Abstract
OBJECTIVE
It has been postulated that the effectiveness of bariatric surgery varies between ethnic groups. However, data regarding this topic are inconclusive, as most studies included few patients from minority groups. We conducted a meta-analysis to determine the difference in percentage of excess weight loss (%EWL) 1–2 years after bariatric surgery in people of African and Caucasian descent. We also studied differences in diabetes mellitus (DM) remission.
RESEARCH DESIGN AND METHODS
We performed a MEDLINE and EMBASE search for studies reporting %EWL and/or DM remission after bariatric surgery and including both African Americans and Caucasians. The 613 publications obtained were reviewed. We included 14 studies (1,087 African Americans and 2,714 Caucasians); all provided data on %EWL and 3 on DM remission. We extracted surgery type, %EWL, and DM remission 1–2 years after surgery. After analyzing %EWL for any surgery type, we performed subanalyses for malabsorptive and restrictive surgery.
RESULTS
The overall absolute mean %EWL difference between African Americans and Caucasians was −8.36% (95% CI −10.79 to −5.93) significantly in favor of Caucasians. Results were similar for malabsorptive (−8.39% [−11.38 to −5.40]) and restrictive (−8.46% [−12.95 to −3.97]) surgery. The remission of DM was somewhat more frequent in African American patients than in Caucasian patients (1.41 [0.56–3.52]). However, this was not statistically significant.
CONCLUSIONS
In %EWL terms, bariatric surgery is more effective in Caucasians than in African Americans, regardless of procedure type. Further studies are needed to investigate the exact mechanisms behind these disparities and to determine whether ethnic differences exist in the remission of comorbidities after bariatric surgery.
Obesity and its associated morbidities have become a major public health problem in both developed and developing countries (1). Compared with conventional behavioral and pharmacological interventions, bariatric surgery is the only long-lasting, effective treatment for morbidly obese patients (2). Besides weight loss, another remarkable effect of bariatric surgery is the profound and durable remission of type 2 diabetes (3).
However, the beneficial results after bariatric surgery seem to differ interindividually; indeed, it is postulated that the effectiveness of bariatric surgery, in terms of weight loss, varies between ethnic groups (4–12). Unfortunately, the data published concerning this topic are inconclusive, as most studies included only a few patients from minority groups and/or did not find statistically significant differences between the ethnic groups studied. We conducted a systematic review and meta-analysis to determine the difference in percentage of excess weight loss (%EWL) 1–2 years after bariatric surgery in people of African and Caucasian descent. As a secondary outcome, we studied differences in diabetes mellitus (DM) remission after surgery.
RESEARCH DESIGN AND METHODS
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) was used as a guideline for this study (13).
Together with the clinical librarian at our institution, we performed an electronic search of MEDLINE and EMBASE. We searched publications from 1 January 1978 through 1 November 2011 to identify studies that included patients of both African and Caucasian descent and that reported on %EWL and/or DM remission after bariatric surgery. The following text terms and medical subheading (Mesh) terms were combined: “Bariatric Surgery”[Mesh], bariatric surger*[tiab], gastroplast*[tiab], gastric bypass*[tiab], jejunoileal bypass*[tiab], gastric banding*[tiab], “Obesity, Morbid/surgery”[Mesh], “Obesity/surgery”[Mesh], “Ethnic Groups”[Mesh], ethni*[tiab], multiethnic*, racial[tiab], race[tiab], “African Continental Ancestry Group”[Mesh], blacks[tiab], negroes[tiab], negroid[tiab], ethnology[sh], OR ethnol*[tiab]. We limited our search to research performed in humans and reported in English. The reference lists of included studies were searched manually for further relevant studies.
Study selection
Two reviewers (W.M.A. and F.C.) independently screened the records. Inclusion and exclusion criteria were defined a priori. Agreement on final inclusion was reached by consensus.
A study was included if it reported on %EWL and/or DM remission after bariatric surgery and if it studied patients of both African and Caucasian descent. We excluded studies that had a mean follow-up time of <1 or >2 years after surgery. Studies including patients <18 years of age or with a BMI <35 kg/m2 were excluded as well. No restrictions were imposed regarding publication date and study design. Furthermore, any type of bariatric surgery was included in our analysis (restrictive and malabsorptive procedures as well as a combination of both). Restrictive bariatric surgery was defined as bariatric surgery without any malabsorptive component, whereas malabsorptive bariatric surgery was defined as any type of bariatric surgery that did include a malabsorptive component. We allowed co-interventions such as cholecystectomy.
