Abstract
Background
Delays in receiving effective care during labor and at birth may be fatal for the mother and fetus, contributing to 2 million annual intrapartum stillbirths and intrapartum-related neonatal deaths each year.
Objective
We present a systematic review of strategies to link families and facilities, including community mobilization, financial incentives, emergency referral and transport systems, prenatal risk screening, and maternity waiting homes.
Results
There is moderate quality evidence that community mobilization with high levels of community engagement can increase institutional births and significantly reduce perinatal and early neonatal mortality. Meta-analysis showed a doubling of skilled birth attendance and a 35% reduction in early neonatal mortality. However, no data are available on intrapartum-specific outcomes. Evidence is limited, but promising, that financial incentive schemes and community referral/transport systems may increase rates of skilled birth attendance and emergency obstetric care utilization; however, impact on mortality is unknown. Current evidence for maternity waiting homes and risk screening is low quality.
Conclusions
Empowering communities is an important strategy to reduce the large burden of intrapartum complications. Innovations are needed to bring the poor closer to obstetric care, such as financial incentives and cell phone technology. New questions need to be asked of “old” strategies such as risk screening and maternity waiting homes. The effect of all of these strategies on maternal and perinatal mortality, particularly intrapartum-related outcomes, requires further evaluation.
Keywords: Asphyxia neonatorum, Birth asphyxia, Cash transfers, Community-based health insurance, Community mobilization, Community transport system, Demand for obstetric care, Hypoxia, Maternity waiting homes stillbirth, Neonatal mortality, Risk screening, Vouchers
1. Introduction
Each year there are around 136 million births, of which ~60 million occur outside facilities [1]. At the time of an obstetric emergency, every moment of delay in seeking and receiving skilled obstetric care increases the risks of stillbirth, neonatal or maternal death, or disability. For some emergencies such as antepartum hemorrhage, even hours can be the difference between life and death for mother and fetus. For the baby not breathing at birth, every minute counts. Many of the estimated 1.02 million intrapartum stillbirths and 904 000 intrapartum-related neonatal deaths could be avoided by access to skilled care at birth, timely emergency obstetric care, and immediate newborn care. Intrapartum-related neonatal deaths were previously loosely termed “birth asphyxia” [2], but in this Supplement we follow the recommended shift in terminology [1] based on a series of international consensus statements to use the terms “intrapartum-related deaths” for cause-of-death and “neonatal encephalopathy” for the acute complications manifesting soon after birth [3–5].
There are many real and perceived barriers to accessing care, particularly for women in rural areas of low-income countries. The delays in accessing care for women with obstetric emergencies, the fetus, and neonate are usually described in 3 groups [6–8]: (1) delay in the decision to seek care; (2) delay in reaching a health facility; and (3) delay in receiving quality care.
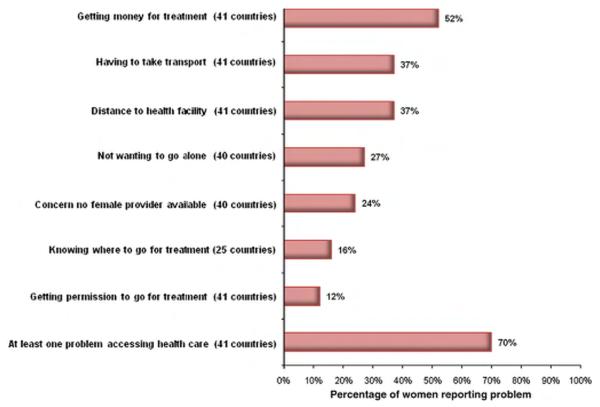
In an analysis of DHS data from 41 countries (Fig. 1), the most common obstacles to seeking obstetric care included financial barriers (>50%), challenges with transport (37%), and distance (37%). Furthermore, many social factors may influence the decision to seek care, such as lack of knowledge about seriousness of complications or where to receive services, requiring permission from family decision makers, and cultural beliefs that may prevent the removal of the mother or newborn from the home [9]. Unavailability and high costs of transportation, poor road conditions, and time to arrange transport may increase the time to reach a health facility. In rural Bangladesh, the use of skilled birth attendance decreased by half when the distance to a health center was beyond 1 kilometer [10]. The delay in receiving quality obstetric care may be caused by understaffing, lack of supplies and equipment, staff incompetence, and lack of trained personnel. In Indonesia, the requirement for prepayment for supplies and medications, lack of resuscitation equipment in the emergency room, and unavailability of staff trained in neonatal resuscitation led to delays in receiving prompt intervention for a newborn with “birth asphyxia” [9]. In an audit of perinatal deaths in a Tanzanian hospital, the first, second, and third delays contributed to 19%, 21%, and 73% of perinatal deaths, respectively [11].
Fig. 1.
Maternal perceptions of barriers to obstetric care based on analysis of large-scale household surveys (2000–2007). Source: Based on new analysis of DHS data (2000–2007) from Macro DHS Statcompilier, May 2009. Since the specific questions vary by country, the number of countries with data per question is given.
A functioning continuum of care between home and hospital is required to minimize these potentially deadly delays and effectively link women and newborns with care [12]. Much of the literature on provision of effective care at birth focuses on the content of care or the provider. There has been limited attention to review of the evidence for linkages between home and hospital and between levels within the health system. While some of these issues may be context specific depending on local constraints such as distance, difficult terrain, or cultural seclusion practices [1], there are also shared constraints and possible strategies.
Strategies to build this household-to-hospital continuum and overcome the first and second delays are the focus of the present paper and may involve two main approaches. Firstly, delays can be reduced by “moving” the community toward facilities, for example through mobilizing and empowering families to seek health care with birth preparedness planning, transportation systems, as well as financing strategies to reduce the up-front costs of transport or hospital care. Further delays in transportation may occur between first level health facilities and the referral hospital, especially if emergency obstetric care is not available at the first level, and may be reduced by communication and referral systems. Secondly, the formal healthcare system can reduce delays by bringing the necessary care closer to the community; for example, providing community midwives or birthing centers in the community [13], or identifying women at highest risk to come to maternity waiting homes near a hospital with emergency obstetric care. Some interventions may be provided at community level by skilled attendants or community cadres, although this is typically not feasible for emergency obstetric care [13]. Strategies to address the third delay by improving the quality and supply of care in the facility are reviewed in the second (intrapartum care) [14], third (neonatal resuscitation), and sixth (perinatal audit) [15] papers in this Supplement.
1.1. Objectives
This paper is the fourth in a series that focuses on reduction of intrapartum-related deaths. The objectives of this paper are to describe the evidence for interventions to link mothers with skilled care during pregnancy, labor, and birth, and to summarize the implications for programs. We describe the content of the interventions, summarize the evidence using the modified GRADE system [16] (Grading of Recommendations Assessment, Development, and Evaluation system for rating strength of evidence and recommendations), and present data on effects, when available, on early neonatal mortality rate (ENMR), intrapartum-related neonatal mortality rate (IPR-NMR), stillbirth rate (SBR), intrapartum stillbirth rate (IP-SBR), and perinatal mortality rate (PMR) [17,18]. We also present evidence on the effects on intermediate outcomes such as care seeking, skilled birth attendance and facility delivery rates, cost and cost-effectiveness. The strategies reviewed in this paper are shown in Table 1.
Table 1.
Strategies included in the present review.
| Increasing community demand for obstetric care (Section 3 in this paper) |
| 3.1 Community mobilization |
| 3.2 Financing strategies |
| • Elimination of user fees |
| • Community-based health insurance |
| • Community loans |
| • Conditional cash transfers |
| • Voucher schemes |
| • Contracting out and pay for performance |
| Bringing pregnant women closer to the formal health system (Section 4 in this paper) |
| 4.1 Community referral systems and transport approaches |
| 4.2 Antenatal risk screening by health workers |
| 4.3 Maternity waiting homes |
2. Methods
Details of the searches undertaken and the selection criteria for inclusion are described in the first paper of this series [1]. Searches of the following databases of the medical literature were conducted: PubMed, Popline, EMBASE, LILACS, IMEM, African Index Medicus, Cochrane, and World Health Organization (WHO) documents. The initial search was conducted during 2002 and was updated to May 2009. Keywords utilized in the searches included “birth asphyxia/asphyxia neonatorum,” “hypoxic ischemic encephalopathy,” “neonatal encephalopathy,” or “neonatal-perinatal mortality” in various combinations with “emergency transport,” “information communication technology,” “community based insurance,” “emergency loans,” “emergency funds,” “community mobilization,” “community action cycle,” “public private partnership,” “maternity waiting homes,” and “risk screening.” Under each subheading we review the background of, the evidence of effectiveness, data on cost if available, and summarize the implications for programs. All effect sizes reported are relative percentage mortality rate reduction, as opposed to absolute percentage reduction. The level of evidence was assessed using the GRADE system [16] criteria to evaluate the quality of the evidence (strong, moderate, low, or very low) and given a recommendation for programmatic application (strong, weak, conditional). We use an adaptation of GRADE developed by the Child Health Epidemiology Reference Group (CHERG) specifically for low- and middle-income settings [19]. Our particular interest is in intrapartum-related (“birth asphyxia”) outcomes, this is a particular constraint since cause-specific data are limited [1]. Costing data are from the actual year reported and not adjusted for inflation.
We also conducted a meta-analysis of community mobilization using the Mantel-Haenszel pooled relative risk (RR) and corresponding 95% confidence interval (CI). When significant heterogeneity was detected (P<0.10) a random effects model was used to estimate the RR and CIs. Studies were considered for inclusion if the study design was a randomized controlled trial or quasi-experimental study with replication of intervention and control units, reporting the outcomes of interest (skilled birth attendance, PMR, or ENMR). Meta-analysis of all-cause NMR was not conducted since most packages addressed multiple neonatal conditions, and in the absence of cause-specific mortality data, PMR and ENMR may more specifically reflect the burden of intrapartum-related events. Studies were excluded if they were observational before-and-after studies or did not report the desired outcomes. All analyses were conducted using STATA 10.0 statistical software (StataCorp, College Station, TX, USA).
3. Increasing demand for obstetric care
3.1. Community mobilization
3.1.1. Background
Community mobilization is a process of enabling people to organize themselves, recognize opportunities, identify their collective potential, and utilize available resources to realize a shared goal through unified action. Strategies to “mobilize” communities are diverse, and may entail differing levels of intensity of engagement, community involvement, and ownership (see Panel 1 at the end of the paper) [20,21]. Mobilization strategies for maternal-newborn care include approaches to:
Change individual behaviors to implement key preventative practices: for example, peer counseling and home visitation to promote healthy pregnancy and birth behaviors, immediate newborn care, and rapid care seeking [22].
Increase collective knowledge and practice of preventative behaviors, as well as recognition, identification, and care seeking for danger signs and symptoms: for example, women’s groups and engaging key stakeholders to enhance individual behavior change and to shift community norms [23,24].
Promote broader community action to address major barriers to care: for example, engaging with village health committees to address transport and financial barriers to care.
Panel 1. Strategies to mobilize communities to seek skilled birth care.
Women’s Groups with Community Action Cycle
The community action cycle was originally developed in the Warmi project and involves 4 main processes [23]: (1) identification and prioritization of key maternal and newborn health problems in the local community; (2) developing a formal action plan; (3) implementation of solutions as a community; and (4) evaluation of the progress of the program, assessing challenges and solutions.
In the Warmi [23] and Makwanpur projects [24,114,127], the community-designed interventions included a wide range of activities from creation of community funds for transport, acquisition of stretchers, and education regarding danger signs in pregnancy with interactive picture card games and role playing.
Photograph reprinted with permission granted by Anne CC Lee.
· Community Action Cycle: Figure reprinted with permission granted by Lancet.
· Photograph reprinted with permission granted by Anne CC Lee.
Community groups with socio-contextualized behavior change messages
The Saksham study conducted extensive formative research regarding childbirth practices and engaged stakeholders at multiple levels, from household members, village leaders, priests, teachers, traditional birth attendants, other practitioners, and community volunteers [22]. Newborn care interventions were tailored to the local traditions and customs at birth, and disseminated at community group meetings and one-on-one community health worker visits. The Skilled Care Initiative in Burkino Faso also used community groups to map local health beliefs, engage local traditional and religious leaders, and implement activities using existing social platforms [33].
Community education meetings
Many programs use community group meetings to educate women and families about prenatal care, danger signs during pregnancy, signs and symptoms to refer, essential newborn care, and postnatal care. Educational strategies may include lecturing, flip charts, role playing, and video. Group leaders may include CHWs, TBAs, key community members, or program staff.

Photograph from Shivgarh, Uttar Pradesh, India, reprinted with permission granted by Bill & Melinda Gates Foundation/Jeffrey Spector.
Village health committees
Village health committees may organize community members to develop actions to address key issues, such as the development and administration of emergency funds and transport driver systems. Members may include key stakeholders, and those with specific expertise, such as members of the local bank to assist administration of local funds [38]l.
Community campaigns
Social marketing campaigns have been used to generate awareness of maternal and newborn health issues, including a wide range of activities from public concerts, radio campaigns, video, and TV commercials. The Prevention of Maternal Mortality Group in Nigeria has promoted childbirth health awareness, particularly focusing on male decision makers and used a range of media such as puppets and a video drama of a maternal death [28,64,128].
Over the last decade, more focus has been placed on community approaches specifically designed for a given setting and purpose based on formative research to understand local culture, beliefs, and practices. [20,22]. Community mobilization may have the most power to change behaviors and enable access to care where neonatal deaths are seen as inevitable, and community norms, such as seclusion for pregnant women and new mothers, preclude care seeking in the formal health sector [1].
3.1.2. Evidence for community mobilization
There are an increasing number of studies of community mobilization to improve maternal, newborn, and child health (Table 2), predominantly from South Asia, with a few from Latin America or Africa [22,24–29]. Here we focus on studies that illustrate key mechanisms for mobilization or that report specific intrapartum-related or mortality outcomes.
Table 2.
Evidence for community mobilization: Mortality effect and intermediate outcomes.
