Abstract
We previously showed that a pandemic virus, A/Tennessee/560/09(H1N1), had the potential to adapt to human bronchial epithelial cells by the acquisition of hemagglutinin (HA) K154Q and polymerase acidic (PA) protein L295P mutations that conferred a more virulent phenotype. To better elucidate the role of each mutations, we generated recombinant viruses carrying single mutations or both mutations concurrently. The replication of all mutant viruses was significantly higher than that of the wild-type A/Tennessee/560/09 virus in human cells. The HA K154Q mutation reduced the receptor binding affinity of A/Tennessee/560/09 virus to 6-Su-6’SLN and biantennary 6’SLN receptors. In ferrets, H1N1 virus with HA K154Q and PA L295P mutations exhibited significantly higher titers in the upper respiratory tract compared to all other viruses 6 days post-infection. Our results suggest that both single mutations HA K154Q and PA L295P are necessary for delayed virus clearance of A/Tennessee/560/09(H1N1) influenza virus in a ferret animal model.
Keywords: influenza virus, H1N1, ferret, shedding
Introduction
We previously showed that the 2009 A(H1N1) pandemic influenza virus (A(H1N1)pdm09) could be further adapted to normal human bronchial epithelial (NHBE) cells through the acquisition of two mutations (hemagglutinin K154Q and polymerase acidic protein L295P). The adapted virus replicated more efficiently in NHBE cells and had a delayed clearance phenotype in ferrets as compared to the unadapted virus. The polymerase acidic (PA) protein mutation increased polymerase activity by 20% at 37°C, and the hemagglutinin (HA) change affected binding of the virus to α2,6-sialyl receptors (Ilyushina, Ducatez, et al. 2010). It was not determined, however, which of these mutations was responsible for the ferret delayed clearance phenotype. To better understand the role of each of these 2 mutations in increasing the pathogenicity and delaying virus clearance, single mutants were generated, and their pathogenicity was studied in the ferret model.
Material and Methods
Viruses
The gene segments of the A(H1N1)pdm09 virus A/Tennessee/560/09 (TN/09) were cloned into a dual-promoter plasmid, pHW2000 (Hoffmann, Stech, et al. 2001). Site-directed mutagenesis was performed using the QuickChange Site-Directed Mutagenesis kit (Stratagen, La Jolla, CA) on A/Tennessee/560/09 pHW2000 HA and PA plasmids. Four reverse genetics (rg) viruses were generated by DNA transfection as described previously (Hoffmann, Stech, et al. 2001): (rg)-A/Tennessee/560/09 (TN/09), rg-A/Tennessee/560/09-PA L295P mutant (PAmut), rg-A/Tennessee/560/09-HA K154Q mutant (HAmut, H1 numbering), and rg-A/Tennessee/560/09-HA K154Q mutant and PAL295P mutant (HAmutPAmut). Each viral gene segment was sequenced to confirm the identity of the virus.
Replication kinetics of rg H1N1 influenza viruses
We used primary NHBE cells from human tracheal/bronchial tissues obtained from Lonza (Walkersville, MD) and they were grown and differentiated as previously described (Matrosovich et al., PNAS, 2004). To determine multistep growth curve kinetics on NHBE cells, triplicate cell cultures growing in 12-mm-diameter inserts were inoculated via the apical side with each virus at a multiplicity of infection (MOI) of 0.1 at 33°C or 37°C. After 1 h of incubation, the inoculum was removed. Viruses released into the apical compartment of NHBE cells were harvested at the indicated time points by the apical addition and collection of 300 µl of medium allowed to equilibrate for 30 min at 33°C or 37°C. The virus titers were determined as log10 numbers of plaque-forming units (PFU)/ml in Madin-Darby canine kidney (MDCK) cells.
