Abstract
Non-alcoholic fatty liver disease (NAFLD), one of the most common liver diseases, is caused by the disruption of hepatic lipid homeostasis. It is associated with insulin resistance as seen in type 2 diabetes mellitus. Glucagon-like peptide-1 (GLP-1) is an incretin that increases insulin sensitivity and aids glucose metabolism. In recent in vivo and in vitro studies, GLP-1 presents a novel therapeutic approach against NAFLD by increasing fatty acid oxidation, decreasing lipogenesis, and improving hepatic glucose metabolism. In this report, we provide an overview of the role and mechanism of GLP-1 in relieving NAFLD.
Keywords: Fatty acid oxidation, Glucagon-like peptide 1, Non-alcoholic fatty liver disease
INTRODUCTION
Excess accumulation of fat in the liver is known as fatty liver disease. Non-alcoholic fatty liver disease (NAFLD) is one of the most common liver diseases in the Western hemisphere, affecting 20% to 30% of the adult population [1]. Approximately 10% to 25% patients with NAFLD can progress to non-alcoholic steatohepatitis (NASH) and 10% to 15% patients with NASH develop hepatocellular carcinoma [2,3]. In addition, NAFLD is closely associated with metabolic syndrome, type 2 diabetes mellitus (T2DM) and cardiovascular morbidity and mortality. Despite these associated pathologies, there is still no specific treatment for NAFLD.
Glucagon-like peptide-1 (GLP-1) is an incretin secreted by L-cells in the small intestine in response to food intake [4]. The main roles of GLP-1 are stimulation of glucose-dependent insulin secretion, inhibition of postprandial glucagon release, delay of gastric emptying, and induction of pancreatic β-cell proliferation [5].
Once in circulation, GLP-1 has a short half-life (1 to 2 minutes) due to rapid degradation by the ubiquitous endogenous enzyme dipeptidyl peptidase-4 (DPP-4). To overcome this obstacle, GLP-1 receptor agonists that have increased resistance to DPP-4 (such as exenatide and liraglutide) or DPP-4 inhibitors (such as sitagliptin, vildagliptin, saxagliptin, alogliptin, and linagliptin) have been used in animal and human studies [6,7].
Recent studies have shown that exendin-4 could improve hepatic steatosis by modulation of lipid metabolism and hepatic insulin signaling in ob/ob mice and in human hepatocyte [8,9]. Additional studies have demonstrated that treatment with exendin-4 and liraglutide could reduce steatosis by enhancing autophagy. Treatment with exendin-4 and liraglutide leads to reduced endoplasmic reticulum (ER) stress-related apoptosis in human hepatocytes treated with fatty acids as well as in mice fed a high fat diet, respectively [10]. In this review, we present the pleiotropic effects of GLP-1 on reducing NAFLD.
LIPID METABOLISM IN NORMAL AND NAFLD PATIENTS
The liver, as a key organ for lipid homeostasis, has roles in various aspect of energy metabolism. Hepatic lipid homeostasis is usually maintained through balance between the influx or production of fatty acids and their use for oxidation or secretion as very low density lipoprotein (VLDL) triglycerides [11-13]. Disruption of hepatic lipid homeostasis causes liver dysfunction, eventually leading to liver disease.
Hepatic steatosis is associated with the alteration of nuclear receptors, membrane transport proteins and cellular enzymes [14,15]. Sterol regulatory element binding protein1c (SREBP-1c) transcription factor and peroxisome proliferator-activated receptor α (PPARα) are essential regulators for steatosis in obese patients. Enhancement in the SREBP-1c/PPARα ratio, an indication that lipogenesis is higher than fatty acid oxidation, was found in obese patients with hepatic steatosis [16]. Additional studies demonstrated that SREBP-1c -/- mice had impaired induction of hepatic genes coding for fatty acid biosynthesis (e.g., acetyl-CoA carboxylase, fatty acid synthase, and stearoyl-CoA desaturase) compared to wild type mice [17]. These results suggest that NAFLD is caused by both increased lipid storage (from circulating fatty acid uptake and de novo lipogenesis) and decreased lipid removal (via fatty acid oxidation or VLDL-triglycerides secretion).