| Intervention/study (date order) | Setting | Percent skilled attendance |
Baseline mortality rate |
Mortality Effect: Percentage relative reduction in mortality rate (number of deaths in intervention or end line group); RR or OR (95% CI) |
Intermediate outcomes | Investigator and year |
||||
|---|---|---|---|---|---|---|---|---|---|---|
| SBR | ENMR | PMR | NMR | MMR | ||||||
| Before-and-after comparison of community empowerment specifically through women’s groups. |
Rural Bolivia | 23% | PMR 117 | 47% (21) | - | 62% (31) | 76% (10) | Pre vs Post Comparison • Received prenatal care 49% to 64% (P=0.009) for control subjects |
O’Rourke et al. [23] 1998 |
|
| RR 0.53 (0.31– 0.89) |
RR 0.37 (0.25–0.56) |
RR 0.24 (0.12– 0.47) |
• Breastfeeding on first day of life 25% vs 50% (P<0.001) |
|||||||
| Cluster RCT of community mobilization through participatory women’s groups using action-learning cycle to identify perinatal problems and create community strategies to address. Upgrading of health services in both intervention and control arms. |
Rural Makwanpur District, Nepal |
<13% | NMR 25.4 (intervention) |
Nonsignificant change |
30% (76) aOR 0.70 (0.53–0.94) |
78% (2) aOR 0.22 (0.05–0.90) |
Intervention vs Control • Any prenatal care 55% vs 30% (OR 2.82; 1.41–5.62) |
Manandhar et al. [24] 2004 |
||
| Populations 170 000 | NMR 25.1 (control) |
• Iron-folate 49% vs 27% (OR 1.99; 1.14–3.46) |
||||||||
| Intervention area (14 884 households) |
MMR 539 | aOR 1.06 (0.76–1.47) |
• Iron-folate 49% vs 27% (OR 1.99; 1.14–3.46) • Institutional delivery 7% vs 2% (OR 3.55; 1.56–8.05) |
|||||||
| Control area (14 047 households) |
• Birth attended by skilled provider 7% vs 2% (RR 3.53; 1.54–8.10) |
|||||||||
| Before-and-after comparison of community mobilization with formation of village health committees, establishment of emergency loan/transport funds, and training of Home-based Life Saving Skills |
Rural Uttar Pradesh, India Population 20 000 |
20% | NMR 42 | Nonsignificant changea |
17%b (21) | 60%c (3) | Pre vs Post Comparison • Birth preparedness index, any of 3 indicators 15% vs 82% (P<0.001) |
Fullerton et al. [27] 2005 |
||
| Cluster randomized trial of package of birth and newborn care preparedness (BNCP) interventions in Home vs Community care. In Home-care group CHWs provided prenatal visit, promoted BNCP, postnatal visits in first week of life, referred sick newborns, and treated sepsis at home with injectable antibiotics. In Community care arm, community mobilizers promoted BNCP in group sessions. In comparison and intervention arms, promoted improvement of government health facilities. |
Rural Sylhet district, Bangladesh Population 200 000 Home care: (14 880 pregnancies) Community care: (16 449 pregnancies) Comparison: (15 779 pregnancies) |
CHWs attended 5% of births |
NMR 48 | Community Care 5% aRR 0.95 (0.69–1.31) Home Care armd 34% aRR 0.66 (0.47–0.93) |
Community Care vs Control • Any prenatal care 62% vs 49% (P=0.13) • Iron-folate 45% vs 25% (P<0.001) |
Baqui et al. [29] 2008 |
||||
| Pilot study training of Lady health workers (LHW, CHW) and Dais (TBAs) in home-based newborn care (including basic resuscitation), improvement of linkages between LHWs and Dais, and community mobilization with group educational sessions and establishment of health committees and emergency transport funds. Strengthening of health facilities in intervention/control areas with training and upgrading equipment. |
Hala and Matiari sub districts, rural Sindh province, Pakistan Intervention: 2672 Control: 2462 |
Baseline skilled attendance 18% LHWs attended 5% of births in intervention areas |
Baseline stillbirth 65.9 (intervention) Baseline NMR 57.3 (intervention) |
35%e (132) | 36.2% e (90) |
34.6%e (222) | 28%e (121) | Intervention areas Before vs After • Home births 79% vs 65% (P=0.01) • Skilled birth attendant 18% vs 30% (P=0.03) |
Bhutta et al. [25] 2008 |
|
| Cluster randomized trial of essential newborn care package delivered by CHWs via collective meetings, prenatal and postnatal visits. Participatory social mapping and formative research conducted in local community to develop behavior-change strategies for intervention package. Intervention clusters received either essential newborn care (ENC) package or ENC plus use of a hypothermia indicator (Thermospot). |
Shivgarh, rural Uttar Pradesh, India Total population of study area 104 123 |
Baseline skilled attendance in all groups <5% |
Baseline stillbirth 24.4 (ENC) 27.2 (control) Baseline NMR 64.1 (ENC) 54.2 (control) |
ENC: 28% (59) RR 0.72 (0.52–1.00) ENC+TS: 15% (48) RR 0.85 (0.56–1.29) |
ENC: 44% (51) ENC +TS: 47% (36) |
ENC: 41% (113) aRR 0.59 (0.47–0.74) ENC+TS: 38% (96) aRR 0.62 (0.47–0.81 |
ENC: 54% (64) aRR 0.46 (0.35–0.60) ENC+TS: 52% (48) aRR 0.48 (035–0.66) |
Intervention vs Control • Any prenatal care 26% vs 14% (RR 1.84; 1.08–3.14) • Birth Preparedness Identification facility 14% vs 4% (RR 3.43; 2.12–5.14) Identification attendant 22% vs 5% (RR 4.94; 3.19–7.63) Arrange money 25% vs 15% (RR 1.55; 1.15–2.09) • Institutional Delivery 19.7% vs 14% (RR 1.41; 0.93–2.13) |
Kumar et al. [22] 2008 |
|
| Quasi-experimental study of Skilled Care Initiative including health systems strengthening and community mobilization interventions including advocacy, social marketing, behavior change communication and capacity strengthening. Including analysis and prioritization of community problems, birth preparedness activities and promotion of emergency funds |
Rural Ouargaye district Burkino Faso |
Baseline institutional births 30%–35% |
PMR 33 | 28% aOR 0.72 (0.68–0.77) |
31.5% f | Institutional births increased significantly in intervention areas OR 1.23 per yr (95% CI, 1.018–1.28) more than in comparison area 1.08 per yr (95% CI, 1.05–1.12). Significant difference in trend (P<0.001) |
Hounton et al. [33] 2009 |
|||
| Community mobilization activities for birth planning. Development of Community Support System with emergency funds for transport, hospital fees, volunteer for support or blood donation. Improvement in quality of care in health facilities through community input and hospital audit. Health facilities were upgraded in comparison and intervention regions. |
Dinajpur, Northewestern Bangladesh Pop: 200,000 |
16% | NS | • Proportion of facility-based births in intervention area increased from 2% to 21%; comparison area (facility upgrade only) from7% to 13%; with no change in control area • Skilled attendance at delivery 19% in intervention areas, 5% in control area • Met need for EmOC services increased 24% in intervention area, 13% in comparison, and 1% in control areas • 15 Community groups purchased riskshaw-van for transport and 13 established loan funds. 52 women used money from emergency funds, 23 were transported and accompanied to health facility |
Hossain et al., 2006 |
|||||
Abbreviations: SBR, Stillbirth Rate; ENMR, Early Neonatal Mortality rate; PMR, Perinatal Mortality Rate; NMR, Neonatal Mortality Rate; IPR-NMR, Intrapartum-related Neonatal Mortality Rate.
Nonsignificant change in stillbirth rate (baseline rate 2.7 per 1000 vs end line 4.4 per 1000, P=0.095).
Nonsignificant reduction in NMR (baseline rate 4.2 per 1000 vs end line 3.5 per 1000, P=0.56).
Significant reduction in MMR (baseline rate 1.5 per 100 000 vs end line 0.4 per 100 000, P=0.053).
Community care arm includes mobilization; home care arm includes mobilization and home management of sepsis.
Before-and-after comparison in intervention clusters.
In intervention district MMR decreased from 446 to 305 per 100 000 vs control district decreased from 562 to 473 per 100 000.
The Warmi project in rural Bolivia was the originator of the “Community Action Cycle” methodology (Panel 1) and worked with women’s organizations and community members in 50 rural communities to galvanize women around health issues [11]. At the end of the project period, there were improvements in prenatal care utilization and PMR was reduced from a baseline level of 117 per 1000 to 44 per 1000 from 1990 to 1993 (RR 0.37; 95% CI, 0.25–0.56), primarily due to a reduction in deaths on the first day of life, which probably included a reduction in intrapartum-related neonatal mortality (IPR-NMR). In 1994, the program was expanded into the Bolivian National Health plan to over 500 communities, and while no mortality data are available, rates of skilled birth attendance reportedly increased in the target communities [30].
The MIRA (Mother and Infant Research Activities) project in Nepal adapted the methodology of the Warmi project to link women with primary maternal-neonatal services [10]. A cluster randomized controlled trial (cRCT) was conducted in Makwanpur district, a mountainous region with 94% home births, in which 12 groups of villages convened monthly participatory women’s groups led by a local female facilitator, using the community action cycle (Panel 1). In these intervention clusters there was a 30% reduction in neonatal mortality (OR 0.70; 95% CI, 0.53–0.94), and a 78% reduction in maternal mortality (OR 0.22; 95% CI, 0.05–0.90) compared with the control clusters. Women in the intervention areas had significantly improved care-seeking behaviors, including increased prenatal care visits, visits to health facilities for acute illness of the mother or infant, institutional delivery, and skilled birth attendance (Table 2). Although improvements in the early identification of pregnancy complications and access to prenatal and intrapartum care may have reduced the burden of intrapartum events [31,32], preliminary analysis has failed to show a reduction in intrapartum-related mortality, possibly due to the low rates of skilled birth attendance even after the intervention (7%) (Personal communication, D. Osrin, June 2009).
In the Saksham (Hindi for empowerment) Study in Shivgarh, India [22], formative research regarding childbirth and newborn care practices was conducted, risk factors for mortality were identified, behavior change messages targeting key risk factors were developed, home-based counseling on newborn care was conducted by Community Health Workers (CHWs), and a variety of community stakeholders were engaged in group meetings to stimulate behavior change tailored to be compatible with local customs and childbirth practices (Panel 1). In the intervention areas, mothers were more prepared for birth, with significantly higher rates of identification of health facility and birth attendant, arrangement of money in case of emergency prior to delivery, and care seeking from a qualified practitioner for signs of maternal illness. Neonatal mortality was reduced in the intervention arms (combined) versus comparison arm (adjusted RR 0.47; 95% CI, 0.37–0.59). The reduction in stillbirths (adjusted RR 0.77; 95% CI, 0.62–1.23) and in early neonatal deaths (adjusted RR 0.53; 95% CI, 0.42–0.65) indicates that primary prevention through birth preparedness may have been effective in reducing adverse intrapartum events; cause-specific mortality data will help elucidate this effect.
The Skilled Care Initiative in Ouargaye district, Burkina Faso, utilized community mobilization strategies to generate higher demand for skilled obstetric care in parallel with supply-side quality improvement [33,34]. Behavior change communication was a key component of community workshops in addition to social marketing and stakeholder engagement. PMR was 25% lower in the intervention versus comparison district (OR 0.75; 95% CI, 0.70–0.80), and rates of institutional delivery increased in the intervention district (OR 1.23 per year; 95% CI, 1.18–1.28) more quickly than in the comparison district (OR 1.08; 95% CI, 1.05–1.12). There was no difference in cesarean delivery rates between districts (0.34% vs 0.46% in intervention vs control).
The creation of village health committees was a key strategy to increase demand for skilled birth care in a pilot study in Hala and Matiari subdistricts of rural Sindh province [25]. Lady Health Workers from within the government health system, along with community volunteers, established village health committees and led 3-monthly group educational sessions. Most villages (86%) in intervention clusters established community health committees, of which 31% established emergency funds for transport and hospital fees. In the intervention clusters there was an increase in the proportion of births taking place in public sector facilities (from 18% to 30%), a reduction in home-births (from 79% to 65%), and reductions in stillbirth (65.9 to 43.1 per 1000) and neonatal mortality (57.3 to 41.3 per 1000) rates following the intervention in the absence of major changes in the concurrent control areas. Although data on intrapartum-related neonatal mortality rates are not yet available, the substantial reductions in early neonatal mortality and stillbirths may reflect the impact of these interventions on intrapartum-related hypoxia via improved intrapartum management, and emphasize the potential effectiveness of a public sector program approach.
Program experience with village health committees in Bangladesh and India has also demonstrated significant improvements in birth preparedness, improved rates of institutional delivery, and met need for emergency obstetric care services (Table 2) [27,132].
Community education sessions of lower intensity or without active solution-making processes may not mobilize communities as effectively. In Sylhet, Bangladesh, group education meetings alone did not appear to improve neonatal outcomes or care-seeking behaviors [29]. The interactions were of relatively low intensity (meetings once every 4 months with a mobilizer:population ratio of 1:18 000) and the mobilization activities did not utilize an action-oriented approach, which may have contributed to the lack of effect. In Siraha, Nepal, monthly community education sessions resulted in improvements in knowledge of birth preparedness and prenatal, postnatal, and essential newborn care, but no improvements in intrapartum care seeking [26].
Meta-analysis of 4 studies of community mobilization was conducted [22,24,25,29]. The Skilled Care Initiative and Dinjapur Safe Motherhood Initiative studies were excluded as there were 2 districts compared, which had large pre-existing differences between the areas at the beginning of the study; it is thus impossible to properly account for the uncertainty associated with between-area variation [33,34]. The Projahnmo study community care arm was used to evaluate the effect of isolated mobilization on facility delivery; the home-care arm was not included as this also involved the home-based management of sepsis with antibiotics. The meta-analysis indicated evidence of increase in demand for skilled obstetric care, as the proportion of institutional births increased by 71% (RR 1.71; 95% CI 1.10–2.64) (Fig. 2A); however, the mobilization strategies were heterogeneous between studies, and in a sensitivity analysis that included only the more intensive and participatory mobilization strategies [22,24,25], the proportion of institutional births doubled (RR 2.08; 95% CI 1.23–3.49) (Fig. 2B). For these studies there was also evidence of a reduction in PMR (RR 0.75; 95% CI, 0.59–0.96) and ENMR (RR 0.64; 95% CI, 0.48–0.85). These studies did not differentiate cause-specific fetal or neonatal mortality due to intrapartum-related events; however, approximately one-third of stillbirths [2] and 30% of early neonatal deaths are estimated to be intrapartum-related in settings with low skilled attendance at birth [1,35]. As community mobilization could prevent intrapartum-related deaths by reducing delays in receiving obstetric care and increasing facility delivery rates, it is plausible that reductions in perinatal and early neonatal deaths reflect some level of reduction in intrapartum-related mortality.
Fig. 2.
Estimates of the effect of community mobilization on institutional delivery. (A) All community mobilization studies meeting inclusion criteria. (B) High-intensity community mobilization studies.
3.1.3. Cost-effectiveness of community mobilization
Cost data for community mobilization packages are limited and variable depending on the specific components implemented and the economic methods used. In the initial Warmi Project covering 50 communities (population 15 000), the cost of training materials, women’s group facilitators, and related program expenses was about US $100 000 per year, with an average cost of US $6 per population, and about US $1923 per perinatal death averted. When the program was scaled to the national level, the budget was US $1.25 million per year. In the Makwanpur trial, Nepal, the total cost of the women’s group interventions including training, equipment, transportation, and upgrading the local health services was US $77 765 per year, with an average cost of US $0.90 per person (population 86 704), US $5.22 per married woman of reproductive age, US $6912 per neonatal death averted, and US $251 per life year saved [36].
3.1.4. Implications regarding community mobilization
Three cRCTs, 2 quasi-experimental studies, and 1 before-and-after study gave moderate-quality evidence that community mobilization programs can reduce early neonatal and perinatal mortality and increase skilled birth attendance. Our meta-analysis showed a 71% increase in institutional deliveries, with a two-fold increase for high intensity mobilization strategies. While none of these indicators is a direct measure of intrapartum-related mortality, it is plausible that skilled birth attendance is an important pathway to reduce intrapartum stillbirths and intrapartum-related neonatal deaths. Programs demonstrating mortality reduction had high levels of active community participation, contextualized newborn problems in the local customs and culture, involved a broad range of key community stakeholders, and included home visitation and peer counseling. Programs with passive community involvement, low frequency contacts, or which provided education without addressing problems generally failed to demonstrate effectiveness. The GRADE recommendation for implementation of intensive, participatory community mobilization is strong, however, additional research is needed to determine the effect of community mobilization on cause-specific mortality, cost-effectiveness, and effectiveness in different settings, particularly Africa. While the quality of evidence for an effect of community mobilization on perinatal and neonatal mortality is moderate, there are no data on intrapartum-related mortality, and limited data from Africa, and hence, the GRADE quality of evidence for interventions affecting this specific outcome is not available (Table 3).
Table 3.
