Abstract
Musculoskeletal conditions of the foot and ankle are an important public health challenge due to their increasing incidence combined with their substantial negative impact on patients’ quality of life. Non-pharmacological treatments serve as the first line of treatment and are frequently used for patients with musculoskeletal conditions of the foot and ankle. This review provides a summary of the assessments and non-invasive treatment options based upon available evidence.
Recent studies show that individuals with foot and ankle pain have multiple co-existing impairments in alignment, motion, load distribution and muscle performance that may be evident in static and/or dynamic tasks. Additionally, both clinical and epidemiological studies support the inter-dependence between the foot and proximal joints. For instance, aberrant foot structure has been linked to foot osteoarthritis (OA), as well as OA and pain at the knee and hip. Most recently, advances in motion capture technology and plantar load distribution measurement offer opportunities for precise dynamic assessments of the foot and ankle.
In individuals with musculoskeletal conditions of the foot and ankle, the chief objectives of treatment are to afford pain relief, restore mechanics (alignment, motion and/or load distribution) and return the patient to their desired level of activity participation. Given that most patients present with multiple impairments, combinational therapies that target foot-specific as well as global impairments have shown promising results. In particular, in individuals with rheumatoid arthritis and other rheumatic diseases, comprehensive rehabilitation strategies including early detection, foot-based interventions (such as orthoses) and wellness-based approaches for physical activity and self-management have been successful.
While significant improvements have been made in the last decade to the assessment and treatment of foot and ankle conditions, few randomized clinical trials specifically have investigated patients with foot or ankle conditions to provide global insights into this area. Consequently, current recommendations vary based upon the scope of studies presented in this review as well as the strength of studies. This review indicates a need for more in-depth investigations into the components of assessment and treatment options for foot and ankle musculoskeletal conditions.
Keywords: Foot, ankle, musculoskeletal, treatment, rheumatoid arthritis, osteoarthritis, footwear
1. INTRODUCTION AND PURPOSE
Foot and ankle conditions are major public health problems, and with the increasing numbers of older adults in the population, the burden of these problems will escalate. In persons with rheumatoid arthritis (RA), these conditions are about double the rates observed in the general population. Yet, foot and ankle conditions have thus far received minimal attention by rheumatology professionals. Compared to non-invasive corrections for joint malalignment at the knee and hip, very little work has focused on the foot and non-surgical foot interventions that might benefit foot pain and related rheumatic diseases. The purpose of this review is to provide an overview of current knowledge on ankle and foot musculoskeletal conditions with a focus on assessment and noninvasive, non-pharmacology treatment options. In the following sections, we will present assessment and treatment of foot pain and ankle pain separately. However, it is conceivable that foot and ankle problems are related, and the concept of regional interdependence is introduced to address the overlap in musculoskeletal conditions of the foot and ankle with respect to assessment and treatment. While this review is not a systematic review of the literature, it is intended to provide a comprehensive review of common assessments and non-pharmacologic treatment strategies of foot and ankle pain in adults.
2. FOOT PAIN
2A. OVERVIEW
Foot pain has emerged as a significant clinical and public health challenge due to its high prevalence and substantial negative impact on physical function and quality of life. Foot pain affects 20–37% of community dwelling adults 45 years and older [1–3]. In older adults without disabling foot pain at baseline, 8.1% reported it at 3 year follow up [4]. Individuals with foot pain experience significant physical disability [2, 5], have difficulty with activities of daily living [6] and are at increased of falling [7]. Foot pain has a substantial negative impact on general and foot specific quality of life [8, 9].
The etiology of foot pain is multi-factorial, and poor footwear choices may play a key role in its development [10–12]. Wearing shoes that are too small [12] or shoes that lack support and sound structure (high heels, sandals, slippers) has been associated with foot pain [10]. In recent years, an increase in the incidence of foot injuries secondary to motor vehicle trauma has been noted with the advent of airbags and seat belts [13]. The plantar impact sustained by restrained front seat passengers may cause injury including ligamentous disruption and metatarsal fractures[14]. In particular, an increase in the frequency and severity of tarso-metatarsal, talo-navicular and ankle joints has been reported with motor vehicle trauma [15]. Foot pain may also be related to the presence of health conditions (e.g. RA, gout or osteoarthritis (OA)) or involve specific body structures (e.g. plantar fasciitis, Morton’s neuroma). A recent study evaluating the prevalence of foot symptoms in individuals with RA noted that 93.5% of respondents had experienced foot pain, and 35.4% reported that foot pain was their presenting symptom [16]. In patients with acute gout flares, 70% (14/20) reported foot pain and disability [17]. Severity of foot pain has shown a modest association with the presence of osteophytes [18] and higher body mass index (BMI) [19] in individuals with 1st metatarso-phalangeal joint OA.
2B. CLINICAL ASSESSMENT
Patient Reported Outcome Measures (PROMs)
The presence of generalized foot pain is usually documented by the care provider during a physical examination [17, 20], or using interviewer-administered [2] or self-response questionnaires [4]. Questionnaires and surveys have also been used to quantify the severity of pain and assess patients’ self-reported foot function and disability. Foot-specific outcomes instruments often have subscales that evaluate pain, pain severity, activity limitation, foot function and psychosocial issues [21], as well as participation in sports [22]. Two recent systematic reviews have critically evaluated surveys that are currently used: one summarized surveys used in individuals with RA [23] and the other encompasses clinical and population-based studies [24]. These reviews suggest that while several instruments are available, few have been studied extensively to establish their psychometric properties (for e.g. Foot Function Index, Leeds Foot Impact Scale). In particular, limited evidence is available regarding responsiveness to change following non-operative and non-pharmacologic interventions. While most region-specific PROMs include both, the foot and ankle, some are specific to a region or clinical population (Table 1). In clinical practice, the Lower Extremity Functional Scale (LEFS), though not foot-specific, is often used, given that its reliability, construct validity and 90% confidence interval of minimal detectable change (MDC90) have been previously established [25, 26].
Table 1.
Content of patient-reported ankle health questionnaires.
| Ankle Pain | Ankle Function | Functional Limitation/Disability | Self-Perception Body Image | Psychological | Social | Orthotics/Shoewear/Bracing | Sport or Exercise Related | |
|---|---|---|---|---|---|---|---|---|
| American Academy of Orthopedic Surgeons Foot and Ankle Score [128] | + | + | + | − | − | − | + | + |
| Ankle Instability Instrument [139] | − | + | + | − | − | − | − | + |
| Ankle OA Scale [129] | + | − | + | − | − | − | + | − |
| Ankle Scoring Scale (Karlsson) [132] | + | + | + | − | − | − | − | + |
| Cumberland Ankle Instability Tool [138] | + | + | + | − | − | − | − | + |
| Foot and Ankle Ability Measure (FAAM) [22] | − | + | + | − | − | − | − | + |
| Foot and Ankle Disability Index (FADI) [131] | + | − | + | − | − | − | − | + |
| Foot and Ankle Outcome Score (FAOS) [133] | + | + | + | − | + | − | − | + |
| Juvenile Arthritis Foot Disability Index (JAFI) [141] | + | − | + | − | + | + | + | + |
| Kaikkonen Scale [135] | − | + | + | − | − | − | − | + |
| Lower Extremity Function Score (Ankle) [25, 26, 142] | − | − | + | − | − | − | + | + |
| Olerud and Molander Ankle Score [140] | + | + | + | − | − | − | − | + |
Key Aspects of the Clinical Examination
A clinical examination of the foot includes ‘traditional’ components such as history, palpation, and assessments of sensation, range of motion and strength, as well as special tests that provoke specific tissues. On observation, toe deformities and skin health (dryness, sweating, perfusion) should be noted. A detailed review of foot examination techniques and their reliability has been presented by Wrobel and Armstrong (2008)[27]. Salient features are highlighted in subsequent paragraphs.
Static Foot Structure and Alignment
Foot structure has been quantified in terms of the alignment of the medial longitudinal arch, as well as by characterizing foot types (Figure 1). However, the predictive value of arch alignment remains contentious [28], and objective data quantifying the diagnostic accuracy (sensitivity, specificity, receiver operating characteristic, or ROC, curves) of arch alignment are lacking. Arch alignment has been assessed using clinical (palpation-based), radiographic and foot-print based methods that have varying levels of reliability and validity. Radiographic measures are considered the “gold standard” measure of arch alignment but are susceptible to measurement errors due to magnification and beam positioning [29]. Due to its high concurrent validity and relative ease of use, navicular height is frequently used in clinical practice [30]. Arch height index, defined as the ratio of dorsum height to truncated foot length, can be measured using a relatively low-cost jig and offers both, high reliability and concurrent validity [31]. Hybrid methods that combine two or more assessments of arch alignment, such as the Foot Posture Index, a six item rating system [32] and a screening protocol, combining clinical and radiographic methods [33] have been proposed.
Figure 1.
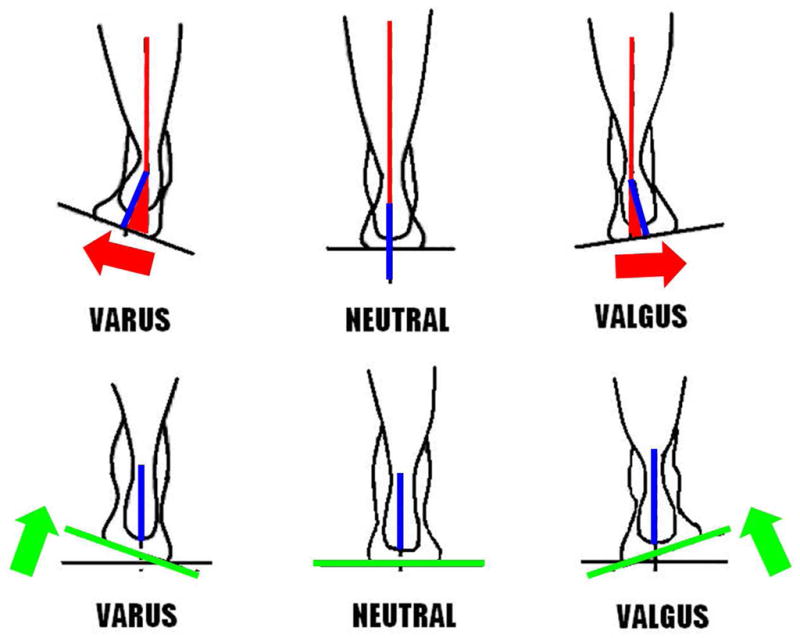
The traditional approach proposed by Root et al. focused on identifying and correcting foot malalignment. Ideal foot alignment was defined as “subtalar neutral”, the position in which the calcaneal bisection (blue line) is parallel with the bisection of the lower third of the leg (red line), and 2) the plane passing through all five metatarsal heads (green line) is perpendicular to the calcaneal bisection (blue line). Based on the relationship of the rearfoot and forefoot in subtalar neutral, chief malalignments include rearfoot varus and valgus (top row), forefoot varus and valgus (bottom row) are identified. Adapted from [76].
Aberrant foot structure such as an elevated first ray [34, 35], hypermobile first ray [36] and long second metatarsal [37] have been linked with the development of 1st metatarso-phalangeal joint OA, hallux valgus and midfoot OA respectively. Aberrant foot structure has also been linked to the development of pain and OA changes at the knee and hip (Figure 2). Gross et al. found a modest relationship between forefoot varus and ipsilateral hip pain [38]. Limbs with low arched feet had 1.3 times the odds of knee pain [39]. Self-reported toe out may play a significant role in the development radiographic medial patella-femoral knee OA [40].
Figure 2.
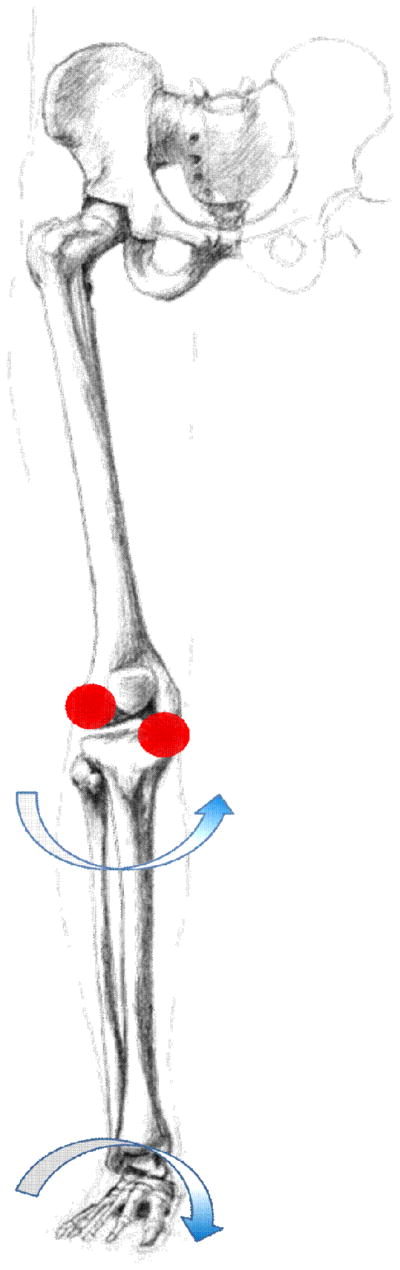
Theorized links between foot (arch alignment), knee and hip mechanics. Low arch alignment and consequent tibial internal rotation have been linked to the development of medial knee pain.
Joint Range of Motion
Joint range of motion, quantified using a goniometer with one degree resolution, has shown good reliability at the 1st metatarso-phalangeal joint [41] and subtalar joint [42]. The ankle is reviewed in detail in the subsequent sections. The rater should note the position used to perform testing (supine, prone or seated), method of stabilizing proximal joints, and whether the measurement was obtained in the weight-bearing position, to improve consistency.
Muscle Performance
Muscle strength, quantified using a hand hand-held dynamometer, has demonstrated good reliability (Intra-rater (0.78–0.94) and Inter-rater (0.77–0.88)). Intraclass Correlation Coefficient (3,1), respectively) [43]. Standardized patient positioning and dynamometer placement are key to achieving inter-rater consistency. Decreased toe flexor strength and foot pain are independently associated with fall risk [7, 9]. Strength deficits have also been reported in individuals with foot pain secondary to tibialis posterior tendinopathy [44, 45].
