Abstract
Purpose
An estimated 30% of cancer patients are expected to experience clinically significant psychological distress during the treatment phase of their disease. Despite significant attention being directed to the mental health needs of individuals undergoing and completing treatment, there is less known about the mental health needs of survivors and the role of potential protective factors in survivorship, such as coping self-efficacy and social support.
Method
One hundred and twenty-four post-treatment cancer survivors (mean age = 62.23 years, female = 70%, average 9.3 years post-treatment) were asked to complete measures of physical symptoms, coping self-efficacy, social support, and depression as part of a national convenience sample of cancer patients and survivors.
Results
About 20% of participants possessed scores on the CES-D indicative of clinically-relevant depression. Coping self-efficacy was not only a significant predictor of depression (43% VAC); it also partially mediated the relationship between symptoms and depression. Social support accounted for limited variance and was not a significant predictor of depression in a model containing both social support and coping self-efficacy as predictors.
Conclusion
A substantial minority of post-treatment survivors reported depression symptomatology. Coping self-efficacy may be an important component of patients’ adjustment and possible target for intervention. These results highlight the ongoing mental health and support needs of cancer survivors.
Keywords: Depression, Cancer Survivorship, Coping self-efficacy
Cancer is the second leading cause of death in the United States of America [1] and has a profound impact upon individuals, families, health care providers, and society at large. Advancements in medical treatment, along with increased awareness of screening guidelines, have substantially increased the number of people living with cancer [2], with two thirds of those diagnosed predicted to live beyond five years [3]. These statistics have brought the treatment and long-term management of cancer to the forefront of the health care agenda [2, 4].
The diagnosis, treatment and long-term management of cancer can present an individual with a multitude of stressors; these may include not only physical symptoms, but also emotional distress, difficulty maintaining interpersonal relationships, and financial strains. An estimated 30% of individuals diagnosed with cancer experience significant levels of distress at some stage of the disease trajectory [5], with depression and anxiety the most frequently documented disorders in adult cancer patients [6–8]. That is three times the general prevalence rate in the US [9]. In response to these prevalence statistics, the National Institutes of Health [10] and the Institute Of Medicine [11] have emphasized the need for health-care providers to address the psychological needs of cancer patients, both through the effective detection of distress and the provision of appropriate support services. Importantly, psychological co-morbidity associated with cancer has been linked with a range of negative health outcomes, including impaired quality of life, difficulties maintaining personal and professional roles and interpersonal relationships, as well as impaired immunoregulation and disease recovery [12–15]. Further research has established an association between distress and reduced medical compliance [16], prolonged hospitalization [17], lower levels of satisfaction with care [18, 19] and greater dropout rates in clinical trials [20]. Importantly, once detected, treatment of cancer-related distress has proven effective[e.g. 21, 22], as well as cost-effective in reducing the negative economic impact of untreated psychological disorders such as depression [23].
Despite the acknowledged importance of identifying and treating distress associated with cancer, there remains limited clinical attention and a paucity of empirical research pertaining to the psychological well-being of post-treatment cancer survivors compared to those undergoing treatment or transitioning off treatment. Those studies that do exist have consistently identified significant levels of distress in a significant minority of members of this growing population [24–32]. In a recent review of literature examining the quality of life of long-term survivors, Foster and colleagues [33] established pooled rates of 20–30% of individuals reporting ongoing physiological and psychological problems associated with cancer survivorship. Disconcertingly, these rates are similar to those reported by individuals undergoing primary treatment and belie the popular perception that patients are able to return to their pre-morbid functioning and lifestyles post-treatment.
A significant portion of psychosocial cancer research has focused on the adjustment of women with breast cancer, with findings indicating that the majority of women adjust well [25, 27, 34], particularly those with early stage disease [31]. Further research, however, has established higher rates of distress in those who are diagnosed with cancer at a younger age [28], while impaired quality of life has been reported in women suffering a recurrence of their cancer [26, 30].
In a recent longitudinal study of survivors, Lebel and colleagues [35] examined a range of hypothesized protective and risk-related factors in the prediction of stress-related problems six years post-primary treatment. The authors reported that symptoms associated with intrusion (e.g. intrusive thoughts) and avoidance (e.g. avoidance of feelings) in the first three months post-treatment was predictive of ongoing stress-related problems six years later. Hoffman and colleagues [36] examined data collected in the large scale National Health Interview Study (2002–2006) in which over four thousand survivors were compared to over 122,000 participants never diagnosed with cancer. It was reported that after controlling for a range of sociodemographic and clinical factors, survivors were significantly more likely to report higher levels of serious psychological distress. Risk factors identified included being of younger age, unmarried, less education, and greater difficulty with activities of daily living. Importantly, 60% of those survivors who reported significant distress had not seen a mental health professional in the past year, with 18% of these individuals indicating that they could not afford such care.
Other studies have however reported the psychological well-being of post-treatment survivors to be equitable to the general population [e.g. 37]. The authors of a recent study published in the Journal of Clinical Oncology reported that long-term survivors of cancer possessed equivalent risk for major depressive disorder (MDD) to a population based comparison group [38]. Whereas this is encouraging news, it is important to note that an individual can possess significant symptoms of depression or distress or impaired quality of life without meeting the strict criteria for diagnosable MDD. It is possible that survivors may experience a greater level of distress and impaired quality of life than their population-based counterparts but not meet the criteria for a psychiatric disorder. Furthermore, this study suggested that for those who did meet criteria for MDD, survivors may report a greater level of impairment across domains such as work and social life than those without a cancer history; however, these differences did not reach significance, possibly due to small number of depressed survivors. These important findings reveal a complex picture of long-term adjustment and survival that can be influenced by a range of dynamic physiological, psychosocial, and demographic factors.
As the number of individuals living with cancer grows, and this illness becomes more akin to a chronic disease that requires ongoing management, the importance of effective identification and treatment of distress becomes essential. A critical component of research in this empirical domain will be the identification of predictors of distress, both at time of treatment and during long-term survivorship. This information will guide the development of effective screening tools and clinical interventions.
