to provide better health care? | 2 (13) | 4 (28) | 8 (54) | 38 (247) | 20 (130) | 27 (173) | 1.18 (0.15) | |
Items were assessed against the construct of the original scale. Values >1 are considered to be discriminating, indicating that each unit increase in the item score corresponds to more than one unit increase in the summed subscale score.
Calculation of a discriminant parameter in a two-item scale is inappropriate
Table 2 presents the descriptive statistics by subscales. Scores are normalized to 0 to 10 to permit direct comparisons. The whole-person (community) subscales have very different means but their distribution approximates a normal curve. The comprehensive services scores are skewed towards positive values, with the PCAT-S First-Contact Utilization subscale being highly skewed; its score does not resemble that of the CPCI Comprehensive Care subscale, to which it is most similar in item content. Internal consistency (.65 to .83) is lower than for most subscales of other attributes, partly explained by the small number of items in some subscales.
TABLE 2.
Mean and distributional scores for comprehensiveness subscales, showing normalized scores from 0 to 10 (n=645)*
| Developer's Scale Name (# items in scale) | Cronbach's Alpha | Mean | SD | Quartiles | ||
|---|---|---|---|---|---|---|
| Q1 (25%) | Q2 (50%) | Q3 (75%) | ||||
| Comprehensiveness of Services | ||||||
| CPCI Comprehensive Care (6) | .83 | 7.7 | 2.1 | 6.7 | 8.0 | 9.3 |
| PCAT-S Comprehensiveness (Services Available) (4) | .72 | 7.7 | 2.5 | 6.7 | 8.3 | 10.0 |
| PCAT-S First-Contact Utilization (3) | .68 | 9.1 | 1.6 | 8.9 | 10.0 | 10.0 |
| Whole-Person Care | ||||||
| CPCI Community Context (2) | .82 | 6.5 | 3.1 | 4.0 | 7.0 | 10.0 |
| PCAT-S Community Orientation (3) | .65 | 4.9 | 2.9 | 3.3 | 5.0 | 6.7 |
Subscale scores calculated as mean of item values and only calculated for observations where >50% of items were complete.
Table 3 presents the Pearson correlations between the comprehensiveness subscales. The comprehensive service subscales have low to modest correlation with one another, and whole-person (community) subscales correlate only modestly (.32). The highest correlation (r=.49) is between the two CPCI Comprehensive Care and Community Context subscales. The PCAT-S subscales do not correlate well with each other; the Services Available and First-Contact Utilization subscales correlate only weakly (r=.08), suggesting that they measure different facets of comprehensiveness. When correlated with subscales of other attributes, both CPCI subscales correlate equally or higher with measures of relational continuity (.45 to .71) than with other comprehensiveness subscales. The PCAT-S subscales correlate as well or better with measures of other attributes, though still more modestly than do the CPCI subscales; the PCAT-S Community Orientation subscale correlates most strongly (r=.37) with patient-centred decision-making from the Interpersonal Processes of Care instrument (Stewart et al. 2007).
TABLE 3.
Mean partial Pearson correlations between comprehensiveness subscales and with other subscales included in the questionnaires.* Only correlations significantly different from zero are provided.
| Questionnaire Subscale | CPCI: Comprehensive Care | PCAT-S: Services Available | PCAT-S: First-Contact Utilization | CPCI: Community Context | PCAT-S: Community Orientation | |
|---|---|---|---|---|---|---|
| Comprehensiveness of Services | ||||||
| CPCI Comprehensive Care | 1.00 | 0.28 | 0.34 | 0.49 | 0.22 | |
| PCAT Services Available | 0.28 | 1.00 | 0.08 | 0.22 | 0.23 | |
| PCAT First-Contact Utilization | 0.34 | 0.08 | 1.00 | 0.20 | 0.09 | |
| Whole-Person Care | ||||||
| CPCI Community Context | 0.49 | 0.22 | 0.20 | 1.00 | 0.32 | |
| PCAT Community Orientation | 0.22 | 0.23 | 0.09 | 0.32 | 1.00 | |
Note: Controlling for study design variables (language, educational achievement, geographic location).