Footwear assessment
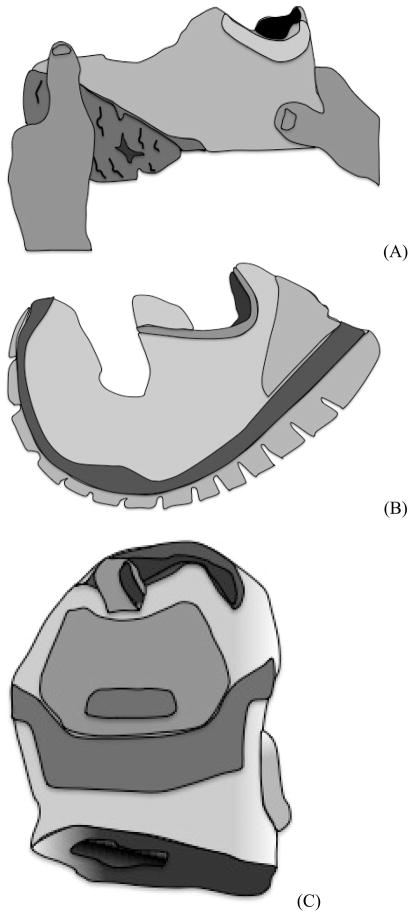
Footwear should be inspected for fit (length and width) and design features such as the presence of a heel cup, arch support, torsional and toe-break flexibility (Figure 3). Patterns of wear on the sole of the shoe and/or or scuffing should be noted. The Footwear Assessment Form is a simple and well-organized tool with established reliability and face-validity [46]. Additional work may be needed to establish its suitability across cultures and clinical populations. Individuals’ perception of footwear comfort can be assessed using the Footwear Comfort Scale [47].
Figure 3.
Clinical assessment of A) torsional flexibility, B) toe break flexibility and C) wear patterns. Wear patterns assessed with the shoes on a flat surface indicate excessive lateral wear.
Dynamic Assessment of Foot Motion (including Gait Analysis)
Dynamic assessment of foot function involves an observational or quantitative assessment of foot and lower extremity mechanics during a weight-bearing task (e.g., walking, running, single limb squat, step down). Dynamic assessments are particularly relevant in a clinical foot exam because evidence indicates that there is only a weak relationship between static and dynamic measures of arch height [48–50] and large between-person variability [51]. The reliability of observational assessments has been questioned by some authors [52], while others have found acceptable reliability [48, 50, 53] using video-based gait analysis. The studies that found acceptable reliability used ordinal scales to quantify dynamic foot alignment [53] and standardized video position and measurement procedures [48, 50]. Advances in three-dimensional motion capture technology have provided higher resolution and large capture volume, and afford the opportunity to simultaneously assess in vivo segmental foot motion concurrently with the motion of larger proximal joints [54–56].
Dynamic Assessment of Plantar Load Distribution
When performing a clinical assessment, the plantar aspect of the foot should be inspected for patterns of calluses and weight-bearing. More recently, load distribution (plantar pressure) at the foot-floor or the foot-shoe interface has been quantified during functional activities such as walking, stair ascent and descent and running [57, 58]. The reliability of both, barefoot as well as in-shoe pressure measuring devices has been established [59–61]. Early applications of this technology focused on individuals with diabetes and neuropathy who demonstrate loss of protective sensation. The evaluation of the at-risk diabetic foot is covered in an excellent review [62], and thus, will not be described in this paper. More recently, in individuals with foot pain, elevated and prolonged plantar loading has been postulated to contribute to the evolution of patients’ self-reported pain. Consistent with this mechanical overloading theory, recent reports have found increased regional plantar pressure accompanying foot pain [63, 64] In contrast, some authors postulate that individuals experiencing foot pain adopt an antalgic strategy to avoid exacerbating their foot pain. For instance, individuals with 1st metetarso-phalangeal OA may shift their weight laterally in an attempt to unload the painful region during walking [65]. Similarly, lower lateral forefoot loading has been reported in patients with RA and low Health Assessment Questionnaire (HAQ) score (more disability, more pain) compared to RA patients with high HAQ scores [66]. While pressure measurement technology and appropriate measurement methods are increasingly common in clinical and population-based research studies, their use in routine clinical practice is infrequent.
Provocational Tests
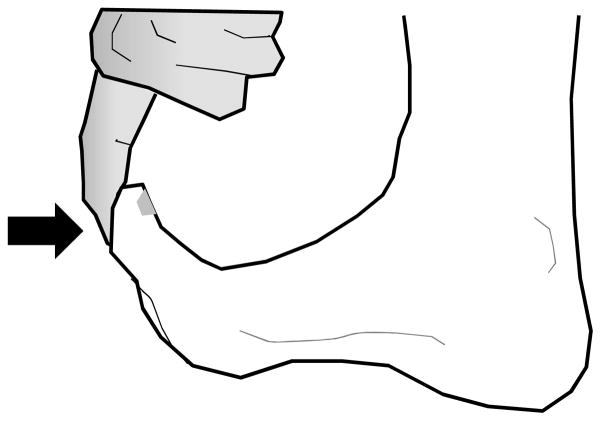
The final part of the clinical examination comprises provocational tests that provoke specific tissues. The Windlass test (Figure 4) is used to stretch the plantar fascia and is considered positive if the patient reports pain when the 1st metatarso-phalanegeal joint is passively dorsiflexed [67, 68]. Limited extensibility in the gastrocnemius-soleus complex or the flexor hallucis longus can be assessed using passive muscle length testing. Symptoms related to the sesamoids may manifest as plantar pain and localized tenderness to palpation. Custom devices have been developed to objectively quantify 1st ray dorsal mobility [69, 70] and 1st metatarso-phalangeal joint mobility [71] in in vivo research studies; however these devices are not in widespread use in clinical practice.
Figure 4.
Flexor Hallucis Longus tightness. First, the interphalangeal joint extended and dorsiflexion of the 1st metatarsophalangeal joint is measured. Next, the interphalangeal joint is flexed and dorsiflexion of the 1st metatarsophalangeal joint is measured. If the latter is greater than the former, tightness of the Flexor Hallucis Longus muscle may present. Dorsiflexion of the 1st metatarsophalangeal joint may also stretch the plantar fascia in which case pain is reported in the middle the heel (Windlass test).
2C. TREATMENT OF FOOT PAIN
Overview and General Approach
The primary aim of treatment is to afford pain relief, restore mechanics (alignment, motion and/or load distribution) and return the patient to their desired level of activity participation. The plan of care should be designed with the goal of targeting impairments noted during assessment. The most frequently used treatment modalities in this clinical population include orthoses and footwear, stretching and therapeutic exercises, manual therapy, taping and combinational therapies, and are discussed in detail in subsequent subsections.
Orthoses and Footwear
Over the last decade, significant evolution has occurred in clinical decision-making related to the prescription of foot orthoses. Three theoretical approaches can be distinguished. The traditional approach proposed by Root et al. [72] focused on identifying impairments in foot alignment and used orthoses to restore static and dynamic foot alignment. Subtalar neutral position, operationally defined as the position in which the calcaneal bisection is parallel with the bisection of the lower third of the leg, and 2) the plane passing through all five metatarsal heads is perpendicular to the calcaneal bisection, was considered ideal foot alignment [72]. Based on the relationship of the rearfoot and forefoot in subtalar neutral, four chief malalignments were delineated (rearfoot varus, rearfoot valgus, forefoot varus, forefoot valgus (Figure 1)). While Root et al.’s approach had a substantial influence on orthoses prescription, increasing concerns emerged related to its reliability and validity. Studies examining the inter-rater reliability of clinicians in positioning the foot in subtalar neutral have reported measurement errors of 4 degrees, with better reliability reported in weight-bearing measures [73–77]. Measurement error is extremely important because it can lead to errors in classification of foot malalignment. Questions have been raised related to the validity of Root et al.’s classification system and limited normative data are available. For example, one study found forefoot valgus in 45% limbs assessed in women (mean age: 23 years) [78] while another group found forefoot varus in 87% limbs assessed in women (mean age: 28 years) [79]. Lastly, while Root et al. postulated that static foot alignment and dynamic foot function are strongly linked, objective evidence has challenged the predictive value of static alignment. In asymptomatic adults, Root-based static foot alignment was not significantly related to dynamic foot motion [80].
As an alternative, the Tissue Stress Model has been proposed as a paradigm to guide the evaluation and management of foot disorders [81]. This model is based on an individual-specific load deformation curve and postulates that deformation within the elastic region of the curve will not provoke symptoms. However, tissue stress in the micro-failure or plastic region of the load deformation curve may result in injury and inflammation. Consequently, tissue-specific interventions [82, 83] incorporating orthoses, stretching and targeted exercises have been proposed in individuals with foot pain. Similarly, the Preferred Movement Pathway theory proposes that that orthoses do not function by realigning the skeleton but rather by altering input signals (forces) acting on the foot during the stance phase and resultant muscle activation [84]. Additional evidence is needed to establish the utility of these theoretical models in clinical decision-making.
Orthoses and footwear have been postulated to relieve foot pain by restoring alignment [85], redistributing plantar loads [86] or limiting motion and ‘splinting’ the painful joints [87]. In individuals with midfoot pain, footwear modifications such as steel shanked shoes and rocker shoes are prescribed to limit motion at the painful joints [88]. However, these modifications are often cosmetically unacceptable, resulting in poor compliance with therapeutic footwear. As an alternative, low profile and stiff carbon graphite orthoses have been used in this population more recently [87, 89]. In individuals with tibialis posterior tendinopathy, braces incorporating design features (e.g. air bladder) that allow subject-specific correction of aberrant foot motion are available. Objective data suggests that while braces have a robust effect on correcting hindfoot eversion in individuals with tibialis posterior tendinopathy, their effect in controlling forefoot abduction may be variable [90].
A recent systematic review indicates that custom foot orthoses should be used judiciously in the treatment of foot pain [91]. Yet, custom-made foot orthoses were effective for painful pes cavus and rearfoot pain in rheumatoid arthritis (studies show a remarkably small number needed-to-treat of only 4–5 patients for either of these specific conditions to show a benefit). Custom orthoses were as effective as over-the-counter orthoses in juvenile idiopathic arthritis, and surgery was more effective than custom orthoses in painful hallux valgus [91]. There is no evidence to support the use of custom orthoses in plantar heel pain [92]. While the use of custom orthoses has been accompanied by very few side effects, they can be expensive ($300–700 per pair) and their efficacy can be variable. Some authors have suggested the use of a treatment direction test to predict determine whether orthoses will be successful in providing pain relief [93]. Briefly, the patient’s history and physical examination are used to identify specific tasks that provoke symptoms. Taping is applied (low dye taping, with felt pads if needed), and if the patient reports greater than 50% resolution of symptoms, orthoses are prescribed. If the patient reports modest symptomatic relief with taping, orthoses are unlikely to be effective.
Taping
In individuals with plantar heel pain (plantar fasciitis), low dye taping has been used to provide short-term pain relief. In a recent clinical trial, week-long application of low-dye taping produced a small but significant reduction in ‘first-step’ pain compared with sham ultrasound [94]. This trial also noted that 28% of patients treated with taping reported mild to moderate adverse effects such as discomfort from the tape being too tight, emergence of a new pain or an allergic reaction. Adverse reactions may limit compliance with taping. More recently, taping has been used to determine if the patient is a candidate for custom orthoses (see Treatment Direction Test in the section on Orthoses and Footwear above).
Stretching
Stretching is a key component of rehabilitation interventions for foot pain, particularly in individuals with heel pain. Stretching protocols in heel pain involve weight-bearing and non-weight bearing calf stretches and a plantar fascia stretch performed with the patient seated The patient is instructed to perform at least 10 repetitions of each stretch, with a 10–20 second hold, at least twice a day [82]. In a recent clinical trial, tissue-specific plantar fascia stretching demonstrated superior pain relief and improvement self-reported outcomes at eight week follow up compared to calf stretching [82].
Therapeutic Exercise
Targeted as well as generalized strength training have been prescribed for individuals with foot pain, and have been associated with positive outcomes. In individuals with tibialis posterior tendinopathy, participation in a structured, 10–12 week eccentric strengthening program was associated with symptomatic relief and improvement in physical function [95, 96]. In a recent clinical trial, a home based program of foot and ankle exercises combined with routine footcare demonstrated a 36% reduction in falls rate in community dwelling older adults [97]. In addition to exercises, this community based intervention included orthoses, advice on and subsidy for footwear, a falls prevention education booklet, and routine foot care for 12 months. Additional examples of stretching and therapeutic exercises are presented in the section on Combinational Therapy below.
Manual Therapy
Manual therapy includes soft tissue techniques (such as trigger point release, strain counterstrain) and joint mobilizations to address restrictions at the foot (subtalar, talo-crural and inter-tarsal joints) as well as proximal joints (hip, knee, ankle) [26]. Promising recent studies indicate that soft tissue mobilization may provide short-term pain relief in individuals with heel pain. The addition of myofascial trigger point release to a self-stretching protocol provided superior short-term (single session) pain relief compared to a self-stretching protocol [98]. Studies using joint mobilizations in conjunction with other modalities are covered in the section on Combinational Therapy below.
Combinational Therapy
Consistent with the concept of functional phenotypes (sub-groups) of foot pain that are characterized by the existence of multiple impairments (e.g., pain, loss of range of motion, poor muscle performance), a number of recent studies have proposed combinational therapies to alleviate pain and maximize return to activity participation. For instance, in individuals with 1st metatarso-phalangeal joint pain, the addition of sesamoid mobilization, flexor hallucis strengthening and gait training resulted in superior pain relief, restoration of range of motion and strength, compared to a control group that received physical modalities (whirlpool, ultrasound, cold packs, and electrical stimulation) and general lower extremity exercises (calf and hamstring stretching, marble pick-up exercise) [99]. Similarly, individuals with heel pain treated with combinational therapy including joint mobilizations and stretching demonstrated superior pain relief and self-reported physical function at four-week follow-up compared to those treated with electro physical agents (ultrasound and ionophoresis) and stretching [26].
Individuals with RA are particularly susceptible to foot pain, deformities and disability. Consequently, aggressive preventive and monitoring strategies have been deployed in this population. In parallel with tight disease control through medical management, early detection of forefoot pain, and diagnostic ultrasonography and corticosteroid injection therapies for localized synovitis are strongly advocated [100]. In a recent systematic review of the role of orthoses in rheumatoid arthritis, the use of rigid, full-length custom molded orthoses was accompanied by pain relief and reduction in forefoot plantar loading [101]. In addition to foot-specific interventions, rehabilitation interventions including elements of physical activity, strength training, and self-management are critical to maintaining physical health and wellness in individuals with rheumatoid arthritis [102]. While high quality evidence in the form of clinical trials is relatively scarce, two recent reviews have summarized key features of rehabilitation interventions that are beneficial in the management of individuals with rheumatoid arthritis [102, 103]. These reviews indicate that while the benefits of physical activity programs in improving outcomes in individuals with RA are well-established, limited objective data are available examining the effects of dosage and intensity. Critical aspects of successful programs include access to multi-disciplinary care, and the use of cognitive behavioral approaches, therapeutic exercise and joint protection strategies.
