Abstract
The H275Y oseltamivir resistance mutation confers high-level resistance to oseltamivir in isolates of human A(H1N1) influenza. We report the recovery and identification of an influenza B virus with the H273Y neuraminidase point mutation directly from a human patient. The H273Y influenza B isolate is resistant to oseltamivir and peramivir but sensitive to zanamivir.
TEXT
Resistance to oseltamivir is conferred on seasonal and pandemic A(H1N1) neuraminidase (NA) by a histidine-to-tyrosine mutation at position 275 (corresponds to 273 in B and 274 in N2 NA amino acid numbering) which causes a structural change in the protein active site that weakens the binding of oseltamivir (4). Although initially rare, this mutation became prevalent in clinical samples from treated patients during the 2007 to 2008 influenza season. Seasonal influenza A(H1N1) viruses with this mutation reached a prevalence of nearly 11% by the end of the season in North America and began to spread globally to near fixation by the 2008 to 2009 season (2, 6, 12). Resistance to oseltamivir in the pandemic A(H1N1) virus subtype [A(H1N1)pdm09] appears to be rare despite the widespread use of this drug during the 2009 influenza A(H1N1) pandemic (10, 13) (R. R. Higgins, M. Beniprashad, E. Chong-King, A. Marchand-Austin, Y. Li, , D. E. Low, and J. B. Gubbay, unpublished data). Although amino acid residues at the neuraminidase active site are highly conserved in influenza A and B types, known neuraminidase substitutions identified in resistant viruses from humans tend to be virus type or subtype specific. For example, E119V (Glu119Val), R292K (Arg292Lys), and N294S (Asn294Ser) are specific to the A(H3N2) subtype, H275Y (His275Tyr) is specific to the A(H1N1) and A(H5N1) subtypes, and R152K (Arg152Lys), D198N (Asp198Asn), I222T (Ile222Thr), and R371K (Arg371Lys) are specific to the influenza B type (1, 9, 11, 12, 17). All these substitutions are associated with catalytic or framework residues in the active site of the neuraminidase protein (5). The H275Y specific to the N1 subtype was shown to arise in one influenza B (H273Y) isolate after 15 passages in cell culture and in the presence of increasing concentrations of the neuraminidase inhibitor (NAI) peramivir (3). Another study described the detection of a similar influenza B virus from a clinical specimen with the H275Y point mutation and reduced sensitivity to oseltamivir (17). Here we report the recovery and identification of an influenza B virus with the H273Y oseltamivir mutation directly from a human patient with no known history of previous oseltamivir treatment. We show that the H273Y influenza B isolate is resistant to oseltamivir and peramivir but sensitive to zanamivir.
On 10 April 2011, a patient with fever and cough presented at the emergency room of a regional hospital but was not admitted. The patient was male and age 33. No history of the patient is available, and it is not known if the patient was previously treated with antiviral or neuraminidase inhibitor. A nasopharyngeal swab was taken and tested for influenza by a virus culture. Influenza B was detected, and the sample, designated B/Ontario/006876/2011, was submitted for further testing.
As part of the Public Health Ontario (PHO) pandemic surveillance program, the specimen was cultured in rhesus monkey kidney cells and subjected to NAI testing for resistance to oseltamivir carboxylate, peramivir, and zanamivir. Specimens with elevated 50% inhibitory concentrations (IC50s) were further subjected to strain typing and DNA sequencing of NA or the whole genome using a modified World Health Organization protocol. Chemiluminescent NAI testing of B/Ontario/006876/2011 showed sensitivity to zanamivir (IC50 = 0.93 ± 0.66 nM) but elevated IC50s to both oseltamivir and peramivir. The IC50 for oseltamivir was 19.4 ± 0.65 nM and for peramivir was 11.12 ± 0.23 nM, 11.4-fold and 34.8-fold increases, respectively, relative to the IC50 of the reference influenza B virus (Table 1).
Table 1.