A central aspect of individuals’ ability to cope with the transition from treatment to survivorship can be the coping skills they bring to the situation. Coping self-efficacy, or confidence in coping with cancer, has been associated with a wide range of cancer-related outcomes, including better disease adjustment and management and improved quality of life [39–46]. Bandura [47] posited that compared to those with low self-efficacy, individuals who possess a high degree of self-efficacy are better able to manage potential challenges or stressors. Moreover, Bandura proposed that coping self-efficacy is a mediator that accounts for the relationship between certain physical or mental states and outcomes [43]. Thus, coping self-efficacy may be expected to mediate the relationship between symptoms or some aspect of the impact of illness and outcomes such as psychosocial adjustment.
Indeed there exists evidence that supports the mediating influence of coping self-efficacy in a number of patient populations and situations, including the management of pain and depression in rheumatoid arthritis [48], and the management of pain in a large sample of chronic pain patients [49, 50]. Further, in a study of cancer-related fatigue Hoffman and colleagues established patients’ coping self-efficacy as a mediating factor between the symptom of fatigue and physical functioning, with those patients who possessed higher levels of perceived coping self-efficacy also demonstrating a less pronounced direct relationship between their symptoms of fatigue and impairments in their functioning [51]. An individual’s coping self-efficacy has been further associated with a number of important health outcomes; with a higher degree of coping self-efficacy associated with successful weight control [42], pain management [44] and more successful disease adjustment[52], as well as fewer episodes of psychological distress [40]. Similar associations have been established in the domain of psychosocial oncology with research suggesting that individuals who possess a higher degree of coping self-efficacy are better adjusted [45], and have better quality of life [46, 53]. An individual’s confidence or coping self-efficacy for executing coping behaviors may mediate the relationship between the impact of a disease and the manifestation of symptoms of distress, and thus represent an important target of investigation and intervention [54].
Importantly, the role of such factors as coping self-efficacy and social support may change over the course of cancer treatment and through survivorship. For example, the diagnosis and treatment of cancer can be associated with acute elevated distress, fear and uncertainty, ongoing treatment commitments, physical side-effects, and significant disruption of personal and professional responsibilities. During this intensive period, emotional and instrumental support mechanisms are often mobilized in order assist the patient in managing this challenge. Once primary treatment is complete however, an individual will transition to the survivorship phase, and support structures will likely decrease. As a patient’s time off-treatment extends, they will likely be expected to return to personal and professional roles, as well as manage ongoing symptoms of distress or treatment side-effects with greater independence. Therefore, in survivorship, an individual’s coping self-efficacy may become increasingly important as they are expected to assert greater responsibility in coping with their illness [4], while received social support will become less critical. If indeed this is the case, interventions that focus on coping self-efficacy and empowerment may be particularly effective in assisting survivors to manage distress over time. The dynamic nature of coping in cancer requires that research investigate possible mediators of distress across the disease trajectory, both at the time of treatment and in survivorship.
The current study will examine the role of coping self-efficacy and social support in a national convenience sample of post-treatment cancer survivors. The role of coping self-efficacy in mediating the relationship between the intensity of symptoms and depression will be examined, as well as the role of different domains of coping self-efficacy in predicting symptoms of depression. It is hypothesized that a significant proportion of this group will report clinically significant depression and that coping self-efficacy will mediate the relationship between symptom impact and depression. Received social support will not be a significant predictor of depression in this sample of survivors.
Method
Procedure
Individuals were recruited as part of a larger study, which included placement of ads in newspapers in major cities, contacting national support groups and alumni associations of universities, physician referrals, and involvement with local research consortiums to engage people in research concerning quality of life, coping in cancer, and cancer survivorship. Participants represented most geographical regions of the United States, except the northeast. A random subsample of the original database (N=742) was chosen from those who reported being off-treatment in the initial testing; 307 were invited to participate and 156 responded, constituting an overall return rate of 51%. Of those who responded, 15 indicated that the individual had died and 17 were returned incomplete, thus resulting in a study sample of 124 individuals. Examination of demographic and medical characteristics of sampled respondents and the larger survivor sample did not reveal any notable differences. Participants had to be 18 years old, able to read English, and off active treatment. Individuals who consented to participate received a packet of materials and were asked to complete each questionnaire and return it using the postage paid envelope provided. The questionnaires took approximately forty minutes to complete and participants who completed and returned the questionnaire were compensated $20 for their effort. Participants, as part of their involvement in the larger project, were also asked to complete a medical release to enable access to medical records to collect information regarding the patient’s disease status; however, not all physicians’ offices responded to this request in the larger sample. All information was handled with the utmost care and in accordance with HIPPA regulations. For those for whom this information was available, the date of diagnosis, the course of treatments, and, if applicable, the ending date of treatments was verified.
Measures
Coping Self-Efficacy
The Cancer Behavior Inventory [CBI, 46] is a 33-item measure of self-efficacy expectations about coping with cancer. Participants’ report their level of confidence for the items on a 9-point Likert-type scale (‘not at all confident’ to ‘totally confident’), which are summed for each of six subscales. These include 1) Maintaining activity and independence, 2) Coping with side-effects, 3) Maintaining positive attitude, 4) Understanding medical information, 5) Affective regulation, 6) Managing stress and 7) Seeking support. A total coping efficacy score is calculated by summing the scale scores. Cronbach’s alphas for the seven factors range from .82 to .89 and the alpha for the entire scale is .94 [46]. The CBI is applicable to survivorship as the efficacy items assess expectations about coping behaviors, which do apply and only 6 items actually mention cancer.
Depression
The Center for Epidemiologic Studies-Depressed Mood Scale [CES-D, 55] is a 20-item scale that assesses current level of depressed affect. Patients rate the frequency of each item on a four-point scale that ranges from rarely (‘less than 1 day’) to most of the time (‘5–7 days’). A score of 16 generally represents a moderately severe degree of depressive symptomatology [55, 56]. Internal consistency for this scale has been reported at .89 in a sample of cancer patients [57]. There exists limited research pertaining to the accuracy of the CES-D in identifying clinical diagnoses of depression; however, in a study of female breast cancer patients, the CES-D was found to possess adequate sensitivity (0.70) and specificity (0.80), but its positive predictive value was poor (0.263) [58]. In a non-cancer sample, Schein and Koenig [59] utilized a structured psychiatric interview to identify cases of depression in medically ill elderly. They reported the CES-D to possess a sensitivity of 0.73, specificity of 0.84 and positive predictive value of 0.62. Both studies utilized a cut-off score of 16.