Data extraction
From the included publications, the following data were extracted: first author, year of publication, study design, type of bariatric surgery, and number of included patients of African and Caucasian descent and their sex and age. Furthermore, we extracted baseline BMI, baseline prevalence of DM, (mean) follow-up time, %EWL 1–2 years after surgery, and the prevalence of DM 1–2 years after surgery. %EWL was defined as described by Deitel et al. (14). The criteria used to classify DM were not the same in all included studies. Therefore, DM was either defined as an HbA1c ≥6.5% and/or use of antidiabetic drugs (15,16) or as a fasting plasma glucose >150 mg/dL and/or use of antidiabetic drugs (12). DM remission was defined as the percentage of those with DM at baseline that had an HbA1c <6.5% (15,16) or a fasting plasma glucose <120 mg/dL (12) and discontinued the use of antidiabetic drugs 1–2 years after surgery.
If data concerning %EWL or DM remission were only available for the total population (and not stratified by ethnic group), we contacted the corresponding author for additional information up to five times, provided that there were >10 patients of African and Caucasian descent included in the study. Furthermore, if only data on %EWL were reported, the corresponding author was contacted for additional information on DM remission in both ethnic groups and vice versa. If we were not able to obtain data on either %EWL or DM remission in patients of both African and Caucasian descent, the study was excluded.
Quality assessment for individual studies and overall quality of evidence
Two reviewers (W.M.A. and F.C.) independently assessed the quality and the risk of bias in each included study using the Newcastle-Ottawa Scale, which has been developed to assess the quality of nonrandomized studies (17). The scale awards a maximum of 9 points to each included study: 4 points for an adequate selection of the study population, 2 points for comparability of case subjects and control subjects (e.g., African Americans and Caucasians) included in the study on the basis of the design and analysis, and 3 points for the adequate ascertainment of the outcome in the study. We defined studies of high quality as those that scored the maximum 9 points on the Newcastle-Ottawa Scale; studies of medium quality scored 7–8 points, and studies that scored <7 points were defined as low quality.
We rated the overall quality of our evidence by considering the quality (as measured by the Newcastle-Ottawa Scale), generalizability, and heterogeneity of included studies, according to recommendations by the Grading of Recommendations Assessment, Development, and Evaluation Working Group (18).
Statistical analysis
The meta-analysis was performed using Review Manager 5.1 (The Cochrane Collaboration, Oxford, U.K.). First, we analyzed the mean absolute difference in %EWL between patients of African and Caucasian descent for any surgery type. Subsequently, we performed subanalyses for malabsorptive and restrictive procedures. For these analyses, data were synthesized using inverse variance with mean difference in %EWL and 95% CIs as the effect measures. If only a P value for the difference between ethnic groups was given without the 95% CI, the SE and 95% CI were calculated using the inverse Student t test. A negative mean difference suggested a %EWL in favor of the patients of Caucasian descent. The data were pooled using a random-effects model. Heterogeneity was assessed using the I2 statistic.
Furthermore, we analyzed the difference in DM remission between patients of African and Caucasian descent. We calculated the number of patients with DM remission from the extracted prevalence of DM before and after surgery. Data were synthesized using Mantel-Haenszel with odds ratios (ORs) as the effect measure. An OR >1 suggested a DM remission in favor of the patients of African descent. Again, the data were pooled using a random-effects model and heterogeneity was assessed using the I2 statistic.
For the analyses concerning %EWL, we performed sensitivity analyses in order to explore the robustness of the data and the influence of certain factors on effect size. Therefore, we repeated our %EWL analysis while excluding studies that did not have follow-up data available at 12 months exactly (for example, studies that had a mean follow-up time of 18 months or studies with 12–24 months of follow-up time). Furthermore, as it has been published that baseline BMI may be negatively associated with weight loss after bariatric surgery (19), we repeated the analysis for %EWL while excluding studies that reported a difference in baseline BMI between patients of African and Caucasian descent >1 kg/m2. Last, we performed a sensitivity analysis in which we only included high-quality studies, based on their Newcastle-Ottawa Scale score.
