Abstract
Objective
To illustrate the complex patterns that emerge when race/ethnicity, socioeconomic status (SES), and gender are considered simultaneously in health care disparities research and to outline the needed research to understand them by using disparities in lung cancer risks, treatment, and outcomes as an example.
Principal Findings
SES, gender, and race/ethnicity are social categories that are robust predictors of variations in health and health services utilization. These are usually considered separately, but intersectionality theory indicates that the impact of each depends on the others. Each reflects historically and culturally contingent variations in social, economic, and political status. Distinct patterns of risk and resilience emerge at the intersections of multiple social categories and shape the experience of health, health care access, utilization, quality, and outcomes where these categories intersect. Intersectional approaches call for greater attention to understand social processes at multiple levels of society and require the collection of relevant data and utilization of appropriate analytic approaches to understand how multiple risk factors and resources combine to affect the distribution of disease and its management.
Conclusions
Understanding how race/ethnicity, gender, and SES are interactive, interdependent, and social identities can provide new knowledge to enhance our efforts to effectively address health disparities.
Keywords: Health care disparities, smoking, lung cancer, race/ethnicity, socioeconomic status, gender
Socioeconomic status (SES) as measured by income, education, or occupational status, is a robust predictor of variations in health and health service utilization (Braveman et al. 2010). Racial/ethnic differences in health status and health service use have also been well documented (Williams et al. 2001). Although racial/ethnic and SES disparities overlap to some degree, health disparities researchers tend to study them separately. Race/ethnicity is correlated with SES, such that SES differences between racial/ethnic groups account for a substantial part of the observed racial/ethnic differences in health, including cancer (Krieger et al.2008; Howard et al. 2006; Albano et al. 2008). Typically, adjustment for SES substantially reduces but does not eliminate disparities in health risks and outcomes by race/ethnicity. Moreover, large gender differences exist in health and health service use (Williams 2002;Read and Gorman 2007). Importantly, race/ethnicity, SES, and gender converge in complex ways that can enhance or impair health (Weber and Parra-Medina 2008). This article explores how the simultaneous consideration of race/ethnicity, SES, and gender can provide novel insights into disease risks, patterns of health service utilization, and effective interventions to reduce health care disparities.
An intersectional approach emphasizes the importance of intersecting inequalities, multiple vulnerabilities, and the need to examine how multiple dimensions of social statuses combine to facilitate or restrict exposure and response to risk factors and resources relevant for a disease and its treatment (Schulz and Mullings 2006; Weber and Fore 2004). Intersectional theory posits that multiple social statuses are experienced simultaneously and dynamic interdependent processes arise when race/ethnicity, SES, and gender (and/or other social statuses) combine to affect patterns of risks and resources, privilege and disadvantage that can affect health risks and health service utilization across different social contexts (Cole 2010).
The intersectionality framework emphasizes that social identities and categories should not be viewed as independent variables that capture individual characteristics; instead, they are markers of institutional processes (Cole 2010). Cole 2010) identifies at least three implications for researchers. First, heterogeneity within social categories should be examined, especially attending to categories that have been neglected to facilitate the identification of how the meaning and consequences of one social category depend on other categories. Second, the intersectionality perspective highlights that membership in a social category often embodies institutional policies and practices that structure social inequalities and stigma in ways that shape opportunity and life chances. Third, intersectionality calls for exploring how macro-level social processes create commonalities across different social categories. Thus, an intersectional lens calls for research on health disparities to unpack the lived experiences of social groups at the convergence of multiple identities. It emphasizes that various social inequalities do not act independently but interact in ways that can transform and alter processes and outcomes of inequality from one setting or context to another. This approach can also delineate potential avenues of improving population health and inform targeted interventions to effectively address disparities in health care.
Using lung cancer as an exemplar, this conceptual article illustrates the complex patterns that can emerge when race/ethnicity, SES, and gender are considered simultaneously and outlines health services research considerations to understand and address disparities across the continuum of lung cancer.
Intersection of Race/Ethnicity, SES, and Gender in Lung Cancer and Tobacco Use
Lung cancer is the leading cause of cancer deaths for men and women in the United States and is responsible for 80 percent of all deaths from tobacco-related illnesses annually (Thun et al. 2007), and for more American deaths each year than breast, prostate, colon, and pancreatic cancer combined (American Cancer Society 2009). The risks linked to lung cancer mortality and cigarette smoking vary by race, SES, and gender. Lung cancer mortality is 10 percent higher for Black men than White men but 31 percent higher for White women than Black women (American Cancer Society 2011). As shown in Table 1, SES differences within each gender are consistently larger than racial differences (Albano et al. 2008). Moreover, Black men have lower or equivalent mortality risks compared to those of White men at the two lowest SES levels, but higher lung cancer mortality rates at higher levels of education. Black women have markedly lower mortality risk than their White counterparts at low levels of education, equivalent risks in the middle educational categories, and elevated risks at the two highest levels of education. Table 2 presents current smoking levels by race/ethnicity with income and education for men and women in the United States. Black and White in these data refer to non-Hispanic Black and non-Hispanic Whites.1 For Blacks and Whites of each gender, there are large variations in smoking by income and education with low SES Blacks and Whites, regardless of gender, being two to three times more likely to smoke cigarettes than their high SES counterparts. However, at every level of SES, Black and Hispanic women are less likely than White women to smoke. And although Black, Hispanic, and White men have comparable smoking rates at high income levels, they diverge at low income levels.
Table 1.
U.S. Lung Cancer Death Rates* for 2001, by Gender, Race, and Education
| Men | Women | |||||
|---|---|---|---|---|---|---|
| White | Black | B/W Ratio | White | Black | B/W Ratio | |
| All | 281.1 | 305.7 | 1.09 | 180.3 | 137.9 | 0.76 |
| Education | ||||||
| 0–8 years | 94.5 | 84 | 0.89 | 51 | 22.8 | 0.45 |
| 9–11 years | 81.9 | 84 | 1.03 | 56.1 | 29 | 0.52 |
| 12 years | 53.6 | 69.7 | 1.30 | 33.3 | 34.2 | 1.03 |
| 13–15 years | 23.8 | 29.9 | 1.26 | 16.6 | 18.2 | 1.10 |
| 16 years | 16.6 | 22.5 | 1.36 | 12.4 | 19.6 | 1.58 |
| 17+ years | 10.7 | 15.6 | 1.46 | 10.9 | 14.1 | 1.29 |
| Low/high ratio | 8.8 | 5.4 | 4.7 | 1.6 | ||
Deaths per 100,000 for persons aged 25–64 years.
Source: Albano et al. 2008.
Table 2.