In summary, the management of foot pain has grown to include combinational therapies that address multiple foot-specific impairments as well as maintain physical health. While robust evidence supports the use of custom molded orthoses in individuals with rheumatoid arthritis, there is limited support for the use of custom devices in plantar heel pain or midfoot pain. Additional studies are needed to assess if non-pharmacologic interventions such as taping and soft-tissue mobilization provide long-term pain relief. There is a need for community-based and self-management interventions in individuals with foot pain.
2D. EMERGING AREAS IN THE ASSESSMENT AND TREATMENT OF FOOT PAIN
Recent research emphasizes the importance of assessing impairments in pain processing in individuals with long-standing musculoskeletal pain. In individuals with foot pain, peripheral and central pain sensitization may be quantified using pressure pain threshold [104]. Individuals with foot pain may also demonstrate fear avoidance behaviors [105], which in turn, may exacerbate the activity limitation and participation restrictions noted in this population. Increasingly, clinical and research studies support the presence of multiple, co-existing impairments in individuals with foot pain. As few prospective studies or large randomized clinical trials have been performed, a strict attention to study design will be important to aid our understanding of the causal connections between foot conditions and interventions that lessen their impact. Future studies are warranted to define functional phenotypes as well as the distinct sub-groups of individuals with foot pain. Genetic studies are sorely lacking and the delineation of foot phenotypes is the necessary step to identify individuals at greatest risk for progression and disability. While functional phenotypes of foot conditions, including pain, impairments (e.g., decrease in range of motion or poor balance, etc.) are relatively new concepts in rheumatology rehabilitation, these entities will provide the foundation to further our understanding.
3. ANKLE PAIN
3.A. OVERVIEW
Approximately 15% of middle-age and older adults have experienced ankle pain in the last month [3] and 10% of older adults show radiographic signs of ankle osteoarthritis (OA) [106]. Ankle pain and dysfunction are significant contributors to poor health outcomes with aging, such as reduced physical function [107–109], balance [107], and gait speed [109, 110] as well as increased disability [108] and fall risk [7].
The ankle joint complex, defined as the talocrucral and subtalar joints [111], contributes between 40% [112] to 70% [113] of forward propulsion during walking, but only accounts for 7–26% of the metabolic cost [114]. With a loss of ankle function, hip flexors and extensors are more heavily utilized during gait [115], increasing the physiologic expenditure [116]. This shift from relying on the ankle to relying on the hip to deliver forward propulsion during gait may explain the relatively higher energetic costs of walking that older adults experience in comparison to their younger counterparts [117]. Further, comparisons of high and low-performing community-residing older adults suggest that those with better ankle function have higher mobility and functional status relative to those with poor ankle function [109].
A common cause of ankle dysfunction is equinus, or failure to achieve 10° of dorsiflexion during gait [118]. Equinus, which results in poor ankle movement and function, can be the result of a stiffening gastrocnemius and/or soleus muscle [119]. Two important risk factors of equinus are aging and lack of physical activity, which tend to decrease flexibility [120].
Poor ankle function may also be the result of ankle osteoarthritis (OA). The prevalence of ankle OA is approximately 10% in individuals over 65 years of age [106]. The underlying etiology of ankle OA is predominately post-traumatic ankle OA, occurring in approximately 4 out of 5 cases [121]. Fracture events, mostly malleolar or tibial plafond fractures, which are often a result of motor vehicle accidents, are the most common cause of post-traumatic OA, whereas ligamentous injuries accounted for 16% of the cases [121]. Primary OA occurs in just under 10% of ankle OA cases [121].
Lastly, although acute ankle injuries are one of the leading bodily injuries that lead to emergency room visits [122], the focus of this section will be on the assessment and non-pharmacologic treatment modalities of chronic ankle dysfunction, such as that which results from equinus or arthritis.
3B. CLINICAL ASSESSMENT
Patient-reported outcome measures (PROMs)
Patient-reported outcome measures (PROMs) are instruments for assessing patients’ perceptions of their health and function [123]. Ankle PROMs typically have questions addressing the pain, mobility, function, and quality of life. As a measurement tool they are used to assess the effect of disease or injury on function and effect of treatment [123] and to determine possible meaningful changes on an individual basis [124].
A systematic review evaluating PROMs in ankle function, pain and health reported that many surveys have been utilized in outcome-based studies with little or no evidence to support their use [125]. From their work, they noted 49 different rating scales of ankle-specific instruments [125], but many PROMs lacked construct and content validity as well as reliability and evidence of responsiveness [126]. Recent systematic reviews have noted twelve ankle-related PROMs as having construct validity, reliability, and content validity (Table 1) [125–127]. However, it is important to note that most instruments do not include questions that address the psychosocial component of ankle pain and dysfunction, and only two PROMs address the role of footwear selection and orthotics [128, 129].
As the PROMs are validated in specific populations, care should be taken when utilizing PROMs to ensure the outcome measure of interest has been validated in the population and address the appropriate content domains of the study. Of the common conditions affect the ankle, five PROMs assess ankle ligament or acute injuries [130–135], four PROMs support the use of generalized orthopaedic and pathological conditions of the foot and ankle [22, 128, 131, 136, 137], two PROMs evaluate chronic ankle instability [138, 139], and one addresses ankle joint complex fractures [140], juvenile arthritis [141], lower extremity function [25, 26, 142]and ankle osteoarthritis (OA) [129]. Future directives for ankle PROMs should address the usefulness of computerized adaptive testing, which can reduce assessment time and improve the ability to compare PROM results across studies.
Key Aspects of the Clinical Examination
In addition to the patient-reported information, such as medical history and prior injuries, assessments of sensation, joint alignment, range of motion, and strength, as well as functional mobility (e.g., walking, cutting) are important when evaluating the patient with ankle pain.
Static Structure and Alignment
Foot-ankle alignment is a key factor in ankle arthritis, pain, and disability [143], has been quantified as resting calcaneal stance position (RCSP). RCSP can be evaluated using various methods, but a composite measure that includes malleolar valgus index (MVI), rearfoot alignment view, and long leg calcaneal axial view has shown high accuracy (r = 0.814) [144]. MVI is a static measurement taken with a flatbed computer scan of the plantar foot [144, 145]. MVI is calculated by dividing the distance between the center of the transmalleolar width to the foot bisection at the heel multiplied by 100. Rearfoot alignment in terms of rearfoot varus/valgus is discussed in the section on Static Structure and Alignment of the Foot (Figure 1) [146]; however, different cut-off angles are also used [147, 148]. The long leg calcaneal axial view is a radiographic technique that provides a view of the subtalar space and alignment of the calcaneus with the tibia [144, 149, 150]. Yet since these measures require extensive equipment and set-up, it can be challenging to incorporate these assessments into clinical settings.
Joint Range of Motion
Measurement techniques vary widely when assessing ankle ROM [151, 152]. Key considerations include the amount of weight bearing and the degree of knee flexion when ROM was measured, and whether ankle ROM was measured actively or passively [153–155]. ROM is typically higher in weightbearing than in non-weightbearing [156]. An example of a weightbearing measure is the Norkin and White method, in which participants place one foot in front of the other and, with their hands resting on a support, bend the knee of the forward limb in a squat as low as possible with their trunk upright and their heels on the ground [157, 158], or a weight bearing lunge [159]. As the ankle normally functions in partial or full weightbearing during movement, researchers question the external validity of ROM measured in the non-weightbearing position [156], and studies often report both a weightbearing and non-weightbearing measure of ankle ROM [153, 160, 161].
Active measures of ROM have the individual move the ankle joint through the ROM, whereas passive measures of ROM have the clinician or a device more the ankle joint through the ROM. A common problem with ankle ROM measures is the lack of consistency between examiners [151]. Although intra-rater reliabilities and intraclass correlation coefficients (ICCs) are typically greater than 0.9 regardless of the technique [152], inter-rater goniometric measurements have low to moderate (0.5–0.8) reliability, regardless of technique or rater experience [151]. Inter-rater measurements can have a difference of 7° between testers [152], which is problematic, as normal ankle dorsiflexion ROM ranges from 0° to 13.1° [162] and total ankle ROM 50°[163] to 75° [164]. The wide range of goniometer measures and the generally low reliability of these measurements points to a need for the use of standard, reliable, and valid techniques to assess ankle ROM.
Muscle Strength
Muscle strength s frequently evaluated by using manual muscle testing (MMT). MMT assesses strength using an ordinal grading scale without quantifying strength [165]. MMT at the ankle joint include heel rises, where the participant is asked to repeat heel rises as many times as possible to assess plantarflexor strength. Participants who complete more repetitions are noted as having greater strength [166]. MMT can also be assessed by the muscle’s ability to resist the examiner’s strength, with the degree of resistance categorized in ordinal rank: 5=normal, 4=good, 3=fair, 2=poor,1= trace, 0= zero or lack of contraction [167], although a number of ranking systems exist (e.g., [168, 169]). While the rating system is subjective, well-trained, experienced evaluators can make MMT highly reliable (ICCs greater than 0.93) [170]. Studies of examiner-assessed MMT also suggest that ICC variability is high range 0.58–0.92) in dorsiflexion [171] and that the frequency and severity of plantarflexion muscle weakness frequency and severity of plantarflexion muscle weakness is underestimated [172].
Instrumented measures of ankle strength and power include quantification of dorsiflexion and plantarflexion power and torque using dynamometers. When using hand-held dynamometer, the testing style can affect the reliability, as patient-initiated intra-rater and inter-rater ICCs are 0.95 or higher, whereas clinician-initiated ICCs are generally less than 0.80 [173]. The ICCs of computerized dynamometry for highest peak torque, average peak torque, power and work to range from 0.84 to 0.99[174–176]. However, Capranica et al. reported lower ICCs, ranging from 0.29 to 0.80 for average peak torque, power and work and maximum torque, but their speeds were higher at 90°/second [177], compared to 60°/second [174]. It is worthwhile to note that the patient’s trunk should be secured and the proximal segment stabilized so the patient is mechanically grounded. Muscle strength assessment is particularly relevant in individuals with ankle OA, who show substantially lower ankle plantarflexion strength [178] compared to the contralateral limb.
Proprioception
Proprioception, defined as the body’s ability to detect its movement and position, is a key component in balance and injury prevention [179]. There are two main means for testing proprioception: 1) threshold of detecting passive motion (TDPM) and 2) joint angle reproduction (JAR). TDPM testing evaluates joint kinesthesia and the body’s ability to detect passive motion in the body. Computerized dynamometers or custom-built devices [180, 181] move the ankle joint at low speeds, approximately 0.4°/s [181, 182], and the amount of sagittal or frontal plane movement that occurs before the individual detects the motion is recorded. The greater the degree of joint movement before detection, the poorer the kinesthetic awareness. In JAR testing, the ankle joint is set to a specific target angle, either passively or actively, and the participant is to replicate the angle. The number degrees away from the target angle is recorded as both a relative angle, representing an offshoot (positive angle) or a undershoot (negative angle), and an absolute angle, representing total number of degrees from the target angle [183]. While TDPM and JAR are common proprioception measures at the knee joint, at the ankle joint there is a need for continued research to understand how joint proprioception affects ankle joint function and increases fall risk and injury [182, 184].
Dynamic Assessment of Ankle Motion (including Gait Analysis)
Gait analysis (three-dimensional motion capture or two-dimensional video) may be employed to evaluate gait [185–188] or other tasks, such as jumping or cutting [189, 190]. Motion capture provides a kinematic (e.g., joint angles, displacements) assessment, and when combined with a force plate for kinetic (e.g., force data) assessment, joint moments can be determined. While these technologies can be costly, they provide a more reliable measure of movement (ICC of > 0.75 for motion capture [191]. versus to ICC < 0.75 for observational gait analysis [192]). In addition, new technologies, bi-planar x-ray fluoroscopy allows for a highly accurate and precise in vivo, measurement of joint motion [193].
Balance tests (instrumented and non-instrumented), particularly single-leg tasks, are often employed to evaluate balance deficits [194–196]. Analysis of sway patterns typically involves a measurement of the center of pressure displacement during quiet standing [197–203]. Other common functional assessments include the Star Excursion Balance Test [204, 205]figure-of-8 hop, side hop, up-down hop, and single-leg hop for distance, agility hop test [206–208].
Provocational Tests
Given the possible risk of ankle OA and high residual disability that follows acute ankle injuries, several tests are available to evaluate ankle laxity. Commonly used tests include the anterior drawer and talar tilt test to assess the integrity of the lateral ligaments [209, 210]. When injury to the tibio-fibular syndesmosis is suspected, the external rotation (Kleiger) or squeeze tests are indicated [211, 212]. However, syndesmotic tests are noted for their high specificity but relatively low sensitivity [211, 212], consequently a high index of suspicion is warranted. In recent years, ankle impingement has been recognized as a source of lateral sided ankle pain, particularly in individuals who have previously sustained an ankle sprain. While a provocational test for antero-lateral impingement has recently been published, limited sensitivity and specificity information is available as of this review [213]. Persistent deep, aching lateral sided ankle pain may be indicative of an ostochondral lesion of the talar dome. Deltoid ligament injuries are rare, consequently the differential diagnosis of medial sided ankle pain should include tibialis posterior tendinopathy [45]. Pain on the posterior aspect of the ankle may occur due to Achilles tendinopathy, posterior impingement and retro-calcaneal bursitis.
3C. TREATMENT OF ANKLE PAIN
Overview and General Approach
Similar to the treatment of foot pain, the chief objectives of treatment in individuals with ankle pain are to reduce symptoms, improve mechanics (e.g., alignment, motion and/or load distribution), and return the patient to his or her desired level of activity participation. The plan of care should be designed with the goal of targeting impairments noted during assessment. The most frequently used treatment modalities in this clinical population include stretching, manual therapy, therapeutic exercises, footwear modification and orthoses, and are discussed in detail in subsequent subsections.
