Abstract
Context:
Few population-based studies have examined the incidence of meniscal injuries, and limited information is available on the influence of patient's demographic and occupational factors.
Objective:
To examine the incidence of meniscal injuries and the influence of demographic and occupational factors among active-duty US service members between 1998 and 2006.
Design:
Cohort study.
Setting:
Using the International Classification of Diseases (9th revision) codes 836.0 (medial meniscus), 836.1 (lateral meniscus), and 836.2 (meniscus unspecified), we extracted injury data from the Defense Medical Surveillance System to identify all acute meniscal injuries among active-duty military personnel.
Patients or Other Participants:
Active-duty military personnel serving in all branches of military service during the study period.
Main Outcome Measure(s):
Incidence rate (IR) per 1000 person-years at risk and crude and adjusted rates by strata for age, sex, race, rank, and service.
Results:
During the study period, 100201 acute meniscal injuries and 12115606 person-years at risk for injury were documented. The overall IR was 8.27 (95% confidence interval [CI] = 8.22, 8.32) per 1000 person-years. Main effects were noted for all demographic and occupational variables (P< .001), indicating that age, sex, race, rank, and service were associated with the incidence of meniscal injuries. Men were almost 20% more likely to experience an acute meniscal injury than were women (incidence rate ratio = 1.18, 95% CI = 1.15, 1.20). The rate of meniscal injury increased with age; those older than 40 years of age experienced injuries more than 4 times as often as those under 20 years of age (incidence rate ratio = 4.25,95% CI = 4.08, 4.42).
Conclusions:
The incidence of meniscal injury was sub-stantially higher in this study than in previously reported studies. Male sex, increasing age, and service in the Army or Marine Corps were factors associated with meniscal injuries.
Keywords: knee injuries, lower extremity injuries, military athletes, injury epidemiology
Key Points.
To our knowledge, this is the largest population-based study to examine the incidence of meniscal tears within a physically active population that is at elevated risk of sport- and training-related knee injuries.
The overall incidence rate for meniscal injury was more than 10 times that previously documented in civilian populations.
Factors associated with a greater incidence of meniscal injury were male sex, increasing age, and Army or Marine Corps service.
The menisci in the medial and lateral tibiofemoral compartments of the knee are critical to normal joint function.1 The primary function of the meniscus is to assist with distributing compressive forces during dynamic knee joint movements and static loading.2,3 In addition, the menisci also play important roles in knee joint lubrication and proprioception and serve as secondary joint stabilizers.4–6 Meniscal injuries in the knee can compromise joint function and lead to increased contact pressures in the affected compartment.7 Meniscal injuries have also been associated with long-term dysfunction, degenerative joint changes, and osteoarthritis in the knee.8,9
Injuries to the menisci in the knee that necessitate surgery are commonly reported in both the general10 and physically active populations,11 and approximately 1 million meniscal surgeries are performed in the United States annually.12 Lohmander et al8 noted that the cumulative risk of a meniscal injury that necessitates surgery in patients between the ages of 10 and 64 years may be as high as 15%, but this estimate does not include injuries that are not diagnosed or are treated nonoperatively. Although these studies provide crude estimates of the incidence of meniscal injury, they offer some insight into the magnitude and burden of this clinical problem. Precise population-based estimates of the incidence of symptomatic meniscal tears are less available and more difficult to ascertain, and the available data on the incidence of meniscal injuries probably underestimate the true incidence of meniscal tears.8
The public health burden and long-term effects of meniscal injuries are substantial, particularly in physically active populations, because of the increased risk for early-onset osteoarthritis and long-term disability and the health care costs associated with degenerative joint disease. Even though multiple reports8,9 suggested that 50% of all patients with meniscal injuries develop osteoarthritis within 10 to 20 years of injury, few authors11,13 have examined the incidence and risk factors associated with meniscal tears in a young, physically active population. Previously reported incidence rates for meniscal injury in physically active populations have ranged between 0.33 and 0.61 per 1000 person-years.11,13 Active-duty US service members represent a large, physically active cohort at high risk for sport- and physical training-related musculoskeletal injuries.13,14 Therefore, the purpose of our study was to describe the incidence rate of meniscal injuries in the knee and associated demographic and occupational risk factors in an active-duty military population, which has been noted to be at high risk for sport- and physical training-related musculoskeletal injuries.13
METHODS
Design and Setting
We conducted a retrospective cohort study to examine the incidence and risk factors associated with the primary occurrence of meniscal tears in the knee among active-duty US service members from 1998 through 2006. Injury data were extracted from the Defense Medical Surveillance System (DMSS), which serves as the central repository for all medical surveillance data and captures all health care encounters between providers and beneficiaries for all 4 branches of military service15,16 using established methods.17 The structure, utility, and capabilities of the DMSS for public health surveillance and epidemiologic research have been described previously in the literature.15–18 An emerging line of research has begun to use the data contained in the DMSS to examine the incidence and risk factors for a number of upper19–22 and lower17,23–25 extremity musculoskeletal injuries and conditions.14,26 Data for hospitalizations and ambulatory visits are summarized in DMSS by major diagnostic categories at the 3-digit level using the International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM) codes to document every patient encounter occurring in military treatment facilities and through outpatient referrals covered by Tricare.15 An exemption for human subject research, under the provision for the "Secondary Use of Existing Data for Epidemiological Research," was granted for this investigation by the Institutional Review Board at Keller Army Hospital, West Point, New York, with secondary review from the US Army Clinical Investigation Regulatory Office (Fort Sam Houston, TX).