Percent of U.S. Adults who were Current Cigarette Smokers, U.S., 2007–2009*
| Men | Women | |||||
|---|---|---|---|---|---|---|
| White | Black | Hispanic | White | Black | Hispanic | |
| All | 24.1 | 24.0 | 18.0 | 20.9 | 17.3 | 9.4 |
| Poverty level | ||||||
| Below 100% | 37.8 | 37.9 | 19.6 | 38.9 | 26.6 | 12.0 |
| 100–199% | 34.5 | 31.1 | 18.6 | 31.6 | 19.1 | 8.4 |
| 200–399% | 27.8 | 21.1 | 18.9 | 21.9 | 11.9 | 9.4 |
| 400% or more | 16.9 | 15.8 | 16.4 | 13.8 | 9.2 | 7.7 |
| Income difference | 20.9 | 22.1 | 3.2 | 25.1 | 17.4 | 4.3 |
| Education level | ||||||
| <HS | 44.0 | 36.5 | 18.8 | 44.5 | 28.1 | 8.3 |
| HS or GED | 34.4 | 27.8 | 20.4 | 29.8 | 22.6 | 10.6 |
| ≥ Some college | 15.8 | 20.0 | 15.0 | 15.1 | 13.2 | 10.5 |
| Education difference | 28.2 | 16.5 | 5.4 | 29.4 | 14.9 | 2.3 |
The categories Black and White refer to non-Hispanic Blacks and non-Hispanic Whites.
The data in Tables 1 and 2 document complex associations among race/ethnicity, gender, and SES. These patterns may reflect confounding between race/ethnicity and SES or the noncomparability of SES indicators across racial/ethnic groups. Other mediating factors could include exposure to distinctive environmental conditions linked to residential segregation, genetic differences, resilience factors, nativity/migration, and cultural practices and beliefs (Williams et al. 2001). Understanding how race/ethnicity, SES, and gender combine to affect disparities across the continuum of lung cancer prevention and care will require careful attention for unpacking both the risks and resources that each of these variables may represent.
Confounding between Race/Ethnicity and SES
Each indicator of SES (e.g., income, education, occupation) is more often than not predictive of variations in health and health service use, but SES indicators are not interchangeable and each has strengths and limitations (Krieger, Williams, and Moss 2006). In Table 1, even with the truncated education distribution, the differences by education are larger than those by income for White men and women, whereas the opposite is true for Blacks. Researchers should be sensitive to the possibility that mechanisms of social inequality as captured by different indicators of SES could reflect different patterns of adversity over the life course or varying exposure to risks and resources that can contribute to different patterns of health risks, health status, and disease management for various social groups. For example, one national study found that although education played a greater role than income in the onset of illness, income was a stronger predictor of its course (Herd, Goesling, and House 2001).
The degree of confounding between race and SES can vary across different indicators of SES (LaVeist 2002). For example, racial/ethnic differences in wealth are markedly larger than those for income or education, with White households having 15 times as much total wealth and 100 times as much financial wealth (excluding home equity) as the average Black or Latino household (Domhoff 2011). Even the operationalization of an SES indicator can differentially capture confounding with race/ethnicity, with there being little variation between Blacks and Whites in high school graduation rates but marked differences in college completion (Williams et al. 2001). Thus, the association between SES and lung cancer risk and treatment can vary by the time, place, specific SES indicator utilized, and the particular group under consideration.
Nonequivalence of SES
For both men and women, the data in Table 1 showed an elevated risk of lung cancer mortality for college-educated Blacks compared to their White peers. Research on middle-class minorities suggests that the nonequivalence of SES across race/ethnicity is a contributor to these differences. Compared to Whites, Blacks and Latinos tend to have lower levels of income at every level of education, less wealth at every level of income, higher exposure to occupational risks within the same occupational categories, and less purchasing power at a given level of income (Williams et al. 2001). Table 2 also indicates that for both Blacks and Hispanics, men and women, the prevalence of smoking is more similar to Whites at high levels of education and income, compared to the reduced prevalence at lower SES levels. Elevated levels of stress for middle class minorities compared to their White peers may contribute to this pattern. Research indicates, for example, that middle-class status is often recent, tenuous, and marginal for African Americans and other minorities (Jackson and Williams 2007; Council of Economic Advisers 2009). Compared to Whites, middle-class minorities are more likely to experience unemployment and are less likely to translate their higher economic status into desirable housing and neighborhood conditions (Alba, Logan, and Stults 2010; Jackson and Williams 2007).
Other race-related stressors, some of which are gender specific, contribute to this economically fragile position and can affect patterns of health care utilization and treatment. First, perceived racial discrimination is a stressor that is positively related to SES and adversely associated with health risks including tobacco use (Williams and Mohammed 2003). Second, the responsibility of providing support to poorer relatives is often an added burden. Compared to White women, middle-class Black women receive less social and material support and provide more of these resources to poorer relatives (Jackson and Williams 2007). Third, thwarted aspirations may contribute to unrealized economic gains in ways that differ by gender. For Blacks and Hispanics, compared to Whites, the racial gap in earnings at comparable levels of education are larger for men than for women and since the 1960s, minority women have made larger gains in reducing the racial gap in income than men (Council of Economic Advisers 2009).
Segregation and the Role of Place
In addition to considerations of SES at the individual and household level, exposures linked to place can be key predictors of social disparities in health risks, health care, and outcomes as detailed elsewhere in this special issue (White et al. in press). A remarkably constant feature of Black life in the United States has been a high level of residential segregation (Williams and Collins 2012). Prior research has identified residential segregation by race as a key confounder of the relationship between race and SES and a critical determinant of variations in neighborhood quality and conditions (Acevedo-Garcia et al. 2008). Segregation also varies for ethnic subgroups with mainland Puerto Ricans living under the highest level of segregation among Latinos (Massey 2003) and Black Caribbean immigrants residing in areas of higher segregation than African Americans (Logan and Deane 2003).
Segregation can adversely affect smoking and lung cancer outcomes via multiple pathways (Williams et al. 2001). The concentration of economic hardship and other psychosocial stressors in segregated neighborhoods can make it more difficult for residents to lead healthy lives and seek needed care. The levels of cigarette smoking are higher in some racially segregated, economically disadvantaged residential areas than would be predicted by national data (Dell et al. 1998; Delva et al. 2010). Stressors can facilitate the onset of smoking, make quitting more difficult and adherence to medical regimens more challenging (Webb and Carey 2011; Berg et al. 2008). In fact, in those rare instances where Whites reside in similar neighborhood conditions to African Americans, their level of smoking and other health risks are similar to or worse than those of African Americans (LaVeist et al. 2005).
Segregation can also restrict socioeconomic mobility by limiting access to education and employment opportunities, and it can encourage high-risk behaviors such as tobacco smoking because of the disproportionate targeting of tobacco advertising to disadvantaged minority communities (Primack et al. 2008). Prior research indicates that the same amount of tobacco has more negative effects on the health of Blacks compared to Whites (Haiman et al. 2006). Institutional neglect in segregated communities could contribute to this pattern by leading to higher levels of exposure to toxic chemicals (Morello-Frosch and Jesdale 2009), which in turn can interact with tobacco exposure to markedly exacerbate health risks. Although the pattern is not uniform (Earle et al. 2011; Potosky et al. 2004), geographic variation that captures neighborhood deprivation and segregation is associated with an elevated risk of lung cancer mortality and the receipt of poorer treatment for lung cancer (Earle et al. 2000; Major et al. 2010).