Stretching
Current exercise recommendations for adults call for a minimum of 30 minutes of moderate-intensity aerobic exercise five days per week plus two days of muscle strengthening activities and two to three days of flexibility exercises [214]. Per these guidelines, flexibility exercise includes stretches that should be held 10–30 seconds to the point of tightness or slight discomfort, repeated two to four times for a total of 60 seconds per stretch [214]. Studies evaluating the effects of stretching the muscles of the ankle joint complex (e.g., gastrocnemius, soleus, anterior tibialis) have shown mixed results, with some studies suggesting ankle ROM can be enhanced [215, 216], whereas other noting no significant gains [217, 218], with a meta-analysis suggesting that the clinical relevance of stretching in asymptomatic younger adults is unknown. In contrast, studies show older adults can significantly improve ankle ROM [153–155], and that longer stretch durations per repetition (e.g., holding each stretch 60 seconds as opposed to 15 or 30 seconds) are more likely to improve ankle ROM in older adults [219]. Concomitant with the improvements in ankle ROM in older adults are improvements in passive stiffness [154, 215, 216, 220], with gait speed increasing in some studies [153, 154], but not in all [155].
Manual Therapy
Studies on the short-term effect of a single intervention of trigger point massage [221] and joint mobilization or manipulation [222] in individuals with restricted active ankle dorsiflexion showed gains of almost 5 degrees. However, high-velocity thrust manipulations have shown no significant improvements in ankle ROM [223] or in muscle activation [224] in individuals with lateral ankle sprain. As there are few studies investigating manual therapies at the ankle joint, further research is needed to evaluate its effects on ankle joint function as well as on physical function and mobility.
Therapeutic Exercise
Strengthening the ankle typically includes isometric exercises performed against an immovable object in plantarflexion, dorsiflexion, inversion and eversion, as well as dynamic resistive exercises using ankle weights, surgical tubing, or resistance bands. In particular, high resistance eccentric exercise is advocated for individuals with Achilles tendinopathy [225, 226].
Interventions combining ankle and foot exercises have also shown positive outcomes. Hartman et al. reported that a generalized exercise program with foot gymnastics improved foot and ankle function relative to the generalized exercise program without foot gymnastics [157]. The foot gymnastics included three components: (1) 2-min warm-up activity of heel land toe lifts as well as walking on heels and toes, (2) 4-min foot exercises that included moving and spreading toes, grabbing small objects (e.g., marbles), and playing different skill games with toes, and (3) 4-min static ankle stretching [157]. After 12 weeks of exercise and foot gymnastics, participants in this group showed improvements in muscle strength and gait speed over the participants who only had the generalized exercise program. Similarly, Benedetti et al. that an exercise program targeting flexibility and strength gain resulted in participants improving strength, ROM and posture, relative to non-specific exercises [161].
Therapeutic exercise in the form of Tai Chi has been accompanied by improved ankle mobility and strength. A recent meta-analysis demonstrated that Tai Chi exercise in older adults improves ankle flexor and extensor muscle strength [227], and long-term Tai Chi practitioners display better ankle proprioception relative to long-term swimmers, runners, and sedentary individuals [181]. However, a 16-week program, failed to show that Tai Chi practice benefited ankle proprioception [228]. Taken together, these results suggest that gains in ankle functionality obtained through exercise programs can improve mobility, but more research in needed to define specific features related to dosage, intensity and patient selection to optimize outcomes.
Footwear modifications and orthoses
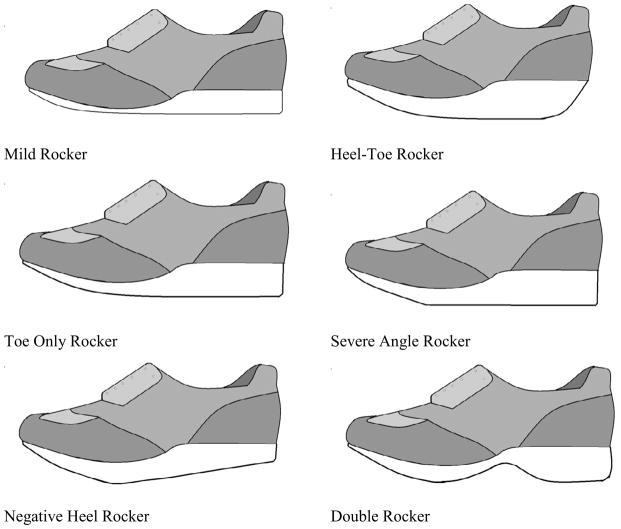
Footwear modification and orthoses have been used to treat individuals with ankle pain. In particular, rocker-style shoes have been used to treat individuals with poor ankle ROM and function. Adding rocker soles to the shoe can aid ankle motion and improves forward propulsion when sagittal plane ankle movement restricted [88, 229]. The primary role of the rocker sole shoe is to promote heel-toe gait, to limit shoe flexion to restore ankle function, and offload areas of high pressure in the foot. Of the different styles of rocker soles (Figure 5), individuals with ankle dysfunction will typically utilize heel-toe or negative heel rockers [88]. In rocker-style shoes, the pitch of the rocker should be suited to the specific ankle position (such as an ankle fixed in dorsiflexion) using a negative rocker or act within the available ankle ROM, utilizing heel-toe or negative rocker soles [88, 230]. The negative style rocker accommodates is contraindicated for those with reduced balance or with contracture of the Achilles tendon. Further, using heel lifts with mild rocker-style shoe can create a negative rocker sole and can promote a heel-toe gait [231]. In patients with arthritis, rocker-style shoes can be used alone or in tandem with a cushioned heel can aid in foot function to improve gait and ankle ROM [232]. However, determining the correct rocker position can be challenging, and in-sole plantar pressure system can be used to evaluate the effectiveness of the treatment [233].
Figure 5.
Different styles of soles in rocker shoes (adapted from [88])
Orthoses by themselves can also benefit those with ankle pain and dysfunction. Studies comparing a custom-made ankle-foot orthosis, rigid hindfoot orthosis, and articulated hindfoot orthosis reported that in patients with subtalar[234] and ankle OA[235], the rigid hindfoot orthosis provided significant ankle motion restriction, with adequate forefoot movement when walking in various conditions (e.g., on a ramp). Because of the controlled motion provided by the rigid hindfoot orthosis optimal, this treatment may be beneficial for people with ankle pain arising from subtalar or ankle OA [234, 235]. Those who benefit the most from an orthotic intervention for ankle dysfunction include men, older adults, and those with less pain [236], which suggests that alternative interventions are needed to fill the treatment gap for other populations. While substantial pain relief is afforded by devices that restrict motion, prolonged use may result in loss of joint mobility and muscle strength, and compromise the ability of the ankle to generate power at push off during walking. Consequently, there is increasing emphasis on light-weight low-profile elastic recoil ankle-foot orthoses.
3D. EMERGING AREAS IN THE ASSESSMENT AND TREATMENT OF ANKLE PAIN
Residual ankle disability and dysfunction are common following acute ankle injuries, which can lead to chronic ankle pain and mobility limitations as well as a “feeling of giving way” [237]. There is an increasing awareness that chronic ankle instability and concomitant osteochondral injuries may predispose to the development of ankle pain and OA. Consequently, early detection and high index of suspicion are warranted during assessment. Ankle ROM, strength and balance deficits are recognized as potential contributors to high fall risk in older adults. Intervention strategies should not only focus on pain relief and gait retraining, but emphasize fall prevention and neuromuscular training with the overall goal of returning the patient to their desired level of activity participation and preventing re-injury.
4. REGIONAL INTERDEPENDENCE OF THE FOOT AND ANKLE
Lower extremity function during most weight bearing activities of daily living occurs in a closed kinematic chain, and consequently may be interdependent (e.g., [238, 239]). This regional interdependence may be evident during assessment, and may offer valuable strategies for intervention. For instance, clinical studies indicate that ankle and foot mechanics may be related. In terms of assessment, limited ankle dorsiflexion (equinus deformity) has been noted in individuals with heel pain (plantar fasciitis) [240] and in individuals with forefoot or midfoot pain [162]. Consistent with these findings, combinational therapies targeting ankle dorsiflexion have been accompanied by positive outcomes in terms of pain relief and mitigation of disability in individuals with heel pain [26].
Regional interdependence may also be reflected in relationships between proximal (hip or knee) and distal (foot and ankle) function. For instance, in individuals with compromised ankle power generation during push off phase of walking (apropulsive gait strategy) increased hip flexion has been noted in order to maintain gait speed [115]. In this case, regional interdependence is reflected in proximal joints (hip flexion) compensating for reduced ankle function. In contrast, decreased proximal muscle strength has been noted in women with tibialis posterior tendinopathy [44]. In a recent study, women with tibialis posterior tendinopathy demonstrated 63% lower plantarflexor strength and 33% and 28% lower hip extensor and abductor strength respectively compared to age, gender and BMI-matched controls [44]. These findings suggest that proximal resources may not always be available to substitute for distal impairments. Pain and disuse atrophy secondary to limited physical activity may modulate the availability of proximal resources. In the section on Assessment of Foot Structure, the relationship between low arched foot structure and hip or knee pain has been discussed. In terms of intervention, recent studies have attempted to leverage the interdependence between the foot and knee (consistent with Figure 2) to provide symptomatic relief in individuals with knee pain using foot orthoses [241, 242]. Despite the strong postulated biomechanical relationship between the foot and proximal joints, the effects of lateral wedged insoles were modest in individuals with knee OA [242]. Individuals with anterior knee pain, foot orthoses provided superior pain relief compared to flat inserts at six week follow up, however no significant differences were found between foot orthoses and physiotherapy, or between physiotherapy and physiotherapy plus orthoses [241]. In subsequent analyses of this clinical trial, the investigators attempted to identify predictors of foot orthoses efficacy. They reported that individuals with greater dynamic foot mobility [243] and individuals who responded favorably to a treatment direction test (pain relief with foot orthoses when performing a single leg squat) were more likely to benefit from foot orthoses [244]. Taken together, these studies highlight the need for a critical appreciation of regional interdependence and its judicious application to clinical practice.
5. CONCLUSIONS
This review presented our current understanding of assessments and non-invasive, non-pharmacologic treatment options for musculoskeletal conditions of the ankle and foot. Recent studies show that individuals with foot and ankle pain have multiple co-existing impairments in alignment, motion, load distribution and muscle performance. Consequently, a comprehensive assessment of the foot and ankle should include patients’ self-reported outcomes and measures of alignment, motion, strength and provocational tests. As new data quantifying the diagnostic accuracy (sensitivity, specificity, receiver operating characteristic, or ROC, curves) becomes available, choice of assessments may be refined. Increasing evidence highlights the importance of evaluating dynamic function and regional interdependence. Advances in motion capture and plantar load distribution offer exciting opportunities to obtain precise, clinically relevant measures.
Non-surgical interventions are important factors to ease foot pain and slow the disease-related progression of foot and ankle conditions often seen with the rheumatic diseases. Increasingly, studies are showing that orthoses, footwear and other rehabilitation interventions may play an important role in rheumatology-related foot treatment. While reliable and valid measurements of function are needed for intervention studies to succeed, an emphasis upon study design will also be needed to further our understanding of treatments of important subgroups, possibly including genetic links, for many musculoskeletal conditions of the foot and ankle in order to lessen the impact of rheumatic diseases.
Too few prospective studies have been performed and more randomized clinical trials are needed, especially evaluating specific foot conditions and possible interventions. There remain enormous gaps in our current knowledge, particularly around pediatric foot issues as well as the biomechanical pathways of foot pain and foot biomechanics. Our field and our patients will benefit from longer-term prospective controlled intervention studies to determine whether treatment with specific foot interventions or alterations in biomechanics can improve physical functioning, or decrease the likelihood of mobility disability associated with the burden of rheumatic diseases affecting the feet.
Acknowledgments
The authors acknowledge the helpful assistance and comments from Thomas Hagedorn at Hebrew SeniorLife, Boston MA.
Drs. Rao and Riskowski were supported by American College of Rheumatology REF Research Scientist Development Awards.
Dr. Riskowski was also supported by the NIH’s National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01-AR047853) and National Institute of Aging (T32-AG023480).
Dr. Hannan was supported by the NIH’s National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01-AR047853 and R01-AR060492) as well as from the National Institute of Aging (R01-AG026316).