GLP-1 SIGNALING IN NORMAL AND NAFLD PATIENTS
Pleiotropic effects of GLP-1 on glucose metabolism, appetite, weight, blood pressure, cardiovascular risk factors, cardiovascular function, and the central nervous system have been reported [18]. GLP-1 achieves its roles by binding to its specific receptor (GLP-1R) on human hepatocytes [9]. In addition, we recently reported that exendin-4 increases expression of GLP-1R in a dose-dependent manner in human hepatoma cell lines [19].
Several human and animal studies have demonstrated the therapeutic effects of GLP-1 receptor agonist in slowing the progression of NAFLD. Exenatide therapy decreased hepatic fat accumulation, insulin resistance, and the risk of cardiovascular disease in patient with T2DM [20] and also improved fatty acid β-oxidation and insulin sensitivity in the livers of rats on a high fat diet [21]. Hepatic gluconeogenesis and insulin sensitivity were improved in ob/ob mice treated with recombinant adenovirus expressing GLP-1 (rAd-GLP-1) [22].
Protective effects of GLP-1 against hepatic steatosis were found in only diet-induced obese mice [23]. Sitagliptin, a DPP-4 inhibitor, showed a decrease in liver triglyceride content, expression of lipogenesis genes and gluconeogenesis in wild type mice [24]. Ultimately, exendin-4 may play role as a novel treatment of NAFLD via direct effect on hepatic lipid and glucose metabolism.
GLP-1 EFFECT ON FATTY ACID OXIDATION IN LIVER
In mammalian liver, fatty acids oxidation serves as a source for energy generation and occurs in both the mitochondria and the peroxisomes. Short and medium-chain fatty acids (SCFAs: <6 carbons long and MCFAs: 6 to 12 carbons long) are oxidized in the mitochondria, long-chain fatty acids (LCFAs: C12 to C20) are oxidized in both the mitochondria and peroxisomes, and very long-chain fatty acids (VLCFAs: >C20) are preferentially oxidized in the peroxisomes [25]. However, excess fatty acids can impair fatty acid oxidation by inhibiting the activities of enzymes involved in fatty acid oxidation [26]. PPARα is a transcriptional factor regulating the expression of a number of genes involved in mitochondrial and peroxisomal fatty acid β-oxidation [27,28].
Exendin-4 significantly increases the expression of PPARα and acyl-Coenzyme A oxidase (ACOX) mRNA in ob/ob mice [8]. Hepatocytes isolated from rats with NASH demonstrated reduced expression of hepatic PPARα and its downstream target genes: ACOX and carnitine palmitoyltransferase 1A (CPT1A). ACOX is a rate-limiting enzyme involved in peroxisomal fatty acid β-oxidation and CPT1A is a key enzyme allowing the initial transport of fatty acids into mitochondria for β-oxidation. Expression of PPARα, and subsequently ACOX and CPT1A, was improved by exendin-4 treatment [21].
GLP-1 EFFECT ON AMPK, NAMPT, AND SIRT SIGNALING
AMP-activated protein kinase (AMPK) and silent mating type information regulation 2 homolog (sirtuin, SIRT) 1 are metabolic sensors regulating energy homeostasis and various intracellular systems. These include fatty acid oxidation, lipogenesis, glucose uptake, gluconeogenesis, mitochondria biosynthesis, and insulin sensitivity [29,30]. They are also involved in mediating the effect of adiponectin in inhibiting the accumulation of liver fat [31]. AMPK and SIRT1 are activated by an AMP and NAD+ dependent mechanism and acts through regulation of phosphorylation and deacetylation of their targets, respectively. PGC-1α is a common target of the two metabolic sensors, and has been shown to have protective effects in patients with metabolic diseases [29].