Genetic differences and Gene-Environment Interactions
High levels of residential segregation ensure that a large number of social, psychological, residential, and other physical-chemical environmental variables differ by racial/ethnic status. SES and racial/ethnic groups are often located in different residential and occupational environments. Gender groups often occupy different occupational contexts. Biology, including genetics, is adaptive to environmental exposures and the distinctive environments of social groups suggest that more systematic attention should be given to identifying potential epigenetic effects (changes in gene expression and tissue and organ function that are not caused by changes in the DNA sequence). Variations in genetic susceptibility to disease also occur in human populations, although these variations tend not to be strongly patterned by race (Kaufman and Cooper 2010). Research is needed to identify the extent to which genetic variants of lung cancer are differentially distributed by race, and the potential of gene-environment interactions to play a role in lung cancer risk and disparities (Ramos and Rotimi 2004).
Racial and ethnic categories are likely to capture simultaneous confounding by both biological and environmental variables that are often unmeasured. The findings of greater vulnerability to tobacco among Blacks compared to Whites (Haiman et al. 2006) could reflect racial differences in particular genetic variants, gene-environment interactions, and/or differences in gene expression linked to different environments. Research on lung cancer has given scant attention to the extent to which gene frequency and gene expression may vary by race, SES, or gender. This information is critical to ensure that these groups benefit equally from the development of genomic tests and tailored treatments, as described elsewhere in this special issue (Shields and Crown 2006).
Resilience Factors
In addition to identifying risk factors and vulnerabilities, research also needs to identify and examine the health consequences of the capacities and resources that exist at the intersections of social groups at both the individual and area level (Ahern et al. 2008). Exposure to protective resources and the patterns of response that are mobilized to deal with potential threats can minimize the negative effects of risk factors. Table 2 indicated, surprisingly, that Black women have lower rates of smoking than their White peers at every level of SES. This suggests that even in contexts of low SES, other aspects of the social environment can enhance health. Material and psychosocial resources can be mobilized to adapt and cope with risk. These interactions can lead to variations in vulnerability across groups that reflect differential preparedness, ability to recover, and capacity to capitalize on and use available resources including medical care (deFur et al. 2007).
Higher levels of religious engagement by Black compared to White women may contribute to Black women's lower levels of smoking. Religious attendance, which may influence both individual behaviors and social networks, has been associated with lower levels of smoking in national (Gillum and Sullins 2002) and regional studies (Whooley et al. 2007). Higher level of religious involvement by Black than White teens contributes to the lower level of smoking among Black adolescents (Wallace et al. 2003). In addition, communities vary in their skills, knowledge, and resources to address local problems (Goodman et al. 2011). Various community institutions (families, neighborhoods, schools, churches, businesses, and voluntary agencies) can be agents of change to seek solutions to local problems (McLeroy et al. 2003).
Migration, Cultural Beliefs, and Behavior
Hispanic women are less likely than men to smoke cigarettes and the SES gradient in smoking among Latinos is much less marked than that for Blacks and Whites (Table 2). This profile of smoking behavior is influenced by migration and failure to disaggregate the data by nativity status is likely to obscure important patterns of variation. Hispanic, White, Asian, and Black immigrants all have lower current rates of smoking than their native-born counterparts (Dey and Lucas 2005), but their risk increases with length of stay in the United States(Clegg et al. 2002). Moreover, the increasing prevalence of smoking with length of stay in the United States among Latinos is more marked for women than for men (Lara et al. 1999). Prior research also indicates that SES is less strongly related to health status and health risks among recently arrived immigrants than among longer duration immigrants and also among first-generation immigrants relative to second- or later generation immigrants (Angel, Buckley, and Finch 2001; Acevedo-Garcia et al. 2010). Immigrants of all major racial groups also have markedly lower lung cancer mortality rates than their native-born counterparts (Singh and Miller 2005).
Cultural factors play an important role in affecting the current and future health of immigrant and U.S.-born populations and their interactions with the health care system (Kagawa-Singer et al. 2000). Culturally shaped beliefs, attitudes, and behaviors can affect prevention, help seeking, treatment, and adherence to medical regimens in ways that can shed light on the complex interactions among race/ethnicity, gender, and SES. For example, men are often socialized to demonstrate strength, autonomy, dominance, and physical aggression, and to avoid the expression of emotion or vulnerability (Courtenay 2009; Williams 2002). These cultural beliefs about manhood can discourage men from engaging in preventive health behaviors. Men are markedly more likely than women to engage in a broad range of health damaging behaviors and less likely to make preventive health care visits (Courtenay 2009). Tobacco companies have often capitalized on these cultural beliefs to develop marketing strategies that link tobacco with independence, social success, and sexual attraction (National Cancer Institute 2008). Cultural factors can also influence the structure and functioning of health care organizations and the attitudes and behavior of health care providers (Kagawa-Singer et al. 2000). For example, compared to women, health care providers spend less time with men and provide men with fewer services, less health information, and less advice to change behaviors (such as smoking) to improve health (Courtenay 2009). Thus, cultural influences on lung cancer risks and outcomes deserve more research attention with better conceptual and empirical tools.
Research Considerations for Understanding the Intersection of Race/Ethnicity, SES, and Gender across the Continuum of Lung Cancer
The complexities that emerge at the intersections of race/ethnicity, SES, and gender are more recognized in research on the social determinants of health than in research on health services utilization. To inform conceptual models and empirical analyses of disparities in health care utilization, we selectively highlight some of the needed research on intersectionality along the continuum of lung cancer prevention, treatment, and outcomes.
Analytic Implications of Intersectionality
Inadequate attention has been given to analytic methods needed for the quantitative study of intersectionality. The limited understanding of the relative magnitude of various social inequalities is in part a function of the limited methodological approaches that have been used to assess it (Sen, Iyer, and Mukherjee 2009). Recently, Sen, Iyer, and Mukherjee (2009) have proposed an analytic approach that makes meaningful distinctions between various intersecting categories. They begin by developing a unique identity for each intersecting category by creating a set of indicator variables for each category (e.g., indicators for poor Black men, poor Black women, poor White men, poor White women, etc.). This approach allows for the testing of the significance of each indicator variable relative to a reference group, of any category compared to all other categories, and of differences in the size of social gaps. Moreover, by ranking odds ratios for each category and plotting them on a log scale, one can readily create a visual representation of the relative positions of the various categories on the social scale. This approach can provide critical insights with regard to which population subgroups are most affected, in what settings, and can also facilitate the precise targeting of interventions. New analytic approaches such as this one may also require disproportionate sampling methods to provide adequate statistical power and to investigate within- and between-group differences in cancer risks, treatments, and survival. However, Cole (2010) cautions that given intersectionality theory's emphasis on how social status is experienced, statistical models and interactions may not always capture the subtle ways in which the meaning of one social category is shaped by the level of another.
