Abstract
Rheumatoid arthritis (RA) is an autoimmune synovitis characterized by the presence of anticitrullinated protein Abs, although the exact targets and role of anticitrullinated protein autoimmunity in the pathogenesis of RA remain to be defined. Fibrinogen, which can be citrullinated, has recently emerged as a candidate autoantigen. To determine whether autoimmunity against fibrinogen can mediate inflammatory arthritis, we immunized a variety of common mouse strains with fibrinogen and found that DBA/1 and SJL mice developed an inflammatory and erosive arthritis. Mice with fibrinogen-induced arthritis (FIA) possess fibrinogen-reactive T cells that produce the proinflammatory cytokines IL-6, IL-17, TNF-α, and IFN-γ. FIA can be adoptively transferred with either plasma or fibrinogen-specific T cells from diseased mice. Mice with FIA possess rheumatoid factor, circulating immune complexes, and anticyclic citrullinated peptide Abs, all of which are characteristic of human RA. These observations demonstrate that fibrinogen is arthritogenic in mice and that the pathogenesis of FIA is mediated by both autoantibodies and fibrinogen-reactive T cells.
Rheumatoid arthritis (RA), a chronic inflammatory disease of the synovial joints, afflicts up to 1.0% of the adult population worldwide, yet our understanding of the cause and pathogenesis of RA remains limited (1). In RA, synovial inflammation results in the growth of the synovial lining to form pannus tissue, which contributes to cartilage and joint destruction. Both genetic and environmental factors are associated with RA; for instance, individuals who both smoke and possess the HLA-DR4+ shared epitope have an increased risk of having RA develop (2). RA is characterized by the production of autoantibodies, including rheumatoid factor (RF) (IgM Ab against the Fc portion of IgG) and anticitrullinated protein Abs (ACPAs) that react with citrulline-containing proteins, such as perinuclear factor, vimentin, filaggrin, and fibrinogen (1, 3, 4). Citrullination (also known as deimination) is the posttranslational conversion of peptidyl-arginine to peptidyl-citrulline by peptidyl arginine deiminase (PAD) enzymes. Abs against cyclic citrullinated peptides (CCP) and RF can predate RA by years (5), and provide a sensitivity of ~70% and a specificity of 97% for the diagnosis of RA (6–9). More recently, Abs against in vitro citrullinated fibrinogen were reported to provide a sensitivity and specificity comparable to that of anti-CCP Abs for the diagnosis of RA (10–12).
Growing evidence suggests that fibrin and its precursor fibrinogen may play a role in the pathogenesis of RA. RA is characterized by the deposition and excessive, local generation of fibrin in the inflamed joint (13). The accumulation of fibrin in the arthritic joint is thought to arise because of a local imbalance between coagulation and fibrinolysis (14). The citrulline-modified α- and β-chains of fibrin were identified as targets of RA-specific anti-CCP autoantibodies, the most specific serological markers of RA (10). In addition, a positive correlation between the presence of anti-in vitro citrullinated fibrinogen Abs and the presence of anti-CCP Abs was reported (15–18). The reactivity of autoantibodies to in vitro citrullinated fibrinogen correlates with their reactivity to CCP and provides a high specificity for the diagnosis of RA (10, 15).
Mice with type II collagen (CII)-induced arthritis (CIA) develop Abs against both CCPs and in vitro citrullinated fibrinogen, and the transfer of an anticitrullinated fibrinogen monoclonal Ab worsened the mild arthritis induced by anti-CII Ab transfer (19). These findings indicate that Abs against citrullinated fibrinogen can exacerbate arthritis induced by a distinct autoantigen. To investigate a potential role for fibrinogen as a central autoantigen in the pathogenesis of RA, we developed a fibrinogen-induced arthritis (FIA) mouse model using human fibrinogen, which naturally contains several citrulline modifications, as the immunizing Ag. Our data suggest that FIA is a T cell and autoantibody-mediated autoimmune synovitis that is highly representative of the subset of RA patients who possess anticitrullinated fibrinogen autoantibodies.
Materials and Methods
Mice
Male DBA1/J mice and female SJL/J, BALB/c, and C57BL/6 mice were obtained from The Jackson Laboratory (Bar Harbor, ME) and were between 7 and 9 wk of age when the experiments were initiated. Adoptive transfer recipients were between 5 and 7 wk of age. All animal protocols were approved by the Committee of Animal Research at Stanford University, in accordance with the National Institutes of Health guidelines.
Arthritis induction
FIA induction
Mice were immunized s.c. with 0.2 mg human fibrinogen, which contains citrulline modifications, (Sigma-Aldrich, St. Louis, MO, or Calbiochem, Gibbstown, NJ) in PBS (without calcium or magnesium) emulsified with an equal volume of CFA consisting of IFA (Sigma-Aldrich) and 0.5 mg heat-inactivated Mycobacterium tuberculosis (strain H37 RA; Difco Laboratories, Detroit, MI). Twenty-one days later, the mice were boosted s.c. with a second injection of human fibrinogen in IFA.
CIA induction
Mice were immunized intradermally at the tail base with 0.2 mg bovine CII in 0.05 M acetic acid (immunization grade, Chondrex, Redmond, WA) emulsified with an equal volume of CFA. Twenty-one days later, the mice were boosted s.c. at the base of the tail with a second injection of bovine CII in IFA.
FIA-CIA induction
Mice were immunized s.c. to induce FIA and intradermally to induce CIA, as described previously, and boosted 21 d later with fibrinogen emulsified in IFA as described previously. Control mice were given the equivalent amount of CFA and IFA at the corresponding sites of injection.
Adoptive transfer of FIA
For T cell transfer, whole splenocytes and lymphocytes from mice with FIA were cultured in vitro for 72 h with 0.01 mg/ml fibrinogen. Cells were harvested and washed with PBS. CD3+ T cells were isolated using CD3+ T cell enrichment columns (R&D Systems, Minneapolis, MN). Fifty million T cells were injected i.v. into naive recipients. For plasma transfer, 0.3 ml pooled plasma from mice with FIA was injected i.v. on days 0 and 2 into naive recipients.
Animals were scored every 2–3 d for arthritis by using the following scale: grade 0, no erythema or swelling; grade 1, erythema and mild swelling extending from the ankle to the mid paw; grade 2, erythema and moderate swelling extending from the ankle to the metatarsal joint; grade 3, erythema and severe swelling encompassing the ankle, paw, and digits. Each paw was graded and the four scores totaled such that the maximal possible score per mouse was 12.
Proliferation assay
The 5 × 105 bulk splenocytes were cultured in 96-well microtiter plates and stimulated with 0.01 mg/ml human fibrinogen in triplicate wells for 72 h. Enriched tissue culture media consisted of RPMI 1640 supplemented with HEPES buffer (25 mM), L-glutamine (2 mM), sodium pyruvate (1 mM), nonessential amino acids (0.1 mM), penicillin (100 U/ml), streptomycin (0.1 mg/ml), 2-mercaptoethanol (5 × 10−5 M), and 10% FBS. Cells were pulsed with 1 μCi [3H]TdR (GE Healthcare Bio-Sciences, Piscataway, NJ) for the final 16 h of culture, and incorporated radioactivity measured by using a betaplate scintillation counter.
Cytokine analysis
Bulk splenocytes were incubated in enriched RPMI-1640 and 0.01 mg/ml human fibrinogen. After 72 h of culture, the supernatants were collected and assayed in triplicate for levels of IL-6, IL-17, IFN-γ, and TNF-α by using commercial ELISA kits (BD Pharmingen, San Diego, CA, and eBio-science, San Diego, CA).
Ab detection
The levels of autoantibodies to fibrinogen or in vitro citrullinated fibrinogen were determined by ELISA. In brief, ELISA plates (Nunc Maxisorp, Thermo Fisher Scientific, Rochester, NY) were coated with 0.01 mg/ml fibrinogen or in vitro citrullinated fibrinogen in 1 × PBS (no calcium or magnesium) overnight at 4°C. Plates were blocked with PBS, 0.05% Tween 20, and 3% FBS for 1 h at room temperature. Plasma samples were diluted 1:100 and incubated in duplicate wells for 2 h at room temperature. HRP-conjugated goat anti-mouse secondary Abs specific for IgG, IgG1, and IgG2a (Southern Biotechnology Associates, Birmingham, AL) were diluted 1:5000 and incubated for 1 h at room temperature. Tetramethylbenzidine substrate was added for 30 min and OD values determined at 450 nm. Average absorbance from blank wells (no plasma added) was subtracted.
Detection of immune complexes, anti-CCP Abs, and RF
ELISA plates were coated with 0.02 mg/ml C1q (Sigma-Aldrich) in PBS overnight at 4°C. Subsequent incubations and washes were performed at room temperature. The plates were blocked with PBS, 0.05% Tween 20, and 3% BSA for 1 h. After washing, plasma from immunized or naive mice was diluted 1:50 and incubated on a shaker for 1.5 h. Immune complexes (ICs) were detected with HRP-conjugated rabbit antiserum specific for mouse IgG (Jackson ImmunoResearch Laboratories, West Grove, PA).
