Abstract
OBJECTIVE:
To evaluate the effect of 2 anticipatory guidance styles (maternal focused [MOMS] and infant focused [Ounce of Prevention]) directed at mothers of infants aged newborn to 6 months on their infant feeding behaviors at 1 year compared with routine advice as outlined in Bright Futures (BF).
METHODS:
This is a cluster randomized trial. A total of 292 mother/infant dyads were enrolled at their first well-child visit to 3 urban pediatric clinics in Columbus, Ohio. Intervention-specific brief advice and 1-page handouts were given at each well visit. In addition to infant weights and lengths, surveys about eating habits and infant feeding practices were completed at baseline and 12 months.
RESULTS:
Baseline data revealed a group with high rates of maternal overweight (62%) and obesogenic habits. At 12 months, the maternal-focused group gave their infants less juice (8.97 oz vs 14.37 oz, P < .05), and more daily servings of fruit (1.40 vs 0.94, P < .05) and vegetables (1.41 vs 1.03, P < .05) compared with BF mothers. Ounce of Prevention mothers also gave less juice (9.3 oz, P < .05) and more fruit servings (1.26 P < .05) than BF.
CONCLUSIONS:
Brief specific interventions added to well-child care may affect obesogenic infant feeding behaviors of mothers and deserves further study as an inexpensive approach to preventing childhood obesity.
KEY WORDS: well-child visit, obesity prevention, anticipatory guidance, infant feeding
WHAT’S KNOWN ON THIS SUBJECT:
Childhood obesity occurs in 20% of children before they enter kindergarten. Treatment is difficult, making prevention desirable, but little is known about effective methods using anticipatory guidance to prevent obesity in pediatric primary care.
WHAT THIS STUDY ADDS:
This study provides a comparison of 2 approaches versus usual care using anticipatory guidance to improve infant feeding during the first year of life, and demonstrates positive specific feeding behavior differences at 1 year in the intervention groups.
Childhood obesity is a growing concern in the United States and the world.1–7 The difficulty of losing weight and keeping it off has led to an intense interest in the prevention of obesity. Among school-aged children, prevention programs have varying degrees of success.8–10 Unfortunately, more than 20% of children are overweight before they begin kindergarten.11 Recent reviews of the literature reveal a dearth of prevention interventions in children younger than 5 years.12,13
Risk factors for childhood obesity suggest strategies for obesity prevention. These include parental overweight,14,15 obesogenic parental eating,16 high rates of television watching,17–19 low family income20,21 and education,22,23 low intake of vegetables and fruit, and high intake of fast food and sweet drinks.14,18,24 Anderson and Whitaker25 recently found associations among 3 family habits (eating the evening meal together, adequate child sleep, and restriction of screen time) with lower rates of preschool obesity. Some of these factors are more readily modifiable than others.
One avenue for obesity prevention is through anticipatory guidance (AG) delivered at well-child visits. AG provides an opportunity for the clinician to share information with parents regarding child health, nutrition, safety, and optimized development. Some elements of AG can enhance the family environment of children, including improving child literacy readiness,26 decreasing parental smoking,27 and screening mothers for postpartum depression.28
Addressing maternal health behaviors at the pediatric health care visit may be particularly helpful.29,30 This strategy is logical, as improving the mother’s health may improve the child’s health. Parents may be willing to change to improve their children’s habits. For instance, African American parents who are consciously acting as role models for their children were found to eat less fat and fewer calories themselves.31
A review of the literature revealed no published assessment of the effect of AG on obesity prevention in young children or using AG as an avenue to address maternal diet and behaviors. The goal of this study was to examine the role of AG in changing mothers’ obesogenic feeding behaviors during the child’s first year of life.
Methods
Study Design and Description of Population
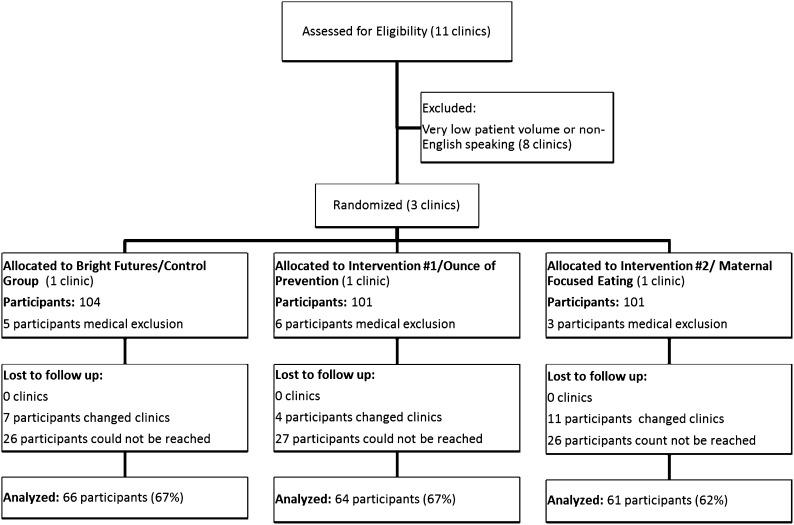
A cluster randomized trial design was used. Clinic sites were randomized to 1 of 3 study conditions as outlined below (see Fig 1).