Lung Cancer Risk
Smoking
Smoking is the foremost contributor to lung cancer risk and disparities. Data on smoking show somewhat inconsistent patterns over time among certain racial/ethnic groups. For example, among high school students 19.4 percent of Whites report smoking compared to only 7.4 percent of African Americans (United States Centers for Disease Control and Prevention 2011). This early use trend then changes in adulthood with Whites (22 percent) and African Americans (21 percent) reporting similar rates (United States Centers for Disease Control and Prevention 2011). Currently the extent to which this pattern varies for specific subgroups of these populations and the driving factors behind these variations over time are not well defined. To better understand these patterns, we recommend routine reporting of the prevalence of cigarette smoking simultaneously by race/ethnicity, SES (income or education), and gender. Newer methods of data collection such as the use of electronic medical records to track smoking over time would not only allow for longitudinal assessment among large sample sizes necessary to conduct examination of intersectionality, but these data systems would also allow agencies such as public health departments to examine local and dynamic trends over time.
Moreover, there are a variety of drivers that may potentially explain changing patterns. These include differential and targeted exposure to tobacco marketing and promotions, social networks and peer pressures, and exposure to stressors such as discrimination as young adults enter the workforce. Future research should include surveillance of the marketing/promotions environment in different contexts as defined by geography, workplace, and retail environments. Data on youth and adult risk behaviors as well as the tobacco retail environment and promotions are often collected by various state and federal agencies as well as the private sector. What is needed is the integration of these data systems to facilitate comprehensive analyses of the exposures that influence tobacco use. Such reporting will lay the foundation for identifying vulnerable subgroups and patterns of risk to more clearly understand the conditions under which particular social processes combine to influence the initiation and subsequent trajectories of smoking.
Second, future research should routinely report racial/ethnic data for populations with a high proportion of immigrants, such as Asians and Hispanics, by nativity status (U.S.-born versus foreign-born), and generational status, whenever feasible. Generational status can be easily obtained by obtaining the place of birth data for the respondent and his or her parents and grandparents (Takeuchi et al. 2004).
Third, there is a need for greater research attention to delineating the relevant protective factors that may be linked to lower cigarette use among African American youth but appear to dissipate in adulthood, as well as the resilience factors responsible for the low rates of cigarette smoking among Hispanic adults. To achieve this goal, variables such as parental involvement, religious involvement, social support, social and gender norms, and acculturation should be included in large-scale studies of youth such as the Youth Risk Behavior Surveys and Monitoring the Future survey. The dynamic nature of these factors must also be addressed across the life course and these variables should also be considered for inclusion in the newly announced Tobacco Control Act National Longitudinal Study of Tobacco Users (Food and Drug Administration 2011). This large-scale national study, jointly sponsored by the FDA and the National Institutes of Health, seeks to assess and monitor the behavioral and health effects of new tobacco regulations. By following a cohort of more than 40,000 users of tobacco products and those at risk for tobacco use, aged 12 and older, over time, this survey will provide an excellent opportunity to document the root causes of differential smoking rates among U.S. adults as researchers investigate how multiple variables unfold over the life course and interact with each other. Research on smoking also needs to take a multilevel approach in assessing environmental factors along with individual-level variables such as the potential protective factors listed above and psychosocial factors such as anxiety, depression, perceived chronic stress, and discrimination. Data collection and multilevel analyses of this nature may help clarify the mechanisms at play at the intersection of race/ethnicity, SES, and gender and what factors either limit or enhance the impact of prevention interventions (Greaves, Vallone, and Velicer 1998; National Cancer Institute 2008).
Lung Cancer Outcomes
Diagnosis and Screening
Lung cancer often presents with common and often nonspecific symptoms such as a cough, lacks definitive screening recommendations, and typically requires invasive staging tests, thereby making early diagnosis challenging for clinicians. Delays in diagnosis for lung cancer are common and these vary by patient insurance status, region, and hospital (Ward et al. 2006; Molina et al. 2001; Yorio et al. 2010). Patients of color and low-SES often present with late stage disease, and then have fewer opportunities for curative interventions (Alberg, Brock, and Samet 2000; Albano et al. 2008). However, inadequate attention has been devoted to social influences on diagnosis. Prior research reveals that characteristics of the health care environment interact with patient demographics to shape provider behavior (Wright and Perry 2009). However, our understanding is limited regarding the extent to which similar processes occur for lung cancer and how they may vary by race/ethnicity, SES, and gender. In an effort to better understand this interplay, future research must collect and analyze data with the intent of focusing on the course of lung cancer. Inclusion of such variables in a longitudinal dataset, merged with claims-level data, would allow for a more complete look at patterns of risk and potential targets of intervention across the lung cancer spectrum. In addition, the potential impact of national screening recommendations for smokers must be considered in existing and future research related to lung cancer diagnosis in an effort to track and minimize further exacerbation of existing disparities by gender, race/ethnicity, and SES.
Treatment
Most patients with lung cancer present with advanced disease, and early stage lung cancer is usually discovered incidentally. Surgery for early stage disease is the only treatment modality that is potentially curative, and Black race and inadequate insurance are associated with lower rates of surgery (Bach et al. 2008). More severe comorbid disease (Blackstock et al. 1999), differences in patient preferences due to mistrust and prevalent beliefs (Margolis et al. 2007), poor physician and patient communication (Gordon et al. 2008), and access to care may all contribute to these disparities (Cykert et al. 2000). Unfortunately, prior research has not examined how all these identified risk factors combine at the intersection of race/ethnicity, SES, and gender in the treatment of early stage lung cancer. Similar limitations exist in research on advanced disease. Although disparities by race are well documented for the treatment of advanced disease with chemotherapy and radiation (Earle et al. 2000; Potosky et al. 2004) future studies should jointly evaluate the effects of SES, race/ethnicity, and gender in the treatment of end-stage disease and the extent to which these patterns may vary by region.
A final consideration for future disparities research on the treatment of lung cancer is the increasing development and use of targeted therapies and their implications across gender, racial/ethnic, and SES groups. Although molecular/genetic determinants have long been recognized for their decisive roles in tumor biology and clinical behavior, these factors are rarely measured in population-based studies of cancer health outcomes. However, several intriguing lines of evidence support the notion that significant differences in “druggable” somatic genetic variations exist across racial and ethnic groups. Non-small cell lung cancer patients who are East Asian in origin more frequently harbor mutations in the epidermal growth factor receptor (EGFR) than do White patients (Shepherd et al. 2009). When patients with EGFR mutations are treated with specific inhibitors, nearly all respond, compared to patients without EGFR mutations (Paez et al. 2010; Mok et al. 2003). Future studies should assess the additional joint contribution of SES and gender to this line of research, as these variables may indicate differential, more effective targeted therapies in the future. Related, the lack of adequate inclusion of minorities in clinical trials must also be considered. Significant disparities in clinical trial participation is particularly problematic for genomically targeted treatments. If we were to effectively reduce disparities in the treatment of lung cancer and to adequately investigate the role of intersectionality, there must be significant attention directed to inclusion of racial minorities, women, and low SES groups in clinical trials.