Quanta Lite CCP3 IgG ELISA (Inova Diagnostics, San Diego, CA) and mouse RF Igs (total IgG) ELISA (Alpha Diagnostic International, San Antonio, TX) were performed according to the manufacturer’s protocol (plasma diluted 1:100), except that the secondary Abs used were HRP-conjugated goat anti-mouse secondary Abs specific for IgG (H+L), IgG1, and IgG2a (1:5,000 dilution, Jackson ImmunoResearch Laboratories, and Southern Biotechnology Associates). Anti-CCP Ab values were expressed as concentration units, and RF values were expressed as OD. Samples were run in duplicate and averaged.
Mass spectrometry analysis
Proteins were treated with trypsin overnight at 37°C. The tryptic peptides were resolved by HPLC by using a Zorbax 300SB-C18 nanocolumn (Agilent Technologies, Palo Alto, CA) and eluted at 300 nl/min with a 60-min linear gradient from 0% to 95% acetonitrile containing 0.1% formic acid. Separated peptides were electrosprayed into an ion trap mass spectrometer (XCT Plus, Agilent Technologies). Peptides were identified by using Mascot (Matrix Science, Boston, MA) to compare raw MS/MS data with a SwissProt database (Matrix Science).
Ag array analysis
Synovial Ag arrays and the associated methods used in this work were previously described in detail (20). The 1536-feature synovial Ag arrays contain 225 Ags, including proteins and overlapping peptides representing candidate autoantigens relevant to RA. The Ag arrays were produced by using a robotic microarrayer to attach peptides and proteins to Array It SuperEpoxy microscope slides (TeleChem International, Sunnyvale, CA). Arrays were probed with 1:200 dilutions of plasma from individual mice. Reactive Abs were detected using Cy3-conjugated goat anti-human or goat anti-mouse IgG/IgM secondary Ab (1:4,000 dilution, Jackson ImmunoResearch Laboratories) prior to scanning. GenePix Pro 5.0 software (Molecular Devices, Union City, CA) was used to determine the net median pixel intensities for each Ag feature. Data analysis was performed using Significance Analysis for Microarrays (SAM) software version 1.21 (www-stat-class.stanford.edu/SAM/servlet/SAMServlet) to identify Ag features with statistically significant differences in reactivities between the experimental groups. Cluster 3.0 software was then used to hierarchically group the samples and Ag features on the basis of a pairwise similarity function, and Java Treeview 1.60 software was used to display the data as a heat map [(21), http://rana.lbl.gov/EisenSoftware.htm]. False-discovery rate (q) values for the following figure panels are as follows: Fig. 3A: q < 9.1%; Fig. 3B: q < 0.2%; Fig. 4B: q < 2.8%; and Fig. 5C: q < 19.7%. An accession number (GSE18073) for our complete microarray data has been assigned and approved in the GEO public database. The URL for the database is as follows: (www.ncbi.nlm.nih.gov/projects/geo/query/acc.cgi?acc=GSE18073).
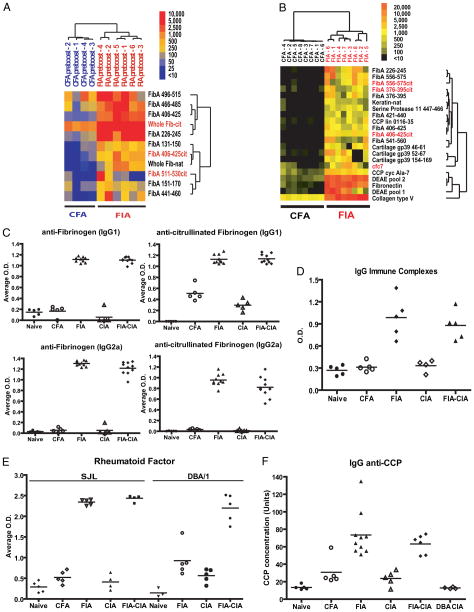
FIGURE 3.
Mice with FIA develop antinative and anti-in vitro citrullinated fibrinogen Abs, anti-CCP Abs, RF, and ICs. A–B, Synovial Ag arrays were probed with 1:150 dilutions of plasma derived from SJL mice immunized with fibrinogen emulsified in CFA or with CFA alone. Autoantibody binding was detected with a Cy3-conjugated goat-anti-mouse IgG/M secondary Ab. SAM was applied to identify Ags with statistically significant differences in array reactivity between FIA and CFA control plasma obtained from mice before boosting (A) or 27 d after boosting (B). The SAM hits were subjected to hierarchical cluster analysis and are displayed as a heatmap. Synovial array profiling of FIA plasma demonstrated autoreactive B cell responses against peptides representing native fibrinogen, and B cell epitope spreading resulting in additional targeting of citrullinated fibrinogen in the samples obtained before boosting, with further spreading to target CCPs, collagen type V, and cartilage gp39 in samples obtained after boosting. C, Plasma samples from SJL and DBA/1 mice, immunized as indicated, were diluted 1:100 and assayed for isotype-specific IgG1 and IgG2 Abs to native and in vitro citrullinated fibrinogen. D, ELISA was used to measure IgG ICs, (E) RF, and (F) IgG anti-CCP Abs in plasma samples.
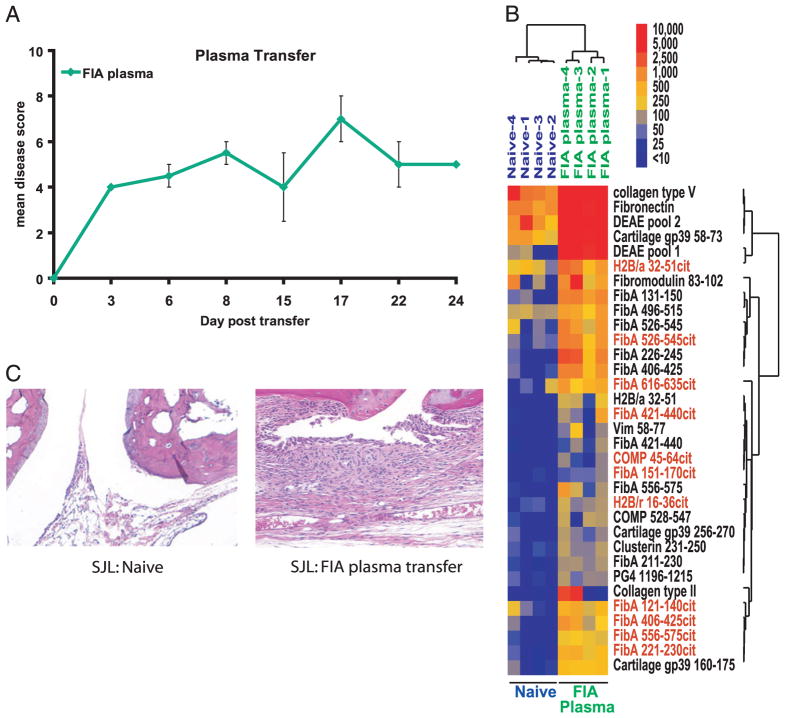
FIGURE 4.
FIA plasma induces arthritis in naive mice. Plasma collected from mice with FIA were pooled, and 0.3 ml was injected i.v. into 6-wk-old naive SJL mice on days 0 and 2 (A). Synovial Ag array profiling of plasma from the arthritic recipient mice demonstrated autoreactive B cell responses against peptides representing native fibrinogen and citrullinated fibrinogen, and further epitope spreading resulting in additional targeting of fibronectin, collagen type V, cartilage gp39, and clusterin (B). Joints from naive mice that developed arthritis after FIA plasma transfer (without boosting) demonstrated mononuclear cell infiltrates and synoviocyte proliferation (C). Data are representative of three independent experiments with three to five mice per group in each experiment. Error bars represent SEM.
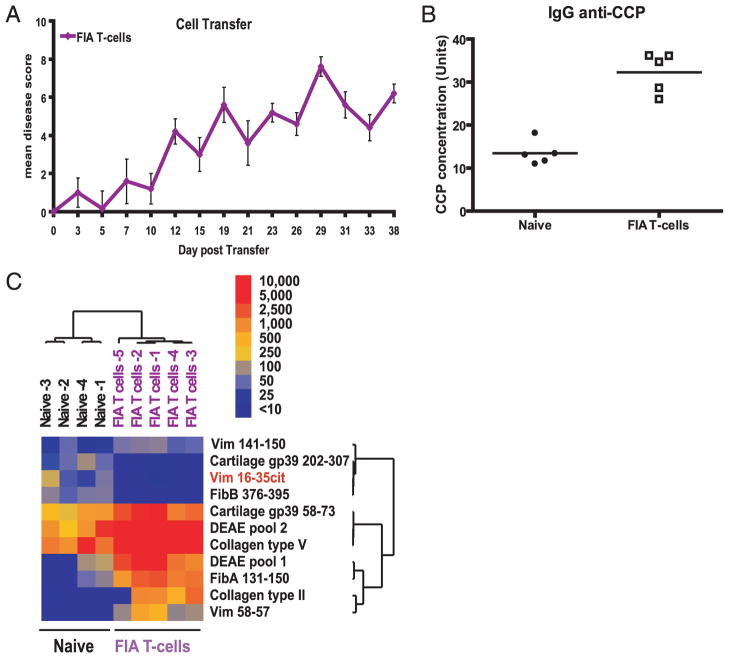
FIGURE 5.