FIGURE 1.
Consort diagram.
Pediatric primary care clinics in Nationwide Children’s Hospital Primary Care Network serve families in low-income metropolitan areas in Columbus, Ohio. In these geographic areas, 75% of adults are overweight or obese. The population served by this network is 50% African American, 40% non-Hispanic white, and 10% Hispanic, and 85% receive Medicaid. Of the 11 clinics in this network, the 3 clinics with the largest number of newborn and 2-month-old well-child visits for the previous year were selected for the project. These 3 clinics were then monitored for 1 week for the number of well-child visits for full-term infants younger than 3 months as well as the number of these families requiring translators. After determining that these clinics had a sufficient number of newborns and mothers who were eligible to participate, each clinic was randomly assigned to implement 1 of 3 intervention conditions.
The following paragraphs describe the intervention conditions (Table 1 shows a comparison of visits among conditions):
TABLE 1.
Intervention Timing and Content
| Well Visit | BF | MOMS | OP |
|---|---|---|---|
| 2 wk and/or 2 mo | No solids in bottle for bottle feeding; Appropriate formula mixing; No microwave for warming; No honey | Eat 3 meals/day; Eat 5–7 servings of fruits/vegetables; No meal skipping | Feed breast milk or formula only; No juice or cereal in bottle; Not all crying means hungry; Increase nighttime feeding interval at 2 mo |
| 4 mo | Same as 2 mo; Introduction to cereal with spoon | Reiterate above, plus Avoid liquid calories; Create a structure for eating; Eat in one place, turn off television, eat together, let infant watch you, eat good foods; Discuss solids | Breast milk or formula only; If formula limit to 4–6 oz, 4–5/day; No cereal in bottle; No juice or soft drinks; If ready: start single-grain cereal 1–2 T by spoon not bottle |
| 6 mo | Introduction of new foods; No bottle in bed; Limit juice | Reiterate above, plus Mother drink 16–24 oz of milk if can; Drink water; Avoid fast food; Teach infant good nutrition | Continue breastmilk or formula w/Fe; Begin infant food with vegetables; Explain extrusion reflex; Add new food every 3–4 d; Offer new foods >10 times; Portion size 2 T twice daily; Cereal 2–4 T twice daily |
| 9 mo | Same as 6 mo; Introduce cup; Self-feeding soft foods | Reiterate messages | Breastmilk or formula to 12 mo; Start weaning to cup; Offer variety; New foods up to 10 times for acceptance; Limit 100% juice to 2–4 oz; No sweet drinks; Serving sizes fruits/vegetables 1–2 T (1/8 cup) twice daily; Protein/lean meat 6–8 T/d; Food is not a reward |
| 12 mo | Switch to whole milk; Self-feeding; Wean from bottle; 3 meals/2 snacks | Reiterate messages, plus It is normal for infant’s appetite to drop; Change to whole milk 16–24 oz/d; Wean and reinforce no bottle in bed; Have consistent routines | Same as 9 mo with added serving sizes; Juice 2–4 oz; Milk/yogurt 1/2 cup; Cheese 1/2 oz; Fruits/vegetables 1/2 cup fresh or 1/3 cup canned; Cereal 1/4 cup; Bread 1/2 slice; Do not force child to eat; Avoid sweet drinks |
Maternal-focused intervention (MOMS): In this intervention, we approached child obesity prevention via anticipatory guidance aimed at maternal eating habits. We crafted simple messages to increase behaviors thought to be protective against the development of obesity. The underlying concept for our unique intervention is that mothers are role models for their children.
Mothers in this group received direct guidance regarding their own eating patterns. Message development focused on how mothers ate and the influence of mothers’ behaviors on their children. Specifically, participants were reminded that children imitate their mothers, and were asked to incorporate the following 7 elements into their eating behaviors: (1) eat 3 planned meals and 2 snacks every day and avoid skipping meals, (2) eat in 1 place in the home, (3) turn off the television while eating, (4) eat together with the family whenever possible, (5) drink 2 glasses of milk daily, (6) eat 5 servings of fruits and vegetables, and (7) limit soda and fast food (see Fig 2 for 6-month MOMS AG handout). This AG was provided by advising on a few items at the first visit. At subsequent visits, the items were reviewed and new items were added.
FIGURE 2.
Sample MOMS handout.
Ounce of Prevention (OP): Mothers in this group received a detailed program of infant feeding AG focusing on serving size and tips for introducing different foods for the infant. Mothers were encouraged to allow the infant to determine when he or she is full, not to force the child to eat, and not to use food as a reward. This program had been pilot tested in a large private pediatric practice in Cincinnati, Ohio, refined based on the experience there and is available at http://healthyohioprogram.org/healthylife/nutri2/nutrikids2/ounce.aspx. (See Fig 3 for 6-month OP AG handout.) This program provides far more details in terms of portion size suggestions and order of food introduction than the usual-care control condition (see following paragraph).