Data Acquisition and Operational Definitions
For the current study, the DMSS was queried to identify all incident cases of acute meniscal tear among active-duty US service members from 1998 through 2006 by sex, age, race, branch of military service, and grade or military rank. All years for which complete injury data were available were included in the current study. Specifically, the DMSS was queried for ICD-9-CM codes 836.0 (tear of medial cartilage or meniscus of knee, current), 836.1 (tear of lateral cartilage or meniscus of knee, current), and 836.2 (other tear of cartilage or meniscus of knee, current). Standard age categories in the DMSS were used and included <20,20 through 24,25 through 29,30 through 34, 35 through 39, and ≥40 years. The race categories were white, black, and other, which are also standard categories used in the DMSS.16 Other included Latinos, Asians, Native Americans, and other racial groups. The service categories were US Army, US Marine Corps, US Navy, and US Air Force, representing each branch of military service. The categories for military rank included junior enlisted (E1–E4), senior enlisted (E5–E9), junior officer (O1–O4), and senior officer (O5–O9). Only data from ambulatory visits were used to determine the total number of incident cases, with meniscal tear documented as a primary diagnosis for the ICD-9-CM codes listed earlier for each strata. We limited events to first occurrences to exclude repeat coding for the same initial injury for all service members during the study period. As in previous investigations,22,25 the first occurrence was operationalized so that all incident injuries during the study period represented the first meniscal tear for each person from the time he or she entered military service and excluded all subsequent health care visits for meniscal tear.
Outcome Measures
The incidence rate of meniscal tears per 1000 person-years at risk during the study period was our primary outcome of interest. Incidence rates are calculated by dividing the number of incident cases observed in a population by a measure of exposure or person-time at risk for the outcome of interest and are interpreted as the number of new cases occurring during a specified period of time per unit of person-time at risk for injury.27 Precise time-at-risk denominator data (person-time) for incidence rate calculations, which were validated against personnel data contained in the Defense Manpower Data Center database, were available through the DMSS by strata (eg, sex, age, race) for the entire population of interest. During the study period, person-time at risk for meniscal tear was calculated from the beginning of the study period (January 1, 1998) until the service member sustained an incident meniscal tear, was separated from military service, or reached the administrative end of the study on December 31, 2006. For all service members who joined the military after January 1, 1998, person-time at risk began accumulating on the date of entry into military service until one of the study end points described earlier was reached.
Statistical Analysis
We calculated the overall incidence rate for meniscal injuries in the study population and the 95% confidence interval (CI) by dividing the total number of incident injuries by the total person-years at risk and expressing the rate per 1000 person-years. We developed a multivariable Poisson regression model and used it to estimate the rate of meniscal injury per 1000 person-years by strata (eg, age) while statistically controlling for the influence of the other variables in the model (eg, sex, race, rank, and service). We also used a linear regression model to estimate the percentage increase in the incidence rate for meniscal injuries by age. We estimated incidence rates, rate ratios, and 95% CIs for each variable using the subset with the lowest incidence rate as the referent category. Injury rate comparisons between strata for each variable (eg, age) were conducted using model-adjusted incidence rates and rate ratios to evaluate the independent effect of each of the 5 variables on the incidence of meniscal injury while holding the other variables constant. All data were analyzed using SAS software (version 9.1; SAS Institute Inc, Cary, NC).
RESULTS
In a population with 12115606 person-years at risk, we documented 100201 meniscal injuries during the study period. Over the 9 years, an average of 11133 acute meniscal injuries were diagnosed each year. The overall incidence rate was 8.27 (95% CI=8.22, 8.32) per 1000 person-years. The incidence rate for meniscal injuries varied significantly by sex, age, race, branch of military service, and military rank. Main effects were observed for all 5 demographic and occupational variables (P< .001), indicating that all factors were independently associated with meniscal injury.
Meniscal Injury Patterns
The overall proportional distribution of meniscus injuries by ICD-9-CM code within the study population demonstrated that 50.3% (n=50401) of meniscus injuries involved the medial meniscus (ICD-9-CM code 836.0), 22.4% (n=22445) affected the lateral meniscus (ICD-9-CM code 836.1), and 27.3% (n=27355) of the meniscus injuries were not specified as either a medial or lateral tear (ICD-9-CM code 836.2). The proportional distribution of meniscus injuries remained consistent when men (n=88187) and women (n= 11986) were examined separately. Among men, 50.3% (n=44412) of the injuries affected the medial meniscus, 22.4% (n=19776) affected the lateral meniscus, and 27.2% (n=24027) were not specified as medial or lateral tears. Similarly, among women, 49.7% (n=5961) of meniscal tears involved the medial meniscus, 22.6% (n=2710) involved the lateral meniscus, and 27.7% (n=3315) were not specified.