Footnotes
The authors have no conflicts of interest to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Dunn JE, et al. Prevalence of foot and ankle conditions in a multiethnic community sample of older adults. Am J Epidemiol. 2004;159(5):491–8. doi: 10.1093/aje/kwh071. [DOI] [PubMed] [Google Scholar]
- 2.Golightly YM, et al. Association of foot symptoms with self-reported and performance-based measures of physical function: The Johnston County osteoarthritis project. Arthritis care & research. 2011;63(5):654–9. doi: 10.1002/acr.20432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomas MJ, et al. The population prevalence of foot and ankle pain in middle and old age: a systematic review. Pain. 2011;152(12):2870–80. doi: 10.1016/j.pain.2011.09.019. [DOI] [PubMed] [Google Scholar]
- 4.Roddy E, Muller S, Thomas E. Onset and persistence of disabling foot pain in community-dwelling older adults over a 3-year period: a prospective cohort study. J Gerontol A Biol Sci Med Sci. 2011;66(4):474–80. doi: 10.1093/gerona/glq203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Keysor JJ, et al. Are foot disorders associated with functional limitation and disability among community-dwelling older adults? J Aging Health. 2005;17(6):734–52. doi: 10.1177/0898264305280998. [DOI] [PubMed] [Google Scholar]
- 6.Benvenuti F, et al. Foot pain and disability in older persons: an epidemiologic survey. J Am Geriatr Soc. 1995;43(5):479–84. doi: 10.1111/j.1532-5415.1995.tb06092.x. [DOI] [PubMed] [Google Scholar]
- 7.Menz HB, Morris ME, Lord SR. Foot and ankle risk factors for falls in older people: a prospective study. J Gerontol A Biol Sci Med Sci. 2006;61(8):866–70. doi: 10.1093/gerona/61.8.866. [DOI] [PubMed] [Google Scholar]
- 8.Menz HB, et al. Impact of hallux valgus severity on general and foot-specific health-related quality of life. Arthritis care & research. 2010 doi: 10.1002/acr.20396. [DOI] [PubMed] [Google Scholar]
- 9.Mickle KJ, et al. Cross-sectional analysis of foot function, functional ability, and health-related quality of life in older people with disabling foot pain. Arthritis care & research. 2011;63(11):1592–8. doi: 10.1002/acr.20578. [DOI] [PubMed] [Google Scholar]
- 10.Dufour AB, et al. Foot pain: is current or past shoewear a factor? Arthritis Rheum. 2009;61(10):1352–8. doi: 10.1002/art.24733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Riskowski J, Dufour AB, Hannan MT. Arthritis, foot pain and shoe wear: current musculoskeletal research on feet. Curr Opin Rheumatol. 2011;23(2):148–55. doi: 10.1097/BOR.0b013e3283422cf5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Menz HB, Morris ME. Footwear characteristics and foot problems in older people. Gerontology. 2005;51(5):346–51. doi: 10.1159/000086373. [DOI] [PubMed] [Google Scholar]
- 13.Chong M, et al. The interaction of ‘occupant factors’ on the lower extremity fractures in frontal collision of motor vehicle crashes based on a level I trauma center. J Trauma. 2007;62(3):720–9. doi: 10.1097/01.ta.0000222577.43192.a6. [DOI] [PubMed] [Google Scholar]
- 14.Smith BR, et al. A mechanism of injury to the forefoot in car crashes. Traffic Inj Prev. 2005;6(2):156–69. doi: 10.1080/15389580590931635. [DOI] [PubMed] [Google Scholar]
- 15.Richter M, et al. Foot fractures in restrained front seat car occupants: a long-term study over twenty-three years. J Orthop Trauma. 2001;15(4):287–93. doi: 10.1097/00005131-200105000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Otter SJ, et al. Foot pain in rheumatoid arthritis prevalence, risk factors and management: an epidemiological study. Clin Rheumatol. 2010;29(3):255–71. doi: 10.1007/s10067-009-1312-y. [DOI] [PubMed] [Google Scholar]
- 17.Rome K, et al. Foot pain, impairment and disability in patients with acute gout flares; a prospective observational study. Arthritis care & research. 2011 doi: 10.1002/acr.20670. [DOI] [PubMed] [Google Scholar]
- 18.Keen HI, et al. An ultrasonographic study of metatarsophalangeal joint pain: synovitis, structural pathology and their relationship to symptoms and function. Annals of the rheumatic diseases. 2011;70(12):2140–3. doi: 10.1136/annrheumdis-2011-200349. [DOI] [PubMed] [Google Scholar]
- 19.Munteanu SE, Zammit GV, Menz HB. Factors associated with foot pain severity and foot-related disability in individuals with first metatarsophalangeal joint OA. Rheumatology. 2012;51(1):176–83. doi: 10.1093/rheumatology/ker344. [DOI] [PubMed] [Google Scholar]
- 20.Zammit GV, Munteanu SE, Menz HB. Development of a diagnostic rule for identifying radiographic osteoarthritis in people with first metatarsophalangeal joint pain. 8. Vol. 19. Osteoarthritis and cartilage/OARS, Osteoarthritis Research Society; 2011. pp. 939–45. [DOI] [PubMed] [Google Scholar]
- 21.Budiman-Mak E, et al. Theoretical model and Rasch analysis to develop a revised Foot Function Index. Foot Ankle Int. 2006;27(7):519–27. doi: 10.1177/107110070602700707. [DOI] [PubMed] [Google Scholar]
- 22.Martin RL, et al. Evidence of validity for the Foot and Ankle Ability Measure (FAAM) Foot Ankle Int. 2005;26(11):968–83. doi: 10.1177/107110070502601113. [DOI] [PubMed] [Google Scholar]
- 23.van der Leeden M, et al. A systematic review of instruments measuring foot function, foot pain, and foot-related disability in patients with rheumatoid arthritis. Arthritis Rheum. 2008;59(9):1257–69. doi: 10.1002/art.24016. [DOI] [PubMed] [Google Scholar]
- 24.Riskowski J, Hagedorn T, Hannan MT. Measures of Foot Function, Foot Health, and Foot Pain. Arthritis care & research. 2011;63(S11):S229–S239. doi: 10.1002/acr.20554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Binkley JM, et al. The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. North American Orthopaedic Rehabilitation Research Network. Phys Ther. 1999;79(4):371–83. [PubMed] [Google Scholar]
- 26.Cleland JA, et al. Manual physical therapy and exercise versus electrophysical agents and exercise in the management of plantar heel pain: a multicenter randomized clinical trial. J Orthop Sports Phys Ther. 2009;39(8):573–85. doi: 10.2519/jospt.2009.3036. [DOI] [PubMed] [Google Scholar]
- 27.Wrobel JS, Armstrong DG. Reliability and validity of current physical examination techniques of the foot and ankle. J Am Podiatr Med Assoc. 2008;98(3):197–206. doi: 10.7547/0980197. [DOI] [PubMed] [Google Scholar]
- 28.Zammit GV, Menz HB, Munteanu SE. Structural factors associated with hallux limitus/rigidus: a systematic review of case control studies. J Orthop Sports Phys Ther. 2009;39(10):733–42. doi: 10.2519/jospt.2009.3003. [DOI] [PubMed] [Google Scholar]
- 29.Saltzman CL, et al. Reliability of standard foot radiographic measurements. Foot Ankle Int. 1994;15(12):661–5. doi: 10.1177/107110079401501206. [DOI] [PubMed] [Google Scholar]
- 30.Menz HB, Munteanu SE. Validity of 3 clinical techniques for the measurement of static foot posture in older people. J Orthop Sports Phys Ther. 2005;35(8):479–86. doi: 10.2519/jospt.2005.35.8.479. [DOI] [PubMed] [Google Scholar]
- 31.Butler RJ, et al. Arch height index measurement system: establishment of reliability and normative values. J Am Podiatr Med Assoc. 2008;98(2):102–6. doi: 10.7547/0980102. [DOI] [PubMed] [Google Scholar]
- 32.Keenan AM, et al. The Foot Posture Index: Rasch analysis of a novel, foot-specific outcome measure. Arch Phys Med Rehabil. 2007;88(1):88–93. doi: 10.1016/j.apmr.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 33.Murley GS, Menz HB, Landorf KB. A protocol for classifying normal- and flat-arched foot posture for research studies using clinical and radiographic measurements. J Foot Ankle Res. 2009;2:22. doi: 10.1186/1757-1146-2-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Usuelli F, et al. Radiographic considerations of hallux valgus versus hallux rigidus. Foot Ankle Int. 2011;32(8):782–8. doi: 10.3113/FAI.2011.0782. [DOI] [PubMed] [Google Scholar]
- 35.Coughlin MJ, Shurnas PS. Hallux rigidus. Grading and long-term results of operative treatment. J Bone Joint Surg Am. 2003;85-A(11):2072–88. [PubMed] [Google Scholar]
- 36.Glasoe WM, Nuckley DJ, Ludewig PM. Hallux valgus and the first metatarsal arch segment: a theoretical biomechanical perspective. Phys Ther. 2010;90(1):110–20. doi: 10.2522/ptj.20080298. [DOI] [PubMed] [Google Scholar]
- 37.Davitt JS, et al. An association between functional second metatarsal length and midfoot arthrosis. J Bone Joint Surg Am. 2005;87(4):795–800. doi: 10.2106/JBJS.C.01238. [DOI] [PubMed] [Google Scholar]
- 38.Gross KD, et al. Varus foot alignment and hip conditions in older adults. Arthritis Rheum. 2007;56(9):2993–8. doi: 10.1002/art.22850. [DOI] [PubMed] [Google Scholar]
- 39.Gross KD, et al. Association of flat feet with knee pain and cartilage damage in older adults. Arthritis care & research. 2011;63(7):937–44. doi: 10.1002/acr.20431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McWilliams DF, et al. Self-reported knee and foot alignments in early adult life and risk of osteoarthritis. Arthritis care & research. 2010;62(4):489–95. doi: 10.1002/acr.20169. [DOI] [PubMed] [Google Scholar]
- 41.Hopson MM, McPoil TG, Cornwall MW. Motion of the first metatarsophalangeal joint. Reliability and validity of four measurement techniques. Journal of the American Podiatric Medical Association. 1995;85(4):198–204. doi: 10.7547/87507315-85-4-198. [DOI] [PubMed] [Google Scholar]
- 42.Menadue C, et al. Reliability of two goniometric methods of measuring active inversion and eversion range of motion at the ankle. BMC musculoskeletal disorders. 2006;7:60. doi: 10.1186/1471-2474-7-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Spink MJ, Fotoohabadi MR, Menz HB. Foot and ankle strength assessment using hand-held dynamometry: reliability and age-related differences. Gerontology. 2010;56(6):525–32. doi: 10.1159/000264655. [DOI] [PubMed] [Google Scholar]
- 44.Kulig K, et al. Women with posterior tibial tendon dysfunction have diminished ankle and hip muscle performance. J Orthop Sports Phys Ther. 2011;41(9):687–94. doi: 10.2519/jospt.2011.3427. [DOI] [PubMed] [Google Scholar]
- 45.Neville C, Flemister AS, Houck JR. Deep posterior compartment strength and foot kinematics in subjects with stage II posterior tibial tendon dysfunction. Foot Ankle Int. 2010;31(4):320–8. doi: 10.3113/FAI.2010.0320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Barton CJ, Bonanno D, Menz HB. Development and evaluation of a tool for the assessment of footwear characteristics. J Foot Ankle Res. 2009;2:10. doi: 10.1186/1757-1146-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mundermann A, et al. Development of a reliable method to assess footwear comfort during running. Gait Posture. 2002;16(1):38–45. doi: 10.1016/s0966-6362(01)00197-7. [DOI] [PubMed] [Google Scholar]
- 48.Bencke J, et al. Measuring medial longitudinal arch deformation during gait. A reliability study. Gait Posture. 2011 doi: 10.1016/j.gaitpost.2011.10.360. [DOI] [PubMed] [Google Scholar]
- 49.Cashmere T, Smith R, Hunt A. Medial longitudinal arch of the foot: stationary versus walking measures. Foot Ankle Int. 1999;20(2):112–8. doi: 10.1177/107110079902000208. [DOI] [PubMed] [Google Scholar]
- 50.Nielsen RG, et al. Video based analysis of dynamic midfoot function and its relationship with Foot Posture Index scores. Gait Posture. 2010;31(1):126–30. doi: 10.1016/j.gaitpost.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 51.Franettovich MM, et al. The ability to predict dynamic foot posture from static measurements. J Am Podiatr Med Assoc. 2007;97(2):115–20. doi: 10.7547/0970115. [DOI] [PubMed] [Google Scholar]
- 52.Keenan AM, Bach TM. Video assessment of rearfoot movements during walking: a reliability study. Arch Phys Med Rehabil. 1996;77(7):651–5. doi: 10.1016/s0003-9993(96)90003-9. [DOI] [PubMed] [Google Scholar]
- 53.Piva SR, et al. Reliability of measures of impairments associated with patellofemoral pain syndrome. BMC Musculoskelet Disord. 2006;7:33. doi: 10.1186/1471-2474-7-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rao S, et al. Comparison of in vivo segmental foot motion during walking and step descent in patients with midfoot arthritis and matched asymptomatic control subjects. J Biomech. 2009;42(8):1054–60. doi: 10.1016/j.jbiomech.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 55.Khazzam M, et al. Kinematic changes of the foot and ankle in patients with systemic rheumatoid arthritis and forefoot deformity. J Orthop Res. 2007;25(3):319–29. doi: 10.1002/jor.20312. [DOI] [PubMed] [Google Scholar]
- 56.Woodburn J, et al. Multisegment foot motion during gait: proof of concept in rheumatoid arthritis. J Rheumatol. 2004;31(10):1918–27. [PubMed] [Google Scholar]
- 57.Burnfield JM, et al. Variations in plantar pressure variables across five cardiovascular exercises. Med Sci Sports Exerc. 2007;39(11):2012–20. doi: 10.1249/mss.0b013e318148bdfa. [DOI] [PubMed] [Google Scholar]
- 58.Rao S, Carter S. Regional plantar pressure during walking, stair ascent and descent. Gait Posture. 2012 doi: 10.1016/j.gaitpost.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 59.Putti AB, et al. The Pedar in-shoe system: repeatability and normal pressure values. Gait Posture. 2007;25(3):401–5. doi: 10.1016/j.gaitpost.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 60.Zammit GV, Menz HB, Munteanu SE. Reliability of the TekScan MatScan(R) system for the measurement of plantar forces and pressures during barefoot level walking in healthy adults. J Foot Ankle Res. 2010;3:11. doi: 10.1186/1757-1146-3-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gurney JK, Kersting UG, Rosenbaum D. Between-day reliability of repeated plantar pressure distribution measurements in a normal population. Gait Posture. 2008;27(4):706–9. doi: 10.1016/j.gaitpost.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 62.Cavanagh PR, Bus SA. Off-loading the diabetic foot for ulcer prevention and healing. Plast Reconstr Surg. 2011;27(Suppl 1):248S–256S. doi: 10.1097/PRS.0b013e3182024864. [DOI] [PubMed] [Google Scholar]