Antiviral susceptibility and genotype of an influenza B virus with an H273Y substitution that was recovered from a patient in Ontario, Canada, during the 2010 to 2011 influenza seasona
| Virus strain | Type/subtype | Passage/virus subsetb | NA mutation | Oseltamivir carboxylate |
Peramivir |
Zanamivir |
|||
|---|---|---|---|---|---|---|---|---|---|
| Mean IC50 ± SD (nM) | Fold difference | Mean IC50 ± SD (nM) | Fold difference | Mean IC50 ± SD (nM) | Fold difference | ||||
| B/Ontario/006876/2011 | B | Primary | H273Y | Not tested | Not tested | Not tested | Not tested | Not tested | Not tested |
| B/Ontario/006876/2011 | B | 1 | H273Y | 19.4 ± 0.65 | 11.4 | 11.12 ± 0.23 | 34.8 | 0.93 ± 0.66 | 1 |
| B/Memphis/20/96 | B | Reference | WT | 1.32 ± 0.85 | 1 | 0.32 ± 0.23 | 1 | 1.35 ± 0.37 | 1 |
| B/Memphis/20/96 | B | Reference | R152K | 156.25 ± 70.04 | 118 | 43.14 ± 15.32 | 134.8 | 38.82 ± 29.33 | 28.75 |
| A/California/07/2009 | A(H1N1)2009 | Reference | WT | 0.12 ± 0.04 | 1 | 0.08 ± 0.04 | 1 | 0.10 ± 0.06 | 1 |
| A/North Carolina/39/2009 | A(H1N1)2009 | Reference | H275Y | 81.25 ± 42.16 | 677 | 9.05 ± 1.54 | 113.1 | 0.26 ± 0.07 | 1 |
| A/Wuhan/395/95 | A(H3N2) | Reference | WT | 0.27 ± 0.11 | 1 | 0.23 ± 0.14 | 1 | 0.73 ± 0.29 | 1 |
| A/Wuhan/395/95 | A(H3N2) | Reference | E119V | 5.01 ± 2.18 | 18.5 | 0.19 ± 0.09 | 1 | 0.54 ± 0.17 | 1 |
Susceptibility to the neuraminidase inhibitors oseltamivir and zanamivir was measured by a chemiluminescent assay using the NA-Star kit (Applied Biosystems Inc.). NA inhibition was assayed with equivalent NA enzyme activity and incubated with increasing concentrations of NAI from 0.0316 to 1,000 nM. Curve fitting and the 50% inhibitory concentration were calculated by plotting percent inhibition relative to the NAI concentration using GraphPad Prism 4 software. NA, neuraminidase; NAI, neuraminidase inhibition; IC50, 50% inhibitory concentration; WT, wild type; SD, standard deviation; V, valine; H, histidine; Y, tyrosine; R, arginine; K, lysine. Mean IC50s for wild-type reference control viruses for each type/subtype are in boldface and were used to calculate the fold differences for their respective types/subtypes as indicated. IC50s for reference viruses represent the average taken from at least 5 replicates.
Reference, susceptible and resistant reference viruses used as controls in NAI assays.
The B/Ontario/006876/2011 isolate showed elevated oseltamivir and peramivir IC50s compared with those of the reference wild-type influenza B, wild-type pandemic A(H1N1)pdm09, and wild-type A(H3N2) viruses (Table 1). When comparing the pandemic A(H1N1)pdm09 virus with the oseltamivir resistance-conferring H275Y (N1 numbering) substitution and an influenza A(H3N2) virus with the oseltamivir resistance-conferring E119V substitution, the B/Ontario/006876/2011 B viruses showed intermediate susceptibility (Table 1). The reference influenza B virus carrying the R152K substitution was resistant to all NAIs, compared with the influenza B viruses with H273Y, which is resistant only to oseltamivir and peramivir (Table 1). Strain typing performed at Canada's National Microbiology Laboratory (NML) identified the isolate as a B/Wisconsin/01/2008-like strain. Additionally, H273Y resistance results for oseltamivir and zanamivir were independently confirmed by the NML.