Incidence Rates Associated With Demographic and Occupational Factors
Sex.
Although the proportional distribution of meniscal injuries was similar between men and women, men experienced meniscal tears at a higher rate than did women. When all other factors were controlled, we found that men were nearly 20% more likely to sustain a meniscal injury than were women. Unadjusted and adjusted incidence rates, rate ratios, and 95% CIs for all demographic and occupational variables are presented in Table 1.
Table 1.
Unadjusted and Adjusted Incidence Rates and Rate Ratios for Meniscal Injuries by Demographic or Occupational Group Among Active-Duty US Service Members From 1998 Through 2006
| Demographic or Occupational Factor | Observed Data |
Unadjusted Data |
Adjusted Dataa |
|||
| Injuries | Person-Years | Rate per 1000 Person-Years | Rate Ratio (95% Confidence Interval) | Rate per 1000 Person-Years | Rate Ratio (95% Confidence Interval) | |
| Sex | ||||||
| Male | 88187 | 10350949 | 8.52 | 1.25 (1.23, 1.28) | 7.08 | 1.18(1.15, 1.20) |
| Female | 11986 | 1764657 | 6.79 | 1.00 | 6.02 | 1.00 |
| Age, y | ||||||
| <20 | 4451 | 1000653 | 4.44 | 1.00 | 2.99 | 1.00 |
| 20–24 | 26082 | 3967051 | 6.57 | 1.48 (1.43, 1.53) | 4.64 | 1.55 (1.50, 1.60) |
| 25–29 | 19349 | 2474621 | 7.82 | 1.76 (1.70, 1.82) | 6.29 | 2.11 (2.03, 2.18) |
| 30–34 | 15499 | 1804494 | 8.59 | 1.93 (1.87,2.00) | 7.37 | 2.47 (2.38, 2.56) |
| 35–39 | 17764 | 1640730 | 10.83 | 2.44 (2.36, 2.52) | 9.49 | 3.18(3.06,3.30) |
| ≥40 | 17056 | 1228057 | 13.89 | 3.13(3.03,3.23) | 12.68 | 4.25 (4.08, 4.42) |
| Race | ||||||
| White | 71036 | 8511036 | 8.35 | 1.25 (1.22, 1.28) | 7.07 | 1.25 (1.23, 1.28) |
| Black | 21225 | 2416641 | 8.78 | 1.31 (1.28, 1.35) | 6.97 | 1.24 (1.20, 1.27) |
| Other | 7940 | 1187929 | 6.68 | 1.00 | 5.64 | 1.00 |
| Service | ||||||
| Army | 41000 | 4226233 | 9.70 | 1.41 (1.39, 1.43) | 7.73 | 1.44 (1.41, 1.46) |
| Marines | 12858 | 1504511 | 8.55 | 1.24 (1.21, 1.27) | 7.60 | 1.41 (1.38, 1.44) |
| Air Force | 23935 | 3133031 | 7.64 | 1.11 (1.09, 1.13) | 5.74 | 1.07 (1.05, 1.09) |
| Navy | 22408 | 3251831 | 6.89 | 1.00 | 5.38 | 1.00 |
| Rank | ||||||
| Junior enlisted | 37264 | 5369399 | 6.94 | 1.05 (1.02, 1.07) | 8.39 | 1.58 (1.54, 1.62) |
| Senior enlisted | 46516 | 4803841 | 9.68 | 1.46 (1.43, 1.50) | 7.00 | 1.32(1.29, 1.35) |
| Junior officers | 7781 | 1175667 | 6.62 | 1.00 | 5.31 | 1.00 |
| Senior Officers | 8640 | 766699 | 11.27 | 1.70 (1.65, 1.76) | 5.81 | 1.09 (1.06, 1.13) |
aRate per 1000 person-years, adjusted for sex, age, race, service, and rank.
Age.
Increased age was associated with higher incidence rates for meniscal injury (Table 1). Service members in the oldest age group experienced meniscal injuries at a rate that was more than 4 times as high as that in the youngest age group (Figure). On average, the adjusted incidence rate for meniscal tears increased by 61% in every 5-year age group.
Figure.
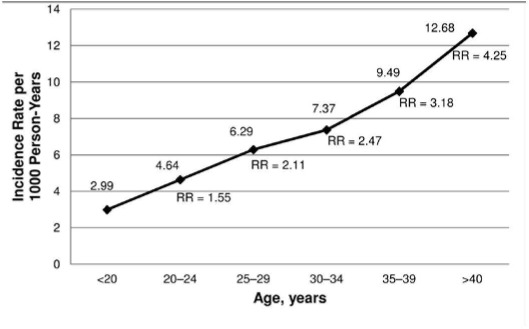
Adjusted incidence rates and rate ratios for meniscal injuries among all active-duty US service members by age from 1998 through 2006. Referent=age <20 years. Abbreviation: RR, incidence rate ratio.