Survival
Unfortunately, only about 15 percent of lung cancer patients survive 5 years after diagnosis (American Cancer Society 2008), and available data show inconsistent patterns of survival by gender, race, and SES. For example, Figure highlights that in the most affluent counties Black men have decreased survival relative to White men but Black women have markedly better survival relative to White women (Singh et al. 2012). The factors underlying these racial/ethnic, SES, and gender disparities in survival are multilayered and complex, relating to patients, providers, health care systems, and communities (Smedley, Stith, and Nelson 2003; Ayanian 2005). Identifying the contribution of each factor is necessary to design focused strategies to eliminate disparities. Collection of SES data at the individual and area levels is also needed. With the absence of individual-level SES in cancer registries, income and education are typically estimated using area-based measures.
Figure 1.
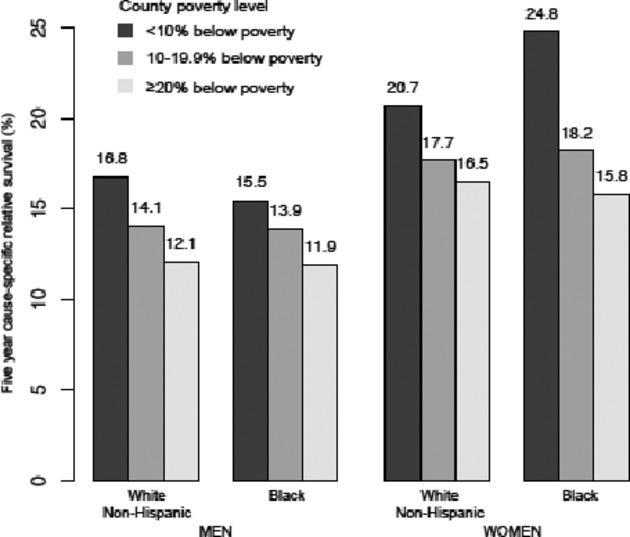
Five-Year Cause-Specific Relative Survival by Gender, Race/Ethnicity, and Area-Level SES. (Source: Singh et al. 2012)
Analyses that rely only on area-based measures may be subject to ecologic bias (Greenland 2006). This bias can be reduced by using area-based SES measures derived from Census tract data instead of broad county-level data (Krieger et al. 1997). However, efforts to fully understand the interactions of race/ethnicity, area-level, and individual-level SES and gender will require multilevel data and modeling techniques to inform health policy interventions (Zaslavsky and Ayanian 2010). If between-hospital or between-community differences are a major component of disparities in survival, then policy solutions can focus on improving care in hospitals and communities with large numbers of disadvantaged patients or on expanding access for patients in these communities to better hospitals. Alternately, if racial/ethnic, gender, and socioeconomic disparities are mainly evident within hospitals and communities, then attention can focus on addressing reasons why some groups have worse outcomes in these settings.
Conclusion
The intersectional perspective helps to identify population subgroups that are most at risk. It highlights the importance of understanding the local context in terms of both identifying patterns of risk and in targeting interventions to vulnerable groups. It also emphasizes that many of the observed social variations in health in general and lung cancer risks in particular are not biologically inevitable but are shaped by social processes and institutions including the response of the health care system. A multilevel life-course perspective is essential given the interactive nature of these exposures across the life span and the dynamic and heterogeneous patterning of risks. Adequate sample sizes for small populations defined by patient's race/ethnicity, SES, and gender are also critical. Future research should give increased attention to quantifying social exposures at multiple levels of analysis and documenting the extent to which they have consequences for health and patterns of health service utilization. This approach will require transdisciplinary approaches that are informed by quantitative and qualitative research that attempts to capture all relevant aspects of the social environment and seeks to identify how these factors combine with biological susceptibility to affect the organization, need, use, and outcomes of care across the entire continuum of disease.
Acknowledgments
This work was conducted with support from the National Cancer Institute/x92s Lung Cancer Disparities Center grant 1P50CA148596 and in part (for Drs. Ayanian and Haas) with support from Harvard Catalyst | The Harvard Clinical and Translational Science Center (NIH Award UL1 RR 025758 and financial contributions from Harvard University and its affiliated academic health care centers). The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic health care centers, the National Center for Research Resources, or the National Institutes of Health. The authors would also like to thank the Center/x92s Program Coordinator, Maria Simoneau, for her dedication to the formatting of this manuscript and the administrative oversight of the submission process. The co-authors report no conflict of interest.
Note
We acknowledge that labeling these categories as if they did not overlap obscures the reality of multiple identities linked to race and ethnicity.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- Acevedo-Garcia D, Osypuk TL, McArdle N, Williams DR. “Toward a Policy-Relevant Analysis of Geographic and Racial/Ethnic Disparities in Child Health”. Health Affairs. 2008;27((2)):321–33. doi: 10.1377/hlthaff.27.2.321. [DOI] [PubMed] [Google Scholar]
- Acevedo-Garcia D, Bates LM, Osypuk TL, McArdle N. “The Effect of Immigrant Generation and Duration on Self-Rated Health among Us Adults 2003–2007”. Social Science and Medicine. 2010;71((6)):1161–72. doi: 10.1016/j.socscimed.2010.05.034. [DOI] [PubMed] [Google Scholar]
- Ahern J, Galea S, Hubbard A, Karpati A. “Population Vulnerabilities and Capacities Related to Health: A Test of a Model”. Social Science and Medicine. 2008;66((3)):691–703. doi: 10.1016/j.socscimed.2007.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alba RD, Logan JR, Stults BJ. “How Segregated Are Middle-Class African Americans?”. Social Problems. 2000;47:543–58. [Google Scholar]
- Albano JD, Ward E, Jemal A, Anderson R, Cokkinides VE, Murray T, Henley J, Liff J, Thun MJ. “Cancer Mortality in the United States by Education Level and Race”. Journal of the National Cancer Institute. 2007;99((18)):1384–94. doi: 10.1093/jnci/djm127. [DOI] [PubMed] [Google Scholar]
- Alberg AJ, Brock MV, Samet JM. “Epidemiology of Lung Cancer: Looking to the Future”. Journal of Clinical Oncology. 2005;23((14)):3175–85. doi: 10.1200/JCO.2005.10.462. [DOI] [PubMed] [Google Scholar]
- American Cancer Society. 2008. “Cancer Facts & Figures 2008” [accessed on November 20, 2011]. Available at: http://www.cancer.org/Research/CancerFactsFigures/cancer-facts-figures-2008.
- American Cancer Society. 2009. “Cancer Facts & Figures 2009” [accessed on November 20, 2011]. Available at: http://www.cancer.org/Research/CancerFactsFigures/cancer-facts-figures-2009.
- American Cancer Society. 2011. “ Cancer Facts & Figures for African Americans 2011-2012 ” [accessed on March 7, 2012]. Available at: http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-027765.pdf.