Symptoms
The Symptom Impact Inventory (SII) is a measure of symptoms experienced by cancer patients and survivors [60]. In the initial development of the SII, patients and survivors rated each of 27 symptoms on three scales: frequency, 1(‘never’) to 5 (‘all the time’); intensity, 1(‘mild’), 2(‘moderate’), 3(‘severe’), and disruption 1(‘not at all’) to 5 (‘a lot’). On a sample of mixed diagnosis cancer patients and survivors (N=255, 155 women, M age= 58, range 22–84), the scales of the SII demonstrated normality of distributions with skewness and kurtosis less than 1. The internal consistency (Cronbach’s alpha) of the SII was .91 and the correlation of the scales was high with Disruption and Intensity correlated .94. Thus, if a symptom was very intense, it was also very disruptive. The following statistically significant validity correlations with the SII were obtained: FACT Physical QOL, −.60; Sickness Impact Profile (Physical scales), .47; FACT Functional QOL, −.40; CBI Maintenance of Activity and Independence scale, −.40; FACT Emotional QOL, −.27. The SII was not correlated with the FACT Social QOL scale (−.09 ns). The SII Intensity scale showed no “ceiling” or “floor” effects, no odd distributional characteristics, and was highly correlated with the SII-Disruption Scale. Because of the high correlation among the scales of the SII only the Intensity scale was used in this study.
Social Support
The Inventory of Socially Supportive Behaviors (ISSB) is a 24-item measure to assess actual, received socially supportive behaviors [61]. Participants are asked to rate the frequency by which they have received types of social support over the past 30 days on a 5-point Likert scale ranging from ‘never’ to ‘about every day’. Participants’ responses are then summed to provide a total score. Test-retest reliability has been shown to be adequate, and reported coefficent alphas have ranged from .93 to .94 [61].
Statistical Analysis
Data were assessed to ensure that assumptions of normality and homoscedacity were appropriately met. Missing items represented less than 5% of data and there were no patterns associated with these items. An averaged mean replacement technique was therefore employed to manage missing data. Depressive symptomatology endorsed by the study sample was then assessed, as well as the degree of variance accounted for by coping self-efficacy and social support. Finally, analyses were conducted to examine the role of study predictors (coping self-efficacy, social support) in mediating the relationship between symptom burden and depression.
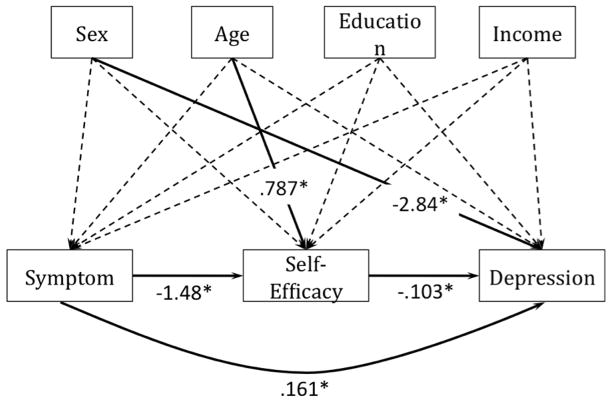
To investigate the mediation effect of self-efficacy, a mediation model in Figure 1 was used. Possible confounding effects of demographic variables -- sex, age, education level, and income -- were controlled by including them in the mediation model. The mediation model was estimated as a path model in Mplus [62]. To test the significance of the mediation effect and the direct effect, the 95% bias-corrected confidence intervals from bootstrap resampling procedure [63] were constructed. In the bootstrap approach, if a confidence interval for any parameter does not include 0, then that indicates the significance of the parameter. In dealing with missing data in the mediation analysis, the full information maximum likelihood (FIML) method was used [64].
Figure 1.
Self-Efficacy modeled as a mediator between symptom intensity and depression. The dotted lines represent insignificant coefficients (p > 0.05).
Results
Participants
Participants (N = 124) were recruited by mail from the Laboratory for Psycho-Oncology Research Participant Database at the University of Notre Dame. The majority of those involved in the current study were female (70%), married (68.3%) and Caucasian (80%), although a concerted effort in recruiting resulted in African Americans constituting 16.7% of the sample. The mean age of this group was 62.23 years (SD = 11.92) with ages ranging from 22 to 86 years old. The majority of participants had been diagnosed with cancer of the breast (51.6%), prostate (15.3%) or colon/rectum (5.6%). Participants were an average of 9.3 years post-treatment, with a median of six and one half years. For those for whom staging data was available, 37% were stage 0 or 1, 46% stage 2 and 17% stage 3 or 4 at the time of diagnosis. All participants were treated in accordance with the Ethical Standards of the American Psychological Association. The authors have no conflicts of interest to report with regard to the conduct of this research project.
Analyses
Preliminary analysis revealed that participants possessed a mean score of 59.3 (SD=21.0, range 25–110) on the social support measure, 8.7 (SD=8.5, range 0–45) on the depression measure, 243.1 (SD=37.8, range 99–297) on the coping self-efficacy measure and 40.0 (SD=13.8, range 1–81) on the measure of symptom impact. Participants endorsed a range of symptomatology; however the most frequently endorsed were fatigue (58%), muscle or join stiffness (40%), muscle or joint pain (37%), numbness and tingling (36%), sexual problems (29%), undesired weight gain (25%), bladder problems (22%) and skin problems (22%). Further analysis revealed significant correlations between coping self-efficacy and depression (r = −.62, p< .01), symptom impact and depression (r = .44, p< .01) and social support and depression (r = −.20, p< .05). The subscales of the CBI were each correlated with depression, with all except one (confidence in understanding information) in the range of .50 to .60 (all p<.01). The relationship between the Emotional Regulation subscale and depression was 0.60 (p<.01).