Receptor-binding assay
The binding specificity of the A(H1N1)pdm09 viruses was investigated in a direct binding assay as described previously (Gambaryan & Matrosovich 1992). Plates were coated with viruses at a titer of 4–8 hemagglutination units (50 µl/well) at 4°C for 16 h, followed by washing with 0.05% Tween 20 in phosphate-buffered saline (PBS-T). After the addition of biotinylated sialoglycopolymer (Table 1), 30 µl/well in a working buffer of PBS supplemented with 0.02% of Tween 20, 0.02% bovine serum albumin, and 3 µM neuraminidase inhibitor oseltamivir ([3R,4R,5S]-4-acetamido-5-amino-3-[1-ethylpropoxy]-1-cyclohexene-1-carboxylic acid) was plated and incubated at 4°C for 1 h. The starting concentration of biotinylated sialoglycopolymers was 20 µM on sialic acid, and 2-fold serial dilutions were used. Plates were washed with a cold PBS-T and incubated with streptavidin peroxidase in the working buffer at 4°C for 1 h. After washing, 100 µl/well of substrate solution (0.1 M sodium acetate, pH 5.0, containing 4 mM o-phenylenediamine and 0.004% H2O2) was added, and the reaction was stopped with 2 M H2SO4. Optical density was determined at 492 nm with a Multiscan plate reader (Labsystems, Finland). The dissociation constants (Kass) were determined as 1/Neu5Ac concentration at the point Amax/2 of Scatchard plots. The reported data represent the mean of at least two individual experiments for each virus.
Table 1.
Synthetic oligosaccharide-polyacrylamides in form of sialoglycopolymers (conjugates with soluble polyacrylamide) used to test the receptor specificity of H1N1 viruses
| Structure of oligosaccharide | Abbreviation |
|---|---|
| Neu5Acα2–3Galβ1–4Glcβ | 3′SL |
| Neu5Acα2–3Galβ1–4GlcNAcβ | 3′SLN |
| Neu5Acα2–6Galβ1–4Glcβ | 6′SL |
| Neu5Acα2–6Galβ1–4GlcNAcβ | 6′SLN |
| Neu5Gcα2-6Galβ1-4GlcNAcβ | 6'SLN(Gc) |
| (Neu5Acα2-6Galβ1-4GlcNAcβ1-2Man)2-3,6-Manβ1-4-GlcNAcβ1-4GlcNAcβ | biantennary 6’SLN |
| Neu5Acα2-6Galβ | Neu5Ac6Gal |
| Neu5Acα2-6GalNAcα | SiaTn |
| Neu5Gcα2-6GalNAcα | Neu5Gc-Tn |
| Neu5Acα2-6Galβ1-4-(6-Su)GlcNAcβ | 6-Su-6’SLN |
| Galβ1-3 | 6-SiaTF |
| GalNAcα | |
| Neu5Acα2-6 | |
| Neu5Acα2-3 | 3,6-SiaTn |
| GalNAcα | |
| Neu5Acα2-6 | |
| (9-NAc-Neu5Acα2-6)Galβ1-4GlcNAcβ | 6’-(Neu5,9-NAc2)LacNAc |
| Neu5Acα-OCH2C6H4 | Neu5AcBn |
Sulfated trisaccharide 6-Su-6’SLN was synthesized as described previously (Pazynina et al., 2008). Biotinylated sialoglycopolymers (~30 kDa) with different saccharide residues were synthesized as previously described (Bovin et al., 1993) and were used to characterize the receptor specificity of H1N1 influenza A viruses.