Do all items measure a single attribute?
Missing values drastically reduced the effective sample size for factor analysis from 645 to 322 (listwise missing). The majority of exclusions (79% or 255/323) were due to selecting the “not sure/don't know” option. Respondents excluded were older and in worse health than those included, but were otherwise similar in all measured variables. Imputing values for missing responses increased the analytic sample to 490 and slightly improved the fit statistics but did not change the conclusions, suggesting that we principally lost statistical power and did not introduce bias by using the more conservative approach for factor analysis.
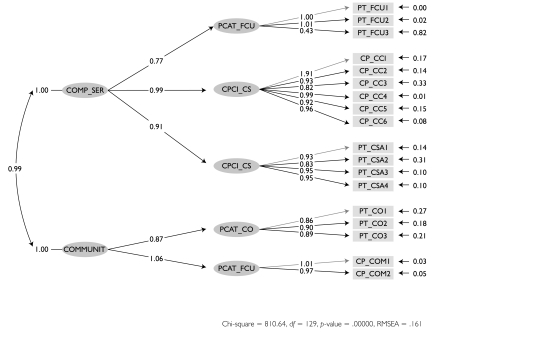
We had little expectation that all items would load on a single factor because we had two operational definitions. Indeed, a one-factor model with structural equation modelling generated fit statistics suggesting poor fit, with a root mean squared error of approximation (RMSEA) of p=.184, considerably higher than the .05 standard for good fit. We removed PCAT-S First-Contact Utilization and the RMSEA fit improved (p=.134), but at the expense of the normed fit index (NFI), which went from .96 to .91, though still higher than the .90 standard for good fit. However, removing the two whole-person (community) subscales improved model fit overall (RMSEA, p=.125; NFI=.94). Even when items are grouped within their original subscales loading on a single construct, presumed to be comprehensiveness (usually expected to improve fit), the model does not fit a single underlying factor (RMSEA, p=.165; NFI=.97). We concluded that the community subscales measure a separate construct and need to be examined in independent models. Figure 1 presents the model with items grouped within their parent instrument subscales as five first-order latent variables, which in turn emerge from two separate, though correlated, second-order constructs, community and comprehensive services (RMSEA, p=.165; NFI=.97). Remaining analyses examine community and comprehensive cervices constructs separately.
FIGURE 1.
Parameter estimations for a structural equation second-order model where a single underlying construct (second-order latent variable) leads to the five subscales (first-order variables) with loadings on their respective items
How do underlying factors fit with operational definitions?
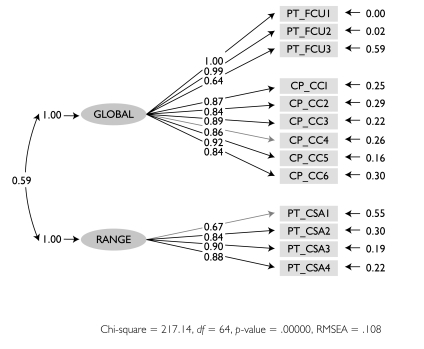
For comprehensive services, exploratory factor analysis suggested two underlying factors. Using our operational definitions as a guide to infer the factors, we judged that the first (eigenvalue=3.80) captures “meeting most of the patient's healthcare needs” or Most Needs. This item was composed of items from the CPCI Comprehensive Care and the PCAT-S First-Contact Utilization subscales. The second factor (eigenvalue=1.03) corresponds to “the provision directly of a full range of services,” or Range, and consists only of items from the PCAT-S Services Available subscale. When items are grouped by Range and Most Needs, model goodness-of-fit statistics improve dramatically over the one-dimensional model (Figure 2). However, fit is only adequate (RMSEA, p=.108; NFI=.95), and Range and Most Needs correlate only modestly (.59).
FIGURE 2.
Parameter estimations for a structural equation first-order model where sub-dimensions are correlated
For whole-person care, it is clear that the CPCI Community Context and PCAT-S Community Orientation subscales respond only to the social or community elements of the operational definition. They hold together as a single factor but do not represent whole-person care completely. Exploratory factor analysis with other attributes of care found that the community items load relatively well with items from the Accumulated Knowledge subscale in relational continuity and modestly with the Elicit construct of interpersonal communication.