Results indicated that 19% of participants in the current sample possessed scores indicative of clinically significant depression (i.e., scores greater than 16 on the CES-D). Female participants reported significantly higher rates of depression than male participants (t(120), = 2.56, p< .05). In order to examine the variance accounted for by coping self-efficacy and social support, regression analyses were computed controlling for age, sex, education, and income. Staging data was not available for all participants and given the post-treatment status of the sample was not included in the analyses. Relevant medical variables (e.g. time since treatment) were not associated with the study variables and were therefore also not included as co-variates. The final regression analysis identified participants’ coping self-efficacy to be a highlym significant predictor, accounting for 43% of the variance in depression (β =−.64, p<.001). Social support accounted for a marginal level of variance (VAC = 9%) and was not a significant predictor of depression in a model containing both predictors, whereas coping self-efficacy remained highly significant. Social support was therefore not included in further analyses. Further preliminary analysis of participants’ coping self-efficacy suggested two subscales to be prominent in predicting depressive symptoms; individuals’ confidence in regulating emotion (β =−.34, p<.05) and their confidence in maintaining activity (β =−.25, p=.07).
Mediation analysis
To test the hypothesis that coping self-efficacy mediated the relationship between symptom impact and depression, a mediation model was applied to the data. Based on the model, the estimated mediation effect of coping self-efficacy was 0.152 and the direct effect from symptom intensity to depression was 0.161 (Table 2). These results are summarized and presented in Table 2 and Figure 1.
Table 2.
Path coefficient estimates for the mediation model in Figure 1.
| Estimate | Confidence intervals | Standardized | ||
|---|---|---|---|---|
| Self-Efficacy → Depression | −0.103 | −0.134 | −0.079* | −0.569 |
| Symptom → Depression | 0.161 | 0.058 | 0.264* | 0.236 |
| SEX → Depression | −2.839 | −5.104 | −0.65* | −0.149 |
| AGE → Depression | −0.036 | −0.144 | 0.055 | −0.046 |
| EDUC → Depression | −0.132 | −0.946 | 0.745 | −0.022 |
| INCOME → Depression | −0.012 | −0.591 | 0.723 | −0.003 |
|
| ||||
| Symptom → Self-Efficacy | −1.479 | −2.232 | −0.791* | −0.392 |
| SEX → Self-Efficacy | −14.597 | −31.759 | 1.452 | −0.139 |
| AGE → Self-Efficacy | 0.787 | 0.171 | 1.46* | 0.179 |
| EDUC → Self-Efficacy | 3.245 | −3.283 | 8.831 | 0.096 |
| INCOME → Self-Efficacy | 4.979 | −0.142 | 9.749 | 0.196 |
|
| ||||
| SEX → Symptom | −1.176 | −5.684 | 3.35 | −0.042 |
| AGE → Symptom | 0.103 | −0.163 | 0.341 | 0.088 |
| EDUC → Symptom | 0.441 | −1.092 | 2.526 | 0.049 |
| INCOME → Symptom | −0.521 | −2.021 | 1.009 | −0.077 |
|
| ||||
| Mediation effect | 0.152 | 0.075 | 0.257* | 0.223 |
| Direct effect | 0.161 | 0.058 | 0.264* | 0.236 |
| Total effect | 0.314 | 0.18 | 0.451* | 0.460 |
Note. Educ, education. A → B represents a path from A to B.*Confidence interval does not contain zero.
As indicated in Table 2, both the path coefficient from symptom intensity to coping self-efficacy and the coefficient from coping self-efficacy to depression are significant. The confidence interval [0.075, 0.257] for the mediation effect does not include 0, which indicates that coping self-efficacy does play a mediation role between symptom intensity and depression. Furthermore, the confidence interval [0.058, 0.264] for the direct effect does not include 0, which indicates a significant direct effect; thus, coping self-efficacy partially mediates the relationship between symptom intensity and depression.
Discussion
The current study found that a substantial minority of off-treatment cancer survivors reported clinically-relevant depressive symptomatology (19%) despite this sample being, on average, six to ten years post-treatment. Importantly, coping self-efficacy was found to both account for a significant level of variance in reported depressive symptoms and to partially mediate the relationship between symptom burden and depression. These findings together reinforce the importance of ongoing screening protocols and support services for cancer survivors, and may potentially indicate an important role for interventions that enhance patient coping self-efficacy.
The psychosocial difficulties reported in the current study are consistent with previous research examining the adjustment of long-term cancer survivors, the majority of which has involved breast cancer survivors. Whereas most patients adjust well after cancer treatment (e.g. [26, 35]), a significant minority still experience difficulties [31, 32, 65]. Indeed, in a study by Earle [66], cancer survivors five years from treatment were more likely to possess a mental health diagnosis than those without a history of cancer. In addition, breast cancer survivors, a diagnosis reported by 50% of the current study sample, were more likely to possess a major affective disorder than a matched control group [66].
Despite successful adjustment and stable global quality of life for most patients (e.g. [26, 27, 30, 37, 67]), evidence suggests that certain symptomatology may be prominent in the survivorship phase, including fear of recurrence and illness uncertainty, sexual problems, numbness, neuropathy, and post-traumatic stress symptoms [31, 32, 68, 69]. These findings, along with those of the current study, reinforce the need for further investigation of the needs of survivors [70] and the establishment of effective support services.
Participants’ coping self-efficacy was a highly significant predictor of depression, accounting for 43% of variance in depression scores. In concordance with past findings [45, 46], individuals who endorsed a higher level of coping self-efficacy were less-likely to report clinically significant symptoms of depression than those who endorsed lower coping self-efficacy. Participants’ coping self-efficacy, or confidence in their ability to execute coping behaviors in the face of stressors and challenges, was assessed across a range of domains, including, for example, confidence in affective regulation, managing stress and maintaining activities. Importantly, participants were asked to report their level of confidence in performing coping behaviors regardless of whether they had current need for the coping behavior. Thus, coping self-efficacy was as much about what was currently needed to cope as it was about future expectations of coping. Perhaps it is the confidence to be able to manage yet-unseen stressors that distinguishes those who successfully navigate survivorship from those who are less successful.