Bright Futures (BF), second edition Pocket Guide: This was the usual-care condition, based on the preexisting BF nutrition pocket guide (2002) for children in the first year of life. Messages consisted of traditional feeding AG focused on recommending breastfeeding, the introduction of infant food and table food, and avoidance of honey and foods that may lead to choking.32 (See Fig 4 for 6-month BF AG handout.)
FIGURE 3.
Sample Ounce of Prevention handout.
FIGURE 4.
Sample Bright Futures handout.
Project Implementation: Intervention Design and Delivery
Site-specific and age-specific handouts were developed by the research team. These were tailored for ease of readability and reading level at grade 6. Clinic physicians, nurses, and medical assistants were trained by research staff in implementing the appropriate AG program for their respective clinic before the start of the project, with a refresher session at 6 months after the project began. The staff were all told that they were implementing an intervention to optimize nutrition and good eating habits in the first year of life and were unaware of group assignment. Research staff did not participate in delivery of any component of the intervention. Brief reminders for clinicians were embedded in AG checklists in the infant’s chart. The intervention was designed to be delivered at the 2-, 4-, 6-, 9-, and 12-month pediatric well-child visit corresponding handouts. All mothers received the same clinic-specific AG regardless of their enrollment in the study; in other words, mothers who were not eligible or refused study participation still received the same AG. Nurses and medical assistants weighed and measured the infant per usual clinic protocol, recorded the data in the medical record, and ensured that the AG handout was given to the mother.
Study Procedures: Enrollment, Consent, and Inclusion and Exclusion Criteria
The institutional review board at Nationwide Children’s Hospital approved the project protocol. All recruitment and data collection were done by research staff. Sample size was determined to be 63 per group by statistical analysis of differences between proportions with an α of 0.5, power = 0.80, and a moderate effect size (0.5). Potential participants were identified by screening clinic schedules for infants 2 months of age or younger and by screening of waiting families by research staff. Once a potential participant was identified, research staff obtained written, informed consent and described the study in depth. Inclusion criteria were English-speaking mother (research staff could not be sure of the fidelity of AG delivered via interpreters), healthy full-term infant, lives with biological mother, and infant aged 2 months or younger. Exclusion criteria were history of NICU stay, gestation <37 weeks, chronic disease, foster placement, or known genetic disorder.
Timing and Content of Data Collection
Mothers were interviewed by research staff at baseline and when their infants were 6 and 12 months old. Maternal information collected included self-reported height and weight, demographics, and family and personal health history of obesity-related diseases. Maternal nutritional intake was assessed by using questions from the Behavior Risk Factor Surveillance Fruit and Vegetable module,33 with additional questions to assess protein, carbohydrate, soda, fast food, and water intake. Eating habits with regard to breakfast consumption, family meals, meal skipping, dining location, television watching during meals, and meal planning were measured. Health numeracy, maternal depression, and food security were assessed as potential confounders of maternal feeding and eating habits. Child variables included weights and lengths that were obtained via chart review. Infant nutrition information collected included formula volumes, satiety cues, feeding preparation, juice intake, and additions made to the bottle. Child feeding behavior questions regarding food restriction or pressuring were added at 12 months. Further details on study design, methods, and evaluation tools have been published elsewhere.34 A summary of the survey instruments is outlined in Table 2.
TABLE 2.
Survey Instruments at Baseline and 12 Months
| Sample Items | Baseline Survey | 12-mo Survey | |
|---|---|---|---|
| Maternal BMI (self-report) | O | O | |
| Health & other demographics | O | O | |
| Nutritional intake (Behavioral Risk Factor Surveillance System): 5 items | Not counting carrots, potatoes, or salad, how many servings of vegetables do you usually eat? (For example, a serving of vegetables at both lunch and dinner would be TWO SERVINGS.) | O (Cronbach α = 0.39) | O (Cronbach α = 0.44) |
| Eating behavior patterns questionnaire (EBPQ): 14 items, 9 from EBPQ | How often do you eat breakfast? | O (Cronbach α = 0.68) | O (Cronbach α = 0.73) |
| Where do you usually eat your main meal of the day? | |||
| How often do you skip meals? | |||
| Center for Epidemiologic Study-Short Depression Scale: 10 items | I was bothered by things that don’t usually bother me? I was depressed. | O (Cronbach α = 0.69) | x |
| Positive & Negative Affect Schedule: 20 items | During the past week to what extent have you felt scared? | x | O (Cronbach α = 0.86 NA) |
| Attentive? 1–5 very slightly to very much | (Cronbach α = 0.88 PA) | ||
| US Department of Agriculture Food Security/hunger scale: 1 item | In the past 12 mo, did you or other adults in the household ever cut the size of your meals or skip meals because there wasn’t enough money for food? | O | O |
| Health numeracy: 2 items | A label on your prescription bottle reads – “Take 1 tablet by mouth every 6 hours as needed.” If you take the first tablet at 7:00 am, when should you take the next one? | O | x |
| Eating habits | How many meals do you eat in a day? | O 9 items | O 7 items |
| How often do you eat food together with your family? | |||
| Meal planning: 14 items | I am able to plan meals for my family. | O (Cronbach α = 0.70) | x |
| I take a grocery list to the store when I shop. | |||
| I never know what I am going to eat for my next meal. | |||
| 5-point Likert scale | |||
| Child height and weight | O | O | |
| Child feeding questionnaire: 8 items, 4 of Pressure to Eat | When your child is at home, how often are you responsible for feeding him/her? | x | O (Cronbach α = 0.70) |
| I have to be careful not to feed my child too much. | |||
| 4-point Likert scale | |||
| Infant nutrition | How often does your child eat grains (Cheerios, oatmeal, bread, pancakes)? | O 17 items–all 6 items-only for exclusive breastfeeding | O 36 items |
| How often does your child eat vegetables (green beans, sweet potatoes)? |
O, survey instrument included; x, survey instrument not included.