Fibrinogen-reactive T cells transfer disease to naive mice. Splenocytes harvested from mice with FIA were cultured in vitro and stimulated with 0.01 mg/ml fibrinogen for 3 d. Enriched T cells were transferred into 6-wk-old naive SJL mice, which developed visible signs of arthritis within 2 wk (A). Plasma samples taken from the diseased mice 38 d after cell transfer were assayed for IgG anti-CCP Abs (B). Synovial array profiling of plasma from the arthritic recipient mice demonstrated autoreactive B cell responses against peptides representing native fibrinogen, and further spreading the responses to target collagen type V, cartilage gp39, and citrullinated vimentin (C). Data are representative of three independent experiments with three to five mice per group in each experiment. Error bars represent SEM.
Pathology
Mice were euthanized and both hind limbs dissected, formalin-fixed, and decalcified. The samples were embedded in paraffin, sectioned, and stained with H&E or toluidine blue (Premier Laboratory, Boulder, CO) according to standard procedures. Representative sections are shown at 4× and 20× magnifications. Sections were evaluated by a blinded investigator for synovitis, pannus, and bone and/or cartilage destruction on the basis of a previously described scoring system: grade 0 = normal; grade 1 = mild inflammation, mild hyperplasia of the synovial lining layer, and mild cartilage destruction without bone erosion; grades 2–4 = increasing degrees of inflammatory cell infiltrates, synovial lining hyperplasia and pannus formation, and cartilage and bone destruction (22).
Statistical evaluation
Mann-Whitney U test was used for statistical evaluation of diseased mice. An unpaired Student t test was used for statistical evaluation of groups with unknown and potentially disparate variances.
Results
Immunization with human fibrinogen induces an inflammatory arthritis in mice
Because autoantibodies target citrullinated fibrinogen in a subset of anti-CCP Ab-positive (anti-CCP+) RA patients (10–12), we sought to determine whether immunization of mice with fibrinogen would induce autoimmune arthritis. We selected a variety of commonly available mouse strains, including C57BL/6, DBA/1, BALB/c, and SJL mice, and immunized them s.c. with human fibrinogen (0.1 mg/mouse) emulsified in CFA. Twenty-one days later, the mice received a s.c. boost immunization with human fibrinogen (0.1 mg/mouse) emulsified in IFA. Two weeks after boosting, both DBA/1 and SJL mice developed an inflammatory arthritis involving the paw(s) on one or more limbs (Fig. 1A). The incidence of arthritis in most experiments approached 100% (Supplemental Fig. 1). Mass spectrometry analysis of commercially purified human fibrinogen revealed several citrulline modifications on both the α- and β-chains of fibrinogen (Table I). This demonstrates that the fibrinogen purified from human blood, which was used for immunization of mice to induce FIA, is already citrullinated to a certain degree.
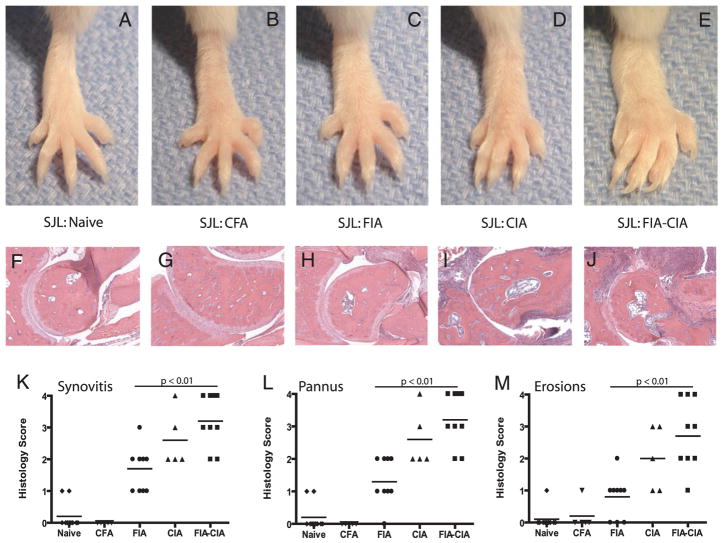
FIGURE 1.
Immunization with fibrinogen induces arthritis in SJL and DBA/1 mice. A, SJL (n = 5) and DBA/1 (n = 5), but not BALB/c (n = 3) or C57BL/6 (n = 3), mice develop inflammatory arthritis after immunization and boosting with human fibrinogen emulsified in CFA. B, SJL mice immunized to develop FIA (n = 10) or a combination of FIA and CIA (n = 10) exhibit chronic inflammatory arthritis, whereas mice immunized with CFA alone (n = 10) exhibit only minimal signs of arthritis. Data are representative of >5 independent experiments with 5–10 mice per group in each experiment. C, Splenocytes isolated from mice with FIA were stimulated with human fibrinogen (0.01 mg/ml), and after 72 h proliferative responses were quantitated by [3H]-thymidine incorporation. Stimulation with human fibrinogen induced robust proliferative responses in splenocytes isolated from mice with FIA but not in splenocytes from naive or CFA-immunized mice. D, Fibrinogen-stimulated splenocytes from FIA mice, but not from naive or CFA-immunized mice, produced the proinflammatory cytokines IL-6, TNF-α, IFN-γ, and IL-17. Error bars represent the SD of triplicate measurements.
Table I.
Mass spectrometry identified citrulline modifications in fibrinogen purified from human blood
| Sequence | Ion Score | p-Value |
|---|---|---|
| Fibrinogen α-chain (gi: 223918) | ||
| RNPSSAGSWNSGSSGPGSTGNcitN | 67 | 0.0058 |
| RMELEcitPGGNEITRG | 43 | 0.2800 |
| KGLIDEVNQDFTNcitI | 50 | 0.0870 |
| RHcitHPDEAAFFDTASTGKT | 63 | 0.0035 |
| Fibrinogen β-chain (gi: 399492) | ||
| K. REEAPSLcitPAPPPISGGGYRA | 61 | 0.0230 |
| KGGETSEMYLIQPDSSVKPYcitV | 82 | 5.00E-05 |
| RTPCTVSCNIPVVSGKECEEIIcitK | 69 | 0.0011 |
| REEAPSLcitPAPPPISGGGYRA | 46 | 0.1100 |
Boldface type represents arginine residue identified by mass spectrometry to be citrullinated.
Immunization with fibrinogen resulted in significantly more severe arthritis than did immunization with CFA alone (Fig. 1B, p < 0.05, by Mann-Whitney). CIA can be induced in SJL mice and is significantly more severe than the mild arthritis associated with CFA immunization (data not shown). Coimmunization of SJL mice with FIA-CIA resulted in arthritis that was more severe than that resulting from immunization with fibrinogen alone (p < 0.05 on days 22 and 24, by Mann-Whitney). We also observed increased severity in arthritis after coimmunization of DBA/1 mice with FIA-CIA as compared with immunization with CII CIA alone (Supplemental Fig. 2).
To determine whether FIA is associated with T cell responses to fibrinogen, we harvested whole splenocytes from naive mice, mice with FIA, or CFA-immunized mice and cultured the cells in the presence of human fibrinogen (0.01 mg/ml). Splenocytes from mice with FIA proliferated robustly in response to fibrinogen, as measured by [3H]-thymidine incorporation (Fig. 1C). Splenocytes derived from mice with FIA exhibited evidence of basal activation, based on their increased proliferation (Fig. 1C) and cytokine production (Fig. 1D) in the absence of stimulation. We also analyzed the cytokine profiles in the cell culture supernatants from these stimulation assays. Compared with cells derived from naive and CFA-immunized mice, splenocytes derived from mice with FIA produced high levels of the proinflammatory cytokines IL-6, TNF-α, IFN-γ, and IL-17 in response to fibrinogen (Fig. 1D). Collectively, the data demonstrate that immunization with human fibrinogen containing several citrulline modifications induces autoimmune arthritis in SJL mice, and that diseased mice possess fibrinogen-specific T cells that secrete proinflammatory cytokines.
FIA results in moderate arthritis involving the digits, mid paw, and ankle
Images of representative hind paws of naive mice, CFA-immunized mice, and mice with FIA, CIA, and FIA-CIA show the clinical features of FIA (Fig. 2A–E). The images were taken 50 d after the initial immunization to induce disease, which is 2 wk after the time at which mice with FIA develop clinical arthritis. CFA immunization induced mild swelling and erythema of the digits and mid paw (Fig. 2A, 2B). FIA is characterized by arthritis involving the digits, mid paw, and to a lesser degree, the ankle (Fig. 2C). Mice with CIA (Fig. 2D) and FIA-CIA (Fig. 2E) developed more severe arthritis involving the paw and ankle. Bone erosions were observed in approximately one in five mice with FIA.
FIGURE 2.