Further examination of the relationship between coping self-efficacy and levels of depression revealed preliminary evidence of critical domains of coping self-efficacy. In the current study, participants’ reported confidence in maintaining activity and regulating emotion emerged as the most predictive factors of subsequent depressive symptoms. These findings are similar to those reported by Kohno and colleagues [71] who found that efficacy for regulating emotion and maintaining activities of daily living to be important predictors of depression and quality of life respectively in a small sample of gastrointestinal survivors. Whereas these results require further replication and will be explored in future research, these findings may possess important implications for the development of effective support services and psychological interventions for cancer patients and survivors. Perhaps support or adaptation in order to maintain or return to activities (e.g., employment, work at home, volunteering) would be critical in staving off depression. Also, consistent with prior work on survivorship and the results reported herein, the self-regulation of emotion (e.g., anger, sadness, etc.) is critical for maintaining positive and productive mood states. This is a critical finding in light of research that has indicated that emotion regulation increases with age [72]; thus low confidence in the ability to manage emotions may be more prevalent in younger survivors and is a risk factor for older individuals who report low rates of emotional regulation.
In contrast to coping self-efficacy, received social support did not emerge as a prominent factor in predicting depression, providing preliminary evidence that as patients move further beyond treatment, individual coping mechanisms may become critical as social support structures are withdrawn. Thus, as post-treatment survivorship progresses, there may be an attenuation of social support and a concomitant increase or maintenance of coping self-efficacy. Longitudinal tracking of patients’ symptoms of distress and dynamic predictors, such as coping self-efficacy and social support, will be required in order to fully elucidate these complex processes. Finally, these processes may map on to extant theory and research on resilience as there may be a decrement in coping self-efficacy for some followed by a recovery [73], which then serves to enhance quality of life and attenuate distress.
This study also supports the mediating role of coping self-efficacy, which is consistent with previous findings [46–48, 51]. The partial mediation accounted for by coping efficacy indicates that there may be some alternative mechanisms in accounting for depression rather than just the direct relationship between symptoms and depression. The indirect path does follow a logical progression: more symptoms are associated with less efficacy, which in turn may be a more proximal, albeit partial cause of depression. However, the partial mediation also provides some avenues for reducing depression in addition to symptom management. This interpretation should be taken cautiously as longitudinal and intervention-based studies are needed to untangle the causal direction of these effects; that is depression may be influential in determining the perceived intensity of symptoms and coping self-efficacy expectations. Nonetheless, given the paucity of research of this nature in cancer survivorship, the current study establishes a direction for future research on the mediating role of coping self-efficacy.
The significant role of coping self-efficacy in the current study provides preliminary evidence for the importance of psychological interventions and support services that promote coping self-efficacy and empowerment in assisting individuals to cope with survivorship in the long-term. Self-efficacy expectations are amenable to intervention; thus, assessing weaknesses in coping efficacy and then enhancing those skills could have an impact on the level of depression associated with the presence of ongoing symptoms. Empirically supported treatments for depression, such as cognitive behavioral therapy (CBT), possess elements consistent with the promotion of coping self-efficacy and could be incorporated into behavioral medicine and medical settings. For example, cognitive restructuring and stress management skills, both of which are frequently employed techniques taught within CBT, improve the ability to manage negative cognitions and emotional states and can serve to increase individuals’ confidence in their coping.
The results of the current study provide important insight into the psychological well-being of a growing population of cancer survivors. These findings must however be considered in light of the study’s limitations. The cross-sectional design of the study provides only a ‘snapshot’ of participants’ psychological functioning, and therefore does not allow for a strict causal analysis of constructs; that is, the potentially bidirectional nature of the constructs examined in the current study must be acknowledged. Whereas past research within this domain has generally examined coping self-efficacy as a predictor variable, it is entirely possible for this relationship to work in reverse; whereby an individual may become less confident in their ability to manage stressors as their level of depression increases. Further, the current study sought to elucidate the relationship between coping self-efficacy and depression in post-treatment cancer survivors, and although substantial efforts were made to recruit a diverse sample, we did not seek nor intend to establish prevalence rates of depression in this growing population. Further, the current study sample includes a substantial number of African American survivors, however it must be noted that given the majority of participants are Caucasian or African American, the application of our findings to other groups must be made cautiously. Finally, the finding that social support was not a significant predictor in the current study warrants further examination and replication before firm conclusions can be drawn on the role of psychosocial predictors in off-treatment survivors.
Despite these limitations, the current study provides exciting and fertile ground for future research in the emerging field of cancer survivorship, particularly in regard to psychology and mental health services. It remains to be established whether factors such as coping self-efficacy could be assessed at time of diagnosis and be predictive of long-term disease adjustment and psychological well-being. Moreover, more complex longitudinal resilience models may be used to determine the role of coping efficacy in the trajectory of physical and emotional symptoms over time. Further, there remains considerable work to be done in establishing appropriate distress screening protocols for survivors, along with flexible, brief interventions for both patients and survivors, and in assessing the short and long-term impact of such interventions on psychological and physiological outcomes.
The current research identified a substantial minority of off-treatment cancer survivors who endorsed clinically-relevant symptoms of depression despite this sample being, on average, six to ten years post-treatment. Participants’ coping self-efficacy was a highly significant predictor of depression and a partial mediator of the relationship between the intensity of the symptoms and depression, which establishes coping self-efficacy as a logical target for intervention. Finally, these results highlight the ongoing support needs of cancer survivors long after treatment and the prominent role of mental health providers in treating psychological co-morbidity associated with cancer and cancer survivorship.
Table 1.
Summary of Demographic and Health Information (N (%))
| Gender | Cancer Diagnosis* |
|---|---|
| Male | 36 (30) |
| Female | 86 (70) |
| Age | |
| Range | 22–86 |
| Mean | 62.23 |
| Ethnicity | |
| Caucasian | 96 (80) |
| African American | 20 (17) |
| Religious Preference | |
| Christian Faith | 105 (88) |
| Annual Income | |
| $0–$14,999 | 7 (6) |
| $15,000–$49,999 | 53 (45) |
| Over $70,000 | 36 (31) |
| Marital Status | |
| Married | 107 (68) |
| Divorced/Separated | 16 (13) |
| Education^ | |
| Completed High School | 105 (93) |
| Graduate Degree | 18 (15) |
| Employment | |
| Employed | 61 (50) |
| Retired | 54 (44) |
| Breast | 64 (52) |
| Prostate | 19 (15) |
| Colon/Rectum | 7 (6) |
| Non-Hodgkin’s Lymphoma | 5 (4) |
| Time Since Diagnosis | |
| 3 years or less | 23 (19) |
| 4 – 8 Years | 52 (43) |
| More than 8 Years | 45 (38) |
| Stage** | |
| 0 | 5 (9) |
| 1 | 15 (28) |
| 2 | 25 (46) |
| 3 | 4 (7) |
| 4 | 5 (9) |
| Treatment Type*** | |
| Chemotherapy | 70 (59) |
| Radiation | 82 (69) |
| Surgery | 105 (87) |
Note: This table presents the highest percentage entries. A complete list of all categories is available from the authors.