- 63.Ellis SJ, et al. Plantar pressures in patients with and without lateral foot pain after lateral column lengthening. J Bone Joint Surg Am. 2010;92(1):81–91. doi: 10.2106/JBJS.H.01057. [DOI] [PubMed] [Google Scholar]
- 64.Rao S, Baumhauer JF, Nawoczenski DA. Is barefoot regional plantar loading related to self-reported foot pain in patients with midfoot osteoarthritis. Osteoarthritis Cartilage. 2011 doi: 10.1016/j.joca.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 65.Nawoczenski DA, Ketz J, Baumhauer JF. Dynamic kinematic and plantar pressure changes following cheilectomy for hallux rigidus: a mid-term followup. Foot Ankle Int. 2008;29(3):265–72. doi: 10.3113/FAI.2008.0265. [DOI] [PubMed] [Google Scholar]
- 66.Schmiegel A, et al. Assessment of foot impairment in rheumatoid arthritis patients by dynamic pedobarography. Gait Posture. 2008;27(1):110–4. doi: 10.1016/j.gaitpost.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 67.Bolgla LA, Malone TR. Plantar fasciitis and the windlass mechanism: a biomechanical link to clinical practice. Journal of athletic training. 2004;39(1):77–82. [PMC free article] [PubMed] [Google Scholar]
- 68.De Garceau D, et al. The association between diagnosis of plantar fasciitis and Windlass test results. Foot Ankle Int. 2003;24(3):251–5. doi: 10.1177/107110070302400309. [DOI] [PubMed] [Google Scholar]
- 69.Glasoe WM, et al. A comparison of device measures of dorsal first ray mobility. Foot Ankle Int. 2005;26(11):957–61. doi: 10.1177/107110070502601111. [DOI] [PubMed] [Google Scholar]
- 70.Glasoe WM, et al. Criterion-related validity of a clinical measure of dorsal first ray mobility. J Orthop Sports Phys Ther. 2005;35(9):589–93. doi: 10.2519/jospt.2005.35.9.589. [DOI] [PubMed] [Google Scholar]
- 71.Rao S, et al. The effect of foot structure on 1st metatarsophalangeal joint flexibility and hallucal loading. Gait Posture. 2011;34(1):131–7. doi: 10.1016/j.gaitpost.2011.02.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Root ML, Orien WP, Weed JH. Clin Biomech (Bristol, Avon) 1. xxiii. Los Angeles: Clinical Biomechanics Corp; 1977. Normal and abnormal function of the foot; p. 478. [Google Scholar]
- 73.Houck JR, Tome JM, Nawoczenski DA. Subtalar neutral position as an offset for a kinematic model of the foot during walking. Gait Posture. 2008;28(1):29–37. doi: 10.1016/j.gaitpost.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 74.Elveru RA, et al. Methods for taking subtalar joint measurements. A clinical report. Phys Ther. 1988;68(5):678–82. doi: 10.1093/ptj/68.5.678. [DOI] [PubMed] [Google Scholar]
- 75.Smith-Oricchio K, Harris BA. Interrater reliability of subtalar neutral, calcaneal inversion and eversion. J Orthop Sports Phys Ther. 1990;12(1):10–5. doi: 10.2519/jospt.1990.12.1.10. [DOI] [PubMed] [Google Scholar]
- 76.Torburn L, Perry J, Gronley JK. Assessment of rearfoot motion: passive positioning, one-legged standing, gait. Foot Ankle Int. 1998;19(10):688–93. doi: 10.1177/107110079801901007. [DOI] [PubMed] [Google Scholar]
- 77.Keenan AM, Bach TM. Clinicians’ assessment of the hindfoot: a study of reliability. Foot Ankle Int. 2006;27(6):451–60. doi: 10.1177/107110070602700611. [DOI] [PubMed] [Google Scholar]
- 78.McPoil TG, Knecht HG, Schuit D. A Survey of Foot Types in Normal Females between the Ages of 18 and 30 Years*. J Orthop Sports Phys Ther. 1988;9(12):406–109. doi: 10.2519/jospt.1988.9.12.406. [DOI] [PubMed] [Google Scholar]
- 79.Garbalosa JC, et al. The frontal plane relationship of the forefoot to the rearfoot in an asymptomatic population. J Orthop Sports Phys Ther. 1994;20(4):200–6. doi: 10.2519/jospt.1994.20.4.200. [DOI] [PubMed] [Google Scholar]
- 80.McPoil TG, Cornwall MW. The relationship between static lower extremity measurements and rearfoot motion during walking. J Orthop Sports Phys Ther. 1996;24(5):309–14. doi: 10.2519/jospt.1996.24.5.309. [DOI] [PubMed] [Google Scholar]
- 81.McPoil TG, Hunt GC. Evaluation and management of foot and ankle disorders: present problems and future directions. J Orthop Sports Phys Ther. 1995;21(6):381–8. doi: 10.2519/jospt.1995.21.6.381. [DOI] [PubMed] [Google Scholar]
- 82.Digiovanni BF, et al. Plantar fascia-specific stretching exercise improves outcomes in patients with chronic plantar fasciitis. A prospective clinical trial with two-year follow-up. J Bone Joint Surg Am. 2006;88(8):1775–81. doi: 10.2106/JBJS.E.01281. [DOI] [PubMed] [Google Scholar]
- 83.Neville CG, Houck JR. Choosing among 3 ankle-foot orthoses for a patient with stage II posterior tibial tendon dysfunction. J Orthop Sports Phys Ther. 2009;39(11):816–24. doi: 10.2519/jospt.2009.3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Nigg BM. The role of impact forces and foot pronation: a new paradigm. Clin J Sport Med. 2001;11(1):2–9. doi: 10.1097/00042752-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 85.Woodburn J, Helliwell PS, Barker S. Changes in 3D joint kinematics support the continuous use of orthoses in the management of painful rearfoot deformity in rheumatoid arthritis. J Rheumatol. 2003;30(11):2356–64. [PubMed] [Google Scholar]
- 86.Burns J, et al. Interventions for the prevention and treatment of pes cavus. Cochrane Database Syst Rev. 2007;4:CD006154. doi: 10.1002/14651858.CD006154.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Rao S, et al. Orthoses alter in vivo segmental foot kinematics during walking in patients with midfoot arthritis. Arch Phys Med Rehabil. 2010;91(4):608–14. doi: 10.1016/j.apmr.2009.11.027. [DOI] [PubMed] [Google Scholar]
- 88.Janisse DJ, Janisse E. Shoe modification and the use of orthoses in the treatment of foot and ankle pathology. J Am Acad Orthop Surg. 2008;16(3):152–8. doi: 10.5435/00124635-200803000-00006. [DOI] [PubMed] [Google Scholar]
- 89.Rao S, et al. Shoe inserts alter plantar loading and function in patients with midfoot arthritis. J Orthop Sports Phys Ther. 2009;39(7):522–31. doi: 10.2519/jospt.2009.2900. [DOI] [PubMed] [Google Scholar]
- 90.Neville C, Flemister AS, Houck JR. Effects of the AirLift PTTD brace on foot kinematics in subjects with stage II posterior tibial tendon dysfunction. J Orthop Sports Phys Ther. 2009;39(3):201–9. doi: 10.2519/jospt.2009.2908. [DOI] [PubMed] [Google Scholar]
- 91.Hawke F, et al. Custom-made foot orthoses for the treatment of foot pain. Cochrane Database Syst Rev. 2008;3:CD006801. doi: 10.1002/14651858.CD006801.pub2. [DOI] [PubMed] [Google Scholar]
- 92.Landorf KB, Keenan AM, Herbert RD. Effectiveness of foot orthoses to treat plantar fasciitis: a randomized trial. Archives of internal medicine. 2006;166(12):1305–10. doi: 10.1001/archinte.166.12.1305. [DOI] [PubMed] [Google Scholar]
- 93.Vicenzino B. Foot orthotics in the treatment of lower limb conditions: a musculoskeletal physiotherapy perspective. Manual therapy. 2004;9(4):185–96. doi: 10.1016/j.math.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 94.Radford JA, et al. Effectiveness of low-Dye taping for the short-term treatment of plantar heel pain: a randomised trial. BMC Musculoskelet Disord. 2006;7:64. doi: 10.1186/1471-2474-7-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Alvarez RG, et al. Stage I and II posterior tibial tendon dysfunction treated by a structured nonoperative management protocol: an orthosis and exercise program. Foot Ankle Int. 2006;27(1):2–8. doi: 10.1177/107110070602700102. [DOI] [PubMed] [Google Scholar]
- 96.Kulig K, et al. Effect of eccentric exercise program for early tibialis posterior tendinopathy. Foot Ankle Int. 2009;30(9):877–85. doi: 10.3113/FAI.2009.0877. [DOI] [PubMed] [Google Scholar]
- 97.Spink MJ, et al. Effectiveness of a multifaceted podiatry intervention to prevent falls in community dwelling older people with disabling foot pain: randomised controlled trial. BMJ. 2011;342:d3411. doi: 10.1136/bmj.d3411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Renan-Ordine R, et al. Effectiveness of myofascial trigger point manual therapy combined with a self-stretching protocol for the management of plantar heel pain: a randomized controlled trial. J Orthop Sports Phys Ther. 2011;41(2):43–50. doi: 10.2519/jospt.2011.3504. [DOI] [PubMed] [Google Scholar]
- 99.Shamus J, et al. The effect of sesamoid mobilization, flexor hallucis strengthening, and gait training on reducing pain and restoring function in individuals with hallux limitus: a clinical trial. J Orthop Sports Phys Ther. 2004;34(7):368–76. doi: 10.2519/jospt.2004.34.7.368. [DOI] [PubMed] [Google Scholar]
- 100.Woodburn J, et al. Looking through the ‘window of opportunity’: is there a new paradigm of podiatry care on the horizon in early rheumatoid arthritis? J Foot Ankle Res. 2010;3:8. doi: 10.1186/1757-1146-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Hennessy K, Woodburn J, Steultjens MP. Custom foot orthoses for rheumatoid arthritis: A systematic review. Arthritis care & research. 2011 doi: 10.1002/acr.21559. [DOI] [PubMed] [Google Scholar]
- 102.Vliet Vlieland TP, van den Ende CH. Nonpharmacological treatment of rheumatoid arthritis. Curr Opin Rheumatol. 2011;23(3):259–64. doi: 10.1097/BOR.0b013e32834540fb. [DOI] [PubMed] [Google Scholar]
- 103.Vliet Vlieland TP, Pattison D. Non-drug therapies in early rheumatoid arthritis. Best Pract Res Clin Rheumatol. 2009;23(1):103–16. doi: 10.1016/j.berh.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 104.Xiong S, Goonetilleke RS, Jiang Z. Pressure thresholds of the human foot: measurement reliability and effects of stimulus characteristics. Ergonomics. 2011;54(3):282–93. doi: 10.1080/00140139.2011.552736. [DOI] [PubMed] [Google Scholar]
- 105.Lentz TA, et al. Pain-related fear contributes to self-reported disability in patients with foot and ankle pathology. Arch Phys Med Rehabil. 2010;91(4):557–61. doi: 10.1016/j.apmr.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 106.Felson DT, et al. The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum. 1987;30(8):914–8. doi: 10.1002/art.1780300811. [DOI] [PubMed] [Google Scholar]
- 107.Docherty CL, Valovich McLeod TC, Shultz SJ. Postural Control Deficits in Participants with Functional Ankle Instability as Measured by the Balance Error Scoring System. Clinical Journal of Sport Medicine. 2006;16(3):203–208. doi: 10.1097/00042752-200605000-00003. [DOI] [PubMed] [Google Scholar]
- 108.Gerber JP, et al. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. 10. Vol. 19. Foot & ankle international/American Orthopaedic Foot and Ankle Society [and] Swiss Foot and Ankle Society; 1998. pp. 653–60. [DOI] [PubMed] [Google Scholar]
- 109.Graf A, et al. The effect of walking speed on lower-extremity joint powers among elderly adults who exhibit low physical performance. Arch Phys Med Rehabil. 2005;86(11):2177–83. doi: 10.1016/j.apmr.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 110.Jonkers I, Delp S, Patten C. Capacity to increase walking speed is limited by impaired hip and ankle power generation in lower functioning persons post-stroke. Gait Posture. 2009;29(1):129–37. doi: 10.1016/j.gaitpost.2008.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Siegler S, et al. A six-degrees-of-freedom instrumented linkage for measuring the flexibility characteristics of the ankle joint complex. Journal of Biomechanics. 1996;29(7):943–947. doi: 10.1016/0021-9290(95)00165-4. [DOI] [PubMed] [Google Scholar]
- 112.Chen IH, Kuo KN, Andriacchi TP. The influence of walking speed on mechanical joint power during gait. Gait & Posture. 1997;6(3):171–176. [Google Scholar]
- 113.Winter DA. Energy generation and absorption at the ankle and knee during fast, natural, and slow cadences. Clin Orthop Relat Res. 1983;175(175):147–54. [PubMed] [Google Scholar]
- 114.Sawicki GS, Ferris DP. Powered ankle exoskeletons reveal the metabolic cost of plantar flexor mechanical work during walking with longer steps at constant step frequency. J Exp Biol. 2009;212(Pt 1):21–31. doi: 10.1242/jeb.017269. [DOI] [PubMed] [Google Scholar]
- 115.Cofré LE, et al. Aging modifies joint power and work when gait speeds are matched. Gait & Posture. 2011;33(3):484–489. doi: 10.1016/j.gaitpost.2010.12.030. [DOI] [PubMed] [Google Scholar]
- 116.Kuo AD. Energetics of Actively Powered Locomotion Using the Simplest Walking Model. Journal of Biomechanical Engineering. 2002;124(1):113–120. doi: 10.1115/1.1427703. [DOI] [PubMed] [Google Scholar]
- 117.Malatesta D, et al. Energy cost of walking and gait instability in healthy 65- and 80-yr-olds. J Appl Physiol. 2003;95(6):2248–56. doi: 10.1152/japplphysiol.01106.2002. [DOI] [PubMed] [Google Scholar]
- 118.Charles J, Scutter SD, Buckley J. Static ankle joint equinus: toward a standard definition and diagnosis. J Am Podiatr Med Assoc. 2010;100(3):195–203. doi: 10.7547/1000195. [DOI] [PubMed] [Google Scholar]
- 119.Subotnick SI. Equinus deformity as it affects the forefoot. J Am Podiatry Assoc. 1971;61(11):423–7. doi: 10.7547/87507315-61-11-423. [DOI] [PubMed] [Google Scholar]
- 120.Hill RS. Ankle equinus. Prevalence and linkage to common foot pathology. J Am Podiatr Med Assoc. 1995;85(6):295–300. doi: 10.7547/87507315-85-6-295. [DOI] [PubMed] [Google Scholar]