Interventions reviewed: Evidence GRADE, feasibility, and recommendations.
| Intervention | GRADE evidence level for perinatal mortality outcomes | GRADE recommendations | Feasibility in low- and middle-income settings |
|---|---|---|---|
| Increasing community demand for obstetric care | |||
| Community mobilization |
MODERATE: Two cRCTs, 2 quasi-experimental trials, and 1 before-and- after study have shown benefits of community mobilization in increasing institutional delivery and reducing perinatal mortality. The data is consistent for programs of higher intensity mobilization; one RCT failed to show impact. The evidence is generalizable to low- and middle-income settings, although indirect, as intrapartum-related mortality was not available. |
STRONG: Several moderate-high quality studies have shown benefit of high intensity community mobilization strategies, with the likely indirect effects on intrapartum-events. Given the benefit on all cause perinatal mortality, lack of harm, and low cost, the strategy is strongly recommended. |
Successful program experience has been demonstrated in South Asia, Latin America, particularly with increasing levels of community participation- ownership. Programs may be started with low cost; more evaluation is needed on cost-effectiveness, sustainability, and scalability. |
| Financing Strategies • Elimination of user fees • Community-based health insurance loans • Conditional cash transfers • Vouchers • Community loans |
VERY LOW: There are several low-quality before-and-after program reports showing that different financial strategies may be associated with greater obstetric care seeking. The data is generalizable to low- and middle-income settings, and is primarily from Africa and South Asia. There are no direct data on the impact on perinatal health outcomes or on intrapartum-related events. |
CONDITIONAL: There is promise for these strategies to increase institutional delivery and access to emergency obstetric care for the poor, but more rigorous evaluation of the impact on health outcomes, cost-effectiveness, and sustainability is needed before recommendations for implementation can be made. |
Program experience in several low- and middle-income country settings, primarily Africa and South Asia. Challenges include sustainability, high administrative costs, repayment-defaults of loans. Insurance premiums and loan systems may still marginalize the poor. Most programs may require government support to ensure sustainability. All of the demand-side strategies need to be accompanied by increasing supply of obstetric services maintaining quality of care. |
| Communication and transport systems |
LOW: There are several low-quality before-and-after program reports showing that communication and transport systems may increase obstetric care seeking. Few studies report reduced transport time and maternal case fatality. The data is generalizable to low- and middle-income settings, though most studies were from Africa. There is only 1 program report on perinatal outcomes, with no reports of intrapartum-specific mortality. |
CONDITIONAL: There is promise for communications and transport systems to reduce transport time and increase receipt of obstetric care. However, impact on health outcomes, cost-effectiveness, and sustainability need to be assessed before recommendations for wide-scale implementation can be made. |
Challenging in rural settings with poor road transport and communication infrastructure; high costs of vehicles and maintenance, and 24-7 on call coverage. Potentially sustainable, lower-cost models use existing infrastructure, drivers or transport systems (transport union, taxis, flagging system). |
| Bringing pregnant women closer to the formal health system | |||
| Prenatal risk screening by community-based workers |
VERY LOW: There are several low-quality validation studies of risk screening using observational data, demonstrating poor predictive value. There was one before-and-after observational study demonstrating a reduction in perinatal and intrapartum-relatedmortality in a program including risk screening, and risk-screening for admission to maternity waiting homes has been associated with lower perinatal mortality in 3 low-quality observational studies. |
CONDITIONAL: While early risk screening algorithms used maternal characteristics, there may be a role for testing risk screening algorithms using early pregnancy complications with higher predictive value and low prevalence. Further evaluation of the effects of such algorithms need to be evaluated. |
Simple algorithms to identify high-risk women can be followed by non-professional health workers. However, algorithms or checklists using pregnancy complications (such as breech, multiple pregnancy, late pregnancy, vaginal bleeding, or high blood pressure) need to be evaluated in a program-intervention context considering risk of over referral and overloading health facilities with limited supply. |
| Maternity waiting homes |
LOW: Four low-quality observational cross-sectional studies associated lower perinatal-neonatal mortality with babies of mothers who stayed in maternity waiting homes. However, only 1 study adjusted for the difference in baseline obstetric risk between mothers of intervention and comparison groups. The majority of studies were from Africa and generalizable to low- and middle-income settings. No data on intrapartum-related mortality were available. |
WEAK: There is potential for this strategy in rural settings, however there is a lack of convincing evidence of effectiveness and a need for rigorous evaluation of the impact on maternal and perinatal outcomes, as well as cost-effectiveness. |
Pilot tested in several African settings. Challenges include acceptance and utilization in different cultures, costs of stay, and cost-effectiveness of strategy. Services need to be coordinated and linked with hospital facility with CEmOC. |
3.2. Financial strategies
3.2.1. Background
For the poor, the costs of transportation and obstetric care are frequently prohibitive [37–39]. In the regions with the lowest rates of skilled birth attendance, Sub-Saharan Africa and South Asia, 40%–54% of all health expenses are paid directly out-of-pocket by families who are already in the lowest income countries of the world (Fig. 3). In low-income settings, a normal hospital delivery may cost 3%–26% of annual gross domestic product per capita and the cost of a cesarean delivery may exceed a family’s annual income [40]. Having adequate funds available at the time of need is a challenge for the poor. In Bangladesh, 74% of mothers who had a cesarean delivery did not have the money to pay for it at the point of care [37].
Fig. 3.

Out-of-pocket expenditure as a percentage of total expenditure on health. Source: New analysis using data from National Health accounts available from WHO Statistical Information System, June 2009. The range lines demonstrate the minimum and maximum for each region. Percentages are unweighted regional averages for countries with data on out-of-pocket expenditure as a percentage of total of expenditure on health. Currently, there is no comparable national data on out-of-pocket expenditure specific to maternal, newborn and child health expenditure because National Health Accounts do not routinely split out and report this figure.
In this section we will briefly review several promising financial strategies to increase community demand for obstetric care: elimination of user fees, community-based insurance schemes, community loan funds, conditional cash transfers, vouchers schemes, contracting out and pay for performance (Table 4). Some examples of supply-side interventions will also be discussed. Borghi et al. [40] comprehensively review financial strategies for improving maternal health in the fourth paper of The Lancet Maternal Survival series.
Table 4.
Financial strategies to increase access to obstetric care.
| Strategy | Definition |
|---|---|
| Elimination of user fees | Out-of-pocket expenses for hospital fees for maternal-newborn health care have been abolished in several settings, in an attempt to reduce inequities in access to care for the poor. Families may incur other charges during hospitalization, however, and cost of transport is not typically covered [40]. |
| Community-based insurance schemes |
Insurance plans at the community level aim to reduce out-of-pocket expenses by risk pooling; members typically pre-pay a fixed fee to join a program at the beginning of pregnancy and qualify for free or reduced rate obstetrical services at the time of childbirth. However, fees are often unaffordable for the poor and in programs with small membership, a high frequency of expensive procedures may exceed the gross income, and therefore be unsustainable. Some plans exclude more expensive costs, such as childbirth care [40]. |
| Community loans funds | Funds are generated from contributions of community members and permit families to borrow sums to pay up front for emergency transportation and hospital costs. They are typically managed by appointed community members, and may have varying procedures for repayment and interest; however, repayment is required for fund replenishment and sustainability [38,40,64]. |
| Conditional cash transfers | Conditional cash transfers provide cash payments to pre-selected mothers or families, typically from poor or marginalized groups, on the condition that they use specified services [40]. However, families must locate and afford transport and hospital fees in order to receive care, since conditional cash transfers are not given until after its receipt. |
| Vouchers | Vouchers are given to pre-identified, poor or marginalized mothers and can be redeemed for free health services at specified facilities. These may be advantageous as mothers do not need to pre-pay for services, and thus for a costly procedure such as a cesarean section, the family would not need to come up with a large sum of money before accessing care [40,72,121]. |
| Contracting out and pay for performance |
Contracting and providing financial incentives to private practitioners or organizations to provide obstetric health services for the poor may improve their access to childbirth care. Penalties for non-performance have also been attempted to improve quality of care provided. |
3.2.2. Evidence for financial strategies
We identified many reports of small-scale programs implementing community emergency loan funds and community-based health insurance schemes, primarily from Africa and one from South Asia and Latin America (Table 5) [41–52]. There were fewer reports of conditional cash transfers and voucher schemes, mainly from South Asia and Latin America [53–57]. While some of these reports present data on utilization of obstetric care, we did not identify any that reported on maternal or neonatal health outcomes, long-term sustainability, or cost-effectiveness.
Table 5.
Effect of financing strategies to increase demand for obstetric care.
| Intervention/study (date order) | Setting | Care seeking/demand | Other intermediate outcomes | Investigator and year |
|---|---|---|---|---|
| Elimination of user fees | ||||
| Removal of user fees for pregnant women in 1994. | South Africa | • Increase in prenatal care by 14.9% • Increase in booked facility births by 4.6% |
Schneider et al. [59] 1999 | |
| Exemption for delivery fees in 2004. | Ghana | • 19% increase in births in public institutions • 14%–17% increase in skilled birth attendance |
• Cost US $22 per delivery • Reduction in incidence of catastrophic out-of-pocket payments from 55% to 46% for poorest quintile • No significant effect on maternal mortality |
Witter et al. [58] 2009 |
| Community loan funds | ||||
| Establishment of community loan and transport systems. |
Rural Makarfi District, Nigeria | • 18 women transported to hospital for emergency |
• Raised US $20 500 • 18 loans approved in 9 months • Transport system of 23 permanent, 58 part-time drivers • Skilled attendance increased from b20% to 59% at end program |
Essien et al. [41] 1997 |
| Establishment of community loan fund managed by village health committee. |
Sierra Leone | • Increase in utilization in coverage areas compared with non-covered areas |
Fofana et al. [42] 1997 | |
| Educational campaign regarding use of obstetric services. Community mobilization though loan and transport programs. |
Semi-urban Ikot Omin and rural Ikot Ene, Nigeria |
• Trend of increasing referrals to university hospital for obstetric complications • Decline in utilization of obstetric services; however, parallel inflation, increasing transport costs, and user fees in study areas during period |
• Awareness of obstetric complications increased 5%–63% • 14/39 communities established new loan programs • Loans granted and transport systems established in 9 communities |
Olaniran et al. [64] 1997 |
| Government funding of NGOs to provide basic health services to reach poor, rural, indigenous populations. |
Guatemala | • Substantial increase in coverage an quality of Emergency Obstetric Care • Increase in Hospital Based delivery rates • Increase in met need |
Nieves et al. [43] 2000 | |
| Participatory women’s groups established community funds for maternal health care. |
Nepal | • Increased institutional delivery in women’s group areas 7% vs 2%; (RR 3.55; 1.56–8.05) • Increased birth attended by skilled provider in women’s group areas 7% vs 2%; (RR 3.53; 1.54–8.10) |
• Majority of women’s groups had established funds • Half of funds repaid • Charge 1%–2% interest |
Morrison et al. [44] 2008 |
| Community-level insurance schemes | ||||
| Insurance for prenatal care and pregnancy care. | Gambia | • High uptake of insurance 90% joining | Fox-Rushby et al. [45] 1996 | |
| District-based insurance scheme to cover majority of hospital fees with co-payment. |
Democratic Republic of Congo | • Rate of obstetric admission for insured vs non-insured (7:1) |
Criel et al. [49] 1999 | |
| Community-financing scheme to partially cover costs of health delivery. Insurance providing vehicle and nurse for emergency referrals. |
Rural Samburu district, Kenya | • Referral of 655 patients for emergencies (all cause) in 8 years, average 6 patients per month transported from clinics to higher-level care |
• Average enrollment 324 members per year (25% of households) • Average cost US $16 per year, sliding scale fees |
MacIntyre et al. [46] 1999 |
| Development of community health fund for basic reproductive health and other services at rural health centers. |
Tanzania | • Expansion to 4 districts | Krasovec et al. [50] 2000 | |
| Development of pre-payment schemes in 3 districts. | 3 districts, Rwanda | • Increase of facility births in pilot districts increased 14%–49% in pilot districts • Prenatal visits increased 5%–27% |
Schneider et al. [47] 2001 | |
| Creation of Obstetric Risk Insurance to cover EmOC, hospital care, postnatal care. Poorest enrolled at no charge. |
Nouakchott, Mauritania | • Maternal case fatality 2.8% • Rate increased from 2.6% to 3.5% |
• 95% coverage • Membership premium US $21 vs fee for basic delivery and for non-members $13 and $163 |
Renaudin et al. [48] 2008 |
| • Increase of births in Obstetric Risk Insurance facilities from 29% to 48% |
• Generation US $382 320 in revenue, twice of current user fees | |||
| • Decrease in partograph use (80% to 47%) | ||||
| Community-based health insurance schemes established in Senegal, Mali, and Ghana. |
Mali, Ghana, Senegal | • In Senegal, insurance members with maternal health service coverage had 93% facility delivery compared with 71% of nonmembers. No increase in those belonging to insurance without coverage of maternal services • In Mali, members had 94% facility delivery compared with 65% in nonmembers. |
||
| National maternity referral system: communication systems established between primary and referral level facilities, ambulance transport, and cost sharing scheme |
Mali | • Institutional births increased from 19% to 39% from 2003–2006 |
• Obstetric emergencies treated increased from 0.9% to 1.9% • Obstructed labor management increased from 22% to 38% • Number of cesarean deliveries tripled over 3 years • Maternal mortality reduced by 50% |
Fournier et al. [51] 2009 |
| Conditional cash transfers | ||||
| cRCT of monthly cash transfers for making routine prenatal visits. |
Honduras | • Prenatal care utilization 18%–20% higher in intervention clusters |
Morris et al. [53] 2004 | |
| Retrospective case report of users of conditional cash transfer program vs nonusers. |
Mexico | • Conditional cash transfer participants 12% more likely to use prenatal screening |
Barber et al. [54] 2009 | |
| Janini Suraksha Yojna program to pay for impoverished women for institutional delivery, transport expenses |
India | Increase in number of annual institutional births from 10.9 to 13.6 million over 2 years |
Lahariya [55] 2009 | |
| Vouchers | ||||
| Maternal Health Voucher Scheme piloted in 21 upazillas for impoverished residents. |
Bangladesh | • Increase in prenatal care, at least 1 visit from 30% to 60% in 1 year • Increase in health facility delivery from <10% to 40% and end of first year |
Helal S [56] | |
| Public-private partnership providing free delivery care to impoverished families via private sector. |
India | • Institutional births for the poor increased from 27% to 48% |
• Contracted 852 doctors, subsidized 165 278 births | Unicef [57] |
| Contracting out and pay for performance | ||||
| Ministry of health contracted out health service network in El Alto city to an NGO, providing incentives for meeting process and outcomes indicators. |
• Institutional births by 41% and births at primary care centers increased from 5% to 9% in study district |
Lavadenz F [71] 2001 | ||
| Ministry of health contracted out services to NGOs to delivery health services as alternative to conventional government provision. Contractors have full responsibility of services in district and management control. |
Cambodia | • Greater increase in prenatal care use in contracted districts vs. control (402% vs 160% increase in contract out vs control areas) • Greater increase in facility births (142% vs 0% increase in contract out vs control areas) |
Bushahan [69] 2002 | |
3.2.2.1. Elimination of user fees
The removal of user fees for maternal health services has been piloted in several African countries (Ghana, South Africa, Burundi) [58] and several districts in Nepal. In South Africa, user fees for pregnant women were removed in 1994 and resulted in increases in prenatal care attendance (14.9%) and booked facility births (4.6%) [59]. However, the increase in care for acute services also resulted in reductions in preventative medical care [60], and concerns about the quality of care provided have arisen [59].
In Ghana, exemptions for childbirth fees were instituted in 2004 and resulted in higher proportions of births supervised by skilled birth attendants (14%–17%) and births in public institutions (19%) [58,61]. The proportion of catastrophic out-of-pocket payments was reduced for the poorest quintile, but the proportionate decrease in out-of-pocket payments was even greater for the rich [58]. Furthermore, with increasing utilization, Ghana faces many challenges including that of overworked public midwives and doctors, who increased their working hours by 27% and deterioration in quality of services [58].
In the poorest districts in Nepal, free institutional delivery has been offered along with cash payments to cover transport costs for all pregnant women. However, this policy has been implemented in only a few districts and no formal evaluation has yet been published [36].
3.2.2.2. Community-based health insurance schemes
Community-based health insurance programs have been implemented in several African settings [45–49,51,52]. These have been successful in increasing institutional delivery rates when obstetric care was included in the insurance package [52]. While the financial viability of small-scale programs may be tenuous because of fluctuating membership levels and low recuperation of operating costs with membership fees (as low as 2%) [46], the incorporation into national health financing strategies has been more sustainable [45–49,52]. In the Gambia [62], Rwanda [47], Senegal [52] and Mali [52] community insurance schemes were associated with 12%–45% increases in facility delivery, and in the Democratic Republic of Congo, a 7-fold increase in obstetric hospital admissions was found [49]. In West Africa, over 600 community-based insurance schemes had been established by 2004, including at least 5 national health insurance strategies.
In Nouakchott, Mauritania, the Ministry of Health implemented an Obstetric Risk Insurance Plan that achieved high coverage and financial viability [48]. Membership covered prenatal care, emergency transportation, basic care at birth, and cesarean delivery, and the fee was waived for the poorest. Membership coverage achieved 95% in the urban catchment area. From 2003–2005, the number of births in participating hospitals increased by 31% and the number of cesarean deliveries increased by 60% (2.8% to 3.5% of births). The program generated positive revenue, doubling that of user fees, and covered all recurring costs other than health worker salaries.
3.2.2.3. Community loans
Community loans for emergency transport and obstetric care have been established in several safe motherhood initiatives in Nigeria; however, the long-term sustainability and impact on maternal and newborn outcomes remains unclear. In two small pilot projects in Nigeria [41,63], emergency loan funds were successfully established, providing loans that were repaid with low interest rates charged to families (0%–2%). However, in Cross River State, while a majority of villages had established community loan funds, fewer than half had been accessed during the study, and in many villages there were insufficient funds [64].
In Makwanpur, Nepal, community maternal and child funds helped to enable care seeking for some mothers, but there is some evidence that they did not reach the poorest and most marginalized community members [38]. Most women’s groups established funds with voluntary monthly donations (US $0.15) and charged 1%–2% interest on loans. Three years into the program, the funds had an average of US $31 per group, and across all funds US $6764 had been distributed with approximately half repaid. Loan funds were, however, a disincentive to joining women’s groups for the poorest women, who saw mandatory contribution as an obstacle to participation. In some cases, the poorest women were not allowed to take loans because of a perceived risk of default. While community funds may have contributed to improved maternal and neonatal outcomes, it is impossible to determine their role in the overall effect.