Recruitment and Retention of the Study Population
Our overall approach to recruitment and retention of subjects was to use multiple strategies simultaneously. These included piloting recruitment procedures, getting “buy-in” from clinic staff, using participant incentives, establishing a dedicated research phone line for families to schedule appointment, maintaining contact with participants, establishing a project identity through logos and mailings to participants, emphasizing convenience for participants, and establishing personal contact between families and the research staff. A full discussion of these methods has been published.35 There were no measured differences between those subjects who were retained and those who were lost to follow-up.
Statistical Analysis
The unit of analysis was the individual. Analyses were conducted to describe differences in maternal behaviors and child feeding behaviors across the 3 study conditions: BF, MOMS, and OP. Because intraclass correlation (shared variance) among the women who were within the same clinic is not likely to be meaningfully significant, individual-level analyses were deemed to be the appropriate unit of analysis. All analyses used the BF (usual care) group as the reference group. All regression analyses were adjusted for maternal demographics (race, education, age, BMI, marital status) and maternal behaviors (ever breastfed, often snacking while watching television). The only factors not adjusted for were Supplemental Nutrition Program for Women, Infants, and Children, food stamps, and private insurance. Given that this was almost entirely a low-income sample of women, this adjustment would not have influenced the study results. To evaluate differences in continuous variables, general linear regressions were conducted to evaluate the least-square means by 3 study conditions at the child’s 12-month visit. To evaluate dichotomous outcomes, logistic regression analyses were conducted to evaluate differences in the odds of each outcome by study condition at the child’s 12-month visit. Statistical significance was evaluated at P < .05. The analyses for this article were generated by using SAS/STAT software, Version 9.2 of the SAS System for PC (SAS Institute Inc., Cary, NC).
Results
An initial sample of 306 mother-child dyads was recruited for the baseline survey during 11 months between June 2005 and March 2006 (see Fig 1). Fourteen infants were excluded because of entry into foster care or diagnosis of pyloric stenosis or hypothyroidism; 292 mother-child dyads remained. The retention rate across all groups (proportion of enrolled subjects who could be reached for follow-up) was 75% and 64% at 6 months and 12 months after recruitment respectively, with 57% of participants having complete data at the 3 time points of baseline, 6 months, and 12 months. At 12 months (data presented in this article), there was no difference in retention by race or maternal education.
Demographic Data
Demographic data are presented in Table 3. This was a young, low-income group of mothers. By their own report, most of the mothers were overweight (average BMI 28; 62% overweight or obese). The 3 groups were equivalent in most baseline measures with 3 exceptions: both the OP and BF moms were more likely to be single, the BF group was more likely to have finished high school, and the MOMS group was less likely to be African American (MOMS 20%; OP 74%; BF 61%, P < .05).
TABLE 3.
Baseline Demographics
| BF (n = 99), n (%) | MOMS (n = 98), n (%) | OP (n = 95), n (%) | |
|---|---|---|---|
| Mother's age, mean | 23.89 | 23.49 | 23.25 |
| Mother's BMI, mean | 27.55 | 29.17 | 28.09 |
| CES-D10 score >11 (depression) | 71(73.1) | 61 (61.3) | 53 (56.4) |
| Mother's education | |||
| < High school | 19 (19)a | 35 (36) | 32 (34)b |
| High school diploma | 47 (47) | 40 (41) | 32 (34) |
| Some college or more | 33 (33) | 23 (23) | 31 (33) |
| Both health numeracy questions correct | 74 (75) | 72 (74) | 59 (62) |
| Mother's marital status | |||
| Single | 49 (49)a | 26 (27) | 49 (52)a |
| Cohabiting | 30 (30) | 38 (39) | 23 (24) |
| Married | 18 (18) | 30 (31) | 18 (19) |
| Widow | 1 (1) | 4 (4) | 2 (2) |
| Chose not to answer | 1 (1) | 3 (3) | |
| Mother's race | |||
| Black | 60 (61)a | 20 (20) | 70 (74)a |
| White | 24 (24)a | 65 (66) | 20 (21)a |
| Other | 15 (15) | 13 (13) | 5 (5)b |
| WIC recipient | 92 (93) | 89 (91) | (91) 96 |
| Food stamps | 59 (60) | 52 (53) | 65 (68) |
| Private insurance | 18 (18) | 11 (11) | 7 (7) |
| Infant is female | 45 (45) | 52 (53) | 43 (45) |
| Infant weight/height z scorec | −0.22 | −0.29 | −0.40 |
WIC, Supplemental Nutrition Program for Women, Infants, and Children.