- 121.Valderrabano V, et al. Etiology of ankle osteoarthritis. Clin Orthop Relat Res. 2009;467(7):1800–6. doi: 10.1007/s11999-008-0543-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Nawar EW, Niska RW, Xu J. National Hospital Ambulatory Medical Care Survey: 2005 emergency department summary. Adv Data. 2007;386:1–32. [PubMed] [Google Scholar]
- 123.Simmons BP, et al. Outcomes assessment in the information age: available instruments, data collection, and utilization of data. Instr Course Lect. 1999;48:667–85. [PubMed] [Google Scholar]
- 124.Westaway MD, Stratford PW, Binkley JM. The patient-specific functional scale: validation of its use in persons with neck dysfunction. J Orthop Sports Phys Ther. 1998;27(5):331–8. doi: 10.2519/jospt.1998.27.5.331. [DOI] [PubMed] [Google Scholar]
- 125.Button G, Pinney S. A meta-analysis of outcome rating scales in foot and ankle surgery: is there a valid, reliable, and responsive system? Foot Ankle Int. 2004;25(8):521–5. doi: 10.1177/107110070402500802. [DOI] [PubMed] [Google Scholar]
- 126.Martin RL, Irrgang JJ. A survey of self-reported outcome instruments for the foot and ankle. J Orthop Sports Phys Ther. 2007;37(2):72–84. doi: 10.2519/jospt.2007.2403. [DOI] [PubMed] [Google Scholar]
- 127.Farrugia P, Goldstein C, Petrisor BA. Measuring foot and ankle injury outcomes: common scales and checklists. Injury. 2011;42(3):276–80. doi: 10.1016/j.injury.2010.11.051. [DOI] [PubMed] [Google Scholar]
- 128.Johanson NA, et al. American Academy of Orthopaedic Surgeons lower limb outcomes assessment instruments. Reliability, validity, and sensitivity to change. J Bone Joint Surg Am. 2004;86-A(5):902–9. doi: 10.2106/00004623-200405000-00003. [DOI] [PubMed] [Google Scholar]
- 129.Domsic RT, Saltzman CL. Ankle osteoarthritis scale. Foot Ankle Int. 1998;19(7):466–71. doi: 10.1177/107110079801900708. [DOI] [PubMed] [Google Scholar]
- 130.Alcock GK, Stratford PW. Validation of the Lower Extremity Function Scale on athletic subjects with ankle sprains. Physiother Can. 2002;54:233–240. [Google Scholar]
- 131.Hale SA, Hertel J. Reliability and Sensitivity of the Foot and Ankle Disability Index in Subjects With Chronic Ankle Instability. J Athl Train. 2005;40(1):35–40. [PMC free article] [PubMed] [Google Scholar]
- 132.Karlsson J, Peterson L. Evaluation of the ankle joint function: the use of a scoring scale. Foot (Edinb) 1991;1(1):15–19. [Google Scholar]
- 133.Roos EM, Brandsson S, Karlsson J. Validation of the foot and ankle outcome score for ankle ligament reconstruction. Foot Ankle Int. 2001;22(10):788–94. doi: 10.1177/107110070102201004. [DOI] [PubMed] [Google Scholar]
- 134.Delbaere K, et al. The Physical Performance Test as a predictor of frequent fallers: a prospective community-based cohort study. Clin Rehabil. 2006;20(1):83–90. doi: 10.1191/0269215506cr885oa. [DOI] [PubMed] [Google Scholar]
- 135.Kaikkonen A, Kannus P, Jarvinen M. A performance test protocol and scoring scale for the evaluation of ankle injuries. Am J Sports Med. 1994;22(4):462–9. doi: 10.1177/036354659402200405. [DOI] [PubMed] [Google Scholar]
- 136.Niki H, et al. Development of the patient-based outcome instrument for foot and ankle: part 2: results from the second field survey: validity of the outcome instrument for the foot and ankle version 2. J Orthop Sci. 2011;16(5):556–64. doi: 10.1007/s00776-011-0131-6. [DOI] [PubMed] [Google Scholar]
- 137.Bennett PJ, et al. Development and validation of a questionnaire designed to measure foot-health status. J Am Podiatr Med Assoc. 1998;88(9):419–28. doi: 10.7547/87507315-88-9-419. [DOI] [PubMed] [Google Scholar]
- 138.Hiller CE, et al. The Cumberland ankle instability tool: a report of validity and reliability testing. Arch Phys Med Rehabil. 2006;87(9):1235–41. doi: 10.1016/j.apmr.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 139.Docherty CL, et al. Development and reliability of the ankle instability instrument. J Athl Train. 2006;41(2):154–8. [PMC free article] [PubMed] [Google Scholar]
- 140.Olerud C, Molander H. A scoring scale for symptom evaluation after ankle fracture. Arch Orthop Trauma Surg. 1984;103(3):190–4. doi: 10.1007/BF00435553. [DOI] [PubMed] [Google Scholar]
- 141.Andre M, Hagelberg S, Stenstrom CH. The juvenile arthritis foot disability index: development and evaluation of measurement properties. J Rheumatol. 2004;31(12):2488–93. [PubMed] [Google Scholar]
- 142.Willits K, et al. Outcome of Posterior Ankle Arthroscopy for Hindfoot Impingement. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2008;24(2):196–202. doi: 10.1016/j.arthro.2007.08.025. [DOI] [PubMed] [Google Scholar]
- 143.Pagenstert G, et al. Realignment surgery for valgus ankle osteoarthritis. Oper Orthop Traumatol. 2009;21(1):77–87. doi: 10.1007/s00064-009-1607-9. [DOI] [PubMed] [Google Scholar]
- 144.Lamm BM, et al. Static rearfoot alignment: a comparison of clinical and radiographic measures. J Am Podiatr Med Assoc. 2005;95(1):26–33. doi: 10.7547/0950026. [DOI] [PubMed] [Google Scholar]
- 145.Song J, et al. Foot type biomechanics. comparison of planus and rectus foot types. J Am Podiatr Med Assoc. 1996;86(1):16–23. doi: 10.7547/87507315-86-1-16. [DOI] [PubMed] [Google Scholar]
- 146.Eng JJ, Pierrynowski MR. The effect of soft foot orthotics on three-dimensional lower-limb kinematics during walking and running. Phys Ther. 1994;74(9):836–44. doi: 10.1093/ptj/74.9.836. [DOI] [PubMed] [Google Scholar]
- 147.Donovan A, Rosenberg ZS. Extraarticular Lateral Hindfoot Impingement With Posterior Tibial Tendon Tear: MRI Correlation. American Journal of Roentgenology. 2009;193(3):672–678. doi: 10.2214/AJR.08.2215. [DOI] [PubMed] [Google Scholar]
- 148.Graves SC, Mann RA, Graves KO. Triple arthrodesis in older adults. Results after long-term follow-up. J Bone Joint Surg Am. 1993;75(3):355–62. doi: 10.2106/00004623-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 149.Mendicino R, Catanzariti AR, Reeves CL. Distal Tibial Osteotomies. In: Chang TJ, editor. Master Techniques in Podiatric Surgery: The Foot and Ankle. Lippincott Williams & Wilkins; Philadelphia, PA: 2004. [Google Scholar]
- 150.Reilingh ML, et al. Measuring hindfoot alignment radiographically: the long axial view is more reliable than the hindfoot alignment view. Skeletal Radiol. 2010;39(11):1103–8. doi: 10.1007/s00256-009-0857-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Kim PJ, et al. Interrater and Intrarater Reliability in the Measurement of Ankle Joint Dorsiflexion is Independent of Examiner Experience and Technique Used. J Am Podiatr Med Assoc. 2011;101(5):407–14. doi: 10.7547/1010407. [DOI] [PubMed] [Google Scholar]
- 152.Martin RL, McPoil TG. Reliability of ankle goniometric measurements: a literature review. J Am Podiatr Med Assoc. 2005;95(6):564–72. doi: 10.7547/0950564. [DOI] [PubMed] [Google Scholar]
- 153.Christiansen CL. The effects of hip and ankle stretching on gait function of older people. Arch Phys Med Rehabil. 2008;89(8):1421–8. doi: 10.1016/j.apmr.2007.12.043. [DOI] [PubMed] [Google Scholar]
- 154.Gajdosik RL, et al. Effects of an eight-week stretching program on the passive-elastic properties and function of the calf muscles of older women. Clin Biomech (Bristol, Avon) 2005;20(9):973–83. doi: 10.1016/j.clinbiomech.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 155.Gras LZ, et al. A Comparison of Hip versus Ankle Exercises in Elders and the Influence on Balance and Gait. Journal of Geriatric Physical Therapy. 2004;27(2):39–46. [Google Scholar]
- 156.Baggett BD, Young G. Ankle joint dorsiflexion. Establishment of a normal range. J Am Podiatr Med Assoc. 1993;83(5):251–4. doi: 10.7547/87507315-83-5-251. [DOI] [PubMed] [Google Scholar]
- 157.Hartmann A, et al. The effect of a foot gymnastic exercise programme on gait performance in older adults: a randomised controlled trial. Disabil Rehabil. 2009;31(25):2101–10. doi: 10.3109/09638280902927010. [DOI] [PubMed] [Google Scholar]
- 158.Norkin W. Measurements of joint motion: a guide to goniometry. 3. Philadelphia: F.A. Davis Company; 2003. [Google Scholar]
- 159.Munteanu SE, et al. A weightbearing technique for the measurement of ankle joint dorsiflexion with the knee extended is reliable. J Sci Med Sport. 2009;12(1):54–9. doi: 10.1016/j.jsams.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 160.Kerrigan DC, et al. Effect of a hip flexor-stretching program on gait in the elderly. Arch Phys Med Rehabil. 2003;84(1):1–6. doi: 10.1053/apmr.2003.50056. [DOI] [PubMed] [Google Scholar]
- 161.Benedetti MG, et al. Effects of an adapted physical activity program in a group of elderly subjects with flexed posture: clinical and instrumental assessment. J Neuroeng Rehabil. 2008;5:32. doi: 10.1186/1743-0003-5-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.DiGiovanni CW, et al. Isolated gastrocnemius tightness. J Bone Joint Surg Am. 2002;84-A(6):962–70. doi: 10.2106/00004623-200206000-00010. [DOI] [PubMed] [Google Scholar]
- 163.Roach KE, Miles TP. Normal Hip and Knee Active Range of Motion: The Relationship to Age. Physical Therapy. 1991;71(9):656–665. doi: 10.1093/ptj/71.9.656. [DOI] [PubMed] [Google Scholar]
- 164.Sepic SB, et al. Strength and range of motion in the ankle in two age groups of men and women. Am J Phys Med. 1986;65(2):75–84. [PubMed] [Google Scholar]
- 165.Smidt GL, Rogers MW. Factors contributing to the regulation and clinical assessment of muscular strength. Phys Ther. 1982;62(9):1283–90. doi: 10.1093/ptj/62.9.1283. [DOI] [PubMed] [Google Scholar]
- 166.Jan MH, et al. Effects of Age and Sex on the Results of an Ankle Plantar-Flexor Manual Muscle Test. Physical Therapy. 2005;85(10):1078–1084. [PubMed] [Google Scholar]
- 167.Cook JD, Glass DS. Strength evaluation in neuromuscular disease. Neurol Clin. 1987;5(1):101–23. [PubMed] [Google Scholar]
- 168.Wadsworth CT, et al. Intrarater Reliability of Manual Muscle Testing and Hand-held Dynametric Muscle Testing. Physical Therapy. 1987;67(9):1342–1347. doi: 10.1093/ptj/67.9.1342. [DOI] [PubMed] [Google Scholar]
- 169.Daniels L, Worthingham C. Muscle Testing: Techniques of Manual Examination. 4. Philadelphia, PA: W B Saunders Co; 1980. [Google Scholar]
- 170.Florence JM, et al. Intrarater reliability of manual muscle test (Medical Research Council scale) grades in Duchenne’s muscular dystrophy. Phys Ther. 1992;72(2):115–22. doi: 10.1093/ptj/72.2.115. discussion 122–6. [DOI] [PubMed] [Google Scholar]
- 171.Escolar DM, et al. Clinical evaluator reliability for quantitative and manual muscle testing measures of strength in children. Muscle Nerve. 2001;24(6):787–93. doi: 10.1002/mus.1070. [DOI] [PubMed] [Google Scholar]
- 172.Andersen H, Jakobsen J. A comparative study of isokinetic dynamometry and manual muscle testing of ankle dorsal and plantar flexors and knee extensors and flexors. Eur Neurol. 1997;37(4):239–42. doi: 10.1159/000117450. [DOI] [PubMed] [Google Scholar]
- 173.Hsieh CY, Phillips RB. Reliability of manual muscle testing with a computerized dynamometer. J Manipulative Physiol Ther. 1990;13(2):72–82. [PubMed] [Google Scholar]
- 174.Hartmann A, et al. Reproducibility of an isokinetic strength-testing protocol of the knee and ankle in older adults. Gerontology. 2009;55(3):259–68. doi: 10.1159/000172832. [DOI] [PubMed] [Google Scholar]
- 175.Symons TB, et al. Reliability of isokinetic and isometric knee-extensor force in older women. J Aging Phys Act. 2004;12(4):525–37. doi: 10.1123/japa.12.4.525. [DOI] [PubMed] [Google Scholar]
- 176.Symons TB, et al. Reliability of a single-session isokinetic and isometric strength measurement protocol in older men. J Gerontol A Biol Sci Med Sci. 2005;60(1):114–9. doi: 10.1093/gerona/60.1.114. [DOI] [PubMed] [Google Scholar]
- 177.Capranica L, et al. Reliability of isokinetic knee extension and flexion strength testing in elderly women. J Sports Med Phys Fitness. 1998;38(2):169–76. [PubMed] [Google Scholar]
- 178.Valderrabano V, et al. Lower leg muscle atrophy in ankle osteoarthritis. J Orthop Res. 2006;24(12):2159–69. doi: 10.1002/jor.20261. [DOI] [PubMed] [Google Scholar]
- 179.Mattacola CG, Lloyd JW. Effects of a 6-week strength and proprioception training program on measures of dynamic balance: a single-case design. J Athl Train. 1997;32(2):127–35. [PMC free article] [PubMed] [Google Scholar]
- 180.Lentell G, et al. The contributions of proprioceptive deficits, muscle function, and anatomic laxity to functional instability of the ankle. J Orthop Sports Phys Ther. 1995;21(4):206–15. doi: 10.2519/jospt.1995.21.4.206. [DOI] [PubMed] [Google Scholar]
- 181.Xu D, et al. Effect of tai chi exercise on proprioception of ankle and knee joints in old people. Br J Sports Med. 2004;38(1):50–4. doi: 10.1136/bjsm.2002.003335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.McChesney JW, Woollacott MH. The effect of age-related declines in proprioception and total knee replacement on postural control. J Gerontol A Biol Sci Med Sci. 2000;55(11):M658–66. doi: 10.1093/gerona/55.11.m658. [DOI] [PubMed] [Google Scholar]
- 183.Riskowski JL, et al. Proprioception, gait kinematics, and rate of loading during walking: are they related? J Musculoskelet Neuronal Interact. 2005;5(4):379–87. [PubMed] [Google Scholar]
- 184.Payne KA, Berg K, Latin RW. Ankle injuries and ankle strength, flexibility, and proprioception in college basketball players. J Athl Train. 1997;32(3):221–5. [PMC free article] [PubMed] [Google Scholar]