Ferret experiments
Pathogenicity was tested in 4- to 5-month-old male ferrets obtained from Marshall Farms (North Rose, NY). All ferrets were seronegative for circulating influenza A(H1N1) and A(H3N2) and influenza B viruses. Ferrets (three per group) were inoculated intranasally under light isoflurane anesthesia with 106 plaque forming units (PFU) of TN/09, HAmut, PAmut, or HAmutPAmut virus in 1 ml of sterile PBS. Clinical signs of infection, relative inactivity index (Reuman et al. 1989), weight, and temperature were recorded daily. To monitor virus shedding, nasal washes were collected from ferrets 1, 2, 4, 6, and 8 days post inoculation (dpi). The virus titers were determined as log10PFU/ml in Madin-Darby canine kidney (MDCK) cells. Protein concentrations in nasal washes were also determined to assess the level of inflammation and measured by using BioRad Protein Assay Dye Reagent (Hercules). One animal per group was euthanized under isoflurane anesthesia by intracardiac injection of Euthanasia V solution 3 dpi, and tissue samples (~0.5 g each) were collected from lungs (4 to 5 lobes tested separately), nasal turbinate, trachea, spleen, liver, and small intestine. Samples were homogenized in 1 ml of culture medium with antibiotics, and the virus titer (log10PFU per gram of tissue) was determined in MDCK cells. Tissues (lung, nasal turbinate, trachea, spleen, liver, and small intestine) were also collected at the time of necropsy for histopathologic analysis. They were fixed in 10% neutral-buffered formalin and embedded in paraffin. Sections 5 µm thick were stained with hematoxylin and eosin and studied by light microscopy. Serum samples were collected from ferrets 3 weeks after inoculation, treated with receptor-destroying enzyme, heat-inactivated at 56°C for 30 minutes, and tested by hemagglutination inhibition (HI) assay with 0.5% packed turkey red blood cells by a standard method as described previously in the World Health Organization manual on animal influenza diagnosis and surveillance (WHO n.d.). All animal experiments were performed in biosafety level 2+ facilities at St. Jude Children’s Research Hospital (Memphis, TN). All animal studies were approved by the St. Jude animal care and use committee and were conducted according to applicable laws and guidelines.
Results and Discussion
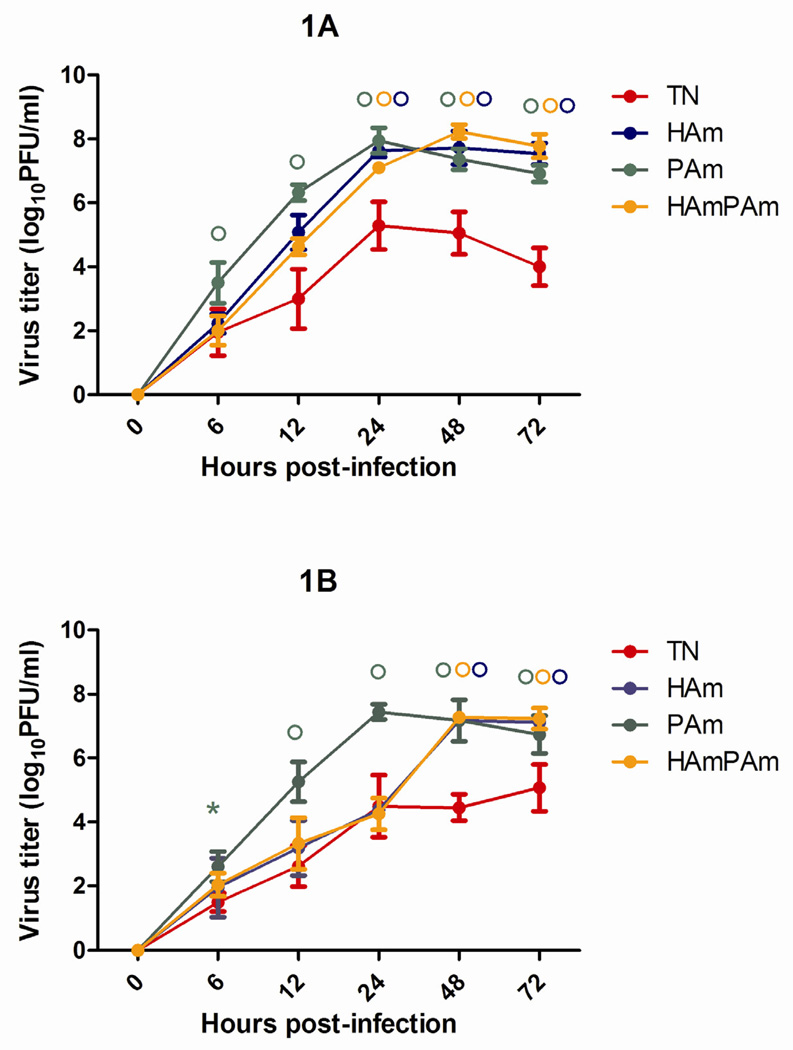
We first studied the replication kinetics of recombinant A(H1N1)pdm09 viruses by assessment of their viral yields in comparison with wild-type TN/09 after multiple replication cycles in NHBE cells (Figure 1). The replication levels of HAmut, PAmut, and HAmutPAmut were significantly higher than that of TN/09 12, 24, 48, and 72 hours after infection at 37°C (>0.9–3.2 logs; P<0.05, Figure 1A). The yield of the PAmut virus was significantly higher compared to wild-type virus at all post-infection time points at 33°C (P<0.05) and higher titers of HAmut and HAmutPAmut compared to TN/09 were observed 48 and 72 hours after infection at 33°C (>2.0–2.8 logs; P<0.01, Figure 1B). Therefore, our results showed that both single mutations HA K154Q and PA L295P confer significantly higher replication of A/Tennessee/560/09 strain in human epithelial cells (P<0.05).