P < .05 compared with BF.
P < .05 compared with MOMS.
Reported in z scores by using Centers for Disease Control and Prevention Growth Charts 2000 (Centers for Disease Control and Prevention, National Center for Health Statistics. CDC growth charts: United States. Available at: www.cdc.gov/growthcharts/. Accessed May 30, 2000); represents average distance from mean weight-for-height for gender in SDs.
Baseline Maternal Eating Habits and Infant Feeding Practices
At baseline, the mothers had high rates of obesogenic personal eating habits, including fast food consumption, snacking during television viewing, and meal skipping. There were significant differences between groups in the rate of pizza consumption, and consumption of food and soda during television viewing (Table 4). The groups were also different at baseline in terms of infant feeding methods and attitudes (Table 5).
TABLE 4.
Baseline Rates of Maternal Eating Behaviors That Promote Obesity per Group
| BF (n = 99), n (%) | MOMS (n = 98), n (%) | OP (n = 95), n (%) | P | |
|---|---|---|---|---|
| Consume <3 glasses of water per day | 69 (66.4) | 58 (57.4) | 67 (66.3) | .31 |
| Consume >2 glasses of juice or soda per day | 31 (29.8) | 40 (39.6) | 38 (37.6) | .30 |
| Consume <1 serving of dairy per day | 20 (19.2) | 11(10.9) | 16 (15.8) | .25 |
| Consume fast food on weekly basis | 85 (81.7) | 71 (70.3) | 75 (74.3) | .15 |
| Consume pizza on weekly basis | 53 (58.9) | 29 (34.1) | 29 (35.8) | <.01 |
| Skip at least 1 meal per day | 31 (30.1) | 31 (30.7) | 33 (32.7) | .92 |
| Snack in place of meal at least 1 per day | 30 (28.9) | 36 (36.0) | 38 (38.0) | .35 |
| Snack while watching television half or all of the time | 54 (51.9) | 39 (38.6) | 55 (55.5) | .04 |
| Consume soda while watching television half or all of the time | 33 (31.7) | 41 (40.6) | 49 (48.5) | .049 |
| Food insecurity (scaling back or skipping meals in the past year) | 25 (24.1) | 18 (17.8) | 16 (15.8) | .30 |
Centers for Disease Control and Prevention, National Center for Health Statistics. CDC growth charts: United States. Available at: www.cdc.gov/growthcharts/. Accessed May 30, 2000.
TABLE 5.
Maternal Infant Feeding Behaviors per Group at Baseline
| BF (n = 99), n (%) | MOMS(n = 98), n (%) | OP (n = 95), n (%) | P | |
|---|---|---|---|---|
| Feeding type | ||||
| Breastfeed exclusively | 18 (17.3) | 14 (13.9) | 8 (7.9) | .04 |
| Formula | 66 (63.5) | 78 (77.2) | 72 (71.3) | |
| Both breastfeed and formula | 20 (19.2) | 9 (8.9) | 21 (20.8) | |
| Feed infant >24 oz of formula per day | 28 (34.6) | 39 (48.2) | 32 (31.7) | .06 |
| Add cereal to infant bottle | 17 (17.7) | 13 (13.8) | 11 (11.5) | .46 |
| Add juice to infant bottle | 9 (8.7) | 8 (8.1) | 9 (8.9) | .98 |
| Mothers supplement >50% of infant’s feeding with formula when breastfeeding (n = 69) | 7 (26.9) | 5 (35.7) | 13 (44.8) | .39 |
| Continue to feed infant after infant falls asleep | 27 (26.0) | 41 (41.0) | 20 (19.8) | <.01 |
| Agrees that infant crying indicates hunger | 55 (52.9) | 60 (59.4) | 50 (49.5) | .36 |
There was no difference in the physician-reported rate of delivering interventions (60%) or in the maternal reported rate of having read the handouts at 6 months (40%).
Adjusted Group Differences at 12 Months
At 12 months, the groups demonstrated significant differences (Table 6) after adjusting for maternal education, race, marital status, having ever breastfed the child, and baseline snacking behavior while watching television. Both the MOMS and OP groups gave their children less juice and more servings of whole fruit than the BF group mothers. The MOMS mothers gave their children more servings of vegetables than the BF group. Mothers in the OP group were less likely to have daily family meals than mothers in the other 2 groups. There was no difference in reported television watching while eating among the 3 groups. There were no differences among groups for infant growth parameters.
TABLE 6.