Individual item performance
In confirmatory factor analysis, many items have a high proportion of residual error (shown to the right of each item label in Figures 1 and 2), which may reflect either poor conceptual fit or poor item performance.
Indeed, graphs of non-parametric item response analysis suggest that item performance may be largely responsible for poor model fit. Only two items show adequate discriminability and response behaviour for Most Needs, both from the CPCI Comprehensive Care subscale: “take care of almost any medical problem” and “help with a personal or emotional problem” (CP_cc4). The discriminatory capacity of “doctor handles emergencies” (CP_cc2), while modest overall, is concentrated in the central zone of Most Needs, consequently making an important contribution to the precision of the subscale. In remaining items, the most positive option is predominantly endorsed, even at low levels of Most Needs, providing adequate differentiation between low and average levels of Most Needs but no discrimination between above-average levels. Skewed items towards positive values provide excellent discrimination and information yield in the negative range of the attribute of interest. Conversely, skewing towards negative values provides good discrimination in the positive range, as for PCAT-S Community Orientation items on home visits and knowing the important problems in the patient's neighbourhood.
Discussion
Although comprehensiveness is a core PHC attribute, we encountered difficulties in both its definition and its measurement. The definitional challenge was resolved by distinguishing between comprehensive services and whole-person care, suggesting the need for two different measures. However, we found problems with measures of both operational definitions.
Comprehensive services referring to scope of services is the most common use of comprehensiveness in the PHC and evaluation literature. However, our consensus consultation with experts indicates that providers – not patients – are the best source of information on this attribute because providers need to plan service delivery to meet the needs of a broad group of patients (Haggerty et al. 2007). This disparity may explain the poor performance items eliciting the availability of specific services. Patients can validly assess only the availability of services that they or their close associates have needed. Although the “don't know” option in the PCAT-S Services Available subscale allows patients to state their level of knowledge, this option counts as a missing value for measurement purposes, compromising the subscale's psychometric performance and resulting in loss of information. Program evaluators and policy makers interested in evaluating range of comprehensive services are advised to obtain data from the providers themselves or the records of service provision.
Given the importance of this attribute to PHC and health system performance, it would be important to define minimal standards for PHC comprehensiveness in Canada. An environmental scan of Canadian policy documents provides a composite profile of expected services: rapid management of acute and urgent health problems; timely provision of non-urgent routine care (including wellness care and chronic illness management); coverage with recommended preventive services; referral to hospitals and specialists; follow-up care after hospitalization or specialty care; primary mental healthcare; full maternity and child care; coordinated care of the frail elderly; and end-of-life care (Haggerty and Martin 2005). These services are potentially traceable with medical service billings, but not all elements can be captured in each province or compared among provinces. Some of these elements are elicited in the National Physician Survey (CFPC et al. 2007). These periodic surveys indicate that urban physicians are increasingly developing areas of expertise and working in group settings, or with other professionals, to ensure a wide range of services, whereas rural doctors retain a comprehensive profile in their personal practice (CFPC 2008).
The dimension of whole-person care is best measured from the patient's perspective, but no subscales mapped principally to this attribute – a surprising finding, given its philosophic centrality in PHC. However, attention to both emotional and physical needs are covered in other subscales. Accumulated Knowledge subscales within relational continuity measure the primary care physician's knowledge about various dimensions of the person (medical, family, work, values) and whether the patient is known as a person and not merely as someone with a medical problem (Burge et al. 2011). Attentiveness to the patient's felt concerns are addressed in the Elicit dimension of interpersonal communication (Beaulieu et al. 2011). In contrast, the subscales in this study covered only the “social aspects of care.” Whole-person care may be inferred from the use of multiple subscales, including the community scales covered in this paper.
Whole-person care relates closely to the concept of person-centred care. Two relevant instruments assessing patient-centredness of clinical encounters were not included in our study because they are visit-based (Stewart et al. 2000, 2003; Little et al. 2001). Positive assessments on both instruments have been linked to better satisfaction and symptom resolution (Little et al. 2001; Stewart et al. 2000).