Race.
White and black service members experienced higher incidence rates for meniscal injuries than did those in the other racial category (Table 1). After controlling for sex, age, branch of military service, and rank, we noted that white service members experienced meniscal tears at a rate that was 25% higher than did those in the other racial category. Similarly, black service members experienced meniscal tears 24% more often than did those in the other group for race. No statistical differences were seen in the rates of meniscal tears for those in the white and black racial categories.
Military Service and Rank. Meniscal injury rates were also associated with branch of military service and military rank (Table 1). Those serving in the Army and Marine Corps had the highest adjusted rates of injury, followed by those serving in the Air Force and Navy. Junior enlisted service members experienced the highest adjusted incidence rate of meniscal injuries, followed by senior enlisted service members, senior officers, and junior officers.
DISCUSSION
The current study is the largest population-based study to examine the incidence of meniscal injury in an active population, with 100201 documented meniscal injuries over a 9-year period in a population that experienced 12115606 person-years at risk. The incidence of meniscal injury in the current study was 10 times higher than the rates previously reported in the population-based studies by Nielsen and Yde10 and Baker et al11 (Table 2). Authors17,22,23,25 who examined the incidence of other musculoskeletal injuries in active-duty military populations reported similar findings, with rates an order of magnitude higher than in the general population. This finding probably results from the greater physical demands associated with military service and the availability of accurate injury and exposure information in this population. Furthermore, military personnel regularly engage in physical activity, organized sports, and military training, and sport- and training-related musculoskeletal injuries place a major burden on this population.13,14,17,22–26 These factors may explain, in part, the greater incidence of meniscal tears observed in military populations than in the general population. Finally, in contrast to authors10,11,13 of previous hospital-based studies, we examined the incidence of meniscal injuries requiring ambulatory care in a large, closed health care system.
Table 2.
Incidence Rates for Meniscallnjuries in Previous Population-Based Studies
| Study (Duration) | Population | Injuries | Person-Years | Age Range, y | Incidence Rate per 1000 Person-Years |
| Baker et al, 198511 (10y)a | Civilian, urban | 1515 | 514000 | NA | 0.61 |
| Nielsen and Yde, 199110 (1 y) | Civilian, urban | 188 | 253753 | 9–50+ | 0.74 |
| Lauder etal,200013 (6 y) | US military | 1261 | 3866660 | 17–65 | 0.33 |
| Current (9 y) | US military | 100173 | 12115606 | 17–40+ | 8.27 |
Abbreviation: NA, not available.
aHow incidence rates were calculated is unclear. Also, no data were available about the age range for the patient population.
Previous Population-Based Studies and Meniscal Injuries
A limited number of authors have examined the incidence of meniscal injuries in population-based studies (Table 2). Nielsen and Yde10 estimated the incidence of acute meniscal injuries in patients seen at 2 Danish emergency departments in 1986 to be 0.74 per 1000 inhabitants in the general population. The rate of meniscectomies performed at 5 local hospitals in Syracuse, New York, over a 10-year period was reported to be 0.61 per 1000 people per year.11 Both of these hospital-based studies probably underestimate the true incidence of meniscal injury,8 because the researchers did not include ambulatory visits and did not precisely measure person-time at risk during the study period. Furthermore, meniscectomy was an inclusion criterion for incident cases in the study performed by Baker et al,11 which would have excluded acute symptomatic meniscal lesions that did not result in surgery.
In only 1 published study was the incidence of meniscal injuries in a physically active military population addressed, with precise exposure data used to calculate incidence rates. Lauder et al13 reported that the incidence rate for meniscal tears in this population was 0.33 per 1000 person-years; however, key differences between this investigation and ours limit our ability to compare the results in a meaningful way. Lauder et al13 looked only at injuries resulting from participation in sports and physical training among soldiers serving in the US Army that necessitated hospitalization. Thus, it is not surprising that the rate of meniscal injuries necessitating ambulatory care in the current study was significantly higher than the rate of hospitalizations for sport- and training-related injuries.
Injury Patterns
A limitation is that 27% of the meniscal injuries in the current study were not classified as either medial or lateral; however, the overall proportional distribution, with a ratio of 2:1 medial to lateral meniscus injuries, is consistent with the existing literature, which demonstrated that the medial meniscus is injured 2 to 4 times more frequently than the lateral meniscus.11,28–30 Campbell et al29 reviewed 2572 knee magnetic resonance imaging studies and reported that the proportional distribution of medial to lateral meniscal injuries was 2:1. Ma-jewski et al28 and Nielsen and Yde10 calculated ratios of medial to lateral meniscus injuries at 3:1. Higher ratios for medial to lateral meniscal injuries (eg, 4:1) have been reported by other authors9,11,31; however, these authors examined the proportional distribution in patients needing meniscectomy, which may be different from the distribution of meniscal injuries among those not needing surgical intervention. The disproportionate number of medial meniscal injuries observed in these studies has been attributed to the anatomical differences between the medial and lateral menisci. The medial meniscus is firmly attached to the joint capsule and is less mobile than the lateral meniscus; therefore, it is more susceptible to injury.1,32
Incidence Rates Associated With Demographic Factors
Sex.