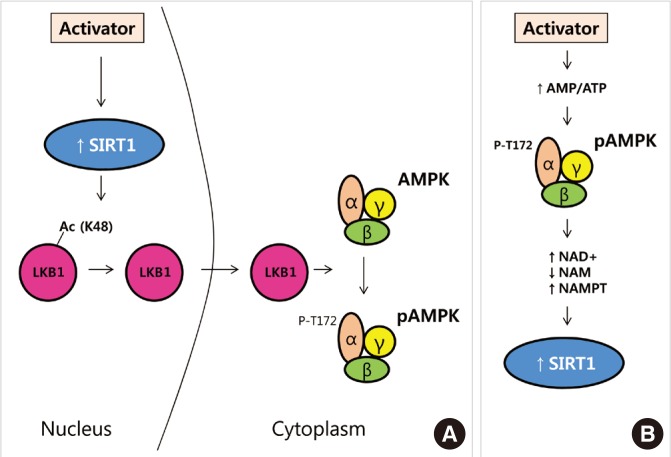
Nampt/visfatin is a mammalian NAD+ biosynthetic enzyme that controls SIRT1 activity by mediating the conversion of nicotinamide (NAM) to NAD+ [30]. Activated SIRT1 enhances AMPK activity via an LKB1-dependent manner in human hepatocytes (Fig. 1A) [32]. However, the precise mechanism of interaction between AMPK and SIRT1 is still controversial and varies with tissue and condition. Cantó et al. [33] reported that AMPK regulates SIRT1 activity by increasing cellular NAD+ levels in mouse skeletal muscle (Fig. 1B).
Fig. 1.
Proposed regulatory mechanisms between silent mating type information regulation 2 homolog (SIRT1) and AMP-activated protein kinase (AMPK). (A) Activation of SIRT by activator leads to deacetylation of Lys48 residues on LKB1. LKB1 moves to the cytoplasm and then, phosphorylates and activates the AMPK. (B) The enhancement of AMP/ATP ratio stimulates AMPK activity. Activated AMPK regulates SIRT1, an NAD+-dependent protein deacetylase, by increasing NAD+ levels. NAM, nicotinamide; NAMPT, nicotinamide phosphoribosyltransferase (Adapted from Cantó et al., Curr Opin Lipidol 2009;20:98-105 [29]).
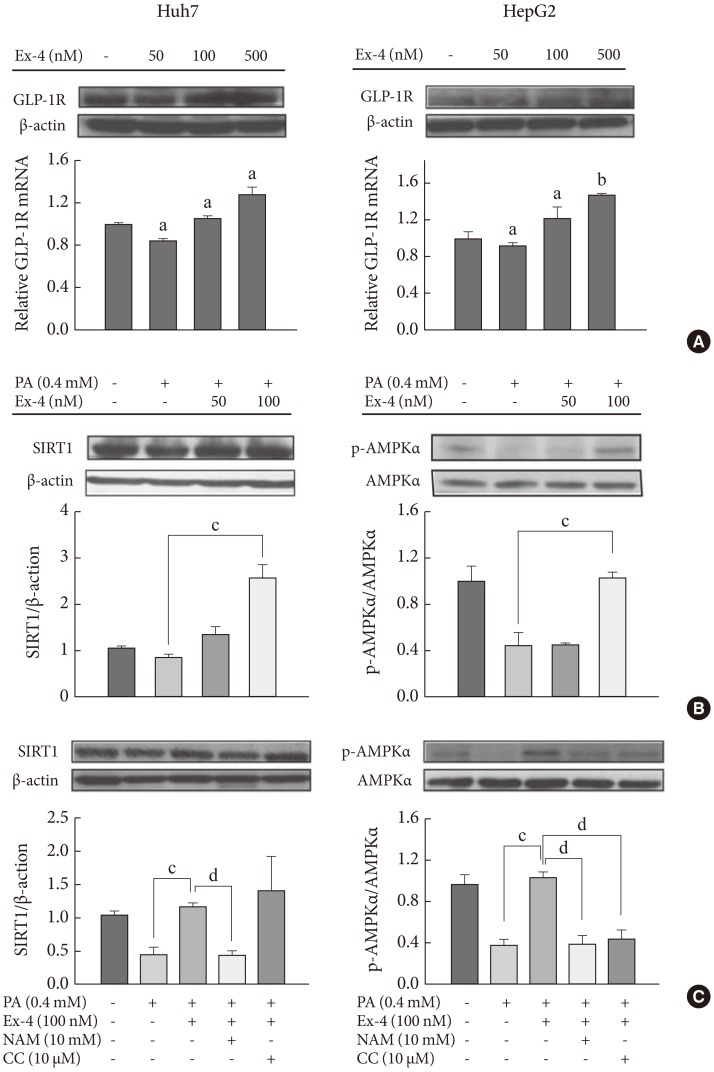
Recent studies reported that GLP-1 increases the phosphorylation of AMPK in hepatocytes and reverses hepatic steatosis by stimulating fatty acid oxidation [8,31,32]. Moreover, we recently demonstrated that activating GLP-1 receptor by exendin-4 treatment enhances the expression of NAMPT, SIRT1, and AMPK in mouse liver. SIRT1 inhibitor (NAM) leads to a decrease in phosphorylation of AMPK in human hepatocytes, indicating that SIRT1 stimulates AMPK (Fig. 2) [19]. Thus, GLP-1 could improve hepatic lipid metabolism by regulation of NAMPT/SIRT1/AMPK signaling.