RESULTS
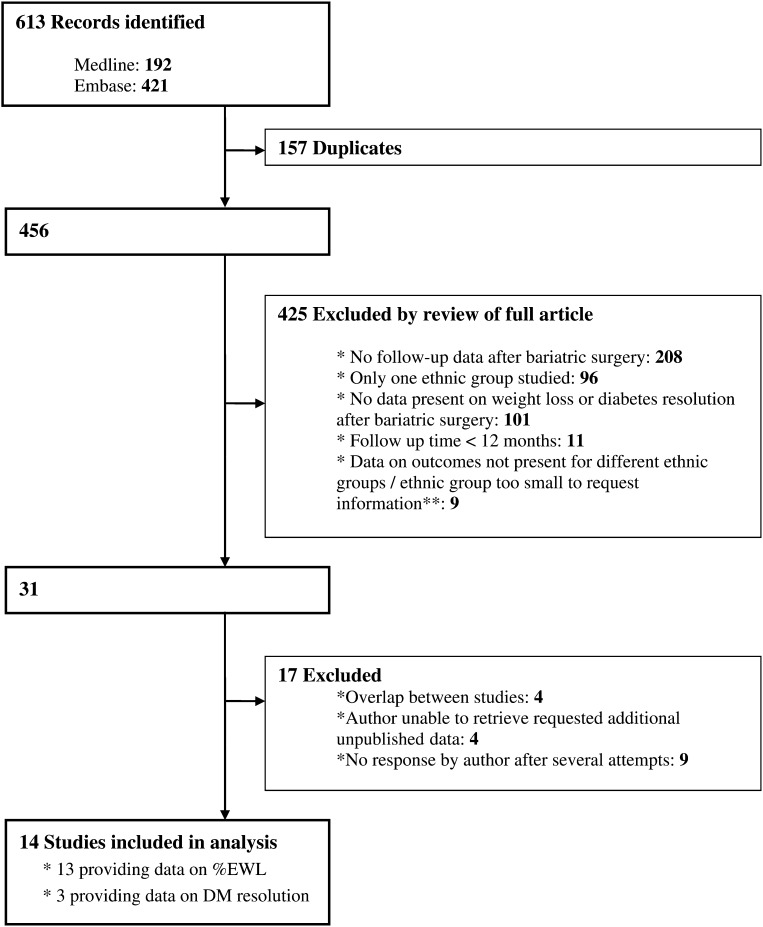
Figure 1 summarizes the study identification and selection process. After removal of duplicates in the EMBASE and MEDLINE search, 456 potentially relevant records were identified. After reviewing these publications, 425 were subsequently excluded: 208 because there were no follow-up data available after bariatric surgery, 96 because there was no inclusion of both African American and Caucasian patients in the study, 101 because there were no follow-up data available on either %EWL or DM remission, 11 because the follow-up time was <12 months, and 9 because data on %EWL and DM remission were missing in a study population that included <10 patients of African and Caucasian descent.
Figure 1.
Study selection. **If data concerning %EWL or DM resolution were only available for the total population (and not stratified by ethnic group), we contacted the corresponding author for additional information, provided that there were more than 10 patients from African and Caucasian descent included in the study.
Of the remaining 31 records, 4 were excluded because the study population in these records was reported in other included research as well (20–23). Thirteen records were excluded after data extraction, as there were no data available on either %EWL or DM remission in both African American and Caucasian patients, and the data could either not be retrieved or there was no response after repeatedly contacting the authors.
Finally, 14 studies were included in the analysis of difference in %EWL (n = 13) (4–12,16,24–26) and difference in DM remission (n = 3) (12,15,16) between patients of African and Caucasian descent. Of the 14 included studies, 9 reported outcomes of malabsorptive bariatric surgery (4,5,7,9,10,12,16,24,26), 4 on restrictive procedures (8,11,25). One study investigated two separate groups in which the effect of either vertical banded gastroplasty (restrictive) or vertical banded gastroplasty combined with gastric bypass (malabsorptive) was studied (6). We entered the data of these two groups separately in our analyses, defining the study as Capella VBG 1993 and Capella VBG-GB 1993.