Although the proportional distribution of meniscal injuries remained consistent for group comparisons by sex in our study, the overall incidence rate of injury by sex differed significantly. Men were nearly 20% more likely to experience a meniscal injury than were women when the influence of age, race, rank, and branch of military service was held constant. Baker et al11 reported that males experienced twice as many meniscal injuries as females in the general population; however, after accounting for sport exposure, they found that the incidence rates for male and female skiers were similar. As we did, previous investigators17,22,23,25,33,34 of military populations have noted sex differences between men and women in relation to the incidence of other musculoskeletal injuries and conditions. The disparities in the incidence rates between men and women for certain musculoskeletal injuries may reflect different activity levels and occupational exposures. Specifically, the types of jobs in which men and women serve, including noncombat roles for women and other cultural factors in the military, may increase the risk among men for certain types of injuries.22
Age.
Increased age was associated with significantly higher rates of meniscal injury in the present study. The higher rate of meniscal injury with increasing age may result from the natural course of meniscal degeneration with age,35 which may increase the risk for acute meniscal tears. This natural course may partially explain why active-duty service members experienced a 61% increase, on average, in the incidence of meniscal tears with every 5 years of advancing age. Because all service members are medically screened through the Department of Defense Medical Evaluation Review System upon entry to military service24,36 and service members receive their health care through a closed system, it is unlikely that prevalent cases of meniscal injury contributed to the higher rates of injury seen in older service members. To our knowledge, we are the first to document that age is associated with a significant increase in the incidence of meniscal injuries in a young, physically active population; however, further research is needed to develop a better understanding of how age is related to the development of the specific types of meniscal lesions observed in younger patients.1,8,37
Increased age at the time of meniscal tear has also been associated with the development and progression of osteoarthritis after injury.38 Roos et al38 reported that the average time from traumatic meniscal injury to the onset of radiographic signs of osteoarthritis in patients between the ages of 17 and 30 years was 15 years. In contrast, for patients older than 30 years, the time from meniscal injury to the onset of radiographic signs of osteoarthritis was only 5 years. These findings suggest that older people not only are at greater risk for acute meniscal tears but also may be at greater risk for the accelerated progression of degenerative joint changes after injury. These risks may be compounded by the physical demands associated with military service and sports participation in older people who experience meniscal tears.
Race.
Race was associated with the incidence of meniscal injury in the current study. To our knowledge, the association between race and the incidence of meniscal tear has not been examined previously; however, other authors22,25,39,40 have noted racial differences related to the incidence of other musculoskeletal injuries and conditions in military populations. The racial categories we used are standard categories within the DMSS, and our ability to analyze and interpret the results relative to race in the current study is limited by the inherent characteristics associated with these data.25 The complex heterogeneity in the other racial category precludes our ability to make meaningful interpretations of the findings relative to race in the current study, but the possibility of a predisposition for meniscal injury associated with race warrants further investigation.
Incidence Rates Associated With Occupational Factors
The higher incidence of injury sustained by those serving in the Army and Marine Corps may result from different levels of occupational risk between these branches of military service. Specifically, each branch of service has a distinct operational mission with unique physical fitness and training requirements.17,25 Researchers17,22,25 have reported that service members in the Army and Marine Corps experience significantly higher rates of other acute musculoskeletal injuries than do service members in the Navy and Air Force. It is interesting to note the increase in the incidence rate ratio for meniscal tears among those serving in the Marine Corps after adjusting for other variables in the statistical model. This increase results in part from the smaller size of the population younger than 20 years in the referent group (Navy) compared with the Marines Corps and a significantly higher incidence of meniscal injuries for those serving in the Marines Corps in this age category when compared with the Navy (6.30 versus 4.09).
Military rank was also associated with meniscal injuries in the current study, which showed that junior enlisted service members had the highest incidence. Previous authors17,22,25 have consistently reported that those in the junior and senior enlisted ranks are at greater risk for various musculoskeletal injuries and conditions when compared with officers. As a result, it is not surprising that junior enlisted service members were at the highest risk for acute meniscal injuries in our study after we controlled for the influence of age and other demographic and occupational factors. It is interesting to note the substantially different incidence rate ratios after adjustment in the junior enlisted and senior officer groups, which can be attributed to the size of the younger population (categories of younger than 20 years and 20–24 years) for this group compared with the referent group (junior officers) and the greater incidence of injuries for the junior enlisted group in these 2 categories. This can be explained in part by the lack of junior officers in the group that was younger than 20 years (26 versus 1000627) and few in the 20–24 years group (170631 versus 3315825) when compared with the junior enlisted group. The opposite effect can be observed for the senior officers: Few senior officers were in any age group younger than 30–34 years (ie, younger than 20 years, 20–24 years, and 25–29 years). Many junior enlisted service members in these age groups are new recruits going through the physical rigors of basic training or those who may not have adjusted to the physical demands of military service. Military rank may also be a surrogate measure associated with engaging in physical activities, such as running, jumping, and cutting, that are often associated with increased risk for meniscal tears.