Patients can be represented in both categories.
Low prevalence diagnoses not listed
Staging data not available for all patients.
Patients may have undergone more than one treatment modality.
Acknowledgments
Support for this research was provided by grants from the National Cancer Institute (CA094914) for T.V. Merluzzi (PI) and the National Institute of Mental Health (F31MH086977) for E.J. Philip.
Contributor Information
Errol J. Philip, Department of Psychiatry and Behavioral Science, Memorial Sloan Kettering Cancer Center
Thomas V. Merluzzi, Department of Psychology, University of Notre Dame
Zhiyong Zhang, Department of Psychology, University of Notre Dame.
Carolyn A. Heitzmann, University of Delaware
References
- 1.ACS. Cancer Facts and Figures. Atlanta: American Cancer Society; 2010. [Google Scholar]
- 2.Jemal A, et al. Cancer Statistics, 2007. CA Cancer J Clin. 2007;57:43–66. doi: 10.3322/canjclin.57.1.43. [DOI] [PubMed] [Google Scholar]
- 3.CDC. Cancer survivorship-United States, 1971–2001. MMWR Morb Mortal Wkly Rep. 2004;53(24):526–529. [PubMed] [Google Scholar]
- 4.Stanton AL, et al. Promoting adjustment after treatment for cancer. Cancer. 2005;104(11 Suppl):2608–13. doi: 10.1002/cncr.21246. [DOI] [PubMed] [Google Scholar]
- 5.Zabora J, et al. The prevalence of psychological distress by cancer site. Psychooncology. 2001;10(1):19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 6.Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr. 2004;(32):57–71. doi: 10.1093/jncimonographs/lgh014. [DOI] [PubMed] [Google Scholar]
- 7.Newport DJ, Nemeroff CB. Assessment and treatment of depression in the cancer patient. J Psychosom Res. 1998;45(3):215–37. doi: 10.1016/s0022-3999(98)00011-7. [DOI] [PubMed] [Google Scholar]
- 8.Stark DP, House A. Anxiety in cancer patients. Br J Cancer. 2000;83(10):1261–7. doi: 10.1054/bjoc.2000.1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kessler RC, et al. Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R) Archives of General Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adler NE, Page AE, editors. Joint report by the National Institutes of Health and Institute of Medicine. National Academies Press; Washington D.C: 2007. Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. [PubMed] [Google Scholar]
- 11.Hewitt M, Greenfield S, Stovall E, editors. Committee on Cancer Survivorship: Improving Care and Quality of Life. Institute of Medicine and National Research Council; 2005. From cancer patient to cancer survivor: Lost in transition. [Google Scholar]
- 12.Hopko DR, et al. The phenomenology and screening of clinical depression in cancer patients. J Psychosoc Oncol. 2008;26(1):31–51. doi: 10.1300/j077v26n01_03. [DOI] [PubMed] [Google Scholar]
- 13.Glaser R. Stress-associated immune dysregulation and its importance for human health: a personal history of psychoneuroimmunology. Brain Behav Immun. 2005;19(1):3–11. doi: 10.1016/j.bbi.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 14.Kiecolt-Glaser JK, et al. Psycho-oncology and cancer: psychoneuroimmunology and cancer. Ann Oncol. 2002;13(Suppl 4):165–9. doi: 10.1093/annonc/mdf655. [DOI] [PubMed] [Google Scholar]
- 15.Maier SF, Watkins LR. Immune-to-central nervous system communication and its role in modulating pain and cognition: Implications for cancer and cancer treatment. Brain Behav Immun. 2003;17(Suppl 1):S125–31. doi: 10.1016/s0889-1591(02)00079-x. [DOI] [PubMed] [Google Scholar]
- 16.Kennard B, et al. Nonadherence in Adolescent Oncology Patients: Preliminary Data on Psychological Risk Factors and Relationships to Outcome. Journal of Clinical Psychology. 2004;11:30–39. [Google Scholar]
- 17.Prieto JM, et al. Psychiatric morbidity and impact on hospital length of stay among hematologic cancer patients receiving stem-cell transplantation. J Clin Oncol. 2002;20(7):1907–17. doi: 10.1200/JCO.2002.07.101. [DOI] [PubMed] [Google Scholar]
- 18.Von Essen L, et al. ‘Satisfaction with care’: associations with health-related quality of life and psychosocial function among Swedish patients with endocrine gastrointestinal tumours. Eur J Cancer Care (Engl) 2002;11(2):91–9. doi: 10.1046/j.1365-2354.2002.00293.x. [DOI] [PubMed] [Google Scholar]
- 19.Bui QU, et al. Relationship of depression to patient satisfaction: findings from the barriers to breast cancer study. Breast Cancer Res Treat. 2005;89(1):23–8. doi: 10.1007/s10549-004-1005-9. [DOI] [PubMed] [Google Scholar]
- 20.Kelly C, Ghazi F, Caldwell K. Psychological distress of cancer and clinical trial participation: a review of the literature. Eur J Cancer Care (Engl) 2002;11(1):6–15. [PubMed] [Google Scholar]
- 21.Newell SA, Sanson-Fisher RW, Savolainen NJ. Systematic review of psychological therapies for cancer patients: overview and recommendations for future research. J Natl Cancer Inst. 2002;94(8):558–84. doi: 10.1093/jnci/94.8.558. [DOI] [PubMed] [Google Scholar]
- 22.Osborn RL, Demoncada AC, Feuerstein M. Psychosocial interventions for depression, anxiety, and quality of life in cancer survivors: meta-analyses. Int J Psychiatry Med. 2006;36(1):13–34. doi: 10.2190/EUFN-RV1K-Y3TR-FK0L. [DOI] [PubMed] [Google Scholar]