FIA involves the digits and mid paw. Images from representative hind paws of naive mice (A), CFA-immunized mice (B), and mice with FIA (C), CIA (D), or FIA-CIA (E) are presented. Photomicrographs were taken 50 d after the initial disease-inducing immunization and ~2 wk after the development of clinical arthritis in mice with FIA. FIA is characterized by inflammation of the digits and mid paw, with general sparing of the ankles (C), whereas CIA and FIA-CIA are characterized by a fulminant synovitis that involves the whole paw and ankle (F–J). Hind paws harvested 2 wk after the development of arthritis were embedded in paraffin, sectioned, and stained with H&E (original magnification ×400). Histopathological analysis demonstrates mononuclear cell infiltration and synoviocyte proliferation suggestive of pannus formation in mice with FIA (H). Paws from mice with CIA and FIA-CIA exhibited intense inflammatory infiltrates, as well as extensive joint destruction and bone erosions. Representative hind paws that were paraffin-embedded, sectioned, and stained with toluidine blue were scored for synovitis (K), pannus (L), and bone erosions (M). Mice with FIA, CIA, and FIA-CIA exhibited significantly more severe synovitis, pannus, and erosion than did naive and CFA-treated mice (p < 0.01, unpaired t test).
Comparisons of H&E-stained ankle joints between the groups of mice revealed a range of histopathological features. Mice immunized with CFA exhibited minimal mononuclear cell infiltrates in the periarticular tissue (Fig. 2F, 2G), whereas mice immunized with fibrinogen (i.e., mice with FIA) exhibited moderate mononuclear cell infiltrates in the periarticular tissue and proliferation of synovial lining cells suggestive of pannus formation (Fig. 2H). Mice with CIA and FIA-CIA exhibited massive mononuclear cell infiltrates and marked pannus formation (Fig. 2I, 2J, respectively).
To further characterize the differences in disease severity between the groups, we performed histological scoring of synovitis (Fig. 2K), pannus formation (Fig. 2L), and bone erosions (Fig. 2M) in a blinded fashion. Minimal synovitis, pannus formation, and bone erosions were evident in both naive and CFA-immunized mice (histology score 0–1). Mice with FIA exhibited intermediate histological scores for synovitis, pannus formation, and bone erosions, which were significantly higher than the scores for naive and CFA-treated mice (histology score 1–2; p < 0.01 by unpaired t test). Mice with CIA exhibited moderate to severe synovitis, pannus formation, and bone erosions (histology score 2–4; p < 0.01 comparing CIA mice with naive and CFA-immunized mice by unpaired t test). Mice with FIA-CIA had the highest scores for synovitis, pannus formation, and bone erosions (histology score 2–4; p < 0.01 comparing FIA-CIA mice with naive and CFA-immunized mice by unpaired t test).
Together, the clinical and histopathological data indicate that FIA results in a moderate inflammatory arthritis that is less severe than CIA. Mice with FIA-CIA exhibit severe arthritis that is more destructive than CIA.
FIA is characterized by autoantibody responses to native fibrinogen that spread to additionally target citrullinated fibrinogen and other synovial autoantigens
We next used arrays containing synovial Ags to profile the IgG/IgM Abs in the plasma of fibrinogen-immunized and CFA-immunized mice 21 d after the first immunization (i.e., before boosting; Fig. 3A), and 27 d after the second immunization (i.e., after boosting and at the time of arthritis onset; Fig. 3B). SAM analysis of autoantibody reactivity before boosting demonstrated a significant increase in Ab reactivity (false-discovery rate q < 0.01) to human “native” fibrinogen protein (fibrinogen purified from human blood that contains several citrulline modifications as demonstrated in Table I), in vitro citrullinated fibrinogen protein, as well as unmodified and citrulline-modified fibrinogen peptides, in response to immunization with fibrinogen. CFA-immunized mice exhibited minimal autoantibody reactivity to native fibrinogen protein and moderate reactivity to in vitro citrullinated fibrinogen protein. These data demonstrate that immunization of mice with human fibrinogen induces autoimmunity against both native and citrullinated fibrinogen, and that the autoimmune response to fibrinogen precedes the onset of arthritis.
Synovial array analysis of plasma derived from mice with established FIA (27 d after boosting with fibrinogen emulsified in IFA) demonstrated extensive autoantibody reactivity against unmodified and citrulline-modified peptides derived from fibrinogen. Moreover, plasma from these mice exhibited additional spreading of autoantibody responses to target additional candidate RA autoantigens, including cartilage gp39 and collagen type V (Fig. 3B). In contrast, plasma from CFA-immunized mice did not exhibit autoantibody reactivity to these Ags, indicating that FIA is an Ag-driven disease and not simply an adjuvant-induced arthritis. Autoantibody reactivity to fibronectin and the DEAE extraction pools, which also contain fibronectin, in FIA plasma (Fig. 3B) is likely attributable to the binding of fibronectin to the Fc region of Ig in an Ag-independent manner. No Ab reactivity was detected to the vast majority of the 225 candidate Ags on the synovial arrays.
FIA is associated with Ab isotype class switching of antifibrinogen and RF B cell responses
We analyzed plasma derived from SJL mice immunized with CFA and from SJL mice with FIA, CIA, and FIA-CIA to determine the IgG Ab isotype(s) of the antifibrinogen, anti-CCP, and RF responses. In mice with FIA or FIA-CIA, we detected class switching of antinative fibrinogen B cell responses to both IgG1 and IgG2a (Fig. 3C, left panels; p < 0.01 comparing FIA and FIA-CIA mice with naive, CFA-treated, and CIA-induced mice by unpaired t test). Of note, IgG1 Ab responses to in vitro citrullinated fibrinogen were found in all groups, with the highest levels observed in mice with FIA and FIA-CIA. In contrast, IgG2a Ab responses to in vitro citrullinated fibrinogen were only observed in mice with FIA or FIA-CIA (Fig. 3C, right panels, p < 0.01, by unpaired t test).
A C1q capture assay demonstrated an increase in levels of IgG circulating immune complexes (CICs) in mice with FIA and FIA-CIA (p < 0.01, by unpaired t test) but not in mice with CIA or in CFA-immunized mice (Fig. 3D). An assay for RF revealed highly elevated levels in both SJL and DBA mice with FIA and FIA-CIA compared with mice with CIA and CFA-immunized mice (Fig. 3E, p < 0.01, by unpaired t test).
To determine whether mice with FIA possess IgG anti-CCP Abs, we performed anti-CCP3 IgG ELISAs on plasma samples. Anti-CCP IgG Ab levels were higher in plasma from mice with FIA compared with plasma from naive mice (average of 73.4 units from 10 mice, p < 0.05, by unpaired t test). Mice with FIA-CIA also had elevated levels of anti-CCP IgG Abs in their plasma (average of 63.1 units from six mice, p < 0.05, by unpaired t test). Interestingly, compared with DBA/1 mice with CIA, SJL mice with CIA developed low but significantly elevated levels of anti-CCP IgG Abs (average of 23.6 units from five mice) (Fig. 3F, p < 0.05, by unpaired t test). CFA immunization of SJL mice was associated with low level but not statistically significant amounts of anti-CCP IgG Abs (average of 30.8 units from five mice, p = 0.0689, by unpaired t test).
Induction of arthritis by transfer of plasma or fibrinogen-activated T cells from mice with FIA
Plasma from mice with FIA was collected and 0.3 ml pooled plasma injected i.v. into naive SJL mice on days 0 and 2. Three days later, the hind paws of the mice exhibited mild to moderate arthritis, which persisted for 3 wk (Fig. 4A). Synovial array analysis of FIA plasma demonstrated autoantibody targeting of both native and citrullinated fibrinogen and of epitopes representing additional candidate autoantigens, including collagen type V, cartilage gp39, clusterin, and histone 2B (Fig. 4B). H&E staining of joint sections showed infiltration of mononuclear cells and proliferation of synovial lining cells in the ankle joint derived from a representative FIA plasma recipient (Fig. 4C, right panel). No mononuclear cell infiltration or synovial proliferation was observed in the ankle joint derived from a healthy control mouse (Fig. 4C, left panel).
Splenocytes and lymphocytes derived from mice with FIA were cocultured for 72 h in the presence of human fibrinogen (0.01mg/ml). Cultured cells were washed twice and enriched for CD3+ T cells, and 108 cells were injected i.v. into naive recipient SJL mice (n = 8). Within 2 wk, the recipients exhibited moderate arthritis, which was still evident 38 d after the adoptive transfer, at which time 100% of the mice exhibited clinical arthritis (Fig. 5A). Plasma taken from recipient mice 38 d after the transfer of activated FIA T cells contained significant titers of anti-CCP IgG Abs (Fig. 5B, average of 32.3 units from five mice, p < 0.01, by unpaired t test). Synovial array analysis of the plasma identified a small set of statistically significant autoantibody reactivities that included reactivity against fibrinogen, vimentin, and CII (Fig. 5C).
Together, these studies demonstrate that the transfer of plasma or fibrinogen-reactive T cells from mice with FIA induces arthritis in naive recipients, and that plasma and T cell transfer can induce the production of autoantibodies to CCPs and other candidate RA autoantigens.
