Abstract
Cytotoxic CD8+ T cells are major players of anti-tumor immune responses, as their functional activity can limit tumor growth and progression. Data show that cytotoxic T cells efficiently control the proliferation of tumor cells through major histocompatibility complex class I-mediated mechanisms; nevertheless, the presence of tumor-infiltrating CD8+ T cells in lesional tissue does not always correlate with better prognosis and increased survival of cancer patients. Similarly, adoptive transfer of tumor-specific cytotoxic T cells has only shown marginal improvement in life spans of patients with metastatic disease. In this report, we discuss experimental evidence showing that expression of tumor-derived galectins, galectin (Gal)-1, Gal-3 and Gal-9, and concomitant presence of their ligands on the surface of anti-tumor immunocytes directly compromise anti-tumor CD8+ T cell immune responses and, perhaps, undermine the promise of adoptive CD8+ T cell immunotherapy. Furthermore, we describe novel strategies designed to counteract Gal-1-, Gal-3- and Gal-9-mediated effects and highlight their targeting potential for creating more effective anti-tumor immune responses. We believe that Gal and their ligands represent an efficacious targeted molecular paradigm that warrants clinical evaluation.
Keywords: Galectins, Cancer immunotherapy, Carbohydrate therapeutics, Anti-tumor immunity, Glycoimmunology, T cell
Introduction
Galectins are a family of fifteen β-galactoside-binding proteins which regulate the survival, proliferation, and cytokine synthesis of effector helper and cytotoxic T cells [1]. In general, galectins are known by their pro-adhesive potential [2], and their negative effects on T cell proliferation and survival [3, 4]. While virtually all galectins mediate homotypic and heterotypic cell interactions, three galectins in particular have been extensively studied due to their capacity to modulate adaptive immune responses, galectin (Gal)-1, Gal-3 and Gal-9.
Gal-1, Gal-3 and Gal-9 have been considered biomarkers of poor prognosis for a variety of cancer types [5–7], and their influence in promoting tumor immune evasion has recently bolstered efforts to further elucidate how they trigger T cell apoptosis, exhaustion, and cytokine synthesis. Indeed, while cytotoxic CD8+ T cells commonly infiltrate tumors, their effector function, proliferative capacity and cytokine profile often resemble the phenotype of exhausted T cells typically found in chronic viral infections [8]. Exhausted cytotoxic T cells are defined as CD8+ cells that, upon encountering their cognate antigen, fail to proliferate and/or synthesize their effector molecules (IFN-γ, perforin, granzyme B) [9]. Exhausted T cells can be identified by the expression of members of the CD28 family, such as the programmed death-1 (PD-1), and as recently described, by co-expression of the Gal-9 ligand, T cell immunoglobulin mucin-3 (TIM-3) [10]. PD-1 is a surface-bound member of the CD28 family, which upon binding its ligands (PD-L1 and PD-L2), induces immunoregulatory and anergic effects on the immune system [10, 11]. Of note, PD-1 expression chronologically parallels that of Gal-1 during the peak and resolution phases of experimental autoimmune encephalomyelitis (EAE) [12], suggesting a causative relationship between Gal-1 and PD-1 expression. Furthermore, the use of synthetic galectin-binding carbohydrates or blocking antibodies has been shown to restore the effector function of both CD4+ and CD8+ tumor-infiltrating T cells [10, 13], cementing the critical role of galectins as major modifiers of anti-tumor immune responses.
In this review, we describe most current data that address how Gal-1, Gal-3 and Gal-9 dampen effective cytotoxic immune responses in cancer, while describing potential therapeutic strategies to interfere with their lectin-mediated immunomodulatory activity.
The Gal-1 – Gal-1 ligand axis and its influence in tumor immune escape
Gal-1, the prototype S-type lectin, is a ~14 kDa cytokine-like molecule exhibiting a single carbohydrate recognition domain (CRD) [14]. Gal-1, as other members of the galectin family, lacks canonical secretion signal sequences, though can be extruded from a cell via Golgi-independent pathways which are not fully understood [15].Within the cell, Gal-1 is present predominantly in monomeric forms and interacts via protein-protein interactions with nuclear and cytoplasmic elements [16]. However, extracellular Gal-1 forms dimers, which engage with cell surface glycoproteins bearing N-acetyllactosamine (LacNAc) units on N- and O-glycans, which lack terminal α2,6 sialylation [17]. The combination of these glycans moieties presented on distinct membrane protein scaffolds are operationally described as ‘Gal-1 ligands’.
Gal-1 is produced by virtually all hematopoietic lines, where its secretion is significantly enhanced upon activation [18, 19]. Similarly, malignant transformation enhances Gal-1 synthesis, becoming a hallmark biomarker for metastatic potential and poor prognosis in a variety of cancers [20–22]. Numerous Gal-1 ligands have been described on human leukemic T cell lines and on primary T cells (e.g. CD4, CD7, CD43, and CD45), most of them related to the induction of pro-apoptotic activities [18]. In addition, dimeric Gal-1 has been implicated as a factor driving T helper type-2 (Th2) polarization [23], and induction of IL-10+ and FoxP3+ regulatory T cells [24–27].
Gal-1-driven immunoregulation in the cancer microenvironment has been fully documented in several syngeneic murine models of melanomas, lymphomas, and lung carcinomas; where knocking down tumor-derived Gal-1 resulted in significant tumor rejection mediated by higher expression of IFN-γ [22, 28, 29]. Similarly, the immune escape of Hodgkin’s lymphoma has been associated with increased Gal-1 levels that determine a predominant Th2 cytokine signature, accompanied by a greater presence of Tregs [25]. More recently, pancreatic stellate cells and neuroblastoma cells have been shown to be a major source of Gal-1, determining the behavior of these highly malignant neoplasms [30, 31]. Abundant Gal-1 presence in the pancreatic cancer and neuroblastoma microenvironment induces a Th2 cytokine milieu, and prevents effective dendritic cell function and anti-tumor CD4 and CD8-mediated responses, validating Gal-1’s role in the establishment of immune privilege sites in cancer [30].