- 23.Carlson LE, Bultz BD. Benefits of psychosocial oncology care: improved quality of life and medical cost offset. Health Qual Life Outcomes. 2003;1:8. doi: 10.1186/1477-7525-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ashing-Giwa K, Ganz PA, Petersen L. Quality of life of African-American and white long term breast carcinoma survivors. Cancer. 1999;85(2):418–26. doi: 10.1002/(sici)1097-0142(19990115)85:2<418::aid-cncr20>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 25.Casso D, Buist DS, Taplin S. Quality of life of 5–10 year breast cancer survivors diagnosed between age 40 and 49. Health Qual Life Outcomes. 2004;2:25. doi: 10.1186/1477-7525-2-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dorval M, et al. Long-term quality of life after breast cancer: comparison of 8-year survivors with population controls. J Clin Oncol. 1998;16(2):487–94. doi: 10.1200/JCO.1998.16.2.487. [DOI] [PubMed] [Google Scholar]
- 27.Ganz PA, et al. Quality of life in long-term, disease-free survivors of breast cancer: a follow-up study. J Natl Cancer Inst. 2002;94(1):39–49. doi: 10.1093/jnci/94.1.39. [DOI] [PubMed] [Google Scholar]
- 28.Ganz PA, et al. Breast cancer in younger women: reproductive and late health effects of treatment. J Clin Oncol. 2003;21(22):4184–93. doi: 10.1200/JCO.2003.04.196. [DOI] [PubMed] [Google Scholar]
- 29.Halttunen A, et al. Getting free of breast cancer. An eight-year perspective of the relapse-free patients. Acta Oncol. 1992;31(3):307–10. doi: 10.3109/02841869209108177. [DOI] [PubMed] [Google Scholar]
- 30.Helgeson VS, Tomich PL. Surviving cancer: a comparison of 5-year disease-free breast cancer survivors with healthy women. Psychooncology. 2005;14(4):307–17. doi: 10.1002/pon.848. [DOI] [PubMed] [Google Scholar]
- 31.Kornblith AB, et al. Long-term adjustment of survivors of early-stage breast carcinoma, 20 years after adjuvant chemotherapy. Cancer. 2003;98(4):679–89. doi: 10.1002/cncr.11531. [DOI] [PubMed] [Google Scholar]
- 32.Kornblith AB, Ligibel J. Psychosocial and sexual functioning of survivors of breast cancer. Semin Oncol. 2003;30(6):799–813. doi: 10.1053/j.seminoncol.2003.08.025. [DOI] [PubMed] [Google Scholar]
- 33.Foster C, et al. Psychosocial implications of living 5 years or more following a cancer diagnosis: a systematic review of the research evidence. Eur J Cancer Care (Engl) 2009;18(3):223–47. doi: 10.1111/j.1365-2354.2008.01001.x. [DOI] [PubMed] [Google Scholar]
- 34.Kornblith AB, et al. Long-term psychosocial adjustment of older vs younger survivors of breast and endometrial cancer. Psychooncology. 2007;16(10):895–903. doi: 10.1002/pon.1146. [DOI] [PubMed] [Google Scholar]
- 35.Lebel S, et al. Predicting stress-related problems in long-term breast cancer survivors. J Psychosom Res. 2008;65(6):513–23. doi: 10.1016/j.jpsychores.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 36.Hoffman KE, et al. Psychological distress in long-term survivors of adult-onset cancer: results from a national survey. Arch Intern Med. 2009;169(14):1274–81. doi: 10.1001/archinternmed.2009.179. [DOI] [PubMed] [Google Scholar]
- 37.Boyes AW, et al. Anxiety and depression among long-term survivors of cancer in Australia: results of a population-based survey. Med J Aust. 2009;190(7 Suppl):S94–8. doi: 10.5694/j.1326-5377.2009.tb02479.x. [DOI] [PubMed] [Google Scholar]
- 38.Pirl W, et al. Major Depressive Disorder in Long-Term Cancer Survivors: Analysis of the National Comorbidity Survey Replication. Journal of Clinical Oncology. 2009;27(25):4130–4134. doi: 10.1200/JCO.2008.16.2784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bandura A. Human agency in social cognitive theory. American Psychologist. 1989;44:1175–1184. doi: 10.1037/0003-066x.44.9.1175. [DOI] [PubMed] [Google Scholar]
- 40.Bandura A. Self-efficacy: The exercise of control. New York: Freeman; 1997. [Google Scholar]
- 41.Giese-Davis J, et al. Self-efficacy with emotions predicts high quality of life in primary breast cancer patients. In Self-efficacy and Cancer: Theory, Assessment, and Treatment. Symposium at the Annual Meeting of Society of Behavioral Medicine; 1999; San Diego. [Google Scholar]
- 42.Linde JA, et al. The impact of self-efficacy on behavior change and weight change among overweight participants in a weight loss trial. Health Psychology. 2006;25(3):282–292. doi: 10.1037/0278-6133.25.3.282. [DOI] [PubMed] [Google Scholar]
- 43.Merluzzi TV, Nairn RC. An exploration of self-efficacy and longevity in persons with cancer. In Self-efficacy and Cancer: Theory, Assessment, and Treatment. Symposium conducted at the Annual Meeting of the Society of Behavioral Medicine; 1999; San Diego. [Google Scholar]
- 44.Meredith P, Strong J, Feeney JA. Adult attachment, anxiety, and pain self-efficacy as predictors of pain intensity and disability. Pain. 2006;123(1–2):146–154. doi: 10.1016/j.pain.2006.02.025. [DOI] [PubMed] [Google Scholar]
- 45.Merluzzi TV, Martinez Sanchez MA. Assessment of self-efficacy and coping with cancer: development and validation of the cancer behavior inventory. Health Psychol. 1997;16(2):163–70. doi: 10.1037//0278-6133.16.2.163. [DOI] [PubMed] [Google Scholar]
- 46.Merluzzi TV, et al. Self-efficacy for coping with cancer: revision of the Cancer Behavior Inventory (version 2.0) Psychooncology. 2001;10(3):206–17. doi: 10.1002/pon.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bandura A. Social cognitive theory of self-regulation. Organizational Behavior and Human Decision Processes. 1991;50:248–287. [Google Scholar]