Two studies reported on the combined outcome of DM improvement and/or DM remission after bariatric surgery (10,11). As we could not retrieve isolated data on DM remission, we did not include these studies in our analysis of DM remission. Table 1 contains the characteristics of the 14 included studies.
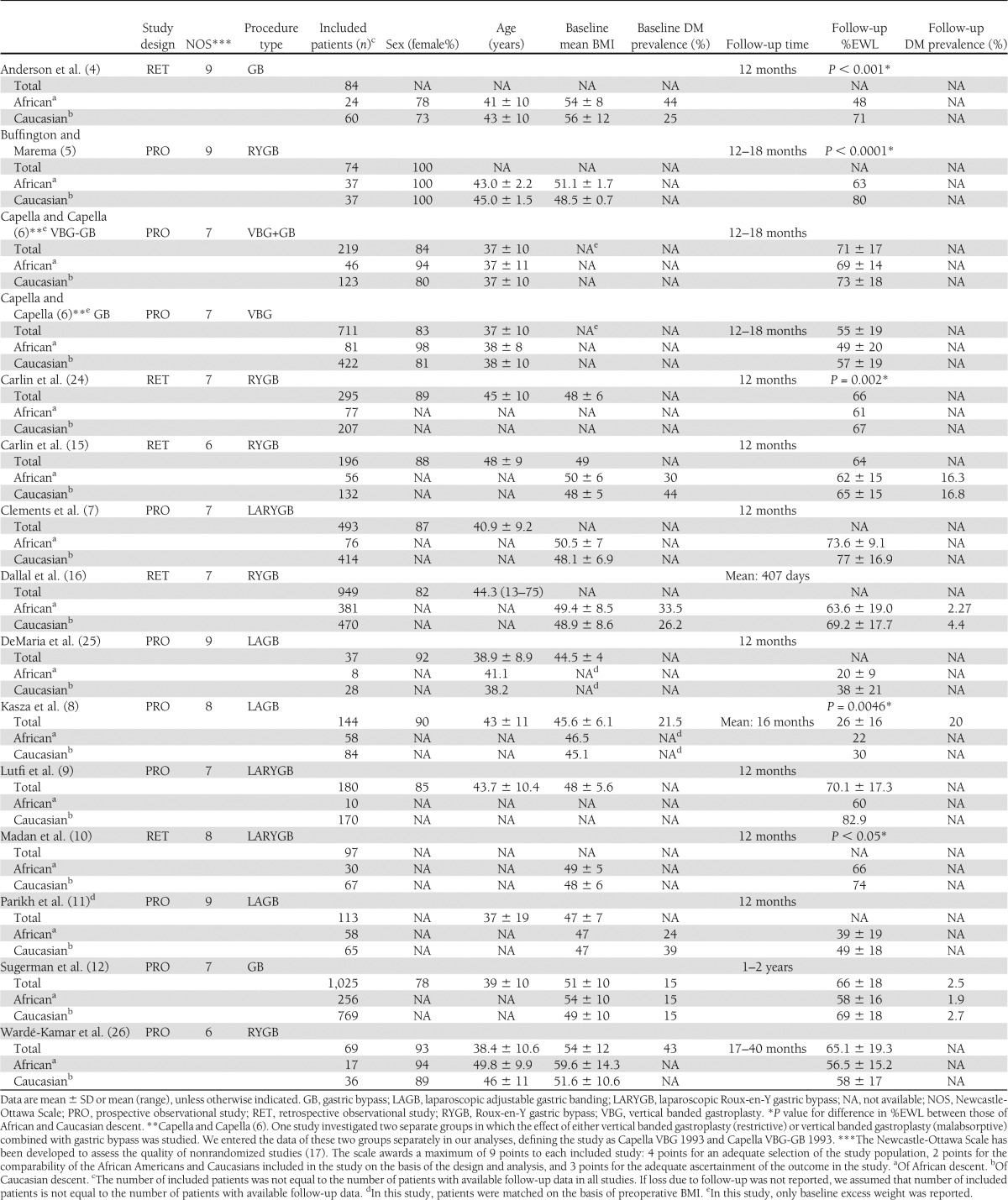
Table 1.
Characteristics of included studies
Risk of bias assessment
Four studies were deemed to be of high quality (4,5,11,25), eight of medium quality (6–10,12,16,24), and two of low quality with a Newcastle-Ottawa Scale score of 6 points (15,26) (Table 1). The studies defined as medium and low quality all had in common that they did not specifically aim at comparing African Americans and Caucasians in the study population. As the comparability of certain factors that might have influenced our outcome, such as baseline BMI or age, was therefore reduced, these studies automatically lost one or two points of the Newcastle-Ottawa Scale score. The two studies that were defined as low quality lost an additional point for other potential bias: the first showed potential participant selection bias because only patients with a diagnosis of hypertension were included (15), and in the second, weight loss results were based on self-reported weight data of the patients (26).
Across studies, the main bias related to difference in the type of bariatric surgery and follow-up time. Furthermore, as criteria used to classify DM were not the same in all included studies, the comparability of the prevalence of DM in these studies was reduced.
Difference in %EWL between patients of African and Caucasian descent
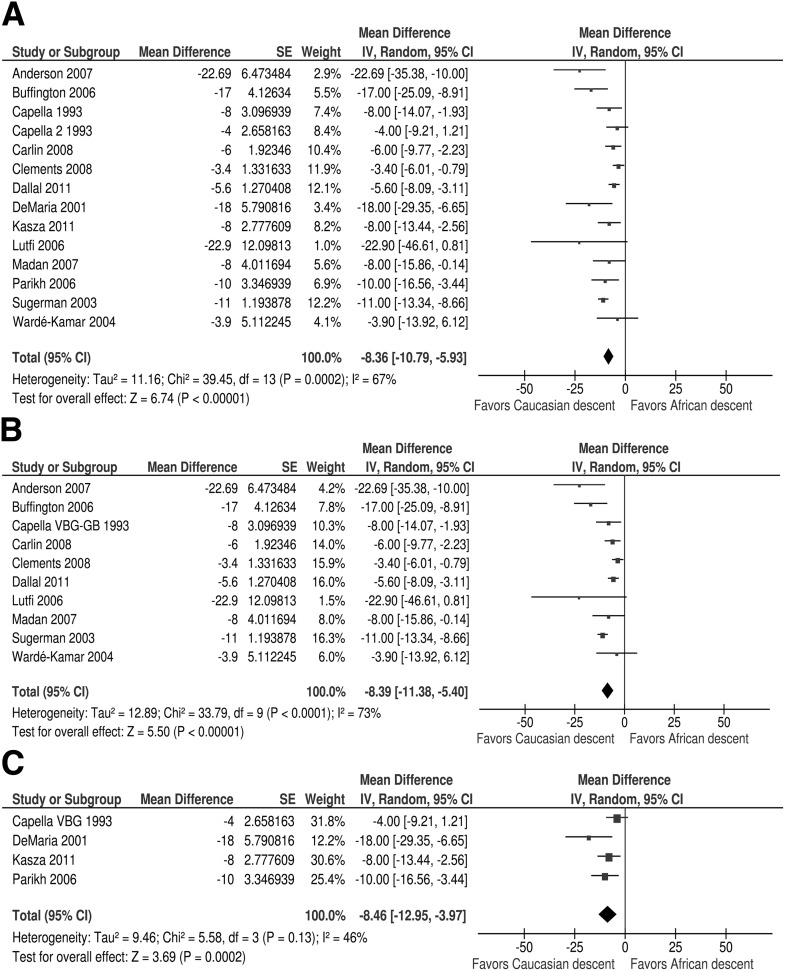
The analysis of the pooled data on difference in %EWL 1–2 years after surgery contained 1,087 patients of African descent and 2,714 patients of Caucasian descent (Fig. 2A). When we included all types of bariatric surgery in the analysis, the mean difference in %EWL between the ethnic groups was −8.36% (95% CI −10.79 to −5.93), significantly in favor of the patients of Caucasian origin.