Strengths and Limitations
Certain limitations associated with the present study should be considered when interpreting the results; many of these limitations have been discussed in previous reports.17,22,25 The quality of the administrative data extracted from the DMSS depends on the completeness, validity, consistency, timeliness, and accuracy of the data contained in the system.16 Coding errors associated with injury diagnoses cannot be ruled out when large administrative databases such as the DMSS are used for epidemiologic research purposes. Misclassification of the outcome of interest introduces the potential for information bias, which could have led to either overestimation or underestimation of the true incidence of meniscal tears. Yet the likelihood of any differential misclassification in the present study is limited.25 Another limitation is that we were unable to determine reinjury rates because incident cases were restricted to first occurrences. By confining our search to first occurrences, we eliminated follow-up visits for the same injury but may have also missed reinjuries to the same body part, as well as injuries to the contralateral limb. Also, the present study probably represents the incidence of isolated meniscal tears and does not account for meniscal tears sustained with a concomitant injury, such as an anterior cruciate ligament tear, because we included only meniscal tears listed as the primary diagnosis. Because of the large number of observed injuries in this population-based study, we were unable to confirm the diagnosis in all cases through a review of each patient's medical records. Finally, the injury data contained in the DMSS are not linked to data that could be used to assess the effect of meniscal injuries in the current study. Specifically, data for rehabilitation workload, time loss due to injury, and injury-related disability and subsequent discharge from military service as a result of injury are not currently available within the DMSS.
Despite the limitations listed here, several strengths are associated with using data from the DMSS, and many of these have been described previously.17,22,25 Ours is the largest known population-based study to examine the incidence of meniscal injuries in a physically active population that is at greater risk for sport- and physical training-related knee injuries.13,23,25 Previous authors8 have had difficulty obtaining precise population-based estimates of the true incidence of meniscal injury because they have documented only a limited number of observed injuries and typically included only hospital-based injuries or surgical cases. More than 100000 injuries were documented for the present study, in contrast to the next largest population-based study, which documented slightly more than 1500 injuries.11 This was possible because the DMSS captures injury and precise exposure data for the entire population of active-duty service members, and data were available for the population of interest during the entire study period. Therefore, we had the opportunity to examine the incidence rate for the primary occurrence of meniscal injury in a large, physically active population that receives medical care within a closed health care system. The current study used a large administrative database to examine the incidence of meniscal injuries and the influence of occupational and demographic risk factors on the rate of injury. The Armed Forces Health Surveillance Center exerts great effort to ensure a standardized, consistent approach to data processing and validation, and only records considered complete are processed into the DMSS.16 As a result, it is likely that nearly every patient encounter in a military treatment facility, as well as civilian purchased care, was documented in the DMSS during the study period. It is likely that nearly all incident meniscal injuries during the study period were documented within the DMSS.
CONCLUSIONS
This is the largest known population-based study to examine the incidence of meniscal injuries in a physically active population that is at greater risk for experiencing sport- and training-related knee injuries. The overall incidence rate for meniscal injury documented in the current study was more than 10 times greater than rates previously reported in civilian populations. Several nonmodifiable demographic and occupational factors, including sex, age, race, rank, and branch of service, were associated with the incidence of meniscal injury in this active-duty military population, and these results may have implications for other physically active populations. Future researchers should focus on identifying and characterizing the modifiable risk factors associated with meniscal injuries to facilitate the development of effective injury-prevention programs. Such programs are particularly important given the high rate of degenerative joint disease and osteoarthritis associated with meniscal damage and the burden these conditions place on the health care system and society.
Acknowledgments
The views and opinions expressed in this manuscript are those of the authors and do not reflect the official policy of the Department of the Army, the Department of Defense, or the US Government. We acknowledge the US service members on active duty during the study period between 1998 and 2006 for their selfless commitment to serve our nation. We also recognize the active duty and civilian providers and support staff who coordinated and delivered the medical care for this cohort throughout the Military Health System.