The French word for “comprehensiveness,” globalité, connotes both scope of services and a bio-psycho-social approach. The CPCI Comprehensive Care subscale has items relating both to scope (the doctor handles emergencies) and bio-psycho-social approach (can help with a personal or emotional problem). It would be the best measure of globalité. Item response analysis suggests that the performance of this subscale would be improved by dropping non-informative or redundant items (most medical care and checkups) and adjusting the response scale.
There are limitations to this study. Most notably, our decision to map entire subscales to our operational definitions led to our representing whole-person care only by subscales addressing community care, providing only limited coverage of whole-person care. It would be more appropriate to view our results for these subscales as assessing community-oriented care, which was the original intention. Though some measurement problems persist, “community-oriented care” is a more valid representation of the construct. Finally, the lack of another data source on the actual services offered by the provider limits our capacity to assess the validity of patients' reports of available services.
Conclusion and Lessons Learned
In sum, the CPCI Comprehensive Care subscale provides a good assessment of patients' confidence in their physician's ability to meet most of their healthcare needs, including emotional problems (globalité). The bio-psycho-social approach is partially covered in instruments measuring relational continuity and interpersonal communication. Demonstrated provider knowledge of the patient's community with the PCAT-S Community Orientation subscale would indicate excellent accumulated and global knowledge.
Physician report or billing data is the best source for evaluating range of services. Given the importance of PHC comprehensiveness to system performance, it is critical for policy makers to define minimal standards for service provision across provinces and to ensure that these are adequately captured in billing data or electronic medical records used to assess this critical aspect of care.
Acknowledgements
This research was funded by the Canadian Institutes for Health Research. During this study Jeannie L. Haggerty held a Canada Research Chair in Population Impacts of Healthcare at the Université de Sherbrooke. The authors wish to thank Beverley Lawson for conducting the survey in Nova Scotia and Christine Beaulieu in Quebec and Donna Riley for support in preparation and editing of the manuscript.
Contributor Information
Jeannie L. Haggerty, Department of Family Medicine, McGill University, Montreal, QC.
Marie-Dominique Beaulieu, Chaire Dr Sadok Besrour en médecine familiale, Centre de recherche du Centre hospitalier de l'Université de Montréal, Montréal, QC.
Raynald Pineault, Département de Médecine sociale et préventive, Université de Montréal, Montreal, QC.
Frederick Burge, Department of Family Medicine, Dalhousie University, Halifax, NS.
Jean-Frédéric Lévesque, Centre de recherche du Centre hospitalier de l'Université de Montréal, Montréal, QC.
Darcy A. Santor, School of Psychology, University of Ottawa, Ottawa, ON.
Fatima Bouharaoui, St. Mary's Research Centre, St. Mary's Hospital Center, Montreal, QC.
Christine Beaulieu, St. Mary's Research Centre, St. Mary's Hospital Center, Montreal, QC.
References
- Beaulieu M.-D., Haggerty J.L., Beaulieu C., Bouharaoui F., Lévesque J.-F., Pineault R., et al. 2011. “Interpersonal Communication from the Patient Perspective: Comparison of Primary Healthcare Evaluation Instruments.” Healthcare Policy 7 (Special Issue): 108–23 [PMC free article] [PubMed] [Google Scholar]
- Burge F., Haggerty J.L., Pineault R., Beaulieu M.-D., Lévesque J.-F., Beaulieu C., et al. 2011. “Relational Continuity from the Patient Perspective: Comparison of Primary Healthcare Evaluation Instruments.” Healthcare Policy 7 (Special Issue): 124–38 [PMC free article] [PubMed] [Google Scholar]
- College of Family Physicians of Canada (CFPC) 2006. Standards for Accreditation of Family Medicine Residency Training Programs (“The Red Book”). Mississauga, ON: Author [Google Scholar]
- College of Family Physicians of Canada (CFPC) 2008. The Face of Family Medicine Today: Results of the National Physician Survey. Mississauga, ON: Author [Google Scholar]
- College of Family Physicians of Canada (CFPC), Canadian Medical Association and Royal College of Physicians and Surgeons of Canada 2007. 2007 National Physician Survey. Retrieved July 28, 2011. <http://www.nationalphysiciansurvey.ca/nps/2007_Survey/2007nps-e.asp>.