Gal-3, a Chimeric galectin and its putative role in tumor-infiltrating T cell anergy
Gal-3 is a ~30 kDa multimeric lectin, described in several species with many different names (CBP-35, RL-29, HL-29, hL-31, among others) [32]. Gal-3, a chimera-type galectin, displays a single CRD, and a flexible amino-terminal tail, composed of a collagen-like structure represented by 7–14 repeats of a 9-amino acid sequence [33, 34]. Of note, in comparison with the CRD of other galectins, Gal-3 displays an amino acid sequence (Asp-Trp-Gly-Arg) that resembles that of the anti-apoptotic mitochondrial factor Bcl-2 [35]. Actually, mitochondrial localization of Gal-3 normally correlates with anti-apoptotic effects in T cells, counteracting the pro-apoptotic activity of different death inducers, namely Gal-1 [36].
Gal-3 has numerous intracellular ligands (e.g. synexin [37], Bcl-2 [38], Ras [39], Gemin-4 [40, 41]), mainly regulating cell growth and apoptosis. In addition, when secreted, it can be found in monomeric, homodimeric or even pentamer forms due to special arrangements between components of the poly-amino tail and carbohydrate ligands [42]. Extracellular Gal-3 binds to CD29 and CD7 on activated T cells, inducing apoptosis through caspase-3 activation and cytochrome c release [43, 44]. In fact, loss of CD7 in different leukemias and lymphomas is associated to poor prognosis, which could theoretically impact the expansion of the malignant T cell clone through insensitivity to Gal-1 and Gal-3 [45, 46].
In cancer, Gal-3 is significantly upregulated in patients with metastatic disease [47]. Gal-3 expression correlates with tumor aggressiveness and poor prognosis of colon, thyroid, pancreas, bladder, stomach, kidney and squamous cell carcinomas [48, 49]. Its role as a pro-adhesive factor, regulating interactions between cancer cells and the endothelium via binding proteins of the MUC family has been extensively studied [50]; however, its pro-apoptotic potential and its ability to induce anergic features in activated T cells has made interference of the Gal-3 – Gal-3 ligand axis an attractive approach to promote anti-cancer immune activity.
Indeed, tumor-derived Gal-3 modulates the effector function of cytotoxic T cells, promoting tumor growth in mice, even those mice that have received adoptively-transferred tumor-specific CD8+ T cells [51]. In fact, enhanced Gal-3 expression correlates with lower proliferative capacity and diminished levels of IFN-γ and IL-17 in B16F10 melanoma-bearing mice [52], and higher levels of FoxP3+ regulatory T cells in gliomas [53]. Additionally, Gal-3 has been shown to reduce the affinity of the NK-activating receptor, NKG2D, for the major histocompatibility complex class I-related chain A, which impairs NK cell activation and thereby promotes immune evasion and tumor progression [54].
Gal-9 and its ligand TIM-3 and their role in the exhaustion of anti-tumor cytotoxic T cells
Gal-9 (formerly known as ecalectin) is a ~36 kDa tandem-repeat galectin, with 2 different N- and C-terminal carbohydrate recognition domains connected by a peptide linker region [55]. Gal-9 was originally described as an eosinophil chemoattractant [56, 57], but, more recently, has become a major molecule of interest due to its negative influence in adaptive immune responses. Similar to Gal-1, the expression of this β-galactoside-binding lectin is constitutively expressed by Foxp3+ Tcells [58], and by activated but not naïve Th cells [59]. Gal-9 has been shown to bind N-acetyllactosamine polyvalent repeats similar to other members of the galectin family; where the C-terminal CRD is the major domain for carbohydrate specificity, and the N-terminal CRD and the flexibility conferred by the peptide linker region confer a higher potency [36]. To date, the only Gal-9 ligand fully characterized is TIM-3 [3]. TIM-3 is member of the TIM (T cell immunoglobulin mucin) protein family, a group of Type 1 membrane proteins composed by an extracellular immunoglobulin variable-like domain, a transmembrane domain, and an intracellular tail enriched with tyrosine phosphorylation motifs through which intracellular signaling help regulate T cell activation, tolerance and induction of cell death [9]. While 8 different TIM molecules have been described in mice, only TIM-1, -3 and -4 have been described in humans. TIM-3 is expressed in Th1, Th17 and cytotoxic T cells [8, 60], in addition to NK cells, monocytes, macrophages, dendritic cells and mast cells [9].
Gal-9 – TIM-3 binding interactions inhibit Th17 polarization [61], drive the expansion of FoxP3+ Tregs [61], and induce apoptosis/necrosis activity in pro-inflammatory T cell subsets [3]. In fact, while Gal-1 and Gal-9 induce proapoptotic features in pro-inflammatory T cell subsets, they use significantly different pathways, in which mitochondrial Bcl-2 blocks Gal-9 but not Gal-1-induced apoptosis; and conversely, intracellular Gal-3 inhibits Gal-1 but not Gal-9-driven cell death [36]. In addition to cell death induction, Gal-9 – TIM-3 interactions are strongly associated to decreased synthesis of IFN-γ, and to an exhausted phenotype, as TIM-3 seems to co-localize with PD-1 on the cell surface of CD4 and CD8 T cells [10, 11, 62].