Fig. 2.
Regulation of glucagon-like peptide-1 receptor (GLP-1R), SIRT1 and AMPK by exendin-4 (Ex-4) in HepG2 and Huh7 cells. (A) Cells were treated with 50, 100, or 500 nM Ex-4 for 24 hours. GLP-1R and β-actin were measured by western blot and real-time PCR. GLP-1R was normalized to β-actin. (B) Cells given 0.4 mM palmitic acid (PA) were treated with either vehicle or 50 to 100 nM Ex-4 for 24 hours. (C) Cells given 0.4 mM palmitic acid were treated with 100 nM Ex-4 in the absence or presence of 10 mM nicotinamide (NAM) or 10 µM compound C (CC) for 24 hours. (B, C) SIRT1, phosphorylated AMPKα at threonine 172, AMPK, and β-actin were measured by Western blot in HepG2 cells. SIRT1 and phosphorylated AMPKα were normalized to the β-actin and total AMPKα of each sample, respectively. aP<0.05, bP<0.01 compared with control, cP<0.05, compared with PA, and dP<0.05 compared with Ex-4 (Adapted from Lee J, et al. PLoS One 2012;7:e31394 [19]).
GLP-1 EFFECT ON LIVER FUNCTION AND GLUCOSE METABOLISM IN HUMAN
The liver has a vast range functions in the body, including immunity against infection, synthesis of proteins and cholesterol, detoxification, glycogen storage, excretion of bile for fat digestion, and regulation of metabolism. However, insults such as alcohol, autoimmune malfunction, hereditary diseases, and metabolic diseases could result in liver dysfunction.
In a study investigating human hepatocytes treated with fatty acids, exenatide was shown to reduce fatty acid storage and improve hepatocyte viability and markers of autophagy [10]. A clinical trial evaluating the effects of exenatide in patients with T2DM over a period of 3 years revealed that treatment lead to significant improvements in hepatic markers, such as elevated liver enzymes, and other cardiovascular risk factors were significantly improved [34]. A case study exploring the efficacy of exenatide therapy in a 59-year-old NAFLD patient, reported a 73% reduction in hepatic fat content and significant improvements in liver enzymes 44 weeks post-treatment [20].
GLP-1 has recently been shown to increase hepatic insulin signaling and sensitivity [9]. A modified glucose clamp study demonstrated that exenatide reduces postprandial glucose by increasing the hepatic uptake of exogenous glucose [35]. Furthermore, GLP-1 in obese mice reduces hepatic gluconeogenesis by inhibiting phosphoenolpyruvate carboxykinase (PEPCK) and glucose-6-phosphatase (G6Pase) [22]. Park et al. [36] reported that exendin-4 treatment decreases hepatic glucose output at hyperinsulinemic states and promotes hepatic insulin signaling by potentiating tyrosine phosphorylation of the insulin receptor substrate-2 in 90% pancreatectomized diabetic rats fed high fat (40% energy from fat) diets.
CONCLUSION
Disruption of lipid metabolic homeostasis has been recognized as a major cause of NAFLD, which is associated with insulin resistance, T2DM, obesity, and cardiovascular disease. Although the incretin GLP-1 has been widely studied for its effects on stimulation of glucose-dependent insulin secretion in pancreatic β-cell, GLP-1 receptor agonists have other important effects in peripheral tissues. Treatment with GLP-1 mimetics improves hepatic insulin signaling in NAFLD animal models, and these effects could be invoked by direct stimulation of hepatic GLP-1 receptor. GLP-1 is expected to have pleiotropic effects on the liver, and more research is needed to explore its mechanism.