Differences in Maternal Eating and Child Feeding Behaviors at 12 Months, by Condition
| BF (n = 64)a | MOMS (n = 61) | OP (n = 59) | |
|---|---|---|---|
| Mean (SE) | Mean (SE) | Mean (SE) | |
| Linear regression | |||
| Mom eats breakfast per week | 5.08 (0.34) | 5.26 (0.37) | 5.21 (0.35) |
| Meals eaten with family per day | 2.60 (0.26) | 2.34 (0.29) | 1.89 (0.29)c |
| Child juice (oz) per day | 14.37 (1.23) | 8.97 (1.36)b | 9.30 (1.31)c |
| Child fruit per day (servings) | 0.94 (0.10) | 1.40 (0.11)b | 1.26 (0.11)c |
| Child vegetables per day (servings) | 1.03 (0.10) | 1.41(0.11)b | 1.20 (0.11) |
| Child milk (oz) per day | 24.05 (1.74) | 25.11 (1.91) | 22.75 (1.94) |
| Infant weight/height z scorec | 0.41 | 0.39 | 0.64 |
| Logistic regression | Odds ratio (CI) | Odds ratio (CI) | Odds ratio (CI) |
| Child tries to feed self | Reference | 0.97 (0.06–15.83) | 0.13 (0.01–1.61) |
| Child drinks juice from cup | Reference | 1.51 (0.31–7.48) | 0.69 (0.19–2.52) |
| Eat main meal in kitchen (versus living room or other) | Reference | 0.67 (0.27–1.65) | 1.26 (0.54–2.92) |
| Television on 8+ hours per day | Reference | 0.90 (0.43–1.91) | 0.96 (0.50–1.84) |
| Child watches <2 h of television per day | Reference | 2.04 (0.76–5.50) | 2.68 (1.13–6.32) |
Analyses adjusted for maternal demographics (race, age, BMI, marital status) and behaviors (ever breastfed and frequent snacking) at baseline. CI, confidence interval.
Note n now omits subjects lost to follow-up.
P < .05 compared with BF.
Reported in z scores by using Centers for Disease Control and Prevention Growth Charts 2000; represents average distance from mean weight-for-height for gender in SDs.
Discussion
This pilot study adds to the emerging data on the effectiveness of specific anticipatory guidance. The mothers in both intervention groups (MOMS and OP) had healthier child feeding habits than those in the BF control group, with the maternal-focused MOMS group performing well in the number of servings of fruits and vegetables given to the infants, in spite of having no direct instructions to do so. Additionally, the OP group of mothers reported fewer family meals than MOMS and BF (usual care) by age 12 months.
There are positive differences in what mothers feed their infants following simple advice to reduce obesogenic maternal-eating habits, such as snacking instead of meals, television watching while eating and caloric beverage and fast food consumption, when compared with mothers who did not receive such advice. Although there has been a virtual storm of publication about childhood obesity in the past 5 years, there have been few attempts to study interventions and fewer still looking at prevention interventions. Those that have been published have generally taken place in schools and other institutions where there is some level of control of the subjects.
This is the first publication of an intervention in infancy in the pediatric office. Our choice to work with maternal eating patterns was made as we realized that the eating patterns of children are closely related to that of their families. Recent correlational work by Anderson and Whitaker25 would suggest that the recommendations of eating scheduled meals with other family members and turning off the television might be particularly helpful. The ecology of family eating is one that is built on over time. The difficulty of changing behaviors after they are well established has been demonstrated by our difficulties in treating obesity. The approach of improving maternal eating habits allows us to attempt to improve the eating environment without intruding into the feeding of the infant with specific discussions of serving size and running the risk of interfering with infant satiety signals. It also has the potential advantage of avoiding the intercultural miscommunications that may occur with the recommendation of specific foods.
This study has some very clear limitations. Because of the risk of intervention contamination had we tried to randomize at the patient level, we randomized at the clinic level. In spite of our attempts to select clinics with similar demographics, the samples had differences in race, marital status, and educational level, which may explain some of the baseline differences in maternal eating habits. Although the differences we found remained even after controlling for baseline differences, it is certainly possible that these differences are accompanied by others that were undetected and affected the outcome, making this a major weakness in the study. Variables that differed among the groups and variables that are known to relate to infant obesity, such as breastfeeding were controlled for, but owing to small sample sizes, the model could not be expanded to include all of the variables that were collected. We did not correct for use of the Supplemental Nutrition Program for Women, Infants, and Children, food stamps, and public insurance. This adjustment would not have influenced the study results owing to the high prevalence of participation in all of these programs. As a pilot, it was done in one community and it may not generalize to other communities. Finally, the study is primarily a study of self-report. Although the items came from validated tools, it is possible that the mothers were telling us what we wanted to hear; however, it is interesting that infant feeding was not part of the instructions given to the MOMS mothers, yet the group had significant differences in reported infant intake.
Although it would have been gratifying to demonstrate differences in weight among groups, it is not surprising that at this early age such a difference would not be found. This was a short trial that did not go past 12 months. The next step may be to carry out both intervention and evaluation into the toddler years when children are even more integrated into family eating style.
In spite of the apparent positive effects of the intervention, there is much room for improvement in all groups. For instance, none of the groups came close to the recommendations of the Centers for Disease Control and Prevention for fruit and vegetable servings per day. Although the MOMS group had the lowest juice intake, the 12-month-olds were still drinking more than 8 oz of juice a day and 23% were watching more than 2 hours of television per day with 39% of homes having the television on for more than 8 hours per day. It is also worth noting that the interventions may have had unintended effects. For example, the OP group reported eating fewer family meals than the BF and MOMS groups at 12 months. This may be related to some unmeasured baseline difference in the groups, or may be that the very specific portion size suggestions disrupted family meals because of the need to monitor what the infant ate more closely.