- Angel JL, Buckley CJ, Finch BK. “Nativity and Self-Assessed Health among Pre-Retirement Age Hispanics and Non-Hispanic Whites”. International Migration Review. 2001;35((3)):784–803. [Google Scholar]
- Ayanian JZ. “Determinants of Racial and Ethnic Disparities in Surgical Care”. World Journal of Surgery. 2008;32((4)):509–15. doi: 10.1007/s00268-007-9344-4. [DOI] [PubMed] [Google Scholar]
- Bach PB, Cramer LD, Warren JL, Begg CB. “Racial Differences in Treatment of Early-State Lung Cancer”. New England Journal of Medicine. 1999;341:1198–200. doi: 10.1056/NEJM199910143411606. [DOI] [PubMed] [Google Scholar]
- Berg CJ, Thomas JL, Guo HF, An LC, Okuyemi KS, Collins TC, Ahluwalia JS. “Predictors of Smoking Reduction among Blacks”. Nicotine & Tobacco Research. 2010;12((4)):423–31. doi: 10.1093/ntr/ntq019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackstock WB, Paskett ED, Perry MC, Grazinao SL, Muscato JJ, Kosty MP, Akerley WL, Holland J, Fleishman S, Green MR. “Outcomes among African-American/Non African American Patients with Advanced Non Small Cell Lung Carcinoma: Report from the Cancer and Leukemia Group B”. Journal of the National Cancer Institute. 2002;94:284–90. doi: 10.1093/jnci/94.4.284. [DOI] [PubMed] [Google Scholar]
- Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E. “Socioeconomic Disparities in Health in the United States: What the Patterns Tell Us”. American Journal of Public Health. 2010;100(Suppl 1):S186–96. doi: 10.2105/AJPH.2009.166082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clegg LX, Reichman ME, Miller BA, Hankey BF, Singh GK, Lin YD, Goodman MT, Lynch CF, Schwartz SM, Chen VW, Bernstein L, Gomez SL, Graff JJ, Lin CC, Johnson NJ, Edwards BK. “Impact of Socioeconomic Status on Cancer Incidence and Stage at Diagnosis: Selected Findings from the Surveillance, Epidemiology, and End Results: National Longitudinal Mortality Study”. Cancer Causes and Control. 2009;20((4)):417–35. doi: 10.1007/s10552-008-9256-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole ER. “Intersectionality and Research in Psychology”. American Psychologist. 2009;64((3)):170–80. doi: 10.1037/a0014564. [DOI] [PubMed] [Google Scholar]
- Council of Economic Advisers. Changing America: Indicators of Social and Economic Well-Being by Race and Hispanic Origin. Washington, DC: U.S. Government Printing Office; 1998. [Google Scholar]
- Courtenay WH. “Constructions of Masculinity and Their Influence on Men's Well-Being: A Theory of Gender and Health”. Social Science and Medicine. 2000;50:1385–401. doi: 10.1016/s0277-9536(99)00390-1. [DOI] [PubMed] [Google Scholar]
- Cykert S, Dilworth-Anderson P, Monroe MH, Walker P, McGuire FR, Corbie-Smith G, Edwards LJ, Bunton AJ. “Factors Associated with Decisions to Undergo Surgery among Patients with Newly Diagnosed Early-Stage Lung Cancer”. Journal of the American Medical Association. 2010;303((23)):2368–76. doi: 10.1001/jama.2010.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dell JL, Whitman S, Shah AM, Silva A, Ansell D. “Smoking in 6 Diverse Chicago Communities–A Population Study”. American Journal of Public Health. 2005;95((6)):1036–42. doi: 10.2105/AJPH.2004.051169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delva J, Tellez M, Finlayson TL, Gretebeck KA, Siefert K, Williams DR, Ismail AI. “Cigarette Smoking among Low-Income African Americans: A Serious Public Health Problem”. American Journal of Preventive Medicine. 2005;29((3)):218–20. doi: 10.1016/j.amepre.2005.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dey AN, Lucas JW. “Physical and Mental Health Characteristics of U.S. And Foreign-Born Adults: United States.” Advance Data from Vital and Health Statistics. Hyattsville, Maryland: National Center for Health Statistics; 2006. [PubMed] [Google Scholar]
- Domhoff GW. 2011. “Who Rules America? Power in America. Wealth, Income, and Power” [accessed on November 20, 2011]. Available at: http://www2.ucsc.edu/whorulesamerica/power/wealth.html.
- Earle CC, Venditti LN, Neumann PJ, Gelber RD, Weinstein MC, Potosky AL, Weeks JC. “Who Gets Chemotherapy for Metastatic Lung Cancer?”. Chest. 2000;117((5)):1239–46. doi: 10.1378/chest.117.5.1239. [DOI] [PubMed] [Google Scholar]
- Earle CC, Neumann PJ, Gelber RD, Weinstein MC, Weeks JC. “Impact of Referral Patterns on the Use of Chemotherapy for Lung Cancer”. Journal of Clinical Oncology. 2002;20((7)):1786–92. doi: 10.1200/JCO.2002.07.142. [DOI] [PubMed] [Google Scholar]
- Food and Drug Administration. “Tobacco Control Act National Longitudinal Study of Tobacco Users” [accessed on November 20, 2011]. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm274626.htm.
- deFur PL, Evans GW, Cohen Hubal EA, Kyle AD, Morello-Frosch RA, Williams DR. “Vulnerability as a Function of Individual and Group Resources in Cumulative Risk Assessment”. Environmental Health Perspectives. 2007;115((5)):817–24. doi: 10.1289/ehp.9332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillum RF, Sullins DP. “Cigarette Smoking during Pregnancy: Independent Associations with Religious Participation”. Southern Medical Journal. 2008;101((7)):686–92. doi: 10.1097/SMJ.0b013e31817a76cc. [DOI] [PubMed] [Google Scholar]
- Goodman RM, Speers MA, McLeroy K, Fawcett S, Kegler M, Parker E, Rathgeb Smith S, Sterling TD, Wallerstein N. “Identifying and Defining the Dimensions of Community Capacity to Provide a Basis for Measurement”. Health Education and Behavior. 1998;25((3)):258–78. doi: 10.1177/109019819802500303. [DOI] [PubMed] [Google Scholar]
- Gordon HS, Street RL, Jr, Sharf BF, Kelly PA, Souchek J. “Racial Differences in Trust and Lung Cancer Patients' Perceptions of Physician Communication”. Journal of Clinical Oncology. 2006;24((6)):904–9. doi: 10.1200/JCO.2005.03.1955. [DOI] [PubMed] [Google Scholar]
- Greaves L, Vallone D, Velicer W. “Special Effects: Tobacco Policies and Low Socioeconomic Status Girls and Women”. Journal of Epidemiology and Community Health. 2006;60(suppl 2):ii1–2. doi: 10.1136/jech.2006.052480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenland S. “Ecologic Versus Individual-Level Sources of Bias in Ecologic Estimates of Contextual Health Effects”. International Journal of Epidemiology. 2001;30:1343–50. doi: 10.1093/ije/30.6.1343. [DOI] [PubMed] [Google Scholar]