Figure 2.
A: %EWL in people of African and Caucasian descent 1–2 years after bariatric surgery. B: %EWL in people of African and Caucasian descent 1–2 years after bariatric surgery (malabsorptive bariatric surgery). C: %EWL in people of African and Caucasian descent 1–2 years after bariatric surgery (restrictive bariatric surgery). Forest plots showing mean difference and 95% CIs.
The subanalysis for malabsorptive surgery contained 920 patients of African descent and 2,424 patients of Caucasian descent (Fig. 2B). The mean difference in %EWL was −8.39% (95% CI −11.38 to −5.40), significantly in favor of the Caucasian patients as well. The subanalyses for restrictive surgery, containing 167 African American and 290 Caucasian patients, showed similar results (a mean difference in %EWL of −8.46% [−12.95 to −3.97] in favor of Caucasian patients) (Fig. 2C).
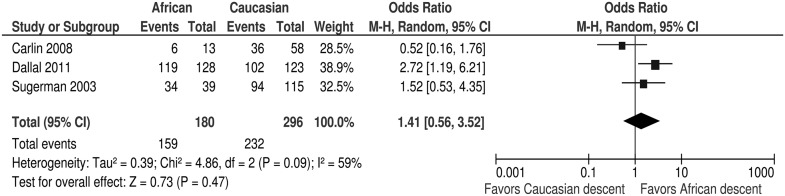
Difference in DM remission
The analysis of the pooled data on difference in remission of DM contained 195 African American and 342 Caucasian patients (Fig. 3). The remission of DM was somewhat more frequent in African American than in Caucasian patients (1.41 [95% CI 0.56–3.52]). However, this was not statistically significant.
Figure 3.
Remission of DM in people of African and Caucasian descent 1–2 years after bariatric surgery. Forest plot showing OR and 95% CIs. M-H, Mantel-Haenszel.
Sensitivity analyses
First, we investigated whether the difference in %EWL between patients of African and Caucasian descent after any type of bariatric surgery would be influenced if the studies that reported only mean follow-up times, or variable follow-up times (i.e., a follow-up time of 12–18 months) different than exactly 12 months, were excluded. Therefore, we removed four studies with a follow-up time of between 1 and 2 years (5,6,8,12) and two studies with a mean follow-up time of 407 days (16) and 17–40 months (26) from the analysis. The subsequent sensitivity analysis (including African American and Caucasian patients) did not alter our earlier findings; the mean difference in %EWL after any type of bariatric surgery between the ethnic groups was −9.41% (95% CI −13.82 to −4.99), still in favor of the Caucasian patients (data not shown).
Furthermore, we examined the effect of differences in baseline BMI between the ethnic groups on the difference in %EWL after surgery. In this second sensitivity analysis, we therefore only included studies that reported a difference in baseline BMI of ≤1 kg/m2 between patients of African and Caucasian origin (four studies, including 475 African Americans and 624 Caucasians) (10,11,16,25). Again, our findings remained similar; the mean difference in %EWL was −8.49% (95% CI −12.74 to −4.23) in favor of the Caucasian patients (data not shown).
Last, we only included studies that were considered high quality based on Newcastle-Ottawa scores (four studies, including 110 African Americans and 165 Caucasians) (4,5,11,25). In this analysis, the mean difference in %EWL was −14.72 (95% CI −19.09 to −10.36), still in favor of the Caucasian patients (data not shown).
Publication bias
Supplementary Fig. 1 shows a funnel plot examining possible publication bias of the results on the difference in %EWL between those of African and Caucasian descent. One study showed possible small-study publication bias (9). After excluding this study from the analysis of the pooled data on difference in %EWL, our findings remained similar; the mean difference in %EWL was −7.33 (95% CI −8.50 to −6.17) in favor of the Caucasian patients (data not shown). We did not examine possible publication bias of the results on difference in DM remission, as guidelines do not recommend testing for funnel plot asymmetry in analyses of <10 studies (27).