Conclusions
Providing mothers with information aimed at changing their own eating patterns showed positive differences in reported infant feeding behaviors. There was not a difference in weight at this early age. The approach appears to have been successful in introducing habits associated with lean families into obesity-prone families and thus may ultimately help reduce childhood obesity. Having a newborn may be a “teachable moment” for a mother, allowing her to change her own lifestyle habits for the sake of improved health of her child. Unlike obesity-prevention models that require extra time and personnel and the development of new infrastructures, this model uses a system already in place, the well-child visit, substituting 1 to 2 minutes of more effective anticipatory guidance for the guidance that was already being given, therefore leaving the time cost of the visit unchanged. Brief effective interventions incorporated into well-child care accessed by most parents in the United States could have significant impact on obesogenic behaviors of families, and thus play an important role in the community’s effort to prevent obesity in young children and their families. Currently, however, there is little evidence to support the specific content and style of anticipatory guidance. This study offers a small step in that direction. Both interventions were more effective than the routine BF recommendations, but neither was as helpful as we had hoped. Future work might include combining child-directed and mother-directed intervention and continuing interventions and follow-up into early childhood. Such studies of specific content and style could provide a “brighter future” for anticipatory guidance.
Glossary
- AG
anticipatory guidance
- BF
Bright Futures
- MOMS
maternal-focused advice
- OP
Ounce of Prevention
Footnotes
All of the authors made contributions meeting the criteria for authorship, including substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; drafting the article or revising it critically for important intellectual content; and final approval of the version to be published.
This trial has been registered at www.clinicaltrials.gov (identifier NCT01565525).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by Eunice Kennedy Shriver National Institute of Child Health and Human Development grant 1 R21 HD050944-01 and The Research Institute at Nationwide Children’s Hospital. Funded by the National Institutes of Health (NIH).
References
- 1.Freedman DS, Srinivasan SR, Valdez RA, Williamson DF, Berenson GS. Secular increases in relative weight and adiposity among children over two decades: the Bogalusa Heart Study. Pediatrics. 1997;99(3):420–426 [DOI] [PubMed] [Google Scholar]
- 2.Flegal KM. The obesity epidemic in children and adults: current evidence and research issues. Med Sci Sports Exerc. 1999;31(suppl 11):S509–S514 [DOI] [PubMed] [Google Scholar]
- 3.Dwyer JT, Stone EJ, Yang M, et al. Prevalence of marked overweight and obesity in a multiethnic pediatric population: findings from the Child and Adolescent Trial for Cardiovascular Health (CATCH) study. J Am Diet Assoc. 2000;100(10):1149–1156 [DOI] [PubMed] [Google Scholar]
- 4.Kimm SY, Obarzanek E. Childhood obesity: a new pandemic of the new millennium. Pediatrics. 2002;110(5):1003–1007 [DOI] [PubMed] [Google Scholar]
- 5.Lobstein T, Frelut ML. Prevalence of overweight among children in Europe. Obes Rev. 2003;4(4):195–200 [DOI] [PubMed] [Google Scholar]
- 6.Hotu S, Carter B, Watson PD, Cutfield WS, Cundy T. Increasing prevalence of type 2 diabetes in adolescents. J Paediatr Child Health. 2004;40(4):201–204 [DOI] [PubMed] [Google Scholar]
- 7.Baskin ML, Ard J, Franklin F, Allison DB. Prevalence of obesity in the United States. Obes Rev. 2005;6(1):5–7 [DOI] [PubMed] [Google Scholar]
- 8.Story M. School-based approaches for preventing and treating obesity. Int J Obes Relat Metab Disord. 1999;23(suppl 2):S43–S51 [DOI] [PubMed] [Google Scholar]
- 9.Robinson TN. Can a school-based intervention to reduce television use decrease adiposity in children in grades 3 and 4? West J Med. 2000;173(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Going S, Thompson J, Cano S, et al. The effects of the Pathways Obesity Prevention Program on physical activity in American Indian children. Prev Med. 2003;37(6 pt 2):S62–S69 [DOI] [PubMed] [Google Scholar]
- 11.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007-2008. JAMA. 2010;303(3):242–249 [DOI] [PubMed] [Google Scholar]
- 12.Bluford DA, Sherry B, Scanlon KS. Interventions to prevent or treat obesity in preschool children: a review of evaluated programs. Obesity (Silver Spring). 2007;15(6):1356–1372 [DOI] [PubMed] [Google Scholar]
- 13.Birch LL, Ventura AK. Preventing childhood obesity: what works? Int J Obes (Lond). 2009;33(suppl 1):S74–S81 [DOI] [PubMed] [Google Scholar]