- Haiman CA, Stram DO, Wilkens LR, Pike MC, Kolonel LN, Henderson BE, Le Marchand L. “Ethnic and Racial Differences in the Smoking-Related Risk of Lung Cancer”. New England Journal of Medicine. 2006;354((4)):333–42. doi: 10.1056/NEJMoa033250. [DOI] [PubMed] [Google Scholar]
- Herd P, Goesling B, House JS. “Socioeconomic Position and Health: The Differential Effects of Education Versus Income on the Onset Versus Progression of Health Problems”. Journal of Health and Social Behavior. 2007;48((3)):223–38. doi: 10.1177/002214650704800302. [DOI] [PubMed] [Google Scholar]
- Howard G, Anderson RT, Russell G, Howard VJ, Burke GL. “Race, Socioeconomic Status, and Cause-Specific Mortality”. Annals of Epidemiology. 2000;10((4)):214–23. doi: 10.1016/s1047-2797(00)00038-7. [DOI] [PubMed] [Google Scholar]
- Jackson PB, Williams DR. “The Intersection of Race, Gender and SES: Health Paradoxes.”. In: Schulz AJ, Mullings L, editors. Gender, Race, Class & Health: Intersectional Approaches. San Francisco: Jossey-Bass Publishers; 2006. pp. 131–62. [Google Scholar]
- Kagawa-Singer M, Valdez Dadia A, Yu MC, Surbone A. “Cancer, Culture, and Health Disparities: Time to Chart a New Course?”. CA: A Cancer Journal for Clinicians. 2010;60((1)):12–39. doi: 10.3322/caac.20051. [DOI] [PubMed] [Google Scholar]
- Kaufman JS, Cooper RS. “Telomeres and Race: What Can We Learn About Human Biology from Health Differentials?”. Aging Cell. 2008;7((4)):448–50. doi: 10.1111/j.1474-9726.2008.00396.x. [DOI] [PubMed] [Google Scholar]
- Krieger N, Williams DR, Moss N. “Measuring Social Class in U.S. Public Health Research: Concepts, Methodologies, and Guidelines”. Annual Review of Public Health. 1997;18:341–78. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- Krieger N, Quesenberry C, Jr, Peng T, Horn-Ross P, Stewart S, Brown S, Swallen K, Guillermo T, Suh D, Alvarez-Martinez L, Ward F. “Social Class, Race/Ethnicity, and Incidence of Breast, Cervix, Colon, Lung, and Prostate Cancer among Asian, Black, Hispanic, and White Residents of the San Francisco Bay Area, 1988-92 (United States)”. Cancer Causes and Control. 1999;10((6)):525–37. doi: 10.1023/a:1008950210967. [DOI] [PubMed] [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramaniam SV, Carson R. “Geocoding and Monitoring of Us Socioeconomic Inequalities in Mortality and Cancer Incidence: Does the Choice of Area-Based Measure and Geographic Level Matter? The Public Health Disparities Geocoding Project”. American Journal of Epidemiology. 2002;156:471–82. doi: 10.1093/aje/kwf068. [DOI] [PubMed] [Google Scholar]
- Lara M, Gamboa C, Kahramanian M, Morales LS, Bautista DE. “Acculturation and Latino Health in the United States: A Review of the Literature and Its Sociopolitical Context”. Annual Review of Public Health. 2005;26:367–97. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVeist TA. “Disentangling Race and Socioeconomic Status: A Key to Understanding Health Inequalities”. Journal of Urban Health. 2005;82(2 Suppl 3):26–34. doi: 10.1093/jurban/jti061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVeist TA, Thorpe RJ, Mance GA, Jackson J. “Overcoming Confounding of Race with Socio-Economic Status and Segregation to Explore Race Disparities in Smoking”. Addiction. 2007;102(Suppl. 2):65–70. doi: 10.1111/j.1360-0443.2007.01956.x. [DOI] [PubMed] [Google Scholar]
- Logan JR, Deane G. “Black Diversity of Metropolitan America” [accessed on November 20, 2011]. Available at: http://mumford1.dyndns.org/cen2000/BlackWhite/BlackDiversityReport/Black_Diversity_final.pdf.
- Major JM, Doubeni CA, Freedman ND, Park Y, Lian M, Hollenbeck AR, Schatzkin A, Graubard BI, Sinha R. “Neighborhood Socioeconomic Deprivation and Mortality: NIH-AARP Diet and Health Study”. PLoS ONE. 2010;5((11)):e15538. doi: 10.1371/journal.pone.0015538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margolis ML, Christie JD, Silvestri GA, Kaiser L, Santiago S, Hansen-Flaschen J. “Racial Differences Pertaining to a Belief About Lung Cancer Surgery: Results of a Multicenter Survey”. Annals of Internal Medicine. 2003;139((7)):558–63. doi: 10.7326/0003-4819-139-7-200310070-00007. [DOI] [PubMed] [Google Scholar]
- Massey DS. “Residential Segregation and Neighborhood Conditions in US Metropolitan Areas”. In: Smelser NJ, Wilson WJ, Mitchell F, National Research Council (US), editors. America Becoming: Racial Trends and Their Consequences. Washington, DC: National Academy Press; 2001. pp. 391–434. [Google Scholar]
- McLeroy KR, Norton BL, Kegler MC, Burdine JN, Sumaya CV. “Community-Based Interventions”. American Journal of Public Health. 2003;93((4)):529–33. doi: 10.2105/ajph.93.4.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mok TS, Wu YL, Thongprasert S, Yang CH, Chu DT, Saijo N, Sunpaweravong P, Han B, Margono B, Ichinose Y, Nishiwaki Y, Ohe Y, Yang JJ, Chewaskulyong B, Jiang HJ, Duffield EL, Watkins CL, Armour AA, Fukuoka M. “Gefitinib or Carboplatin-Paclitaxel in Pulmonary Adenocarcinoma”. New England Journal of Medicine. 2009;361((10)):947–57. doi: 10.1056/NEJMoa0810699. [DOI] [PubMed] [Google Scholar]
- Molina JR, Yang P, Cassivi SD, Schild SE, Adjei AA. “Non-Small Cell Lung Cancer: Epidemiology, Risk Factors, Treatment, and Survivorship”. Mayo Clinic Proceedings. 2008;83((5)):584–94. doi: 10.4065/83.5.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morello-Frosch R, Jesdale BM. “Separate and Unequal: Residential Segregation and Estimated Cancer Risks Associated with Ambient Air Toxics in US Metropolitan Areas”. Environmental Health Perspectives. 2006;114((3)):386–93. doi: 10.1289/ehp.8500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Cancer Institute. Bethesda, MD: U.S. Department of Health and Human Services, National Institues of Health, National Cancer Institute; 2008. “The Role of the Media in Promoting and Reducing Tobacco Use.”. Tobacco Control Monograph No. 19. [Google Scholar]
- National Center for Health Statistics. Health, United States. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2010. [Google Scholar]
- Paez JG, Janne PA, Lee JC, Tracy S, Greulich H, Gabriel S, Herman P, Kaye FJ, Lindeman N, Boggon TJ, Naoki K, Sasaki H, Fujii Y, Eck MJ, Sellers WR, Johnson BE, Meyerson M. “EGFR Mutations in Lung Cancer: Correlation with Clinical Response to Gefitinib Therapy”. Science. 2004;304((5676)):1497–500. doi: 10.1126/science.1099314. [DOI] [PubMed] [Google Scholar]
- Potosky AL, Saxman S, Wallace RB, Lynch CF. “Population Variations in the Initial Treatment of Non-Small-Cell Lung Cancer”. Journal of Clinical Oncology. 2004;22((16)):3261–8. doi: 10.1200/JCO.2004.02.051. [DOI] [PubMed] [Google Scholar]