Overall quality of evidence
The overall quality of the evidence on the difference in %EWL between African American and Caucasian patients was moderate. Most studies in our meta-analysis consistently showed a greater %EWL in patients of Caucasian descent than those of African descent. Apart from one study that only scored 6 points (26), all studies were graded 7 points or above on the 9-point Newcastle-Ottawa Scale for quality. The studies were heterogeneous (67%) (Fig. 2A), and we used random-effects models for the meta-analyses. Sensitivity analyses showed good robustness of the data concerning %EWL. Overall, we regarded our results on the difference in %EWL between African American and Caucasian patients to be generalizable to other populations undergoing bariatric surgery.
We regarded the overall quality of evidence on the difference in DM remission between the ethnic groups as poor, as there were only three studies included in the analysis (12,15,16). One of these studies only had a score of 6 points on the Newcastle-Ottawa Scale (15). Furthermore, the studies were heterogeneous (59%) (Fig. 3). Due to the few included studies on DM remission, we were not able to perform subgroup analyses on DM remission.
CONCLUSIONS
This meta-analysis shows that in terms of %EWL, bariatric surgery is more effective in patients of Caucasian descent than in patients of African descent, regardless of the type of surgery. Sensitivity analyses show good robustness of the data concerning %EWL. Furthermore, although based on limited data, this meta-analysis suggests that despite the difference in %EWL, there are no statistically significant differences in remission of DM between these ethnic groups after surgery.
The etiology of the difference in weight loss between patients of African and Caucasian descent is not clear. Biological, psychological, genetic, and socioeconomic factors have all been suggested to play a role. Several studies have shown that Caucasians have greater improvement in energy expenditure and maximum uptake of oxygen in response to diet and exercise weight loss interventions than African Americans, suggesting a decreased weight loss efficiency among African Americans (28–30).
Although it has been published that African Americans are less physically active and consume a diet higher in calories than their Caucasian counterparts (31), Buffington and Marema (5) and Wardé-Kamar et al. (26) did not find any significant differences in calorie or nutrient composition of intake after bariatric surgery between African Americans and Caucasians. This suggests that diet may not be a major contributor to the difference in %EWL after bariatric surgery.
In the U.S., African Americans usually have a lower socioeconomic background than their Caucasian counterparts (7). As a low socioeconomic status is known to be associated with obesity and most studies included were conducted in the U.S. (32), this might partly explain the ethnic difference in weight loss after bariatric surgery as well. However, because socioeconomic data were not reported in the studies analyzed, this remains speculative.
We found that, despite the difference in %EWL, there were no statistically significant differences in remission of DM between African American and Caucasian patients after surgery. This finding has to be interpreted with caution, as the results of the analysis concerning DM remission were based on the pooled data of only three studies, yielding a wide confidence interval of the reported OR. Furthermore, aspects that may have influenced DM remission after bariatric surgery, such as the duration of DM at baseline, remaining β-cell function, and amount of antidiabetic medication used by the patients, could not be taken into account in this meta-analysis, as data on these topics were not reported in the included studies. For these reasons, we cannot be certain of the extent to which our results concerning DM remission can be attributed to biological differences between the ethnic groups. However, as it is known that ethnic differences in the regulation of glucose homeostasis, as well as insulin secretion, action, and metabolism, exist (33), a contributing explanation for our finding might be that DM in the African American patients is determined more by insulin resistance than in the Caucasian patients.
The knowledge that ethnic differences in weight loss after bariatric surgery exist is useful because this can help professionals provide realistic treatment expectations to all patients. It should be taken into account, however, that the achieved amount of %EWL in African American patients is not necessarily disappointing; in most of the studies on malabsorptive surgery, the %EWL in African American patients was >60%. Furthermore, our finding that there was no ethnic difference in DM remission despite a lower amount of %EWL in African American patients, although based on limited data, suggests that the metabolical significance of the difference in %EWL between African American and Caucasian patients may be limited. Indeed, Parikh et al. (11) have shown that even with moderate weight loss, comorbidity remission can be achieved. As for mortality benefit, this is related to comorbidity remission and not weight loss per se (34). Further prospective studies are needed to determine ethnic differences in remission of comorbidities after bariatric surgery.
This meta-analysis has its limitations. First of all, we have to accept the disadvantage of a meta-analysis of observational studies; it is inevitable that the differences in study design between the included studies will somewhat bias the results of the pooled data (35).