Figure 1.
Replication of rg-A/Tennessee/560/09 (TN/09, in red), rg-A/Tennessee/560/09-HA K154Q mutant (HAmut, in blue), rg-A/Tennessee/560/09-PA L295P mutant (PAmut, in green), and rg-A/Tennessee/560/09-HA K154Q mutant and PA L295P mutant (HAmutPAmut, in orange) in NHBE cells. NHBE cultures were infected via the apical side with each virus at an MOI 0.1 at either 37°C (A) or 33°C (B). The progeny viruses released from the apical surfaces of infected cultures were collected at the indicated time points and titrated in MDCK cells by performing a plaque assay. Representative results expressed as log10 numbers of PFU/ml from two independent experiments are shown. * P < 0.05, ° P < 0.01 compared with the value for TN/09 virus (one-way ANOVA).
We previously observed similar polymerase activities for G1 (with the PA L295P mutation) and TN/09 viruses at 33°C (Ilyushina, Ducatez et al., 2010). The present study unexpectedly shows that PAmut replicates significantly better than HAmutPAmut (rg-G1) at 33°C on NHBE cells (Figure 1B). We could speculate that although no increase in polymerase activity was observed with PA L295P mutation at 33°C, the mutation may still contribute to increasing the level of RNA transcription for example. If real, this virus replication advantage conferred by PA L295P at both temperatures could explain why this mutation prevails in all A(H1N1)pdm09 strains.
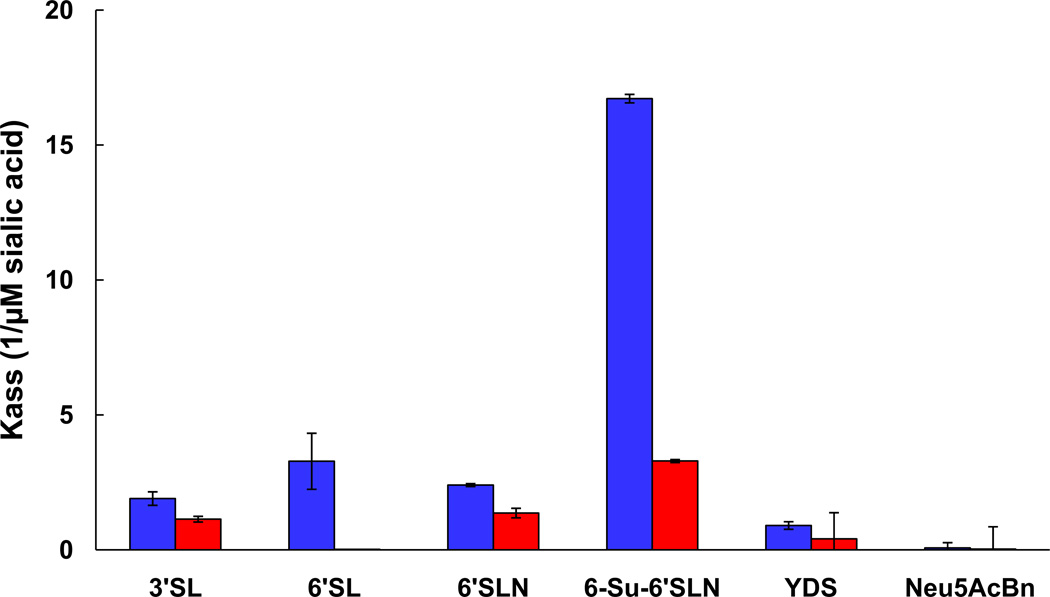
We then compared the binding properties of TN/09 and HAmut in more detail using a direct binding assay (Gambaryan & Matrosovich 1992). As previously observed, the viruses had similar affinity for 6’-SLN sialoglycopolymer, but HAmut was unable to bind to 6’-SL (Ilyushina, Ducatez, et al. 2010). In addition, we compared the binding affinity of the viruses to ten α2,6-and two α2,3-sialyl receptors (Table 1) and observed less binding of HAmut than of TN/09 to 3’SL, 6-Su-6’SLN, and biantennary 6’SLN receptors (Figure 2) and no binding of either virus