In mice, TIM-3 expression has been reported in tumor-infiltrating CD8+ T cells in syngeneic murine CT26 colon adenocarcinomas, 4T1 mammary adenocarcinomas, B16F10 melanomas, and in carcinogen-induced sarcomas [10, 63]. In humans, TIM-3 expression has been demonstrated in exhausted cytotoxic T cells of patients with advanced melanoma [64] and acute myelogenous leukemia [11], suggesting that the reversal of the anergic phenotype achieved in tumor-bearing mice through the use of neutralizing anti-TIM-3 antibodies, could potentially translate to enhanced immunotherapy in cancer patients.
Targeting galectins and their ligands: the future of cancer immunotherapy
Galectins are largely viewed as negative regulators of tumor immune responses. Due to their immunosuppressive capacity in inflammatory processes and capacity to facilitate immune escape of tumors, there is a growing translational interest in developing effective methods to regulate their influence on cancer and autoimmunity.
To date, certain strategies have shown promise in abrogating galectin-mediated effects. These strategies include: (1) neutralization of galectin-binding via blocking antibodies against galectins [65, 66], (2) competitive inhibition of galectin-binding through synthetic analogs of galectin carbohydrate-binding determinants [67–70], (3) modification of the glycosylation profiles necessary for galectin-binding on anti-tumor immunocytes via fluorinated analogs of glucosamine [27, 71, 72].
Recently, the use of anti-human Gal-1, Gal-9 and TIM-3 neutralizing antibodies has demonstrated their efficacy in blocking Gal-mediated apoptosis of Epstein-Barr virus-specific CD8+ T cells in the context of lymphomas and nasopharyngeal carcinomas [65, 66]. Similarly, although not proven to enhance the survival of anti-tumor immunocytes, an anti-Gal-3 neutralizing antibody decreased ischemia-induced angiogenesis [73].
Alternatively, a number of groups have now shown that competitive inhibition of galectin-binding by the use of synthetic ligands is quite efficacious. Both Stannard et al. and Ito et al., have shown that diminution of Gal-1-driven effects by using the synthetic oligosaccharide, thiodigalactoside (TDG) boosts anti-tumor activity in murine models of cancer [67, 68]. Similarly, treatment with GCS-100, a polysaccharide now in clinical development, dissociates bound Gal-3 on tumor-infiltrating T cells, resulting in heightened effector function and IFN-γ production [13]. Giguere et al. have developed a synthetic, stable dimeric galactosides, which effectively inhibit Gal-1 and/or Gal-3 binding [69]. Likewise, Rabinovich et al. have observed therapeutic efficacy using low molecular weight synthetic lactulose amines to counteract Gal-mediated biological effects [70].
Most recently, we have found that lowering N-acetyllactosamine on N- and O-glycans with a metabolic inhibitor of glycosylation, peracetylated 4-fluorinated analog of glucosamine (4-F-GlcNAc), can effectively abrogate Gal-1 binding to effector T cells, including tumor-specific CD8+ T cells [27, 71, 72]. 4-F-GlcNAc treatment of tumor-bearing mice significantly enhances anti-tumor immunity by increasing the number of anti-tumor T cells, notably tumor antigen-specific CD8+ T cells, which translates into elevated levels of IFN-γ+ CD4+ and CD8+ T cells and lower levels of the immunoregulatory molecule, IL-10, in tumor-draining lymph nodes [27].
Concluding remarks
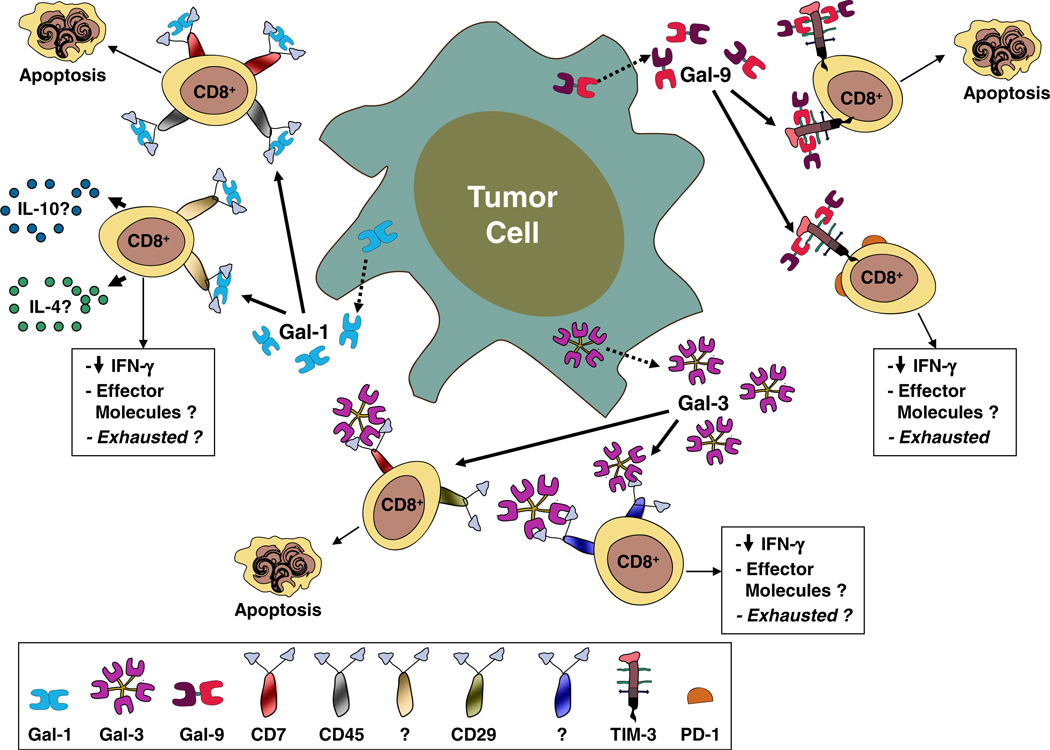
As our understanding of Gal-binding interactions continues to clarify, we are more inspired about the possibility of altering these interactions to bolster or antagonize immune mechanisms necessary for fighting cancer or limiting inflammatory responses. Of the data summarized here, it is becoming increasing clear that Gal-1-, Gal-3- and Gal-9-binding to counter-receptor ligands on effector T cells can alter T cell subset composition, favoring a tolerogenic immune environment for tumor growth and progression (Fig. 1). These Gal-binding interactions are critically involved in cell death induction pathways, stimulating immunoregulatory cytokine synthesis and/or establishment of an exhausted phenotype in tumor-specific CD8+ T cells. Furthermore, data presented on molecular strategies to thwart Gal-binding heighten our enthusiasm that such methods interfering with Gal-binding to anti-tumor T cells can potentially be used as immunotherapeutic approaches to treat cancer in humans. Blocking either arm of the Gal – Gal ligand axis appears to be sufficient for eliciting anti-tumor efficacy and can potentially be used as an adjuvant with current chemotherapeutic treatments. Indeed, agents that interfere with multiple Gal molecules or multiple Gal-binding determinants, such as TDG and 4-F-GlcNAc, could prove to be even more efficacious approach, particularly against tumors capable of producing Gal-1, Gal-3 and/or Gal-9 at high levels. These experimental approaches evoke great promise and warrant forthcoming clinical evaluation in patients with cancer.