- 48.Rhee SH, et al. Stress management in rheumatoid arthritis: what is the underlying mechanism? Arthritis Care Res. 2000;13(6):435–42. [PubMed] [Google Scholar]
- 49.Arnstein P. The mediation of disability by self efficacy in different samples of chronic pain patients. Disabil Rehabil. 2000;22(17):794–801. doi: 10.1080/09638280050200296. [DOI] [PubMed] [Google Scholar]
- 50.Arnstein P, et al. Self efficacy as a mediator of the relationship between pain intensity, disability and depression in chronic pain patients. Pain. 1999;80(3):483–91. doi: 10.1016/S0304-3959(98)00220-6. [DOI] [PubMed] [Google Scholar]
- 51.Hoffman AJ, et al. Testing a theoretical model of perceived self-efficacy for cancer-related fatigue self-management and optimal physical functional status. Nurs Res. 2009;58(1):32–41. doi: 10.1097/NNR.0b013e3181903d7b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Beckham JC, et al. Self-efficacy and adjustment in cancer patients: A preliminary report. Behavioral Medicine. 1997;23(3):138–142. doi: 10.1080/08964289709596370. [DOI] [PubMed] [Google Scholar]
- 53.Heitzmann CA, et al. Assessing self-efficacy for coping with cancer: development and psychometric analysis of the brief version of the Cancer Behavior Inventory (CBI-B) Psychooncology. 2011;20(3):302–12. doi: 10.1002/pon.1735. [DOI] [PubMed] [Google Scholar]
- 54.Howsepian BA, Merluzzi TV. Religious beliefs, self-efficacy, and adjustment to cancer. Psycho-Oncology. 2009;18:1069–1079. doi: 10.1002/pon.1442. [DOI] [PubMed] [Google Scholar]
- 55.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 56.Myers JK, Weissman MM. Use of a self-report symptom scale to detect depression in a community sample. Am J Psychiatry. 1980;137(9):1081–4. doi: 10.1176/ajp.137.9.1081. [DOI] [PubMed] [Google Scholar]
- 57.Antoni MH, et al. Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychol. 2001;20(1):20–32. doi: 10.1037//0278-6133.20.1.20. [DOI] [PubMed] [Google Scholar]
- 58.Pasacreta J. Depressive phenomenam physical symptom distress and functional status among women with breast cancer. Nursing Research. 1997;46:214–221. doi: 10.1097/00006199-199707000-00006. [DOI] [PubMed] [Google Scholar]
- 59.Schein RL, Koenig HG. The Centre for Epidemiological Studies-Depression (CES-D) scale: assessment of depression in the medically ill elderly. Int J Geriatric Psychiatry. 1997;12:436–446. [PubMed] [Google Scholar]
- 60.Merluzzi TV, Nairn RC, Hegde K. Society of Behavioral Medicine. Salt Lake City: 2003. Development and initial validation of the Symptom Impact Inventory. [Google Scholar]
- 61.Barrera M, Sandler IN, Ramsay TB. Preliminary development of a scale of social support: Studies on college students. American Journal of Community Psychology. 1981;9:435–447. [Google Scholar]
- 62.MacKinnon DP. Introduction to statistical mediation analysis. New York: Taylor & Francis; 2008. [Google Scholar]
- 63.Erwin DO, et al. Contextualizing diversity and culture within cancer control interventions for Latinas: changing interventions, not cultures. Soc Sci Med. 2010;71(4):693–701. doi: 10.1016/j.socscimed.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 64.Little RJA, Rubin DB. Statistical analysis with missing data. 2. New York: Wiley-Interscience; 2002. [Google Scholar]
- 65.Mehnert A, Koch U. Psychological comorbidity and health-related quality of life and its association with awareness, utilization, and need for psychosocial support in a cancer register-based sample of long-term breast cancer survivors. J Psychosom Res. 2008;64(4):383–91. doi: 10.1016/j.jpsychores.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 66.Earle CC. Failing to plan is planning to fail: improving the quality of care with survivorship care plans. J Clin Oncol. 2006;24(32):5112–6. doi: 10.1200/JCO.2006.06.5284. [DOI] [PubMed] [Google Scholar]
- 67.Knobf MT. Clinical update: psychosocial responses in breast cancer survivors. Semin Oncol Nurs. 2011;27(3):e1–e14. doi: 10.1016/j.soncn.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 68.Amir M, Ramati A. Post-traumatic symptoms, emotional distress and quality of life in long-term survivors of breast cancer: a preliminary research. J Anxiety Disord. 2002;16(2):195–206. doi: 10.1016/s0887-6185(02)00095-6. [DOI] [PubMed] [Google Scholar]
- 69.Gill KM, et al. Triggers of uncertainty about recurrence and long-term treatment side effects in older African American and Caucasian breast cancer survivors. Oncol Nurs Forum. 2004;31(3):633–9. doi: 10.1188/04.onf.633-639. [DOI] [PubMed] [Google Scholar]
- 70.Ganz PA. Survivorship: adult cancer survivors. Prim Care. 2009;36(4):721–41. doi: 10.1016/j.pop.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 71.Kohno Y, et al. Relationship of psychological characteristics and self-efficacy in gastrointestinal cancer survivors. Psychooncology. 2010;19(1):71–6. doi: 10.1002/pon.1531. [DOI] [PubMed] [Google Scholar]
- 72.Gross J, et al. Emotion and aging: Experience, expression and control. Psychology and Aging. 1997;12(4):590–599. doi: 10.1037//0882-7974.12.4.590. [DOI] [PubMed] [Google Scholar]
- 73.Helgeson VS, Snyder P, Seltman H. Psychological and physical adjustment to breast cancer over 4 years: Identifying distinct trajectories of change. Health Psychology. 2004;23:3–15. doi: 10.1037/0278-6133.23.1.3. [DOI] [PubMed] [Google Scholar]