to the remaining receptors tested (data not shown). Our findings suggest a refinement of receptor-binding properties of HAmut. The observed reduced binding to a few receptors might explain why HA K154Q does not seem prevalent in nature: of 8546 A(H1N1)pdm09 HA sequences available on GenBank, only 2 have K154Q: A/Arequipa/WRAIR9939F/2009 (accession number: ADX97028) and A/Dakar/WRAIR0020T/2010 (accession number: ADX96288).
Figure 2.
Receptor specificity of rg-A/Tennessee/560/09 (TN/09, in blue) and rg-A/Tennessee/560/09-HA K154Q mutant (HAmut, in red) (H1N1) influenza viruses. Association constants (Kass) of virus complexes with sialylglycopolymers conjugated to 3’SL, 6´SL, 6´SLN, 6-Su-6’SLN, biantennary 6’SLN, and Neu5AcBn are shown. Higher Kass values indicate stronger binding.
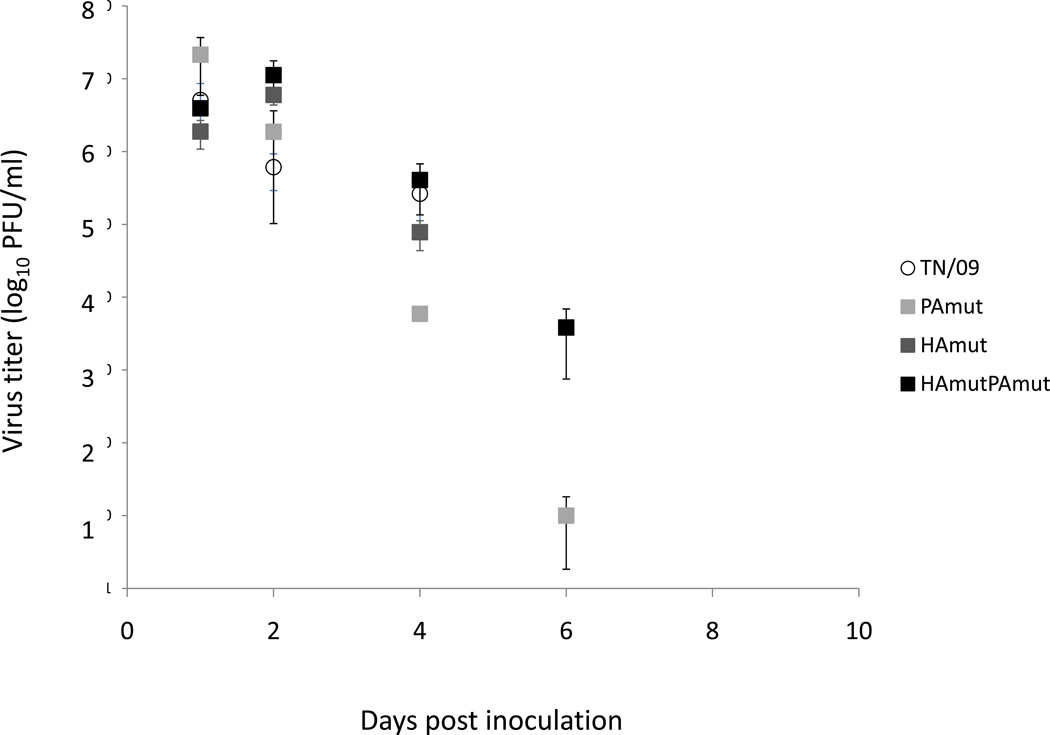
In our previous study, G1 (TN/09 with HA K154Q and PA L295P mutations) showed an increased virulence and delayed clearance in vivo in the ferret model (Ilyushina, Ducatez, et al. 2010). In the present study, all ferrets infected with TN/09 as well as the 3 mutant viruses had very mild clinical signs, and no difference between groups was observed. Until 4 dpi, there was no significant difference in nasal wash titers between mutants and the parental strain, but we observed a delayed virus clearance for HAmutPAmut (just as observed with G1), illustrated by a nasal wash titer 6 dpi of 3.6 log10 PFU/ml, while all other ferrets had cleared their virus (except for one PAmut-infected animal still shedding 1.3 log10 PFU/ml in the upper respiratory tract, Figure 3). Table 2 summarizes the data from the ferret organs collected 3 dpi. Although the necropsy of a single animal per group does not allow for statistical analysis, we observed slightly higher virus titers and larger tissue tropism for HAmutPAmut than for HAmut and PAmut. Interestingly, only the animals infected with HAmutPAmut had detectable virus titers in the small intestine, as did the G1-infected