Fig. 1.
Role of Gal-1, Gal-3 and Gal-9 in Tumor Immune Escape. This illustration depicts the collaborative relationship between Gal-1, Gal-3 and Gal-9 in controlling effector CD8+ T cell function and promoting a tolerogenic environment for tumor growth. Gal-1 secreted at high levels by certain tumor types can induce apoptosis through binding interactions with CD7 and/or CD45 on the cell surface of effector CD8+ T cells [18, 74, 75]. In a similar manner, Gal-3 and Gal-9 can also induce apoptosis through binding interactions with CD7 and/or CD29 or with TIM-3, respectively [8, 10]. Alternatively, Gal-1 can theoretically trigger the synthesis of IL-10 and Th2 cytokines, whereas Gal-1, Gal-3 and Gal-9 can all suppress IFN-γ production and potentially other, yet to be described, effector cytolytic molecules [3, 12, 23, 25, 76]. These effects ultimately result in an “exhausted” phenotype, resembling the effects of PD-1 – PD-L1-mediated interactions, through binding to ligands that have yet to be fully characterized
Contributor Information
Filiberto Cedeno-Laurent, Department of Dermatology, Brigham and Women’s Hospital, HIM, Rm. 662, 77 Avenue Louis Pasteur, Boston, MA 02115, USA; Harvard Medical School, Boston, MA 02115, USA.
Charles J. Dimitroff, Email: cdimitroff@rics.bwh.harvard.edu, Department of Dermatology, Brigham and Women’s Hospital, HIM, Rm. 662, 77 Avenue Louis Pasteur, Boston, MA 02115, USA; Harvard Medical School, Boston, MA 02115, USA.
References
- 1.Liu FT, Rabinovich GA. Galectins as modulators of tumour progression. Nat. Rev. 2005;1:29–41. doi: 10.1038/nrc1527. [DOI] [PubMed] [Google Scholar]
- 2.Camby I, Le Mercier M, Lefranc F, Kiss R. Galectin-1: a small protein with major functions. Glycobiology. 2006;11:137R–157R. doi: 10.1093/glycob/cwl025. [DOI] [PubMed] [Google Scholar]
- 3.Zhu C, Anderson AC, Schubart A, Xiong H, Imitola J, Khoury SJ, Zheng XX, Strom TB, Kuchroo VK. The Tim-3 ligand galectin-9 negatively regulates T helper type 1 immunity. Nat. Immunol. 2005;12:1245–1252. doi: 10.1038/ni1271. [DOI] [PubMed] [Google Scholar]
- 4.Dhirapong A, Lleo A, Leung P, Gershwin ME, Liu FT. The immunological potential of galectin-1 and -3. Autoimmun. Rev. 2009;5:360–363. doi: 10.1016/j.autrev.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 5.Saussez S, Glinoer D, Chantrain G, Pattou F, Carnaille B, Andre S, Gabius HJ, Laurent G. Serum galectin-1 and galectin-3 levels in benign and malignant nodular thyroid disease. Thyroid. 2008;7:705–712. doi: 10.1089/thy.2007.0361. [DOI] [PubMed] [Google Scholar]
- 6.Szoke T, Kayser K, Baumhakel JD, Trojan I, Furak J, Tiszlavicz L, Horvath A, Szluha K, Gabius HJ, Andre S. Prognostic significance of endogenous adhesion/growth-regulatory lectins in lung cancer. Oncology. 2005;2:167–174. doi: 10.1159/000087841. [DOI] [PubMed] [Google Scholar]
- 7.Liang MY, Lu YM, Zhang Y, Zhang SL. Serum galectin-9 in cervical cancer. Zhonghua yi xue za zhi. 2008;39:2783–2785. [PubMed] [Google Scholar]
- 8.Zhu C, Anderson AC, Kuchroo VK. TIM-3 and its regulatory role in immune responses. Current topics in microbiology and immunology. :1–15. doi: 10.1007/82_2010_84. [DOI] [PubMed] [Google Scholar]
- 9.Rodriguez-Manzanet R, DeKruyff R, Kuchroo VK, Umetsu DT. The costimulatory role of TIM molecules. Immunol. Rev. 2009;1:259–270. doi: 10.1111/j.1600-065X.2009.00772.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sakuishi K, Apetoh L, Sullivan JM, Blazar BR, Kuchroo VK, Anderson AC. Targeting Tim-3 and PD-1 pathways to reverse T cell exhaustion and restore anti-tumor immunity. J. Exp. Med. 2010;10:2187–2194. doi: 10.1084/jem.20100643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhou Q, Munger ME, Veenstra RG, Weigel BJ, Hirashima M, Munn DH, Murphy WJ, Azuma M, Anderson AC, Kuchroo VK, et al. Coexpression of Tim-3 and PD-1 identifies a CD8+ T-cell exhaustion phenotype in mice with disseminated acute myelogenous leukemia. Blood. 2011;17:4501–4510. doi: 10.1182/blood-2010-10-310425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ilarregui JM, Croci DO, Bianco GA, Toscano MA, Salatino M, Vermeulen ME, Geffner JR, Rabinovich GA. Tolerogenic signals delivered by dendritic cells to T cells through a galectin-1-driven immunoregulatory circuit involving interleukin 27 and interleukin 10. Nat. Immunol. 2009;9:981–991. doi: 10.1038/ni.1772. [DOI] [PubMed] [Google Scholar]