- Cueto M. 2004. “The Origins of Primary Health Care and Selective Primary Health Care.” American Journal of Public Health 94: 1864–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flocke S. 1997. “Measuring Attributes of Primary Care: Development of a New Instrument.” Journal of Family Practice 45(1): 64–74 [PubMed] [Google Scholar]
- Haggerty J.L., Burge F., Beaulieu M.-D., Pineault R., Beaulieu C., Lévesque J.-F., et al. 2011. “Validation of Instruments to Evaluate Primary Healthcare from the Patient Perspective: Overview of the Method.” Healthcare Policy 7 (Special Issue): 31–46 [PMC free article] [PubMed] [Google Scholar]
- Haggerty J., Burge F., Lévesque J.-F., Gass D., Pineault R., Beaulieu M.-D., Santor D.A. 2007. “Operational Definitions of Attributes of Primary Health Care: Consensus among Canadian Experts.” Annals of Family Medicine 5: 336–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haggerty J.L., Lévesque J.-F., Santor D.A., Burge F., Beaulieu C., Bouharaoui F., et al. 2011. “Accessibility from the Patient Perspective: Comparison of Primary Healthcare Evaluation Instruments.” Healthcare Policy 7 (Special Issue): 94–107 [PMC free article] [PubMed] [Google Scholar]
- Haggerty J., Martin C.M. 2005. Evaluating Primary Health Care in Canada: The Right Questions to Ask. Ottawa: Health Canada, Primary and Continuing Healthcare Division [Google Scholar]
- Health Canada 2007. (March 1). Primary Health Care Transition Fund. Retrieved July 28, 2011. <http://www.hc-sc.gc.ca/hcs-sss/prim/phctf-fassp/index-eng.php>.
- Little P., Everitt H., Williamson I., Warner G., Moore M., Gould C., et al. 2001. “Observational Study of Effect of Patient Centredness and Positive Approach on Outcomes of General Practice Consultations.” British Medical Journal 323: 908–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macinko J., Montenegro H., Nebot C.PAHO Working Group on Primary Health Care 2007. Renewing Primary Health Care in the Americas: A Position Paper of the Pan American Health Organization/World Health Organization (PAHO/WHO). Washington, DC: Pan American Health Organization [Google Scholar]
- Madore Odette. 2005. The Canada Health Act: Overview and Options. Report no. CIR94-4E. Ottawa: Library of Parliament, Parliamentary Information and Research Service [Google Scholar]
- Merriam-Webster's Collegiate Dictionary. 1998. Springfield, MA: Author [Google Scholar]
- Romanow R.J. 2002. Building on Values: The Future of Health Care in Canada. Final Report. Regina: Commission on the Future of Health Care in Canada [Google Scholar]
- Santor D.A., Haggerty J.L., Lévesque J.-F., Burge F., Beaulieu M.-D., Gass D., et al. 2011. “An Overview of Confirmatory Factor Analysis and Item Response Analysis Applied to Instruments to Evaluate Primary Healthcare.” Healthcare Policy 7 (Special Issue): 79–92 [PMC free article] [PubMed] [Google Scholar]
- Stewart A.L., Nápoles-Springer A.M., Gregorich S.E., Santoyo-Olsson J. 2007. “Interpersonal Processes of Care Survey: Patient-Reported Measures for Diverse Groups.” Health Services Research 42: 1235–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart M., Brown J.B., Donner A., McWhinney I.R., Oates J., Weston W.W., Jordan J. 2000. “The Impact of Patient-Centered Care on Outcomes.” Journal of Family Practice 49: 796–804 [PubMed] [Google Scholar]
- Stewart M., Brown J.B., Weston W.W., McWhinney I.R., McWilliam C.L., Freeman T.R. 2003. Patient-Centered Medicine: Transforming the Clinical Method (2nd ed). Oxford: Radcliffe Medical Press [Google Scholar]