3.2.2.4. Conditional cash transfers
Conditional cash transfers have been effective in increasing utilization of prenatal care services and rates of institutional delivery [53–55]. A cRCT was conducted in 70 cities in Honduras, in which intervention households were given monthly cash vouchers in exchange for attending routine prenatal and well-child clinics. Compared with the control households, those receiving cash transfers in intervention areas utilized prenatal care 18%–20% more often [53]. In a retrospective case report from rural Mexico, women participating in a conditional cash transfer program were 12% more likely than nonparticipants to receive prenatal screening or case management procedures [54]. In India, the National Rural Health Mission established the “Janini Suraksha Yojna” (JSY) program in 2001 to pay poor, marginalized women for institutional delivery. In this national-level scheme, pregnant women in rural areas are given cash incentives at the time of institutional delivery, with additional payments for emergency transport, cesarean delivery, and postdelivery expenses [55]. Nationally, institutional births increased from an estimated 10.9 million in 2005–6 to 13.6 million in 2007–8, although this cannot be attributed directly to the program. No evaluation of impact of the JSY program on health outcomes is available. Cash transfer programs are also being implemented in Bangladesh and Nepal to increase maternal healthcare utilization [36,65,66].
3.2.2.5. Voucher schemes
Many countries have adopted fee waiver programs to increase utilization of services. A variant of this is voucher programs, which not only reduce financial barriers to access but also permit the beneficiary to purchase care from a provider of their choice. As vouchers are targeted at the poor, they improve equity. Voucher schemes are being piloted in India, Bangladesh, Tanzania, Cambodia, Uganda, and Kenya [56,67]. However, there are limited data from long-term evaluations. In Bangladesh, the Maternal Health Voucher Scheme, piloted in 21 subdistricts, targets poor residents without a regular source of income and covers the costs of prenatal care and care at birth, including care for obstetric complications, and transport. In the preliminary first year evaluation, 73% of targeted beneficiaries had utilized services covered by the scheme, the proportion of mothers receiving at least one prenatal visit had increased from 30% to 60%, and their use of public facilities for delivery had increased from less than 10% to 40%. Challenges identified included ensuring the quality of care and access to EmOC at the subdistrict level, and retention of specialists (obstetricians and anesthesiologists).
In Gujarat, India, a public-private partnership, “Chiranjeevi Yojana,” was initiated in 2005 that provides free obstetric care for impoverished families via the private sector [68]. The government compensates participating private obstetricians for providing maternal healthcare services free to women below the poverty line, and provides a small stipend to mothers to cover transport and lost wages for her accompanying partner. By 2008, the program had expanded from 5 to all 25 districts of Gujarat, enlisting 852 private doctors, subsidizing 165 278 births, with an increase in institutional births for the poor from 27% to 48% [57]. Since its inception in 2005, there were 599 neonatal deaths and 32 maternal deaths reported among the beneficiaries, for an estimated NMR of 3.4 per 1000 and an MMR of 19 per 100 000 among the enrolled. However, while the estimated baseline preprogram NMR was 40 per 1000 and the MMR was 400 per 100 000, there are no population-based data against which to evaluate the program’s effectiveness.
3.2.2.6. Contracting out and pay for performance
Changes in how providers are compensated can be a powerful tool to change their behaviors and align their incentives with those of the payor or government. The “Chiranjeevi Yojana” discussed above is an example of a program that pays providers a capitated or per beneficiary amount for a bundle of services. In Cambodia, NGOs were contracted to provide maternal and child health services. In addition to a capitation rate per person, there was a penalty for nonperformance. The outcomes from this were compared with the government delivery system as well as one in which the emphasis was on strengthening management. Assessments [69,70] showed that the contractual model worked better than the other two, resulting in an increase in prenatal care use (402% vs 106% increase in contracted-out vs control areas) and facility births (142% vs 0% increase in contracted-out vs control areas). In Bolivia, achievement of process and outcome indicators was used as an incentive to pay providers for delivering maternal and child health services, which led to increased institutional births by 41% and births in primary care centers increased from 5% to 9% [71].
3.2.3. Costs of financial strategies to increase demand for obstetric care
There are limited costing data on financial strategies for maternal and newborn health, and given the lack of data on mortality effects, cost-effectiveness cannot be reliably estimated. In Markafi District, Nigeria, the establishment of a loan fund cost US $3409 and a transport fund cost US $2272, with 60% covered by the community and 40% by the Prevention of Maternal Mortality project. In Mauritania, the starting costs of the Obstetric Risk Insurance Plan was US $60 000 to serve a population of 200 000, and within the first year the income generated was sufficient to cover annual operating costs, excluding health worker salaries. By 3 years US $382 320 had been generated.
Preliminary costing analysis of conditional cash transfer programs indicates substantial operating and administrative costs, emphasizing the urgent need for data on cost-effectiveness [54,72]. In Mexico the conditional cash transfer program covered 5 million beneficiaries (20% of households) and was 4% of the total health budget, with an average cost of US $560 per family beneficiary and US $20 transferred to each household, indicating substantial overhead and administrative costs. In Honduras, the program served 411 000 beneficiaries (about 35% of households) comprising 28% of the total national health budget, with an average cost per household of US $60.83, and a mean transfer of US $17 to the household.
The cost of the Chiranjeevi voucher scheme for the entire state of Gujarat, India was US $12.6 million per year, which was approximately 3.6% of the annual health budget. Since its inception in 2005, the program has cost US $18.1 million, and has been roughly estimated to have saved about 6000 newborns and 610 mothers, although this is not based on a rigorous evaluation [68]. However, using this rough estimate, the cost per newborn and mother saved was approximately US $3000 and US $30 000, respectively.
3.2.4. Implications for financial strategies
While the available data suggest that financial strategies may increase obstetric services utilization, evidence on health outcomes for the mother and newborn is lacking. Hence, the quality of evidence is graded very low. Community-based insurance schemes have been piloted in several, primarily African, settings, and while small-scale programs may have limited financial viability, national programs partnering with governments have been successful in increasing rates of facility-based delivery and access to emergency obstetric care. The elimination of user fees has been piloted in Africa and parts of Nepal, and initial evaluations indicate increased coverage rates of skilled birth attendance. However, strategies to increase demand for services need to be accompanied by actions to ensure the supply side can cope with the increased demand, as illustrated in Mauritania, where the rapid increase in hospital births met with insufficient capacity and resulted in deterioration in quality of care [48].
There is limited evidence available currently to support community-based emergency loan funds, conditional cash transfers, and voucher schemes. While community-based loan funds have been successfully initiated in many settings, they are often difficult to sustain, infrequently utilized, and may not reach the poorest families. Conditional cash transfers and voucher schemes can increase utilization of services and, furthermore, preliminary data from the Chiranjeevi program suggest lower neonatal mortality among beneficiaries. However, further studies are needed to evaluate the impact of these programs on maternal and perinatal health outcomes and their cost-effectiveness to determine the sustainability and affordability for scale up of these programs. Provider payment reforms show promise, but once again the evidence is sparse and rigorous impact evaluations are needed. Where both demand and supply-side interventions are used, it is difficult to estimate their relative impacts.
4. Bringing pregnant women closer to the formal health system
4.1. Community referral and transport systems
4.1.1. Background
Delays in transportation are associated with low utilization of skilled obstetric care and increased risk of maternal-neonatal morbidity and mortality [11,39,73,74]. In an assessment of 10 low- and middle-income countries, over 80% of the population did not live within 5 km of a hospital [75]. Lack of transportation was the primary preventable cause of death in 28% of maternal deaths in rural Zimbabwe [39], and 21% of perinatal deaths in Tanzania [11].
Reducing transport time to emergency obstetric care is challenging in rural settings, where roads, public transportation, and communication infrastructure are poor, and the terrain may be formidable. Improving communication between a home birth attendant and trained staff via two-way radios or mobile phone technology may reduce delays in recognizing the need for referral and arranging timely transport to a first level facility [76]; and communication between peripheral and Comprehensive Emergency Obstetric Care (CEmOC) hospitals may reduce delays in receiving cesarean delivery [51]. Innovative transportation approaches are required in remote and resource-limited settings and may involve adaptation of low-cost vehicles, use of all terrain vehicles, optimizing existing transport mechanisms, and arrangement of on-call driver coverage (Panel 2).
Panel 2. Community referral, transport schemes, and communication technologies.
For the 60 million women who deliver at home each year, distance and transport are major barriers to seeking skilled obstetric care. In certain regions of the world, such as Nepal, almost 85% of the population does not live within 2 km of an all-weather road.
Communication Strategies
The use of one-way or two-way radios, telephones, cell phones, flagging mechanisms along common travel routes, computers-internet, satellite phones, and global positioning systems may help families notify drivers of the need for transportation, and improve the communication across all levels of care, from the community birth attendant, to first level and referral facilities.
Vehicles
Innovative strategies have been developed to transport women in labor in low-resource settings and rugged terrain. The capacity to accommodate the recumbent patient is preferred, and methods have included stretcher schemes, tractors, ox carts, bicycle or motor cycle ambulances, motor boats or canoes, trucks, 4-wheel drive vehicles, and formal ambulances [24,83,124,129,130].
Driver coverage
24-7 coverage is needed as obstetric emergencies may occur at any time of day. Solutions have included on-call rotations for village drivers; pre-negotiated agreements with existing bus, truck, or taxi services; use of transport unions; and flagging systems along ordinary trucking and travel routes [50].
A Case Study: Motorcycle ambulances in Malawi [83]
In the rural district of Mangochi, Malawi, motorcycle ambulances were stationed at 3 primary health centers to facilitate transfer of patients with obstetric emergencies to the district hospital. The health centers were on average 70 km from the referral hospital, and connected by dirt roads difficult to handle during the rainy season. The use of a motorcycle ambulance was estimated to reduce the referral time by 2–4.5 hours (35%–76%). The purchase price of the motorcycle ambulance was US $1965, approximately 19 times cheaper than an automobile ambulance, and the annual operating costs were US $508 annually, approximately 24 times cheaper than a car ambulance.
Challenges to implementation, sustainability, and scale up
High costs of all-terrain vehicles.
Frequent breakdown and high maintenance costs of repairs, parts, fuel; require fund for recurring costs.
Challenge to provide in low population density.
Need for improvement in basic road infrastructure.
Require communication from family in need to transport mechanisms.
4.1.2. Evidence for community referral and transport systems
We identified numerous program reports of community referral and transport systems from Safe Motherhood programs from Africa and South Asia (Table 6). A wide range of strategies for communication and transportation were identified and are shown in Panel 2. In this section, we highlight studies reporting intrapartum-related or mortality outcomes, or that underline key program experiences and challenges.
Table 6.
Effect of transport referral systems on care seeking and intermediate outcomes.
| Intervention/study (date order) | Setting | Care seeking/demand | Other intermediate outcomes | Investigator and year |
|---|---|---|---|---|
| Faisalabad Obstetric Flying Squad provided free ambulance services staffed by skilled obstetric personnel for women in rural areas, free maternity services. |
Pakistan | • 394 transports from 1989–1992 • Common indications: labor pains, abortion, eclampsia, postpartum hemorrhage • Referrals comprised 2%–5% of hospital admissions • Challenges to contacting the service |
Andina et al. [122] 1995 |
|
| Establishment of communications system, emergency transport, and 24-hr driver to bring mothers with obstetric emergency to referral hospital. |
Rural Bo District, Sierra Leone |
Transports increased from 0.9 to 2.6 per month |
• Maternal case fatality from obstetric complications reduced from 20% (3/15) to 10% (2/21) |
Samai [77] 1997 |
| Two villages provided bicycle ambulances and community transport plans. |
Nsanje District, Malawi |
Home delivery rates in case villages decreased from 37% to 18% |
• Time of transport was 90 minutes for all transport used, no change in ambulance villages • Cultural beliefs deterred most pregnant women from using bicycle ambulances, used primarily for nonobstetric transport |
Lungu et al. [82] 2001 |
| Community Capacity Building and Empowerment Imitative developed community-level transport systems, ranging from canoes, ox carts or loan of truck. |
Rural Tanzania | Obstetric complications attended at district hospitals increased from 4% to 15% |
• Most of 52 villages had a written action plan for transport with varying methods • At 2-year follow-up only 12 (27%) villages had put the plan into action and the transport system was only used in 10 villages (23%) in previous 3 months |
Schmid et al. [123] 2001 Ahluwalia et al. [124,125] 1999, 2003 |
| TBAs used wireless telecom systems to call for and arrange ambulance transport to hospital. |
Balochistan, Pakistan |
• NMR 48 (intervention area) to 32.4 (control) • PMR 49 (intervention) vs 85 (control) |
Midhet [84] 2006 |
|
| National maternity referral system: communication systems established between primary and referral level facilities, ambulance transport, and cost-sharing scheme. |
Mali | Institutional births increased from 19% to 39% from 2003–2006 |
• Obstetric emergencies treated increased from 0.9% to 1.9% • Obstructed labor management increased from 22% to 38% • Number of cesarean delivereis tripled over 3 years • Maternal mortality reduced by 50% |
|
| Motorcycle ambulances to transfer mother from primary health facility to referral hospital for EmOC. |
Rural Malawi | • Reduction in median delay to referral hospital 2–4.5 hours (35%–76%) • Price of motorcycle 19 times cheaper than car ambulance • Annual operating costs 24 times cheaper than car ambulance |
Hofman et al. [83] 2008 |
|
| Establishment of emergency obstetric transport service, with emergency obstetric supplies, radios. |
Rural Brong Ahafo, Ghana |
• Transfer of 364 mothers and 2 babies in 15 months • 30% of mothers transferred required medical interventions |
MaterCare International [126] |
|
| Referral system developed in rural district including walkie-talkies, ambulance transport via 4-wheel drive vehicles, 24-hour drivers. |
Rural Iganga district, Uganda |
Supervised births increased from 15% to 27% |
• Hospital-based maternal case fatality reduced 50% • Increased coverage to 56 districts, however difficult to sustain maintenance costs |
UNFPA [76] |
4.1.2.1. Improved communication systems
Enhanced communication between community-based workers and medical professionals, as well as between primary and referral health centers, may reduce transport delays and improve referral rates. In the Ugandan program, Rural Extended Services and Care for Ultimate Emergency Relief (RESCUER), Traditional Birth Attendants (TBAs) attending home births were given mobile walkie-talkies to call medical staff in the event of labor complications to triage problems and call for emergency transport to the home; TBA referral rates increased over the project period. In Bo District, Sierra Leone [77], messengers from primary health centers were sent by motorbike to summon referral vehicles but often encountered difficulties with curfews or vehicle malfunction; the establishment of solar-powered radio communications reduced the referral time to the district hospital by 2 hours from the most peripheral centers. In Malawi, repeater-based VHF radio communication systems were established in district health centers to assist in the dispatching of ambulances to health centers [78]. After establishment of the system, the number of monthly obstetric admissions, referral rates, and referrals within one hour of decision all increased, with a reduction in median time of transport from three to two hours. However, for many mothers the transport time was still too long, due to the paucity of available ambulances.
4.1.2.2. Private-public partnerships
Existing transportation mechanisms may be modified to create solutions for transport of mothers. In West Africa, a local truck drivers’ union volunteered to provide emergency transport for pregnant women. Families placed a yellow flag along regular truck routes to notify truck drivers of the need for transportation [79]. In Nigeria, a local transport union of bus drivers negotiated to provide free transport for women with obstetric emergencies on market days [80]. In Pakistan, the largest private ambulance service is run by philanthropic donations and contributions of community members. The Edhi foundation has established an extensive communication network and a fleet of over 400 ambulances, a helicopter, and 2 airplanes that provide emergency transport for the whole country and serve the most remote areas, where government services do not reach [81].
4.1.2.3. Community-based emergency transport systems
Alternative means to transport pregnant women have been piloted in remote regions with varied success. In Malawi, the introduction of bicycle ambulances did not reduce transport time and they were infrequently used because of cultural beliefs that publicizing labor resulted in summoning evil spirits [82]. However, motorcycle ambulances were found to be both effective and culturally acceptable in another district in Malawi and this experience is highlighted in Panel 2 [83].
In the Balochistan Safe Motherhood Initiative, Pakistan, TBAs played a central role in strengthening the referral-transport chain for obstetric emergencies that resulted in significant reductions in neonatal and perinatal mortality. TBA were trained to recognize, stabilize, and refer for obstetric emergency and were given wireless telecom systems to call for and organize ambulance transportation. In the intervention areas the perinatal mortality rate was 49.4 per 1000 compared with 85.2 per 1000 in the comparison areas, and the neonatal mortality was 32.4 per 1000 compared with 48 per 1000 in the comparison area [84].
In the Sierra Leone and Ugandan RESCUER programs, enhanced communication systems coupled with emergency transport via 4-wheel drive ambulances significantly increased obstetric referrals, and reduced maternal case fatality. In Sierra Leone [77], the number of successful referrals increased from 0.9 to 2.6 per month, and the case fatality of mothers with obstetric complications was reduced from 20% to 10%. In the Ugandan RESCUER program, from 1995 to 1998, the proportion of supervised births increased from 15% to 27% and hospital-based maternal case fatality was reduced by 50%. However, by 2005, when the program was scaled up to 56 districts, the high demand and cost of vehicle maintenance were difficult to sustain and there were insufficient funds [76].