REFERENCES
- 1.Englund M, Guermazi A, Lohmander SL. The role of the meniscus in knee osteoarthritis: a cause or consequence? Radiol Clin North Am. 2009;47(4):703–712. doi: 10.1016/j.rcl.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 2.Walker PS, Erkman MJ. The role of the menisci in force transmission across the knee. Clin Orthop Relat Res. 1975;109:184–192. doi: 10.1097/00003086-197506000-00027. [DOI] [PubMed] [Google Scholar]
- 3.Kurosawa H, Fukubayashi T, Nakajima H. Load-bearing mode of the knee joint: physical behavior of the knee joint with or without menisci. Clin Orthop Relat Res. 1980;149:283–290. [PubMed] [Google Scholar]
- 4.Levy IM, Torzilli PA, Gould JD, Warren RF. The effect of lateral meniscectomy on motion of the knee. J Bone Joint Surg Am. 1989;71(3):401–406. [PubMed] [Google Scholar]
- 5.Levy IM, Torzilli PA, Warren RF. The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am. 1982;64(6):883–888. [PubMed] [Google Scholar]
- 6.Assimakopoulos AP, Katonis PG, Agapitos MV, Exarchou EI. The innervation of the human meniscus. Clin Orthop Relat Res. 1992;275:232–236. [PubMed] [Google Scholar]
- 7.Din JC, Kim SJ, Park IH. In vitro study of contact area and pressure distribution in the human knee after partial and total meniscectomy. Int Orthop. 1993;17(4):214–218. doi: 10.1007/BF00194181. [DOI] [PubMed] [Google Scholar]
- 8.Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35(10):1756–1769. doi: 10.1177/0363546507307396. [DOI] [PubMed] [Google Scholar]
- 9.Englund M, Roos EM, Roos HP, Lohmander LS. Patient-relevant outcomes fourteen years after meniscectomy: influence of type of meniscal tear and size of resection. Rheumatology (Oxford). 2001;40(6):631–639. doi: 10.1093/rheumatology/40.6.631. [DOI] [PubMed] [Google Scholar]
- 10.Nielsen AB, Yde J. Epidemiology of acute knee injuries: a prospective hospital investigation. J Trauma. 1991;31(12):1644–1648. doi: 10.1097/00005373-199112000-00014. [DOI] [PubMed] [Google Scholar]
- 11.Baker BE, Peckham AC, Pupparo F, Sanborn JC. Review of meniscal injury and associated sports. Am J Sports Med. 1985;13(1):1–4. doi: 10.1177/036354658501300101. [DOI] [PubMed] [Google Scholar]
- 12.Cook JL. The current status of treatment for large meniscal defects. Clin Orthop Relat Res. 2005;435:88–95. doi: 10.1097/00003086-200506000-00014. [DOI] [PubMed] [Google Scholar]
- 13.Lauder TD, Baker SP, Smith GS, Lincoln AE. Sports and physical training injury hospitalizations in the army. Am J Prev Med. 2000;18(3 suppl):118–128. doi: 10.1016/s0749-3797(99)00174-9. [DOI] [PubMed] [Google Scholar]
- 14.Hauret KG, Taylor BJ, Clemmons NS, Block SR, Jones BH. Frequency and causes of nonbattle injuries air evacuated from operations Iraqi Freedom and Enduring Freedom, U.S. Army, 2001–2006. Am J Prev Med. 2010;38(1 suppl):S94–S107. doi: 10.1016/j.amepre.2009.10.022. [DOI] [PubMed] [Google Scholar]
- 15.Rubertone MV, Brundage JF. The Defense Medical Surveillance System and the Department of Defense serum repository: glimpses of the future of public health surveillance. Am J Public Health. 2002;92(12):1900–1904. doi: 10.2105/ajph.92.12.1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Army Medical Surveillance Activity. Defense Medical Epidemiological Database User's Guide. Version 3.6.4. Silver Springs, MD: Armed Forces Health Surveillance Center; 2004. [Google Scholar]
- 17.Cameron KL, Owens BD, DeBerardino TM. Incidence of ankle sprains among active-duty members of the United States Armed Services from 1998 through 2006. J Athl Train. 2010;45(l):29–38. doi: 10.4085/1062-6050-45.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sleet DA, Jones BH, Amoroso PJ. Military injuries and public health: an introduction. Am J Prev Med. 2000;18(3 suppl):1–3. doi: 10.1016/s0749-3797(00)00105-7. [DOI] [PubMed] [Google Scholar]
- 19.Wolf JM, Dawson L, Mountcastle SB, Owens BD. The incidence of scaphoid fracture in a military population. Injury. 2009;40(12):1316–1319. doi: 10.1016/j.injury.2009.03.045. [DOI] [PubMed] [Google Scholar]
- 20.Wolf JM, Mountcastle S, Owens BD. Incidence of carpal tunnel syndrome in the US military population. Hand (NY). 2009;4(3):289–293. doi: 10.1007/s11552-009-9166-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wolf JM, Sturdivant RX, Owens BD. Incidence of de Quervain's tenosynovitis in a young, active population. J Hand Surg Am. 2009;34(1):112–115. doi: 10.1016/j.jhsa.2008.08.020. [DOI] [PubMed] [Google Scholar]