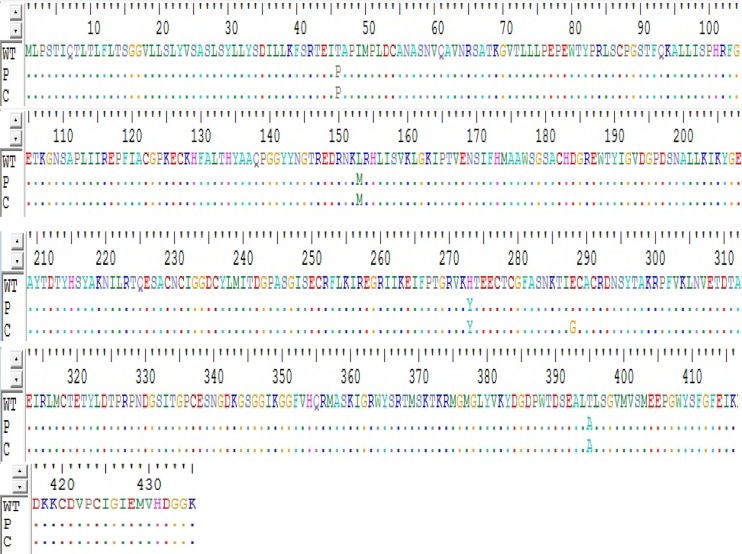
Sequence analysis for the NA gene of B/Ontario/006876/2011 showed a novel substitution for influenza B, present as a change from histidine to tyrosine at position 273 (corresponds to position 275 in N1 and 274 in N2 NA amino acid numbering). A total of 251 influenza B virus isolates from patients (ages 4 months to 92 years) across Ontario that were submitted to Public Health Ontario (PHO) between November 2010 and May 2011 for routine testing and surveillance were screened for susceptibility to the neuraminidase inhibitors oseltamivir and zanamivir. None of these isolates had the H273Y mutation. A substitution of Y for H at position 273 has previously been associated with reduced susceptibility to NAIs in one B virus isolate generated in tissue culture passage 15 and in response to increasing concentrations of peramivir (3, 7, 11, 17). Moreover, reduced susceptibility to oseltamivir has been reported in viruses with variation at the corresponding residue (275, N1 NA numbering) in the pandemic A(H1N1)pdm09 virus (14, 18) and in influenza A(H5N1) (8). Furthermore, because some susceptibility-altering NA mutations have been shown to arise from virus propagation in tissue culture (15), sequencing of the neuraminidase gene was also performed on primary clinical specimens to rule out cell culture selection. The H273Y substitution was identified in the matching primary clinical specimen (Fig. 1). Notably, the presence of the H273Y mutation in the primary clinical specimen, as well as in the matching cultured virus isolates, may indicate a potential selective pressure for this mutation. In comparison with the NA gene of B/Wisconsin/10/2008 (influenza B, accession number ACT20880), four additional nonsynonymous mutations were identified in the NA gene of the newly deposited sequence B/Ontario/006876/2011, T46P (Thr46Pro), L153M (Leu153Met), E288M (Glu288Gly), and T395M (Thr395Met), with E288G appearing only in the first-passage culture and the remaining three mutations appearing in both the first-passage culture and the primary specimen (Fig. 1). In summary, sequencing the neuraminidase gene of the influenza B isolate taken from this patient revealed the presence of the H273Y oseltamivir resistance mutation in both primary and cultured specimens as well as four additional mutations whose phenotypic and genotypic roles in the onset of resistance to NAI are yet to be elucidated (Fig. 1).
Fig 1.
Nucleic acid sequence of the neuraminidase gene from the B/Ontario/006876/2011 virus isolated from matching primary (P) and culture (C) specimens. In comparison to the wild-type (WT) reference control strain (B/Wisconsin/10/2008 ACT20880), position 273 in the wild-type virus contains a histidine (H) residue whereas tyrosine is present at this position in B/Ontario/006876/2011. Note also the genetic alterations at positions 46 (T46P), 153 (L153M), 288 (E288G), and 395 (T395A).
Although the NA change H275Y has been seen among the N1 NA subtype of influenza A (7, 16) and influenza B (3, 17) viruses, such a change has not been directly identified and characterized in influenza B viruses isolated from human patients. Amino acid 273 is known to be a highly conserved residue of the NA enzyme active site in influenza B. To date, all influenza viruses with the H275Y substitution appear to be limited to the N1 type, H1N1 and H5N1. Resistance to NAI in influenza is scored based on two criteria: a high IC50 (that is at least 10-fold greater than the mean) and the presence of a previously described mutation in the NA, arising in drug-treated patients (17). Accordingly, oseltamivir IC50s obtained with the influenza B viruses carrying the H273Y substitution are comparable to those seen with influenza A(H1N1) viruses carrying the oseltamivir resistance-conferring substitution H275Y. The clinical significance of the altered susceptibility associated with H273Y in influenza B viruses is unknown at this time and warrants further investigation. Furthermore, such variants with elevated IC50s highlight the need for establishing a correlation between laboratory-determined IC50s and clinical resistance.
Nucleotide sequence accession number.
The sequence of the NA gene of B/Ontario/006876/2011 was deposited into GenBank under accession no. JN601140.
ACKNOWLEDGMENTS
We thank GlaxoSmithKline (GSK) for funding this study.
We thank Larisa Gubareva and the Molecular Epidemiology Team at the CDC for contributions to this project.