ACKNOWLEDGMENTS
This work was supported by the Young Investigator Award 2011 from the Korean Diabetes Association and the Korea Science and Engineering Foundation by the Ministry of Education, Science and Technology (S-2010-1115-000) to Won-Young Lee.
Footnotes
No potential conflicts of interest relevant to this article were reported.
References
- 1.Ruhl CE, Everhart JE. Epidemiology of nonalcoholic fatty liver. Clin Liver Dis. 2004;8:501–519. doi: 10.1016/j.cld.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 2.Vanni E, Bugianesi E, Kotronen A, De Minicis S, Yki-Jarvinen H, Svegliati-Baroni G. From the metabolic syndrome to NAFLD or vice versa? Dig Liver Dis. 2010;42:320–330. doi: 10.1016/j.dld.2010.01.016. [DOI] [PubMed] [Google Scholar]
- 3.Kim CH, Younossi ZM. Nonalcoholic fatty liver disease: a manifestation of the metabolic syndrome. Cleve Clin J Med. 2008;75:721–728. doi: 10.3949/ccjm.75.10.721. [DOI] [PubMed] [Google Scholar]
- 4.Kim W, Egan JM. The role of incretins in glucose homeostasis and diabetes treatment. Pharmacol Rev. 2008;60:470–512. doi: 10.1124/pr.108.000604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.MacDonald PE, El-Kholy W, Riedel MJ, Salapatek AM, Light PE, Wheeler MB. The multiple actions of GLP-1 on the process of glucose-stimulated insulin secretion. Diabetes. 2002;51(Suppl 3):S434–S442. doi: 10.2337/diabetes.51.2007.s434. [DOI] [PubMed] [Google Scholar]
- 6.Ahren B, Schmitz O. GLP-1 receptor agonists and DPP-4 inhibitors in the treatment of type 2 diabetes. Horm Metab Res. 2004;36:867–876. doi: 10.1055/s-2004-826178. [DOI] [PubMed] [Google Scholar]
- 7.Bourdel-Marchasson I, Schweizer A, Dejager S. Incretin therapies in the management of elderly patients with type 2 diabetes mellitus. Hosp Pract (Minneap) 2011;39:7–21. doi: 10.3810/hp.2011.02.369. [DOI] [PubMed] [Google Scholar]
- 8.Ding X, Saxena NK, Lin S, Gupta NA, Anania FA. Exendin-4, a glucagon-like protein-1 (GLP-1) receptor agonist, reverses hepatic steatosis in ob/ob mice. Hepatology. 2006;43:173–181. doi: 10.1002/hep.21006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta NA, Mells J, Dunham RM, Grakoui A, Handy J, Saxena NK, Anania FA. Glucagon-like peptide-1 receptor is present on human hepatocytes and has a direct role in decreasing hepatic steatosis in vitro by modulating elements of the insulin signaling pathway. Hepatology. 2010;51:1584–1592. doi: 10.1002/hep.23569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharma S, Mells JE, Fu PP, Saxena NK, Anania FA. GLP-1 analogs reduce hepatocyte steatosis and improve survival by enhancing the unfolded protein response and promoting macroautophagy. PLoS One. 2011;6:e25269. doi: 10.1371/journal.pone.0025269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adiels M, Taskinen MR, Boren J. Fatty liver, insulin resistance, and dyslipidemia. Curr Diab Rep. 2008;8:60–64. doi: 10.1007/s11892-008-0011-4. [DOI] [PubMed] [Google Scholar]
- 12.Donnelly KL, Smith CI, Schwarzenberg SJ, Jessurun J, Boldt MD, Parks EJ. Sources of fatty acids stored in liver and secreted via lipoproteins in patients with nonalcoholic fatty liver disease. J Clin Invest. 2005;115:1343–1351. doi: 10.1172/JCI23621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu Q, Bengmark S, Qu S. The role of hepatic fat accumulation in pathogenesis of non-alcoholic fatty liver disease (NAFLD) Lipids Health Dis. 2010;9:42. doi: 10.1186/1476-511X-9-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reddy JK, Rao MS. Lipid metabolism and liver inflammation II Fatty liver disease and fatty acid oxidation. Am J Physiol Gastrointest Liver Physiol. 2006;290:G852–G858. doi: 10.1152/ajpgi.00521.2005. [DOI] [PubMed] [Google Scholar]