- 14.Agras WS, Mascola AJ. Risk factors for childhood overweight. Curr Opin Pediatr. 2005;17(5):648–652 [DOI] [PubMed] [Google Scholar]
- 15.Svensson V, Jacobsson JA, Fredriksson R, et al. Associations between severity of obesity in childhood and adolescence, obesity onset and parental BMI: a longitudinal cohort study. Int J Obes (Lond). 2011;35(1):46–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hood MY, Moore LL, Sundarajan-Ramamurti A, Singer M, Cupples LA, Ellison RC. Parental eating attitudes and the development of obesity in children. The Framingham Children’s Study. Int J Obes Relat Metab Disord. 2000;24(10):1319–1325 [DOI] [PubMed] [Google Scholar]
- 17.Crespo CJ, Smit E, Troiano RP, Bartlett SJ, Macera CA, Andersen RE. Television watching, energy intake, and obesity in US children: results from the third National Health and Nutrition Examination Survey, 1988-1994. Arch Pediatr Adolesc Med. 2001;155(3):360–365 [DOI] [PubMed] [Google Scholar]
- 18.Ariza AJ, Chen EH, Binns HJ, Christoffel KK. Risk factors for overweight in five- to six-year-old Hispanic-American children: a pilot study. J Urban Health. 2004;81(1):150–161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dennison BA, Erb TA, Jenkins PL. Television viewing and television in bedroom associated with overweight risk among low-income preschool children. Pediatrics. 2002;109(6):1028–1035 [DOI] [PubMed] [Google Scholar]
- 20.Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79(1):6–16 [DOI] [PubMed] [Google Scholar]
- 21.Wells NM, Evans GW, Beavis A, Ong AD. Early childhood poverty, cumulative risk exposure, and body mass index trajectories through young adulthood. Am J Public Health. 2010;100(12):2507–2512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ebenegger V, Marques-Vidal PM, Nydegger A, et al. Independent contribution of parental migrant status and educational level to adiposity and eating habits in preschool children. Eur J Clin Nutr. 2011;65(2):210–218 [DOI] [PubMed] [Google Scholar]
- 23.Howe LD, Tilling K, Galobardes B, Smith GD, Ness AR, Lawlor DA. Socioeconomic disparities in trajectories of adiposity across childhood. Int J Pediatr Obes. 2011;6(2-2):e144–e153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dubois L, Farmer A, Girard M, Peterson K. Regular sugar-sweetened beverage consumption between meals increases risk of overweight among preschool-aged children. J Am Diet Assoc. 2007;107(6):924–934; discussion 934-925 [DOI] [PubMed]
- 25.Anderson SE, Whitaker RC. Household routines and obesity in US preschool-aged children. Pediatrics. 2010;125(3):420–428 [DOI] [PubMed] [Google Scholar]
- 26.Needlman R, Silverstein M. Pediatric interventions to support reading aloud: how good is the evidence? J Dev Behav Pediatr. 2004;25(5):352–363 [DOI] [PubMed] [Google Scholar]
- 27.Hymowitz N, Pyle SA, Haddock CK, Schwab JV. The pediatric residency training on tobacco project: four-year parent outcome findings. Prev Med. 2008;47(2):221–224 [DOI] [PubMed] [Google Scholar]
- 28.Chaudron LH, Szilagyi PG, Kitzman HJ, Wadkins HI, Conwell Y. Detection of postpartum depressive symptoms by screening at well-child visits. Pediatrics. 2004;113(3 pt 1):551–558 [DOI] [PubMed] [Google Scholar]
- 29.Mendelsohn AL, Mogilner LN, Dreyer BP, et al. The impact of a clinic-based literacy intervention on language development in inner-city preschool children. Pediatrics. 2001;107(1):130–134 [DOI] [PubMed] [Google Scholar]
- 30.Sharif I, Rieber S, Ozuah PO. Exposure to Reach Out and Read and vocabulary outcomes in inner city preschoolers. J Natl Med Assoc. 2002;94(3):171–177 [PMC free article] [PubMed] [Google Scholar]
- 31.Tibbs T, Haire-Joshu D, Schechtman KB, et al. The relationship between parental modeling, eating patterns, and dietary intake among African-American parents. J Am Diet Assoc. 2001;101(5):535–541 [DOI] [PubMed] [Google Scholar]
- 32.Green M, Palfrey JS, Clark EM. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents, Revised Pocket Guide. 2nd ed. Georgetown University, Washington DC; 2002 [Google Scholar]
- 33.Wolfe WS, Frongillo EA, Cassano PA. Evaluating brief measures of fruit and vegetable consumption frequency and variety: cognition, interpretation, and other measurement issues. J Am Diet Assoc. 2001;101(3):311–318 [DOI] [PubMed] [Google Scholar]
- 34.Groner JA, Skybo T, Murray-Johnson L, et al. Anticipatory guidance for prevention of childhood obesity: design of the MOMS project. Clin Pediatr (Phila). 2009;48(5):483–492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nicholson LM, Schwirian PM, Klein EG, et al. Recruitment and retention strategies in longitudinal clinical studies with low-income populations. Contemp Clin Trials. 2011;32(3):353–362 [DOI] [PMC free article] [PubMed] [Google Scholar]