The Government of Mali launched a national maternity referral system in 2002 to improve access to and quality of comprehensive obstetric care [51]. The maternity referral program established radio communications between primary health centers and district hospitals, an ambulance system, and community cost-sharing schemes to cover the majority of health costs. An evaluation of the program was conducted in Kayes, a rural region with poor roads where 56% of the population lived more than 5 km from a primary health center. Within 2 years of implementation (2003–2006), the proportion of institutional births increased from 19% to 39%, and the proportion of obstetric emergencies treated increased from 0.9% to 1.9% of births; with a higher absolute number and proportion of cases of obstructed labor managed, from 107 (22.5% of obstetric emergencies) to 351 (38.4%). The number of cesarean deliveries increased from 112 (24% of obstetric emergencies) to 383 (42%). The overall case fatality among facility births was reduced by half (OR 0.48; 95% CI, 0.30–0.76); however, neonatal outcomes were not reported.
4.1.3. Costs of community referral and transport systems
Several programs report running costs of communications and transport systems, which may be substantial and often prohibitive in low-resource settings. The Uganda RESCUER program cost US $236 700 in the first pilot district and the annual maintenance was US $6000 per year [76], after scale up to the entire district, the maintenance costs were unsustainable. In Sierra Leone, the cost of start up in Bo District (population 53 000) was US $74 836, with annual operating and maintenance costs of US $5486. In Niger, an emergency referral system in a rural district included a 4-wheel drive ambulance and a solar-powered radio communication system for health centers (serving 66 500 rural inhabitants). The annual cost for replacement and recurrent costs was US $21 799 ($9120 for communication, $11675 for ambulance with $7625 generated by user fees), costing US $49 per successful transport [64,85].
4.1.4. Implications for community referral and transport systems
Community referral and transport schemes may increase rates of facility delivery, reduce referral time, improve access to emergency obstetric care for women with obstetric complications, and reduce maternal morbidity and case fatality. However, there was only 1 program report perinatal outcomes, and thus the overall GRADE level of evidence for intrapartum-related mortality is low (Table 3). Effective communication systems are key components of transport systems. Challenges include the high cost of vehicles and maintenance, establishing effective communication systems in remote settings, maintaining driver coverage, and sustainability within a resource-constrained health system. Recent data from Mali’s National Maternity Referral System demonstrate that the key components of program success were the integration of the communication and transport system into the existing government health system and parallel efforts to reduce point of care costs. The evaluation of the impact of community and referral transport systems on perinatal outcomes should be prioritized in addition to evaluation of long-term program sustainability and cost-effectiveness. Additionally, new technologies, such as alternative transportation vehicles or mobile phones, are becoming available in low-income settings and need to be evaluated in the context of maternal-newborn health referral systems.
4.2. Prenatal risk screening
4.2.1. Background
A key recommendation of the 1987 Nairobi Safe Motherhood Conference was that women at “high obstetric risk” (defined as age younger than 20 years or older than 35 years, height less than 145 cm, parity 0 or more than 4, and poor obstetric history such as prior cesarean delivery, complication, or perinatal loss), deliver in a health facility [86]. In settings where the majority of births occur unassisted at home, the early identification of mothers at high risk for developing childbirth complications could help to ensure that they receive skilled care during delivery, to book for delivery at hospitals with CEmOC capacity, or to bring them closer to facilities before anticipated delivery via a maternity waiting home. However, several studies that demonstrated the poor predictive value of this risk-based approach led to the rejection of this strategy at the 1997 Sri Lanka Safe Motherhood Conference, to advocate for skilled birth attendance at all births.
In this section, we revisit the strategy of prenatal risk screening, to assess whether there may be a role for focused risk screening using more predictive risk factors of lower prevalence. In a review of risk factors and complications, Lawn et al. [1] showed that intrapartum conditions are more predictive of perinatal mortality (risk range, 2–85) than prenatal conditions such as anemia (risk range, 2–14), which in turn are more predictive than conditions present before pregnancy such as age, height, etc (risk range, 1–5) [1]. The role of the community provider in triaging and identifying complications during labor is discussed by Darmstadt et al. [13]. Here, we focus on the strategy of risk screening by community-based workers that may be detected before the time of labor, including both maternal risk factors and pregnancy complications to bring high-risk mothers and babies closer to skilled birth care.
4.2.2. Evidence for prenatal risk screening
4.2.2.1. Predictive accuracy of prenatal risk screening
Studies have examined the predictive value of prenatal “risk scoring” for intrapartum stillbirths and first-day neonatal deaths. Bartlett et al. [87] found that for 342 births in rural Guatemala, identification of antepartum maternal characteristics (defined as primigravida, or multipara with previous obstetric problem, short birth interval or mortality of more than half of previous infants) predicted 100% of intrapartum stillbirths and first day neonatal deaths. However, 70% of all women were categorized as “at risk,” with a positive predictive value of 9%, which was infeasible to address in a setting with limited obstetric care [87]. Different prenatal risk screening algorithms including maternal age, parity, height and/or obstetric history have been evaluated in Kasongo, Zaire [88], Zimbabwe[89], and Tanzania [90] with relatively low positive predictive values reported ranging from 42%–53%, largely because of low risk and high prevalence of these conditions. An analysis from Matlab, Bangladesh showed that while some prenatal risk factors may have a moderately high associated risk, many were very prevalent resulting in a low positive predictive value (e.g. 33% of the women were primigravida giving a positive predictive value of 33%). Furthermore, many newborns requiring resuscitation may not have any predicable risk factors [91,92].
However, early prenatal identification and management of low prevalence but high-risk pregnancy complications holds more promise and should not be discarded in the rush to leave risk screening behind. In Matlab, twin pregnancy, vaginal bleeding, and diastolic blood pressure greater than 90 mm Hg had a positive predictive value of 56%–67% for labor complications and each condition was present in only 1% of pregnancies [93]. In the MOMA study (Morbidite Maternelle en Afrique de l’Ouest)–a 7-center prospective population-based study in West Africa–noncephalic presentation, eclampsia, and vaginal bleeding after the eighth month of pregnancy were highly predictive and of low prevalence, and accounted for a significant attributable risk percentage for potentially viable late-term stillbirths (which were more likely to be intrapartum-related) [94].
4.2.2.2. Prenatal risk screening: Mortality impact
In a rural district in Shunyi, China [95], village midwives assigned risk scores to pregnant women during prenatal care, and those with a “high risk” score were prebooked at the county hospital for delivery; those with zero risk were required to deliver at home or in primary health facilities. The specifics of the risk scoring system are not described in detail. Physicians at the primary health facilities were taught to recognize early pregnancy complications (such as breech presentation) and manage or refer complicated cases (eclampsia) to the county hospital. Over the 4 years of the program, PMR was reduced 34% from 25.9 to 17.1 (RR 0.65; 95% CI, 0.44–0.98), intrapartum-related perinatal mortality was reduced from 4.1 per 1000 births in 1984 to 3.0 per 1000 births in 1986, and mortality associated with breech presentation from 3.6 per 1000 in 1982 to 1.7 per 1000 in 1986 (confidence intervals not provided). Furthermore, several maternity waiting homes have used risk stratification to determine eligibility for admission and these results are reported in the next section.
4.2.3. Implications for prenatal risk screening
In several early studies, risk screening algorithms had low positive predictive value, often including very prevalent conditions, thus resulting in frequent referrals of uncomplicated pregnancies. Few rigorous evaluations were undertaken and the overall quality of evidence for risk screening is very low (Table 3). In settings with limited resources, efficient allocation of available personnel requires screening tools that have a positive predictive value for complications and are easy to use [87,93]. Screening may be warranted for a few identifiable conditions that are of lower prevalence and associated with substantially elevated risk for perinatal and maternal death (OR >3). Candidate maternal risk factors include primiparous mothers under the age of 16 years [96], multiple pregnancy and malpresentation [94], and pregnancy complications for inclusion in an algorithmic approach would include vaginal bleeding in late pregnancy, hypertensive disorders, and severe anemia [94]. There is limited evidence, from low-quality observational studies, that triaging mothers with high obstetric risk for hospital delivery or to a maternity waiting home (see below) may be associated with improved perinatal outcomes. Additional research is needed to develop and validate improved focused risk screening algorithms or checklists for women in different settings and to evaluate the tool as an intervention in combination with access to obstetric care.
4.3. Maternity waiting homes
4.3.1. Background
A maternity waiting home is defined as a “residential facility located near a qualified medical facility where women defined as “high risk” can await their delivery and be transferred… shortly before delivery or earlier should a complication arise” [97]. As one part of a system of care, the maternity waiting home may provide a “geographical bridge,” bringing the woman and her baby closer to emergency care. Although maternity waiting homes seem a simple, attractive, low-cost intervention, it must be emphasized that they are only a “link in a larger chain of comprehensive maternity care, all the components of which must be available… of sufficient quality... and linked with the (maternity) home” [97]. The key links in this chain are selection criteria for women and determination of gestation at referral; a system for identification and referral of women; skilled obstetric and newborn care available; and support of the community, especially to encourage women to use the home (adapted from WHO 1996) [97].
4.3.2. Evidence for maternity waiting homes
There are 6 cross-sectional studies that report perinatal outcomes among women admitted to maternity waiting homes, primarily from Africa. However, there are no population-based studies and few controlling for confounding risk factors affecting admission, therefore results are difficult to interpret. We also identified historical data from Cuba, and program reports from Mongolia, Bangladesh, and Peru, but perinatal outcome data were not available. Table 7 displays evidence from studies of waiting homes with impact data, and Panel 3 highlights further programmatic considerations.
Table 7.
Evidence for the impact of maternity waiting homes (MWHs): Mortality effect.
| Intervention/study (date order) | Setting | Percentage skilled attendance |
Baseline mortality rates |
Mortality Effect: Percentage relative reduction in mortality rate (number of deaths in intervention or end line group); RR or OR (95% CI) |
Investigator and year |
||||
|---|---|---|---|---|---|---|---|---|---|
| SBR | ENMR | PMR | NMR | MMR | |||||
| Evaluation of outcome for 151 women admitted to the MWH in 1987 compared with women admitted from home. No adjustment for baseline differences in maternal risk. |
Ethiopia Rural central Nearest hospital about 2 days walk |
NS | SBR 253 (direct admission group) |
90% (4) RR 0.10 (0.04–0.28) |
- | - | - | - | Poovan et al. [102] 1990 |
| Evaluation of 822 singleton and 32 twin births at a rural hospital in 1987. 502 women stayed at the MWH, remainder admitted in labor from home. No adjustment for baseline differences in maternal risk. |
Zimbabwe Rural | NS | PMR 24 (direct admission group) |
56% (9) RR 0.44 (0.19-1.01) |
51% (17) RR 0.49 (0.27–0.90) |
46% (8) RR 0.54 (0.22– 1.35) |
- | Millard et al. [101] 1991 |
|
| Evaluation of pre-existing MWH attached to rural district hospital. 1573 mothers using the MWH compared with 2915 women delivering at the hospital without using the MWH (twins, and preterm births excluded). Risk adjusted for maternal risk factors. |
Zimbabwe Rural eastern district Population 208 000 Nearest hospital up to 140 km away |
NS | PMR 32 (overall) |
- | 33% (30) aRR 0.66 (0.40–1.05) 40%a (20) aRR 0.53 (0.29–0.91) |
- | Chandramohan et al. [98] 1995 |
||
| Evaluation of MWH established in a comprehensive Maternal and Child Programme including improvement of prenatal care, increasing quality and utilization of hospital facilities (63% to 99%) from 1962–1989. 148 MWHs established, with 30% of all births admitted through MWH. Pregnant women admitted from rural areas or urban areas with risk factors. |
Cuba | Cuba: 63% in 1962 |
MMR 118 PMR 15.7 |
75%b | Figa-Talamanca [103] 1996, Riveron et al. [105] 1989 |
||||
| Comparison of 280 women using MWHs with 790 women admitted from home. No adjustment for baseline differences in maternal risk. |
Zimbabwe Rural | NS | PMR 29.8 (direct admission group) |
48% (3) RR 0.52 (0.15–1.76) |
NS (4) RR 1.56 (0.46–5.29) |
16% (7) RR 0.84 (0.36–1.94) |
- | - | Tumwine et al. [100] 1996 |
| Comparison of risk status and pregnancy outcomes of all high-risk pregnant women admitted to MWHs vs those directly admitted to hospital during study periodc. |
Rural eastern Zambia, Population about 60 000. Nearest hospital about 80 km |
NS | PMR: 0.53 at MWH |
No significant differenced |
No significant differenced |
Lonkhuijzen et al. [104] 2003 |
|||
| Six satellite maternity homes attached to tertiary care hospital in India. Comparison of pregnancy outcomes in mothers cared for in MWHs vs national average. |
India | PMR 70 national |
PMR 21 in MWH vs 90 national average |
Guruvare [107] 2007 |
|||||
Abbreviations: SBR, Stillbirth Rate; ENMR, Early Neonatal Mortality rate; PMR, Perinatal Mortality Rate; NMR, Neonatal Mortality Rate; IPR-NMR, Intrapartum-related Neonatal Mortality Rate; NS, not significant.
Adjusted RR for mothers with at least 1 prenatal risk factor.
Historical reduction in MMR from 118 to 29 per 100 000 from 1962 to 1989.
Women admitted to MWH were more likely to have prenatal risk factors, experience labor complications, and have assisted delivery (cesarean or vacuum). No significant difference in mean birth weight or proportion of low birth weight.
PMR in waiting group 53 per 1000 vs 54 per 1000 in non-waiting group. Study may not have been adequately powered to detect mortality difference. Mothers in maternity waiting were at higher obstetric risk (nulliparity, history of cesarean delivery, breech or transverse position, or hypertension) than “non-waiters.”
Panel 3. Maternity waiting homes.
Brief history
Since the beginning of the 20th century, waiting homes have existed in Europe, Canada, and the USA to serve women from remote communities. Maternity waiting homes (MWHs) may be instigated from within healthcare facilities or from the community, such as Casa Materna [98], the result of an initiative by the Nicaraguan Women’s Organization [97]. Others result from governmental initiatives such as in Cuba.
Range of services
Maternity waiting homes may provide prenatal care and birth preparedness counseling for the waiting women, informing them about danger signs for themselves and their newborn, and preparing them to breastfeed and provide other aspects of basic newborn care. Other homes include care for “high-risk” women and newborns for several days after delivery, helping to establish breastfeeding and identify early complications [97].
Considerations for program implementation
Selection of women for admission
Medical risk factors may be considerations for admission (nulliparity, multiple pregnancy) or a broader social definition including poverty and distance from a facility. Such criteria for selection, including gestation at referral (eg 2–4 weeks before), must be set locally, depending on transport systems and cultural acceptability, as well as medical risk. The role of TBAs in referring women to maternity waiting homes and their continued involvement within the home is not reported in the literature, but would be a consideration in settings where TBAs conduct significant numbers of births.
Cultural acceptability is crucial to the utilization of maternity waiting homes. One maternity waiting home in Ghana was built next to the hospital mortuary and was virtually unused [131]. MWHs have been piloted in Africa and Latin America, whereas there is little experience in South Asia, where traditions of privacy and confinement during pregnancy and labor may affect use.
Challenges to implementation
Length of waiting time may be associated with substantial opportunity costs as this is often 3–4 weeks. Mothers require caretakers and food for other children and family members. There are case reports of mothers attempting to induce labor with herbal teas to reduce waiting time [97].
Mothers must bring a relative to attend to her during her stay because of staffing shortages.
MHWs often lack kitchens and it is difficult to support a mother’s normal diet.
Lack basic supplies and materials, such as sheets and blankets.
Need for strong government support: In Mongolia and Mozambique, the lack of political and financial support were key contributors to the deterioration and underutilization of maternity waiting homes.
Case example: Cuba
In 1989, 30% of Cuban women who delivered had stayed in a waiting home [97]. While in the home, women rested, were given special food, and community groups helped to take care of other children. Twice-weekly prenatal clinics were carried out and 24-hour care was available for emergencies. Building and maintenance of the homes were community tasks, and agricultural cooperatives donated food. Careful evaluation of the impact of these homes has not been carried out, but the government credits maternity waiting homes as an important factor in reducing MMR from 118 to 29 per 100 000 between 1962 and 1989, as well as in facilitating transition to facility-based delivery. Now, 99% of births occur in hospital and 30% follow admission to a maternity waiting home [103]. In Cuba, successful expansion of the maternity waiting home program may have been aided by effective partnership with communities, as community-based organizations contributed to maintenance, food, and care [97].
Photograph reprinted with permission granted by Bill & Melinda Gates Foundation/Jeffrey Spector.
· Boat picture: photograph reprinted with permission granted by Indu Alhuwhalia.
· Bike picture: photograph reprinted with permission granted by Save the Children/Michael Bisceglie. Mozambique.