- 15.Musso G, Gambino R, Cassader M. Recent insights into hepatic lipid metabolism in non-alcoholic fatty liver disease (NAFLD) Prog Lipid Res. 2009;48:1–26. doi: 10.1016/j.plipres.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 16.Pettinelli P, Del Pozo T, Araya J, Rodrigo R, Araya AV, Smok G, Csendes A, Gutierrez L, Rojas J, Korn O, Maluenda F, Diaz JC, Rencoret G, Braghetto I, Castillo J, Poniachik J, Videla LA. Enhancement in liver SREBP-1c/PPAR-alpha ratio and steatosis in obese patients: correlations with insulin resistance and n-3 long-chain polyunsaturated fatty acid depletion. Biochim Biophys Acta. 2009;1792:1080–1086. doi: 10.1016/j.bbadis.2009.08.015. [DOI] [PubMed] [Google Scholar]
- 17.Shimomura I, Bashmakov Y, Horton JD. Increased levels of nuclear SREBP-1c associated with fatty livers in two mouse models of diabetes mellitus. J Biol Chem. 1999;274:30028–30032. doi: 10.1074/jbc.274.42.30028. [DOI] [PubMed] [Google Scholar]
- 18.Pratley RE. The new science of GLP-1: effects beyond glucose control. Johns Hopkins Adv Stud Med. 2008;8:393–399. [Google Scholar]
- 19.Lee J, Hong SW, Chae SW, Kim DH, Choi JH, Bae JC, Park SE, Rhee EJ, Park CY, Oh KW, Park SW, Kim SW, Lee WY. Exendin-4 improves steatohepatitis by increasing Sirt1 expression in high-fat diet-induced obese C57BL/6J mice. PLoS One. 2012;7:e31394. doi: 10.1371/journal.pone.0031394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tushuizen ME, Bunck MC, Pouwels PJ, van Waesberghe JH, Diamant M, Heine RJ. Incretin mimetics as a novel therapeutic option for hepatic steatosis. Liver Int. 2006;26:1015–1017. doi: 10.1111/j.1478-3231.2006.01315.x. [DOI] [PubMed] [Google Scholar]
- 21.Svegliati-Baroni G, Saccomanno S, Rychlicki C, Agostinelli L, De Minicis S, Candelaresi C, Faraci G, Pacetti D, Vivarelli M, Nicolini D, Garelli P, Casini A, Manco M, Mingrone G, Risaliti A, Frega GN, Benedetti A, Gastaldelli A. Glucagon-like peptide-1 receptor activation stimulates hepatic lipid oxidation and restores hepatic signalling alteration induced by a high-fat diet in nonalcoholic steatohepatitis. Liver Int. 2011;31:1285–1297. doi: 10.1111/j.1478-3231.2011.02462.x. [DOI] [PubMed] [Google Scholar]
- 22.Lee YS, Shin S, Shigihara T, Hahm E, Liu MJ, Han J, Yoon JW, Jun HS. Glucagon-like peptide-1 gene therapy in obese diabetic mice results in long-term cure of diabetes by improving insulin sensitivity and reducing hepatic gluconeogenesis. Diabetes. 2007;56:1671–1679. doi: 10.2337/db06-1182. [DOI] [PubMed] [Google Scholar]
- 23.Tomas E, Wood JA, Stanojevic V, Habener JF. GLP-1-derived nonapeptide GLP-1(28-36)amide inhibits weight gain and attenuates diabetes and hepatic steatosis in diet-induced obese mice. Regul Pept. 2011;169:43–48. doi: 10.1016/j.regpep.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 24.Shirakawa J, Fujii H, Ohnuma K, Sato K, Ito Y, Kaji M, Sakamoto E, Koganei M, Sasaki H, Nagashima Y, Amo K, Aoki K, Morimoto C, Takeda E, Terauchi Y. Diet-induced adipose tissue inflammation and liver steatosis are prevented by DPP-4 inhibition in diabetic mice. Diabetes. 2011;60:1246–1257. doi: 10.2337/db10-1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bechmann LP, Hannivoort RA, Gerken G, Hotamisligil GS, Trauner M, Canbay A. The interaction of hepatic lipid and glucose metabolism in liver diseases. J Hepatol. 2012;56:952–964. doi: 10.1016/j.jhep.2011.08.025. [DOI] [PubMed] [Google Scholar]