Although most studies scored considerably well in the Newcastle-Ottawa Scale, many of these studies probably did not control for all possible confounders. For example, we were not able to adjust our results for baseline BMI. In most of the included studies, the baseline BMI was (slightly) higher in African American patients than in Caucasian patients. As it has been published that a higher baseline BMI may negatively affect the amount of %EWL (19), this may have affected the outcomes of our study. However, when we excluded the studies that had a difference in BMI >1 kg/m2 between African American and Caucasian patients, this did not alter our results. Another factor that might have biased the results of this meta-analysis was that we were not able to adjust for socioeconomic status, sex, and age, as there was no or limited data present on these variables stratified by ethnic group in the included studies. These and other hidden confounders, as well as the differing study designs used, might have affected the results of the individual studies and hence the results of the pooled data.
Concerning our results on DM remission, a major limitation is the few studies we were able to include in our analysis. The published data on an ethnic difference in DM remission after bariatric surgery are scarce. Furthermore, the definition of DM was not the same in all studies, which reduced comparability of the prevalence of DM in these studies. Moreover, some studies that did provide follow-up data on DM did not distinguish DM remission from improvement and were therefore excluded from our analysis (10,11). In addition, we were not able to adjust for factors that might have influenced our results concerning DM remission, such as DM duration at baseline, remaining β-cell function, and the amount of antidiabetic medication used. Finally, as DM remission after bariatric surgery is lower after 10 years than after 2 years (36), our limited follow-up time precludes a definitive statement about long-term DM status.
All in all, this meta-analysis shows that in terms of %EWL, bariatric surgery is less successful in patients of African descent than in patients of Caucasian descent. Despite these ethnic differences, bariatric surgery should absolutely be considered as a long-lasting and effective treatment for morbidly obese individuals of African and Caucasian descent. Further prospective studies are needed to both determine ethnic differences in remission of comorbidities after bariatric surgery and to investigate the exact mechanism behind these ethnic disparities.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
W.M.A. reviewed literature, extracted data, and wrote the manuscript. F.C. reviewed literature, extracted data, and drafted the manuscript. V.E.G. and J.B.H. reviewed and critiqued the manuscript. R.M.D. extracted data and reviewed and critiqued the manuscript. F.H. provided supervision and reviewed and critiqued the manuscript. All authors significantly contributed to the work and approved the manuscript for submission. W.M.A. and F.C. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Parts of this study were presented in abstract form at the 72nd Scientific Sessions of the American Diabetes Association, 8–12 June 2012, Philadelphia, Pennsylvania.
The authors acknowledge Heleen C. Dyserinck (Academic Medical Centre) for her help in performing the electronic search and Rob J. Scholten (Academic Medical Centre) for his excellent support in the data synthesis.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc12-0260/-/DC1.
References
- 1.Finucane MM, Stevens GA, Cowan MJ, et al. Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Body Mass Index) National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet 2011;377:557–567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sjöström L, Narbro K, Sjöström CD, et al. Swedish Obese Subjects Study Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med 2007;357:741–752 [DOI] [PubMed] [Google Scholar]
- 3.Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med 2009;122:248–256, e5 [DOI] [PubMed] [Google Scholar]
- 4.Anderson WA, Greene GW, Forse RA, Apovian CM, Istfan NW. Weight loss and health outcomes in African Americans and whites after gastric bypass surgery. Obesity (Silver Spring) 2007;15:1455–1463 [DOI] [PubMed] [Google Scholar]
- 5.Buffington CK, Marema RT. Ethnic differences in obesity and surgical weight loss between African-American and Caucasian females. Obes Surg 2006;16:159–165 [DOI] [PubMed] [Google Scholar]
- 6.Capella RF, Capella JF. Ethnicity, type of obesity surgery and weight loss. Obes Surg 1993;3:375–380 [DOI] [PubMed] [Google Scholar]
- 7.Clements RH, Yellumahanthi K, Wesley M, Ballem N, Bland KI. Hyperparathyroidism and vitamin D deficiency after laparoscopic gastric bypass. Am Surg 2008;74:469–474 [PubMed] [Google Scholar]
- 8.Kasza J, Brody F, Vaziri K, et al. Analysis of poor outcomes after laparoscopic adjustable gastric banding. Surg Endosc 2011;25:41–47 [DOI] [PubMed] [Google Scholar]