Anti-CCP Ab-positive RA is characterized by autoantibodies targeting citrullinated fibrinogen
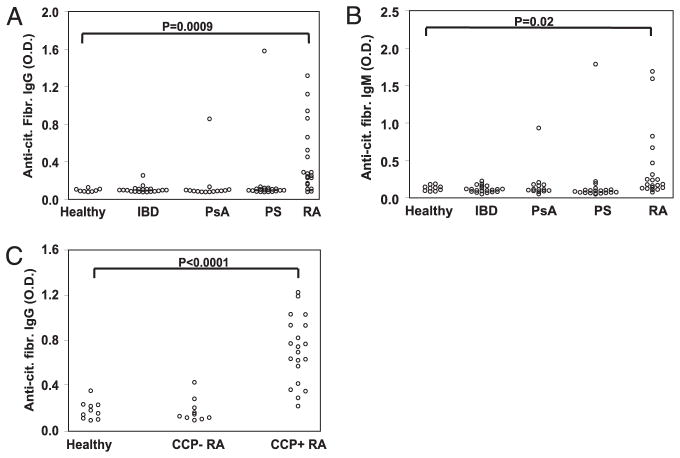
To further demonstrate the relevance of FIA to human RA, we characterized the autoantibody reactivity against in vitro citrullinated fibrinogen in a cohort of RA and control patients. ELISA plates were coated with in vitro citrullinated fibrinogen, and IgG/IgM-specific secondary Abs were used to detect antifibrinogen Ab reactivity in plasma derived from healthy individuals (n = 10) and from patients diagnosed with inflammatory bowel disease (n = 20), psoriatic arthritis (n = 14), psoriasis (n = 20), or RA (n = 20). A subset of RA patients possessed IgG (Fig. 6A, p = 0.0009, by unpaired t test) and IgM (Fig. 6B, p = 0.02, by unpaired t test) autoantibodies against in vitro citrullinated fibrinogen, whereas no autoantibody reactivity was detected against native fibrinogen, which contains several citrulline modifications (data not shown). Analysis of a larger set of anti-CCP Ab-negative (anti-CCP−) and anti-CCPAb-positive (anti-CCP+) RA patients demonstrated that 80% of anti-CCP+ RA patients possessed elevated titers of IgG autoantibodies to in vitro citrullinated fibrinogen (p < 0.0001, by unpaired t test), whereas only 10% of anti-CCP− RA patients exhibited such an elevation in autoantibody titers (Fig. 6C).
FIGURE 6.
Anti-CCP–positive RA patients possess Abs that recognize in vitro citrullinated fibrinogen. IgG (A) and IgM (B) autoantibodies targeting in vitro citrullinated fibrinogen were measured by ELISA in plasma samples derived from healthy individuals (n = 10) and patients with inflammatory bowel disease (n = 20), psoriatic arthritis (n = 14), psoriasis (n = 20), or RA (n = 20). Statistical comparisons were made using an unpaired t test with Welch correction. C, Anti-in vitro citrullinated fibrinogen IgG Abs were measured by ELISA in plasma samples from healthy patients (n = 10), anti-CCP Ab-negative RA patients (CCP+ RA, n = 10), and anti-CCP Ab-positive RA patients (CCP+ RA, n = 20).
Discussion
In this study, we describe the development and characterization of FIA as a murine model for the study of RA. Importantly, native fibrinogen that contains several citrulline modifications based on mass spectrometry analysis (Table I) was capable of inducing inflammatory arthritis. In addition, the development of inflammatory arthritis after immunization with fibrinogen was associated with the expansion of autoantibody responses to target both native and citrullinated peptides derived from fibrinogen (Fig. 3A, 3B). Clinical symptoms include swelling and erythema that encompass the digits, mid paw, and ankle/wrist. Joint sections from mice with FIA exhibit mononuclear cell infiltrates within the inflamed synovial membrane, pannus formation, and in some instances, bone erosions. FIA in mice is associated with strong T cell reactivity to fibrinogen and production of the proinflammatory cytokines IL-6, TNF-α, IFN-γ, and IL-17. Using synovial Ag microarrays, we demonstrated that immunization with fibrinogen induces strong B cell reactivity to both native fibrinogen, which contains several citrulline modifications, and in vitro citrullinated fibrinogen before the onset of clinical arthritis, with autoantibody responses expanding to include targeting of other candidate RA autoantigens in established FIA. We also show that arthritis can be adoptively transferred to naive mice with either plasma or fibrinogen-reactive T cells derived from mice with FIA.
Importantly, mice with FIA possess elevated levels of RF, CICs, and anti-CCP Abs. Detection of RF and anti-CCP Abs is frequently used in the diagnosis of RA. RF, although associated with more active disease and with the development of bone erosions, is not specific for RA (23, 24). ACPAs, on the other hand, are highly specific for RA and are also associated with the development of more severe joint destruction (25). Wipke et al. (26) demonstrated a critical role for CICs in activating neutrophils and mast cells to thereby enable autoantibodies to enter joint tissue and initiate inflammatory arthritis. It is likely that these same mechanisms and cell types are also critical to the induction of arthritis by CICs in FIA. We recently demonstrated the presence of CICs containing citrullinated fibrinogen in half of anti-CCP+ RA patients, and found that there is a positive correlation between the presence of these complexes and the presence of anti-in vitro citrullinated fibrinogen autoantibodies (12). The disparity between our findings and previous findings in the exact percentages of anti-CCP+ patients whose sera react with citrullinated fibrinogen may be due to differences in the degree to which fibrinogen was in vitro citrullinated in the different studies. In addition, our data are based on samples from a U.S. cohort, whereas most of the reported data are based on samples from European cohorts; differences in cigarette smoking, gingivitis, and other factors might also influence the percentage of patients exhibiting reactivity to citrullinated fibrinogen. Our observation that both anti-CCP and anticitrullinated fibrinogen Ab titers are elevated in mice with FIA further suggests that FIA is representative of anti-CCP+ and anticitrullinated fibrinogen Ab-positive RA.
Synovial Ag array analysis of plasma derived from mice with established FIA demonstrated expansion of the autoantibody response to target additional native and citrullinated fibrinogen epitopes, as well as epitopes derived from synovial Ags, including fibronectin, type V collagen, and cartilage gp39. Therefore, we propose that the initial immunization with fibrinogen induces autoantibody responses against native and citrullinated fibrinogen epitopes, and that progression to clinical arthritis is associated with the expansion of autoantibody responses to target additional synovial Ags. Similarly, ACPA responses in RA can predate clinical arthritis by years, and there is evidence that such responses evolve over time (27, 28). Abs to several citrullinated proteins, including filaggrin, fibrinogen, vimentin, CII, and α-enolase, are observed in human RA (29). The expansion of ACPA responses in FIA could contribute to more severe and chronic disease (30). Additional characterization of anticitrullinated fibrinogen Ab responses in human RA will be needed to determine whether such responses, and the evolution of these responses, are associated with the development and/or severity of RA.
Although anti-CCP Abs are specific to RA (5), increased citrullination of fibrin and other proteins is a phenomenon associated with multiple different inflammatory arthritides (31, 32). It remains to be determined whether qualitative or quantitative differences in the citrullination of fibrinogen, fibrin, and/or other proteins are specific to RA, and whether, within the spectrum of anticitrulline responses, certain ACPAs are more arthritogenic than others.
Mass spectrometry analysis demonstrated that the fibrinogen purified from human blood and used to induce FIA contains several citrulline modifications (Table I). Native fibrinogen present in human blood may indeed contain several citrulline modifications; alternatively, it is possible that the process of purifying fibrinogen from human blood results in the citrullination of fibrinogen. Despite the low-level citrullination of fibrinogen purified from human blood, ACPAs derived from RA patients do not react with this native fibrinogen (data not shown). Not all citrulline modifications render a protein immunoreactive with ACPAs (17); however, citrullinated fibrin(ogen) is a known target of ACPAs, and CICs containing citrullinated fibrinogen are detected in a subset of RA patients (10, 12). Therefore, these findings suggest that ACPAs target citrullinated fibrinogen epitopes that are not normally present in fibrinogen in the blood but are generated during inflammation-associated citrullination of fibrinogen in synovial joints. Mononuclear cells that infiltrate the synovium during joint inflammation contain PAD enzymes (33), and the level of both PAD4 and citrullinated proteins in the joints of mice with CIA correlates with the severity of inflammation (34). Extracellular proteins, such as fibrinogen, are the primary targets of PADs in inflamed joints (34, 35); inflammation-driven generation of additional citrullinated epitopes on fibrinogen may thus elicit an ACPA response and contribute to RA pathogenesis.
Our findings suggest that immunization with fibrinogen results in the generation of anticitrullinated fibrinogen responses that can also target citrullinated proteins present in tissues other than the synovial joint. This possibility is supported by the reactivity of human RA sera with not only citrullinated proteins generated in inflamed joint tissue but also with citrullinated filaggrin, a protein expressed in stratified epithelium but not in joints (29). Multiple proteins are citrullinated as part of physiological processes, including formation of the myelin sheath (during which myelin basic protein is citrullinated), cornification of the epidermis (keratin), late-stage differentiation of the epidermis (filaggrin), and modulation of chromatin structure (histones) (35). Kuhn et al. (19) showed that a monoclonal Ab specific for in vitro citrullinated fibrinogen exacerbated tissue injury in rodent models of arthritis. We postulate that in vitro citrullination of substrate proteins results in their hyper-citrullination and in the generation of many citrulline-containing epitopes that are not representative of the citrulline-containing epitopes formed in vivo; some of these hyper-citrullinated epitopes may be cross recognized by ACPAs. It remains unclear why anticitrullinated fibrinogen responses induce arthritis in the mouse without affecting other tissues that contain citrullinated proteins.