- Primack BA, Bost JE, Land SR, Fine MJ. “Volume of Tobacco Advertising in African American Markets: Systematic Review and Meta-Analysis”. Public Health Reports. 2007;122((5)):607–15. doi: 10.1177/003335490712200508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramos E, Rotimi C. “The A's, G's, C's, and T's of Health Disparities”. BMC Medical Genomics. 2009;2:29. doi: 10.1186/1755-8794-2-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JnG, Gorman BK. “Gender Inequalities in US Adult Health: The Interplay of Race and Ethnicity”. Social Science and Medicine. 2006;62((5)):1045–65. doi: 10.1016/j.socscimed.2005.07.009. [DOI] [PubMed] [Google Scholar]
- Schulz AJ, Mullings L. Gender, Race, Class, and Health: Intersectional Approaches. San Francisco: Jossey-Bass; 2006. [Google Scholar]
- Sen G, Iyer A, Mukherjee C. “A Methodology to Analyse the Intersections of Social Inequalities in Health”. Journal of Human Development and Capabilities. 2009;10((3)):397–415. [Google Scholar]
- Shepherd FA, Rodrigues Pereira J, Ciuleanu T, Tan EH, Hirsh V, Thongprasert S, Campos D, Maoleekoonpiroj S, Smylie M, Martins R, van Kooten M, Dediu M, Findlay B, Tu D, Johnston D, Bezjak A, Clark G, Santabárbara P, Seymour L. “Erlotinib in Previously Treated Non–Small-Cell Lung Cancer”. New England Journal of Medicine. 2005;353((2)):123–32. doi: 10.1056/NEJMoa050753. [DOI] [PubMed] [Google Scholar]
- Shields AE, Crown WH. “Incorporating Genomic Information into Disparities Research Methods: Reducing Measurement Error and Selection Bias”. Health Services Research. 2012 doi: 10.1111/j.1475-6773.2012.01413.x. doi: 10.1111/j.1475-6773.2012.01413.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh GK, Miller BA. “Health, Life Expectancy, and Mortality Patterns among Immigrant Populations in the United States”. Canadian Journal of Public Health. 2004;95((3)):I14–21. doi: 10.1007/BF03403660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh GK, Miller BA, Hankey BF, Edwards BK. Area Socioeconomic Variations in Us Cancer Incidence, Mortality, Stage, Treatment, and Survival, 1975-1999. Bethesda: National Cancer Institute; 2003. NCI Cancer Surveillance Monograph Series, Number 4. [Google Scholar]
- Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- Takeuchi DT, Zane N, Hong S, Chae DH, Gong F, Gee GC, Walton E, Sue S, Alegria M. “Immigration-Related Factors and Mental Disorders among Asian Americans”. American Journal of Public Health. 2007;97((1)):84–90. doi: 10.2105/AJPH.2006.088401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thun MJ, Henley SJ, Burns D, Jemal A, Shanks TG, Calle EE. “Lung Cancer Death Rates in Lifelong Nonsmokers”. Journal of the National Cancer Institute. 2006;98((10)):691–9. doi: 10.1093/jnci/djj187. [DOI] [PubMed] [Google Scholar]
- United States Centers for Disease Control and Prevention. 2011. “Youth and Tobacco Use” [accessed on November, 2011]. Available at: http://www.cdc.gov/tobacco/data_statistics/fact_sheets/youth_data/tobacco_use/index.htm.
- Wallace JM, Brown TN, Bachman JG, Laveist TA. “The Influence of Race and Religion on Abstinence from Alcohol, Cigarettes and Marijuana among Adolescents”. Journal of Studies on Alcohol. 2003;64:843–8. doi: 10.15288/jsa.2003.64.843. [DOI] [PubMed] [Google Scholar]
- Ward E, Jemal A, Cokkinides V, Singh GK, Cardinez C, Ghafoor A, Thun M. “Cancer Disparities by Race/Ethnicity and Socioeconomic Status”. CA: A Cancer Journal for Clinicians. 2004;54((2)):78–93. doi: 10.3322/canjclin.54.2.78. [DOI] [PubMed] [Google Scholar]
- Webb MS, Carey MP. “Tobacco Smoking among Low-Income Black Women: Demographic and Psychosocial Correlates in a Community Sample”. Nicotine & Tobacco Research. 2008;10((1)):219–29. doi: 10.1080/14622200701767845. [DOI] [PubMed] [Google Scholar]
- Weber L, Fore ME. “Race, Ethnicity, and Health: An Intersectional Approach”. In: Vera H, Feagin JR, editors. Handbooks of the Sociology of Racial and Ethnic Relations. New York: Springer US; 2007. pp. 191–218. [Google Scholar]
- Weber L, Parra-Medina D. “Intersectionality and Women's Health: Charting a Path to Eliminating Health Disparities”. Advances in Gender Research. 2003;7:181–230. [Google Scholar]
- White KR, Haas JS, Williams DR. “Elucidating the Role of Place in Health Care Disparities: The Example of Racial/Ethnic Residential Segregation “. Health Services Research. 2012 doi: 10.1111/j.1475-6773.2012.01410.x. doi: 10.1111/j.1475-6773.2012.01410.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whooley MA, Boyd AL, Gardin JM, Williams DR. “Religious Involvement and Cigarette Smoking in Young Adults — the Cardia Study”. Archives of Internal Medicine. 2002;162((14)):1604–10. doi: 10.1001/archinte.162.14.1604. [DOI] [PubMed] [Google Scholar]
- Williams DR. “The Health of Men: Structured Inequalities and Opportunities”. American Journal of Public Health. 2003;93((5)):724–31. doi: 10.2105/ajph.93.5.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Collins C. “Racial Residential Segregation: A Fundamental Cause of Racial Disparities in Health”. Public Health Reports. 2001;116:404–16. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA. “Discrimination and Racial Disparities in Health: Evidence and Needed Research”. Journal of Behavioral Medicine. 2009;32((1)):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA, Leavell J, Collins C. “Race, Socioeconomic Status, and Health: Complexities, Ongoing Challenges, and Research Opportunities”. Annals of the New York Academy of Sciences 1186. 2010:69–101. doi: 10.1111/j.1749-6632.2009.05339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright ER, Perry BL. “Medical Sociology and Health Services Research”. Journal of Health and Social Behavior. 2010;51(Suppl 1):S107–19. doi: 10.1177/0022146510383504. [DOI] [PubMed] [Google Scholar]
- Yorio JT, Xie Y, Yan J, Gerber DE. “Lung Cancer Diagnostic and Treatment Intervals in the United States: A Health Care Disparity?”. Journal of Thoracic Oncology. 2009;4((11)):1322–30. doi: 10.1097/JTO.0b013e3181bbb130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaslavsky AM, Ayanian JZ. “Integrating Research on Racial and Ethnic Disparities in Health Care over Place and Time”. Medical Care. 2005;43((4)):303–7. doi: 10.1097/01.mlr.0000159975.43573.8d. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