- 26.Hettema EH, Tabak HF. Transport of fatty acids and metabolites across the peroxisomal membrane. Biochim Biophys Acta. 2000;1486:18–27. doi: 10.1016/s1388-1981(00)00045-7. [DOI] [PubMed] [Google Scholar]
- 27.Minnich A, Tian N, Byan L, Bilder G. A potent PPARalpha agonist stimulates mitochondrial fatty acid beta-oxidation in liver and skeletal muscle. Am J Physiol Endocrinol Metab. 2001;280:E270–E279. doi: 10.1152/ajpendo.2001.280.2.E270. [DOI] [PubMed] [Google Scholar]
- 28.Hashimoto T, Fujita T, Usuda N, Cook W, Qi C, Peters JM, Gonzalez FJ, Yeldandi AV, Rao MS, Reddy JK. Peroxisomal and mitochondrial fatty acid beta-oxidation in mice nullizygous for both peroxisome proliferator-activated receptor alpha and peroxisomal fatty acyl-CoA oxidase. Genotype correlation with fatty liver phenotype. J Biol Chem. 1999;274:19228–19236. doi: 10.1074/jbc.274.27.19228. [DOI] [PubMed] [Google Scholar]
- 29.Canto C, Auwerx J. PGC-1alpha, SIRT1 and AMPK, an energy sensing network that controls energy expenditure. Curr Opin Lipidol. 2009;20:98–105. doi: 10.1097/MOL.0b013e328328d0a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ruderman NB, Xu XJ, Nelson L, Cacicedo JM, Saha AK, Lan F, Ido Y. AMPK and SIRT1: a long-standing partnership? Am J Physiol Endocrinol Metab. 2010;298:E751–E760. doi: 10.1152/ajpendo.00745.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shen Z, Liang X, Rogers CQ, Rideout D, You M. Involvement of adiponectin-SIRT1-AMPK signaling in the protective action of rosiglitazone against alcoholic fatty liver in mice. Am J Physiol Gastrointest Liver Physiol. 2010;298:G364–G374. doi: 10.1152/ajpgi.00456.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hou X, Xu S, Maitland-Toolan KA, Sato K, Jiang B, Ido Y, Lan F, Walsh K, Wierzbicki M, Verbeuren TJ, Cohen RA, Zang M. SIRT1 regulates hepatocyte lipid metabolism through activating AMP-activated protein kinase. J Biol Chem. 2008;283:20015–20026. doi: 10.1074/jbc.M802187200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Canto C, Gerhart-Hines Z, Feige JN, Lagouge M, Noriega L, Milne JC, Elliott PJ, Puigserver P, Auwerx J. AMPK regulates energy expenditure by modulating NAD+ metabolism and SIRT1 activity. Nature. 2009;458:1056–1060. doi: 10.1038/nature07813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Klonoff DC, Buse JB, Nielsen LL, Guan X, Bowlus CL, Holcombe JH, Wintle ME, Maggs DG. Exenatide effects on diabetes, obesity, cardiovascular risk factors and hepatic biomarkers in patients with type 2 diabetes treated for at least 3 years. Curr Med Res Opin. 2008;24:275–286. doi: 10.1185/030079908x253870. [DOI] [PubMed] [Google Scholar]
- 35.Zheng D, Ionut V, Mooradian V, Stefanovski D, Bergman RN. Exenatide sensitizes insulin-mediated whole-body glucose disposal and promotes uptake of exogenous glucose by the liver. Diabetes. 2009;58:352–359. doi: 10.2337/db08-0875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Park S, Hong SM, Ahn IS. Exendin-4 and exercise improve hepatic glucose homeostasis by promoting insulin signaling in diabetic rats. Metabolism. 2010;59:123–133. doi: 10.1016/j.metabol.2009.06.026. [DOI] [PubMed] [Google Scholar]