Footnotes
Published ahead of print 25 April 2012
REFERENCES
- 1. Abed Y, Baz M, Boivin G. 2006. Impact of neuraminidase mutations conferring influenza resistance to neuraminidase inhibitors in the N1 and N2 genetic backgrounds. Antivir. Ther. 11:971–976 [PubMed] [Google Scholar]
- 2. Baranovich T, et al. 2010. Emergence of H274Y oseltamivir-resistant A(H1N1) influenza viruses in Japan during the 2008-2009 season. J. Clin. Virol. 47:23–28 [DOI] [PubMed] [Google Scholar]
- 3. Baum EZ, et al. 2003. A point mutation in influenza B confers resistance to peramivir and loss of slow binding. Antiviral Res. 59:13–22 [DOI] [PubMed] [Google Scholar]
- 4. Collins PJ, et al. 2008. Crystal structures of oseltamivir-resistant influenza virus neuraminidase mutants. Nature 453:1258–1262 [DOI] [PubMed] [Google Scholar]
- 5. Colman PM, Hoyne PA, Lawrence MC. 1993. Sequence structure alignment of paramyxovirus hemagglutinin-neuraminidase with influenza virus neuraminidase. J. Virol. 67:2972–2980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dharan NJ, et al. 2009. Infections with oseltamivir-resistant influenza A(H1N1) virus in the United States. JAMA 301:1034–1041 [DOI] [PubMed] [Google Scholar]
- 7. Hatakeyama S, et al. 2007. Emergence of influenza B viruses with reduced sensitivity to neuraminidase inhibitors. JAMA 297:1435–1442 [DOI] [PubMed] [Google Scholar]
- 8. Hurt AC, Holien JK, Barr IG. 2009. In vitro generation of neuraminidase inhibitor resistance in A(H5N1) influenza viruses. Antimicrob. Agents Chemother. 53:4433–4440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Le QM, et al. 2005. Avian flu: isolation of drug-resistant H5N1. Nature 437:1108 (Erratum, 438:754.) [DOI] [PubMed] [Google Scholar]
- 10. Longtin J, et al. 2011. Neuraminidase-inhibitor resistance testing for pandemic influenza A(H1N1) 2009 in Ontario, Canada. J. Clin. Virol. 50:257–261 [DOI] [PubMed] [Google Scholar]
- 11. Monto AS, et al. 2006. Detection of influenza viruses resistant to neuraminidase inhibitors in global surveillance during the first 3 years of their use. Antimicrob. Agents Chemother. 50:2395–2402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Moscona A. 2009. Global transmission of oseltamivir-resistant influenza. N. Engl. J. Med. 360:953–956 [DOI] [PubMed] [Google Scholar]
- 13. MRC National Institute for Medical Research, WHO Influenza Centre London Report prepared for the WHO annual consultation on the composition of influenza vaccine for the Northern Hemisphere, February 2012, September 2011, February 2011, September 2010, and February 2010. Accessed April 2012 http://www.nimr.mrc.ac.uk/who-influenza-centre/annual-and-interim-reports/
- 14. Nguyen HT, Fry AM, Loveless PA, Klimov AI, Gubareva LV. 2010. Recovery of a multidrug-resistant strain of pandemic influenza A 2009 (H1N1) virus carrying a dual H275Y/I223R mutation from a child after prolonged treatment with oseltamivir. Clin. Infect. Dis. 51:983–984 [DOI] [PubMed] [Google Scholar]
- 15. Okomo-Adhiambo M, et al. 2010. Detection of E119V and E119I mutations in influenza A(H3N2) viruses isolated from an immunocompromised patient: challenges in diagnosis of oseltamivir resistance. Antimicrob. Agents Chemother. 54:1834–1841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sheu TG, Deyde VM, Garten RJ, Klimov AI, Gubareva LV. 2010. Detection of antiviral resistance and genetic lineage markers in influenza B virus neuraminidase using pyrosequencing. Antiviral Res. 85:354–360 [DOI] [PubMed] [Google Scholar]
- 17. Sheu TG, et al. 2008. Surveillance for neuraminidase inhibitor resistance among human influenza A and B viruses circulating worldwide from 2004 to 2008. Antimicrob. Agents Chemother. 52:3284–3292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. van der Vries E, Stelma FF, Boucher CAB. 2010. Emergence of a multidrug-resistant pandemic influenza A (H1N1) virus. N. Engl. J. Med. 363:1381–1382 [DOI] [PubMed] [Google Scholar]