ferrets in our previous study (Table 2 and (Ilyushina, Ducatez, et al. 2010)). All ferrets seroconverted to similar levels with HI titers >640 and no difference was observed between groups as far as inflammation was concerned (protein concentrations in nasal washes, data not shown). In conclusion for the in vivo experiments, both HA K154Q and PA L295P mutations contribute to increasing A(H1N1)pdm09 pathogenicity, and they are both necessary for delayed virus clearance.
Figure 3.
Ferrets’ virus titers in the upper respiratory tract (nasal washes) after infection with rg-A/Tennessee/560/09 (TN/09, open circles), rg-A/Tennessee/560/09-PA L295P mutant (PAmut, light gray squares), rg-A/Tennessee/560/09-HA K154Q mutant (HAmut, dark gray squares), and rg-A/Tennessee/560/09-HA K154Q mutant and PAL295P mutant (HAmutPAmut, black squares). Values are the mean ± SD for two ferrets (or three ferrets on days 1 and 2 post infection) and expressed as log10 PFU/ml. The limit of virus detection was 1 log10PFU/ml. For calculation of the mean, samples with a virus titer <1 log10PFU/ml were assigned a value of 0.
Table 2.
Histopathology and virus titers in ferret organs
| Challenge virus |
Organ/tissue | Virus titer (log10 PFU/ml)1 |
Histopathology score in the lung2 |
|---|---|---|---|
| HAmut | Nasal turbinate | 6.62 | |
| Lung | 5.40 (4/5) | 12.5 (4/4) | |
| Trachea | 5.67 | ||
| Small intestine | – | ||
| Spleen | – | ||
| Liver | – | ||
| PAmut | Nasal turbinate | 5.41 | |
| Lung | 4.46 (2/4) | 14 (3/4) | |
| Trachea | 4 | ||
| Small intestine | – | ||
| Spleen | – | ||
| Liver | – | ||
| HAmutPAmut | Nasal turbinate | 6.48 | |
| Lung | 4.52 (4/4) | 17.75 (4/4) | |
| Trachea | 6.62 | ||
| Small intestine | 2.04 | ||
| Spleen | – | ||
| Liver | – | ||
Organs were sampled from a single ferret in each group. For the lung, mean viral titer for the 4 to 5 lung lobes sampled per ferret. Number of lung lobes positive/total number of lobes tested is indicated in parenthesis.