- 185.Valderrabano V, et al. Gait analysis in ankle osteoarthritis and total ankle replacement. Clin Biomech (Bristol, Avon) 2007;22(8):894–904. doi: 10.1016/j.clinbiomech.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 186.Nüesch C, et al. Gait patterns of asymmetric ankle osteoarthritis patients. Clinical Biomechanics. (0) doi: 10.1016/j.clinbiomech.2011.12.016. [DOI] [PubMed] [Google Scholar]
- 187.Thomas R, Daniels TR, Parker K. Gait analysis and functional outcomes following ankle arthrodesis for isolated ankle arthritis. J Bone Joint Surg Am. 2006;88(3):526–35. doi: 10.2106/JBJS.E.00521. [DOI] [PubMed] [Google Scholar]
- 188.Gribble PA, Robinson RH. Alterations in knee kinematics and dynamic stability associated with chronic ankle instability. J Athl Train. 2009;44(4):350–5. doi: 10.4085/1062-6050-44.4.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Caulfield BM, Garrett M. Functional instability of the ankle: differences in patterns of ankle and knee movement prior to and post landing in a single leg jump. Int J Sports Med. 2002;23(1):64–8. doi: 10.1055/s-2002-19272. [DOI] [PubMed] [Google Scholar]
- 190.Delahunt E, Monaghan K, Caulfield B. Ankle function during hopping in subjects with functional instability of the ankle joint. Scandinavian Journal of Medicine & Science in Sports. 2007;17(6):641–648. doi: 10.1111/j.1600-0838.2006.00612.x. [DOI] [PubMed] [Google Scholar]
- 191.Kangas J, Dankaerts W, Staes F. New approach to the diagnosis and classification of chronic foot and ankle disorders: Identifying motor control and movement impairments. Manual Therapy. 2011;16(6):522–530. doi: 10.1016/j.math.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 192.Wright CJ, et al. Repeatability of the modified Oxford foot model during gait in healthy adults. Gait & Posture. 2011;33(1):108–112. doi: 10.1016/j.gaitpost.2010.10.084. [DOI] [PubMed] [Google Scholar]
- 193.Ackland DC, Keynejad F, Pandy MG. Future trends in the use of X-ray fluoroscopy for the measurement and modelling of joint motion. Proceedings of the Institution of Mechanical Engineers Part H: Journal of Engineering in Medicine. 2011;225(12):1136–1148. doi: 10.1177/0954411911422840. [DOI] [PubMed] [Google Scholar]
- 194.Ryan L. Mechanical stability, muscle strength and proprioception in the functionally unstable ankle. Aust Physiother. 1994;40(1):41–47. doi: 10.1016/S0004-9514(14)60453-0. [DOI] [PubMed] [Google Scholar]
- 195.Rozzi SL, et al. Balance training for persons with functionally unstable ankles. J Orthop Sports Phys Ther. 1999;29(8):478–86. doi: 10.2519/jospt.1999.29.8.478. [DOI] [PubMed] [Google Scholar]
- 196.Eils E, Rosenbaum D. A multi-station proprioceptive exercise program in patients with ankle instability. Med Sci Sports Exerc. 2001;33(12):1991–8. doi: 10.1097/00005768-200112000-00003. [DOI] [PubMed] [Google Scholar]
- 197.Beynnon BD, et al. Ankle ligament injury risk factors: a prospective study of college athletes. J Orthop Res. 2001;19(2):213–20. doi: 10.1016/S0736-0266(00)90004-4. [DOI] [PubMed] [Google Scholar]
- 198.Tropp H, Ekstrand J, Gillquist J. Stabilometry in functional instability of the ankle and its value in predicting injury. Med Sci Sports Exerc. 1984;16(1):64–6. [PubMed] [Google Scholar]
- 199.Leanderson J, et al. Proprioception in classical ballet dancers. A prospective study of the influence of an ankle sprain on proprioception in the ankle joint. Am J Sports Med. 1996;24(3):370–4. doi: 10.1177/036354659602400320. [DOI] [PubMed] [Google Scholar]
- 200.Willems TM, et al. Intrinsic risk factors for inversion ankle sprains in females--a prospective study. Scand J Med Sci Sports. 2005;15(5):336–45. doi: 10.1111/j.1600-0838.2004.00428.x. [DOI] [PubMed] [Google Scholar]
- 201.Willems TM, et al. Intrinsic risk factors for inversion ankle sprains in male subjects: a prospective study. Am J Sports Med. 2005;33(3):415–23. doi: 10.1177/0363546504268137. [DOI] [PubMed] [Google Scholar]
- 202.Holme E, et al. The effect of supervised rehabilitation on strength, postural sway, position sense and re-injury risk after acute ankle ligament sprain. Scand J Med Sci Sports. 1999;9(2):104–9. doi: 10.1111/j.1600-0838.1999.tb00217.x. [DOI] [PubMed] [Google Scholar]
- 203.McGuine TA, et al. Balance As a Predictor of Ankle Injuries in High School Basketball Players. Clinical Journal of Sport Medicine. 2000;10(4) doi: 10.1097/00042752-200010000-00003. [DOI] [PubMed] [Google Scholar]
- 204.Gribble PA, et al. The effects of fatigue and chronic ankle instability on dynamic postural control. J Athl Train. 2004;39(4):321–329. [PMC free article] [PubMed] [Google Scholar]
- 205.Gribble PA, Hertel J, Denegar CR. Chronic Ankle Instability and Fatigue Create Proximal Joint Alterations during Performance of the Star Excursion Balance Test. Int J Sports Med. 2007;28:236, 242. doi: 10.1055/s-2006-924289. (EFirst) [DOI] [PubMed] [Google Scholar]
- 206.Ross SE, Guskiewicz KM. Effect of coordination training with and without stochastic resonance stimulation on dynamic postural stability of subjects with functional ankle instability and subjects with stable ankles. Clin J Sport Med. 2006;16(4):323–8. doi: 10.1097/00042752-200607000-00007. [DOI] [PubMed] [Google Scholar]
- 207.Ross SE, Guskiewicz KM, Yu B. Single-leg jump-landing stabilization times in subjects with functionally unstable ankles. J Athl Train. 2005;40(4):298–304. [PMC free article] [PubMed] [Google Scholar]
- 208.Ross SE, et al. Assessment tools for identifying functional limitations associated with functional ankle instability. J Athl Train. 2008;43(1):44–50. doi: 10.4085/1062-6050-43.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Gaebler C, et al. Diagnosis of lateral ankle ligament injuries. Comparison between talar tilt, MRI and operative findings in 112 athletes. Acta Orthop Scand. 1997;68(3):286–90. doi: 10.3109/17453679708996703. [DOI] [PubMed] [Google Scholar]
- 210.van Dijk CN, et al. Diagnosis of ligament rupture of the ankle joint. Physical examination, arthrography, stress radiography and sonography compared in 160 patients after inversion trauma. Acta Orthop Scand. 1996;67(6):566–70. doi: 10.3109/17453679608997757. [DOI] [PubMed] [Google Scholar]
- 211.Beumer A, Swierstra BA, Mulder PG. Clinical diagnosis of syndesmotic ankle instability: evaluation of stress tests behind the curtains. Acta Orthop Scand. 2002;73(6):667–9. doi: 10.1080/000164702321039642. [DOI] [PubMed] [Google Scholar]
- 212.de Cesar PC, Avila EM, de Abreu MR. Comparison of magnetic resonance imaging to physical examination for syndesmotic injury after lateral ankle sprain. Foot Ankle Int. 2011;32(12):1110–4. doi: 10.3113/FAI.2011.1110. [DOI] [PubMed] [Google Scholar]
- 213.Molloy S, Solan MC, Bendall SP. Synovial impingement in the ankle. A new physical sign. J Bone Joint Surg Br. 2003;85(3):330–3. doi: 10.1302/0301-620x.85b3.12873. [DOI] [PubMed] [Google Scholar]
- 214.Nelson ME, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1435–45. doi: 10.1249/mss.0b013e3180616aa2. [DOI] [PubMed] [Google Scholar]
- 215.Guissard N, Duchateau J. Effect of static stretch training on neural and mechanical properties of the human plantar-flexor muscles. Muscle Nerve. 2004;29(2):248–55. doi: 10.1002/mus.10549. [DOI] [PubMed] [Google Scholar]
- 216.Gajdosik RL, et al. A stretching program increases the dynamic passive length and passive resistive properties of the calf muscle-tendon unit of unconditioned younger women. Eur J Appl Physiol. 2007;99(4):449–54. doi: 10.1007/s00421-006-0366-7. [DOI] [PubMed] [Google Scholar]
- 217.Muir IW, Chesworth BM, Vandervoort AA. Effect of a static calf-stretching exercise on the resistive torque during passive ankle dorsiflexion in healthy subjects. J Orthop Sports Phys Ther. 1999;29(2):106–13. doi: 10.2519/jospt.1999.29.2.106. discussion 114–5. [DOI] [PubMed] [Google Scholar]
- 218.Youdas JW, et al. The effect of static stretching of the calf muscle-tendon unit on active ankle dorsiflexion range of motion. J Orthop Sports Phys Ther. 2003;33(7):408–17. doi: 10.2519/jospt.2003.33.7.408. [DOI] [PubMed] [Google Scholar]
- 219.Fau Feland Jb, Myrer JW, et al. The effect of duration of stretching of the hamstring muscle group for increasing range of motion in people aged 65 years or older. (Print) [PubMed] [Google Scholar]
- 220.Yeh CY, Tsai KH, Chen JJ. Effects of prolonged muscle stretching with constant torque or constant angle on hypertonic calf muscles. Arch Phys Med Rehabil. 2005;86(2):235–41. doi: 10.1016/j.apmr.2004.03.032. [DOI] [PubMed] [Google Scholar]
- 221.Grieve R, et al. The immediate effect of soleus trigger point pressure release on restricted ankle joint dorsiflexion: A pilot randomised controlled trial. J Bodyw Mov Ther. 2011;15(1):42–9. doi: 10.1016/j.jbmt.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 222.Dananberg HJ, Shearstone J, Guillano M. Manipulation method for the treatment of ankle equinus. J Am Podiatr Med Assoc. 2000;90(8):385–9. doi: 10.7547/87507315-90-8-385. [DOI] [PubMed] [Google Scholar]
- 223.Andersen S, Fryer GA, McLaughlin P. The effect of talo-crural joint manipulation on range of motion at the ankle joint in subjects with a history of ankle injury. Australas Chiropr Osteopathy. 2003;11(2):57–62. [PMC free article] [PubMed] [Google Scholar]
- 224.Grindstaff TL, et al. Immediate effects of a tibiofibular joint manipulation on lower extremity H-reflex measurements in individuals with chronic ankle instability. J Electromyogr Kinesiol. 2011;21(4):652–8. doi: 10.1016/j.jelekin.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 225.van der Plas A, et al. A 5-year follow-up study of Alfredson’s heel-drop exercise programme in chronic midportion Achilles tendinopathy. Br J Sports Med. 2012;46(3):214–8. doi: 10.1136/bjsports-2011-090035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Alfredson H, et al. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med. 1998;26(3):360–6. doi: 10.1177/03635465980260030301. [DOI] [PubMed] [Google Scholar]
- 227.Liu B, et al. Effects of tai chi on lower-limb myodynamia in the elderly people: a meta-analysis. J Tradit Chin Med. 2011;31(2):141–6. doi: 10.1016/s0254-6272(11)60029-0. [DOI] [PubMed] [Google Scholar]
- 228.Li JX, Xu DQ, Hong Y. Effects of 16-week Tai Chi intervention on postural stability and proprioception of knee and ankle in older people. Age Ageing. 2008;37(5):575–8. doi: 10.1093/ageing/afn109. [DOI] [PubMed] [Google Scholar]
- 229.Marzano R. Orthotic Considerations and Footwear Modifications Following Ankle Fusions. Techniques in Foot & Ankle Surgery. 2002;1(1):46–49. [Google Scholar]
- 230.Myers KA, et al. Biomechanical implications of the negative heel rocker sole shoe: gait kinematics and kinetics. Gait Posture. 2006;24(3):323–30. doi: 10.1016/j.gaitpost.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 231.Johanson MA, et al. Heel lifts and the stance phase of gait in subjects with limited ankle dorsiflexion. J Athl Train. 2006;41(2):159–65. [PMC free article] [PubMed] [Google Scholar]
- 232.Cracchiolo A. The use of shoes to treat foot disorders. Orthopaedics Review. 1979;8:73–83. [Google Scholar]
- 233.Praet SFE, Louwerens JWK. The Influence of Shoe Design on Plantar Pressures in Neuropathic Feet. Diabetes Care. 2003;26(2):441–445. doi: 10.2337/diacare.26.2.441. [DOI] [PubMed] [Google Scholar]
- 234.Huang YC, et al. Effects of ankle-foot orthoses on ankle and foot kinematics in patients with subtalar osteoarthritis. Arch Phys Med Rehabil. 2006;87(8):1131–6. doi: 10.1016/j.apmr.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 235.Huang YC, et al. Effects of ankle-foot orthoses on ankle and foot kinematics in patient with ankle osteoarthritis. Arch Phys Med Rehabil. 2006;87(5):710–6. doi: 10.1016/j.apmr.2005.12.043. [DOI] [PubMed] [Google Scholar]
- 236.Malkin K, et al. A year of foot and ankle orthotic provision for adults: Prospective consultations data, with patient satisfaction survey. The Foot. 2008;18(2):75–83. doi: 10.1016/j.foot.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 237.Freeman MA. Treatment of ruptures of the lateral ligament of the ankle. J Bone Joint Surg Br. 1965;47(4):661–8. [PubMed] [Google Scholar]
- 238.Reiman MP, Bolgla LA, Lorenz D. Hip functions influence on knee dysfunction: a proximal link to a distal problem. J Sport Rehabil. 2009;18(1):33–46. doi: 10.1123/jsr.18.1.33. [DOI] [PubMed] [Google Scholar]
- 239.Teichtahl AJ, et al. Foot rotation—A potential target to modify the knee adduction moment. Journal of Science and Medicine in Sport. 2006;9(1–2):67–71. doi: 10.1016/j.jsams.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 240.Patel A, DiGiovanni B. Association between plantar fasciitis and isolated contracture of the gastrocnemius. Foot Ankle Int. 2011;32(1):5–8. doi: 10.3113/FAI.2011.0005. [DOI] [PubMed] [Google Scholar]
- 241.Collins N, et al. Foot orthoses and physiotherapy in the treatment of patellofemoral pain syndrome: randomised clinical trial. Br J Sports Med. 2009;43(3):169–71. doi: 10.1136/bmj.a1735. [DOI] [PubMed] [Google Scholar]
- 242.Bennell KL, et al. Lateral wedge insoles for medial knee osteoarthritis: 12 month randomised controlled trial. BMJ. 2011;342:d2912. doi: 10.1136/bmj.d2912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Barton CJ, et al. Greater peak rearfoot eversion predicts foot orthoses efficacy in individuals with patellofemoral pain syndrome. Br J Sports Med. 2011;45(9):697–701. doi: 10.1136/bjsm.2010.077644. [DOI] [PubMed] [Google Scholar]
- 244.Barton CJ, Menz HB, Crossley KM. Clinical predictors of foot orthoses efficacy in individuals with patellofemoral pain. Med Sci Sports Exerc. 2011;43(9):1603–10. doi: 10.1249/MSS.0b013e318211c45d. [DOI] [PubMed] [Google Scholar]