The induction of arthritis by immunization with fibrin or with native or in vitro citrullinated fibrinogen has been previously studied. Chronic arthritis was induced in rabbits by systemic immunization with heterologous or autologous fibrin, followed by intraarticular injection of fibrin (36). Immunization of BALB/c mice with native or in vitro citrullinated fibrinogen induced Abs to citrullinated fibrinogen and CCP but did not evoke arthritis (37). Likewise, FIA was not induced in BALB/c mice in our studies. Rubin and Sonderstrup (38) immunized several mouse strains with in vitro citrullinated human fibrinogen and observed high titers of Abs against human, but not mouse, fibrinogen and relatively low titers of anticitrulline Abs. None of the 600 mice on the various background strains tested (BALB/c, DBA/1, and C57BL/10) developed arthritis. Furthermore, immunization of DBA/1 mice expressing a transgene encoding HLA-DR4*0401 with denatured in vitro citrullinated human fibrinogen induced Abs against citrullinated fibrinogen but did not evoke arthritis (38). We also attempted to induce FIA with in vitro citrullinated fibrinogen, and, despite the generation of high-titer anti-CCP Ab responses, no mice developed arthritis (data not shown). Thus, the induction of arthritis by fibrinogen is restricted both by the degree of fibrinogen citrullination and by genetic susceptibility.
Tertiary antigenic structures are frequently targeted in autoimmune responses and in protective immune responses against microbial pathogens (39). Artificial in vitro citrullination likely results in hyper-citrullination of fibrinogen (i.e., conversion of more pep-tidylarginines to peptidyl-citrullines than would occur in vivo in RA or in rodent models of RA), which could disrupt the tertiary antigenic structures that are critical for the generation of arthritogenic immune responses against citrullinated fibrinogen; this may explain why we (data not shown) and others failed to induce arthritis in wild-type mice with in vitro citrullinated fibrinogen (19, 37, 38). Immunization and boosting of DR4-IE transgenic mice (on the C57BL/6 background) with nondenatured in vitro citrullinated human fibrinogen was recently shown to induce arthritis in nearly 35% of the mice after 10 wk (40). Nondenatured in vitro citrullinated fibrinogen may have tertiary antigenic structures intact that may mimic the endogenously citrullinated fibrinogen generated within inflamed synovial joints.
Table II summarizes the more commonly used mouse models of RA and compares these models to FIA. The K/BxN spontaneous mouse model of RA begins as a T cell–dependent response to glucose-6-phosphoisomerase (GPI) and differentiates into an autoantibody-dependent disease involving anti-GPI IgG (41). K/BxN mice possess high levels of ICs containing GPI but do not develop RF and are weakly positive for anti-CCP Abs. Matsumoto et al. (42) reported that only 15% of RA patients possess anti-GPI Abs (12–29% range), and that anti-GPI autoantibodies are also present in other arthritides and are thus not specific for RA. Therefore, GPI does not appear to be a primary autoantigen in human RA.
Table II.
Comparison of mouse models of RA
| Mouse Models of RA | Dominant Ag | T cell Specificity | B cell Specificity | Cell Transfer | Plasma Transfer | RF | Anti-CCP | ICs | Human RA Relevance (%) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Spontaneous | ||||||||||
| K/BxN (41, 42) | RNase TCR transgenic | GPI | GPI | GPI | Yes | Yes | Negative | Positive | Yes | 15 |
| SKG (43) | ZAP-70 mutation | Undefined | Undefined | CII | Yes | No | Positive | Positive | Yes | None |
| Inducible | ||||||||||
| CIA (44–51) | DBA/1, SJL | CII | CII | CII | No | Yes | Positive | Positive | No | 5–15 |
| FIA | SJL, DBA/1 | Fibrinogen | Fibrinogen | Fibrinogen | Yes | Yes | Positive | Positive | Yes | 35 |
The SKG spontaneous mouse model of RA arose from a mutation of the ζ-associated–protein of the 70 kDA (ZAP-70) that results in abnormal thymic T cell selection and survival of autoreactive clones (43). Anti-CII autoantibodies are present in sera derived from SKG mice. T cells, thymocytes, and bone marrow cells transfer disease, but transfer of SKG serum does not induce arthritis in recipients. Although this model is positive for RF, anti-CCPAbs, and ICs (Table II), analogous mutations in CD45 and immunologic alterations have not been observed in human RA patients.
In the CIA model CII is used as the immunizing Ag to induce arthritis in rodents (44). This model is negative for RF, weakly positive for anti-CCP Abs, and negative for ICs (Table II). Although one group described cell-based adoptive transfer of CIA (45), most laboratories have not been able to induce arthritis by cell-based adoptive transfer. Transfer of CII-specific T cells has been reported in rats (44), and the only successful transfer in mice has been the induction of microscopic evidence of arthritis by intrasynovial injection of cloned T cell lines (45). Moreover, the frequency of Abs reactive to native CII in RA is low (5–15% of RA patients) (45, 46), which suggests that native CII is not a major pathogenic autoantigen in RA (47–49). In a cohort of 286 early RA patients, 40% possessed detectable IgG Abs directed against the citrullinated form of the immunodominant CII epitope C1 (50). Recently, it was shown that anticitrullinated CII Abs are pathogenic in a rodent model (51), suggesting that such responses against citrullinated CII might contribute to arthritis. Additional studies will be needed to determine the relevance and role of anticitrullinated CII responses in RA.
In the FIA model described in this study, the native form of fibrinogen is used as the immunizing Ag. FIA involves robust T cell reactivity to native fibrinogen and B cell reactivity to native fibrinogen, citrullinated fibrinogen, and other candidate RA auto-antigens. Disease can be transferred with either fibrinogen-reactive T cells or plasma from FIA mice. Mice with FIA possess RF, anti-CCP Abs, and IgG ICs, all of which are characteristic of a subset of RA patients. Moreover, citrullinated fibrinogen is a prominent target of the autoantibody response in half of anti-CCP+ RA patients (12). Compared with the arthritis that develops in other murine models of RA, FIA is mild to moderate and therefore more closely resembles human RA. Another advantage of the FIA model is that it does not rely on genetically altered mice expressing a TCR-encoding transgene or mutated form of CD45, but rather uses wild-type SJL or DBA/1 mice, which are common mouse strains that are readily available.
Recent observations have linked the inflammatory and coagulation systems in several autoimmune diseases. Articular inflammation in CIA is accompanied by the upregulation of tissue factor, tissue factor pathway inhibitor, urokinase, and plasminogen activator, suggesting that increased extravascular coagulation may contribute to fibrin deposition within the joint (52). Thus, the increased deposition and citrullination of fibrinogen in inflamed joints in human RA could potentiate arthritogenic autoimmune responses against citrullinated fibrinogen. In support of a pathogenic role for components of the coagulation system in inflammatory arthritis, the thrombin inhibitor hirudin was shown to be efficacious in treating CIA (53). The coagulation cascade has also been implicated in several pathological stages of multiple sclerosis: treatment of experimental autoimmune encephalomyelitis, a Th1–Th17 Ag-driven mouse model of multiple sclerosis, with either hirudin or activated protein C (an anticoagulant) ameliorated disease (54).
In conclusion, we demonstrate that immunization with human fibrinogen containing native citrulline modifications induces an inflammatory arthritis that shares clinical, histological, and immunological features with RA. Our results suggest that fibrinogen can be arthritogenic in mice and that FIA is mediated by both autoreactive T cell and autoantibody responses. Finally, in contrast to the other three mouse models of RA listed in Table II, we believe FIA is a highly relevant model for the study of human RA because it is based on autoimmunity against a known autoantigen targeted in approximately half of anti-CCP+ RA patients.
Supplementary Material
Acknowledgments
This work was funded by National Institutes of Health National Heart, Lung, and Blood Institute contract N01 HV 28183, National Institutes of Health National Institute of Arthritis and Musculoskeletal and Skin Diseases R21 AI069160, and Veterans Affairs Health Care System funding (to W.H.R). The mass spectrometry work was supported by the Stanford Digestive Disease Center grant National Institutes of Health P30 DK56339. P.P.H is the recipient of an Arthritis Foundation Northern California Chapter Grant.
We thank members of the Steinman and Robinson laboratories for their scientific input. We also thank Dr. Tamsin Lindstrom for her critical review of the manuscript.
Abbreviations used in this paper
- ACPA
anticitrullinated protein Abs
- CCP
cyclic citrullinated peptides
- CIA
collagen-induced arthritis
- CIC
circulating immune complex
- CII
collagen type II
- FIA
fibrinogen-induced arthritis
- GPI
glucose-6-phosphoisomerase
- IC
immune complexes
- PAD
peptidyl arginine deiminase
- RA
rheumatoid arthritis
- RF
rheumatoid factor
- SAM
significance analysis for microarrays
Footnotes
The online version of this article contains supplemental material
Disclosures
The authors have no financial conflicts of interests.