Scores indicated correspond to mean scores for symptomatic ferret lung lobes tested. Lesions were scored from 0 to 29 taking into account the percentage of tissue involved (scored from 0 to 3 for none to >75%) and the lesion intensity (0 for none to 3 for diffuse or compact) in the bronchi, submucosal glands, bronchioles, alveoli, and interstitium. Number of lung lobes positive/total number of lobes tested is indicated in parenthesis.
Molecular determinants of H1N1 influenza virus pathogenicity have been described. Mutations of HA have been linked with an increased binding to α2,6-sialyl receptors 90D and 225D (R. Xu et al. 2012), T200A and E227A synergistically (R. P. de Vries et al. 2011), E227A (van Doremalen et al. 2011), and I219K (Jayaraman et al. 2011) or a decreased binding for D222G (Belser et al. 2011; Abed et al. 2011). HA K119N, G155E, S183P, R221K, D222G, and D225G lead to increased virulence in mice (L. Xu et al. 2010; Ilyushina, Khalenkov, et al. 2010; L. Xu et al. 2010; Abed et al. 2011; Zheng et al. 2010). The role of HA K154Q and PA L295P in modification of receptor binding affinity and increased pathogenicity has so far been described only in our previous study (Ilyushina, Ducatez, et al. 2010). However, a synergistic role of influenza HA and PA proteins has recently been reported with HA D222G, HA K163E, and PA F35L together increasing A(H1N1)pdm09 virulence in mice. HA D222G altered the receptor binding properties of the virus, and PA F35L increased its polymerase activity (Seyer et al. 2012); the mutant virus was therefore similar to our G1 or HAmutPAmut strain. Although HA- and PA-associated mutations in A(H1N1)pdm09 virus had previously been reported (Ilyushina, Khalenkov, et al. 2010; Sakabe et al. 2011; Ye et al. 2010), our study together with the work of Seyer et al. clearly show the synergy between the two proteins and may contribute to a better understanding of viral protein interactions.
Highlights.
-
-
HA K154Q and PA L295P mutations increase the replication of A/Tennessee/560/09 in NHBE cells
-
-
HA K154Q results in a refinement of receptor-binding properties of H1N1 2009 pandemic virus
-
-
HA K154Q and PA L295P have a synergistic or additive effect to increase H1N1 virus pathogenicity
-
-
HA K154Q and PA L295P have a synergistic or additive effect to delay virus clearance in ferrets
Acknowledgments
We thank Jeri Carol Crumpton, Jennifer DeBeauchamp, and Ashley Webb for excellent technical assistance; Beth Little, Lisa Kercher, and David Carey for the assistance with animal work in the ABSL2+ laboratory; and David Galloway for editorial assistance. We acknowledge the Hartwell Center for Bioinformatics and Biotechnology at St. Jude Children’s Research Hospital for assistance with the sequencing. This study was supported by the National Institute of Allergy and Infectious Diseases, National Institutes of Health, Department of Health and Human Services under Contract No. HHSN266200700005C, by the American Lebanese Syrian Associated Charities (ALSAC), and by RAS Presidium program "Molecular and Cell Biology" (N.V.Bovin).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Abed Y, et al. The 2009 pandemic H1N1 D222G hemagglutinin mutation alters receptor specificity and increases virulence in mice but not in ferrets. J. Infect. Dis. 2011;204(7):1008–1016. doi: 10.1093/infdis/jir483. [DOI] [PubMed] [Google Scholar]
- 2.Belser JA, et al. Effect of D222G mutation in the hemagglutinin protein on receptor binding, pathogenesis and transmissibility of the 2009 pandemic H1N1 influenza virus. PloS One. 2011;6(9):e25091. doi: 10.1371/journal.pone.0025091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bovin NV, et al. Synthesis of polymeric neoglycoconjugates based on N-substituted polyacrylamides. Glycoconj. J. 1993;10(2):142–151. doi: 10.1007/BF00737711. [DOI] [PubMed] [Google Scholar]