- 9.Lutfi R, Torquati A, Sekhar N, Richards WO. Predictors of success after laparoscopic gastric bypass: a multivariate analysis of socioeconomic factors. Surg Endosc 2006;20:864–867 [DOI] [PubMed] [Google Scholar]
- 10.Madan AK, Whitfield JD, Fain JN, et al. Are African-Americans as successful as Caucasians after laparoscopic gastric bypass? Obes Surg 2007;17:460–464 [DOI] [PubMed] [Google Scholar]
- 11.Parikh M, Lo H, Chang C, Collings D, Fielding G, Ren C. Comparison of outcomes after laparoscopic adjustable gastric banding in African-Americans and whites. Surg Obes Relat Dis 2006;2:607–610 [DOI] [PubMed] [Google Scholar]
- 12.Sugerman HJ, Wolfe LG, Sica DA, Clore JN. Diabetes and hypertension in severe obesity and effects of gastric bypass-induced weight loss. Ann Surg 2003;237:751–756; discussion 757–758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009;151:264–269, W64 [DOI] [PubMed]
- 14.Deitel M, Gawdat K, Melissas J. Reporting weight loss 2007. Obes Surg 2007;17:565–568 [DOI] [PubMed] [Google Scholar]
- 15.Carlin AM, Yager KM, Rao DS. Vitamin D depletion impairs hypertension resolution after Roux-en-Y gastric bypass. Am J Surg 2008;195:349–352 [DOI] [PubMed]
- 16.Dallal RM, Hatalski A, Trang A, Chernoff A. Longitudinal analysis of cardiovascular parameters after gastric bypass surgery. Surg Obes Relat Dis. 6 October 2011 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 17.Wells GA, O'Connell D, Peterson J, Welch V, Lossos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses, 2011. Available from http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp Accessed 1 November 2011
- 18.Guyatt GH, Oxman AD, Vist GE, et al. GRADE Working Group GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924–926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Livhits M, Mercado C, Yermilov I, et al. Preoperative predictors of weight loss following bariatric surgery: systematic review. Obes Surg 2012;22:70–89 [DOI] [PubMed] [Google Scholar]
- 20.Carlin AM, Rao DS, Yager KM, Genaw JA, Parikh NJ, Szymanski W. Effect of gastric bypass surgery on vitamin D nutritional status. Surg Obes Relat Dis 2006;2:638–642 [DOI] [PubMed] [Google Scholar]
- 21.O'Connor EA, Carlin AM. Lack of correlation between variation in small-volume gastric pouch size and weight loss after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis 2008;4:399–403 [DOI] [PubMed] [Google Scholar]
- 22.Parikh M, Ayoung-Chee P, Romanos E, et al. Comparison of rates of resolution of diabetes mellitus after gastric banding, gastric bypass, and biliopancreatic diversion. J Am Coll Surg 2007;205:631–635 [DOI] [PubMed] [Google Scholar]
- 23.Parikh MS, Fielding GA, Ren CJUS. experience with 749 laparoscopic adjustable gastric bands: intermediate outcomes. Surg Endosc 2005;19:1631–1635 [DOI] [PubMed] [Google Scholar]
- 24.Carlin AM, O'Connor EA, Genaw JA, Kawar S. Preoperative weight loss is not a predictor of postoperative weight loss after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis 2008;4:481–485 [DOI] [PubMed] [Google Scholar]
- 25.DeMaria EJ, Sugerman HJ, Meador JG, et al. High failure rate after laparoscopic adjustable silicone gastric banding for treatment of morbid obesity. Ann Surg 2001;233:809–818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wardé-Kamar J, Rogers M, Flancbaum L, Laferrère B. Calorie intake and meal patterns up to 4 years after Roux-en-Y gastric bypass surgery. Obes Surg 2004;14:1070–1079 [DOI] [PubMed] [Google Scholar]
- 27.Higgins JPT and Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org. Accessed 1 November 2011
- 28.Foster GD, Wadden TA, Swain RM, Anderson DA, Vogt RA. Changes in resting energy expenditure after weight loss in obese African American and white women. Am J Clin Nutr 1999;69:13–17 [DOI] [PubMed] [Google Scholar]
- 29.Washburn RA, Kline G, Lackland DT, Wheeler FC. Leisure time physical activity: are there black/white differences? Prev Med 1992;21:127–135 [DOI] [PubMed] [Google Scholar]
- 30.Weinsier RL, Hunter GR, Zuckerman PA, et al. Energy expenditure and free-living physical activity in black and white women: comparison before and after weight loss. Am J Clin Nutr 2000;71:1138–1146 [DOI] [PubMed] [Google Scholar]
- 31.Burke GL, Sprafka JM, Folsom AR, Luepker RV, Norsted SW, Blackburn H. Trends in CHD mortality, morbidity and risk factor levels from 1960 to 1986: the Minnesota Heart Survey. Int J Epidemiol 1989;18(Suppl. 1):S73–S81 [PubMed] [Google Scholar]
- 32.Bove CF, Olson CM. Obesity in low-income rural women: qualitative insights about physical activity and eating patterns. Women Health 2006;44:57–78 [DOI] [PubMed] [Google Scholar]
- 33.Osei K, Schuster DP. Ethnic differences in secretion, sensitivity, and hepatic extraction of insulin in black and white Americans. Diabet Med 1994;11:755–762 [DOI] [PubMed] [Google Scholar]
- 34.Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA 2004;292:1724–1737 [DOI] [PubMed] [Google Scholar]
- 35.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008–2012 [DOI] [PubMed] [Google Scholar]
- 36.Sjöström L, Lindroos AK, Peltonen M, et al. Swedish Obese Subjects Study Scientific Group Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med 2004;351:2683–2693 [DOI] [PubMed] [Google Scholar]