References
- 1.Firestein GS. Evolving concepts of rheumatoid arthritis. Nature. 2003;423:356–361. doi: 10.1038/nature01661. [DOI] [PubMed] [Google Scholar]
- 2.Klareskog L, Padyukov L, Alfredsson L. Smoking as a trigger for inflammatory rheumatic diseases. Curr Opin Rheumatol. 2007;19:49–54. doi: 10.1097/BOR.0b013e32801127c8. [DOI] [PubMed] [Google Scholar]
- 3.McInnes IB, Schett G. Cytokines in the pathogenesis of rheumatoid arthritis. Nat Rev Immunol. 2007;7:429–442. doi: 10.1038/nri2094. [DOI] [PubMed] [Google Scholar]
- 4.van Boekel MA, Vossenaar ER, van den Hoogen FH, van Venrooij WJ. Autoantibody systems in rheumatoid arthritis: specificity, sensitivity and diagnostic value. Arthritis Res. 2002;4:87–93. doi: 10.1186/ar395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rantapöö-Dahlqvist S, de Jong BA, Berglin E, Hallmans G, Wadell G, Stenlund H, Sundin U, van Venrooij WJ. Antibodies against cyclic citrullinated peptide and IgA rheumatoid factor predict the development of rheumatoid arthritis. Arthritis Rheum. 2003;48:2741–2749. doi: 10.1002/art.11223. [DOI] [PubMed] [Google Scholar]
- 6.Goldbach-Mansky R, Lee J, McCoy A, Hoxworth J, Yarboro C, Smolen JS, Steiner G, Rosen A, Zhang C, Ménard HA, et al. Rheumatoid arthritis associated autoantibodies in patients with synovitis of recent onset. Arthritis Res. 2000;2:236–243. doi: 10.1186/ar93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schellekens GA, Visser H, de Jong BA, van den Hoogen FH, Hazes JM, Breedveld FC, van Venrooij WJ. The diagnostic properties of rheumatoid arthritis antibodies recognizing a cyclic citrullinated peptide. Arthritis Rheum. 2000;43:155–163. doi: 10.1002/1529-0131(200001)43:1<155::AID-ANR20>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 8.Nielen MM, van Schaardenburg D, Reesink HW, van de Stadt RJ, van der Horst-Bruinsma IE, de Koning MH, Habibuw MR, Vandenbroucke JP, Dijkmans BA. Specific autoantibodies precede the symptoms of rheumatoid arthritis: a study of serial measurements in blood donors. Arthritis Rheum. 2004;50:380–386. doi: 10.1002/art.20018. [DOI] [PubMed] [Google Scholar]
- 9.Jansen AL, van der Horst-Bruinsma I, van Schaardenburg D, van de Stadt RJ, de Koning MH, Dijkmans BA. Rheumatoid factor and antibodies to cyclic citrullinated Peptide differentiate rheumatoid arthritis from undifferentiated polyarthritis in patients with early arthritis. J Rheumatol. 2002;29:2074–2076. [PubMed] [Google Scholar]
- 10.Masson-Bessière C, Sebbag M, Girbal-Neuhauser E, Nogueira L, Vincent C, Senshu T, Serre G. The major synovial targets of the rheumatoid arthritis-specific antifilaggrin autoantibodies are deiminated forms of the α- and β-chains of fibrin. J Immunol. 2001;166:4177–4184. doi: 10.4049/jimmunol.166.6.4177. [DOI] [PubMed] [Google Scholar]
- 11.Nielen MM, van der Horst AR, van Schaardenburg D, van der Horst-Bruinsma IE, van de Stadt RJ, Aarden L, Dijkmans BA, Hamann D. Antibodies to citrullinated human fibrinogen (ACF) have diagnostic and prognostic value in early arthritis. Ann Rheum Dis. 2005;64:1199–1204. doi: 10.1136/ard.2004.029389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhao X, Okeke NL, Sharpe O, Batliwalla FM, Lee AT, Ho PP, Tomooka BH, Gregersen PK, Robinson WH. Circulating immune complexes contain citrullinated fibrinogen in rheumatoid arthritis. Arthritis Res Ther. 2008;10:R94. doi: 10.1186/ar2478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sánchez-Pernaute O, López-Armada MJ, Calvo E, Díez-Ortego I, Largo R, Egido J, Herrero-Beaumont G. Fibrin generated in the synovial fluid activates intimal cells from their apical surface: a sequential morphological study in antigen-induced arthritis. Rheumatology (Oxford) 2003;42:19–25. doi: 10.1093/rheumatology/keg021. [DOI] [PubMed] [Google Scholar]
- 14.Sánchez-Pernaute O, Largo R, Calvo E, Alvarez-Soria MA, Egido J, Herrero-Beaumont G. A fibrin based model for rheumatoid synovitis. Ann Rheum Dis. 2003;62:1135–1138. doi: 10.1136/ard.2003.011767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hill JA, Al-Bishri J, Gladman DD, Cairns E, Bell DA. Serum autoantibodies that bind citrullinated fibrinogen are frequently found in patients with rheumatoid arthritis. J Rheumatol. 2006;33:2115–2119. [PubMed] [Google Scholar]
- 16.Vander Cruyssen B, Cantaert T, Nogueira L, Clavel C, De Rycke L, Dendoven A, Sebag M, Deforce D, Vincent C, Elewaut D, et al. Diagnostic value of anti-human citrullinated fibrinogen ELISA and comparison with four other anti-citrullinated protein assays. Arthritis Res Ther. 2006;8:R122. doi: 10.1186/ar2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sebbag M, Moinard N, Auger I, Clavel C, Arnaud J, Nogueira L, Roudier J, Serre G. Epitopes of human fibrin recognized by the rheumatoid arthritis-specific autoantibodies to citrullinated proteins. Eur J Immunol. 2006;36:2250–2263. doi: 10.1002/eji.200535790. [DOI] [PubMed] [Google Scholar]
- 18.Pérez ML, Gómara MJ, Ercilla G, Sanmartí R, Haro I. Antibodies to citrullinated human fibrinogen synthetic peptides in diagnosing rheumatoid arthritis. J Med Chem. 2007;50:3573–3584. doi: 10.1021/jm0701932. [DOI] [PubMed] [Google Scholar]
- 19.Kuhn KA, Kulik L, Tomooka B, Braschler KJ, Arend WP, Robinson WH, Holers VM. Antibodies against citrullinated proteins enhance tissue injury in experimental autoimmune arthritis. J Clin Invest. 2006;116:961–973. doi: 10.1172/JCI25422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hueber W, Kidd BA, Tomooka BH, Lee BJ, Bruce B, Fries JF, Sønderstrup G, Monach P, Drijfhout JW, van Venrooij WJ, et al. Antigen microarray profiling of autoantibodies in rheumatoid arthritis. Arthritis Rheum. 2005;52:2645–2655. doi: 10.1002/art.21269. [DOI] [PubMed] [Google Scholar]
- 21.Eisen MB, Spellman PT, Brown PO, Botstein D. Cluster analysis and display of genome-wide expression patterns. Proc Natl Acad Sci U S A. 1998;95:14863–14868. doi: 10.1073/pnas.95.25.14863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deng GM, Zheng L, Chan FK, Lenardo M. Amelioration of inflammatory arthritis by targeting the pre-ligand assembly domain of tumor necrosis factor receptors. Nat Med. 2005;11:1066–1072. doi: 10.1038/nm1304. [DOI] [PubMed] [Google Scholar]
- 23.Emery P. The Dunlop-Dottridge Lecture: prognosis in inflammatory arthritis: the value of HLA genotyping and the oncological analogy. J Rheumatol. 1997;24:1436–1442. [PubMed] [Google Scholar]
- 24.Nakamura RM. Progress in the use of biochemical and biological markers for evaluation of rheumatoid arthritis. J Clin Lab Anal. 2000;14:305–313. doi: 10.1002/1098-2825(20001212)14:6<305::AID-JCLA10>3.0.CO;2-P. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rönnelid J, Wick MC, Lampa J, Lindblad S, Nordmark B, Klareskog L, van Vollenhoven RF. Longitudinal analysis of citrullinated protein/peptide antibodies (anti-CP) during 5 year follow up in early rheumatoid arthritis: anti-CP status predicts worse disease activity and greater radiological progression. Ann Rheum Dis. 2005;64:1744–1749. doi: 10.1136/ard.2004.033571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wipke BT, Wang Z, Nagengast W, Reichert DE, Allen PM. Staging the initiation of autoantibody-induced arthritis: a critical role for immune complexes. J Immunol. 2004;172:7694–7702. doi: 10.4049/jimmunol.172.12.7694. [DOI] [PubMed] [Google Scholar]
- 27.Verpoort KN, Jol-van der Zijde CM, Papendrecht-van der Voort EA, Ioan-Facsinay A, Drijfhout JW, van Tol MJ, Breedveld FC, Huizinga TW, Toes RE. Isotype distribution of anti-cyclic citrullinated peptide antibodies in undifferentiated arthritis and rheumatoid arthritis reflects an ongoing immune response. Arthritis Rheum. 2006;54:3799–3808. doi: 10.1002/art.22279. [DOI] [PubMed] [Google Scholar]