- 4.van Doremalen N, et al. A single amino acid in the HA of pH1N1 2009 influenza virus affects cell tropism in human airway epithelium, but not transmission in ferrets. PloS One. 2011;6(10):e25755. doi: 10.1371/journal.pone.0025755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gambaryan AS, Matrosovich MN. A solid-phase enzyme-linked assay for influenza virus receptor-binding activity. J. Virol.Methods. 1992;39(1–2):111–123. doi: 10.1016/0166-0934(92)90130-6. [DOI] [PubMed] [Google Scholar]
- 6.Hoffmann E, Stech J, et al. Universal primer set for the full-length amplification of all influenza A viruses. Arch. Virol. 2001;146(12):2275–2289. doi: 10.1007/s007050170002. [DOI] [PubMed] [Google Scholar]
- 7.Ilyushina NA, Ducatez MF, et al. Does pandemic A/H1N1 virus have the potential to become more pathogenic? [Accessed January 25, 2012];mBio. 2010 1(5) doi: 10.1128/mBio.00249-10. Available at: http://www.ncbi.nlm.nih.gov/pubmed/21116343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ilyushina NA, Khalenkov AM, et al. Adaptation of pandemic H1N1 influenza viruses in mice. J. Virol. 2010;84(17):8607–8616. doi: 10.1128/JVI.00159-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jayaraman A, et al. A single base-pair change in 2009 H1N1 hemagglutinin increases human receptor affinity and leads to efficient airborne viral transmission in ferrets. PloS One. 2011;6(3):e17616. doi: 10.1371/journal.pone.0017616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matrosovich MN, et al. Human and avian influenza viruses target different cell types in cultures of human airway epithelium. PNAS. 2004;101(13):4620–4624. doi: 10.1073/pnas.0308001101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pazynina GV, et al. Synthesis of mono-, di- and tri-O-sulfated N-acetyllactosamines in a form suitable for glycochip printing. Mendeleev Commun. 2008;18:238–240. [Google Scholar]
- 12.Reuman PD, Keely S, Schiff GM. Assessment of signs of influenza illness in the ferret model. J. Virol. Methods. 1989;24(1–2):27–34. doi: 10.1016/0166-0934(89)90004-9. [DOI] [PubMed] [Google Scholar]
- 13.Sakabe S, et al. Mutations in PA, NP, and HA of a pandemic (H1N1) 2009 influenza virus contribute to its adaptation to mice. Virus Res. 2011;158(1–2):124–129. doi: 10.1016/j.virusres.2011.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seyer R, et al. Synergistic Adaptive Mutations in the Hemagglutinin and Polymerase Acidic Protein Lead to Increased Virulence of Pandemic 2009 H1N1 Influenza A Virus in Mice. J. Infect. Dis. 2012;205(2):262–271. doi: 10.1093/infdis/jir716. [DOI] [PubMed] [Google Scholar]
- 15.de Vries RP, et al. Only two residues are responsible for the dramatic difference in receptor binding between swine and new pandemic H1 hemagglutinin. J. Biol. Chem. 2011;286(7):5868–5875. doi: 10.1074/jbc.M110.193557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.WHO. [Accessed March 18, 2012];WHO manual on animal diagnosis and surveillance. Available at: http://whqlibdoc.who.int/publications/2011/9789241548090_eng.pdf.
- 17.Xu L, et al. A single-amino-acid substitution in the HA protein changes the replication and pathogenicity of the 2009 pandemic A (H1N1) influenza viruses in vitro and in vivo. Virol. J. 2010;7:325. doi: 10.1186/1743-422X-7-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xu R, et al. Structural Characterization of the Hemagglutinin Receptor Specificity from the 2009 H1N1 Influenza Pandemic. J. Virol. 2012;86(2):982–990. doi: 10.1128/JVI.06322-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ye J, et al. Variations in the hemagglutinin of the 2009 H1N1 pandemic virus: potential for strains with altered virulence phenotype? PLoS Pathog. 2010;6(10):e1001145. doi: 10.1371/journal.ppat.1001145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zheng B, et al. D225G mutation in hemagglutinin of pandemic influenza H1N1 (2009) virus enhances virulence in mice. Exp. Biol. Med. (Maywood) 2010;235(8):981–988. doi: 10.1258/ebm.2010.010071. [DOI] [PubMed] [Google Scholar]