· Stretcher picture: photograph reprinted with permission granted by Luwei Pearson.
Three studies from rural hospitals in Zimbabwe report perinatal mortality among infants of mothers admitted to maternity waiting homes. Chandramohan et al. [98] reported on a hospital-based cohort study in rural eastern Zimbabwe. The maternity waiting home provided free self-catering accommodation beside the hospital, and preferentially admitted women starting from 36 weeks of pregnancy with the following risk factors: parity 0 or more than 6; history of perinatal death or of previous operative delivery; medical risk factors; height less than 150 cm; noncephalic presentation; and multiple pregnancy. After adjusting for confounding risk factors, among women with antepartum risk factors, the PMR for women who were admitted from the maternity waiting home was half that of the nonwaiting mothers (21 vs 43 per 1000; RR of non-waiters vs waiters 1.9; 95% CI, 1.1–3.4); however, this was not significant for all mothers admitted. Although the cesarean delivery rate was the same for the women in the maternity waiting home as for those coming from home, the delay to cesarean delivery may be the key factor for reducing intrapartum-related stillbirths and neonatal deaths. A parallel paper from the same hospital assessed the screening criteria used and found a 78% sensitivity, 51% specificity, and 25% positive predictive value for dystocia [99], concluding that these screening criteria (Zimbabwean MOH policy) were of use in this setting. The remaining studies report perinatal outcomes of admissions to maternity waiting home versus direct admissions and are shown in Table 7, but none adjust for baseline characteristics of the mothers [98,100–107].
4.3.3. Cost of maternity waiting homes
Only one study, from Ethiopia, reported cost data [102]. The maternity waiting home was built in the style of a local house at a cost of US $1000 in 1976. The community supplied all the labor and most of the materials. Annual overheads were estimated in 1990 at US $500 per year to cover maintenance, laundry, and a watchman. In Cuba, the Ministry of Health reported that the average cost of maternity waiting homes in 1988 was about US $10 per day for each pregnant woman [103]. The average user admission fee for a maternity waiting home in Nyanje, Zambia was 1000 Kwacha (US $3), including the cost of hospital birth [104].
4.3.4. Implications regarding maternity waiting homes
In certain settings, maternity waiting homes may have been associated with lower neonatal mortality and a similar if not greater effect on stillbirths (Table 7). However, the majority of evidence is based on low-quality observational studies from Africa that do not control for differences in mothers’ underlying baseline risk and thus the quality of evidence is low (Table 3). For example, if maternity waiting homes admit higher-risk women, then the effectiveness may be underestimated, whereas if direct admissions to hospitals are at higher obstetric risk, then the effectiveness may be overestimated. Panel 3 highlights additional programmatic experiences with maternity waiting homes. There is a need to assess the impact and cost-effectiveness of maternity waiting homes, ideally in a randomized trial design and in various settings. Asian data on acceptability as well as effectiveness is a key gap.
5. Considerations
The present paper highlights several promising strategies to improve links between homes, communities, and health facilities by generating community demand for institutional obstetric care, and by extending the reach of health systems to bring pregnant women closer to skilled care.
Community mobilization interventions educate, motivate, and empower mothers and families to practice preventive care and to seek care for complications, and those with high stakeholder participation and ownership have resulted in significant positive effects on health outcomes. There is promising evidence that community mobilization, when successfully implemented, increases institutional births (2-fold for high intensity strategies in our meta-analysis) and is associated with a 36% reduction in early neonatal mortality, which is likely to reflect a reduction also in intrapartum-related neonatal deaths. In addition, behavior change interventions may reduce the risk of maternal infections during pregnancy and, hence, minimize the potential synergistic effect of infections with intrapartum hypoxia [108,109]. While cause-specific mortality data are required to better understand the mechanisms whereby community mobilization results in the reduction of perinatal deaths, the 2-fold increase in facility births is a probable pathway to mortality reduction. Community mobilization should be prioritized as a key strategy to link women in poor, rural communities with skilled obstetric care.
How can community mobilization be implemented and brought to scale? Not all methods of mobilization are equal or applicable in every context. Programs with increasing community participation and ownership have had greater impact particularly with one-on-one peer counseling through home visits [22,24,25]. Modifying behaviors may vary substantially across cultures and settings, and requires local formative research [22]. Program considerations are shown in Table 8. The community action cycle methodology may empower communities and be a mobilization tool that can be readily adapted for different cultures, as participatory groups are led by facilitators from within the community, and it has been successfully implemented in Latin America and South Asia [21,24]. Engaging a wide range of key newborn stakeholders, from fathers to faith healers, was instrumental in invoking behavior change in Shivgarh [22]. Furthermore, mobilization activities can be integrated into national newborn health strategies and NGOs may partner with governments to deliver these interventions, particularly in poor, remote areas. NGOs were instrumental in the national scale up of the Warmi project in Bolivia [30], as well as the national ReproSalud program in Peru [110,111].
Table 8.
Implementation considerations for programs.
| Increasing community demand for obstetric care | |
|---|---|
| Community mobilization | • Formative research to identify key newborn stakeholders, opinion leaders (both traditional, formal, and informal sector), excluded/marginalized groups (usually at most risk), resources, map barriers, co-set goals and determine plan of action and measures of success. • Identify community institutions/community-based organizations to institutionalize/integrate the community mobilization processes and ensure sustainability. • Determining level of responsibilities, supervision, and funding from different stakeholders: community, NGOs, local and national government. • Careful selection of community mobilizers and application of human resource management including training, supportive supervision, evidence- based appraisal, and coordination with other cadre of workers. • Encourage greater level of community ownership, facilitated by community mobilizers. • Appropriate mix of community mobilization methods for optimal impact. • Alignment and integration between communication strategies and targeted home visitation. • Identify inter-sectoral opportunities for synergizing health mobilization activities (agriculture extension worker, self-help groups). |
| Financial strategies to increase demand for obstetric care |
• Source of funds (government, donor agency) and implications for long-term sustainability, cost-effectiveness. • Purpose of funds eg transport costs and emergency obstetric or neonatal care. • Groups targeted to receive conditional cash transfers or vouchers. • Determining level of insurance premium, affordability to poor, or if loan then level of interest charged, terms of repayment and estimated success of repayment. • Determining size of the conditional cash transfer needed to stimulate demand. • Monitoring of fund use and administrative costs of funds, risk for black market selling of vouchers. |
|
| |
| Bringing pregnant women closer to the formal health system | |
| Communication and transport systems |
• Existing road and transportation infrastructure. • Cultural beliefs regarding transport in labor. • Use of information communication technology for rapid communication notification of need of emergency transport (cell phone, text message, walkie-talkies, two way radio). • High expense of vehicle and parts for all-terrain, 4-wheel drive vehicles, difficulty obtaining parts for repair. • How to modify vehicles to transport reclining women in labor, +/− family member. • Drivers: how to cover 24-7 (on call), cost of drivers, willingness to transport women with obstetric emergency. • Recurrent costs of fuel and repair. • Monitoring costs. |
| Risk screening | • Capacity of health system: Are facilities staffed and equipped to handle a substantial increase in referrals, particularly if risk screening algorithms may have poor positive predictive value? • Which lower prevalence prenatal risk factors accurately predict intrapartum complications, and can these be detected before birth (e.g. twins, breech)? • Level of provider with skills to conduct risk screening, likelihood that family will comply. |
| Maternity waiting homes | • Determining criteria for admission – risk factors, distance from health facility. • Community-cultural beliefs regarding place of birth, participants involved, and need for confinement; formative research on acceptability in different settings and cultures. • Strategies to promote community development and involvement in maternity waiting homes. • Costs of staffing and overhead. • Determining appropriate costs charged to “waiters” that is affordable and not barrier to use. |
There is low-quality evidence that community-level financing, financial incentives, and referral transport systems may increase rates of facility delivery, access to CEmOC, and reduce maternal case fatality; however, data on perinatal outcomes are lacking. Arranging for transport and hospital fees are essential components of birth planning packages, and the impact of the individual components is reflected to some degree in the mortality reduction observed in mobilization packages. Furthermore, there are preliminary data from Gujarat that voucher programs may be associated with reductions in neonatal and maternal mortality among beneficiaries. Additional research is needed to determine the impact of these programs on perinatal and intrapartum-related mortality, and access to emergency obstetric care, in addition to operational research on sustainability and cost-effectiveness, before recommending wide-scale implementation. Specific considerations for financing programs are highlighted in Table 8. To bring these programs to scale, ensure sustainability and broader impact, government support is key, particularly for transportation and health finance infrastructure.
Since 1997, the “Risk Approach” to care during pregnancy has been widely criticized and abandoned by the Safe Motherhood Programs [86,112,113]. Several early prenatal risk screening algorithms utilized prevalent, low-risk characteristics, with poor positive predictive value resulting in high rates of referral. However, certain risk factors and pregnancy complications that were not previously used in these checklists, such as multiple pregnancy, malpresentation, hypertensive disease, and late vaginal bleeding are associated with substantially increased risk of intrapartum-related hypoxia in addition to maternal mortality; have a high positive predictive value; are relatively infrequent; and could be identified during routine prenatal care. Risk screening linked with facility births in rural China or with maternity waiting homes has been associated with reductions of intrapartum-related and perinatal mortality [95,98,101]. The quality of the evidence is low, and thus, insufficient to recommend the implementation of risk screening. However, evaluating risk screening algorithms that incorporate risk factors with high attributable risk and lower prevalence deserves further attention.
While maternity waiting homes have been a cornerstone of many, particularly African, safe motherhood programs, the limited observational data are presently insufficient to recommend their widespread use. While it is plausible that this intervention, particularly in regions with low access to facilities, would reduce the burden of intrapartum-related hypoxic events, further evaluation is needed to assess the impact, cost-effectiveness, and cultural acceptability of maternity waiting homes in other regions of the world.
The ultimate success of demand-based strategies requires parallel supply-side efforts to reduce intrapartum-related mortality. Health system strengthening and improving the quality and quantity of obstetric care must accompany or even precede demand-side strategies [114]. Supply-side strategies are discussed further in the second (intrapartum care) and sixth (perinatal audit) papers in this Supplement [14,15]. In Mauritania, implementation of the national high-risk obstetric insurance scheme and maternal transport system resulted in a substantial increase in institutional births, but also in a subsequent deterioration in the quality of obstetric care [48]. Skilled birth attendants, without timely access to CEmOC, may not directly improve maternal-perinatal outcomes [115], and conversely, in certain settings, unskilled birth attendants may safely assist domiciliary births with the proper recognition and referral for CEmOC within the health system [114,116]. In Pakistan, this model of strengthening primary health care through a community-based approach with obstetric service availability at first and second level health facilities has been estimated to be capable of averting 20% of intrapartum-related neonatal deaths at an achievable coverage level [117].
5.1. Data tracking, challenges, and research gaps
The effectiveness of community mobilization in increasing skilled care and reducing perinatal mortality is promising, however the impact on intrapartum-related mortality, while plausible, remains to be established. While cause-specific mortality may soon be available from several trials, verbal autopsy ascertainment of intrapartum-related neonatal deaths in community settings may be nonspecific, particularly with multiple comorbidities, and results vary substantially depending on case definitions and hierarchies used to assign cause of death [118–120]. Improved validatedand validated methods are required to determine the burden of intrapartum-related mortality, including intrapartum stillbirths, in community settings to evaluate the impact of interventions and track the progress of programs.
Furthermore, when measuring the effectiveness of programs to link pregnant mothers and skilled obstetric care, the health outcomes of the mother and infant are inextricably linked and there need to be conscious efforts among researchers and programmers to monitor and report both. For many of the studies of maternal transport and referral, perinatal outcomes were not reported, and may be more responsive to reductions in transport time and statistically easier to detect. For evaluating community mobilization, met obstetric need would be a valuable indicator of care reaching those at high risk for intrapartum hypoxia. Furthermore, process indicators to track program effectiveness are inconsistently reported by investigators (for example time to reach referral hospital) [83]. Finally, perinatal audit has been used in Tanzania to determine the contribution of the 3 delays to perinatal death, and may be an indirect method to track program progress [11].
6. Conclusion
There is increasing evidence that strategies to link mothers to skilled facility-based obstetric care may reduce perinatal mortality, and presumably affect intrapartum-related deaths. Our meta-analysis shows that high intensity, participatory community mobilization programs resulted in a 2-fold increase in institutional births and prevented 1 out of 3 early neonatal deaths. There is limited program experience that financial strategies, community referral and transport systems, and cell phone technologies increase use of skilled obstetric care and may reduce maternal case fatality. These strategies are promising and require further evaluation of their impact on perinatal outcomes, cost-effectiveness, and sustainability. Maternity waiting homes may also have potential, although well-designed evaluations are needed to evaluate their effect on perinatal-maternal outcomes and acceptability in different regions. Risk screening, while previously rejected, deserves re-evaluation to determine the potential validity and impact of refined algorithms. New questions need to be asked of these “old” strategies.
Creative demand-side strategies appear to increase use of skilled childbirth care for the poor, and have the potential to contribute to reducing the 2 million intrapartum-related stillbirths and neonatal deaths each year. Increasing investment in the supply side of obstetric care should be partnered with investment and more rigorous evaluation of demand-side strategies to ensure mothers and newborns can and do link with the care they need, especially at the time of birth.
Acknowledgments
We acknowledge Rachel Haws for her assistance with the literature searches and reference database, and Mary Kinney for assistance with the analysis of DHS and National Health Account Data and referencing. We thank Abdullah Baqui, Emma Williams, and Yoonjoung Choi for preparing the Projahnmo data for the meta-analysis. We also thank Robert Goldenberg, Department of Obstetrics and Gynecology, Drexel University; Rajiv Bahl, Department of Child and Adolescent Health and Development, WHO; Leslie Elder, Save the Children-USA; and Lynn Sibley, Nell Hodgson Woodruff School of Nursing and Rollins School of Public Health, Emory University for serving as expert reviewers of the paper.
Footnotes
7. Conflict of interest All authors declare that they have no conflicts of interest to disclose.
References
- [1].Lawn JE, Lee AC, Kinney M, Sibley L, Carlo WA, Paul VK, et al. Two million intrapartum-related stillbirths and neonatal deaths: Where, why, and what can be done? Int J Gynecol Obstet. 2009;107:S5–S19. doi: 10.1016/j.ijgo.2009.07.016. [DOI] [PubMed] [Google Scholar]
- [2].Lawn J, Shibuya K, Stein C. No cry at birth: global estimates of intrapartum stillbirths and intrapartum-related neonatal deaths. Bull W H O. 2005;83(6):409–17. [PMC free article] [PubMed] [Google Scholar]
- [3].ACOG committee opinion Inappropriate use of the terms fetal distress and birth asphyxia. Number 197, February 1998 (replaces no.137, April 1994). Committee on Obstetric Practice. American College of Obstetricians and Gynecologists. Int J Gynecol Obstet. 1998;61(3):309–10. [PubMed] [Google Scholar]
- [4].MacLennan A. A template for defining a causal relation between acute intrapartum events and cerebral palsy: international consensus statement. Brit Med J. 1999;319(7216) doi: 10.1136/bmj.319.7216.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Use and abuse of the Apgar score. Committee on Fetus and Newborn, American Academy of Pediatrics, and Committee on Obstetric Practice, American College of Obstetricians and Gynecologists. Pediatrics. 1996;98(1) [PubMed] [Google Scholar]
- [6].Barnes-Josiah D, Myntti C, Augustin A. The three delays as a framework for examining maternal mortality in Haiti. Soc Sci Med. 1998;46(8):981–93. doi: 10.1016/s0277-9536(97)10018-1. [DOI] [PubMed] [Google Scholar]
- [7].Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Soc Sci Med. 1994;38(8):1091–110. doi: 10.1016/0277-9536(94)90226-7. [DOI] [PubMed] [Google Scholar]
- [8].Lawn JE, McCarthy BJ, Ross SR. The Healthy newborn: A reference guide for program managers. CDC and CARE; Atlanta, Georgia: 2001. [Google Scholar]
- [9].PATH . Reducing Birth Asphyxia Through the Bidan di Desa Program in Cirebon, Indonesia: Final report submitted by Program for Appropriate Technology in Health (PATH) to Save the Children US. PATH; Jakarta, Indonesia: Mar 15, 2006. [Google Scholar]
- [10].ICDDRB [Accessed July 7, 2009];Posting of trained birthing attendants: a comparison of home- and facility-based obstetric care. ICDDRB website 2005. Available at: http://www.icddrb.org/pub/publication.jsp?classificationID=56&pubID=5902.