- 13.Demotte N, Wieers G, Van Der Smissen P, Moser M, Schmidt C, Thielemans K, Squifflet JL, Weynand B, Carrasco J, Lurquin C, et al. A galectin-3 ligand corrects the impaired function of human CD4 and CD8 tumor-infiltrating lymphocytes and favors tumor rejection in mice. Cancer Res. 2010;19:7476–7488. doi: 10.1158/0008-5472.CAN-10-0761. [DOI] [PubMed] [Google Scholar]
- 14.Lopez-Lucendo MF, Solis D, Andre S, Hirabayashi J, Kasai K, Kaltner H, Gabius HJ, Romero A. Growth-regulatory human galectin-1: crystallographic characterisation of the structural changes induced by single-site mutations and their impact on the thermodynamics of ligand binding. J. Mol. Biol. 2004;4:957–970. doi: 10.1016/j.jmb.2004.08.078. [DOI] [PubMed] [Google Scholar]
- 15.Nickel W. Unconventional secretory routes: direct protein export across the plasma membrane of mammalian cells. Traffic. 2005;8:607–614. doi: 10.1111/j.1600-0854.2005.00302.x. [DOI] [PubMed] [Google Scholar]
- 16.Paz A, Haklai R, Elad-Sfadia G, Ballan E, Kloog Y. Galectin-1 binds oncogenic H-Ras to mediate Ras membrane anchorage and cell transformation. Oncogene. 2001;51:7486–7493. doi: 10.1038/sj.onc.1204950. [DOI] [PubMed] [Google Scholar]
- 17.Leppanen A, Stowell S, Blixt O, Cummings RD. Dimeric galectin-1 binds with high affinity to alpha2,3-sialylated and non-sialylated terminal N-acetyllactosamine units on surface-bound extended glycans. J. Biol. Chem. 2005;7:5549–5562. doi: 10.1074/jbc.M412019200. [DOI] [PubMed] [Google Scholar]
- 18.Perillo NL, Pace KE, Seilhamer JJ, Baum LG. Apoptosis of T cells mediated by galectin-1. Nature. 1995;6558:736–739. doi: 10.1038/378736a0. [DOI] [PubMed] [Google Scholar]
- 19.Cedeno-Laurent F, Dimitroff CJ. Galectin-1 research in T cell immunity: past, present and future. Clin. Immunol. 2012;2:107–116. doi: 10.1016/j.clim.2011.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jung EJ, Moon HG, Cho BI, Jeong CY, Joo YT, Lee YJ, Hong SC, Choi SK, Ha WS, Kim JW, et al. Galectin-1 expression in cancer-associated stromal cells correlates tumor invasiveness and tumor progression in breast cancer. Int. J. Cancer. 2007;11:2331–2338. doi: 10.1002/ijc.22434. [DOI] [PubMed] [Google Scholar]
- 21.Nagy N, Legendre H, Engels O, Andre S, Kaltner H, Wasano K, Zick Y, Pector JC, Decaestecker C, Gabius HJ, et al. Refined prognostic evaluation in colon carcinoma using immunohistochemical galectin fingerprinting. Cancer. 2003;8:1849–1858. doi: 10.1002/cncr.11268. [DOI] [PubMed] [Google Scholar]
- 22.Rubinstein N, Alvarez M, Zwirner NW, Toscano MA, Ilarregui JM, Bravo A, Mordoh J, Fainboim L, Podhajcer OL, Rabinovich GA. Targeted inhibition of galectin-1 gene expression in tumor cells results in heightened T cell-mediated rejection; A potential mechanism of tumor-immune privilege. Cancer Cell. 2004;3:241–251. doi: 10.1016/s1535-6108(04)00024-8. [DOI] [PubMed] [Google Scholar]
- 23.Motran CC, Molinder KM, Liu SD, Poirier F, Miceli MC. Galectin-1 functions as a Th2 cytokine that selectively induces Th1 apoptosis and promotes Th2 function. Eur. J. Immunol. 2008;11:3015–3027. doi: 10.1002/eji.200838295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van der Leij J, van den Berg A, Harms G, Eschbach H, Vos H, Zwiers P, van Weeghel R, Groen H, Poppema S, Visser L. Strongly enhanced IL-10 production using stable galectin-1 homodimers. Mol. Immunol. 2007;4:506–513. doi: 10.1016/j.molimm.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 25.Juszczynski P, Ouyang J, Monti S, Rodig SJ, Takeyama K, Abramson J, Chen W, Kutok JL, Rabinovich GA, Shipp MA. The AP1-dependent secretion of galectin-1 by Reed Sternberg cells fosters immune privilege in classical Hodgkin lymphoma. Proc. Natl. Acad. Sci. U. S. A. 2007;32:13134–13139. doi: 10.1073/pnas.0706017104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cedeno-Laurent F, Opperman M, Barthel SR, Kuchroo VK, Dimitroff CJ. Galectin-1 triggers an immunoregulatory signature in Th cells functionally defined by IL-10 expression. J. Immunol. 2012;7:3127–3137. doi: 10.4049/jimmunol.1103433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cedeno-Laurent F, Opperman MJ, Barthel SR, Hays D, Schatton T, Zhan Q, He X, Matta KL, Supko JG, Frank MH, et al. Metabolic inhibition of galectin-1-binding carbohydrates accentuates antitumor immunity. J. Investig. Dermatol. 2012;2:410–420. doi: 10.1038/jid.2011.