- 28.Makrygiannakis D, af Klint E, Lundberg IE, Löfberg R, Ulfgren AK, Klareskog L, Catrina AI. Citrullination is an inflammation-dependent process. Ann Rheum Dis. 2006;65:1219–1222. doi: 10.1136/ard.2005.049403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Klareskog L, Rönnelid J, Lundberg K, Padyukov L, Alfredsson L. Immunity to citrullinated proteins in rheumatoid arthritis. Annu Rev Immunol. 2008;26:651–675. doi: 10.1146/annurev.immunol.26.021607.090244. [DOI] [PubMed] [Google Scholar]
- 30.Kidd BA, Ho PP, Sharpe O, Zhao X, Tomooka BH, Kanter JL, Steinman L, Robinson WH. Epitope spreading to citrullinated antigens in mouse models of autoimmune arthritis and demyelination. Arthritis Res Ther. 2008;10:R119. doi: 10.1186/ar2523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chapuy-Regaud S, Sebbag M, Baeten D, Clavel C, Foulquier C, De Keyser F, Serre G. Fibrin deimination in synovial tissue is not specific for rheumatoid arthritis but commonly occurs during synovitides. J Immunol. 2005;174:5057–5064. doi: 10.4049/jimmunol.174.8.5057. [DOI] [PubMed] [Google Scholar]
- 32.Vossenaar ER, Smeets TJ, Kraan MC, Raats JM, van Venrooij WJ, Tak PP. The presence of citrullinated proteins is not specific for rheumatoid synovial tissue. Arthritis Rheum. 2004;50:3485–3494. doi: 10.1002/art.20584. [DOI] [PubMed] [Google Scholar]
- 33.Vossenaar ER, Nijenhuis S, Helsen MM, van der Heijden A, Senshu T, van den Berg WB, van Venrooij WJ, Joosten LA. Citrullination of synovial proteins in murine models of rheumatoid arthritis. Arthritis Rheum. 2003;48:2489–2500. doi: 10.1002/art.11229. [DOI] [PubMed] [Google Scholar]
- 34.Lundberg K, Nijenhuis S, Vossenaar ER, Palmblad K, van Venrooij WJ, Klareskog L, Zendman AJ, Harris HE. Citrullinated proteins have increased immunogenicity and arthritogenicity and their presence in arthritic joints correlates with disease severity. Arthritis Res Ther. 2005;7:R458–R467. doi: 10.1186/ar1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vossenaar ER, Zendman AJ, van Venrooij WJ, Pruijn GJ. PAD, a growing family of citrullinating enzymes: genes, features and involvement in disease. Bioessays. 2003;25:1106–1118. doi: 10.1002/bies.10357. [DOI] [PubMed] [Google Scholar]
- 36.Dumonde DC, Glynn LE. The production of arthritis in rabbits by an immunological reaction to fibrin. Br J Exp Pathol. 1962;43:373–383. [PMC free article] [PubMed] [Google Scholar]
- 37.Hida S, Miura NN, Adachi Y, Ohno N. Influence of arginine deimination on antigenicity of fibrinogen. J Autoimmun. 2004;23:141–150. doi: 10.1016/j.jaut.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 38.Rubin B, Sønderstrup G. Citrullination of self-proteins and auto-immunity. Scand J Immunol. 2004;60:112–120. doi: 10.1111/j.0300-9475.2004.01457.x. [DOI] [PubMed] [Google Scholar]
- 39.Robinson WH, DiGennaro C, Hueber W, Haab BB, Kamachi M, Dean EJ, Fournel S, Fong D, Genovese MC, de Vegvar HE, et al. Autoantigen microarrays for multiplex characterization of autoantibody responses. Nat Med. 2002;8:295–301. doi: 10.1038/nm0302-295. [DOI] [PubMed] [Google Scholar]
- 40.Hill JA, Bell DA, Brintnell W, Yue D, Wehrli B, Jevnikar AM, Lee DM, Hueber W, Robinson WH, Cairns E. Arthritis induced by posttranslationally modified (citrullinated) fibrinogen in DR4-IE transgenic mice. J Exp Med. 2008;205:967–979. doi: 10.1084/jem.20072051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Korganow AS, Ji H, Mangialaio S, Duchatelle V, Pelanda R, Martin T, Degott C, Kikutani H, Rajewsky K, Pasquali JL, et al. From systemic T cell self-reactivity to organ-specific autoimmune disease via immunoglobulins. Immunity. 1999;10:451–461. doi: 10.1016/s1074-7613(00)80045-x. [DOI] [PubMed] [Google Scholar]
- 42.Matsumoto I, Lee DM, Goldbach-Mansky R, Sumida T, Hitchon CA, Schur PH, Anderson RJ, Coblyn JS, Weinblatt ME, Brenner M, et al. Low prevalence of antibodies to glucose-6-phosphate isomerase in patients with rheumatoid arthritis and a spectrum of other chronic autoimmune disorders. Arthritis Rheum. 2003;48:944–954. doi: 10.1002/art.10898. [DOI] [PubMed] [Google Scholar]
- 43.Sakaguchi N, Takahashi T, Hata H, Nomura T, Tagami T, Yamazaki S, Sakihama T, Matsutani T, Negishi I, Nakatsuru S, Sakaguchi S. Altered thymic T-cell selection due to a mutation of the ZAP-70 gene causes autoimmune arthritis in mice. Nature. 2003;426:454–460. doi: 10.1038/nature02119. [DOI] [PubMed] [Google Scholar]
- 44.Trentham DE, Townes AS, Kang AH. Autoimmunity to type II collagen an experimental model of arthritis. J Exp Med. 1977;146:857–868. doi: 10.1084/jem.146.3.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Choi EK, Gatenby PA, McGill NW, Bateman JF, Cole WG, York JR. Autoantibodies to type II collagen: occurrence in rheumatoid arthritis, other arthritides, autoimmune connective tissue diseases, and chronic inflammatory syndromes. Ann Rheum Dis. 1988;47:313–322. doi: 10.1136/ard.47.4.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cook AD, Rowley MJ, Mackay IR, Gough A, Emery P. Antibodies to type II collagen in early rheumatoid arthritis. Correlation with disease progression. Arthritis Rheum. 1996;39:1720–1727. doi: 10.1002/art.1780391015. [DOI] [PubMed] [Google Scholar]
- 47.Terato K, Shimozuru Y, Katayama K, Takemitsu Y, Yamashita I, Miyatsu M, Fujii K, Sagara M, Kobayashi S, Goto M, et al. Specificity of antibodies to type II collagen in rheumatoid arthritis. Arthritis Rheum. 1990;33:1493–1500. doi: 10.1002/art.1780331006. [DOI] [PubMed] [Google Scholar]
- 48.Tarkowski A, Klareskog L, Carlsten H, Herberts P, Koopman WJ. Secretion of antibodies to types I and II collagen by synovial tissue cells in patients with rheumatoid arthritis. Arthritis Rheum. 1989;32:1087–1092. doi: 10.1002/anr.1780320906. [DOI] [PubMed] [Google Scholar]
- 49.Rönnelid J, Lysholm J, Engström-Laurent A, Klareskog L, Heyman B. Local anti-type II collagen antibody production in rheumatoid arthritis synovial fluid. Evidence for an HLA-DR4-restricted IgG response. Arthritis Rheum. 1994;37:1023–1029. doi: 10.1002/art.1780370707. [DOI] [PubMed] [Google Scholar]
- 50.Burkhardt H, Sehnert B, Bockermann R, Engström A, Kalden JR, Holmdahl R. Humoral immune response to citrullinated collagen type II determinants in early rheumatoid arthritis. Eur J Immunol. 2005;35:1643–1652. doi: 10.1002/eji.200526000. [DOI] [PubMed] [Google Scholar]
- 51.Uysal H, Bockermann R, Nandakumar KS, Sehnert B, Bajtner E, Engström A, Serre G, Burkhardt H, Thunnissen MM, Holmdahl R. Structure and pathogenicity of antibodies specific for citrullinated collagen type II in experimental arthritis. J Exp Med. 2009;206:449–462. doi: 10.1084/jem.20081862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Salvi R, Péclat V, So A, Busso N. Enhanced expression of genes involved in coagulation and fibrinolysis in murine arthritis. Arthritis Res. 2000;2:504–512. doi: 10.1186/ar132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Marty I, Péclat V, Kirdaite G, Salvi R, So A, Busso N. Amelioration of collagen-induced arthritis by thrombin inhibition. J Clin Invest. 2001;107:631–640. doi: 10.1172/JCI11064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Han MH, Hwang SI, Roy DB, Lundgren DH, Price JV, Ousman SS, Fernald GH, Gerlitz B, Robinson WH, Baranzini SE, et al. Proteomic analysis of active multiple sclerosis lesions reveals therapeutic targets. Nature. 2008;451:1076–1081. doi: 10.1038/nature06559. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.