- [11].Mbaruku G, van RJ, Kimondo I, Bilango F, Bergström S. Perinatal audit using the 3-delays model in western Tanzania. Int J Gynecol Obstet. 2009;106(1):85–8. doi: 10.1016/j.ijgo.2009.04.008. [DOI] [PubMed] [Google Scholar]
- [12].Kerber KJ, de Graft-Johnson JE, Bhutta ZA, Okong P, Starrs A, Lawn JE. Continuum of care for maternal, newborn, and child health: from slogan to service delivery. Lancet. 2007;370(9595):1358–69. doi: 10.1016/S0140-6736(07)61578-5. [DOI] [PubMed] [Google Scholar]
- [13].Darmstadt GA, Lee AC, Cousens S, Sibley L, Bhutta ZA, Donnay F, et al. 60 million nonfacility births: Who can deliver in community settings to reduce intrapartum-related deaths? Int J Gynecol Obstet. 2009;107:S89–S112. doi: 10.1016/j.ijgo.2009.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Hofmeyr GJ, Haws RA, Bergstrom S, Lee AC, Okong P, Darmstadt GL, et al. Obstetric care in low resource settings: what, who, how, and overcoming challenges to scale up. Int J Gynecol Obstet. 2009;107:S21–S45. doi: 10.1016/j.ijgo.2009.07.017. [DOI] [PubMed] [Google Scholar]
- [15].Pattinson R, Kerber K, Waiswa P, Day L, Mussell F, Asiruddin S, et al. Perinatal mortality audit: Counting, accountability, and overcoming challenges in scaling up. Int J Gynecol Obstet. 2009;107:S113–S122. doi: 10.1016/j.ijgo.2009.07.011. [DOI] [PubMed] [Google Scholar]
- [16].Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Schünemann HJ, Oxman AD, Brozek J, Glasziou P, Jaeschke R, Vist GE, et al. Grading quality of evidence and strength of recommendations for diagnostic tests and strategies. BMJ. 2008;336(7653):1106–10. doi: 10.1136/bmj.39500.677199.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Schünemann HJ, Oxman AD, Brozek J, Glasziou P, Bossuyt P, Chang S, et al. GRADE: assessing the quality of evidence for diagnostic recommendations. ACP J Club. 2008;149(6):2. [PubMed] [Google Scholar]
- [19].Walker N, Walker CL Fischer, Bryce J, Bahl R, Simon CE. writing for the CHERG Review Groups on Intervention Effects. Standards for CHERG reviews of intervention effects on child health. Int J Epidemiol. 2009 doi: 10.1093/ije/dyq036. [in press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Howard-Grabman L. Demystifying Community Mobilization: An effective strategy to improve maternal and newborn health. ACCESS/USAID; Baltimore, Maryland: Feb, 2007. [Google Scholar]
- [21].Rosato M, Laverack G, Grabman LH, Tripathy P, Nair N, Mwansambo C, et al. Community participation: lessons for maternal, newborn, and child health. Lancet. 2008;372(9642):962–71. doi: 10.1016/S0140-6736(08)61406-3. [DOI] [PubMed] [Google Scholar]
- [22].Kumar V, Mohanty S, Kumar A, Misra RP, Santosham M, Awasthi S, et al. Effect of community-based behaviour change management on neonatal mortality in Shivgarh, Uttar Pradesh, India: a cluster-randomised controlled trial. Lancet. 2008;372(9644):1151–62. doi: 10.1016/S0140-6736(08)61483-X. [DOI] [PubMed] [Google Scholar]
- [23].O’Rourke K, Howard-Grabman L, Seoane G. Impact of community organization of women on perinatal outcomes in rural Bolivia. Rev Panam Salud Publica. 1998;3(1):9–14. doi: 10.1590/s1020-49891998000100002. [DOI] [PubMed] [Google Scholar]
- [24].Manandhar DS, Osrin D, Shrestha BP, Mesko N, Morrison J, Tumbahangphe KM, et al. Effect of a participatory intervention with women’s groups on birth outcomes in Nepal: cluster-randomised controlled trial. Lancet. 2004;364(9438):970–9. doi: 10.1016/S0140-6736(04)17021-9. [DOI] [PubMed] [Google Scholar]
- [25].Bhutta ZA, Memon ZA, Soofi S, Salat MS, Cousens S, Martines J. Implementing community-based perinatal care: results from a pilot study in rural Pakistan. Bull W H O. 2008;86(6):452–9. doi: 10.2471/BLT.07.045849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].McPherson RA, Khadka N, Moore JM, Sharma M. Are birth-preparedness programmes effective? Results from a field trial in Siraha district, Nepal. J Health Popul Nutr. 2006;24(4):479–88. [PMC free article] [PubMed] [Google Scholar]
- [27].Fullerton JT, Killian R, Gass PM. Outcomes of a community-and home-based intervention for safe motherhood and newborn care. Health Care Women Int. 2005;26(7):561–76. doi: 10.1080/07399330591004881. [DOI] [PubMed] [Google Scholar]
- [28].Gummi FB, Hassan M, Shehu D, Audu L. Community education to encourage use of emergency obstetric services, Kebbi State, Nigeria. The Sokoto PMM Team. Int J Gynecol Obstet. 1997 Nov;59(Suppl 2):S191–200. doi: 10.1016/s0020-7292(97)00165-3. [DOI] [PubMed] [Google Scholar]
- [29].Baqui AH, El-Arifeen S, Darmstadt GL, Ahmed S, Williams EK, Seraji HR, et al. Effect of community-based newborn-care intervention package implemented through two service-delivery strategies in Sylhet district, Bangladesh: a cluster-randomised controlled trial. Lancet. 2008;371(9628):1936–44. doi: 10.1016/S0140-6736(08)60835-1. [DOI] [PubMed] [Google Scholar]
- [30].Gonzales F, Arteaga E, Howard-Grabman L. Scaling up the Warmi Project:lessons learned mobilizing Bolivian communities around reproductive health. Save the Children Federation, Inc./Bolivia Field Office; Jun, 1998. [Google Scholar]
- [31].Lee AC, Wall S, Cousens S, Carlo W, Niermeyer S, Keenan W, et al. Neonatal resuscitation and simple immediate newborn care for the prevention of neonatal deaths. Int J Epidemiol. 2009 [in press] [Google Scholar]
- [32].Lee AC, Blencowe H, Hofmeyr J, Moran N, Darmstadt GL, Bhutta S, et al. Care during labour and birth for the prevention of neonatal deaths. Background paper and Delphi panel consensus for LiST. Int J Epidemiol. 2009 [in press] [Google Scholar]
- [33].Hounton S, Byass P, Brahima B. Towards Reduction of Maternal and Perinatal Mortality in Rural Burkina Faso: Communities are not empyy vessels. Global Health Action. 2009 May;:2. doi: 10.3402/gha.v2i0.1947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Hounton S, Chapman G, Menten J, De BV, Ensor T, Sombie I, et al. Accessibility and utilisation of delivery care within a Skilled Care Initiative in rural Burkina Faso. Trop Med Int Health. 2008;13(Suppl 1):44–52. doi: 10.1111/j.1365-3156.2008.02086.x. [DOI] [PubMed] [Google Scholar]
- [35].Lawn JE, Cousens S, Zupan J. 4 million neonatal deaths: when? Where? Why? Lancet. 2005;365(9462):891–900. doi: 10.1016/S0140-6736(05)71048-5. [DOI] [PubMed] [Google Scholar]
- [36].Borghi J, Thapa B, Osrin D, Jan S, Morrison J, Tamang S, et al. Economic assessment of a women’s group intervention to improve birth outcomes in rural Nepal. Lancet. 2005;366(9500):1882–4. doi: 10.1016/S0140-6736(05)67758-6. [DOI] [PubMed] [Google Scholar]
- [37].Nahar S, Costello A. The hidden cost of ’free’ maternity care in Dhaka, Bangladesh. Health Policy Plan. 1998 Dec;13(4):417–22. doi: 10.1093/heapol/13.4.417. [DOI] [PubMed] [Google Scholar]
- [38].Morrison J, Tamang S, Mesko N, Osrin D, Shrestha B, Manandhar M, et al. Women’s health groups to improve perinatal care in rural Nepal. BMC Pregnancy Childbirth. 2005;5(1):6. doi: 10.1186/1471-2393-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Fawcus S, Mbizvo M, Lindmark G, Nystrom L. A community-based investigation of avoidable factors for maternal mortality in Zimbabwe. Stud Fam Plann. 1996 Nov;27(6):319–27. [PubMed] [Google Scholar]
- [40].Borghi J, Ensor T, Somanathan A, Lissner C, Mills A. Mobilising financial resources for maternal health. Lancet. 2006;368(9545):1457–65. doi: 10.1016/S0140-6736(06)69383-5. [DOI] [PubMed] [Google Scholar]
- [41].Essien E, Ifenne D, Sabitu K, Musa A, ti-Mu’azu M, Adidu V, et al. Community loan funds and transport services for obstetric emergencies in northern Nigeria. Int J Gynecol Obstet. 1997;59(Suppl 2):S237–44. doi: 10.1016/s0020-7292(97)00171-9. [DOI] [PubMed] [Google Scholar]
- [42].Fofana P, Samai O, Kebbie A, Sengeh P. Promoting the use of obstetric services through community loan funds, Bo, Sierra Leone. The Bo PMM Team. Int J Gynecol Obstet. 1997;59(Suppl 2):S225–30. doi: 10.1016/s0020-7292(97)00169-0. [DOI] [PubMed] [Google Scholar]
- [43].Nieves I, La Forgia GM. Guatemala-Large-sale government contracting of NGOs to extend basic health services to poor populations in Guatemala - a public-private partnership for health care. In: Rosenmoller M, editor. Challenges of Health Reform. IESE. Business School, University of Navarra; Barcelonia: 2000. [Google Scholar]
- [44].Morrison J, Osrin D, Shrestha B, Tumbahangphe KM, Tamang S, Shrestha D, et al. How did formative research inform the development of a women’s group intervention in rural Nepal? J Perinatol. 2008;28(Suppl 2):S14–22. doi: 10.1038/jp.2008.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Fox-Rushby JA, Foord F. Costs, effects and cost-effectiveness analysis of a mobile maternal health care service in West Kiang, The Gambia. Health Policy. 1996 Feb;35(2):123–43. doi: 10.1016/0168-8510(95)00774-1. [DOI] [PubMed] [Google Scholar]
- [46].Macintyre K, Hotchkiss DR. Referral revisited: community financing schemes and emergency transport in rural Africa. Soc Sci Med. 1999;49(1473):1487. doi: 10.1016/s0277-9536(99)00201-4. [DOI] [PubMed] [Google Scholar]
- [47].Schneider P, Diop F, Maceira D, Butera D. Utilization, Cost, and Financing of District Health Services in Rwanda. Partnership for Health Reform Project, Abt Associates Inc; Bethesda, MD: Mar. 2001. Report No.: Technical Report No. 61. [Google Scholar]
- [48].Renaudin P, Prual A, Vangeenderhuysen C, Ould AM, Ould MV, Ould El JD. Ensuring financial access to emergency obstetric care: three years of experience with Obstetric Risk Insurance in Nouakchott, Mauritania. Int J Gynecol Obstet. 2007;99(2):183–90. doi: 10.1016/j.ijgo.2007.07.006. [DOI] [PubMed] [Google Scholar]
- [49].Criel B, Van der SP, Van LW. The Bwamanda hospital insurance scheme: effective for whom? A study of its impact on hospital utilization patterns. Soc Sci Med. 1999;48(7):897–911. doi: 10.1016/s0277-9536(98)00391-8. [DOI] [PubMed] [Google Scholar]
- [50].Krasovec K, Shaw R. Reproductive Health and Health Sector Reform: Linking outcomes to action. World Bank Institute; Washington, DC: 2000. [Google Scholar]
- [51].Fournier P, Dumont A, Tourigny C, Dunkley G, Drame S. Improved access to comprehensive emergency obstetric care and its effect on institutional maternal mortality in rural Mali. Bull W H O. 2009;87(1):30–8. doi: 10.2471/BLT.07.047076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Smith KV, Sulzbach S. Community-based health insurance and access to maternal health services: evidence from three West African countries. Soc Sci Med. 2008;66(12):2460–73. doi: 10.1016/j.socscimed.2008.01.044. [DOI] [PubMed] [Google Scholar]
- [53].Morris SS, Flores R, Olinto P, Medina JM. Monetary incentives in primary health care and effects on use and coverage of preventive health care interventions in rural Honduras: cluster randomised trial. Lancet. 2004;364(9450):2030–7. doi: 10.1016/S0140-6736(04)17515-6. [DOI] [PubMed] [Google Scholar]
- [54].Barber SL, Gertler PJ. Empowering women to obtain high quality care: evidence from an evaluation of Mexico’s conditional cash transfer programme. Health Policy Plan. 2009;24(1):18–25. doi: 10.1093/heapol/czn039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Lahariya C. Cash Incentives for Institutional Delivery: Linking with antenatal and post natal care may ensure ’continuum of care’ in India. Indian J Community Med. 2009;34(1):15–8. doi: 10.4103/0970-0218.45370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Helal MS. Demand Side Financing Maternal Health Voucher Scheme in Bangladesh. Directorate General of Health Services; Bangladesh: [Accessed July 7, 2009]. 2009. Available at: http://www.searo.who.int/LinkFiles/FCH_d3-4voucher-scheme-Ban.pdf. [Google Scholar]
- [57].Chiranjeevi-Gujarat: An innovative partnership with the private sector obstetricians to provide skilled care at birth to the poor in India. Health & Family Welfare Department Government of Gujarat; [Accessed July 7, 2009]. 2009. Available at: http://gujhealth.gov.in/Chiranjeevi%20Yojana/pdf/Chiranjivi_paper_for_ARC_26032008.pdf. [Google Scholar]
- [58].Witter S, Adjei S, Armar-Klemsesu M, Graham W. Providing free maternal health care: Ten lessons from an evaluation of the National Delivery Exemption Policy in Ghana. Global Health Action. 2009 Apr;:2. doi: 10.3402/gha.v2i0.1881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Schneider H, Gilson L. The impact of free maternal health care in South Africa. In: Berer M, Ravindran TK Dundari, editors. Safe Motherhood Initiatives: Critical Issues. Blackwell Science for Reproductive Health Matters; Oxford: 1999. pp. 93–101. [Google Scholar]
- [60].Wilkinson D, Gouws E, Sach M, Karim SS. Effect of removing user fees on attendance for curative and preventive primary health care services in rural South Africa. Bull W H O. 2001;79(7):665–71. [PMC free article] [PubMed] [Google Scholar]
- [61].Grepin K. Free Delivery: The effect of a delivery fee exemption policy on the utilization of maternity services in Ghana Harvard University. 2009.
- [62].Fox-Rushby JA. The Gambia: cost and effectiveness of a mobile maternal health care service, West Kiang. World Health Stat Q. 1995;48(1):23–7. [PubMed] [Google Scholar]
- [63].Chiwuzie J, Okojie O, Okolocha C, Omorogbe S, Oronsaye A, Akpala W, et al. Emergency loan funds to improve access to obstetric care in Ekpoma, Nigeria. The Benin PMM Team. Int J Gynecol Obstet. 1997;59(Suppl 2):S231–6. doi: 10.1016/s0020-7292(97)00170-7. [DOI] [PubMed] [Google Scholar]
- [64].Olaniran N, Offiong S, Ottong J, Asuquo E, Duke F. Mobilizing the community to utilize obstetric services, Cross River State, Nigeria. The Calabar PMM Team. Int J Gynecol Obstet. 1997;59(Suppl 2):S181–9. doi: 10.1016/s0020-7292(97)00164-1. [DOI] [PubMed] [Google Scholar]
- [65].Ensor T, Cooper S. Overcoming barriers to health service access: influencing the demand side. Health Policy Plan. 2004;19(2):69–79. doi: 10.1093/heapol/czh009. [DOI] [PubMed] [Google Scholar]
- [66].World Health Organization . Make every mother and child count. WHO; Geneva: 2005. [Google Scholar]
- [67].Anschutz K. Kenya: Voucher scheme for reproductive health services targeting the poor. PPT presentation for the International Health Financing Workshop. ENTWICKLUNGSBANK; 2008 October 28; [Accessed July 7, 2009]. Available at: http://www.gfa-group.de/publications/webdownloads/552845/12_Anschuetz_Kenya_Vouchers_for_reproductive_health.pdf. [Google Scholar]
- [68].UNICEF . ’Chiranjeevi Yojana’ (Plan for a long life) Public-private partnership to reduce maternal deaths in Gujarat; India: [Accessed July 7, 2009]. Available at: http://www.unicef.org/devpro/46000_47108.html. [Google Scholar]
- [69].Bhushan I, Keller S, Schwartz B. Achieving the twin objectives of efficiency and equity: Contracting health services in Cambodia. Asian Development Bank; Manila: 2002. Report No.: 6. [Google Scholar]
- [70].Palmer N, Mueller DH, Gilson L, Mills A, Haines A. Health financing to promote access in low income settings-how much do we know? Lancet. 2004;364(9442):1365–70. doi: 10.1016/S0140-6736(04)17195-X. [DOI] [PubMed] [Google Scholar]
- [71].Lavadenz F, Schwab N, Straatman H. Public, decentralized and community health networks in Bolivia. Rev Panam Salud Publica. 2001;9(3):182–9. doi: 10.1590/s1020-49892001000300008. [DOI] [PubMed] [Google Scholar]
- [72].Lagarde M, Haines A, Palmer N. Conditional cash transfers for improving uptake of health interventions in low- and middle-income countries: a systematic review. JAMA. 2007;298(16):1900–10. doi: 10.1001/jama.298.16.1900. [DOI] [PubMed] [Google Scholar]
- [73].van Eijk AM, Bles HM, Odhiambo F, Ayisi JG, Blokland IE, Rosen DH, et al. Use of antenatal services and delivery care among women in rural western Kenya: a community based survey. Reprod Health. 2006;3:2. doi: 10.1186/1742-4755-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Hamlin C. Preventing Fistula: Transport’s role in empowering communities for health in Ethiopia. The World Bank; Washington, DC: 2004. [Google Scholar]
- [75].World Health Organization . World Health Day: Safe motherhood 7 April 1998. WHO; Geneva: 1998. [Google Scholar]
- [76].UNFPA Uganda. Ndifuna I. The Uganda Rescuers Project: Establishing linkages with ongoing safe motherhood programmes. Available at: http://mauritania.unfpa.org/Fistula2007/Documents/JOUR%202/The%20Uganda%20Rescuer%20Project.ppt%20(UNFPA%20LOG).ppt.