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zacarias Fluck MF, Hess L, Salatino M, Croci DO, Stupirski JC, Di Masso RJ, Roggero E, Rabinovich GA, Scharovsky OG. The aggressiveness of murine lymphomas selected in vivo by growth rate correlates with galectin-1 expression and response to cyclophosphamide. Cancer Immunol. Immunother. 2011 doi: 10.1007/s00262-011-1114-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Banh A, Zhang J, Cao H, Bouley DM, Kwok S, Kong C, Giaccia AJ, Koong AC, Le QT. Tumor Galectin-1 Mediates Tumor Growth and Metastasis through Regulation of T-Cell Apoptosis. Cancer Res. 2011;13:4423–4431. doi: 10.1158/0008-5472.CAN-10-4157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tang D, Yuan Z, Xue X, Lu Z, Zhang Y, Wang H, Chen M, An Y, Wei J, Zhu Y, et al. High expression of Galectin-1 in pancreatic stellate cells plays a role in the development and ma1intenance of an immunosuppressive microenvironment in pancreatic cancer. International journal of cancer. 2011 doi: 10.1002/ijc.26290. [DOI] [PubMed] [Google Scholar]
- 31.Soldati R, Berger E, Zenclussen AC, Jorch G, Lode HN, Salatino M, Rabinovich GA, Fest S. Neuroblastoma triggers an immunoevasive program involving galectin-1-dependent modulation of T cell and dendritic cell compartments. Int. J. Cancer. 2011 doi: 10.1002/ijc.26498. [DOI] [PubMed] [Google Scholar]
- 32.Dumic J, Dabelic S, Flogel M. Galectin-3: an open-ended story. Biochim. Biophys. Acta. 2006;4:616–635. doi: 10.1016/j.bbagen.2005.12.020. [DOI] [PubMed] [Google Scholar]
- 33.Raz A, Pazerini G, Carmi P. Identification of the metastasis-associated, galactoside-binding lectin as a chimeric gene product with homology to an IgE-binding protein. Cancer Res. 1989;13:3489–3493. [PubMed] [Google Scholar]
- 34.Varki A, Cummings R, Esko JD. Essentials of Glycobiology. 2nd edn. New York: Cold Spring Harbor Laboratory Press; 2009. [PubMed] [Google Scholar]
- 35.Akahani S, Nangia-Makker P, Inohara H, Kim HR, Raz A. Galectin-3: a novel antiapoptotic molecule with a functional BH1 (NWGR) domain of Bcl-2 family. Cancer Res. 1997;23:5272–5276. [PubMed] [Google Scholar]
- 36.Bi S, Earl LA, Jacobs L, Baum LG. Structural features of galectin-9 and galectin-1 that determine distinct T cell death pathways. J. Biol. Chem. 2008;18:12248–12258. doi: 10.1074/jbc.M800523200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yu F, Finley RL, Jr, Raz A, Kim HR. Galectin-3 translocates to the perinuclear membranes and inhibits cytochrome c release from the mitochondria. A role for synexin in galectin-3 translocation. J. Biol. Chem. 2002;18:15819–15827. doi: 10.1074/jbc.M200154200. [DOI] [PubMed] [Google Scholar]
- 38.Yang RY, Hsu DK, Liu FT. Expression of galectin-3 modulates T-cell growth and apoptosis. Proc. Natl. Acad. Sci. U. S. A. 1996;13:6737–6742. doi: 10.1073/pnas.93.13.6737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Elad-Sfadia G, Haklai R, Balan E, Kloog Y. Galectin-3 augments K-Ras activation and triggers a Ras signal that attenuates ERK but not phosphoinositide 3-kinase activity. J. Biol. Chem. 2004;33:34922–34930. doi: 10.1074/jbc.M312697200. [DOI] [PubMed] [Google Scholar]
- 40.Davidson PJ, Davis MJ, Patterson RJ, Ripoche MA, Poirier F, Wang JL. Shuttling of galectin-3 between the nucleus and cytoplasm. Glycobiology. 2002;5:329–337. doi: 10.1093/glycob/12.5.329. [DOI] [PubMed] [Google Scholar]
- 41.Park JW, Voss PG, Grabski S, Wang JL, Patterson RJ. Association of galectin-1 and galectin-3 with Gemin4 in complexes containing the SMN protein. Nucleic Acids Res. 2001;17:3595–3602. doi: 10.1093/nar/29.17.3595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Morris S, Ahmad N, Andre S, Kaltner H, Gabius HJ, Brenowitz M, Brewer F. Quaternary solution structures of galectins-1, -3, and −7. Glycobiology. 2004;3:293–300. doi: 10.1093/glycob/cwh029. [DOI] [PubMed] [Google Scholar]
- 43.Fukumori T, Takenaka Y, Yoshii T, Kim HR, Hogan V, Inohara H, Kagawa S, Raz A. CD29 and CD7 mediate galectin-3-induced type II T-cell apoptosis. Cancer Res. 2003;23:8302–8311. [PubMed] [Google Scholar]
- 44.Stillman BN, Hsu DK, Pang M, Brewer CF, Johnson P, Liu FT, Baum LG. Galectin-3 and galectin-1 bind distinct cell surface glycoprotein receptors to induce T cell death. J. Immunol. 2006;2:778–789. doi: 10.4049/jimmunol.176.2.778. [DOI] [PubMed] [Google Scholar]
- 45.Liu TY, Chen CY, Tien HF, Lin CW. Loss of CD7, independent of galectin-3 expression, implies a worse prognosis in adult T-cell leukaemia/lymphoma. Histopathology. 2009;2:214–220. doi: 10.1111/j.1365-2559.2008.03199.x. [DOI] [PubMed] [Google Scholar]