- 22.Owens BD, Dawson L, Burks R, Cameron KL. Incidence of shoulder dislocation in the United States military: demographic considerations from a high-risk population. J Bone Joint Surg Am. 2009;91(4):791–796. doi: 10.2106/JBJS.H.00514. [DOI] [PubMed] [Google Scholar]
- 23.Owens BD, Mountcastle SB, Dunn WR, DeBerardino TM, Taylor DC. Incidence of anterior cruciate ligament injury among active duty U.S. military servicemen and servicewomen. Mil Med. 2007;172(1):90–91. doi: 10.7205/milmed.172.1.90. [DOI] [PubMed] [Google Scholar]
- 24.Scher DL, Belmont PJ, Jr, Mountcastle S, Owens BD. The incidence of primary hip osteoarthritis in active duty US military servicemembers. Arthritis Rheum. 2009;61(4):468–475. doi: 10.1002/art.24429. [DOI] [PubMed] [Google Scholar]
- 25.Hsiao M, Owens BD, Burks R, Sturdivant RX, Cameron KL. Incidence of acute traumatic patellar dislocation among active-duty United States military service members. Am J Sports Med. 2010;38(10):1997–2004. doi: 10.1177/0363546510371423. [DOI] [PubMed] [Google Scholar]
- 26.Hauret KG, Jones BH, Bullock SH, Canham-Chervak M, Canada S. Musculoskeletal injuries: description of an under-recognized injury problem among military personnel. Am J Prev Med. 2010;38(1 suppl):S61–S70. doi: 10.1016/j.amepre.2009.10.021. [DOI] [PubMed] [Google Scholar]
- 27.Knowles SB, Marshall SW, Guskiewicz KM. Issues in estimating risks and rates in sports injury research. J Athl Train. 2006;41(1):207–215. [PMC free article] [PubMed] [Google Scholar]
- 28.Majewski M, Susanne H, Klaus S. Epidemiology of athletic knee injuries: a 10-year study. Knee. 2006;13(3):184–188. doi: 10.1016/j.knee.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 29.Campbell SE, Sanders TG, Morrison WB. MR imaging of meniscal cysts: incidence, location, and clinical significance. AJR Am J Roentgenol. 2001;177(1):409–413. doi: 10.2214/ajr.177.2.1770409. [DOI] [PubMed] [Google Scholar]
- 30.McDermott ID, Amis AA. The consequences of meniscectomy. J Bone Joint Surg Br. 2006;88(12):1549–1556. doi: 10.1302/0301-620X.88B12.18140. [DOI] [PubMed] [Google Scholar]
- 31.Roos H, Lauren M, Adalberth T, Roos EM, Jonsson K, Lohmander LS. Knee osteoarthritis after meniscectomy: prevalence of radiographic changes after twenty-one years, compared with matched controls. Arthritis Rheum. 1998;41(4):687–693. doi: 10.1002/1529-0131(199804)41:4<687::AID-ART16>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 32.Renstrom P, Johnson RJ. Anatomy and biomechanics of the menisci. Clin Sports Med. 1990;9(3):523–538. [PubMed] [Google Scholar]
- 33.Jones BH, Bovee MW, Harris JM, III, Cowan DN. Intrinsic risk factors for exercise-related injuries among male and female army trainees. Am J Sports Med. 1993;21(5):705–710. doi: 10.1177/036354659302100512. [DOI] [PubMed] [Google Scholar]
- 34.Jones BH, Knapik JJ. Physical training and exercise-related injuries: surveillance, research and injury prevention in military populations. Sports Med. 1999;27(1):111–125. doi: 10.2165/00007256-199927020-00004. [DOI] [PubMed] [Google Scholar]
- 35.Jerosch J, Castro WH, Assheuer J. Age-related magnetic resonance imaging morphology of the menisci in asymptomatic individuals. Arch Orthop Trauma Surg. 1996;115(3–4):199–202. doi: 10.1007/BF00434553. [DOI] [PubMed] [Google Scholar]
- 36.Cameron KL, Duffey ML, DeBerardino TM, Stoneman PD, Jones CJ, Owens BD. Association of generalized joint hypermobility with a history of glenohumeral joint instability. J Athl Train. 2010;45(3):253–258. doi: 10.4085/1062-6050-45.3.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Englund M. The role of the meniscus in osteoarthritis genesis. Med Clin North Am. 2009;93(1):37–43. x. doi: 10.1016/j.mcna.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 38.Roos H, Adalberth T, Dahlberg L, Lohmander LS. Osteoarthritis of the knee after injury to the anterior cruciate ligament or meniscus: the influence of time and age. Osteoarthritis Cartilage. 1995;3(4):261–267. doi: 10.1016/s1063-4584(05)80017-2. [DOI] [PubMed] [Google Scholar]
- 39.Owens BD, Mountcastle SB, White D. Racial differences in tendon rupture incidence. Int J Sports Med. 2007;28(7):617–620. doi: 10.1055/s-2007-964837. [DOI] [PubMed] [Google Scholar]
- 40.Jones BH, Thacker SB, Gilchrist J, Kimsey CD, Jr, Sosin DM. Prevention of lower extremity stress fractures in athletes and soldiers: a systematic review. Epidemiol Rev. 2002;24(1):228–247. doi: 10.1093/epirev/mxf011. [DOI] [PubMed] [Google Scholar]