- [77].Samai O, Sengeh P. Facilitating emergency obstetric care through transportation and communication, Bo, Sierra Leone. The Bo PMM Team. Int J Gynecol Obstet. 1997;59(Suppl 2):S157–64. doi: 10.1016/s0020-7292(97)00161-6. [DOI] [PubMed] [Google Scholar]
- [78].Lungu K. Does the upgrading of the radio communications network in health facilities reduce the delay in the referral of obstetric emergencies in Southern Malawi? Malawi Med J. 2007;19(1):1–8. doi: 10.4314/mmj.v19i1.10924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].BBC Worldservice [Accessed July 7, 2009];Millennium Development Goals, Goal 5: Improve maternal health, Case study: West Africa. Available at: http://www.bbc.co.uk/worldservice/specials/1112_mdg/page6.shtml.
- [80].Shehu D, Ikeh AT, Kuna MJ. Mobilizing transport for obstetric emergencies in northwestern Nigeria. The Sokoto PMM Team. Int J Gynecol Obstet. 1997;59(Suppl 2):S173–80. doi: 10.1016/s0020-7292(97)00163-x. [DOI] [PubMed] [Google Scholar]
- [81].Edhi Foundation [Accessed July 7, 2009];Edhi Foundation Services. Available at: http://www.edhifoundation.com/edhi-foundation-services.asp.
- [82].Lungu K, Kamfosa V, Hussein J, Ashwood-Smith H. Are bicycle ambulances and community transport plans effective in strengthening obstetric referral systems in Southern Malawi? Malawi Med J. 2001;12(2):16–8. [Google Scholar]
- [83].Hofman JJ, Dzimadzi C, Lungu K, Ratsma EY, Hussein J. Motorcycle ambulances for referral of obstetric emergencies in rural Malawi: do they reduce delay and what do they cost? Int J Gynecol Obstet. 2008;102(2):191–7. doi: 10.1016/j.ijgo.2008.04.001. [DOI] [PubMed] [Google Scholar]
- [84].Midhet F. [Accessed July 8, 2009];Best Practices in Maternal and Neonatal Health in Pakistan. Available at: http://74.125.93.132/search?q=cache:5bmf9-e4jxQJ:www.mopw.gov.pk/icbp/data/21%2520Nov%252006/8%2520Dr%2520Farid%2520Midhet/Midhet-MNH-BestPractices.ppt+balochistan+and+midhet+best+practices&cd=1&hl=en&ct=clnk&gl=us.
- [85].Bossyns P, Abache R, Abdoulaye MS, Lerberghe WV. Unaffordable or cost-effective?: introducing an emergency referral system in rural Niger. Trop Med Int Health. 2005;10(9):879–87. doi: 10.1111/j.1365-3156.2005.01459.x. [DOI] [PubMed] [Google Scholar]
- [86].Starrs AM. Safe motherhood: 20 years and counting. Lancet. 2006;368:1130–2. doi: 10.1016/S0140-6736(06)69385-9. [DOI] [PubMed] [Google Scholar]
- [87].Bartlett A. Paz de Bocaletti E, Bocaletti MA. Reducing perinatal mortality in developing countries: high risk or improved labor management? Health Policy Plan. 1993;8(4):360–8. [Google Scholar]
- [88].Antenatal screening for fetopelvic dystocias. A cost-effectiveness approach to the choice of simple indicators for use by auxiliary personnel. The Kasongo Project Team. J Trop Med Hyg. 1984;87(4):173–83. [PubMed] [Google Scholar]
- [89].Tsu VD. Antenatal screening: its use in assessing obstetric risk factors in Zimbabwe. J Epidemiol Community Health. 1994;48(3):297–305. doi: 10.1136/jech.48.3.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Walther FJ. At-risk selection and outcome studied at the Kibara Hospital antenatal clinic in Tanzania. Trop Geogr Med. 1980;32(4):336–9. [PubMed] [Google Scholar]
- [91].Palme-Kilander C. Methods of resuscitation in low-Apgar-score newborn infants–a national survey. Acta Paediatr. 1992;81(10):739–44. doi: 10.1111/j.1651-2227.1992.tb12094.x. [DOI] [PubMed] [Google Scholar]
- [92].Mitchell A, Niday P, Boulton J, Chance G, Dulberg C. A prospective clinical audit of neonatal resuscitation practices in Canada. Adv Neonatal Care. 2002;2(6):316–26. doi: 10.1053/adnc.2002.36831. [DOI] [PubMed] [Google Scholar]
- [93].Vanneste AM, Ronsmans C, Chakraborty J, de Francisco A. Prenatal screening in rural Bangladesh: from prediction to care. Health Policy Plan. 2000;15(1):1–10. doi: 10.1093/heapol/15.1.1. [DOI] [PubMed] [Google Scholar]
- [94].Chalumeau M, Bouvier-Colle MH, Breart G, Ouedraogo C, Sondo B, Testa J, et al. Can clinical risk factors for late stillbirth in West Africa be detected during antenatal care or only during labour? Int J Epidemiol. 2002;31(3):661–8. doi: 10.1093/ije/31.3.661. [DOI] [PubMed] [Google Scholar]
- [95].Yan RY. How Chinese clinicians contribute to the improvement of maternity care. Int J Gynecol Obstet. 1989;30(1):23–6. doi: 10.1016/0020-7292(89)90209-9. [DOI] [PubMed] [Google Scholar]
- [96].Kulmala T, Vaahtera M, Rannikko J, Ndekha M, Cullinan T, Salin ML, et al. The relationship between antenatal risk characteristics, place of delivery and adverse delivery outcome in rural Malawi. Acta Obstet Gynecol Scand. 2000;79(11):984–90. [PubMed] [Google Scholar]
- [97].World Health Organization . Maternity waiting homes: a review of experiences. WHO; Geneva: 1996. [Google Scholar]
- [98].Chandramohan D, Cutts F, Millard P. The effect of stay in a maternity waiting home on perinatal mortality in rural Zimbabwe. J Trop Med Hyg. 1995;98(4):261–7. [PubMed] [Google Scholar]
- [99].Chandramohan D, Cutts F, Chandra R. Effects of a maternity waiting home on adverse maternal outcomes and the validity of antenatal risk screening. Int J Gynecol Obstet. 1994;46(3):279–84. doi: 10.1016/0020-7292(94)90406-5. [DOI] [PubMed] [Google Scholar]
- [100].Tumwine JK, Dungare PS. Maternity waiting shelters and pregnancy outcome: experience from a rural area in Zimbabwe. Ann Trop Paediatr. 1996;16(1):55–9. doi: 10.1080/02724936.1996.11747804. [DOI] [PubMed] [Google Scholar]
- [101].Millard P, Bailey J, Hanson J. Antenatal village stay and pregnancy outcome in rural Zimbabwe. Cent Afr J Med. 1991;37(1):1–4. [PubMed] [Google Scholar]
- [102].Poovan P, Kifle F, Kwast BE. A maternity waiting home reduces obstetric catastrophes. World Health Forum. 1990;11(4):440–5. [PubMed] [Google Scholar]
- [103].Figa’-Talamanca I. Maternal mortality and the problem of accessibility to obstetric care: the strategy of maternity waiting homes. Soc Sci Med. 1996;42(10):1381–90. doi: 10.1016/0277-9536(95)00286-3. [DOI] [PubMed] [Google Scholar]
- [104].van Lonkhuijzen L, Stegeman M, Nyirongo R, van Roosmalen J. Use of maternity waiting home in rural Zambia. Afr J Reprod Health. 2003;7(1):32–6. [PubMed] [Google Scholar]
- [105].Riveron Corteguera R, Rois Massabot N, Cario Sabatela R. Infant mortality in Cuba, 1969–1987. Bol Oficina Sanit Panam. 1987;106(1):1–12. [Google Scholar]
- [106].Lawson JB, Stewart DB. Obstetrics and gynaecology in the tropics and developing countries. Edward Arnold; London: 1967. [Google Scholar]
- [107].Guruvare S, Rai L. Taming perinatal mortality by catering the rural population through satellite maternity centers. ISA; 2007. [Google Scholar]
- [108].Willoughby RE, Jr, Nelson KB. Chorioamnionitis and brain injury. Clin Perinatol. 2002;29(4):603–21. doi: 10.1016/s0095-5108(02)00058-1. [DOI] [PubMed] [Google Scholar]
- [109].Bang AT, Reddy HM, Bang RA, Deshmukh MD. Why do neonates die in rural Gadchiroli, India? (Part II): Estimating population attributable risks and contribution of multiple morbidities for identifying a strategy to prevent deaths. J Perinatol. 2005;25(Suppl 1):S35–43. doi: 10.1038/sj.jp.7211270. [DOI] [PubMed] [Google Scholar]
- [110].Howard-Grabman L, Snetro G. How to mobilize communities for health and social change. Health Communication Partnership [HCP], USAID; Baltimore, Maryland: 2003. [Google Scholar]
- [111].Coe A. An Analysis of the ReproSalud Project in Peru. CHANGE working paper. Centre for Health and Gender Equity; Takoma, Park, MD, USA: 2001. [Google Scholar]
- [112].De Brouwere V, Tonglet R, Van Lerberghe W. Strategies for reducing maternal mortality in developing countries: what can we learn from the history of the west? Trop Med Int Health. 1998;3(10):771–82. doi: 10.1046/j.1365-3156.1998.00310.x. [DOI] [PubMed] [Google Scholar]
- [113].De Brouwere V, Van Lerberghe W, editors. Save Motherhood Strategies: A review of the evidence. ITG Press; Antwerp, Belgium: 2001. [Google Scholar]
- [114].Koblinsky MA, editor. Reducing Maternal Mortality: Learning from Bolivia, China, Egypt, Hondoras, Indonesia, Jamaica, and Zimbabwe. World Bank; Washington, DC: 2003. [Google Scholar]
- [115].Ronsmans C, Vanneste AM, Chakroborty J, van Ginnekin J. Decline in maternal mortality in Matlab, Bangladesh: a cautionary tale. Lancet. 1997;350(9094):1810–4. doi: 10.1016/S0140-6736(97)08012-4. [DOI] [PubMed] [Google Scholar]
- [116].Jokhio AH, Winter HR, Cheng KK. An intervention involving traditional birth attendants and perinatal and maternal mortality in Pakistan. N Engl J Med. 2005;352(20):2091–9. doi: 10.1056/NEJMsa042830. [DOI] [PubMed] [Google Scholar]
- [117].Bhutta ZA, Ali S, Cousens S, Ali TM, Haider BA, Rizvi A, et al. Alma-Ata: Rebirth and Revision 6 Interventions to address maternal, newborn, and child survival: what difference can integrated primary health care strategies make? Lancet. 2008;372(9642):972–89. doi: 10.1016/S0140-6736(08)61407-5. [DOI] [PubMed] [Google Scholar]
- [118].Anker M, Black RE, Coldham C, Kalter HD, Quigley MA, Ross D, et al. A standard verbal autopsy method for investigating cause of death in infants and children. WHO; Geneva: 1999. [Google Scholar]
- [119].Freeman JV, Christian P, Khatry SK, Adhikari RK, LeClerq SC. Evaluation of neonatal verbal autopsy using physician review versus algorithm-based cause-of-death assignment in rural Nepal. Paediatr Perinat Epidemiol. 2005;19(4):323–31. doi: 10.1111/j.1365-3016.2005.00652.x. [DOI] [PubMed] [Google Scholar]
- [120].Lee AC, Mullany LC, Tielsch JM, Katz J, Khatry SK, LeClerq SC, et al. Risk factors for neonatal mortality due to birth asphyxia in southern Nepal: a prospective, community-based cohort study. Pediatrics. 2008;121(5):e1381–90. doi: 10.1542/peds.2007-1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [121].Bhutta ZA, Darmstadt GL, Haws RA, Yakoob MY, Lawn JE. Delivering interventions to reduce the global burden of stillbirths: improving service supply and community demand. BMC Pregnancy Childbirth. 2009;9(Suppl 1):S7. doi: 10.1186/1471-2393-9-S1-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [122].Andina MM, Fikree FF. Pakistan: the Faisalabad Obstetric Flying Squad. World Health Stat Q. 1995;48(1):50–4. [PubMed] [Google Scholar]
- [123].Schmid T, Kanenda O, Ahluwalia I, Kouletio M. Transportation for maternal emergencies in Tanzania: Empowering communities through participatory problem solving. Am J Public Health. 2001;91(10):1613–4. doi: 10.2105/ajph.91.10.1589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [124].Ahluwalia I, Kouletio M, Curtis K, Schmid T. Community empowerment: CDC collaboration with the CARE community-based reproductive health project in two districts in Tanzania. J Womens Health Gender-based Med. 1999;8(8):1015–9. doi: 10.1089/jwh.1.1999.8.1015. [DOI] [PubMed] [Google Scholar]
- [125].Ahluwalia IB, Schmid T, Kouletio M, Kanenda O. An evaluation of a community-based approach to safe motherhood in northwestern Tanzania. Int J Gynecol Obstet. 2003;82(2):231–40. doi: 10.1016/s0020-7292(03)00081-x. [DOI] [PubMed] [Google Scholar]
- [126].MaterCare International [Accessed July 7, 2009];Maternal Health Project in Nkoranza. Available at: http://www.matercare.org/Nkoranza.asp.
- [127].World Health Organization . Making pregnancy safer: the critical role of the skilled attendant, A joint statement by WHO, ICM and FIGO. WHO; Geneva, Switzerland: 2004. [Google Scholar]
- [128].Nwakoby B, Akpala C, Nwagbo D, Onah B, Okeke V, Chukudebelu W, et al. Community contact persons promote utilization of obstetric services, Anambra State, Nigeria. The Enugu PMM Team. Int J Gynecol Obstet. 1997;59(Suppl 2):S219–24. doi: 10.1016/s0020-7292(97)00168-9. [DOI] [PubMed] [Google Scholar]
- [129].Alisjahbana A, Williams C, Dharmayanti R, Hermawan D, Kwast BE, Koblinsky M. An integrated village maternity service to improve referral patterns in a rural area in West-Java. Int J Gynecol Obstet. 1995;48(Suppl):S83–94. doi: 10.1016/0020-7292(95)02323-5. [DOI] [PubMed] [Google Scholar]
- [130].Krasovec K. Auxiliary technologies related to transport and communication for obstetric emergencies. Int J Gynecol Obstet. 2004;85(Suppl 1):S14–23. doi: 10.1016/j.ijgo.2004.02.007. [DOI] [PubMed] [Google Scholar]
- [131].Wilson JB, Collison AH, Richardson D, Kwofie G, Senah KA, Tinkorang EK. The maternity waiting home concept: the Nsawam, Ghana experience. The Accra PMM Team. Int J Gynecol Obstet. 1997;59(Suppl 2):S165–72. doi: 10.1016/s0020-7292(97)00162-8. [DOI] [PubMed] [Google Scholar]
- [132].Hossain J, Ross SR. The effectof addressing demand for as well as supply of emergency obstetric care in Dinajpur, Bangladesh. Int J Gynecol Obstet. 2006;92:320–8. doi: 10.1016/j.ijgo.2005.09.029. [DOI] [PubMed] [Google Scholar]