- 46.Rappl G, Abken H, Muche JM, Sterry W, Tilgen W, Andre S, Kaltner H, Ugurel S, Gabius HJ, Reinhold U. CD4+CD7-leukemic T cells from patients with Sezary syndrome are protected from galectin-1-triggered T cell death. Leukemia. 2002;5:840–845. doi: 10.1038/sj.leu.2402438. [DOI] [PubMed] [Google Scholar]
- 47.Iurisci I, Tinari N, Natoli C, Angelucci D, Cianchetti E, Iacobelli S. Concentrations of galectin-3 in the sera of normal controls and cancer patients. Clin. Cancer Res. 2000;4:1389–1393. [PubMed] [Google Scholar]
- 48.van den Brule F, Califice S, Castronovo V. Expression of galectins in cancer: a critical review. Glycoconj J. 2004;7–9:537–542. doi: 10.1023/B:GLYC.0000014083.48508.6a. [DOI] [PubMed] [Google Scholar]
- 49.Newlaczyl AU, Yu LG. Galectin-3 - A jack-of-all-trades in cancer. Cancer Lett. 2011;2:123–128. doi: 10.1016/j.canlet.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 50.Byrd JC, Bresalier RS. Mucins and mucin binding proteins in colorectal cancer. Cancer Metastasis Rev. 2004;1–2:77–99. doi: 10.1023/a:1025815113599. [DOI] [PubMed] [Google Scholar]
- 51.Peng W, Wang HY, Miyahara Y, Peng G, Wang RF. Tumor-associated galectin-3 modulates the function of tumor-reactive T cells. Cancer Res. 2008;17:7228–7236. doi: 10.1158/0008-5472.CAN-08-1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Radosavljevic G, Jovanovic I, Majstorovic I, Mitrovic M, Lisnic VJ, Arsenijevic N, Jonjic S, Lukic ML. Deletion of galectin-3 in the host attenuates metastasis of murine melanoma by modulating tumor adhesion and NK cell activity. Clin. Exp. Metastasis. 2011;5:451–462. doi: 10.1007/s10585-011-9383-y. [DOI] [PubMed] [Google Scholar]
- 53.Wei J, Barr J, Kong LY, Wang Y, Wu A, Sharma AK, Gumin J, Henry V, Colman H, Sawaya R, et al. Glioma-associated cancer-initiating cells induce immunosuppression. Clin. Cancer Res. 2010;2:461–473. doi: 10.1158/1078-0432.CCR-09-1983. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 54.Tsuboi S, Sutoh M, Hatakeyama S, Hiraoka N, Habuchi T, Horikawa Y, Hashimoto Y, Yoneyama T, Mori K, Koie T, et al. A novel strategy for evasion of NK cell immunity by tumours expressing core2 O-glycans. EMBO J. 2011;15:3173–3185. doi: 10.1038/emboj.2011.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dunphy JL, Barcham GJ, Bischof RJ, Young AR, Nash A, Meeusen EN. Isolation and characterization of a novel eosinophil-specific galectin released into the lungs in response to allergen challenge. J. Biol. Chem. 2002;17:14916–14924. doi: 10.1074/jbc.M200214200. [DOI] [PubMed] [Google Scholar]
- 56.Matsumoto R, Matsumoto H, Seki M, Hata M, Asano Y, Kanegasaki S, Stevens RL, Hirashima M. Human ecalectin, a variant of human galectin-9, is a novel eosinophil chemoattractant produced by T lymphocytes. J. Biol. Chem. 1998;27:16976–16984. doi: 10.1074/jbc.273.27.16976. [DOI] [PubMed] [Google Scholar]
- 57.Hirashima M. Ecalectin/galectin-9, a novel eosinophil chemoattractant: its function and production. Int. Arch Allergy Immunol. 2000:6–9. doi: 10.1159/000053623. [DOI] [PubMed] [Google Scholar]
- 58.Elahi S, Dinges WL, Lejarcegui N, Laing KJ, Collier AC, Koelle DM, McElrath MJ, Horton H. Protective HIV-specific CD8+ T cells evade Treg cell suppression. Nat. Med. 8:989–995. doi: 10.1038/nm.2422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Imaizumi T, Kumagai M, Sasaki N, Kurotaki H, Mori F, Seki M, Nishi N, Fujimoto K, Tanji K, Shibata T, et al. Interferon-gamma stimulates the expression of galectin-9 in cultured human endothelial cells. J. Leukoc. Biol. 2002;3:486–491. [PubMed] [Google Scholar]
- 60.Oikawa T, Kamimura Y, Akiba H, Yagita H, Okumura K, Takahashi H, Zeniya M, Tajiri H, Azuma M. Preferential involvement of Tim-3 in the regulation of hepatic CD8+ T cells in murine acute graft-versus-host disease. J. Immunol. 2006;7:4281–4287. doi: 10.4049/jimmunol.177.7.4281. [DOI] [PubMed] [Google Scholar]
- 61.Seki M, Oomizu S, Sakata KM, Sakata A, Arikawa T, Watanabe K, Ito K, Takeshita K, Niki T, Saita N, et al. Galectin-9 suppresses the generation of Th17, promotes the induction of regulatory T cells, and regulates experimental autoimmune arthritis. Clinical immunology (Orlando, Fla. 2008;1:78–88. doi: 10.1016/j.clim.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 62.McMahan RH, Golden-Mason L, Nishimura MI, McMahon BJ, Kemper M, Allen TM, Gretch DR, Rosen HR. Tim-3 expression on PD-1+ HCV-specific human CTLs is associated with viral persistence, and its blockade restores hepatocyte-directed in vitro cytotoxicity. J. Clin. Investigation. 12:4546–4557. doi: 10.1172/JCI43127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ngiow SF, von Scheidt B, Akiba H, Yagita H, Teng MW, Smyth MJ. Anti-TIM3 antibody promotes T cell IFN-gamma-mediated antitumor immunity and suppresses established tumors. Cancer Res. 10:3540–3551. doi: 10.1158/0008-5472.CAN-11-0096. [DOI] [PubMed] [Google Scholar]
- 64.Fourcade J, Sun Z, Benallaoua M, Guillaume P, Luescher IF, Sander C, Kirkwood M, Kuchroo V, Zarour HM. Upregulation of Tim-3 and PD-1 expression is associated with tumor antigen-specific CD8+ T cell dysfunction in melanoma patients. J. Exp. Med. 10:2175–2186. doi: 10.1084/jem.20100637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ouyang J, Juszczynski P, Rodig SJ, Green MR, O’Donnell E, Currie T, Armant M, Takeyama K, Monti S, Rabinovich GA, et al. Viral induction and targeted inhibition of galectin-1 in EB1V+posttransplant lymphoproliferative disorders. Blood. 2011;16:4315–4322. doi: 10.1182/blood-2010-11-320481. [DOI] [PubMed] [Google Scholar]
- 66.Klibi J, Niki T, Riedel A, Pioche-Durieu C, Souquere S, Rubinstein E, Le Moulec S, Guigay J, Hirashima M, Guemira F, et al. Blood diffusion and Th1-suppressive effects of galectin-9-containing exosomes released by Epstein-Barr virus-infected nasopharyngeal carcinoma cells. Blood. 2009;9:1957–1966. doi: 10.1182/blood-2008-02-142596. [DOI] [PubMed] [Google Scholar]
- 67.Stannard KA, Collins PM, Ito K, Sullivan EM, Scott SA, Gabutero E, Darren Grice I, Low P, Nilsson UJ, Leffler H, et al. Galectin inhibitory disaccharides promote tumour immunity in a breast cancer model. Cancer Lett. 2010;2:95–110. doi: 10.1016/j.canlet.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 68.Ito K, Scott SA, Cutler S, Dong LF, Neuzil J, Blanchard H, Ralph SJ. Thiodigalactoside inhibits murine cancers by concurrently blocking effects of galectin-1 on immune dysregulation, angiogenesis and protection against oxidative stress. Angiogenesis. 2011 doi: 10.1007/s10456-011-9213-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Giguere D, Bonin MA, Cloutier P, Patnam R, St-Pierre C, Sato S, Roy R. Synthesis of stable and selective inhibitors of human galectins-1 and −3. Bioorg. Med. Chem. 2008;16:7811–7823. doi: 10.1016/j.bmc.2008.06.044. [DOI] [PubMed] [Google Scholar]
- 70.Rabinovich GA, Cumashi A, Bianco GA, Ciavardelli D, Iurisci I, D’Egidio M, Piccolo E, Tinari N, Nifantiev N, Iacobelli S. Synthetic lactulose amines: novel class of anticancer agents that induce tumor-cell apoptosis and inhibit galectin-mediated homotypic cell aggregation and endothelial cell morphogenesis. Glycobiology. 2006;3:210–220. doi: 10.1093/glycob/cwj056. [DOI] [PubMed] [Google Scholar]
- 71.Barthel SR, Antonopoulos A, Cedeno-Laurent F, Schaffer L, Hernandez G, Patil SA, North SJ, Dell A, Matta KL, Neelamegham S, et al. Peracetylated 4-fluoro-glucosamine reduces the content and repertoire of N- and O-glycans without direct incorporation. J. Biol. Chem. 2011;24:21717–21731. doi: 10.1074/jbc.M110.194597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Woynarowska B, Skrincosky DM, Haag A, Sharma M, Matta K, Bernacki RJ. Inhibition of lectin-mediated ovarian tumor cell adhesion by sugar analogs. J. Biol. Chem. 1994;36:22797–22803. [PubMed] [Google Scholar]
- 73.Yan YP, Lang BT, Vemuganti R, Dempsey RJ. Galectin-3 mediates post-ischemic tissue remodeling. Brain research. 2009:116–124. doi: 10.1016/j.brainres.2009.06.073. [DOI] [PubMed] [Google Scholar]
- 74.Pace KE, Hahn HP, Pang M, Nguyen JT, Baum LG. CD7 delivers a pro-apoptotic signal during galectin-1-induced T cell death. J. Immunol. 2000;5:2331–2334. doi: 10.4049/jimmunol.165.5.2331. [DOI] [PubMed] [Google Scholar]
- 75.Amano M, Galvan M, He J, Baum LG. The ST6Gal I sialyltransferase selectively modifies N-glycans on CD45 to negatively regulate galectin-1-induced CD45 clustering, phosphatase modulation, and T cell death. J. Biol. Chem. 2003;9:7469–7475. doi: 10.1074/jbc.M209595200. [DOI] [PubMed] [Google Scholar]
- 76.Stowell SR, Qian Y, Karmakar S, Koyama NS, Dias-Baruffi M, Leffler H, McEver RP, Cummings RD. Differential roles of galectin-1 and galectin-3 in regulating leukocyte viability and cytokine secretion. J. Immunol. 2008;5:3091–3102. doi: 10.4049/jimmunol.180.5.3091. [DOI] [PubMed] [Google Scholar]